Duke Heart March 26th 2023
Highlights of the week:
Turek Receives Everest Award from Marfan Foundation
 Late last year, the Marfan Foundation announced that it had selected Joseph Turek, MD, PhD, chief of pediatric cardiac surgery in Duke’s division of cardiovascular and thoracic surgery as the first-ever recipient of their Everest Award, the Foundation’s largest research grant to date. The award will provide up to four years of funding, for a total of $800,000, as long as annual milestone goals are met. The initial year of funding provides $200,000.
Late last year, the Marfan Foundation announced that it had selected Joseph Turek, MD, PhD, chief of pediatric cardiac surgery in Duke’s division of cardiovascular and thoracic surgery as the first-ever recipient of their Everest Award, the Foundation’s largest research grant to date. The award will provide up to four years of funding, for a total of $800,000, as long as annual milestone goals are met. The initial year of funding provides $200,000.
The Marfan Foundation is a nonprofit organization created to support individuals with Marfan syndrome as well as other genetic aortic and vascular conditions, including Loeys-Dietz and Vascular Ehlers-Danlos syndromes.
Marfan syndrome is a genetic condition that affects connective tissue. It is caused by a mutation in the FBN1 gene, which limits the body’s ability to make proteins required to build connective tissue. This can lead to damaged blood vessels, as well as damage to the heart, eyes, skin, lungs, and the bones of the hips, spine, feet, and rib cage, according to the Centers for Disease Control and Prevention. A serious complication of Marfan syndrome is the development of an aortic aneurysm, which can eventually rupture.
In the US, there are about 75,000 patients with known Marfan Syndrome. Most of them will need surgery to repair an aneurysm, according to Turek.
Typically, surgery is not performed until a patient reaches early adulthood. Children diagnosed with Marfan are usually monitored over time in order to detect changes to their aorta. Most first surgeries occur due to an aneurysm that has developed on the ascending aorta.
We spoke with Turek to learn more about the work he’s doing on Marfan and the project that is being funded with the Everest Award.
“I’ve seen how devastating this disease can be,” says Turek. “The fact is, patients who do not get treated in time die from these aneurysms. Patients who do get treated in time undergo large operations — extensive heart surgery to repair an aortic aneurysm — and in many cases have to come back to get additional surgeries to fix other parts of their aorta. The best thing we could ever do for these patients would be to get to the point where we could just manage this with medicine and avoid surgery altogether.”
There is a well-characterized pathway in the mediation of Marfan syndrome. It has been pretty well studied, so a lot is known about it, Turek adds.
“The problem is that when you treat this well-known pathway with medications, it still doesn’t stop the growth of aneurysms in Marfan. It slows it, but it doesn’t stop it. So, there are clearly other pathways involved that are leading to aneurysm growth.”
Dating back to his time as a pediatric cardiac surgeon at the University of Iowa, he and his team have been investigating alternate pathways that could also be causing aneurysms to form in Marfan patients. The team’s persistence has been paying off.
“We found a new pathway that, when treated in animal models, completely blocked that pathway in addition to the well-characterized pathway,” added Turek. “We actually didn’t get aneurysms forming at all in our animal studies. Of course, we need more research and a path forward towards drug discovery.”
Turek hopes the Everest Award will allow him to do just that. He says the goal is to be able to get to the point where Marfan patients can effectively be medically managed, and hopefully keep them from needing surgery at all.
“Without the Everest grant I don’t think we could push this through the preclinical stages as quickly as we’d like,” he says. “This award really changes everything for us by allowing us to take a deeper dive into exploring this promising pathway and treatment modality. We’d really like to have something we could take into clinical trials for people with Marfan syndrome.”
We look forward to tracking this project as it moves forward.
If you’d like to see the video announcement made by Josephine Grima, PhD, Chief Science Officer of the Marfan Foundation, please check it out here: https://duke.is/wxyc2.
Beyond the Everest Award, the Marfan Foundation bestowed $600,000 in new grants to physician-scientists as part of its Research Grant program, bringing total current grant funding to $1,285,500.
Congratulations, Joe!
Support Marfan Patients & Duke Heart!
Speaking of Marfan syndrome and the Marfan Foundation… if you’d like to help Duke Heart in supporting patients with Marfan and other connective tissue disorders, please consider joining us at the upcoming 2023 NC Walk for Victory.
The 2023 NC Walk for Victory is planned for Saturday, April 22 from Noon-3 p.m. at Laurel Hills Park, 3808 Edwards Mill Rd., Raleigh (27612). Duke Heart is serving as the presenting sponsor, with Dr. Chad Hughes serving as the Walk’s Medical Director.
This event is held to gather patients, family members and friends who are affected by genetic aortic and vascular conditions, including Marfan Syndrome, Loeys-Dietz, and Vascular Ehlers-Danlos syndromes. Attendees come from all over the southeast region of the U.S. to celebrate one another and to forge friendships with others going through similar experiences.
The Walk for Victory is a fun, family-friendly event that recognizes an incredible group of people and their caregivers. The Walk helps to create awareness in the community, and is one way the Marfan Foundation raises funding for much-needed research into these genetic conditions.
Please consider supporting any of the walkers/teams — maybe throw your support behind Duke Aorta and our team captain Melissa Burkett! Check out Duke Aorta’s team fundraising page for The Marfan Foundation: https://give.marfan.org/team/482581) or behind Team James (“giving hugs and raising awareness since 2018!”). Even small contributions will help!
To learn more about the event or the Marfan Foundation in general, please visit: https://duke.is/pkjnw. Thank you!
Benkert Receives NHLBI Research Fellowship Award
 Congratulations to Abigail Benkert, a PGY-4 in our Integrated Cardiothoracic Surgery training program (I6 resident), who was recently notified that she has been selected for a Research Fellowship Award from the National Heart, Lung, and Blood Institute. The award funding, which begins August 21, 2023, includes $76,292 in funding for Year 1.
Congratulations to Abigail Benkert, a PGY-4 in our Integrated Cardiothoracic Surgery training program (I6 resident), who was recently notified that she has been selected for a Research Fellowship Award from the National Heart, Lung, and Blood Institute. The award funding, which begins August 21, 2023, includes $76,292 in funding for Year 1.
The award is for her project, Evaluation of adeno-associated viral (AAV) mediated gene replacement therapy as a therapeutic option for SLC25A4 deficiency (award #F32HL167559), which will fund part of a project Benkert has been working on for several years. She has been conducting research into a form of inherited hypertrophic cardiomyopathy that captured her interest while in medical school at Tufts, and ties back to her experiences as an undergraduate student at Franklin & Marshall College.
At Franklin & Marshall, Benkert began working in a laboratory that collaborated with the Clinic for Special Children (CSC), located in Strasburg, PA. CSC is a pediatric medical genetics clinic that treats children with a myriad of conditions, but historically focused on the treatment of Amish and Mennonite children with rare genetic, biochemical, and other disorders.
Benkert says her exposure to the physicians at the Clinic for Special Children was instrumental to her not only because the experience piqued her interest in medical genetics, but also in shaping her initial career choices. “The pediatricians and research team at CSC are devoted to providing innovative and high-quality care to a very underserved population.,” she says. “I originally thought I’d become a pediatrician and practice in a rural location at some point, maybe even go back to working at the Clinic.”
She headed to medical school at Tufts University, which has a partnership program with Maine Medical Center that focuses on primary care in rural settings. Benkert signed on for the program and during her final year of medical school worked with the CSC once again to study the natural history of an inherited skeletal myopathy and form of hypertrophic cardiomyopathy (HCM) among a cohort of Mennonite patients.
Unfortunately, for a lot of patients with HCM there aren’t many effective therapies, and that was true for these particular Mennonite patients.
Fast forward to now. Benkert says the lack of therapies for these patients was the impetus for her project.
“Nothing is available to help modify their disease or effectively help their symptoms,” she adds. “The reality is we have to wait until they’re in heart failure, and then treat the heart failure and perhaps consider heart transplantation.”
Her Research Fellowship Award from the NHLBI will allow her to focus on gene therapy strategies that could potentially help. Her project aims to develop an adeno-associated virus (AAV) gene replacement strategy. She’ll be working with Aravind Asokan, PhD, professor in the department of surgery, and director of gene therapy at Duke. Benkert has been working with Asokan’s basic science lab in Duke’s department of Biomedical Engineering to develop the construct that can be used for gene therapy, and test it in a transgenic mouse model and in patient-derived cells. They’ll be getting blood samples from HCM patients, dedifferentiating them into pluripotent stem cells, and from there turning them into cardiomyocytes so they can actually test the gene therapy on heart cells.
“The award will give me a good launching point for my career as a surgeon-scientist, and I believe demonstrates my commitment to this work. It’s really nice to have the funding to continue pursuing a project and interest that started while I was a medical student.”
When asked to reflect on why she chose to go into medicine, Benkert thinks back to her childhood. “Since I was a young kid, I knew I wanted to be in medicine. I enjoy helping people and I thought it would be something that I’d be good at, because I felt passionate about it,” she says. “I realized that while I love doing research, I also really enjoy interacting with patients. I wanted a combination of the two.”
In medical school, eventually her love of heart physiology won out over her interest in pediatrics. Benkert says she “basically did a 180” by deciding to go into cardiothoracic surgery. “I love taking care of critically ill patients. And once I was exposed to surgery, I couldn’t imagine doing anything outside of the field,” she added.
Benkert is excited by the prospect of working as a clinician while conducting research and working in the translational space. “I hope to be involved in translational projects and eventually clinical trials with patients. I think this grant sets a nice foundation for that by allowing me the time and the funding to work in the lab so that I am able to get research years as part of my residency training.”
Congratulations, Abby! We’re excited to see your career take off!
ACC.23: Lerman’s Paragonix Interview; Burkett Poster Presentation
 We missed these items a couple of weeks ago, but still wanted to share! Cardiology fellow Joe Lerman was interviewed by Mary Jacoski, senior director of Scientific and Medical Affairs for Paragonix Technologies during the ACC Scientific Sessions. Lerman presented a sub-study analysis on post-transplant outcomes in patients on a durable LVAD from of the GUARDIAN-Heart trial. You can see her interview with Lerman here: https://duke.is/n4m7e.
We missed these items a couple of weeks ago, but still wanted to share! Cardiology fellow Joe Lerman was interviewed by Mary Jacoski, senior director of Scientific and Medical Affairs for Paragonix Technologies during the ACC Scientific Sessions. Lerman presented a sub-study analysis on post-transplant outcomes in patients on a durable LVAD from of the GUARDIAN-Heart trial. You can see her interview with Lerman here: https://duke.is/n4m7e.
And, Melissa Burkett, nurse practitioner in cardiothoracic surgery, presented her poster, Adherence to Antibiotic Prophylaxis After Valve Replacement Surgery.
Nicely done, Joe and Melissa!
Quick Reminders & Updates
- Please do not hold doors open for non-Duke Health employees! You’re not being rude, you’re maintaining safety for our patients and for each other.
- The AANC site visit for DUH Magnet re-designation will take place March 28-31.
- New funding opportunity for fellows! See Mario Family Foundation Award announcement under Opportunities, below. Deadline to apply is May 1.
- National Doctor’s Day is Thursday, March 30!
Upcoming Events & Opportunities
Cardiology Grand Rounds
March 28: The Global Burden of Cardiovascular Diseases and Risks with Gregory Roth, director of the Program in Cardiovascular Health Metrics and associate professor of medicine in cardiology at the University of Washington in Seattle. 5 p.m., DN 2002 or via Zoom.
April 25: Regulatory Guidance for Cardiovascular Outcomes Trials of Antihyperglycemic Agents: Connecting the Past with the Future with Darren K. McGuire, University of Texas Southwestern Medical Center & Parkland Health and Hospital System; Deputy Editor, Circulation. 5 p.m., DN 2002 and via Zoom.
ICYMI: Links to Recent CGRs
March 14: Italo Biaggioni of Vanderbilt University Medical Center, Role of Sympathetic Nervous System in Obesity Hypertension. https://duke.is/v73n9 (Please note, the CGR begins at 00:16:55).
March 15: Patrick O’Gara of Brigham and Women’s Hospital and Harvard Medical School, Asymptomatic Valvular Heart Disease. https://duke.is/zd96e (Please note, the CGR begins at 00:10:05)
March 21: Emily S. Lau of Mass General and Harvard Medical School presentation, What Can Sex Differences Teach Us about HFpEF ? https://duke.is/9f78c (Please note, CGR begins at 00:12:05)
2023 Dean’s Research Series
The Dean’s Research Series continues on Thursday, March 30 and Thursday, April 20. Full schedule and details can be found at medschool.duke.edu/research-series. The Zoom link for all faculty lectures is https://bit.ly/Duke-DDRS.
The Duke University School of Medicine’s Dean’s Distinguished Research Series showcases groundbreaking research from the basic, clinical, and translational sciences. All faculty, staff, trainees and students are welcome to attend.
Funding Opportunity: The Mario Family Foundation Award
Training the next generation of biomedical researchers is an important core mission of the Department of Medicine. We admit the most promising, dedicated fellows into our programs, and provide experiences that will allow them to put their passion for medicine to work. These fellows will be tomorrow’s leaders in science and medicine. The Mario Family Foundation has generously supported this mission to support junior investigators in training to make the transition to become independent scientists and planning for their first extra-mural funding.
The Department of Medicine is accepting applications from fellows in specialty training for the Mario Family Foundation Award, which funds two patient-oriented research (clinical or translational) proposals for one year of funding. The total funding for all proposal expenses is $35,000.
Applications must be submitted electronically no later than Monday, May 1, 2023, 5p.m.
Applications will be peer reviewed by a panel of senior scientists from the Department of Medicine. Proposals will be judged on scientific-merit, rigor, and quality of project. Our intent is to complete reviews and start funding by July 1, 2023.
Additional details and application information can be found on the Mario Family Foundation Award webpage. For project-related questions, please contact Saini Pillai, MBA, Senior Program Coordinator, Chair’s Office.
Cardiac Safety Research Consortium Think Tank Meeting, June 7
The Cardiac Safety Research Consortium will hold a Think Tank meeting on June 7. The event, CSRC Think Tank: Update on Regulatory Status of Hypertension, Biomarkers and Arrhythmia Monitoring in Clinical Trials will be held at the FDA.
In Session 1, these leading industry professionals will speak on panels discussing:
- Regulations for ECG/QT
- The double-negative conundrum
- Alternative methods for assay sensitivity assessment in routine Phase 1 QT Studies
- Covid-19 and prolonged QT
In Session 2, we will discuss:
- Small increases in blood pressure and CV risk I
- Intermittent versus chronic use hypertension drugs
In Session 3, the meeting faculty will dive into:
- Biomarkers
In Session 4, the panelists will discuss hot topics in the field such as:
- Biologics/cardiomyopathy and vaccine development
- MACE
- Gene therapies
- Wearables
The event will include professionals from FDA Regulatory, Cardiac Safety Consultants, Ltd., Eli Lilly, Richmond Pharmacology, University of Connecticut, Stanford University, University of Pennsylvania, Cleveland Clinic, Clario, Mass General, DSI, Penn Medicine, and UCSF.
There is a registration fee for attendance, for academics it is $275. Registration and more information is available here: https://cardiac-safety.org/
The meeting will be held in person; a recording of the meeting and slide presentations will become available a month after the event occurs.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart Pulse 3-19-2023
Chief’s message: Spring Breaks and March Madness
This was a particularly busy week for Duke Heart with several visiting professors as noted before. Italo Biaggioni of Vanderbilt University Medical Center gave a great grand rounds on Role of Sympathetic Nervous System in Obesity Hypertension. For those with Duke access can use the link below to see the lectures. We also had a wonderful visit from Pat O’Gara who gave the 17th J.G. Reves Lecture – a lecture started by Jerry Reves in honor of building and starting the Duke Heart Center over 30 years ago. The time for coordinated care and working through how we get closer to serving our patients could not be more important. Dr. O’Gara gave the lecture, visited with fellows and faculty across Duke Heart, and then was also able to give cardiology grand rounds. We are appreciative of his inspirational visit.
We were out of town this week and were able to visit the Grand Canyon National Park, Upper Antelope, and Horseshoe Bend Arizona (pictured) where the Colorado River turns back on itself when faced with significant opposing rock formations. The natural wonders were great to see with family and provide perspective on how change happens in nature and the delicate balance between ecosystems. We were able to find a heart in Upper Antelope Canyon (pictured) where 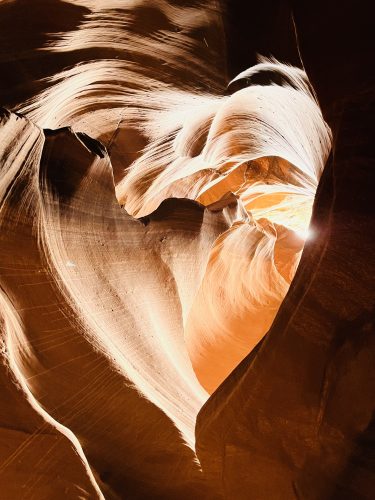 depending on day and time the light can make quite a few amazing streams. Also, during the travels we saw other members from Duke Heart on spring breaks to similar and distant locations.
depending on day and time the light can make quite a few amazing streams. Also, during the travels we saw other members from Duke Heart on spring breaks to similar and distant locations.
Finally, many of us are following March Madness basketball and the twists and turns for teams. The Duke Basketball team lost on Saturday to Tennessee, but the year in reflection highlighted the impact that teamwork, coaching, and effort can have as all of the school will be proud of the accomplishments of the team, wonder about what could have been, and hope springs eternal for returning players and next year’s team. Hopefully all of you will get sometime this spring to be with family.
Highlights of the week:
Annual Reves Lecture Held
The 17th annual J. G. Reves, MD Lecture was held on Wednesday with Patrick O’Gara, MD, as the guest speaker. His lecture, Research and Decision-Making at the Interface Between Cardiac Surgery and Cardiology, was well received! O’Gara is the Watkins Family Distinguished Chair in Cardiology and professor of medicine, Harvard Medical School, and the director of Strategic Planning for the cardiovascular division of Brigham and Women’s Hospital. We enjoyed having him at Duke – and especially delighted that he was able to spend some quality time with our fellows!


The Annual Reves Lecture is arranged by Duke’s Department of Anesthesiology and honors Dr. Jerry Reves, a former Duke cardiac anesthesiologist and a founding member of the Duke Heart Center.
Dr. O’Gara gave a special Cardiology Grand Rounds lecture as part of his visit to Duke. A link can be found below, in the CGR section.
We’d like to add a very special shout-out to Christy Johnson for her efforts in helping to organize his visit to Duke. Thanks, Christy!
Patel to Receive AHA National 2023 Physician of the Year Award
We’re pleased to share that Manesh Patel, MD will receive the American Heart Association’s 2023 Physician of the Year Award. The announcement was made on Thursday by Nancy Brown, CEO of the AHA. Patel is among nearly two dozen people and organizations who will be recognized during the AHA’s National Volunteer Awards event on Wednesday, June 14. The event will be held virtually.

The AHA’s Physician of the Year Award honors a physician with a longstanding commitment to the highest ideals of patient care and exemplary leadership in the AHA mission. Patel currently serves on the Board of the Triangle AHA, has led programming for the AHA Scientific Sessions and committees, and is a strong advocate for research, safety, and quality care for cardiovascular patients. He regularly gives his time to advocacy, and is a long-time supporter of the annual Triangle Heart Walk.
Manesh stated “I am humbled by the award, and it speaks to the longstanding ethos of service and work with the AHA that so many of my mentors and colleagues have instilled as part of our culture at Duke. I hope to be able to give back as they have to our community and mentor the next generation.”
Great Catch, McGugan!
Lynn McGugan, one of our nurse practitioners on 7 West received a Great Catch this week from DUH administration! McGugan  recognized a discrepancy in an order set for temporary mechanical circulatory support that contraindicated the specific device policy and would have resulted in asking nurses to practice outside of their scope. Appropriate stakeholders were engaged, and the order set was immediately updated.
recognized a discrepancy in an order set for temporary mechanical circulatory support that contraindicated the specific device policy and would have resulted in asking nurses to practice outside of their scope. Appropriate stakeholders were engaged, and the order set was immediately updated.
Kudos to Lynn for calling out this discrepancy in a long-standing order set, showing willingness to question the status quo in the name of safety!
Way to go, Lynn!
Shout-out to CICU Nursing Staff!
A big shout-out to nurses from the Cardiology Intensive Care Unit – they were able to arrange for one of our long-term patients to go outside for a bit. The patient was deeply appreciative of this. Special recognition to nurses Yu Wang and Morgan Stone, and to nursing assistant Allyson Blake.
According to Jason Katz, “It was the first time this patient had seen the sun or felt fresh air in over two months – and the last time (the patient had been outdoors) was on the tarmac to be flown to Duke University Hospital for emergent care. We topped things off with a vanilla milkshake from Chick-Fil-A — it was his favorite and he enjoyed it quite a lot.”
Our nursing team is amazing!!! Thank you for all that you do.

Cardiac Cath Team Featured in Working @Duke
Hat tip to the “Cath Us If You Can” team, comprised of members of Duke Heart’s cardiac catheterization unit. They’re featured in the most recent issue of Working@Duke for their participation in Duke’s Get Moving Challenge. Thanks for literally walking the walk and getting your steps and exercise in! To read the story, visit https://duke.is/mpapm.
ICYMI: Quick Thinking Mother Saves Daughter with CPR, AED
A really terrific story out of Duke pediatric cardiology this week, which was featured on the Today show, Good Morning America, and several local news outlets here in the Triangle. The mother of a cheerleader recognized that her daughter had gone into cardiac arrest, and quickly began performing CPR until an AED was brought to her. Her daughter survived and was transported to Duke University Hospital, where she received care from Dr. Zebulon Spector. Links to the news stories are below under News.
This is another great example of why knowing CPR and having access to AEDs is important!
Quick Reminders & Updates
- Please do not hold doors open for non-Duke Health employees! You’re not being rude, you’re maintaining safety for our patients and for each other.
- The AANC site visit for DUH Magnet re-designation will take place March 28-31.
- New funding opportunity for fellows! See Mario Family Foundation Award announcement under Opportunities, below. Deadline to apply is May 1.
Updates to COVID Protocols
Leadership announced earlier today several changes to the COVID protocols:
“As we head into the home stretch of the academic year, we find our campus’ COVID risk to be far less serious than any time during the pandemic. During the last 18 months, we have seen immunity through vaccination or natural infection increase to about 90 percent of our population. This has led to a steep decline in cases and severe illness. As a result, we are making several changes to our COVID protocols.
- Masking: Masking on Duke buses and vans is now recommended, but will no longer be required. Masks will be available on buses for those who request one. Masking is still required in all patient-care and clinical settings and for anyone who is symptomatic and around others, regardless of location or test results.
- COVID Vaccination: Duke’s medical experts are currently assessing potential changes in the COVID vaccination policy given the increase in community immunity levels and decline in severity of illness. More information will be shared once decisions are finalized.
- Surveillance Testing: The last two remaining surveillance test sites ended operation before spring break. Symptomatic testing will continue to be available on campus through Student Health or the Employee Exposure Hotline, 919-385-0431, option 1.
- Rapid Antigen Tests: At-home antigen tests are available through the Duke Stores’ Service Desk in the Bryan Center. One test kit per week is available at no charge to anyone with a valid DukeCard.
- SymMon App: The SymMon app used for reporting symptoms or test results will be retired on April 3. Employees can use the My COVID Link to report symptoms or test results, and students should contact Student Health to do the same.
- Student Case Management: Formal student COVID case management will conclude on Sunday, March 19. Going forward, students who test positive for COVID should isolate in place for at least 5 days from symptom onset and wear a mask when indoors or around others for 10 days. For nurse advice or to make an appointment with a medical provider, students can call Duke Student Health at 919-681-9355.
As has been the case throughout the pandemic, these changes are based on the data, trends and science. We acknowledge the possibility that a new COVID variant could change the current trends and require us to modify our approach regarding vaccination, masking and other safety protocols. We will continue to monitor and assess global and local data to determine if such changes are needed in the future. Anyone testing positive should continue to report to Employee Health or Student Health, mask and isolate in place as required before returning to work, class or academic activities.
Thank you for your ongoing support and collective efforts during these difficult years. Working together as a community, we have learned, adapted, and overcome so many challenges.”
DHIP update
Distribution of Employment Agreements for transitioning members is ongoing. Please monitor your inbox for critical communication from DHIP@duke.edu, your department chair, and Adobe Sign.
Reminder: The Duke Guarantee offers the minimum compensation each Member can expect to receive. Additional compensation opportunities which exist today will continue to be available to members within DHIP.
All members will be given four weeks to consider employment and sign their Employment Agreements.
Benefits:
- A benefits transition FAQ for PDC Direct staff is available on org.
- Information regarding Duke Benefits is available on SharePoint.
- All benefits related questions can be sent to DHIPBenefits@Duke.edu.
All other questions can be sent to DHIP@duke.edu, and all DHIP updates can be found at https://dhip.org.
Upcoming Events & Opportunities
Cardiology Grand Rounds
March 21: What Can Sex Differences Teach Us about HFpEF ? with Emily S. Lau, Director, Cardiometabolic Health and Hormones Clinic, Massachusetts General Hospital; Instructor in Medicine, Harvard Medical School. 5 p.m., Zoom only.
ICYMI: Links to Recent CGRs
In case you were unable to join us, we have links available to our most recent Cardiology Grand Rounds:
February 16: Haider Warraich of VA Boston Healthcare System, State of the Heart: What the History of Heart Disease Teaches Us About Its Future. https://duke.is/26j5p
February 28: Sandeep Nathan of the University of Chicago, Percutaneous Mechanical Circulatory Support (pMCS) in High Risk PCI and Shock: Facts, Fiction & Future Devices. https://duke.is/g2dzh (Please note, the CGR begins at 00:21:47).
March 14: Italo Biaggioni of Vanderbilt University Medical Center, Role of Sympathetic Nervous System in Obesity Hypertension. https://duke.is/v73n9 (Please note, the CGR begins at 00:16:55).
March 15: Patrick O’Gara of Brigham and Women’s Hospital and Harvard Medical School, Asymptomatic Valvular Heart Disease. https://duke.is/zd96e (Please note, the CGR begins at 00:10:05)
2023 Dean’s Research Series
The Dean’s Research Series continues on Thursday, March 30 and Thursday, April 20. Full schedule and details can be found at medschool.duke.edu/research-series. The Zoom link for all faculty lectures is https://bit.ly/Duke-DDRS.
The Duke University School of Medicine’s Dean’s Distinguished Research Series showcases groundbreaking research from the basic, clinical, and translational sciences. All faculty, staff, trainees and students are welcome to attend.
Funding Opportunity: The Mario Family Foundation Award
Training the next generation of biomedical researchers is an important core mission of the Department of Medicine. We admit the most promising, dedicated fellows into our programs, and provide experiences that will allow them to put their passion for medicine to work. These fellows will be tomorrow’s leaders in science and medicine. The Mario Family Foundation has generously supported this mission to support junior investigators in training to make the transition to become independent scientists and planning for their first extra-mural funding.
The Department of Medicine is accepting applications from fellows in specialty training for the Mario Family Foundation Award, which funds two patient-oriented research (clinical or translational) proposals for one year of funding. The total funding for all proposal expenses is $35,000.
Applications must be submitted electronically no later than Monday, May 1, 2023, 5p.m.
Applications will be peer reviewed by a panel of senior scientists from the Department of Medicine. Proposals will be judged on scientific-merit, rigor, and quality of project. Our intent is to complete reviews and start funding by July 1, 2023.
Additional details and application information can be found on the Mario Family Foundation Award webpage. For project-related questions, please contact Saini Pillai, MBA, Senior Program Coordinator, Chair’s Office.
Cardiac Safety Research Consortium Think Tank Meeting, June 7
The Cardiac Safety Research Consortium will hold a Think Tank meeting on June 7. The event, CSRC Think Tank: Update on Regulatory Status of Hypertension, Biomarkers and Arrhythmia Monitoring in Clinical Trials will be held at the FDA.
In Session 1, these leading industry professionals will speak on panels discussing:
- Regulations for ECG/QT
- The double-negative conundrum
- Alternative methods for assay sensitivity assessment in routine Phase 1 QT Studies
- Covid-19 and prolonged QT
In Session 2, we will discuss:
- Small increases in blood pressure and CV risk I
- Intermittent versus chronic use hypertension drugs
In Session 3, the meeting faculty will dive into:
- Biomarkers
In Session 4, the panelists will discuss hot topics in the field such as:
- Biologics/cardiomyopathy and vaccine development
- MACE
- Gene therapies
- Wearables
The event will include professionals from FDA Regulatory, Cardiac Safety Consultants, Ltd., Eli Lilly, Richmond Pharmacology, University of Connecticut, Stanford University, University of Pennsylvania, Cleveland Clinic, Clario, Mass General, DSI, Penn Medicine, and UCSF.
There is a registration fee for attendance, for academics it is $275. Registration and more information is available here: https://cardiac-safety.org/
The meeting will be held in person; a recording of the meeting and slide presentations will become available a month after the event occurs.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
March 10 — John Alexander
Pharmacist.com/APhA
Statin alternative joins drugs that could reduce heart attack risk
https://duke.is/6g5mk
March 13 — John Alexander
NPR/Morning Edition
Got muscle pain from statins? A cholesterol-lowering alternative might be for you
https://duke.is/p5j62
March 14 — Tony Gutierrez
El Confidencial
¿Podemos de verdad morir de la risa? Esto es lo que dice la ciencia y la historia
https://duke.is/ys84c
March 14 — Neha Pagidipati
HealthDay
ACC: Coordinated Intervention Increases Rx for Evidence-Based T2DM Therapies
https://duke.is/zjk5r
*also carried by 65 additional outlets including Drugs.com, Physician’s Weekly
March 14 — Keianna & Andrea Joe
WCNC NBC-36 Charlotte
NC cheerleader recovering after going into cardiac arrest during competition
https://duke.is/ms52v
March 14 — Keianna & Andrea Joe
WRAL NBC-5
Mother saves life of 17-year-old daughter who went into cardiac arrest at Raleigh high school
https://duke.is/8ejc5
March 15 — Zebulon Spector (pediatrics) and Keianna & Andrea Joe
Today show, NBC
Mom saves teen daughter’s life after she had cardiac arrest at a cheerleading competition
https://duke.is/c48sy
March 15 — Danielle Wood (pediatrics)
Clinical Advisor
Protocol Reduces Opioid Exposure in Pediatric Cardiac ICU
https://duke.is/wvkds
March 15 — Zebulon Spector and Keianna & Andrea Joe
People.com
https://duke.is/633yb
Consumer news coverage will return on April 2. Thanks for reading!
Division of Cardiology Publications: March 9-15, 2023
Blumer V, Zhbannikov IY, Douglas PS. Contributions of Women to Cardiovascular Science Over Two Decades: Authorship, Leadership, and Mentorship. J Am Heart Assoc 2023 Mar 7;12(5):e026828. PM: 36847072.
Chi G, Violi F, Pignatelli P, Vestri A, Spagnoli A, Loffredo L, Hernandez AF, Hull RD, Cohen AT, Harrington RA, Goldhaber SZ, Gibson CM. External validation of the ADA score for predicting thrombosis among acutely ill hospitalized medical patients from the APEX Trial. J Thromb Thrombolysis 2023 Feb;55(2):211- 221. PM: 36566304.
Desai MY, Owens A, Geske JB, Wolski K, Saberi S, Wang A, Sherrid M, Cremer PC, Naidu SS, Smedira NG, Schaff H, McErlean E, Sewell C, Balasubramanyam A, Lampl K, Sehnert AJ, Nissen SE. Dose-Blinded Myosin Inhibition in Patients With Obstructive Hypertrophic Cardiomyopathy Referred for Septal Reduction Therapy: Outcomes Through 32 Weeks. Circulation 2023 Mar 14;147(11):850-863. PM: 36335531.
Filbey L, Zhu JW, D’Angelo F, Thabane L, Khan MS, Lewis E, Patel MR, Powell-Wiley T, Miranda JJ, Zuhlke L, Butler J, Zannad F, Van Spall HGC. Improving representativeness in trials: a call to action from the Global Cardiovascular Clinical Trialists Forum. Eur Heart J 2023 Mar 14;44(11):921-930. PM: 36702610.
Greene SJ, Felker GM. Considering Addition of Acetazolamide to Loop Diuretics as Treatment for Acute Heart Failure: ADVOR Reappraisal. JACC Heart Fail 2023 Mar;11(3):365-367. PM: 36889884.
Hsueh YC, Pratt RE, Dzau VJ, Hodgkinson CP. Novel method of differentiating human induced pluripotent stem cells to mature cardiomyocytes via Sfrp2. Sci Rep 2023 Mar 9;13(1):3920. PM: 36894665.
Khedagi A, Hoke C, Kelsey M, Coviello A, Jones WS, Jackson LR, Patel MR, McGarrah RW, Pagidipati NJ, Shah NP. Call to action: Understanding the differences in the use of SGLT-2 inhibitors and GLP-1 receptor agonists. Am J Prev Cardiol 2023 Feb 24;13:100477. PM: 36915710.
Maia IS, Marcadenti A, Veiga VC, Miranda TA, Gomes SPC, Carollo MBS, Negrelli KL, Gomes JO, Tramujas L, Abreu-Silva EO, Westphal GA, Fernandes RP, Horta JGA, Oliveira DC, Flato UAP, Paoliello RCR, Fernandes C, Zandonai CL, Coelho JC, Barros WC, Lemos JC, Bolan RS, Dutra MM, et al. Antivirals for adult patients hospitalised with SARS-CoV- 2 infection: a randomised, phase II/III, multicentre, placebo-controlled, adaptive study, with multiple arms and stages. COALITION COVID-19 BRAZIL IX-REVOLUTIOn trial. Lancet Reg Health Am 2023 Apr;20:100466. PM: 36908503.
Montalescot G, Alexander JH, Cequier-Fillat A, Solomon SD, Redheuil A, Hudec M, Silvain J, Kachenoura N, Janas A, Orban M, Josse I, Balavoine F, Besse B. Firibastat Versus Ramipril After Acute Mechanical Reperfusion of Anterior Myocardial Infarction: A Phase 2 Study. Am J Cardiovasc Drugs 2023 Mar;23(2):207- 217. PM: 36757536.
Schnittman SR, Jung W, Fitch KV, Zanni MV, McCallum S, Lee JS, Shin S, Davis BJ, Fulda ES, Diggs MR, Giguel F, Chinchay R, Sheth AN, Fichtenbaum CJ, Malvestutto C, Aberg JA, Currier J, Lauffenburger DA, Douglas PS, Ribaudo HJ, Alter G, Grinspoon SK. Effect of host factors and COVID-19 infection on the humoral immune repertoire in treated HIV. JCI Insight 2023 Mar 8;8(5):e166848. PM: 36805331.
Selvaraj S, Kosiborod MN, Shah SH. Response by Selvaraj et al to Letter Regarding Article, “Metabolic Profiling of the Effects of Dapaglifozin in Heart Failure with Reduced Ejection Fraction: DEFINE-HF.” Circulation 2023 Mar 14;147(11):922-923. PM: 36913500
Duke Heart Pulse March 12th 2023
Cheif’s Message
This week marks the start of March Madness – with Duke winning the ACC tournament, the NCAA tournament starting, and lots of excitement as many in our faculty start to go on spring breaks and vacations. This week we are blessed to have two visiting professors for important talks. Italo Biaggionni will be giving grand rounds on Tuesday on the importance of the sympathetic nervous system in obesity and hypertension. On Wednesday, we have Pat O’Gara giving the annual Reves Lecture in the morning 7-8 AM on “Research and Decision-Making at the Interface Between Cardiac Surgery and Cardiology” and Special Cardiology Grand Rounds at 5 pm on Asymptomatic Valve Disease. These talks and the week will be jam packed for our faculty and fellows. Hopefully many will have a chance to enjoy this season and these important topics and lectures.
Highlights of the week:
ACC.23: Intervention Helps Clinicians Meet Guidelines for Prescribing Diabetes, Heart Drugs
Patients who have diabetes and heart disease do best when both conditions are treated according to established guidelines, but far too many are not prescribed the effective therapies.
A recent study — designed and led by the Duke Clinical Research Institute (DCRI) and an academic steering committee — found that a coordinated care approach between cardiologists and diabetes specialists resulted in more patients receiving the recommended therapies. The study was funded by Boehringer Ingelheim and Eli Lilly and Company.
 The findings were presented March 6 at the 2023 American College of Cardiology scientific meeting and simultaneously published in the Journal of the American Medical Association.
The findings were presented March 6 at the 2023 American College of Cardiology scientific meeting and simultaneously published in the Journal of the American Medical Association.
“There’s a clear gap between what we know we should be doing and what is actually occurring in clinical practice,” said lead author Neha Pagidipati, MD, associate professor in the Division of Cardiology at Duke University School of Medicine and a member of the DCRI. “Our study demonstrates that coordinated, multi-disciplinary care can result in patients receiving the therapies that have been proven effective.”
Pagidipati and colleagues — including senior author Christopher Granger, MD, professor of medicine in Duke’s cardiology division and DCRI member – partnered with 43 cardiology clinics across the U.S. as part of a clinical trial titled COORDINATE-Diabetes.
The clinics were randomly assigned to provide usual care or to implement a multi-faceted intervention. It was designed to remove barriers that keep cardiology clinicians from prescribing medications recommended for patients with diabetes and atherosclerotic cardiovascular disease, a narrowing of the arteries.
The recommended drug regimen includes high-intensity statins for cholesterol; angiotensin-converting enzyme inhibitors or angiotensin receptor blockers to lower blood pressure and protect heart and kidney health; and, for diabetes along with heart and kidney health, sodium-glucose cotransporter-2 inhibitors and/or glucagon-like peptide-1 receptor agonists.
The intervention required clinicians/clinics to:
- Assess barriers in the clinic that prevent or impede the patients from receiving the recommended prescriptions;
- Build interdisciplinary care teams to address barriers, including cardiologist, diabetes care specialists, pharmacists and others to address costs and access issues;
- Coordinate care between all participating clinicians and care teams;
- Provide clinician education through online learning modules and monthly calls to address questions and concerns;
- Provide feedback with real-time data, including comparative reports showing patient prescription numbers across all sites;
- Support patients with education tools about why the therapies are important and how they impact health markers.
More than 1,000 patients were enrolled and followed for up to 12 months. Among the clinics providing usual care, 14.5% patients were prescribed all the recommended therapies, while 37.9% of patients at the intervention sites received all three prescriptions.
“A 23-percent greater absolute use of three evidence-based therapies shows that coordinated efforts to implement effective therapies can result in markedly improved care,” Granger said. “Given the many treatments that are known to improve health, now the most important need is to generate high-level, randomized evidence to improve the use of these treatments. This is what we did in this trial.”
The study was not designed to measure the impact of the drug regimen on health risks, but an analysis showed that the intervention had a trend of risk reduction that would be expected with better use of the medications studied. Death or hospitalization for myocardial infarction, stroke, heart failure, or urgent revascularization occurred in 23 of the intervention participants (5%) compared to 40 of the usual care participants (6.8%).
“This was an evaluation of an intervention to see if it could improve prescribing behavior for three proven, recommended therapies,” Pagidipati said. “It not only is effective, it is also scalable to clinical use in real-world settings.”
In addition to Pagidipati and Granger, study authors include Adam J. Nelson, Lisa A. Kaltenbach, Monica Leyva, Darren K. McGuire, Rodica Pop-Busui, Matthew A. Cavender, Vanita R. Aroda, Melissa L. Magwire, Caroline R. Richardson, Ildiko Lingvay, Julienne K. Kirk, Hussein R. Al-Khalidi, Laura Webb, Tanya Gaynor, Jonathan Pak, Cagri Senyucel, Renato D. Lopes, and Jennifer B. Green.
Pagidipati and Granger receive institutional research support from funders Boehringer Ingelheim and Lilly; a full listing of author conflicts is provided in the study manuscript.
The study was initiated and led by an academic steering committee. The two pharmaceutical funders participated in the design and conduct of the study, interpretation of the data, and review and approval of the manuscript.
Wrapping Up ACC.23
Congratulations to all of our Duke presenters on a very successful ACC!
Presenting fellows included: Willard Applefeld, Balim Senman, Kelly Arps, Anthony Peters, Jamie Diamond, Karen Flores Rosario, Joe Lerman, Josephine Harrington, and Jessica Duran.
Faculty speakers, panelists, and moderators included: Marat Fudim, Jason Katz, Karen Alexander, Neha Pagidipati, Pamela Douglas, Jenn Rymer, Schuyler Jones, Rob Mentz, Stephen Greene, Mike Felker, and Adam DeVore.
Overall, we had more than 25 speakers, 19 moderated sessions, 26 posters presented, and two Late-Breaking sessions. Lots of interviews were done — all news coverage appears below in our News section. Be sure to check it out!

Three Duke Cardiologists Ranked Among Best in the World for Science
Three of our cardiologists have made Research.com‘s first-ever list of top female scientists in the world. Congratulations go to Pamela S. Douglas, Yongmei Liu, and L. Kristin Newby!!!
The Research.com ranking of top female scientists in the world includes leading female scientists from all major areas of science. It is based on a meticulous examination of 166,880 scientists on Google Scholar and Microsoft Academic Graph, according to the publication.
Douglas, Liu, and Newby are prolific researchers dedicated to their area of specialty within the cardiovascular space. They are among 13 women from Duke who made the list.
Pamela S. Douglas, the Ursula Geller Professor of Research in Cardiovascular Diseases in the division of cardiology and a member in the Duke Clinical Research Institute. Douglas was recently awarded the 2022 James B. Herrick Award at the American Heart Association’s annual meeting in November. She is past president of the American College of Cardiology and a tireless advocate for equity and diversity in healthcare.
Yongmei Liu, professor of medicine in cardiology and in population health sciences, is a member of the  Duke Molecular Physiology Institute. Liu is a genetic epidemiologist whose primary interests are to better understand the molecular mechanisms of aging-related inflammatory diseases — including diabetes, atherosclerosis, and Alzheimer’s disease.
Duke Molecular Physiology Institute. Liu is a genetic epidemiologist whose primary interests are to better understand the molecular mechanisms of aging-related inflammatory diseases — including diabetes, atherosclerosis, and Alzheimer’s disease.

Kristin Newby, professor of medicine in cardiology and a member of the DCRI, focuses her clinical research on on the process and treatment of acute and chronic coronary artery disease and systems issues for delivery of care to patients with these illnesses.
To see the full list, please visit: https://research.com/scientists-rankings/best-female-scientists.
Congratulations, Pam, Yongmei, and Kristin! This is outstanding news and well-deserved recognition.
Shout-out to Shadrin!
High praise this week goes out to cardiology fellow, Ilya Shadrin! We received a note this week from Anita Kelsey, which was shared with Anna Lisa Chamis and Lawrence Liao: 
“I just wanted to take a moment to thank Ilya Shadrin who I worked with in the echo lab today. He was post call and doing procedures with Lawrence Laio, in the echo lab all day. At 5 pm, when he finished his regular day’s work, he went with 2 different sonographers to perform stat echocardiograms in the ED. He didn’t stop there in his dedication to our patients, he spoke with both teams taking care of the patients to make sure they knew the critical results found on the echocardiograms. Ilya should be recognized for going above and beyond for our patients. Way to go Ilya!” – Anita Kelsey
Solid work!
Fellow Presentations at Dean’s Research Series
Cardiology fellows Jessica Regan and Joe Lerman each presented posters on Thursday at the 2023 Dean’s Distinguished Research Series.
 Jessica Regan presented Peroxisomal and Mitochondrial Metabolites Associate with Clonal Hematopoiesis of Indeterminate Potential, while Joe Lerman presented Use of the SherpaPak Cardiac Transport System for donor heart preservation associated with Improved Short-Term Outcomes as comparted to the use of traditional cold storage in LVAD patients undergoing Heart Transplantation.
Jessica Regan presented Peroxisomal and Mitochondrial Metabolites Associate with Clonal Hematopoiesis of Indeterminate Potential, while Joe Lerman presented Use of the SherpaPak Cardiac Transport System for donor heart preservation associated with Improved Short-Term Outcomes as comparted to the use of traditional cold storage in LVAD patients undergoing Heart Transplantation.
The Dean’s Research Series continues on Thursday, March 30 and Thursday, April 20. Full schedule and details can be found at medschool.duke.edu/research-series. The Zoom link for all faculty lectures is https://bit.ly/Duke-DDRS.
and details can be found at medschool.duke.edu/research-series. The Zoom link for all faculty lectures is https://bit.ly/Duke-DDRS.
The Duke University School of Medicine’s Dean’s Distinguished Research Series showcases groundbreaking research from the basic, clinical, and translational sciences. All faculty, staff, trainees and students are welcome to attend.
Well done, Jessica and Joe! Congratulations!
ICYMI: Morgenstern’s Featured in Working@Duke
Administrative manager for the division of cardiology Chris Morgenstern, and his wife, are featured in the latest issue of Working@Duke magazine. They’re shown in the lead story, Three Years Later: How the Pandemic Changed Us under ‘Rethinking What’s Most Important’.
Great photo, Chris! You can see the story here on Duke Today.

Quick Reminders
- This week is Patient Safety Awareness week, Pulmonary Rehabilitation week and Medical Genetics Awareness week; March is National Nutrition and Women’s History
- Please do not hold doors open for non-Duke Health employees! You’re not being rude, you’re maintaining safety for our patients and for each other.
- The Duke Health Quality and Safety Conference starts this week. Registration is required. There are virtual and in-person sessions. To learn more, visit: https://duke.is/5ek53.
- There will be an AANC site visit for DUH Magnet re-designation taking place March 28-31.
- Jacob Schroder is celebrating a birthday this month. Check out this amazing cake he received! Happy Birthday, Jacob!

DHIP update
Distribution of Employment Agreements for transitioning members is ongoing. Please monitor your inbox for critical communication from DHIP@duke.edu, your department chair, and Adobe Sign.
Reminder: The Duke Guarantee offers the minimum compensation each Member can expect to receive. Additional compensation opportunities which exist today will continue to be available to members within DHIP.
All members will be given four weeks to consider employment and sign their Employment Agreements.
Benefits:
- A benefits transition FAQ for PDC Direct staff is available on org.
- Information regarding Duke Benefits is available on SharePoint.
- All benefits related questions can be sent to DHIPBenefits@Duke.edu.
All other questions can be sent to DHIP@duke.edu, and all DHIP updates can be found at https://dhip.org.
Upcoming Events & Opportunities
Cardiology Grand Rounds
March 14: Role of Sympathetic Nervous System in Obesity Hypertension with Italo Biaggioni of Vanderbilt University Medical Center. 5 p.m., Zoom.
March 15: 17th Annual J.G. Reves, MD Lecture, Research and Decision-Making at the Interface Between Cardiac Surgery and Cardiology with Patrick O’Gara, Watkins Family Distinguished Chair in Cardiology and Professor of Medicine, Brigham and Women’s Hospital and Harvard Medical School. 7 a.m., Duke North 2001 and via Zoom.
March 15: Asymptomatic Valvular Heart Disease with Patrick O’Gara, Watkins Family Distinguished Chair in Cardiology and Professor of Medicine, Brigham and Women’s Hospital and Harvard Medical School. 5 p.m., Duke North 2002 and via Zoom.
March 21: What Can Sex Differences Teach Us about HFpEF ? with Emily S. Lau, Director, Cardiometabolic Health and Hormones Clinic, Massachusetts General Hospital; Instructor in Medicine, Harvard Medical School. 5 p.m., Zoom only.
Duke REACH Equity Center Funding Opportunities:
Research Voucher, Scholars Development, Transdisciplinary Think Tank
Now accepting applications through March 17 for July 2023 funding.
The Duke REACH Equity Center awards support students, trainees, and faculty who are interested in conducting research that promotes health equity. All proposals should broadly address the REACH Equity theme: to reduce racial and ethnic disparities in health by improving the quality of patient-centered care in the clinical encounter across diseases, stages of illness, care settings, and throughout the life course. Proposals may include any research topic and method (quantitative, qualitative, etc.).
There are four funding opportunities:
The Research Vouchers Program will supplement currently funded research or support standalone research projects conducted by faculty at any level. Funding: One year, up to $12,500 per award.
- Full Research Vouchers Program RFA and application instructions are available here.
- Current awardee list is available here.
The Research Scholars Development Program is intended to support early-stage investigators (residents, fellows, postdoctoral students, nursing trainees, and other trainees at a similar career stage). Scholars work with a faculty mentor (identified by the trainee) to develop a research proposal and complete a project. Funding: Up to $5,000 for one- or two-year project per award.
- Full Research Scholars Development RFA and application instructions are available here.
- Current awardee list is available here.
The Transdisciplinary Think Tank (TTT) provides support to bring together faculty across disciplines who have a common interest in addressing racial and ethnic disparities in the clinical encounter. The TTT’s aim is to catalyze and support research related to the REACH Equity theme and to foster collaboration among health disparities researchers across Duke University. Funding: One year, up to $1,500 per award.
- The Full Transdisciplinary Think Tank RFA and application instructions are available here.
- Current awardee list is available here.
The Medical Student and Nursing Student Research Award is intended to support a third-year medical student or a third-year PhD nursing student conducting research related to the REACH Equity theme. Scholars work with a faculty mentor (identified by the student) to develop a research proposal and complete a project. Funding: Up to $5,000 for one-year project.
- Full Medical Student Research and Nursing Student Research Award and application instructions are available here.
- Current awardee list is available here.
Application submission deadline: March 17 for July 2023 funding.
Email reachequitycenter@duke.edu with questions.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
February 28 — Victor Dzau
Medpage Today/The Doctor’s Art
Victor Dzau on Leading the National Academy of Medicine
https://duke.is/veu92
March 4 — John Alexander
tctMD
Clear CVD Benefit With Bempedoic Acid: CLEAR Outcomes
https://duke.is/c3usz
March 4 — John Alexander
The Washington Post
Cholesterol drug lowers heart attack risk, avoids muscle side effects
https://duke.is/j6uxq
March 4 — John Alexander
HCP Live
Bempedoic Acid Reduces Risk of MACE by 13%, But Proves No Benefit on Cardiovascular Death
https://duke.is/ycgkr
March 4 — John Alexander
CNN Health
Bempedoic acid improved heart health in patients who can’t tolerate statins, study finds
https://duke.is/rhspj
March 4 — John Alexander
Medscape
Bempedoic Acid Cuts CV Events in Statin-Intolerant Patients: CLEAR Outcomes
https://duke.is/5aryp
March 4 — John Alexander
Healio/Cardiology
Bempedoic acid an ‘effective alternative’ for statin-intolerant patients: CLEAR Outcomes
https://duke.is/nfsdf
March 4 — John Alexander
Fox News
New cholesterol pill, Nexletol, lowers heart attack risk for patients who can’t take statins: study
https://duke.is/pnre4
March 4 — John Alexander
The New York Times
A Statin Alternative Joins Drugs That Can Reduce Heart Attack Risk
https://duke.is/49wr6
March 4 — Pamela Douglas
tctMD
On-site Machine Learning-Based FFRCT Feasible, Informative: TARGET
https://duke.is/zug5y
March 4 — Manesh Patel
Healio/Cardiology
Imaging data may predict best responders to evolocumab therapy: YELLOW III
https://duke.is/m5sts
March 4 — Manesh Patel
Medpage Today
Atorvastatin Tied to Cardioprotection for Lymphoma Patients on Anthracyclines
https://duke.is/8hrx3
March 5 — Stephen Greene
HCP Live
Don’t Miss a Beat: Top Takeaways from NUDGE FLU at ACC 2023
https://duke.is/c6w8t
March 5 — John Alexander
Voice of America & Listin Dario (via AP)
¿No puedes tomar estatinas? Nueva píldora reduce el colesterol y los ataques cardíacos
https://duke.is/6x6na
March 5 — John Alexander
Daily Sabah
Opposed to statins? Novel pill lowers cholesterol, heart attack risk
https://duke.is/2rnqm
March 6 — John Alexander
El Vocero
Nueva pastilla podría reducir el colesterol alto y los infartos
https://duke.is/pks6q
March 6 — Neha Pagidipati
DAIC.com
Multifaceted Strategy Boosts Preventive Care for Diabetes, Heart Disease
https://duke.is/rbuzu
March 6 — John Alexander
BioPharmaDive
Esperion shares sink on highly anticipated heart drug results
https://duke.is/5gghj
March 6 — Neha Pagidipati
Cardiovascular Business
Day 3 at ACC.23 features late-breaking studies on pulsed-field ablation, other new technologies
https://duke.is/5gghj
March 6 — Neha Pagidipati
HCP Live
https://duke.is/begff
March 6 — Neha Pagidipati
MDEdge
COORDINATEd effort boosts optimal therapy in patients with T2D and ASCVD
https://duke.is/g3kab
March 7 — John Alexander
Popular Science
Safer statin alternative could be a better way to lower ‘bad’ cholesterol levels
https://duke.is/44sgx
March 7 — Neha Pagidipati and Kristen Campbell
tctMD
Multifaceted Approach to COORDINATE Diabetes Care Improves GDMT
https://duke.is/98r96
March 7 — John Alexander
Medscape
https://duke.is/jfvce
March 8 — Stephen Greene
Healio/Cardiology
Lower use of guideline-recommended HF therapies at rural vs. urban hospitals
https://duke.is/6z3gm
March 8 — Manesh Patel
tctMD
HALO: Baxdrostat No Better Than Placebo in Uncontrolled Hypertension
https://duke.is/ps9wv
March 8 — Tony Gutierrez
Mental Floss
Can You Really Laugh Yourself to Death?
https://duke.is/54vqy
March 8 — Brittany Zwischenberger
Medscape
Worse Cardiac Outcomes Persist for Women: What’s the Problem?
https://duke.is/ngavq
March 9 — Brittany Zwischenberger
Espanol News
Peores resultados cardíacos persisten para las mujeres: ¿cuál es el problema?
https://duke.is/b58br
March 9 — Jason Katz
Medscape/InDiscussion HF Podcast (Ep. 4)
How to Mix Touch and Tech in Advanced Heart Failure
https://duke.is/cq9xj
March 9 — Nishant Shah
ACC.org
Division of Cardiology Publications: March 2-8, 2023
Ackerson BG, Sperduto W, D’Anna R, Niedzwiecki D, Christensen J, Patel P, Mullikin TC, Kelsey CR. Divergent Interpretations of Imaging After Stereotactic Body Radiation Therapy for Lung Cancer. Pract Radiat Oncol 2023 ;13(2):e126-e133. PM: 36375770.
Friedman DJ, Al-Khatib SM, Dalgaard F, Fudim M, Abraham WT, Cleland JGF, Curtis AB, Gold MR, Kutyifa V, Linde C, Tang AS, Ali-Ahmed F, Olivas- Martinez A, Inoue LYT, Sanders GD. Cardiac Resynchronization Therapy Improves Outcomes in Patients With Intraventricular Conduction Delay But Not Right Bundle Branch Block: A Patient-Level Meta- Analysis of Randomized Controlled Trials. Circulation 2023 Mar 7;147(10):812-823. PM: 36700426.
Hlatky MA, Wilding S, Stuart B, Nicholas Z, Shambrook J, Eminton Z, Fox K, Connolly D, O’Kane P, Hobson A, Chauhan A, Uren N, Mccann GP, Berry C, Carter J, Roobottom C, Mamas M, Rajani R, Ford I, Douglas PS, Curzen N. Randomized comparison of chest pain evaluation with FFR or standard care: Factors determining US costs. J Cardiovasc Comput Tomogr 2023 ;17(1):52-59. PM: 36216700.
Jain V, Maqsood MH, Siddiqi TJ, Siddiqi AK, Baloch ZQ, Kittleson MM, Fudim M, Felker GM, Greene SJ, Butler J, Khan MS. Trajectory of Decongestion and Mortality in Young Adults with Acute Heart Failure. Curr Probl Cardiol 2023 Apr;48(4):101579. PM: 36592843.
Kaniusas E, Fudim M, Czura CJ, Panetsos F. Editorial: Neuromodulation in COVID-19: From basic research to clinical applications. Front Physiol 2023 Feb 16;14:1148819. PM: 36875048.
Ostrer IR, Wang TY. Are We Ready for Prehospital Troponin Testing? JAMA Intern Med 2023 Mar 1;183(3):211-212. PM: 36716048.
Sadeghpour A, Kim H, Chamis AL. Undiagnosed Atrial Septal Defect in the Setting of Comorbidities and Ventricular Failure: Seemingly Simple Disease with a Challenging Diagnosis. CASE (Phila) 2022 Nov 21;7(2):72-80. PM: 36861103.
Talha KM, Jain V, Yamani N, Fatima K, Rashid AM, Hernandez GA, Dani SS, Fudim M, Minhas AMK. Temporal Trends and Outcomes of Implantable Cardioverter Defibrillators in Heart Failure and Chronic Kidney Disease in the United States. Curr Probl Cardiol 2023 Apr;48(4):101548. PM: 36566952.
Division of Cardiology Publications: February 23 – March 1, 2023
Badhwar V, Chikwe J, Gillinov AM, Vemulapalli S, O’Gara PT, Mehaffey JH, Wyler von Ballmoos M, Bowdish ME, Gray EL, O’Brien SM, Thourani VH, Shahian DM, Habib RH. Risk of Surgical Mitral Valve Repair for Primary Mitral Regurgitation. Ann Thorac Surg 2023 Mar;115(3):600-610. PM: 36669963.
Chew DS, Piccini JP, Au F, Frazier-Mills CG, Michalski J, Varma N. Alert-driven vs scheduled remote monitoring of implantable cardiac defibrillators: A cost-consequence analysis from the TRUST trial. Heart Rhythm 2023 Mar;20(3):440-447. PM: 36503177.
Docherty KF, McMurray JJV, Claggett BL, Miao ZM, Adams KF, Arias-Mendoza A, Cleland JGF, Diaz R, Echeverria Correa LE, Felker GM, Fonseca C, Li J, Metra M, Sliwa-Hahnle K, Solomon SD, Vandekerckhove HJ, Vinereanu D, Voors AA, Heitner SB, Kupfer S, Malik FI, Meng L, Teerlink JR. Efficacy of omecamtiv mecarbil in heart failure with reduced ejection fraction according to N-terminal pro-B- type natriuretic peptide level: insights from the GALACTIC-HF trial. Eur J Heart Fail 2023 Feb;25(2):248-259. PM: 36597719.
Du J, Zhou X, Clark-Boucher D, Hao W, Liu Y, Smith JA, Mukherjee B. Methods for large-scale single mediator hypothesis testing: Possible choices and comparisons. Genet Epidemiol 2023 Mar;47(2):167-184. PM: 36465006.
Felker GM, North R, Mulder H, Jones WS, Anstrom KJ, Patel MJ, Butler J, Ezekowitz JA, Lam C, O’Connor CM, Roessig L, Hernandez AF, Armstrong PW. Clinical Implications of Negatively Adjudicated Heart Failure Events: Data From the VICTORIA Study. Circulation 2023 Feb 21;147(8):694-696. PM: 36802884.
Go AS, Al-Khatib SM, Desvigne-Nickens P, Bansal N, Bushnell CD, Fang MC, Freeman JV, Gage BF, Hanke T, Hylek EM, Lopes RD, Noseworthy PA, Reddy VY, Singer DE, Thomas KL, True Hills M, Turakhia MP, Zieman SJ, Cooper LS, Benjamin EJ. Research Opportunities in Stroke Prevention for Atrial Fibrillation: A Report From a National Heart, Lung, and Blood Institute Virtual Workshop. Stroke 2023 Mar;54(3):e75-e85. PM: 36848427.
Harrington J, Piccini JP, Alexander JH, Granger CB, Patel MR. Clinical Evaluation of Factor XIa Inhibitor Drugs: JACC Review Topic of the Week. J Am Coll Cardiol 2023 Feb 28;81(8):771-779. PM: 36813377.
Marquis-Gravel G, Faulkner M, Merritt G, Farrehi P, Zemon N, Robertson HR, Jones WS, Kraschnewski J. Importance of patient engagement in the conduct of pragmatic multicenter randomized controlled trials: The ADAPTABLE experience. Clin Trials 2023 Feb;20(1):31-35. PM: 35999816.
Moulson N, Petek BJ, Baggish AL, Harmon KG, Kliethermes SA, Patel MR, Churchill TW, Drezner JA. The Cardiac Effects of COVID-19 on Young Competitive Athletes: Results from the Outcomes Registry for Cardiac Conditions in Athletes (ORCCA). J Cardiovasc Dev Dis 2023 Feb 6;10(2):72. PM: 36826568.
Parikh RV, Hebbe A, Barón AE, Grunwald GK, Plomondon ME, Gordin J, Yeh RW, Jneid H, Swaminathan RV, Waldo SW, Monto A, Secemsky E, Hsue PY. Clinical Characteristics and Outcomes Among People Living With HIV Undergoing Percutaneous Coronary Intervention: Insights From the Veterans Affairs Clinical Assessment, Reporting, and Tracking Program. J Am Heart Assoc 2023 Feb21;12(4):e028082. PM: 36789851.
Peikert A, Claggett BL, Kim K, Udell JA, Joseph J, Desai AS, Farkouh ME, Hegde SM, Hernandez AF, Bhatt DL, Gaziano JM, Talbot HK, Yancy C, Anand I, Mao L, Cooper LS, Solomon SD, Vardeny O. Association of post-vaccination adverse reactions after influenza vaccine with mortality and cardiopulmonary outcomes in patients with high-risk cardiovascular disease: the INVESTED trial. Eur J Heart Fail 2023 Feb;25(2):299-310. PM: 36335639.
Porras Fimbres DC, Patel P, Li G, Ronald JSC, Martin JG. Factors Predictive of Failure of Medical Management in Spontaneous Rectus Sheath Hematoma. J Vasc Interv Radiol 2023 Mar;34(3):493-494. PM: 36563932.
Rao VN, Shah A, McDermott J, Barnes SG, Murray EM, Kelsey MD, Greene SJ, Fudim M, DeVore AD, Patel CB, Blazing MA, O’Brien C, Mentz RJ. In-Hospital Virtual Peer-to-Peer Consultation to Increase Guideline-Directed Medical Therapy for Heart Failure: A Pilot Randomized Trial. Circ Heart Fail 2023Feb;16(2):e010158. PM: 36314130.
Rosa RG, Cavalcanti AB, Azevedo LCP, Veiga VC, de Souza D, Dos Santos RDRM, Schardosim RFC, Rech GS, Trott G, Schneider D, Robinson CC, Haubert TA, Pallaoro VEL, Brognoli LG, de Souza AP, Costa LS, Barroso BM, Pelliccioli MP, Gonzaga J, Studier NDS, Dagnino APA, Neto JM, da Silva SS, Gimenes BDP, Dos Santos VB, Estivalete GPM, Pellegrino CM, Polanczyk CA, Kawano-Dourado L, Tomazini BM, Lisboa TC, Teixeira C, Zampieri FG, Zavascki AP, Gersh BJ, Avezum Á, Machado FR, Berwanger O, Lopes RD, Falavigna M. Association between acute disease severity and one-year quality of life among post-hospitalisation COVID-19 patients: Coalition VII prospective cohort study. Intensive Care Med 2023 Feb;49(2):166-177. PM: 36594987.
Selvaraj S, Greene SJ, Ayodele I, Alhanti B, Allen LA, Lewsey SC, Adusumalli S, Reza N, Hernandez AF, Yancy CW, Jena AB, Fonarow GC, Bhatt DL. Assessing Heuristic Bias During Care for Patients Hospitalized for Heart Failure: Get With The Guidelines-Heart Failure. Circ Heart Fail 2023 Feb;16(2):e010069. PM: 36458538.
Sun K, Eudy AM, Rogers JL, Criscione-Schreiber LG, Sadun RE, Doss J, Maheswaranathan M, Barr AC, Eder L, Corneli AL, Bosworth HB, Clowse MEB. Pilot Intervention to Improve Medication Adherence Among Patients With Systemic Lupus Erythematosus Using Pharmacy Refill Data. Arthritis Care Res (Hoboken) 2023Mar;75(3):550-558. PM: 34739191.
Turer AT, Wang A. Cardiac Myosin Inhibitors: Unlocking Potential to Improve Treatment in Hypertrophic Cardiomyopathy. Circulation 2023 Feb 28;147(9):700-702. PM: 36848411.
Uriel N, Milano C, Agarwal R, Lee S, Cleveland J, Goldstein D, Wang A, Crandall D, Mehra MR. Incidence and clinical correlates of de-novo aortic regurgitation with a fully magnetically levitated left ventricular assist device: a MOMENTUM 3 trial portfolio analysis. Eur J Heart Fail 2023 Feb;25(2):286-294. PM: 36404406.
Vargas LB, Lange LA, Ferrier K, Aguet F, Ardlie K, Gabriel S, Gupta N, Smith JD, Blackwell TW, Ding J, Durda P, Tracy RP, Liu Y, Taylor KD, Craig Johnson W, Rich SS, Rotter JI, Lange EM, Konigsberg IR. Gene expression associations with body mass index in the Multi-Ethnic Study of Atherosclerosis. Int J Obes (Lond) 2023 Feb;47(2):109-116. PM: 36463326.
Wang X, Vaduganathan M, Claggett BL, Hegde SM, Pabon M, Kulac IJ, Vardeny O, O’Meara E, Zieroth S, Katova T, McGrath MM, Pouleur AC, Jhund PS, Desai AS, Inzucchi SE, Kosiborod MN, de Boer RA, Kober L, Sabatine MS, Martinez FA, Ponikowski P, Shah SJ, Hernandez AF, Langkilde AM, McMurray JJV, Solomon SD, Lam CSP. Sex Differences in Characteristics, Outcomes, and Treatment Response With Dapagliflozin Across the Range of Ejection Fraction in Patients With Heart Failure: Insights From DAPA-HF and DELIVER. Circulation 2023 Feb 21;147(8):624-634. PM: 36342789.
Wolder LD, Graff C, Baadsgaard KH, Langgaard ML, Polcwiartek C, Ji-Young Lee C, Skov MW, Torp-Pedersen C, Friedman DJ, Atwater B, Overvad TF, Nielsen JB, Hansen SM, Sogaard P, Kragholm KH. Electrocardiographic P terminal force in lead V1, its components, and the association with stroke and atrial
fibrillation or flutter. Heart Rhythm 2023 Mar;20(3):354-362. PM: 36435351.
Duke Heart Center Pulse – March 5th 2024
Highlights of the week:
March & ACC.23
We hope everyone is having a great weekend – on this first weekend of March, what could be better than seeing our colleagues in person at #ACC.23 in New Orleans? That Blue Devil win over Carolina last night was just the icing on the cake!
A few things to know as we kick off the month: U.S. News Best Hospitals Voting is currently open and underway in Doximity. Check your account and vote! Also, March is National Nutrition Month, Women’s History Month, and Wednesday (3/8) is International Women’s Day. A shout-out to all the women throughout Duke Heart!
In ACC.23 news thus far, across Duke Heart and Duke Clinical Research Institute: 
- 2 Late-Breaking sessions
- 6+ Presentations
- 19 Moderated sessions
- 26+ Poster sessions
- 25+ Speaker/Oral contributions
Regarding the work our fellows are presenting throughout ACC, please try to attend their session if you are able to do so:
Sunday 3/5:
9:00 am-12:00 pm: Willard Applefeld, Balim Senman; Learn By Doing: Immersive Simulation Experiences in Critical Care Cardiology, Telemedicine, HOCM, and Syncope Management (session 303-02, 303-25 Personalized Skills Center Simulation Station).
12:15-12:20 pm: Kelly Arps; Electrical storm: Interdisciplinary Approach to Care (case presentation & panelist session 673, Rm 357)
12:45-1:30 pm: Anthony Peters; Characteristics and outcomes of trial-eligible vs ineligible patients with heart failure with mildly reduced or preserved ejection fraction (session 1560-161, Poster Hall, Hall F)
Monday 3/6:
9:00-11:00 am: Balim Senman; Learn By Doing: Immersive Simulation Experiences in Critical Care Cardiology, Telemedicine, HOCM, and Syncope Management (session 305-1, Personalized Skills Center Simulation Station).
9:45-9:55 am: Jamie Diamond; Characterizing the digital divide & access to mobile health interventions in heart failure: insights from the CONNECT-HF MHEALTH substudy (session 1081-03 Pulmonary Vascular Disease/Valvular Heart Disease/Special Topics Moderated Poster Theater 4_Hall F)
9:45-9:55 am: Karen Flores Rosario; ACC Complex Clinical Cases: Mimicking the great mimicker: LMNA cardiomyopathy presenting as isolated cardiac sarcoidosis (session 1084-03, Complex Clinical Cases Moderated Poster Theater 6_Hall F)
10:00-10:10 am: Joe Lerman; Early post-transplant outcomes in LVAD patients undergoing heart transplant via use of the SherpaPak Cardiac Transport System as compared with traditional cold storage: Insights from the GUARDIAN registry (session 1077, Heart Failure and Cardiomyopathies Moderated Poster Theater 9_Hall F)
3:20-3:30 pm: Willard Applefeld; Top Developments in Critical Care Cardiology (session 454-11, Rm 245)
Congratulations to the follows who presented yesterday, 3/4:
Willard Applefeld; Decoding the ABCs of the Cardiac ICU and Learn By Doing: Immersive Simulation Experiences in Critical Care Cardiology, Telemedicine, HOCM, and Syncope Management
Josephine Harrington; Applicability of the GALACTIC-HF trial and omecamtiv mecarbil to patients hospitalized for heart failure in the United States: from the GWTG-HF registry and Proteomic markers of cardiac fibrosis and endothelial function associated with heart failure in patients with diabetes: an EXSCEL biomarker sub-study
Jessica Duran; Bedside Risk Prediction of Adverse Outcomes in Medically Treated Patients with Severe Tricuspid Regurgitation
Duke Periop Echo is First in U.S. to Receive IAC Accreditation
We are excited to share that our perioperative echocardiography service has received accreditation by the Intersocietal Accreditation Commission (IAC). In a letter sent this week by Katherine Gibson, RDCS, director of accreditation – echocardiography for the IAC to Dr. Alina Nicoara, cardiac anesthesiologist and director of the Perioperative Echocardiography service, Gibson wrote, “I would like to take this opportunity to congratulate you on seeking and achieving Echocardiography accreditation by the IAC. You and your staff are to be commended for demonstrating your facility’s pursuit of excellence in documenting quality patient care in the field of Echocardiography. Upon receipt and review of recently submitted material, your facility has been awarded accreditation in Perioperative Transesophageal Echocardiography.”
Gibson went on to add, “Duke University Medical Center is the first to achieve this designation. Congratulations!”
“We are thrilled to have received the seal of accreditation from the IAC and grateful for a legacy of excellence in perioperative echocardiography starting with Dr. Fiona Clemens and Dr. Joseph Kisslo, and continuing with Dr. Joseph Mathew, and Dr. Madhav Swaminathan,” said Nicoara, who is Director, Perioperative Echocardiography. “This could not have been achieved without sustained collaboration with our colleagues, cardiologists, and sonographers, and support from the Heart Center. We are also looking forward to working together with other imaging modalities accredited by the IAC within the Duke Heart Center towards achieving a Center of Quality status through joint quality improvement programs.” image
We reached out to both Madhav Swaminathan, MD and Mihai Podgoreanu, MD for their thoughts on the accreditation news.
“IAC accreditation in perioperative echo is a significant milestone in the rich history of Duke Echocardiography. From pioneering echo in the operating room in the early ‘90s with Joe Kisslo and Fiona Clements, to the establishment of quality improvement guidelines led by Joseph Mathew, to now being the nation’s first periop accredited echo lab, Duke CT Anesthesia remains a leader and beacon of excellence in perioperative echo. Dr. Alina Nicoara led this effort with remarkable perseverance, while Ashlee Davis, in the CDU, was instrumental in helping us achieve this milestone. Congratulations to the entire group!” — Madhav Swaminathan, MD
“The evolution of the Duke Perioperative Echocardiography Program is a history of firsts. From the early pioneers who introduced echocardiography to the cardiac surgical operating rooms (Drs. Norbert de Bruijn, Fiona Clements and Joe Kisslo), to national leadership in standardizing image acquisition and interpretation, to development of the first digital database and reporting for perioperative echocardiography (Dr. Joseph Mathew), to the first anesthesiologist president of the American Society of Echocardiography (Dr. Madhav Swaminathan). Befittingly, as a continuation of its trailblazing tradition, Duke is the first program in the nation to be accredited by the IAC under the leadership and vision of its current Director, Dr. Alina Nicoara. Congratulations to the team and all the Duke Heart collaborators!” — Mihai Podgoreanu, MD
Duke’s rich history in and contributions to echocardiography continue! Well done, all!
D’Amico Selected for TBJ Award
 Please join us in congratulating thoracic surgeon Thomas A. D’Amico, MD! On Friday, we learned he has been named one of 14 winners of the Triangle Business Journal’s 2023 Health Care Leadership Awards. D’Amico, the Gary Hock Endowed Professor of Surgery and a faculty member within Duke’s Division of Cardiovascular and Thoracic Surgery, is one of four award winners from across Duke University Health System. The winners will be celebrated during an awards dinner on April 13th, when they will also learn more details about their nomination and the category in which they are being awarded. We look forward to sharing more details at that time.
Please join us in congratulating thoracic surgeon Thomas A. D’Amico, MD! On Friday, we learned he has been named one of 14 winners of the Triangle Business Journal’s 2023 Health Care Leadership Awards. D’Amico, the Gary Hock Endowed Professor of Surgery and a faculty member within Duke’s Division of Cardiovascular and Thoracic Surgery, is one of four award winners from across Duke University Health System. The winners will be celebrated during an awards dinner on April 13th, when they will also learn more details about their nomination and the category in which they are being awarded. We look forward to sharing more details at that time.
Congratulations, Dr. D’Amico!
CTO 2023 Held
The 2023 Chronic Total Occlusion (CTO) conference, organized by the Cardiovascular Research Foundation, was held Feb. 23-24 at the New York Marriott Marquis in New York City.
Jennifer Rymer, MD, presented research conducted by herself and Drs. Izzy Othman, Caitlin Drescher, Schuyler Jones, and Anna Lisa Chamis on the use of MRI to assess viability for CTOs; their abstract, Utilization of Cardiac Magnetic Resonance Imaging for Management of Coronary Chronic Total Occlusions, received top abstract designation by the conference and was presented during the Award-winning Abstract Presentations section of the conference.
Way to go!
Update: Relocation of DUH Unit 7100 Scheduled for April
The relocation date for Duke University Hospital Unit 7100 has been scheduled for April 14th. This is for the renovation of DUH bed tower 100, which is currently in the process of being renovated. Unit 7100 will be relocated to Duke North 2200 (a 16-bed unit) and 3200 (also a 16-bed unit) in April.
Kudos to McVeigh, Kamneva & Members of 2F2G
Several members of our Heart Failure multidisciplinary team in 2F2G were called into action this week for a code blue. We received comments about several team members for how well each of them handled a difficult situation:
“Having Oksana (Kamneva) in clinic today was a godsend and she did an amazing job in the support of our clinic staff and medication administration. We cannot thank her enough for her support, especially being brand new in her role. Todd McVeigh absolutely deserves recognition for everything that he did throughout entire code, and his follow up care and compassion with the family after. He was truly remarkable in his care, and we were lucky to have him here.” – Jamie Hilton, nurse manager, operations
The 2F2G team demonstrated excellent teamwork and compassionate care – thank you for all you do, especially during difficult experiences.
Kudos to Diaz!
We received a note this week from Dr. Mihai Podgoreanu regarding one of our perfusion team members, Sebastian Diaz, who  serves as associate chief of Extracorporeal Life Support (ECLS).
serves as associate chief of Extracorporeal Life Support (ECLS).
“The recent OR case with a high-risk patient reminded me to highlight Sebastian’s many contributions to our overall Duke Heart team work. His knowledge, engagement, professionalism and communication style are superlative, whether in the CTOR or CTICU. He is a model of compassion, and always willing to pay it forward by educating others. I wanted to take a moment to recognize and celebrate him.” – Mihai Podgoreanu, MD
Excellent work, Sebastian! Well-deserved praise!
Shout-out to MRI team!
We received some warm feedback this week from a patient regarding members of our MRI team. The patient has a background in clinical care and wanted to send their thanks. In a note to Jill Engel and Mary Lindsey, the patient wrote:
“Good morning, I wanted to share with you the wonderful experience I had with my stress MRI last Thursday morning. I was pretty nervous, as sometimes our experience working in the clinical world causes our minds to go places we wish they wouldn’t.
I had the best experience with Tracy, as the nurse who got me prepped and ready for the MRI, she was the first person to put me at ease. Nester was awesome as well. He explained everything, and everything he said was exactly what I experienced. He and Julie made me feel very comfortable throughout the MRI, as did Tracy when we did the stress portion of the exam. I do not recall the names of the Radiologists but they were also so great at explaining exactly what was going to happen and it made the entire experience much easier, being my first time having any type of MRI.
I just wanted to let you both know, being clinical in my previous life I know the clinical teams don’t always hear when they are doing a great job and I wanted to share. Thank you.” – a grateful patient (name withheld to protect their privacy)
We have the best teams throughout Duke Heart! Keep up the great work!
Dean’s Distinguished Research Series 2023
The Duke University School of Medicine’s Dean’s Distinguished Research Series showcases groundbreaking research from the basic, clinical, and translational sciences. Formerly called “Research Week”, the reimagined series will be held in-person and live-streamed. All faculty, staff, trainees and students are welcome to attend.

March 9:
Trainee Poster Session, 2:30 – 4 p.m., 6th Floor, Trent Semans Center for Health Education
Faculty Lectures, 4 – 5 p.m., 6th Floor, Trent Semans Center for Health Education.
Chris Beyrer, MD, MPH, director of Duke Global Health Institute, and Keisha Bentley-Edwards, PhD, associate director of research, Samuel DuBois Cook Center on Social Equity will present. Light bites and refreshments provided on a first-come, first-served basis. (live stream available: https://duke.is/vgf7u)
For the full schedule, please visit https://medschool.duke.edu/research/deans-distinguished-research-series-2023.
DHIP update
Distribution of Employment Agreements for transitioning members is ongoing. Please monitor your inbox for critical communication from DHIP@duke.edu, your department chair, and Adobe Sign.
Reminder: The Duke Guarantee offers the minimum compensation each Member can expect to receive. Additional compensation opportunities which exist today will continue to be available to members within DHIP.
All members will be given four weeks to consider employment and sign their Employment Agreements.
Benefits:
- A benefits transition FAQ for PDC Direct staff is available on org.
- Information regarding Duke Benefits is available on SharePoint.
- All benefits related questions can be sent to DHIPBenefits@Duke.edu.
All other questions can be sent to DHIP@duke.edu, and all DHIP updates can be found at https://dhip.org.
Upcoming Events & Opportunities
Cardiology Grand Rounds
March 14: Topic TBA with Italo Biaggioni of Vanderbilt University Medical Center. 5 p.m., Zoom.
Duke REACH Equity Center Funding Opportunities:
Research Voucher, Scholars Development, Transdisciplinary Think Tank
Now accepting applications through March 17 for July 2023 funding.
The Duke REACH Equity Center awards support students, trainees, and faculty who are interested in conducting research that promotes health equity. All proposals should broadly address the REACH Equity theme: to reduce racial and ethnic disparities in health by improving the quality of patient-centered care in the clinical encounter across diseases, stages of illness, care settings, and throughout the life course. Proposals may include any research topic and method (quantitative, qualitative, etc.).
There are four funding opportunities:
The Research Vouchers Program will supplement currently funded research or support standalone research projects conducted by faculty at any level. Funding: One year, up to $12,500 per award.
- Full Research Vouchers Program RFA and application instructions are available here.
- Current awardee list is available here.
The Research Scholars Development Program is intended to support early-stage investigators (residents, fellows, postdoctoral students, nursing trainees, and other trainees at a similar career stage). Scholars work with a faculty mentor (identified by the trainee) to develop a research proposal and complete a project. Funding: Up to $5,000 for one- or two-year project per award.
- Full Research Scholars Development RFA and application instructions are available here.
- Current awardee list is available here.
The Transdisciplinary Think Tank (TTT) provides support to bring together faculty across disciplines who have a common interest in addressing racial and ethnic disparities in the clinical encounter. The TTT’s aim is to catalyze and support research related to the REACH Equity theme and to foster collaboration among health disparities researchers across Duke University. Funding: One year, up to $1,500 per award.
- The Full Transdisciplinary Think Tank RFA and application instructions are available here.
- Current awardee list is available here.
The Medical Student and Nursing Student Research Award is intended to support a third-year medical student or a third-year PhD nursing student conducting research related to the REACH Equity theme. Scholars work with a faculty mentor (identified by the student) to develop a research proposal and complete a project. Funding: Up to $5,000 for one-year project.
- Full Medical Student Research and Nursing Student Research Award and application instructions are available here.
- Current awardee list is available here.
Application submission deadline: March 17 for July 2023 funding.
Email reachequitycenter@duke.edu with questions.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
February 23 — Duke University School of Nursing
StudyFinds.org
Best Nursing Schools For 2023: Top 5 Schools Most Recommended By Experts
https://duke.is/pjgfv
February 24 — Joseph Turek
WFMY CBS-2 (Greensboro)
Grey’s Anatomy features Duke Health Surgery in mid-season premiere
https://duke.is/4zsg2
February 27 — Stephen Greene
HCP Live
Heart Failure Community Argues for Omecamtiv Mecarbil Approval, Citing Unmet Need
https://duke.is/9srwy
February 27 — Duke Health/RACE CARS
WGPH Fox-8 (Greensboro)
https://duke.is/28vc6
*clip begins @ 09:23:10
February 27 — Duke School of Medicine
Becker’s ASC Review
10 top-ranked medical schools for surgeons, per US News
https://duke.is/gpu4b
March 1 — Joseph Turek, M. Louise Markert and Laura Hale
Gizmodo
A New Heart-Thymus Transplant Could Someday Let Kids Live Without Anti-Rejection Drugs
https://duke.is/vund4
March 1 — Brittany Zwischenberger
Medpage Today
Women Still Face Higher Risks for Mortality After CABG
https://duke.is/rurf8
March 1 — Brittany Zwischenberger
JAMA News
https://duke.is/53xqz
March 2 — Adrian Hernandez
Medpage Today
Stella Immanuel Highest U.S. Prescriber of Ivermectin and HCQ
https://duke.is/6cv82
March 2 — Duke Cardiology/Duke University Hospital
Newsweek
World’s Best Specialized Hospitals 2023
https://duke.is/pruby
Recent Comments