Duke Heart Pulse – Updates from the week ending April 24th 2022
Sunil Rao, MD to take New Role Leading Interventional Cardiology at NYU Langone
It is bittersweet that we announce that Sunil Rao has accepted the position of Director of Interventional Cardiology for the NYU Langone Health System where he will work to facilitate coordination, program development, uniform quality standards, operational efficiency, financial goals and best practices across the NYULH System Cardiac Catheterization Laboratories.
We are extremely excited for Sunil and thrilled that he will be taking on this important leadership opportunity to continue to innovate the care of patients undergoing invasive procedures, and certain his impact and skill will be immediately felt across the NYU Langone cath labs.
He will be missed at Duke where he has been a friend, trusted colleague, mentor, teacher, and consummate interventionalist over the last 26 years. Sunil came to Duke after completing medical school at The Ohio State University and did his medical residency and cardiology, and interventional fellowship at Duke. Since coming on Faculty, he has been a north star for our invasive labs – studying, teaching, and ushering in radial procedures, best cath practices, and playing an instrumental role in how we think about and train the next generation of leaders in cardiology. His impact can be seen based on the number of fellows, trainees, and colleagues that look to work with him. He has been the repeatedly been the recipient of fellowship mentorship and teaching awards. Academically, he is an internationally recognized clinical investigator involved in many of the seminal trials in interventional cardiology around management of patients undergoing invasive procedures, including devices, access site, and treatment strategies.
He is also the current Chief of Cardiology at the Durham VA where is has helped transform the cardiovascular care of our veterans while supporting the faculty. He is currently the editor of Circulation Cardiovascular Interventions and will be the President of the Society for Cardiovascular Angiography and Intervention (SCAI) in May 2022. He is the true triple threat.
Personally, what I will miss most is the camaraderie, fun, and drive for excellence that Sunil brought to Duke every day.
Reflecting on his time at Duke, Sunil said, “Duke has been my home for 26 years and I consider the Cardiology division my family. The mentorship, collaborations, and friendships over the years have been integral to my personal and professional life. Although I will be leaving Duke, Duke will always be part of who I am. It’s really been a privilege to be part of Duke Heart.”
Congratulations Sunil – you will certainly be missed and we look forward to collaborating in the future.
Duncan Recognized for 36 Years of Service in Heart
Lisa Duncan will be retiring on May 2, 2022 after more than 36 years of service. Lisa has worked in the Heart Center since 1987  in varying roles including professional nursing assistant, nursing assistant, staff nurse, assistant head nurse and, since the 1990’s, as 7100 Nurse Manager of Operations. Throughout her time at Duke, she served on many task forces and committees.
in varying roles including professional nursing assistant, nursing assistant, staff nurse, assistant head nurse and, since the 1990’s, as 7100 Nurse Manager of Operations. Throughout her time at Duke, she served on many task forces and committees.
She received the highly esteemed Mary Ann Peter Friends of Nursing Award for excellence. Lisa is known for her approachability, fair and consistent practice, and patient/staff advocacy.
On behalf of the entire Duke Heart Center Leadership team, we thank Lisa for her loyalty and dedication to our patients, the faculty and staff of Duke Heart, as well as to Duke University Hospital.
Please join us in wishing her well in her retirement!
Heart Transplant Team Celebrates Donate Life Month
April is Donate Life Month and members of our heart transplant team were overjoyed to celebrate in person this year by attending the NC Gift of Life Gala which was held Thursday, April 21 at the Prestonwood Country Club in Cary. There, they enjoyed interacting as a team, bidding on artwork by local artists, hearing from organ recipients, and enjoying the delicious dinner and the silent auction.
The theme of the Gala this year was the HeART of the Matter, marking the use of the red heart on NC state drivers’ licenses for all those who promise to give the gift of life by becoming an organ donor. The team asks if you are not a registered organ donor, please consider becoming one!

Shown here are (L to R): Rotunda Kearney, Melissa Shreve, Tia Thompson, Emily Schneidewind, Sam Murari, Kris Barnes, Cathy Alligood and Sonia Leon.
Rotunda is a program specialist for the heart transplant team. Sonia and Sam are pre-heart transplant coordinators. Tia, Emily, Melissa, Kris and Cathy are post-heart transplant coordinators.
Special thanks to Chet Patel and Adam DeVore for giving their team the opportunity to attend and represent Duke Heart Transplant.
NC Organ Donation Fast Fact: In 2019, when North Carolina Governor Roy Cooper signed into law SB 210 Organ and Tissue Donation/Heart Heroes, it brought North Carolina into parity with the rest of the nation by including tissue for transplantation along with organs and eyes when one says “Yes” to donation at the DMV. Today, anyone who says “Yes” to donation at the NCDMV will be making a legal first-person authorization to become an organ, eye, and tissue donor upon death. Those who had the heart symbol placed on their drivers’ license or ID card before October 1, 2019 must take an extra step to add tissue donation to their registry status by visiting DonateLifeNC.org. Changes to your donor registration status can be made at any time by visiting the same site.

Shout-Out to Duke’s HF Guidelines Contributors
A big shout-out to Duke Heart team members who served as authors, reviewers or ACC/AHA/HFSA Joint Committee Members for the recently published 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. We are deeply grateful for the effort each of you have put into this effort – your work helps educate others and saves lives. Well done, Adrian Hernandez, Carmelo Milano, Sana Al-Khatib, Schuyler Jones and Dan Mark!
Kudos to Senman!
We are always pleased to hear about the great work our fellows are doing. This week, we heard about Balim Senman from  Corey Fry, our APP Team Lead in the Cardiac Intensive Care Unit via a note to Anna Lisa Chamis:
Corey Fry, our APP Team Lead in the Cardiac Intensive Care Unit via a note to Anna Lisa Chamis:
“I’d like to take a moment to recognize Dr. Balim Senman for the exceptional work she’s doing in CICU. Dr. Senman has been a leader, communicator, and positive source of support in CICU through the changes we’ve faced as a team over the past year.
“The CICU runs smoothly when Dr. Senman is working …and APP’s feel supported and heard. Her solution-based focus has made her a valuable partner in addressing workflow processes with the APP group… I appreciate her input and feedback. She’s an exceptional fellow with a bright future and I’m glad to have opportunity to work with her.”
Nicely done, Balim!!
Kudos to Lin!
Shu Lin was recently commended by Andrea Carpenter, president of the Thoracic Surgery Directors Association (TSDA) and Matthew Romano, the In-Training Exam Cardiac Subcommittee Chair of the TSDA, for his contributions to the TSDA’s 2022 In-Training Exam and for his work as a member of the ITE Cardiac Subcommittee. Great work Shu! Thank you for representing Duke Heart!

Cybersecurity Advisory Alert
A critical message was issued to all employees on Thursday by Jeff Ferranti, MD, chief digital officer and senior vice president for DUHS and Randy Arvay, PhD, chief information security officer for DUHS.
Due to the Russian invasion of Ukraine, the U.S. Department of Health & Human Services Health Sector Cybersecurity Coordination Center and Health-ISAC has issued a joint advisory for credible cybersecurity threats to U.S. critical infrastructure sectors.
Duke Health has been responsive and continues to expand our defense strategies. Initial actions prioritized leveraging our strong vendor partnerships and intelligence feeds to monitor for indicators of threats. But, we still need all Duke Health employees to remain vigilant and assist in protecting our systems and resources.
How to Safeguard Against Cyber Threats
We have seen an increase in suspicious email, phone calls, and text messaging to Duke staff, including some that have spoofed/faked prominent Duke leader names.
At this time, we feel that it is important to remind all staff of key steps that you can take, including:
- Staying vigilant around the potential for social engineering and phishing via email, phone (vishing), text (smishing) and social media. Do not click links or attachments or give out personal or sensitive information. Always independently verify that requests are coming from a known, trusted source.
- Using strong, unique passwords and multi-factor authentication (MFA) on all accounts. Duke offers a free password manager to all staff (oit.duke.edu/what-we-do/services/1password) and encourages staff to set their MFA preference to “Always” (idms-mfa.oit.duke.edu).
- Patching/Updating all software and running current Antivirus on personal devices.
- Avoiding use of free or untrusted Wi-Fi.
- Report all suspicious emails using ReportPhish in Outlook or other concerning activity or by contacting security@duke.edu.
Each of us, working together, can do our part to ensure the safety of our patients, their loved ones and each other.
Thank you for your continued vigilance!
NC Walk for Victory Raises $50K
Duke Heart was very proud to serve as the presenting sponsor of the NC Walk for Victory held yesterday at Laurel Hills Park in  Raleigh. The NC Walk for Victory raises much needed funding to support patients with Marfan syndrome, Loeys-Dietz, VEDS and related conditions. We had a really great day – and the teams exceeded their $50K fundraising goal — a testament to their dedication to research, programming and services offered by the Marfan Foundation
Raleigh. The NC Walk for Victory raises much needed funding to support patients with Marfan syndrome, Loeys-Dietz, VEDS and related conditions. We had a really great day – and the teams exceeded their $50K fundraising goal — a testament to their dedication to research, programming and services offered by the Marfan Foundation
Chad Hughes served as the medical director for the event. Hughes, Melissa Burkett and their team have done an incredible job of welcoming more patients and their families to Duke and providing access to treatment and support not readily available elsewhere. Great job!
Thanks to all who donated and walked to support our patients and their families!

Sports Cardiology & Sudden Death in Athletes CME
The Duke Sports Cardiology & Sudden Death in Athletes Symposium was held yesterday, April 23 with course directors Jim Daubert and Bill Kraus. The virtual event drew just over 160 registrants. Guest speakers included Duke faculty members Igor Klem, Howard Rockman, Jeff Bytomski, Hap Zarzour, Al Sun and Kenzie Johnston along with Aaron Baggish (Mass General) and Norbert Guettler (Central Military Hospital, Koblenz, Germany). Shout-out to Christy Darnell for terrific planning! The CME was free to attend; enduring material can be accessed for up to two years by registering and obtaining the link. To do so, please visit https://duke.is/gkffw.
directors Jim Daubert and Bill Kraus. The virtual event drew just over 160 registrants. Guest speakers included Duke faculty members Igor Klem, Howard Rockman, Jeff Bytomski, Hap Zarzour, Al Sun and Kenzie Johnston along with Aaron Baggish (Mass General) and Norbert Guettler (Central Military Hospital, Koblenz, Germany). Shout-out to Christy Darnell for terrific planning! The CME was free to attend; enduring material can be accessed for up to two years by registering and obtaining the link. To do so, please visit https://duke.is/gkffw.
Reves Lecture
Mark F. Newman, MD, Executive Vice President of Health Affairs at the University of Kentucky, former president of the Duke PDC and former chair of Duke Anesthesiology delivered Cardiology Grand Rounds on Tuesday evening and the Reves Lecture/Anesthesiology Grand Rounds on Wednesday morning. It was great to have Mark back on campus! (Pictured are Joe Mathew and Newman.) If you were unable to attend the Reves Lecture, it can be viewed here: https://dukemed.mediasite.com/Mediasite/Play/bd690445bc724c8488afab4226b6891a1d. Note, the main presentation begins approximately 17 minutes into the video.

COVID-19 Update
All the latest Clinical Operations updates related to COVID can be found at https://covid-19.dukehealth.org. Patient-facing resources on DukeHealth.org can be found here: https://www.dukehealth.org/covid-19-update/resources. Duke University maintains a resource page as well, which can be accessed here: https://coronavirus.duke.edu/updates/for-staff.
Upcoming Events & Opportunities
Cardiology Grand Rounds
April 26: Clinicopathologic Conference with Francis Ugowe. 5 p.m. via Webex.
May 3: Topic TBA with Navid Nafissi. Details forthcoming.
May 10: Topic TBA with Caitlin Dresher. Details forthcoming.
MDEpiNet Spring 2022 Virtual Mini-Think Tank
May 5: MDEpiNet Spring 2022 Virtual Mini-Think Tank. Noon – 5:30 p.m., ET
MDEpiNet Predictable And SuStainable Implementation Of National CardioVascular Registries (PASSION CVR) Registry-Supported Prospective Clinical Trials
Join and invite your colleagues to join for updates from, and dialogues across our Registry-supported Prospective Trials Working Groups:
- Data Governance & Access
- Operational Roles & Responsibilities
- Global Regulatory Acceptance
- Use Cases:
- Aortic Intervention
- Heart Valves
- Mechanical Circulatory Support
- Peripheral Arterial Intervention
Registration now open: https://duke.qualtrics.com/jfe/form/SV_2f6JBD6WfaF9jBc.
Evening with Heart Raleigh
An Evening with Heart Raleigh, which has been rescheduled from earlier this year, will benefit Marfan families as well as those with Loeys-Dietz (LDS), Vascular Ehlers-Danlos (VEDS), and related conditions.
May 5, 2022
The Maxwell
7-10 p.m.
Cocktail attire
Tickets for the event include open bar, taco bar, heavy appetizers, dessert, silent auction, DJ, and a fun photo booth. For those unable to attend in person but who would like to participate, the silent auction items can be bid on online from anywhere. Lots of cool items have been donated so far! For tickets, more information or silent auction viewing and bidding, please visit: https://marfan.ejoinme.org/raleigh22.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
April 15 — Richard Shannon
WNCN, CBS-17
Annual campaign aims to improve maternal health outcomes for Black women
https://duke.is/zwp56
April 15 — Jonathan Piccini
DotMed/HealthCareBusiness News
Patients with infected cardiac implants should have them removed
https://duke.is/nmm2j
April 16 — Robert Mentz
Healio/Cardiology Today
Editors of HF journal question use of the word ‘candidate’
https://duke.is/b67cp
April 21 — Kevin Oeffinger (Duke Cancer Institute)
Healio/Hematology-Oncology
Cardiovascular care of pediatric cancer survivors: Mitigating a lifelong risk
https://duke.is/whpd9
April 22 — Sean Pokorney
Cardiology Advisor
ACC: Infected CV Implantable Electronic Devices Often Not Removed
https://duke.is/jvyyc
Duke Heart Pulse week ending April 17th 2022
Chief’s message:
This weekend hopefully you all got some time to spend with family around Easter, Ramadan, Passover, or just to get time spend together. The last few years have taught all of use to ensure we enjoy the moments with friends and family to recharge. Personally, we want to thank the Duke Heart teams that have continued to pull together for our patients and each other in the ever changing world of health care.
Highlights of the week:
Shout-out to Duke Heart teams
A tremendous shout-out to Duke Heart team members throughout our clinical care areas, in particular to our interventional teams. As many of you know, the EP and Cath Labs were tremendously busy this past week!

According to Anna Mall, cases in the cath lab began to spike on Friday, April 8 with a record setting 38 cases completed. She added that on Monday alone, 44% of cases were PCI, including four STEMI. Tuesday, the trend continued with 32 cases and multiple STEMI activations. Volume hadn’t waned toward the end of the week — the teams continued to see busy outpatient and inpatient case volumes.
“Special thanks to the cath lab staff, fellows and faculty for the amazing teamwork handling incredibly busy days – all with a smile!!” — Anna Mall
The interventional teams really pulled together to establish unique work flows in order to manage this uptick in patient cases, according to Jill Engel, associate VP, Duke Heart.
We’d like to add a special shout-out to Andrew Wang, MD, who has been exceptional with morning bed flow call. Across the board, we thank all cardiologists and nursing teams for helping manage bed capacity and patient care. This has been a truly busy time for everyone and Duke Heart leadership appreciates the way everyone has pulled together to help.
THANK YOU! We appreciate all that you and your teams are doing to take great care of our patients and to keep everyone safe. Great job, everyone!!!
Wrobel Named Chief Cardiology Fellow
We are pleased to share the wonderful news that our Duke Cardiology fellows have selected Dr. Christopher Wrobel as their 2022-2023 Chief Cardiology Fellow. The announcement was made earlier this week by fellowship director Anna Lisa Chamis, MD.

Wrobel was born and raised in Valparaiso, IN. He obtained a BS in chemistry from Duke in 2009. After teaching high school chemistry in New Orleans for two years, he returned to Indiana for medical school. There he met his wife, Dr. Heather Wolfe. Wrobel completed his internal medicine residency at University of Texas Southwestern (UTSW) in 2018. He worked as a hospitalist for one year at UTSW before returning to Duke for cardiology fellowship.
He will complete his Advanced Heart Failure and Transplant Cardiology fellowship in June. Heather and Chris are expecting their first child later this month. In his spare time, Chris enjoys traveling, moonlighting as an amateur restaurant critic, exploring Old World wine, and irrationally supporting his favorite sports teams.
Wrobel will transition to his new role in June. (Photo shows Drs. Chris and Heather Wrobel.)
Please join us in congratulating Chris and welcoming him to his new role!
Thank-you to Coniglio!
Please join us in thanking Dr. Amanda Coniglio for serving as the Cardiology fellowship Chief Fellow this past year. She has worked tirelessly to advocate for the fellows. In a message to the team this week, Dr. Anna Lisa Chamis shared the following:
“Dr. Coniglio’s impact on our fellowship program has been substantial! In particular, she started a bi-monthly fellows’ Critical Care conference, sent weekly educational and informational summaries to all the fellows with references and championed the return to in-person gatherings – in addition to the routine Chief Fellow responsibilities.

Coniglio will be joining the advanced heart failure team at Rochester General Hospital after graduation.” Amanda is shown here with her husband, Dr. Andrew Coniglio.
When asked about her experience this year, Dr. Coniglio said, “I am incredibly grateful for the opportunity to have served as chief this past year and am hopeful that the initiation of CICU case conferences and weekly conference summaries have been an educational resource to all. Congratulations and best wishes to Dr. Wrobel on being elected as chief!”
Coniglio will transition the Chief Fellow role to Dr. Chris Wrobel during June.
Great job, Amanda!
Patel Receives SOM Faculty Award
Manesh Patel, MD, professor of medicine and chief of the Division of Cardiology, has been selected to receive the School of Medicine’s Career Mentoring Award in Clinical Research – Population Health. Patel commented that he was “Humbled for the opportunity to work with some of the best colleagues, fellows, and faculty in cardiovascular medicine. Also appreciative of those that have supported, mentored and taught me including Bob Harrington, Rob Califf, Pam Douglas, Chris O’Connor and many others.”
Chen Inducted to ASA
Congratulations to Edward P. Chen, MD, chief of the Division of Cardiovascular and Thoracic Surgery! Chen was inducted into the American Surgical Association during their 142nd annual meeting held April 7-9 in Chicago at the Chicago Marriott Downtown Magnificent Mile.
Way to go!
Shah to Lead ASPC Group
Congratulations to Nishant Shah! He has been selected to serve a 1-year term as Chair of the Fellow-in-Training and Early Career Working Group of the American Society for Preventive Cardiology.
Mark Newman to Deliver Reves Lecture
This week, Dr. Mark F. Newman, Executive Vice President of Health Affairs at the University of Kentucky, former president of the Duke PDC and former chair of Duke Anesthesiology, will deliver Cardiology Grand Rounds and the Reves Lecture. Both events promise to be excellent and both are listed in the event section below. Not to be missed!
COVID-19 Update
Second Booster Shot Available for Eligible Faculty, Staff and Students
Duke is now offering second booster shots of the COVID-19 vaccine for eligible faculty, staff and students over the age of 50, as well as anyone who is considered severely immunocompromised to increase their protection against severe disease.
Following approval by the U.S. Food and Drug Administration and the Centers for Disease Control and Prevention last week, Duke will offer the Pfizer vaccine as a second booster shot for those who have had their first booster shot at least four months ago. The second booster shot is not currently required for Duke students, faculty or staff, but it is offered as an option for those who are eligible.
Second booster shots are available by appointment or walk-in at the Duke Medical Pavilion in Conference Room 2w91, Duke Clinic 1J, Duke Regional Hospital and Duke Raleigh Hospital. For more information or to schedule an appointment, visit the Duke COVID Vaccine website. Eligible faculty, staff and students are also encouraged to consider vaccination options at local pharmacies or their healthcare provider.
All the latest Clinical Operations updates related to COVID can be found at https://covid-19.dukehealth.org. Patient-facing resources on DukeHealth.org can be found here: https://www.dukehealth.org/covid-19-update/resources. Duke University maintains a resource page as well, which can be accessed here: https://coronavirus.duke.edu/updates/for-staff.
Upcoming Events & Opportunities
Cardiology Grand Rounds
April 19: Treating the Epidemic after the Pandemic with Mark Newman, University of Kentucky. 5 p.m., DN 2002 or online via Webex.
Reves Lecture/Anesthesiology Grand Rounds
April 20: Reves Lecture: Creating Alignment for a Healthier State with Mark Newman, University of Kentucky. 7 a.m., DN 2001 or online via Webex. (Link will not be available until 4/18)
Dr. Mark Newman currently serves as Executive Vice President of Health Affairs at the University of Kentucky. The Reves Visiting Professorship and Lecture is supported by the philanthropic efforts of our donors in honor of Jerry Reves, MD, former chair of Duke Anesthesiology.
Note: seating for the in-person lectures on April 19 & 20 will be limited to half the room capacity due to COVID protocols.
Duke Heart CME
April 23: Duke Sports Cardiology & Sudden Death in Athletes Symposium with course directors Jim Daubert and Bill Kraus. Virtual. For information or to register, please visit: https://duke.is/gkffw. If you have additional questions, please contact Christy Darnell christy.darnell@duke.edu or 919-880-8686.
MDEpiNet Spring 2022 Virtual Mini-Think Tank
May 5: MDEpiNet Spring 2022 Virtual Mini-Think Tank. Noon – 5:30 p.m., ET
MDEpiNet Predictable And SuStainable Implementation Of National CardioVascular Registries (PASSION CVR) Registry-Supported Prospective Clinical Trials
Join and invite your colleagues to join for updates from, and dialogues across our Registry-supported Prospective Trials Working Groups:
- Data Governance & Access
- Operational Roles & Responsibilities
- Global Regulatory Acceptance
- Use Cases:
- Aortic Intervention
- Heart Valves
- Mechanical Circulatory Support
- Peripheral Arterial Intervention
Registration now open: https://duke.qualtrics.com/jfe/form/SV_2f6JBD6WfaF9jBc.
Marfan NC Walk for Victory, April 23
The North Carolina Walk for Victory to support Marfan patients and their families will take place on Saturday, April 23, 2022 from Noon to 3 p.m. at Laurel Hills Park on Edwards Mill Road in Raleigh.
Duke Heart is proud to serve as the presenting sponsor and we are excited for Chad Hughes, MD to serve as medical chair for the walk.
Please help us support all Marfan families as well as those with Loeys-Dietz (LDS), Vascular Ehlers-Danlos (VEDS), and related conditions. Donate or come join us at the event! Parking is easy to access and free.
Walk for Victory is The Marfan Foundation’s global walk program. The event is low-key, fun and family-oriented. To learn more or to register for this event, please visit: https://give.marfan.org/event/2022-north-carolina-walk-for-victory/e353032.
To learn more about The Marfan Foundation, please visit marfan.org.
Evening with Heart Raleigh
May 5, 2022
The Maxwell
7-10 p.m.
Cocktail attire
(This event was rescheduled from earlier in the year.) For those unable to attend in person but who would like to participate, the silent auction items can be bid on online from anywhere. Lots of cool items have been donated so far! Tickets for the event include open bar, taco bar, heavy appetizers, dessert, silent auction, DJ, and a fun photo booth. Proceeds benefit The Loeyz-Dietz and Marfan Foundation. For tickets, more information or silent auction viewing and bidding, please visit: https://marfan.ejoinme.org/raleigh22.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
April 8 — G. Michael Felker
tctMD
METEORIC-HF: Omecamtiv Mecarbil Doesn’t Boost Exercise Capacity in HFrEF
https://duke.is/v4q88
April 8 — Sean Pokorney
U.S. News & World Report
Few People Get Infected Heart Devices Removed, Despite Benefit
https://duke.is/z8zbz
*this story was carried by 10 additional news outlets including UPI, HealthDay and MSN News
April 10 — Mark Sendak and Cara O’Brien (DIHI)
The Wall St. Journal
How Hospitals Are Using AI to Save Lives
https://duke.is/mucf7
April 11 — Sean Pokorney
Cardiovascular Business
VIDEO: Lowering mortality rates from infected EP implantable cardiac devices
https://duke.is/jypq3
April 11 — Jonathan Piccini
Healio/Cardiology
Fitbit receives FDA clearance for algorithm to detect AF
https://duke.is/ywqnc
April 11 — Sean Pokorney
HealthDay
ACC: Infected CV Implantable Electronic Devices Often Not Removed
https://duke.is/rfc5n
April 12 — Christopher Granger
tctMD
Managing AF Patients Undergoing PCI—Some Lingering Questions
https://duke.is/zmez8
April 12 — Duke University (CIED ACC LBCT)
Becker’s Hospital Review
https://duke.is/6vcuk
Duke Heart Pulse week ending April 10th 2022
Highlights of the week:
ACC.22: Looking Back
There were so many excellent presentations across ACC – great job, everyone! Sana Al-Khatib submitted the following thoughts to us regarding the outstanding presentations by our cardiology fellows:
It was very uplifting to connect with friends and colleagues at ACC22 and learn about the latest scientific discoveries that will benefit our patients. To me, the main highlight of the meeting was our fellows’ strong presence and participation.
 Vishal Rao gave a very informative and interesting presentation on intravascular blood volume analysis and hemodynamic measures of vascular compliance in patients hospitalized with heart failure. Kelly Arps did a great job presenting novel data on time to relapse after weaning immune suppressive therapy in cardiac sarcoidosis. Vanessa Blumer gave a very engaging and insightful presentation on whether a PA catheter is needed for the cardiogenic shock patient (to which my answer is always ‘yes ’; my view on this has not changed since my fellowship ). Josephine Harrington did an excellent job presenting powerful data on NOAC use in patients with atrial fibrillation and reduced renal function in the COMBINE-AF database (the largest analysis on this topic to date). Anthony Peters gave a very important and clinically relevant presentation on decongestion, quality of life and outcomes among patients hospitalized for HFrEF versus HFpEF. Michelle Kelsey masterfully facilitated a discussion on managing the patient with obesity, new onset diabetes, and a family history of CV disease. Both Josephine and Vanessa did a great job moderating poster sessions.
Vishal Rao gave a very informative and interesting presentation on intravascular blood volume analysis and hemodynamic measures of vascular compliance in patients hospitalized with heart failure. Kelly Arps did a great job presenting novel data on time to relapse after weaning immune suppressive therapy in cardiac sarcoidosis. Vanessa Blumer gave a very engaging and insightful presentation on whether a PA catheter is needed for the cardiogenic shock patient (to which my answer is always ‘yes ’; my view on this has not changed since my fellowship ). Josephine Harrington did an excellent job presenting powerful data on NOAC use in patients with atrial fibrillation and reduced renal function in the COMBINE-AF database (the largest analysis on this topic to date). Anthony Peters gave a very important and clinically relevant presentation on decongestion, quality of life and outcomes among patients hospitalized for HFrEF versus HFpEF. Michelle Kelsey masterfully facilitated a discussion on managing the patient with obesity, new onset diabetes, and a family history of CV disease. Both Josephine and Vanessa did a great job moderating poster sessions.
Seeing our fellows share their research findings and knowledge on a national stage was incredibly  rewarding. Indeed, having the opportunity to work with superb trainees is one of the best aspects of our work at Duke. Kudos to our fellows and the faculty mentoring them!
rewarding. Indeed, having the opportunity to work with superb trainees is one of the best aspects of our work at Duke. Kudos to our fellows and the faculty mentoring them!
We agree, Sana! Our trainees are superb and we are so proud of them!
Additionally, Schuyler Jones let us know that the VALOR HCM team presented positive trial results on Saturday at ACC. Duke was the 6th highest enrolling site and Kim Biever was one of the CRCs recognized on the enrollment ranking. Great job, Kim and to Duke’s VALOR HCM team!
We also learned that Midge Bowers led Cardio-OB simulations at ACC. Way to go!



Our late-breaker teams received quite a bit of news coverage this week. Check it out below in our news section.
Mentz Recognized with Master CardioNerd Award

We were thrilled to learn this week that Robert Mentz was selected for the Master CardioNerd Award by the CardioNerds team.
“It is with the utmost respect, gratitude, and privilege that we offer you the Master CardioNerd Award. This honor is awarded to a faculty who ‘supports the mission to democratize cardiovascular education.’
The CardioNerds Clinical Trials Network is a major credit to your mentorship, innovation, and vision. We are hopeful that the lessons from this program will be applicable to other subspecialties as we learn how best to enhance trial enrollment that is both efficient and equitable as well as nurture careers in clinical research.
We are also very excited to produce the Decipher the Guidelines Series for the 2022 HF Guidelines with yourself and Dr. Anu Lala as Series Mentors.
CardioNerds is just a 28-month old toddler. Your constant support, mentorship, and encouragement has helped us mature into the platform it is today. We are eternally grateful and will continue benefiting from your inspiration as we look beyond our terrible twos.”
The message was signed by CardioNerds co-founders Amit Goyal, MD, cardiovascular fellow at the Cleveland Clinic and Daniel Ambinder, MD, interventional/structural cardiology fellow at Johns Hopkins.
The video is a must-see: https://twitter.com/i/status/1512374750114459654
Congratulations, Rob!!!
Rymer, Greene Receive AHA Career Development Awards

Congratulations to Jennifer Rymer, MD and Stephen Greene, MD! Both have

been notified that they’ll be receiving Career Development Awards from the American Heart Association.
Rymer’s project title is Implementation of a Medication Adherence Instrument Among Patients with Symptomatic Peripheral Artery Disease after PVI. Her mentors include: Tracy Wang, Schuyler Jones, Hayden Bosworth, Sharron Docherty, and Manesh Patel. Her funding is for three years, effective April 1.
Greene’s project title is Use and Effectiveness of Outpatient Intravenous Diuretic Therapy as Treatment of Worsening Heart Failure. He will study the clinical and economic implications of treating select patients with worsening heart failure using an outpatient IV diuretic strategy, as compared with a traditional strategy centered on hospitalization. His mentors include G. Michael Felker, Adrian Hernandez, Brad Hammill, Javed Butler of the University of Mississippi Medical Center, and Greg Fonarow at UCLA. Funding is for three years, effective April 1.
Such great news! Congratulations!
Kudos to Glower
We received the following note regarding Donald Glower, MD:

“Good Afternoon, I had the opportunity to spend time this afternoon with a patient who was being discharged from 3300 after valve surgery by Dr. Glower. He was effusive in his praise for his team. He noted that Dr. Glower communicated well and rounded on him, personally, often 2 times/day. He felt lucky to have had the very best for his surgery. He noted that his nurses, especially all in the ICU (whose names he could not recall) and Connie on 3300 were outstanding. He also called out by name Valerie, who kindly took his food order and was so professional and caring. He feels like he has a new lease on life and is grateful for your care. Thank you all for the part you have played and please forward this to those whose last names I do not have. Very best wishes, Lisa”
Lisa Clark Pickett MD FACS
Assistant Professor of Surgery and Medicine, Duke University & Chief Medical Officer, Duke University Hospital
Great work, Don!
Harpole Named Geller Distinguished Professor
We are pleased to share with you that thoracic surgeon David H. Harpole, Jr., MD, professor of surgery in the Division of Cardiovascular and Thoracic Surgery, will be named the George Barth Geller Distinguished Professor for Research in Cancer effective July 1, 2022.
Wonderful news, David! Congratulations!!
Kudos to Carlisle
 We received the following note regarding cardiology fellow Matt Carlisle:
We received the following note regarding cardiology fellow Matt Carlisle:
“Dr. Matt Carlisle came to see a rapidly decompensating patient in the Emergency Department recently. He had just began his shift when he received a phone call from the ED Cardiology Consult provider about an unstable patient. He came immediately to bedside to assess the patient. Ultimately, he placed an urgent temporary pacemaker in the patient. Dr. Matt Carlisle is always attentive to patient needs, and is super kind and helpful to his coworkers.” — Jordan Hausladen, Advanced Practice Provider, Division of Cardiology
Way to go, Matt!
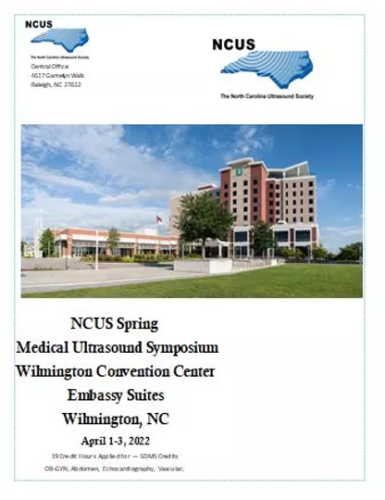
Duke Sonographers Attend NCUS
The North Carolina Ultrasound Society’s 42nd annual Spring Symposium was held last weekend in Wilmington, NC. Congratulations to the Duke Heart CDU and Duke Cardiac Ultrasound Program for representing Duke at the conference this year!
Cardiac Sonographer Jon Owensby gave the Saturday morning lecture on Aortic Stenosis Evaluation and cardiac sonographer Jayne Leypoldt gave the Sunday morning lecture on Mitral Regurgitation; student Courtney Snyder entered the Scientific Exhibit competition, winning 3rd place for a stellar exhibit on Pericardiocentesis!
We have an incredible and active sonography team within Duke Heart! Great job!



Duke Heart Network Visit to Frey Regional
Members of the Duke Heart Network and Duke Heart leadership team received a warm welcome at Frey Regional during a site visit held on March 21.
Shown L-R are: Jill Engel, Katie Troxler, Desiree Bonadonna, Lisa Kotyra, Trevor Krawchuk, Dr. Edward P. Chen, Dr. Brett Starr (CT surgeon at Frey) and Pam Peaks.

Palma Appointed Commissioner for CAAHEP
Richard Palma, program director of the Duke Cardiac Ultrasound Certificate Program, has been  appointed as a commissioner for the Commission on Accreditation of Allied Health Education Programs (CAAHEP) representing Hospital/VA Based Educational Institutions.
appointed as a commissioner for the Commission on Accreditation of Allied Health Education Programs (CAAHEP) representing Hospital/VA Based Educational Institutions.
His 3-year term began late last month. Congratulations, Richie!
Join the NC Walk for Victory, April 23 – Support Marfan!
We are looking forward to the upcoming NC Walk for Victory in support of the Marfan Foundation and the many families they help. The walk is coming up on Saturday, April 23. Event details are below, under “events”. We have 125 registered participants with seven new families joining the walking teams from 2021. Please consider joining us! To learn more, visit: https://duke.is/phzdy.
COVID-19 Updates
Second Booster Shot Available for Eligible Faculty, Staff and Students
Duke is now offering second booster shots of the COVID-19 vaccine for eligible faculty, staff and students over the age of 50, as well as anyone who is considered severely immunocompromised to increase their protection against severe disease.
Following approval by the U.S. Food and Drug Administration and the Centers for Disease Control and Prevention last week, Duke will offer the Pfizer vaccine as a second booster shot for those who have had their first booster shot at least four months ago. The second booster shot is not currently required for Duke students, faculty or staff, but it is offered as an option for those who are eligible.
Second booster shots are available by appointment or walk-in at the Duke Medical Pavilion in Conference Room 2w91, Duke Clinic 1J, Duke Regional Hospital and Duke Raleigh Hospital. For more information or to schedule an appointment, visit the Duke COVID Vaccine website. Eligible faculty, staff and students are also encouraged to consider vaccination options at local pharmacies or their healthcare provider.
All the latest Clinical Operations updates related to COVID can be found at https://covid-19.dukehealth.org. Patient-facing resources on DukeHealth.org can be found here: https://www.dukehealth.org/covid-19-update/resources. Duke University maintains a resource page as well, which can be accessed here: https://coronavirus.duke.edu/updates/for-staff.
Upcoming Events & Opportunities
Cardiology Grand Rounds
April 19: Treating the Epidemic after the Pandemic with Mark Newman (University of Kentucky). 5 p.m. In-person, DN2002. Online link coming soon.
April 20: Alignment for a Healthier State (Reves Lecture) with Mark Newman (University of Kentucky). 7 a.m. In-person, DN 2001. Online link coming soon.
Dr. Mark Newman currently serves as Executive Vice President of Health Affairs at the University of Kentucky. The Reves Visiting Professorship and Lecture is supported by the philanthropic efforts of our donors in honor of Jerry Reves, MD, former chair of Duke Anesthesiology and a co-founder of Duke Heart Center. Note: seating for the in-person lectures will be limited to half the room capacity due to COVID protocols.
Duke Heart CME
April 23: Duke Sports Cardiology & Sudden Death in Athletes Symposium with course directors Jim Daubert and Bill Kraus. Virtual. For information or to register, please visit: https://duke.is/gkffw. If you have additional questions, please contact Christy Darnell christy.darnell@duke.edu or 919-880-8686.
Marfan NC Walk for Victory, April 23
The North Carolina Walk for Victory to support Marfan patients and their families will take place on Saturday, April 23, 2022 from Noon to 3 p.m. at Laurel Hills Park on Edwards Mill Road in Raleigh.
Duke Heart is proud to serve as the presenting sponsor and we are excited for Chad Hughes, MD to serve as medical chair for the walk.
Please help us support all Marfan families as well as those with Loeys-Dietz (LDS), Vascular Ehlers-Danlos (VEDS), and related conditions. Donate or come join us at the event! Parking is easy to access and free.
Walk for Victory is The Marfan Foundation’s global walk program. The event is low-key, fun and family-oriented. To learn more or to register for this event, please visit: https://give.marfan.org/event/2022-north-carolina-walk-for-victory/e353032.
To learn more about The Marfan Foundation, please visit marfan.org.
MDEpiNet Spring 2022 Virtual Mini-Think Tank
May 5: MDEpiNet Spring 2022 Virtual Mini-Think Tank. Noon – 5:30 p.m., ET
MDEpiNet Predictable And SuStainable Implementation Of National CardioVascular Registries (PASSION CVR) Registry-Supported Prospective Clinical Trials
Join and invite your colleagues to join for updates from, and dialogues across our Registry-supported Prospective Trials Working Groups:
- Data Governance & Access
- Operational Roles & Responsibilities
- Global Regulatory Acceptance
- Use Cases:
- Aortic Intervention
- Heart Valves
- Mechanical Circulatory Support
- Peripheral Arterial Intervention
Registration now open: https://duke.qualtrics.com/jfe/form/SV_2f6JBD6WfaF9jBc.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
March 31 — Harold Koenig (psychiatry) and Rachel Tobin (internal medicine)
Medscape
Spiritual Interventions Improve QOL, Outcomes in HF
https://duke.is/mq7ba
April 3 — Sean Pokorney and Jonathan Piccini
Cardiac Rhythm News
ACC.22: Analysis shows low rate of device removal in case of CIED infection
https://duke.is/rttj3
April 4 — Robert Mentz
CBS News*
https://duke.is/b6cpq
*carried by 152 additional news outlets
April 4 — Manesh Patel and Jonathan Piccini
News-Medical.net
New type of anti-clotting drug reduces bleeding incidents among patients with atrial fibrillation
https://duke.is/c5puu
April 4 — Stephen Greene
Practical Cardiology
Q&A on SODIUM-HF and Impact of Salt Restriction, with Stephen Greene, MD
https://duke.is/5kpcc
April 4 — Sean Pokorney
News-Medical.net
Just 18% of patients have their infected heart devices removed, even though removal is recommended
https://duke.is/w7f3j
April 4 — Sean Pokorney and Jonathan Piccini
Cardiology Today
Most patients with implantable device infections do not receive extraction
https://duke.is/6jtwe
April 4 — Sean Pokorney
tctMD
Most Infected Cardiac Implanted Electronic Devices Not Removed Fast Enough
https://duke.is/p4p5m
April 4 — Sean Pokorney
Modern Healthcare
Doctors aren’t removing infected heart implants, resulting in patient deaths, study finds
https://duke.is/4szqk
April 4 — G. Michael Felker
News-Medical.net
Experimental heart failure drug has little impact on exercise tolerance
https://duke.is/jrq7t
April 4 — G. Michael Felker
Cardiovascular Business
Cholesterol medications, flu shots and heart failure: Day 2 at ACC.22
https://duke.is/ybzsn
April 4 — Manesh Patel
Endpoints News
Running behind Bristol Myers and J&J, Bayer inches forward in the next-gen blood thinner race
https://duke.is/9ecn2
April 5 — Sean Pokorney and Jonathan Piccini
Medtech Dive
Nearly 80% of patients with infection following cardiac implant not treated appropriately: study
https://duke.is/2ycax
April 5 — Stephen Greene
Practical Cardiology
Don’t Miss a Beat: ACC.22 Recap of DIAMOND, SODIUM-HF, and PROMPT-HF
https://duke.is/gwet6
April 5 — Sean Pokorney
ScienceBlog.com
Few Patients Have Infected Heart Devices Removed Despite Lifesaving Benefits
https://duke.is/v3qrf
April 6 — Manesh Patel
Medscape
Less Bleeding With Factor XI Inhibitor Anticoagulant? PACIFIC-AF
https://duke.is/7mz84
April 6 — G. Michael Felker
Medical Dialogues
Omecamtiv Mecarbil Has Little Impact on Exercise Tolerance in HF Patient: METEORIC-HF Trial
https://duke.is/mv7y6
April 6 — Sean Pokorney
MDEdge.com
Extraction of infected implanted cardiac devices rare, despite guidelines
https://duke.is/65qs2
April 7 — Sean Pokorney
Medscape
Extraction of Infected Implanted Cardiac Devices Rare, Despite Guidelines
https://duke.is/8pcgb
Division of Cardiology Publications Indexed in PubMed March 31 – April 6, 2022
Avezum Á, Oliveira GBF, Oliveira H, Lucchetta RC, Pereira VFA, Dabarian AL, D O Vieira R, Silva DV, Kormann APM, Tognon AP, De Gasperi R, Hernandes ME, Feitosa ADM, Piscopo A, Souza AS, Miguel CH, Nogueira VO, Minelli C, Magalhães CC, Morejon KML, Bicudo et al. Hydroxychloroquine versus placebo in the treatment of non-hospitalised patients with COVID-19 (COPE – Coalition V): A double-blind, multicentre, randomised, controlled trial. Lancet Reg Health Am 2022 Jul;11:100243. PM: 35378952.
Bishawi M, Lee FH, Abraham DM, Glass C, Blocker SJ, Cox DJ, Brown ZD, Rockman HA, Mao L, Slaba TC, Dewhirst MW, Truskey GA, Bowles DE. Late onset cardiovascular dysfunction in adult mice resulting from galactic cosmic ray exposure. iScience 2022 Mar 16;25(4):104086. PM: 35378858.
Coylewright M, Dodge SE, Bachour K, Hossain S, Zeitler EP, Kearing S, Douglas PS, Holmes D, Reddy VY, Nair D. Women in procedural leadership roles in cardiology: The Women In Local Leadership (WILL) observational study. Heart Rhythm 2022 Apr;19(4):623-629. PM: 34923161.
Dong OM, Poonnen PJ, Winski D, Reed SD, Vashistha V, Bates J, Kelley MJ, Voora D. Cost-Effectiveness of Tumor Genomic Profiling to Guide First-Line Targeted Therapy Selection in Patients With Metastatic Lung Adenocarcinoma. Value Health 2022 Apr;25(4):582-594. PM: 35365302.
Dzau VJ, Ellaissi WF, Krishnan KRR, Balatbat CA. How Academic Health Systems Can Be Ready for the Next Pandemic. Acad Med 2022 Apr 1;97(4):479-483. PM: 34966030.
Khan MS, Segar MW, Usman MS, Singh S, Greene SJ, Fonarow GC, Anker SD, Felker GM, Januzzi JL, Butler J, Pandey A. Frailty, Guideline-Directed Medical Therapy, and Outcomes in HFrEF: From the GUIDE-IT Trial. JACC Heart Fail 2022 Apr;10(4):266-275. PM: 35361446.
Martin CK, Höchsmann C, Dorling JL, Bhapkar M, Pieper CF, Racette SB, Das SK, Redman LM, Kraus WE, Ravussin E. Challenges in defining successful adherence to calorie restriction goals in humans: Results from CALERIE™ 2. Exp Gerontol 2022 Jun 1;162:111757. PM: 35240264.
Morrill J, Qirko K, Kelly J, Ambrosy A, Toro B, Smith T, Wysham N, Fudim M, Swaminathan S. A Machine Learning Methodology for Identification and Triage of Heart Failure Exacerbations. J Cardiovasc Transl Res 2022 Feb;15(1):103-115. PM: 34453676.
Rao VN, Fudim M, Wang J. Beyond the Anatomy of Renal Nerves: Functional Diversity of Renal Nerves. J Cardiovasc Transl Res 2022 Feb;15(1):27-28. PM: 35212975.
Tobin RS, Cosiano MF, O’Connor CM, Fiuzat M, Granger BB, Rogers JG, Tulsky JA, Steinhauser KE, Mentz RJ. Spirituality in Patients With Heart Failure. JACC Heart Fail 2022 Apr;10(4):217-226. PM: 35361439.
Vinson AJ, Singh S, Chadban S, Cherney D, Gaber O, Gill JS, Helgeson E, Herzog CA, Jardine M, Jha V, Kasiske BL, Mannon RB, Michos ED, Mottl AK, Newby K, Roy-Chaudhury P, Sawinski D, Sharif A, Sridhar VS, Tuttle KR, Vock DM, Matas A. Premature Death in Kidney Transplant Recipients: The Time for Trials is Now. J Am Soc Nephrol 2022 Apr;33(4):665-673. PM: 35292438.
Xiong X, Nazo N, Revoori R, Rajagopal S, Sparks MA. G protein- and -arrestin Signaling Profiles of Endothelin Derivatives at the Type A Endothelin Receptor. Kidney360 2021 May 17;2(7):1124-1131. PM: 35368349.
Xu H, Granger BB, Drake CD, Peterson ED, Dupre ME. Effectiveness of Telemedicine Visits in Reducing 30-Day Readmissions Among Patients With Heart Failure During the COVID-19 Pandemic. J Am Heart Assoc 2022 Apr 5;11(7):e023935. PM: 35229656.
Duke Heart week ending April 3rd 2022
Chief’s message:
Living in the Moment:
If anything, the last few years have taught us how fragile our usual way life is and how much things can change quickly. This week’s Pulse is notable for the fact that the American College of Cardiology conference has been going on both virtually but also in-person this weekend. The conference has had vaccination confirmation and masking, but still has quite a bit of great science and clinical sessions that our fellows and faculty have worked to present. You will see some of it here and more over the upcoming months. More importantly has been the ability to see people (not on zoom) and exchange ideas and just be back together has been important. The weekend of course has also had the ups and downs (depending on your shades of blue) around the Final Four. The outcome of the game, despite not being favorable for the Duke side of the world, has also underscored the refrain from the pandemic to Coach K of living in the moment. The ability to appreciate your colleagues, friends, and most importantly family. As we continue to go through the changes in our healthcare environment, the unknown around virus resurgences or getting back to life, we hope you all have time to spend with loved ones. The conference this week has highlighted for Duke Cardiology the value of our colleagues, alumni, fellows, and friend near and far. More than ever – it has also provided an opportunity to enjoy and live in the moment for our group.


Highlights of the week:
ACC.22: Few Patients Have Infected Heart Devices Removed Despite Lifesaving Benefits
Medicare patients whose implantable heart devices became infected were less likely to die from the complication if they had the hardware removed compared to patients who only received antibiotics, according to the largest study on the topic, led by the Duke Clinical Research Institute.
The study showed that just 18 percent of patients with device infections underwent surgeries to have their pacemakers or defibrillators removed, even though removal is recommended by all leading medical society treatment guidelines. There is a 43-percent lower risk of death in these patients if guidelines are followed.
The findings, reported earlier today as a late-breaker presentation at the 2022 American College of Cardiology Scientific Sessions, highlight that cardiac device infection is a major public health issue, and there are large gaps in guideline adherence.
“This is an important message about a persistent gap in care: These devices should be removed when an

infection occurs, and their removal saves lives,” said lead author Sean D. Pokorney, MD, an electrophysiologist and cardiologist in the Department of Medicine at Duke University School of Medicine. Pokorney is also a member of the Duke Clinical Research Institute.
Pokorney and colleagues launched the study in 2021, using Medicare data for nearly 1.1 million patients who received cardiac implantable electronic devices, or CIEDs, between 2006 and 2019.
Of those study patients, 11,619 (about 1 percent) developed infections a year or more after implantation. Only 13 percent of the patients had the device removed within six days of infection, and an additional 5 percent had them removed from day 7 to 30.
The vast majority — nearly 82 percent — were treated solely with antibiotics, despite numerous earlier studies showing antibiotics fail to wipe out infections involving CIEDs.
Those earlier studies led to a 2017 consensus of leading health organizations to recommend removal of CIEDs when a definitive infection is identified.
In the current study, the researchers found that removing the devices had a clear survival benefit. The death rate for those who did not have their devices removed was 32.4 percent in the year after an infection was diagnosed, compared with a rate of 18.5 percent among patients who underwent extraction within six days and 23.2 percent for patients who had extractions on days 7 to 30.
“Any extraction was associated with lower mortality when compared to no extraction, but the highest benefit was to those who had devices removed within six days of an infection,” Pokorney said. “This speaks to the importance of putting systems in place to identify these patients and get them quickly and appropriately treated, because delays in care result in higher mortality.”
The Duke Clinical Research Institute, with funding from Philips and leadership from Pokorney and Christopher B. Granger, MD, is acting on this data and launching a quality improvement demonstration project to address the gap in care for CIED infection patients within three health care systems in the US.
In addition to Pokorney, study authors include Lindsay Zepel, Melissa A. Greiner, Eric Black-Maier, Robert K. Lewis, Donald D. Hegland, Christopher B. Granger, Laurence M. Epstein, Roger G. Carrillo, Bruce L. Wilkoff, Chantelle Hardy and Jonathan P. Piccini.
The study received funding support from Philips, which markets devices used in CIED extraction procedures. The funder had no role in the design, implementation or publication of the study. Six study authors — Pokorney, Lewis, Epstein, Carillo, Wilkoff, and Piccini — reported ties to the company; a full disclosure is provided in the study manuscript.
ACC.22: Investigational Anti-Clotting Drug Reduces Bleeding Risk Among AF Patients
A new type of anti-clotting drug caused fewer bleeding incidents among patients with atrial fibrillation than the commonly prescribed apixaban, according to results from a head-to-head comparison of the two.
The study, led by cardiologists at Duke, was reported today as a late-breaking presentation at the 2022 American College of Cardiology Scientific Sessions being held in Washington, DC. The results were simultaneously published in the journal The Lancet.
“Anti-clotting therapy is a lifesaver for people who develop atrial fibrillation, which can increase the risk of stroke by five-fold,” said presenter and senior author Manesh Patel, MD, chief of the Division of Cardiology at Duke University School of Medicine and member of the Duke Clinical Research Institute. “But a serious complication associated with anti-clotting therapies is bleeding, leading many patients to reduce or stop taking their medications. As a result, there is great interest in alternatives that reduce this risk.”
Asundexian is a new class of anti-clotting drug that is under investigation. It works by inhibiting a blood protein called Factor XI, which contributes to the development of blood clots but is not involved in the process of healing blood vessels.
In the PACIFIC-AF trial — a phase 2 study funded by Bayer AG, which manufactures the investigative therapy — the researchers focused on bleeding outcomes arising from two different doses among patients with atrial fibrillation.
Both doses of asundexian taken once daily, 20 mg and 50 mg, were tested in comparison to similar dosages of apixaban, which is one of several commonly prescribed anti-clotting therapies that affect a different blood clotting protein.
The trial included 755 patients with an average age of about 74 years old. At both doses, patients who took asundexian had a 67-percent lower risk of bleeding compared to patients taking apixaban.
“Reducing bleeding risks for atrial fibrillation patients is encouraging,” said lead author Jonathan Piccini, MD, clinical cardiac electrophysiologist at Duke. “One in four people will develop atrial fibrillation — it’s the leading cause of heart arrhythmia and is a risk factor for stroke — so it’s important that we have safe and effective therapies. We’re eager to see the research move into phase 3 studies.”
MD, clinical cardiac electrophysiologist at Duke. “One in four people will develop atrial fibrillation — it’s the leading cause of heart arrhythmia and is a risk factor for stroke — so it’s important that we have safe and effective therapies. We’re eager to see the research move into phase 3 studies.”
In addition to Piccini and Patel, study authors include Valeria Caso, Stuart J. Connolly, Keith A.A. Fox, Jonas Oldgren, W. Schuyler Jones, Diana A. Gorog, Václav Durdil, Thomas Viethen, Christoph Neumann, Hardi Mundl, on behalf of the PACIFIC-AF Investigators.

ACC.22: Investigational Drug for Heart Failure has Little Impact on Exercise Tolerance
Heart failure patients taking the investigational drug omecamtiv mecarbil, which has been previously shown to improve long-term outcomes, see little impact on their ability to exercise compared to a placebo, according to a study supported by Duke Clinical Research Institute (DCRI).
The study was designed to test whether the new therapy — a selective cardiac myosin activator — could yield improvements in overall exercise capacity for patients with heart failure. Therapies that help heart failure patients better tolerate exercise remains an unmet need.
The findings were reported today as a late-breaking presentation at the 2022 American College of Cardiology Scientific Sessions. Circulation: Heart Failure published the study design in March 2022.
“We are fortunate to have a lot of medications in heart failure that can help patients live longer or stay out of the hospital — all very important goals,” said Duke cardiologist Michael Felker, MD, study co-chair and a member of DCRI.
“However, exercise tolerance is the main symptom patients with heart failure have,” Felker said. “They get tired or out of breath very easily. This is a major impediment for their quality of life. Unfortunately, many of the guideline-directed drugs that improve survival don’t improve exercise tolerance.”
The research study, called the Multicenter Exercise Tolerance Evaluation of Omecamtiv Mecarbil Related to Increased Contractility in Heart Failure (METEORIC-HF), recruited patients across 64 sites in nine countries. It included 276 adult heart failure patients with reduced ejection fraction; they were randomly assigned to receive the study medication or a placebo. The results were blinded to the investigators, the study sponsor, and the participants.
As its primary outcome, METEORIC-HF sought to examine the changes omecamtiv mecarbil had on peak oxygen uptake during cardiopulmonary exercise over a 20-week period. Secondary outcome measurements included assessing overall exercise capacity, ventilator efficiency, and daily activity.
“We found in the trial that even though omecamtiv mecarbil was safe and well-tolerated, it did not improve exercise tolerance over placebo,” Felker said. “I think what that tells us is finding interventions that can improve people’s exercise tolerance is still an unsolved/unmet need for our patients with heart failure. What our trial has done is helped better define what this medication does and doesn’t do.”
During the METEORIC-HF trial, study authors for the Global Approach to Lowering Adverse Cardiac Outcomes Through Improving Contractility in Heart Failure (GALACTIC-HF) trial published their own results. That trial examined outcomes between omecamtiv mecarbil and a placebo in a broad population of over 8,000 symptomatic patients. GALACTIC-HF found that omecamtiv mecarbil decreased the rate of heart failure or death from cardiovascular causes.
Felker and Gregory Lewis, MD, at Massachusetts General Hospital, co-chaired the study.
In addition to Felker and Lewis, study authors include Kieran Docherty, Adriaan Voors, Alain Cohen-Solal, Marco Metra, David Whellan, Justin Ezekowitz, Piotr Ponikowski, Michael Böhm, John Teerlink, Stephen Heitner, Stuart Kupfer, Fady Malik, and Lisa Meng.
Impressive work by all! Please note: We will have additional coverage from ACC.22 next weekend. Stay tuned! Please consider submitting photos from your ACC experience as well as information related to your presentation for inclusion in Pulse; please email your submissions to Tracey Koepke by EOB Wednesday, 4/6. Thank you!
Rymer to Host Post-ACC.22 Twitter Space
Duke Heart is collaborating with Med-IQ to conduct a Twitter Space ‘live’ on Wednesday, April 6 at 6:30 p.m. Join interventional cardiologist Dr. Jennifer Rymer for a recap of highlights from the ACC! Rymer will lead a free-flowing discussion highlighting data presented during the 2022 ACC Scientific Sessions and provide expert insight on the trials. You can follow Jenn on Twitter @jennifer_rymer. You can also follow Med-IQ (@MedIQCME).
When: Wednesday, April 6 at 6:30 p.m. ET
Where: https://twitter.com/i/spaces/1vAxRkbplgqKl
If you’re not familiar with Twitter, all you’ll need to do is visit the Twitter Space at https://twitter.com/i/spaces/1vAxRkbplgqKl and drop in. You DO NOT need a Twitter account just to listen in (simply click the link to join). You only need a Twitter account if you’d like to request to “speak” during the Twitter Space event.
If you can’t join the live space, Med-IQ will have the recording on their Facebook page (https://www.facebook.com/MedIQCME) later next week.
We’re looking forward to this and hope you’ll join us!
Karra & Team Score Grant Funding to Explore Sarcoidosis
 Congratulations to Ravi Karra, MD, MHS, and team — they were recently notified that their project, Epithelioid Mechanisms of Sarcoidosis, has been selected for award funding by the Ann Theodore Foundation Breakthrough Sarcoidosis Initiative, supported by the Ann Theodore Foundation.
Congratulations to Ravi Karra, MD, MHS, and team — they were recently notified that their project, Epithelioid Mechanisms of Sarcoidosis, has been selected for award funding by the Ann Theodore Foundation Breakthrough Sarcoidosis Initiative, supported by the Ann Theodore Foundation.
Sarcoidosis is a systemic disease defined by the presence of granulomas provoked by an unknown trigger. Although central to sarcoidosis, granulomas also occur in other diseases where they serve to contain bacteria or foreign materials. In prior work on infectious granulomas, David Tobin, PhD, an associate professor of Molecular Genetics and Microbiology at Duke and his team have determined that epithelioid cells, found in the granuloma interior, are responsible for the barrier function of the granuloma. Interfering with macrophage epithelioid transformation can loosen the granuloma and allow for inflammatory cells to clear the infection. Karra – who is partnering with Tobin on this project — and team hypothesize that specific targeting of epithelioid cells in sarcoidosis might similarly improve treatment responses. However, before such treatments can be developed, the biology of epithelioid cells in sarcoidosis needs to be better understood.
The goal of the Epithelioid Mechanisms of Sarcoidosis project is to identify key pathways and events that lead to the emergence of epithelioid cells. Their first aim is to use spatial RNA sequencing to profile granuloma formation following the Kveim test, the only system available to induce and follow sarcoid granulomas over time in humans. Their experiments will illuminate where and when signaling pathways are activated in different cell types during granuloma formation and provide a better understanding of how epithelioid cells form in sarcoidosis. Their second aim is to profile changes in DNA and RNA of individual circulating cells. They believe their work will identify why patients with sarcoidosis develop epithelioid cells in response to a trigger, while individuals without sarcoidosis do not.
The team hopes their project can lead to new therapeutic targets for treating sarcoidosis and new diagnostic tests for identifying sarcoidosis.
Duke Heart launched a multidisciplinary sarcoid clinic about one year ago, which has seen regular growth over time. According to Karra, the team has treated 50 sarcoid patients in the past year and are now seeing 2-3 new patients for evaluation each week and that a number of our cardiology fellows have been involved in the work, including Kelly Arps, MD, who will be presenting on arrhythmia concerns related to sarcoid during our next Cardiology Grand Rounds on Tuesday, April 5 (Webex link included in events listing, below).
Congratulations to Ravi and our sarcoid team — this is excellent news!
Shout-out to Barnes, Dimsdale!
The North Carolina Nurses Association held its annual Nurse Practitioner Spring Symposium in Asheville, NC from March 20-23. Presenters from Duke Heart included Stephanie Barnes and Allison Dimsdale.
Way to go!!!


In Memoriam: Kelly Ann Machovec, MD, MPH, Peds Cardiac Anesthesiologist
It is with deep sadness that we share the news of the passing of our colleague, Kelly Ann Machovec, MD, MPH, a pediatric cardiac anesthesiologist and team member with the Duke Pediatric and Congenital Heart Center. She passed away on March 30 at the age of 43.
She will be remembered as an exceptional academician and physician who dedicated her career to improving the lives of children undergoing cardiothoracic or vascular surgery, and for her special impact that was palpable to her colleagues and patients throughout the Duke Children’s Heart Center.
Originally from Baltimore, Maryland, Machovec received her Master of Public Health degree in 2005 and her Doctor of Medicine degree in 2006, both at the University of North Carolina. She went on to complete a residency in anesthesiology at Drexel University College of Medicine in Philadelphia and a fellowship in pediatric anesthesiology at Duke University School of Medicine. In 2013, Dr. Machovec joined Duke Anesthesiology faculty as an assistant professor of anesthesiology; she was appointed an associate professor of anesthesiology in 2019. She was an accomplished pediatric anesthesiologist whose research primarily focused on the hemostasis management of children following open heart surgery performed on cardiopulmonary bypass.
Earlier this year she received the Duke Pediatric and Congenital Heart Center Impact Award, recognizing her exceptional impact on the clinical practice around hemostasis, on both local and national levels. She was a fierce advocate for child-centered health care policies and always questioned the status quo. For example, she led the charge to discontinue preoperative blood testing in children to prevent them from having unnecessary painful blood draws in the preoperative clinic.
Dr. Machovec’s excellence and research led to her invitation to write the book chapter on “Anesthesia for Pediatric Cardiac Surgery” in Miller’s Anesthesia textbook. In 2015, she co-founded the Hemostasis Interest Group, a committee within the Congenital Cardiac Anesthesia Society which she served on for six years as committee chair, member and mentor; she also served as an at-large member on the Board of Directors of the Congenital Cardiac Anesthesia Society. Dr. Machovec was a passionate educator, serving as chair of the Clinical Competency Committee for Duke’s Pediatric Anesthesiology Fellowship and as a question writer and committee member for the American Board of Anesthesiology’s Pediatric Maintenance of Certification.
In addition to being an outstanding clinician and a dedicated educator, she was recognized with the high honor of the Leonard Tow Humanism in Medicine Award at the Duke University School of Medicine in March of this year. Recipients of this distinguished award are recognized as exemplars of humanism in the care of their patients, their compassionate delivery of care and respectfulness given to their patients and health care colleagues, as well as for their clinical excellence.
Beyond her career, Dr. Machovec advocated and raised funds for basic science research. From 2013-2017, she also advocated for pediatric health care on a global scale by taking part in medical missions in India, the Philippines and Haiti for Operation Smile, which helps children with cleft lip and cleft palate, and Gift of Life International, which provides lifesaving cardiac treatment to children in need from developing countries.
When introduced by Dr. Edmund Jooste prior to her delivery of Duke Anesthesiology Grand Rounds last year, Dr. Machovec was described as having “the determination of Ruth Bader Ginsberg, the curiosity of Marie Curie and fierceness of Wonder Woman” and these are the qualities that her work family loved and admired in her. She was also described as funny, strong-willed and energetic, and a dedicated team member who will be deeply missed by her pediatric anesthesiology colleagues and all of her interprofessional friends and colleagues within Duke Anesthesiology and the Pediatric Heart Center.
To preserve Dr. Machovec’s legacy at Duke, the Department of Anesthesiology has formally established the Kelly Machovec Humanism Award. The recipient of this annual departmental award will exemplify grace and compassion in their delivery of patient-centered care, reverence for patients, their loved ones and colleagues, ethical principles, and a continuous commitment to clinical excellence.
Most importantly, Dr. Machovec’s legacy will live on through her family. She was a dedicated and loving wife to her husband, Scott Matthews, and proud mother to her three young daughters, Vivienne, Eva and Caroline. Her loved ones will remember her as an engaged, talented and powerful woman with unwavering passion and optimism, who loved spending time with her family and friends, running, practicing yoga, reading, and baking.
A Celebration of Life will be held on Monday, April 11 from 5:00 – 8:00 p.m. at the Rigmor House, 5501 NC Highway 54, in Chapel Hill. All are welcome to attend. The family kindly requests that if you do plan to attend, please respond via this link for catering purposes.
We extend our deep condolences to Dr. Machovec’s family, friends and colleagues. Duke flags were lowered on Friday in honor of her life and legacy. They will remain lowered through Monday. At the request of her family, in lieu of flowers, memorial gifts may be made in her name to the Dana-Farber Cancer Institute.
COVID-19 Updates
All the latest Clinical Operations updates related to COVID can be found at https://covid-19.dukehealth.org.
Upcoming Events & Opportunities
Cardiology Grand Rounds
April 5: Cardiac Sarcoidosis: Updates and Contemporary Challenges with Kelly Arps. 5 p.m. via Webex.
Duke Heart CME
April 23: Duke Sports Cardiology & Sudden Death in Athletes Symposium with course directors Jim Daubert and Bill Kraus. Virtual. For information or to register, contact Christy Darnell christy.darnell@duke.edu or 919-880-8686.
Marfan NC Walk for Victory, April 23
The North Carolina Walk for Victory to support Marfan patients and their families will take place on Saturday, April 23, 2022 from Noon to 3 p.m. at Laurel Hills Park on Edwards Mill Road in Raleigh. Duke Heart is proud to serve as the presenting sponsor and we are excited for Chad Hughes, MD to serve as medical chair for the walk.
Please help us support all Marfan families as well as those with Loeys-Dietz (LDS), Vascular Ehlers-Danlos (VEDS), and related conditions. Donate or come join us!
Walk for Victory is The Marfan Foundation’s global walk program. The event is low-key, fun and family-oriented. To learn more or to register for this event, please visit: https://give.marfan.org/event/2022-north-carolina-walk-for-victory/e353032.
To learn more about The Marfan Foundation, please visit marfan.org.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
March 17 — Pamela Douglas
Medscape
ACC Looks to Build Inclusive, Bully-Free Cardiology Workplaces
https://duke.is/zrp29
March 19 — Adrian Hernandez
The Western Journal
https://duke.is/v2tjr
March 22 – Joseph Turek, Mary Louise Markert and Allan Kirk
Medical News Today
Novel heart-thymus transplant technique may spell end of lifelong drugs
https://duke.is/ydzhp
March 24 — Nishant Shah
Cardiology Advisor
Mean Monthly BP Increased Among US Adults During COVID-19
https://duke.is/j7q7j
March 27 — Renato Lopes
Healio/Cardiology Today
Alirocumab does not impact AF risk after ACS
https://duke.is/wffkg
March 29 — Duke University/Duke Health
Becker’s Hospital Review
Best medical schools for 2023: US News
https://duke.is/ckpuc
March 29 — Duke University/Duke Health
Becker’s Hospital Review
10 best nursing schools for master’s and DNPs, as ranked by US News
https://duke.is/bgcp8
March 30 — Joseph Turek
Nation (Kenya)
New procedure gives hope to transplant patients
https://duke.is/nb7bn
March 31 — Sunil Rao
Cardiovascular News
SCAI aims to minimise risks in medical proctoring of new techniques and technologies
https://duke.is/5jcmw
Division of Cardiology Publications Indexed in PubMed March 17-23, 2022
Blumer V, Parsons JB, Anderson DR, Bloomfield GS, Ward C. Hemophagocytic Lymphohistiocytosis Associated With Endocarditis: A Case Years in the Making. Circulation 2022 Mar 22;145(12):934-939. PM: 35312382.
Dangas G, Baber U, Sharma S, Giustino G, Sartori S, Nicolas J, Goel R, Mehta S, Cohen D, Angiolillo DJ, Zhang Z, Camaj A, Cao D, Briguori C, Dudek D, Escaned J, Huber K, Collier T, Kornowski R, Kunadian V, Moliterno DJ, Ohman EM, Weisz G, Gil R, Krucoff M. Safety and efficacy of ticagrelor monotherapy according to drug-eluting stent type: the TWILIGHT-STENT study. EuroIntervention 2022 Mar 18;17(16):1330-1339. PM: 34881696.
El-Chami MF, Bockstedt L, Longacre C, Higuera L, Stromberg K, Crossley G, Kowal RC, Piccini JP. Leadless vs. transvenous single-chamber ventricular pacing in the Micra CED study: 2-year follow-up. Eur Heart J 2022 Mar 21;43(12):1207-1215. PM: 34788416.
Fagundes A, Berg DD, Bohula EA, Baird-Zars VM, Barnett CF, Carnicelli AP, Chaudhry SP, Guo J, Keeley EC, Kenigsberg BB, Menon V, Miller PE, Newby LK, van Diepen S, Morrow DA, Katz JN. End-of-life care in the cardiac intensive care unit: a contemporary view from the Critical Care Cardiology Trials Network (CCCTN) Registry. Eur Heart J Acute Cardiovasc Care 2022 Mar 16;11(3):190-197. PM: 34986236.
Friedman DJ, Qin L, Parzynski C, Heist EK, Russo AM, Ranasinghe I, Zeitler EP, Minges KE, Akar JG, Freeman JV, Curtis JP, Al-Khatib SM. Longitudinal Outcomes of Subcutaneous or Transvenous Implantable Cardioverter-Defibrillators in Older Patients. J Am Coll Cardiol 2022 Mar 22;79(11):1050-1059. PM: 35300816.
Gallagher EJ, Rockey DC, Kontos CD, Vyas JM, Brass LF, Hu PJ, Isales CM, Ajijola OA, Rathmell WK, Conlin PR, Baiocchi RA, Kazmierczak BI, Akabas MH, Williams CS. Pearls of wisdom for aspiring physician-scientist residency applicants and program directors. JCI Insight 2022 Mar 22;7(6):10.1172/jci.insight.158467. PM: 35315364.
Gulati M, Korn RM, Wood MJ, Sarma A, Douglas PS, Singh T, Merz NB, Lee J, Mehran R, Andrews OA, Williams JC. Childbearing Among Women Cardiologists: The Interface of Experience, Impact, and the Law. J Am Coll Cardiol 2022 Mar 22;79(11):1076-1087. PM: 35300820.
Haeusler KG, Eichner FA, Heuschmann PU, Fiebach JB, Engelhorn T, Blank B, Callans D, Elvan A, Grimaldi M, Hansen J, Hindricks G, Al-Khalidi HR, Mont L, Nielsen JC, Piccini JP, Schotten U, Themistoclakis S, Vijgen J, Di Biase L, Kirchhof P. MRI-Detected Brain Lesions and Cognitive Function in Patients With Atrial Fibrillation Undergoing Left Atrial Catheter Ablation in the Randomized AXAFA-AFNET 5 Trial. Circulation 2022 Mar 22;145(12):906-915. PM: 35135308.
Mansour M, Radaideh Q, Alaiwah MN, Alnimer Y, Devabhaktuni SR, Dhar G, Vallurupalli S, Michos ED, Newby DE, Williams MC, Fudim M, Al’Aref SJ. Major adverse cardiac events in symptomatic women with non-obstructive CAD on coronary CTA: pooled analysis from PROMISE and SCOT-HEART. Int J Cardiovasc Imaging 2022 Mar;38(3):683-693. PM: 34628593.
Parker DC, Wan M, Lohman K, Hou L, Nguyen AT, Ding J, Bertoni A, Shea S, Burke GL, Jacobs DR, Post W, Corcoran D, Hoeschele I, Parks JS, Liu Y. Monocyte miRNAs Are Associated With Type 2 Diabetes. Diabetes 2022 Apr 1;71(4):853-861. PM: 35073575.
Pinsker BL, Serfas JD, Krasuski RA. Burden and Impact of Arrhythmias in Repaired Tetralogy of Fallot. Curr Cardiol Rep 2022 Mar;24(3):225-234. PM: 35138576.
Salah HM, Minhas AMK, Khan MS, Khan SU, Ambrosy AP, Blumer V, Vaduganathan M, Greene SJ, Pandey A, Fudim M. Trends and characteristics of hospitalizations for heart failure in the United States from 2004 to 2018. ESC Heart Fail 2022 Apr;9(2):947-952. PM: 35098700.
Usman MS, Khan MS, Fonarow GC, Greene SJ, Friede T, Vaduganathan M, Filippatos G, Coats AJS, Anker SD, Butler J. Robustness of outcomes in trials evaluating sodium-glucose co-transporter 2 inhibitors for heart failure. ESC Heart Fail 2022 Apr;9(2):885-893. PM: 35029056.
Voors AA, Angermann CE, Teerlink JR, Collins SP, Kosiborod M, Biegus J, Ferreira JP, Nassif ME, Psotka MA, Tromp J, Borleffs CJW, Ma C, Comin-Colet J, Fu M, Janssens SP, Kiss RG, Mentz RJ, Sakata Y, Schirmer H, Schou M, Schulze PC, Spinarova L, Volterrani. The SGLT2 inhibitor empagliflozin in patients hospitalized for acute heart failure: a multinational randomized trial. Nat Med 2022 Mar;28(3):568-574. PM: 35228754.
Zheng K, Smith JS, Eiger DS, Warman A, Choi I, Honeycutt CC, Boldizsar N, Gundry JN, Pack TF, Inoue A, Caron MG, Rajagopal S. Biased agonists of the chemokine receptor CXCR3 differentially signal through Gα:β-arrestin complexes. Sci Signal 2022 Mar 22;15(726):eabg5203. PM: 35316095.
Division of Cardiology Publications Indexed in PubMed March24-30, 2022
Alexander JH. Equipoise in Clinical Trials: Enough Uncertainty in Whose Opinion? Circulation 2022 Mar 29;145(13):943-945. PM: 35344405.
Elgendy IY, Wegermann ZK, Li S, Mahtta D, Grau-Sepulveda M, Smilowitz NR, Gulati M, Garratt KN, Wang TY, Jneid H. Sex Differences in Management and Outcomes of Acute Myocardial Infarction Patients Presenting With Cardiogenic Shock. JACC Cardiovasc Interv 2022 Mar 28;15(6):642-652. PM: 35331456.
Komisarow JM, Toro C, Curley J, Mills B, Cho C, Simo GM, Vavilala MS, Laskowitz DT, James ML, Mathew JP, Hernandez A, Sampson J, Ohnuma T, Krishnamoorthy V. Utilization of Brain Tissue Oxygenation Monitoring and Association with Mortality Following Severe Traumatic Brain Injury. Neurocrit Care 2022 Apr;36(2):350-356. PM: 34845596.
Rao SV. RESPONSE: Navigating the Transition From Fellowship to Early Career: “Sink or Swim” to “Lifting All Boats”. J Am Coll Cardiol 2022 Mar 29;79(12):1218-1219. PM: 35331418.
Xian Y, Xu H, Smith EE, Saver JL, Reeves MJ, Bhatt DL, Hernandez AF, Peterson ED, Schwamm LH, Fonarow GC. Achieving More Rapid Door-to-Needle Times and Improved Outcomes in Acute Ischemic Stroke in a Nationwide Quality Improvement Intervention. Stroke 2022 Apr;53(4):1328-1338. PM: 34802250.
Recent Comments