Home » 2020
Yearly Archives: 2020
Duke Heart Pulse – Week Ending 12-20-20
Chief’s message:
Our final pre-holiday weekly Pulse for 2020 makes me think back a year from now. Last year as we celebrated the New Year we would not have imagined that 2020 would bring a global pandemic that stresses and puts our health care systems in our country at the center of public health battle. It is in this tumult, that the Duke Heart Community responded with much more involvement and innovation in clinical care and multiple organized research grants nationally and locally in an attempt to continue to move the scientific field forward, and many outreach efforts to improve our community health in hopes of better days.
It is with your relentless commitment and resilience that we have endured and worked as a group. This has been highlighted over the last week as the Pfizer-BioNTech Covid-19 arrived across the country and groups mobilized to get frontline and essential groups vaccinated. At Duke and we worked as hard as possible to ensure all of our groups were informed, registered, and appropriately getting in line to get vaccination slots. But this was not without angst as we were ensuring we register, get our groups aligned and communicated to how and when people will get the vaccine. It’s hard to be patient at the end of a 10-month pandemic. We were encouraged by the increase in vaccinations given even today on Sunday, with many of our that our trainees and staff and faculty starting to move through the process.
 It is with this background, that I was most struck this week by the CT surgery final faculty meeting with Peter Smith as Division Chief. As the Division Chief for CT surgery at Duke for the last 25 years, it is hard to put into words what he has meant to the group. For 2 hours we heard from all parts of our health system, network, clinical practice, research infrastructure and most importantly numerous faculty and staff as to the affect he has had on our Heart Center. We are glad he will be around support our group and Ed Chen and the CT surgery group, and look forward to his continued leadership.
It is with this background, that I was most struck this week by the CT surgery final faculty meeting with Peter Smith as Division Chief. As the Division Chief for CT surgery at Duke for the last 25 years, it is hard to put into words what he has meant to the group. For 2 hours we heard from all parts of our health system, network, clinical practice, research infrastructure and most importantly numerous faculty and staff as to the affect he has had on our Heart Center. We are glad he will be around support our group and Ed Chen and the CT surgery group, and look forward to his continued leadership.
I am proud of the work our staff, fellows, and faculty have done to care for our patients. As we look forward into 2021, we are aware of the need for your continued partnership, local leadership for the health of your community, and the importance of keeping our patients involved and engaged in our science. We are ever grateful for all of our people, the people that make Duke Heart. We will need all of your continued collaboration and support in this upcoming year.
Highlights of the week:
Duke Heart Talent Show ‘Spectacular’ Held
As this crazy year began winding down and vaccine planning ramped up, a different sort of challenge was thrown down – with several brave souls stepping up for the first-ever Duke Heart talent show… The event was held via Zoom on Friday evening. Contestants representing areas within the Division of Cardiology competed in short videos demonstrating the wide range of talents (or lack thereof, depending on who you ask) in front of a panel of judges and an audience of 75+ colleagues. Our co-hosts were Manesh Patel, Vanessa Blumer and Sipa Yankey; our judges were Kevin Friede, Zack Wegermann, Navid Nafissi and Angela Lowenstern.
The event kicked off with a surprise visit by “the Masked Santa” and moved on to the cooking talent of John Alexander, (in photos he was accompanied by Mango, the African lovebird); Alexander had – prior to the Zoom event –delivered his Slow Cooker Red Lentil Cauliflower Curry direct to the homes of each of our four judges as well as instructions on how to reheat, etc. The curry was a hit!
Next up were:
- Chris Granger & Tilley, with an impressive juggling performance
- Beckett Mentz, 8, in a convincing performance of the aftershave scene from Home Alone
- Members of the Duke Heart Failure Team singing the 12 Days of COVID with a cameo performance by Joe Rogers
- Tony Carnicelli on acoustic guitar with a twist on Let It Be
- Adam Barnett, accompanied by adorable daughter Lily, playing classical piano
- Schuyler Jones reading hiaku
- Mikael “Mik” Templeton, from our interventional team, on saxophone with The Christmas Song (chestnuts roasting on an open fire).
- The Adult Congenital team’s “Kazoo Khoir” in a rousing performance of Rudolph the Red-Nosed Reindeer. Rich Krasuski with some wonderful ad libs.
- Future Tik Tok star Manesh Patel, encouraging vaccination for COVID-19, with cameos by Anna Lisa Crowley, Jacob Schroder and Carmelo Milano
- Sipa Yankey rapping his day-in-the-pandemic-life experiences with “Ain’t No Thrombus“
The showstopper of the evening proved to be a stunning rendition of ‘Ave Maria’ featuring the gorgeous voice of Ashli Carnicelli accompanied Tony Carnicelli on acoustic guitar; the judges agreed this was the winning performance.
Thanks to all who were able to join our Zoom event. The commentary in the ‘chat’ was a vital part of the evening – it was great to see so many members of our team and we hope that coming together in this way helped you celebrate the holidays and one another. To quote Tracy Wang via chat at the end, “Needed the pick me up, thanks to all; this was special…. happy holidays!”
We especially appreciate the generosity of our contestants – we know it took effort to pull your videos together on short notice. We thank our judges and the hosts for the evening – you did a great job with commentary and keeping things lively.
Great job, everyone, and happy holidays to you and yours. Thanks for making Duke Heart such a special place at Duke.
7200 Moved Successfully!
The Cardiac Stepdown Unit on Duke North 7200 moved to Duke North 7700 with a capacity for 12 patients on Friday, Dec. 18. Thanks to everyone who helped make this a successful, seamless move! In one of the photos you can see the code response for move with Greg Flynn. Also shown are Faith Williams, Diane Sauro, and Sarah Kirby. Another photo shows the team debrief. Many, many thanks everyone!



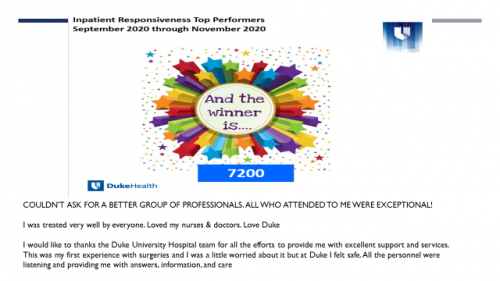
Commendation for Lisa Duncan and 7100/7200 Team
 Special thanks to Lisa Duncan, 7100 Nurse Manager and Clinical Leads Antoniette Embler, Brittany Stephenson, and Katherine Adams for their leadership on 7200. This leadership team opened 7200 in the fall of 2017 by hiring and onboarding a team of nurses to complement the existing 7100 team. During their tenure, the unit received top performance accolades from senior leadership for Patient Experience metrics on several occasions (unit cleanliness and staff responsiveness to name a few). In FY20, the unit excelled with quality metrics, having no CAUTI or CLABSI infections or hospital acquired pressure injuries. As the coverage for 7200 has now transitioned, we want to acknowledge the efforts and contribution of the 7100/7200 leadership team and staff under Lisa’s guidance for their care of patients and their loved ones, and support of the Hospital’s capacity needs.
Special thanks to Lisa Duncan, 7100 Nurse Manager and Clinical Leads Antoniette Embler, Brittany Stephenson, and Katherine Adams for their leadership on 7200. This leadership team opened 7200 in the fall of 2017 by hiring and onboarding a team of nurses to complement the existing 7100 team. During their tenure, the unit received top performance accolades from senior leadership for Patient Experience metrics on several occasions (unit cleanliness and staff responsiveness to name a few). In FY20, the unit excelled with quality metrics, having no CAUTI or CLABSI infections or hospital acquired pressure injuries. As the coverage for 7200 has now transitioned, we want to acknowledge the efforts and contribution of the 7100/7200 leadership team and staff under Lisa’s guidance for their care of patients and their loved ones, and support of the Hospital’s capacity needs.
Informatics Expert Joe Kelly Earns Black Belt
Congratulations to Joe Kelly, Duke Heart’s Director of Cardiovascular Informatics & PI/QI, for earning his black belt in karate – specifically in the Shito-Ryu Motobu-Ha style.
 According to Joe, it usually takes about 10 years to get a black belt in this style. “We also practice Jiu Jitsu (Hakko-Ryu), and Kobudo (weapons – Ryu Kyu Kobudo Hozon ShintoKai), he said. “All these are from the island of Okinawa.”
According to Joe, it usually takes about 10 years to get a black belt in this style. “We also practice Jiu Jitsu (Hakko-Ryu), and Kobudo (weapons – Ryu Kyu Kobudo Hozon ShintoKai), he said. “All these are from the island of Okinawa.”
His testing/demonstration was done via Zoom (see photo). The Zoom panel photo shows Sensei Devorah Dometrich who is a 9th Degree Black belt (10 is highest) and was the first female Okinawan 7th Degree black belt in 1997.
During the testing, Joe had to perform and then show application for the exact same Kata (forms) that have been done for over 200 years and derived from other Kata that date as early as 600 C.E.
According to Joe, his sensei will often have kids with special needs in the class for children; he teaches special needs classes in Durham County, and anyone of any shape-age-weight, provided they can partake of physical activity, can make adjustments and take the classes.
“I picked the Dojo because they are not at all “macho” or “rough” but instead are humble and excellent teachers,” he added.
Please join us in congratulating Joe on this accomplishment! He will soon be teaching classes via Zoom, so if you’re interested, drop him a note.
Way to go, Joe!!!

7200 Earns Top Performer Status
Congrats to the team of 7200 for earning Inpatient Responsiveness Top Performer Status for Sept. – Nov. 2020.
Zoom Retirement Party Held for Karen Craig
A virtual retirement celebration was held via Zoom for Karen Craig of the CardioPulmonary Rehab team on Wednesday evening, Dec. 16. Craig is retiring from Duke on December 31st. It is hoped that we’ll be able to offer a celebration in-person sometime in the future, but the team gathered this week via Zoom to share stories and reflect on Karen’s remarkable contributions throughout her career.
Zoom guests were asked to prepare a few words to share with Karen, and creative Zoom backgrounds that reminded people of Karen were encouraged, many of which can be seen in this screen shoot.
Congrats, Karen!


Steve Guerrant Retirement Celebrated
Steve Guerrant, who has served Duke University Hospital for 29 years and has been the Engineering Specialist in the Duke Electrophysiology Lab for 13 years, is retiring this month from Duke; he was celebrated this week on the unit. His knowledge of EP equipment, lab construction, and troubleshooting will be sorely missed. His ability to share knowledge and teach EP staff members the equipment side of EP is one-of-a-kind. He has been an integral part of the EP team and we are all grateful to have worked with him. Many thanks to Jill Engel for photos and Elizabeth Watts for helping Pulse share this news!

Lowers Named CardioPulmonary Rehabilitation Manager
We are excited to share that Sean T. Lowers, PT, DPT, CCS has accepted the Manager, Clinical Services position with our CardioPulmonary Rehabilitation team. The announcement was made last week by Brian Wofford, Vice President of Heart Operations for Durham County.
In his announcement, Wofford offered special thanks to our HR, Recruitment, and Interview teammates for an efficient and effective recruitment process. Lowers started in his new role on Tuesday, December 15th in order to maximize the formal handoff between him and Karen Craig before her retirement on December 31st.
“We will miss Karen more than words can express, but Sean has been a pivotal member of the team both as a Physical Therapist and Clinical Services Coordinator,” said Wofford. “His experience and work with Karen has prepared him to lead the team through our next chapter, and I am personally excited for what is in store for all of us.”
Lowers’ previous position on the team was Clinical Services Coordinator, Rehabilitation; as he transitions, leadership is changing the scope of his previous role. The replacement position will have a Cardiac Rehabilitation focus instead of a focus on Pulmonary Rehabilitation and we anticipate the job to be posted soon.
Please join us in congratulating Sean on his promotion!
Shout-out to Banks & the Fellows Team
We received a great note this weekend from Cary Ward regarding Adam Banks, which led to additional observations about the Cardiology Fellows team:
“I first want to give a shout out to Adam Banks for helping the DHP team with a patient who was very sick with mitral regurgitation and needed a diagnostic cath in preparation for surgery. The patient was frightened and anxious and intermittently refusing care. She had even signed out AMA the week before. Adam was able to develop a rapport with the patient who then agreed to cath and eventually a balloon pump. This took a lot of time and emotional energy on Adam’s part and he could have easily taken the easy way out instead by reporting back that she was not willing to sign consents. We were all very appreciative of all the extra time he took with her.
After noticing Adam’s contributions in the beginning of the week, I began to see all the other times in which the fellows ensure that our patients get excellent care: Chris Wrobel managing the DHP team all week while needing little input from me … Alyson Corley spending most of her CCU call resuscitating one of our patients…Toi Spates and others helping the nurses with an off service patient who had fallen in 7200…Kelly Arps who cared for a very sick AS patient all Friday night…the list goes on.
And then on Friday we watched the talent show in which Tony Carnicelli and Adam Barnett showed off incredible musical talent, the emcees were hilarious and Sipa performed “Ain’t No Thrombus.”
During this holiday, I feel grateful to work with such an amazingly talented and vibrant group of young people, and want them to know how incredibly valued they are.
Happy Holidays to all the fellows!”
Indeed, we have a gifted team of fellows, faculty and staff comprising Duke Heart. Thank you to all!
Good Catch, Spikes!
Jasmine Spikes received a Good Catch Award on December 11; the “catch” occurred on October 22 – the award reads, “For ensuring patient safety by recognizing that a patient had a red identity flag and that the patient’s identity had not yet been confirmed during a recent admission from the ED. She immediately contacted unit leadership for support on how to handle the situation. It was determined that the patient identity was not verified while in the ED and the patient’s identity was subsequently confirmed.”
Thank you to Antoniette Embler, Clinical Team Lead for Cardiology Stepdown 7100/7200, for sharing this with Pulse!

Shout Out to Siffring & Perfusion Team!
Travis Siffring and our Perfusion team have two publications in the latest issue of The Journal of ExtraCorporeal Technology, the official journal of AmSECT, as well as a prominent accolade from the JECT editor:
Academic Perfusion at Its Best and New Tradition:
Our final Journal of ExtraCorporeal Technology issue for 2020 showcases the myriad of ways that our clinical perfusion community conducts academic work that contributes to our practices. The impressive work published here not only shares the knowledge they have generated but also will, I hope, inspire others to partake in the enrichment of our clinical skills and enhancement of our profession.
The first example of such an enhancement that I would like to highlight is that of AmSECT, our sponsoring society, now have a published set of standards and guidelines for pediatric congenital perfusion! Molly Oldeen and her co-authors have meticulously compiled a much needed, previously non-existent set of standards and guidelines for our colleagues practicing pediatric and congenital perfusion. AmSECT’s service to these perfusionists is now on par in this regard with what it provides to adult perfusionists. Furthermore, these standards and guidelines were reviewed and endorsed by both the Congenital Heart Surgeons and Congenital Cardiac Anesthesia societies. With its co-publication in the World Journal for Pediatric and Congenital Heart Surgery, these standards and guidelines will be widely available and shared broadly within this specialty. My congratulations to Molly Oldeen and her co-authors who are all well-known, long-time contributors to AmSECT, for their latest accomplishment!
Another group of perfusionists I would like to congratulate and highlight in this issue is Travis Siffring and his Duke University team. They have two publications in this issue, not only showing us a new optimized perfusion strategy for Norwood reconstructions but also demonstrating how perfusionists can participate in investigating and innovating along with their physician partners and then share their findings in their respective profession’s journals. The work shared in this issue first describes their early in vitro evaluation of their sustained total all-region perfusion technique. This is followed by their second article describing the clinical implementation of this technique from the perfusionists’ perspective. Also referenced in their work is a third publication by their physician colleagues who described the surgical technique aspect of this effort. Siffring and co-authors should be commended not only for their contributions in developing this technique but also for making that extra effort to share their relevant efforts with our perfusion community through these articles. This is clinically driven academic perfusion done right!
A PDF of the full message from JECT Editor-in-Chief Raymond K. Wong, PhD, CCP, is available here. The full issue is available now, online, to AmSECT members.
Way to go, Perfusion!!!!
Thoughts on “LV”
It comes as no surprise that the people we work with each day make a pretty significant impact in our work lives. In healthcare, the work is personal and especially so when we become ‘the patient’. The retirement of Lavetta “LV” Staton spurred the following note to her, which was shared this week with Pulse. It’s printed here with permission of the writer, name withheld:
“LV,
I have thought about this for 5 years but have never had the right opportunity to share it with you. Now you are retiring.
In 2016 I had chest pain, got a stress test, and then a cath. It turned out to be normal.
As familiar as I am with health care and the Duke Cath Lab it is still a humbling and anxiety producing experience to be on the other side of the table as a patient.
I am privileged and got to choose Sunil Rao to be the attending but it was your being there that made me feel comfortable and that I was in good hands.
You were familiar, professional, competent, and kind. Thank you. Somehow I don’t remember anybody else.
All the best in your retirement!”
The work we do together is important; our skills and expertise matter. But at the end of the day, how you treat people makes a bigger impression.
COVID-19 Updates:
All the latest official DUHS information regarding coronavirus/COVID-19 response at the following locations:
NOTE: Today is our last issue of Pulse for 2020. We will return on Jan. 10. Enjoy the holidays!
Upcoming Opportunities/Save the Date:
Cardiology Grand Rounds
Dec. 22: No Cardiology GR. Happy Holidays!
Dec. 29: No Cardiology GR. Happy Holidays!
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged.
Duke Heart in the News:
December 14 — Rob Califf
CNBC/Squawk on the Street
Historic vaccination effort underway
https://bit.ly/3mwEEIL
*clip begins @ 10:33:40
December 15 — Rob Califf
Bloomberg Surveillance
https://bit.ly/38oyGVd
*clip begins @ 08:19:28
This story also carried on Bloomberg Radio
Duke Heart Week Ending December 13th
Updates of the week:
Sondej Leaving Duke Heart in January; Heading to OneMedical
 Sean Sondej will be leaving his role as Associate Vice President of Heart & Vascular Services for Duke University Health System (DUHS) to accept a position with One Medical as Vice President of Strategic Partnerships. The announcement was made Friday by William Fulkerson, MD, Executive Vice President of DUHS.
Sean Sondej will be leaving his role as Associate Vice President of Heart & Vascular Services for Duke University Health System (DUHS) to accept a position with One Medical as Vice President of Strategic Partnerships. The announcement was made Friday by William Fulkerson, MD, Executive Vice President of DUHS.
“We are truly sorry to see Sean leave our team, but we’re also happy for him as he begins a new career challenge,” said Fulkerson. “As many of you know, One Medical is one of our clinically integrated partners and a valued member of our growing network.”
Sean has been a member of the Duke family for more than 17 years, starting as an administrative fellow in 2003. His talents were quickly recognized, and he advanced here to fulfill many important roles, including partnering with physician and nursing leaders to lead our Heart Center CSU during a critical period of growth. Instrumental in creating our Heart Care Plus collaboration with WakeMed and working with many other local hospitals to expand high quality care in their communities, Sean is admired as a relationship-builder, a strategic thinker and an effective leader of great character. Throughout his career at Duke, he has mentored many colleagues and developed the people around him, including sponsoring our MINDS affinity group to support our young professionals.
Sean leaves behind a strong team, and I’m grateful to Jill Engel for agreeing to serve as Interim AVP of Heart & Vascular Services. Over the next two months, we’ll be working with Sean to ensure a smooth transition.
Sean will be with us until the end of January 2021. He and his family are planning to remain here in Durham, and we look forward to staying connected and working with him in his new role.
The announcement concluded with Fulkerson thanking Sean for his work here at Duke and for helping to build a team that will continue to deliver the highest quality care to our patients and families for many years to come.
Congratulations, Sean!
CVRC Announces Annual Mandel Awards
The Duke Cardiovascular Research Center (CVRC) has recently announced their annual Mandel Awards. The team made three awards in the Seed program, two awards in the Fellow program, and one in the Scholar program. We are pleased to share the projects and scholars receiving funding for the 2021 project period (Jan. 1- Dec. 31, 2021):
Mandel Scholar Award
Dennis Abraham, MD
Project: Mechanosensitive TREK-1 modulates myofibroblast driven fibrosis
According to the CDC, nearly one in three people in the US suffer from Hypertension and are at risk for developing the dreaded

complication of congestive heart failure. Once heart failure develops, hypertensive patients are at risk of becoming debilitated and dying prematurely. Both death and debilitation remain largely unchecked amongst hypertensive patients who develop a form of heart failure called Heart Failure with Preserved Ejection Fraction (HFpEF), due to the lack of effective drug therapies. A key event in the development of HFpEF is scar tissue formation produced by cardiac cells called fibroblasts. In response to conditions like Hypertension, fibroblasts are activated (myofibroblasts) to produce scar tissue (fibrosis) that causes the heart to become stiff. Our lab has found that the potassium channel TREK-1 has a profound influence on scar tissue formation after hypertensive injury. In this proposal, we will examine how TREK-1 affects the activation of fibroblasts in response to conditions that mimic an injured heart. If successful, we anticipate discoveries that may lead to therapeutic strategies to mitigate cardiac stiffness and the development of HFpEF.
Mandel Fellow Awards
Qiao Zhang, PhD, mentored by George Truskey, PhD
Project: Clinically relevant human microphysiological system disease model to investigate the effects of cellular force disruption in Cardiovascular diseases and Hutchinson-Gilford Progeria Syndrome
Cardiovascular disease (CVD) is the leading cause of death among persons aged 65 and older in the United States and the risk of developing CVD increases with age. Understanding the role of aging in the development of CVD can help early diagnosis and treatment to reduce the likelihood of subsequent serious events such as development of ischemia and stroke. Hutchinson-Gilford Progeria syndrome (HPGS) is rare but fatal disease that happens to young children and cause premature aging. Children with HGPS develop CVD and die of complications from CVD at an average of 13 years. The cause of HPGS is by the accumulation of progerin, a modified form of the nuclear envelope protein lamin A which produces an irregularly shaped cell nucleus. The nucleus is under force balance and performed as olive shape with smooth edges. Irregular nuclear shape shown in HPGS cells indicates a disruption of force balance on nucleus, which will cause alterations in gene expression and subsequently contribute to the progression of atherosclerosis in HGPS. Restoring the force balance on the nucleus may correct some of the phenotypes caused by accumulation of progerin. As progerin accumulation has been shown to increase with normal aging, the findings from this proposal could also help reveal the role of progerin accumulation in aging blood vessels.
Gayathri Viswanathan, PhD, mentored by Sudarshan Rajagopal, MD PhD
Project: Chronic thromboembolic pulmonary hypertension (CTEPH) and Pulmonary arterial hypertension (PAH)
Chronic thromboembolic pulmonary hypertension (CTEPH) is a disease of the pulmonary vasculature characterized by persistent thrombotic occlusion or stenosis of the pulmonary arteries resulting in pulmonary hypertension (PH). CTEPH is a serious and often fatal disease. Although pulmonary thromboendarterectomy (PTE) remains the treatment of choice for patients with CTEPH (Fig. 1), not all patients will benefit from or receive this highly specialized surgery. Patients whose CTEPH is deemed inoperable are candidates for medical therapy, for which only riociguat, a soluble guanylate cyclase stimulator, is FDA-approved. Thus, there is a significant unmet need for novel medical therapies for CTEPH. At this time it is not known what specific receptors are expressed in CTEPH thrombus and how they contribute to thrombus proliferation. Directly addressing this knowledge gap would aid in our long-term goal of developing novel medical therapies for CTEPH. The overall objective for this application is to identify up- and down-regulated GPCRs in thrombus isolated from CTEPH patients who have undergone PTE surgery and test the effects of targeting those receptors in culture models of thrombus. We will do this by performing GPCR profiling globally using single cell RNA sequencing (scRNAseq). These studies will allow us to differentiate receptor expression in different cell types, such as myofibroblasts, endothelial cells and immune cells that compose the thrombus. We will then test the effects of modulating signaling through these receptors in ex vivo models of CTEPH thrombus. The expected outcomes of this project is a deeper mechanistic understanding of the cells that contribute to and dysregulated signaling in CTEPH. This will aid in our long-term goal of developing novel CTEPH medical therapies.
Mandel Seed Awards
Laura Wingler PhD
Project: A High-Throughput Discovery Platform for Deep Mutational Scanning of GPCR Kinases
G protein-coupled receptors (GPCRs) are the targets of numerous drugs used in the treatment of cardiovascular diseases such as hypertension (e.g., beta-blockers targeting b-adrenergic receptors and angiotensin receptor blockers [ARBs] targeting angiotensin receptors). Typically, activation of GPCRs initiates numerous events within cells, but it has now become clear that certain drugs selectively trigger only some of these myriad cellular effects. This exciting revelation means it may be possible to design new drugs with finely tuned profiles (e.g., improved effectiveness and reduced side effects). However, we will not be able to leverage this phenomenon rationally until we understand the molecular-level details of how GPCRs “turn on” each of the three main families of proteins that they directly interact with in the cell. Recent breakthroughs in GPCR structural biology have begun to provide such insights for two of these protein families, but understanding of the third key family, GPCR kinases (GRKs), has lagged far behind. This is principally due to the fact that the interactions between GPCRs and GRKs are relatively brief and unstable, making it difficult to “capture” and study activated GRKs. To circumvent this technical challenge, we propose a unique approach to elucidate the changes that GRKs undergo. During the funding period, we will develop a high-throughput system to generate millions of GRK mutants and screen for those that assume activated states even before they interact with GPCRs. Successful completion of our specific aims will deliver a toolkit of GRK mutants whose activated states can be readily studied using powerful structural biology methods. This will provide a critical missing “piece of the puzzle” as to why certain GPCR drugs turn on different effects in the cell. Ultimately, this information could inform the development of next-generation cardiovascular drugs with optimized therapeutic profiles.
Ravi Karra, MD and Dennis Ko, MD PhD
Project: Genetic Regulators of Human Cardiomyocyte Proliferation
The human heart was once considered to be static, but recent work has challenged this dogma. The human heart is now known to be capable of a low-level of muscle turnover. While cardiac cycling occurs at a low rate, the absolute amount of heart tissue that is replaced over a lifetime could be substantial. However, no tools exist to understand the relative contribution of cardiac turnover to cardiovascular disease. Here, we will use human genetics to 1) understand how the risk for heart failure relates to heart muscle turnover and 2) identify new markers that can be used to track how cardiac turnover impacts cardiovascular disease
Sudha Shenoy PhD, collaborating with Jonathan Campbell, PhD
Project: Ubiquitin-dependent signaling bias at the glucagon family receptors and its impact on pancreatic β cell function
Note: This team received funding last year, and made significant progress. However, additional progress was prevented by the pandemic and accompanying Duke research curtailment. This led reviewers to prioritize funding for this team and their high caliber work.
Type 2 diabetes (T2D) and associated insulin resistance contribute to the etiology of atherosclerosis and constitute major risk factors leading to morbidity and mortality from cardiovascular disease. The peptide hormone glucagon and the class B seven-transmembrane G protein-coupled receptors that are activated by glucagon play a fundamental role in regulating blood glucose levels. These receptors, namely the glucagon receptor (GCGR) and the glucagon-like peptide 1 receptor (GLP-1R) also regulate insulin release from pancreatic beta cells and are currently major targets for developing new treatments and drugs for T2D. Glucagon binding elevates the second messenger cAMP through the activation of G proteins, and furthermore, the activated receptors are subjected to desensitization and internalization through recruitment of additional proteins, namely, GPCR kinases, ꞵ-arrestin and RAMPs. GLP-1R agonists enhance insulin secretion and reduce food intake, which promotes glucose lowering and reductions in body weight in patients with T2D. Glucagon agonists also increase satiety and induce energy expenditure, suggesting the combination of GCGR and GLP-1R agonism could have additive effects on weight reduction and further improve glycemia. Consequently, the GCGR is an emerging target in anti-diabetic therapy, particularly in the development of GCGR/GLP-1R co-agonists. However, there still remains an incomplete understanding of the signaling mechanisms invoked by either the GCGR or the GLP-1R, which limits the drug discovery to tackle T2D and associated morbidity. In this context, we have now identified that GCGR is subjected to ubiquitin-dependent regulation. Ubiquitin is a small protein that acts as a signaling code when appended to active protein complexes. Our data suggests that ubiquitination of the GCGR increases signaling through G proteins, whereas ligand binding causes de-ubiquitination, leading to decreased G protein coupling and increased ꞵ-arrestin binding and activity. There is limited information on the regulation of GLP-1R by ubiquitination. Thus, our studies will test the role of GCGR and GLP-1R ubiquitination in the propagation of signaling via these transducers and identify the molecular mechanism(s) that link ubiquitin-dependent signaling to cellular function.
Congratulations to all Mandel funding recipients!!
Shout-out to Spates
In a note from Sudarshan Rajagopal to Anna Lisa Crowley this week, we received a shout-out for Toi Spates:
“Just wanted to give a shout out to Toi Spates who helped last week when a patient decompensated overnight. She did a great job getting in touch with the patient’s family and managing the situation.”
Great work, Toi!
“LV” Retirement Celebration Held
We mentioned last week that Lavetta “LV” Staton was retiring – the Cath Lab hosted a socially-distanced gathering to celebrate & thank her this week. Hat tip to Jill Engel and Elizabeth Watts for sharing the following photos with us this week. According to Watts, “LV has been at Duke for 28 years and a member of the Cath Team since 1997. Her charisma and commitment to her patients and team will be sorely missed. She has touched many lives along the way and we are all grateful to have worked with her.”
We will miss you, LV!!!


Duke Emergency Alert Test: Wednesday, Dec. 16
Duke University & Duke University Health System will conduct a test of the DukeAlert system on Wednesday, December 16 using all existing channels. Regular tests that had been scheduled for March and October were postponed due to the pandemic… but, with winter upon us, we need to ensure all new students, faculty and staff understand how they would hear about an emergency incident at Duke. To read more about this, check out the article from Duke Today: https://today.duke.edu/2020/12/dukealert-test-scheduled-dec-16
DUHS Well-being Survey: Please Complete!
A survey link was sent to all Duke Health team members last week; the survey is to better understand how everyone is holding up during this challenging year. If you have not yet taken it, please look for it in Outlook – it came from survey@smdhr.com — and complete it this week; it’s short and will take less than five minutes.
NOTE: The survey is being administered by a 3rd party survey partner (SMD) in order to maintain confidentiality; it is safe to open the link. The survey will ask specific questions to understand how DUHS can improve things that may increase our resilience and well-being. The effort will also check how we’re doing with our effort to increase our diversity, inclusion and belonging. We will use your thoughts to guide these efforts going forward. Please participate – thank you!!

COVID-19 Updates:
All the latest official DUHS information regarding coronavirus/COVID-19 response at the following locations:
NOTE: A reminder that Pulse will not be published on Dec. 27 or Jan. 3 so that we may enjoy some time off.
Upcoming Opportunities/Save the Date:
Cardiology Grand Rounds
Dec. 22: No Cardiology GR. Happy Holidays!
Dec. 29: No Cardiology GR. Happy Holidays!
Radiothon for Duke Children’s Dec. 15-16
The annual Radiothon for Duke Children’s will be held on Dec. 15-16. Tune in to MIX 101.5 FM during the Radiothon to hear incredible and moving stories from our Duke Children’s patient families and pledge your support. Together, we can continue to advance care and give hope to the children and families who need it most. Donate today at bit.ly/DukeRadiothon2020.

Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged.
Duke Heart in the News:
December 4 — Joseph Rogers, Cameron Wolfe (ID) & Rita Oakes (Nursing)
WRAL
With scores of infected workers, Duke Health preps to vaccinate staff
https://bit.ly/3gty98e
December 4 — Joseph Rogers, Cameron Wolfe (ID) & Rita Oakes (Nursing)
WRAL
Challenges with COVID vaccine distribution
https://bit.ly/3n6jmTE
December 6 – Duke, Eugene Stead
MedpageToday
Remembering the Past to Inspire the Future for Advanced Practice Professionals
https://bit.ly/3nlN3QM
December 8 — Manesh Patel
docwirenews
Manesh Patel, MD Talks Atherosclerotic Disease Updates
https://bit.ly/37fVZBr
Duke Heart Week Ending December 6th 2020
Chief’s Message: Moments of Brightness
Being on call for the cath lab this weekend highlighted for me the continued dedication and strain our teams are facing in the Winter of 2020 as we struggle with the Pandemic for hopefully the last time. All of our health systems and communities have been strained, but perhaps not as much as they are now. Although the health system entry points, the routine of masking and PPE, visitation, clinical care, and communication and distancing procedures have now been going on for many months – there is still a sense of new found struggle. I see the calm and resolve that our faculty, staff, fellows, and teams exhibit hourly to help care for our patients and each other. And it is the hope and now the expectation with vaccines and improved treatments that there will be a light at the end of a long tunnel. It is in this journey that I ask for all of your in this upcoming Holiday time to take a moment to get any rest possible, appreciate those in our lives, and recognize the moments of brightness that are happening.
This weekend was the last weekend of call with Lavetta Staton “LV” (a long standing Duke Cath lab nurse – over 22 years in the cath lab and 30 years at Duke). If you have been in the Duke lab, you have heard the LV sayings – “Teamwork makes the Dreamwork”, “If you stay ready, you don’t have to get ready,” and many more. Generations of patients, fellows, faculty, and staff have been touched by LV. We will be holding a proper retirement when we can – but until then it was an honor to take care of the last Acute MI patient with her as another class of diagnostic and interventional fellows will have there own personal sayings and lessons from LV. Perhaps the most important lesson from a long career in the Duke Cath Lab that LV imparted was the sense of vigilance, readiness that we continually strive for to ensure our patient care is as good as it can be. The fun, the interaction, all of it came after ensuring we could get patients the care they needed in times of acute and sometimes unexpected need. Therefore, as we near a hopeful end to a long winter, we should all appreciate the moments of joy/brightness this holiday season while we strive to stay ready and safe as we care for our patients and each other.
the cath lab and 30 years at Duke). If you have been in the Duke lab, you have heard the LV sayings – “Teamwork makes the Dreamwork”, “If you stay ready, you don’t have to get ready,” and many more. Generations of patients, fellows, faculty, and staff have been touched by LV. We will be holding a proper retirement when we can – but until then it was an honor to take care of the last Acute MI patient with her as another class of diagnostic and interventional fellows will have there own personal sayings and lessons from LV. Perhaps the most important lesson from a long career in the Duke Cath Lab that LV imparted was the sense of vigilance, readiness that we continually strive for to ensure our patient care is as good as it can be. The fun, the interaction, all of it came after ensuring we could get patients the care they needed in times of acute and sometimes unexpected need. Therefore, as we near a hopeful end to a long winter, we should all appreciate the moments of joy/brightness this holiday season while we strive to stay ready and safe as we care for our patients and each other.
Highlights of the week
Duke Cardiology Fellowship Program Announces 2021 Class
 The newest fellows to the Duke Cardiology fellowship program were announced earlier this week. They’ll join us in July, 2021. Please join us in celebrating with:
The newest fellows to the Duke Cardiology fellowship program were announced earlier this week. They’ll join us in July, 2021. Please join us in celebrating with:
- Willard Applefeld, Osler Medicine Training Program, The Johns Hopkins Hospital
- Sara Coles, Duke University Health System
- Ijeoma Eleazu, Massachusetts General Hospital
- Mohammad Shahzeb Khan, Cook County Health & Hospital System
- Veraprapas Mark Kittipibul, Jackson Memorial Hospital/University of Miami
- Nkiru “Kiki” Osude, Loyola University Medical Center
- Balimkiz Senman, Brigham & Women’s Hospital
- Ilya Shadrin, Mayo Clinic
- Lonnie Sullivan, Duke University Health System
- Manasi Tannu, Emory University School of Medicine
Congratulations to all! Hat tip to Anna Lisa Crowley, Arlene Martin and all the fellows and faculty who helped during this recruitment season. Great job!
Barnes named Clinical Director, Advanced HF Services, Effective Jan. 1
 Duke Heart is pleased to announce that effective January 1, 2021, Stephanie Barnes, MSN, AGPCNP-C, PCCN will assume the role of Clinical Director for Advanced Heart Failure Services at Duke University Hospital. As the Clinical Director, she will be responsible for programmatic oversight of services providing care to the advanced heart failure patients, including the medical heart failure patients and durable mechanical circulatory support population. In this role, Stephanie will partner with the focus on programmatic development, regulatory compliance, evidence based care, and overall quality outcomes and improvement for the heart failure population in partnership with the Heart Failure and Ventricular Assist Device Medical and Duke Heart Center leadership teams.
Duke Heart is pleased to announce that effective January 1, 2021, Stephanie Barnes, MSN, AGPCNP-C, PCCN will assume the role of Clinical Director for Advanced Heart Failure Services at Duke University Hospital. As the Clinical Director, she will be responsible for programmatic oversight of services providing care to the advanced heart failure patients, including the medical heart failure patients and durable mechanical circulatory support population. In this role, Stephanie will partner with the focus on programmatic development, regulatory compliance, evidence based care, and overall quality outcomes and improvement for the heart failure population in partnership with the Heart Failure and Ventricular Assist Device Medical and Duke Heart Center leadership teams.
Stephanie completed her BSN at the University of South Carolina and MSN with Adult Gerontology Primary Care Nurse Practitioner focus at the University of North Carolina. Stephanie has experience as a heart failure and LVAD nurse and Nurse Practitioner at both Duke University Hospital and Tufts Medical Center. Most recently, she has served as a Nurse Practitioner and Team Leader on the Duke Cardiology inpatient Advanced Practice Provider team.
“Steph has been a brilliant and dedicated team member and team leader for the Cardiology APPs for over 3 years,” her team of cardiology APPs said. “She is an outstanding provider and will be greatly missed. We are excited about this new opportunity for her and look forward to seeing her in her new role.”
Stephanie has presented and published on heart failure and LVAD topics and serves as a clinical preceptor for NP students. Please help us congratulate Stephanie in her new role in Duke Heart.
Blumer Recognized by Patient Family
Anna Lisa Crowley shared an email she received this week from the family member of a patient cared for by Vanessa Blumer. We wanted to share it with all of you:
Dr. Crowley,
I’m writing this email to commend a trainee from your cardiovascular disease program. I saw your name listed as director on the Duke webpage, but if I should be directing this email to another person, please accept my apologies.
Often times, I feel we fail to recognize the efforts of those who go out of their way for others’ wellness. In our case, we didn’t want to miss out on the opportunity to openly highlight the kindness, aptitude, and extraordinary work ethic of Dr. Vanessa Blumer. She cared for my mother while she was in the intensive care and never have we encountered someone so caring. You could easily tell her high level of competency and in-depth knowledge but, more importantly, she had humanity. Like my mom said: “there’s an angel in her”. Sometimes physicians forget what it’s like to be a patient or a family member; in this regard and all others, Dr. Blumer was exemplary.
Thank you for your leadership and for allowing my family the opportunity to be cared by world-class physicians.
Grateful,
Megan*
Way to go, Vanessa! We are blessed to have you on our amazing team of care providers. (*Shared with permission of the family.)
Kudos to Coles, Narcisse & Durham VAMC Cath Lab Staff
In a note from Raj Swaminathan to Anna Lisa Crowley this week, we heard about a great save at the Durham VAMC this week:

 “Just wanted to give some praise to our fellow, Dennis Narcisse, and our incoming fellow, Sara Coles, for a great save late in the day yesterday at the VA. A veteran in the MICU with a history of advanced heart failure quickly went into shock with rising lactate and Cr, and reduced urine output. [The patient] was ice cold and not mentating well. Sara and Dennis quickly notified the cath lab team, performed a bedside ECHO confirming poor ejection and volume overload, obtained telephone consent from family, and triaged [the patient] to the lab. Dennis then performed the RHC confirming severe cardiogenic shock and placed an IABP. Overnight, [the patient] turned the corner with improving labs, brisk urine output, and is now off pressors.
“Just wanted to give some praise to our fellow, Dennis Narcisse, and our incoming fellow, Sara Coles, for a great save late in the day yesterday at the VA. A veteran in the MICU with a history of advanced heart failure quickly went into shock with rising lactate and Cr, and reduced urine output. [The patient] was ice cold and not mentating well. Sara and Dennis quickly notified the cath lab team, performed a bedside ECHO confirming poor ejection and volume overload, obtained telephone consent from family, and triaged [the patient] to the lab. Dennis then performed the RHC confirming severe cardiogenic shock and placed an IABP. Overnight, [the patient] turned the corner with improving labs, brisk urine output, and is now off pressors.
[The patient] would not have made it overnight had it not been for our amazing house staff expediting care. I also want to recognize our VA cath lab staff who stayed late to get this case done. Strong work all around!”
In a follow-up note to Raj’s from Sunil Rao, we got a second round of accolades for Narcisse and Coles for the same patient case:
“Dennis and Sara are awesome! An additional word about Dennis – he was in the MICU to see an entirely different patient but noticed that this particular patient wasn’t doing well. So he took the initiative and, with Sara, diagnosed [the patient] appropriately with severe cardiogenic shock.”
Great job, everyone!
Yankey Receives High-5
Congrats to Sipa Yankey for receiving a High-5 this week! He was nominated by Michel Khouri who said, “Dr. Yankey spent a  lot of time providing comfort to a patient and their family. He helped ease the patient’s transition to another treatment course after a complex hospitalization.”
lot of time providing comfort to a patient and their family. He helped ease the patient’s transition to another treatment course after a complex hospitalization.”
Nicely done, Sipa!
DUHS Well-being Survey: Dec. 7
A short survey will be sent to all Duke Health team members starting Dec. 7 to better understand how everyone is holding up during this challenging year. DUHS leadership wants to hear the organization’s voice on two things that have changed our world dramatically – the COVID-19 pandemic and racial injustice. DUHS nursing and house staff will each have a unique, short set of additional questions.
The survey is being administered by a 3rd party survey partner (SMD) in order to maintain confidentiality. The survey will ask specific questions to understand how DUHS can improve things that may increase our resilience and well-being. The effort will also check how we’re doing with our effort to increase our diversity, inclusion and belonging. We will use your thoughts to guide these efforts going forward. Please participate.
Duke Voice Mail upgrade, Dec. 10
On the evening of Thursday, December 10, the Office of Information Technology (OIT) will upgrade Duke’s voice mail system and move it to new servers. Users will not lose access to voice mail during the cutover. After the cutover:
- New messages will be available immediately and can be accessed as usual from 919-613-MAIL (6245).
- Messages up to 12 months old will be migrated to the new servers. These may not be available for up to 48 hours, while they are imported. Users may access messages on the old servers by calling 919-385-0090 and following the standard procedure for listening to messages (see https://oit.duke.edu/help/articles/kb0025163).
- Messages older than 12 months will not be migrated. These messages may be recovered upon request by contacting the Service Desk (see below).
OIT expects the import will be complete by 6:00am on Monday, December 14.
If users experience any issues with voice mail, they should contact their Service Desk:
- Duke Health Service Desk, 919-684-2243 or http://dhts.duke.edu
- OIT Service Desk, 919-684-2200 or https://oit.duke.edu/help
COVID-19 Updates:
All the latest official DUHS information regarding coronavirus/COVID-19 response at the following locations:
NOTE: A reminder that Pulse will not be published on Dec. 27 or Jan. 3 so that we may enjoy some time off.
Upcoming Opportunities/Save the Date:
Cardiology Grand Rounds
Dec. 8: Duke Faculty/Fellow grand rounds — COVID plans updates
Dec. 10: Cardio-Pulmonary Joint Grand Rounds: Ryan Tedford of MUSC, Assessment of Right Ventricular Function: The Role of RV-PA Coupling and RV Reserve. 12 pm, Webex.
Dec. 22: No Cardiology GR. Happy Holidays!
Dec. 29: No Cardiology GR. Happy Holidays!
Moments to Movement Virtual Town Hall, Dec. 7
 Join us for our next Moments to Movement (M2M) virtual town hall on Monday, Dec. 7 from 4:30 to 5:30 p.m. During this town hall, leaders will discuss the Duke University School of Medicine’s work to dismantle racism and create a just, diverse and equitable school and community. Submit questions in advance to M2M@duke.edu.
Join us for our next Moments to Movement (M2M) virtual town hall on Monday, Dec. 7 from 4:30 to 5:30 p.m. During this town hall, leaders will discuss the Duke University School of Medicine’s work to dismantle racism and create a just, diverse and equitable school and community. Submit questions in advance to M2M@duke.edu.
Join the Zoom meeting here.
Radiothon for Duke Children’s Dec. 15-16
The annual Radiothon for Duke Children’s will be held on Dec. 15-16. Tune in to MIX 101.5 FM during the Radiothon to hear  incredible and moving stories from our Duke Children’s patient families and pledge your support. Together, we can continue to advance care and give hope to the children and families who need it most. Donate today at bit.ly/DukeRadiothon2020.
incredible and moving stories from our Duke Children’s patient families and pledge your support. Together, we can continue to advance care and give hope to the children and families who need it most. Donate today at bit.ly/DukeRadiothon2020.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged.
Duke Heart in the News:
November 24 — Joseph Rogers
News & Observer
North Carolina hits record hospitalizations again as new mask rules set to take effect
https://bit.ly/39BXIT5
November 25 — Tracy Wang
Medscape
Fish Oils and CV Prevention — Now What?
https://www.medscape.com/viewarticle/940810
December 1 — Muath Bishawi and Amanda Randles, Mike Kaplan & Simbarashe Chidyagwai (Biomedical Engineering)
Microsoft/the AI Blog
https://bit.ly/3olE1Da
December 1 — Joseph Rogers
CBS17/WNCN
Some Triangle hospitals expecting to have a COVID-19 vaccine in as few as 2 weeks
https://bit.ly/3mBGFUR
December 2 — Amanda Randles (Biomedical Engineering)
Becker’s Hospital Review
Duke University, Microsoft develop ventilator splitting tech for COVID-19 patients
https://bit.ly/37vsXN3
Thanksgiving Week 2020 – Duke Heart Updates
Updates from the Week:
Mentz Named Editor-in-Chief, Journal of Cardiac Failure

We are happy to share that Rob Mentz has been named the new Editor-in-Chief of the Journal of Cardiac Failure, the official journal of the Heart Failure Society of America and the Japanese Heart Failure Society.
Mentz is an associate professor of medicine in the Division of Cardiology and is our Chief of the Heart Failure Section. He assists with the care of patients with heart failure, cardiac transplants, and ventricular assist devices at Duke University Hospital. He is an NIH and industry-funded clinical trialist involved in ongoing trials designed to inform the care of cardiac patients.
Author of more than 300 peer-reviewed publications, Mentz has also authored several book chapters (including Braunwald’s Heart Failure textbook), was a topic editor for the Heart Failure Self-Assessment Program (HF-SAP) and a writer for the ACCSAP on heart failure. He has also served as an Associate Editor for Circulation: Heart Failure.
“I am honored to take on the role of editor-in-chief of the Journal of Cardiac Failure,” said Mentz. “I look forward to serving the HFSA members as well as the broader heart failure community as we work to publish high-quality original research, reviews, scientific statements and position pieces that are interesting and practice changing. I’m eager to collaborate with the talented editorial team and HFSA leadership to elevate the journal to new heights and bring increased awareness to the field.”
Launched in 1994 and a joint endeavor by the Heart Failure Society of America and the Japanese Heart Failure Society, the Journal of Cardiac Failure publishes peer-reviewed manuscripts of interest to clinicians and researchers in the field of heart failure and related disciplines. These include original communications of scientific importance and review articles involving clinical research, health services and outcomes research, animal studies, and bench research with potential clinical applications to heart failure. The Journal also publishes manuscripts that report the design of ongoing clinical trials and editorial perspectives that comment on new developments pertinent to the field of heart failure or manuscripts published in other journals.
Mentz will begin his term as Editor-in-Chief on December 1.
In Memoriam: John J. Gallagher, MD
We were saddened this week to learn of the passing of Dr. John J. Gallagher, a pioneer in clinical cardiac electrophysiology and a beloved mentor and former faculty member at Duke.
 We are grateful to Drs. David Benditt and Eric Prystowsky for sharing the following tribute with Pulse:
We are grateful to Drs. David Benditt and Eric Prystowsky for sharing the following tribute with Pulse:
John J. Gallagher, MD was born in Brooklyn, New York on March 3, 1943. He received a B.S. in physics from Holy Cross in Worcester, MA, and an MD Cum Laude from Georgetown University School of Medicine in 1968. Thereafter, John moved to Duke where he completed his internship and residency in Internal Medicine in 1970, after which he joined the US Public Health Service as a research associate in the Cardiopulmonary Laboratory at Staten Island. It was there that he became strongly influenced by the early advances in clinical cardiac electrophysiology taking place in Dr. Anthony Damato’s laboratory.
In 1972, John returned to Duke as a Fellow in Cardiology, and joined the faculty as an Assistant Professor of Medicine in 1974. Under the guidance of then Chief of Cardiology, Dr. Andrew Wallace, John quickly became a principal driving force behind Duke’s rapidly growing reputation as a world leader in basic science and clinical cardiac electrophysiology. In this setting, allied principally with Will Sealy, MD of the Department of Surgery, John pioneered electrophysiological evaluation and surgical cure of patients with Wolff-Parkinson-White syndrome and related forms of ventricular preexcitation. Working with a talented technical (in particular Jackie Kassel) and surgical team (notably Dr. Sealy, as well as Robert Anderson, MD; Jimmie Cox, MD; and Steve Ring, MD), John devised the ‘sock-map’ technique for computer-based epicardial activation sequence mapping, and was among the first to innovate the use of cryoablation in arrhythmia surgery.
In 1980, John was appointed Edward S. Orgain Professor of Medicine at Duke University attesting to his many accomplishments. In the years leading up to and following this appointment, John’s efforts attracted worldwide attention, and his laboratory became a magnet for post-graduate trainees. We count ourselves fortunate to have been among these; some others in alphabetic order included Gust Bardy, MD; Ronnie Campbell, MD; Larry German, MD; Roosevelt F. Gilliam, MD; Augustus Grant, MD; Stephen Hammill, MD; Charlie Kerr, MD; George Klein, MD; Douglas Packer, MD; Edward L.C. Pritchett, MD, and Andrew Tonkin, MD to name a few. Many of John’s students subsequently became noted teachers, innovators and thought leaders in cardiac electrophysiology around the world.
In 1983, John moved to Charlotte, NC, where he became Director of Electrophysiology at the Carolinas Medical Center and Carolinas Heart Institute. In that position, he continued to be regarded internationally as one of cardiac electrophysiology’s most masterful analysts of complex arrhythmias. Later in life, John became an avid horseman and enjoyed the country life. Despite multiple health issues over the years, John maintained an extensive hospital-based practice until his untimely death this past month.
As a teacher, John Gallagher was unfailingly passionate and uncompromising. He always demanded clear thinking, detailed analysis, precise writing, and the most attentive patient care. He demonstrated to us how one could pursue physiologic research in the clinical electrophysiology laboratory with the same rigor demanded in basic research. He was never easily pleased. These qualities, and a sometimes unpredictable demeanor, combined to incite trepidation even among his most talented trainees. Nevertheless, his students also recognized the quality of education they were receiving, and that their mentor was in fact a warm and thoughtful individual, with a marvelous sense of humor, and a nose for a good time. John’s passing is a great loss to cardiology, and especially to the worldwide EP community that has long admired his skill and intellect.
We offer our sincere condolences to his family, colleagues and many friends. May his memory be a blessing.
David G. Benditt, MD
Professor of Medicine, University of Minnesota, Minneapolis, Minnesota
Eric N. Prystowsky, MD
Consulting Professor, Duke University Medical School
St. Vincent’s Medical Center, Indianapolis, Indiana
Duke Heart to Serve as Presenting Sponsor of 2021 NC Walk for Victory
We are pleased to share that Duke Heart, on behalf of the Duke Center for Aortic Disease, will again serve as the Presenting Sponsor for the North Carolina Walk for Victory. The event raises awareness of and funds to support The Marfan Foundation. Dr. Chad Hughes, director of the Duke Center for Aortic Disease will serve as the 2021 Medical Chair of the event, which is scheduled for April 17, 2021 from noon to 3 p.m. at Laurel Hills Park in Raleigh. If it becomes evident that a safe in-person, physically distanced event is not possible at that time, the event will be held virtually on the same date.
COVID-19 Updates:
All the latest official DUHS information regarding coronavirus/COVID-19 response at the following locations:
NOTE: Pulse will not be published on Dec. 27 or Jan. 3 so that we may enjoy some time off.
Upcoming Opportunities/Save the Date:
Nov. 30: Translating Duke Health-CV Symposium. 9-11:15 am. Virtual. To register, please visit: https://duke.qualtrics.com/jfe/form/SV_eXSYvFY7Luu2LJ3
Please try to attend – should be a good update on our progress with TDH-CV.
Cardiology Grand Rounds
Dec. 1: Fellow presentation with Vishal Rao. 5 pm, Webex.
Dec. 8: Heart Center Grand Rounds (multi-disciplinary): DCD Heart Transplantation. 5 pm, Webex.
Dec. 10: Cardio-Pulmonary Joint Grand Rounds: Ryan Tedford of MUSC, Assessment of Right Ventricular Function: The Role of RV-PA Coupling and RV Reserve. 12 pm, Webex.
Dec. 22: No Cardiology GR. Happy Holidays!
Dec. 29: No Cardiology GR. Happy Holidays!
Conferences, Symposia & Webinars
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged.
Duke Heart in the News:
November 23 — L. Kristin Newby
Medscape
Many Patients With Type 2 MI Don’t Get Cardiologist Evaluation
https://www.medscape.com/viewarticle/941462
Duke Heart Week Ending November 22nd 2020
Highlights of the week:
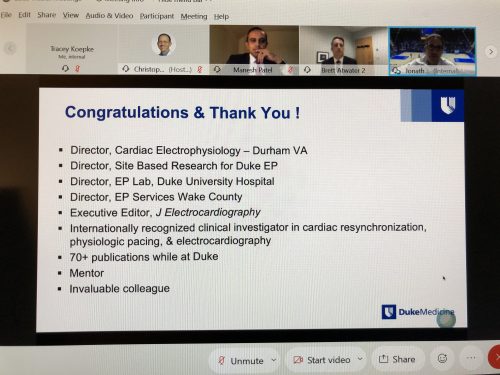
Brett Atwater Celebrated During CGR; Headed to Inova
The team celebrated Brett Atwater and his contributions to Duke Electrophysiology (and the overall field) in a special Cardiology Grand Rounds held Nov. 17. Most of you are aware that Atwater has been named Director of Cardiac Electrophysiology and Electrophysiology Research at the Inova Heart & Vascular Institute in Fairfax, VA; his new position is effective December 14.
During this special CGR virtual event, we heard from an array of presenters, including two of his mentees: Daniel Friedman (Yale) and Zak Loring (Duke EP Fellow), as well as Jon Piccini and Manesh Patel.
We wish you and your family all the best with your move to Fairfax, Brett! You will be missed but we look forward to lots of collaboration.
AHA Scientific Sessions Wraps Up
We want to thank all of our faculty and fellows for the dedication and presentations.
Please find a slide from Dr. Fauci’s presentation at AHA on the vaccines.

Duke Regional Named Among Top 50 CV Hospitals for 2021
IBM Watson Health has released its annual ranking of 50 top hospitals for cardiovascular care in collaboration with Fortune. Duke Regional Hospital has again made their list – a link to the story appears in our news list, below (see Becker’s Hospital Review). This is terrific recognition of the extraordinary care our team provides there every day. Special thanks to Shu Lin for his excellent leadership there – we are proud of the work your team is doing!
Remembrance: Joe Greenfield, MD
We received the following note last weekend from David Benditt, MD:
I have been reading the wonderful memories of Joe Greenfield published in Pulse (11-15-20). Several comments focused on his invaluable and so often unanswerable criticisms offered at Rounds. These brought to mind an experience dating to the late 1970s. As a Fellow, I presented a case of Carotid Sinus Syndrome focusing on the mystery of the vasodepressor mechanism in Reflex faints. After what I perceived to be a thoughtful examination of a difficult unknown, Joe simply but politely said (I paraphrase as so many years have passed), “Thank you, David, but I think you will find that ‘beta-adrenergic blockade’ will take care of it.” I was very much taken aback by the certainty of his remark. How could I have missed something so obvious? Of course, that was not Joe’s point at all. The gauntlet had been thrown. The challenge was to dig deeper and ultimately to derive new science and better understanding. Now, more than 40 years later, having made some progress, I am still working on the mystery, and many times a year, I silently thank Joe for the remark that focused a career.
With fond memories,
David G. Benditt, MD,Professor of Medicine, Cardiac Arrhythmia Center, University of Minnesota, Minneapolis
Duke Heart Clinics Hold Thanksgiving Food Drive
The Duke Southpoint and South Durham Cardiology Clinics sponsored a Thanksgiving food drive to collect items that will be given to the Durham Rescue Mission. Carolyn Richards, Foretta Davis and Phyllis Upchurch helped organize the drive, which collected three tables worth of donations. Special thanks to Annette Moore for sharing this news with us.
Great job, everyone – and thanks to all who donated!


CICU Move Successful
Our Cardiac Intensive Care Unit (CICU) moved this weekend from DUH 7700 to DMP 7E. Many thanks to the staff and provider teams for making this a successful move – Greg Flynn and our CICU nurses did an amazing job of facilitating the process. Great job everyone!!!



Duke Heart Leadership Council Holds Fall Meeting
The Duke Heart Leadership Council met virtually on Friday afternoon. Three new members were introduced: Dennis Wicker, Chuck Swoboda and Julian “Brad” Branch were warmly welcomed. The meeting, led by Council chair Bob Keegan, included a tribute to Phil Kohl, a member of the Council who passed away earlier this year. He was recognized as a great advocate with a competitive spirit who will be deeply missed. Peter Smith and Manesh Patel provided an overview of our work and accomplishments over the past year, particularly as we dealt with COVID; Edward Chen, incoming CT Surgery division chief was introduced to the members, and the Council heard an engaging presentation by Eric Richardson of Duke Design Health.

Register Now: TDH-CV Symposium, Nov. 30
Please plan to join us for the Translating Duke Health Cardiovascular Disease symposium on Monday, Nov. 30 from 9 to 11:15 am. This will be a virtual event to update our community on the latest findings among our funded projects. To register, please visit: https://duke.qualtrics.com/jfe/form/SV_eXSYvFY7Luu2LJ3
Updated Grief Resources Available
A free half-day virtual symposium called Matters of Grief was held this week and moderated by Anthony Galanos (Geriatrics/Palliative Care); it included a presentation by Jessica Regan, who is the Duke Cardiovascular Research Center’s 2020 Mandel Fellow. New and updated resources were presented for addressing grief not only in our personal lives, but grief arising in the workplace through the loss of colleagues, mentors or patients. All materials can be accessed via: bit.ly/mattersofgrief
Grief is a normal part of the course of human life and each of us will have unique experiences with it. Importantly, grief is not always the result of a death. It can be tied to other types of losses, too. The resources made available at Duke have been enriched over the past year in light of the pandemic. There are materials that address ways to support others or to help yourself through the very real grief we will all, at some point, endure.
The Matters of Grief website is well put together and easy to navigate. We highly recommend acquainting yourself with the resources available there – which, by the way — are available to anyone, anywhere – please share them inside and outside of Duke.
As you navigate the upcoming holidays, stay safe and please take care of yourselves!

COVID-19 Updates:
All the latest official DUHS information regarding coronavirus/COVID-19 response at the following locations:
NOTE: Pulse will not be published on Dec. 27 or Jan. 3 so that we may enjoy some time off.
Upcoming Opportunities/Save the Date:
Cardiology Grand Rounds
Nov. 24: Overview of 2020 AHA Scientific Sessions with Kristin Newby. 5 pm. Webex.
Dec. 1: Fellow presentation with Vishal Rao. 5 pm, Webex.
Dec. 8: Heart Center Grand Rounds (multi-disciplinary): DCD Heart Transplantation. 5 pm, Webex.
Dec. 10: Cardio-Pulmonary Joint Grand Rounds: Ryan Tedford of MUSC, Assessment of Right Ventricular Function: The Role of RV-PA Coupling and RV Reserve. 12 pm, Webex.
Dec. 22: No Cardiology GR. Happy Holidays!
Dec. 29: No Cardiology GR. Happy Holidays!
Conferences, Symposia & Webinars
Nov. 30: Translating Duke Health-CV Symposium. 9-11:15 am. Virtual. To register, please visit: https://duke.qualtrics.com/jfe/form/SV_eXSYvFY7Luu2LJ3
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged.
Duke Heart in the News:
November 12 — Yuichiro Yano (Family Medicine & Community Health)
Medscape
Masked Asleep Hypertension Common in US Adults
https://www.medscape.com/viewarticle/940875
November 13 — Pamela Douglas
tctMD/the heart beat
SCAPIS: CTA Finds Silent CAD in 42% of Middle-aged Adults
https://bit.ly/33k5gpV
November 13 — Pamela Douglas
Medscape
SCAPIS: Simple Questionnaire Can Identify Silent Atherosclerosis
https://www.medscape.com/viewarticle/941000
November 13 — Manesh Patel
tctMD/the heart beat
As US Cardiologists Mull a Biden Presidency, COVID-19 Trumps All
https://www.tctmd.com/news/us-cardiologists-mull-biden-presidency-covid-19-trumps-all
November 13 — Jonathan Piccini
Medscape
Omega-3 Caps, Vitamin-D Both Fail for Atrial Fib Primary Prevention: VITAL-Rhythm
https://www.medscape.com/viewarticle/941002
November 14 — Eric Peterson
Healio.com/Cardiology Today
BP control, frequency of measurements minimally impacted during COVID-19
https://bit.ly/2ULwTU0
November 15 — L. Kristin Newby
Medpage Today
Omega-3s Humbled by Corn Oil Placebo in Two Trials
https://www.medpagetoday.com/meetingcoverage/aha/89683
November 17 – Duke Regional Hospital
Becker’s Hospital Review
50 top cardiovascular hospitals for 2021, ranked by IBM Watson Health
https://bit.ly/2UKCzgT
November 18 — Manesh Patel
Medscape
No Extra Cardiopulmonary Event Reduction With High-Dose Flu Vaccine
https://www.medscape.com/viewarticle/941188
November 20 — Pamela Douglas
Physician’s Weekly
AHA: Silent CVD Common in ’Healthy’ People
https://bit.ly/3pHpCTv
Duke Heart Week ending November 15th 2020
American Heart Association Scientific Sessions are Underway
The virtual AHA Annual Scientific Sessions is underway, filled with great science and lots of interaction despite the pandemic. Some of the Highlighted Duke presentations can be found on the DCRI webpage: https://dcri.org/dcri-aha, including news briefs on RIVER (with Renato Lopes and John Alexander) and GALACTIC-HF (with Mike Felker). Of note, Pamela Douglas is presenting the annual Laennec Clinician/Educator Lecture. Her presentation is titled, “Imaging, Imaging Quality and Chest Pain Evaluation” We also had several faculty involved in moderating and discussing late breaking clinical trials. The AHA also had an vitally important opening session on Structural Racism and mechanisms to change. The sessions with several faculty and fellow presentations will be on-demand until January.




ACC Clinical Trials Research: Upping Your Game
Pam Douglas, Tracy Wang and Minnow Walsh (St. Vincent Heart Center), are planning committee co-chairs for the ACC Clinical Trials Research: Upping Your Game program this year. The course is part of the ACC’s Diversity and Inclusion Initiative and seeks to support cardiologists and PhD researchers who are seeking to succeed in clinical research. The course kicked off this month with a virtual two-day session. Larry Jackson was in attendance as well as some former Duke fellows/faculty, including Melvin Echols and Gwen Bernacki. To learn more, please visit: https://bit.ly/35ur1EO
Save the Date: TDH-CV Symposium, Nov. 30
Please plan to join us for the Translating Duke Health Cardiovascular Disease symposium on Monday, Nov. 30 from 9 to 11:15 am. This will be a virtual event to update our community on the latest findings among our funded projects. Agenda:
9:00-9:05 am Welcome, Overall TDH Updates – Manesh Patel
Session I
9:05-9:30 am Translating Duke Health Scholar Highlight, Aravind Asokan
9:30-9:55 am Pilot Project Awardee, Hope Weissler and Ricardo Henao
9:55-10:05 am Moderated Q&A Session I
10:05-10:15 am BREAK
Session II
10:15-10:40 am Translating Duke Scholar Highlight, Mei Liu
10:40-11:05 am Pilot Project Awardee, Conrad Hodgkinson
11:05-11:15 am Moderated Q&A Session II
11:15 am Closing and Thank You
To register, please visit: https://duke.qualtrics.com/jfe/form/SV_eXSYvFY7Luu2LJ3

Celebrating Duke Heart NPs
We’ve just wrapped up celebrating National Nurse Practitioners Week, which runs November 8-14, in recognition of the NP  profession and its contributions to the nation’s health. In the midst of this challenging year, we are deeply grateful for the efforts and contributions of these vital members of the Duke Heart team.
profession and its contributions to the nation’s health. In the midst of this challenging year, we are deeply grateful for the efforts and contributions of these vital members of the Duke Heart team.
NP Week is the ideal time to celebrate the high-quality health care NPs provide through more than 1 billion patient visits each year. This year is particularly special as 2020 marks the 100th birthday of Dr. Loretta C. Ford, the co-founder of the first NP program at the University of Colorado and the first champion of the NP role.
As highly skilled multidisciplinary care team members, NPs provide exceptional patient care in virtually all medical specialties and settings. NPs are pivotal in the nation’s health care deliver and serve in critical roles throughout patient care, medical education, health administration, leadership, and research.
A very special thank you to all NPs throughout Duke Heart for the great work you’re doing!
Shout-Out to Kesler!
Many thanks to Autumn Kesler, one of our amazing cardiology nurses, for going above and beyond for our patients! Jen Rymer shared the following with Pulse:
“We had a patient scheduled to see me who was coming from Virginia, had limited access/resources, and had a special van bringing him. Autumn had already put in a lot of effort to get him to the appointment. The patient got lost for the appointment in the parking lot after checking in, and Autumn went out to look for the patient and retrieve him. She brought him upstairs, made sure to walk him to get labs, and escorted him to his van so he wouldn’t get lost again. In addition to this example, she brought stickers for an appointment I had with a patient who has developmental delays and loves Paw Patrol characters.
During these tough times, when so many of our patients are struggling, I think we can all learn a lesson from Autumn. Patient care is not just about the clinical decisions that are made, but making sure the experience is hopefully a good one too!”
We completely agree! Way to go, Autumn!
Moments to Movement Features Kevin Thomas
Held on Nov. 12, the Duke’s Moments to Movement series continued with the panel discussion Clinicians on Racism and Health Inequities featuring Duke Heart’s Kevin Thomas as one of the panel participants. Additional panelists included Theresa Williamson (NSU resident); Vicky Ortho of Duke Regional; and Rick Shannon, Chief Quality Officer, Duke Health. Thanks to all who were able to join the discussion.
Publication Lands Among Top 10 in JAMIA
We learned this week that a manuscript co-authored by Jedrek Wosik, Marat Fudim, Blake Cameron, Ziad Gellad, Alex Cho, Donna Phinney, Simon Curtis, Matthew Roman, Eric Poon, Jeff Ferranti, Jason Katz, and Jimmy Tcheng is listed at #2 among the Top 10 articles in Journal of the American Medical Informatics Association (#1 journal in the informatics space) for the past 12 months. Congrats to the full team! To see their publication, Telehealth transformation: COVID-19 and the rise of virtual care, please visit: https://academic.oup.com/jamia/article/27/6/957/5822868
COVID-19 Updates:
All the latest official DUHS information regarding coronavirus/COVID-19 response at the following locations:
Upcoming Opportunities/Save the Date:
Cardiology Grand Rounds
Nov. 17: Special CGR: Celebrating Dr. Brett Atwater’s Contributions to EP. 5 pm, Webex.
Our speakers will include:
- Jonathan Piccini – Introduction
- Daniel Friedman (Yale) – Physiology, Pathophysiology, & Epidemiology of LBBB in HFpEF and HFmrEF: Opportunities for Resynchronization
- Zak Loring – Use of Electrocardiographic Patterns to Improve Patient Selection for Device Therapies
- Brett Atwater – The Future of Innovation in EP
Nov. 24: Kristin Newby, Overview of the 2020 AHA. 5 pm. Webex.
Conferences, Symposia & Webinars
Nov. 19: Matters of Grief: The Duke Response. 1-5 p.m.
A free half-day symposium where we will learn about ways that we can support each other through both personal and professional grief, share stories of support, and identify resources available at Duke.
Matters of Grief: The Duke Response will feature diverse and multidisciplinary panels, engaging didactic sessions, and surprise guests from across the university. Just some of the highlights include:
- Coach K delivers a special message
- Duke medical students will discuss the research behind grief and finding support through peers
- Well-Being experts and Duke Health leadership discuss normalizing discussions about grief
The virtual event runs from 1-5PM on November 19th, 2020. Sessions will be recorded for those who cannot attend the live event. Reserve your space today at bit.ly/mattersofgrief
Nov. 30: Translating Duke Health-CV Symposium. 9-11:15 am. Virtual. To register, please visit: https://duke.qualtrics.com/jfe/form/SV_eXSYvFY7Luu2LJ3
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged.
Duke Heart in the News:
November 10 — Manesh Patel
Medpage Today
AHA Meeting Spotlights HF Management, Statin Acceptance
https://www.medpagetoday.com/meetingcoverage/aha/89594
November 10 — Thomas Price (endocrinology)
US News & World Report
AHA News: Early Menopause Predicts Early Heart Trouble for White Women
https://bit.ly/3ndnsIY
(*also carried by 8 additional outlets including in Little Rock, Colorado Springs & West Palm Beach)
November 10 — Jay Shavadia
Healio/Cardiology
Statin use may not meaningfully reduce CV events in patients on dialysis
https://bit.ly/35xQYTR
November 11 – Joseph Rogers
WRAL
NC’s COVID hospitalizations at an all-time high. Here’s who is the sickest
https://bit.ly/2Ulswie
November 11 — Chetan Patel
News & Observer
Duke Hospital expands pool of heart donors. Now it has reached a transplant milestone.
https://bit.ly/2IAjX0b
(This story was carried by 7 additional outlets including in Charlotte, Durham & Myrtle Beach)
November 11 — Schuyler Jones
tctMD/the heart beat
PCI at Ambulatory Centers: More Bleeding but No Penalty in Overall Outcomes
https://bit.ly/2GTnrdN
November 11 — Jason Katz
Medpage Today
Patient’s Ventricles Removed as Bridge to Heart Transplant
https://www.medpagetoday.com/surgery/thoracicsurgery/89615
November 12 — David Pisetsky (rheumatology & immunology)
Healthcentral.com
Here’s Why Having RA Increases Your Heart-Disease Risk
https://bit.ly/35Cnu7D
November 12 — Michael Nanna
tctMD/the heart beat
Statin Benefits Confirmed in Elderly, Along With Harmful Effects of High Cholesterol
https://bit.ly/3f2yHBe
Duke Heart Week Ending November 8th 2020
Chief’s message:
Duke Heart Center is pleased to announce the Hearts of Athletes Program with philanthropic support from the Joel Cornette Foundation.
During development the cardiovascular system forms in a uniform way. A young person’s environment, exposure to sports, nutrition, other elements then affect the development of the heart and the cardiovascular system. Along this spectrum some individuals become world-class athletes. As they do so, the ability to determine variation on normal compared to disease anatomy, function can be difficult. To date the scientific community has lacked a large “library” with information/data on the spectrum on hearts of people who have performed at the highest levels of athletic competition. Additionally, once done competing in high level sports there is little guidance on the management and medical care of the cardiovascular system. This problem has only been exacerbated with COVID-19, an infectious disease that has posed an unprecedented public health challenge and has been reported to involve the heart. Recent reports have identified inflammation of the heart – termed myocarditis.
For young adults, student athletes, and others without known cardiovascular disease, the true incidence of myocardial involvement after COVID-19 infection and the rate of detection via different testing modalities is not known. This has led to differential testing programs and return to athletics around the United States.
It is with this background and the generous support from the Joel Cornette Foundation, that the Duke Heart Center lead by Dr. Manesh Patel will be launching the Hearts of Athletes Program, aimed at recruiting college athletes both with and without COVID-19 to help identifying the rate of myocardial involvement and effects on their ability to return to athletic activity. The study will capture cardiovascular imaging including cardiac MRI studies on these athletes.
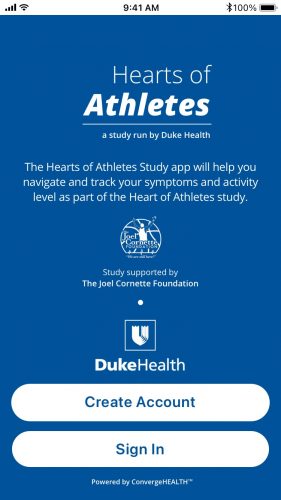 Dr. Patel noted, “We will leverage our expertise in Sports Cardiology with Bill Kraus, electrophysiology expertise with Jim Daubert, and Cardiac MRI imaging from our group including Han Kim and Igor Klem. This study will provide critical information linking symptoms, physical activity, and cardiac imaging in athletes with and without COVID-19 – allowing us to start to understand both the disease and the athletic heart. We are honored to gain the support of the Christi Cornette and the Joel Cornette Foundation, without whom we wouldn’t have been able to quickly start this study. Having met Christi Cornette and understanding her vision to improve the lives of athletes in honor of Joel, we are humbled to partner with the foundation.” The study will shortly be recruiting via a novel Hearts of Athlete’s Study APP that will allow athletes to capture their symptoms and cardiovascular images.
Dr. Patel noted, “We will leverage our expertise in Sports Cardiology with Bill Kraus, electrophysiology expertise with Jim Daubert, and Cardiac MRI imaging from our group including Han Kim and Igor Klem. This study will provide critical information linking symptoms, physical activity, and cardiac imaging in athletes with and without COVID-19 – allowing us to start to understand both the disease and the athletic heart. We are honored to gain the support of the Christi Cornette and the Joel Cornette Foundation, without whom we wouldn’t have been able to quickly start this study. Having met Christi Cornette and understanding her vision to improve the lives of athletes in honor of Joel, we are humbled to partner with the foundation.” The study will shortly be recruiting via a novel Hearts of Athlete’s Study APP that will allow athletes to capture their symptoms and cardiovascular images.
Christi Cornette stated “We are excited to work with the Cardiology group at Duke and Dr. Patel to identify ways to help better understand COVID-19 and support athletes during this time. We are confident that research like this will improve our understanding of athlete’s heart so that we may prevent and improve their lives.
Dr. Patel noted that the Duke group is also working with several sports medicine colleagues to coordinate the efforts of the Hearts of Athlete’s study with ongoing registry work around COVID-19 involvement in NCAA athletes. The group envisions that this program will provide more in depth information needed for both athletes and non-athletes recovering from COVID-19.
Updates from the week:
Nakela L. Cook, MD, MPH gives Eugene Stead Medical Grand Rounds on “PCORI 2.0”
Nakela L. Cook, MD, MPH, is Executive Director at the Patient-Centered Outcomes Research Institute (PCORI). She is a cardiologist and health services researcher with a distinguished career leading key scientific initiatives engaging patients, clinicians, and other healthcare stakeholders at one of the nation’s largest public health research funders.
She provided a fantastic wide ranging talk aimed at providing the vision for PCORI over the next 10 years which included ensuring working to generate patient centered research that improves the outcomes of our communities. She discussed patient engagement, big data, the role of funding and open science and her own journey to PCORI Leadership. Like Dr. Stead, she described the importance of understanding the whole person, removing disparities and inequities in health, and how we will be working in research and care delivery to do that.

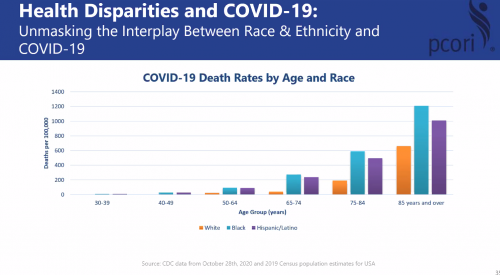

EP Updates:
Kevin Jackson Named Director of Duke Center for Atrial Fibrillation

We are very pleased to announce that Kevin Jackson, MD will be assuming the role of Director of the Duke Center for Atrial Fibrillation at Duke University. Dr. Jackson completed his residency training at UCSF and his cardiology and electrophysiology fellowships at Duke before joining the faculty in 2007. Dr. Jackson is a key leader and recognized expert in the treatment of atrial fibrillation locally and across the country. He provides care for AF throughout our health system, including at Duke University Hospital, Duke Raleigh Hospital, and through HeartCare Plus at Wake Med in Wake County. He is uniquely poised to help lead our care efforts in this arena. Dr. Jackson will be working with Janice Febre, RN (DCAF Nurse Coordinator) to improve the consistency and data-driven approach within our hospitals and clinics. I am very pleased to see Dr. Jackson take on this new role. He has a strong reputation as a top notch clinician in our community and excels at efficient and high-quality care delivery. Please congratulate KJ when you see him.
Rebeccal Yapejiaan elected Associate of the ACC
Sana Al Khatib shared great news this week. “I am writing to share with you the great news that Rebecca Yapejiaan – one of our EP NPs, was just elected as an Associate of the ACC. The approval happened in record time (24 hours)”. Congrats Rebecca – well deserved

American Heart Associate Scientific Sessions to Start this week.
Many of our Faculty and Fellows will be presenting at the upcoming Virtual AHA sessions. The sessions will have an all star cast of Keynote Speakers including Dr. Toni Fauci on the Cardiovascular Effects of COVID-19. We will also have many of our Faculty and fellows presenting, with many faculty moderating and involved with Late Breaking Science.

Registration Links can be found here: the website
Image of the Week:
After a contentious political season – Joe Biden was declared President-Elect with Kamala Harris as Vice-President Elect. Hopefully our country that has been deeply divided will find a way towards common ground and a way forward for some of the most pressing issues in our country right now – many of which touch our lives in health care. No matter what your political beliefs, the election of the first woman, a women of color as Vice-President elect is historic, hopeful and inspiring to generations.

COVID-19 Updates:
All the latest official DUHS information regarding coronavirus/COVID-19 response at the following locations:
Upcoming Opportunities/Save the Date:
Cardiology Grand Rounds
Nov. 10: Michelle Kelsey – Presenting Morbidity and Mortality Case to the Faculty and Fellows
Nov. 17: Special Grand Rounds – Celebrating Brett Atwater’s Contributions to EP
Conferences, Symposia & Webinars
Nov. 13: 12th Annual NC Research Triangle Pulmonary Hypertension Symposium. Noon – 4:30 p.m. For more information, please visit this page. This event will be held virtually and is co-sponsored by Duke and the University of North Carolina in partnership with the Pulmonary Hypertension Association through the Building Medical Education in PH program. Please join us!
Nov. 13–17: AHA Scientific Sessions 2020, a virtual experience. Registration is now open. See the website for details.
Conversations with Colleagues: A Deeper Dive on Racial Justice
During the initial Conversations with Colleagues (CwC): Racial Justice sessions attendees shared that they wanted a deeper dive and more action steps related to racial justice. During this next edition of CwC attendees will sign up for 6 weeks of conversations. Participants will be placed into small cohorts and will walk with this same group of colleagues throughout the entire 6 weeks. These cohorts will allow staff to build relationships, have colleagues to bounce ideas off of and have accountability partners to help them stay true to the mission of the deeper dive. You will read articles, watch videos and engage in other activities that will deepen your knowledge about racial justice. Attendees will also learn action steps that they can take to make a difference.
Dates/Links for CwC
The conversations will take place weekly, starting this week and running through 12/7 (with a break Thanksgiving Week). Conversations will be 1 hour long.
Mondays 2-3pm (10/16 – 12/7)
https://duke.zoom.us/meeting/register/tJUvdOCqrDgsEtQYipTJ7F4eZnPQZFTIx2ZD
Tuesdays 8-9am (10/27 – 12/8)
https://duke.zoom.us/meeting/register/tJAtde-grTsqGtxJl7M6huHcgA3yFQ18pO6P
Wednesdays 12noon-1pm (10/28 – 12/9)
https://duke.zoom.us/meeting/register/tJUkce-rqjIrHdPmAvmnM_L0GEaFrkeFZq5L
Thursdays 5-6pm (10/29 – 12/10)
https://duke.zoom.us/meeting/register/tJ0lcu6rqTMiEtOIeRMiWtRQcInZLR6LnmPB
Fridays 12 noon-1pm (10/30 – 12/11)
https://duke.zoom.us/meeting/register/tJMrf–trTwrHtB3TEX5B-7UUXW2RgDJWGko
Sundays 4-5pm (11/1 – 12/13)
https://duke.zoom.us/meeting/register/tJEucuqtrjIpGdx8gdnQst1yAS-5NDrgzrD2
Matters of Grief: The Duke Response
On Thursday, November 19th, join us for a free half-day symposium where we will learn about ways that we can support each other through both personal and professional grief, share stories of support, and identify resources available at Duke.
Matters of Grief: The Duke Response will feature diverse and multidisciplinary panels, engaging didactic sessions, and surprise guests from across the university. Just some of the highlights include:
- Coach K delivers a special message
- Duke medical students will discuss the research behind grief and finding support through peers
- Well-Being experts and Duke Health leadership discuss normalizing discussions about grief
The virtual event runs from 1-5PM on November 19th, 2020. Sessions will be recorded for those who cannot attend the live event. Reserve your space today at bit.ly/mattersofgrief
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged.
Have a good week, everyone!
Duke Heart Week Ending November 1st 2020
Chief’s message: Adapting Halloween
Adapting Halloween for COVID-19 was something that we were struggling for a few weeks. I had promised my daughter that I would build a haunted house (in our home) so that she and her brother could have fun without going out. So, it was a nice break from the usual evenings, to be creative and make a scavenger hunt in three rooms with characters from Narnia including our dog as Aslan the lion, clues to solve for treats, and several “spooky areas”. The kids really seemed to enjoy it and we got to spend a bit more time on an evening that in the past has been a race to get around places, feed the family, and get back home. The COVID-19 pandemic has drained all of us of energy and presented challenges that will undoubtedly continue. As we continue to reduce the tragedies, we often struggle to stay vigilant with many of the public health recommendations. This weekend, however, provided a glimpse of how many in our community are adapting and moving forward, something that we continue to see across our health system and Duke Heart. Keeping up the personal and public health battle remains our primary focused mission as we care for our patients and each out.
Highlights of the week:
Halloween: the Kids, the Pets & the Pumpkins!
We hope everyone throughout Duke Heart has had a safe, fun and treat-filled weekend!!! We loved checking out these great costumes – a special hat tip to Jamie Jollis for collecting and sharing these with Pulse.

Shown here are: Jellybean (Sandra Anton’s pup) as a Hot Dog; a couple of pups dressed as wedding attendants; the Pokorney kids as a fireman and Wonder Woman; Katie Thompson’s kids as a dragon and an old lady; Mike Rehorn’s kids as Captain America and a cow. Also included: the contestants in the Cath Lab pumpkin contest. You’re all winners to us!







Celebrating Respiratory Care Week (Oct. 25-31)
Many thanks to all our wonderful respiratory therapists throughout Duke Heart! This was their special week to celebrate. Shown here are some images of our RT group having some fun with our daily COVID-safe treat cart (leadership decorated and brought the cart to the units each shift to prevent any large gatherings with shared food.) We were also able to present a large Thank You card that we have been circulating through the units for a few months (will be framed and will eventually hang in the department).
“In all we were able to celebrate with ice cream sandwiches, breakfast, our ‘Woot! Woot! Express’ cart, and Relax, Reflect, and Recharge gift bags aimed at helping the team to unwind on days off,” said Charlotte Reikofski, DUHS director of Respiratory Care Services. “We’ll wrap up with a full day of 8 Free CEUs and Superlatives on Friday, along with a team hike at Eno Park and COVID-safe Trunk or Treat afterward on Saturday. It has been a great week to celebrate the team!
Thanks for all that you do, Respiratory Care team!!!!



Duke Heart Grows Again!
We are very pleased to share that cardiology APP Tiffany McEwen and her husband Kevin have welcomed their first child. Please join us in welcoming Colton James McEwen, born Oct. 28; 9 lbs., 4 oz., 22”. “Dad, Mom and Colton doing well!

EVS Worker Recognized for Emergency Intervention
On Thursday, Ali Dahham, an Environmental Services associate assigned to 7100 was recognized with a special celebration and certificate to honor his efforts to assist a patient. Thanks to his observation skills and quick-thinking, he noticed a problem with a patient and immediately notified nursing staff. Because of his decision, the patient was able to receive advanced stroke therapies within the appropriate window of time.
“We are all here because we want to make a difference in our patient’s lives. When you think about who saves lives in a hospital, the first thing that comes to mind is the doctors, the nurses or the paramedics, and rightly so,” said Louisa Joy, Duke System Patient Experience Manager. “Rarely do you think of Environmental Services. Housekeepers sanitize patient rooms to keep the patients in a safe environment and at times they come across situations where they play a more active role in saving someone’s life.”
Dahham received a certificate and a star pin. The team helped celebrate with refreshments.
Congratulations, Ali! We are really proud of his actions and we are grateful for the efforts of the full housekeeping staff throughout Duke Heart.
Pictured are: Lisa Pickett, MD, Floreasa Scott, Ali Dahham, Elizabeth Webb, Isaac Johnson, Megan Steele, Brittany Stephenson, Louisa Joy, Julio Rodriguez and several additional staff members.
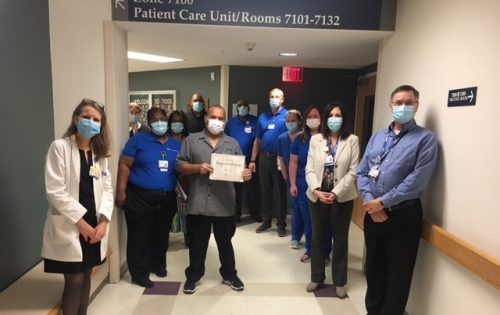
Nazo Honored by CVRC
You may recall that, earlier this year, Nour Nazo was selected as the 2020 CVRC Research Staff Appreciation award recipient. Due to the research curtailment, the team was not able to inscribe Nour’s name on their award plaque until recently. The plaque is located in the lobby of the Duke Cardiovascular Research Center, first floor of the Carl Building.
Congratulations once again, Nour!

Important Reminders
- Election Day is Tuesday. VOTE!
- Please get your Flu Vaccination: All team members must get their vaccination or otherwise demonstrate policy compliance by Tuesday, Nov. 10. Details and resources all available on the Duke Health Influenza Resources site (NET ID required): https://influenza.dh.dukehealth.org.
COVID-19 Updates:
All the latest official DUHS information regarding coronavirus/COVID-19 response at the following locations:
Upcoming Opportunities/Save the Date:
Medicine Grand Rounds: Friday November 8th – 8 AM: Stead Lecture from Nakela Cook, MD, MPH: Envisioning PCORI 2.0: Accelerating Innovation to Implementation
Cardiology Grand Rounds
Nov. 10: TBA
Nov. 17: No CGR. AHA Scientific Sessions
Conferences, Symposia & Webinars
Moments to Movement Series:
Nov. 12, 1 p.m., the Moments to Movement series continues with the panel discussion, Clinicians on Racism and Health Inequities.
Our panel participants are:
- Theresa Williamson, MD, Neurosurgery Resident, Duke University Health System
- Kevin Thomas, MD, Associate Professor, Department of Medicine, Assistant Dean for Underrepresented Faculty Development, Duke School of Medicine
- Vicky Orto, DNP, RN, NEA-BC, Chief Nursing and Patient Care Services Officer, Duke Regional Hospital
- Rick Shannon, MD, Chief Quality Officer, Duke Health
Panelists will discuss how and why people of color experience different clinical outcomes. They’ll explain the meaning of health equity and explain what Duke is doing to ensure the same level of excellence is accessible to all.
To access the livestream, use this link.

Exclusive Event for Duke Community
Nov. 12: Common Hour/Fireside Chat with Adam Silver, T ’84, Commissioner of the NBA and Duke Board Member (named to TIME’s 100 Most Influential People, Fortune’s World’s 50 Greatest Leaders, The Bloomberg 50, etc.). 5 – 6 p.m., Virtual event.
This event will be open exclusively for the Duke Community: faculty, students, staff, alumni, and families both on the university and health system side. This will be an off-the-record conversation with Adam as he touches on many key topics, i.e. his leadership of the NBA during Black Lives Matter & COVID-19 and the NBA’s involvement in China. Registration is available via: bit.ly/AdamSilver. Hosted by Duke University’s Student Government Vice President of Academic Affairs.

Nov. 13: 12th Annual NC Research Triangle Pulmonary Hypertension Symposium. Noon – 4:30 p.m. For more information, please visit this page. This event will be held virtually and is co-sponsored by Duke and the University of North Carolina in partnership with the Pulmonary Hypertension Association through the Building Medical Education in PH program. Please join us!
Nov. 13–17: AHA Scientific Sessions 2020, a virtual experience. Registration is now open. See the website for details.
Matters of Grief: The Duke Response
On Thursday, November 19th, join us for a free half-day symposium where we will learn about ways that we can support each other through both personal and professional grief, share stories of support, and identify resources available at Duke.
Matters of Grief: The Duke Response will feature diverse and multidisciplinary panels, engaging didactic sessions, and surprise guests from across the university. Just some of the highlights include:
- Coach K delivers a special message
- Duke medical students will discuss the research behind grief and finding support through peers
- Well-Being experts and Duke Health leadership discuss normalizing discussions about grief
The virtual event runs from 1-5PM on November 19th, 2020. Sessions will be recorded for those who cannot attend the live event. Reserve your space today at bit.ly/mattersofgrief
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged.
Duke Heart in the News:
October 23 — James Jollis
Medpage Today
Disparities Abound in Chinese Heart Attack Care
https://bit.ly/3jRInPH
October 23 — Victor Dzau
Healio
Speaker: Medical community needs to determine ethics of genomic editing
https://bit.ly/2JgOArV
October 21 — Chetan Patel
WRAL
Duke completes 1,500th heart transplant
https://www.wral.com/duke-completes-1-500th-heart-transplant/19347521/
October 20 — Duke Health
WTVD
1500 Heart Transplants at Duke Health
https://bit.ly/3jPaCyu
October 20 — Stephen Greene
MDEdge.com
Experts tout immediate quadruple therapy for HFrEF patients
https://bit.ly/38e9Ucj
October 20 — Duke Hospital
Becker’s Hospital Review
Healthgrades’ best hospitals for cardiac care 2021
https://bit.ly/380xnNH
October 20 — Betty Tong
MedPage Today
Radiomics Could Help ID Lung Cancer Prognosis After Screening
https://www.medpagetoday.com/meetingcoverage/naclc/89219
October 20 — Betty Tong
MedPage Today
‘License’ to Smoke After Negative Lung Screening?
https://www.medpagetoday.com/meetingcoverage/naclc/89197
October 19 — Adrian Hernandez
Triangle Business Journal (subscription required)
For another Covid-19 study, this Durham CRO is given $44 million
https://bit.ly/3kR10og
October 18 — Manesh Patel
tctMD/the heart beat
Fewer Events and Symptoms With iFR-Optimized PCI, Suggests DEFINE-PCI Trial
https://www.tctmd.com/news/fewer-events-and-symptoms-ifr-optimized-pci-suggests-define-pci-trial
Duke Heart week ending October 25th 2020
Chief’s message: The Greater Good
Hubert Humphrey once said that “the moral test of government is how that government treats those who are in the dawn of life, the children; those who are in the twilight of life, the elderly; and those who are in the shadows of life, the sick, the needy and the handicapped.” This statement has been uttered and is quoted in meetings and actions of Health and Human Services (CMS) in Washington DC. Both Hubert Humphrey, and the greater part of America would have to wait until the promise and potential of President Lyndon Johnson’s “Great Society”. Healthcare progress has always been a slow, and often difficult, and unfortunately political battle, when in many regards it is much more of an economic battle rather than a moral battle. On July 30, 1965, President Johnson traveled to the Truman Library in Independence, Missouri to sign the Medicare Bill into law…which would forever change what it means to be elderly and disabled in America. Something that we all now know moved our nation closer to good. Unfortunately, over the last few weeks we have had more and more members of our community lose their jobs, insurance and access to health care, and even more tragically their lives. This week the cardiology group started to brainstorm ways in which we can grow services including telehealth for minimal or no cost care to ensure medication refills, urgent care identification, and ways to integrate in the growing safety nets programs in our area. This is a small part of what Duke Heart can do and hopefully add to the large local and regional care provided by organizations such as federally accredited community health centers like Lincoln in Durham and others in the area. Regardless of political beliefs or outcomes of elections, we will continue to work in our community to be part of the greater good – the organized efforts to help our community. As the upcoming weeks and months stress our resources, resolve, and community, I am optimistic based on the people at Duke Health that I see every day.
Highlights of the week:
 1500th Heart Transplant Performed at Duke University Hospital
1500th Heart Transplant Performed at Duke University Hospital
Congratulations to the Duke Heart Transplant Program!! The team reached a major milestone recently when they performed the program’s 1,500th heart transplant. Only five other centers in the U.S. have achieved this distinction. We are proud of you and your dedication to excellence!
Taking a look back with Dr. Andrew S. Wechsler, emeritus professor of Cardiothoracic Surgery at Drexel University, who performed Duke’s first heart transplant and who shared part of that story with us this week:
 “The first heart transplant at Duke was performed 1985 on a 55-year-old plumber who was totally disabled by his heart failure. It was the first heart transplant to be performed in North Carolina. The only other nearby centers performing heart transplants were the Medical College of Virginia and the University of Alabama in Birmingham. I had flown to Richmond the week before to observe the procedure.”
“The first heart transplant at Duke was performed 1985 on a 55-year-old plumber who was totally disabled by his heart failure. It was the first heart transplant to be performed in North Carolina. The only other nearby centers performing heart transplants were the Medical College of Virginia and the University of Alabama in Birmingham. I had flown to Richmond the week before to observe the procedure.”
Heart transplants were controversial at that time, according to Wechsler.
“Initially, many transplants performed had problems associated with immune rejection which resulted in most programs ceasing the activity with the exception of MCV and Stanford University. David C. Sabiston, Jr., MD, who was the chairman of the Duke Surgical Department at the time, was initially quite reluctant to allow the procedure and after extensive discussions with me finally agreed to allow the operation if I could obtain permission from the hospital CEO, Dr. Andrew Wallace, a highly respected cardiologist.
“There were concerns about the financial implications of the procedure. Blue Cross finally indicated that they would make payment decisions on a “case by case” basis. Dr. Wallace approved the procedure and the heart team was assembled. It included myself as lead surgeon and Drs. Robert Jones and James Lowe.
The operation was performed on a hot summer day and the helicopter struggled a bit during takeoff, as it was quite full. The donor heart was retrieved from the Eastern part of the state by the operating team. The patient’s recovery was rapid and he was discharged from the hospital in good spirits.”
(See photo, courtesy of Dr. Andrew Wechsler. Shown are Dr. Wechsler, the patient and his wife, as well as various hospital staff members.)
Thirty-five years later, Duke boasts one of the top five centers for heart transplant by volume in the country and offers some of the shortest wait times in the region, according to the Organ Procurement and Transplantation Network.
Incredible work on the part of so many people over the years in order to transform lives. We are especially grateful to the donors and their families for making the decision to donate life.
Passings: Eric S. Williams, MD, Electrophysiologist; Former Duke Fellow
 Eric Sean Williams, MD, a cardiac electrophysiologist at Mercy Clinic Heart and Vascular Hospital (St. Louis, MO) passed away on October 15, 2020. He was 44.
Eric Sean Williams, MD, a cardiac electrophysiologist at Mercy Clinic Heart and Vascular Hospital (St. Louis, MO) passed away on October 15, 2020. He was 44.
Eric was born and raised in Brooklyn, New York. He attended the prestigious Stuyvesant High School and then matriculated at Cornell University, where he earned his Bachelor’s degree in Applied and Engineering Physics. He graduated with honors from Harvard Medical School in 2004. An avid traveler, he spent two years conducting medical research and learning Spanish in Costa Rica during his time in medical school. He then trained at the University of California, San Francisco (UCSF) for his residency in internal medicine, serving an additional year as chief resident before moving to Duke University for his Cardiology fellowship and then University of Washington, Seattle, for his electrophysiology fellowship.
His full obituary can be found here: https://www.luptonchapel.com/obituary/eric-williams-md-facc-fhrs?fh_id=15972.
He is remembered at Duke as a kind and great clinician and friend.We extend our condolences to the Williams family and to his friends and colleagues.
DMP 7 East Moved To 6 East October 24
The cardiothoracic stepdown unit on DMP 7 East moved to DMP 6 East on Saturday, October 24. This was the first move as part of the planned move sequence for Heart Services. Special thanks to 6 East Nurse Manager, Eric McClenny and 6 East Clinical Leads, Ciarra Ashley and Amanda Rooney for the significant role they played in making this a successful move! We are also grateful for additional leadership team members, staff, and support services who also contributed to the move. Some of our team members are pictured during preparation and move-day action.
Great work, everyone! Your teamwork helped the day go as smoothly as possible!


Fellowship Recruitment Wraps Up
The Duke Cardiology fellowship program completed their 7th and final day of virtual CV fellowship interviews. The team interviewed 64 incredibly talented fellowship applicants with diverse backgrounds and interests (~8.5% of the total applications we received). Anna Lisa Crowley, MD, fellowship program director, in a note to faculty, fellows and several staff members, wrote: “I personally want to thank each of you for rising to the challenge this new recruitment process presented by participating in virtual interviews, breakout groups, big sib-little sib conversations, virtual happy hours, and informal conversations. In addition, I want to recognize the extra efforts of Arlene Martin & Christina Ryerson this year who became Zoom experts and helped us all navigate the virtual interview days. In fact, many applicants shared that our interview day was the best organized and executed one they had. It is a tribute to all of your efforts so THANK YOU again! I feel privileged to work with such an AMAZING and inspiring team!”
Well done, everyone!!
Shout-out to Carlisle, Narcisse, Flores Rosario & Spates
We received a very special shout-out this week to the fellows team. In a note to Anna Lisa Crowley:
“I just wanted to send a very personal thank you and kudos to your fellows. Specifically this group: Matthew Carlisle, Dennis Narcisse, Karen Flores Rosario and Toi Spates.
My [family member] came to the hospital yesterday with 3rd degree heart block and was pretty close to death. Your fellows provided rapid triage in the ER, mobilized a bed in the CCU, and then placed a temp wire under significant duress (dopamine @ 20, transcutaneous pacing going, and my family member actively vomiting).
Basically, your fellows saved my family member’s life yesterday and for that I am deeply grateful!”
-Yuriy Bronshteyn, MD
Way to go, Duke Heart fellows!!!
Poster Earns Top 10 Score at Duke’s Annual Quality and Safety Conference
Congratulations to Myra Ellis, Bradi Granger, Debra Farrell, Heather Pena, Allen Cadavero, Mollie Kettle, Tonda Thomas and Kamrouz Ghadimi — their poster presentation, Race to the Finish: Engaging the Team in an Early Extubation Quality Improvement Project was one of the top ten scoring posters for the 2020 Duke Health Annual Quality and Safety Conference, originally scheduled for March 26, but cancelled due to COVID-19.
According to Myra Ellis, “the 7West Nursing Research committee collaborated with a CT Surgery multidisciplinary team to conduct a quality improvement initiative to increase the number of cardiac surgery patients that achieved early extubation cardiac surgery. The Society of Thoracic Surgeons defines early extubation as occurring within 6 hours after admission to the ICU. Early liberation from the mechanical ventilator important because it increases patient comfort and is associated with improved outcomes and lower costs. Our collaborative team worked to reduce barriers to extubation and promote early extubation by the use of a standardized Fast-track Extubation (FTE) Protocol and staff education. In data collected prior to implementation of the project, 49 percent (49/101) of patients were extubated in under six hours. In the first month after protocol implementation, this improved to 72 percent (60/83) and even included patients with high-disease severity that had undergone complex operations. One year after FTE protocol initiation, 75 percent (582/779) of FTE eligible patients were extubated within the six-hour window.
“Part of the success of the project was the use of the Influencer Change Model (K Patterson, et al) that posits that results are achieved by changing personal and group aspects of behavior through 6 sources of influence. Team performance was reported with the percentage of eligible patients achieving early extubation each week. We used a racetrack that was updated weekly to include the names of the “pit crew” (nurse, respiratory therapist and advanced practice provider) who successfully extubated patients within the recommended time period. Social influence can be a key factor in the individuals’ adoption of new innovations. The racetrack generated enthusiasm and captured the power of peer influence. Having your name on the racetrack created healthy competition between peers, making best practice socially desirable.”
The conference received more than 100 abstracts. The posters were scored by a blinded, multidisciplinary team based on these criteria: practical to implement, effective use of patient safety/ performance improvement tools and methods, improvement documented with pre/post analysis, and includes strategies to sustain outcomes.
Great work, everyone! Thank you for all that you do to provide the best care possible while keeping patients safe.
Important Reminders
- Open Enrollment ends this week!!!!
- Please get your Flu Vaccination: All team members must get their vaccination or otherwise demonstrate policy compliance by Tuesday, Nov. 10. Details and resources all available on the Duke Health Influenza Resources site (NET ID required): https://influenza.dh.dukehealth.org.
- DON’T FORGET TO VOTE!
COVID-19 Updates:
All the latest official DUHS information regarding coronavirus/COVID-19 response at the following locations:
Upcoming Opportunities/Save the Date:
Cardiology Grand Rounds
Oct. 27: Cardiology Faculty meeting
Nov. 10: TBA
Nov. 17: No CGR. AHA Scientific Sessions
Conferences, Symposia & Webinars
Nov. 13: 12th Annual NC Research Triangle Pulmonary Hypertension Symposium. Noon – 4:30 p.m. For more information, please visit this page. This event will be held virtually and is co-sponsored by Duke and the University of North Carolina in partnership with the Pulmonary Hypertension Association through the Building Medical Education in PH program. Please join us!
Nov. 13–17: AHA Scientific Sessions 2020, a virtual experience. Registration is now open. See the website for details.
Conversations with Colleagues: A Deeper Dive on Racial Justice
During the initial Conversations with Colleagues (CwC): Racial Justice sessions attendees shared that they wanted a deeper dive and more action steps related to racial justice. During this next edition of CwC attendees will sign up for 6 weeks of conversations. Participants will be placed into small cohorts and will walk with this same group of colleagues throughout the entire 6 weeks. These cohorts will allow staff to build relationships, have colleagues to bounce ideas off of and have accountability partners to help them stay true to the mission of the deeper dive. You will read articles, watch videos and engage in other activities that will deepen your knowledge about racial justice. Attendees will also learn action steps that they can take to make a difference.
Dates/Links for CwC
The conversations will take place weekly, starting this week and running through 12/7 (with a break Thanksgiving Week). Conversations will be 1 hour long.
Mondays 2-3pm (10/16 – 12/7)
https://duke.zoom.us/meeting/register/tJUvdOCqrDgsEtQYipTJ7F4eZnPQZFTIx2ZD
Tuesdays 8-9am (10/27 – 12/8)
https://duke.zoom.us/meeting/register/tJAtde-grTsqGtxJl7M6huHcgA3yFQ18pO6P
Wednesdays 12noon-1pm (10/28 – 12/9)
https://duke.zoom.us/meeting/register/tJUkce-rqjIrHdPmAvmnM_L0GEaFrkeFZq5L
Thursdays 5-6pm (10/29 – 12/10)
https://duke.zoom.us/meeting/register/tJ0lcu6rqTMiEtOIeRMiWtRQcInZLR6LnmPB
Fridays 12 noon-1pm (10/30 – 12/11)
https://duke.zoom.us/meeting/register/tJMrf–trTwrHtB3TEX5B-7UUXW2RgDJWGko
Sundays 4-5pm (11/1 – 12/13)
https://duke.zoom.us/meeting/register/tJEucuqtrjIpGdx8gdnQst1yAS-5NDrgzrD2
Matters of Grief: The Duke Response
On Thursday, November 19th, join us for a free half-day symposium where we will learn about ways that we can support each other through both personal and professional grief, share stories of support, and identify resources available at Duke.

Matters of Grief: The Duke Response will feature diverse and multidisciplinary panels, engaging didactic sessions, and surprise guests from across the university. Just some of the highlights include:
- Coach K delivers a special message
- Duke medical students will discuss the research behind grief and finding support through peers
- Well-Being experts and Duke Health leadership discuss normalizing discussions about grief
The virtual event runs from 1-5PM on November 19th, 2020. Sessions will be recorded for those who cannot attend the live event. Reserve your space today at bit.ly/mattersofgrief
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged.
Have a good week, everyone!
Duke Heart Week Ending October 18th 2020
Chief’s message:
 Although this year, more than any others, we have become aware of the limitations and sanctity of life, we were still deeply saddened this week to learn of the passing of Joseph Greenfield, MD, Professor and Chair Emeritus, Dept. of Medicine. He passed away on his farm in the Duke Forest. He lived a remarkable life, notable for an amazing academic career, mentorship, and a love of nature evidenced through collecting butterflies, raising hunting dogs, and many trips.
Although this year, more than any others, we have become aware of the limitations and sanctity of life, we were still deeply saddened this week to learn of the passing of Joseph Greenfield, MD, Professor and Chair Emeritus, Dept. of Medicine. He passed away on his farm in the Duke Forest. He lived a remarkable life, notable for an amazing academic career, mentorship, and a love of nature evidenced through collecting butterflies, raising hunting dogs, and many trips.
With his passing, the Division of Cardiology and the Department of Medicine suffered not only the loss of a visionary leader, but of someone who helped set the division and department on a course of research and clinical excellence. Among his many accomplishments, he will be remembered for his impact on the lives of many residents, fellows and faculty, including mine.
What I remember most over the 23 years that I had the honor of knowing him, was his overall humility, honesty, and how much he cared about your well-being. As I described in the note to our Division, he was fiercely honest with a drive for excellence in care and discovery. We all have many stories with Dr. Greenfield. My favorite revolve around both his honesty and this drive to get the clinical answer; always seeking excellence in both care and research.
In 2001, when he retired to the VA, I was the Chief Resident in Medicine and had the privilege of asking him to do morning report with the residents every week. He committed to one day a week, and would always show up 5-10 minutes early and sit in the Chief Residents office with me at the VA and ask about how things were going, how the residents were doing, and “if I was making anything of my time with research.” During the morning reports, he would quickly get to the key clinical issues and push the residents to look at the primary data, and then ensure they were sufficiently supported for the day. He would also pop in and join interns and residents for midnight pizza rounds on many of the Fridays, even back then. He would often say the key to most things was to “get the best people and get out of their way.”
Once when I gave a cardiology grand rounds as a junior faculty member, he sat in the front row and looked as if  he was asleep or bored during the majority of the talk. At the end, as was routine, he asked a question that I could not answer. He then approached me afterwards when people were congratulating me on the talk and asked me to let him know if I was going to give a talk like that again, because as he put it…. “Although small, there was a risk he could get hit by a car crossing the street from the VA and he didn’t want to risk it if I was giving another talk of that quality.”
he was asleep or bored during the majority of the talk. At the end, as was routine, he asked a question that I could not answer. He then approached me afterwards when people were congratulating me on the talk and asked me to let him know if I was going to give a talk like that again, because as he put it…. “Although small, there was a risk he could get hit by a car crossing the street from the VA and he didn’t want to risk it if I was giving another talk of that quality.”
I was honored to be named a Greenfield Scholar in 2006, and when I provided him with the manuscript we had worked on for 5 years to determine the myocardial involvement with cardiac sarcoid on cardiac MRI, which was published in Circulation with acknowledgment of the supporting funds, he simply stated he was proud of us. He went on to ask a few more important questions around the arrhythmogenic potential based on imaging findings, work that the group today is still working on.
Dr. Joseph Greenfield was and will remain the beacon for how we care for our patients and study medicine.
He leaves behind his beloved family of three daughters Mary Agnes, Ruth Ann, and Susan Lee, all of Durham. Ruth Ann, who described him as her best friend, will be helping us determine a way to celebrate his memory in the future.

Below are some thoughts and notes from others
From Chris O’Connor, MD, President, Inova Heart and Vascular Institute and former division chief, Duke Cardiology:
“What I respect the most about Dr. Greenfield was his deep commitment to people: their well-being, their families, and their professional careers as leaders. Two examples come to mind: as a first year cardiovascular fellow, my father passed at the age of 56; the first person to call was Dr. Greenfield to let me know that he was there for me if I needed anything. A second example was during every other night intern call, I was running late for a.m. rounds and got on the elevator at Duke North the same time Dr. Greenfield did. He looked at me and said, “Son, where is your tie?” (In my haste I forgot to put one on) He stopped the elevator, handed me a five-dollar bill and told me to go to the VA hospital gift shop and purchase a tie so that I could look respectable to the patients and the staff. (I never forgot to wear a tie again nor did I get on another elevator with Dr. Greenfield.)”
From Richard Stack, MD, Professor Emeritus of Medicine in Cardiology at Duke University; President and Managing Partner of Synecor, LLC:
A sad end to a great era in Academic Medicine. My thoughts are simple: “I owe my entire career to Joe Greenfield.”
Updates from the week:
Passing of Joseph Greenfield, MD, Professor and Chair Emeritus, Dept. of Medicine
In an announcement to all faculty members within the Department of Medicine this week, Mary E. Klotman, MD, Dean of the School of Medicine, and Kathleen A. Cooney, MD, Chair, Department of Medicine wrote:
It is with great sadness that we write to inform you that Joseph Greenfield, MD, died on Wed., Oct. 14.
Dr. Greenfield was the James B. Duke Distinguished Professor of Medicine and chair of the Department of Medicine from 1983 to 1995. He received his medical degree from Emory University in 1956 and completed his internal medicine residency at Duke University in 1959. He joined the National Institutes of Health (NIH) before returning to Duke as assistant professor in 1962.
In addition to his role as chair, Dr. Greenfield served in numerous other leadership positions including chief of Cardiology at the Durham Veteran’s Administration Hospital from 1963 to 1983, chief of the Division of Cardiology at Duke University Medical Center from 1981 to 1989, and director of the ECG service at Duke from 1971 to 2001, and at the Veteran’s Administration Hospital from 1996 until he retired in 2017.
Dr. Greenfield was a pioneer in cardiovascular medicine, promoting innovative care models and studying reperfusion therapies in acute coronary syndromes. He created new, forward-thinking care paradigms to ensure that rural areas had access to emergent cardiovascular care by sending cardiologists on helicopters to outlying hospitals to administer thrombolytic therapy.
With the goal of delivering more efficient acute myocardial infarction care, Greenfield reorganized the cardiac catheterization lab to be adjacent to Duke University Hospital’s emergency room. He advocated for greater use of randomized clinical trials and patient data registries to advance knowledge and improve patient care. Over his career, Greenfield authored more than 150 research articles.
Dr. Greenfield was passionately committed to the professional development of faculty and trainees and will be remembered as great mentor. He started the Greenfield Scholars Program that continues to support many resident and junior faculty research careers. In his honor, the Department of Medicine established the Joseph Greenfield Research Mentorship Award to recognize faculty members who excel in research mentorship.
In 1984, Greenfield was awarded the Distinguished Science Award from the American College of Cardiology and Duke’s Eugene A. Stead Award for excellence in teaching (and again in 1995). He received the MERIT Award from the National Heart, Lung and Blood Institute in 1986. In 1990, he became a member of the National Academy of Medicine.
Please join us in extending our deepest condolences to Dr. Greenfield’s family and friends. The Duke flag was lowered on Thursday in his memory.
Memorial service information will be provided when it becomes available. In lieu of flowers donations can be made to The Greenfield Scholars Program at Duke University.
Duke Regional Earns Top Rating for Adult Cardiac Surgery Procedure
For the second year in a row, Duke Regional Hospital’s coronary artery bypass grafting (CABG) procedure in adult cardiac surgery has earned a top rating – three stars – from The Society of Thoracic Surgeons (STS).
This annual rating is calculated by examining quality measures of Duke Regional’s CABG procedures during calendar year 2019, to include absence of mortality, absence of morbidity, use of internal mammary artery (IMA) grafting, and how medications were prescribed.
“This recognition shows that Duke Regional Hospital team members take exceptional care of our CABG patients, by not only ensuring a safe and successful surgery but also by helping the patient swiftly recover,” said Shu Lin, MD, Ph.D., Duke Regional division chief for Cardiothoracic Surgery and Duke associate professor of Surgery. Lin shared the news with the team at Duke Regional earlier this week.
More than 75 percent of Duke Regional’s CABG patients are discharged within five days after surgery, compared to only 42 percent of CABG patients from comparable hospitals, Lin added. On average, CABG patients are extubated five hours after surgery, and none of Duke Regional’s CABG patients had spent prolonged time on a ventilator in the past two years.
STS’ star rating system is one of the most sophisticated and highly regarded overall measures of quality in health care, rating the benchmarked outcomes of cardiothoracic surgery programs in the U.S.
Lin said this top rating was achieved by the highest-quality, compassionate care that team members provided across Duke Regional Hospital, to include clinical staff and support staff.
“The achievement of this STS three-star recognition exemplifies what a teamwork can do, especially when fundamentals of patient care are meticulously followed and when each member of the team takes pride in his or her role in the process,” he said. “Congratulations to everyone involved.”
Gutierrez Receives CDA Funding

Duke Heart
Congratulations to Tony Gutierrez, MD, MHS, who received word that his VA Career Development Award (CDA) has been funded! This competitive award provides five years of support for early career investigators. Tony is the first person in the Cardiology Division to successfully receive a CDA, according to Sunil Rao, MD, Section Chief, Cardiology at Durham VA Medical Center.
Gutierrez’s project, titled “Telehealth to improve functional status and quality of life in veterans with PAD,” will establish a veteran-centric program of telehealth-facilitated exercise using the Durham VA’s robust home-based cardiac rehabilitation program and will assess long-term outcomes in patients with peripheral artery disease.
Tony’s mentors on the CDA include Rao, Miriam Morey, PhD, Kelli Allen, PhD, Katherine Hall, PhD, Matthew Maciejewski, PhD, Shirling Tsai, MD, and David Edelman, MD, MHS.
Congrats, Tony!! Well deserved!
Shout-Out to Rio Landa, APP!
“I think Rio Landa deserves special commendation for picking up an abnormality totally unrelated to cardiology,” wrote Neil Freedman, MD, in a message this week to Stephanie Barnes, NP. His note goes on to describe the event:
“Rio was meeting a patient for the first time on Monday, Oct. 12. We were trying to push to discharge the patient (because symptoms were from GERD, and patient had been cath’d the previous week). Rio noticed that nothing had been noted or done about a new finding of probable R renal cell CA discovered [days earlier] by abdominal CT—so, after seeing this abnormality, Rio herself coordinated oncology and IR to get the issue taken care of as an outpatient. [Patient has history of cancer.]
Rio is not unique in her terrific efforts, of course, but this episode illustrates highly commendable conscientiousness and initiative. Brava!”
Barnes added, in a message this week to Pulse, “This highlights Rio’s true attention to detail, even on a busy day! She leads by example and we thank Dr. Freedman for taking the time to recognize her great catch.”
Freedman signed off his letter with the statement, “It is a real privilege to work with the APPs.”
We could not agree more! Well done, Rio – and many thanks to our terrific APP team!
Three CVIS Clinical Ladder Promotions in Interventional Lab
We are excited to share with you that the following clinical team members are the first three to be promoted within the interventional lab space under the recently revised Clinical Ladder Program for CVIS.
Meek Myoung: CVIS I to CVIS II – Adult Cardiac Cath Lab, DUH. Meek holds a BS in Radiologic Science and has been a CVIS in the Adult Cath lab since 2018. She maintains her RT(R) as well as the RCIS certification.
Cassidy Johnson: CVIS I to CVIS II – Adult Cardiac Cath Lab, DUH. Cassidy holds a BS in Radiologic Science and has been a CVIS in the Adult Cath Lab since 2018. She maintains her RT(R) as well as the RCIS certification.
Catherine Bennett: CVIS II to CVIS III – Adult EP Lab, DUH. Catherine holds an Associates of Science in Cardiovascular Technology and has been an employee at DUH since 1998. She started her career in the Adult Cath Lab and transferred to the Adult EP Lab in 2016. She maintains the RCIS certification.
“We are very proud of all of their hard work and dedication to their patients as well as their team here at Duke University Hospital,” said Elizabeth Watts, Duke Heart Nurse Manager, Operations for the Adult Cardiac Cath Lab, Cardiovascular Short Stay Unit, and the Adult Electrophysiology Lab.
Congratulations, Meek, Cassidy and Catherine!
Planning for Move to 7 East
 The Cardiac ICU Charge Nurse group held a meeting on Oct. 14 to discuss workflows and practices related to the upcoming move to 7 East. Manesh Patel and Jill Engel stopped by to express their gratitude for the team’s leadership and talked about the great opportunities coming along with the move, which is currently scheduled for November 21.
The Cardiac ICU Charge Nurse group held a meeting on Oct. 14 to discuss workflows and practices related to the upcoming move to 7 East. Manesh Patel and Jill Engel stopped by to express their gratitude for the team’s leadership and talked about the great opportunities coming along with the move, which is currently scheduled for November 21.
Special thanks to Kirsten Butler for coordinating the meeting and to the charge nurses who participated.
CT SDU Moving to DMP 6 East, Oct. 24
One of the Cardiothoracic Stepdown Units will be moving from Duke Medical Pavilion (DMP) 7 East to DMP 6 East on Saturday, Oct. 24. This is the first move to occur as part of the planned move sequence for Heart Services. Thank you to the staff, providers, and team members who are working hard to make this a successful move!
Additional communications regarding “move day” will be forthcoming.
Duke Solid Organ Transplant Summit Held Oct. 10
 The 2020 Duke Solid Organ Transplant Summit was held as a virtual event on Saturday Oct. 10. A pre-summit Duke Transplant APP Bootcamp was held on Friday, Oct. 9. Duke Heart was well represented for both portions of last weekend’s events. Presenters included:
The 2020 Duke Solid Organ Transplant Summit was held as a virtual event on Saturday Oct. 10. A pre-summit Duke Transplant APP Bootcamp was held on Friday, Oct. 9. Duke Heart was well represented for both portions of last weekend’s events. Presenters included:
- Stephanie Barnes, NP- “DCD in Cardiac Transplantation”
- Callie Tennyson, NP- “Identifying and Managing Complications of Cardiac Transplantation”
- Benjamin Bryner, MD- “Lessons Learned in DCD Heart Transplant”
- Richa Agarwal, MD- “Emerging Mechanical Circulatory Support Devices”
- Kam Ghadimi, MD- “Inhaled Pulmonary vasodilators in the perioperative setting-iNO vs. EPO”
“Everybody delivered beautifully, it was a really well run weekend by Duke Surgery,” said Callie Tennyson.
Course directors were Deb Sudan, MD and Carl Berg, MD. Great work, everyone!
We’ve Grown Again!
We are very pleased to welcome Natalie Claire Lerman, born October 7, to our Duke Heart family! “Baby and Mom are doing great!” says dad, Joe Lerman, one of our cardiology fellows.
Congrats, Lerman family!! We look forward to meeting her!

Important Reminders
- Open Enrollment for Duke Benefits is October 19-30.
- Please get your Flu Vaccination: All team members must get their vaccination or otherwise demonstrate policy compliance by Tuesday, Nov. 10. Details and resources all available on the Duke Health Influenza Resources site (NET ID required): https://influenza.dh.dukehealth.org.
Upcoming Opportunities/Save the Date:
Cardiology Grand Rounds
Oct. 20: The Albert L. Williams Cardiovascular Genetics Lecture Series. Presenter: Wendy Chung, MD, PhD, of Columbia. 5 p.m., Webex. Details in email invitation.
Oct. 27: Cardiology Faculty meeting
Nov. 10: TBA
Nov. 17: No CGR. AHA Scientific Sessions
Conferences, Symposia & Webinars
Nov. 13: 12th Annual NC Research Triangle Pulmonary Hypertension Symposium. Noon – 4:30 p.m. For more information, please visit this page. This event will be held virtually and is co-sponsored by Duke and the University of North Carolina in partnership with the Pulmonary Hypertension Association through the Building Medical Education in PH program. Please join us!
Nov. 13–17: AHA Scientific Sessions 2020, a virtual experience. Registration is now open. See the website for details.
COVID-19 Updates:
All the latest official DUHS information regarding coronavirus/COVID-19 response at the following locations:
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged.
Duke Heart in the News:
October 14 — Adrian Hernandez
STAT
Covid-19 clinical trial pauses ‘show the system is working’
https://bit.ly/3m51lUR
Recent Comments