Duke Heart Pulse week ending 10-31-2021
Albanese Named EVP, COO of DUHS Effective Jan. 17
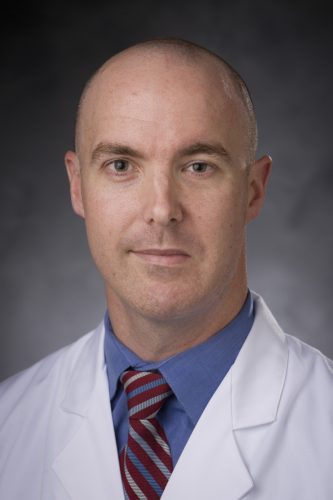
 Craig Albanese, a seasoned health care executive and distinguished academic pediatric surgeon, has been named executive vice president and chief operating officer of Duke University Health System (DUHS).
Craig Albanese, a seasoned health care executive and distinguished academic pediatric surgeon, has been named executive vice president and chief operating officer of Duke University Health System (DUHS).
Albanese comes to DUHS from New York-Presbyterian Hospital, where he’s currently group senior vice president and chief medical officer of the $9.2 billion, 10-hospital academic health system. He will start his new role at Duke on Jan. 17, 2022.
“Dr. Albanese is a passionate and collaborative executive with deep experience in leading cutting-edge academic health systems such as ours in becoming the best place to work, delivering highest-quality patient care, and helping to advance our other missions, including research, education and community health,” said A. Eugene Washington, MD, chancellor for health affairs and DUHS president and CEO.
“Given his impressive achievements and commitment to our values, I am confident that Duke University Health System will begin a new era of excellence and impact under his leadership,” Washington said.
As executive vice president, Albanese will serve as the senior leader overseeing the timely execution of DUHS goals and strategic priorities. He will work with other clinical enterprise leaders to deliver outstanding outcomes and care across Duke’s network, from the hospital to ambulatory clinics to care in homes and the community. He will also bring new insights to manage the organization’s COVID pandemic response, to support the health system’s faculty and staff and to further advance the clinical enterprise strategic plan.
“I am honored to accept this position and to join the Duke family,” Albanese said. “I look forward to growing Duke’s footprint in the community and building upon the existing quality improvement work that contributes to Duke’s reputation as a world-class health system.”
Albanese succeeds William Fulkerson, MD, who held the executive vice president position since 2010 and announced he would step down at the end of the year.
In his current role at NYP, Albanese is responsible for the chief medical officers and all eight service lines, including oversight for enterprise clinical standardization, network integration and medical affairs. He also oversees quality, safety, and infection prevention and control for the enterprise.
His more than 25 years of health care management experience includes overseeing the redesign of service line strategy at NYP to drive integration and single standards of care across 10 hospitals and two medical schools, Columbia Vagelos College of Physicians and Surgeons and the Weill Cornell Medical College.
He also served as the COO of New York-Presbyterian’s Morgan Stanley Children’s Hospital and the Sloane Hospital for Women, which is located within the Children’s Hospital.
Prior to NYP, Albanese held senior leadership roles at Stanford University and Stanford Health Care. A respected surgeon-scientist and clinical investigator, he co-directed the team that pioneered in-utero fetal surgery.
Albanese received his medical degree from SUNY Health Science Center in Brooklyn and was a resident and chief resident in general surgery at Mount Sinai Medical Center. He completed pediatric general surgery and critical care research fellowships at Children’s Hospital of Pittsburgh. Albanese also holds a Master’s in Business Administration from the Leavey School of Business at Santa Clara University.
“Dr. Albanese is a seasoned health care leader who possesses a collaborative management style and is committed to the same core ideals we value here at Duke,” said Duke University President Vincent E. Price.
Jackson Receives K Award
 Congratulations to Duke electrophysiologist Larry R. Jackson, MD, assistant professor of medicine in cardiology! He has received notification of a K-award from the National Institutes of Health’s National Heart, Lung, and Blood Institute for his project, Shared Decision-Making to Reduce Racial Disparities in Oral Anticoagulation Use in Patients with Non-Valvular Atrial Fibrillation.
Congratulations to Duke electrophysiologist Larry R. Jackson, MD, assistant professor of medicine in cardiology! He has received notification of a K-award from the National Institutes of Health’s National Heart, Lung, and Blood Institute for his project, Shared Decision-Making to Reduce Racial Disparities in Oral Anticoagulation Use in Patients with Non-Valvular Atrial Fibrillation.
Jackson, a faculty member at Duke since 2016, says this award “will allow him finalize the skill set that will lead him toward independence as a physician scientist with a research program focused on addressing racial differences and abnormal heart rhythm care.”
We look forward to sharing more about this important project as it gets underway.
Thanking Respiratory Therapists
Duke Heart’s leadership team took time to recognize our Respiratory Care Team this week during Respiratory Care Week by thanking each of them for their professional accomplishments and contributions over the last year.
“We recognize that the past 18 months has been filled with challenges like we have not seen before and that each of you have stepped up to support our patients, their loves ones and the entire Duke Health team. We have all seen the amazing outcomes and even miracles that have positively impacted patients and families due to the contributions made by each of you. Duke Respiratory Therapists are recognized as the best in the country because of the amazing things that each of you make possible for our patients each and every day (and night). The number of lives you touch is immeasurable as you set the bar for others in your profession.
Please take time to reflect on and celebrate your personal and team successes during the 2021 Respiratory Therapy Week. We thank you for everything you have done and continue to do for Duke Health patients.”
Shown in photo collage are some celebratory shots of our Respiratory Care Team members. We think you’re awesome – thank you for all you do!

Adams Named Nurse Manager for 7700 Effective Nov. 1
The Duke Heart Leadership team is pleased to announce Katherine Adams as the new 7700 Nurse Manager, effective November 1, 2021. Adams has been a Duke Heart Nurse since September 2015 after obtaining her BSN at Liberty University. She has served as a Clinical Team Lead for Cardiology Step-Down since June 2019, including units 7100 and 7700.
Adams has been instrumental in the opening and establishing of 7700 as a new Cardiology Step-Down Unit since it opened in December 2020. She has helped 7700 grow through her mentorship of new team members, leadership of committees and assisting in various champion roles as the staff have developed experience and embraced various leadership roles of their own. We are looking forward to all that she has planned for the future of 7700.
Please join us in congratulating Katherine on her new role!
Shout-Out to Haney
We received a patient compliment on behalf of Jack Haney this week — passed along to us by Lisa Clark Pickett, Chief Medical Officer for Duke University Hospital.
“Jack, While reading comments on our Patient Satisfaction Survey, I found another wonderful compliment about you and your team!
Thank you for giving me such great care. The nurses and staff were amazing! Dr. Haney did a great job!
Thank you so much for your dedication, excellence, and positive spirit!” – Lisa Clark Pickett
Mother and Daughter Receive Organ Transplants at Duke One Month Apart
 Tyra Ingram, 19, of Laurinburg, NC was born with more than one congenital heart defect and needed three major heart surgeries and a pacemaker before she was five years old. She underwent a heart transplant at Duke in 2021, but the family couldn’t relax just yet. Within weeks of Tyra’s transplant, her mother, Teyanna, received a kidney transplant at Duke. Now, months later, mom and daughter are feeling great, going on family vacations again, and looking forward to a healthy future.
Tyra Ingram, 19, of Laurinburg, NC was born with more than one congenital heart defect and needed three major heart surgeries and a pacemaker before she was five years old. She underwent a heart transplant at Duke in 2021, but the family couldn’t relax just yet. Within weeks of Tyra’s transplant, her mother, Teyanna, received a kidney transplant at Duke. Now, months later, mom and daughter are feeling great, going on family vacations again, and looking forward to a healthy future.
A Journey Not for the Faint of Heart
Tyra was born with several heart defects, including congenitally corrected transposition of the great arteries (also called L-transposition of the great arteries, or L-TGA). This rare defect caused two of Tyra’s four heart chambers to be switched, one of which was too small to function properly. By the time she was in kindergarten, Tyra had undergone a series of complex heart surgeries at Duke University Hospital. She had a pulmonary artery band surgery at two months old, a bidirectional Glenn procedure at 14 months old, and a Fontan surgery with a pacemaker placement when she was four. As she grew, Tyra struggled to keep up with other kids.
“I was the worrywart,” Teyanna, now 41, said. “I’d see her trying to run, and I would tell her not to. I’d be like, ‘No, baby. You might need to sit down. You look tired.’”
Kidney Failure Complicates Things
In June 2019, Teyanna was diagnosed with kidney failure due to complications from diabetes. She started dialysis, which required four-hour treatments, three times a week. Within a few months, Teyanna’s doctors suggested she be evaluated for a kidney transplant. She was added to the national waitlist.
Two Organ Transplants Within One Month
Two years later, in February 2021, Tyra started having trouble breathing while she was a student at North Carolina Central University. “I called my grandma. They were like, ‘let’s call the doctor,’” Tyra said.
Michael Carboni, MD, Tyra’s Duke pediatric cardiologist since she was five years old, knew that she needed advanced therapy or a heart transplant. About two weeks after Tyra was put on the transplant waitlist, a heart became available.
“She had a really complicated surgery because of her complex congenital heart disease. But the transplant went really well, and she thrived afterward,” said Duke transplant cardiologist Adam DeVore, MD, MHS, who was part of her care team.
Just a few weeks later, Teyanna got the call that a kidney was available for her and she underwent the transplant. Six weeks later, her kidney transplant surgeon Kadiyala Ravindra, MBBS, was pleased with her progress. “She was really sick prior to her transplant,” he said. “It’s gratifying to see how well she’s done.”
Figuring Out What’s Next
Both Teyanna and Tyra are getting stronger every day. “I can walk a lot more without getting tired,” Tyra said.
“My experience was great. Some of my Duke nurses were the same ones who took care of Tyra, so they remembered me. They would ask how she was doing,” Teyanna said. “It felt like a second home.”
According to Dr. Carboni, Duke has the resources and collaborative expertise to help people like Tyra and Teyanna Ingram. “We can do the same for others like them,” he said.
Upcoming Events & Opportunities
Cardiology Grand Rounds
November 2: Coronary Microvascular Dysfunction with Jessica Duran. 5 p.m. Webex.
November 9: Case Conference – Lessons Learned in Peri-Operative LVAD Care with Amanda Coniglio. 5 p.m. Webex.
Upcoming Duke Heart CME
November 5: 13th Annual NC Research Triangle Pulmonary Hypertension Symposium. Course directors are H. James Ford (UNC) and Terry Fortin. 8:30 a.m. to 4:20 p.m. Morning case-based workshops have been cancelled due to Covid. Afternoon portion will be held via Zoom. For more information and to register, please visit: https://bit.ly/3DrZwuv.
Request for Nominations: Samuel DuBois Cook Society Award
The Samuel DuBois Cook Society invites nominations of individuals from every sector of the Duke Community: staff, administrators, and students — undergraduate, graduate or professional.
Founded to be an instrument of social engagement and change, the Cook Society seeks to recognize members of the Duke community who reflect in their work or in their academic pursuits, the objectives to which Dr. Cook dedicated his professional life — social justice, mentoring, the University’s relationship to the black community, and his vision of the “beloved community,” seeking to improve relations among persons of all backgrounds.
Nominations are due November 8, 2021, and winners will be notified in the first week of December.
Awards will be presented during the annual Cook Society Awards Ceremony on February 22, 2022, at the Washington Duke Inn & Golf Club.
In evaluating nominees, the committee seeks members of the Duke community who:
- Actively nurture a sense of community and belonging for Black people.
- Commit to translate the promise and potential of Black people at Duke into fulfillment and actuality
- Foster positive and constructive interpersonal and intergroup relations within both Duke University’s and Durham’s Black communities
- Cultivate positive relations between Black people and other ethnic, racial, and national groups on the basis of an enlightened appreciation and knowledge of our historic interdependence
To learn more/make a nomination please click here.
Request for Nominations: Raymond Gavins Distinguished Faculty Award
The Samuel DuBois Cook Society invites nominations of faculty whose teaching, mentoring, research, publishing, and engagement with faculty, students and staff have helped to improve relations among people of all backgrounds at Duke and beyond.
Nominations are due November 8, 2021, and winners will be notified in the first week of December. Awards will be presented during the annual Cook Society Awards Dinner on February 22, 2022, at the Washington Duke Inn & Golf Club.
In evaluating nominees, the committee seeks faculty who:
- Actively nurture a sense of community and belonging for Black people.
- Commit to translate the promise and potential of Black people at Duke into fulfillment and actuality
- Foster positive and constructive interpersonal and intergroup relations within both Duke University’s and Durham’s Black communities
- Cultivate positive relations between Black people and other ethnic, racial, and national groups on the basis of an enlightened appreciation and knowledge of our historic interdependence
To learn more/make a nomination please click here.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged.
Duke Heart in the News:
October 18 — Kevin Thomas
Cardiovascular Business
Exploring reports of discrimination, burnout and job satisfaction among US cardiologists
https://duke.is/yzge9
October 18 — Kevin Thomas
tctMD
ACC Survey Reveals Racial/Ethnic Gaps but Also Job Satisfaction
https://duke.is/jwuar
October 18 — Kevin Thomas
Medscape
Survey Spotlights Double-Edged Sword for Minority Cardiologists
https://www.medscape.com/viewarticle/961101
October 20 — Kevin Thomas
HealthDay
Many Minority, Women Cardiologists Face Discrimination
https://duke.is/vmsrp
October 20 — Joseph Turek
Medscape
US Surgeons Successfully Test Pig Kidney Transplant in Human Patient
https://www.medscape.com/viewarticle/961240?src
October 20 — Manesh Patel
Healio/Cardiology
For patients with HFpEF, medical therapy options now abound
https://duke.is/wxumz
October 20 — Kevin Thomas
Cardiovascular News
Ethnic and racial minority cardiologists face professional discrimination and exclusion
https://duke.is/cerq8
October 21 — Kevin Thomas
Becker’s Hospital Review
Discrimination in the cardiology field: 5 survey findings
https://duke.is/b8n9g
October 22 — Robert Califf
Politico
Biden meets with top FDA candidate
https://duke.is/n4wwc
October 25 — Sunil Rao
tctMD
OPTIMIZE: 2-Year DES Data Affirm Need for Meaningful MI Definitions
https://duke.is/zjrvh
October 26 — Adrian Hernandez
Fox13 Memphis
Woman says controversial COVID-19 treatment Ivermectin saved her life
https://duke.is/mhuks
October 26 — Jonathan Piccini
AHA Newsroom
New heart clinical trial to shine light on early atrial fibrillation treatment
https://duke.is/8ag33
October 26 — G. Michael Felker
Cardiology Today
GALACTIC-HF: Omecamtiv mecarbil effective in patients with severe HF
https://duke.is/ccsyt
October 28 — Andrew Almond (Respiratory Therapy)
ABC11/WTVD (Raleigh/Durham)
Raleigh man credits Duke respiratory therapists for saving him from COVID-19
https://duke.is/wvrwn
Division of Cardiology Publications Indexed in PubMed October 14-27, 2021
Ageno W, Lopes RD, Goldin M, Yusen RD, Albers GW, Elliott GC, Halperin JL, Hiatt WR, Maynard G, Steg PG, Weitz JI, Suh E, Lu W, Barnathan ES, Raskob GE, Spyropoulos AC. Rivaroxaban for extended thromboprophylaxis in acutely ill medical patients 75 years of age or older. J Thromb Haemost 2021;19(11):2772-2780. PM: 34314574.
Arps K, Piccini JP, Yapejian R, Leguire R, Smith B, Al-Khatib SM, Bahnson TD, Daubert JP, Hegland DD, Jackson KP, Jackson LR, Lewis RK, Pokorney SD, Sun AY, Thomas KL, Frazier-Mills C. Optimizing mechanically sensed atrial tracking in patients with atrioventricular-synchronous leadless pacemakers: A single-center experience. Heart Rhythm O2 2021;2(5):455-462. PM: 34667960.
Barnett AS, Bahnson TD. Recurrent atrial fibrillation after pulmonary vein isolation: Box it or not? Heart Rhythm O2 2021;2(5):498-499. PM: 34667965.
Bossone E, Cademartiri F, AlSergani H, Chianese S, Mehta R, Capone V, Ruotolo C, Tarrar IH, Frangiosa A, Vriz O, Maffei V, Annunziata R, Galzerano D, Ranieri B, Sepe C, Salzano A, Cocchia R, Majolo M, Russo G, Longo G, Muto M, Fedelini P, Esposito C, et al. Preoperative Assessment and Management of Cardiovascular Risk in Patients Undergoing Non-Cardiac Surgery: Implementing a Systematic Stepwise Approach during the COVID-19 Pandemic Era. J Cardiovasc Dev Dis 2021;8(10):126. PM: 34677195.
Bracamonte-Baran W, Gilotra NA, Won T, Rodriguez KM, Talor MV, Oh BC, Griffin J, Wittstein I, Sharma K, Skinner J, Johns RA, Russell SD, Anders RA, Zhu Q, Halushka MK, Brandacher G, Čiháková D. Endothelial Stromal PD-L1 (Programmed Death Ligand 1) Modulates CD8 T-Cell Infiltration After Heart Transplantation. Circ Heart Fail 2021;14(10):e007982. PM: 34555935.
Careau V, Halsey LG, Pontzer H, Ainslie PN, Andersen LF, Anderson LJ, Arab L, Baddou I, Bedu-Addo K, Blaak EE, Blanc S, Bonomi AG, Bouten CVC, Buchowski MS, Butte NF, Camps SGJA, Close GL, Cooper JA, Das SK, Cooper R, Dugas LR, Eaton SD, Ekelund U, et al. Energy compensation and adiposity in humans. Curr Biol 2021;31(20):4659-4666. PM: 34453886.
Edmonston DL, Matsouaka R, Shah SH, Rajagopal S, Wolf M. Noninvasive Risk Score to Screen for Pulmonary Hypertension With Elevated Pulmonary Vascular Resistance in Diseases of Chronic Volume Overload. Am J Cardiol 2021;159:113-120. PM: 34497006.
Gautam N, Saluja P, Fudim M, Jambhekar K, Pandey T, Al’Aref S. A Late Presentation of COVID-19 Vaccine-Induced Myocarditis. Cureus 2021;13(9):e17890. PM: 34660088.
Gelijns AC, Moskowitz AJ, O’Gara PT, Giustino G, Mack MJ, Mancini DM, Bagiella E, Hung J, Ailawadi G, Leon MB, Acker MA, Alexander JH, Dickert NW, Taddei-Peters WC, Miller MA. Transcatheter mitral valve repair for functional mitral regurgitation: Evaluating the evidence. J Thorac Cardiovasc Surg 2021;162(5):1504-1511. PM: 32359794.
Gutierrez JA, Patel MR. Crossing Peripheral Chronic Total Occlusions: More Tolls and More Questions. J Am Heart Assoc 2021;10(20):e023423. PM: 34612087.
Holder TA, Gutierrez JA, Aday AW. Medical Management of Peripheral Artery Disease. Cardiol Clin 2021;39(4):471-482. PM: 34686260.
Jackson LR, Ugowe F. Epidemiology and Outcomes Associated with PR Prolongation. Card Electrophysiol Clin 2021;13(4):661-669. PM: 34689893.
Kuno T, Claessen B, Cao D, Chandiramani R, Guedeney P, Sorrentino S, Krucoff M, Kozuma K, Ge J, Seth A, Makkar R, Bangalore S, Bhatt DL, Angiolillo DJ, Saito S, Neumann FJ, Hermiller J, Rau V, Ruster K, Wang J, Valgimigli M, Mehran R. Impact of renal function in high bleeding risk patients undergoing percutaneous coronary intervention: a patient-level stratified analysis from four post-approval studies. J Thromb Thrombolysis 2021;52(2):419-428. PM: 33709255.
Lopes RD, Higano CS, Slovin SF, Nelson AJ, Bigelow R, Sørensen PS, Melloni C, Goodman SG, Evans CP, Nilsson J, Bhatt DL, Clarke NW, Olesen TK, Doyle-Olsen BT, Kristensen H, Arney L, Roe MT, Alexander JH. Cardiovascular Safety of Degarelix Versus Leuprolide in Patients With Prostate Cancer: The Primary Results of the PRONOUNCE Randomized Trial. Circulation 2021;144(16):1295-1307. PM: 34459214.
Martinez Campos C, Tsai K, Courtney DG, Bogerd HP, Holley CL, Cullen BR. Mapping of pseudouridine residues on cellular and viral transcripts using a novel antibody-based technique. RNA 2021;27(11):1400-1411. PM: 34376564.
Pani B, Ahn S, Rambarat PK, Vege S, Kahsai AW, Liu A, Valan BN, Staus DP, Costa T, Lefkowitz RJ. Unique Positive Cooperativity Between the -Arrestin-Biased -Blocker Carvedilol and a Small Molecule Positive Allosteric Modulator of the 2-Adrenergic Receptor. Mol Pharmacol 2021;100(5):513-525. PM: 34580163.
Perino AC, Gummidipundi SE, Lee J, Hedlin H, Garcia A, Ferris T, Balasubramanian V, Gardner RM, Cheung L, Hung G, Granger CB, Kowey P, Rumsfeld JS, Russo AM, True Hills M, Talati N, Nag D, Tsay D, Desai S, Desai M, Mahaffey KW, Turakhia MP, Perez MV. Arrhythmias Other Than Atrial Fibrillation in Those With an Irregular Pulse Detected With a Smartwatch: Findings From the Apple Heart Study. Circ Arrhythm Electrophysiol 2021;14(10):e010063. PM: 34565178.
Polcwiartek C, Loewenstein D, Friedman DJ, Johansson KG, Graff C, Sørensen PL, Nielsen RE, Kragholm K, Torp-Pedersen C, Søgaard P, Jensen SE, Jackson KP, Atwater BD. Clinical Heart Failure Among Patients With and Without Severe Mental Illness and the Association With Long-Term Outcomes. Circ Heart Fail 2021;14(10):e008364. PM: 34587762.
Sheikh FH, Ravichandran AK, Goldstein DJ, Agarwal R, Ransom J, Bansal A, Kim G, Cleveland JC, Uriel N, Sheridan BC, Chomsky D, Patel SR, Dirckx N, Franke A, Mehra MR. Impact of Race on Clinical Outcomes After Implantation With a Fully Magnetically Levitated Left Ventricular Assist Device: An Analysis From the MOMENTUM 3 Trial. Circ Heart Fail 2021;14(10):e008360. PM: 34525837.
Siddiqi TJ, Arshad MS, Sreenivasan J, Blumer V, Almani MU, Usman MS, Kolawole JO, Fudim M, Hernandez GA, Khan MS. Readmissions in Patients With Heart Failure and Mental Health Disorders (from a National Database). Am J Cardiol 2021;159:142-143. PM: 34493385.
Siegbahn A, Lindbäck J, Hijazi Z, Åberg M, Alexander JH, Eikelboom JW, Lopes RD, Pol T, Oldgren J, Granger CB, Yusuf S, Wallentin L. Multiplex protein screening of biomarkers associated with major bleeding in patients with atrial fibrillation treated with oral anticoagulation. J Thromb Haemost 2021;19(11):2726-2737. PM: 34390530.
Starks MA, Jackson LR, Hellkamp A, Al-Khatib SM, Mark DB, Thomas KL, Nichol G, Lee KL, Davidson-Ray L, Poole J, Anderson J, Johnson G, Bardy GH. Outcomes for patients with anterior myocardial infarction and prior cardiac arrest in the home automated external defibrillator trial (HAT). Resuscitation 2021;168:75-83. PM: 34500022.
Thomas KL, Mehta LS, Rzeszut AK, Lewis SJ, Duvernoy CS, Douglas PS. Perspectives of Racially and Ethnically Diverse U.S. Cardiologists: Insights From the ACC Professional Life Survey. J Am Coll Cardiol 2021;78(17):1746-1750. PM: 34674820.
Tran AT, Fonarow G\C, Arnold SV, Jones PG, Thomas LE, Hill CL, DeVore AD, Butler J, Albert NM, Spertus JA. Risk Adjustment Model for Preserved Health Status in Patients With Heart Failure and Reduced Ejection Fraction: The CHAMP-HF Registry. Circ Cardiovasc Qual Outcomes 2021;14(10):e008072. PM: 34615366.
Yoon S, Goh H, Fung SM, Tang S, Matchar D, Ginsburg GS, Orlando LA, Ngeow J, Wu RR. Experience and Perceptions of a Family Health History Risk Assessment Tool among Multi-Ethnic Asian Breast Cancer Patients. J Pers Med 2021;11(10):1046. PM: 34683187.
Krantz MJ, Debus SE, Hsia J, Patel MR, Anand SS, Nehler MR, Hess CN, Capell WH, Bracken T, Szarek M, Mátyás L, Krievins DK, Nault P, Stefanov S, Haskell LP, Berkowitz SD, Muehlhofer E, Hiatt WR, Bauersachs RM, Bonaca MP. Low-dose rivaroxaban plus aspirin in older patients with peripheral artery disease undergoing acute limb revascularization: insights from the VOYAGER PAD trial. Eur Heart J 2021 Oct 14;42(39):4040-4048. PM: 34430972.
Duke Heart Week Ending 10-24-2021
Updates from the week:
Passing: Robert W. Anderson, MD, Professor of Surgery
It is with great sadness that we inform you of the passing of Robert W. Anderson, Professor of Surgery and former Chair of the Department of Surgery, on October 19, 2021.
 Dr. Anderson served as chair of Duke Department of Surgery from 1994–2003. An accomplished cardiothoracic surgeon with additional training in business administration, Dr. Anderson successfully led a department that had been seeded as the epitome of traditional surgical education and training, research, and clinical excellence by his predecessor Dr. David C. Sabiston, Jr. Dr. Anderson’s leadership as chair solidified Duke Surgery’s stature as a world-class institution and fortified its continued dedication to a tripartite mission of clinical, educational, and investigational achievement.
Dr. Anderson served as chair of Duke Department of Surgery from 1994–2003. An accomplished cardiothoracic surgeon with additional training in business administration, Dr. Anderson successfully led a department that had been seeded as the epitome of traditional surgical education and training, research, and clinical excellence by his predecessor Dr. David C. Sabiston, Jr. Dr. Anderson’s leadership as chair solidified Duke Surgery’s stature as a world-class institution and fortified its continued dedication to a tripartite mission of clinical, educational, and investigational achievement.
Dr. Anderson’s surgical career spanned more than five decades, beginning with his surgical training at Duke University in 1967. After his residency, Dr. Anderson was appointed as Assistant Professor of Surgery at Duke. A true surgeon–scientist committed to both clinical care and investigative discovery, Dr. Anderson launched his clinical practice while also serving as Director of the CORE Cardiovascular Research Laboratory at Duke University Medical Center until 1977.
“Dr. Anderson was one of my most important mentors and a close friend,” said Peter K. Smith, MD, Mary and Deryl Hart Professor of Surgery in the division of cardiovascular and thoracic surgery at Duke. “I was lucky to meet him on my first day of medical school, and he was instrumental in my decision to become a thoracic surgeon. I worked in his lab during my third year of medical school, forming lasting relationships with him, his family and with his close friend and confidant Walter Wolfe. I cherish all the connections thus made with Bob at the center, and all returned full circle when he returned to become the Chairman of Surgery. To his enormous credit, he was singularly responsible for the critical transition from Dr. Sabiston’s leadership to a more modern, diverse department built to thrive in the 21st century. I do not believe that anyone else could have done a better job, and I will miss his larger than life presence every day.”
Strong leadership was the defining characteristic of Dr. Anderson’s career. He served as Chief of Cardiovascular and Thoracic Surgery at University of Minnesota Hospitals from 1979–1984, and held the same role at Evanston-Northwestern Hospital in Illinois from 1984–1986. He then served a dual-leadership role as Chair of the Department of Surgery at Evanston Hospital from 1986–1994, while concurrently serving as Chief of Cardiothoracic Surgery at Northwestern Memorial Hospital in Chicago from 1990–1994.
Prior to his surgical career, Dr. Anderson served in the military as Captain of the U.S. Army at the 3rd Surgical Hospital in Vietnam, and Director of the Trauma Research Unit at Walter Reed Army Medical Center. He received the Army Commendation Medal and Vietnam Service Medal for his service.
Our thoughts go out to the family and many friends of Dr. Anderson. He will be remembered as a skilled clinician, an accomplished investigator, and a respected leader, mentor, and colleague.
Information about memorial services will be shared as his family makes it available.
Program Partnership between AKU and Duke Receives 1.2 Million in NIH Funding
 A training program designed by researchers at Aga Khan University (AKU) in partnership with researchers at Duke University has been awarded a research training grant of $1.2 million over five years by the National Institutes of Health. The training program is designed to address a critical gap in response to a growing world-wide epidemic of non-communicable diseases (NCDs) such as cardiovascular and cerebrovascular disease. The NIH’s Fogarty International Center will administer the grant.
A training program designed by researchers at Aga Khan University (AKU) in partnership with researchers at Duke University has been awarded a research training grant of $1.2 million over five years by the National Institutes of Health. The training program is designed to address a critical gap in response to a growing world-wide epidemic of non-communicable diseases (NCDs) such as cardiovascular and cerebrovascular disease. The NIH’s Fogarty International Center will administer the grant.
Aga Khan University, located in Karachi, Pakistan, is situated in an area of the world with a pressing need to develop a cohort of trained researchers who can contribute to the understanding of NCD prevalence and risk factors as well as develop and test safe, effective, and low-cost solutions to them.
“This grant brings together research and intellectual expertise from two major institutions across the world with the shared vision of enhancing research capacity to tackle NCDs in Pakistan. This can be achieved as we keep equity and our drive for data at the core of our strategy. I look forward to working with our team at AKU and my long term colleagues at Duke to fulfill the goals of the Aga Khan University – Pakistan Initiative for NCDs program,” said Dr. Zainab Samad, Ibn-e-Sina endowed professor and chair of the Department of Medicine at the AKU, project director and contact principal investigator (PI) of this project. Samad is a cardiologist and adjunct associate professor of medicine in the Duke Division of Cardiology.
vision of enhancing research capacity to tackle NCDs in Pakistan. This can be achieved as we keep equity and our drive for data at the core of our strategy. I look forward to working with our team at AKU and my long term colleagues at Duke to fulfill the goals of the Aga Khan University – Pakistan Initiative for NCDs program,” said Dr. Zainab Samad, Ibn-e-Sina endowed professor and chair of the Department of Medicine at the AKU, project director and contact principal investigator (PI) of this project. Samad is a cardiologist and adjunct associate professor of medicine in the Duke Division of Cardiology.
The epidemic of NCDs presents an extraordinary crisis world-wide. Over three quarters of all NCD related deaths and 82 percent of premature NCD related deaths occur in low-and middle-income countries like Pakistan, where locally relevant and high-quality research data is scarce. According to the World Health Organization, nearly 50 percent of deaths in Pakistan are from NCDs, creating barriers to development goals including poverty reduction, human security, economic stability and health equity. The most prevalent NCDs are cardiovascular diseases, an area the comprehensive, integrated, multi-disciplinary research training program will focus on.
The training program leverages AKU and the AKU Institute for Global Health and Development’s extensive development network platform and infrastructure at its flagship site in Pakistan. The aim is to build sustainable research capacity, and develop a pool of Pakistani experts in cardio-cerebrovascular disease surveillance and implementation science who will provide the vision and leadership necessary to produce high-quality research of relevance to tackle NCDs in Pakistan and other low-and middle-income countries. This is in line with the Fogarty International Center’s mission of supporting and facilitating global health research conducted by U.S. and international investigators, building partnerships between health research institutions in the U.S. and abroad, and training the next generation of scientists to address global health needs.
 “This award is another milestone signaling the incredibly valuable collaboration between our mutual institutions. We are excited to join this effort as meaningful collaborators, researchers, and mentors. I am humbled to have the opportunity to lead collaborators from Duke University to assist Dr. Samad and her team to deliver on this important goal, and anticipate much success that will lead to improved health and lives saved,” said Dr. Gerald S. Bloomfield, associate professor of medicine in cardiology at Duke and associate research professor of global health at the Duke Global Health Institute. Bloomfield will serve as a PI on this project.
“This award is another milestone signaling the incredibly valuable collaboration between our mutual institutions. We are excited to join this effort as meaningful collaborators, researchers, and mentors. I am humbled to have the opportunity to lead collaborators from Duke University to assist Dr. Samad and her team to deliver on this important goal, and anticipate much success that will lead to improved health and lives saved,” said Dr. Gerald S. Bloomfield, associate professor of medicine in cardiology at Duke and associate research professor of global health at the Duke Global Health Institute. Bloomfield will serve as a PI on this project.
A large part of the grant will include research training that leverages digital information technology—with an opportunity to work with AKU’s Clinical and Translational Research Incubator (CITRIC) Health Data Science Center. Additional PIs based at AKU include Drs. Aysha Almas and Ayeesha Kamal.
Congratulations to all those at Duke and AKU involved in this important work!
Shout-Out to Dixson!
We received a terrific note this week regarding Jeff Dixson, a cardiology fellow.
Dear Dr. Crowley,
I am writing to recognize Dr. Jeff Dixson, who volunteered several hours of his time yesterday to teach our first-year medical students basic cardiac ultrasound. The students clearly loved learning from Dr. Dixson, and have been raving about the experience!
Thank you for sharing your gifted educators with our medical students!
Julian
Julian Hertz, MD, MScGH
Assistant Professor of Surgery & Global Health
Course Director, Longitudinal Point-of-care Ultrasound Curriculum
Duke University School of Medicine
Well done, Jeff!!!
Respiratory Care Week 2021: Oct. 24-31
Please join us in thanking and celebrating all respiratory therapists at Duke and elsewhere! Today is the start of Respiratory Care Week 2021. To mark the occasion, the Duke Heart respiratory care team has received a special message from Duke men’s basketball coach, Mike Krzyzewski.

October is Medical Ultrasound Awareness Month
Please join us in celebrating Medical Ultrasound Awareness Month (MUAM) throughout the month of October. MUAM is  held annually to raise awareness of the role diagnostic medical sonographers play in the medical community and to educate the public about medical ultrasound and its many uses in healthcare. We want to celebrate all Medical Sonographers with a special shout-out to our Duke Heart Center vascular and cardiac sonographers. We are grateful for the positive impact our sonography team has on the care of our patients.
held annually to raise awareness of the role diagnostic medical sonographers play in the medical community and to educate the public about medical ultrasound and its many uses in healthcare. We want to celebrate all Medical Sonographers with a special shout-out to our Duke Heart Center vascular and cardiac sonographers. We are grateful for the positive impact our sonography team has on the care of our patients.
Cardiac and vascular sonographers are the eyes of the providers by assessing important cardiovascular findings such as ejection fraction, valvular regurgitation, valvular stenosis, flow limiting lesions, and dangerous thrombus formation. Many diagnoses would fail to be identified without the skills and expertise of cardiovascular sonographers.
The history of cardiovascular sonography runs deep at Duke Health, starting with the first phased array ultrasound development, live 3D scanning, and the most recent developments in high speed ultrasound. This is thanks to many years of collaboration between the Cardiac Diagnostic Unit and Biomedical Engineering program, pioneered by colleagues and friends Joseph Kisslo, MD and Olaf Von Ram, PhD.
A heartfelt thank you to all of the medical sonographers throughout Duke Health!
Upcoming Events & Opportunities
Cardiology Grand Rounds
October 26: Sleep Disordered Breathing and Cardiovascular Disease with Jonathan Piccini, Marat Fudim and Andrew Spector. 5 p.m. Webex.
November 2: Coronary Microvascular Dysfunction with Jessica Duran. 5 p.m. Webex.
November 9: Case Conference – Lessons Learned in Peri-Operative LVAD Care with Amanda Coniglio. 5 p.m. Webex.
Upcoming Duke Heart CME
November 5: 13th Annual NC Research Triangle Pulmonary Hypertension Symposium. Course directors are H. James Ford (UNC) and Terry Fortin. 8:30 a.m. to 4:20 p.m. Morning case-based workshops have been cancelled due to Covid. Afternoon portion will be held via Zoom. For more information and to register, please visit: https://bit.ly/3DrZwuv.
Child Educational Rights Webinar
October 27: Heart Heroes Webinar. The American Heart Association- Southeast invites parents to join a FREE webinar to learn how to be their child’s best advocate in school. This webinar will be a great opportunity for parents to learn when, why & how to get involved in creating the best school environment for their child. Special needs, education plans and meetings at the school are just a few important discoveries parents can make in shaping their child’s learning experiences. Guest speaker: Lorilynn V. Bowie, EdD, Behavior Resource Teacher. Families of children with a congenital heart defect may find the information particularly helpful. Seminar is free, but registration is required: https://bit.ly/3vE1Yug.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged.
Duke Heart in the News:
October 15 — Jonathan Piccini
Medscape
Half-Dose DOACs Cut Bleeding, Thrombus Risk Post-Watchman LAA Closure
https://www.medscape.com/viewarticle/960974
Duke Heart Week ending October 17th 2021
Highlights of the week:
Friede & Nafissi at NCYIF 2021
Kevin Friede and Navid Nafissi presented their work at the 17th Annual Northwestern Cardiovascular Young Investigator’s Forum this weekend in Chicago. Friede presented his abstract, A Gene Expression Signature Reflective of Exposure to Antiplatelet Therapy is Associated with Bleeding. Mentor: Deepak Voora. Nafissi presented his abstract, Integration of Electronic Health Records with Genetics in Monogenic Electrophysiologic Disorders. Mentor: Svati Shah.

Both presentations were well received. Congratulations to Nafissi who was awarded 3rd place in the Basic Science category during the awards ceremony on Saturday evening, Oct. 16.


The event was presented by Northwestern University Feinberg School of Medicine and Creative Educational Concepts, Inc., and supported by an independent educational grant from AstraZeneca.
Nicely done, Kevin and Navid!!!
Latest by Tcheng is Hot Off the Press!

Congratulations to James Tcheng and his co-authors at the University of Nebraska Medical Center and University of Nebraska-Omaha for their newly published article “A Roadmap to a More Useful and Usable Electronic Health Record” in Cardiovascular Digital Health Journal:
Windle JR, Windle TA, Shamavu KY, Nelson QM, Clarke MA, Fruhling AL,Tcheng JE, A Roadmap to a More Useful and Usable Electronic Health Record, Cardiovascular DigitalHealth Journal (2021), doi: https://doi.org/10.1016/j.cvdhj.2021.09.007
Kudos to TRANSFORM-HF Team!
Congratulations to Tracy DeWald, Kim Biever and the entire Duke TRANSFORM-HF team for reaching 200 participants enrolled in the TRANSFORM-HF study. The team was notified this week that the Duke site is the highest enroller in TRANSFORM to date and is, so far, the only site to reach 200 participants. Way to go!!

Daubert Member of Championship Hockey Team
Fun fact: Duke Electrophysiologist James Daubert stays active by playing in a couple of local hockey leagues. He and his teammates in the ‘Summer Over-40 league’ recently won their league championship!
Daubert says his team includes a rather interesting cast of characters — professors, restaurant owners, recording studio owner-managers, business owners and at least one electrophysiologist… He adds that, for a team of players over 40, “the level of sportsmanship is pretty good although good natured competition for sure.”
His team had made it to the final game in the past two seasons, but had lost to their arch rivals, the “green” team both times. This season, however, Daubert’s “blue” team prevailed.
Congratulations, Jim!!!

Upcoming Events & Opportunities
Cardiology Grand Rounds
October 19: New Approaches to the Mitral Valve, with Jeff Gaca. 5 p.m. Webex.
October 20: Special Grand Rounds from Jonathan Lindner on Advanced Imaging and Cardiovascular Drug Development
October 26: Sleep Disordered Breathing and Cardiovascular Disease with Jonathan Piccini, Marat Fudim and Andrew Spector. 5 p.m. Webex.
November 2: Coronary Microvascular Dysfunction with Jessica Duran. 5 p.m. Webex.
Upcoming Duke Heart CME
November 5: 13th Annual NC Research Triangle Pulmonary Hypertension Symposium. Course directors are H. James Ford (UNC) and Terry Fortin. 8:30 a.m. to 4:20 p.m. Morning case-based workshops have been cancelled due to Covid. Afternoon portion will be held via Zoom. For more information and to register, please visit: https://bit.ly/3DrZwuv.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged.
Duke Heart in the News:
October issue– Division of Cardiology
Newsweek
World’s Best Specialized Hospitals 2021
https://www.newsweek.com/worlds-best-specialized-hospitals-2021
October 11 — William Kraus
Physician’s Weekly
Pandemic Intensifies Push for Home-Based Cardiac Care
https://duke.is/p4gs6
October 11 — Jacob Schroder
The Brunswick Beacon
Shallotte heart recipient one step closer to coming home
https://duke.is/cfsc8
October 12 — Mitch Krucoff
tctMD
Conversations in Cardiology: Do You Use Antibiotics in the Cath Lab?
https://duke.is/g3n65
October 13 — G. Michael Felker
tctMD
HF Care Didn’t Suffer as Clinicians Turned to Telehealth in COVID-19
https://duke.is/nyusc
October 13 — G. Michael Felker
HCPLive
Omecamtiv Mecarbil May Reduce Time To Event in Patients with Severe Heart Failure
https://duke.is/b9gdg
October 14 — Robert Califf
CBSNews.com*
Robert Califf is the leading contender for FDA commissioner
https://duke.is/6znt4
*story appears in dozens of news outlets
October 14 — Robert Califf
The Hill*
Biden likely to tap Robert Califf to return as FDA head
https://duke.is/phhxw
October 14 — Robert Califf
WSJ.com
Biden Weighs Nominating Former FDA Commissioner Robert Califf to Lead Agency Again
https://duke.is/r6u8b
October 15 — G. Michael Felker
Medpage Today
Analysis Makes Stronger Case for Omecamtiv Mecarbil in Severe HF
https://duke.is/5cgb7
Division of Cardiology Publications Indexed in PubMed Oct 4-13, 2021
Andonian BJ, Hardy N, Bendelac A, Polys N, Kraus WE. Making Cardiopulmonary Exercise Testing Interpretable for Clinicians. Curr Sports Med Rep 2021;20(10):545-552. PM: 34622820.
Blumenthal JA, Hinderliter AL, Smith PJ, Mabe S, Watkins LL, Craighead L, Ingle K, Tyson C, Lin PH, Kraus WE, Liao L, Sherwood A. Effects of Lifestyle Modification on Patients With Resistant Hypertension: Results of the TRIUMPH Randomized Clinical Trial. Circulation 2021;144(15):1212-1226. PM: 34565172.
Bossard M, Gao P, Boden W, Steg G, Tanguay JF, Joyner C, Granger CB, Kastrati A, Faxon D, Budaj A, Pais P, Di Pasquale G, Valentin V, Flather M, Moccetti T, Yusuf S, Mehta SR. Antiplatelet therapy in patients with myocardial infarction without obstructive coronary artery disease. Heart 2021;107(21):1739-1747. PM: 33504513.
Butala NM, Secemsky E, Kazi DS, Song Y, Strom JB, Faridi KF, Brennan JM, Elmariah S, Shen C, Yeh RW. Applicability of Transcatheter Aortic Valve Replacement Trials to Real-World Clinical Practice: Findings From EXTEND-CoreValve. JACC Cardiovasc Interv 2021;14(19):2112-2123. PM: 34620389.
Camp J, Glaubitz L, Filla T, Kaasch AJ, Fuchs F, Scarborough M, Kim HB, Tilley R, Liao CH, Edgeworth J, Nsutebu E, López-Cortés LE, Morata L, Llewelyn M, Fowler VG, Thwaites G, Seifert H, Kern WV, Kuss O, Rieg S. Impact of Immunosuppressive Agents on Clinical Manifestations and Outcome of Staphylococcus aureus Bloodstream Infection: A Propensity Score-Matched Analysis in 2 Large, Prospectively Evaluated Cohorts. Clin Infect Dis 2021;73(7):1239-1247. PM: 33914861.
Carnicelli AP, Hellkamp AS, Mahaffey KW, Singer DE, Breithardt G, Halperin JL, Hankey GJ, Piccini JP, Becker RC, Nessel CC, Berkowitz SD, Fox KAA, Califf RM, Patel MR. Termination Based on Event Accrual in Per Protocol Versus Intention to Treat in the ROCKET AF Trial. J Am Heart Assoc 2021;10(19):e022485. PM: 34569249.
Chunawala ZS, Fudim M, Arora S, Qamar A, Vaduganathan M, Mentz RJ, Pandey A, Caughey MC. Clinical and Echocardiographic Characteristics of Patients Hospitalized With Acute Versus Chronic Heart Failure With Preserved Ejection Fraction (From the ARIC Study). Am J Cardiol 2021;158:59-65. PM: 34474908.
Curzen N, Nicholas Z, Stuart B, Wilding S, Hill K, Shambrook J, Eminton Z, Ball D, Barrett C, Johnson L, Nuttall J, Fox K, Connolly D, O’Kane P, Hobson A, Chauhan A, Uren N, Mccann G, Berry C, Carter J, Roobottom C, Mamas M, Rajani R, Ford I, Douglas P. Fractional flow reserve derived from computed tomography coronary angiography in the assessment and management of stable chest pain: the FORECAST randomized trial. Eur Heart J 2021;42(37):3844-3852. PM: 34269376.
Debus ES, Nehler MR, Govsyeyev N, Bauersachs RM, Anand SS, Patel MR, Fanelli F, Capell WH, Brackin T, Hinterreiter F, Krievins D, Nault P, Piffaretti G, Svetlikov A, Jaeger N, Hess CN, Sillesen HH, Conte M, Mills J, Muehlhofer E, Haskell LP, Berkowitz SD. Effect of Rivaroxaban and Aspirin in Patients With Peripheral Artery Disease Undergoing Surgical Revascularization: Insights From the VOYAGER PAD Trial. Circulation 2021;144(14):1104-1116. PM: 34380322.
Eisenstein EL, Zozus MN, Terry SF, Davidson-Ray L, Anstrom KJ. Ascertaining Nonfatal Endpoints in Clinical Trials: Central Adjudication Versus Patient Insurance Claims. Ther Innov Regul Sci 2021;55(6):1250-1257. PM: 34228318.
Flumignan RL, Trevisani VF, Lopes RD, Baptista-Silva JC, Flumignan CD, Nakano LC. Ultrasound guidance for arterial (other than femoral) catheterisation in adults. Cochrane Database Syst Rev 2021;10:CD013585. PM: 34637140.
Gardner RS, Capodilupo RC, Ahmed R, Stolen CM, An Q, Averina V, Hernandez AF, Boehmer JP. Multiparameter diagnostic sensor measurements in heart failure patients presenting with SARS-CoV-2 infection. ESC Heart Fail 2021;8(5):4026-4036. PM: 34184428.
Ginsburg G, Penny M, Feero WG, Miller M, Addie S, Beachy SH. The National Academies’ Roundtable on Genomics and Precision Health: Where we have been and where we are heading. Am J Hum Genet 2021;108(10):1817-1822. PM: 34626581.
Greene SJ, Butler J. Investigator-Reported Versus Adjudicated Clinical Events: 2 Versions of the Truth? J Am Coll Cardiol 2021;78(15):1538-1540. PM: 34620411.
Johnson JN, Mandell JG, Christopher A, Olivieri LJ, Loke YH, Campbell MJ, Darty S, Kim HW, Clark DE, Frischhertz BP, Fish FA, Bailey AL, Mikolaj MB, Hughes SG, Oneugbu A, Chung J, Burdowski J, Marfatia R, Bi X, Craft J, Umairi RA, Kindi FA, Williams JL. Society for Cardiovascular Magnetic Resonance 2020 Case of the Week series. J Cardiovasc Magn Reson 2021;23(1):108. PM: 34629101.
Jones RC, Creutzfeldt CJ, Cox CE, Haines KL, Hough CL, Vavilala MS, Williamson T, Hernandez A, Raghunathan K, Bartz R, Fuller M, Krishnamoorthy V. Racial and Ethnic Differences in Health Care Utilization Following Severe Acute Brain Injury in the United States. J Intensive Care Med 2021;36(11):1258-1263. PM: 32912070.
Kim HJ, Snyder LD, Adegunsoye A, Neely ML, Bender S, White ES, Conoscenti CS, Strek ME. Hospitalizations in patients with idiopathic pulmonary fibrosis. Respir Res 2021;22(1):257. PM: 34592998.
Kim HW, Jenista ER, Wendell DC, Azevedo CF, Campbell MJ, Darty SN, Parker MA, Kim RJ. Patients With Acute Myocarditis Following mRNA COVID-19 Vaccination. JAMA Cardiol 2021;6(10):1196-1201. PM: 34185046.
Levy KD, Blake K, Fletcher-Hoppe C, Franciosi J, Goto D, Hicks JK, Holmes AM, Kanuri SH, Madden EB, Musty MD, Orlando L, Pratt VM, Ramos M, Wu R, Ginsburg GS. Correction: Opportunities to implement a sustainable genomic medicine program: lessons learned from the IGNITE Network. Genet Med 2021;23(10):2020. PM: 33288881.
Lopes RD, de Barros E Silva PGM, Furtado RHM, Alexander JH, Berwanger O. Age-adjusted D-dimer cutoffs to guide anticoagulation in COVID-19 – Authors’ reply. Lancet 2021;398(10308):1304. PM: 34627488.
Mentz RJ, Whellan DJ, Reeves GR, Pastva AM, Duncan P, Upadhya B, Nelson MB, Chen H, Reed SD, Rosenberg PB, Bertoni AG, O’Connor CM, Kitzman DW. Rehabilitation Intervention in Older Patients With Acute Heart Failure With Preserved Versus Reduced Ejection Fraction. JACC Heart Fail 2021;9(10):747-757. PM: 34246602.
Mirza KK, Szymanski MK, Schmidt T, de Jonge N, Brahmbhatt DH, Billia F, Hsu S, MacGowan GA, Jakovljevic DG, Agostoni P, Trombara F, Jorde U, Rochlani Y, Vandersmissen K, Reiss N, Russell SD, Meyns B, Gustafsson F. Prognostic Value of Peak Oxygen Uptake in Patients Supported With Left Ventricular Assist Devices (PRO-VAD). JACC Heart Fail 2021;9(10):758-767. PM: 34391745.
O’Neill BP, Grines C, Moses JW, Ohman EM, Lansky A, Popma J, Kapur NK, Schreiber T, Mannino S, O’Neill WW, Medjamia AM, Mahmud E. Outcomes of bailout percutaneous ventricular assist device versus prophylactic strategy in patients undergoing nonemergent percutaneous coronary intervention. Catheter Cardiovasc Interv 2021;98(4):E501-E512. PM: 34051033.
Oyama K, Giugliano RP, Blazing MA, Park JG, Tershakovec AM, Sabatine MS, Cannon CP, Braunwald E. Baseline Low-Density Lipoprotein Cholesterol and Clinical Outcomes of Combining Ezetimibe With Statin Therapy in IMPROVE-IT. J Am Coll Cardiol 2021;78(15):1499-1507. PM: 34620406.
Piccini JP, El-Chami M, Wherry K, Crossley GH, Kowal RC, Stromberg K, Longacre C, Hinnenthal J, Bockstedt L. Contemporaneous Comparison of Outcomes Among Patients Implanted With a Leadless vs Transvenous Single-Chamber Ventricular Pacemaker. JAMA Cardiol 2021;6(10):1187-1195. PM: 34319383.
Povsic TJ, Henry TD, Ohman EM, Pepine CJ, Crystal RG, Rosengart TK, Reinhardt RR, Dittrich HC, Traverse JH, Answini GA, Mokadam NA. Epicardial delivery of XC001 gene therapy for refractory angina coronary treatment (The EXACT Trial): Rationale, design, and clinical considerations. Am Heart J 2021;241:38-49. PM: 34224684.
Sharma A, Januzzi JL, Suchindran S, Coles A, Hoffmann U, Ferencik M, Patel MR, Ginsburg GS, Douglas PS. Utility of High-Sensitivity Troponin Among Stable Patients With Chest Pain Undergoing Stress Imaging (from PROMISE). Am J Cardiol 2021;158:148-149. PM: 34454709.
Sullivan AE, Nanna MG, Wang TY, Bhatt DL, Angiolillo DJ, Mehran R, Banerjee S, Cantrell S, Jones WS, Rymer JA, Washam JB, Rao SV, Ohman EM. Bridging Antiplatelet Therapy After Percutaneous Coronary Intervention: JACC Review Topic of the Week. J Am Coll Cardiol 2021;78(15):1550-1563. PM: 34620413.
Temu TM, Macharia P, Mtui J, Mwangi M, Ngungi PW, Wanjalla C, Bloomfield GS, Farquhar C, Nyanjau L, Gathecha GK, Kibachio J. Obesity and risk for hypertension and diabetes among Kenyan adults: Results from a national survey. Medicine (Baltimore) 2021;100(40):e27484. PM: 34622879.
Wang L, Wang E, Prado Balcazar J, Wu Z, Xiang K, Wang Y, Huang Q, Negrete M, Chen KY, Li W, Fu Y, Dohlman A, Mines R, Zhang L, Kobayashi Y, Chen T, Shi G, Shen JP, Kopetz S, Tata PR, Moreno V, Gersbach C, Crawford G, Hsu D, Huang E, Bu P, Shen X. Chromatin Remodeling of Colorectal Cancer Liver Metastasis is Mediated by an HGF-PU.1-DPP4 Axis. Adv Sci (Weinh) 2021;8(19):e2004673. PM: 34378358.
White PJ, McGarrah RW, Herman MA, Bain JR, Shah SH, Newgard CB. Insulin action, type 2 diabetes, and branched-chain amino acids: A two-way street. Mol Metab 2021;52:101261. PM: 34044180
Duke Heart week ending October 10th 2021
2021 Triangle Heart Walk Held Today
On behalf of the Duke Heart leadership team, we thank all of our colleagues who joined us in today’s Triangle Heart Walk. Together, our teams raised a significant amount of funding for the American Heart Association. With the many challenges each of us face not only at work, but in our personal lives, we remain grateful to all of you for the excellent work you’re doing each day throughout Duke Heart. We hope you took time today to walk at one of the Heart Walk pop-up locations here in the Triangle or at a location of your choosing.
A special thanks to the following team members who served as team captains representing Duke Heart this year: Edna Taylor, Jason Stokes, Madi Baublis, Manesh Patel, Allen Stephens and Jill Engel.
A very special thank you to Richard Shannon for serving as the DUHS Heart Walk Chair this year. Attached are some great shots of the Walk he and Brandy Patterson hosted at their home today that was specifically for kids. What a great way to model heart healthy behavior!




It’s National PA Week, Oct. 6-12
 Please join us in celebrating National Physician Assistants Week from October 6-12, in recognition of the PA profession and the many contributions they make to Duke Health and the nation’s health. In the midst of this challenging year, we are deeply grateful for the efforts and contributions of these vital members of the Duke Heart team.
Please join us in celebrating National Physician Assistants Week from October 6-12, in recognition of the PA profession and the many contributions they make to Duke Health and the nation’s health. In the midst of this challenging year, we are deeply grateful for the efforts and contributions of these vital members of the Duke Heart team.
The PA profession is dynamic and they have served as pioneers and leaders in health care delivery across all ages, populations, and settings. This year saw another first for the profession. Hayley Arceneaux, a PA at St. Jude Children’s Hospital, served as the Chief Medical Officer for the first all-civilian space trip aboard SpaceX – appropriately called Inspiration4.
As highly skilled multidisciplinary care team members and healthcare leaders, PAs provide exceptional patient care in virtually all medical specialties and settings. PAs are pivotal in the nation’s health care delivery and serve in critical roles throughout patient care, medical education, health administration, leadership, and research.
A very special thank you to all PAs throughout Duke Heart for the great work you’re doing!
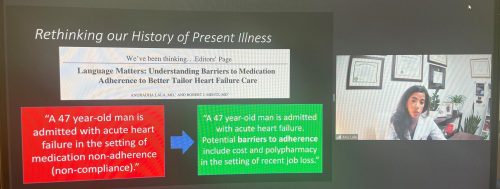
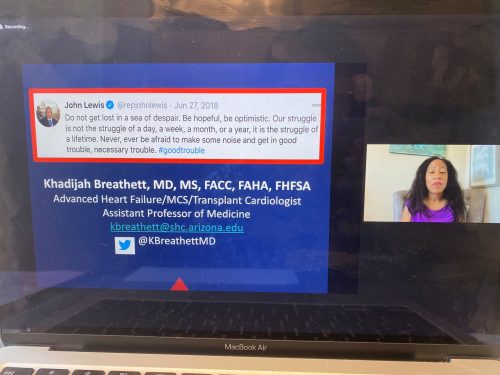
Heart Failure Symposium Success
The Duke Heart Failure Symposium: The Leading Edge of Heart Failure Management went exceedingly well on Friday. Great job by course directors Richa Agarwal and Rob Mentz!
Some highlights:
- More than 480 participants registered for the symposium.
- Attendees logged in from 34 different states and 27 different countries around the world.
- Participants included physicians, nurses, NPs, PAs, pharmacists, fellows, residents, students, research scientists, allied health professionals, industry representatives and patients!
Outstanding job and lots of great feedback and comments on Twitter!


Shout-out to Osude!
Congratulations to first year cardiology fellow Kiki Osude for running and completing the Bank of America Chicago Marathon today! Way to go Kiki!

Kudos, Duke Heart!
We received a wonderful note this week regarding care for a patient:
“On Monday evening (September 27), I called 911 for my mother. She was in a lot of pain and uncomfortable. EMS asked what hospital would they like me to take her to. As she was scheduled to meet for the first time with the Duke Heart TAVR team on October 11, I asked them to take her to Duke Hospital. It was a good call to make because she deteriorated on the short ride over.
The ED team were incredibly responsive, informative and kind. She was quickly moved to our CICU in 7E where she stayed until Tuesday around 5 pm. She then headed to 7700 where she stayed until her TAVR procedure this morning. I write this from 7W where she is recovering under the care of Shemia, who has been so helpful in addressing our questions and helping Mom manage any pain and discomfort.
I wanted to take a moment to let you know how wonderful her care has been, which I’m sure is no surprise to you. The entire Heart Care Team – from nursing to cardiologists, the ICU team, the surgeons to HUC and Food Services – have been so kind, so responsive, so helpful throughout her stay.
Many thanks to Drs. Ryan Plichta, Andrew Wang, Chris Granger and the attending physicians on 7E and 7700. They all visited Mom frequently and took time to explain the procedure and answer any questions she had. She went into the procedure with great confidence in them. The nursing team in ALL the areas have been AMAZING! I wish I would have done a better job getting their names. Their expertise, attentiveness and care have been phenomenal, especially RNs Becca and Ashleigh and NAs Leah, Amanda and Sherana on 7700. Alexandra from Food Service was super helpful and delightful as well.
We have another day or two here so I’m sure there will be people to add to the list, but my siblings, her 14 grandchildren, 7 great grandchildren and I are incredibly grateful.” – Name withheld for confidentiality
Nicely done, team!
Upcoming Events & Opportunities
Cardiology Grand Rounds
October 5: Critical Care Cardiology in the 21st Century with Anthony Carnicelli. 5 p.m. Webex.
October 12: Lessons from ADAPTABLE and PREVENTABLE: Is Pragmatism the Answer? with Schuyler Jones. 5 p.m. Webex.
October 19: CGR title pending, with Jeff Gaca. 5 p.m. Webex.
October 26: Sleep Disordered Breathing and Cardiovascular Disease with Jonathan Piccini, Marat Fudim and Andrew Spector. 5 p.m. Webex.
Upcoming Duke Heart CME
November 5: 13th Annual NC Research Triangle Pulmonary Hypertension Symposium. Course directors are H. James Ford (UNC) and Terry Fortin. 8:30 a.m. to 4:20 p.m. Morning case-based workshops have been cancelled due to Covid. Afternoon portion will be held via Zoom. For more information and to register, please visit: https://bit.ly/3DrZwuv.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged.
Duke Heart in the News:
October 5 — Robert Mentz
Cardiovascular Business
Heart failure patients benefit from rehabilitation intervention
https://duke.is/jku9g
October 6 — Manesh Patel
AARP
Myocarditis and COVID Vaccines: What You Need to Know Now
https://duke.is/yqg5d
October 6 — Manesh Patel
AARP
Las vacunas contra la COVID y la miocarditis: Esto es lo que debes saber
https://duke.is/z5rnx
October 6 — Tom Povsic
CBS17.com
https://duke.is/vgsmz
October 7 — Crystal Johnson (Duke Regional ICU)
WRAL.com
ICU nurse turns her COVID-19 experience into effort to promote heart health awareness
https://duke.is/b2gaj
Duke Heart Pulse week ending October 3rd 2021
Chief’s message:
Hopefully everyone is finding some time to be with family and friends in over the weekend. The Cath lab had some delayed summer games out at a park this weekend. Some fun photos attached as Dr. Sketch was the judge for the team competition.



Highlights of the week:
CICU Expansion
On Friday, October 1, 2021, the Cardiac Intensive Care Unit located on 7E in Duke Medical Pavilion expanded from 20 beds to 24 beds. Thanks to all who helped us with our expansion! We want to especially thank the Nursing leadership and nurses who are everyday at the bedside caring for our patients, our CICU pharmacist Jeff Washam who has helped ensure we deliver safe and evidence based care, and our faculty and fellows who have worked to ensure that we have been able to support our patients and teams. Additionally, we are excited to have our APPs lead by Corey Fry fully staffed and helping with the care of our patients and expansion. Shown here are (L-R): Manasi Tannu, Jocelyn Goodall, Abbie Prodruck, Sipa Yankey and Chris Granger on our opening day.
Great job, everyone!

Pulmonary Hypertension CME Update
Hosted by Duke and UNC in collaboration with the Pulmonary Hypertension Association, the 13th Annual NC Research Triangle Pulmonary Hypertension Symposium will be held on Friday, November 5, 2021. The previously scheduled morning case-based workshop is cancelled due to the resurgence of COVID-19, however the afternoon symposium/webinar will still take place from 12:00-4:20 p.m. Eastern on Zoom. Registration is complimentary but required. Register here. Please contact Christy Darnell with questions.
Triangle Heart Walk – One Week from Today
We have one week left before the Triangle Heart Walk! The walk is scheduled for Sunday, October 10 and there is still time for you to help us make this a great year, despite the ongoing pandemic. You can sign up as either a captain or a walkers, or simply donate to a member of an existing team. Registration and donations are quick and easy – you can start your own team or join an existing one: simply visit triangleheartwalk.org/dukehealth2021. Looking for a team to join? Manesh Patel and Jill Engel are both team captains and would be happy to have you join them! If you have any questions or need help, feel free to email Kimberly Burrows, senior director of development for the Triangle AHA, at kimberly.burrows@heart.org.
The American Heart Association will have “pop-up” starting lines for walkers at various locations throughout the Triangle:
- NC State Campus – LexisNexis, 1801 Varsity Dr. in Raleigh, NC 27606
- Healthy Mile – Holton Trail, 401 N. Driver St. in Durham, NC 27703
- Healthy Mile – Northgate Park Trail, 302 W. Club Blvd. in Durham, NC 27704
- Shelley Lake Loop, 1400 W. Millbrook Rd. in Raleigh, NC 27612
- Worthdale Park, 1001 Cooper Rd. in Raleigh, NC 27610
Or, you can choose to walk on your own, wherever is most convenient to you. Too busy to walk? You can support any Duke Heart team by making a general donation to a walker to support their fundraising efforts.
Thanks for considering. We appreciate every dollar!
Chmielewski Retires
Carl Chmielewski, administrative assistant in the division of cardiology, retired from Duke Heart this past week after 29 years of service to the Division of Cardiology. We collected thoughts from a range of team members this past week and a small team was able to treat him to lunch recently.
“Carl – a short note of acknowledgement and deep appreciation for being the “glue” for our faculty, staff, and Division. Your tireless attention to details to make the “magic happen” is one of the untold secrets underlying the success of Duke Cardiology. The endless hours you spent “herding the cats” – what a journey! Remember PDA’s? (For those of you who don’t know the acronym, PDA stands for personal digital assistant – yes, there was a time we used Palm Pilots and Windows Mobile devices). Remember the tape cartridge Dictaphones you deployed for our clinical documentation – and the work to convert to digital Dictaphones? Then remember converting from digital Dictaphones to direct voice to text in Epic? Thank you for making sure that we had just the right information at just the right time to make our lives work, not too much and not too little – plus the patience and persistence to make the exceptions work. And each of us was an exception! And you are truly the QGenda master – but before QGenda, there was AMION. And before AMION – there was Carl! Through it all, your even-keeled demeanor and consistent willingness to tackle the toughest of assignments stand out as best characteristics for us to emulate. Thank you for everything you mastered, the details you attended to, and your leadership, guidance and counsel you provided all of us – you will be deeply missed! Best wishes on the well-deserved next chapter of your journey of life.” – Jimmy Tcheng, MD
“Carl was one of the people in the Division that I first met, when I came to Duke 6 years ago. It was immediately clear that he was the go-to guy, who could demystify so many of the complex and confusing systems here at Duke. He was always very responsive as well as direct—if Carl said it, you could take it to the bank!” – Maria Price Rapoza, PhD
“Duke Cardiology is such a better place thanks to Carl. He has worked in the Division for past 29 years and has been truly committed to making it a better place. He has quietly done so much behind the scenes to help so many people. He will be so missed but truly deserves to be able to enjoy his pontoon boat!” – Mike Sketch, MD
“My work relationship with Carl begin over thirty plus years ago. During that time, Carl proved to be an amazing and dedicated employee to the Division of Cardiology and a valuable asset to the staff assistants. Any task or question the staff assistants needed help with, Carl had a solution. If there was a process we did not understand, Carl took the time to meet with you and walk you through every step. When I was given the administrative responsibilities in the Cardiovascular Research Center, Carl was instrumental in providing me with all of the resources needed to ensure a successful transition. Carl will be truly missed as he was our “go to” person in the Division of Cardiology.” — Cheryl Woodard
“Carl is one of those unsung heroes that is the “glue” that holds any diverse organization together. He is pretty much the proverbial “jack of all trades.” His job description includes fixing hardware (such as a monitor or a printer) and software (Qgenda has been his baby). His resourcefulness is evident from his office space where, much like a family hardware store, he can reach into one of his desk drawers and come up with a solution to most any problem. He is a master at using paper clips or twistee wire or duct tape to piece together whatever is needed to keep something up and running. And he always does so with enthusiasm, a smile and occasionally a corny joke. Hopefully he will get in more fishing and boating now. He will certainly be sorely missed.” – Tom Bashore, MD
We wish Carl all the best in his retirement!
Upcoming Events & Opportunities
Cardiology Grand Rounds
October 5: Critical Care Cardiology in the 21st Century with Anthony Carnicelli. 5 p.m. Webex.
October 12: Lessons from ADAPTABLE and PREVENTABLE: Is Pragmatism the Answer? with Schuyler Jones. 5 p.m. Webex.
October 26: Sleep Disordered Breathing and Cardiovascular Disease with Jonathan Piccini, Marat Fudim and Andrew Spector. 5 p.m. Webex.
Upcoming Duke Heart CME
October 8: Duke Heart Failure Symposium: The Leading Edge of Heart Failure Management. Course directors are Richa Agarwal and Robert Mentz. 12 – 4:30 p.m. Zoom Webinar. To learn more and to register, please visit: http://duke.is/Q1sBtf
November 5: 13th Annual NC Research Triangle Pulmonary Hypertension Symposium. Course directors are H. James Ford (UNC) and Terry Fortin. 8:30 a.m. to 4:20 p.m. Morning case-based workshops have been cancelled due to Covid. Afternoon portion will be held via Zoom. For more information and to register, please visit: https://bit.ly/3DrZwuv.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged.
Duke Heart in the News:
September 27 — James Blumenthal (psychiatry)
Healio/Cardiology
Structured lifestyle program for resistant hypertension improves BP, multiple biomarkers
https://duke.is/bc5x2
September 27 — James Blumenthal
MD Edge
Lifestyle interventions improve resistant hypertension
https://duke.is/che8m
September 27 — James Blumenthal
CNN Health*
DASH diet and exercise helps uncontrolled high blood pressure, study finds
https://duke.is/jppmf
*carried by 62 additional news outlets
September 27 — James Blumenthal
U.S. News & World Report*
Better Diet, More Exercise Equals Better Blood Pressure
https://duke.is/ygf64
*carried by 59 additional news outlets
September 29 — Duke University Hospital
WNCN CBS-17*
NC man home with family 3 months after receiving new-generation artificial heart at Duke Hospital
https://duke.is/r32z6
*also carried by FOX-8 Greensboro, CBS-3 Charlotte, & ABC-24 Wilmington
September 29 — Geoffrey Ginsburg
STAT News
https://duke.is/wxhhp
Recent Comments