Home » Articles posted by Manesh Patel, M.D. (Page 6)
Author Archives: Manesh Patel, M.D.
Duke Heart Pulse – July 31st 2022
Highlights of the week:
Beckerman Joins Division of Cardiovascular & Thoracic Surgery Faculty

We are pleased to welcome Ziv Beckerman, MD, congenital and aortic surgeon, to the Duke faculty in the division of cardiovascular and thoracic surgery of the Department of Surgery. He will serve as a vital member of the pediatric heart surgery team along with Drs. Joe Turek and Nick Andersen. His position was effective July 1. Beckerman joins the team after having served as the surgical director of the Adult Congenital Heart Disease Program at the Texas Center for Pediatric and Congenital Heart Disease at Dell Children’s Medical Center in Austin.
Beckerman, who was born in Israel, says he had always known he wanted to work in the field of medicine, but had been unsure in what capacity. After turning 18, he was required to serve in the Israeli Defense Force and spent three years as a medic assigned to a combat unit. It was during this time tending to a variety of injuries and trauma, that he realized caring for patients was a passion and that he wanted to do it for the rest of his life. Upon completion of his military service to Israel, he started medical school in Hungary at the Medical University of Debrecen. Beckerman went on to complete residency in cardiac surgery at the Ruth and Bruce Rappaport Faculty of Medicine at Technion Israel Institute of Technology in Haifa. He then completed fellowships in Congenital Heart at Sheba Medical Center (Israel); Congenital Heart at Baylor College of Medicine, and in Advanced Aortic Surgery at Emory.
Once he began medical school, Beckerman says he knew from the get-go that he wanted to be a heart surgeon.
“Nothing in the body can function well without a well-functioning heart,” says Beckerman. “It is the most amazing organ and the source of life. Unfortunately, I had a few friends who died because of injuries to their chest and hearts. As I began my training, it was clear to me that this was where I’d place my focus.
“I have always, always felt that if you want to do something and really understand it, you should do it from the very beginning,” he added. “This is why I trained to care for the youngest patients – babies with congenital heart defects and even those still in the womb. If you’re able to take care of problems early enough – perhaps even before they start, then you’re on the way to success.”
Beckerman trained in congenital heart surgery and has dedicated his career to that, but he also decided to take a somewhat unusual path by completing advanced training in aortic surgery. It made great sense to do this, he says, because of the population of adults with congenital heart problems.
In the United States, Beckerman says, there are two types of congenital patients. They are either pediatric congenital patients who were born with identifiable heart defects or they are adult congenital patients. Of the adults, they are either people who were identified and treated as children or they are patients who were never diagnosed in childhood and they are now symptomatic adults. Either way, he says, these patients have complex needs.
Interestingly, there are actually more adults in the U.S. with congenital heart defects than there are kids, adds Beckerman. He says this population is comprised of well over two million people.
“When I thought about this patient subset and the problems they would have – many of them have aortic problems such as issues with dilation or problems with the aortic valve. Most of these adult patients end up as very, very complex surgical candidates,” he says. “So it made a lot of sense to me to train in aortic surgery. I think having this skill set that allows me to care for patients from fetal life all the way to adulthood is special in what it allows me to do, and it is something I feel very passionate about.”
He says that Duke offers an excellent space in which to care for patients. An issue the medical community experiences with congenital patients is “people falling through the cracks” during the transition from childhood to adulthood.
“We frequently lose patients during this transition into adulthood. They’re young adults, they feel strong and healthy, and decide to move away for college or a new job. Unless you have taken very good care to educate this young patient and help them understand their medical history and condition, the importance of keeping follow-ups with their current care team or establishing a relationship with a new care team in their new community, they can put themselves at risk by not getting regular monitoring. If they then resurface when something bad happens or their heart starts to fail, it can be too late.”
As Duke cares for both pediatric and adult patients under the same roof, it allows continuity of care and a unique opportunity to improve education and transition of care for congenital patients.
“One of the biggest advantages that Duke has over many other centers is the structure and the opportunity to maintain the care of the patients throughout their entire life,” says Beckerman. “Duke offers a truly world-class adult heart center and an excellent pediatric center that is one of the best in the country. Coming here offers the perfect opportunity to truly provide patients with the care they need. This is an extraordinary opportunity for me.”
Ziv and his wife, Anett, have two sons: Ben (13) and Ron (12). He says they are enjoying Durham and exploring the area. He said the community members they are meeting are kind and helpful, that their new neighbors are wonderful and welcoming. The family enjoys hiking, fishing, and sports – his sons especially enjoy soccer. He and Anett both enjoy cooking and are somewhat competitive about who is the better chef. They are very happy with their move and are looking forward to meeting more people.
“One of the things I really love about being here is the medical community,” Beckerman adds. “From a physician perspective, this offers me a terrific opportunity to do something meaningful. It is also the kind of community where we can really make an impact. We love being part of the community we live in and really getting to know people. I believe this will allow me to provide a more personalized level of care to my patients and allow me to feel closer to the community overall. We are really glad to be here.”
Please join us in offering Ziv a warm welcome when you see him!
Old-School Health Assessment Beats Genetic Test for Predicting Heart Disease
A genetic risk for heart disease is far less predictive of problems than actual lifestyle risk factors such as high blood pressure, high cholesterol and diabetes — even among younger adults.
high blood pressure, high cholesterol and diabetes — even among younger adults.
In a finding published July 26 in the journal Circulation, researchers led by a team at Duke AI Health found that genetic tests do little to accurately identify cardiovascular risks compared to a simple risk equation that uses basic health measures.
“It’s important to intervene early to prevent cardiovascular disease from progressing,” said senior author Michael Pencina, PhD, vice dean for data science at Duke University School of Medicine and director of Duke AI Health, which develops, evaluates and implements artificial intelligence initiatives at Duke Health and elsewhere.
“A lot of young people can be given a false sense of security if it looks like they have a low risk of inherited disease from their family,” Pencina said. “But in the nature vs. nurture battle, it’s nurture that is the stronger factor for cardiovascular disease: how a person lives throughout adulthood is a much bigger factor in the course of this disease.”
Pencina and colleagues analyzed two large databases — the Framingham Offspring Study and the Atherosclerosis Risk in Communities study — and stratified participants into three groups by age: Younger adults (median 30 years old); early mid-life (median 43 years old); and late mid-life (median 52 years old).
They applied two predictive models. The first, called a polygenic risk score, calculates the number of inherited genetic variants that are likely to put a person at risk of developing cardiovascular disease.
The second was a scoring model that uses traditional long-term risk factors — including high blood pressure, smoking, diabetes and high cholesterol levels — which are largely preventable depending on lifestyle choices.
In their analysis, the researchers found that the polygenic risk score provided limited predictive accuracy for cardiovascular disease risk compared to the traditional health assessment. Even when a genetic score was added in as a factor among the traditional health measurements, it made little difference.
“What we find is consistent in all three age groups, even in the youngest, the risk factor-based model was superior to the genetics-based model for predicting cardiovascular disease,” Pencina said.
“While genetic tests use new technology, they can be high-priced,” Pencina said. “People should instead visit their doctor and have their actual, clinical factors measured, because this will do a much better job of determining their state of health. And for those who have a high risk of developing cardiovascular disease — especially young people — they should eat healthy foods, exercise and begin proper medications as warranted.”
In addition to Pencina, study authors include Sadiya S. Khan, Courtney Page, Daniel M. Wojdyla, Yosef Y. Schwartz, and Philip Greenland. The study received funding from the National Institutes of Health (P30AG059988, RO1HL159250, U01HL160279, 5R01-EB025020-03).
Douglas Awarded Honorary Fellowship by ASPC
 Pamela S. Douglas, MD, the Ursula Geller Distinguished Professor for Research in Cardiovascular Disease, was awarded with an honorary fellowship by the American Society of Preventative Cardiology on Friday, July 29 during the 2022 ASPC Congress on CVD Prevention. The event is being held at the Omni Louisville Hotel from July 29-31 in Louisville, KY.
Pamela S. Douglas, MD, the Ursula Geller Distinguished Professor for Research in Cardiovascular Disease, was awarded with an honorary fellowship by the American Society of Preventative Cardiology on Friday, July 29 during the 2022 ASPC Congress on CVD Prevention. The event is being held at the Omni Louisville Hotel from July 29-31 in Louisville, KY.
“Each year the ASPC identifies someone who has made extraordinary contributions to the field of preventive cardiology through groundbreaking research, exemplary clinical care or excellence in education. Rarely, we find someone who meets all three of these aspects, but in Dr. Pam Douglas, we have,” said Martha Gulati, MD, director of preventive cardiology at Cedars-Sinai Medical Center’s Smidt Heart Institute and president of the ASPC. “Dr. Douglas has led several landmark clinical trials that have changed the workup and management of patients being evaluated for ischemia. She also has helped establish important specialty areas, including heart disease in women, sports cardiology and cardio-oncology. She has also been an outspoken advocate for women in cardiology, in addition to pushing all our cardiology societies to achieve equity and diversity in our ranks of cardiology. She has led the DEI task force for the American College of Cardiology, but this has had a trickle-down effect on all of our cardiology societies. I had the honor of working with her on a landmark paper — published this year in JACC — about what women in cardiology who bear children experience when they are pregnant and how it affects their careers. We outlined actionable solutions to improve the inclusion and advancement of  child-bearing persons in the field of cardiology. This is but one example of her numerous papers that are pushing to make our field welcoming to everyone.
child-bearing persons in the field of cardiology. This is but one example of her numerous papers that are pushing to make our field welcoming to everyone.
“Additionally, she has been a role model and mentor to so many, myself included. She pushes for what is right, she counsels us when we are lost (this she personally did for me in the past year), and she cares about everyone’s success — certainly at Duke Cardiology, but actually beyond Duke’s borders. We are excited to celebrate Dr. Douglas as our 2022 Honorary FASPC.”
Congratulations, Pam!
Krasuski Named Editor-in-Chief Elect of PHA’s Journal
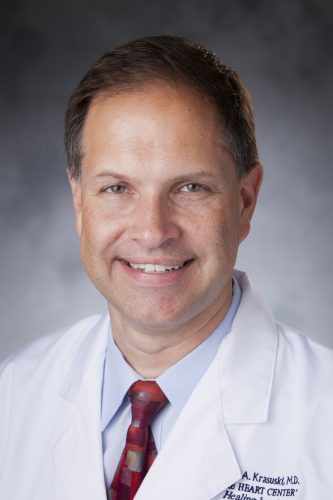 Richard Krasuski, MD, professor of medicine in cardiology, has been named Editor-in-Chief elect of the journal Advances in Pulmonary Hypertension (APH). The position is effective as of July 25. His term as Editor-in-Chief will begin next July and run through June 2025.
Richard Krasuski, MD, professor of medicine in cardiology, has been named Editor-in-Chief elect of the journal Advances in Pulmonary Hypertension (APH). The position is effective as of July 25. His term as Editor-in-Chief will begin next July and run through June 2025.
Krasuski has served on the editorial board of APH for the past four years.
Congratulations, Rich!
Legath to Serve as Nurse Manager DUH 7300, Effective September 1st
Duke Heart is pleased to announce that Jessie Legath, BSN, RN, PCCN, CNIV will become Nurse  Manager Operations for Duke University Hospital’s Cardiology Stepdown Unit 7300 effective September 1st. Jessie will co-manage 7300 with Monica Harper until Monica retires in December. Jessie earned a Bachelor of Science in Nursing from Duke University School of Nursing in 2015. She joined the Duke Heart Team as a new graduate nurse on 3100 in March 2016 and has served as Clinical Lead, now Assistant Nurse Manager, since September 2020.
Manager Operations for Duke University Hospital’s Cardiology Stepdown Unit 7300 effective September 1st. Jessie will co-manage 7300 with Monica Harper until Monica retires in December. Jessie earned a Bachelor of Science in Nursing from Duke University School of Nursing in 2015. She joined the Duke Heart Team as a new graduate nurse on 3100 in March 2016 and has served as Clinical Lead, now Assistant Nurse Manager, since September 2020.
During her time at Duke, Jessie advanced on the clinical ladder by becoming a CNIV and has held a variety of roles on 3100 including Preceptor, Charge Nurse, and Skin Care Champion. As Clinical Lead/Assistant Nurse Manager, she has been heavily involved with safety and quality initiatives including pressure injury prevention and assisting with the creation and implementation of the Heart Center SD Pressure Injury Prevention Bundle. She has been part of many team building and leadership activities throughout the Heart Center, including Heart Center chart navigator for Division of Health Service Regulation (DHSR) visits, organizing and leading monthly CTSD leadership meetings, and currently serves as one of the DUH Heart Core Class presenters.
Please join us in congratulating and welcoming Jessie to her new role.
Temporary Cath Lab Space Opens
Congratulations to the Cardiac Catheterization team on the opening this week of their newest (albeit temporary) lab space in Duke University Hospital. “Cath 4” is located in the area that was vacated by the pediatric team earlier this year. Leadership repurposed the space to support select procedures in order to enhance through-put and operations as we accommodate construction and growth in the DUH adult cardiac catheterization and electrophysiology labs.
The cath team performed their first case in the temporary space on Thursday, July 28. With the help of Duke Heart administrators, nursing and physician leadership, the cath lab super users (Jake Chastain, Adam Edmundson, Ashely Kinney and Miranda Olson), Drs. Larry Crawford and Caitlyn Drescher performed a successful RHC!!
To commemorate the event and to offer homage to Schuyler Jones (who was not in the lab this week), the team crafted this verse:
A cath lab haiku:
The volume was high
The lab space was so low
We opened Cath 4!

Shown here (L-R) are: Larry Crawford, Anna Mall, Miranda Olson, Caitlin Drescher, Jake Chastain, Ashley Kinney and Adam Edmundson


Shown L-R are: Jake Chastain, Larry Crawford and Caitlin Drescher

A big shout-out to Anna Mall and Joe Kelly who were instrumental in getting the room up and running, and many thanks to the entire team for their support. Cheers to our many cases to come!
WiC Event Held
The Duke program for Women in Cardiology met this week at the home of Pam Douglas. All attendees benefited from a great group discussion on mentorship and sponsorship with faculty members Karen Alexander, Anna Lisa Chamis, Pam Douglas, Camille Frazier Mills, Neha Pagidipati, Jennifer Rymer, and Tracy Wang. Thank you to Pam Douglas for hosting and to Joey Harrington, Ali Corley and Paula Rambarat for organizing and participating in this insightful discussion!

Photos of the Week
A belated congratulations to John and Karen Alexander on their daughter Emily‘s entry to medical school. Members of Dr. John Alexander’s clinical team are excited to see her pursuing a career in medicine! When his team members saw recent photos they couldn’t help but notice the stark contrast between Emily’s fresh white coat and John’s less-than-pristine one.
We are told the team has wondered if a ‘GoFundMe‘ campaign is needed to get a replacement. “That coat,” they said, “should probably go already.”

Karen, Emily, and John Alexander, July 2022

John, holding a much younger Emily, and Karen Alexander along with faculty and fellows of the division of cardiology circa 1997. For those that look carefully – you will also see some other notable Duke Cardiology Alums

John Alexander & the coat
Photos submitted by Sasmrita Belbase, cardiology APP.
In all seriousness, congratulations to Emily — we are thrilled for her and look forward to all she will accomplish!
ICYMI: USNWR ‘Best Hospitals’ Ratings Released for 2022-2023
Tom Owens, MD, president of Duke University Hospital commented:
Duke University Hospital is privileged to serve all of our patients and communities, and one of my favorite things is to read the many grateful patient comments and notes we receive every day, thanks to your excellent, compassionate care.
It also is gratifying to receive recognition from outside organizations. We are pleased that Duke University Hospital again has been recognized among the best hospitals in the country in the U.S. News & World Report rankings for 2022-2023. We have improved overall from 24 to 21 in the national ranking, and we remain No. 1 in North Carolina.
We also have been nationally ranked in 11 adult specialties, we saw improvement in most of the specialty groups, and we received the highest rating for 19 of 20 common procedures and conditions.
Congratulations to each of our specialties for these outstanding designations, with national rankings from USNWR as follows:
- Cancer – Ranked 22
- Cardiology & Heart Surgery – Ranked 34
- Ear, Nose & Throat – Ranked 29
- Gastroenterology & GI Surgery – Ranked 29
- Geriatrics – Ranked 30
- Obstetrics & Gynecology – Ranked 33
- Neurology & Neurosurgery – Ranked 23
- Ophthalmology – Ranked 6
- Orthopedics – Ranked 19
- Pulmonology – Ranked 31
- Urology – Ranked 26
In addition, our hospital is recognized this year as high performing in two adult specialties (endocrine and rheumatology), as well as in 19 procedures and conditions:
- Abdominal aortic aneurysm
- Aortic valve stenosis
- Coronary artery bypass grafting
- Colon Cancer Surgery
- Congestive Heart Failure
- Chronic Obstructive Pulmonary Disease (COPD)
- Hip replacement
- Knee replacement
- Lung cancer surgery
- Transcatheter Aortic Valve Replacement (TAVR)
- Heart attack
- Stroke
- Pneumonia
- Diabetes
- Kidney failure
- Hip fracture
- Back surgery (spinal fusion)
- Ovarian cancer surgery
- Prostate cancer surgery
Although pleased with the improving USNWR recognition and rankings, we know that the quality of the care we deliver is not defined by a single ranking system. We continue to deliver outstanding care to some of the country’s most vulnerable patients and diverse communities, which is may not always be reflected in the USNWR models.
This can be especially seen at times with regards to the Cardiology and Heart Surgery care – where our performance on care in our quality and national registries is substantially better than some of the claim’s data based measure. Nevertheless, we continue to work on our processes to improve and capture the care we deliver in addition to working on ways to innovate and improve patient outcomes. We have seen some of the recent changes due to these efforts and will anticipate continuing to see those in upcoming years. Additionally, these efforts are often recognized in other measures some of which are provided below.
- Newsweek ranking of the World’s Best specialized hospitals for heart care (July 2022)
- https://www.newsweek.com/worlds-best-specialized-hospitals-2022, Duke University Hospital – Division of Cardiology ranked 13th
- STS 3 Star ratings for CT surgery
- “A” distinction from The Leapfrog Group for upholding patient safety
- Achieving an Overall Hospital Quality Star Rating of 4 Stars from the Centers for Medicare and Medicaid (CMS)
- Maintaining the 1 ranking of our Children’s Hospital in North Carolina
- Achieving Healthcare Equality Index Leader 2022 from the Human Rights Campaign
COVID-19 Update
Please continue to practice safe COVID-19 protocols in your day-to-day interactions with others. Be particularly vigilant about masking, and avoid eating indoors in group settings. The health of our team members and our patients remains a priority as we continue to monitor the COVID-19 trends throughout our community.
Stay home if you are not feeling well. Employees who begin to experience any COVID-19 symptoms should report symptoms through the Duke SymMon app, which is available in both the Apple and Google app stores.
Donate blood if you’re able to. Click here for Duke-sponsored blood drives through the Red Cross.
All the latest Clinical Operations updates related to COVID can be found at https://covid-19.dukehealth.org. Patient-facing resources on DukeHealth.org can be found here: https://www.dukehealth.org/covid-19-update/resources. Duke University maintains a resource page as well, which can be accessed here: https://coronavirus.duke.edu/updates/for-staff.
Upcoming Events & Opportunities
August 17: Duke GME DEI ‘First Look’. The Duke Office of Graduate Medical Education is holding a virtual DEI ‘First Look’ event for potential incoming residents and fellows. It’s specifically designed for underrepresented applicants and any applicant interested in DEI issues. Registration is required.
September 25: Triangle Heart Walk. PNC Arena, Raleigh. Check-in starts at 11 am. Walk begins at Noon. Join us!
October 14: Cardio-Oncology in the Era of Precision Medicine. Symposium to be held at the J.B. Duke Hotel, Durham, NC. Registration is open: https://bit.ly/CardioOnc22. Email Beth Tanner with questions: beth.tanner@duke.edu.
Cardiology Grand Rounds
Cardiology Grand Rounds has concluded and will resume in September.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
July 23 — Stephen Greene
Practical Cardiology
Don’t Miss a Beat: Understanding GFR Slope, with Brendon Neuen, MBBS, MSc
https://duke.is/5zn99
July 26 — Richard Shannon
The News Courier
How the Dobbs decision affects women and children
https://duke.is/4nw5f
July 26 — Duke University Hospital, Duke Regional Hospital
CBS17.com
The Triangle is home to 5 of NC’s top 10 hospitals, says US News & World Report
https://duke.is/92n74
July 27 — Michael Pencina
CLPmag.com
Traditional Health Assessment Beats Genetic Test for Heart Disease Prediction, Study Shows
https://duke.is/b7v66
July 27 — Duke University Health System
Becker’s Hospital Review
https://duke.is/zqnyt
July 27 — Sujay Kansagra (Pediatrics)
CBS17.com
Study finds frequent naps linked to high blood pressure, stroke
https://duke.is/mr69s
July 27 — Duke University Hospital and Duke Regional Hospital
Newsobserver.com
Where Triangle hospitals land in new US News & World rankings
https://duke.is/88s53
July 28 — Shahzeb Khan
HealthDay*
More Young Americans Are Dying of Heart Failure
https://duke.is/rnvvu
*carried by additional 196 news outlets
July 28 — Julie Doberne
Medscape
World’s First HIV+ to HIV+ Heart Transplant Performed
https://duke.is/69wea
Duke Heart Pulse – July 24th 2022
Highlights of the week:
DBAP Outing with the Cardiology Fellows
Our newest cardiology fellows got a taste of downtown Durham with an outing on Saturday night to see our Triple-A affiliate, the Durham Bulls, at Durham Bulls Athletic Park. The Bulls played the Norfolk Tides and picked up a 9-8 win in game two of their three game set. Game three is this afternoon. We believe our Duke Heart attendance at the game really gave the Bulls an edge – thanks to all who joined us!
Although it was warm out – the right field picnic area provided a great place to have the families watch the game with some shade, food and drinks. Thanks to Anna Lisa and the fellowship team for helping set up this fun event.



Fudim Presents MGR
On Friday, July 22 Marat Fudim, assistant professor of medicine in cardiology, led a very informative Medicine Grand Rounds on pressure and volume management in patients with chronic heart failure. His presentation covered how volume is distributed throughout the body, the contribution of vasoconstriction to increased intra-cardiac pressures, and several new treatment avenues for patients. In case you missed it, you can view the full recording here: https://warpwire.duke.edu/w/e_MGAA/
pressure and volume management in patients with chronic heart failure. His presentation covered how volume is distributed throughout the body, the contribution of vasoconstriction to increased intra-cardiac pressures, and several new treatment avenues for patients. In case you missed it, you can view the full recording here: https://warpwire.duke.edu/w/e_MGAA/
This work has opened up many more interesting physiologic studies, devices, and work that Marat and team are helping Duke take the lead on nationally.
Great job, Marat!
Nurse Scientists in Academic-Practice Partnership Improve Rigor of Nursing Science
Asking the right clinical questions is second nature for a nurse, but asking clinical questions in ways that are amenable to scientific solutions is a critical skill that takes time, expertise and mentorship to develop. Faculty at Duke University School of Nursing and Duke University Health System (DUHS) are partnering to help clinical inquiry flourish through collaboration between bedside nurses and nurse scientists. Fruits of the partnership are leading to improved rigor in research and quality improvement design that, in turn, help to improve outcomes for patients and families.
Bradi Granger, MSN, PhD, RN, a professor and director of Duke Heart Center Nursing Research Program, Staci Reynolds, PhD, RN, associate professor and clinical nurse specialist at Duke University Hospital (DUH), and Anna Mall, MSN, RN, assistant nurse manager for the adult cardiac catheterization labs at DUH, recently co-authored an article on clinical inquiry in the American Association of Critical-Care Nurses (AACN) Advanced Critical Care Summer 2022 journal.

Their work is one of many projects and activities that are an outcome of the Duke Advancement of Nursing, Center of Excellence (DANCE), an academic practice partnership between nurses in the School of Nursing and DUHS, which leverages the experience, knowledge, and aspirations of nurses across both entities.
In an example of the relationships DANCE fosters, Granger immediately thought of Reynolds and Mall when a question came up at a national conference: How can any small-scale, single-site study be valuable to growing and expanding nursing science?
The authors answered that question by creating a pyramid structure outlining a step-by-step approach to clinical inquiry that results in generalizable data that can impact the national or even global health care research priorities for improving health and patient care.
“There is, at the end of the day, a randomized trial that can contribute causal evidence to a patient problem and provide data to change practice and leverage policy,” Granger said.
Mall says that she and her team noticed that patients consistently experience discomfort in response to catheter insertion, despite the administration of pre-procedural pain medicine.
“My whole question was, why are we giving this medication? Is it doing what we need it to do? Can we do it a different way,” she said.
The first step of the pyramid examined current research and recommendations in the literature about what to do when there was breakthrough pain during the procedure. The next step was designing a study to analyze existing cath lab data for clues to the precursors of pain during the procedure. The next step was designing and conducting the randomized trial that compared two pre-procedural sedation intervals. The last step was taking the results of that trial and building further questions based on focus groups with the nurses and the patients, expanding the inquiry to include additional studies, each addressing the patient experience from different angles.
Reynolds’s study focused on central line-associated bloodstream infections, or CLABSIs. Because the infections are costly to treat and create a longer, and possibly more complicated recovery for patients, Reynolds was interested in how to mitigate the rate of infections. Protocol calls for chlorohexidine gluconate (CHG) bathing, but Reynolds found that there was low compliance by nurses across the U.S., partly because patients didn’t like the baths, which some find uncomfortable or because they dislike the smell.
Reynolds partnered with Granger, who had connections with Wake Med, and conducted a collaborative study that found that, with greater compliance and procedural understanding, the rate of infection decreased. But they took results of the study a step further to talk to patients and nurses about their experiences.
“There were just a lot of little one-offs from that larger study that we were able to do to keep the ball rolling and answer further clinical inquiry questions as they came up,” she said, noting that having a randomized trial as the primary source was critical. “It’s not until you get to talking to the bedside nurses and patients that you get into the nitty gritty details of maybe why the intervention of CHG bathing treatments, as recommended in the evidence-based CDC guideline, isn’t working so well [in real world clinical practice].”
Implementing the pyramid approach to clinical inquiry requires the type of collaboration DANCE offers.
“The whole premise of DANCE as an academic health system partnership is to bring academicians on the school side, who are experts in the science and design of clinical inquiry, together with the health system nurses to support health system science,” Granger said. “Clinical inquiry, when it’s done well, requires a rigorous scientific design so that the study can effectively inform practice.”
Mall agrees that the questions can often come from clinical nurses, but they need the support and structure that a nurse scientist offers.
“I think what’s very unique in the partnership with DANCE is we have those relationships established,” she said. “It makes that nurse scientist accessible to the bedside nurse.”
Mall said her experience collaborating with the nurse scientists has improved her leadership skills by allowing her time to help with the design study, data collecting, team-building and number-crunching that she would not have been able to do otherwise.
Granger is interested in ensuring that more health systems, including those without academic-practice partnerships like DANCE, have opportunities for collaboration with nurse scientists.
“That’s one thing we’re working on at Duke through DANCE, to make the resources of a nurse scientist more accessible for our smaller community hospitals, and also around the country, to share this model we’re using at Duke,” she said.
The co-authors’ work helps to demonstrate how nurse scientists and researchers have a key role in advancing nurses’ leadership skills, autonomy, and decision-making skills, in turn, improving professional practice environments and health outcomes for real people, families and communities.
Great Catch, Nelson!
We were excited to learn this week that our Duke Heart cath lab team member Eric Nelson, CVIS, received a ‘Great Catch!‘ award.
Eric quickly spoke up to prevent the premature removal of an arterial introducer sheath in an anticoagulated patient in the Cardiac Catheterization Lab at Duke University Hospital. His timely action helped ensure that the introducer remained in place until the patient’s clotting time returned to a safe level, which minimized the risk of bleeding after sheath removal.
Excellent job, Eric! Congrats!!

COVID-19 Update
Please continue to practice safe COVID-19 protocols in your day-to-day interactions with others. Be particularly vigilant about masking, and avoid eating indoors in group settings. The health of our team members and our patients remains a priority as we continue to monitor the COVID-19 trends throughout our community.
Stay home if you are not feeling well. Employees who begin to experience any COVID-19 symptoms should report symptoms through the Duke SymMon app, which is available in both the Apple and Google app stores.
Donate blood if you’re able to. Click here for Duke-sponsored blood drives through the Red Cross.
All the latest Clinical Operations updates related to COVID can be found at https://covid-19.dukehealth.org. Patient-facing resources on DukeHealth.org can be found here: https://www.dukehealth.org/covid-19-update/resources. Duke University maintains a resource page as well, which can be accessed here: https://coronavirus.duke.edu/updates/for-staff.
Upcoming Events & Opportunities
July 25: Women in Cardiology. 6:30 p.m. Dinner and discussion on mentorship and sponsorship. For more information and location, please contact cardiology fellow Karen Flores Rosario, MD.
August 17: Duke GME DEI ‘First Look’. The Duke Office of Graduate Medical Education is holding a virtual DEI ‘First Look’ event for potential incoming residents and fellows. It’s specifically designed for underrepresented applicants and any applicant interested in DEI issues. Registration is required.
October 14: Cardio-Oncology in the Era of Precision Medicine. Symposium to be held at the J.B. Duke Hotel, Durham, NC. Registration is open: https://bit.ly/CardioOnc22. Email Beth Tanner with questions: beth.tanner@duke.edu.
Cardiology Grand Rounds
Cardiology Grand Rounds has concluded and will resume in September.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
July 15 — Robert Mentz
tctMD
US Dobutamine Shortage a ‘Huge Problem’—What’s the Solution?
https://duke.is/2vwsb
July 15 — Andrew Wang
Cardiology Today
‘Patients feel better’: New hope for obstructive hypertrophic cardiomyopathy
https://duke.is/gpnd7
July 18 — Robert Lefkowitz
GQ.com (Mexico)
Las reglas de oro para ser exitoso, según los ganadores del Nobel
https://duke.is/vxvcw
July 19 — John Haney and Matthew Hartwig
Yahoo.com*
Paragonix Expands Research for Advanced Organ Preservation Clinical Registries
https://duke.is/zku4a
*this story was also carried in Baltimore, Pittsburgh & Sacramento
July 19 — Mihai Podgoreanu and Negmeldeen Mamoun
Medpage Today
Fluid Therapy Showdown in Cardiac Surgery Disfavors Albumin
https://duke.is/m2k87
July 20 — Stuart Russell
Medscape
Pig Heart Transplants and the Ethical Challenges That Lie Ahead
https://duke.is/ysnaf
July 21 — Sreekanth Vemulapalli
WPTF (Raleigh-Durham-Fayetteville)
https://duke.is/2yknw
July 21 — Jason Katz
CardioNerds
Early Struggles, Notable Changes, and Ongoing Challenges in Cardiac Critical Care
https://duke.is/g9w6a
Division of Cardiology Publications Indexed in PubMed July 14-20, 2022
Al Rifai M, Newby LK, Nair AP, Misra A, Rogers JG, Fedson S, Virani SS. SGLT-2 Inhibitors for Patients with Heart Failure: What Have We Learned Recently? Curr Atheroscler Rep 2022;24(8):627-634. PM: 35653033.
Araújo TP, Borges LGS, Barroso WKS, Brandão AA, Barbosa ECD, Feitosa ADM, Malachias MVB, Mota Gomes M, Amodeo C, Povoa RMDS, Jardim PCBV, Lopes RD, Batista SRR, Vitorino PVO. Factors associated with uncontrolled blood pressure in hypertensive Brazilians. J Clin Hypertens (Greenwich) 2022;24(7):814-824. PM: 35770852.
Bahit MC, Vora AN, Li Z, Wojdyla DM, Thomas L, Goodman SG, Aronson R, Jordan JD, Kolls BJ, Dombrowski KE, Vinereanu D, Halvorsen S, Berwanger O, Windecker S, Mehran R, Granger CB, Alexander JH, Lopes RD. Apixaban or Warfarin and Aspirin or Placebo After Acute Coronary Syndrome or Percutaneous Coronary Intervention in Patients With Atrial Fibrillation and Prior Stroke: A Post Hoc Analysis From the AUGUSTUS Trial. JAMA Cardiol 2022;7(7):682-689. PM: 35612866.
Bikdeli B, Zahedi Tajrishi F, Sadeghipour P, Talasaz AH, Fanikos J, Lippi G, Siegal DM, Eikelboom JW, Monreal M, Jimenez D, Connors JM, Ageno W, Barnes GD, Piazza G, Angiolillo DJ, Parikh SA, Kirtane AJ, Lopes RD, Bhatt DL, Weitz JI, Mehran R, Krumholz HM. Efficacy and Safety Considerations With Dose-Reduced Direct Oral Anticoagulants: A Review. JAMA Cardiol 2022;7(7):747-759. PM: 35648414.
Chatterjee R, Kwee LC, Pagidipati N, Koweek LH, Mettu PS, Haddad F, Maron DJ, Rodriguez F, Mega JL, Hernandez A, Mahaffey K, Palaniappan L, Shah SH. Multi-dimensional characterization of prediabetes in the Project Baseline Health Study. Cardiovasc Diabetol 2022;21(1):134. PM: 35850765.
Collins KA, Ross LM, Slentz CA, Huffman KM, Kraus WE. Differential Effects of Amount, Intensity, and Mode of Exercise Training on Insulin Sensitivity and Glucose Homeostasis: A Narrative Review. Sports Med Open 2022;8(1):90. PM: 35834023.
Defilippis EM, Truby LK, Clerkin KJ, Donald E, Sinnenberg L, Varshney AS, Cogswell R, Kittleson MM, Haythe JH, Givertz MM, Hsich EM, Agarwal R, Topkara VK, Farr M. Increased Opportunities for Transplantation for Women in the New Heart Allocation System. J Card Fail 2022;28(7):1149-1157. PM: 35470056.
Gaudino M, Audisio K, Di Franco A, Alexander JH, Kurlansky P, Boening A, Chikwe J, Devereaux PJ, Diegeler A, Dimagli A, Flather M, Lamy A, Lawton JS, Tam DY, Reents W, Rahouma M, Girardi LN, Hare DL, Fremes SE, Benedetto U. Radial artery versus saphenous vein versus right internal thoracic artery for coronary artery bypass grafting. Eur J Cardiothorac Surg 2022;62(1):ezac345. PM: 35678560.
Giroux NS, Ding S, McClain MT, Burke TW, Petzold E, Chung HA, Rivera GO, Wang E, Xi R, Bose S, Rotstein T, Nicholson BP, Chen T, Henao R, Sempowski GD, Denny TN, De Ussel MI, Satterwhite LL, Ko ER, Ginsburg GS, Kraft BD, Tsalik EL, Shen X, Woods C. Differential chromatin accessibility in peripheral blood mononuclear cells underlies COVID-19 disease severity prior to seroconversion. Res Sq 2022;:rs.3.rs-1479864. PM: 35411343.
Greene SJ, Ezekowitz JA, Anstrom KJ, Demyanenko V, Givertz MM, Piña IL, O’Connor CM, Koglin J, Roessig L, Hernandez AF, Armstrong PW, Mentz RJ. Medical Therapy During Hospitalization for Heart Failure With Reduced Ejection Fraction: The VICTORIA Registry. J Card Fail 2022;28(7):1063-1077. PM: 35301107.
Jorbendaze A, Young R, Shaburishvili T, Demyanchuk V, Buriak R, Todurov B, Rudenko K, Zuber M, Stämpfli SF, Tanner FC, Erne P, Mirro M, Fudim M, Goldberg LR, Cleland JGF. Synchronized diaphragmatic stimulation for heart failure using the VisONE system: a first-in-patient study. ESC Heart Fail 2022;9(4):2207-2214. PM: 35619238.
Lala A, Mentz RJ. Fostering Belonging at JCF. J Card Fail 2022;28(7):1047. PM: 35840183.
Minhas AMK, Sagheer S, Ijaz SH, Nazir S, Khan MS, Zaidi SH, Fudim M, Rodriguez F, Johnson HM, Virani SS. Persistent Racial/Ethnic Disparities in Cardiology Trainees in the United States. J Am Coll Cardiol 2022;80(3):276-279. PM: 35835499.
Oslin DW, Lynch KG, Shih MC, Ingram EP, Wray LO, Chapman SR, Kranzler HR, Gelernter J, Pyne JM, Stone A, DuVall SL, Lehmann LS, Thase ME, , Aslam M, Batki SL, Bjork JM, Blow FC, Brenner LA, Chen P, Desai S, Dieperink EW, Fears SC, Fuller MA, Goodman CS. Effect of Pharmacogenomic Testing for Drug-Gene Interactions on Medication Selection and Remission of Symptoms in Major Depressive Disorder: The PRIME Care Randomized Clinical Trial. JAMA 2022;328(2):151-161. PM: 35819423.
Prabhakaran D, Singh K, Kondal D, Raspail L, Mohan B, Kato T, Sarrafzadegan N, Talukder SH, Akter S, Amin MR, Goma F, Gomez-Mesa J, Ntusi N, Inofomoh F, Deora S, Philippov E, Svarovskaya A, Konradi A, Puentes A, Ogah OS, Stanetic B, Issa A, Thienemann F. Cardiovascular Risk Factors and Clinical Outcomes among Patients Hospitalized with COVID-19: Findings from the World Heart Federation COVID-19 Study. Glob Heart 2022;17(1):40. PM: 35837356.
Prattipati S, Sakita FM, Tarimo TG, Kweka GL, Mlangi JJ, Maro AV, Coaxum LA, Galson SW, Limkakeng AT, Rugakingira A, Urasa SJ, Okeke NL, Mmbaga BT, Bloomfield GS, Hertz JT. Prevalence and Correlates of Ischemic ECG Findings among Adults With and Without HIV in Tanzania. Glob Heart 2022;17(1):38. PM: 35837355.
Rehorn MR, Daubert JP. Editorial commentary: Pulsed field catheter ablation in atrial fibrillation: The promising future of an old technology. Trends Cardiovasc Med 2022;32(6):388-389. PM: 34508849.
Salah HM, Fudim M, O’Neil ST, Manna A, Chute CG, Caughey MC. Post-recovery COVID-19 and incident heart failure in the National COVID Cohort Collaborative (N3C) study. Nat Commun 2022;13(1):4117. PM: 35840623.
Scirica BM, Im K, Murphy SA, Kuder JF, Rodriguez DA, Lopes RD, Green JB, Ruff CT, Sabatine MS. Re-adjudication of the Trial Evaluating Cardiovascular Outcomes with Sitagliptin (TECOS) with study-level meta-analysis of hospitalization for heart failure from cardiovascular outcomes trials with dipeptidyl peptidase-4 (DPP-4) inhibitors. Clin Cardiol 2022;45(7):794-801. PM: 35715946.
Duke Heart Pulse Week ending July 17th 2022
Highlights of the week:
The Duke Transplant Center Performs 10,000th Transplant
The Duke Transplant Center recently performed its 10,000th transplant per data from the Organ Procurement & Transplantation Network (OPTN) since performing its first organ transplant, a kidney, in 1965. This is a milestone that only 18 other centers in the U.S. have achieved and the first in North Carolina to meet that mark.
The Duke Transplant Center has reached this lifesaving goal by focusing on research and innovation to expand access to organs for patients on waiting lists. Recent examples include:
- Duke Heart surgeons were the first in the U.S. to successfully implant a new-generation artificial heart to bridge the gap until the patient successfully received a human heart transplant.
- Duke Heart surgeons were the first in the U.S. to perform a “donation after circulatory death” (DCD) heart transplant in adult and pediatric patients. More than 80 DCD heart procedures have been completed at Duke since our first procedures in 2019.
- The Southeast’s first living liver transplant between an HIV-positive donor and recipient.
- Use of organ preservation systems: The devices circulate warm, oxygenated blood, medications, and nutrients through the organ to preserve it and allow for testing before transplantation. It also means organs can travel farther to reach recipients.
- Duke Heart transplant’s wait time continued its trend from the last several years, reducing median time-to-transplant to 63 days against a U.S. median wait time of 149 days.
- The kidney transplant achieved high marks in their 1-year conditional survival with a functioning graft. Duke’s 1-year conditional survival rate for kidney was 99.69 percent against a U.S. rate of 97.03 percent.
Congratulations to all members of the Duke transplant teams past and present for contributing to this remarkable achievement (with very special kudos to all members of our heart and lung transplant teams!). Most especially we want to thank our donor patients and their families for giving the gift of life to our recipient patients who also deserve a big shout-out. We thank all of them for entrusting their care to us.1000th Tx graphic
Study to Prevent Heart Disease in Breast Cancer Patients Receives NHLBI Funding
The National Heart, Lung and Blood Institute (NHLBI) has awarded a five-year grant to Atrium Health Wake Forest Baptist  Comprehensive Cancer Center, Duke Cancer Institute and Virginia Commonwealth University Massey Cancer Center to collaborate in a first-of-its-kind prospective study about the long-term heart health of young breast cancer survivors.
Comprehensive Cancer Center, Duke Cancer Institute and Virginia Commonwealth University Massey Cancer Center to collaborate in a first-of-its-kind prospective study about the long-term heart health of young breast cancer survivors.
The Cardiac Outcomes With Near Complete Estrogen Deprivation (CROWN) study will investigate preclinical cardiovascular effects of estrogen deprivation therapy for the treatment of breast cancer in premenopausal women and is expected to start enrollment in August. The investigators will use novel imaging methods with CT and CMR, as well as biomarkers of cardiotoxicity and inflammation to advance the understanding the effects of estrogen deprivation has on the cardiovascular system, with the goal to better predict, prevent, and treat cardiovascular disease associated with breast cancer treatment.
This is one of many collaborative efforts currently underway in the Duke Cardio-Oncology program. Susan Dent, MD, a medical oncologist who focuses on breast cancer and who serves as associate director of clinical research  for the Duke Cancer Institute Breast Cancer Disease Group and Igor Klem, MD, a cardiologist specializing in imaging for the division of cardiology will serves as lead investigators for the Duke site.
for the Duke Cancer Institute Breast Cancer Disease Group and Igor Klem, MD, a cardiologist specializing in imaging for the division of cardiology will serves as lead investigators for the Duke site.
To read more, please visit: https://duke.is/navh.
Duke-UNC Project Wins 3rd Place in American Heart Association Heart Failure Data Challenge
A team from Duke University School of Medicine and the University of North Carolina School of Medicine was awarded third place by the American Heart Association for a project addressing the elements of structural racism that lead to poor heart health.
The American Heart Association and the Association of Black Cardiologists hosted a six-month heart failure data challenge in which research groups tested the relationships between heart failure and health disparities, social determinants of health and structural determinants of health. The results were evaluated by a peer review group of nearly 30 experts in the field.
“Congratulations to these researchers for their exceptional work in the heart failure data challenge,” said Michelle A. Albert, MD, past president of the Association of Black Cardiologists and current president of the American Heart Association.
“Improving our understanding of how social determinants of health impact certain populations in order to develop consequential targeted solutions requires harmonization of different types of data,” Albert said. “These teams must be commended for their efforts at addressing health equity, one of the most pressing areas in healthcare.”
 The Duke/UNC project was led by Vishal Rao, MD, an advanced heart failure and transplant cardiology fellow at Duke, Rob Mentz, MD, section chief of heart failure in the Duke Division of Cardiology, and Melissa Caughey, PhD, a cardiovascular epidemiologist from the University of North Carolina School of Medicine.
The Duke/UNC project was led by Vishal Rao, MD, an advanced heart failure and transplant cardiology fellow at Duke, Rob Mentz, MD, section chief of heart failure in the Duke Division of Cardiology, and Melissa Caughey, PhD, a cardiovascular epidemiologist from the University of North Carolina School of Medicine.
Collaborators included Gregg C. Fonarow, MD, who serves on the steering committee for the American Heart Association’s Get with the Guidelines program and as interim chief of UCLA’s Division of Cardiology and director of the Ahmanson-UCLA Cardiomyopathy Center; Amanda Coniglio, MD, former Duke cardiology chief fellow now on faculty at Rochester Regional Hospital; and Duke cardiology and DCRI faculty Adam DeVore, MD, Marat Fudim, MD, Michelle Kelsey, MD, and Roland Matsouaka, MD.
The project explored the association between socioeconomic status disadvantage and in-hospital heart failure outcomes in patients from diverse neighborhoods in the Get With The Guidelines-Heart Failure registry.
This project was inspired by Duke University School of Medicine Division of Cardiology-led efforts to improve heart failure outcomes across central North Carolina. The work prompted the research collaboration between Duke and UNC to better understand how neighborhoods were associated with quality of care and in-hospital outcomes for patients with heart failure.
The project team used the Precision Medicine Platform to investigate key questions around socioeconomic disparities and heart failure outcomes. The Precision Medicine Platform is an easy-to-use research interface that allows researchers to collaborate from anywhere in the world in a secure, cloud-based environment.
With artificial intelligence and deep machine learning capabilities, the Precision Medicine Platform gives researchers the power and speed to bring their data together collaboratively and accelerate their findings into impactful discoveries for patients faster than ever before.
The team hopes to translate the results into local implementation efforts to characterize and mitigate gaps in care defined by socioeconomic groups or neighborhoods.
The research findings from all the winning studies are currently under consideration for publication in peer-reviewed scientific journals and are not yet publicly available.
You can read more about the data challenge here.
Congratulations, Vishal, Rob and team!!!
New Cardiology Stepdown Unit Assistant Nurse Manager Appointments, Effective July 18
Duke Heart is pleased to announce three new assistant nurse manager appointments that will go into effect on Monday, July 18, 2022.
 Olivia Gunter, BSN, RN, PCCN will become the Assistant Nurse Manager of Operations for Duke University Hospital’s Cardiology Stepdown Unit 7100. Olivia started out as a new graduate nurse on 7100 in 2019 and is honored to continue working with her coworkers in this new position. Olivia will continue making positive impacts on orientation and quality improvement efforts on 7100, both of which are her passions. Outside of work, Olivia enjoys trying out new recipes in the kitchen and is a recent newlywed!
Olivia Gunter, BSN, RN, PCCN will become the Assistant Nurse Manager of Operations for Duke University Hospital’s Cardiology Stepdown Unit 7100. Olivia started out as a new graduate nurse on 7100 in 2019 and is honored to continue working with her coworkers in this new position. Olivia will continue making positive impacts on orientation and quality improvement efforts on 7100, both of which are her passions. Outside of work, Olivia enjoys trying out new recipes in the kitchen and is a recent newlywed!
Dylan Coombs, BSN, RN, will become the Assistant Nurse Manager of Operations for Duke University Hospital’s Cardiology Stepdown Unit 7300. Dylan obtained an Associate of Applied Science in Nursing from Durham Technical Community College in 2013 and a Bachelor of Science in Nursing from Winston Salem State University in 2021. He began his career in nursing working in transitional rehabilitation, long term elder care, and hospice. Dylan started working at Duke University Hospital in 2017 as a CN II on 7300 where he has remained an integral part of the unit. In his time on 7300, Dylan has functioned in the role of bedside RN, Preceptor, and Charge Nurse as well as Co-Chair for the Heart Center Clinical Practice Committee. Additionally, he works as a Clinical Instructor for Duke University School of Nursing where he teaches ABSN students on surgical unit 6300 at Duke University Hospital. Prior to his endeavors in nursing, he has over a decade of experience in sales, marketing, and retail management.
University Hospital’s Cardiology Stepdown Unit 7300. Dylan obtained an Associate of Applied Science in Nursing from Durham Technical Community College in 2013 and a Bachelor of Science in Nursing from Winston Salem State University in 2021. He began his career in nursing working in transitional rehabilitation, long term elder care, and hospice. Dylan started working at Duke University Hospital in 2017 as a CN II on 7300 where he has remained an integral part of the unit. In his time on 7300, Dylan has functioned in the role of bedside RN, Preceptor, and Charge Nurse as well as Co-Chair for the Heart Center Clinical Practice Committee. Additionally, he works as a Clinical Instructor for Duke University School of Nursing where he teaches ABSN students on surgical unit 6300 at Duke University Hospital. Prior to his endeavors in nursing, he has over a decade of experience in sales, marketing, and retail management.
 Katia Anello, BSN, RN, will become the Assistant Nurse Manager of Operations for Duke University Hospital’s Cardiology Stepdown Unit 7300. Katia earned a Bachelor of Science in Nursing at the University of Lynchburg in 2019. She completed a summer PNA externship and was a clinical nurse for three years on 4100 General Medicine. She is a CAUTI and CLABSI Champion, Maestro Care User Group member, Magnet Ambassador, and Clinical Practice Council member. Katia was a 2021 CHG EBP Fellow and implemented a health system-wide charting change to help increase CHG bathing compliance. Katia will be attending Duke University this fall to get her Master’s in Nursing and Healthcare Leadership.
Katia Anello, BSN, RN, will become the Assistant Nurse Manager of Operations for Duke University Hospital’s Cardiology Stepdown Unit 7300. Katia earned a Bachelor of Science in Nursing at the University of Lynchburg in 2019. She completed a summer PNA externship and was a clinical nurse for three years on 4100 General Medicine. She is a CAUTI and CLABSI Champion, Maestro Care User Group member, Magnet Ambassador, and Clinical Practice Council member. Katia was a 2021 CHG EBP Fellow and implemented a health system-wide charting change to help increase CHG bathing compliance. Katia will be attending Duke University this fall to get her Master’s in Nursing and Healthcare Leadership.
Congratulations to each of them. Please join us in welcoming Olivia, Dylan, and Katia to their new roles!
Ohman Celebration Held
Dr. Magnus Ohman was celebrated by dozens of friends, coworkers and family on Thursday evening, July 14th at the Washington Duke Inn. It was a special evening for guests to gather, mingle and reflect on their long-standing ties to Magnus and gave him an opportunity to see and thank colleagues from across the years.




Alumni News: Forging the Future of Biotech and the Business of Health Care
Duke alumnus Dr. Michael Cuffe is among four alumni profiled in the recent issue of DukeMed alumni news magazine as well as the SOM’s Magnify. Cuffe, a former Duke cardiology fellow, is now executive vice president and chief clinical officer at HCA Healthcare. Read the full story here: https://duke.is/5wu8g.

Photo of the Week
In a sight rarer than observing Halley’s Comet, all three Duke heart transplant surgeons arrived at clinic 2F2G to evaluate candidate heart transplant patients along with the Cardiothoracic OR APP Team! This was such a rare sight to have them together it required photo evidence for the archives. We appreciate all of the work being done by Drs. Carmelo Milano, Jacob Schroder and Ben Bryner — and the CT OR APP Team appreciated the sudden influx of expertise arriving to clinic!

Special thanks to Richard Sabulsky for the photo!
COVID-19 Update
All the latest Clinical Operations updates related to COVID can be found at https://covid-19.dukehealth.org. Patient-facing resources on DukeHealth.org can be found here: https://www.dukehealth.org/covid-19-update/resources. Duke University maintains a resource page as well, which can be accessed here: https://coronavirus.duke.edu/updates/for-staff.
Upcoming Events & Opportunities
July 22: Pressure and Volume Management in Heart Failure with Marat Fudim for Medicine Grand Rounds, 8 a.m. DUH 2002 or via Zoom.
July 26: Women in Cardiology. The WIC team postponed their event originally planned for June 30. Details will be announced soon. For more information, please contact cardiology fellow Karen Flores Rosario, MD.
August 17: Duke GME DEI ‘First Look’. The Duke Office of Graduate Medical Education is holding a virtual DEI ‘First Look’ event for potential incoming residents and fellows. It’s specifically designed for underrepresented applicants and any applicant interested in DEI issues. Registration is required.
October 14: Cardio-Oncology in the Era of Precision Medicine. Symposium to be held at the J.B. Duke Hotel, Durham, NC. Registration is open: https://bit.ly/CardioOnc22. Email Beth Tanner with questions: beth.tanner@duke.edu.
Cardiology Grand Rounds
Cardiology Grand Rounds has concluded and will resume in September.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
July 8 — Nishant Shah
CBS-17/WNCN Raleigh
Most Americans don’t have optimal heart health
https://duke.is/97hpk
*story begins around 16:21:05
July 8 — Susan Dent
Cardiovascular Business
Could an effective breast cancer therapy be bad for the heart? NIH awards $3.1M to find out
https://duke.is/2rs6z
July 9 — Duke Cancer Institute
Winston-Salem Journal
Atrium Wake Forest Baptist center participates in heart-cancer link study
https://duke.is/gbrjx
July 12 — Manesh Patel
Health Digest
This Is When You Should Worry About Leg Pain
https://duke.is/znguf
July 13 — Stuart Russell
Medscape
The Heartache of Bereavement Can Be Fatal in Heart Failure
https://duke.is/m76wq
July 13 — Adrian Hernandez
Healthcare Purchasing News
Studies reveal fluticasone furoate ineffective against COVID-19 symptoms
https://duke.is/8ss5r
July 13 — Adrian Hernandez
CBS17.com/WNCN
Researchers settle debate on another off-label COVID treatment
https://duke.is/cjkmj
July 13 — Andrew Wang
HealthCentral
Sneaky Signs You Could Have HCM
https://duke.is/w4wnp
July 14 — Adrian Hernandez
USnews.com
Asthma Drug Fluticasone Fails as Potential COVID Treatment
https://duke.is/6uwen
July 14 — Sunil Rao
Medscape
Interventional Imagers Take on Central Role, and More Radiation
https://duke.is/pfnt8
July 14 — Vishal Rao and Robert Mentz
CBS17.com/WNCN
https://duke.is/ryvvc
Division of Cardiology Publications Indexed in PubMed July 7-13, 2022
Abramov D, Minhas AMK, Fudim M, Chung JS, Patel JN, Rabkin DG. Impact of the heart transplant allocation policy change on inpatient cost of index hospitalization. Clin Transplant 2022 Jul;36(7):e14692. PM: 35499219.
Filippatos G, Pitt B, Agarwal R, Farmakis D, Ruilope LM, Rossing P, Bauersachs J, Mentz RJ, Kolkhof P, Scott C, Joseph A, Bakris GL, Anker SD. Finerenone in patients with chronic kidney disease and type 2 diabetes with and without heart failure: a prespecified subgroup analysis of the FIDELIO-DKD trial. Eur J Heart Fail 2022 Jun;24(6):996-1005. PM: 35239204.
Giroux NS, Ding S, McClain MT, Burke TW, Petzold E, Chung HA, Rivera GO, Wang E, Xi R, Bose S, Rotstein T, Nicholson BP, Chen T, Henao R, Sempowski GD, Denny TN, De Ussel MI, Satterwhite LL, Ko ER, Ginsburg GS, Kraft BD, Tsalik EL, Shen X, Woods CW. Differential chromatin accessibility in peripheral blood mononuclear cells underlies COVID-19 disease severity prior to seroconversion. Sci Rep 2022 Jul 9;12(1):11714. PM: 35810186.
Keshvani N, Mehta A, Alger HM, Rutan C, Williams J, Zhang S, Young R, Alhanti B, Chiswell K, Greene SJ, DeVore AD, Yancy CW, Fonarow GC, Pandey A. Heart failure quality of care and in-hospital outcomes during the COVID-19 pandemic: findings from the Get With The Guidelines-Heart Failure registry. Eur J Heart Fail 2022 Jun;24(6):1117-1128. PM: 35289038.
Kochav JD, Kim J, Judd R, Tak KA, Janjua E, Maciejewski AJ, Kim HW, Klem I, Heitner J, Shah D, Zoghbi WA, Shenoy C, Farzaneh-Far A, Polsani V, Villar-Calle P, Parker M, Judd KM, Khalique OK, Leon MB, Devereux RB, Levine RA, Kim RJ, Weinsaft JW. Myocardial Contractile Mechanics in Ischemic Mitral Regurgitation: Multicenter Data Using Stress Perfusion Cardiovascular Magnetic Resonance. JACC Cardiovasc Imaging 2022 Jul;15(7):1212-1226. PM: 35798397.
Kuneman JH, El Mahdiui M, van Rosendael AR, van den Hoogen IJ, Patel MR, Nørgaard BL, Fairbairn TA, Nieman K, Akasaka T, Berman DS, Hurwitz Koweek LM, Pontone G, Kawasaki T, Rønnow Sand NP, Jensen JM, Amano T, Poon M, Øvrehus KA, Sonck J, Rabbat MG, et al. Coronary volume to left ventricular mass ratio in patients with diabetes mellitus. J Cardiovasc Comput Tomogr Jul-Aug 2022;16(4):319-326. PM: 35190274.
Moll-Bernardes R, Fortier SC, Sousa AS, Lopes RD, Vera N, Conde L, Feldman A, Arruda G, Cabral-Castro M, Albuquerque DC, Paula TC, Furquim T, Loures VA, Giusti K, Oliveira N, Macedo A, Barros E Silva P, De Luca F, Kotsugai M, Domiciano R, Silva FA, et al. NKG2A Expression among CD8 Cells Is Associated with COVID-19 Progression in Hypertensive Patients: Insights from the BRACE CORONA Randomized Trial. J Clin Med 2022 Jun 27;11(13):3713. PM: 35806995.
Patel RA, Musharoff SA, Spence JP, Pimentel H, Tcheandjieu C, Mostafavi H, Sinnott-Armstrong N, Clarke SL, Smith CJ, , Durda PP, Taylor KD, Tracy R, Liu Y, Johnson WC, Aguet F, Ardlie KG, Gabriel S, Smith J, Nickerson DA, Rich SS, Rotter JI, Tsao PS, et al. Genetic interactions drive heterogeneity in causal variant effect sizes for gene expression and complex traits. Am J Hum Genet 2022 Jul 7;109(7):1286-1297. PM: 35716666.
Vaduganathan M, Piccini JP, Camm AJ, Crijns HJGM, Anker SD, Butler J, Stewart J, Braceras R, Albuquerque APA, Wieloch M, Hohnloser SH. Dronedarone for the treatment of atrial fibrillation with concomitant heart failure with preserved and mildly reduced ejection fraction: a post-hoc analysis of the ATHENA trial. Eur J Heart Fail 2022 Jun;24(6):1094-1101. PM: 35293087.
Duke Heart Pulse – July 10th 2022
Highlights of the week:
Yaport Joins CT Anesthesia Faculty
Mihai Podgoreanu, MD, announced the arrival this week of the newest faculty member to join the CT Anesthesia team. Dr. Miguel Yaport comes to Duke after serving for the past two years as a faculty member at Tufts, including as an attending in their Cardiovascular Center ICUs.
 After obtaining his medical degree at Icahn School of Medicine at Mount Sinai, Miguel completed anesthesiology residency at the University of Pennsylvania, followed by a pediatric anesthesia fellowship at Montefiore and a Critical Care Fellowship at the Brigham and Women’s Hospital.
After obtaining his medical degree at Icahn School of Medicine at Mount Sinai, Miguel completed anesthesiology residency at the University of Pennsylvania, followed by a pediatric anesthesia fellowship at Montefiore and a Critical Care Fellowship at the Brigham and Women’s Hospital.
Miguel will start in the CTICU later this month and will also participate in the care of non-CT critically ill patients. His research interests include pulmonary hypertension, cardiogenic shock, value-based healthcare, and process-based improvement.
Welcome, Miguel!
Farrell Retires from Duke CTICU
Congratulations to Deb Farrell, an absolutely terrific Cardiothoracic Intensive Care Unit (CTICU) nurse, who retired from Duke at the end of June. She joined the Duke team in 1995, having already worked elsewhere as a nurse for 16 years (she has been an RN since 1979).

During her time in the CTICU, she served as preceptor, charge nurse, chair of the unit’s scheduling committee, as a member of the unit research committee and a member of the Duke University Hospital Informatics Council. She has been a member of our Maestro workgroup and the Rapid Response Team. She also cross-trained to both the DUH Dialysis team and Hyperbarics team in order to help those departments.
Deb is a winner of the 2021 American Association of Critical-Care Nurses Circle of Excellence Award, one of 25 given nationally each year to outstanding ICU nurses. She also was the recipient of a Duke Friends of Nursing Award in 2007.
Deb has been instrumental in shaping the care delivered to our cardiothoracic patients over the years and as a mentor and colleague to countless nurses on the CTICU. She will be missed! We wish her all the best in retirement.
Congrats, Deb!
Sangvai Named Interim President, Duke Regional
Devdutta Sangvai, MD, has accepted the role of interim president for Duke Regional Hospital. The search for a successor to Katie Galbraith, who announced her retirement from the role will take place in August, is now underway.
Sangvai stepped down this year as out-going Chair of the Durham County Hospital Corporation Board of Trustees, which is responsible for Duke Regional Hospital. He is well-known and admired by the Durham community. At Duke Health, Sangvai is vice chair for strategy for the Department of Family Medicine and Community Health and Vice President for Population Health Management, leading the Population Health Management Office (PHMO) at Duke University Health System. Complementing the work of PHMO, Sangvai is also Executive Director of Duke Connected Care, Duke’s accountable care organization/clinically integrated network.
Barbara Griffith, MD, President of Duke Raleigh Hospital and former Chief Medical Officer for Duke Regional Hospital, will co-chair the search committee for the new president of Duke Regional with Craig Albanese, MD.
Congratulations, Dev!
Alumni News: Echols Named Chief DEI Officer for ACC
 Melvin R. Echols, MD, associate professor of medicine in cardiology at Morehouse School of Medicine and alumnus of Duke’s internal medicine and cardiology training programs, has been named Chief Diversity, Equity and Inclusion Officer by the American College of Cardiology (ACC).
Melvin R. Echols, MD, associate professor of medicine in cardiology at Morehouse School of Medicine and alumnus of Duke’s internal medicine and cardiology training programs, has been named Chief Diversity, Equity and Inclusion Officer by the American College of Cardiology (ACC).
The news was announced Thursday, July 7. Echols will lead the ACC’s diversity, equity and inclusion strategy and programs, while also maintaining a portion of his current clinical and research responsibilities at Morehouse School of Medicine in Atlanta. His term begins July 18.
“The discovery of commonalities between people and culture while providing quality cardiovascular care to all is strengthened by diversity, and will ultimately improve health equity in our society,” Echols said. “Everyone has a part to play in this mission and should feel included in helping to make our society and the world better than yesterday.”
Congratulations, Melvin!!
Kudos to Laura Blue, Lead VAD Coordinator
There are members of our team who serve as something of a backbone for us – people who work relentlessly toward the goal of ensuring great patient care, access to clinical trials, and excellent patient education. One of those team members is Laura Blue, RN, AGNP, DNP, who has served as our lead Ventricular Assist Device (VAD) coordinator since 2003.
We received a really terrific note about her recently which made us think about the hundreds of lives she has touched during her time with us at Duke. She has done this not only through direct patient care and training, but also through her work on some of the largest device clinical trials that Duke Heart has participated in. We reached out to a number of her closest colleagues and a patient for their thoughts about her and the work she has done. But first, the original note stated:
“I wanted to send a big thank you to Laura. As you know, she means a lot to her patients especially the patients who were implanted years ago. Last week, a family decided to withdraw VAD support from a patient. The family said, “We want Laura to be here, she has known us since we were little and gave grandmom so many great years.” While speaking, the family member gestured the height of a small child. In this time of sadness, the thought of Laura being with the family brought them so much comfort. Laura rounded with us earlier that day and returned to the hospital for another 4 hours that evening and night to be with the patient and assist with the VAD. This was really kind of Laura to do and to stay with the family for some time after.” — Rio Landa, Co-team leader, Cardiology APPs
We know this story is not uncommon when it comes to Laura. She is extremely dedicated to our patients, to helping them learn about their condition and how to prepare for a device as well as how to care for it. She works hard to ensure caregivers understand how to best help their loved one.
“I met Laura in May of 2013 when I got my first VAD. I built up a relationship with Laura and all the people on the VAD team over the years. They’ve done a lot for me. I didn’t know what a VAD was until I got to Duke. I had never heard of it before. I had been living with congestive heart failure, couldn’t walk – certainly not much of a distance – I’d just give out. Once I got the VAD and got rehab, I was walking 20 miles a week with it. Laura Blue trained me and my wife, who was my caretaker at the time. Laura trained us both in how to maintain the VAD. She taught us everything we needed to know – especially that the main thing we had to do was maintain it and keep it clean so I wouldn’t get an infection, and I never got one in the seven years I had it. In between VADs, I was treated for cancer. In order to be eligible for transplant, I’d have to be cancer-free for 5 years. About a year before I was eligible for my second VAD, I ended up at Duke with double pneumonia and the doctor mentioned my weight to me, but you know, it was Laura who came to me and said, “I’m gonna shoot it to you straight. You’ve got to lose some weight if you want to get on transplant.” So, when I got better from the pneumonia, I got after it seven days a week. I’d get up at 5 a.m. and I’d start walking, maybe a quarter of a mile. I eventually got up to 3 miles per day and I did that seven days a week. I lost the weight, changed my eating habits, and lost 100 pounds. When I got my transplant, I said, “I might come back to Duke for something, but it ain’t going to be because of my heart.” So, I kept up the program and I still walk about 20 miles a week now. I’ve dropped another 100 pounds since my transplant. I thank Laura for this; I wouldn’t be here today without her help. She really took time with me and encouraged me and made a big difference in my life.” — Glen Barron, two-time Duke VAD recipient & grateful heart transplant patient
Helen Barnes has supported Laura for more than 10 years at Duke. She has come to know the patients, too, and says that Laura is often the first person that any patient asks for – she is the face at Duke that they recognize most and she’s the person they request if they’re in distress.
“Laura is such an encourager. She is so great at rooting for her team members and for her patients. She encouraged me to continue my education and she really helped motivate me along the way. She is a great person – I have seen her stay at Duke at night with families if a patient isn’t doing well. I’ve seen her take food to their homes. She goes 110 percent for her patients. She truly cares — she treats them as she’d like to see her family treated. She encourages her team to do the same – to treat them like individuals. She may come across as having a hard exterior sometimes, but inside she has such a big heart and she really loves all her team members, too. She’s a team player and a great asset to Duke.” – Helen Barnes, staff assistant
“Laura has been working with LVAD patients since the start of the program in the 1990s. Her amazing dedication to the field and to our Duke patients has resulted in care improvements that are implemented around the world. Despite her international reputation, the patients at Duke think of her as one of them and it is no surprise that a long-time Duke patient and family would feel this way about Laura. She always has the patient’s best interest at heart. It is a privilege to work with her.” – Stu Russell, MD
“Laura is a true professional. You can call on her for LVAD emergencies at all times of the day, night and weekend. She’s responsive and really helps our patients. She is always on call for the LVAD patient. She has enabled the Duke Heart Center to be the leading enroller in numerous national LVAD trials including the Heartmate II Thoratec trial, ENDURANCE (Heartware Medtronic trial) and most recently the MOMENTUM trial (Heartmate III Abbott trial). Because of our leading role in these trials, Duke has become a national leader in mechanical circulatory support, in general. I’d say she has been instrumental.” – Carmelo Milano, MD
“I’d like to take a moment to express gratitude for Laura and the work done to expand access to VAD care both inside the walls of Duke University Hospital and across the state. Laura has taught thousands of patients, families and healthcare team members how to safely care for VADs so patients can receive care both here at DUH and in the community.” – Stephanie G. Barnes, MSN, Clinical Director for Advanced Heart Failure Services
“Dr. Laura Blue is an icon in the mechanical circulatory support specialty at Duke and across the country. Her knowledge and experience are unmatched. Laura has partnered to support numerous trials and new devices to literally change and shape this technology over the years. She is always an advocate for the patients and their loved ones and has been a pivotal team member in the development and success of the Duke Mechanical Circulatory Support program. We are fortunate to have Laura on the Duke Heart team!” – Jill Engel, DNP, Associate Vice President for Duke Heart Services
Kudos to Hoke!
Anna Lisa Chamis shared a terrific note she received this week from Melissa Daubert regarding cardiology fellow Cara Hoke:
“Thank you for the terrific work and long hours you put in today! You handled a very full TEE board and many other requests today with aplomb. We had some great cases, and your reports were terrific with descriptive and quantitative detail. Your thoughtfulness is truly appreciated. It has been a pleasure to work with you!”
Way to go, Cara!
Shout-out to the DUH Cath Lab team!
A big shout-out to the Duke University Hospital cardiac catheterization lab team – a note from Jenn Rymer sent to Anna Mall stated:
“I had an ICU patient pending discharge on June 24 (but needed cath before discharge). JP and several others stayed to help get the patient a diagnostic cath with Dr. Othman so the patient could go home. I really appreciate the willingness to do what is right for the patient so that he could get home that weekend.”
Shown here are cath lab team members (L-R): Miranda Olson, Nicole Mee, Gloria Gonde, JP Maarschalk, and Jen Lutz.

Great patient-centered teamwork! Thanks, everyone!
Thompson Receives ‘High 5’
Cardiology nurse practitioner Shelley Thompson recently earned a ‘High Five’ as part of the DUHS peer recognition program. She was nominated by Richa Agarwal, who said in the nomination:
”Shelley is a fierce patient advocate and provided amazing support to a patient and their spouse during a very difficult time.”
Congrats, Shelley!

Photos of the Week
Pamela Douglas and Tracy Wang along with Minnow Walsh of St. Vincent Health, chair the ACC’s Clinical Trial Research (CRT) Program, the three are shown here with other members of the faculty from across the U.S. The team aims to further develop the skill sets of cardiologists and PhD researchers seeking to succeed in clinical research. Their 2022 cohort was held recently. Well done!

Jack Haney celebrated the start of the training year with new chief residents for Duke cardiovascular and thoracic surgery (L-R): Julie Doberne, James Meza, Haney, Jessica Hudson and Mike Mulvihill.

Cardiology fellow Balim Senman styling one of her fabulous blazers with “Balim’s Blazer Boys” (Joshua Neal and Derek Woodruff, PGY-1s, Duke internal medicine). In a post to Twitter, Senman stated: “Congratulations to these two phenomenal interns for absolutely KILLING it in their first week of intern year!!” Way to go!

And this great pic, courtesy of Jenn Rymer, of our incoming first year cardiology fellows after their procedural bootcamp. Here they are again, enjoying an evening out at Bull McCabe’s in downtown Durham. Looking good everyone — we are so glad you’re here!


A Dose of Inspiration
Who doesn’t need a little inspiration from time to time? Here are two items we came across last week that are worth checking out:
Handle Hard Better with Kara Lawson of Duke Women’s Basketball
https://www.youtube.com/watch?v=oDzfZOfNki4
The Washington Post
Their dad was drowning. They saved him using CPR they saw in movie scenes. Washington Post article: https://duke.is/yehz8
Enjoy the coming week!
COVID-19 Update
All the latest Clinical Operations updates related to COVID can be found at https://covid-19.dukehealth.org. Patient-facing resources on DukeHealth.org can be found here: https://www.dukehealth.org/covid-19-update/resources. Duke University maintains a resource page as well, which can be accessed here: https://coronavirus.duke.edu/updates/for-staff.
Upcoming Events & Opportunities
July 26: Women in Cardiology. The WIC team postponed their event originally planned for June 30. Details will be announced soon. For more information, please contact cardiology fellow Karen Flores Rosario, MD.
August 17: Duke GME DEI ‘First Look’. The Duke Office of Graduate Medical Education is holding a virtual DEI ‘First Look’ event for potential incoming residents and fellows. It’s specifically designed for underrepresented applicants and any applicant interested in DEI issues. Registration is required.
Cardiology Grand Rounds
Cardiology Grand Rounds has concluded and will resume in September.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
June 21 — Harry Severance
EP Monthly
Should You Stay or Should You Go?
https://duke.is/v3xqx
July 1 — Allan Kirk
DailyMail.com
https://duke.is/9emtm
July 6 — William Kraus
eatthis.com
Everyday Habits That Make You Live Longer, Say Experts
https://duke.is/gwh9f
July 6 — Michael Pencina
tctMD
Few Adults Eligible for Primary Prevention With Statins in Latest ESC Guidelines
https://duke.is/7mgn6
July 6 — Jonathan Piccini
HRtv
HRtv Update: Residual Leaks Post Left Atrial Appendage Occlusion
https://duke.is/mvwjf
Division of Cardiology Publications Indexed in PubMed June 30 – July 6, 2022
Aulin J, Hijazi Z, Lindbäck J, Alexander JH, Gersh BJ, Granger CB, Hanna M, Horowitz J, Lopes RD, McMurray JJV, Oldgren J, Siegbahn A, Wallentin L. Biomarkers and heart failure events in patients with atrial fibrillation in the ARISTOTLE trial evaluated by a multi-state model. Am Heart J 2022 Sep;251:13-24. PM: 35569564.
Blumenthal JA, Smith PJ, Jiang W, Hinderliter A, Watkins LL, Hoffman BM, Kraus WE, Mabe S, Liao L, Davidson J, Sherwood A. Longer term benefits of exercise and escitalopram in the treatment of anxiety in patients with coronary heart disease: Six month follow-up of the UNWIND randomized clinical trial. Am Heart J 2022 Sep;251:91-100. PM: 35609671.
Cantor WJ, Tan M, Berwanger O, Lavi S, White HD, Nicolau JC, Dehghani P, Tajer CD, Lopes RD, Moia DDF, Nicholls SJ, Parkhomenko A, Averkov O, Brass N, Lutchmedial S, Malaga G, Damiani LP, Piegas LS, Granger CB, Goodman SG. Morphine and clinical outcomes in patients with ST segment elevation myocardial infarction treated with fibrinolytic and antiplatelet therapy: Insights from the TREAT trial. Am Heart J 2022 Sep;251:1-12. PM: 35533724.
DeVore AD, Bosworth HB, Granger BB. Improving implementation of evidence-based therapies for heart failure. Clin Cardiol 2022 Jun;45 Suppl 1:S52-S59. PM: 35789019.
Florido R, Daya NR, Ndumele CE, Koton S, Russell SD, Prizment A, Blumenthal RS, Matsushita K, Mok Y, Felix AS, Coresh J, Joshu CE, Platz EA, Selvin E. Cardiovascular Disease Risk Among Cancer Survivors: The Atherosclerosis Risk In Communities (ARIC) Study. J Am Coll Cardiol 2022 Jul 5;80(1):22-32. PM: 35772913.
Greene SJ, Lautsch D, Gaggin HK, Djatche LM, Zhou M, Song Y, Signorovitch J, Stevenson AS, Blaustein RO, Butler J. Contemporary outpatient management of patients with worsening heart failure with reduced ejection fraction: Rationale and design of the CHART-HF study. Am Heart J 2022 Sep;251:127-136. PM: 35640728.
Johnson JN, Loriaux DB, Jenista E, Kim HW, Baritussio A, De Garate Iparraguirre E, Bucciarelli-Ducci C, Denny V, O’Connor B, Siddiqui S, Fujikura K, Benton CW, Weinsaft JW, Kochav J, Kim J, Madamanchi C, Steigner M, Kwong R, Chango-Azanza D, Chapa M, et al. Society for Cardiovascular Magnetic Resonance 2021 cases of SCMR and COVID-19 case collection series. J Cardiovasc Magn Reson 2022 Jul 4;24(1):42. PM: 35787291.
Kir D, Zhang S, Kaltenbach LA, Fonarow GC, Matsouaka RA, Piccini JP, Desai NR. Patterns of care for first-detected atrial fibrillation: Insights from the Get With The Guidelines® – Atrial Fibrillation registry. Heart Rhythm 2022 Jul;19(7):1049-1057. PM: 35247626.
Lunardi M, Louvard Y, Lefèvre T, Stankovic G, Burzotta F, Kassab GS, Lassen JF, Darremont O, Garg S, Koo BK, Holm NR, Johnson TW, Pan M, Chatzizisis YS, Banning A, Chieffo A, Dudek D, Hildick-Smith D, Garot J, Henry TD, Dangas G, Stone GW, Krucoff MW, et al. Definitions and Standardized Endpoints for Treatment of Coronary Bifurcations. J Am Coll Cardiol 2022 Jul 5;80(1):63-88. PM: 35597684.
Maia IS, Marcadenti A, Zampieri FG, Damiani LP, Santos RHN, Negrelli KL, Gomes SPDC, Gomes JO, Carollo MBDS, Miranda TA, Santucci E, Valeis N, Laranjeira LN, Westphal GA, Horta JGA, Flato UAP, Fernandes C, Barros WC, Bolan RS, Gebara OCE, Alencar Filho MS. Antivirals for adult patients hospitalized with SARS-CoV-2 infection: A randomized, Phase II/III, multicenter, placebo-controlled, adaptive study, with multiple arms and stages. COALITION COVID-19 BRAZIL IX – REVOLUTIOn: protocol and statistical analysis. Rev Bras Ter Intensiva Jan-Mar 2022;34(1):44-55. PM: 35766657.
Park DY, Wang P, An S, Grimshaw AA, Frampton J, Ohman EM, Rao SV, Nanna MG. Shortening the duration of dual antiplatelet therapy after percutaneous coronary intervention for acute coronary syndrome: A systematic review and meta-analysis. Am Heart J 2022 Sep;251:101-114. PM: 35654162.
Pierce JB, Mentz RJ, Sun JL, Alhanti B, Whellan DJ, Kraus WE, Piña IL, Fiuzat M, O’Connor CM, Greene SJ. Titration of medical therapy and clinical outcomes among patients with heart failure with reduced ejection fraction: Findings from the HF-ACTION trial. Am Heart J 2022 Sep;251:115-126. PM: 35640729.
Sag AA, Patel P. CT-Guided Cooled Radiofrequency Denervation for Chronic Arthritis Pain of the Hip and Shoulder. Semin Intervent Radiol 2022 Jun 30;39(2):150-156. PM: 35781997.
Ten Lohuis CC, Burke SC, Jannuzzo CJ, Barker NA, Chen EP, Busse LW. Protocol Compliance Guiding Angiotensin II Use in Post Cardiovascular Surgery Vasoplegia. Crit Care Explor 2022 May 13;4(5):e0687. PM: 35783549.
Vader JM, Givertz MM, Starling RC, McNulty SE, Anstrom KJ, Desvigne-Nickens P, Hernandez AF, Braunwald E, Mann DL. Tolerability of Sacubitril/Valsartan in Patients With Advanced Heart Failure: Analysis of the LIFE Trial Run-In. JACC Heart Fail 2022 Jul;10(7):449-456. PM: 35772853.
Duke Heart Pulse – July 3rd 2022
Chief’s message: Happy July 4th
As noted over the last few weeks of the pulse, we welcome in new Cardiology fellows and CT surgery residents this week. We will share their experiences, more about each of the individuals, and our continual work to improve how we deliver cardiovascular care in the upcoming weeks. We also hope you all have some time to celebrate July 4th with Friends and family this weekend.
Highlights of the week:
Mark Leithe, MD, Retires from Duke Health
Mark Leithe, MD, has officially retired from Duke as of June 30. Leith, a cardiologist who did his fellowship training in cardiology at Duke, worked for a number of years at Wake Med — including as chairman of their department of medicine — before rejoining the Duke Heart team in 2010. Leithe has served as chief of Duke Cardiology of Raleigh since that time, as well as director of the Cardiac Catheterization Lab at Duke Raleigh Hospital.
 “It has been a true privilege to begin and end my cardiology career at Duke,” says Leithe. “I began my cardiology fellowship in 1987, with Magnus Ohman, Paul Gurbel, and Bill Parsons. My career path was somewhat unusual in that I left the academic center and worked for 19 years in a very busy interventional cardiology practice prior to returning to Duke Cardiology 12 years ago. Due to this anomalous course, Manesh has described me as ‘a unicorn’.
“It has been a true privilege to begin and end my cardiology career at Duke,” says Leithe. “I began my cardiology fellowship in 1987, with Magnus Ohman, Paul Gurbel, and Bill Parsons. My career path was somewhat unusual in that I left the academic center and worked for 19 years in a very busy interventional cardiology practice prior to returning to Duke Cardiology 12 years ago. Due to this anomalous course, Manesh has described me as ‘a unicorn’.
“While at Wake Med, I frequently held up Duke as the example of excellence in cardiology, which they may not have appreciated,” Leith adds. “Practicing at Duke has enabled me to deliver the best care to my patients due to excellence in specialized services, such as rhythm management, structural heart, and advanced heart failure, to mention just a few. In addition, participation in teaching and in clinical research at Duke have enriched my career immensely.
“I will miss my many patients, some of whom I’ve known for 29 years, and who have become friends. One such patient came to the office this month with a retirement gift for me and told our staff that she has been with me longer than she was with either of her two husbands.
“I will miss my partners at Duke Cardiology of Raleigh, who are collectively the finest group of physicians and people that I know.  Some of my best friends in my life I have met during my time at Duke, and we have shared vacations, holidays and raising families. I plan to step back now and meditate on the things that I will attach the most importance to. I can see that exercising my right brain with art, music and reading will be in my future. I can also see that trips to New Jersey to spend time with our grandchildren will also be a priority.”
Some of my best friends in my life I have met during my time at Duke, and we have shared vacations, holidays and raising families. I plan to step back now and meditate on the things that I will attach the most importance to. I can see that exercising my right brain with art, music and reading will be in my future. I can also see that trips to New Jersey to spend time with our grandchildren will also be a priority.”
Mark’s wife, Linda Leithe, MD, a neuroradiologist at Duke, is planning to cut back her hours over the coming year and then retire next summer. Leithe added that all of his team members have been extremely gracious by holding a number of celebrations in his honor and that he’s been deeply touched by the outpouring.
The physician members of the Duke Cardiology of Raleigh practice and their spouses held a retirement dinner for Mark on Friday, June 10 in the wine cellar of the Angus Barn in Raleigh. The Duke Cardiology of Raleigh team hosted a retirement luncheon on Tuesday, June 28 at their clinic on the Duke Raleigh Hospital Campus — a number of former team members from the past twelve years joined to congratulate Leithe in person, and the Cath team at Duke Raleigh hosted a celebratory dinner on Thursday, June 30.
 We spoke with several Duke Heart team members about Mark’s lasting impact on them. Here is some of what they shared with us:
We spoke with several Duke Heart team members about Mark’s lasting impact on them. Here is some of what they shared with us:
“Mark retiring is a big loss for the Duke Cardiology of Raleigh group and the division of cardiology, but most importantly, it is a loss for our cardiology patients. Mark has been a dedicated clinician and physician leader within our community for decades. His patients adore him, and many of them think of him as family. He makes a major effort to connect with his patients on a personal level that extends beyond the typical patient-physician relationship. The staff in clinic and in the cath lab appreciate his kindness, patience, and level of respect. He is admired by his colleagues, and he has been in invaluable mentor to many of us. Mark is humble and eager to listen and learn from others. Mark has always been dedicated to the mission of lifelong learning and focused on providing the highest level of patient care. This is exemplified by the fact that he regularly attends the Mayo Clinic Board Review, taking time away from his family and personal life, simply to make sure that he stays up to date on the latest cardiovascular care. While I am excited for Mark to enjoy his retirement, he will certainly be missed, as he is irreplaceable.” — Sean Pokorney, MD
“Mark has been an outstanding cardiologist in Wake county for over 30 years. His care for cardiac patients is renowned, but his biggest contribution was to build the Duke Cardiology practice at Duke Raleigh into the premier multi-disciplinary cardiology group in Wake county. Thousands of patients have been touched by Mark’s care. Many of us have occasionally seen his patients in follow-up and you immediately recognize the patient’s great admiration for the care that Mark provided to them. His clinical acumen will be very hard to follow but we wish him the very best in retirement.” — Magnus Ohman, MD
biggest contribution was to build the Duke Cardiology practice at Duke Raleigh into the premier multi-disciplinary cardiology group in Wake county. Thousands of patients have been touched by Mark’s care. Many of us have occasionally seen his patients in follow-up and you immediately recognize the patient’s great admiration for the care that Mark provided to them. His clinical acumen will be very hard to follow but we wish him the very best in retirement.” — Magnus Ohman, MD
“Dr. Leithe has been amazing to work with for the last 12 years. He’s the type of leader that every team wishes for – thoughtful, caring, compassionate, a great listener and available. He leaves Duke Cardiology of Raleigh with a strong team and great leadership in place. I’ll be forever thankful for the opportunity he gave me 12 years ago. He will be greatly missed.”
— Cheri Wills, HCA, Duke Cardiology of Raleigh
 “I will greatly miss Mark as he begins well-deserved retirement. Mark welcomed me to the Raleigh office a few years ago after working with me in the cath lab during my fellowship. As I started there, he made sure it was easy and fun (and busy!) to work with the group at Duke Cardiology of Raleigh. He, along with James Mills, have been a constant source of support as we navigated building this new clinic, and from early on has been enthusiastic about supporting its growth. I have also noticed, countless times, Mark’s dedication to his large panel of patients — many of whom have seen him for decades and always speak glowingly of him. Mark has been a great friend, colleague and leader over the years. I wish him the best in retirement!” — Kishan Parikh, MD
“I will greatly miss Mark as he begins well-deserved retirement. Mark welcomed me to the Raleigh office a few years ago after working with me in the cath lab during my fellowship. As I started there, he made sure it was easy and fun (and busy!) to work with the group at Duke Cardiology of Raleigh. He, along with James Mills, have been a constant source of support as we navigated building this new clinic, and from early on has been enthusiastic about supporting its growth. I have also noticed, countless times, Mark’s dedication to his large panel of patients — many of whom have seen him for decades and always speak glowingly of him. Mark has been a great friend, colleague and leader over the years. I wish him the best in retirement!” — Kishan Parikh, MD
“Mark has done an outstanding job here at Duke Cardiology of Raleigh. He has overseen and facilitated a lot of growth in the  practice and set a really good leadership example for the group. On top of that, as a clinician, he has been a fantastic interventionalist — a very careful and considered cardiologist who always, always made himself available to look at films and talk about cases. I couldn’t have asked for a better colleague. His patients have been very loyal to him and rightly so. He’s personable, deeply caring and just a good guy to have around, not only clinically but for his collegiality and friendship. He has always been a triple-threat, so to speak. He’s skilled in the cath lab, great clinically, and he gets along so beautifully with the team and patients. He’s got high marks in all those areas and we are going to miss him.” — James Peterson, MD
practice and set a really good leadership example for the group. On top of that, as a clinician, he has been a fantastic interventionalist — a very careful and considered cardiologist who always, always made himself available to look at films and talk about cases. I couldn’t have asked for a better colleague. His patients have been very loyal to him and rightly so. He’s personable, deeply caring and just a good guy to have around, not only clinically but for his collegiality and friendship. He has always been a triple-threat, so to speak. He’s skilled in the cath lab, great clinically, and he gets along so beautifully with the team and patients. He’s got high marks in all those areas and we are going to miss him.” — James Peterson, MD
Speaking for James Mills and the whole Duke Raleigh team, and our entire faculty, I can say that Mark will be missed. He represents some of the best of Duke Cardiology and, as noted by many, was the standard bearer for interventional and clinical cardiology in Wake county for more than 30 years. His leadership, focus on clinical care and education, and continual work to drive our practice in a patient-centered way will be lasting legacies.
Duke Stanford Symposium Held
 We were very excited this week for the long-awaited Duke-Stanford Cardiovascular Research Symposium, hosted by Duke. The event took place in the Great Hall of the Mary Duke Biddle Trent Semans Center. This was the third such event held as part of the Duke-Stanford cardiovascular partnership and is jointly organized by teams at Duke and Stanford University. The hybrid symposium, with more than 160 attendees registered to attend virtually and in-person, offered 30 speakers on a wide range of cardiovascular research.
We were very excited this week for the long-awaited Duke-Stanford Cardiovascular Research Symposium, hosted by Duke. The event took place in the Great Hall of the Mary Duke Biddle Trent Semans Center. This was the third such event held as part of the Duke-Stanford cardiovascular partnership and is jointly organized by teams at Duke and Stanford University. The hybrid symposium, with more than 160 attendees registered to attend virtually and in-person, offered 30 speakers on a wide range of cardiovascular research.
“The quality of the science presented this week was excellent,” said Howard Rockman, MD, the Edward S. Orgain Distinguished Professor of Cardiology and director of the CVRC. “The event offered great recognition of the many ties between Duke and Stanford cardiovascular researchers.”
Keynotes included Dr. Deepak Srivastava, president of the Gladstone Institutes and Dr. Chris Newgard of the Duke Molecular  Physiology Institute. Other highlights included an Innovation Panel with Dr. Howard Rockman, director of the Duke CVRC, Dr. Joe Wu, director of the Stanford Cardiovascular Institute, Dr. Victor Dzau, president of the National Academy of Medicine, former chancellor for health affairs at Duke and a CVRC faculty member, and chief of Duke’s division of cardiology, Dr. Manesh Patel, as well as a mentorship session with Dr. Robert Lefkowitz and the CURE students — a group of Duke undergraduates participating in the DCRC’s Cardiovascular Undergraduate Research Experiences (CURE) educational enrichment program which launched this summer.
Physiology Institute. Other highlights included an Innovation Panel with Dr. Howard Rockman, director of the Duke CVRC, Dr. Joe Wu, director of the Stanford Cardiovascular Institute, Dr. Victor Dzau, president of the National Academy of Medicine, former chancellor for health affairs at Duke and a CVRC faculty member, and chief of Duke’s division of cardiology, Dr. Manesh Patel, as well as a mentorship session with Dr. Robert Lefkowitz and the CURE students — a group of Duke undergraduates participating in the DCRC’s Cardiovascular Undergraduate Research Experiences (CURE) educational enrichment program which launched this summer.
“It was terrific to finally hold this symposium,” said Maria Price-Rapoza, PhD, executive director of Duke CVRC. “We appreciate the many colleagues who contributed to make this event a success.”
The Duke Stanford Symposium was supported by a grant from the Edna and Fred L. Mandel Jr. Foundation. Funding for the CURE program is also provided by the Mandel Foundation.


Galbraith Retiring; Heading to Lankenau
Katie Galbraith, president of Duke Regional Hospital, has announced her retirement from this role, which will take effect in mid-August. She will begin a new position as president of Lankenau Medical Center, part of Main Line Health in the Philadelphia area, this fall.
In a message to DUHS leadership this week, Craig Albanese, MD, executive vice president and chief operating officer, thanked her for her many years of service to Duke Health.
“We will sorely miss her and her irreplaceable spirit and leadership here at Duke,” said Albanese. “Let’s all express our enormous gratitude for her more than two decades of achievements that have improved health care access and quality for hundreds of thousands of patients and family members that Duke Health serves each year.”
Galbraith’s remarkable and exemplary 26-year career at Duke Health began as a temporary receptionist. Her talent was recognized early, and soon she was asked to apply her expertise and skills to tell our Duke Health story, progressing through roles in media relations, communications and marketing. She served Duke Children’s Hospital for five years in public relations and development, and, in 2001, accepted a role at Duke Regional Hospital. She made Duke Regional her home, taking on higher and higher scopes of accountability, from marketing and business development to strategic planning to hospital operations, and finally serving as vice president, and then as president in May 2014.
During Galbraith’s tenure as president, Duke Regional Hospital consistently has been recognized for excellence in patient care, including achieving Five Stars from CMS in 2019 and 2020, and Four Stars in 2021 and 2022. The hospital has received the Governor’s Award for Performance Excellence in 2015 and 2016 and has been ranked among the top hospitals in North Carolina by U.S. News & World Report and by Healthgrades America’s 100 Best Hospitals in 2018 and 2019, America’s 250 Best Hospitals 2017, 2018 and 2019, and Patient Safety Excellence Award 2017, 2018 and 2019. Duke Regional Hospital has been recognized as a leader in LGBTQ+ Healthcare Equality by the Human Rights Campaign Foundation since 2013.
Her most enduring legacy may be the 2021 opening of Duke Behavioral Health Center North Durham, a 112,000-square-foot comprehensive center bringing together inpatient, outpatient and emergency behavioral health services in what was the largest construction project in the history of Duke Regional Hospital. Today, the behavioral health center serves patients from throughout the state, meeting an urgent community need for highest quality inpatient and outpatient behavioral health care for both adults and children.
Galbraith credits much of this success to the collaborative spirit and commitment to continuous improvement that characterize teamwork at Duke Regional Hospital and all of Duke Health.
For those of you who have worked with her over the years, you know what a warm, welcoming person she is and that her commitment to Duke has been exceptional. She will be missed. Please join us in congratulating her on an incredible career at Duke Health and wishing her well in her new role.
ICYMI: Year-End Messages from Duke’s DOS, DOM
Duke’s Department of Surgery and Department of Medicine each held their annual “State of the Department” year-end presentations recently. Both events included highlights of work done by the Duke Heart team over the past year and are worth viewing.
Dr. Allan D. Kirk, chair of the Department of Surgery presented his address, Moving Forward Together, on Friday, June 17. To view it, please visit: https://duke.is/46ucr.
Dr. Kathleen Cooney, chair of the Department of Medicine presented her address, Trailblazing Toward Tomorrow, during Medicine Grand Rounds on Friday, June 24. To view it, please visit: https://duke.is/bhhdp.
Congratulations to all Duke Heart team members for the work you did over the past year. Together we are doing great things!
ICYMI: Klotman Reappointed Dean, Duke SOM
Mary E. Klotman, MD, has been reappointed for a second five-year term as dean of the Duke University School of Medicine, vice chancellor for health affairs at Duke University, and chief academic officer for Duke University Health System. Her new term began on July 1, 2022.
Pagidipati at HID2022
Neha Pagidipati, MD, presented on cardiovascular risk factors during pregnancy during the 6th annual Heart in Diabetes (HID) conference held June 24-26 in Philadelphia. Her presentation on this critical topic was very well received.
Way to go, Neha!

Palma Named to CAAHEP Board, Effective July 1
Richard Palma, program director of the Duke Cardiac Ultrasound Certificate Program, has been elected to the Board of  Directors for the Commission on Accreditation of Allied Health Education Programs (CAAHEP); the role is effective as of July 1. Palma will represent the Hospital/VA Educational membership category and his term will run until June 30, 2025.
Directors for the Commission on Accreditation of Allied Health Education Programs (CAAHEP); the role is effective as of July 1. Palma will represent the Hospital/VA Educational membership category and his term will run until June 30, 2025.
Earlier this year, Palma was appointed a commissioner to the CAAHEP, a role he vacates due to his election to the Board of Directors.
Congratulations, Richie!
William Harvey Golf Tourney Results
The U.S. team, including Magnus Ohman, Larry Crawford and Kristin Newby (team captain) from Duke, did their best to bring home the William Harvey Trophy. Heading into the final day of competition during the William Harvey Golf Tournament being held in northern Italy, the US team had a mathematical chance (note the hopeful faces in the team picture, which was taken prior to the final-day matches), but could not overcome history and fell just short in a very respectable second place finish after four days of match play competition: EU 15.5, US 11, Great Britain & Ireland 8.5.
Amazingly, in 11 William Harvey tournaments spanning 20 years of competition, the home team has always won the William Harvey Trophy!! We now look forward to the 2024 tournament which will take place on home soil in the US, giving us the chance to keep this historical streak alive!

COVID-19 Update
All the latest Clinical Operations updates related to COVID can be found at https://covid-19.dukehealth.org. Patient-facing resources on DukeHealth.org can be found here: https://www.dukehealth.org/covid-19-update/resources. Duke University maintains a resource page as well, which can be accessed here: https://coronavirus.duke.edu/updates/for-staff.
Upcoming Events & Opportunities
July 26: Women in Cardiology. The WIC team postponed their event originally planned for June 30. Details will be announced soon. For more information, please contact cardiology fellow Karen Flores Rosario, MD.
Cardiology Grand Rounds
Cardiology Grand Rounds has concluded and will resume in September.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
June 29 — Robert Mentz
Medpage Today
Bye-Bye, ‘Life’s Simple 7’: AHA Redefines Cardiovascular Health by Adding Sleep
https://duke.is/58hb5
June 29 — Stuart Russell
Diagnostic and Interventional Cardiology
https://duke.is/nznsj
(Last two week of Division of Cardiology Publications)
Division of Cardiology Publications Indexed in PubMed June 23-29, 2022
Anjorin AC, Greiner MA, Vemulapalli S, Svetkey L, Southerland KW, Bosworth HB. Underutilization of Guideline-based Abdominal Aortic Aneurysm Screening in an Academic Health System. Ann Vasc Surg 2022 Jul;83:184-194. PM: 34942338.
Baksh SS, Pratt RE, Gomez J, Dzau VJ, Hodgkinson CP. A novel Cbx1, PurB, and Sp3 complex mediates long-term silencing of tissue- and lineage-specific genes. J Biol Chem 2022 Jun;298(6):102053. PM: 35605661.
Davis TME, Giczewska A, Lokhnygina Y, Mentz RJ, Sattar N, Holman RR. Effect of race on cardiometabolic responses to once-weekly exenatide: insights from the Exenatide Study of Cardiovascular Event Lowering (EXSCEL). Cardiovasc Diabetol 2022 Jun 27;21(1):116. PM: 35761271.
Grego S, Welling CM, Miller GH, Coggan PF, Sellgren KL, Hawkins BT, Ginsburg GS, Ruiz JR, Fisher DA, Stoner BR. A hands-free stool sampling system for monitoring intestinal health and disease. Sci Rep 2022 Jun 27;12(1):10859. PM: 35760855.
Hess CN, Szarek M, Anand SS, Bauersachs RM, Patel MR, Debus ES, Nehler MR, Capell WH, Beckman JA, Piazza G, Henkin S, Bura-Rivière A, Lawall H, Roztocil K, Hsia J, Muehlhofer E, Berkowitz SD, Haskell LP, Bonaca MP. Rivaroxaban and Risk of Venous Thromboembolism in Patients With Symptomatic Peripheral Artery Disease After Lower Extremity Revascularization. JAMA Netw Open 2022 Jun 1;5(6):e2215580. PM: 35731517.
Krychtiuk KA, Fordyce CB, Hansen CM, Hassager C, Jentzer JC, Menon V, Perman SM, van Diepen S, Granger CB. Targeted temperature management after out of hospital cardiac arrest: quo vadis? Eur Heart J Acute Cardiovasc Care 2022 Jun 22;11(6):512-521. PM: 35579006.
Minhas AS, Goldstein SA, Vaught AJ, Lewey J, Ward C, Schulman SP, Michos ED. Instituting a Curriculum for Cardio-Obstetrics Subspecialty Fellowship Training. Methodist Debakey Cardiovasc J 2022 Jun 3;18(3):14-23. PM: 35734150.
Napp LC, Westenfeld R, Møller JE, Pappalardo F, Ibrahim K, Bonello L, Wilkins C, Pershad A, Mannino SF, Schreiber TL, Hall PA, Medjamia AM, Haurand JM, Sieweke JT, Schäfer A, Grines CL, Burkhoff D, Moses JW, Ohman EM, O’Neill WW, Kapur NK, Bauersachs J. Impella Mechanical Circulatory Support for Takotsubo Syndrome With Shock: A Retrospective Multicenter Analysis. Cardiovasc Revasc Med 2022 Jul;40:113-119. PM: 34916157.
Overton ET, Weir IR, Zanni MV, Fischinger S, MacArthur RD, Aberg JA, Fitch KV, Frank M, Albrecht H, Goodenough E, Rhame FS, Fichtenbaum CJ, Bloomfield GS, Malvestutto C, Supparatpinyo K, McCallum S, Douglas PS, Alter G, Ribaudo H, Grinspoon SK. Asymptomatic SARS-CoV-2 Infection Is Common Among ART-Treated People With HIV. J Acquir Immune Defic Syndr 2022 Aug 1;90(4):377-381. PM: 35413022.
Schmitz LL, Zhao W, Ratliff SM, Goodwin J, Miao J, Lu Q, Guo X, Taylor KD, Ding J, Liu Y, Levine M, Smith JA. The Socioeconomic Gradient in Epigenetic Ageing Clocks: Evidence from the Multi-Ethnic Study of Atherosclerosis and the Health and Retirement Study. Epigenetics 2022 Jun;17(6):589-611. PM: 34227900.
Smith PJ, Sherwood A, Hinderliter AL, Mabe S, Watkins LL, Craighead L, Ingle K, Tyson C, Avorgbedor F, Lin PH, Kraus WE, Liao L, Blumenthal JA. Lifestyle modification and cognitive function among individuals with resistant hypertension: cognitive outcomes from the TRIUMPH trial. J Hypertens 2022 Jul 1;40(7):1359-1368. PM: 35703293.
Song A, Lusk JB, Roh KM, Jackson KJ, Scherr KA, McNabb RP, Chatterjee R, Kuo AN. Practice Patterns of Fundoscopic Examination for Diabetic Retinopathy Screening in Primary Care. JAMA Netw Open 2022 Jun 1;5(6):e2218753. PM: 35759262.
Wilson NA, Tcheng JE, Graham J, Drozda JP. Advancing Patient Safety Surrounding Medical Devices: Barriers, Strategies, and Next Steps in Health System Implementation of Unique Device Identifiers. Med Devices (Auckl) 2022 Jun 21;15:177-186. PM: 35761948.
Younis A, Goldenberg I, Farooq S, Yavin H, Daubert J, Raitt M, Mazur A, Huang DT, Mitchell BL, Rashtian MR, Winters S, Vloka M, Aktas M, Bernabei MA, Beck CA, McNitt S, Zareba W. Reduction in Ventricular Tachyarrhythmia Burden in Patients Enrolled in the RAID Trial. JACC Clin Electrophysiol 2022 Jun;8(6):754-762. PM: 35738852.
Division of Cardiology Publications Indexed in PubMed June 16-22, 2022
Angraal S, Hejjaji V, Tang Y, Gosch KL, Patel MR, Heyligers J, White CJ, Tutein Nolthenius R, Mena-Hurtado C, Aronow HD, Moneta GL, Fitridge R, Soukas PA, Abbott JD, Secemsky EA, Spertus JA, Smolderen KG. One-Year Health Status Outcomes Following Early Invasive and Noninvasive Treatment in Symptomatic Peripheral Artery Disease. Circ Cardiovasc Interv 2022 Jun;15(6):e011506. PM: 35579010.
Butler J, Stebbins A, Melenovský V, Sweitzer NK, Cowie MR, Stehlik J, Khan MS, Blaustein RO, Ezekowitz JA, Hernandez AF, Lam CSP, Nkulikiyinka R, O’Connor CM, Pieske BM, Ponikowski P, Spertus JA, Voors AA, Anstrom KJ, Armstrong PW. Vericiguat and Health-Related Quality of Life in Patients With Heart Failure With Reduced Ejection Fraction: Insights From the VICTORIA Trial. Circ Heart Fail 2022 Jun;15(6):e009337. PM: 35656822/
de Barros E Silva PGM, Macedo TA, Lopes RD, Okada MY, Frigini T, Roveri PO, Balada R, de Macedo LS, Furlan V. Chest Pain Network with Support of Telemedicine: Impact on Reperfusion Therapy and Clinical Outcomes After 8 Years of Experience. Telemed Rep 2021 Dec 22;2(1):284-292. PM: 35720760.
Haddad F, Ataam JA, Amsallem M, Cauwenberghs N, Kuznetsova T, Rosenberg-Hasson Y, Zamanian RT, Karakikes I, Horne BD, Muhlestein JB, Kwee L, Shah S, Maecker H, Knight S, Knowlton K. Insulin Growth Factor Phenotypes in Heart Failure With Preserved Ejection Fraction, an INSPIRE Registry and CATHGEN Study. J Card Fail 2022 Jun;28(6):935-946. PM: 34979242.
Hess CN, Baumgartner I, Anand SS, Nehler MR, Patel MR, Debus ES, Szarek M, Capell W, Muehlhofer E, Berkowitz SD, Haskell LP, Bauersachs RM, Bonaca MP, Hsia J. Sex-Based Differences in Outcomes Following Peripheral Artery Revascularization: Insights From VOYAGER PAD. J Am Heart Assoc 2022 Jun 21;11(12):e024655. PM: 35699170.
Johansen KL, Acharya A, Cizman B, Cobitz AR, Correa-Rotter R, Dasgupta I, Kher V, Lopes RD, Matsumoto L, Meadowcroft AM, Merege Vieira Neto O, Okabe M, Rayner B, Silva A, Thomas H, Singh AK. Challenges of Conducting Clinical Trials during the SARS-CoV-2 Pandemic: The ASCEND Global Program Experience. Kidney360 2022 Feb 10;3(4):728-733. PM: 35721625.
Kamat I, Hajduczok AG, Salah H, Lurz P, Sobotka PA, Fudim M. Catheter-Based Management of Heart Failure: Pathophysiology and Contemporary Data. Interv Cardiol Clin 2022 Jul;11(3):267-277. PM: 35710282.
Kolb P, Kenakin T, Alexander SPH, Bermudez M, Bohn LM, Breinholt CS, Bouvier M, Hill SJ, Kostenis E, Martemyanov KA, Neubig RR, Onaran HO, Rajagopal S, Roth BL, Selent J, Shukla AK, Sommer ME, Gloriam DE. Community guidelines for GPCR ligand bias: IUPHAR review 32. Br J Pharmacol 2022 Jul;179(14):3651-3674. PM: 35106752.
Lala A, Mentz RJ. Advancing Our Common Purpose Through “Coopetition”. J Card Fail 2022 Jun;28(6):881-882. PM: 35715020.
Lopes RD, Guimarães PO, Schwartz GG, Bhatt DL, Bittner VA, Budaj A, Dalby AJ, Diaz R, Goodman SG, Harrington RA, Jukema JW, Kiss RG, Loy M, Pordy R, Poulouin Y, Szarek M, White HD, Steg PG. Effect of Alirocumab on Incidence of Atrial Fibrillation After Acute Coronary Syndromes: Insights from the ODYSSEY OUTCOMES Trial. Am J Med 2022 Jul;135(7):915-918. PM: 35296402.
Mastoris I, Spall HGCV, Sheldon SH, Pimentel RC, Steinkamp L, Shah Z, Al-Khatib SM, Singh JP, Sauer AJ. Emerging Implantable-Device Technology for Patients at the Intersection of Electrophysiology and Heart Failure Interdisciplinary Care. J Card Fail 2022 Jun;28(6):991-1015. PM: 34774748.
Shah A, Mentz RJ, Sun JL, Rao VN, Alhanti B, Blumer V, Starling R, Butler J, Greene SJ. Emergency Department Visits Versus Hospital Readmissions Among Patients Hospitalized for Heart Failure. J Card Fail 2022 Jun;28(6):916-923. PM: 34987009.
Sheikh AB, Fudim M, Garg I, Minhas AMK, Sobotka AA, Patel MR, Eng MH, Sobotka PA. The Clinical Problem of Pelvic Venous Disorders. Interv Cardiol Clin 2022 Jul;11(3):307-324. PM: 35710285.
Duke Heart Pulse: Week ending June 26th 2022
Highlights of the week:
Welcome New Cardiology Fellows; New CT Surgery Resident!
We are excited to welcome our new first-year cardiology fellows and a new resident for the cardiovascular and thoracic surgery I-6 training program this week. We are thrilled to have them join us! Please give a warm welcome to:
Cardiology Fellows:
Andrew Andreae, MD, completed residency at Duke; a graduate of Virginia Commonwealth University School of Medicine.

Michael Cosiano, MD, completed residency at Duke; a graduate of Weill Cornell Medicine.

David Elliott, MD, completed residency at Duke; a graduate of Duke University School of Medicine

Nathan Goodwin, MD, completed residency at Duke; a graduate of the University of Missouri School of Medicine

Aman Kansal, MD, completed residency at Duke; a graduate of Duke University School of Medicine.
 Allie Levin, MD, completed residency at Massachusetts General Hospital; a graduate of Columbia University Vagelos College of Physicians and Surgeons.
Allie Levin, MD, completed residency at Massachusetts General Hospital; a graduate of Columbia University Vagelos College of Physicians and Surgeons.
Anthony Lin, MD, completed residency at the University of California at San Francisco; a graduate of Duke University School of Medicine.

Paula Rambarat, MD, completed residency with Massachusetts General Hospital; a graduate of Columbia University Vagelos College of Physicians and Surgeons.

Jessica Regan, MD, completed residency at Duke; a graduate of Virginia Commonwealth University School of Medicine.

Belal Suleiman, MD, completed residency at University of Texas Southwestern; a graduate of the University of Kentucky College of Medicine.
Cardiovascular & Thoracic Surgery resident:
Rebekah Boyd, MD, joins us from Columbia University Vagelos College of Physicians and Surgeons.

Rymer Named John Bush Simpson Assistant Professor of Medicine
Jennifer Rymer, MD, has been named the John Bush Simpson Assistant Professor of Medicine.
Rymer joined the Duke Cardiology faculty in July, 2020 as an interventional cardiologist. She was a fellow in cardiovascular medicine at Duke from 2014 to 2019 and did her internal medicine residency here from 2011 to 2014 following her graduation from Vanderbilt University School of Medicine.

Rymer has 70 publications to her credit and serves on leadership and publication committees for the American Heart Association, the American College of Cardiology, the Society for Vascular Medicine and the Society for Cardiovascular Angiography and Interventions. She is also the recipient of the Walter Floyd Award for Excellence in Clinical Cardiology, the DCRI Harrington Research Award for Excellence in Clinical Research, the Women as One Research Award, the William Keating Career Development Award from the American College of Cardiology, and a Career Development Award from the American Heart Association.
The work she did during fellowship, particularly on the Inclusion and Diversity Task Force, led Rymer to devote some of her time to increasing the representation of representation in the field of cardiology. She was recently named the trainee liaison for the Department of Medicine’s Program for Women in Internal Medicine (PWIM) where she has helped create and facilitate programs tailored to the needs of women trainees.
She hopes to demonstrate, through her work with PWIM and elsewhere, that a career in cardiology is a fulfilling and rewarding choice for women. Rymer is also member in the Duke Clinical Research Institute.
Congratulations, Jenn!
EP Fellows Celebrated at Year-End Dinner
Our graduating EP fellows were celebrated last weekend (Saturday, June 18) at The Roof restaurant on top of the Durham Hotel, which is an annual tradition for the EP section. A shout-out to Don Hegland, MD, EP Program Director, who continues to lead an outstanding fellowship program! Great work!
“Words cannot express how special these graduates are,” said Jon Piccini, MD, director of the electrophysiology section. “They are among the best fellows we have ever graduated from our program.”
Graduating fellows:
Adam Barnett, MD, is joining Prisma Health in Greenville, SC.
Eric Black-Maier, MD is joining Maine Medical Center in Portland, ME.
Zak Loring, MD, is joining the EP faculty here at Duke.
Mike Rehorn, MD, is joining Virginia Cardiovascular Specialists in Richmond, VA.
Shown in photos are:
Graduating fellows, L-R: Barnett, Black-Maier, Rehorn and Loring.
Graduating fellows with EP faculty.
Graduating fellows with their spouses and faculty.
Congratulations to all!



Latest AHA GWTG HF, CAD Awards for Duke Hospital Announced
We are pleased to announce the latest American Heart Association Get With The Guidelines (GWTG) Awards for Duke University Hospital, announced earlier this week. We have achieved the following:
GWTG Heart Failure Award — Gold Plus with Heart Failure Honor Roll and Type 2 Diabetes Honor Roll.
This is the highest recognition level by the American Heart Association.
GWTG Coronary Artery Disease (CAD) — Mission: Lifeline Award: NSTEMI – Gold
GWTG CAD — Mission Lifeline: STEMI Receiving Center — Gold Plus
These achievements are based upon participation in GWTG-CAD and meeting the required Mission: Lifeline recognition criteria for data submitted through the 2021 calendar year. This accomplishment signifies a commitment to guideline adherence and quality improvement, not only on behalf of Duke University Hospital but for the entire STEMI System of Care.
Excellent teamwork!!! Congratulations to all!
Duke Heart at AAHFN 2022
Duke Heart was well represented at the American Association of Heart Failure Nurses (AAHFN) 18th annual meeting held June 15-18, 2022 in Orlando, Florida. Stephanie Barnes served as the Planning Chair for the meeting. Shelley Thompson, Robert Mentz, Marat Fudim and Joey Harrington were speakers at the conference. There were also many past Duke nurses and physicians who were speakers and in attendance.
We have it on great authority that planning committee chair Stephanie Barnes did an absolutely fantastic job.
“The conference was a wonderful opportunity to learn and network and the quality of presentations was outstanding,” said Shelley Thompson, a conference speaker and nurse practitioner with the Duke Heart Failure team.
Rob Mentz concurred, “The AAHFN meeting, that Steph helped lead, was a tremendous success. I had never been to the meeting before and was truly impressed by the engagement, high quality talks, and phenomenal community the society has built.”
Great work, Stephanie! Congratulations to all presenters!


Tcheng: Patient Safety Surrounding Medical Devices
Congrats to Jimmy Tcheng, MD and team. Their latest research article, Advancing Patient Safety Surrounding Medical Devices: Barriers, Strategies, and Next Steps in Health System Implementation of Unique Device Identifiers, was published this week in the journal Medical Devices: Evidence and Research. To check it out, visit: https://doi.org/10.2147/MDER.S364539

Harrington Article to be Featured by ACC.org
Congratulations to cardiology fellow Josephine Harrington, MD — her recently published expert analysis piece (co-authored with  Manesh Patel, MD), The Next Wave of Anticoagulation: Results of PACIFIC-AF and the Future Role of Factor XIa Inhibition in Atrial Fibrillation, which appears on ACC.org, was selected by Dr. Kim Eagle, Editor-in-Chief of ACC.org, to appear as a featured item on the ACC.org homepage. Starting on Tuesday, June 28 and running through the weekend, the article will be one of the three images cycling across the top of www.acc.org.
Manesh Patel, MD), The Next Wave of Anticoagulation: Results of PACIFIC-AF and the Future Role of Factor XIa Inhibition in Atrial Fibrillation, which appears on ACC.org, was selected by Dr. Kim Eagle, Editor-in-Chief of ACC.org, to appear as a featured item on the ACC.org homepage. Starting on Tuesday, June 28 and running through the weekend, the article will be one of the three images cycling across the top of www.acc.org.
Well done!
Ohman, Newby Participating in International Golf Tournament
Magnus Ohman and Kristin Newby participated in the William Harvey Golf Tournament held this past week in Europe. The tournament, according to Ohman, was developed by Drs. Will Fennel (Ireland), Peter Sleight (UK), and Tom Ryan, Sr. (US) in 1999 to foster international academic camaraderie. Teams from Great Britain, Ireland, the EU, and the US compete for a trophy over 4 days in a Ryder Cup style format. Dr. Kristin Newby is leading the US team as captain at Lake Garda, Italy. The team includes past presidents from ACC and AHA and “will do their best to take home the trophy among stiff competition from similar leaders on the European continent,” Ohman added.
We look forward to learning the results!!

Duke Health’s Commitment to Addressing Workplace Violence
At Duke Health, the safety and security of our patients and team members are our highest priorities. With recent violent incidents in health care settings and elsewhere, we have redoubled efforts to provide a safe environment at our facilities. Among additional and expanded security measures, we are:
- Evaluating and optimizing security presence at key hospital and clinic locations
- Providing additional emergency alert resources and support to care teams, notably those tending patients with behavioral health concerns
- Reviewing and revising the policies, procedures and training requirements for the management of security-related events
- Making fewer entrances accessible to visitors
All entities of Duke Health are gun-free zones for patients, visitors, students, providers and staff. We are continuing to evaluate and implement additional measures that foster an environment of wellbeing and health.
Remain Vigilant with Spam, Cybersecurity Concerns
There has been a recent uptick in patients and team members receiving health-related scam phone calls. If an employee or a patient room receives a scam call, please report the number that that received the call and the number that made the call to the Duke Health Service Desk at 919-684-2243 immediately.
Reminder: Exterior Doors
As part of this overall effort, it is critical to keep exterior doors closed. Allowing them to be propped open presents a security risk to our patients and our team members. Please do not prop exterior doors. Thank you!
COVID-19 Update
All the latest Clinical Operations updates related to COVID can be found at https://covid-19.dukehealth.org. Patient-facing resources on DukeHealth.org can be found here: https://www.dukehealth.org/covid-19-update/resources. Duke University maintains a resource page as well, which can be accessed here: https://coronavirus.duke.edu/updates/for-staff.
Upcoming Events & Opportunities
Duke-Stanford Cardiovascular Research Symposium
June 27 & 28. The Duke-Stanford Cardiovascular Research Symposium returns to Durham this year and is offered as a hybrid event. This symposium is sponsored by the Edna and Fred L. Mandel, Jr. Foundation.
Registration required. In person: Great Hall, Mary Duke Biddle Trent Semans Center, Durham, NC. For those who wish to attend virtually, the event will offer live-streaming. The link will be emailed prior to the program. Registrants who choose the virtual live-streamed webinar option will be able to obtain CE credit for the course. For more information, contact Christy Darnell.
June 28: The Changing Landscape and Economics of Perfusion Technology. 2-3 p.m. Virtual. Part of The Alliance Conversation Series offered by The Organ Donation and Transplantation Alliance (The Alliance). Wendy Swafford, Sarah Casalinova & Amber Johnson of Duke will join Jeff Orlowski, LifeShare of Oklahoma as presenting speakers. Kevin Myer of LifeGift will serve as moderator. Registration is required. The event is free. Event is geared toward transplant center, OPO, QI professionals and leadership.
June 30: Women in Cardiology. Arrive by 6:30 p.m. The WIC team has announced their next meeting will be at the home of Dr. Pamela Douglas. The theme of the event will be ‘Mentorship and Sponsorship’ with panelists Dr. Douglas, Dr. Jenn Rymer, Dr. Tracy Wang, and Dr. Camille Frazier-Mills. We are lucky to have such a group of incredibly accomplished women and we can’t wait to hear about their mentorship and sponsorship experiences and advice. Dinner will be provided. For more details, please contact cardiology fellow Karen Flores Rosario, MD.
Cardiology Grand Rounds
Cardiology Grand Rounds has concluded and will resume in September.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
June 21 — Peter Ubel (internal medicine)
MediQuality
Jury still out on vitamin, mineral supplements to prevent heart disease, cancer
https://duke.is/4cnp8
June 22 — Carol Krucoff (Duke Health & Wellness)
Yoga Journal
Ask the Teacher: Can I Practice Yoga with a Pacemaker?
https://duke.is/9rhyz
June 23 — Adrian Hernandez
Newsobserver.com
Coronavirus updates for June 23: Here’s what to know in North Carolina this week
https://duke.is/jksjr
June 23 — Jonathan Piccini
Courier-Gazette (Camden, ME)
Pen Bay Medical Center receives achievement award
https://duke.is/yqr29
June 23 — Richard Shannon and Beverly Gray (ob/gyn)
Full Frontal with Samantha Bee
https://duke.is/vgghp
June 23 — Karen Alexander
Salisbury Post
Clinical research programs aim to improve lives, recruit local participants at NCRC
https://duke.is/z5msh
Duke Heart – Week Ending June 19th 2022
Chief’s message: Remembering, celebrating, and working to improve our future.
Happy Father’s day to all the dads and dad-figures throughout our team and in each of our lives.
This year, the holiday happens to coincide with Juneteenth, providing an opportunity to reflect how we can be better. In his all-staff letter, Vincent E. Price, president of Duke University wrote, “As we mark Juneteenth, we are reminded that racial equity and justice are not end goals to be reached or achieved—they are ongoing institutional and personal principles that must guide all that we do as a university.” In a message to all DUHS team members, Dr. A. Eugene Washington, chancellor for health affairs at Duke, wrote, “At Duke Health, we honor the full spectrum of diversity, and we value the richness that our differences bring to us. We have pledged that equity is our goal, inclusion is our practice, and belonging is the desired result. This is how we build upon the gifts that each of us brings to our mission of advancing health together.”
Like a lot of academic programs, this week also marked our end of year celebrations for graduating fellows and residents. We were reminded about the amazing accomplishments of our fellows, the efforts of our wonderful faculty to teach, and the ability to recognize truly outstanding contributions. We hope each of you has an opportunity to reflect upon year-end and to celebrate not only our dads and our graduates, but our individual and collective blessings.
Highlights of the week:
Duke Heart Celebrates Year-End Graduates
Each of our fellowship and residency training programs celebrated their graduating trainees this week. We are pleased to share updates and photos with you. Congratulations to each of our graduates and a big shout-out to all of our program directors and associate directors: Anna Lisa Chamis; Camille Frazier-Mills; Chris Holley; Rob Mentz; Neha Pagidipati; Schuyler Jones; Kevin Harrison; Donald Hegland; Ben Bryner; Betty Tong, and Jack Haney.
The Interventional Cardiology and Structural Fellowship programs held their year-end celebration on Thursday evening at The Roof restaurant on top of the Durham Hotel in downtown Durham. They celebrated four graduates: Zach Wegermann, Sipa Yankey and Kevin Friede from the interventional cardiology fellowship and John D. Serfas from the structural fellowship.

- John D. Serfas, MD, has completed the Structural Heart fellowship and is entering Interventional Cardiology fellowship at Duke.
- Kevin Friede, MD, is joining the faculty at UNC Chapel Hill.
- Zach Wegermann, MD, is entering the Advanced Training in Cardiology fellowship as the Structural Heart fellow at Duke.
- Sipa Yankey, MD, is leaving Duke to enter the Structural Heart Fellowship at UNC Chapel Hill
The annual Gloria and Warren Newman Award, established in honor of Robert H. “Jess” Peter, MD, was presented to Zach Wegermann. Congratulations, Zach!



Our Cardiology Fellowship programs held their year-end appreciation event on Friday, June 17, at the Washington Duke Inn.
They celebrated the following graduates:

From the Cardiovascular Disease Fellowship:
- Amanda Coniglio, MD, our outgoing chief fellow, is joining the advanced heart failure faculty at Rochester Regional Hospital.
- Jeff Dixson, MD, is going into general invasive cardiology practice with Alaska Heart and Vascular Institute in Anchorage, Alaska.
- Michelle Kelsey, MD, is joining the cardiology faculty at Duke. She will be a part of our prevention team at Duke Heart.
- Vanessa Blumer, MD, is heading to the Cleveland Clinic in Ohio for Advanced Heart Failure and Transplantation fellowship.
- Lauren Truby, MD, is heading to University of Texas Southwestern Medical Center for Advanced Heart Failure and Transplantation fellowship.
From the Adult Congenital Heart Disease Fellowship:
- Sarah Goldstein, MD, has accepted a position with the congenital heart disease team at Yale University.
The following graduates are transitioning to another training program within Duke:
- Kelly Arps, MD, is entering Clinical Cardiac Electrophysiology
- Caitlin Drescher, MD, is entering Interventional Cardiology
- Navid Nafissi, MD, is entering Clinical Cardiac Electrophysiology
- Vishal Rao, MD, is entering the Advanced Heart Failure and Transplant Cardiology
- Toi Spates, MD, is entering the Adult Congenital Heart Disease
- Francis Ugowe, MD, is entering Clinical Cardiac Electrophysiology
The following trainees have completed the Advanced Heart Failure and Transplant Cardiology Fellowship:
- Anthony Carnicelli, MD, has accepted a position with the Medical University of South Carolina, Charleston.
- Marc Samsky, MD, has accepted a position with Yale University.
- Christopher Wrobel, MD, is returning to the Cardiovascular Disease fellowship program for his third year. He will serve as Duke’s chief cardiology fellow for 2022-2023.
Graduating from the Clinical Cardiology Electrophysiology Fellowship are:
- Adam Barnett, MD, is joining Prisma Health in Greenville, SC.
- Eric Black-Maier, MD is joining Maine Medical Center in Portland, ME.
- Zak Loring, MD, is joining the cardiology faculty here at Duke. He will be on the electrophysiology team.
- Mike Rehorn, MD, is joining Virginia Cardiovascular Specialists in Richmond, VA.
The following fellows are transitioning from the Cardiovascular Disease fellowship to Advanced Training in Cardiology: Jessica Duran, Josephine Harrington and Anthony Peters.




As is the custom at year-end, the following annual recognition awards were presented on Friday evening during the Cardiology Fellowship celebration:
Fellow-selected awards
The Outstanding Service Award was presented to Emily Towery. This award is for a hospital staff member who demonstrates dedication and excellence in fellow education.
The Bashore Faculty Teaching Award was presented to Nishant Shah, MD. This award is given to a faculty member demonstrating dedication and excellence in teaching.
The Fellow Mentorship Award was presented to Neha Pagidipati, MD. This award is given to a faculty member demonstrating dedication and excellence in mentoring fellows’ careers.
Faculty-selected awards, which are made possible through the generosity of Duke philanthropic donors:
The Walter F. Floyd Award is a peer-selected award that goes to a fellow demonstrating the most outstanding clinical skills and acumen. This year’s recipient is Willard Applefield, MD.
The Joseph G. Greenfield Award is given to a fellow demonstrating excellence, dedication and contribution to research. This year’s recipient is Vishal Rao, MD, MPH.
The Cassell-Saperstein Award is given to a fellow demonstrating commitment to teaching and a passion for clinical education. This year’s recipient is Michelle Kelsey, MD.
The Brandt and Belinda Louie Award is given to a fellow demonstrating excellence in all three missions of Duke Heart: clinical, education, and research. This year’s recipient is Kelly Arps, MD.
The year-end celebration for our trainees in Cardiovascular and Thoracic Surgery was celebrated as a virtual event on Friday, June 17.
Congratulations to the following:



- Babatunde Yerokun, MD has taken a surgery position at Saint Thomas Hospital for Specialty Surgery in Nashville, TN.
- David Ranney, MD has taken a surgery position at Spectrum Health in Grand Rapids, MI.
- Doug Overbey, MD will remain at Duke as our very first trainee in the new Congenital Cardiac Surgery Fellowship.
As you can see, it was a big week for trainees throughout Duke Heart – congratulations to all of you. Your hard work, commitment and excellence shines and we are so proud of all that you’ve accomplished!
Duke Heart at ASE 2022
Duke Heart was well represented at the American Society of Echocardiography (ASE) Scientific Sessions held June 10-13 in Seattle, WA. Madhav Swaminathan, MD, MBBS, MMCi, FASE, Vice Chair for Faculty Development, Duke Anesthesiology, and Professor of Anesthesiology, Duke University School of Medicine, served as the President of ASE from 2021-2022. By all accounts an amazing year of leadership and well represented the entire field and Duke Heart. Dr. Pamela Douglas was honored during the ASE gala event. A number of our faculty and staff spoke and presented research, including Pamela Douglas, MD; Anita M. Kelsey, MD; Joseph Kisslo, MD; David Adams, ACS; Alicia Armour, ACS; Colin Dunbar II, RDCS; Dallas Gardner, RDCS; Melissa Lefevre, RDCS, and Richard Palma, ACS. Cardiology fellow Manasi Tannu, MD, an ASE Foundation Top Investigator grant winner, also presented (see below “kudos”). Two students from our Cardiac Ultrasound Certificate Program received ASE Foundation student scholarships — Nick Medlock received the Waggoner Award and Daisy Chang received the Katanick Award.




Congratulations to all!
Kudos to Tannu
First-year cardiology fellow Manasi Tannu, MD, who was awarded an American Society of Echocardiography (ASE) Foundation top investigator grant in early May, presented her work at the ASE scientific sessions in Seattle this past weekend. Her presentations included:
- Echocardiography based estimation of pulmonary vascular resistance and outcomes in patients with pulmonary hypertension.
- Prognostic value of right ventricular-pulmonary artery coupling in patients with pulmonary hypertension.
Congratulations to Dr. Tannu and her co-authors!

DUHS AONL Nurse Leaders Advocate on Capitol Hill
Roughly 120 nurse leaders from 33 states – including several from Duke — met last week with state and federal representatives on Capitol Hill in Washington, D.C. to advocate for the American Organization of Nursing Leadership’s (AONL) 2022 legislative priorities. This included national strategies to address the nursing shortage and support legislation that promotes safety from violence for healthcare employees. DUHS nursing leaders (shown in photos) met with the offices of Representative David Rouzer, Representative David Price, Senator Thom Tillis, Senator Richard Burr, and Representative Ted Budd.
Pictured below from left to right are Katrina Green (Administrative Director Clinical Education & Professional Development), Frank Demarco (Associate CNO Emergency Services), and Laura Dickerson (Clinical Operations Director Heart Services)
Great work – and thank you for representing Duke Health and North Carolina!

Duke Heart Grows by One
Congratulations to Emily and Mike Towery on the birth of their son, Amos. The family reported, “After 72 hours of labor, Amos Richard Towery came into the world weighing 7 lbs, 15 oz! We are so in love with him and we are all doing great!”
Emily, a cardiology device nurse, and Mike, a PA, are both members of our cardiology team. We are so excited for them and can’t wait to meet Amos!


Photos of the Week
In a move that surprised us all, Terry Fortin has traded in her flip phone for an iPhone. Congratulations, Terry!

Mike Sketch, Richard Stack, and Chris O’Connor ran into one another as they were out and about town this weekend. They first met in 1988 at Duke. They shared a photo with us – it’s always great to see friends and colleagues!

Duke Children’s Hospital #1 in NC
Duke Children’s Hospital & Health Center continues to rank as the No. 1 children’s hospital in North Carolina by U.S. News & World Report, with nine pediatric specialties ranked among the best in the nation. Duke Children’s also retained a prominent position in the region and nationally – ranking fourth in the southeast and 27th in the nation in the magazine’s annual listing. Duke also received top marks in this year’s list for pediatric cardiology and heart surgery, placing seventh nationally. To read the full news release, please visit: https://duke.is/zphv9. Congratulations to all!

Medicine Grand Rounds Update
The Department of Medicine announced last week that they are moving Medicine Grand Rounds to an 8 a.m. time slot in order to maximize in-person attendance, especially among trainees. The time change from noon to 8 a.m. went into effect on Friday, June 17. MGR will continue to be offered both in-person and virtually. All sessions are recorded and available for viewing on the Duke Medicine Grand Rounds website.
Reminder: Exterior Doors
It is critical to keep exterior doors closed. Allowing them to be propped open presents a security risk to our patients and our team members. Please do not prop exterior doors. Thank you!
COVID-19 Update
All the latest Clinical Operations updates related to COVID can be found at https://covid-19.dukehealth.org. Patient-facing resources on DukeHealth.org can be found here: https://www.dukehealth.org/covid-19-update/resources. Duke University maintains a resource page as well, which can be accessed here: https://coronavirus.duke.edu/updates/for-staff.
Upcoming Events & Opportunities
AHA Aortic Stenosis Webinar features Vemulapalli
June 21: Undertreatment of Aortic Stenosis: A Conversation to Understand the Problem and Consider Solutions. Panelists include Sreekanth Vemulapalli, MD. 6-7 p.m. EDT. This national webinar is part of the American Heart Association’s Target: Aortic Stenosis initiative. For a full list of presenters and panelists or to register (registration is required), please visit: https://bit.ly/3OrktdS.
June 24: Be The Match Registry Drive. 8 a.m. – 3 p.m., Duke University Hospital outside of Atrium Café. If you’re between the ages of 18-35 years old, consider registering as a potential stem cell/bone marrow donor via Be The Match. Help support our cardiology team member and ALL survivor, Dayana Ramos.
Did you know that every three minutes, someone is diagnosed with a blood cancer? You can help be part of their cure. It’s quick and easy — with just a swab kit, it can be determined if your bone marrow or stem cells can save a patient’s life. Come to event to learn more or visit https://bethematch.org. Test kits are available through the registry website.
June 30: Women in Cardiology. Arrive by 6:30 p.m. The WIC team has announced their next meeting will be at the home of Dr. Pamela Douglas. The theme of the event will be ‘Mentorship and Sponsorship’ with panelists Dr. Douglas, Dr. Jenn Rymer, Dr. Tracy Wang, and Dr. Camille Frazier-Mills. We are lucky to have such a group of incredibly accomplished women and we can’t wait to hear about their mentorship and sponsorship experiences and advice. Dinner will be provided. For more details, please contact cardiology fellow Karen Flores Rosario, MD.
Duke-Stanford Cardiovascular Research Symposium
June 27 & 28. The Duke-Stanford Cardiovascular Research Symposium returns to Durham this year and is offered as a hybrid event. This symposium is sponsored by the Edna and Fred L. Mandel, Jr. Foundation.
Registration required. In person: Great Hall, Mary Duke Biddle Trent Semans Center, Durham, NC. For those who wish to attend virtually, the event will offer live-streaming. The link will be emailed prior to the program. Registrants who choose the virtual live-streamed webinar option will be able to obtain CE credit for the course. For more information, contact Christy Darnell.
Cardiology Grand Rounds
Cardiology Grand Rounds has concluded and will resume in September.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
June 11 — Robert Mentz
CBS Mornings/Eye on America (Boston, MA)
Spirituality can improve outcomes for patients with heart failure
https://duke.is/pk2j9
June 12 — Adrian Hernandez
The New York Times
Ivermectin Has Little Effect on Recovery Time From Covid, Study Finds
https://duke.is/rbb7p
June 15 — Adrian Hernandez
Newsobserver.com
Ivermectin does not shorten COVID-19 illness, according to large Duke clinical trial
https://duke.is/yvrcu
June 16 — Christopher Granger
Medpage Today
Out-of-Hospital Cardiac Arrest: Impact on Long-term Survival
https://duke.is/cwnys
June 16 — Sunil Rao
tctMD
Risking COVID-19 for Professional Gain? Spring’s In-Person Meetings in Hindsight
https://duke.is/w5hg3
June 16 — Adrian Hernandez
Axios
Ivermectin doesn’t meaningfully aid COVID-19 recovery, study finds
https://duke.is/jcs27
June 17 — Renato Lopes
World Stock Market/CNN Vital Signs
CNN Vital Signs explains how to avoid thrombosis
Division of Cardiology Publications Indexed in PubMed June 9-15, 2022
Alexander KP. Meaningful Evidence for Anticoagulation in the Gray (Elder) Zone. JAMA Cardiol 2022 Jun 1;7(6):581-582. PM: 35416911.
Del Brutto VJ, Diener HC, Easton JD, Granger CB, Cronin L, Kleine E, Grauer C, Brueckmann M, Toyoda K, Schellinger PD, Lyrer P, Molina CA, Chutinet A, Bladin CF, Estol CJ, Sacco RL. Predictors of Recurrent Stroke After Embolic Stroke of Undetermined Source in the RE-SPECT ESUS Trial. J Am Heart Assoc 2022 Jun 7;11(11):e023545. PM: 35656979.
Don CW, Zwischenberger BA, Kurlansky PA, Rao SV, Sharma G, Lawton JS, Tamis-Holland JE. 2021 ACC/AHA/SCAI Coronary Artery Revascularization Guidelines for Managing the Nonculprit Artery in STEMI. JACC Case Rep 2022 Apr 6;4(7):377-384. PM: 35693904.
Eikelboom J, Rangarajan S, Jolly SS, Belley-Cote EP, Whitlock R, Beresh H, Lewis G, Xu L, Chan N, Bangdiwala S, Diaz R, Orlandini A, Hassany M, Tarhuni WM, Yusufali AM, Sharma SK, Kontsevaya A, Lopez-Jaramillo P, Avezum A, Dans AL, Wasserman S, Felix C, et al. The Anti-Coronavirus Therapies (ACT) Trials: Design, Baseline Characteristics, and Challenges. CJC Open 2022 Jun;4(6):568-576. PM: 35252829.
Figtree GA, Redfors B, Kozor R, Vernon ST, Grieve SM, Mazhar J, Thiele H, Patel MR, Udelson JE, Selker HP, Ohman EM, Maehara A, Karmpaliotis D, Eitel I, Granger CB, Ben-Yehuda O, Stone GW, Kosmidou I. Clinical Outcomes in Patients With ST-Segment Elevation MI and No Standard Modifiable Cardiovascular Risk Factors. JACC Cardiovasc Interv 2022 Jun 13;15(11):1167-1175. PM: 35680197.
Garg A, Rout A, Farhan S, Waxman S, Giustino G, Tayal R, Abbott JD, Huber K, Angiolillo DJ, Rao SV. Dual antiplatelet therapy duration after percutaneous coronary intervention using drug eluting stents in high bleeding risk patients: A systematic review and meta-analysis. Am Heart J 2022 Aug;250:1-10. PM: 35436504.
Kern MJ, Applegate B, Bittl J, Block P, Butman S, Dehmer G, Garratt KN, Henry T, Hirshfeld J, Holmes DR, Kaplan A, King S, Klein LW, Krucoff MW, Kutcher MA, Naidu SS, Pichard A, Ruiz CE, Skelding KA, Tobis JM, Tommaso C, Weiner BH, White C. Conversations in cardiology: Late career transitions-Retool, retire, refocus. Catheter Cardiovasc Interv 2022 Jun;99(7):2136-2144. PM: 35446473.
Mann DL, Hernandez AF, Braunwald E. Could Neprilysin Be Already Inhibited by BNP in the LIFE Trial?-Reply. JAMA Cardiol 2022 Jun 1;7(6):657-658. PM: 35507336.
Memon MM, Siddiqui AA, Amin E, Shaikh FN, Khan MS, Doukky R, Krasuski RA. Novel oral anticoagulants versus vitamin K antagonists in patients with atrial fibrillation after transcatheter aortic valve replacement: A systematic review and meta-analysis. Catheter Cardiovasc Interv 2022 Jun;99(7):2101-2110. PM: 35476221.
Nelson MB, Gilbert ON, Duncan PW, Kitzman DW, Reeves GR, Whellan DJ, Mentz RJ, Chen H, Hewston LA, Taylor KM, Pastva AM. Intervention Adherence in REHAB-HF: Predictors and Relationship With Physical Function, Quality of Life, and Clinical Events. J Am Heart Assoc 2022 Jun 7;11(11):e024246. PM: 35656973.
Pahuja M, Leifer ES, Clarke JD, Ahmad T, Daubert MA, Mark DB, Cooper L, Desvigne-Nickens P, Fiuzat M, Adams K, Ezekowitz J, Whellan DJ, Januzzi JL, O’Connor CM, Felker GM, Piña ILAssessing race and ethnicity differences in outcomes based on GDMT and target NT-proBNP in patients with heart failure with reduced ejection fraction: An analysis of the GUIDE-IT study.Prog Cardiovasc Dis Mar-Apr 2022;71:79-85.PM:35490873
Salah HM, Minhas AMK, Khan MS, Abramov D, Agarwal R, Fudim M. Trends and Characteristics of Hospitalizations in Patients With Heart Transplant. Curr Probl Cardiol 2022 Aug;47(8):101210. PM:35460682
Segar MW, Patel KV, Hellkamp AS, Vaduganathan M, Lokhnygina Y, Green JB, Wan SH, Kolkailah AA, Holman RR, Peterson ED, Kannan V, Willett DL, McGuire DK, Pandey A Validation of the WATCH-DM and TRS-HF Risk Scores to Predict the Risk of Incident Hospitalization for Heart Failure Among Adults With Type 2 Diabetes: A Multicohort Analysis. J Am Heart Assoc 2022 Jun 7;11(11):e024094. PM:35656988
Solomon SD, Claggett BL, Miao ZM, Diaz R, Felker GM, McMurray JJV, Metra M, Corbalan R, Filippatos G, Goudev AR, Mareev V, Serpytis P, Suter T, Yilmaz MB, Zannad F, Kupfer S, Heitner SB, Malik FI, Teerlink JR Influence of atrial fibrillation on efficacy and safety of omecamtiv mecarbil in heart failure: the GALACTIC-HF trial. Eur Heart J 2022 Jun 14;43(23):2212-2220. PM:35325102
Duke Heart Week Ending June 12th 2022
Chief’s message:
As we come to the end of the academic year, we are reminded of the amazing faculty, fellows, residents, administrative and clinical staff and colleagues we have. The year end is punctuated with having to say goodbye to many of our graduating fellows (we have our end of year party this upcoming week), and unfortunately some departures of faculty (you will see the note around Tom Gehrig and Magnus Ohman below). We also have a set of year end recognitions and awards (School of Medicine, Department of Medicine, and Resident awards). These times of change are moments to reflect and hopefully we can all celebrate these amazing life accomplishments and recognitions along with appreciating those that are leaving Duke. We intend to celebrate our entire community over these next few weeks and look forward to sharing in the Pulse.
Highlights of the week:
Gehrig Departs Duke; Heads to UVA Health
Dr. Thomas Gehrig, associate professor of medicine in cardiology, and an integral part of our team for 24 years, will be moving to the University of Virginia in Charlottesville (UVA). His last day with Duke Heart will be June 15.
Tom is one of our most cherished and beloved clinician-educators, a true role model for all of us and someone adored by his huge patient population. To say he will be greatly missed by everyone at Duke is quite the understatement.
For those of you who are unaware of his background, Tom is a hard-core University of Florida Gator, having been born in central Florida. He completed both his undergraduate and medical school studies there (where he, by the way, graduated number one in his class in med school). He went on to internal medicine house staff training at the University of Virginia, staying on as their Chief Resident, before joining the Duke Cardiology program in 1995 to focus on interventional and structural heart disease. He has remained at Duke ever since as a member of the Duke Heart Physicians (DHP) clinical group. He was a star then and remains a star now. As a fellow he won the Floyd Award for Clinical Excellence and as a faculty member won the Bashore Teaching Award, the Waugh Educational Award, and the School of Medicine’s Tow Humanism Award.
Over the last 24 years Tom has had a major impact on all that is Duke cardiology. His incredible work ethic, his outstanding clinical and teaching skills, his photographic memory, his kindness, his ability to work with virtually anyone, his respect for the staff and coworkers, and his loyalty to medicine and to Duke are all just part of who he is. He never knows a stranger, and he is the first to offer a helping hand when there is a need. Tom will be an associate professor of medicine at UVA, and they are extraordinarily lucky to have him. Fortunately, he knows some of the folks there already, and they know him. We can all be honored and proud that we were able to be associated with him while he was at Duke.
Tom would like to continue to be connected with his friends and colleagues here. His email at UVA is TRG2Z@virginia.edu. He says his job description at UVA will be similar to what he does here at Duke with a little more time off. His wife, Dr. Paola Gehrig, will be the W. Norman Thornton Jr. Professor and Chair of the Department of OB/GYN at the University of Virginia.
We all wish Tom and Paola the very best, as they represent the very best.
The above background and the following photos from recent celebrations for Tom and Paola are courtesy of Tom Bashore, MD and Cary Ward, MD – many thanks!
Asked about his time at Duke and in Durham, Gehrig says it’s a bittersweet time for his family. They’ve loved raising their children here, have enjoyed the uniqueness of the Triangle area and being part of their respective healthcare teams (his wife Paola has been on the faculty at UNC School of Medicine/UNC Lineberger). He adds that he’s had fantastic mentors, particularly Kevin Harrison, Tom Bashore and Andrew Wang – but also a great career partnering with the rest of the cardiology faculty. He says he jokes about probably being the only general cardiologist at Duke because he “takes on whatever comes along, so to speak.”
“Duke has been a wonderful place to have a career where I could practice any type of cardiology I wanted to and have supportive people around me,” Gehrig says. “The camaraderie here has always been fantastic. I think it has been unmatched, really, the camaraderie among physicians in our division in particular, but also with the surgical division. And I’m going to miss the patients – the south is known for a lot of things, I suppose, but definitely for its kind, wonderful people. I’ve got 1400 patients I see on a regular basis that are going to be hard to walk away from.”
As he looks to the future in Charlottesville, it’s a circling back to where he and Paola both did residency and where they have a lot of good friendships already in place. The opportunity to return to Virginia was something they always thought they’d be interested in, he says, and it literally came up out of nowhere and everything just fell into place. He jokes that it’s Paola that UVA really wants, that he’s just the ‘baggage’ along for the ride.
We know otherwise, of course. UVA is getting an amazing clinician in Gehrig. He’s a clinician who considers his patients to be the very best population at Duke, and he’s a beloved colleague who will be missed on a daily basis.
In addition to Bashore and Ward, we asked others for their thoughts on Tom. Here is what they shared with us:
From Tom Povsic, MD:
“It has simply been an honor to be a fellow and faculty colleague of Tom’s. I can think of no one who exemplifies a “man for others” better than Tom. With Tom it is always about those around him: his colleagues, the fellows and students who have been lucky enough to learn from him, and most of all his patients. It is daunting to take care of or cath one of his patients, not only because of how they regard him, but because of the level of care he provides (I have it from reliable sources the he broke the curve for the rest of us taking cardiology boards) and the empathy and concern he imparts to them. Duke cardiology, our trainees, staff and Duke cardiology patients will sorely miss Tom. I can think of no one to whom I would rather entrust a family member or loved one’s care. We will find people to see his patients, but he will not be replaced.”
From Andrew Wang, MD:
“Dr. Tom Gehrig, over 24 years as a Duke Cardiology fellow and faculty member, was the epitome of a master clinician and educator. He had a keen sense of what the patient and learners needed in the moment and over time. His care of his patients and the trainees whom he taught were exemplary and highly respected by all. He is the cardiologist that you would want caring for your family or yourself. As a colleague, he was always willing and eager to lend a hand (or two), his sage advice and kind support. His daily contributions to our division will be greatly missed, and UVA is very fortunate to have him on their faculty.”
From Jimmy Tcheng, MD:
“I’ve had the privilege of having Tom as a friend, colleague, and confidant for nearly 25 years. I can recall as if just yesterday when he began his Duke cardiology fellowship in 1998 – inquisitive and eager to learn while already advanced beyond his years in clinical acumen. His humanistic qualities were readily apparent, his remarkable ability to relate to patients, to engender trust – all qualities that set him apart from day one. In the cath lab, he proved to be a “natural”, rapidly mastering the techniques and technologies of interventional cardiology. We have since shared many days shoulder to shoulder in the cath lab, with his facility to integrate clinical knowledge, patient characteristics, and technical command consistently providing the perspectives needed to chart the best possible course for our patients. His steadying influence and balanced approach have been consistent and remarkable qualities that we would all do well to emulate. And not only is he the “physician’s physician” – but a great teacher and educator as well. Tom will be deeply missed – his thoughtfulness, compassion, brilliance, perspectives and wit truly set him apart as the “Best of Duke”. I wish him the best in his future endeavors, he is leaving Duke a better place.”
From Schuyler Jones, MD:
“Tom has been a great teacher and partner for me over the last 20 years. He’s a consummate professional and a master clinician, but more than that, he’s a really great guy and someone I always felt I could reach out to for advice and guidance. Like the rest of the Duke cath lab, I’ll miss his sarcastic banter with the staff and fellows, and his total dedication to patient care and quality. Best of luck to Tom and Paola as they return to Charlottesville.”
From Manesh Patel, MD:
“It’s bittersweet to have someone like Tom Gehrig leave Duke. Tom has been one of our best clinicians with a focus on teaching our fellows, delivering the highest quality care, but most of all just being a great friend and partner. UVA is lucky to have him and I am sure he and Paola will enjoy the return. We will miss someone that we could call at anytime about a patient and he would provide sage and thoughtful guidance, with compassion and understanding. He is truly one of our best, and we wish him well and hope to continue to work together in the future.
Shown in photos are:

DHP GROUP: From Left: Mike Sketch, Tom Bashore, Anita Kelsey, Tom Gehrig, Cary Ward, Andrew Wang, Kevin Harrison

The Gehrigs: their son Joe Gehrig, Tom & Paola Gehrig

Gehrig and OP Staff: Michelle Johnson, Christine Beyer-McFarlane and Edana Christy with Tom

Gehrig and faculty: From Left: Andrew Wang, Paul Rosenberg, Rob Mentz, Cary Ward, Tom
Best wishes, Tom!!
Magnus Ohman to retire from clinical medicine to become Vice-President of Global Development of Cardiometabolic therapeutics for Amgen
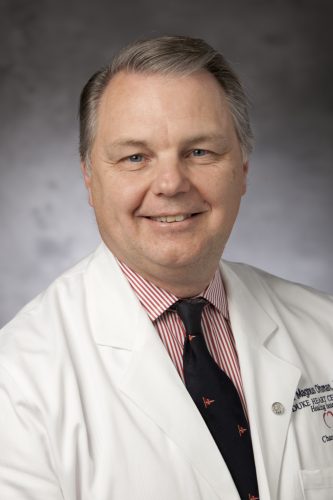
Magnus came to Duke from Dublin, Ireland in 1987 to complete a cardiology fellowship and to build on his translational research work on beta-adrenergic receptors with Dr. Gary Stiles. A meeting with Dr. Galen Wagner changed his trajectory. Galen suggested that Magnus should connect with Dr. Robert Califf to see if Magnus may be some interest in working on clinical trials at Duke, given Magnus’ exposure to the Clinical Trials Unit at University of Oxford with Richard Peto and Rory Collins. Magnus became the 6th Duke Databank fellow and started working with Rob on the TAMI trials. He later became one of the founding members of the Duke Clinical Research Institute in 1996, with Dr. Chris Granger, Dr. Dan Mark, Dr. Chris O’Connor and Dr. Bob Harrington, among others. The Duke Databank and later DCRI collaboration led to a fantastic opportunity to test new strategies in Acute Coronary Syndromes and cardiac devices. Magnus led the first adequately sized randomized clinical trial (RCT) of a device, IABP, in STEMI in the early 1990s. His knowledge from the Oxford days also became helpful as Rob Califf and Chris Granger embarked on the GUSTO trials. Magnus continued to revolutionize clinical trials throughout his career. Some of these included trial designs assessing infarct size in STEMI with Dr Manesh Patel (JAMA); the first dedicated ACS trial for medical management with dual anti-platelet therapy with Dr Matt Roe (NEJM); and testing low-dose oral anti-coagulation with clopidogrel or ticagrelor in ACS without aspirin (Lancet).
One of the spin-offs (sub-study) led by Magnus was the GUSTO-II trial Troponin T study. The study was assessing the ECG, CK-MB, which was the gold standard for diagnosing MI at the time. The new marker, Troponin T, was a potential new way of diagnosing MI. The GUSTO TnT study showed that this marker was better aligned with the cardiovascular risk of the patient and therefore a better marker for determining MI. The first Universal Definition of MI meeting held jointly with ESC, AHA and ACC then led to redefinition of MI using troponin as the new standard. Magnus continued the biomarker work with Dr. Kristin Newby, among others. They published several papers together using biomarkers for risk stratification and linking it to a therapeutic strategy. Some of these have now become standard practice in ACS such as the early invasive strategy based on troponin positive non-STEMI patients.
In the late 1990s after several large RCTs in ACS had been completed, it became clear that there was a gap between the practice of ACS and the findings from the RCT trials. Jointly with Drs Brian Gibler, Eric Peterson and Matt Roe, Magnus led the first large-scale Quality Improvement (QI) registry in ACS, called the CRUSADE program. It evaluated over 250,000 patients from about 400 US hospitals over a 5-year period. One of the most seminal papers from this registry written by Eric Peterson was able to link the better adherence to ACC/AHA guideline recommended therapies with improved survival. This registry was later adopted by the ACC and now forms the basis for the NCDR ACTION registry.
Magnus has been a big advocate for the value of collaboration and mentorship not only within Duke, but across multiple institutions and continents. This collaborative work has been richly rewarded with a large publication record of over 700 peer-reviewed articles, 47 book-chapters, and 3 books. Among these, Magnus authored 16 papers in NEJM, 14 in the Lancet and 15 in JAMA making him one of the top 1% cited researcher worldwide from 2001 to 2020 by Clarivate Analytics.
Because of his large clinical trial experience, Magnus has been a frequent advisor to the FDA. He served on the Circulatory System Device Panel for 7 years and remains an ad-hoc member. He was also a member of the ACCF/AHA Task Force for Practice Guidelines between 2010 and 2019, being one of their longest serving members that helped shape the ACC/AHA guidelines into their present format.
In 1991, Magnus finished his interventional training under Drs Richard Stack and Harry Phillips. Over the years his practice gravitated towards high-risk PCI. This led him to explore innovative solutions to support patients needing PCI with reduced cardiac function. In the late 1990s, he initiated a program at Duke for ECMO supported PCI. This was followed by Impella supported PCI in the late 2000s. His dedication towards the management of high-risk PCI led Magnus to be inducted into the International Andreas Gruentzig Society honoring the innovators of PCI. More recently he collaborated with Dr Tom Povsic on novel therapies for patients with Advanced Coronary Disease including gene therapy. Dr Chris O’Connor and Magnus formally proposed this program in the early 2010. Magnus became its first director with assistance of philanthropic support from the Rawson family. It remains the only endowed Directorship at Duke Health.
In 2000, Magnus became the Chief of Division of Cardiology and the first Director of the UNC Heart Center. While at UNC, Magnus was unaware that he remained a DCRI faculty member. It was therefore a big surprise after spending 5 rewarding years at UNC that he never left Duke! Drs Pam Douglas and Tom Ryan recruited Magnus back to focus on patients with Advanced Coronary Disease and help re-organize the Duke Heart out-patient clinics. The latter included a new model that Magnus and Dr David Zaas (now CEO at MUSC Health) developed that added mid-level providers (NPs and PAs) and nurse-clinicians to facilitate new patients accessing Duke Cardiology. The program continues on now and has created a team-care model that is now being replicated in other parts of Duke Health.
In 2012, Drs John Paat, Jim Kelly, and Magnus started Signature Care at Duke. A concierge system of care within Duke Health; Magnus being the only cardiologist. It was the first concierge practice within an academic setting in the US and has now been replicated by other leading academic centers around the country. The program accelerated philanthropic giving to Duke. Dr Mary Klotman made Magnus the Vice-Chair of Medicine for Development and Innovation (2014-20), where he, with Duke Alumni and Development officers, raised over $12 million over the period towards research programs in Duke Medicine and the Heart Center. Several Cardiology fellows have subsequently benefitted from the Ernest Mario Family Foundation award and outside speakers for the Lynn Williams lecture in Cardiovascular Genetics.
Magnus has followed a large number of patients at Duke over several years. “It has been an honor to be partner with so many wonderful patients. It will be hard to leave them, but I am comforted that they will continue to have outstanding care at Duke by the many exceptional providers at Duke Heart.”
In his new role he hopes to continue to build on the relationship DCRI and Duke Heart has with industry and serve as a mentor to Duke faculty and fellows. He will also help steer philanthropic gifts to Duke. “My journey at Duke over 35 years have been amazing and I am so grateful for all the support and collaboration that I have received from Duke. Our three children were all born at Duke; as a family we will forever love Duke”.
Personally, I believe we will miss the tremendous impact that Magnus had on the way we think about clinical cardiology, interventional cardiology, and his continual desire to push us to innovate and improve how we thought about cardiovascular care. We are sure that Amgen will benefit from his leadership, and look forward to continuing to partner with him on innovating cardiovascular care.
Duke DOM Recognizes Fortin, Shah with Faculty Awards
The Duke Department of Medicine presented their annual faculty awards during their Annual Celebration held on Thursday, June 9 at the University Club in Durham. Congratulations to Drs. Terry Fortin and Nishant Shah! Fortin received the 2022 Master Clinician Award and Shah received the 2022 Excellence in Education Award.
We are so proud of each of them. Well deserved!


Duke IM Chief Residents Award Rymer, Abraham & Loriaux
The Duke Internal Medicine chief residents — Jessica Regan, MD; Dennis Narcisse, MD, MS; Nancy Yang, MD, and Michael Burt, MD — presented the annual awards honoring excellence in the Department of Medicine’s education mission at Medicine Grand Rounds on Friday, June 10. The team recognizes medical students, residents, fellows and faculty for their service and excellence in teaching.
Several awards were given to team members in the division of cardiology:
- Jennifer Rymer received the Greenfield Research Mentor Award
- Dennis Abraham received the Eugene Stead Award for Excellence in Teaching
- Dan Loriaux received the Fellowship Teaching Award

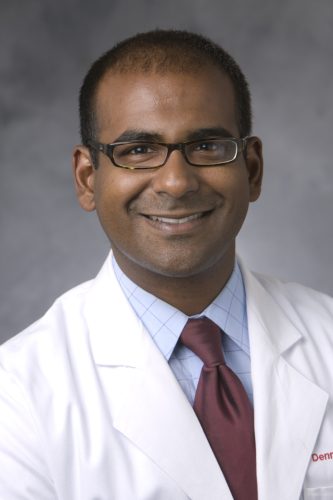
 I
I
Incoming Duke IM chiefs include cardiology fellows Lonnie Sullivan, MD and Sara Coles, MD; rheumatology/immunology fellow Nathanial Harris, MD, PhD and internal medicine resident Ryan Duffy, MD.
Well deserved! Congratulations, Jenn, Dennis and Dan!
Thomas Looks to Lead SOM Toward a More Equitable Future & He’s Up for the Challenge
 Kevin Thomas, MD, associate professor of medicine in cardiology, had little interest in cardiology when he first entered medical school, but it is difficult now to separate his journey toward becoming a cardiologist from his current work advancing equity, diversity, and inclusion (EDI).
Kevin Thomas, MD, associate professor of medicine in cardiology, had little interest in cardiology when he first entered medical school, but it is difficult now to separate his journey toward becoming a cardiologist from his current work advancing equity, diversity, and inclusion (EDI).
In November 2021, Thomas, an electrophysiologist in Duke’s Division of Cardiology, was named the Duke University School of Medicine’s vice dean for equity, diversity, and inclusion by Dean Mary E. Klotman. The role is a first for the school, and was among the key action items outlined in the anti-racism and advancing equity strategic plan launched by the School of Medicine in June 2021.
“The creation of this critical new leadership role reflects the school’s commitment to advancing equity, diversity, and inclusion,” Klotman said. “We needed someone with great strategic vision, perspective, and dedication to lead this effort. Kevin Thomas embodies those qualities. We could not have made a better choice, and he is already making a difference.”
Thomas has been at Duke for more than 22 years, making a mark on health disparities research in the cardiology field. If it weren’t for a few notable encounters with the right people at the right time, Thomas said, he may not have ended up in either role.
An Unexpected Path
Choosing cardiology as a specialty at Duke almost felt clichéd, Thomas said, and he did his best to avoid it initially. As a visiting fourth-year medical student, he became attracted to gastroenterology after a rotation in the division and working under Mark Swaim, MD.
But after a few of his mentors in that discipline left to pursue positions at other institutions, he began to wonder if there was something else in store for him. “This is not coincidence,” he recalled thinking at the time.
Despite his initial resistance to cardiology, events and interactions kept steering him toward it. During Thomas’ first year of training at Duke, close friend Mark East, MD, who was a Duke cardiology fellow at the time told him outright that he was going to become a cardiologist and that he should embrace it. “He said, ‘Kevin, you know you’re going to do cardiology; I don’t know why you’re trying to run from it,’” Thomas said.
Ultimately, as a person of faith, Thomas decided he should pay attention to the signs. “There was this narrative that people kept telling me: ‘Oh, you have to do cardiology.’ Through all those experiences, I said I feel like God is speaking to me, and maybe I need to consider cardiology.”
So he did. Thomas became a cardiology fellow and chief resident at Duke. He has no doubt now that it was the right choice because it put him on the path to his other passion: equity, diversity, and inclusion work. His time as a fellow opened his eyes to health inequities, in cardiology in particular.
“I began to see people being treated differently based on race, ethnicity, and socioeconomic status,” Thomas said. “There were things happening that were making me uncomfortable and made me want to see change. This is really when my passion and interest in health inequities and health disparities came about.”
The realization led Thomas to begin researching the topic, and he has never stopped.
“I found research as a way to try to understand why these differences, disparities, and inequalities existed,” he said. “Cardiovascular disease is the number one killer particularly of African Americans. Cardiology was a great platform and a conduit for me to get into my equity, diversity, and inclusion work.”
Kevin’s story continues in Magnify. To continue reading, please click here.
Holley Team Secures Translational Research Grant
Congratulations to Chris Holley, MD, PhD, associate professor of medicine in cardiology. He and his team have recently secured

a translational research grant through the North Carolina Biotechnology Center for their proposal, “Silencing Small Nucleolar RNAs (snoRNAs) with Antisense Oligonucleotides (ASOs) for Treatment of Atherosclerosis”. Holley’s research lab is located within the Duke Cardiovascular Research Center. The research grant includes $110K in funding.
Exciting news, Chris — congratulations!
Duke Heart Team in Honduras
Our Duke Heart for Honduras team has been having a successful week – they provided photos of their welcome, first patient and an incredible cake that was provided by the Honduras-based team for Carmelo Milano’s birthday. Not only did our Duke team receive a warm celebration upon arrival, they also earned some positive news coverage while in Honduras – be sure to see below in our news section.
We look forward to hearing all about the trip when they return.



Duke Heart NP Plans ‘Be The Match’ Drive
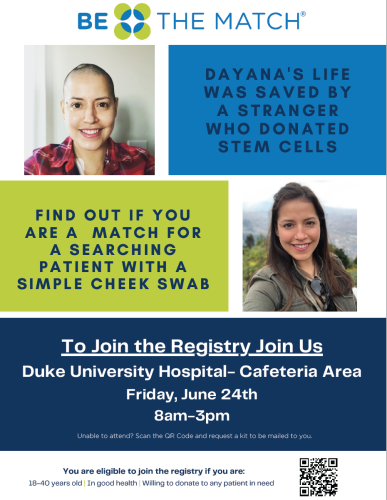 Prior to June 2020 Dayana Ramos, a cardiology nurse practitioner at Duke University Hospital (DUH), was travelling throughout the world as often as she was able to do so. She had run a marathon, was spending time with friends and family, and was engrossed in a fulfilling nursing career. But that month, seemingly out of nowhere, the avid runner and walker started experiencing bouts of fatigue that she, at first, attributed to effects of the pandemic. Of her circle of friends, Ramos and others would tell you she was the most health-conscious and fit among them. Suddenly, going up a short flight of steps left her out of breath and she couldn’t complete an easy afternoon bike ride. Within weeks, Ramos received a diagnosis that stunned her family, friends and coworkers: acute lymphoblastic leukemia (ALL). She had just turned 37 and had no family history of blood cancer.
Prior to June 2020 Dayana Ramos, a cardiology nurse practitioner at Duke University Hospital (DUH), was travelling throughout the world as often as she was able to do so. She had run a marathon, was spending time with friends and family, and was engrossed in a fulfilling nursing career. But that month, seemingly out of nowhere, the avid runner and walker started experiencing bouts of fatigue that she, at first, attributed to effects of the pandemic. Of her circle of friends, Ramos and others would tell you she was the most health-conscious and fit among them. Suddenly, going up a short flight of steps left her out of breath and she couldn’t complete an easy afternoon bike ride. Within weeks, Ramos received a diagnosis that stunned her family, friends and coworkers: acute lymphoblastic leukemia (ALL). She had just turned 37 and had no family history of blood cancer.
She began induction therapy treatment within days of her diagnosis, spending 35 days on 9100 at DUH. Despite two full courses of treatment, it wasn’t enough. She needed a stem cell transplant, but had no family matches. Seventy percent of patients with blood cancers or other disorders don’t have a blood stem cell donor match in their family.
Ramos and her care team turned to the Be The Match registry, operated by the National Marrow Donor Program, and went through 6 or 7 potential matches before a good stem cell donor candidate was found. The transplant was successful and she is now back at work with our cardiology patients. She was away from work for a year and a half during the pandemic. With her family located in PA, northern VA and FL, she limited her contact to just a few close friends and several family members who could rotate through Durham to stay with and care for her during treatment.
She was really lucky. Dayana is Latina. Statistics show the odds of her finding a match based on her ethnic background were only 48 percent. For Blacks/African Americans, the disparity is even worse: 29 percent. For Caucasians, the chances are much higher at 79 percent. Patients are most likely to match with someone of their same ethnicity.
To increase awareness and do what she can to increase representation in the registry, Ramos is holding a Be the Match registration drive at Duke University Hospital on Friday, June 24th from 8 a.m. to 3 p.m. outside the Atrium Café. Her goal is to increase understanding about blood cancers and the National Marrow Donor Registry and to increase the field of potential matches. Ideal registrants are between the ages of 18 and 35. She’d like to emphasize that registering is easy and that if a registrant ends up being a match, the costs associated with the donation process are covered and that donating, overall, is pretty easy. She encourages anyone who is interested to learn more.
Please consider stopping by the Be The Match drive on June 24 and supporting Dayana. She’s amazing and we are so glad she is doing well!
Shout-out to Khan!
A shout-out to cardiology fellow Shahzeb Khan, MD, who presented at the American Diabetes Association’s 82nd annual Scientific Sessions (held as a hybrid event from June 3-7 in New Orleans, LA). Khan presented on the socioeconomics of heart failure.
Way to represent Duke Heart, Shahzeb!

AHA Go Red Luncheon
 The American Heart Association’s 15th Annual Triangle Go Red for Women luncheon was held on Friday, June 3 at the Raleigh Convention Center. The event included health and wellness breakout sessions on mindfulness and well-being, healthy nutrition tips, and heart disease/stroke prevention. A big shout-out to Neha Pagidipati, MD for her ‘Real Talk with a Doc’ session on prevention and what women most need to know. Excellent job, Neha!!
The American Heart Association’s 15th Annual Triangle Go Red for Women luncheon was held on Friday, June 3 at the Raleigh Convention Center. The event included health and wellness breakout sessions on mindfulness and well-being, healthy nutrition tips, and heart disease/stroke prevention. A big shout-out to Neha Pagidipati, MD for her ‘Real Talk with a Doc’ session on prevention and what women most need to know. Excellent job, Neha!!
The luncheon included Margot Ridgeway’s moving stroke survivor story. Ridgeway, an NC State student and soccer player suffered a stroke at the beginning of the pandemic. Although she was displaying multiple signs of stroke, her condition went undiagnosed for several days. Now 21, Ridgeway–along with her mom– talked about her medical crisis and recovery. Both are now dedicated to raising awareness of stroke and heart disease among all ages. To read more about her story, visit: https://duke.is/j6bu9)
The Go Red luncheon included a heart disease survivor fashion show and recognition of local AHA ‘Women of Impact’ including Duke’s own Priscilla Ramseur, DNP, RN, CNOR, NEA-BC, chief nursing officer of Duke Raleigh Hospital.
local AHA ‘Women of Impact’ including Duke’s own Priscilla Ramseur, DNP, RN, CNOR, NEA-BC, chief nursing officer of Duke Raleigh Hospital.
Thanks to everyone who was able to join us and help make this event a success!

COVID-19 Update
All the latest Clinical Operations updates related to COVID can be found at https://covid-19.dukehealth.org. Patient-facing resources on DukeHealth.org can be found here: https://www.dukehealth.org/covid-19-update/resources. Duke University maintains a resource page as well, which can be accessed here: https://coronavirus.duke.edu/updates/for-staff.
Upcoming Events & Opportunities
June 30: Women in Cardiology. Arrive by 6:30 p.m. The WIC team has announced their next meeting will be at the home of Dr. Pamela Douglas. The theme of the event will be ‘Mentorship and Sponsorship’ with panelists Dr. Douglas, Dr. Jenn Rymer, Dr. Tracy Wang, and Dr. Camille Frazier-Mills. We are lucky to have such a group of incredibly accomplished women and we can’t wait to hear about their mentorship and sponsorship experiences and advice. Dinner will be provided. For more details, please contact cardiology fellow Karen Flores Rosario, MD.
June 24: Be The Match Registry Drive. 8 a.m. – 3 p.m., Duke University Hospital outside of Atrium Café. If you’re between the ages of 18-35 years old, consider registering as a potential stem cell/bone marrow donor via Be The Match. Help support our cardiology team member and ALL survivor, Dayana Ramos.
Did you know that every three minutes, someone is diagnosed with a blood cancer? You can help be part of their cure. It’s quick and easy — with just a swab kit, it can be determined if your bone marrow or stem cells can save a patient’s life. Come to event to learn more or visit https://bethematch.org. Test kits are available through the registry website.
Duke-Stanford Cardiovascular Research Symposium
June 27 & 28. The Duke-Stanford Cardiovascular Research Symposium returns to Durham this year and is offered as a hybrid event. This symposium is sponsored by the Edna and Fred L. Mandel, Jr. Foundation.
Registration required. In person: Great Hall, Mary Duke Biddle Trent Semans Center, Durham, NC. For those who wish to attend virtually, the event will offer live-streaming. The link will be emailed prior to the program. Registrants who choose the virtual live-streamed webinar option will be able to obtain CE credit for the course. For more information, contact Christy Darnell.
Cardiology Grand Rounds
Cardiology Grand Rounds has concluded and will resume in September.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
June 6 — William Kraus
CBS/The Today Show
Prescription exercise? How doctors are tailoring workout plans
https://duke.is/paaap
June 7 — Carmelo Milano, Alina Nicoara, Adam Williams & Alejandro Murillo
Hondudiario.com (Honduras)
https://duke.is/jhfgm
June 8 — Carmelo Milano, Alina Nicoara, Adam Williams & Alejandro Murillo
El Pais.hn (Honduras)
El Hospital Honduras Medical Center es Sede de la Brigada Cardiovascular “Unidos por El Corazon”
https://duke.is/ya5wv
June 9 — Stephen Greene
Practical Cardiology
Don’t Miss a Beat: oHCM and Mavacamten, with Anjali Owens, MD
https://duke.is/vcaf2
Division of Cardiology Publications Indexed in PubMed June 2-8, 2022
Allen LaPointe NM, Ali-Ahmed F, Dalgaard F, Kosinski AS, Schmidler GS, Al-Khatib SM. Outcomes of Cardiac Resynchronization Therapy with Image-Guided Left Ventricular Lead Placement at the Site of Latest Mechanical Activation: A Systematic Review and Meta-Analysis. J Interv Cardiol 2022 May 20;2022:6285894. PM: 35655661
Collins KA, Huffman KM, Wolever RQ, Smith PJ, Siegler IC, Ross LM, Hauser ER, Jiang R, Jakicic JM, Costa PT, Kraus WE. Determinants of Dropout from and Variation in Adherence to an Exercise Intervention: The STRRIDE Randomized Trials. Transl J Am Coll Sports Med 2022 ;7(1):e000190. PM: 35669034.
Drozda JP, Graham J, Muhlestein JB, Tcheng JE, Roach J, Forsyth T, Knight S, McKinnon A, May H, Wilson NA, Berlin JA, Simard EP. Multi-institutional distributed data networks for real-world evidence about medical devices: building unique device identifiers into longitudinal data (BUILD). JAMIA Open 2022 May 25;5(2):ooac035. PM: 35663113.
Echouffo-Tcheugui JB, Musani SK, Bertoni AG, Correa A, Fox ER, Mentz RJ. Patients phenotypes and cardiovascular risk in type 2 diabetes: the Jackson Heart Study. Cardiovasc Diabetol 2022 Jun 1;21(1):89. PM: 35650579.
Harrington J, Jones WS, Udell JA, Hannan K, Bhatt DL, Anker SD, Petrie MC, Vedin O, Butler J, Hernandez AF. Acute Decompensated Heart Failure in the Setting of Acute Coronary Syndrome. JACC Heart Fail 2022 Jun;10(6):404-414. PM: 35654525.
Jean-Charles PY, Rajiv V, Sarker S, Han S, Bai Y, Masoudi A, Shenoy SK. A single phenylalanine residue in β-arrestin2 critically regulates its binding to G protein-coupled receptors. J Biol Chem 2022 May;298(5):101837. PM: 35307348.
Lerman JB, Giamberardino SN, Hernandez AF, Felker GM, Shah SH, McGarrah RW. Plasma metabolites associated with functional and clinical outcomes in heart failure with reduced ejection fraction with and without type 2 diabetes. Sci Rep 2022 Jun 2;12(1):9183. PM: 35654972.
Petek BJ, Moulson N, Baggish AL, Drezner JA, Harmon KG, Klein CF, Kliethermes SA, Patel MR, Churchill TW. Electrocardiographic findings in young competitive athletes during acute SARS-CoV-2 infection. J Electrocardiol May-Jun 2022;72:13-15. PM: 35219112.
Pinsker BL, Serfas JD, Awerbach JD, Dizon S, Spector ZZ, Campbell MJ, Krasuski RA. Utility of Cardiac Magnetic Resonance Imaging in Predicting Atrial Arrhythmias in Repaired Tetralogy of Fallot. Am J Cardiol 2022 Jul 1;174:151-157. PM: 35473783.
Rao S, Hurst JH, Zhao C, Goldstein BA, Thomas L, Lang JE, Kelly MS. Asthma and the Risk of SARS-CoV-2 Infection Among Children and Adolescents. Pediatrics 2022 Jun 1;149(6):e2021056164. PM: 35274143.
Rymer JA, Bhatt DL, Angiolillo DJ, Diaz M, Garratt KN, Waksman R, Edwards L, Tasissa G, Salahuddin K, El-Sabae H, Dell’Anna C, Davidson-Ray L, Washam JB, Ohman EM, Wang TY. Cangrelor Use Patterns and Transition to Oral P2Y Inhibitors Among Patients With Myocardial Infarction: Initial Results From the CAMEO Registry. J Am Heart Assoc 2022 Jun 7;11(11):e024513. PM: 35621210.
Singh AK, Cizman B, Carroll K, McMurray JJV, Perkovic V, Jha V, Johansen KL, Lopes RD, Macdougall IC, Obrador GT, Waikar SS, Wanner C, Wheeler DC, Wiecek A, Stankus N, Strutz F, Blackorby A, Cobitz AR, Meadowcroft AM, Paul G, Ranganathan P, Sedani S, Solo. Efficacy and Safety of Daprodustat for Treatment of Anemia of Chronic Kidney Disease in Incident Dialysis Patients: A Randomized Clinical Trial. JAMA Intern Med 2022 Jun 1;182(6):592-602. PM: 35377393.
Szarek M, Hess C, Patel MR, Jones WS, Berger JS, Baumgartner I, Katona B, Mahaffey KW, Norgren L, Blomster J, Rockhold FW, Hsia J, Fowkes FGR, Bonaca MP. Total Cardiovascular and Limb Events and the Impact of Polyvascular Disease in Chronic Symptomatic Peripheral Artery Disease. J Am Heart Assoc 2022 Jun 7;11(11):e025504. PM: 35621222.
Venkatraman V, Ponder M, Gellad ZF, Lad SP, Christy E, Plichta R, Harrison JK, Hughes GC, Doberne J. Feasibility study of a novel digital health platform for patients undergoing transcatheter aortic valve replacement. J Card Surg 2022 Jul;37(7):2017-2022. PM: 35434823.
Wang YZ, Zhao W, Ammous F, Song Y, Du J, Shang L, Ratliff SM, Moore K, Kelly KM, Needham BL, Diez Roux AV, Liu Y, Butler KR, Kardia SLR, Mukherjee B, Zhou X, Smith JA. DNA Methylation Mediates the Association Between Individual and Neighborhood Social Disadvantage and Cardiovascular Risk Factors. Front Cardiovasc Med 2022 May 19;9:848768. PM: 35665255.
Duke Heart Week Ending June 5th 2022
Chief’s message:
In Memoriam: Robb Kociol, MD, former Cardiology Fellow
It is with great sadness that we share the news of the passing of Robb Kociol, MD, a 2011 graduate of our  cardiology fellowship program.
cardiology fellowship program.
A native of the San Francisco Bay area, Kociol came to Duke for fellowship from Brigham and Women’s Hospital. He was noted during fellowship for being caring, fun, smart, and often self-deprecating. He was passionate about advanced heart failure care and after training at Duke, returned to Boston and the Beth Israel Deaconess Medical Center as a faculty member. He eventually became the director of their Transplant Program. Over the last few years, he transitioned to pharma – initially at Boehringer Ingelheim before going to Cytokinetics where he partnered with Duke faculty and company leadership for the omecamtiv mecarbil work.
He is survived by his wife Kristin, their two young daughters, and his parents.
Robb was a friend, gentle and thoughtful, and will be missed by all of us that knew him and by the larger cardiovascular community. His passing, like many of the events over the last few years, reminds us how precious life is and the bonds we have with each other.
At this time, service details have not been announced. We will remain in contact with the family to get details around his service, and ensure that the Duke community works to find any ways that we can support them.
As a start, below is a gofundme site that has been started to support his family.
|
We are raising money for the Kociol family after the unexpected passing of Robb. Th… Colleen Donovan needs your support for Kociol Family Memorial Fund
gofund.me
|
We asked several Duke Heart team members to share their thoughts on Robb with us. Here is what they wrote:
From Adrian Hernandez, MD:
“Robb came to Duke as a cardiology fellow with the triple aim of excellence in clinical care, research, and education. He achieved all of this plus more. What we learned from Robb is there is a 4th aim- excellence in humanity. He cared about people- friends, family, and others. It showed every day.
As we’ve learned about Robb’s passing, I know it brings up so many fond memories of him. Some of my best experiences have been with and because of Robb. At the beginning of his fellowship, I remember when he first met with me and asked if I could be his mentor in his own quirky style. Along the way, I had the privilege to see things differently through his eyes when he had decisions to make, opportunities to consider and difficult times to confront. Each time our conversation turned to what was best for the family and the people around him. He also had plenty of amusing stories to share in his self-deprecating way.
Just one example of his impact comes from several years ago when I had the pleasure of visiting Beth Israel-Deaconess Medical Center. Robb had just started the advanced heart failure program with ventricular assist devices, and it was clearly on its way to success. Every fellow noted how much of an impact Robb had on the place, their lives, and the lives of others. I heard stories from the fellows about Robb and the amount of time he spent with them and the patients selflessly ensuring their success. He led by example and all the fellows wanted to be like Robb. He relentlessly dedicated himself to every patient for the best outcome possible whether on ECMO or getting a VAD or making a tough decision at the end of life. He also wanted everyone to learn together and advance the field. He was so committed and loved it. That was Robb—committed to others. I was thankful Robb had ignored my advice on starting a VAD program- “Don’t do it. It’s impossibly hard, especially in Boston!” His reply, “I know, but its family.”
From Ravi Karra, MD:
“Robb was the best. He was brilliant and led by modeling excellence with humility and a quirky charm that was infectious. No one left a chat, text, or email from Robb without a smile on their face. Robb was always dedicated to serving patients and taking care of his family. Robb loved doctoring more than anyone I have ever met, and Robb was a great doctor. As a new attending, he built up the heart transplant program at the BI, caring for his patients as soon as the cross-clamp came off. He absolutely adored his wife, Kristin, and his girls, Sophia and Olivia. When catching up with Robb, he always gushed about what his girls were up to and always expressed his deep appreciation and love for Kristin. His sudden passing has been heart-breaking. My family has been privileged to know and grow with the Kociol’s – we sorely miss our dear friend.”
From Robert Mentz, MD:
“Robb lived an inspiring life. An exceptional clinician and researcher, he was a role model for many interested in improving care for patients with heart failure. He excelled during his training at Duke and the DCRI. Brilliant, hardworking and engaging, he helped lead a number of foundational projects in outcomes research and trials. Having trailed him at Brigham and Women’s Hospital and Duke, I became used to being referred to as “Robb” – though his shoes would be impossible to fill. He paved the way for many of us and was a thoughtful mentor and friend.
Following his training, he returned to Boston where he went on to lead and expand the advanced heart failure program at Beth Israel. He worked so incredibly hard to provide the best possible care for his patients. He had a remarkable career as a clinician investigator but perhaps even more inspiring was his life as a husband, father and friend. He faced both personal and family health issues with grit, courage and resiliency. It was shocking to hear of his passing and our thoughts go out to his wife and kids in particular. May they find some peace in knowing the tremendous impact he has had on so many of his colleagues and patients’ lives.
We will explore the best ways to support his family and remember his legacy within the walls of Duke and beyond. Back in 2016, he published a thoughtful piece about the need to be a well-rounded clinician – his words extend beyond clinical medicine and truly reflect the well-rounded and caring man he was – he will be missed.”
From Jason Katz, MD:
“Robb was a brilliant cardiologist, but most importantly he was a compassionate, caring, and beautiful human being. He had overcome so many obstacles over the last several years, and yet remained steadfast to the important things in life – his family, friends, and his passion for innovation. I am glad I had the chance to speak with him just a few weeks ago and was able to tell him how lucky we all felt to work with him. He represented the Duke family in such amazing ways.”
Highlights of the week:
Jill Engel named Service Line VP, Heart & Vascular Services
 Jill Engel, RN, DNP, FNP, ACNP, ANP, NEA-BC, FAANP, has been named Service Line Vice President – Heart & Vascular Services, Duke University Health System (DUHS), effective July 1, 2022. She holds a wealth of experience and expertise for our organization and was promoted to the role after an extensive and very competitive national search.
Jill Engel, RN, DNP, FNP, ACNP, ANP, NEA-BC, FAANP, has been named Service Line Vice President – Heart & Vascular Services, Duke University Health System (DUHS), effective July 1, 2022. She holds a wealth of experience and expertise for our organization and was promoted to the role after an extensive and very competitive national search.
Jill is a health care leader specializing in operational care redesign and strategic planning; programmatic design, development and financial planning; and a strong track record of recruiting, retaining, coaching and mentoring diverse and highly functional teams.
As an accomplished Advanced Practice Provider (APP) and nursing leader with an expertise and passion for advancing the mission of the heart and vascular service line, Jill served as interim Service Line VP – Heart & Vascular Services, DUHS, for nearly 18 months. During this time, Jill demonstrated her capabilities to strategically collaborate with physicians and colleagues, improve operational effectiveness and develop people. Prior to this interim role, Jill served as the nursing leader for the heart and vascular service line.
Additionally, she has served since 2020 as Academic Program Advisory Board member for Duke University School of Nursing and the Duke University School of Medicine (School of Cardiac Sonography).
The announcement was made on Thursday, June 2 by Craig Albanese, MD, executive vice president and chief operating officer for DUHS.
Personally, I will just add that Jill’s has been a great partner to work with and we are inspired by her ability to understand the issues that our clinical teams face in our day to day activities, her drive to improve patient care, and her ability to communicate broadly to our teams.
Please join us in congratulating Jill on her new executive leadership role!
Duke CTSI Announces MURDOCK Biorepository Initiative for Investigators
The Duke Clinical and Translational Science Institute (CTSI) has announced a new opportunity for Duke investigators to obtain biospecimens from the MURDOCK Study for research. The MURDOCK study is a landmark longitudinal cohort of more than 12,000 diverse participants linked to clinical data and up to 14 years of outcomes data.
investigators to obtain biospecimens from the MURDOCK Study for research. The MURDOCK study is a landmark longitudinal cohort of more than 12,000 diverse participants linked to clinical data and up to 14 years of outcomes data.
The MURDOCK Biorepository Transformation Initiative, led by the Duke Kannapolis Research group, will work with Duke investigators to convert samples into rich molecular datasets by facilitating access to these samples.
To make the MURDOCK samples easier to access, researchers will only incur costs for biospecimen retrieval and shipment.
“Through this science-forward initiative, we are making thousands of biospecimens and associated clinical and outcome data available to all Duke researchers,” said Svati Shah, MD, MHS, professor of medicine, associate dean for genomics, and director of Duke Kannapolis Research. “We are thrilled for the opportunity to share this powerful resource with more Duke collaborators, and we are incredibly grateful to the greater than 12,000 participants who contributed to one of the most unique biorepositories of its kind.”
The broad phenotypes included in the community-based MURDOCK cohort provide an excellent opportunity to study many different diseases and longitudinal outcomes, as well as serving as matched controls.
To read the full story, please visit: https://duke.is/2627y

Call for Heart Walk Captains, Walkers
Duke Health will once again participate in the Triangle Heart Walk and Dr. Rick Shannon has put out the call for team captains and walkers. Shannon is serving as the 2022 Heart Walk Campaign Chair.
The Heart Walk is the American Heart Association’s (AHA) premiere fundraising event that brings communities across the U.S. together to celebrate progress in the fight against heart disease and stroke, which remain the No. 1 and No. 5 leading causes of death in adult Americans.
In this year of renewal, we especially want to dedicate our efforts in remembrance of those members of the Duke family who have lost their lives or that of a loved one to heart disease and redouble our efforts to prevent these tragic losses.
After two years, the Triangle Heart Walk is planned as an in-person event this fall (date will be announced this summer). Our Duke Health theme is “We’re back—and together, we’re stronger than ever!” This will be a great opportunity to gather and celebrate one another and our efforts to reinvigorate heart-healthy lifestyles as well as raise lifesaving funds for the AHA.
We have set a goal of recruiting 350 team captains and 3,500 walkers to represent Duke Health, with a fundraising target of $350,000. Achieving this would make 2022 our most successful Heart Walk ever – and we can do this, together! Please consider becoming a team captain or committing to join a Duke Heart Walk team.
Registering as a team captain or walker is quick and easy.
- Visit https://www2.heart.org/site/TR/HeartWalk/GSA-GreaterSoutheastAffiliate?pg=entry&fr_id=7037
- Select the “Create new team” or the “Join a Team” button. Then complete the registration page.
- Personalize your page with a photo and send emails inviting others (co-workers, friends and family) to join the team and donate to your fundraiser.
If you have any questions, you can contact Sangeetha Menon, Development Director for the Triangle American Heart Association via email (sangeetha.menon@heart.org). She can help you get started.
Blumer Presents Final CGR of Season
Vanessa Blumer, MD, cardiology fellow, presented our final cardiology grand rounds of the season on Tuesday evening, May 31. Her topic was “Heart Failure Cardiogenic Shock and the Golden Circle.” Vanessa walked us through her “why” for this area of research and provided the current evidence around detection, management, and the working group on cardiogenic shock. Great job!

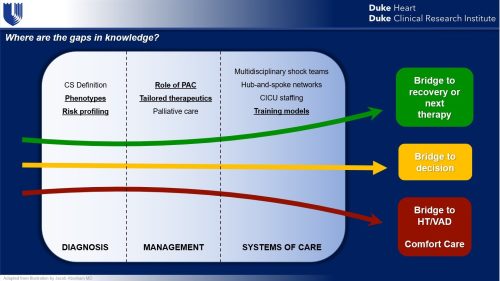
Duke Heart Team Heads to Honduras
A team from Duke Heart, comprised of cardiothoracic surgeons, anesthesiologists, perfusionists, nurses, an engineer, a medical student and a surgery resident have left on a medical mission trip to Honduras. The team, part of an effort known as Duke Heart for Honduras, is headed to the country of approximately 10 million people which has almost no cardiac surgery practitioners or facilities, and a very high incidence of rheumatic valvular heart disease. The team will be in Honduras through June 12 to perform cardiac surgery at Honduras Medical Center in the capital city of Tegucigalpa. This is the second trip for Duke Heart for Honduras. The first trip was in 2019.

COVID-19 Update
All the latest Clinical Operations updates related to COVID can be found at https://covid-19.dukehealth.org. Patient-facing resources on DukeHealth.org can be found here: https://www.dukehealth.org/covid-19-update/resources. Duke University maintains a resource page as well, which can be accessed here: https://coronavirus.duke.edu/updates/for-staff.
Upcoming Events & Opportunities
Cardiology Grand Rounds
Cardiology Grand Rounds has concluded and will resume in September. Thanks for joining us – 2021-2022 has been a great year of presentations!
Duke-Stanford Cardiovascular Research Symposium
June 27 & 28. The Duke-Stanford Cardiovascular Research Symposium returns to Durham this year and is offered as a hybrid event. This symposium is sponsored by the Edna and Fred L. Mandel, Jr. Foundation.
offered as a hybrid event. This symposium is sponsored by the Edna and Fred L. Mandel, Jr. Foundation.
Registration required. In person: Great Hall, Mary Duke Biddle Trent Semans Center, Durham, NC. For those who wish to attend virtually, the event will offer live-streaming. The link will be emailed prior to the program. Registrants who choose the virtual live-streamed webinar option will be able to obtain CE credit for the course. For more information, contact Christy Darnell.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Division of Cardiology Publications Indexed in PubMed May 26 – June 1, 2022
Erickson ML, Wang W, Counts J, Redman LM, Parker D, Huebner JL, Dunn J, Kraus WE. Field-Based Assessments of Behavioral Patterns During Shiftwork in Police Academy Trainees Using Wearable Technology. J Biol Rhythms 2022 Jun;37(3):260-271. PM: 35416084.
Généreux P, Kirtane AJ, Kandzari DE, Armstrong EJ, Krucoff MW, Redfors B, Ben-Yehuda O, Lerew DR, Ali ZA, Maehara A, O’Neill WW, Stone GW. Randomized evaluation of vessel preparation with orbital atherectomy prior to drug-eluting stent implantation in severely calcified coronary artery lesions: Design and rationale of the ECLIPSE trial. Am Heart J 2022 Jul;249:1-11. PM: 35288105.
Jones WS, Wruck LM, Harrington RA, Hernandez AF. Iterative approaches to the use of electronic health records data for large pragmatic studies. Contemp Clin Trials 2022 Jun;117:106789. PM: 35545204.
Macedo AVS, de Barros E Silva PGM, de Paula TC, Moll-Bernardes RJ, Mendonça Dos Santos T, Mazza L, Feldman A, Arruda GDAS, de Albuquerque DC, de Sousa AS, de Souza OF, Gibson CM, Granger CB, Alexander JH, Lopes RD. Discontinuing vs continuing ACEIs and ARBs in hospitalized patients with COVID-19 according to disease severity: Insights from the BRACE CORONA trial. Am Heart J 2022 Jul;249:86-97. PM: 35405099.
Petek BJ, Moulson N, Drezner JA, Harmon KG, Kliethermes SA, Churchill TW, Patel MR, Baggish AL. Cardiovascular Outcomes in Collegiate Athletes After SARS-CoV-2 Infection: 1-Year Follow-Up From the Outcomes Registry for Cardiac Conditions in Athletes. Circulation 2022 May 31;145(22):1690-1692. PM: 35545946.
Pfeiffer CT, Paulo JA, Gygi SP, Rockman HA. Proximity labeling for investigating protein-protein interactions. Methods Cell Biol 2022 ;169:237-266. PM: 35623704.
Pokorney SD, Cocoros N, Al-Khalidi HR, Haynes K, Li S, Al-Khatib SM, Corrigan-Curay J, Driscoll MR, Garcia C, Calvert SB, Harkins T, Jin R, Knecht D, Levenson M, Lin ND, Martin D, McCall D, McMahill-Walraven C, Nair V, Parlett L, Petrone A, Temple R, Zhan. Effect of Mailing Educational Material to Patients With Atrial Fibrillation and Their Clinicians on Use of Oral Anticoagulants: A Randomized Clinical Trial. JAMA Netw Open 2022 May 2;5(5):e2214321. PM: 35639381.
Reading Turchioe M, Volodarskiy A, Pathak J, Wright DN, Tcheng JE, Slotwiner D. Systematic review of current natural language processing methods and applications in cardiology. Heart 2022 May 25;108(12):909-916. PM: 34711662.
Sandhu RK, Seiler A, Johnson CJ, Bunch TJ, Deering TF, Deneke T, Kirchhof P, Natale A, Piccini JP, Russo AM, Hills MT, Varosy PD, Araia A, Smith AM, Freeman J. Heart Rhythm Society Atrial Fibrillation Centers of Excellence Study: A survey analysis of stakeholder practices, needs, and barriers. Heart Rhythm 2022 Jun;19(6):1039-1048. PM: 35428582.
Shavadia JS, Alemayehu W, deFilippi C, Westerhout CM, Tromp J, Granger CB, Armstrong PW, van Diepen S. Novel multi-marker proteomics in phenotypically matched patients with ST-segment myocardial infarction: association with clinical outcomes. J Thromb Thrombolysis 2022 May;53(4):841-850. PM: 34708315.
Singer DE, Atlas SJ, Go AS, Lopes RD, Lubitz SA, McManus DD, Revkin JH, Mills D, Crosson LA, Lenane JC, Aronson RS. ReducinG stroke by screening for UndiAgnosed atRial fibrillation in elderly inDividuals (GUARD-AF): Rationale and design of the GUARD-AF randomized trial of screening for atrial fibrillation with a 14-day patch-based continuous ECG monitor. Am Heart J 2022 Jul;249:76-85. PM: 35472303.
Udell JA, Lu D, Bagai A, Dodson JA, Desai NR, Fonarow GC, Goyal A, Garratt KN, Lucas J, Weintraub WS, Forman DE, Roe MT, Alexander KP. Preexisting frailty and outcomes in older patients with acute myocardial infarction. Am Heart J 2022 Jul;249:34-44. PM: 35339451.
Duke Heart Pulse – week ending May 29th 2022
Memorial Day
This has been a difficult week for our country as we continue to struggle with the pattern of senseless gun violence and the safety of our communities. On behalf of the Duke Heart Leadership team, we’d like to wish all of you a very safe and peaceful Memorial Day weekend. As our nation takes time to remember all those who have been lost while serving in the U.S. military, we hope you’re able to spend some time in self-care, in reflection, and hopefully in the company of those most dear to you. Thank you for all that you do to make Duke Heart one of the very best places to work and care for others.
Duke Execs Kick-off Heart Walk Season
Cardiologist Rick Shannon, MD, Chief Quality Officer for Duke Health, is serving as the Triangle-area campaign chair for the 2022 Triangle Heart Walk. He recently hosted two Heart Walk kick-off events for senior leaders across Duke University Health System. The first was held May 12 at Duke University Hospital and the second was held on Thursday morning at Duke Raleigh.
Duke Heart’s leadership team shared highlights and successes of our ongoing partnership with the American Heart Association (AHA) both locally and nationally, as well as personal accounts of why supporting fundraising efforts like the Heart Walk are important. Cardiovascular disease and stroke have impacted most members of our team in some way — and hearing team members share their “why” stories and our efforts toward research, care and prevention was deeply inspiring.
We’re looking forward to a successful Heart Walk this fall–be on the lookout for more information. We’d like to make this our biggest and most successful year, ever! The date of the walk will be announced this summer.
Speaking of our AHA partnership, congratulations to our colleagues in the Duke Stroke Center! Two of their teams from Duke Raleigh Hospital participated in the Triangle CycleNation event held by the AHA on May 17 at Coastal Credit Union Midtown Park at North Hills in Raleigh. The teams raised funds to help fight stroke and increase awareness around stroke prevention and warning signs. Good work!




Highlights: AATS 2022
The American Association for Thoracic Surgery (AATS) 102nd annual meeting took place the weekend of May 14-17 in Boston.
Duke highlights included:
Presentations by thoracic surgeons Betty Tong and Matt Hartwig – they were each recognized during AATS 2022 with separate news briefs in the AATS Daily News on Monday, May 16 .

Tong was highlighted for her AATS presentation, “Lung Cancer Screening in 2022” which she gave on Saturday, May 14. Tong discussed study findings that demonstrate roughly five percent of screen-eligible patients are getting low-dose computed tomography (LDCT) scans of their chest to screen for lung cancer. Fairly recently, the U.S. Preventative Services Taskforce expanded screening guidelines that make an even larger number of patients screen-eligible, but Tong says, “only time will tell if more people get LDCT scans.” In her interview with AATS Daily News, Tong stated, “Adherence to screening guidelines and follow-up is suboptimal right now.” She discussed accessibility, budget constraints, socio-economic issues and general misconceptions about lung cancer screenings as issues that all contribute to low screening rates. See story on p. 4: https://duke.is/855sp.
Hartwig was highlighted to preview his presentation on proposals for an AATS

consensus document, “The Use of Mechanical Circulatory Support (MCS) for Lung Transplantation” which took place on Monday, May 16. “The AATS believes it’s important to provide the latest
guidance on how to best use modern MCS to benefit our patients before, during, and after lung transplantation,” Hartwig says in the piece. “Establishing an expert consensus document would be the most appropriate way to meet our needs.” See story on p. 6: https://duke.is/855sp.
Jacob Schroder presented the AATS consensus statement on DCD heart transplantation,

“Cardiac Transplantation Utilizing Donors Following Circulatory Death” on Saturday evening, May 15. The consensus statement will soon be published in the Journal of Thoracic and Cardiovascular Surgery; Schroder and Carmelo Milano are the first and senior authors.
Early EXACT Trial Findings Presented as AATS Late Breaker
The Epicardial Delivery of XC001 Gene Therapy for Refractory Angina Coronary Treatment (EXACT) trial is a first-in-human clinical trial examining the safety and efficacy of using an adenoviral vector to more efficiently deliver human vascular endothelial growth factor (VEGF) directly into the myocardium with the goal of stimulating angiogenesis in patients suffering from refractory angina due to advanced coronary artery disease (CAD). Readers may recall the trial launched at Duke last summer when study investigator and cardiothoracic surgeon Adam Williams  performed the first procedure on one of our Duke study participants.
performed the first procedure on one of our Duke study participants.
The preliminary findings in a small sample size of participants suggests a dose-response across several efficacy variables and supports continued investigation in the Phase 2 portion of the trial. Early clinical trial results were presented at AATS by Nahush Mokadam of Ohio State’s Wexner Medical Center, one of the site investigators, on Sunday, May 15.
Additional Duke investigators on the trial include: Tom Povsic, Duke site and national PI, and executive committee member E. Magnus Ohman, who Povsic credits with getting  this study to Duke.
this study to Duke.
- Related EXACT news: Povsic presented the 6-month follow up data “Preliminary Safety, Tolerability and Efficacy of Direct Epicardial Administration of Encoberminogene Rezmadenovec (XC001) to Ischemic Myocardium in Patients with Refractory Angina: Six Month Phase 1 Data for the EXACT Trial” at the American Society of Gene and Cell Therapy

Magnus Ohman in Boston on May 18th.
Additional Duke presenters at AATS included faculty members: Thomas D’Amico, Jacob Klapper, David Harpole, Edward Chen and Chad Hughes, as well as the following members of Duke’s general surgery residency program: Vignesh Raman, Christopher Jensen, Kristen Rhodin and Samuel Kesseli.
Impressive work! Congratulations to all!
NCDR Announces 2022 Chest Pain-MI Awards
 We are excited to share our latest performance achievement awards for the American College of Cardiology’s Chest Pain-MI Registry. This week we were notified by the National Cardiovascular Data Registry (NCRD) of our latest ratings across all three hospitals.
We are excited to share our latest performance achievement awards for the American College of Cardiology’s Chest Pain-MI Registry. This week we were notified by the National Cardiovascular Data Registry (NCRD) of our latest ratings across all three hospitals.
- Duke Regional Hospital: Silver
- Duke Raleigh Hospital: Platinum
- Duke University Hospital: Platinum
More than 2,400 hospitals and over 8,500 outpatient providers worldwide participate in one or more of the ACC’s ten registries, such as Chest Pain-MI, forming a comprehensive network of cardiovascular care providers committed to ensuring evidence-based cardiovascular care, improving patient outcomes and lowering health care costs.
The Chest Pain-MI Registry is the most trusted source for outcomes-based, continuous quality improvement, according to the ACC. It is the go-to registry for hospitals and health systems applying ACC and American Heart Association clinical guideline recommendations.
Congratulations to all!
Shout-out to Haney & Ashley!
We received a terrific note this week from Lisa Clark Pickett, Chief Medical Officer for Duke University Hospital, regarding team members Jack Haney and Ciarra Ashley and wanted to share it with you. Pickett wrote:
“Good Morning, Jack and Ciarra,
While reading comments on our Patient Satisfaction Survey I was just delighted to read this lovely compliment about you and your team. Thank you for your continual dedication to patients, professionalism, and excellence!”
The survey note read: “Dr. Haney and his medical team were awesome! Nurses on the 6 East Floor were very attentive to my needs & took excellent care of me. This was the BEST hospital stay for me.” – a grateful patient
Great job!
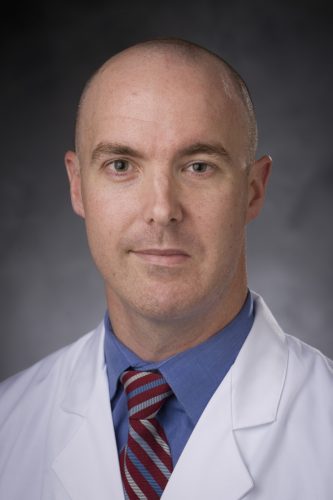

Kudos to Loriaux, Pagidipati!
We’re also sharing some warm compliments we received regarding cardiology fellow Dan Loriaux and faculty member Neha Pagidipati via Duke Health’s StarCard feedback system.

 “Dr. Pagidipati is an exceptional doctor. Dr. Dan Loriaux, fellow at Duke, is a remarkable young man. If he continues with cardiology, there is no one better to add to the Duke team. Both (Dan and Neha) are uniquely gifted,” the patient wrote (names are withheld in StarCard).
“Dr. Pagidipati is an exceptional doctor. Dr. Dan Loriaux, fellow at Duke, is a remarkable young man. If he continues with cardiology, there is no one better to add to the Duke team. Both (Dan and Neha) are uniquely gifted,” the patient wrote (names are withheld in StarCard).
Another wrote, “Excellent, compassionate care by Dr. Pagidipati. None better.”
Well done!
Latorre Nominated For Daisy Award
Amanda Latorre, one of our wonderful nurses on 7100, was recently nominated for a Daisy Award for providing compassionate care. She received the nomination from a patient’s daughter. The daughter had been present with her mother for the duration of the hospitalization as she was hesitant to leave and miss out on important information. Amanda put the daughter’s mind at ease with her excellent bedside manner and strong communication skills which allowed the daughter to leave for a night of good rest. Amanda also provided the patient with fresh toiletries and a moisturizing foot massage.
Thank you, Amanda, for the exceptional care you continue to provide for our Heart patients!

COVID-19 Update
All the latest Clinical Operations updates related to COVID can be found at https://covid-19.dukehealth.org. Patient-facing resources on DukeHealth.org can be found here: https://www.dukehealth.org/covid-19-update/resources. Duke University maintains a resource page as well, which can be accessed here: https://coronavirus.duke.edu/updates/for-staff.
Upcoming Events & Opportunities
Cardiology Grand Rounds
May 31: Heart Failure Cardiogenic Shock and the Golden Circle with Vanessa Blumer. 5 p.m., Webex.
Duke-Stanford Cardiovascular Research Symposium
June 27 & 28. The Duke-Stanford Cardiovascular Research Symposium returns to Durham this year and is offered as a hybrid event. This symposium is sponsored by the Edna and Fred L. Mandel, Jr. Foundation.
Registration required. In person: Great Hall, Mary Duke Biddle Trent Semans Center, Durham, NC. For those who wish to attend virtually, the event will offer live-streaming. The link will be emailed prior to the program. Registrants who choose the virtual live-streamed webinar option will be able to obtain CE credit for the course. For more information, contact Christy Darnell.

Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
May 20 — Richard Shannon
Axios
Red states aren’t prepared for a post-Roe baby boom
https://duke.is/v4vqs
May 23 — Jennifer Rymer
tctMD
DISRUPT PAD III: Lithotripsy Prep Linked to Better PAD Patency at 1 Year
https://duke.is/ycwfv
May 24 — Sunil Rao
Healio
SCAI president discusses results of the DIPRA trial
https://duke.is/5n3s8
May 24 — Marat Fudim
Medscape
Paradigm-Challenging Heart Failure Treatment Strategy Hopeful in Early Trial
https://duke.is/jze4f
Division of Cardiology Publications Indexed in PubMed May 19-25, 2022
Bier EA, Alenezi F, Lu J, Wang Z, Mammarappallil JG, O’Sullivan-Murphy B, Erkanli A, Driehuys B, Rajagopal S. Noninvasive diagnosis of pulmonary hypertension with hyperpolarised Xe magnetic resonance imaging and spectroscopy. ERJ Open Res 2022 May 16;8(2):00035-2022. PM:35586448.
DeVore AD, Hellkamp AS, Thomas L, Albert NM, Butler J, Patterson JH, Spertus JA, Williams FB, Shen X, Hernandez AF, Fonarow GC. The association of improvement in left ventricular ejection fraction with outcomes in patients with heart failure with reduced ejection fraction: data from CHAMP-HF. Eur J Heart Fail 2022 May;24(5):762-770. PM: 35293088.
Jawitz OK, Lawton JS, Thibault D, O’Brien S, Higgins RSD, Schena S, Vemulapalli S, Thomas KL, Zwischenberger BA. Sex Differences in Coronary Artery Bypass Grafting Techniques: A Society of Thoracic Surgeons Database Analysis. Ann Thorac Surg 2022 Jun;113(6):1979-1988. PM: 34280377.
Kelsey MD, Patrick-Lake B, Abdulai R, Broedl UC, Brown A, Cohn E, Curtis LH, Komelasky C, Mbagwu M, Mensah GA, Mentz RJ, Nyaku A, Omokaro SO, Sewards J, Whitlock K, Zhang X, Bloomfield GS. Inclusion and diversity in clinical trials: Actionable steps to drive lasting change. Contemp Clin Trials 2022 May;116:106740. PM: 35364292.
Kwapong YA, Boakye E, Obisesan OH, Shah LM, Ogunwole SM, Hays AG, Blumenthal RS, Creanga AA, Blaha MJ, Cainzos-Achirica M, Nasir K, Douglas PS, Wang X, Sharma G. Nativity-Related Disparities in Preterm Birth and Cardiovascular Risk in a Multiracial U.S. Cohort. Am J Prev Med 2022 Jun;62(6):885-894. PM: 35597568.
O’Brien EC, Sugarman J, Weinfurt KP, Larson EB, Heagerty PJ, Hernandez AF, Curtis LH. The impact of COVID-19 on pragmatic clinical trials: lessons learned from the NIH Health Care Systems Research Collaboratory. Trials 2022 May 21;23(1):424. PM: 35597988.
Rosenberg P. VDAC2 as a novel target for heart failure: Ca at the sarcomere, mitochondria and SR. Cell Calcium 2022 Jun;104:102586. PM: 35429733.
Saldarriaga C, Atar D, Stebbins A, Lewis BS, Abidin IZ, Blaustein RO, Butler J, Ezekowitz JA, Hernandez AF, Lam CSP, O’Connor CM, Pieske B, Ponikowski P, Roessig L, Voors AA, Anstrom KJ, Armstrong PW. Vericiguat in patients with coronary artery disease and heart failure with reduced ejection fraction. Eur J Heart Fail 2022 May;24(5):782-790. PM: 35239245.
Sata SS, Spratt SE, Edmonston DL, Pagidipati N. Clinical progress note: Indications for and management of sodium-glucose cotransporter-2 (SGLT-2) inhibitors in hospitalized patients. J Hosp Med 2022 May;17(5):360-363. PM: 35535917.
Schocken DD. Registry Evidence for Modulation of the Acute Ischemic Heart Disease Pathway: Statins Prevent Heart Failure? J Am Coll Cardiol 2022 May 24;79(20):2034-2036. PM: 35589165.
Stacey RB, Hall ME, Leaverton PE, Schocken DD, Zgibor J. Relation of glycemic status with unrecognized MI and the subsequent risk of mortality: The Jackson Heart Study. Am J Prev Cardiol 2022 May 10;11:100348. PM: 35600110.
Udell JA, Jones WS, Petrie MC, Harrington J, Anker SD, Bhatt DL, Hernandez AF, Butler J. Sodium Glucose Cotransporter-2 Inhibition for Acute Myocardial Infarction: JACC Review Topic of the Week. J Am Coll Cardiol 2022 May 24;79(20):2058-2068. PM: 35589167.

Recent Comments