Duke Heart Week Ending September 27th 2020
Chief’s message: Living in the time of COVID, electronic communication, and bad days.
I got an email from a Faculty member who reported something about the day and discussed how frustrating an issue was. I instinctively, responded and said that they were working very hard and I would call them to discuss how to help. I got a response that made me pause … the faculty member stated they were just venting and more were sending the note more of as a colleague and friend, rather than the Chief of the Division. Aside from getting a better understanding, I sent a note reporting some of the challenges I had faced that day and thanked the colleague for reaching out.
The story stuck in my head as I realized the challenges we are all facing in our Health system, in our communities and schools with the transition to electronic and virtual communication. We have had a large move to Zoom meetings, Grand Rounds and seminars on the web, all of the Scientific Meetings changing to virtual attendance (TCT in October and American Heart Association in November). In this time, even with video on – it becomes difficult to get a sense of the human interactions that makes us laugh, feel, and rejoice with each other’s successes and work to help with obstacles. We are all yearning for some routine and stability, and sometimes just someone to share the bad days and things going on.
 The episode made me think of a favorite children’s book the we use to read to our kids, Alexander and the Terrible, Horrible, No Good, Very Bad Day. Maybe the book for 2020 – a terrible, horrible, no good, very bad year. Sometimes, like Alexander – we all just need someone to hear about all the things that have gone bad in the day. This is not something that can easily be accomplished electronically. So, I have tried and will continue to try to ensure we get some socially distanced interactions, phone calls, and even zooms where we can share our trials and tribulations, but also hopefully the numerous amazing accomplishments despite the obstacles. This Pulse, is often an effort to note those and be part of our fabric in celebrating our fellows, colleagues, and partners.
The episode made me think of a favorite children’s book the we use to read to our kids, Alexander and the Terrible, Horrible, No Good, Very Bad Day. Maybe the book for 2020 – a terrible, horrible, no good, very bad year. Sometimes, like Alexander – we all just need someone to hear about all the things that have gone bad in the day. This is not something that can easily be accomplished electronically. So, I have tried and will continue to try to ensure we get some socially distanced interactions, phone calls, and even zooms where we can share our trials and tribulations, but also hopefully the numerous amazing accomplishments despite the obstacles. This Pulse, is often an effort to note those and be part of our fabric in celebrating our fellows, colleagues, and partners.
And as Alexander’s Mother says in the book, “some days are like that … even in Australia”
I have copies in my office that I am willingly handing out to those with the worst days.
Highlights of the week:
Photo of the Week:
 Those of you on campus during the early morning, evening or overnight hours may have noticed this gesture of thanks emanating from the Hock Building out to care providers. We think it’s a particularly fitting tribute to our Duke Heart team members! Photo is courtesy of Eric McClenny, Nurse Manager Operations, DMP 7 East.
Those of you on campus during the early morning, evening or overnight hours may have noticed this gesture of thanks emanating from the Hock Building out to care providers. We think it’s a particularly fitting tribute to our Duke Heart team members! Photo is courtesy of Eric McClenny, Nurse Manager Operations, DMP 7 East.
Thank you to each and every team member in Duke Heart for being a part of our team and for doing all that you do for our patients, their loved ones and each other.
Note of Gratitude from Cynthia Pierce
Many of you will recall that in May, Cynthia Pierce’s daughter Sam died unexpectedly,  leaving behind three young children. A number of you stepped up to help support Cynthia through contributions to a GoFundMe account (established by Dr. Tom Bashore). Cynthia is a former cardiac catheterization lab nurse and a current Duke Heart TAVR coordinator. She sent us a note this week to share with you:
leaving behind three young children. A number of you stepped up to help support Cynthia through contributions to a GoFundMe account (established by Dr. Tom Bashore). Cynthia is a former cardiac catheterization lab nurse and a current Duke Heart TAVR coordinator. She sent us a note this week to share with you:
Hello to all of you:

It has taken me time to process the passing of my daughter Samantha. I also want you all to know that I have thought constantly of the overwhelming gifts and support given to me and my family especially during these uncertain times. I was able to have a loving and respectful service for Samantha. I will forever be grateful. Please know that I am proud to know and work along great people. A special thanks goes to Dr. Thomas Bashore and Dr. Kevin Harrison for their leadership in accomplishing this.
Thank you over and over!
Always,
Cynthia Pierce
Shout-out to Nishant Shah

We received a really nice note of gratitude this week from the daughter of a patient regarding care provided by Nishant Shah. The note reads:
“My mother and my father cannot speak more highly of Dr. Shah. He graciously saw my mother without question as an add-on to his clinic, after she was unable to be followed up with the hospital system where she was originally seen in the ED and was discharged home.
After my mother’s appointment with Dr. Shah today, he personally called my mother to give her the results of the labs and the ECHO that he graciously added on for my mother.
Often-times, patients and their families do not complement good care to those in leadership and only complain when they can find fault or have an experience when things are even slightly suboptimal. I hope this email finds it to the inbox of those who are able to spotlight the good-hearted nature of physicians.
From the wonderful report my parents gave of Dr. Shah, it is obvious that he is very happy to work for Duke and the PDC. Thank you for allowing this to be an environment where physicians are happy to provide service to the community.”
Nishant responded, “Very sweet family and honored to care for them. Thanks as well to the wonderful South Durham staff for the swift care coordination.”
Nicely done, Nishant and the South Durham Clinic team! We are so glad to have all of you on the Duke Heart team!
Transplant Team Publishes HIV+ Survival Findings
Congratulations to Julie Doberne, Oliver Jawitz, Vignesh Raman, Ben Bryner, Jacob Schroder and Carmelo Milano on their latest publication. In a pre-proof released last weekend in The Annals of Thoracic Surgery, the team has published results of a study looking at HIV positive heart transplant recipients and showed that their survival is comparable to HIV negative recipients. HIV positivity is classically considered a contraindication to listing for heart transplant, so these findings are important; this is the first study to show this result on this scale. To see the journal article, please visit: https://pubmed.ncbi.nlm.nih.gov/32946847.
Nicely done!
Respiratory Care Services Team Receives Statewide Recognition, Awards
We are pleased to announce that our Respiratory Care team recently presented a talk, Translating Literature to Bedside Practice, to the North Carolina Society for Respiratory Care (NCSRC) that was very well received. As a result, the team has been asked to speak in November and December to schools, the NC Board, and nationally for Respiratory Care Week. Presenters from our RCS team included Andrew Miller, Renee Bartle, Jhaymie Cappiello and Charlotte Reikofski; they were joined by fellow Dukies Dr. Dan Gilstrap (MICU Medical Director) and Angela Richardson (Wound Care).
Additionally, Charlotte Reikofski, Health System Director of Respiratory Care Services, has received the NCSRC’s 2020 Harvey Jacobs Leadership Award and Jhaymie Cappiello, Clinical Educator, has received the 2020 Gail Gane Educator of the Year Award.
This is wonderful news! Congratulations to Charlotte, Jhaymie and the entire RCS team! You’re doing outstanding work and it shows.



Abbott & Kurdelmeier Named Clinical Team Leads for 3100
The Duke Heart Leadership team is excited to announce Jessica “Jessie” Abbott and Megan Kurdelmeier as 3100 Clinical Team Leads. Jessie assumed her role on September 14th; Megan will assume her role on October 12th.
Jessie joined the 3100 team in March 2016. She earned her BSN from Duke University School of Nursing and also holds a BSN in health and physical education from Edinboro University. Jessie is currently a CN III and holds a PCCN certification. She has shown a strong interest in professional development by enrolling in a Master of Science in Nursing program and has served in charge nurse, preceptor, and skin care champion roles. She is also a member of the AACN.
Megan joined the 3100 team in August 2016. She earned her BSN from East Carolina University and also holds a BSN in nutrition sciences from North Carolina State University. Megan is currently a CN III and holds a PCCN certification. She is a highly engaged team member who has served in charge nurse, preceptor, and cardiac monitoring champion roles. Megan is also an environment of care super-user and an active member of the work culture committee. She is also a member of the AACN.
Please join us in congratulating Jessie and Megan in their new roles!
Shout-out to 7 East/Cardiothoracic Step-down Unit
On September 11th our 7 East team celebrated two years with NO Pressure Injuries! With utilizing the Dual Skin Assessment and collaborating with the WCON team and Angela Richardson, they were able to meet this amazing milestone, according to Amanda Rooney, Clinical Lead. “This shows the great dedication that the 7 East Team Members have to Quality Improvement and patient care,” she added.
Great job, 7 East!!!
Triangle AHA Seeking Testimonial Videos to Help Kick-Off Heart Walk
Our local American Heart Walk affiliate is seeking short, 30-second to 2-minute testimonial videos (shot with your cell phone) of why you support the annual Heart Walk. The videos will be used at the Heart Walk kick-off event on Friday, Oct. 9. The Heart Walk is Saturday, Oct. 10.
Dubbed “Because of You videos” your testimonial should include the following:
- Introduce yourself: Share your name, the company you work or organization you’re with
- Share your why: Are you or a family member a survivor? Talk about the experience.
- Share the outcome starting with “Because of you…”
Examples: “Because of you, my dad is celebrating more birthdays.” “Because of you, my daughter is growing up strong and brave.” “Because of you, I can walk my daughter down the aisle.”
If you have any questions, please contact Kimberly Burrows of the Triangle AHA, via email: Kimberly.burrows@heart.org. Video submissions are due by Thursday, October 1.
ICYMI:
Ashlee Davis, Richie Palma and Dave Adams have a newly published article – this time on AI. Check it out here: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7289098
Davis A, Billick K, Horton K, et al. Artificial Intelligence and Echocardiography: A Primer for Cardiac Sonographers. J Am Soc Echocardiogr. 2020;33(9):1061-1066. doi:10.1016/j.echo.2020.04.025
Duke-wide Effort Urges Everyone to Register and Vote
An estimated 50 million eligible voters in the United States are not registered to participate in this important privilege and duty.
 Duke has launched a University-wide effort to make it easy and convenient for everyone – faculty, staff and students – to register and to vote. The website vote.duke.edu is Duke’s online resource for how to register in North Carolina or other states, how to request an absentee ballot, and examples of ways you can get involved.
Duke has launched a University-wide effort to make it easy and convenient for everyone – faculty, staff and students – to register and to vote. The website vote.duke.edu is Duke’s online resource for how to register in North Carolina or other states, how to request an absentee ballot, and examples of ways you can get involved.
There will also be an early voting site on campus at the Karsh Alumni and Visitors Center, October 15-31. (If you have not yet visited the new Alumni Center, it’s really beautiful and worth checking out. Location: 2080 Duke University Rd, Durham, NC 27708)
You can also view the recording of a recent Duke Health leadership virtual town hall to learn more about Duke Health’s voter registration and turnout initiatives for the 2020 elections.
Important Reminders
- Please get your Flu Vaccination: All team members must get their vaccination or otherwise demonstrate policy compliance by Tuesday, Nov. 10. Details and resources all available on the Duke Health Influenza Resources site (NET ID required): https://influenza.dh.dukehealth.org.
- Zoom Update: In response to the appeals of Duke and the higher education community, Zoom will NOT enforce the mandatory security requirement originally scheduled for September 27.
- October is Medical Ultrasound Awareness Month (the month formerly known as sonography month). Please thank a sonographer!
Upcoming Opportunities/Save the Date:
Cardiology Grand Rounds
Sept. 22: ESC Wrap-Up and Overview with the Experts. Christopher Granger and Bernard Gersh of the Mayo Clinic, 5 – 6 p.m.
Sept. 29: Managing Pregnancy and Pulmonary Hypertension: A Multidisciplinary Approach to a High Risk Patient. Presenters: Terry Fortin, Sarah Goldstein, Chad Grotegut, Marie-Louise Meng and Cary Ward. 5 p.m. Virtual. Links available in Outlook invitation.
Oct. 6: The Robert J. Lefkowitz, MD, Distinguished Lecture. Presenter: Helen Hobbs, MD, investigator, Howard Hughes Medical Institute and professor, Internal Medicine and Molecular Genetics, UT Southwestern Medical Center. Noon – 1 p.m., part of Duke SOM Research Week. For more information, please visit: https://medschool.duke.edu/research/research-week.
Oct. 6: Special Cardiology Grand Rounds – A Tribute to Dr. Eric Peterson. 5 p.m. Virtual. Links available in Outlook invitation. Presenters:
- Matthew Roe, MD – Origins of CV Registries
- Sreek Vemulapalli, MD – Partnering with Professional Societies
- Jon Piccini, MD – Expanding the Scope: AF/Stroke Care
- Tracy Wang, MD – Implementation Science
- Neha Pagidipati – Possibilities in Prevention
- Ann Marie Navar, MD – Going Digital
- Eric Peterson, MD – The Future
Oct. 13: Michelle Kittleson, MD, PhD, of Cedars-Sinai.
Oct. 20: The Albert L. Williams Cardiovascular Genetics Lecture Series. Presenter: Wendy Chung, MD, PhD, of Columbia.
Oct. 27: Cardiology Faculty meeting
Nov. 10: TBA
Nov. 17: No CGR. AHA Scientific Sessions
Conferences, Symposia & Webinars
Sept. 21: Duke Orthopaedic and Rehab Seminar. 4:30 – 5:30 p.m. Guest speaker is Shane Phillips, PT, PhD, FAHA, Professor and Associate Head of PT and Senior Associate Dean for Clinical Affairs, College of Applied Health Sciences, University of Illinois-Chicago. His topic is Microvascular Function and Cardiac Rehabilitation: A Canary in the Coal Mine? Zoom seminar: https://duke.zoom.us/j/93436455711
Sept. 29: COVID-19 and the Telehealth Transformation, with Jedrek Wosik and Shijing Si. Noon – 1 p.m.
COVID-19 has led to the rapid adoption of telehealth strategies in order to maintain continuity of care. As compared to in-person visits, important changes in patient characteristics were seen in telephone and video visits as well as clinician ordering patterns. In addition, MyChart patient portal usage increased dramatically. We present select initial Duke clinic utilization data before and during COVID-19. To better understand the increasing number of unstructured MyChart messages, we apply both unsupervised and supervised machine learning tools to patient-generated messages. Specifically, 1) we utilize dynamic topic modeling to gain insight into message meaning and monthly trends for patients with (+) and (-) COVID and Flu results; 2) we leverage the state-of-the-art machine learning model (Bidirectional Encoder Representations from Transformers or BERT) to construct an automatic message triaging algorithm or classifier that outperforms other baseline methods.
Registration required to receive link and meeting information. To register, visit: https://training.oit.duke.edu/enroll/common/show/21/175250. This event is co-hosted by the Duke Center for Computational Thinking and Duke+DataScience.
Oct. 5 – 8: Research Week. Sponsored by Duke School of Medicine. Series will be held virtually, via Zoom: https://duke.zoom.us/j/92060873004. More information and a full agenda can be found here: https://medschool.duke.edu/research/research-week
Oct. 7: PROMISE trial webinar. Pam Douglas will lead an overview of the PROMISE trial cohort, and research plan, with insights and panel discussions. 4-6 p.m., To register for the Zoom link, please visit: https://duke.zoom.us/webinar/register/WN_wSz_1UcZRNy0cmqg8q6hgg. Sponsored by DCRI.
Nov. 13: 12th Annual NC Research Triangle Pulmonary Hypertension Symposium. Noon – 4:30 p.m. For more information, please visit this page. This event will be held virtually and is co-sponsored by Duke and the University of North Carolina in partnership with the Pulmonary Hypertension Association through the Building Medical Education in PH program. Please join us!
Nov. 13–17: AHA Scientific Sessions 2020, a virtual experience. Registration is now open. See the website for details.
COVID-19 Updates:
All the latest official DUHS information regarding coronavirus/COVID-19 response at the following locations:
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged.
Duke Heart in the News:
September 18 — Erich Huang (Duke Forge)
U.S. News & World Report
Why Colleges Are Offering Data Science Programs
https://bit.ly/33Uxl6w
September 22 — Michel Zeitouni and Ann Marie Navar
Healio/Cardiology Today
In high-risk younger patients, cholesterol guideline suitability questioned
https://bit.ly/33T5tQ0
September 23 — Robert Califf
STAT
Fast, low-cost testing is essential for averting a second wave of Covid-19
https://bit.ly/3kN57kN
Duke Heart Week ending September 20th 2020
Chief’s message: RBG and Resilience
I try not to interrupt my kids (13-year-old daughter and 15-year-old son) as they tell me about their day during dinner time. They go first so they get the most time, then my wife, and then me. This has become an even more important ritual during COVID-19 times and is one of the few things that we have fought hard to ensure we have time for. Given the stressful times for kids and parents, the ability to sit and hear the joys and struggles of each member of the family’s day has brought us even closer together if not sometimes led to other frustrations. It is with this backdrop that I was hesitant to interrupt my “daughter’s day” on Friday when I got the news at dinner that Ruth Bader Ginsburg has passed away. Both kids over the last two years for some reason had read the “Notorious RBG”, and shared with the parents her empowering statements, her writing through the night, the way she picked cases, and even making people like Bill Clinton cry. All politics aside, I knew she meant a lot to the country and she meant a lot to my children. So, I interrupted and said I had some bad news for the family to hear and told them that Ruth Bader Ginsburg had passed away surrounded by family and friends. Both kids, and my wife, and my daughter in particular were saddened and took a moment. We shared some of the impact and accomplishments, and unfortunately were worried that this would further divide an already polarized community and country. As we cleaned up and started to plan what we might do for a “fun” Friday night, my daughter and son both asked if they could go use their cell phones to text and discuss her death with friends. My wife started getting texts from her high school girlfriends. An hour later we settled into watching a series we have been watching on Netflix, and my kids described ways in which they and their friends will try to carry on the lessons and legacy of RBG.
I share the story as I was struck by how much the Duke Heart community has had challenges and similar responses in 2020. We have faced as a community and group, the COVID-19 pandemic, continued evidence of racial injustice and health inequity, and other innumerable challenges in the ways in which we care for our patients and each other. These have included at times, some of our most trusted colleagues and partners getting sick, operational struggles in care delivery and research, limitations in how we can share and discuss both clinical care and our ongoing “days” and lives, and in some instances our colleagues taking important roles at other institutions. Through all of this, we are blessed to have the Duke Heart community – the people that every day support and work to carry out the mission and legacy of our group to discovery and deliver better health. 2020 is not over by any stretch and we will all be challenged more as we work to improve the structure and manner in which we care for patients and conduct science. But, I remain encouraged by the resilience of you all who support and continue to push our collective desire to for clinical and research excellence forward.
A few quotes from Ruth Bader Ginsburg – known for her Resilience
“Fight for the things that you care about. But do it in a way that will lead others to join you.”
“Real change, enduring change, happens one step at a time.”
“I would like to be remembered as someone who used whatever talent she had to do her work to the very best of her ability.”
Highlights of the week:
Atwater Named Director, Cardiac Electrophysiology at Inova

We are excited to announce that Brett D. Atwater, Associate Professor of Medicine with Tenure in the Division of Cardiology will assume the role of Director of Cardiac Electrophysiology and Electrophysiology Research at the Inova Heart & Vascular Institute in Fairfax, VA, a position that is effective December 14, 2020.
Brett graduated from the Pritzker School of Medicine at the University of Chicago, completed his internal medicine training at Duke, and completed his cardiology training at the University of Wisconsin. He returned to Duke for his electrophysiology fellowship and joined the faculty in 2010. Brett has been dedicated to patient care, education, and research. He has many accomplishments during his time here at Duke. He has served as the Director of Electrophysiology at the Durham Veterans Administration Medical Center. He has also served as the Director of the EP Lab at Duke University Medical Center and led Duke’s Electrophysiology Services in Wake County. He has a great track record for helping to build and grow robust clinical programs. Moreover, through his leadership, he has also established new programs at Duke University Hospital, including the physiologic His pacing program and our clinical service line at Wake Med.
He is an internationally recognized clinical investigator in cardiac resynchronization therapy and electrocardiography and has co-authored more than 70 peer reviewed articles during his time at Duke. Recently, he performed the first in-man use of the His-Pro sheath for conduction system pacing lead implantation here at Duke. He has also served as a valuable teacher and mentor to many medical students, residents and fellows. He is leaving Duke to lead a talented EP section where he will work alongside several notable Duke alumni.
“This is a bittersweet moment for Duke EP,” said Jon Piccini, Duke’s director of Cardiac Electrophysiology. “While we will miss working with Dr. Atwater and learning from Dr. Atwater, we are extremely excited and thrilled so see him take on this important leadership opportunity in cardiac electrophysiology. Inova will be poised for exceptional success and innovation under his leadership.”
Atwater says he is especially grateful for the mentorship, partnership and friendship he has enjoyed with members of the Duke faculty and staff.
“I have thoroughly enjoyed all of the opportunities to work with the exceptional physicians, fellows, APPs, nurses and staff,” said Atwater. “Duke is and will remain a very special place because of the talented, caring people who choose to work here.”
Atwater and Piccini are both looking forward to opportunities to strengthen collaboration between Inova and Duke.
Congratulations, Brett – you will certainly be missed at Duke!
Bonadonna Named Chief Perfusionist, Effective Oct. 1
 Duke Heart is pleased to announce that Desiree Bonadonna has been named Chief Perfusionist for Duke Health. Bonadonna has led the Extracorporeal Membrane Oxygenation program (ECMO) at Duke for the last seven years, and most recently has served as the Director of Extracorporeal Life Support (ECLS) for Duke University Hospital and Duke University Health System. In her director role, she coordinated medical center resources to efficiently deliver high quality respiratory and cardiac extracorporeal support — neonatal through adult — throughout the health system and our referral network.
Duke Heart is pleased to announce that Desiree Bonadonna has been named Chief Perfusionist for Duke Health. Bonadonna has led the Extracorporeal Membrane Oxygenation program (ECMO) at Duke for the last seven years, and most recently has served as the Director of Extracorporeal Life Support (ECLS) for Duke University Hospital and Duke University Health System. In her director role, she coordinated medical center resources to efficiently deliver high quality respiratory and cardiac extracorporeal support — neonatal through adult — throughout the health system and our referral network.
She has provided clinical expertise and oversight of patient care for more than 250 ECLS cases per year and managed ECLS continuing education and care delivery training for 40 ECMO specialists and 34 perfusionists, as well as multidisciplinary teams serving four intensive care units, the operating rooms, and emergency services. She has built and maintained the relationships necessary to conceive and establish an inter-hospital ECMO transport program inclusive of ground, rotor, and fixed wing aircraft, which have supported more than 100 inter-hospital ECLS transports annually. Her collaborations with internal data and quality experts have allowed us to better benchmark outcomes, as well as identify and implement performance improvement and research opportunities, all of which have led to quality improvements.
Under her leadership, the ECMO Program has received an ELSO Award for Excellence in Extracorporeal Life Support and she will continue to support the ECLS program in her Chief of Perfusion role.
We welcomed Bonadonna to the Duke team in 2007 when she started as a perfusionist; she maintains clinical competence in both pediatric and adult cardiothoracic surgery and is actively involved in multiple perfusion societies, including the American Academy of Cardiovascular Perfusion, to which she was nominated as a Fellow earlier this year. She is widely published in the perfusion and ECMO literature, and has been an invited speaker regionally, nationally, and internationally.
Bonadonna earned a Bachelor of Science in Engineering from the University of Pittsburgh; she holds a Certificate in Cardiovascular Perfusion from the Center for Allied Health at Cooper University Health Care, and a Master of Perfusion Science degree from University of Nebraska Medical Center.
Congratulations, Desiree! We are very excited for you and for our Perfusion program!
Shout-Out to Wofford!
 Brian Wofford, vice president of heart operations for Durham County, recently had the opportunity to plan and organize a special event featuring Ibram X. Kendi, author of How to be an Antiracist and director of the Center for Antiracist Research at Boston University.
Brian Wofford, vice president of heart operations for Durham County, recently had the opportunity to plan and organize a special event featuring Ibram X. Kendi, author of How to be an Antiracist and director of the Center for Antiracist Research at Boston University.
The event, A Conversation with Professor Ibram X. Kendi, was held Sept. 16 during the General Session of the National Association of Health Services Executives (NAHSE) 2020 Virtual Educational Conference, which Wofford co-chaired. NAHSE is a non-profit association of Black health care executives founded in 1968 for the purpose of promoting the advancement and development of Black health care leaders, and elevating the quality of health care services rendered to minority and underserved communities. (Fabian Stone, associate vice president of revenue cycle and health information management at DUHS, currently serves as President of NAHSE. Rhonda Brandon, chief human resources officer and senior vice president for the Duke University Health System, and Adia Ross, chief medical officer for Duke Regional Hospital also spoke at the event.)
Way to represent Duke Health and Duke Heart, Brian! Thank you for the work you are doing to support Duke Heart as well as the Moments to Movement initiative at Duke. To read more about Duke’s ties to NAHSE and our sponsored event with Kendi, please visit the Inside Duke Health story.
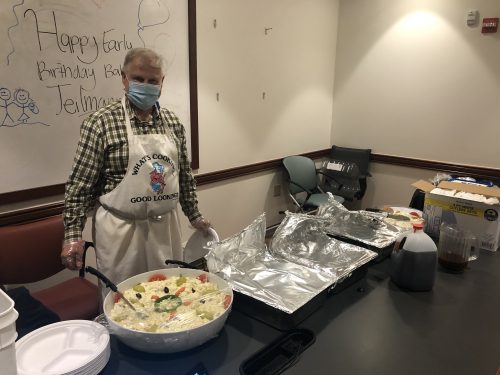
BBQ – Lunch
Thank you to Grateful cardiology patient and Duke fellow alum, Dr. Bob Bauman, cooked us an amazing pork barbeque pork lunch this week. Rich Krasuski noted “It was the best barbeque I’ve ever had!”

Important Reminders
- Please get your Flu Vaccination: All team members must get their vaccination or otherwise demonstrate policy compliance by Tuesday, Nov. 10. Details and resources all available on the Duke Health Influenza Resources site (NET ID required): https://influenza.dh.dukehealth.org.
- Moments to Movement wearables are available
- All members of the Duke University and Duke University Health System community are encouraged to register and vote in the 2020 election. For the most up-to-date information and resources on voting, visit the Duke Votes website: duke.edu
- DHTS has issued additional details related to the new Zoom meeting security requirements that are going into effect on Sept. 27. Please look these over, particularly if you are planning upcoming Zoom events. Attached is a PDF summary, if you can use it.
Upcoming Opportunities/Save the Date:
Cardiology Grand Rounds
Sept. 22: ESC Wrap-Up and Overview with the Experts. Christopher Granger and Bernard Gersh of the Mayo Clinic, 5 – 6 p.m.
Funding Opp: Translating Duke Health – CV Initiative – COVID-19
Duke Health has announced a request for innovative pilot project proposals for high risk/high impact research in the area of the heart disease and COVID-19. The intent of this RFP is to support one to four pilot projects that help us better understand how to prevent the transition from cardiovascular health to disease and/or facilitate the return to health.
We are especially interested in: (1) proposals that span multiple dimensions from basic to clinical to populations, (2) proposals that build new collaborations and/or new teams, and (3) proposals that might lead to extended productive and NIH-funded collaborations.
Applications are due TOMORROW, 9/21. Click here to see the full RFP and to find additional details about eligibility, funding, proposal requirements, selection process and review criteria.
Conferences & Symposia
Sept. 21: Duke Orthopaedic and Rehab Seminar. 4:30 – 5:30 p.m. Guest speaker is Shane Phillips, PT, PhD, FAHA, Professor and Associate Head of PT and Senior Associate Dean for Clinical Affairs, College of Applied Health Sciences, University of Illinois-Chicago. His topic is Microvascular Function and Cardiac Rehabilitation: A Canary in the Coal Mine? Zoom seminar: https://duke.zoom.us/j/93436455711
Sept. 29: COVID-19 and the Telehealth Transformation, with Jedrek Wosik and Shijing Si. Noon – 1 p.m.
COVID-19 has led to the rapid adoption of telehealth strategies in order to maintain continuity of care. As compared to in-person visits, important changes in patient characteristics were seen in telephone and video visits as well as clinician ordering patterns. In addition, MyChart patient portal usage increased dramatically. We present select initial Duke clinic utilization data before and during COVID-19. To better understand the increasing number of unstructured MyChart messages, we apply both unsupervised and supervised machine learning tools to patient-generated messages. Specifically, 1) we utilize dynamic topic modeling to gain insight into message meaning and monthly trends for patients with (+) and (-) COVID and Flu results; 2) we leverage the state-of-the-art machine learning model (Bidirectional Encoder Representations from Transformers or BERT) to construct an automatic message triaging algorithm or classifier that outperforms other baseline methods.
Registration required to receive link and meeting information. To register, visit: https://training.oit.duke.edu/enroll/common/show/21/175250. This event is co-hosted by the Duke Center for Computational Thinking and Duke+DataScience.
Oct. 5 – 8: Research Week. Sponsored by Duke School of Medicine. Series will be held virtually, via Zoom: https://duke.zoom.us/j/92060873004. More information and a full agenda can be found here: https://medschool.duke.edu/research/research-week
Nov. 13: 12th Annual NC Research Triangle Pulmonary Hypertension Symposium. Noon – 4:30 p.m. For more information, please visit this page. This event will be held virtually and is co-sponsored by Duke and the University of North Carolina in partnership with the Pulmonary Hypertension Association through the Building Medical Education in PH program. Please join us!
Nov. 13–17: AHA Scientific Sessions 2020, a virtual experience. Registration is now open. See the website for details.
COVID-19 Updates:
All the latest official DUHS information regarding coronavirus/COVID-19 response at the following locations:
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged.
Duke Heart in the News:
September 14 — Manesh Patel
Becker’s Hospital Review
The most concerning disparities in heart care outcomes: 2 cardiologists discuss
https://bit.ly/2HeAp5
Division of Cardiology Publications: September 10-16, 2020
Aberra T, Peterson ED, Pagidipati NJ, Mulder H, Wojdyla DM, Philip S, Granowitz C, Navar AM. The association between triglycerides and incident cardiovascular disease: What is “optimal”? J Clin Lipidol 2020;14(4):438-447. PM:32571728
AbouEzzeddine OF, Kemp BJ, Borlaug BA, Mullan BP, Behfar A, Pislaru SV, Fudim M, Redfield MM, Chareonthaitawee P. Myocardial Energetics in Heart Failure With Preserved Ejection Fraction. Circ Heart Fail 2019;12(10):e006240. PM:31610726
Al-Bawardy R, Vemulapalli S, Thourani VH, Mack M, Dai D, Stebbins A, Palacios I, Inglessis I, Sakhuja R, Ben-Assa E, Passeri JJ, Dal-Bianco JP, Yucel E, Melnitchouk S, Vlahakes GJ, Jassar AS, Elmariah S. Association of Pulmonary Hypertension With Clinical Outcomes of Transcatheter Mitral Valve Repair. JAMA Cardiol 2020;5(1):47-56. PM:31746963
Bach RG, Cannon CP, Blazing MA. Interpreting the Benefit of Simvastatin-Ezetimibe in Patients 75 Years or Older-Reply. JAMA Cardiol 20201;5(2):235-236. PM:31895449
Bae JA, Curtis LH, Hernandez AF. National Hospital Quality Rankings: Improving the Value of Information in Hospital Rating Systems. JAMA 2020;324(9):839-840. PM:32730574
Bennett AV, Jonsson M, Chen RC, Al-Khatib SM, Weinfurt KP, Curtis LH. Applying patient-reported outcome methodology to capture patient-reported health data: Report from an NIH Collaboratory roundtable. Healthc (Amst) 2020;8(3):100442. PM:32919581
Choi AY, Mulvihill MS, Lee HJ, Zhao C, Kuchibhatla M, Schroder JN, Patel CB, Granger CB, Hartwig MG. Transplant Center Variability in Organ Offer Acceptance and Mortality Among US Patients on the Heart Transplant Waitlist. JAMA Cardiol 2020;5(6):660-668. PM:32293647
Daubert MA, Sivak J, Dunning A, Douglas PS, Coyne B, Wang TY, Mark DB, Velazquez EJ. Implications of Abnormal Exercise Electrocardiography With Normal Stress Echocardiography. JAMA Intern Med 2020;180(4):494-502. PM:31985749
DeVore AD, Braunwald E, Morrow DA, Duffy CI, Ambrosy AP, Chakraborty H, McCague K, Rocha R, Velazquez EJ. Initiation of Angiotensin-Neprilysin Inhibition After Acute Decompensated Heart Failure: Secondary Analysis of the Open-label Extension of the PIONEER-HF Trial. JAMA Cardiol 2020;5(2):202-207. PM:31825471
Ding EY, Svennberg E, Wurster C, Duncker D, Manninger M, Lubitz SA, Dickson E, Fitzgibbons TP, Akoum N, Al-Khatib SM, Attia ZI, Ghanbari H, Marrouche NF, Mendenhall GS, Peters NS, Tarakji KG, Turakhia M, Wan EY, McManus DD. Survey of current perspectives on consumer-available digital health devices for detecting atrial fibrillation. Cardiovasc Digit Health J 2020;1(1):21-29. PM:32924024
Fanaroff AC, Peterson ED, Kaltenbach LA, Cannon CP, Choudhry NK, Henry TD, Anstrom KJ, Cohen DJ, Fonseca E, Khan ND, Fonarow GC, Wang TY. Agreement and Accuracy of Medication Persistence Identified by Patient Self-report vs Pharmacy Fill: A Secondary Analysis of the Cluster Randomized ARTEMIS Trial. JAMA Cardiol 2020;5(5):532-539. PM:32129795
Fanaroff AC, Peterson ED, Kaltenbach LA, Cannon CP, Choudhry NK, Henry TD, Anstrom KJ, Cohen DJ, Fonseca E, Khan ND, Fonarow GC, Wang TY. Association of a P2Y12 Inhibitor Copayment Reduction Intervention With Persistence and Adherence With Other Secondary Prevention Medications: A Post Hoc Analysis of the ARTEMIS Cluster-Randomized Clinical Trial. JAMA Cardiol 2020;5(1):38-46. PM:31721978
Fiuzat M, Ezekowitz J, Alemayehu W, Westerhout CM, Sbolli M, Cani D, Whellan DJ, Ahmad T, Adams K, Piña IL, Patel CB, Anstrom KJ, Cooper LS, Mark D, Leifer ES, Felker GM, Januzzi JL, O’Connor CM. Assessment of Limitations to Optimization of Guideline-Directed Medical Therapy in Heart Failure From the GUIDE-IT Trial: A Secondary Analysis of a Randomized Clinical Trial. JAMA Cardiol 2020;5(7):757-764. PM:32319999
Fudim M, Ali-Ahmed F, Parzynski CS, Ambrosy AP, Friedman DJ, Pokorney SD, Curtis JP, Fonarow GC, Masoudi FA, Hernandez AF, Al-Khatib SM. Periprocedural Risk and Survival Associated With Implantable Cardioverter-Defibrillator Placement in Older Patients With Advanced Heart Failure. JAMA Cardiol 2020;5(6):643-651. PM:32211811
Harskamp RE, Alexander JH, Lopes RD. Clinical Considerations Prior to Transition From Triple Antithrombotic Therapy to Dual Antithrombotic Therapy-Reply. JAMA Cardiol 2020;5(1):111-112. PM:31799984
Inohara T, Kohsaka S, Spertus JA, Masoudi FA, Rumsfeld JS, Kennedy KF, Wang TY, Yamaji K, Amano T, Nakamura M. Comparative Trends in Percutaneous Coronary Intervention in Japan and the United States, 2013 to 2017. J Am Coll Cardiol 2020;76(11):1328-1340. PM:32912447
Kelsey MD, Newby LK. In older patients with NSTE-ACS, clopidogrel safely reduced bleeding compared with ticagrelor at 1 year. Ann Intern Med 2020;173(6):JC28. PM:32926825
Kendsersky P, Krasuski RA. Intensive Care Unit Management of the Adult with Congenital Heart Disease. Curr Cardiol Rep 2020;22(11):136. PM:32910318
Khan MS, Shahid I, Siddiqi TJ, Khan SU, Warraich HJ, Greene SJ, Butler J, Michos ED. Ten-Year Trends in Enrollment of Women and Minorities in Pivotal Trials Supporting Recent US Food and Drug Administration Approval of Novel Cardiometabolic Drugs. J Am Heart Assoc 2020;9(11):e015594. PM:32427023
Liu Y, Baker O, Schuur JD, Weiner SG. Effects of Rescheduling Hydrocodone on Opioid Prescribing in Ohio. Pain Med 2020;21(9):1863-1870. PM:31502638
Lopes RD, Hong H, Harskamp RE, Bhatt DL, Mehran R, Cannon CP, Granger CB, Verheugt FWA, Li J, Ten Berg JM, Sarafoff N, Vranckx P, Goette A, Gibson CM, Alexander JH. Optimal Antithrombotic Regimens for Patients With Atrial Fibrillation Undergoing Percutaneous Coronary Intervention: An Updated Network Meta-analysis. JAMA Cardiol 2020;5(5):582-589. PM:32101251
Lowenstern A, Alexander KP, Hill CL, Alhanti B, Pellikka PA, Nanna MG, Mehta RH, Cooper LS, Bullock-Palmer RP, Hoffmann U, Douglas PS. Age-Related Differences in the Noninvasive Evaluation for Possible Coronary Artery Disease: Insights From the Prospective Multicenter Imaging Study for Evaluation of Chest Pain (PROMISE) Trial. JAMA Cardiol 2020;5(2):193-201. PM:31738382
Madhavan M, Holmes DN, Piccini JP, Freeman JV, Fonarow GC, Hylek EM, Kowey PR, Mahaffey KW, Pieper K, Peterson ED, Chan PS, Allen LA, Singer DE, Naccarelli GV, Reiffel JA, Steinberg BA, Gersh BJ. Effect of Temporary Interruption of Warfarin Due to an Intervention on Downstream Time in Therapeutic Range in Patients With Atrial Fibrillation (from ORBIT AF). Am J Cardiol 2020;132:66-71. PM:32826041
Mahmoudi M, Nicholas Z, Nuttall J, Bresser M, Maishman T, Berry C, Hlatky MA, Douglas P, Rajani R, Fox K, Curzen N. Fractional Flow Reserve Derived from Computed Tomography Coronary Angiography in the Assessment and Management of Stable Chest Pain: Rationale and Design of the FORECAST Trial. Cardiovasc Revasc Med 2020;21(7):890-896. PM:31932171
Mahmud E, Dauerman HL, Welt FGP, Messenger JC, Rao SV, Grines C, Mattu A, Kirtane AJ, Jauhar R, Meraj P, Rokos IC, Rumsfeld JS, Henry TD. Management of Acute Myocardial Infarction During the COVID-19 Pandemic: A Position Statement From the Society for Cardiovascular Angiography and Interventions (SCAI), the American College of Cardiology (ACC), and the American College of Emergency Physicians. J Am Coll Cardiol 2020;76(11):1375-1384. PM:32330544
Marquis-Gravel G, Roe MT, Robertson HR, Harrington RA, Pencina MJ, Berdan LG, Hammill BG, Faulkner M, Muñoz D, Fonarow GC, Nallamothu BK, Fintel DJ, Ford DE, Zhou L, Daugherty SE, Nauman E, Kraschnewski J, Ahmad FS, Benziger CP, Haynes K, Merritt JG. Rationale and Design of the Aspirin Dosing-A Patient-Centric Trial Assessing Benefits and Long-term Effectiveness (ADAPTABLE) Trial. JAMA Cardiol 2020;5(5):598-607. PM:32186653
Nanna MG, Peterson ED. Translating the Secondary Prevention Therapeutic Boom Into Action. JAMA Cardiol 2020;5(2):215-216. PM:31895445
Nathan AS, Xiang Q, Wojdyla D, Khatana SAM, Dayoub EJ, Wadhera RK, Bhatt DL, Kolansky DM, Kirtane AJ, Rao SV, Yeh RW, Groeneveld PW, Wang TY, Giri J. Performance of Hospitals When Assessing Disease-Based Mortality Compared With Procedural Mortality for Patients With Acute Myocardial Infarction. JAMA Cardiol 2020;5(7):765-772. PM:32347890
Navar AM. Questioning the Benefit of Statins for Low-Risk Populations-Medical Misinformation or Scientific Evidence?-Reply. JAMA Cardiol 2020;5(2):233-234. PM:31876926
Navar AM, Mehran R. High Rates of Off-label Prescribing and the Urgent Need for a Randomized Clinical Trial. JAMA Cardiol 2020;5(6):692-693. PM:32319997
Nelson AJ, Navar AM, Mulder H, Wojdyla D, Philip S, Granowitz C, Peterson ED, Pagidipati NJ. Association Between Triglycerides and Residual Cardiovascular Risk in Patients With Type 2 Diabetes Mellitus and Established Cardiovascular Disease (From the Bypass Angioplasty Revascularization Investigation 2 Diabetes [BARI 2D] Trial). Am J Cardiol 2020;132:36-43. PM:32773223
Olivotto I, Oreziak A, Barriales-Villa R, Abraham TP, Masri A, Garcia-Pavia P, Saberi S, Lakdawala NK, Wheeler MT, Owens A, Kubanek M, Wojakowski W, Jensen MK, Gimeno-Blanes J, Afshar K, Myers J, Hegde SM, Solomon SD, Sehnert AJ, Zhang D, Li W, Bhattachar. Mavacamten for treatment of symptomatic obstructive hypertrophic cardiomyopathy (EXPLORER-HCM): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 2020;396(10253):759-769. PM:32871100
Ortega RF, Mehran R, Douglas PS. The Conundrum and Opportunity of Gender Equity for Evidence Generators. JAMA Cardiol 2020;5(6):623-624. PM:32267464
Pandey A, Keshvani N, Khera R, Lu D, Vaduganathan M, Joynt Maddox KE, Das SR, Kumbhani DJ, Goyal A, Girotra S, Chan P, Fonarow GC, Matsouaka R, Wang TY, de Lemos JA. Temporal Trends in Racial Differences in 30-Day Readmission and Mortality Rates After Acute Myocardial Infarction Among Medicare Beneficiaries. JAMA Cardiol 2020;5(2):136-145. PM:31913411
Prabhakaran D, Perel P, Roy A, Singh K, Raspail L, Faria-Neto JR, Gidding SS, Ojji D, Hakim F, Newby LK, Stępińska J, Lam CSP, Jobe M, Kraus S, Chuquiure-Valenzuela E, Piñeiro D, Khaw KT, Bahiru E, Banerjee A, Narula J, Pinto FJ, Wood DA, Sliwa K. Correction: Management of Cardiovascular Disease Patients With Confirmed or Suspected COVID-19 in Limited Resource Settings. Glob Heart 2020;15(1):54. PM:32925986
Prabhakaran D, Perel P, Roy A, Singh K, Raspail L, Faria-Neto JR, Gidding SS, Ojji D, Hakim F, Newby LK, Stępińska J, Lam CSP, Jobe M, Kraus S, Chuquiure-Valenzuela E, Piñeiro D, Khaw KT, Bahiru E, Banerjee A, Narula J, Sliwa K. Management of Cardiovascular Disease Patients With Confirmed or Suspected COVID-19 in Limited Resource Settings. Glob Heart 2020;15(1):44. PM:32923338
Reynolds HR, Shaw LJ, Min JK, Spertus JA, Chaitman BR, Berman DS, Picard MH, Kwong RY, Bairey-Merz CN, Cyr DD, Lopes RD, Lopez-Sendon JL, Held C, Szwed H, Senior R, Gosselin G, Nair RG, Elghamaz A, Bockeria O, Chen J, Chernyavskiy AM, Bhargava B, Newman J. Association of Sex With Severity of Coronary Artery Disease, Ischemia, and Symptom Burden in Patients With Moderate or Severe Ischemia: Secondary Analysis of the ISCHEMIA Randomized Clinical Trial. JAMA Cardiol 2020;5(7):773-786. PM:32227128
Rudski L, Januzzi JL, Rigolin VH, Bohula EA, Blankstein R, Patel AR, Bucciarelli-Ducci C, Vorovich E, Mukherjee M, Rao SV, Beanlands R, Villines TC, Di Carli MF. Multimodality Imaging in Evaluation of Cardiovascular Complications in Patients With COVID-19: JACC Scientific Expert Panel. J. Am. Coll. Cardiol. 2020;76(11):1345-1357. PM:32710927
Samsky MD, Lin L, Greene SJ, Lippmann SJ, Peterson PN, Heidenreich PA, Laskey WK, Yancy CW, Greiner MA, Hardy NC, Kavati A, Park S, Mentz RJ, Fonarow GC, O’Brien EC. Patient Perceptions and Familiarity With Medical Therapy for Heart Failure. JAMA Cardiol 2020;5(3):292-299. PM:31734700
Soloveva A, Fedorova D, Villevalde S, Zvartau N, Mareev Y, Sitnikova M, Shlyakhto E, Fudim M. Addressing Orthostatic Hypotension in Heart Failure: Pathophysiology, Clinical Implications and Perspectives. J Cardiovasc Transl Res 2020;13(4):549-569. PM:32748206
Soloveva A, Fudim M. A Contemporary Picture of Congestion in Heart Failure: from Dropsy Impression to Multifaceted Reality. J Cardiovasc Transl Res 2020;13(4):507-508. PM:32367342
Song Y, Zhou X, Zhang M, Zhao W, Liu Y, Kardia SLR, Roux AVD, Needham BL, Smith JA, Mukherjee B. Bayesian shrinkage estimation of high dimensional causal mediation effects in omics studies. Biometrics 2020;76(3):700-710. PM:31733066
Sumarsono A, Vaduganathan M, Ajufo E, Navar AM, Fonarow GC, Das SR, Pandey A. Contemporary Patterns of Medicare and Medicaid Utilization and Associated Spending on Sacubitril/Valsartan and Ivabradine in Heart Failure. JAMA Cardiol 2020;5(3):336-339. PM:31738371
Tahhan AS, Vaduganathan M, Greene SJ, Alrohaibani A, Raad M, Gafeer M, Mehran R, Fonarow GC, Douglas PS, Bhatt DL, Butler J. Enrollment of Older Patients, Women, and Racial/Ethnic Minority Groups in Contemporary Acute Coronary Syndrome Clinical Trials: A Systematic Review. JAMA Cardiol 2020;5(6):714-722. PM:32211813
van de Hoef TP, Lee JM, Echavarria-Pinto M, Koo BK, Matsuo H, Patel MR, Davies JE, Escaned J, Piek JJ. Non-hyperaemic coronary pressure measurements to guide coronary interventions. Nat Rev Cardiol 2020;17(10):629-640. PM:32409779
Wang TY. Lowering Dietary Sodium Intake-Implementing and Studying the Effectiveness of Public Health Interventions. JAMA Intern Med 2020;180(6):887. PM:32338702
Waweru-Siika W, Barasa A, Wachira B, Nekyon D, Karau B, Juma F, Wanjiku G, Otieno H, Bloomfield GS, Sloth E. Building focused cardiac ultrasound capacity in a lower middle-income country: A single centre study to assess training impact. Afr J Emerg Med 2020;10(3):136-143. PM:32923324
Yancy CW, Fonarow GC, Hernandez AF. Does Guideline-Directed Medical Therapy for Heart Failure Offer Benefits After LVAD Placement?-A Call for a Randomized Clinical Trial. JAMA Cardiol 2020;5(2):183. PM:31738365
Yano Y, Reis JP, Lewis CE, Sidney S, Pletcher MJ, Bibbins-Domingo K, Navar AM, Peterson ED, Bancks MP, Kanegae H, Gidding SS, Muntner P, Lloyd-Jones DM. Association of Blood Pressure Patterns in Young Adulthood With Cardiovascular Disease and Mortality in Middle Age. JAMA Cardiol 2020;5(4):382-389. PM:31968050
Duke Heart Week ending September 13th 2020
Highlights of the week:
New Faculty Spotlight: Jennifer Rymer, MD, MBA, Cardiac Interventional Team

Back in July, we welcomed Jennifer Rymer, MD, MBA, to the Duke faculty as an assistant professor of medicine in the division of cardiology. We spoke recently about her decision to join the Duke faculty, her experiences during fellowship, and her research.
“While I wasn’t fully decided on my path when entering fellowship, my experiences at the DCRI and in the Duke cath lab made me know that academic cardiology/interventional cardiology was the route for me,” said Rymer. “I wanted to be in a place that has the type of infrastructure that allows for clinical lab time as well as research – and Duke has such a large infrastructure for research within the DCRI, population health and within the Heart Center. I had really amazing mentors as a resident and fellow, and building on those relationships made staying at Duke a really easy decision.”
During medical school, Rymer did not envision pursuing fellowship in cardiology. After an extra-long cardiology rotation during her intern year, where she was paired with Joe Rogers, Tom Gehrig, Mike Blazing and Chet Patel, she changed her mind. With that group, she found a kinship – a place and a group of people that felt like a good fit for her. Early on in residency, she began working on research projects with Tracy Wang, who has served as her primary research mentor for more than seven years.
“I remember thinking halfway through my internship year that these were the people I wanted to work with; this was a team of people I respected and I hoped to develop into the kind of doctor that I saw them model,” Rymer reflected. “I think oftentimes careers are decided based not only on clinical and research interests, but also based on the role models you work with.”
She has joined the cardiac catheterization team at Duke University Hospital and will see patients at our Henderson location as well as in South Durham. She will also have research time at the DCRI.
Rymer is currently working on the SOS-AMI trial with Manesh Patel, and the CAMEO Registry with Tracy Wang and Magnus Ohman. Rymer is currently finishing up work funded by several grants. She is co-investigator for the Duke Renal Impairment Initiative to reduce contrast-induced nephropathy in the Duke Cardiac Cath Lab, which is supported by an ACC Foundation Process Improvement Grant. She is principal investigator for work on understanding racial disparities in invasive MI management for patients with AMI and chronic kidney disease, which was supported by the ACCF Merck Award and the DCRI Executive Director Pathway funding. She is also finishing several projects related to BD-STAR and AD-STAR funding. She will be completing her MHS degree this fall based on work she started at the DCRI.
“Duke is a very rare place. It combines a high-volume tertiary care center delivering excellent clinical care with an extraordinarily talented faculty and a world-class research enterprise,” Rymer said. “I feel very lucky to have done training at Duke, and to be transitioning into a faculty role.”
Originally from Tennessee, Rymer received both her MD and MBA in 2011 at Vanderbilt University, where she had done her undergraduate work. She arrived at Duke later that same year to begin her internal medicine residency with Duke School of Medicine. She completed fellowship in cardiovascular medicine here at Duke in 2019 and her fellowship in interventional cardiology at the end of June, just prior to joining our faculty as of July 1.
Rymer has earned a number of accolades while at Duke, including the DCRI-Robert Harrington Award for Excellence in Clinical Research (2019), the Walter Floyd Award for Clinical Excellence in Cardiology (2017); the Joseph R. McClellan, Chief Resident of the Year award (2016); the AHA Women in Cardiology Training award (2015); and was a finalist for the AHA Laennec Young Clinician award (2017). She was a chief resident at Duke University (2015) and clinical chief cardiology fellow (2018). She is a co-author of 48 peer-reviewed publications; serves as a reviewer on five journals (Journal of the American College of Cardiology, Circulation, Circulation: Cardiovascular Interventions, American Heart Journal and Vascular Medicine) and sits on several committees, including the AHA Council Operations Committee and the ACC Peripheral Vascular Intervention R&P Committee.
Rymer has recently taken over Adam DeVore’s former role with managing cardiology grand rounds (CGR). She is eager to continue working to make that a great forum for everyone – especially while it continues to be offered virtually. She says the CGR team is looking for feedback and suggestions on how to make the virtual platform more successful and engaging – so please reach out to her with your ideas.
Rymer’s husband, Daniel, is an investment banker at FMI Capital in Raleigh. She has two children, William (age 6) and Caroline (age 2). She enjoys discovering new restaurants around the Triangle, and being outdoors with her family.
We are very pleased to have her on the Duke Heart faculty. Congratulations, Jenn!
Passing of William Sweezer, Jr., MD
 Earlier this week, Allan Kirk, MD, PhD, Vice Dean for the Section of Surgical Disciplines at Duke announced the following to the team:
Earlier this week, Allan Kirk, MD, PhD, Vice Dean for the Section of Surgical Disciplines at Duke announced the following to the team:
“It is with great sadness that we announce the untimely death of Dr. William P. Sweezer, Jr., our former partner and faculty member in the Division of Cardiovascular and Thoracic Surgery. Bill was an outstanding physician and surgeon, and an exceptional human being. He was an AOA graduate of Meharry Medical College, and trained in surgery at Baylor, Henry Ford Hospital, and Wayne State University for cardiac surgery. After a long and successful career in practice, he joined the Duke faculty in 2010 to serve the Danville, Virginia community.
Those who knew Bill well can speak to his incredible devotion to his patients, his colleagues, his co-workers, and to the Danville community. Although he left for a short while, he returned to his Danville roots with the vigor and enthusiasm that defined him as a physician and the demeanor that defined him as an outstanding human being. Throughout, he maintained close contact with the Duke community of thoracic and vascular surgeons in his unending effort to elevate care for his patients to the highest possible level.
The Duke Surgical community is in shock at this abrupt, tragic, and premature loss. The world would be a far, far better place with Bill Sweezer in it.”
A celebration of life for Sweezer, who died Aug. 26 at age 70, was held on Sept. 5 in Houston. He was interred in Forest Park Woodlands Cemetery in Woodlands, Texas. A news story can be found here: https://bit.ly/3mqcu3w.
Our condolences go out to his family, friends and colleagues – and our Danville Medical Community
CVRC Seminar Series Renamed
 We are pleased to share with you that the Duke Cardiovascular Research Center’s (CVRC) Mandel Seminar Series has been renamed the Victor J. Dzau Lecture Series in Cardiovascular Research supported by the Mandel Foundation.
We are pleased to share with you that the Duke Cardiovascular Research Center’s (CVRC) Mandel Seminar Series has been renamed the Victor J. Dzau Lecture Series in Cardiovascular Research supported by the Mandel Foundation.
“This name change is in recognition of Dr. Victor Dzau’s commitment to cardiovascular research and the longstanding partnership between Dr. Dzau, Duke, and the Mandel Foundation,” said Howard Rockman, MD, the Edward S. Orgain Professor of Cardiology and Director of the CVRC. “I am pleased to implement this name change and we expect that it will continue as long as the Mandel Foundation provides funding support for the seminar series.”
This lecture series has been an important means of sharing knowledge and inspiring further discovery and collaboration within the CVRC and with research partners across the U.S.
“I am honored by this recognition of my role in driving and championing cardiovascular research at Duke including the founding of the CVRC, and the many years of relationship with the Mandel Foundation,” said Victor Dzau, MD, the James B. Duke Distinguished Professor of Medicine and Chancellor Emeritus of Health Affairs at DUHS.
The request for renaming was made by the Edna and Fred L. Mandel, Jr. Foundation, a major supporter of the CVRC and of cardiovascular research throughout Duke. The Foundation has provided regular funding of research projects at Duke Health since 2005, when Dzau first arrived at Duke to serve as Chancellor of Health Affairs. Edna Mandel began supporting Dzau’s research during his tenure at Stanford University; her philanthropic support followed him to Boston when he moved back to Harvard and then to on to Duke University.
Upon her death in 2002, the Edna and Fred L. Mandel, Jr. Foundation was established through her estate to support basic scientific research efforts into the causes and treatment of hypertension, atherosclerosis and cardiovascular diseases. The foundation is administered by three trustees.
Since 2005, all of the Mandel Foundation’s philanthropic efforts, totaling $12,235,594 has gone to projects within the Duke University School of Medicine. In recent years, the annual grant amount has ranged from $800,000 to $900,000, including direct and indirect costs. This funding includes support for the following in the School of Medicine, the Division of Cardiology, and the CVRC:
- Mandel Seed grants for Duke University School of Medicine faculty members
- Mandel Research Fellowship
- Mandel Scholar Award
- Interdisciplinary research grant
- CVRC Small Animal Physiology Core research vouchers
- Translational research award
- Major support for the Duke-Stanford Cardiovascular Research Symposium
- A seminar series co-hosted by the Cardiovascular Research Center (CVRC)
The CVRC was formed in 2011 to provide an intellectual home for cutting-edge, multi-disciplinary, bench-oriented research. Their mission is to solidify, enhance and support outstanding cardiovascular research from the basic discovery end of the translational research spectrum.
FAST FACTS! Did you know?
Most of our 20 CVRC faculty members are housed in co-localized research space in the CARL building, directly connected to Duke University Hospital. They have a combined 33,048 square feet of lab space, giving them one of the largest spaces dedicated to basic cardiovascular research in the U.S. “Our cardiology investigators hold greater than $25 million in active research award funding,” according to Maria Price Rapoza, PhD, Executive Director of the CVRC, “and Duke is in the top five nationally for basic science research funding in the cardiovascular space, based on 2014-2018 data.”
Very impressive, CVRC!
Smith Elected to Associate of the ACC
 Congratulations to Brenda Smith, RN-BC, CSNIII one of our all-star nurses on the clinical cardiac electrophysiology (EP) team, on her election to Associate of the American College of Cardiology! She will receive this honor during the annual convocation ceremony at the 70th Annual Scientific Session in Atlanta, currently scheduled for March 20-22, 2021.
Congratulations to Brenda Smith, RN-BC, CSNIII one of our all-star nurses on the clinical cardiac electrophysiology (EP) team, on her election to Associate of the American College of Cardiology! She will receive this honor during the annual convocation ceremony at the 70th Annual Scientific Session in Atlanta, currently scheduled for March 20-22, 2021.
Smith has worked with Duke EP for 25 years as an outpatient nurse clinician. She is a Fellow in the Heart Rhythm Society, and board certified in cardiac-vascular nursing.
Please join us in congratulating Brenda on this important career milestone!
You & Your Wellness Matter!
Early in the pandemic, infectious disease experts buzzed that this would be a marathon not a sprint. Are you needing a bit of encouragement to keep on going – to keep doing all the good and difficult things you are doing? We could all use some encouragement and perhaps reminders (and permission) that we need breaks. Our wellness matters.
One thing we hope to do with our Duke Heart team this fall is to encourage each one of us to find ways to support our wellness – whether that means giving ourselves a chance to add more movement to our day; providing ourselves time to get to sleep earlier; taking an opportunity to turn off phones and email for a little while; or choosing a healthier meal or buying fewer carb-laden snacks at the grocery store (#guilty).
As a major sponsor of the Triangle Heart Walk, we would, of course, love for you to sign up as a team captain or as a walker. However, we understand that participation might be too much on top of everything else going on right now. What matters more is every member of our team doing something good for themselves and their health. That means you. Your wellness matters.
Stay tuned over the coming weeks and months as we provide tips, reminders and encouragement to address areas of wellness in your life. Do you have tips or a story to share with Pulse readers? What has helped you the most over the past six months? Drop us a note with Wellness in the subject line. We’d like to use your stories to encourage our entire team.
Something to consider this week: Could you make time to add 15-20 more minutes of healthy activity to your week? Or, perhaps you could pick a night to get to sleep 15-20 minutes earlier? Schedule this in your Outlook calendar along with an alarm to prompt you.
If you’re interested and able to do so, sign up as a Heart Walk team captain or join an existing team as a walker so that Duke Heart is well represented. You can register at www.triangleheartwalk.org/duke. If you are already registered, thank you!
Shout-out to CVSSU & our Patient Transport Team!
We learned this week from Kelly Valencia, MSN, FNP-BC, RN-BC, one of our cardiology APPs, that we had a situation develop in a post-PCI (no intervention) patient who was being discharged from the Cardiovascular Short Stay Unit (CVSSU) in Duke University Hospital. The patient was being wheeled out by the transporter when the patient started to complain of lightheadedness. Patient was still in the CVSSU hallway. Jessie Smith, a transporter, turned the wheelchair around and returned the patient to their room; patient became diaphoretic, clammy, and had changes in their level of consciousness. The CVSSU team rushed into action and took excellent care of the patient. A cardiology fellow and attending evaluated the patient event, which was determined to be a vasovagal episode. Our patient did well and has since been discharged safely. “Everyone worked together so well and showed exemplary teamwork!” according to Valencia. Special thanks to Jenna, Britney, Cayley, Amy, Tara, Sharise, Julie and Taylor of the CVSSU for responding immediately. (There were lots of hands on deck, and things moved quickly, so we hope we have included everyone here.)
Well done, team! Hat tip to Stephanie Barnes for the share!
More Good News:
Mollie Kettle, Kelly Kester, Allen Cadavero, Amanda Ornell, Maggie Meyer, Maria Carroll, Jill Engel and Bradi Granger are co-authors on a paper appearing in the Fall 2020 issue of AACN Advanced Critical Care journal. Their article, “COVID-19: Mobilizing Quickly for a Rapid Response,” can be accessed here. Great work, team!
Oliver Jawitz, Jill Engel and Judson Williams have a paper published online ahead of print in the journal Critical Care Clinics. The article, “How to Start an Enhanced Recovery After Surgery Cardiac Program in Critical Care,” can be accessed here. Their co-authors include William Bradford, Gina McConnell, and Jessica Allender, all of Wake Med. Congratulations!
Important Reminders
- Please get your Flu Vaccination: All team members must get their vaccination or otherwise demonstrate policy compliance by Tuesday, Nov. 10. Details and resources all available on the Duke Health Influenza Resources site (NET ID required): https://influenza.dh.dukehealth.org.
- REACH Equity Center seeking candidates – see last week’s post
- Moments to Movement wearables are available
Upcoming Opportunities/Save the Date:
Duke Health Town Hall
Sept. 14: Voter Registration/Town Hall. 4:30 p.m. via Zoom: Link
Monday afternoon, the Duke Health Town Hall will focus on Duke Health’s voter registration and turnout initiative for the 2020 elections. A representative from You Can Vote, a non-partisan voter education organization, will be on hand to provide helpful information and resources. The session begins at 4:30 p.m.
Cardiology Grand Rounds
Sept. 15: Social Media and Academic Cardiology. Panelists include Sunil Rao, Manesh Patel, Adrian Hernandez, Jonathan McCall, and Brian Southwell, 7:15 – 8:15 a.m.
Sept. 22: ESC Wrap-Up and Overview with the Experts. Christopher Granger and Bernard Gersh, 5 – 6 p.m.
Funding Opp: Translating Duke Health – CV Initiative – COVID-19
Duke Health has announced a request for innovative pilot project proposals for high risk/high impact research in the area of the heart disease and COVID-19. The intent of this RFP is to support one to four pilot projects that help us better understand how to prevent the transition from cardiovascular health to disease and/or facilitate the return to health.
We are especially interested in: (1) proposals that span multiple dimensions from basic to clinical to populations, (2) proposals that build new collaborations and/or new teams, and (3) proposals that might lead to extended productive and NIH-funded collaborations.
Applications are due Sept. 21, 2020. Click here to see the full RFP and to find additional details about eligibility, funding, proposal requirements, selection process and review criteria.
Conferences & Symposia
Oct. 5 – 8: Research Week. Sponsored by Duke School of Medicine. Series will be held virtually, via Zoom: https://duke.zoom.us/j/92060873004. More information and a full agenda can be found here: https://medschool.duke.edu/research/research-week
Nov. 13: 12th Annual NC Research Triangle Pulmonary Hypertension Symposium. Noon – 4:30 p.m. For  more information, please visit this page. This event will be held virtually and is co-sponsored by Duke and the University of North Carolina in partnership with the Pulmonary Hypertension Association through the Building Medical Education in PH program. Please join us!
more information, please visit this page. This event will be held virtually and is co-sponsored by Duke and the University of North Carolina in partnership with the Pulmonary Hypertension Association through the Building Medical Education in PH program. Please join us!
COVID-19 Updates:
All the latest official DUHS information regarding coronavirus/COVID-19 response at the following locations:
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged.
Duke Heart in the News:
September 7 — Renato Lopes
Physician’s Weekly
ESC: BRACE CORONA Provides Data to Ease ACEi/ARB Worries in Pandemic
https://www.physiciansweekly.com/esc-brace-corona-provides-data-to-ease-acei-arb-worries-in-pandemic/
September 9 — Ann Marie Navar and Duke Clinical Research Institute
EurekAlert/AAAS (news release)
Generic cholesterol drugs save medicare billions of dollars, study finds
https://www.eurekalert.org/pub_releases/2020-09/usmc-gcd_1090820.php
Division of Cardiology Publications Indexed in PubMed September 3-9, 2020
Ahn S, Shenoy SK, Luttrell LM, Lefkowitz RJ. SnapShot: ?-Arrestin Functions. Cell 2020 Sep 3;182(5):1362-1362. PM:32888497.
Bakovic M, Thakkar D, DeBenedittis P, Chong DC, Thomas MC, Iversen ES, Karra R. Clonal Analysis of the Neonatal Mouse Heart using Nearest Neighbor Modeling. J Vis Exp 2020 Aug 22;(162):10.3791/61656. PM:32894270.
Chen MH, Raffield LM, Mousas A, Sakaue S, Huffman JE, Moscati A, Trivedi B, Jiang T, Akbari P, Vuckovic D, Bao EL, Zhong X, Manansala R, Laplante V, Chen M, Lo KS, Qian H, Lareau CA, Beaudoin M, Hunt KA, Akiyama M, Bartz TM, Ben-Shlomo Y, Beswick A. Trans-ethnic and Ancestry-Specific Blood-Cell Genetics in 746,667 Individuals from 5 Global Populations. Cell 2020 Sep 3;182(5):1198-1213. PM:32888493.
Douglas PS, Walsh MN. Increasing Diversity in Cardiology: It Will Take a Village. J Am Coll Cardiol 2020 Sep 8;76(10):1223-1225. PM:32883416.
Fudim M, Boortz-Marx RL, Ganesh A, DeVore AD, Patel CB, Rogers JG, Coburn A, Johnson I, Paul A, Coyne BJ, Rao SV, Gutierrez JA, Kiefer TL, Kong DF, Green CL, Jones WS, Felker GM, Hernandez AF, Patel MR. Splanchnic Nerve Block for Chronic Heart Failure. JACC Heart Fail 2020 Sep;8(9):742-752. PM:32535123.
Greene SJ, DeVore AD. The Maximally Tolerated Dose: The Key Context for Interpreting Subtarget Medication Dosing for Heart Failure. JACC Heart Fail 2020 Sep;8(9):739-741. PM:32800507.
Hahn VS, Yanek LR, Vaishnav J, Ying W, Vaidya D, Lee YZJ, Riley SJ, Subramanya V, Brown EE, Hopkins CD, Ononogbu S, Perzel Mandell K, Halushka MK, Steenbergen C, Rosenberg AZ, Tedford RJ, Judge DP, Shah SJ, Russell SD, Kass DA, Sharma K. Endomyocardial Biopsy Characterization of Heart Failure With Preserved Ejection Fraction and Prevalence of Cardiac Amyloidosis. JACC Heart Fail 2020 Sep;8(9):712-724. PM:32653448.
Parcha V, Patel N, Kalra R, Arora G, Januzzi JL, Felker GM, Wang TJ, Arora P. Racial Differences in Serial NT-proBNP Levels in Heart Failure Management: Insights From the GUIDE-IT Trial. Circulation 2020 Sep 8;142(10):1018-1020. PM:32897749.
Vuckovic D, Bao EL, Akbari P, Lareau CA, Mousas A, Jiang T, Chen MH, Raffield LM, Tardaguila M, Huffman JE, Ritchie SC, Megy K, Ponstingl H, Penkett CJ, Albers PK, Wigdor EM, Sakaue S, Moscati A, Manansala R, Lo KS, Qian H, Akiyama M, Bartz TM, Ben-Shlomo. The Polygenic and Monogenic Basis of Blood Traits and Diseases. Cell 2020 Sep 3;182(5):1214-1231.e11. PM:32888494.
Zink MD, Chua W, Zeemering S, di Biase L, Antoni BL, David C, Hindricks G, Haeusler KG, Al-Khalidi HR, Piccini JP, Mont L, Nielsen JC, Escobar LA, de Bono J, Van Gelder IC, de Potter T, Scherr D, Themistoclakis S, Todd D, Kirchhof P, Schotten U. Predictors of recurrence of atrial fibrillation within the first 3 months after ablation. Europace 2020 Sep 1;22(9):1337-1344. PM:32725107.
Duke Heart week ending September 6th 2020
Highlights of the week:
Fudim to Receive Zipes Award at ACC 2021

We are pleased to share that Marat Fudim, MD, MHS, one of our three newest faculty members in the Division of Cardiology, has been notified of his selection as the recipient of the 2021 Douglas P. Zipes Distinguished Young Scientist Award. He is the first Duke nominee to receive the honor.
The Zipes award is presented annually at the ACC Scientific Sessions to recognize a young scientist who has made outstanding contributions to the field of cardiovascular medicine and who has amassed an impressive body of scientific research in either the clinical or basic domain.
“This is exciting for Marat, the Division and for all of the people who have mentored him,” said Manesh Patel, MD, chief of the Duke division of cardiology. “I think it speaks to his tireless work ethic and some of the innovation he has done in the early part of his career. Importantly, it also speaks to a great group of people at the divisional level who have taken an interest in mentoring and truly supporting others who are trying to do research, sometimes in different ways.”
Fudim’s nomination was centered upon the body of work he has accumulated researching the use of splanchnic nerve blockade in patients with congestive heart failure.
“I feel very honored to be selected,” Fudim said. “I consider this the highest award that I could qualify for at this stage of my career. It’s very exciting for me and I’m particularly happy for our research team and my mentors as this project was supported and made possible by a diverse group of investigators.”
Robert Mentz, MD, chief of Duke’s heart failure section, served on the ACC Selection Panel for the award and recused himself from voting.
“There was a very high quality group of applicants overall,” Mentz said. “But it was clear amongst the others who were part of the voting that Marat was the ideal recipient for this. The panel members recognized his hypothesis-driven research that really has the potential to change how we approach our understanding of heart failure physiology.”
When asked to reflect on Fudim’s work and his selection for the award, Patel added, “There are a combination of things that were probably very enticing to the panel — the first is a new physiologic principal or opportunity to treat heart failure by thinking about the splanchnic compartment as a vascular sink. The second is the translational work of having the idea, testing it first in humans with a variety of blocks and then taking it to actual clinical trials.”
The award will be presented during the ACC’s Convocation Ceremony of the College’s 70th Annual Scientific Session, currently scheduled for Monday, March 22, 2021 in Atlanta, GA. The Session runs March 20-22. Fudim’s travel, housing, and registration expenses will be paid by ACC. He will also receive a $1,000 monetary prize, and a chance to present his scientific work at ACC.21.
Congratulations, Marat! Way to go!
FAST FACTS: Did you know?
Douglas P. Zipes, MD, is distinguished professor emeritus at Indiana University. He did his postgraduate training at Duke from 1964 to 1968, and in 2007 was presented with the Distinguished Alumnus Award by Duke University Medical Alumni Association. He is also a regular contributor to the Saturday Evening Post as a health columnist. To read more about his lifetime achievements, please visit https://medicine.iu.edu/faculty/6515/zipes-douglas.
Virtual ESC Congress 2020 Wraps Up
The European Society of Cardiology’s 2020 Congress wrapped up this week.
Renato Lopes presented results from BRACE CORONA:
The trial sought to examine whether a 30-day suspension of angiotensin-converting enzyme inhibitors (ACEI) and angiotensin receptor blockers (ARBs) would improve outcomes for COVID-19 patients. The primary outcome of the study was the number of days a patient spent alive and out of the hospital through the 30-day follow-up period. The study was sponsored by the D’Or Institute for Research and Education and the Brazilian Clinical Research Institute.
“These therapies have well-known benefits for patients with hypertension and heart failure, and this trial supplies high-quality randomized evidence to guide their usage while treating hospitalized patients with mild and moderate cases of COVID-19,” Lopes said. “Our trial found no clinical benefit to routinely suspending these medications, and this supports the recommendation that they should generally be continued for those who rely on them for managing hypertension or heart failure.”
Sean Pokorney presented on IMPACT-AFIB:
Although the intervention tested as part of IMPACT-AFib was found not to be effective, the design and implementation of the trial showcased the effective use of a new electronic data system to conduct a large-scale pragmatic trial.
The trial was the first to use the U.S. Food and Drug Administration’s (FDA) FDA-Catalyst System and Sentinel System network of electronic health record (EHRs) and insurance claims data from a diverse group of data partners. The trial enrolled 80,000 patients with atrial fibrillation who were at high risk of stroke and not taking medication.
COMBINE AF was presented by our Cardiology Fellow – Tony Carnicelli who has worked many hours across many institutions to put together the 4-5 large randomized atrial fibrillation trials. This effort represents several years of work and hopefully we will start to soon see some of the important analyses from this work and the ESC presentation.
Registration for ESC was free – don’t forget that all presentations will be available in the ESC Congress platform with access to slides, videos and abstracts until September 30.
Duke Heart Grows By One!
 Congratulations to the Pomeroy family! Jordan Pomeroy, a cardiology fellow, and his wife Summer, welcomed their son, River Scott Pomeroy, on Aug. 28 at 4:17 a.m. Jordan said they are all doing well and that “Everyone, including big sister — Parker Rose (17 months) — are excited to have the little man join our family!”
Congratulations to the Pomeroy family! Jordan Pomeroy, a cardiology fellow, and his wife Summer, welcomed their son, River Scott Pomeroy, on Aug. 28 at 4:17 a.m. Jordan said they are all doing well and that “Everyone, including big sister — Parker Rose (17 months) — are excited to have the little man join our family!”
We are so happy for you and we can’t wait to meet him!
More Good News:
John Alexander was one of 243 people world-wide to be elected this year as a Fellow of the European Society of Cardiology. Congratulations, John!
Robert Harrington has been awarded the American Heart Association’s Distinguished National Leadership Award for contributions to the association. Harrington’s many contributions to the organization have earned him the AHA’s Distinguished National Leadership Award. He will be honored on Oct. 27 in a livestreamed ceremony at the AHA 2020 National Volunteer Awards Event. Congratulations, Bob!
Zak Loring has a paper published online, ahead of print, in Europace this week. The article, “Machine learning does not improve upon traditional regression in predicting outcomes in atrial fibrillation: an analysis of the ORBIT-AF and GARFIELD-AF registries” can be found here. Jon Piccini and Eric Peterson are among his coauthors.
Marat Fudim and team have a paper in the September issue of JACC: Heart Failure. The article, “Splanchnic Nerve Block for Chronic Heart Failure” can be found here. Duke co-authors include Richard Boortz-Marx, Arun Ganesh, Adam DeVore, Chet Patel, Joseph Rogers, Aubrie Coburn, Inneke Johnson, Amanda Paul, Brian Coyne, Sunil Rao, J. Antonio Gutierrez, Todd Kiefer, David Kong, Cynthia Green, Schuyler Jones, Mike Felker, Adrian Hernandez and Manesh Patel.
Forbes has named both Duke University and DUHS among the “Best-in-State Employers” in North Carolina in 2020. According to the rankings released on Monday, Duke Health System placed sixth and the University 26th out of 100 employers in North Carolina.
All three DUHS hospitals have been recognized as LGBTQ+ Healthcare Equality Leaders by the Human Rights Campaign Foundation for perfect scores across areas of patient-centered care, support services, and inclusive health insurance policies for LGBTQ+ patients.
ICYMI: Duke University and Duke University Health System will not be implementing the payroll tax deferment program announced three weeks ago by Presidential Memorandum. Duke will continue to collect payroll taxes on behalf of all employees in order to avoid potential confusion, undue hardships, or other complications that might otherwise emerge during the filing of taxes for 2020 by our employees next year.
Duke Health Heart Walk Rally Day: Thurs. Sept. 10
On Thursday, Sept. 10, Duke will host a Heart Walk Rally Day. DUHS has set a goal to recruit at least 500  participants for this year’s Heart Walk. Ongoing support from those who are already registered for the Heart Walk, and all those who join us on our Rally Day, helps further the American Heart Association’s mission.
participants for this year’s Heart Walk. Ongoing support from those who are already registered for the Heart Walk, and all those who join us on our Rally Day, helps further the American Heart Association’s mission.
Please consider starting a team or joining one so that the Heart Center is well represented. You can register at www.triangleheartwalk.org/duke. If you are already registered as a team captain, between now and Thursday, please encourage your colleagues to join your team.
The local American Heart Association team will host three 15-minute Pep Rallies throughout the day to share more about this year’s event. Feel free to join one of the sessions via Zoom. The Pep Rallies will be held at 10 a.m., 1 p.m. and 5 p.m. and your team members are welcome to attend: Heart Rally Zoom meeting link.
Show Your Care for One Another: Moments to Movement Wearables
In the Duke Health family, we treat people with respect. We value each other‘s differences. We care for each other through kindness, inclusion, and compassion. We do this because it’s the right way to be—and because it’s the first step in giving our patients the excellent care they deserve.
 To help demonstrate our commitment, we are offering two ways you can show your personal support for our collective humanity:
To help demonstrate our commitment, we are offering two ways you can show your personal support for our collective humanity:
- A Black Lives Matter badge reel holder
- A pin featuring the anti-racism ribbon
These items were developed by a team of four Duke Health team members who sought a concrete way to stand up for our values. Read their story here.
Duke Heart has received an initial supply of both items, with more on the way. Our initial batch is available starting Tuesday. For DUH-based heart teams, please see a nurse manager to obtain one or both items, along with a companion card that explains what the items mean.
Wearing these is completely voluntary. You can choose to wear one or both to take a stand for our values. Recognizing that many employees are working from home, we’re also providing virtual Zoom backgrounds and email signature files featuring the emblems. Look for them in an upcoming edition of Inside Duke Health (expected this week).
Flu Vaccination Campaign Began Sept. 1
Annual vaccination against the flu (or an approved medical or religious exemption) is a condition of employment at Duke University Health System. All team members must get their vaccination or otherwise demonstrate policy compliance by Tuesday, Nov. 10.
Details and resources all available on the Duke Health Influenza Resources site (NET ID required): https://influenza.dh.dukehealth.org.
Upcoming Opportunities/Save the Date:
Cardiology Grand Rounds Returns (Virtually)!
Grand Rounds returns — this week we will have an M&M Conference with Kevin Friede. Please join us on Tuesday, Sept. 8, 5 p.m. via Webex. Meeting number: 120 364 2432. Password: hScPc638mjC.
REACH Equity Center Seeking Candidates
The Duke Center for Research to Advance Healthcare Equity (REACH Equity) seeks candidates to co-lead the Research, Education, Training (RET) Subcore.
The RET Subcore is responsible for: (1) Facilitating opportunities for health disparities investigators across the campus at all levels (students, trainees, faculty) to share their work, find collaborators, and identify mentors or mentees. (2) Administer programs to support research education and fund small pilot awards related to the Center’s theme.
Programs currently led by the RET Subcore include:
- REACH Equity Summer Undergraduate Research Program (RESURP): An eight-week summer undergraduate health disparities education and mentored research program
- Research Voucher, Research Scholars Development, Transdisciplinary Think Tank pilot award programs which provide funding for faculty and trainees conducting research related to the Center’s theme
- RWIP: Bi-monthly Research Works in Progress interactive seminar series
- Annual Health Disparities Research Colloquium
Additional administrative duties include participation in monthly Executive Operating Committee meetings, annual Internal Advisory Board, Stakeholder Advisory Board, and Steering Committee meetings, and other activities related to achieving the Center’s aims.
Faculty selected for this position will co-lead the core with Kevin Thomas and work closely with the REACH Equity Director, Kimberly Johnson, to continue current activities and expand activities of the RET Subcore in response to increased interest in health disparities research among trainees and faculty across the campus. The position includes funding to support time associated with the role (approximately 10% effort support).
For more information on the RET Subcore, please visit: https://sites.duke.edu/reachequity/cores/research-education-training-subcore/
Eligibility Criteria:
- Assistant or Associate Professor in any Department, Division, Center, or School
- MD or PhD or equivalent
- Any discipline
- Clinical research experience, preferably in health disparities
If you are interested, please submit your CV and a letter describing your interest in the position and detailing relevant experience (prior leadership roles, research experience, research education and training experience, mentorship, etc.) by October 2 to Cheryl Miller, cheryl.j.miller@duke.edu
REACH Equity faculty will interview a small number of applicants. While there is some flexibility, selected candidate may start position as early as November 1.
Please contact Cheryl Miller for more information: chery.j.miller@duke.edu
NOTE: Duke Heart’s Larry Jackson is a current awardee and can provide details about the experience
DIHI: Request for Applications (RFA 2021 Innovation Projects)
 Duke Institute for Health Innovation (DIHI) announces the next emerging ideas and funding cycle for innovative ideas and projects. Proposed projects should address actual and important problems encountered by care providers, patients and their loved ones and represent urgent health challenges nationally. For the upcoming funding cycle, DIHI is specifically interested in innovations in areas that: (a) Improve value of care through novel strategies, (b) Create digital solutions for care and monitoring (home monitoring, wearables etc.), (c) Advance health equity, (d) Enhance provider and staff experience and well-being, (e) Accelerate population health solutions and strategies, and (f) Enhance patient engagement and experience.
Duke Institute for Health Innovation (DIHI) announces the next emerging ideas and funding cycle for innovative ideas and projects. Proposed projects should address actual and important problems encountered by care providers, patients and their loved ones and represent urgent health challenges nationally. For the upcoming funding cycle, DIHI is specifically interested in innovations in areas that: (a) Improve value of care through novel strategies, (b) Create digital solutions for care and monitoring (home monitoring, wearables etc.), (c) Advance health equity, (d) Enhance provider and staff experience and well-being, (e) Accelerate population health solutions and strategies, and (f) Enhance patient engagement and experience.
Please visit https://dihi.org/events/dihi-rfa for additional information and instructions. The deadline for submitting applications is midnight October 9, 2020. All proposals are required to have a Duke Health operational lead as a cosponsor to be accepted for review. If the DIHI team can be of any assistance in the formulation of ideas or connections, please contact Suresh Balu. We look forward to your innovative solutions.
2020 Triangle Heart Walk Going “Digital”; Will Be Held Oct. 10
Sign up is open for the 2020 Triangle Heart Walk which is going virtual! Instead, the American Heart Association is planning for a nation-wide digital experience across several weeks leading up to the main event on October 10. You can register at: www.TriangleHeartWalk.org/Duke. Pep Rally Day is Sept. 10 – watch your email this week for messages from Dr. Tom Owens, chair of our local Heart Walk.
12th Annual NC Research Triangle Pulmonary Hypertension Symposium
November 13: Zoom Webinar. Noon – 4:30 p.m. For more information, please visit this page.
COVID-19 Updates:
All the latest official DUHS information regarding coronavirus/COVID-19 response at the following locations:
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged.
Something Just for Fun:
Thanks for reading to the end! Hope each of you have a glorious Labor Day! Let’s wrap it up with our colleagues who made the news this week:
Duke Heart in the News:
August 24 — Richard Krasuski
SI.com/Sports Illustrated
SI Survey: Doctors Say They’d Play in the NBA and NHL, but not NFL and MLB
https://www.si.com/nfl/2020/08/24/doctor-covid-survey-daily-cover
August 30 — Renato Lopes
Healio/Cardiology Today
Invasive approach to stable ischemic heart disease may benefit in HF, LV dysfunction
https://www.healio.com/news/cardiac-vascular-intervention/20200830/invasive-approach-to-stable-ischemic-heart-disease-may-benefit-in-hf-lv-dysfunction
August 31 — Jonathan Piccini
MDEdge
RATE-AF trial boosts digoxin for rate control in permanent AFib
https://www.mdedge.com/familymedicine/article/227714/arrhythmias-ep/rate-af-trial-boosts-digoxin-rate-control-permanent
August 31 — Renato Lopes
tctMD/the heart beat
Revascularization Benefits ISCHEMIA Patients With Mild LV Dysfunction or HF
https://www.tctmd.com/news/revascularization-benefits-ischemia-patients-mild-lv-dysfunction-or-hf
September 1 — Renato Lopes
MedPage Today
‘Definitive Data’: Continuing ACE/ARB Tx Safe in COVID-19
https://www.medpagetoday.com/meetingcoverage/esc/88399
September 2 — Renato Lopes
MDedge/Cardiology News
First randomized trial reassures on ACEIs, ARBs in COVID-19
https://www.mdedge.com/cardiology/article/227885/hypertension/first-randomized-trial-reassures-aceis-arbs-covid-19
September 2 — Renato Lopes
Managed Healthcare Executive
Duke Scientist: Patients With COVID-19 Should Stay on ACE Inhibitors, ARBs
https://www.managedhealthcareexecutive.com/view/duke-scientist-patients-with-covid-19-should-stay-on-ace-inhibitors-arbs
September 2 — Sean Pokorney
Medscape
IMPACT-AFib: Single Mailing Fails to Budge Oral Anticoagulant Uptake for AFib
https://www.medscape.com/viewarticle/936781
September 3 — Sean Pokorney
tctMD/the heart beat
Got Mail? Letter-Based Intervention Doesn’t Boost OAC Initiation for A-fib
https://www.tctmd.com/news/got-mail-letter-based-intervention-doesnt-boost-oac-initiation-fib
Recent Comments