Home » Uncategorized
Category Archives: Uncategorized
Duke Heart Pulse — April 21, 2024
Highlights of the week:
Rambarat Named Chief Cardiology Fellow, 2024-2025
 We are excited to share that our Duke cardiology fellows have elected Paula Rambarat, MD to serve as chief cardiology fellow for 2024-2025. Please join us in congratulating Dr. Rambarat and welcoming her to her new role!
We are excited to share that our Duke cardiology fellows have elected Paula Rambarat, MD to serve as chief cardiology fellow for 2024-2025. Please join us in congratulating Dr. Rambarat and welcoming her to her new role!
Rambarat was born and raised in Barbados. She moved to Chapel Hill, NC in her junior year of high school and graduated from East Chapel Hill High School. Then, she attended Duke University, where she majored in biology and minored in Spanish. Subsequently, she received her medical degree from Columbia University Vagelos College of Physicians and Surgeons. During medical school, she was awarded a Howard Hughes Medical Institute research fellowship and worked in the lab of Dr. Robert Lefkowitz here at Duke. Rambarat completed an Internal Medicine residency at Massachusetts General Hospital and returned to Duke for a Cardiovascular Disease fellowship. She is pursuing a Duke Clinical Research Institute fellowship followed by advanced training in heart failure and transplant cardiology. In her free time, she enjoys spending time with her family, hiking, running, and cooking.
Dr. Ramabarat will on-board with Dr. Lerman during May. She officially takes the role at the end of June.
Many thanks to Joseph Lerman, MD for the incredible job he has done serving as chief cardiology fellow this past year!
Congratulations, Paula!
ACC.24: Summary of Duke ACC Presentations
Faculty experts from across Duke Heart and the Duke Clinical Research Institute (DCRI) shared insights and expertise on the latest cardiology research as part of more than 100 late-breaking studies, Meet the Expert opportunities, presentations, panels, and posters during the 2024 American College of Cardiology (ACC) Scientific Sessions held April 6-8 in Atlanta.
Duke kicked off the conference with AEGIS-II and EMPACT-MI presented as part of the opening late-breaking research session. The two presentations culminated in six publications in major medical journals.
Therapy Shows Promise in Delaying Hospitalizations for HF: Results from EMPACT- MI
About 800,000 people in the U.S. suffer a heart attack every year, and approximately 30% of them will go on to develop heart failure. There are limited treatments to prevent or slow that development.
A large international study coordinated and conducted by the DCRI found that the diabetes drug empagliflozin (marketed under the brand name Jardiance) did not reduce deaths. Secondary findings show it did slow the time to first hospitalization for heart failure and reduced the total number of subsequent heart failure hospitalizations. The results from the EMPACT-MI trial were published simultaneously with the ACC presentation in the New England Journal of Medicine, Circulation, and the Journal of the American College of Cardiology. Details of the meta-analysis are in press in The Lancet Diabetes & Endocrinology. The study was led by Schuyler Jones, MD and Adrian Hernandez, MD from the Duke/DCRI.
The study findings on lower rates of heart failure offer some hope and underscore the importance of preventing poor outcomes after a heart attack, according to DCRI executive director and site principal investigator, Adrian Hernandez, MD, MHS.
“Developing heart failure is one of our major public health problems, and any step that gets us closer to preventing it is a step in the right direction,” Hernandez said. “After a heart attack, we should really be focused on how to prevent problems, especially the development of heart failure. This therapy fills in that gap.”
AEGIS-II Misses Primary Endpoint; Data Suggest Further Research into HDL Modification is Warranted
Primary results from the AEGIS-II trial showed that infusions of the human plasma-derived apolipoprotein A-I CSL112 did not significantly lower the risk of major adverse cardiac events through 90 days for people who had recently suffered a heart attack. However, exploratory analysis showed that patients who received the treatment had numerically lower rates of cardiovascular (CV) death and myocardial infarction (MI), type-1 MI, and stent thrombosis-related MI compared to placebo. Primary results were published in the New England Journal of Medicine and exploratory results were published in the Journal of the American College of Cardiology.
cardiac events through 90 days for people who had recently suffered a heart attack. However, exploratory analysis showed that patients who received the treatment had numerically lower rates of cardiovascular (CV) death and myocardial infarction (MI), type-1 MI, and stent thrombosis-related MI compared to placebo. Primary results were published in the New England Journal of Medicine and exploratory results were published in the Journal of the American College of Cardiology.
“It’s probably the most important trial looking at HDL modification or altering HDL efficacy in terms of limiting cardiovascular events,” said Thomas Povsic, MD, PhD, one of the study investigators and first author of the JACC paper. “I think there are signals that it did work, but the overall effects were relatively modest and what we showed is that on certain kinds of heart attacks, it does seem to prevent downstream cardiovascular events. That would need validation in a separate clinical trial.”
Also notable from AEGIS-II was the efficiency of the study’s operations. The AEGIS-II team enrolled more than 18,000 participants across 46 countries amid the COVID-19 pandemic, with only two lost to follow-up. The DCRI managed the study data and managed the 193 U.S. sites, which enrolled more than 1,800 high-risk acute MI patients, with none lost to follow-up.
“We have long-standing relationships with many of our sites in the U.S., so I think one of the things that we bring to the table is that we know a lot of sites that will enroll well and are high quality sites that will follow their patients,” Povsic said during a Meet the Expert event following the late-breaker session. “We have relationships with country leaders throughout the world. I was one of the country leaders in the U.S., and we had a lot of contact with our sites to make sure that they were following patients and doing all the other things that we talk about in clinical trials to make sure the trial is well run, and this trial was really well run.”
Pagidipati Provides Practical Tips for Harnessing the Power of Anti-Obesity Medications
 Anti-obesity medications squarely fit within a cardiologist’s scope of practice and should be used in combination with lifestyle changes, according to cardiologist Neha Pagidipati, MD, MPH, presenting during a Saturday afternoon ACC session.
Anti-obesity medications squarely fit within a cardiologist’s scope of practice and should be used in combination with lifestyle changes, according to cardiologist Neha Pagidipati, MD, MPH, presenting during a Saturday afternoon ACC session.
Referencing studies including STEP HFpEF, SELECT, STEP 1, STEP 4, SURMOUNT 1 and SURMOUNT 4, Pagidipati discussed the relevance and benefits of newer weight loss drugs such as semaglutide, liraglutide, and tirzepatide, and then outlined how she introduces patients to the medications and increases their dosing gradually.
“These therapies don’t just help patients lose weight, they are CV-risk reduction agents,” said Pagidipati, underscoring the relevance of the drugs for cardiologists. She also emphasized the need for lifestyle changes in concert with the medications.
“No amount of medicine is going to help a patient become healthier if they don’t understand what they’re supposed to be doing in their life in terms of exercise and diet,” she said. “All of these studies were predicated upon some lifestyle change happening for all of these patients.”
Pagidipati went on to share the three things she discusses with her patients to ensure the medications are most effective:
- Move more: “Whatever you’re doing, do more than what you’re doing.”
- How much you eat: “It helps if you eat less, for most of us, and these agents will help us do that.”
- What you eat: “In general, I recommend the Mediterranean diet, low salt, low carb, if they’re trying to lose weight, as well.”
- When starting patients on anti-obesity medications, a slow and gradually increasing approach is best.
“The key to remember is start low, go slow,” Pagidipati said. “Start at the lowest dose with patients, and I titrate every four weeks. I only titrate up to the next dose if and when their gastrointestinal symptoms have improved. If they’re queasy, have nausea, and you titrate up for them, it’s just going to get worse. Also, I tend to wait until their weight loss plateaus, and usually at four weeks it does.”
Keys to Improving Healthspan in Older Adults with Ischemic Heart Disease
During a session focused on improving healthspan in older adults with ischemic heart disease, Karen Alexander, MD, first sought to point out the elephant in the room: “everyone dies,” she said.
 “This is not a reason that we shouldn’t be working very hard to improve quality of life before death, but we need to be aware of that, because our patients are aware of that, and as we ask them to participate in research, I think that’s on their mind to a degree.”
“This is not a reason that we shouldn’t be working very hard to improve quality of life before death, but we need to be aware of that, because our patients are aware of that, and as we ask them to participate in research, I think that’s on their mind to a degree.”
In aiming to generate evidence among older adults, Alexander recommended:
- considering the uniqueness of the older population, and the underlying processes unique in that age group.
- appreciating and leveraging new ways of doing research that are virtual and aligned with care.
- thinking about the outcomes that matter to the patients.
Alexander highlighted the approach taken by the ongoing PREVENTABLE study, which is finding potential participants aged 75 and older using a cohort query applied to the electronic health record. Sites then approach patients and randomize them to atorvastatin 40 mg. or placebo. Participants are tracked to determine whether they meet the primary outcome which is one that matters to the patients — survival free of dementia and persisting disability.
Researchers have made participation easy by shipping the study drug directly to patient homes and enrolling about half of the population remotely.
“This can be done,” Alexander said. “We’re having a very simple intervention, which is the atorvastatin 40 mg. versus placebo — but you could imagine how this could be replicated based on our experience in other situations.”
Keeping in mind the participant population’s desire to try new interventions is key, Alexander concluded.
“As we’re beginning to think about these fancy new interventions, we have to stop ourselves and remember the population we’re asking to go on this journey and to be in the trial boat with us. From PREVENTABLE, the one thing we have learned is that older adults are in that phase where they really don’t want to rock the boat. This is an important thing to partner with our participants and make sure they’re interested in joining us.”
What’s Now, and What’s Next for Treating High Blood Pressure?
Nearly half of adults have hypertension or are taking medication to manage hypertension. Hypertension, also known as high blood pressure, is defined as systolic blood pressure greater than 130 mmHg or diastolic blood pressure greater than 80 mmHg.
pressure greater than 130 mmHg or diastolic blood pressure greater than 80 mmHg.
An ACC session focused on high blood pressure reviewed the issue and the forthcoming therapies that could help to better manage the condition.
Highlighting the SPRINT study — which showed a reduction in all-cause mortality, relative risk reduction in heart failure, and reduction in stroke — Duke cardiologist Chris Granger, MD, noted that it provides a helpful example of what can be done, while also showing the limitations.
After emphasizing the study’s impressive results, Granger discussed the aftermath.
“The long-term follow-up, after two or three years after the trial was finished, the blood pressure difference between the two groups had vanished, the benefit for mortality and CV mortality had vanished,” he said. “This is in a setting where people had done the trial, they knew the benefits, it was with the same patients who knew the benefits, so this shows us that our current systems are really a failure, even in optimal settings.”
For now, key strategies for treating hypertension he highlighted include:
- targeting blood pressure less than 130 mmHg systolic for patients with or high-risk for cardiovascular disease using combination drugs titrated monthly.
- home monitoring.
- ensuring patient access to advanced practice providers, pharmacists, and algorithms measuring and promoting medication adherence.
New possibilities on the horizon could improve treatment of hypertension, Granger added.
“New treatments, like zilebesiran, I think will provide important, perhaps transformational opportunities for treating high blood pressure, in this case through a potent, what appears to be safe based on preliminary data, and sustained inhibition of the renin-angiotensin system with a treatment given once every six months as a subcutaneous injection.” he said, adding that more trials are needed and ongoing to assess efficacy and safety.
TRANSFORM-HF Modified On-Treatment Analysis Supports Primary Results
 DCRI Fellow Mark Kittipibul, MD, shared results from a modified on-treatment analysis of the effects of torsemide vs. furosemide after discharge in patients hospitalized with heart failure from the TRANSFORM-HF trial.
DCRI Fellow Mark Kittipibul, MD, shared results from a modified on-treatment analysis of the effects of torsemide vs. furosemide after discharge in patients hospitalized with heart failure from the TRANSFORM-HF trial.
The analysis showed no significant difference in mortality between the on-treatment groups of the two diuretics at discharge or after one month.
“In this post-hoc on-treatment analysis of TRANSFORM-HF — inclusive of all randomized patients, unless they were confirmed to be non-adherent — there was no significant difference in outcomes between torsemide and furosemide,” said DCRI Fellow Mark Kittipibul at ACC reviewing the effects of the two diuretics in heart failure patients after hospital discharge. “These findings support the robustness of the primary trial results.”
Primary results from TRANSFORM-HF were first shared by Robert Mentz, MD, during a late-breaking science session at the 2022 American Heart Association Scientific Sessions.
New Study Shows Fortified Eggs did not Raise Cholesterol
A study led by Duke researchers offers new evidence on fortified eggs’ health effects. In a modest-sized randomized trial, researchers found that fortified eggs — meaning those enriched with various vitamins or nutrients — did not significantly impact bad cholesterol (LDL cholesterol) or good cholesterol (HDL cholesterol) over the course of the four-month study.
 A secondary finding hinted there could be some benefit associated with fortified egg consumption for older patients and patients with diabetes. The finding was not statistically significant due to the number of study participants, but senior researcher and heart failure cardiologist Robert Mentz, MD said it’s an interesting signal that the researchers would like to investigate in future work.
A secondary finding hinted there could be some benefit associated with fortified egg consumption for older patients and patients with diabetes. The finding was not statistically significant due to the number of study participants, but senior researcher and heart failure cardiologist Robert Mentz, MD said it’s an interesting signal that the researchers would like to investigate in future work.
The study’s first author and DCRI Fellow Nina Nouhravesh, MD said the study can be viewed as a pilot.
“While it was modest in size, it did include a broadly generalized population,” Nouhravesh said. “The average age of participants was 66 years, half were women, and more than 25% identified as Black.”
ICYMI: Bill Kraus MGR Presentation, April 19
If you were unable to attend Friday morning Medicine Grand Rounds, the presenter was Bill Kraus, MD on ‘A Detailed Analysis of Cardiac Rehabilitation on 180-day All-Cause Hospital Readmission and Mortality. You can view the recording here: https://duke.is/5/jjy3
Happy Birthday, Chris Granger!
 A belated Happy Birthday to Chris Granger, MD – his team members in the CICU helped celebrate his special day with him this past week. Happy Birthday, Chris!
A belated Happy Birthday to Chris Granger, MD – his team members in the CICU helped celebrate his special day with him this past week. Happy Birthday, Chris!
Culture Pulse Survey Launches This Week
The Duke Health Culture Pulse survey launches tomorrow, April 22, and is available to team members until May 13. The brief, 18-question survey is confidential and mobile-friendly. Visit the Culture Pulse 2024 page on DHN for a Zoom background, flyer, and more.
This year’s Culture Pulse will focus on our commitment to putting people first by asking questions, listening, and seeking diverse perspectives. The Culture Pulse survey aims to strengthen the employee experience and will take you under five minutes to complete.
The link to the survey will arrive via email tomorrow. Check your inbox!
Upcoming Events & Opportunities
- April is National Donate Life Month
- Annual reminder as part of Duke’s “check yourself” campaign: please make sure your contact information is up to date in Duke@Work
- Culture Pulse 2024 April 22-May 13
- Duke Farmers Market season opens this week! Starting April 25, the Farmers Market will be held every Thursday from 11 a.m. to 2 p.m. on the DMP Greenway.
Cardiology Grand Rounds
April 23: No CGR tonight. (Faculty Meeting, division of cardiology)
April 25: New Insight into the Physiology of Heart Failure with Preserved Ejection Fraction with Satyam (Tom) Sarma, MD of UT Southwestern. 5 p.m., DN 2002 or via Zoom. *Please note this is a Thursday evening presentation.
All Duke Cardiology Grand Rounds recordings are housed on Warpwire. To access recordings please visit:
NET ID and password required. Enjoy!
CD Fellows Core Curriculum Conference
April 24: EP Case Presentation with Aman Kansal and Eric Xie. Noon, DMP 2W96 (in-person only).
April 26: EKG Review with Tom Bashore. Noon, Zoom only.
Upcoming CME Symposia
May 4: Duke Heart Failure Symposium
Please reach out to Christy Darnell with any questions.
Working Effectively Across Generations
June 3: Working Effectively Across Generations with Hile Rutledge, of Otto Kroeger Associates (OKA). 8:30 a.m. to Noon. Great Hall, Trent Semans Center. Sponsored by Duke School of Medicine.
Registration required: https://medschool.duke.edu/blog/register-now-working-effectively-across-generations
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
April 12 — Pamela Douglas
Healio
Pamela S. Douglas, MD, highlights need for diversity in clinical trials leadership
April 12 — Neha Pagidipati
tctMD
Triglyceride-Lowering Therapies Provide Favorable Outcomes in Early Testing
April 16 — Charlotte Reikofski
AARC
Want to Work with Kids? Here’s What You Need to Know First!
April 16 — Jennifer Rymer
tctMD
TARGET BP 1: Alcohol-Based RDN Promises Single Treatment for Resistant BP
April 16 — Dawn Coleman
Vascular Specialist
April 16 — Duke Clinical Research Institute
Medscape
Chelation Therapy and CV Risk: Why TACT2 Showed No Benefit
April 17 — Jennifer Rymer
Medscape
Alcohol-Mediated Renal Denervation Promising in Hypertension
April 18 — William Kraus and Kim Huffman
Mirage.News
Research: Calorie Limitation’s Complex Role in Aging
April 18 — Joseph Lerman
tctMD
In Transporting Donor Hearts, SherpaPak Shows Promise Over Traditional Coolers
Duke Heart Pulse — April 14, 2024
Duke Heart Pulse – April 14, 2024
Highlights of the week:
ACC.24: Narcisse Selected for 2024 ACC Career Development Award

 We are excited to share that Duke cardiology fellow Dennis I. Narcisse, Jr., MD, MS, is one of three recipients of the 2024 American College of Cardiology/Association of Black Cardiologists Merck Research Fellowship. The fellowship awards were presented on Monday, during the last day of the ACC Scientific Sessions in Atlanta.
We are excited to share that Duke cardiology fellow Dennis I. Narcisse, Jr., MD, MS, is one of three recipients of the 2024 American College of Cardiology/Association of Black Cardiologists Merck Research Fellowship. The fellowship awards were presented on Monday, during the last day of the ACC Scientific Sessions in Atlanta.
Three awardees are selected each year to receive a one-year fellowship in the amount of $100,000 as salary support for one year of research in adult cardiology. Narcisse was selected along with Colette DeJong, MD of the University of California, San Francisco and Xiaowen Wang, MD, MPH of Massachusetts General Hospital.
The ACC is committed to inspiring and investing in the next generation of cardiovascular clinicians, scientists and leaders. The ACC’s Career Development Awards provide opportunities for rising stars in cardiology to gain access to leadership development, mentorship and knowledge-building that will help them grown in their chosen areas of expertise.
In addition to the ACC/ABC Merck Research Fellowships, other ACC Career Development Awards announced on Monday included the Hani Najm Global Scholar Award and the William A. Zoghbi International Research Awardee.
Congratulations, Dennis!
DHIP Leadership News
Leadership announcements were made this week by Tom Owens, MD executive vice president and chief operating officer of Duke Health Integrated Practice (DHIP), and John Sampson, MD senior vice president of DHIP.
Paul R. Newman, a senior DHIP and DUHS leader, will lead several strategic priorities for Duke Health, including funds  flow and clinical effort models, implementation of mission-based accounting, physician partnership development to enable growth, and the development of other strategic initiatives that may arise.
flow and clinical effort models, implementation of mission-based accounting, physician partnership development to enable growth, and the development of other strategic initiatives that may arise.
 Simon Curtis has been named Chief Operating Officer for DHIP. Reporting to Owens and Sampson, and in collaboration with the DHIP leadership team, Simon will partner with the clinical departments and DUHS to drive operational excellence across the practice in areas such as clinician recruitment planning, clinical operations, access, and patient experience.
Simon Curtis has been named Chief Operating Officer for DHIP. Reporting to Owens and Sampson, and in collaboration with the DHIP leadership team, Simon will partner with the clinical departments and DUHS to drive operational excellence across the practice in areas such as clinician recruitment planning, clinical operations, access, and patient experience.
These updated roles are effective immediately.
Celebrating the Eclipse
 Members of Duke Heart’s cardiology team celebrate the eclipse at a solar eclipse watch party, on April 8, 2024.
Members of Duke Heart’s cardiology team celebrate the eclipse at a solar eclipse watch party, on April 8, 2024.
Shout-out to Goodwin!
 A big shout-out to cardiology fellow Nate Goodwin for his compassion in taking care of a very sick CCU patient.
A big shout-out to cardiology fellow Nate Goodwin for his compassion in taking care of a very sick CCU patient.
“The patient’s family really appreciated his personal touch and his ability to share their pain. I was very impressed. I also applaud the fact that in the middle of a challenging pathophysiology with no clear way out, he never ignored the human component of our job. If my mom or dad got sick, I’d want Nate taking care of them.” — Ivan Nenadic Wood, MD, PhD
Nicely done, Nate. We’re so glad you were present for this family.
Shout-out to Stephanie Buck!
 Duke Heart APP Stephanie Buck was in the right place at the right time for a passenger in distress. On a flight to the Dominican Republic a 15-yr old male went into anaphylaxis after eating goat cheese. The passenger did not have an epi pen. When flight attendants asked if a medical professional was onboard, Buck responded. Although the flight emergency kit did not have an epi pen, the did have epi in a glass ampule. Buck took control of the situation, successfully administering the epi and Benadryl, and managed care for the passenger like the amazing professional she is, even while off-duty! She continued to monitor the patient until the flight safely landed and EMS was able to take over.
Duke Heart APP Stephanie Buck was in the right place at the right time for a passenger in distress. On a flight to the Dominican Republic a 15-yr old male went into anaphylaxis after eating goat cheese. The passenger did not have an epi pen. When flight attendants asked if a medical professional was onboard, Buck responded. Although the flight emergency kit did not have an epi pen, the did have epi in a glass ampule. Buck took control of the situation, successfully administering the epi and Benadryl, and managed care for the passenger like the amazing professional she is, even while off-duty! She continued to monitor the patient until the flight safely landed and EMS was able to take over.
“I think this is a great example of why Duke Providers are the best and can handle even the scariest situations whether at work or out in the community,” said Roman Ross, MSN, ANP-C for the division of cardiovascular and thoracic surgery.
Kudos to Hughes and Duke Aortic team
We received terrific patient feedback on Dr. Chad Hughes and the aortic team this week. Via Press Ganey HCAHPS, we received a note that states:
“Can’t say enough about Dr. Hughes and his team. I received the very best surgical expertise and care. I’m very, very fortunate.” — a grateful patient
Dr. Hughes, we received this nice feedback about the great care you and your team gave to a patient at Duke Hospital on Heart service unit 3300. Thank you for the high quality and compassionate care you provide to patients.” — David Gallagher, MD, Chief Medical Officer, DUH
“Kudos Dr. Hughes for the tremendous comments. Agree that we are fortunate to have you and the entire aortic team at Duke Heart and Health!” — Jill Engel, VP, Duke Heart & Vascular Services
This Coming Saturday: Support Duke’s Aortic Team & NC Walk for Victory
Duke Heart is again serving as the presenting sponsor of the upcoming NC Walk for Victory in support of Marfan Syndrome, LDS, VEDS and related conditions, with Dr. Chad Hughes serving as co-medical chair for the walk along with Carly Scarborough of Levine Children’s Hospital.
The event is scheduled for 12-3 p.m. on Saturday, April 20 at Laurel Hills Park in Raleigh. To learn more, please visit the NC Walk website and consider joining the Duke Aorta team to raise funds for research!
Flu Season is Officially Over
After consultation with Duke Infectious Diseases, the Health System has defined Monday, April 1, as the official end of the flu season. For the purposes of the Duke University Health System (DUHS) Healthcare Worker Flu Vaccination Policy, new staff/providers who have joined DUHS on or after April 1 will not be required to be vaccinated against the flu or have an approved exemption. However, they will be required to comply with flu vaccination policy during the Fall 2024 flu vaccination period.
Upcoming Events & Opportunities
- April is National Donate Life Month
- Annual reminder as part of Duke’s “check yourself” campaign: please make sure your contact information is up to date in Duke@Work
- Culture Pulse 2024 survey period starts April 22!
Cardiology Grand Rounds
April 16: Cancelled
April 23: TBD
April 25: New Insight into the Physiology of Heart Failure with Preserved Ejection Fraction with Tom Sarma, MD of UT Southwestern. 5 p.m., DN 2002 or via Zoom. *Please note this is a Thursday evening presentation.
All Duke Cardiology Grand Rounds recordings are housed on Warpwire. To access recordings please visit:
NET ID and password required. Enjoy!
CD Fellows Core Curriculum Conference
April 17: HF/Txp Case Presentation with Aarti Thakkar. Noon, DMP 2W96 (in-person only).
April 19: Genetics and CVD with Svati Shah. Noon, Zoom only.
Upcoming CME Symposia
May 4: Duke Heart Failure Symposium
Please reach out to Christy Darnell with any questions.
Working Effectively Across Generations
 June 3: Working Effectively Across Generations with Hile Rutledge, of Otto Kroeger Associates (OKA). 8:30 a.m. to Noon. Great Hall, Trent Semans Center. Sponsored by Duke School of Medicine.
June 3: Working Effectively Across Generations with Hile Rutledge, of Otto Kroeger Associates (OKA). 8:30 a.m. to Noon. Great Hall, Trent Semans Center. Sponsored by Duke School of Medicine.
Registration required: https://medschool.duke.edu/blog/register-now-working-effectively-across-generations
Improving Conversation Skills with Seriously Ill Patients
In an effort to ensure that clinicians feel comfortable and empowered to have difficult conversations regarding goals of care with patients and their families, members of the Duke Hospice and Palliative Care team offer VitalTalk communication trainings so that they can help clinicians do their best to take care of our patients.
VitalTalk skills training is open to those involved in conducting or supporting Goals of Care conversations for our patients with serious illness across Duke Health. The course consists of a 30-minute didactic lecture in the LMS system, followed by a 3-4 hour skills practice-session. CME/CEU credits are available once both activities (LMS and live practice) are completed.
A limited number of seats are available in each of the upcoming online VitalTalk skills practice courses – use https://duke.is/VitalTalk to view available dates and times and to register.
If you have any questions, please contact Jonathan Fischer, MD, medical director of palliative care for Duke’s Population Health Management Office.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
April 4 — Nina Nouhravesh
India Today
Eggs may not increase your cholesterol. Study explains
April 6 — Tom Povsic
tctMD
Full AEGIS-II Results: Raising HDL With Apo A-I No Help After Acute MI
April 6 — Stephen Greene
HCP Live
Don’t Miss a Beat: EMPACT-MI at ACC.24, with Javed Butler, MD
April 7 — Wayne Batchelor
Medscape
Ticagrelor Alone Cuts Bleeding Without More Events Post-PCI
April 7 — Mark Kittipibul
HCP Live
April 7 — Manesh Patel
tctMD
Long-Awaited RCT Data Show Survival Benefit With Impella CP: DanGer Shock
April 8 — Robert Mentz
Associated Press
April 8 — Mark Kittipibul
HCP Live
Modified On-Treatment Analysis Confirms Results of TRANSFORM-HF
April 8 — Mitchell Krucoff
NBC News
10 doctors on FDA panel for Abbott heart device had financial ties to the company
April 8 — Madhav Swaminathan
Diagnostic Imaging
April 8 — Wayne Batchelor
Healio/Cardiology Today
Routine use of Impella CP for STEMI-related cardiogenic shock confers survival benefit
April 8 — Wayne Batchelor
Healio/Cardiology Today
Long-term DAPT may not be needed for patients with ACS after angioplasty, stenting
April 8 — Duke University Health System
The People’s Pharmacy
Eggs Are Bad – No, Eggs Are Good – Huh?
April 8 — Nina Nouhravesh
Easy Health Options
Eggs’ Bad Rap Cheats Those Who Need Their Benefits Most
April 8 — Adrian Hernandez
Medical Xpress
ACC: Empagliflozin cuts heart failure hospitalization risk after AMI
April 9 — Neha Pagidipati
Medscape
Early Olezarsen Results Show 50% Reduction in Triglycerides
April 10 — Sreekanth Vemulapalli
Becker’s Hospital Review
The biggest challenges facing cardiology, per 12 leaders
April 10 — Neha Pagidipati
Medscape
Substantial Triglyceride Reduction With Plozasiran
April 10 — Jennifer Rymer
Medpage Today
FFR-Guided Complete Revascularization Did Not Improve Outcomes in MI Patients
April 10 — Duke University Hospital
Becker’s Hospital Review
472 hospitals honored for patient safety, price transparency
April 11 — Manesh Patel
Salt Lake City Star Tribune
Medtronic study puts spotlight on how one of its heart devices can help women
April 11 — Jay Lusk (Population Health)
Healio
Low socioeconomic status raises mortality odds in pulmonary conditions
April 11 — Svati Shah
Time
How to Talk to Your Family About Their Heart Health History
April 12 — Jennifer Rymer
Medscape
Duke Heart Pulse — April 7, 2024
Chief’s message:
The American College of Cardiology 2024 meeting was this weekend with several of our faculty and fellows presenting at the meeting. We also had the opportunity to catch up with colleagues and friends. Please find some pictures from the meeting.






Highlights of the week:
Hughes Named Chief, Section for Aortic Surgery
 Chad Hughes, MD, Professor of Surgery, has been appointed the inaugural Chief for the Section of Aortic Surgery, a new section housed jointly within the Divisions of Cardiothoracic Surgery and Vascular and Endovascular Surgery. Hughes will also serve as co-director, with vascular surgeon Chandler Long, MD, of the Duke Center for Aortic Disease. The announcement was made on April 3 by Dr. Carmelo Milano, chief of Cardiovascular and Thoracic Surgery, and Dr. Dawn Coleman, chief of Vascular Surgery.
Chad Hughes, MD, Professor of Surgery, has been appointed the inaugural Chief for the Section of Aortic Surgery, a new section housed jointly within the Divisions of Cardiothoracic Surgery and Vascular and Endovascular Surgery. Hughes will also serve as co-director, with vascular surgeon Chandler Long, MD, of the Duke Center for Aortic Disease. The announcement was made on April 3 by Dr. Carmelo Milano, chief of Cardiovascular and Thoracic Surgery, and Dr. Dawn Coleman, chief of Vascular Surgery.
Hughes completed his undergraduate training at Wake Forest University and medical school at Duke University. He subsequently completed his training in both general surgery and CT surgery at Duke University. In 2005, he completed an additional aortic surgery fellowship at the University of Pennsylvania under the instruction of Dr. Joseph Bavaria, a renowned leader in aortic surgery.
Hughes joined the faculty here at Duke as an assistant professor of surgery, and in 2020, he rose to the rank of Professor of Surgery. He has developed one of the largest practices of aortic surgery in the country with national and regional referrals. At Duke, he started the transcatheter aortic valve replacement program with Dr. Kevin Harrison. Additionally, along with Dr. Richard McCann, he developed stent grafting for aortic pathology at this institution.
Hughes has served as a model of the academic surgeon with over 250 peer-reviewed publications, multiple national speaking engagements, and a prominent role as an associate editor for the Annals of Thoracic Surgery. He has driven innovation of care for aortic pathology at a national level.
This divisional reorganization is focused on enabling further collaboration between CT surgery, vascular surgery, and cardiology. In this new role, Dr. Hughes will focus on further expansion of aortic surgery, innovation around aortic pathology, and mentoring younger faculty and trainees in aortic surgery.
Congratulations, Chad!
Thomas Receives HRS Youngblood Leadership Award

We were thrilled to learn this week that cardiac electrophysiologist Kevin Thomas, MD, professor of medicine in cardiology and vice dean for Diversity, Equity and Inclusion for Duke School of Medicine, has been selected by the Heart Rhythm Society (HRS) to receive it’s 2024 James H. Youngblood Excellence in Leadership Award.
The Youngblood Leadership Award recognizes a member of the HRS who has demonstrated exemplary leadership by leading an initiative that has had a community-wide impact.
You have certainly done that and more — congratulations, Kevin!
Anne Cherry, MD to Receive Inaugural SCA Presidential Citation

Congratulations to Anne Cherry, MD, associate professor of anesthesiology at Duke. She has been selected as the first recipient of the Society of Cardiovascular Anesthesiology’s (SCA) newest award – the Presidential Citation Award. Cherry was selected by Dr. Kathryn Glas, current president of the SCA and chair of anesthesiology at the University of Arizona.
The Presidential Citation will be awarded annually at the discretion of the President of SCA to an individual who has made an important contribution to the field of cardiovascular anesthesia through one (or several) of the following:
- An early career accomplishment
- Research contribution
- Education contribution
- DEI contribution through the advancement of minority interests
- Service to the SCA
Cherry will be presented with the 2024 Presidential Citation during the SCA Annual Meeting being held in collaboration with the American Association for Thoracic Surgery from April 27-30 in Toronto, Canada.
Congratulations, Anne!
Holley to Receive DOM Excellence in Education Award

We are pleased to share that Christopher Holley, MD, PhD, has been selected as the recipient of Duke’s 2024 Department of Medicine Excellence in Education Award for the division of cardiology. His nomination, in part, reads:
“As a member of our clinical team, Holley teaches cardiovascular disease and advanced heart failure and transplantation fellows during Transplant or VAD rounds and gives high-yield lectures in these areas, receiving stellar teaching evaluations from our trainees. As a skilled researcher, he teaches and mentors undergraduate, graduate, and post-graduate trainees on the role of non-coding RNA (ncRNA) in cardiovascular health and disease.
Furthermore, he is committed to educating the next generation of cardiovascular specialists by actively participating in fellowship recruitment. He serves as an Associate Program Director of the Cardiovascular Disease fellowship, as a co-lead in the Department of Medicine’s Physician Scientist Training program, and as core faculty in the Medical Scientist Training Program. In all these roles, his passion for educating current and future trainees is evident.”
This annual DOM award recognizes one faculty member in each division in recognition of outstanding teaching and commitment to the education and professional development of fellows, residents, and students. He will be recognized during the DOM Annual Celebration on May 2.
Congratulations, Chris!
Small Selected for DOM Administrative Excellence Award
 Congratulations to Duke Cardiology GME coordinator Brianna Small! We learned this week that she has been selected to receive the Department of Medicine’s Rising Star Award for Administrative Excellence.
Congratulations to Duke Cardiology GME coordinator Brianna Small! We learned this week that she has been selected to receive the Department of Medicine’s Rising Star Award for Administrative Excellence.
She will be recognized during the Annual Chair Award dinner celebration later this spring.
Hooray, Brianna!
ACC.24: Therapy Shows Promise in Delaying Hospitalizations for Heart Failure
About 800,000 people in the U.S. suffer a heart attack every year, and about 30% of them will go on to develop heart failure. There are limited treatments to prevent or slow that development.
A large international study led by Duke researchers investigated whether the diabetes drug empagliflozin (marketed under the brand name Jardiance) might prevent heart failure in patients after they had suffered acute myocardial infarction.
While the study found that the drug did not reduce deaths, secondary findings show it did slow the time to first hospitalization for heart failure and reduced the total number of subsequent heart failure hospitalizations.
The secondary findings are published in the journal Circulation and presented at the American College of Cardiology’s Annual Scientific Session on April 6. Other findings from the study, called EMPACT-MI, were also simultaneously published in the New England Journal of Medicine and the Journal of the American College of Cardiology.
Empagliflozin was originally approved for use in patients with diabetes, but investigators chose to study the drug based on earlier findings that it showed benefit in preventing active heart failure from becoming worse. The study was funded by two companies that manufacture the drug – Boehringer Ingelheim and Eli Lilly and Company.
The study enrolled 6,522 patients across 22 countries, with roughly half randomly assigned to receive the therapy and the other half placebo. Both groups otherwise received standard care. Investigators credit the study’s simple design to its broad reach.
The Duke Clinical Research Institute coordinated and led the conduct of the trial.
The study findings on lower rates of heart failure offer some hope and underscore the importance of preventing poor outcomes after a heart attack, according to principal investigator and corresponding author, Adrian Hernandez, MD, director of the Duke Clinical Research Institute.
“Developing heart failure is one of our major public health problems, and any step that gets us closer to preventing it is a step in the right direction,” Hernandez said. “After a heart attack, we should really be focused on how to prevent problems, especially the development of heart failure. This therapy fills in that gap.”
Hernandez said he would be curious to investigate the secondary findings further, especially because there are so many different factors that can play out after a heart attack.
“Heart attacks are pretty dynamic – in the first 24 hours things can change for the better or the worse; you can end up having a small heart attack or a big one,” Hernandez said. “We don’t know if there could be a difference in results from the therapy depending on the type of event and the timing of giving a treatment. Those could be areas to consider.”
In addition to Hernandez, study authors for the Circulation publication include Jacob A. Udell, W. Schuyler Jones, Stefan D. Anker, Mark C. Petrie, Josephine Harrington, Michaela Mattheus, Svenja Seide, Isabella Zwiener, Offer Amir, M. Cecilia Bahit, Johann Bauersachs, Antoni Bayes-Genis, Yundai Chen, Vijay K. Chopra, Gemma Figtree, Junbo Ge, Shaun Goodman, Nina Gotcheva, Shinya Goto, Tomasz Gasior, Waheed Jamal, James L. Januzzi, Myung Ho Jeong, Yuri Lopatin, Renato D. Lopes, Béla Merkely, Puja B. Parikh, Alexander Parkhomenko, Piotr Ponikowski, Xavier Rossello, Morten Schou, Dragan Simic, Philippe Gabriel Steg, Joanna Szachniewicz, Peter van der Meer, Dragos Vinereanu, Shelley Zieroth, Martina Brueckmann, Mikhail Sumin, Deepak L. Bhatt, and Javed Butler.
ACC.24: Congrats to all Duke Researchers & Presenters!
The Annual Scientific Sessions for the American College of Cardiology is well underway this weekend in Atlanta. We’ve had significant news coverage for the poster presentation on the fortified eggs study, findings of which were released last week ahead of the ACC. We anticipate additional news coverage on the EMPACT-MI study results (highlighted above) and look forward to coverage of many other presentations by our Duke Heart team.
Carolyn Lekavich, PhD, presented an abstract on Saturday — Advancing Heart Failure Prevention: Echocardiogram Ventricular-Arterial Coupling (VAC) Signaling Early Heart Failure with Preserved Ejection Fraction (HFpEF).
Heading into ACC, there were 113 presentations planned related to research performed with or by Duke team members, including two late-breakers (EMPACT-MI, and the AEGIS II trial), many poster presentations, abstracts, and contributions including those with:
- Karen Alexander
- John Alexander
- Gerald Bloomfield
- Adam DeVore
- Pamela Douglas
- Michael Felker
- Marat Fudim
- Christopher Granger
- Jennifer Green
- Stephen Greene
- Josephine Harrington
- Adrian Hernandez
- Schuyler Jones
- Michelle Kelsey
- Mark Kittipibul
- Larry Jackson
- Renato Lopez
- Daniel Mark
- Robert Mentz
- Kristin Newby
- Nina Nouhravesh
- Neha Pagidipati
- Kishan Parikh
- Manesh Patel
- Jonathan Piccini
- Sean Pokorney
- Jennifer Rymer
- Nishant Shah
- Svati Shah
- Monique Starks
- Sreekanth Vemulapalli,
Nicely done, all!
Shout-out to Osude!
A hat tip & shout-out to cardiovascular disease fellow Nkiru “KiKi” Osude, MD, for her work in the community to promote heart health!
Osude recently served as a guest speaker — along with faculty member Monique Starks, MD — at the 2024 Shades of Green “Goes Red” Fashion Show and Luncheon, a charity fundraising event to help promote cardiovascular disease awareness throughout the community, sponsored by the Durham chapter of The Links, Incorporated.

The event, in part, highlighted the importance of heart health and community efforts to improve cardiovascular health. The Links, Incorporated is a group of more than 15,000 professional women of color dedicated to improving the well-being of Durham citizens through leadership, philanthropy, and service.
Osude was also featured in a heart-health promotional flyer as part of the work being done by Durham’s Community Health Coalition.
Way to go, KiKi! 
Duke Heart & 2024 NC Walk for Victory
Duke Heart will again serve as the presenting sponsor of the upcoming NC Walk for Victory in support of Marfan Syndrome, LDS, VEDS and related conditions, with Dr. Chad Hughes serving as co-medical chair for the walk with Carly Scarborough of Levine Children’s Hospital.
The event is scheduled for 12-3 p.m. on Saturday, April 20 at Laurel Hills Park in Raleigh. To learn more, please visit the NC Walk website and consider joining the Duke Aorta team to raise funds for research!
ICYMI: April Leadership Town Hall
The most recent DUHS Leadership Town Hall was held on Tuesday, April 2 via Zoom. If you missed it and would like to watch the recording, it is available on Leadership Exchange.
Upcoming Events & Opportunities
- April is National Donate Life Month
- April 6-8, American College of Cardiology Scientific Sessions, Atlanta.
Cardiology Grand Rounds
April 9: Heart Failure: Does Sex Really Matter? with Carolyn Lam, of Duke-NUS MD. 5 p.m., DN 2002 or via Zoom.
April 16: TBD
April 23: TBD
April 25: New Insight into the Physiology of Heart Failure with Preserved Ejection Fraction with Tom Sarma, MD of UT Southwestern. 5 p.m., DN 2002 or via Zoom. *Please note this is a Thursday evening presentation.
All Duke Cardiology Grand Rounds recordings are housed on Warpwire. To access recordings please visit:
NET ID and password required. Enjoy!
CD Fellows Core Curriculum Conference
April 10: Cardiology Fellows Lunch with Carolyn Lam. Noon, DMP 2W96 (in-person only).
April 12: Journal Club with TBD. Noon, Zoom only.
Upcoming CME Symposia
April 12: Duke Sports Cardiology & Sudden Death in Athletes
May 4: Duke Heart Failure Symposium
For any questions you might have about either event, please reach out to Christy Darnell.
2024 Feagin Leadership Forum
Consider joining members from throughout the Duke community for a special Duke Centennial event, the 15th Annual Feagin Leadership Forum at the JB Duke Hotel on May 17-18. The theme for the Forum is Compassion, Collaboration, and Compromise: Leadership in a Polarized World. World class leaders from business, healthcare, the military and athletics will be sharing their leadership expertise and how they address the challenges of our complex world. There will be special welcomes from Duke leaders, and the future leaders of healthcare — this year’s Feagin Leadership Scholars — will share their work and leadership insights.
For more details, go to https://www.feaginleadership.org/schedule-1.
To register, visit: https://www.feaginleadership.org/2023registration-1.
Improving Conversation Skills with Seriously Ill Patients
In an effort to ensure that clinicians feel comfortable and empowered to have difficult conversations regarding goals of care with patients and their families, members of the Duke Hospice and Palliative Care team offer VitalTalk communication trainings so that they can help clinicians do their best to take care of our patients.
VitalTalk skills training is open to those involved in conducting or supporting Goals of Care conversations for our patients with serious illness across Duke Health. The course consists of a 30-minute didactic lecture in the LMS system, followed by a 3-4 hour skills practice-session. CME/CEU credits are available once both activities (LMS and live practice) are completed.
A limited number of seats are available in each of the upcoming online VitalTalk skills practice courses – use https://duke.is/VitalTalk to view available dates and times and to register.
If you have any questions, please contact Jonathan Fischer, MD, medical director of palliative care for Duke’s Population Health Management Office.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
March 20 — Richard Shannon
The Assembly
Why Breast Cancer Screening Fails Many Women
March 29 — Nina Nouhravesh
Everyday Health
Eggs May Actually Be Okay for Your Heart
March 29 — Nina Nouhravesh
Earth.com
Eggs aren’t just for Easter — eating them is no longer considered unhealthy
March 29 — Nina Nouhravesh
The Washington Times
Never mind: New study finds eggs won’t worsen cholesterol, may even improve heart health
March 29 — Nina Nouhravesh
Times Now (India)
High cholesterol diet: Study claims eggs won’t increase your cholesterol levels
March 29 — Nina Nouhravesh
Medical Dialogues (India)
March 29 — Nina Nouhravesh
Arab Times (Kuwait)
New study challenges notion of eggs’ impact on cholesterol levels
March 30 — Nina Nouhravesh
The Mirror (UK)
‘Myth’ that eggs are bad for the heart and raise cholesterol debunked by scientists
April 1 — Nina Nouhravesh
Healio
Top in cardiology: Benefits of fortified eggs; FNIH to study preeclampsia biomarkers
April 2 — Nina Nouhravesh
Scripps News
Eggs might not be that bad for your heart health, study says
*carried by 60+ Scripps affiliates nationally
April 2 — Duke Clinical Research Institute
Code List
According to cardiologists, this long-shunned food is not so bad
April 4 — Duke University Medical Center
Mass Device
Paragonix begins full U.S. launch of donor lung preservation system
April 4 — Duke University Medical Center
Medical Design & Development
Paragonix Begins Full Commercial Launch for Donor Lung Preservation System
Duke Heart Pulse — March 31, 2024
Duke Heart Pulse – March 31, 2024
Highlights of the week:
Happy Elite 8 Easter Weekend
 To all those celebrating the holiday this weekend with family and friends, we wish you a very Happy Easter, and to all those celebrating the
To all those celebrating the holiday this weekend with family and friends, we wish you a very Happy Easter, and to all those celebrating the advancement of their favorite NCAA teams in the men’s and women’s tournaments, a big congratulations!
advancement of their favorite NCAA teams in the men’s and women’s tournaments, a big congratulations!
We’re excited to see Duke MBB take on the Wolfpack today at 5 p.m. and hopefully continue onward to the Final Four. Go Duke!
Gaca Appointed Section Chief, Adult Cardiac Surgery
We are pleased to share that Jeffrey Gaca, MD, has been appointed section chief for Adult Cardiac Surgery. The announcement was made last week by Dr. Carmelo Milano, MD, chief of the division of cardiovascular and thoracic surgery.
Gaca completed his undergraduate degree at Cornell University and medical school at Columbia University. His training in both general surgery and cardiovascular and

thoracic surgery was accomplished at Duke University.
In 2008, after completing an additional aortic surgery fellowship at the University of Pennsylvania, Gaca joined the Duke Surgery faculty as an assistant professor in the Division of CT Surgery. In 2016, he rose to the academic rank of associate professor.
Gaca is one of our most talented cardiac surgeons and has developed a tremendous valvular surgery practice with regional and national referrals, Milano said. He has distinguished himself as a leading educator of our residents and is the recipient of the Dr. Dwight C. McGoon award for commitment to resident development.
In addition, he has been an important mentor for junior faculty, helping them navigate complex cases and challenging intraoperative situations. He is also known for his innovation and has worked closely with Dr. Don Glower to expand minimally invasive heart surgery, making Duke University a leading referral center for these procedures.
He has worked with Dr. Chad Hughes and the cardiologists to grow the transcatheter valve replacement program. In his new role, Gaca will work closely with Milano to develop young cardiac surgery faculty and further drive innovation and growth.
Please join us in congratulating and welcoming Jeff in this new role!
Kelsey to Receive SOM Master Clinician Award

We are excited to share that Anita Kelsey, MD, has been selected as a recipient of the Duke School of Medicine’s Master Clinician/Teacher Award for 2024. This award was created to honor individuals for superlative accomplishment in teaching and/or clinical care at Duke’s School of Medicine. The intent is to honor those individuals who have made an extraordinary commitment “above and beyond” normal expectations. “Dr. Kelsey has certainly met the criteria and is most deserving of the honor,” said Edward Buckley, MD, in his notification letter.
The award will be presented to Kelsey at the annual Faculty Celebration at Duke Gardens on May 13, 2024.
Congratulations, Anita!
ACC.24: Fortified Eggs Did Not Raise Cholesterol in Modest-Sized Cardiology Study
There are often conflicting headlines about whether certain foods are good or bad for you, and the news about eggs has been especially confusing. Search the topic online and you’ll find a wealth of articles spanning back decades.
A study that will be presented during the American College of Cardiology’s Annual Scientific Sessions and led by researchers at Duke, offers new evidence on fortified eggs, which are eggs enriched with various vitamins or nutrients. In a modest-sized randomized trial, researchers found that fortified eggs did not have a negative impact on bad cholesterol (LDL cholesterol) or good cholesterol (HDL cholesterol) over the course of the four-month study.
The study was sponsored by Eggland’s Best, a company that makes and sells fortified eggs. It also provided the eggs used in the research.
The study had 140 participants, all people aged 50 or older, who had experienced at least one cardiac event in the past or had risk factors for cardiovascular disease such as diabetes. Researchers randomized participants into two groups, asking half to eat two or fewer eggs per week for four months. The other half were provided with fortified eggs and asked to eat 12 per week for the same period of time.
While no significant changes in bad or good cholesterol were found, a secondary finding hinted there could be some benefit associated with fortified egg consumption for older patients and patients with diabetes.
That secondary finding was not statistically significant due to the number of study participants, but cardiologist and senior researcher, Robert Mentz, MD, associate professor of medicine at the Duke University School of Medicine, said it’s an interesting signal that the researchers would like to investigate in future work.
“If we can explore this area further, in a larger study, specifically focusing on the type of patients who appear to have potentially experienced some benefit, and over a longer period of time, we could see if it is possible for fortified eggs to improve cholesterol,” Mentz said.
The study’s first author, Nina Nouhravesh, MD, a cardiology fellow at the Duke Clinical Research Institute, said the study can be viewed as a pilot study.
“While it was modest in size, it did include a broadly generalized population,” Nouravesh said. “The average age of participants was 66 years, half were women, and more than 25 percent identified as Black.”
Mentz said the enrollment was representative of the community, especially for a study aimed at cardiology patients.
He said he would like to move forward with a larger study assessing clinical outcomes, particularly when considering the topic of equity and food access.
“There are disparities around access to food,” Mentz said. “Individuals who are the most socially disadvantaged (and likely have more instances of high blood pressure and diabetes), often have less access to healthy foods. Often what we hear described in the community is access to fresh fruits and vegetables. Those are really time-limited foods that may go bad quickly. Fortified eggs can be safely stored in the refrigerator for longer periods of time. Investigating potential health benefits of an easily accessible and less time-limited food is something we should be doing.”
“I think we are in this exciting time where people think of food as medicine,” Mentz said. “Some foods are fortified and nutritionally optimized before they’re disseminated, similar to medications, so it’s exciting to use the same rigor that’s applied in medication trials to food science.”
In addition to Mentz and Nouhravesh, study authors include Josephine Harrington, Laura H. Aberle, Cynthia L. Green, Kathleen Voss, Dave Holdsworth, Kurt Misialek, Bartel T. Slaugh, Mandee Wieand, William S. Yancy, and Neha Pagidipati.
Duke-DCRI Reception at ACC.24
For those of you attending the American College of Cardiology’s Annual Scientific Sessions (April 6-8), please join us at the annual Duke-DCRI Reception taking place on Saturday, April 6, 2024, from 5:30-8:30 p.m. EDT, at the Omni Atlanta Hotel at Centennial Park in Grand C Ballroom, North Tower-M4.
Team Builder’s Gift Launches Heart Innovation Hub
(This story was posted to Giving to Duke Health.)
 Most people understand the importance of team building, but few take it as seriously as Bob Keegan: building innovative and successful teams was the tenet of his professional career. Now Keegan is empowering a pioneering Duke Health team with a transformational gift to kick-start the new Duke Heart Precision and Innovation Collaboratory headed by Manesh Patel, MD, chief of the division of cardiology and the division of clinical pharmacology.
Most people understand the importance of team building, but few take it as seriously as Bob Keegan: building innovative and successful teams was the tenet of his professional career. Now Keegan is empowering a pioneering Duke Health team with a transformational gift to kick-start the new Duke Heart Precision and Innovation Collaboratory headed by Manesh Patel, MD, chief of the division of cardiology and the division of clinical pharmacology.
“I am grateful for the many contributions Bob has made to Duke Heart,” Patel said. “We are excited to use his philanthropy to build our team, expand our cardiovascular knowledge base, and then translate that knowledge into new treatments, disease prevention, health promotion, and outstanding patient care. Most importantly, he is supporting our innovation efforts with the next generation of leaders.”
Keegan grew up around teams. His father was a professional baseball player for the Chicago White Sox, and while Keegan was a talented athlete who grew up thinking baseball was in his future, his love of academics prevailed. What followed was a degree in mathematics from Le Moyne College and an MBA in finance from the University of Rochester. Business, it turns out, was Keegan’s calling. He knew early on that what drove him was a heartfelt desire to build teams that would produce innovative products people would love and benefit from.
Decades later, it was time to scale back, be closer to family, and plan for the future. Keegan knew that living near a top-notch medical facility such as Duke was important, and with four grandchildren nearby, moving to the Triangle was an easy decision.
When he suffered heart trouble, Keegan experienced firsthand the incredible talent and skill of the Duke heart team. “My surgery was an amazing experience,” he said. “I benefitted from a tremendous group of talented people, before and after the procedure.”
The professionalism and team culture he witnessed ignited Keegan’s desire to bolster Duke Heart’s impact and accomplishments. So, when a friend suggested he join the Duke Heart Leadership Council, he leapt at the chance to contribute his time and business expertise. Currently serving as the council chair, Keegan is extending his support with his personal philanthropy toward the development of the new Duke Heart Precision and Innovation Collaboratory.
The Duke Heart Precision and Innovation Collaboratory aims to expand the boundaries of the possible and improve cardiovascular health worldwide with a comprehensive, long-range, and multi-phased team approach. Phase 1 will identify promising discoveries in precision genomics, device innovations, and human performance. Phase 2 will scale those discoveries to launch clinical trials, research grants, and new treatment options.
An effort this visionary and all-encompassing, with the potential for global impact, requires immense resources. With a stellar leadership team in place and eager to see the potential realized, Keegan contributed the first $1.5 million toward the Collaboratory’s $10 million fundraising goal.
This initial funding stimulates the process of collecting and compiling huge swaths of data to build the country’s first comprehensive cardiac genomic database and first comprehensive cardiac performance database. Such large volumes of data will allow Duke Health researchers to conduct in-depth analysis and gain a better understanding of trends and patterns.
A second area of further research is a deeper understanding of human heart performance. The gap between a high-performing heart and a failing one is surprisingly small, and the variations and drivers that account for the difference are not well understood. The Collaboratory aims to close this gap.
In addition to this work, the team will optimize devices capable of improving individual patients’ physiology. Duke Heart is an innovator in this space, with one of the largest heart failure device laboratories in the United States. Personalizing the future of device therapy for patients with heart failure will save countless lives.
Keegan built his successful business career by making teams better. Sometimes it was a matter of switching personnel, but often it was choosing the right stimulus to bring out the best of existing team members.
“Duke Heart is a great team that already produces a great product,” he said. “I’m just doing what I can to keep it moving forward so that people are as proud of Duke’s accomplishments in 40 years as they are today.”
Bova Campell to Join HRS Board
 Kristen Bova Campbell, clinical pharmacist for Duke Electrophysiology, has been appointed to serve on the Board of Trustees of the Heart Rhythm Society (HRS). She will become the first PharmD to serve in this capacity when she begins her term in May during the HRS Scientific Sessions scheduled for May 16-19 at the Boston Convention & Exhibition Center, Boston.
Kristen Bova Campbell, clinical pharmacist for Duke Electrophysiology, has been appointed to serve on the Board of Trustees of the Heart Rhythm Society (HRS). She will become the first PharmD to serve in this capacity when she begins her term in May during the HRS Scientific Sessions scheduled for May 16-19 at the Boston Convention & Exhibition Center, Boston.
“It is an honor to be selected as the first PharmD on the HRS Board and to represent all Allied Health Professionals within HRS,” says Bova Campbell. “I am excited to collaborate and contribute to the Society’s mission of providing optimal care to patients with heart rhythm disorders.”
Bova Campbell is director of the PGY2 Cardiology Pharmacy Residency and director of the Duke Heart Center Anticoagulation Clinic. She will join Jonathan Piccini, MD, section chief of electrophysiology, who also serves as a member of the Board, and Sana Al-Khatib, MD, currently serving as 2nd Vice President for the Board.
Congratulations, Kristen!
Rebecca Dial Named NM, Invasive Labs & CVSSU
 We are happy to announce that Rebecca Dial, BSN, RN will serve as Nurse Manager, Operations for the adult Invasive Labs and Cardiovascular Short Stay Unit effective April 1, 2024.
We are happy to announce that Rebecca Dial, BSN, RN will serve as Nurse Manager, Operations for the adult Invasive Labs and Cardiovascular Short Stay Unit effective April 1, 2024.
Rebecca earned a Bachelor of Science in Nursing from the University of North Carolina Greensboro in 2013. Her career spans cardiovascular telemetry, cardiac-surgical stepdown, and cardiac catheterization lab nursing. She has worked in the Adult Cardiac Catheterization Lab at Duke University Hospital since August 2020 and served in a variety of roles, including preceptor and charge nurse. In July 2023, she transitioned into the Assistant Nurse Manager role within the labs and has focused on improving scheduling practices and providing professional development opportunities to staff.
Rebecca is looking forward to partnering with leaders across the organization. Please join us in welcoming her to her new role!
Frye Regional TAVR Training
Dr. John Morrison, an interventional cardiologist with Frye Regional Medical Center and a community consulting associate with the division of cardiology at Duke, spent time throughout March with our Duke Heart Transcatheter Aortic Valve Replacement (TAVR) team.
Frye Regional Medical Center is a Duke LifePoint hospital and full-service cardiovascular center serving a large geographic area in the Catawba Valley region of NC. As an affiliate partner, members of Duke Heart and the Duke Heart Network have been working closely with the team at Frye Regional to help them prepare for the launch of their new TAVR program.
“The willingness of the Duke Heart team to collaborate with regional partners has been clearly evident to Dr. Morrison and he has commented on how wonderful every interaction has been,” said Lisa Kotyra, senior director, Duke Heart Network.
Under the guidance of Kevin Harrison, MD, Morrison had the opportunity to observe all Duke structural cardiologists, cardiac surgeons, and our multidisciplinary team as they worked through the TAVR process and procedure.
Morrison is shown here with Drs. Harrison and Hughes.


Kudos to Gaca!
In a note forwarded this week from David Gallagher, chief medical officer for Duke University Hospital, we have a kudos for Jeff Gaca, our new section chief for adult cardiac surgery:
“We received this nice feedback (from Press Ganey HCAHPS) about the great care you and your team gave to a patient at Duke Hospital. Thank you for the high quality and compassionate care you provide to patients! I believe this is the third Press Ganey inpatient comment in a short period of time from patients who are so appreciative of you.” — David Gallagher, MD
“I can’t say enough good about the nurses in the ICU unit after open heart surgery. I came to Duke from Naples, FL and so glad I did. Dr. Gaca is an amazing surgeon.” — a grateful patient
Way to go, Jeff!
Shout-out to Cheri Wills!
A note of appreciation to Cheri Wills, health center administrator (HCA) for Duke Cardiology of Raleigh and Duke Cardiology of Morrisville, whose last official day with Duke Health is today, March 31. Erica Bradshaw is the new HCA for these locations; she has been training with Cheri since last summer.
Cheri, we wish you all the best in retirement, and thank you for your terrific work over the years!
Duke Heart & 2024 NC Walk for Victory
Duke Heart will again serve as the presenting sponsor of the upcoming NC Walk for Victory in support of Marfan Syndrome, LDS, VEDS, and related conditions, with Dr. Chad Hughes serving as co-medical chair for the walk with Carly Scarborough of Levine Children’s Hospital.
The event is scheduled for 12-3 p.m. on Saturday, April 20 at Laurel Hills Park in Raleigh. To learn more, please visit the NC Walk website and consider joining the Duke Aorta team to raise funds for research!
Last chance! Mere Days Remain to Support Frazier-Mills!

If you have not already done so, please join us in supporting electrophysiologist Camille Frazier-Mills, MD, one of the Triangle American Heart Association’s Women of Impact in her campaign to raise funds to support Go Red for Women.
Frazier-Mills is representing Duke Health as a Woman of Impact in the 2024 campaign and we want to help her reach her campaign goal. By donating, each of us can support her campaign and help ensure more women have equitable access to cardiovascular care and better representation in critically needed medical research.
** Check out Camille Frazier-Mills’ campaign page and please donate by April 4. **
Every year across the country, a select group of individuals are nominated to be a part of Woman of Impact because of their passion and drive to make a difference. This 9-week blind competition is relentlessly focused on women’s heart health. The campaign launched on National Wear Red Day (Feb. 2) and closes on April 4. During this time, the nominees work to build campaign plans, recruit Impact teams, and inspire their networks to support the American Heart Association’s lifesaving mission.
At the end of the campaign, this special group of changemakers will be celebrated for the overall impact they have on the AHA’s mission and the Triangle community. The nominee who makes the greatest impact and raises the most funds locally will be named a local 2024 Woman of Impact Winner.
Additionally, the nominee who makes the greatest impact nationwide will be named the American Heart Association 2024 National Woman of Impact Winner.
Let’s help her reach and exceed her goal – let’s help her WIN! Go, Camille!
Upcoming Events & Opportunities
- April is National Donate Life Month
- April is Earth Month
- April 6-8, American College of Cardiology Scientific Sessions, Atlanta.
Cardiology Grand Rounds
April 2: SCERRI Stories: Mechanistic Insights Into Sepsis Induced Cardiovascular Dysfunction with Willard Applefeld, MD. 5 p.m., DN 2003 or via Zoom.
April 4: Using Nationwide Registries to Conduct Pragmatic Randomized Trials with Tor Biering-Sorensen, MD of the Center for Translational Cardiology and Pragmatic Randomized Trials, Denmark. 5 p.m., DN 2002 or via Zoom. *Special CGR event*
April 9: Heart Failure: Does Sex Really Matter? with Carolyn Lam, of Duke-NUS MD. 5 p.m., DN 2002 or via Zoom.
All Duke Cardiology Grand Rounds recordings are housed on Warpwire. To access recordings please visit:
NET ID and password required. Enjoy!
CD Fellows Core Curriculum Conference
April 3: EP Case Presentation with Joshua Rushakoff and Jawan Abdulrahim. Noon, DMP 2W96 (in-person only).
April 5: We will not meet today.
Upcoming CME Symposia
April 12: Duke Sports Cardiology & Sudden Death in Athletes
May 4: Duke Heart Failure Symposium
For any questions you might have about either event, please reach out to Christy Darnell.
2024 Feagin Leadership Forum
Consider joining members from throughout the Duke community for a special Duke Centennial event, the 15th Annual Feagin Leadership Forum at the JB Duke Hotel on May 17-18. The theme for the Forum is Compassion, Collaboration, and Compromise: Leadership in a Polarized World. World-class leaders from business, healthcare, the military, and athletics will share their leadership expertise and how they address the challenges of our complex world. There will be special welcomes from Duke leaders, and the future leaders of healthcare — this year’s Feagin Leadership Scholars — will share their work and leadership insights.
For more details, go to https://www.feaginleadership.org/schedule-1.
To register, visit https://www.feaginleadership.org/2023registration-1.
Improving Conversation Skills with Seriously Ill Patients
To ensure that clinicians feel comfortable and empowered to have difficult conversations regarding goals of care with patients and their families, members of the Duke Hospice and Palliative Care team offer VitalTalk communication training so that they can help clinicians do their best to take care of our patients.
VitalTalk skills training is open to those involved in conducting or supporting Goals of Care conversations for our patients with serious illnesses across Duke Health. The course consists of a 30-minute didactic lecture in the LMS system, followed by a 3-4 hour skills practice session. CME/CEU credits are available once both activities (LMS and live practice) are completed.
A limited number of seats are available in each of the upcoming online VitalTalk skills practice courses – use https://duke.is/VitalTalk to view available dates and times and to register.
If you have any questions, please contact Jonathan Fischer, MD, medical director of palliative care for Duke’s Population Health Management Office.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
March 22 — Adrian Hernandez
Medpage Today
Tracking Trends in Lung Cancer Incidence, Death in the U.S.
March 22 — Jenny Wu, Brian Southwell, Jonas Swartz
JAMA Network
Patients Are Turning to TikTok for Health Information—Here’s What Clinicians Need to Know
March 23 — Susan Spratt
Senior Resource
Medicare to Cover Wegovy for Patients with Heart Disease
March 23 — Nishant Shah
Everyday Health
Weight Cycling May Increase the Risk of Heart Attack and Stroke
March 25 — Susan Dent (medical oncology)
The ASCO Post
Cardio-Oncology Is a Growing Subspecialty, but Where Are the Oncologists?
March 26 — Harry Severance
Becker’s Physician Leadership
The erosion of physician autonomy
March 27 — Stephen Greene
tctMD
Most HFrEF Patients Eligible for Quadruple Therapy, but Few Get It
March 28 — Nina Nouhravesh
Good Morning America/ABC News
Eating a dozen eggs a week doesn’t hurt your cholesterol: Study
March 28 — Monique Starks
The Clemmons Courier
Demonstration of historic, first-in-the-nation, AED drone delivery held by FCSO
March 28 — Nina Nouhravesh
Today/NBC News
Are eggs bad for cholesterol? New study reveals how many you can eat
March 28 — Duke Health
The People’s Pharmacy
The Never-Ending Egg Dispute Continues
March 28 — Nina Nouhravesh
Talker
Scientists bust myth that eggs are bad for your heart
*also carried by 80 affiliate outlets including in Chicago, Dallas Ft. Worth and New York
March 28 — Nina Nouhravesh
Healio/Cardiology Today
Routinely eating fortified eggs may not adversely affect cholesterol
March 28 — Nina Nouhravesh
Healthline
Eating 12 Eggs a Week Didn’t Raise Cholesterol Levels, New Study Finds
Duke Heart Pulse — March 24, 2024
Chief’s message:
Thomas Awarded Distinguished Professorship, Effective July 1
 Congratulations to electrophysiologist Kevin Thomas, MD, the newly named Donald F. Fortin, M.D. Distinguished Professor of Cardiology.
Congratulations to electrophysiologist Kevin Thomas, MD, the newly named Donald F. Fortin, M.D. Distinguished Professor of Cardiology.
Thomas is among 32 faculty members at Duke University selected to receive distinguished professorships this year. Approval was made by Duke’s Board of Trustees during their February meeting. Each awardee will be recognized during a ceremony at the Washington Duke Inn on May 23. Their new professorships will be effective on July 1.
“I am very pleased to honor these faculty members with distinguished professorships,” said President Vincent Price. “Their outstanding scholarship has advanced knowledge across a wide variety of fields and made a positive impact on society, and I am proud to have them as colleagues.”
Distinguished professorships honor faculty who are well-established members of the Duke academic community and have also achieved distinction as creative scholars in their field or in their ability to transcend disciplines.
“I congratulate my colleagues on receiving distinguished professorships recognizing their impressive scholarly achievements and leadership in our academic community and beyond,” said Provost Alec D. Gallimore. “Duke is tremendously fortunate to count these bold thinkers among its faculty.”
Well deserved, Kevin! Congratulations!
Gutierrez, Rymer Selected for SCAI ELM Cohort

Congratulations to interventional cardiologists Tony Gutierrez and Jennifer Rymer! We learned this week that both have been selected as fellows for the Society for Cardiovascular Angiography & Interventions (SCAI) 2024-2026 Emerging Leader Mentorship (ELM) Program. Only 12 interventionalists are chosen each year.
The mission of the ELM Program is to take a small, highly select group of up-and-coming physicians and support their transition into the next

generation of great thinkers, presenters, teachers, and leaders. Interaction of the ELM Fellows with a highly accomplished panel of Mentors and other ELM Alumni will be fostered during the program, which will also provide Fellows with individualized tools and resources. SCAI conducts this program in partnership with the American College of Cardiology (ACC) and the Cardiovascular Research Foundation (CRF).
During the cohort period fellows will attend dedicated in-person training sessions three times per year during the SCAI, TCT, and ACC annual meetings. They will also be given opportunities for faculty speaking at SCAI and partnering organizations that are congruent with their interests and area of focus. In this way, the ELM Program will assist participants in reaching maximum potential and transitioning into national and societal leaders.
A core mission of the ELM Program is to encourage participation in service opportunities including positions on Councils and Committees that coincide with each Fellow’s clinical, research, or educational interests.
This is a wonderful opportunity for Drs. Gutierrez and Rymer and we are so excited for them.
Congratulations, Jenn and Tony!
Podgoreanu, Selvaraj & Voora Appointed to CPH Faculty Leadership Team
The Center for Precision Health (CPH) has announced the addition of 10 faculty members, including three Duke Heart team members who will serve on the CPH leadership team: Mihai Podgoreanu, MD, chief, division of cardiac anesthesiology; Senthil Selvaraj, MD, assistant professor of medicine in cardiology, and Deepak Voora, MD, associate professor of medicine in cardiology and executive director of the Veterans Affairs National Pharmacogenomics Program. The leadership team also includes surgical oncologist Shelley Huang, MD, vice chair of research in the Department of Surgery.
CPH is a collaborative effort between Duke Clinical & Translational Science Institute (CTSI) and the Precision Genomics Collaboratory (PGC) that works to harness the power of genomic, biomarker, and health data to transform patient care and population health.
The new faculty team will help CPH expand clinical genetics, conduct clinically relevant translational research, perform cutting-edge implementation science, engage with and build trust in the community, as well as contribute to educating the ‘workforce of tomorrow.’
“We are thrilled to have an amazing cohort of faculty joining the Center for Precision Health,” said cardiologist Svati H. Shah, MD, MHS, the Ursula Geller Distinguished Professor of Research in Cardiovascular Diseases, associate dean for translational research and director of the CPH. “Their talents and expertise will help us expand our basic, translational, and clinical research and allow us to harness the power of genomic, biomarker and health data to transform patient care and population health.”
To read more and see the full list of faculty for CPH, please visit https://duke.is/j/4vud.
Congratulations Mihai, Senthil, and Deepak!
Newest JACC Editors Named; Duke Well Represented
Incoming Journal of the American College of Cardiology (JACC) Editor-in-Chief Harlan M. Krumholz, MD, SM, FACC, cardiologist with Yale University, this week announced the members of his new Editorial Board, each of whom will be responsible for helping to position the journal as the leading beacon for advancing global cardiovascular health, effective July 1.
Several Duke faculty members are on the team, as well as a number of Duke graduates and former trainees, including:
- Lesley H. Curtis, PhD, Duke professor of population health sciences and of medicine. Curtis will serve as a deputy editor.
- Melvin Echols, MD, cardiologist with Morehouse School of Medicine and a former Duke Cardiology fellow. Echols will serve as an associate editor.
- Kushal T. Kadakia, MSc, a Duke graduate and former member of Duke-Margolis Institute for Health Policy. Kadakia will serve as a deputy associate editor.
- Carolyn Lam, MBBS, PhD, cardiologist with Duke-National University of Singapore, will serve as a deputy editor.
- Neha Pagidipati, MD, MPH, cardiologist and director of the Duke Cardiometabolic Prevention Clinic will serve as an associate editor.
- Anne Marie Valente, MD, of Harvard Medical School, is a former Duke fellow in pediatric cardiology and in adult cardiovascular disease. Valente will serve as an associate editor.
Congratulations to all!
Burleson Named Nurse Manager, DUH 3100, Effective April 1
 Duke Heart is pleased to announce that Matt Burleson, BSN, RN will become Nurse Manager, Operations for Duke University Hospital’s Cardiothoracic Stepdown Unit 3100 effective April 1.
Duke Heart is pleased to announce that Matt Burleson, BSN, RN will become Nurse Manager, Operations for Duke University Hospital’s Cardiothoracic Stepdown Unit 3100 effective April 1.
Matt earned a Bachelor of Science in Nursing from the University of Tennessee, Knoxville in 2015 and is currently pursuing his Master of Science in Nursing through East Carolina University. He began his nursing career on a progressive cardiac care unit in Atlanta, Georgia and transitioned to Duke’s Surgical Trauma Intensive Care Unit in September of 2016. His time spent on the Surgical Trauma ICU has been carried out through a variety of roles including Preceptor, Resource Nurse, and Charge Nurse. Over the past 2.5 years, he has served as Assistant Nurse Manger. As ANM, he has contributed to the continuation of the SICU CLABSI Reduction Initiative, lead Mass Casualty Incident Plan preparedness, and facilitated Armed and Dangerous drills.
He enjoys the opportunity to listen to, teach, and coach team members. Matt also has been an active member of Duke’s Patient Response Team where he has appreciated building relationships and caring for patients across a wider breadth of the hospital. Matt is looking forward to joining the Duke Heart Team and continuing his journey as a Duke Nurse Leader.
Please join us in congratulating and welcoming Matt to his new role.
Shout-out to Fox!
 A shout-out to Duke Heart clinical nurse specialist, Allison Fox, who presented at the 2024 National Association for Clinical Nurse Specialists (NACNS) Annual Conference. NACNS 2024 was held on March 10-13 in New Orleans. Fox shared her abstract presentation, “Introducing Subcutaneous Diuretic Therapy in the Ambulatory Setting,” which highlighted the CNS role in bridging the gap between innovation and clinical practice in the heart failure clinic.
A shout-out to Duke Heart clinical nurse specialist, Allison Fox, who presented at the 2024 National Association for Clinical Nurse Specialists (NACNS) Annual Conference. NACNS 2024 was held on March 10-13 in New Orleans. Fox shared her abstract presentation, “Introducing Subcutaneous Diuretic Therapy in the Ambulatory Setting,” which highlighted the CNS role in bridging the gap between innovation and clinical practice in the heart failure clinic.
Way to go, Allison!
Kudos to Heart Care Team & Zwischenberger!
We received a wonderful patient comment this week regarding heart surgeon Brittany Zwischenberger, MD, and the patient’s full care team. The note, captured by Press Ganey HCAHPS, went to David Gallagher, chief medical officer. He then shared it with our team:
“I must commend the following people for their good care – Miles, Colby, Ashley, Erica, Lindsey, Amber, Catherine, Mallory, Taylor, and Dr. Brittany Zwischenberger. Plus Joan in pre-op.” – a grateful patient
Thank you for the high quality and compassionate care you provide to patients! – Dr. David Gallagher
Kudos, Brittany and team – you’re amazing providers and we are fortunate to have you on our team!
Duke-DCRI Reception at ACC.24
For those of you attending the American College of Cardiology’s Annual Scientific Sessions (April 6-8), please join us at the annual Duke-DCRI Reception taking place on Saturday, April 6, 2024, from 5:30-8:30 p.m. EDT, at the Omni Atlanta Hotel at Centennial Park in Grand C Ballroom, North Tower-M4.
USNWR Voting Closes Wednesday
USNWR voting for Best Hospitals by specialty is still open in Doximity. If you are board-certified in the U.S. and have claimed your Doximity profile already, please log into your account by Wednesday, March 27 to complete the brief survey: submit your nominations.
New to Doximity? Find and register your profile to vote. Just go to Doximity’s login page, scroll to the bottom and click on “find your profile” – find yours and claim it/register. You can participate in the survey as long as you register on Doximity prior to the survey closing on March 27.
The survey allows you to list up to five hospitals as Best Hospital in the specialty in which you are board-certified. Your ballot counts even if you vote only for one hospital.
As with primaries and national elections, every vote is important!
Just 11 Days Remain to Support Frazier-Mills!

If you have not already done so, please join us in supporting electrophysiologist Camille Frazier-Mills, MD, one of the Triangle American Heart Association’s Women of Impact in her campaign to raise funds to support Go Red for Women.
Frazier-Mills is representing Duke Health as a Woman of Impact in the 2024 campaign and we want to help her reach her campaign goal. By donating, each of us can support her campaign and help ensure more women have equitable access to cardiovascular care and better representation in critically needed medical research.
** Check out Camille Frazier-Mills’ campaign page and please donate by April 4. **
Every year across the country, a select group of individuals are nominated to be a part of Woman of Impact because of their passion and drive to make a difference. This 9-week blind competition is relentlessly focused on women’s heart health. The campaign launched on National Wear Red Day (Feb. 2) and closes on April 4. During this time, the nominees work to build campaign plans, recruit Impact teams, and inspire their networks to support the American Heart Association’s lifesaving mission.
At the end of the campaign, this special group of changemakers will be celebrated for the overall impact they have on the AHA’s mission and the Triangle community. The nominee who makes the greatest impact and raises the most funds locally will be named a local 2024 Woman of Impact Winner.
Additionally, the nominee who makes the greatest impact nationwide will be named the American Heart Association 2024 National Woman of Impact Winner.
Let’s help her reach and exceed her goal – let’s help her WIN! Go, Camille!
Improving Conversation Skills with Seriously Ill Patients
Did You Know? Patients from Duke cardiology, hepatology and oncology are the most likely to end up in the hospital during their last month of life. These are the patients most in need of goals of care conversations, according to researchers from Duke in their recently published findings in the Journal of Pain and Symptom Management.
To make sure that clinicians feel comfortable and empowered to have these difficult conversations with patients and their families, members of the Duke Hospice and Palliative Care team offer VitalTalk communication trainings so that they can help clinicians do their best to take care of our patients.
VitalTalk skills training is open to those involved in conducting or supporting Goals of Care conversations for our patients with serious illness across Duke Health. The course consists of a 30-minute didactic lecture in the LMS system, followed by a 3-4 hour skills practice-session. CME/CEU credits are available once both activities (LMS and live practice) are completed.
A limited number of seats are available in each of the upcoming online VitalTalk skills practice courses – use https://duke.is/VitalTalk to sign up for one of the following:
- March 19, 1 – 5 pm
- April 10, 8 am to 12 pm
- April 10, 1 – 5 pm
- April 12, 8 am to 12 pm
- April 12, 1 – 5 pm
- May 1, 8 am to 12 pm
- May 1, 1 – 5 pm
- May 16, 8 am to 12 pm
- May 16, 1 – 5 pm
- June 18, 8 am to 12 pm
- June 18, 1 – 5 pm
- June 21, 8 am to 12 pm
- June 21, 1 – 5 pm
Once registered, you will receive an Outlook calendar invite, Zoom details, and instructions for completing the required pre-work module in LMS.
Please keep in mind these trainings are limited to a small number of participants because they are extremely interactive. If you are interested in training but these dates do not work for you, please contact Jennifer Bowen to be added to a distribution list for future signups.
Once registered, if your plans change or you are unable to dedicate your full attention during the course, please let the team know ASAP so that you can be rescheduled and your seat offered to others on the waitlist.
If you have any questions, please contact Jonathan Fischer, MD, medical director of palliative care for Duke’s Population Health Management Office.
Upcoming Events & Opportunities
- March 30 is National Doctor’s Day
- Happy Spring, everyone!
Cardiology Grand Rounds
March 26: New Direction for CABG: Women and Robots with Brittany Zwischenberger, MD. 5 p.m., DN 2002 or via Zoom.
April 2: SCERRI Stories: Mechanistic Insights Into Sepsis Induced Cardiovascular Dysfunction with Willard Applefeld, MD. 5 p.m., DN 2003 or via Zoom.
April 9: Heart Failure: Does Sex Really Matter? with Carolyn Lam, of Duke-NUS MD. 5 p.m., DN 2002 or via Zoom.
All Duke Cardiology Grand Rounds recordings are housed on Warpwire. To access recordings please visit:
NET ID and password required. Enjoy!
CD Fellows Core Curriculum Conference
March 27: DHP Case Presentation with Aubrie Carroll. Noon, DMP 2W96 (in-person only).
March 29: Endocarditis with Andrew Wang. Noon, Zoom only.
Upcoming CME Symposia
April 12: Duke Sports Cardiology & Sudden Death in Athletes
May 4: Duke Heart Failure Symposium
For any questions you might have about either event, please reach out to Christy Darnell.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
March 13 — Christopher Granger
Inside Precision Medicine
March 18 — John Guyton (emeritus/endocrinology)
Medscape
Niacin and CV Risk: Should Advice on Intake Change?
March 18 — Padma Gulur (anesthesiology)
Daily Mail
March 18 — Ralph Snyderman (Chancellor Emeritus)
Medium
Must-Read Books on the Advancement of Healthcare
March 19 — Joseph Turek
Scientific American
Partial Heart Transplants Grow with Their Young Recipients
March 20 — Duke University Hospital (lung tx)
Newson6.com (Oklahoma)
A Breath of Hope: The Remarkable Journey of Oklahoma Triple Lung Transplant Survivor
March 20 — Mary Klotman
WFMY (Greensboro, NC)
First Lady Dr. Jill Biden makes stop in Durham to talk research in women’s health
Duke Heart Pulse — March 17, 2024
Duke Heart Pulse – March 17, 2024
Highlights of the week:
Happy St. Patrick’s Day
 We hope you are having a terrific weekend – Happy St. Patrick’s Day to one and all!
We hope you are having a terrific weekend – Happy St. Patrick’s Day to one and all!
CV Emergencies Summit Held at Duke
The Summit for Regional Systems of Care for Cardiovascular Emergencies, hosted by Duke Heart, was held at University Tower on Friday, March 15. The event was open to regional partners in the care of patients with acute myocardial infarction including referring hospitals, EMS agencies, and other PCI centers. The event allowed participants to collaboratively review data and discuss processes to improve acute MI care across the state and region.
 This was the first such regional CV emergencies summit held since before the COVID pandemic, with nearly 40 attendees representing Alamance, UNC Health, Mariah Parham, the Durham VAMC, the American Heart Association, and other sites across the Triangle participating.
This was the first such regional CV emergencies summit held since before the COVID pandemic, with nearly 40 attendees representing Alamance, UNC Health, Mariah Parham, the Durham VAMC, the American Heart Association, and other sites across the Triangle participating. 
“We had great leadership from Dr. Granger, Duke Cardiology, and the Duke Heart Network to reinvigorate this work post-COVID and continue driving emergency cardiovascular care and response forward,” said Jill Engel, Service Line Vice President, Duke Heart & Vascular.
A big thanks to all who joined us, to Melissa Williams and Natalie Horseman for helping to plan the event, and to Drs. Christopher Granger and Schuyler Jones, and all presenters for taking the time to share your knowledge.
Plans are already underway to host another regional summit in 2025. Great job all — Go Duke!!
Match Day 2024
Congratulations to all future Duke trainees! Duke’s Internal Medicine Residency matched 45 Categorical, 1 PSTP, 2 Medicine-Psychiatry, 6 Medicine-Pediatrics, 7 Neurology Preliminary, and 4 Preliminary trainees. Additionally, the categorical interns will have attended 37 different medical schools, 21 are female, 24 are male, and 17 identify as under-represented in medicine. Matches were announced on Friday, March 15.
To read the full story and find a link to a slide deck of incoming IM residents, please visit https://duke.is/r/y6y9.
A big shout-out to cardiologist and Cardiovascular Research Center member Chris Holley who, along with nephrologist Xunrong Luo, manage the physician-scientist training program (PSTP) recruitment for the Department of Medicine.
Improving Conversation Skills with Seriously Ill Patients
Did You Know? Patients from Duke cardiology, hepatology, and oncology are the most likely to end up in the hospital during their last month of life. These are the patients most in need of goals of care conversations, according to researchers from Duke in their recently published findings in the Journal of Pain and Symptom Management.
To make sure that clinicians feel comfortable and empowered to have these difficult conversations with patients and their families, members of the Duke Hospice and Palliative Care team offer VitalTalk communication training so that they can help clinicians do their best to take care of our patients.
VitalTalk skills training is open to those involved in conducting or supporting Goals of Care conversations for our patients with serious illnesses across Duke Health. The course consists of a 30-minute didactic lecture in the LMS system, followed by a 3-4 hour skills practice session. CME/CEU credits are available once both activities (LMS and live practice) are completed.
A limited number of seats are available in each of the upcoming online VitalTalk skills practice courses – use https://duke.is/VitalTalk to sign up for one of the following:
- March 19, 1 – 5 pm
- April 10, 8 am to 12 pm
- April 10, 1 – 5 pm
- April 12, 8 am to 12 pm
- April 12, 1 – 5 pm
- May 1, 8 am to 12 pm
- May 1, 1 – 5 pm
- May 16, 8 am to 12 pm
- May 16, 1 – 5 pm
- June 18, 8 am to 12 pm
- June 18, 1 – 5 pm
- June 21, 8 am to 12 pm
- June 21, 1 – 5 pm
Once registered, you will receive an Outlook calendar invite, Zoom details, and instructions for completing the required pre-work module in LMS.
The trainings are limited to a small number of participants because they are extremely interactive. If you are interested in training but these dates do not work for you, please contact Jennifer Bowen to be added to a distribution list for future signups.
Once registered, if your plans change or you are unable to dedicate your full attention during the course, please let the team know ASAP so that you can be rescheduled and your seat offered to others on the waitlist.
If you have any questions, please contact Jonathan Fischer, MD, medical director of palliative care for Duke’s Population Health Management Office.
Support Frazier-Mills, Duke Health’s 2024 AHA Woman of Impact!

Please join us in supporting electrophysiologist Camille Frazier-Mills, MD, one of the Triangle American Heart Association’s Women of Impact in her campaign to raise funds to support Go Red for Women.
Frazier-Mills is representing Duke Health as a Woman of Impact in the 2024 campaign and we want to help her reach her campaign goal. By donating, each of us can support her campaign and help ensure more women have equitable access to cardiovascular care and better representation in critically needed medical research.
** Check out Camille Frazier-Mills’ campaign page and please donate by April 4. **
Every year across the country, a select group of individuals are nominated to be a part of Woman of Impact because of their passion and drive to make a difference. This 9-week blind competition is relentlessly focused on women’s heart health. The campaign launched on National Wear Red Day (Feb. 2) and closes on April 4. During this time, the nominees work to build campaign plans, recruit Impact teams, and inspire their networks to support the American Heart Association’s lifesaving mission.
At the end of the campaign, this special group of changemakers will be celebrated for the overall impact they have on the AHA’s mission and the Triangle community. The nominee who makes the greatest impact and raises the most funds locally will be named a local 2024 Woman of Impact Winner.
Additionally, the nominee who makes the greatest impact nationwide will be named the American Heart Association 2024 National Woman of Impact Winner.
Let’s help her reach and exceed her goal – let’s help her WIN! Go, Camille!
Please Vote in USNWR Best Hospitals for Cardiology & Heart Surgery
USNWR voting for Best Hospitals by specialty is still open in Doximity. If you are board-certified in the U.S. and have claimed your Doximity profile already, please log into your account by March 27 to complete the brief survey: submit your nominations.
New to Doximity? Find and register your profile to vote. Just go to Doximity’s login page, scroll to the bottom and click on “find your profile” – find yours and claim it/register. You can participate in the survey as long as you register on Doximity prior to the survey closing on March 27.
The survey allows you to list up to five hospitals as Best Hospital in the specialty in which you are board-certified. Your ballot counts even if you vote only for one hospital.
As with primaries and national elections, every vote is important!
ICYMI: A New Lemur to Visit
 In happy (non-medical) news, the Duke Lemur Center recently announced the birth of Albus, a male Coquerel’s sifaka, who weighed in at 118 grams. Albus, which is Latin for “white,” was a common Roman surname and the moniker for the Roman port city of Portus Albus (“White Harbor”), was born to parents Rodelina and Johann. He has an older sister, Egeria.
In happy (non-medical) news, the Duke Lemur Center recently announced the birth of Albus, a male Coquerel’s sifaka, who weighed in at 118 grams. Albus, which is Latin for “white,” was a common Roman surname and the moniker for the Roman port city of Portus Albus (“White Harbor”), was born to parents Rodelina and Johann. He has an older sister, Egeria.
The Duke Lemur Center, founded in 1966, is an internationally acclaimed non-invasive research center housing over 200 lemurs and bush babies across 13 species—the most diverse population of lemurs on Earth, outside their native Madagascar.
New additions are a great reason to visit the Center! Plan ahead, however, as reservations are required to visit. The main tour season opens in May and runs through the end of September.
Upcoming Events & Opportunities
- March is National Nutrition Month
- USNWR Best Hospitals Voting is open (through March 27). Please check your Doximity account and vote!
Cardiology Grand Rounds
March 19: Beyond the Bump: Navigating the Interplay of Cardiovascular Health and Obstetrics in the Modern Era with Sarah Snow, MD. 5 p.m., DN 2002 or via Zoom.
March 26: New Direction for CABG: Women and Robots with Brittany Zwischenberger, MD. 5 p.m., DN 2002 or via Zoom.
All Duke Cardiology Grand Rounds recordings are housed on Warpwire. To access recordings please visit:
NET ID and password required. Enjoy!
CD Fellows Core Curriculum Conference
March 19: HF/Txp Case Presentation with Aubrie Carroll. Noon. DHN 2201 (in-person only). Note room change!
March 22: Update on Mechanical Circulatory Support with Imran Aslam. Noon, Zoom only.
Upcoming CME Symposia
April 12: Duke Sports Cardiology & Sudden Death in Athletes
May 4: Duke Heart Failure Symposium
For any questions you might have about either event, please reach out to Christy Darnell.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
March 9 — Harry Severance
LinkedIn Pulse
Federal “Anti-Referral/Kickback” Laws – How They Paradoxically End Up Hurting Patient Care
March 11 — Duke Health
Becker’s Hospital Review
16 of nation’s top health systems form AI clinical safety network
March 12 — Duke Health
Medical Automation
First Partial Heart Transplant
March 12 — Nishant Shah
Health Central
Which Chronic Diseases Could New Gene Editing Technology Eradicate?
March 12 — Christopher Granger
NIH.gov
NIH opens long COVID trials to evaluate treatments for autonomic nervous system dysfunction
March 12 — Michael Pencina
Healthcare Dive
Microsoft forms health AI governance network
March 12 — Salim Idriss
U.S. Food & Drug Admin/CDER Science
March 12 — Duke Health
AHA.org (American Hospital Assoc.)
Consortium aims to promote responsible AI use for health
March 13 — Marat Fudim
Healio/Cardiology Today
Scale using biosensor technology detects HF events more often than standard of care
March 13 — Christopher Granger
Philly Voice
New clinical trials to examine treatments for long COVID symptoms
Duke Heart Pulse — March 10, 2024
Chief’s message:
Busy week at Duke Heart with lots of faculty and fellows working hard to get ready for the American College of Cardiology meeting (ACC 2024), taking care of patients with teams working to help solve problems in unique ways (e.g. Nicole Pristera and AHF teams caring for patients with mechanical devices), and Duke – UNC basketball game weekend. This next week starts the spring break season with the upcoming easter week being the most popular week for spring break in the area. So, however you connect with us at Duke Heart, we are grateful for your continued support and hope you and your family get time this spring to spend time to recharge, get perspective, and appreciate the difference we are able to make with Duke Heart. Please find highlights from the week below.
Highlights of the week:
Ramadan Begins Tonight
Now that we’re past the always exciting Battle of the Blues and ESPN Game Day, we hope everyone is adjusting to the return of daylight saving time (which occurred this morning — hopefully you remembered!). Today also marks the start of Ramadan. To all those on our team and beyond who are participating, we wish you, “Ramadan Mubarak!”
Kittipibul Wins Abstract Competition at THT 
We are thrilled to share that Mark Kittipibul, MD, a third-year Duke cardiology fellow, won the Fellows’ Abstract Competition at the Cardiovascular Research Foundation’s (CRF) Technology and Heart Failure Therapeutics (THT) 3rd annual meeting. THT 2024 was held March 4-6 at the Westin Boston Seaport in Boston.
Kittipibul won for his abstract presentation, “Blood Volume Profiles and Correlations with Pressures in Heart Failure with Impaired Renal Function,” which utilized data from the Multi-center Blood Volume Analysis Registry led by Marat Fudim, MD, who is also his mentor.
Great job, Mark!
Cardiac Ultrasound Students Awarded National Scholarships
We’re pleased to announce that three students training in our Duke Cardiac Ultrasound Certificate Program (DCUCP) have been selected as national scholarship award recipients.
Mariah Byington has been selected to receive the Alan Waggoner Award and Anna Lise McGowan has been selected to receive the Sandy Katanick Award from the American Society of Echocardiography (ASE). The awards will be presented to them during ASE’s upcoming 35th Annual Scientific Sessions planned for June 14-16, 2024 at the Oregon Convention Center in Portland, OR. Each award comes with a $1,000 scholarship and $1,000 for travel to the meeting.
Morgan Osborne has been selected as the recipient of the Cardiovascular Credentialing International (CCI) Aaron S. White Educational Grant. Of the two CCI grants awarded annually, only one goes to a student. Osborne will receive $2,500.
This is the third year in a row that DCUCP students have earned ASE awards and the second year in a row that one of our students has won the CCI grant. Congratulations, Morgan, Mariah, and Anna Lise!
Shah to Serve on ACC Faculty Development Work Group

Nishant Shah, MD, assistant professor of medicine in cardiology, has been selected for the Faculty Development Work Group (FDWG) of the American College of Cardiology (ACC). He will serve for two years. The mission of the FDWG is to educate and develop ACC faculty and to support the education endeavors of the College.
Last year, Shah was selected for the ACC’s highly competitive Emerging Faculty Leadership Academy. With this next step, Shah will have the opportunity to help create and lead educational content for the ACC. His first meeting as a member of the FDWG will occur during the ACC Annual Scientific Sessions taking place from April 6-8 in Atlanta, GA.
Congratulations, Nishant!
Think-tanks, CRT Annual Meeting Taking Place in DC
It’s another busy weekend in Washington for cardiovascular leaders from Duke! 
Cardiovascular Research Technologies (CRT) is holding its annual meeting at the Washington Hilton Hotel in Washington, DC (March 9-12). CRT is a leading educational forum on new cardiovascular technology and procedures for physicians and healthcare professionals. For this year’s meeting, Mitch Krucoff, MD is serving as course director for the Cardiogenic Shock, FDA Town Hall, and Japan FDA Town Hall programs.
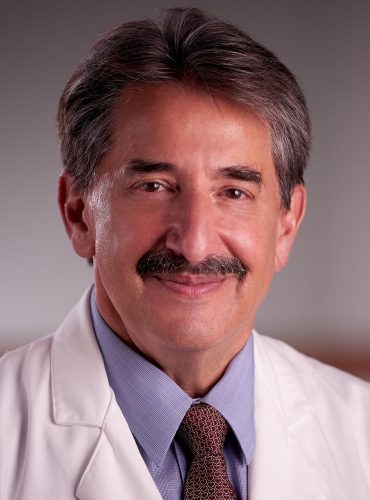 Duke/Duke Clinical Research Institute, in conjunction with the CRT meeting, holds annual in-person think tanks for two of their most mature public-private partnerships (PPP) under Memoranda of Understanding (MOUs) between Duke/DCRI and the U.S. Food & Drug Administration (FDA). Think-tanks are being held this weekend for the Cardiac Safety Research Consortium (CSRC), which is in its 18th year, and the Medical Device Epidemiology Network (MDEpiNet) Predictable And SuStainable Implementation Of National CardioVascular Registries (PASSION CV Registries), a PPP in its 12th year.
Duke/Duke Clinical Research Institute, in conjunction with the CRT meeting, holds annual in-person think tanks for two of their most mature public-private partnerships (PPP) under Memoranda of Understanding (MOUs) between Duke/DCRI and the U.S. Food & Drug Administration (FDA). Think-tanks are being held this weekend for the Cardiac Safety Research Consortium (CSRC), which is in its 18th year, and the Medical Device Epidemiology Network (MDEpiNet) Predictable And SuStainable Implementation Of National CardioVascular Registries (PASSION CV Registries), a PPP in its 12th year.
The CSRC think-tank program will focus on cardiogenic shock and features the American Heart Association’s national Cardiogenic Shock Registry—a part of the AHA’s Get With the Guidelines registry portfolio (and the only professional society-sponsored shock registry in the world) — as the team rolls out their first pilot research directions for 2024. Krucoff co-chairs the Cardiogenic Shock Registry steering committee with David Morrow, MD, director of the Levine Cardiac Intensive Care Unit at Brigham and Women’s Hospital.
The MDEpiNet think-tank program will focus on multiple areas of novel clinical trial approaches to regulatory science and evidence development for heart valves, coronary devices, PAD intervention, mechanical circulatory support devices for shock, and aortic intervention. Drs. Jimmy Tcheng; C. Michael Gibson and Bobby Yeh of Harvard; David Erlinge from the Swedish Coronary Angiography and Angioplasty Registry (SCAAR); and Ernest Spitzer from Cardialysis in Rotterdam, Netherlands, along with multiple industry experts, including Bram Zuckerman from the FDA’s Center for Devices and Radiologic Health (CDRH) who will focus on advancing real-world data interoperability to support better, more efficient and re-usable prospective device trial operations and evidence quality.
Growing Cardiovascular Care Services in Low-Resource Settings
 As part of the Duke Department of Medicine celebration of Black History Month, Titus Ngeno, MD, assistant professor of medicine in cardiology and member of the Duke Global Health Institute was highlighted in a Q&A on Feb. 27.
As part of the Duke Department of Medicine celebration of Black History Month, Titus Ngeno, MD, assistant professor of medicine in cardiology and member of the Duke Global Health Institute was highlighted in a Q&A on Feb. 27.
Born and raised in Kenya, he trained in medicine at the University of Nairobi and then as a medical officer at Moi Teaching and Referral Hospital (MTRH) in Eldoret, Kenya, where he became known to several Duke faculty members as an outstanding clinician with notable leadership qualities.
Ngeno is a graduate of the Master of Science in Global Health program at Duke and he recently completed the global health pathway for a second time as a cardiovascular disease global health fellow. He completed his medical training in 2017, choosing to pursue cardiology and global health as a specialist because the unique combination allowed him to spend time caring for patients at the bedside while working to improve access to health care.
The Q&A piece is well worth checking out, as Titus speaks about his passion for helping improve cardiovascular care both here and abroad.
Shout-out to Thakkar!
 Anna Lisa Chamis shared a wonderful note she received this week regarding patient care and guidance provided by Aarti Thakkar.
Anna Lisa Chamis shared a wonderful note she received this week regarding patient care and guidance provided by Aarti Thakkar.
“Dear Dr. Chamis, I wanted to send a big shout-out filled with gratitude to the cardiology fellow Dr. Aarti Thakkar. I am a neurology resident covering nights this week, and we had a floor stroke patient we were concerned may be developing cardiogenic shock. We walked over to the CCU for advice, and Dr. Thakkar was very kind with some guidance. She then walked over to evaluate the patient herself and recommended transfer to the CCU for further care. She went above and beyond to help us, and she provided the best care for the patient. I just wanted to share how much we appreciated her assistance.” — Jordan Larsen, Neurology PGY3
Nicely done, Aarti!
Kudos to Pinel!
 We are pleased to recognize Duke Heart nursing team member Anna Pinel, CNIV, of our 3200/7200 Cardiology Stepdown unit for her heroic effort at a bowling alley last weekend. Anna was competing in a bowling tournament when another player collapsed. Anna quickly jumped in to administer CPR – providing solo CPR until EMS arrived. The gentleman was transported to a local hospital for further treatment and is expected to make a full recovery. The physicians who received the patient shared that, without Anna’s efforts, the outcome would have been vastly different.
We are pleased to recognize Duke Heart nursing team member Anna Pinel, CNIV, of our 3200/7200 Cardiology Stepdown unit for her heroic effort at a bowling alley last weekend. Anna was competing in a bowling tournament when another player collapsed. Anna quickly jumped in to administer CPR – providing solo CPR until EMS arrived. The gentleman was transported to a local hospital for further treatment and is expected to make a full recovery. The physicians who received the patient shared that, without Anna’s efforts, the outcome would have been vastly different.
“We are so proud to have Anna on our Duke Heart team!!!” – team members from 3200/7200
“Anna, I am truly moved by the incredible courage and selflessness displayed by you! Your swift and unwavering response during the bowling tournament is nothing short of heroic. It’s heartwarming to hear that the gentleman is expected to recover! The fact that you persisted with high-quality CPR for ten minutes is a testament to your determination!!! I can only imagine how emotionally challenging this experience must have been for you. We are all immensely proud to have you as part of the Duke nursing family,” said Chantal Howard, Chief Nursing and Patient Care Services Officer, Duke University Hospital
“Your actions saved this man’s life and truly impacted him and his family. Truly amazing and we are fortunate to have you on the Duke Heart/ Duke team.” – Mary Lindsay, Associate Chief Nursing Officer, Duke Heart Services
“This is amazing and I’m very proud of Anna for jumping in and literally saving a life,” – Jill Engel, Service Line VP, Duke Heart & Vascular Services
Way to go, Anna!
ICYMI: Intramural Basketball Player Rescued with CPR, AED
For another example of Duke team members using CPR to save a life, read about what occurred when a Duke physical therapist collapsed in Wilson Recreation Center and quick-thinking, well-trained individuals revived him. The story was featured in the March 6 issue of Duke Today.
https://today.duke.edu/2024/03/life-saved-intramural-basketball-player-rescued-cpr-aed
DUHS Leadership Updates
Two leadership updates were made on Thurs., March 7 by Tom Owens, executive vice-president and COO, Duke University Health System (DUHS), and Gregory Pauly, president, Duke University Hospital (DUH).
First, Kristie Barazsu, MBA has been named Associate Chief Operating Officer (ACOO) for Patient Flow, Emergency Services, and Support Services at DUH. Kristie has served as ACOO in an interim capacity since May 2023. Kristie assumes this role permanently, effective immediately.
In addition to the service areas mentioned above, Kristie will have oversight of the Operations Administrators (OAs), Patient Information Services, and contractual relationships for Food Services, Environmental Services, and Valet Parking. She will also be responsible for representing DUH as the liaison to Engineering & Operations, Transportation & Parking, Security, and FPDC.
Next, with the departure of Carey Unger as Service Line Vice President for Neurosciences and Behavioral Health at the end of this week (March 15), Unger’s system responsibilities will transition temporarily to Jill Engel, Vice President for Heart & Vascular Services for DUHS. Jill will serve in that role for the next 3-4 months while a sustainable long-term plan is determined.
Congratulations to Kristie and Jill on their expanded roles within DUHS!
Nursing Leaders Attend Specialty Hiring Event
 On Wednesday, March 6, several Duke Heart leaders for our Stepdown Units attended the DUHS RN Specialty Hiring Event at Cameron Stadium. They had the opportunity to meet with over 30 potential candidates and establish shadow/interview experiences. They are hoping this will yield new Heart team members!
On Wednesday, March 6, several Duke Heart leaders for our Stepdown Units attended the DUHS RN Specialty Hiring Event at Cameron Stadium. They had the opportunity to meet with over 30 potential candidates and establish shadow/interview experiences. They are hoping this will yield new Heart team members!
CME Update
Registration is now open for two Duke Heart symposia. Our 9th Annual Duke Sports Cardiology Symposium will take place on April 12 and the Duke Heart Failure Symposium, will take place on May 4. Links also available below under ‘upcoming events’.
Support Frazier-Mills, Duke Health’s 2024 AHA Woman of Impact!
Please join us in supporting electrophysiologist Camille Frazier-Mills, MD, one of the Triangle American Heart Association’s Women of Impact in her campaign to raise

funds to support Go Red for Women.
Frazier-Mills is representing Duke Health as a Woman of Impact in the 2024 campaign and we want to help her reach her campaign goal. By donating, each of us can support her campaign and help ensure more women have equitable access to cardiovascular care and better representation in critically needed medical research.
** Check out Camille Frazier-Mills’ campaign page and please donate by April 4. **
Every year across the country, a select group of individuals are nominated to be a part of Woman of Impact because of their passion and drive to make a difference. This 9-week blind competition is relentlessly focused on women’s heart health. The campaign launched on National Wear Red Day (Feb. 2) and closes on April 4. During this time, the nominees work to build campaign plans, recruit Impact teams, and inspire their networks to support the American Heart Association’s lifesaving mission.
At the end of the campaign, this special group of changemakers will be celebrated for the overall impact they have on the AHA’s mission and the Triangle community. The nominee who makes the greatest impact and raises the most funds locally will be named a local 2024 Woman of Impact Winner.
Additionally, the nominee who makes the greatest impact nationwide will be named the American Heart Association 2024 National Woman of Impact Winner.
Let’s help her reach and exceed her goal – let’s help her WIN! Go, Camille!
Please Vote in USNWR Best Hospitals for Cardiology & Heart Surgery
USNWR voting for Best Hospitals by specialty is now open in Doximity. If you are board-certified in the U.S. and have claimed your Doximity profile already, please log into your account by March 27 to complete the brief survey: submit your nominations.
New to Doximity? Find and register your profile to vote. Just go to Doximity’s login page, scroll to the bottom and click on “find your profile” – find yours and claim it/register. You can participate in the survey as long as you register on Doximity prior to the survey closing on March 27.
The survey allows you to list up to five hospitals as Best Hospital in the specialty in which you are board-certified. Your ballot counts even if you vote only for one hospital.
As with primaries and national elections, every vote is important!
Upcoming Events & Opportunities
- March 10-16 is National Pulmonary Rehab Week & Patient Safety Awareness Week!
- March is National Nutrition Month
- USNWR Best Hospitals Voting is open (through March 27). Please check your Doximity account and vote!
Cardiology Grand Rounds
March 12: Arrhythmias in Myocardial Infarction: Beyond the Substrate with Ching Zhu, MD. 5 p.m., DN 2002 or via Zoom.
March 19: Beyond the Bump: Navigating the Interplay of Cardiovascular Health and Obstetrics in the Modern Era with Sarah Snow, MD. 5 p.m., DN 2002 or via Zoom.
March 26: New Direction for CABG: Women and Robots with Brittany Zwischenberger, MD. 5 p.m., DN 2002 or via Zoom.
All Duke Cardiology Grand Rounds recordings are housed on Warpwire. To access recordings please visit:
NET ID and password required. Enjoy!
CD Fellows Core Curriculum Conference
March 13: Journal Club with Joseph Lerman. Noon. DMP 2W96 (in-person only).
March 15: Antiplatelet Therapy with James Tcheng. Noon, Zoom only.
Upcoming CME Symposia
April 12: Duke Sports Cardiology & Sudden Death in Athletes
May 4: Duke Heart Failure Symposium
For any questions you might have about either event, please reach out to Christy Darnell.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
February 28 — Duke University Medical Center
Cardiovascular Business
Early feasibility study for implantable heart failure monitor moves forward
March 3 — Payal Kohli
Parade
March 4 — Michael Pencina
Becker’s Health IT
Health system leaders join Microsoft-backed nonprofit
March 4 — Stephen Greene
HCP Live
Cardiology Month in Review: February 2024
March 4 — Michael Pencina
Healthcare Innovation
CHAI Names CEO, Directors, Advisory Boards
March 5 — William Kraus
Awaken
Even Short Bursts Of Exercise Can Reduce Americans’ Risk Of Disease And Death, Study Says
March 5 — Duke University Hospital
NC Medical Society
Duke, UNC Hospitals Ranked in Top 100 in Nation
March 6 — Marat Fudim and Richard Krasuski
Mass Device
Gradient begins pulmonary artery denervation trial in the U.S.
March 6 — Marat Fudim
DAIC
March 6 — Marat Fudim
EP Lab Digest
March 6 — Marat Fudim and Richard Krasuski
Endovascular Today
Gradient Begins PreVail-PH2 Early Feasibility Study of Pulmonary Artery Denervation System
March 6 — DCRI & RACE-CARS
The Lexington Dispatch
Inspired by friend’s near-death experience, Davidson County man preaches CPR readiness
March 6 — Duke Health
Drug Discovery & Development
Anosmia to amyloidosis: nference’s AI is decoding healthcare data at scale
Duke Heart Pulse — March 3, 2024
Highlights of the week:
Bashore Selected for TBJ Lifetime Achievement Award
We are excited to share that Thomas Bashore, MD, professor of medicine in cardiology, has been chosen by the Triangle Business Journal (TBJ) as the recipient of their 2024 Health Care Leadership Lifetime Achievement Award.
Bashore was nominated for his decades of service to heart patients at Duke and his outstanding mentorship and skills as an educator. His clinical care specialty has been the care of patients with congenital heart disease. The improvement in both surgical and medical care of infants and children with congenital heart disease in the U.S. has resulted in more children surviving into adulthood and more adults living with adult congenital heart disease. Duke School of Medicine, specifically the division of cardiology, was one of the first programs in the country to recognize the lack of specialists in this area and was one of the first to begin training cardiology fellows in caring for patients with adult congenital heart disease. Bashore was the founder of this training program at Duke along with Duke pediatrician, Tim Garson, MD, in 1993.
Bashore also founded the valvular heart disease program at Duke and he is a co-founder of Duke Heart Center. His career has spanned more than fifty years – the last 40 of which he has spent promoting valvular and adult congenital heart disease clinical care and training. While doing so, he has cared for thousands of patients — helping many of them survive into adulthood and go on to have children of their own.
During his career at Duke, he served as director of the Diagnostic Cardiac Catheterization Laboratories for 10 years, and then as the Director of the Cardiology Fellowship Training Program for 12 years. He has been a member and/or chairman of numerous committees of the American College of Cardiology over the years and is the author of more than 300 manuscripts, over 100 book chapters and reviews, and three books. He has helped train hundreds of cardiologists through his work at Duke, and his mentoring has led many of his trainees into academic teaching careers.
Bashore has been recognized locally and nationally for his clinical care of patients with congenital heart disease and, as a result, he has been the recipient of numerous teaching awards throughout his career. He has been recognized by the Duke University School of Medicine for his skill as an educator with a Master Clinician/Teacher Award (2006); the Leonard Palumbo Jr. Faculty Achievement Award (2014) for clinical care and teaching, as well as a Duke Medical Center Alumni Distinguished Faculty Award (2015). Dr. Bashore has received major national teaching and clinical care awards as well. The American College of Cardiology selected him for its annual Distinguished Teacher Award in 2018, while the American Heart Association awarded him its Laennec Master Clinician Award in 2019.
For the last 40 years, Bashore has been voted into the nation’s Best Doctors and America’s Top Doctors programs where he has consistently been listed among the top 1-5% in the field of cardiology. On a national level, he has continued his commitment to patient care and to educating future clinicians by serving on multiple educational committees, teaching national cardiology board review courses for the Society of Cardiovascular Intervention and the American College of Cardiology (ACC); and he has served as an editor, chairman, or associate editor of many of the ACC self-assessment books and lifelong learning programs, as well as on question-writing committees and assisting with the ACC website educational effort.
The Valvular Disease Program and Adult Congenital Program at Duke are now nationally recognized and Duke continues to serve as a leader in treating complex congenital heart problems — much of this due to Bashore’s commitment and vision.
Bashore and other awardees will be honored by the TBJ at their upcoming awards dinner in April.
Congratulations, Tom – this is very well deserved!
Duke Becomes 1st Enroller for PreVail-PH2 Study
Congratulations to Marat Fudim, Richard Krasuski, Rose Burns, and Khalia Stewart and their team on becoming the first enrolling site for an important clinical trial being conducted through the Duke Early Phase Clinical Research Unit (DEPRU).

Duke has become the first enroller for the Pulmonary Artery DenerVation Clinical Study Using the Gradient Denervation System in Heart Failure Patients with Pulmonary Hypertension Group 2 (PreVail-PH2 Study), an early feasibility, device study enrolling heart failure patients with pulmonary hypertension (PH).
Given the association with higher morbidity and mortality as well as the prevalence of the disease, there is a significant unmet need to develop effective therapeutics for this population as well as reason to explore non-pharmacologic options to effectively reduce PH in patients with heart failure with preserved ejection fraction (HFpEF). The Gradient Denervation System, which is being studied, is indicated for pulmonary artery denervation treatment in these patients and is intended to ablate nerves within the pulmonary artery using ultrasonic ablation. The study will enroll approximately 30 patients and is expected to be conducted across eight recruitment sites.
Gearing up for the first enrollment and first procedure day has not been a light lift and has taken significant investigator involvement as well as all-star coordinator efforts, according to Fudim, study PI. Krasuski serves as co-investigator; Burns is the lead CRNC, and Stewart is CRC for PreVail-PH2.
The investigators are grateful to the entire CRU team and appreciate their commitment to not only ensuring Duke is taking part in important research but also helping the team stand out as top performers and site leaders in the trials we choose to undertake. They want to thank the groups that support the team, especially their specific representatives who helped facilitate the team’s success by helping expedite study set-up requirements, including Diane Bresch of DOCR, Ashley Madison of ORC, Stephanie Minter with DOCR start-up, Helen Bran with the Cath lab, and Aubrie Coburn with CDU. The team is particularly proud of becoming the first enroller just three weeks following site activation.
Congratulations to all – great teamwork!
Heart Transplant Team Recognized During Duke MBB Game
We are thrilled to share that our amazing advanced heart failure and heart transplant team was recognized on the court during a break in play in the Duke vs. Virginia men’s basketball game last night (March 2).

Members of the team were brought onto the court during the second half and recognized for their recent team milestones, contributions to the field of transplantation, and overall excellence in the care of heart transplant patients.
You can read more about the complex care our cardiothoracic transplant program provides in Duke Cardiothoracic Transplant Program Accepts the Most Complex Cases, a recent article for referring providers.
Congratulations!
Krasuski & ACHA In DC
Cardiologist Rich Krasuski had a busy day in Washington on Thursday. Krasuski was at the Capitol with the Adult Congenital Heart Association (ACHA) discussing the work they do and the importance of supporting the Congenital Heart Futures Reauthorization Act, legislation that would extend funding for public health efforts at the Centers for Disease Control and Prevention to improve childhood survival rates, prevent premature death and disability, and increase quality of life for the 2.5 million Americans living with congenital heart disease. This is an important piece of legislation for the future of ACHD.

Krasuski and the team met with Senator Dick Durbin in his office. Left to right: Mark Roeder, CEO of the ACHA; Richard Krasuski, MD; Senator Durbin; Aliza Marlin; Scott Leezer, vice president of Government Relations at CURA Strategies, and Jim Rumple, Chair of the Board of Directors of the ACHA.
Great job, Rich!
ICYMI: Swaminathan Recognized for Advocacy

Madhav Swaminathan, MD, a professor of anesthesiology at Duke specializing in cardiothoracic anesthesiology and critical care medicine, was recently highlighted for his DEI and advocacy work with Duke’s Neurodiversity Initiative Working Group. If you happened to miss the post by Duke School of Medicine last week, it is certainly worth checking out.
Keep up the great work, Madhav!
Please Vote in USNWR Best Hospitals for Cardiology & Heart Surgery
USNWR voting for Best Hospitals by specialty is now open in Doximity. If you are board-certified in the U.S. and have claimed your Doximity profile already, please log into your account by March 27 to complete the brief survey: submit your nominations.
New to Doximity? Find and register your profile to vote. Just go to Doximity’s login page, scroll to the bottom and click on “find your profile” – find yours and claim it/register. You can participate in the survey as long as you register on Doximity prior to the survey closing on March 27.
The survey allows you to list up to five hospitals as Best Hospital in the specialty in which you are board-certified. Your ballot counts even if you vote only for one hospital.
As with primaries and national elections, every vote is important!
Support Frazier-Mills, Duke Health’s 2024 AHA Woman of Impact!
Please join us in supporting electrophysiologist Camille Frazier-Mills, MD, one of the Triangle American Heart Association’s Women of Impact in her campaign to raise funds to support Go Red for Women.

Frazier-Mills is representing Duke Health as a Woman of Impact in the 2024 campaign and we want to help her reach her campaign goal. By donating, each of us can support her campaign and help ensure more women have equitable access to cardiovascular care and better representation in critically needed medical research.
** Check out Camille Frazier-Mills’ campaign page and please donate by April 4. **
Every year across the country, a select group of individuals are nominated to be a part of Woman of Impact because of their passion and drive to make a difference. This 9-week blind competition is relentlessly focused on women’s heart health. The campaign launched on National Wear Red Day (Feb. 2) and closes on April 4. During this time, the nominees work to build campaign plans, recruit Impact teams, and inspire their networks to support the American Heart Association’s lifesaving mission.
At the end of the campaign, this special group of changemakers will be celebrated for the overall impact they have on the AHA’s mission and the Triangle community. The nominee who makes the greatest impact and raises the most funds locally will be named a local 2024 Woman of Impact Winner.
Additionally, the nominee who makes the greatest impact nationwide will be named the American Heart Association 2024 National Woman of Impact Winner.
Let’s help her reach and exceed her goal – let’s help her WIN! Go, Camille!
New CFO announced for DUHS
Lisa M. Goodlett, CPA, MBA, FACHE will join Duke as Senior Vice President, Chief Financial Officer, and Treasurer for Duke University Health System, effective March 4, 2024. Lisa will work closely with leaders across the health system to develop and implement financial, operations, and growth strategies. She joins DUHS from the Medical University of South Carolina where she served as system CFO.
Great Catch Brittenham!
 Congratulations to Kida Brittenham of Duke Heart’s 7 West team — Kida noticed a sudden change in the amount and character of a patient’s drainage in a negative pressure wound therapy suction canister. She immediately escalated her concern to the provider team and continued to advocate for the patient. The provider discovered an aortic leak, and the patient was taken emergently to the OR and received life-saving care.
Congratulations to Kida Brittenham of Duke Heart’s 7 West team — Kida noticed a sudden change in the amount and character of a patient’s drainage in a negative pressure wound therapy suction canister. She immediately escalated her concern to the provider team and continued to advocate for the patient. The provider discovered an aortic leak, and the patient was taken emergently to the OR and received life-saving care.
Way to go, Kida – thank you for your dedication to safe care for our patients!
DUHS Moves to Tier 1 Visitation Status, Tues. March 5
After consulting with Infectious Disease and Infection Prevention experts and closely monitoring respiratory illness in our community, DUHS will move to Tier 1 visitation status on Tuesday, March 5.
Visitation highlights:
- Hospital visiting hours: 8 a.m. – 9 p.m. daily.
- Up to four visitors at a time where space permits; switching is allowed.
- Visitors of all ages are allowed in inpatient, maternity, and ambulatory spaces.
- Visitors must be 18+ in perioperative/surgical/procedural areas.
Note: Additional visitation and masking precautions may apply to certain patient populations.
Exceptions to visitation restrictions may be granted based on special circumstances.
To keep everyone healthy, please remember to practice safe behaviors, including frequent hand hygiene and the proper use of PPE. Please do not come to work if you are sick. More information is available on Duke Health Now.
Adam Silver Elected Chair, Duke University BOT
 Duke alumnus and NBA Commissioner Adam Silver will serve as chair of Duke University Board of Trustees for a three-year term starting July 1, succeeding Laurene Sperling. Silver, who currently serves as vice chair, was elected to the post by the Board of Trustees at its recent quarterly meeting.
Duke alumnus and NBA Commissioner Adam Silver will serve as chair of Duke University Board of Trustees for a three-year term starting July 1, succeeding Laurene Sperling. Silver, who currently serves as vice chair, was elected to the post by the Board of Trustees at its recent quarterly meeting.
Reminder: NC Primary/”Super Tuesday” is March 5
The NC Primary is Tuesday, March 5. To find your polling place, you can click here.
Additional information on voting and voter ID requirements can be found on the Duke Votes website.
Upcoming Events & Opportunities
- Friday, March 8 is International Women’s Day
- March is National Nutrition Month
- USNWR Best Hospitals Voting is open (through March 27). Please check your Doximity account and vote!
Cardiology Grand Rounds
March 5: No CGR today.
March 12: Arrhythmias in Myocardial Infarction: Beyond the Substrate with Ching Zhu, MD. 5 p.m., DN 2002 or via Zoom.
March 19: Beyond the Bump: Navigating the Interplay of Cardiovascular Health and Obstetrics in the Modern Era with Sarah Snow, MD. 5 p.m., DN 2002 or via Zoom.
March 26: Topic TBD with Brittany Zwischenberger, MD. 5 p.m., DN 2002 or via Zoom.
All Duke Cardiology Grand Rounds recordings are housed on Warpwire. To access recordings please visit:
NET ID and password required. Enjoy!
CD Fellows Core Curriculum Conference
March 6: EP Case Presentation with Sara Coles and Jonathan Hanna. Noon. DMP 2W96 (in-person only).
March 8: Pregnancy & Heart Disease with Cary Ward. Noon, DMP 2W96 (in-person only).
Upcoming CME Symposia
March 8: Cardio-Oncology/Amyloid Symposium
The Southeastern Cardio-Oncology Conference, The Future is Now will take place on March 8 at the JB Duke Hotel in Durham, NC. Event registration is open; the registration deadline is March 5.
Duke cardiologists Michel Khouri and Ravi Karra of Duke’s Precision Cardiomyopathy Program will be presenters during the symposium.
Keynote to be provided by Avirup Guha, director of cardio-oncology and assistant professor of medicine at Augusta University’s Georgia Cancer Center.
The symposium is presented by Duke Cancer Network (DCN) in collaboration with Duke Cancer Institute. For more information, please contact Beth Tanner of DCN.
April 12: Duke Sports Cardiology & Sudden Death in Athletes
May 4: Duke Heart Failure Symposium
Registration is not yet open for the April 12 or May 4 symposia, but if you have questions about either event, please reach out to Christy Darnell.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
February 24 — Joseph Turek and the Monroe family
Spectrum News Carolina
North Carolina toddler alive today thanks to a first-of-its-kind procedure
*clip begins @ 15:34:11
February 25 — Taylor Stephenson (lung transplant patient)
WNCN Raleigh
Lifesaving surgery at Duke Hospital gives a young woman a new chance at a better life
*clip begins @ 08:16:30
February 25 — John Reynolds and Taylor Stephenson
WRAL Raleigh
A new lease on life after a woman’s 3rd double-lung transplant
*clip begins @ 06:15:40
February 26 — Carmelo Milano and Krish Dewan
tctMD
Infective Endocarditis in Opioid Users: Care Must Go Beyond the Heart
February 27 — Stephen Greene
Managed Healthcare Executive
Exploring Advances and Challenges in Heart Failure with Stephen Greene of Duke Heart Center
February 28 — Kevin Oeffinger (family medicine & community health)
Diagnostic and Interventional Cardiology
February 28 – Duke University Hospital
Becker’s Hospital Review
43 US hospitals among world’s best: Newsweek
February 29 — Manesh Patel
WRAL
Cardiovascular issues play large role in Black maternal mortality
March 1 — Audrey Blewer (family medicine & community health)
Healio/Cardiology Today
Women with public cardiac arrest less likely than men to receive CPR
March issue — Duke Hospitals (all)
Business North Carolina
Duke Heart Pulse — February 25, 2024
Highlights of the week:
Heart Team Implants 1500th Durable VAD
 Congratulations to our Duke Ventricular Assist Device (VAD) Program for reaching a program milestone: a total of 1500 durable VAD implants have been completed at Duke University Hospital (DUH) as of this past week. The first durable VAD placed at DUH occurred in 1994.
Congratulations to our Duke Ventricular Assist Device (VAD) Program for reaching a program milestone: a total of 1500 durable VAD implants have been completed at Duke University Hospital (DUH) as of this past week. The first durable VAD placed at DUH occurred in 1994.
“Achieving 1500 VAD implants is a testament to the unwavering dedication, clinical expertise, and commitment of each member of our multidisciplinary team and the community partners who identify patients that may benefit from this therapy, said Carmelo A. Milano, Joseph W. and Dorothy W. Beard Distinguished Professor of Experimental Surgery and division chief of cardiovascular and thoracic surgery at Duke Health in a statement to team members.
“As one of the first VAD centers certified by The Joint Commission, we are proud of the high standards and quality care provided to each VAD patient at Duke,” Milano adds. “Each implant represents a life impacted and a step forward in delivering comprehensive advanced heart failure care to the patients of our region.”
VADs are durable mechanical circulatory support devices used in patients who have reached end-stage heart failure. They are mechanical pumps that help a patient’s failing heart continue to pump blood through their body. Some patients receive a VAD as a “bridge-to-transplant” therapy while waiting for a heart transplant; others receive VADs as “destination therapy” — long-term placement without receiving a heart transplant. Early VADs were devices that were solely meant to keep people alive in a hospital until a donor heart could be found for them. Now, the devices have improved so much that many patients can not only leave the hospital but potentially live on VAD support for the rest of their lives.
“When this technology became available, we were fully in it from the beginning because we saw a much-needed gap in available treatments,” says Laura Blue, DNP, nurse practitioner and Duke’s lead VAD coordinator since 2003. “We had the resources and the desire to help more patients and it has been awesome to see people get chunks of their life back. To see them have more time to meet their dreams and have their lives improved. Giving people the ability to complete things they want to do and have more time with their families and accomplish goals has been the best part of this process.”
Milano attributes our VAD success to the many people who have been part of the VAD team over the years, especially those who led the way at the very beginning, including thoracic surgeons Peter van Trigt, MD (now at Moses Cone) and Kevin Landolfo, MD (now at Mayo Jacksonville). The entire current team has great synergy and drive and Milano attributes a lot of that to the two surgeons who are currently driving the VAD program – Jacob Schroder, MD, and Jeffrey Keenan, MD, and cardiology partners including Stu Russell, MD, and lead VAD coordinator Laura Blue, who, he says, has probably put more time into the VAD program than anyone.
VAD technology has evolved from large pulsatile devices to smaller rotary flow pumps over the years and Duke has been a leading site for clinical research in the development of many of the devices. Duke was the leading enroller for the HeartMate II LVAD clinical trial, the HVAD HeartWare clinical trial, and the MOMENTUM HeartMate 3 clinical trials, according to Milano.
“These three devices are probably the most common VADs we’ve used in reaching this 1500th milestone,” said Milano. “And we were leaders in the clinical trials that led to the FDA approval of those devices.”
Stu Russell, MD, Duke’s regional director for advanced heart failure agrees. “If you look back over the years at the kinds of pumps that have been studied, that led us to the ones we’re using today, Duke has been one of the highest enrollers in all of the clinical trials. Our patients have helped pave the way for VADs getting better and better over time.”
Russell says physicians are seeing fewer strokes occurring with VADs and less clotting – that the pumps have gotten better, and smaller, the batteries last longer, and the devices are more reliable than ever.
“Heart failure is the number one discharge diagnosis in most hospitals in America,” Russell says. “It’s everywhere and here in the south, with the rates of hypertension and coronary disease, there is even more of it. There are a ton of people developing and a lot of people dying of heart failure every year. As good as we’ve done and as high a number of VADs as we have implanted — it’s just a drop in the bucket compared to how many more people could probably benefit.”
The team sees reaching this milestone as an accomplishment that goes beyond Duke. They stress the partnerships with referring physicians across the region who choose to send their patients for an evaluation at Duke.
Regionally, the southeast has a very high prevalence of heart failure — higher than anywhere else in the United States,” says Stephanie Barnes, MSN, AGNP, CHFN, clinical director for Advanced Heart Failure at Duke. “Based on our transplant and durable VAD volumes combined, while they’re high and we are leading the way in providing advanced heart failure care to patients, we anticipate there are many patients out there who are not receiving these therapies, simply because they’re not making it to the door of advanced heart failure centers, or they’re making it too late.”
Duke’s durable VAD program has developed alongside its heart failure program, which reached a program milestone of 2000 completed heart transplants in December. The team hit a program and U.S. record of 161 heart transplants completed in 2023.
“Advanced heart failure patients are some of the most severely ill patients we see as cardiologists,” says Chetan Patel, MD, Duke Heart’s Vice Chief for Outreach and Network Development. “Not many heart centers can say they have achieved such a milestone and it’s due to the work of an amazing team over the years.”
We are so proud of this team and the thousands of lives they’ve touched. Congratulations!
Support Frazier-Mills, Duke Health’s 2024 AHA Woman of Impact!

Please join us in supporting electrophysiologist Camille Frazier-Mills, MD, one of the Triangle American Heart Association’s Women of Impact in her campaign to raise funds to support Go Red for Women.
Frazier-Mills is representing Duke Health as a Woman of Impact in the 2024 campaign and we want to help her reach her campaign goal. By donating, each of us can support her campaign and help ensure more women have equitable access to cardiovascular care and better representation in critically needed medical research.
Check out Camille Frazier-Mills’ campaign page and please donate by April 4.
Every year across the country, a select group of individuals are nominated to be a part of Woman of Impact because of their passion and drive to make a difference. This 9-week blind competition is relentlessly focused on women’s heart health. The campaign launched on National Wear Red Day (Feb. 2) and closes on April 4. During this time, the nominees work to build campaign plans, recruit Impact teams, and inspire their networks to support the American Heart Association’s lifesaving mission.
At the end of the campaign, this special group of changemakers will be celebrated for the overall impact they have on the AHA’s mission and the Triangle community. The nominee who makes the greatest impact and raises the most funds locally will be named a local 2024 Woman of Impact Winner.
Additionally, the nominee who makes the greatest impact nationwide will be named the American Heart Association 2024 National Woman of Impact Winner.
Let’s help her reach and exceed her goal – let’s help her WIN! Go, Camille!
Rymer Accepted to ACC Emerging Faculty Leadership Academy

Congratulations to Jenn Rymer, MD, assistant professor of medicine in cardiology! We learned this week that she has been accepted into the 2024 American College of Cardiology (ACC) Rick Nishimura, MD, MACC and Patrick T. O’Gara, MD, MACC Emerging Faculty Leadership Academy.
Established in 2005, the ACC Emerging Faculty Leadership Academy supports early-career academic cardiologists who strive to become clinician educators. Participants learn evidence-based teaching strategies and core skills along with other members of their cohort at Heart House in Washington, DC.
Duke cardiologists recently selected for this highly competitive opportunity include Nishant Shah (2023), Tony Gutierrez, MD (2022), and Adam DeVore, MD (2019).
Congratulations, Jenn! We are so excited for you!
USNWR Best Hospitals Voting Now Open
USNWR voting for Best Hospitals by specialty is now open in Doximity. If you are board-certified in the U.S. and have claimed your Doximity profile already, please log into your account by March 27 to complete the brief survey: submit your nominations.
New to Doximity? Find and register your profile to vote. Just go to Doximity’s login page, scroll to the bottom and click on “find your profile” – find yours and claim it/register. You can participate in the survey as long as you register on Doximity prior to the survey closing on March 27.
The survey allows you to list up to five hospitals as Best Hospital in the specialty in which you are board-certified. Your ballot counts even if you vote only for one hospital.
As with primaries and national elections, every vote is important!
Seriously, stop reading and go vote for Duke University Hospital — best of the best for cardiology and heart surgery! We’ll be here when you’re done – there’s more news below!
Armed and Dangerous Drills, Feb. 26-29
Jonathan Bae, MD, CPPS, Chief Quality Officer for Duke University Hospital, announced last week that Duke University Hospital will conduct Armed and Dangerous Drills this coming week (Feb. 26th – 29th). The drills will be discussion-based with the goal of reinforcing education and encouraging preparedness conversations with your teams.
Trained facilitators will present a scenario and questions for participants to think through as well as verbalize what they would do. Throughout the week there will be sessions conducted in-person on units at various times. Before each session, facilitators will round and gather any staff who are available. If you are available during a session in one of your work areas, you are welcome to participate in that session.
We understand that participation in on-unit sessions can be challenging for physician teams, so Zoom options are also available. If this works better for your schedule, please register for a time below:
- Tuesday, Feb. 27th at 7 a.m. — Click here to register for this time
- Tuesday, Feb. 27th at 12 p.m. — Click here to register for this time
- Wednesday, Feb. 28th at 5 p.m. — Click here to register for this time
- Thursday, Feb. 29th at 7 a.m. — Click here to register for this time
- Thursday, Feb. 29th at 12 p.m. — Click here to register for this time
- Thursday, Feb. 29th at 5 p.m. — Click here to register for this time
All sessions will last approximately 30 minutes. While we aim to provide accessible opportunities, with a drill of this scale, we will not be able to incorporate everyone. If you are unable to participate we do encourage refreshing your knowledge via the virtual Armed and Dangerous Training available online via LMS Course Number 00073596.
If you have questions about the drills, please email workplaceviolenceprevention@duke.edu.
Please take some time this week to refresh your preparedness and/or participate in any session for which you’re available.
Feb. 27: Before They Were Stars Series – Perspectives from Dean Mary Klotman
 We know this is a busy week, but… here’s a great event to consider: the Program for Women in Internal Medicine (PWIM) continues the popular Before They Were Stars series, now open to ALL in the Department of Medicine. This series highlights the career paths of prominent women physicians, capturing the successes, challenges and opportunities facing women in medicine.
We know this is a busy week, but… here’s a great event to consider: the Program for Women in Internal Medicine (PWIM) continues the popular Before They Were Stars series, now open to ALL in the Department of Medicine. This series highlights the career paths of prominent women physicians, capturing the successes, challenges and opportunities facing women in medicine.
This month PWIM is joined by Dean Mary Klotman! Dean Klotman will describe her career journey in academic leadership through her roles as Chair of Medicine and now as Dean of the School of Medicine.
All faculty and trainees are welcome and encouraged to attend. There will be food and beverages provided outside of the meeting venue beginning at 6 p.m. Conversation with Dean Klotman will start promptly at 6:30 p.m. on Tuesday, Feb. 27 in Duke Hospital North 2002.
Please join if your schedule permits. We’d love a great showing from Duke Cardiology if you can stay – this event immediately follows CGR in DN 2002!
NC Primary is March 5; Early Voting Ends March 2
Early voting for the March 5 Primary Elections is open through 3 p.m. on Saturday, March 2.
Duke University has an early voting location on campus at Karsh Alumni and Visitors Center. During the early voting period, voters can cast their ballot at any early voting location in the county where they are registered. Other early voting locations across NC can be found here. Voters who missed the registration deadline last week can also register and vote on the same day at early voting locations.
On Election Day, Tuesday, March 5, voters must cast a ballot at their assigned polling location.
Additional information on registering to vote, voting, and voter ID requirements can be found on the Duke Votes website.
Upcoming Events & Opportunities
- February is Heart Month and Black History Month.
- March is National Nutrition Month
- March 8 is International Women’s Day
- USNWR Best Hospitals Voting is open (through March 27). Please check your Doximity account and vote!
Cardiology Grand Rounds
Feb. 27: CTEPH…The Challenges We Face with William Auger, MD. 5 p.m., DN 2002 or via Zoom.
March 12: Arrhythmias in Myocardial Infarction: Beyond the Substrate with Ching Zhu, MD. 5 p.m., DN 2002 or via Zoom.
March 19: Beyond the Bump: Navigating the Interplay of Cardiovascular Health and Obstetrics in the Modern Era with Sarah Snow, MD. 5 p.m., DN 2002 or via Zoom.
March 26: Topic TBD with Brittany Zwischenberger, MD. 5 p.m., DN 2002 or via Zoom.
All Duke Cardiology Grand Rounds recordings are housed on Warpwire. To access recordings please visit:
NET ID and password required. Enjoy!
CD Fellows Core Curriculum Conference
Feb. 28: HF/Txp Case Presentation with Seamus Hughes. Noon. DMP 2W96 (in-person only).
March 1: EKG Review with Neil Freedman. Noon. Zoom only.
Upcoming CME Symposia for Spring, 2024
March 8: Cardio-Oncology/Amyloid Symposium
The Southeastern Cardio-Oncology Conference, The Future is Now will take place on March 8 at the JB Duke Hotel in Durham, NC. Event registration is open; the registration deadline is March 5.
Duke cardiologists Michel Khouri and Ravi Karra of Duke’s Precision Cardiomyopathy Program will be presenters during the symposium.
Keynote to be provided by Avirup Guha, director of cardio-oncology and assistant professor of medicine at Augusta University’s Georgia Cancer Center.
The symposium is presented by Duke Cancer Network (DCN) in collaboration with Duke Cancer Institute. For more information, please contact Beth Tanner of DCN.
April 12: Duke Sports Cardiology & Sudden Death in Athletes
May 4: Duke Heart Failure Symposium
Registration is not yet open for the April 12 or May 4 symposia, but if you have questions about either event, please reach out to Christy Darnell.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
February 16 — Duke University Hospital/Health System
Becker’s Hospital Review
24 most reputable US academic medical centers
February 18 — Carmelo Milano and Jacob Schroder
Innovando News (Italy)*
Fifty million euros for the first Italian artificial heart
*mention is in photo caption
February 19 — Duke Health
Medical Economics
How to keep your patients happy: 6 steps to reduce long wait times and improve patient satisfaction
February 20 — Duke University (biomechanical engineering)
Healthcare-in-Europe.com
Should these pills go together? ML model predicts drug interactions
February 20 — Stephen Greene
Managed Healthcare Executive
Stephen Greene, MD, Gives Insight on the New Heart Failure Drug Sotagliflozin
February 20 — Christopher Granger
The Laurinburg Exchange
Scotland works to increase cardiac arrest survival rates
February 21 — Stephen Greene
HCP Live
Experts’ Perspectives: Top Issue Facing Cardiology in 2024
February 21 — John Reynolds and Taylor Stephenson (lung tx patient)
WRAL (NBC Raleigh)*
Woman recovering after receiving her third double-lung transplant at Duke Health
*carried also by WRAZ (Fox 50) & WILM (Wilmington, NC Channel 10)
February 21 — John Reynolds and Taylor Stephenson
WNCN (CBS17 Raleigh)
‘I don’t want to die yet’: Woman receives life-saving 3rd double lung transplant at Duke Hospital
February 22 — Jacob Klapper and Taylor Stephenson
New York Post
February 23 — Taylor Stephenson
People.com
Woman, 26, Recovers from 3rd Double Lung Transplant in 8 Years: ‘I Was Getting Another Chance’
Duke Heart Pulse — February 18, 2024
Highlights of the week:
Loring Receives Career Development Award

Congratulations to Duke electrophysiologist Zak Loring, MD, who has been awarded a Veterans Health Administration (VHA) VISN 6 Career Development Award (CDA) for his study Improving Disparities in Atrial Fibrillation Care Through Development of Machine Learning Risk Models. Loring’s research will implement an ECG-based machine learning model to identify high-risk Veterans in the rural community with atrial fibrillation.
Through early identification and timely delivery of advanced treatment strategies, such as catheter ablation, Loring aims to prevent the development of heart failure. J. Antonio Gutierrez, MD will serve as Loring’s primary mentor for this award.
VISN 6 is the VA’s Mid-Atlantic Health Care Network, one of 23 Veterans Integrated Service Networks of the Veterans Health Administration. VISN 6 is comprised of eight VA Medical Centers (including Durham VAMC) and 15 community-based outpatient clinics.
VA Section Chief, Raj Swaminathan, MD, noted that this project directly builds on work Loring is completing through a VA ADAPT COIN grant award.
Gutierrez also holds a full CDA award, so this represents two CDAs awarded to our faculty in the last three years!
Congrats, Zak!!
Pauly Begins as DUH President
Tomorrow, Feb. 19, we welcome Greg Pauly to his new role as president of Duke University Hospital. Pauly will also serve  as group president of Acute Care Services for Duke University Health System and as Duke University School of Medicine’s Vice Dean for Clinical and Academic Integration.
as group president of Acute Care Services for Duke University Health System and as Duke University School of Medicine’s Vice Dean for Clinical and Academic Integration.
In these roles, Pauly will provide oversight of the strategic direction, fiscal management, and program development for all acute care services across DUHS, including Duke University Hospital, Duke Regional Hospital, and Duke Raleigh Hospital campuses.
Pauly is joining Duke after serving as executive vice president and chief operating officer for Massachusetts General Hospital.
Please give him a warm welcome when you see him!
Jessica May Joins Heart Development Team
 Please join us in welcoming Jessica Baga May, a major gifts officer for Duke Health Development and Alumni Affairs (DHDAA), to our Duke Heart team! May is now serving as one of our primary team leads focused on increasing and managing philanthropic support of Duke Heart. May joined Duke Health’s development team in 2021; her transition to Duke Heart officially began on February 1.
Please join us in welcoming Jessica Baga May, a major gifts officer for Duke Health Development and Alumni Affairs (DHDAA), to our Duke Heart team! May is now serving as one of our primary team leads focused on increasing and managing philanthropic support of Duke Heart. May joined Duke Health’s development team in 2021; her transition to Duke Heart officially began on February 1.
May’s efforts while at Duke Health have focused on grateful patient fundraising within the Department of Surgery. She will continue to support several of those surgical areas but will expand her focus to include the Heart team.
May says she is excited to be part of our team and that she hopes to serve as an asset to building philanthropic support for the work we do. We asked her what she’d most like our faculty to know about grateful patient fundraising.
“One of the most important things for faculty to know specifically about grateful patient philanthropy is that it’s a relationship-building process. Part of a development officer’s role is establishing a rapport and a connection with our faculty partners, and identifying if and how each faculty member wants to be involved in the fundraising process.”
May says that her initial goal is to speak with members of the faculty, get to know them, and learn about the experiences they have had with philanthropy. She’ll answer any questions you have about the fundraising process and will look to understand how you prefer to be engaged over time.
“I am here to enable a process for those who want to be engaged with philanthropy, both on the donor side and the faculty side, in a way that is fully respectful of patient care as the top priority.
Before joining Duke, May served as Senior Development Officer for Leadership Gifts at Wellesley College in Wellesley, MA. She has also served as a major gifts officer at the Massachusetts Institute of Technology in Boston, and Vassar College in Poughkeepsie, NY. Although her professional experience is largely rooted in higher education, her background includes growing up as a child of a cardiologist. She says her father, a now-retired private practice interventionalist, taught her how to work an EKG machine and let her play with pacemaker models as a child.
We are excited to have Jessica working with us in Duke Heart. You can anticipate hearing from her as she starts reaching out to introduce herself to faculty members.
Welcome, Jessica!
Thank you, Residents & Fellows!
 Duke is celebrating Graduate Medical Education Week from Feb. 18-26, a time to recognize all our residents and fellows and those who work to lead and support these programs, including program directors, associate program directors, program coordinators, and all vice chairs of education. Enjoy the week!
Duke is celebrating Graduate Medical Education Week from Feb. 18-26, a time to recognize all our residents and fellows and those who work to lead and support these programs, including program directors, associate program directors, program coordinators, and all vice chairs of education. Enjoy the week!
Califf Recognized with Duke Centennial ‘Spotlight’
Duke alum and cardiologist Robert Califf, MD was highlighted this week in a ‘centennial spotlight’ as part of Duke University’s Duke 100 Centennial Celebration. To view the current FDA Commissioner’s spotlight and all those who will be recognized throughout the year, please visit the Duke 100 site.
Cardiac Surgical Innovations Highlighted in SOM’s Magnify
 This week’s feature story in Magnify, Duke School of Medicine’s online magazine, covers recent innovations in pediatric heart surgery for congenital heart defects including partial heart transplantation, “domino” transplants, and the recent heart-thymus co-transplant. Told through a series of interviews with Drs. Joe Turek, Doug Overbey, Louise Markert, and Allan Kirk, Saving More Babies Through Innovation in Pediatric Heart Surgery, looks at lives saved, the challenges of congenital surgery, and hope for the future.
This week’s feature story in Magnify, Duke School of Medicine’s online magazine, covers recent innovations in pediatric heart surgery for congenital heart defects including partial heart transplantation, “domino” transplants, and the recent heart-thymus co-transplant. Told through a series of interviews with Drs. Joe Turek, Doug Overbey, Louise Markert, and Allan Kirk, Saving More Babies Through Innovation in Pediatric Heart Surgery, looks at lives saved, the challenges of congenital surgery, and hope for the future.
ICYMI: Fuller Delivers Sanford Lectureship
Dr. Stephanie Fuller, the Thomas L. Spray Endowed Chair in Pediatric Heart Surgery at Perelman School of Medicine at the University of Pennsylvania delivered the Sanford Lectureship on Wed., February 14th as part of Duke Surgery Grand Rounds. A recording of her lecture, Congenital Heart Surgery: Outcomes, Innovation and Adults can be viewed in Duke Box.
She gave a terrific presentation – the recording is well worth watching.
Early Voting Begins for 2024 Primary Elections
Early voting for the March 5 Primary Elections is now open! The early voting period runs through Saturday, March 2. Duke University has an early voting location on campus at Karsh Alumni and Visitors Center. During the early voting period, voters can cast their ballot at any early voting location in the county where they are registered. Other early voting locations across NC can be found here. Voters who missed the registration deadline last week can also register and vote on the same day at early voting locations. On Election Day, voters must cast a ballot at their assigned polling location.
The primary elections in NC include candidates for President, Governor, all 170 members of the state legislature, 14 congressional seats, one NC Supreme Court seat, various judicial positions, and other Council of State positions including Lieutenant Governor, Attorney General, Commissioner of Agriculture, Superintendent of Public Instruction, Commissioner of Labor, Commissioner of Insurance, Secretary of State, State Treasurer, and State Auditor. Registered Democrats, Republicans, or Libertarians must vote their party’s primary ballot, but Unaffiliated voters can choose which party’s ballot to vote.
NC voters are now required to provide photo ID at the polls. A list of acceptable forms of ID can be found on the State Board of Elections website. Duke University students still have the opportunity to request a student voter ID card approved by the State Board of Elections last year. Additional information on registering to vote, voting, and voter ID requirements can be found on the Duke Votes website.
Upcoming Events & Opportunities
- February is Heart Month and Black History Month.
- It’s GME Week 18-26
Cardiology Grand Rounds
Feb. 20: Closing Arguments on the Management of Atrial Septal Defects with Richard Krasuski. 5 p.m., DN 2002 or via Zoom.
All Duke Cardiology Grand Rounds recordings are housed on Warpwire. To access recordings please visit:
NET ID and password required. Enjoy!
CD Fellows Core Curriculum Conference
Feb. 21: DHP Case Presentation with Eric Xie. Noon. DMP 2W96 (in-person only).
Feb. 23: TBD with TBD. Noon. Zoom only.
Virtual: AHA Hands-Only CPR Demonstration
For team members at Duke who are not required to have BLS certification, please consider participating in the upcoming virtual AHA Triangle Hands-Only CPR demonstration, being held at Noon on Feb. 22. To register please click here. You’ll then receive a confirmation with the Zoom link.
Help us reach 100+ participants from Duke Health!
Office of Faculty — Event with Israni of Stanford Medicine, Feb. 26
Academic Medicine, with all its complexities, naturally includes conflict amongst its crucial collaborators – trainees, faculty, staff, communities and more. 21st century leadership skills require all of us to strategically leverage components of this conflict for constructive change, with intentional and thoughtful actions. This talk will weave together themes from restorative justice and design thinking; and how they can be applied to artificial intelligence and JEDI (justice, equity, diversity, and inclusion), offering a case for new ways of leveraging conflict to advance a culture of connectedness and belonging. The featured speaker will be Sonoo Thadaney Israni of Stanford University’s Presence Center.
February 26: Leveraging Conflict for Constructive Change. 4-5:30 p.m., DN 2002. Presented by the Office for Faculty. Refreshments will follow. To learn more and register: https://duke.is/8/8d7f.
Upcoming CME Symposia for Spring, 2024
March 8: Cardio-Oncology/Amyloid Symposium
The Southeastern Cardio-Oncology Conference, The Future is Now will take place on March 8 at the JB Duke Hotel in Durham, NC. Event registration is open; the registration deadline is March 5.
Duke cardiologists Michel Khouri and Ravi Karra of Duke’s Precision Cardiomyopathy Program will be presenters during the symposium.
Keynote to be provided by Avirup Guha, director of cardio-oncology and assistant professor of medicine at Augusta University’s Georgia Cancer Center.
The symposium is presented by Duke Cancer Network (DCN) in collaboration with Duke Cancer Institute. For more information, please contact Beth Tanner of DCN.
April 12: Duke Sports Cardiology & Sudden Death in Athletes
May 4: Duke Heart Failure Symposium
Registration is not yet open for the April 12 or May 4 symposia, but if you have questions about either event, please reach out to Christy Darnell.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
February 10 — Duke University
Forbes
Top 20 Universities For NIH Funding; Johns Hopkins Ranks First Again
February 12 — Jen Weber (lung tx patient)
Bonnell Foundation Podcast
All things lung transplant with Jen Weber
February 12 — Elisabetta Politi (Lifestyle & Weight Management Center)
Everyday Health
Using a Salt Substitute Can Slash Risk of Developing High Blood Pressure
February 12 — Marat Fudim
tctMD
More Mortality Reduction Signals With Implantable Hemodynamic Monitors in HFrEF: Meta-analysis
February 13 — Reid Chamberlain
WFMY Greensboro (NC) – CBS News 2
Greensboro 8-year-old becomes first in the world to receive this heart surgery
February 15 — Gerald Bloomfield
NIH News/Fogarty International Center
Finding causes of heart failure in Western Kenya
Recent Comments