Home » 2021
Yearly Archives: 2021
Duke Heart Pulse – Week Ending December 19th 2021
Chief’s message:
Dear Duke Heart Faculty, Staff, Fellows, Residents, and Community.

As 2021 comes to an end, we take time to reflect on the amazing accomplishments, resiliency, and teamwork of our entire Duke Heart community. In another difficult year, we were again privileged to be able to provide healthcare to our community, to be able to lean on each other in challenging times, and to be able to celebrate joint successes. Importantly we cherish our ability to continue to be with each other through these difficult times, frequently centering on our mission to train the next generation of heart leaders while we work to discover and deliver heart health.
So, on behalf of the Duke Heart Leadership team, we offer our heartfelt wishes of joy and health to you and your loved ones. More than ever, we recognize life is precious and hope that the season brings you peace — happiness, and warmth that comes from shared moments spent with friends and family.
Happy Holidays and Best Wishes in the upcoming year!
Highlights of the week:
Pediatric Team Receives SVRF Funding
 We learned this week that Andrew Landstrom, MD, PhD, and his colleagues have been awarded a 2021 Single Ventricle Research Fund award. The funding was announced publicly on Wednesday, Dec. 15 by Additional Ventures. Landstrom will receive $660,000 ($220K for three years) to study single ventricle heart disease in the laboratory; his project is titled, “Leveraging induced pluripotent stem cells to define the developmental drivers of hypoplastic left heart syndrome.” Landstrom will serve as principal investigator; Drs. Nick Andersen and Joe Turek will serve as co-investigators.
We learned this week that Andrew Landstrom, MD, PhD, and his colleagues have been awarded a 2021 Single Ventricle Research Fund award. The funding was announced publicly on Wednesday, Dec. 15 by Additional Ventures. Landstrom will receive $660,000 ($220K for three years) to study single ventricle heart disease in the laboratory; his project is titled, “Leveraging induced pluripotent stem cells to define the developmental drivers of hypoplastic left heart syndrome.” Landstrom will serve as principal investigator; Drs. Nick Andersen and Joe Turek will serve as co-investigators.


The grant is particularly notable because it represents the first major funding award for the Single Ventricle Care and Research Program (SVCRP) launched in 2019 and housed within Duke’s Pediatric and Congenital Heart Center. The SVCRP is dedicated to the care of children born with single ventricle heart disease and improving their survival and quality of life. Their multi-disciplinary team is dedicated to the longitudinal care of these patients, from fetal life through adulthood. The program is led by Nick Andersen, surgical director; Andrew McCrary, cardiology director, and Veera Allareddy, medical director.
Congratulations to all!!!
Lee Completes EP Fellowship; Will Return to Military Service
 Joshua Lee, DO, a fellow in the Duke Clinical Cardiac Electrophysiology Fellowship program, is completing his training with us this month and then heading back to San Antonio, TX. There, he will complete his military service with the U.S. Army and put his new skillset to work caring for patients at Brooke Army Medical Center, a 400-bed hospital situated at Fort Sam Houston.
Joshua Lee, DO, a fellow in the Duke Clinical Cardiac Electrophysiology Fellowship program, is completing his training with us this month and then heading back to San Antonio, TX. There, he will complete his military service with the U.S. Army and put his new skillset to work caring for patients at Brooke Army Medical Center, a 400-bed hospital situated at Fort Sam Houston.
Lee joined the EP fellowship in July 2019, spending the bulk of his time at Duke training during the COVID-19 pandemic. He says he chose the Duke program in part based on overall reputation, but also because he had known a former Duke EP fellow serving in the U.S. Army who had raved about their training here.
“When I first came to interview, I immediately sensed the collegiality between the EP attendings, as well as between the fellows and the attendings,” Lee says. “I knew I’d pick up excellent skills and knowledge here, but I also felt that I’d be joining a supportive, encouraging team who would provide great mentorship.”
He says that beyond the supportive environment, one of the things that really stood out to him was the emphasis on the importance of teamwork.
“Patient care is not just about offering a knowledgeable team of physicians,” Lee states. “It’s a holistic partnership involving EP technicians, EP staff, cardiologists, surgeons and general medicine – it’s all about teamwork. This has really been emphasized during my years here at Duke and it’s very similar to my work in the Army where you have a core group of people working together. You really develop a strong bond with others on your team.”
Electrophysiology began to intrigue Lee while he was practicing as a general cardiologist in San Antonio. During that time, he encountered a cardiac sarcoid patient with a recurrent ventricular tachycardia (VT). An electrophysiologist on the team performed a procedure and afterward the patient was shown to have no signs of VT and felt a lot better.
“It’s amazing how procedures, skills and knowledge are always improving in the EP field,” adds Lee. “Medicine is lifelong learning. I now have some great tools and resources that I’ve picked up during my time here at Duke and I am excited to keep learning more.”
Lee has four more years of commitment to fulfill with the Army and is looking forward to assisting in the training of general cardiology fellows when he gets back to Brooke Army Medical Center.
“It is very bittersweet to leave Duke, and while I feel sad about that, I am so excited to move on to another adventure,” Lee says. “I am so thankful to the many people that I have worked with here, especially the small group of EP attendings who work with our fellowship program. Everyone has been so easy to work with and it has been really fun. I felt happy every day to be here.”
It’s clear that Lee made just as big an impact on the EP team as they did on him.
“We are really grateful to have had Josh in our EP fellowship program during the trying and difficult times of the COVID pandemic,” said Jonathan Piccini, MD, associate professor of medicine and director of Duke Electrophysiology. “He has inspired all of us with his eternal optimism, refreshing smile, and the kindness he extends to everyone. He always goes the extra mile for every single one of his patients. We know the San Antonio area and military will be very fortunate to have Lt. Colonel Lee taking care of them and keeping their hearts in rhythm. We salute you Dr. Lee and thank you for your service to Duke, our country, and the US Armed Forces!”
Congratulations, Josh! We look forward to tracking your career and wish you all the best.
Duke Heart Network Welcomes Kotyra as new Senior Director
Duke Network Services is happy to introduce Lisa Kotyra, RN, MSBA, ACNP, as the new Senior Director of the Duke Heart Network.

Lisa comes to Duke Network Services after practicing in the Advanced Heart Failure Program at the University of Rochester Medical Center (URMC) as a Senior Nurse Practitioner and the Program Administrator. Lisa had been with Advanced Heart Failure since 2004 and has experience managing one of the largest VAD centers in the US (behind Duke). Additionally, Lisa’s role included oversight of both CMS and the Joint Commission regulatory processes for Advanced Heart Failure and VAD. Throughout her career, Lisa has cared for cardiovascular patients, including time spent as a nurse practitioner in the URMC Cardiothoracic ICU and in a private, community cardiology practice in both inpatient and outpatient roles. Lisa has been a longstanding member of the American Association of Critical Care Nurses (AACN) and the American College of Cardiology (ACC); most recently serving as the NY State representative for the national ACC CV Team.
Lisa received her Bachelor of Science in Nursing from State University of New York at Binghamton. She received her Masters of Science in Nursing (Acute Care NP Program/Critical Care) from the University of Rochester and her Masters of Science in Business Administration from the Simon Business School at the University of Rochester.
Lisa enjoys paddle boarding, hiking and traveling with family — perfect for our NC landscape. She is married with three children – one of whom is 26, and twins who are 19.
Please give her a warm welcome when you are able to do so!
Outing with Califf
Saturday, December 11, brought a fun outing with Rob Califf – Duke and UNC cardiologists Kristin Newby, Sid Smith (UNC), Magnus Ohman and Chris Granger spent the day out on the links helping to “prep” Califf for his FDA Commissioner Senate hearing, which was held on Tuesday, Dec. 14.
For more on the hearing, please visit: https://www.pbs.org/newshour/politics/watch-live-senate-hearing-on-the-nomination-of-robert-califf-as-commissioner-of-fda.

Ginsburg Celebrated, Pre-Departure for NIH
The team at Duke’s Center for Applied Genomics & Precision Medicine (CAGPM) gathered this week to honor Geoff Ginsburg in his final days as Center director. Ginsburg, a faculty member in our division of cardiology, is leaving Duke to take on the role of Chief Medical and Scientific Officer for the National Institutes of Health (NIH) All of Us Research Program starting next month. In a recent message to the CAGPM, he said, “Transitions are great opportunities for everyone. I am extremely confident in this team, in your future growth and successes, and that Duke CAGPM will continue to be at the forefront of genomics and precision medicine.”
We wish him all the best in his exciting new role and look forward to staying in touch!

Kudos to Ouyang
We received some terrific feedback from a patient recently on behalf of Wendy Chian Ouyang, one of our terrific nurse practitioners.
The patient’s note states: “Wen a gentle spirit, she is. Dr. Glower picked a great lady, caring, kind and a loving spirit. Super attentive.”
Thank you for the care and the compassion you show to all of the patients you provide care for, Wendy! We are very happy that you joined our team. – Diane Sauro, MSN, ANP, NEA-BC, Director-Advanced Practice, Duke Heart Center
Way to go, Wendy!

ICYMI: Final Tributes – Duke Univ & Health System Passings, 2021
We lost several members of our Duke Heart family in 2021. The University published a full list of all staff, faculty and retirees who passed away this past year, through November. To access that publication, please visit: https://bit.ly/3J3zBfB.
Happy Holidays & Reminder from the Pulse!
We wish each of you a calm, peaceful and joy-filled holiday season. Duke Heart Pulse will not be published on Dec. 26 or Jan. 2. We’ll be back on Sunday, Jan. 9. Be safe and healthy out there and we’ll see you in the New Year!
Upcoming Events & Opportunities
Duke Well-Being Ambassador Virtual Course
January 11 – March 15: The Well-being Essentials for Learning Life-Balance (WELL-B) weekly webinar series begins January 11, 2022 at 3 p.m. EST. For only one hour a week for 10 weeks (with an optional 11th week for sharing content with colleagues), healthcare workers can learn about the science and practice of well-being from Dr. Bryan Sexton, Dr. Carrie Adair, and Dr. Kyle Rehder. These strategies can enhance your well-being, and through sharing, the well-being of your co-workers. Available to all Duke Health employees and those outside of Duke as well. More information: bit.ly/dukewellb. Offered by the Duke Center for Healthcare Safety and Quality.
Duke Research Week 2022
January 31 – February 4: Registration is now open for Duke Research Week 2022. Join us virtually for a week-long celebration of research underway at Duke! There is an excellent lineup of faculty lectures, panel discussions, “flash talks” with graduate students, trainees and postdoctoral fellows, and guest presenters for the Robert J. Lefkowitz, MD, Distinguished Lecture and Daubechies Lecture. Check out the full agenda here: https://dukeresearchweek.vfairs.com/en/#distinguishedlectures

Save the Date: Wear Your Red
Friday, Feb. 4: National Wear Red Day. Seriously team, put this one on the calendar! It’s never too early to start thinking of what you can wear on National Wear Red Day — red running shoes? Heart socks? The perfect red top or sweater? A cool red tie? What about that AHA gear you picked up at the last in-person Sessions? Stock up, plan ahead and have plenty of attire to wear throughout heart month to help promote cardiovascular disease awareness — and YES — we would love to have individual and team photos to share in Pulse!!
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion. Note: Pulse is taking a break for the holidays (Dec. 26, Jan. 2). We’ll return on Jan. 9, 2022!
Duke Heart in the News:
December 13 — Manesh Patel
tctMD
World-wise: As In-Person Meetings Resume, Global Voices Hope to Be Heard
https://duke.is/g4tz7
December 14 — Stephen Greene
Medscape
Metformin Benefits Patients Hospitalized for Heart Failure
https://duke.is/w6c3p
December 15 — Svati Shah
Associated Press
$10 million invested to study long-term impact of COVID-19 on heart and brain health
https://duke.is/vdmnw
December 15 — Svati Shah
dicardiology.com
AHA Funds Research on Underlying Causes and Therapies for Cardiovascular Impacts of Long COVID
https://duke.is/ze76a
December 15 — Sunil Rao
Healio/Cardiology Today
DES systems to facilitate transradial PCI receive FDA approval
https://duke.is/mgxbq
December 15 — Rajesh Swaminathan
tctMD
Discharge Safe as Early as a Day After Primary PCI for STEMI
https://duke.is/85yyr
Duke Heart Pulse 12-12-2021
Highlights of the week:
Latest DUH Adult Cardiac Surgery Program STS Ratings
 We learned this week that our Adult Cardiac Surgery program has earned 3-star quality ratings for all ranked categories from the Society of Thoracic Surgeons (STS). The 3-star ratings were earned for isolated coronary artery bypass grafting (CABG) procedures; isolated aortic valve replacement (AVR) surgery; for AVR + CABG, and for isolated mitral valve replacement and repair (MVRR) surgery.
We learned this week that our Adult Cardiac Surgery program has earned 3-star quality ratings for all ranked categories from the Society of Thoracic Surgeons (STS). The 3-star ratings were earned for isolated coronary artery bypass grafting (CABG) procedures; isolated aortic valve replacement (AVR) surgery; for AVR + CABG, and for isolated mitral valve replacement and repair (MVRR) surgery.
The Duke University Hospital STS Risk Adjusted Harvest 3 report includes analyzed results for the 3-year period spanning July 2018 to June 2021.
The STS star rating system is one of the most sophisticated and highly regarded overall measures of quality in health care, rating the benchmarked outcomes of cardiothoracic surgery programs in the U.S. The star rating is calculated using a combination of quality measures for specific procedures performed by an STS Adult Cardiac Surgery Database (ACSD) participant.
Established in 1989 as an initiative for quality improvement and patient safety among cardiothoracic surgeons, the STS ACSD houses more than 6.5 million surgical records and gathers information from more than 3,800 participating physicians, including surgeons and anesthesiologists from more than 90 percent of groups that perform heart surgery in the U.S. The Database includes three other components: the Congenital Heart Surgery Database (CHSD), the General Thoracic Surgery Database (GTSD), and the mechanical circulatory support database (Intermacs). Duke has participated in the STS National Database since its inception.
This achievement is the result of the effort the entire Duke Heart team puts in every day — across the board – our nurses, residents, fellows, CT surgeons, anesthesiologists, ICU teams, cardiologists, pharmacy leaders, cardiac rehabilitation team and all those who support them. Congratulations!
CVRC Announces Annual Mandel Awards
The Duke Cardiovascular Research Center (CVRC) has recently announced their annual Mandel Awards. The Mandel Funding Program Review Committee made three awards in the Seed program, one award in the Fellow program, and one in the Scholar program. We are pleased to share the projects and scholars receiving funding for the 2022 project period which begins January 1.
Mandel Scholar Award
Ravi Karra, MD

Project: Correction of LMNA Cardiomyopathy by Cardioediting
Dilated cardiomyopathies (DCM) due to genetic mutations are common and more likely to progress to end stage heart failure compared to other types of DCM. Here, we propose the development of a system to treat genetic DCM by correcting the causal mutation, using LMNA DCM as an example. We will develop tools to genetically edit LMNA mutations and develop an ultrasound-based method to deliver these tools to the heart. These experiments can establish “cardioediting” as a potential treatment of heritable DCM.
Mandel Fellow Award
 Pavitra Murali, PhD, mentored by Sudha Shenoy, PhD
Pavitra Murali, PhD, mentored by Sudha Shenoy, PhD
Project: Trafficking of Angiotensin Receptors into autophagosomes and its impact on
β-arrestin-dependent signaling
Drugs that bind to the extracellular domains of cell-surface G protein-coupled receptors (GPCRs) are used to treat a variety of cardiovascular diseases including hypertension. Activated GPCRs trigger a signal transduction cascade that produces physiological responses including contraction/relaxation of smooth muscle cells lining arteries. GPCRs, which are bound by drugs at the plasma membrane, rapidly internalize into the cell into intracellular vesicles called endosomes and subsequently traffic into highly acidic vesicles called lysosomes where the GPCR protein is degraded into small peptides. This degradation ensures the long-term desensitization or dampening of signaling and subsiding of the physiological action. We have found that internalized angiotensin type II receptor (AT1R) localizes into a distinct population of vesicles called autophagosomes, which is an unexpected phenomenon because the pathway that invokes formation of autophagosomes called autophagy is known only for recycling organelles and protein catabolism during cell starvation. Since agonist Ang II provokes autophagy trafficking of the AT1R, we believe that this sub-cellular localization may have putative roles in defining AT1R signaling and physiologic effects. The AT1R is an essential target for drugs used to treat many forms of cardiovascular diseases including hypertension; recent evidence reveals that the AT1R mediates its physiologic effects through both G protein and β-arrestin-dependent pathways. In this proposal, I will study how the autophagy trafficking of the AT1R is regulated, and determine the relevance of this trafficking pathway to AT1R signal transduction. The proposed studies will uncover hitherto unknown molecular mechanisms in AT1R trafficking and signaling and might provide new therapeutic angles to treat high blood pressure and cardiovascular disease.
Mandel Seed Awards
Neil Freedman, MD and Christopher Holley, MD, PhD

Project: Atherogenic Mechanisms of Small Nucleolar RNAs
Atherosclerosis fundamentally involves oxidation, a chemical process that is critical for
normal cell function. When oxidation is excessive, it deranges the chemical structure of lipids and proteins and thereby adversely affects their function. The pathogenesis of atherosclerosis initiates with oxidation of the cholesterol-rich low-density lipoprotein particles, and perpetuates with excessive oxidative cell signaling—termed “oxidative stress”—in the inner layers of the artery. This project aims to attenuate excessive oxidative signaling through a novel regulatory mechanism involving particular RNA molecules known as small nucleolar RNAs, or “snoRNAs”, which are expressed throughout the body’s cells. We have found a group of four snoRNAs that augment cellular oxidative stress (Rpl13a-snoRNAs); they appear to do so by facilitating the modification of various messenger RNAs with 2’-O-methylation—a modification that reduces the translation of the messenger RNA into protein.
With previous support from the Mandel Foundation, we found that genetic deficiency of these snoRNAs in Apoe-/- mice reduces arterial levels of reactive oxygen species and attenuates atherosclerosis. Furthermore, we found that snoRNA deficiency in smooth muscle cells dramatically increases the expression of a mitochondrial protein (COX4i2) that reduces mitochondrial production of reactive oxygen species. Therefore, we hypothesize that snoRNAs augment the level of reactive oxygen species in vascular cells by methylating the messenger RNA encoding COX4i2 and thereby reducing the cellular level of COX4i2 protein.
The Mandel Seed Grant will allow us to continue our snoRNA atherosclerosis studies until we can secure NIH funding. Specifically, this new application seeks to achieve the following aims: (1) to determine whether antagonizing snoRNA function with antisense oligonucleotides reduces atherosclerosis in low-density lipoprotein receptor-deficient (Ldlr-/-) mice, and thereby to determine whether snoRNAs can be targeted therapeutically, and (2) to determine in vascular smooth muscle cells and macrophages whether the pre-mRNA encoding COX4i2 is a target of snoRNA-guided methylation, and thereby to elucidate molecular mechanisms underlying the effects of snoRNAs on cellular oxidative stress. Completing these aims will advance our work toward publishing our first manuscript and obtaining NIH support for our ongoing investigations into the anti-atherogenic therapeutic potential of snoRNA-targeted strategies.
Christopher Kontos, MD
Project: Regulation of endothelial metabolism by the Tie1 receptor tyrosine kinase
In the presence of oxygen, cells typically generate energy by breaking down glucose through glycolysis, and then the byproduct, pyruvate, is used by mitochondria to generate ATP through aerobic respiration. Under anaerobic conditions lacking oxygen, cells are unable to utilize mitochondrial respiration, and after glycolysis, pyruvate gets converted to lactate, which is then shuttled out of the cell. Although oxidative metabolism is more efficient than anaerobic glycolytic metabolism in terms of energy production, some cells paradoxically utilize glycolysis as their main form of energy production even in the presence of oxygen.
This phenomenon of “aerobic glycolysis”, was first described by Dr. Otto Warburg (also known as the “Warburg Effect”) in cancer cells. Interestingly, aerobic glycolysis occurs not only in aberrant cancer cells, but it is the primary metabolic pathway that endothelial cells lining the vasculature use to generate energy. Alterations in endothelial cell metabolism are a hallmark of their activation, which occurs during new blood vessel growth and inflammation, and while this activation may be helpful in some contexts, e.g., growth of new blood vessels in response to exercise, the activation of endothelial cells in large arteries can be harmful and lead to atherosclerosis and high blood pressure. When endothelial cells are activated, their metabolism changes to increase their rate of glycolysis, but how they do this is not completely understood.
We hypothesize that the endothelial receptor tyrosine kinase Tie1, which is increased in activated endothelial cells, is partially responsible for altering the metabolism of these activated endothelial cells, and that blocking Tie1’s role in this metabolic shift may help prevent vascular dysfunction and subsequent cardiovascular disease.
Huanghe Yang, PhD
 Project: Demystify flow-activated chloride conductance in endothelium and its role in hypertension
Project: Demystify flow-activated chloride conductance in endothelium and its role in hypertension
Mechanical forces are fundamental in cardiovascular health and disease. Lining the interior surface of blood vessels, the endothelium constantly senses blood flow-induced shear and stretch forces and converts these mechanical stimuli into biochemical signals. Endothelial mechanotransduction is therefore central for both acute vasoregulation and chronic vascular remodeling; and malfunction of endothelial mechanotransduction contributes to cardiovascular diseases including hypertension and atherosclerosis. Mechanosensitive ion channels (MSCs) are the primary mechanotransducers in the endothelium. The endothelial MSCs, including the recently discovered mechanosensitive PIEZO1 calcium permeable channel, have been extensively investigated. Nevertheless, the molecular identity and pathophysiological role of an endothelial flow-activated chloride conductance (FACC) still remain elusive.
Our preliminary results showed that the FACC is significantly upregulated in angiotensin II (Ang II)-treated endothelial cells in vitro, highlighting the urgency to uncover its molecular identity and contribution in hypertension. With this Seed Grant, we aim to acquire critical preliminary results to strengthen our hypothesis that the functional coupling between Piezo1 mechanosensitive calcium channel and TMEM16A calcium-activated chloride channel (CaCC) gives rise to the FACC and enhanced endothelial FACC contributes to hypertension. I anticipate to utilize this opportunity to establish collaborations with CVRC investigators and submit an NIH R01 to further understand FACC in endothelial biology and diseases.
Congratulations to all Mandel funding recipients – we look forward to learning more about your work!
ICYMI: 2021 ACC/AHA/SCAI Guideline for Coronary Artery Revascularization
Congratulations to Brittany Zwischenberger and Sunil Rao, two members of the writing team for the latest Guidelines for Coronary Artery Revascularization which were co-published online in the Journal of the American College of Cardiology and in Circulation on Thursday. ACC/AHA Joint committee members from Duke include: Sana Al-Khatib, Adrian Hernandez, W. Schuyler Jones, and Dan Mark.

Congratulations to Helen Barnes!
Duke Heart’s leadership team wishes to congratulate Helen Barnes who graduated yesterday from University of Mount Olive with a Bachelor of Science degree in Business Administration in Healthcare Management.
“Helen is a great asset who is always willing to partner on new projects with a ready smile and kind words,” said Laura Blue, DNP, VAD Program Team Lead. “I am so proud of her for pursuing her dream of getting her degree and I think she is a great role model for others who wish to pursue their education. Helen was a big supporter of mine when I was working on my doctorate. When she came to me and let me know she felt she could achieve this, I wanted to support her as much as she had supported me. I am really excited for her.”
Barnes, a dedicated member of the Duke family since 1999, has functioned as an administrative assistant with the Duke’s Ventricular Assist Device program for 11 years. Helen partnered with leadership to develop and successfully lead her final project, “Optimizing Incoming Communication in a Multidisciplinary Subspecialty Clinic.”
Congratulations, Helen!
Hofmeister Lands Emerging Leaders Grant
Karl Hofmeister, a 2021 graduate of Duke’s Cardiac Ultrasound Certificate program, has been selected by the Society of Diagnostic Medical Sonography (SDMS) Foundation for their 2022 Emerging Leaders Grant Recipient Program. Hofmeister’s cohort will participate virtually in a variety of leadership education opportunities that are designed to engage them in meaningful dialogue and projects related to the future of the profession and leadership volunteerism.
Hofmeister was the first recipient of our Cardiac Ultrasound Certificate program’s inaugural outstanding student award, which is now named after Joseph Kisslo, MD.
The Emerging Leaders program will culminate with one participant being selected to receive a grant to attend the Fall SDMS and SDMS Foundation Board of Directors Meetings, Liaison Meetings, and the 2022 SDMS Annual Conference.
Congratulations, Karl!
Upcoming Events & Opportunities
SI4R Training Workshop
December 14: Stepping in 4-Respect (SI4R) Workshop for Duke Division of Cardiology. 5-7 p.m. Zoom (Details in email from Kim Dorman)
As part of the Department of Medicine Civility Champion initiatives, a 2-hr zoom workshop for all faculty, staff, and trainees throughout all DOM divisions has been developed. Civility Champions are trained faculty, fellows, and chief residents who provide informal support in response to incidents of bias, harassment, or other unprofessional behaviors, and to help those affected understand their options for intervention and reporting. People generally come to Civility Champions after the fact, and the Champions debrief their experiences every quarter.
The workshop that Drs. John Duronville, Jane Gagliardi, Anita Kelsey, Camille Frazier-Mills, Daniella Zipkin, Laura Previll, and Sophia Weinmann will be presenting to the Cardiology clinical faculty is entitled Stepping In 4-Respect. It is being offered twice and is a new component of these civility efforts designed to teach faculty the skills needed to step in (be an “upstander”) in the moment, with a particular focus on race-, ethnicity- and gender-based incidents. This workshop is supported by Dr. Kathleen Cooney, Chair of the DOM, and will be provided to each division’s faculty over the coming months.
Please be sure to attend the workshop on Dec. 14 if you missed the one on Nov. 30. Additional details about registration, the structure and goals of the workshop appeared in the email invitation.
Duke Well-Being Ambassador Virtual Course
January 11 – March 15: The Well-being Essentials for Learning Life-Balance (WELL-B) weekly webinar series begins January 11, 2022 at 3 p.m. EST. For only one hour a week for 10 weeks, healthcare workers can learn about the science and practice of well-being from Dr. Bryan Sexton, Dr. Carrie Adair, and Dr. Kyle Rehder. These strategies can enhance your well-being, and through sharing, the well-being of your co-workers. Available to all Duke Health employees and those outside of Duke as well. More information: bit.ly/dukewellb. Offered by the Duke Center for Healthcare Safety and Quality.
Duke Research Week 2022
January 31 – February 4: Registration is now open for Duke Research Week 2022. Join us virtually for a week-long celebration of research underway at Duke! There is an excellent lineup of faculty lectures, panel discussions, “flash talks” with graduate students, trainees and postdoctoral fellows, and guest presenters for the Robert J. Lefkowitz, MD, Distinguished Lecture and Daubechies Lecture. Check out the full agenda here: https://dukeresearchweek.vfairs.com/en/#distinguishedlectures

Save the Date: Wear Your Red
Friday, Feb. 4: National Wear Red Day. Seriously team, put this one on the calendar! It’s never too early to start thinking of what you can wear on National Wear Red Day — red running shoes? Heart socks? The perfect red top or sweater? A cool red tie? What about that AHA gear you picked up at the last in-person Sessions? Stock up, plan ahead and have plenty of attire to wear throughout heart month to help promote cardiovascular disease awareness — and YES — we would love to have individual and team photos to share in Pulse!!
Save the Date: Support the Marfan Foundation
February 11: An Evening with Heart to benefit The Marfan Foundation. 7-10 p.m. at The Maxwell in Raleigh, NC. A Valentine’s Day weekend event with silent auction, cocktails, heavy hors d’oeuvres and entertainment. Cocktail attire. Tickets required. For information, visit: https://bit.ly/3cHIBYD.
The Duke Center for Aortic Disease, led by cardiovascular surgeon Chad Hughes, works closely with Marfan patients, their family members and the Marfan Foundation. We are the only location in NC offering access to comprehensive aortic surgical interventions as well as coordinated cardiovascular care and genetic counseling for patients with Marfan syndrome and other connective tissue disorders such as Loeys-Dietz. If you’re interested in learning more about the work being done at Duke or would like to partner or otherwise get involved, please contact Dr. Hughes or Melissa Merrill Burkett, ACNP.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion. Note: Pulse will be taking a break for the holidays from Dec. 26 through Jan. 2; we’ll return on Jan. 9, 2022!
Duke Heart in the News:
December 3 — E. Hope Weissler and W. Schuyler Jones
tctMD
Statins Underprescribed in PAD Before and After Interventions
https://duke.is/722jz
December 7 — E. Hope Weissler and W. Schuyler Jones
Physician’s Weekly
PAD: Statin Prescribing After Revascularization Still Low
https://duke.is/mmhc7
December 8 — Amanda Coniglio
NIH
Rare gene mutation in some Black Americans may allow earlier screening of heart failure
https://bit.ly/3IGG8N5
December 9 — Duke University Hospital
Becker’s Hospital Review
https://bit.ly/3lVQ77f
December 9 — Amanda Coniglio
Clinicalomics
Mutation Linked to Heart Failure in People of African Descent
https://bit.ly/3EKmCNf
Division of Cardiology Publications Indexed in PubMed December 2-8, 2021
Becher PM, Schrage B, Benson L, Fudim M, Corovic Cabrera C, Dahlström U, Rosano GMC, Jankowska EA, Anker SD, Lund LH, Savarese G. Phenotyping heart failure patients for iron deficiency and use of intravenous iron therapy: data from the Swedish Heart Failure Registry. Eur J Heart Fail 2021:10.1002/ejhf.2338. PM: 34476878.
Bernstein E, Wang TY. Point-of-Care Ultrasonography: Visually Satisfying Medicine or Evidence-Based Medicine? JAMA Intern Med 2021:10.1001/jamainternmed.2021.5831. PM: 34633409.
Carnicelli AP, Li Z, Greiner MA, Lippmann SJ, Greene SJ, Mentz RJ, Hardy NC, Blumer V, Shen X, Yancy CW, Peterson PN, Allen LA, Fonarow GC, O’Brien EC. Sacubitril/Valsartan Adherence and Postdischarge Outcomes Among Patients Hospitalized for Heart Failure With Reduced Ejection Fraction. JACC Heart Fail 2021;9(12):876-886. PM: 34509408.
Del Rosario M, Guduguntla V, Wang TY. Nonfatal Myocardial Infarction-Poor Surrogate for Mortality. JAMA Intern Med 2021:10.1001/jamainternmed.2021.5713. PM: 34694340.
Escaned J, Cao D, Baber U, Nicolas J, Sartori S, Zhang Z, Dangas G, Angiolillo DJ, Briguori C, Cohen DJ, Collier T, Dudek D, Gibson M, Gil R, Huber K, Kaul U, Kornowski R, Krucoff MW, Kunadian V, Mehta S, Moliterno DJ, Ohman EM, Oldroyd KG, Sardella G, et al. Ticagrelor monotherapy in patients at high bleeding risk undergoing percutaneous coronary intervention: TWILIGHT-HBR. Eur Heart J 2021;42(45):4624-4634. PM: 34662382.
Hess CN, Debus ES, Nehler MR, Anand SS, Patel MR, Szarek M, Capell WH, Hsia J, Beckman JA, Brodmann M, Diaz R, Habertheuer P, Leeper NJ, Powell RJ, Sillesen H, Muehlhofer E, Berkowitz SD, Haskell LP, Bauersachs RM, Bonaca MP. Reduction in Acute Limb Ischemia with Rivaroxaban versus Placebo in Peripheral Artery Disease after Lower Extremity Revascularization: Insights from VOYAGER PAD. Circulation 2021:10.1161/CIRCULATIONAHA.121.055146. PM: 34637332.
Hsia J, Kavanagh ST, Hopley CW, Baumgartner I, Berger JS, Fowkes GR, Jones WS, Mahaffey KW, Norgren L, Patel MR, Rockhold F, Blomster J, Katona BG, Hiatt WR, Bonaca MP. Impact of chronic kidney disease on hemoglobin among patients with peripheral artery disease treated with P2Y inhibitors: Insights from the EUCLID trial. Vasc Med 2021;26(6):608-612. PM: 34082620.
Ma Z, Viswanathan G, Sellig M, Jassal C, Choi I, Garikipati A, Xiong X, Nazo N, Rajagopal S. β-Arrestin-Mediated Angiotensin II Type 1 Receptor Activation Promotes Pulmonary Vascular Remodeling in Pulmonary Hypertension. JACC Basic Transl Sci 2021;6(11):854-869. PM: 34869949.
Mack M, Carroll JD, Thourani V, Vemulapalli S, Squiers J, Manandhar P, Deeb GM, Batchelor W, Herrmann HC, Cohen DJ, Hanzel G, Gleason T, Kirtane A, Desai N, Guibone K, Hardy K, Michaels J, DiMaio JM, Christensen B, Fitzgerald S, Krohn C, Brindis RG, et al. Transcatheter Mitral Valve Therapy in the United States: A Report From the STS-ACC TVT Registry. J Am Coll Cardiol 2021;78(23):2326-2353. PM: 34711430.
Manolio TA, Bult CJ, Chisholm RL, Deverka PA, Ginsburg GS, Goldrich M, Jarvik GP, Mensah GA, Ramos EM, Relling MV, Roden DM, Rowley R, Williams MS, Green ED. Genomic medicine year in review: 2021. Am J Hum Genet 2021;108(12):2210-2214. PM: 34861172.
Matsue Y, Sama IE, Postmus D, Metra M, Greenberg BH, Cotter G, Davison BA, Felker GM, Filippatos G, Pang P, Ponikowski P, Severin T, Gimpelewicz C, Voors AA, Teerlink JR. Association of Early Blood Pressure Decrease and Renal Function With Prognosis in Acute Heart Failure. JACC Heart Fail 2021;9(12):890-903. PM: 34627724.
Salah HM, Pandey A, Soloveva A, Abdelmalek MF, Diehl AM, Moylan CA, Wegermann K, Rao VN, Hernandez AF, Tedford RJ, Parikh KS, Mentz RJ, McGarrah RW, Fudim M. Relationship of Nonalcoholic Fatty Liver Disease and Heart Failure With Preserved Ejection Fraction. JACC Basic Transl Sci 2021;6(11):918-932. PM: 34869957.
Salisbury AC, Safley DM, Kennedy KF, Bhardwaj B, Aronow HD, Jones WS, Feldman DN, Secemsky E, Tsai TT, Attaran RR, Spertus JA. Development and validation of a predictive model for bleeding after peripheral vascular intervention: A report from the National Cardiovascular Data Registry Peripheral Vascular Interventions Registry. Catheter Cardiovasc Interv 2021;98(7):1363-1372. PM: 34569709.
Samsky MD, Mentz RJ, Stebbins A, Lokhnygina Y, Aday AW, Pagidipati NJ, Jones WS, Katona BG, Patel MR, Holman RR, Hernandez AF, Gutierrez JA. Polyvascular disease and increased risk of cardiovascular events in patients with type 2 diabetes: Insights from the EXSCEL trial. Atherosclerosis 2021;338:1-6. PM: 34741929.
Stefanini GG, Briguori C, Cao D, Baber U, Sartori S, Zhang Z, Dangas G, Angiolillo DJ, Mehta S, Cohen DJ, Collier T, Dudek D, Escaned J, Gibson CM, Gil R, Huber K, Kaul U, Kornowski R, Krucoff MW, Kunadian V, Moliterno DJ, Ohman EM, Oldroyd KG, Sardella G. Ticagrelor monotherapy in patients with chronic kidney disease undergoing percutaneous coronary intervention: TWILIGHT-CKD. Eur Heart J 2021;42(45):4683-4693. PM: 34423374.
Weissler EH, Jones WS. Who Will Own the Responsibility to Prescribe Statins? Tragedy of the Commons. JAMA Netw Open 2021;4(12):e2137605. PM: 34860247.
Duke Heart Pulse week ending 12-5-2021
Highlights of the week:
New Faculty Spotlight: Brandy Patterson, MD

One of our newest faculty members, Brandy Patterson, MD, joined the Duke Heart faculty in July as an assistant professor of medicine in the division of cardiology. She is a welcome addition to our growing cardio-oncology program and member of the general cardiology team, seeing patients at Duke Cardiology’s South Durham clinic; in Clinic 2F/2G, and in the Duke Cancer Center.
Patterson completed fellowship in cardiology at the University of Florida after earning her MD from the Leonard M. Miller School of Medicine at the University of Miami, and completing residency at Allegheny General Hospital in Pennsylvania. During fellowship she became fully attuned to the lack of women enrolled in research clinical trials — particularly those focused on cardiovascular disease — and realized how much work was still needed to educate women about their risk for developing heart disease.
“I was lucky to join the fellowship program in Florida when I did. There were a large number of female faculty members there and they all understood this problem,” Patterson said. “Many women attribute early-onset heart symptoms simply to getting older, or to putting on a bit of weight. I was astounded by the number of female patients I was seeing that did not recognize heart disease as a woman’s disease. I knew I needed to do something about this.”
After fellowship, she joined the faculty at the University of Pennsylvania where her clinical focus was on treating women with heart disease. From there, she headed to the University of Virginia where she launched a number of efforts aimed at women – she started a women’s heart health group called ‘Club Red’; organized regular community talks for women; partnered with a nutritionist to hold regular community cooking classes; and led walks in the community, all to better engage with women around living a heart-healthy lifestyle. She was able to take her messaging further when she became a regular guest on the local NBC news affiliate in Charlottesville, where they had a medical news segment called ‘House Call’ and then developed one with Patterson in mind, called ‘Straight Talk MD’.
As these community efforts were gaining momentum, a fellow faculty member left UVA and Patterson inherited a number of her patients — many of whom had received treatment for breast and other cancers. As she saw more and more heart patients with a history of cancer treatment, she became increasingly interested in understanding the cardiotoxicity associated with the drugs her patients were or had been taking. Her exploration into this area led her to spearhead the creation of UVA’s cardio-oncology program with two other cardiologists there – a team she led as medical director until her departure for Duke.
Patterson, who was raised in South Florida, was drawn to medicine from an early age. Her mother, an operating room nurse, periodically brought her to the hospital in which she worked. There, she had ample opportunity to observe her mother’s work, her interactions with colleagues and patients, and to learn about the OR space. Her father, a former professional baseball player who pitched for the New York Yankees, endured a number of injuries over time that required surgical intervention, rehabilitation and physical therapy.
“I really developed a deep understanding of what the patient experience is like by living in the footsteps of not only my mother, but my father and his experiences with numerous orthopedic surgeries and the toll it took on us as a family,” Patterson said while reflecting on her choice to pursue a career in medicine. “I wanted to develop and maintain a personal connection with people to increase patient’s healthy life years without disability.”
Having grown up with athletic parents, she was involved in multiple sports from an early age and has always been drawn to living a healthy lifestyle, eating right and exercising. She says she has always has been a big advocate for the joy of movement and to following a Mediterranean-style diet. Patterson and husband Richard Shannon, MD, have a 7-year-old daughter. They enjoy playing golf and tennis, as well as hiking, swimming, and traveling.
Shannon was recruited to Duke two years ago. When the opportunity presented itself for Patterson to join Duke Heart’s growing cardio-oncology program, she jumped at the chance.
“I am very humbled to be a part of this prestigious group and am looking forward to seeing where this opportunity leads. Duke has an amazing health system and this is a tremendous opportunity for us,” she added.
If you have not yet had the opportunity to meet Brandy, we hope you’ll take time to do so. We are thrilled to have her as a member of the Duke Heart team!
Daubert & Team Receive $7.9M NHLBI Grant to Examine CAC Scoring

Congratulations to Melissa Daubert and her co-investigators at Johns Hopkins and Wake Forest University. Daubert and her research partners have received a $7.9 million, five-year R01 grant from the National Heart, Lung and Blood Institute (NHLBI) to study the use of coronary artery calcium (CAC) scoring to identify who is the most likely to benefit from statin therapy and in whom preventive therapy with statins may not yield a meaningful clinical benefit. CAC PREVENTABLE, an ancillary study to the Pragmatic Evaluation of Events and Benefits of Lipid-lowering in Older Adults (PREVENTABLE) Trial, will enroll 10,000 participants age 75 years and older to undergo baseline CAC scanning and high-sensitivity troponin testing. The study will be led by Melissa Daubert, MD at Duke; Michael Blaha, MD, MPH at Johns Hopkins University, and Nicholas Pajewski, PhD at Wake Forest University.
“By directly visualizing atherosclerotic plaque with CAC scanning and measuring subclinical myocardial injury with high-sensitivity troponin, we believe CAC PREVENTABLE is the most promising for informing person-centered care in older adults,” says Melissa Daubert, MD, associate professor of medicine in cardiology at Duke and director of the Multimodality Imaging Core Laboratory at Duke Clinical Research Institute. “CAC PREVENTABLE could fundamentally change the approach to preventive therapy, potentially limiting overtreatment and focusing statin therapy on those most likely to benefit.”
Current guideline-approved risk prediction models are heavily weighted by age, indiscriminately assigning high-risk status and therefore recommending treatment for nearly all older adults even before the age of 75. Accurate person-centered risk prediction at older ages remains unachievable using traditional risk factor models as these approaches do not capture lifetime cumulative exposure or account for individual resiliency to disease. It also raises concerns about overmedication, drug-drug interactions, lack of personalization, and misallocation of limited healthcare resources in an aging population which often requires multiple pharmacotherapies.
Grant funding began on Sept. 1, 2021. The team expects to enroll their first patient in March, 2022.
Congratulations, Melissa – we look forward to hearing more about this as the study progresses!
2022 Incoming Cardiology Fellows Announced
We are pleased to announce the newest members of the Duke Heart team — our incoming cardiology fellows for July, 2022. We are thrilled to have them join us!
Andrew Andreae, MD, joining us after completing residency at Duke; a graduate of Virginia Commonwealth University School of Medicine.
Michael Cosiano, MD, joining us after completing residency at Duke; a graduate of Weill Cornell Medicine.
David Elliott, MD, joining us after completing residency at Duke; a graduate of Duke University School of Medicine.
Nathan Goodwin, MD, joining us after completing residency at Duke; a graduate of the University of Missouri School of Medicine.
Aman Kansal, MD, joining us after completing residency at Duke; a graduate of Duke University School of Medicine.
Allie Levin, MD, joining us after completing residency at Massachusetts General Hospital; a graduate of Columbia University Vagelos College of Physicians and Surgeons.
Anthony Lin, MD, joining us after completing residency at the University of California at San Francisco; a graduate of Duke University School of Medicine.
Paula Rambarat, MD, joining us after completing residency with Massachusetts General Hospital; a graduate of Columbia University Vagelos College of Physicians and Surgeons.
Jessica Regan, MD, joining us after completing residency at Duke; a graduate of Virginia Commonwealth University School of Medicine.
Belal Suleiman, MD, joining us after completing residency at University of Texas Southwestern; a graduate of the University of Kentucky College of Medicine.
Congratulations to all!

Photo Submission: Joey Harrington, Journal Club
Our Journal club met this week — shown here is cardiology fellow Joey Harrington (with Tillie) presenting on the Danish LOOP Study along with Bernie Gersh. Photo courtesy of Christopher Granger.

Shout-out to Corley!
We received a note this week in appreciation of cardiology fellow, Ali Corley:
“Anna Lisa, ICC fellows were out of town, so Dr. Corley covered them at the VA today. She did a fantastic job and delivered several stents in the process. She will do great in her ICC year.” — Tony Gutierrez
Nicely done, Ali!

HF section Gathered for Holiday Cheer at the Mentz House.
The HF Section gathered together for a Holiday Party at Rob Mentz’ house on Friday Night. The group had an enjoyable evening with representation from the fellows, APPs, OHT/VAD coordinator teams, research team, cardiologists and surgeons. It was so nice to be able to get together as a group while enjoying a beautiful evening outdoors. Festive food, drinks and karaoke rounded out the evening. Thank you to the whole group for an amazing year!




Upcoming Events & Opportunities
Cardiology Grand Rounds
December 7: Visiting lecture with Anubha Agarwal of Northwestern Medicine Feinberg School of Medicine. 5 p.m. Webex.
SI4R Training Workshop
December 14: Stepping in 4-Respect (SI4R) Workshop for Duke Division of Cardiology. 5-7 p.m. Zoom (Details in email from Kim Dorman)
As part of the Department of Medicine Civility Champion initiatives, a 2-hr zoom workshop for all faculty, staff, and trainees throughout all DOM divisions has been developed. Civility Champions are trained faculty, fellows, and chief residents who provide informal support in response to incidents of bias, harassment, or other unprofessional behaviors, and to help those affected understand their options for intervention and reporting. People generally come to Civility Champions after the fact, and the Champions debrief their experiences every quarter.
The workshop that Drs. John Duronville, Jane Gagliardi, Anita Kelsey, Camille Frazier-Mills, Daniella Zipkin, Laura Previll, and Sophia Weinmann will be presenting to the Cardiology clinical faculty is entitled Stepping In 4-Respect. It is being offered twice and is a new component of these civility efforts designed to teach faculty the skills needed to step in (be an “upstander”) in the moment, with a particular focus on race-, ethnicity- and gender-based incidents. This workshop is supported by Dr. Kathleen Cooney, Chair of the DOM, and will be provided to each division’s faculty over the coming months.
Please be sure to attend the workshop on Dec. 14 if you missed the one on Nov. 30. Additional details about registration, the structure and goals of the workshop appeared in the email invitation.
Duke Well-Being Ambassador Virtual Course
January 11 – March 15: The Well-being Essentials for Learning Life-Balance (WELL-B) weekly webinar series begins January 11, 2022 at 3 p.m. EST. For only one hour a week for 10 weeks, healthcare workers can learn about the science and practice of well-being from Dr. Bryan Sexton, Dr. Carrie Adair, and Dr. Kyle Rehder. These strategies can enhance your well-being, and through sharing, the well-being of your co-workers. Available to all Duke Health employees and those outside of Duke as well. More information: bit.ly/dukewellb. Offered by the Duke Center for Healthcare Safety and Quality.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion. Note: Pulse will be taking a break for the holidays from Dec. 26 through Jan. 2; we’ll return on Jan. 9, 2022!
Duke Heart in the News:
November 24 — Jacob Schroder
WNCN CBS-17* (Raleigh, NC)
NC family thankful after father’s new generation artificial heart replaced with donor heart at Duke
https://duke.is/9mb9a
*story also carried by Fox-8 Greensboro, Fox-43 Myrtle Beach & NBC-10 Norfolk
November 24 — Tracy Wang
tctMD
Select COVID-19 Patients May Benefit From Postdischarge Anticoagulation
https://duke.is/jsp4y
November 26 — Jacob Schroder
WWAY ABC-3 (Wilmington, NC)
https://duke.is/c3eww
November 30 — Joanna Cavalier
Healio/Cardiology
EHR data reveal ‘red flag’ comorbidities years before cardiac amyloidosis diagnosis
https://duke.is/zubb8
November 30 — William Kraus
AARP
How 11 Minutes of Exercise Can Help You Live Longer
https://duke.is/m5z7z
December 1 — Kevin Thomas
Physician’s Weekly
Recognizing the Experience of Racial Minorities in the Cardiology Workforce
https://duke.is/vwf9t
Duke Heart Pulse 11-28-2021
Chief’s message:
Thanksgiving is a time of reflection and gratitude. We hope of our extended Duke Heart Family and colleagues had some time to spend with family, friends and the loved ones. Most importantly, we hope you all had some time to remember and embrace those that enrich our lives.
Highlights of the week:
Carmat Patient Receives New Human Heart
A surgical team led by Drs. Jacob Schroder and Carmelo Milano, has successfully explanted the Carmat new-generation

total artificial heart that was placed into an end-stage heart failure patient at Duke in July. Matthew Moore of Shallotte, N.C., lived with the device for four months. On Monday, Nov. 22, Moore received a donor heart during transplant surgery at Duke University Hospital.
Carmat’s artificial heart, which is approved for use in Europe, is an implantable prosthetic that includes biological valves derived from bovine tissue. It operates on an external power supply. Duke became the first center in North America to implant the prosthetic device, which is currently being studied at four U.S. locations as a bridge to transplant.
“The use of the Carmat total artificial heart system to successfully bridge a patient to heart transplantation at Duke is a milestone for heart failure patients in the United States,” said Schroder, surgical director of Duke’s heart transplant program. “The device is designed to be significantly more hemocompatible, and should greatly reduce thromboembolic events. This is a major advance from previously available devices.”
 If the device receives FDA approval, it would provide a bridge to transplant for patients whose hearts require assistance to pump blood through both chambers. Current technology – notably a left-ventricular assist device (LVAD) — supports just one chamber.
If the device receives FDA approval, it would provide a bridge to transplant for patients whose hearts require assistance to pump blood through both chambers. Current technology – notably a left-ventricular assist device (LVAD) — supports just one chamber.
“The successful performance of heart transplantation in our patient following initial use of the Carmat total artificial heart system as a temporary support measure is a first in this country,” said Edward P. Chen, MD, chief of the Division of Cardiovascular and Thoracic Surgery in Duke’s Department of Surgery. “This device will ultimately transform care of patients with end stage cardiac disease. We are privileged at Duke to have a team which pursues delivery of the highest-quality patient care and is constantly looking to improve upon this care through innovation.”
Congratulations to Schroder and Jason Katz, co-principal investigators at Duke for the Carmat Total Artificial Heart (TAH) Early Feasibility Study, and to their clinical research team; to Carmelo Milano and our cardiothoracic surgical team; to Sharon McCartney, Sachin Mehta and our cardiac anesthesiology team members; to Adam DeVore and our heart failure team; to our mechanical circulatory support program; our VAD coordinators; the perfusion team, and to the nursing staff of the CTICU and clinical stepdown units.
We are truly blessed with amazing team members across Duke Heart!
Kahsai Receives CVRC’s 2021 Headley Family Award
 Alem Kahsai, PhD, an assistant professor of medicine in the division of cardiology, has received the 2021 Headley Family Award for research within the Duke Cardiovascular Research Center (CVRC). The award to Kahsai, a medicinal and chemical biologist, is for his project ‘Towards understanding the roles of β-arrestins in Alzheimer’s Disease and cardiovascular disorders.’
Alem Kahsai, PhD, an assistant professor of medicine in the division of cardiology, has received the 2021 Headley Family Award for research within the Duke Cardiovascular Research Center (CVRC). The award to Kahsai, a medicinal and chemical biologist, is for his project ‘Towards understanding the roles of β-arrestins in Alzheimer’s Disease and cardiovascular disorders.’
His project aims to understand the similarities between amyloid-β peptide deposits that occur between neurons in the brain (a hallmark event in the development of Alzheimer’s disease) and cardiac amyloid-β peptide deposits in heart and vascular tissues that are the hallmark of many cardiovascular diseases. Cardiac amyloid-β peptide deposits are associated with cardiomyocyte dysfunction, while vascular deposits promote stiffening, inflammation, and atherosclerosis.
There appears to be a positive correlation between increased levels of β-arrestins—key regulators of a class of cell surface receptors called G-protein-coupled receptors—with enhanced γ-secretase activity and the production of amyloid-β peptide in post-mortem brains from Alzheimer’s disease patients compared to healthy controls, Kahsai says. The mechanism by which β-arrestins regulate γ-secretase activity is elusive, and it is this mechanism that he plans to explore.
“Thanks to the Headley award, I can move forward in my research and obtain preliminary data to see the bigger picture,” says Kahsai. “We are trying to devise small molecule drugs that target β-arrestins in the context of Alzheimer’s disease as well as a number of cardiovascular problems, in particular atherosclerosis.”
Funding through the Headley Award will enable Kahsai to reconstitute each component of the γ-secretase- β-arrestin complex outside of the cell and determine how β-arrestins directly regulate γ-secretase activity and thus amyloid-β peptide production within neuronal cells. He hopes the findings from his studies will potentially open a new avenue for therapeutic development through targeting γ-secretase regulating proteins, such as β-arrestins.
He says it is paramount to identify therapeutic targets in order to slow the progression of amyloid-β peptide accumulation in the context of both cardiovascular and neurological disease.
“The CVRC is fortunate to have generous support from donors such as Mr. Headley and his family, who are interested in investing in the basic cardiovascular research that’s so necessary to continue to improve patient treatment and outcomes,” says Maria Price-Rapoza, executive director of the CVRC.
The Headley Family Award was established in 2020 and is made possible through the generosity of Harry and Dorothy Headley in support of basic cardiovascular research at Duke. The award provides annual one-year seed grants of $25,000 (plus indirect costs at 15 percent) targeted toward CVRC researchers who are conducting innovative research into the causes and treatment of hypertension, atherosclerosis and related cardiovascular diseases. The leadership of the Duke CVRC is deeply grateful for the support the Headley’s have provided to our research team.
The award is effective as of Nov. 1. Congratulations, Alem!
Katz Featured in CardioNerds Podcast
CardioNerds has launched a Cardiac Critical Care Series on their podcast and have kicked it off with an episode featuring our own Jason Katz, director of Cardiovascular Critical Care and co-director of Mechanical Circulatory Support and the CICU at Duke. Check it out here: https://apple.co/3HQMJEf.
It’s a good interview and well worth checking out. Great job and congratulations, Jason!

Cardiac Sonography Program Update
Congratulations to Richard Palma, director of the Duke Cardiac Ultrasound Certificate Program, who was recently inducted into the Society of Diagnostic Medical Sonography‘s (SDMS) Board of Directors. The SDMS is the largest association of sonographers and sonography students in the world. Congrats, Richie!

Palma gave three presentations at the SDMS national meeting held Sept. 29-Oct. 2 at the Hyatt Regency in Atlanta. Palma is shown here with two of his former students who were also invited speakers at SDMS. On the left in the photo is Daniel Bourque, MS, ACS, FASE who is the lead cardiac sonographer for Orlando Regional Medical Center; in the center is Palma, and to the right is Laura Phillips, BS, RDCS, RVT, who is with Yale New Haven Hospital and serves as program director for the vascular ultrasound program at the Hoffman Heart Institute of Connecticut.
Hanukkah Wishes
On behalf of the Duke Heart leadership team, we wish all who will be celebrating Hanukkah a peaceful holiday filled with unexpected blessings. It’s up to each of us to be a light in the darkness — even a little light can go a long way.

Upcoming Events & Opportunities
Cardiology Grand Rounds
December 1: The Pathophysiology and Natural History of Perioperative Atrial Fibrillation: Transient Nuisance or Cause for Concern with Bernard Gersh of the Mayo Clinic, Rochester, MN. 5 p.m. Webex.
December 7: Visiting lecture with Anubha Agarwal of Northwestern Medicine.
Training Workshop
November 30 & December 14: Stepping in 4-Respect (SI4R) Workshop for Duke Division of Cardiology. 5-7 p.m. Zoom (Details in email from Kim Dorman)
As part of the Department of Medicine Civility Champion initiatives, a 2-hr zoom workshop for all faculty, staff, and trainees throughout all DOM divisions has been developed. Civility Champions are trained faculty, fellows, and chief residents who provide informal support in response to incidents of bias, harassment, or other unprofessional behaviors, and to help those affected understand their options for intervention and reporting. People generally come to Civility Champions after the fact, and the Champions debrief their experiences every quarter.
The workshop that Drs. John Duronville, Jane Gagliardi, Anita Kelsey, Camille Frazier-Mills, Daniella Zipkin, Laura Previll, and Sophia Weinmann will be presenting to the Cardiology clinical faculty is entitled Stepping In 4-Respect. It is being offered twice and is a new component of these civility efforts designed to teach faculty the skills needed to step in (be an “upstander”) in the moment, with a particular focus on race-, ethnicity- and gender-based incidents. This workshop is supported by Dr. Kathleen Cooney, Chair of the DOM, and will be provided to each division’s faculty over the coming months.
Please be sure to attend the workshop on one of these dates (November 30th or December 14th). Additional details about registration, the structure and goals of the workshop appeared in the email invitation.
Save the Date & Support the Marfan Foundation
February 11: An Evening with Heart to benefit The Marfan Foundation. 7-10 p.m. at The Maxwell in Raleigh, NC. A Valentine’s Day weekend event with silent auction, cocktails, heavy hors d’oeuvres and entertainment. Cocktail attire. Tickets required. For information, visit: https://bit.ly/3cHIBYD.
The Duke Center for Aortic Disease, led by cardiovascular surgeon Chad Hughes, works closely with Marfan patients, their family members and the Marfan Foundation. We are the only location in NC offering access to comprehensive aortic surgical interventions as well as coordinated cardiovascular care and genetic counseling for patients with Marfan syndrome and other connective tissue disorders such as Loeys-Dietz. If you’re interested in learning more about the work being done at Duke or would like to partner or otherwise get involved, please contact Dr. Hughes or Melissa Merrill Burkett, ACNP.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
November 19 — Stephen Greene
Medscape
Fewer Strokes on Myosin Activator in Reduced-EF Heart Failure: GALACTIC-HF
https://duke.is/c4e9x
November 19 — Manesh Patel
U.S. News & World Report
Advances in Care, Impact of COVID Highlights of Latest Cardiologists’ Meeting
https://duke.is/8ezmf
November 20 — Manesh Patel
UPI
Pandemic has made heart healthcare more difficult, doctors say at meeting
https://duke.is/w8bz6
November 23 — Sreekanth Vemulapalli
tctMD
US Aortic Valve Trends in Older Patients Hint at Better Outcomes, Access
https://duke.is/ykbht
Duke Heart Pulse – week ending 11-21-2021
Highlights of the week:
AHA Scientific Sessions & Watch Party 
A big congratulations to all members of our team who showcased the outstanding cardiovascular research and clinical care taking place at Duke during the 2021 AHA Scientific Sessions – in an extraordinarily challenging year, we still had a tremendous showing of speakers, moderators, panelists, discussants and collaborators from across Duke Heart and Duke Clinical Research Institute. Congratulations to Karen Alexander, Renato Lopes, Marat Fudim, Sean Pokorney, Neha Pagidipati, Svati Shah, Adrian Hernandez, Magnus Ohman, Schuyler Jones, L.Kristin Newby, Patricia Cowper, Gerald Bloomfield, Monique Starks, Jennifer Rymer, Stephen Greene, Kevin Thomas, Sana Al-Khatib, Dan Mark, Pamela Douglas, Jonathan Piccini, Adam DeVore, Robert Mentz, Manesh Patel, Michael Felker, Chris Granger, Jim Daubert, Sunil Rao, Vishal Rao, Michelle Kelsey, Josephine Harrington and Vanessa Blumer and to all of our amazing staff members who support their research, time and efforts.
A full listing of all presentations by members of the DCRI, including On-Demand Content can be found here: https://duke.is/2s2f8; media coverage appears in our News Section, below.
A big hat tip to Chris and Bradi Granger for hosting an AHA Watch Party at their lovely home in Bahama last weekend – it was a fun event held in lieu of the annual AHA Duke Reception to celebrate Duke Heart’s presence at the AHA. The Watch Party included some serious and not-so-serious awards, including “Most Likely to Succeed (as next FDA Commissioner)” which went to Rob Califf.
Other superlatives included:
- Best Stats awarded to Hillary Mulder and Karen Pieper of the DCRI
- Best BP Cuff Distribution awarded to Holly Biola of the AHA-Duke-PACE Team
- Best Dissemination Award given to the ICU iPad Patient-Family Communication Study
- The Heart Success Champion “Big Gold Belt” Award, given to the Heart Failure team member involved in research that has led to significant improvement in the care of HF patients, went to Steve Green for his presentation of CHAMP-HF. Green is a collaborator or partner on 14 total presentations or posters and, according to his colleagues, “will hunt you down if you fail to prescribe GDMT.”
- The Rising Star Award, given to a trainee who consistently demonstrates commitment to growth, education and involvement with the AHA, was presented to Vanessa Blumer, a finalist for and winner of the 2021 AHA Laennec Award.
- The Bench to Bedside Award, given to an individual who leads the way in basic science research went to Lauren Truby for her work with Svati Shah and others surrounding proteomic profiling to identify pre-transplant biomarkers of renal failure after heart transplantation which was accepted and presented as a rapid fire oral abstract.
- The Master Collaborator Award was awarded to Marat Fudim for his 13 collaborations across the globe during AHA Scientific Sessions ranging in topics from global health to big data in MIs and stroke care to heart failure disparities. “When in doubt, stop, collaborate and listen.”
- The Best Site-Based Randomized Study was awarded to UNTAP-IT team for improving understanding of patient discomfort and pain during cath.
- The 2nd Best Caipirinhas award was presented to Renato Lopes
- Our newest Heart Center Nurse-APP PIs were recognized: Heather Pena, Dustin Tart, Anna Mall, Kelly Brown, Jules Onorato, Jaime McDermott, Callie Tennyson, Shelley Thompson and Kelly Kester
- Most Synergistic was awarded to Neha Pagidipati
We hope everyone enjoyed the evening! Congrats to each and every one of you.




Blumer Wins AHA Laennec Award at Scientific Sessions
 Vanessa Blumer, MD, was awarded the 2021 Laennec Fellow in Training Clinician Award by the American Heart Association (AHA) Council on Clinical Cardiology during the AHA Scientific Sessions held virtually last weekend. The award recognizes the importance of clinical acumen, inductive analytic skills, and teaching ability in future academic cardiologists; it is a highly competitive award category.
Vanessa Blumer, MD, was awarded the 2021 Laennec Fellow in Training Clinician Award by the American Heart Association (AHA) Council on Clinical Cardiology during the AHA Scientific Sessions held virtually last weekend. The award recognizes the importance of clinical acumen, inductive analytic skills, and teaching ability in future academic cardiologists; it is a highly competitive award category.
Blumer, a third year fellow in our cardiovascular disease fellowship program, presented her abstract, A Challenging Case of Endocarditis — Multi-Disciplinary Approach is an Achievable Chimera during the Laennec FIT Award Competition Session. She is the first finalist from Duke to earn the Laennec award, which has been given since 2010.
“I am extremely honored to have been awarded this year’s AHA Laennec FIT Clinician Award,” said Blumer. “All the finalists did an exceptional job and I learned so much from the experience. Mostly, I am beyond grateful to everyone who helped and supported me.”
Congratulations, Vanessa — this is a tremendous accomplishment and we are so excited for you!

New Cardiology Clinic Space Opens at Arringdon in Morrisville
Our newest cardiology ambulatory space, Duke Cardiology of Arringdon, opened on Monday, Nov. 1. Two Open House events were held in late October in order to showcase the location and orient clinicians and staff to the new space.
Special thanks to Matt Fitzsimmons; Drs. Mike Blazing, Camille Frazier-Mills, Sreekanth Vemulapalli and Anita Kelsey; Annette Moore; Karen Strub; Sarah Moore; Allen Stephens, and Amber Stohl for their exceptional work on planning for the space and helping to executing the move from the Southpoint location. This group led the effort, meeting weekly for more than a year, to ensure that perspectives from all stakeholders within Duke Heart Services were taken into account during the planning phase. In addition, the Division’s staff assistant team led by Mitzi Scarlett and Chris Morgenstern provided additional support with a tremendous volume of appointment rescheduling and helping to ensure our patients were informed.
“This was definitely an all hands on deck operation, said Nick Nguyen, MHA, Duke Heart’s administrator for the Division of Cardiology. “We worked to include multiple viewpoints from across our service line before reaching consensus on operations, layout and design. The team met weekly to consider all aspects of the clinical spaces and operations– working and reworking toward an agreed upon solution.”
Arringdon offers a fresh, bright and spacious location with lots of upgrades, including high-low chairs that convert to exam tables, perimeter work spaces that offer individual sit-stand capability and better ergonomics for the team, as well as ample natural lighting. The clinic, located on the 4th floor, offers a 21 exam room clinic; diagnostic imaging capabilities, including echo, stress tests, and nuclear imaging; and a beautiful, relaxing lobby for patients and their family members that offers both standard and electronic check-in. Everything is larger –including hallways — allowing for easier navigation for patients, especially those who are using mobility aids such as walkers, canes or wheelchairs.
Additional clinical areas at Duke offering services at Arringdon include Duke Eye Center, Obstetrics & Gynecology, Orthopedics and Physical Therapy – making cardiovascular visits even more convenient for our patient population. We anticipate an additional cardiology and EP clinic to open on the 2nd floor of Arringdon in early 2022.
Arringdon Clinic is located at 5601 Arringdon Park Drive, Suite 410 in Morrisville. It is very easy to access off of I-40 (take the Page Road Exit), with free, ample parking and picturesque views of the surrounding area.



WIC Gathering Held
On Thursday evening, Nov. 18, members of our Women in Cardiology (WIC) group were able to gather together for the first time in… far too long. The dinner event, which was hosted by Tracy Wang and sponsored by division chief Manesh Patel, was designed to draw together women from throughout the cardiovascular space at Duke as a means of networking and fostering an important community within Duke Heart.
This will hopefully be one of many such events. Those who joined were able to learn more about each other on a personal and professional level, and to plan future initiatives for Duke WIC. The group recently launched a distribution list to help all WIC members and anyone who is interested in joining the group to stay apprised of future events. If you’d like to be included, please drop a note to: womenincardiology@duke.edu.
The group is grateful to all who took time to help organize and attend the dinner – and they are looking forward to future events as well as welcoming newcomers to the group.
Shown L to R in the group photo are: (Back row) Melissa Daubert, Jenn Rymer, Balim Senman, Manasi Tannu, Karen Flores, Cara Hoke, Ali Corley, Jessica Duran, Pam Douglas, Kelly Arps, Ijeoma Eleazu and Vanessa Blumer. (Front row): Josephine Harrington, Karen Alexander, Tracy Wang, Terry Fortin, Toi Spates, and Kiki Osude. Attendees not shown: our newest cardiology faculty member, Brandy Patterson; heart surgeon, Brittany Zwishenberger and electrophysiologist, Camille Frazier-Mills.



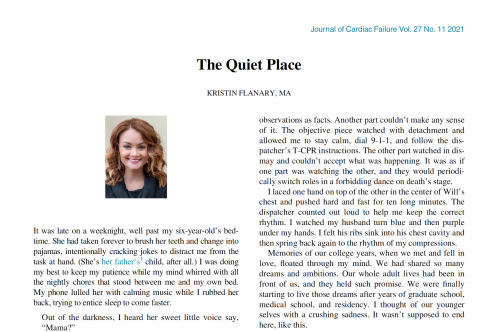
Mentz, Lala Interview Lady & Dr. Glaucomflecken for JCF
Rob Mentz, chief of our Heart Failure Section and Editor-in-Chief, Journal of Cardiac Failure (JCF) recently joined with JCF deputy editor Anu Lala, a cardiologist at Mount Sinai, to interview Kristin and Will Flanary to explore their experience as co-patients/co-survivors in patient care. Will, an ophthalmologist, is a cardiac arrest survivor thanks to Kristin’s use of CPR on him a year ago.
The duo, known in the Twitterverse as “Lady and Dr. Glaucomflecken,” have developed a large and loyal social media fan base. The video is well worth watching. Additionally, Kristin Flanary wrote a special piece for JCF describing their experience with cardiac arrest, the care they received and their overall journey to recovery. The Quiet Place can be accessed here: https://duke.is/gaaqz.
Great job, Rob!

Cardiac MRI Techs Celebrated During Radiologic Technology Week
Duke Heart leadership took time to recognize our cardiac magnetic resonance imaging (CMRI) technologists last week during National Radiologic Technology Week (Nov. 7-13) by thanking each of them for their professional accomplishments, contributions, and the excellent care they provide to patients. National Radiologic Technology Week is celebrated annually to recognize the vital work of imaging professionals across the nation; it takes place each year during the week of November 8th to commemorate the discovery of the x-ray by Wilhelm Conrad Roentgen on November 8, 1895.
Did you know that Duke’s CMRI program was one of the first such dedicated programs in the world? It’s also one of the largest, performing more than 4,000 clinical procedures per year. In fact, their program volume has grown by more than 18 percent in the past year, despite the pandemic.
CMRI technologists start with basic radiologic training but then work to advance their skills and knowledge by becoming specialized in cardiac imaging — gaining a focused understanding of cardiac anatomy, cardiac rhythms, and cardiac disease processes, mastering cardiac terminology, and utilizing MRI technology for all diagnosis and treatment plans.
Duke clinical and research faculty have developed several advances in the field of CMRI, including the development of the Delayed Enhancement technique, which was done with scientists at Siemens. According to the team, this is arguably the single most important advance to propel cardiac magnetic resonance (CMR) into widespread clinical use. Delayed Enhancement CMR detects injury to the heart and, importantly, can differentiate irreversible damage from damage that may recover with appropriate treatment – offering essential guidance for clinical decisions.
We hope that all members of our CMRI team paused to reflect on and celebrate their personal and team successes during Radiologic Technology Week. We thank you for everything you have done and continue to do for cardiovascular patients at Duke Health.
Shown here are members of the CMRI technologist team during one of their recent celebrations. L to R: Jeanne Dement, Stephen Darty, George Gamondea, Vera Kimbrell, Rafael Rojas, Ryan Seward. Not pictured is technologist Nestor Mena. We think you’re awesome – thank you for all you do!

Thanksgiving Wishes to All
Finally, as we close out a busy AHA week and look to the end of the month, we want to wish all of our Pulse readers a very peaceful, safe and happy Thanksgiving holiday. Thank you for all that you have done this year.
We are incredibly grateful for the talented faculty and staff throughout Duke Heart who have showed up 110 percent throughout a rough year. Our fellows have gone above and beyond during the pandemic and with the expansion of our CCU; our APPs have done an incredible job of enhancing continuity of care over the past year, despite the many challenges confronting healthcare. We have so many reasons to feel grateful — your presence, your effort, your collective spirit matters.
Duke Heart is a place unlike any other — thank you for being a part of our team. Please take time to recognize the wonderful people around you this holiday season.
Upcoming Events & Opportunities
Cardiology Grand Rounds
December 1: The Pathophysiology and Natural History of Perioperative Atrial Fibrillation: Transient Nuisance or Cause for Concern with Bernard Gersh of the Mayo Clinic, Rochester, MN. 5 p.m. Webex.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged.
Duke Heart in the News:
November 12 — Manesh Patel
Practical Cardiology
AHA 2021 Scientific Sessions Preview with Manesh Patel, MD
https://duke.is/cze92
November 13 — Manesh Patel
Medscape
Village Health Workers Successfully Treat Hypertension in Rural China
https://duke.is/wsb5y
November 13 — Manesh Patel
tctMD
RAPID CABG: No Penalty to Early Surgery for ACS After Stopping Ticagrelor
https://duke.is/j8pr6
November 13 — Manesh Patel
Healio/Cardiology
‘Feasible’ doctor-led strategy improved blood pressure control in rural China
https://duke.is/8cfwg
November 14 — Sana Al-Khatib
Healio/Cardiology
No increase in atrial arrhythmias, more activity, less sleep with coffee consumption
https://duke.is/ru2e4
November 14 — Geoffrey Ginsburg
WRAL (NBC – Raleigh)
NIH taps Duke researcher for key role
https://duke.is/53atw
November 14 — Sana Al-Khatib
tctMD
Small CRAVE Trial Reassures on Caffeine Safety in Rhythm Disorders
https://duke.is/6ccjn
November 14 — Jonathan Piccini
Healio/Cardiology
No effect of trigger testing on AF-related quality of life, but fewer events
https://duke.is/pre28
November 14 — Sana Al-Khatib
tctMD
Fitbit Joins the AF Hunt, but Effect on Treatment, Outcomes Unknown
https://duke.is/4dfhc
November 14 — Jacob Schroder
The Philadelphia Inquirer
https://duke.is/6pedr
November 14 — Sana Al-Khatib
Medscape
Fitbit Algorithm Successfully Detects AF
https://www.medscape.com/viewarticle/962910#vp_1
November 14 — Sana Al-Khatib
tctMD
Empagliflozin Safe in Acute HF, Improves ‘Clinical Benefit’ Over Time: EMPULSE
https://duke.is/9t5sg
November 14 — Sana Al-Khatib
Medscape
CRAVE: No Spike in Atrial Arrhythmias Among Coffee Drinkers
https://duke.is/2gzpj
November 14 — Jonathan Piccini
Healio/Cardiology
Cognitive outcomes similar at 2 years with dabigatran vs warfarin in older adults with AF
https://duke.is/g52yp
November 14 — Sana Al-Khatib
Medpage Today
Coffee Causes This One Arrhythmia, Trial Shows
https://www.medpagetoday.com/meetingcoverage/aha/95644
November 15 — Tracy Wang
Medscape
Oral Factor XIa Inhibitor Cuts Post-Op VTE Risk: AXIOMATIC-TKR
https://www.medscape.com/viewarticle/963000#vp_1
November 15 — Manesh Patel
Medscape
High-Dose Fish Oil: “Intriguing” Results in COVID-19
https://www.medscape.com/viewarticle/962972
November 15 — Sana Al-Khatib
HealthDay
Your Morning Cup of Coffee Can Affect Your Heart’s Rhythms
https://duke.is/vqbkr
November 16 — Tracy Wang
Physician’s Weekly
AHA: Novel Oral Factor XIa Inhibitor Demonstrates Prevents VTE in Knee Arthroplasty
https://duke.is/7n339
November 16 — Tracy Wang
Medpage Today
Oral Factor XIa Inhibitor Sets the Stage for a Safer Anticoagulant
https://www.medpagetoday.com/meetingcoverage/aha/95710
November 16 — Manesh Patel
Medscape
No Benefit of Antiplatelets in Noncritical COVID: ACTIV-4a
https://www.medscape.com/viewarticle/963093
November 16 — Sana Al-Khatib
Medpage Today
Hospitalized Acute HF Patients See Clinical Benefits With Empagliflozin
https://www.medpagetoday.com/meetingcoverage/aha/95694
November 17 — Sunil Rao
Medscape
Left-Main PCI, CABG Mortality Similar; Choice Remains Complex
https://www.medscape.com/viewarticle/963198
November 19 — Manesh Patel
MSN.com
Advances in Care, Impact of COVID Highlights of Latest Cardiologists’ Meeting
https://duke.is/mjpgc
Duke Heart Center Pulse Week ending 11-14-2021
Chief’s message:
AHA21: This weekend we had the AHA meeting 2021 where we had several of our faculty and fellows presenting. Given the great science and immediate impact on clinical care – we will have updates in the upcoming weeks. Want to personally congratulate and thank all the faculty and fellows presenting at this years scientific sessions.
Highlights of the week:
Thomas named Vice Dean for Diversity, Equity and Inclusion for Duke SOM

Kevin Thomas, MD, associate professor of medicine in cardiology and an electrophysiologist in the Division of Cardiology at Duke, has been named Duke University School of Medicine’s first Vice Dean for Diversity, Equity and Inclusion. Dr. Thomas currently serves as Assistant Dean for Underrepresented Faculty Development for the School of Medicine and as Director of Faculty Diversity and Health Disparities Research for Duke Clinical Research Institute (DCRI).
As Vice Dean for Diversity, Equity and Inclusion, Dr. Thomas will lead the School’s Office of Diversity and Inclusion and will serve as a key advisor and partner to the Dean to advance the School’s goal of cultivating an inclusive, welcoming, respectful and supportive working and learning environment. Dr. Thomas and his team will collaborate with staff, faculty and students across the school to implement the School’s Moments to Movement Strategic Plan to Dismantle Racism and Advance Equity, Diversity and Inclusion and to develop and implement a broad range of policies and programs rooted in equity that foster a greater sense of belonging, engagement, and achievement amongst all members of the School of Medicine and larger Duke Health community.
Dr. Thomas has developed and led a number of programs at Duke that facilitate academic achievement and promotion of Underrepresented Racial and Ethnic Faculty in the School of Medicine, including the School’s Academic Development, Advocacy, Networking Coaching, and Education in Underrepresented Populations (ADVANCE-UP) faculty development program. In 2016, he was the inaugural recipient of the School’s Michelle P. Winn Inclusive Excellence Award, which recognizes individuals who have made significant contributions to diversity and inclusion.
Dr. Thomas received a BS degree from Emory University, his MD from the University of North Carolina at Chapel Hill, and was Chief Resident in Medicine at Duke University in 2003-2004. In 2007, he completed fellowships in cardiology and cardiac electrophysiology at Duke and joined the Duke faculty.
The announcement was made by Mary E. Klotman, MD, Dean of the School of Medicine, on November 8. Dr. Thomas’s service in this role is effective immediately.
Congratulations, Kevin – well deserved!
Perfusion Team Update
 Congratulations to the following members of our Perfusion Team! Andrew (AJ) Jack, CCP, Demetria Middleton, CCP,
Congratulations to the following members of our Perfusion Team! Andrew (AJ) Jack, CCP, Demetria Middleton, CCP,  DeShantra Kelly, CCP, and Heather Keck, CCP have passed both the Perfusion Basic Science Examination (PBSE) and the Clinical Applications in Perfusion Examination (CAPE). They are now designated by the American Board of Cardiovascular Perfusion as Certified Clinical Perfusionists (CCP). We are so proud of them – this accomplishment is the culmination of many years of hard work and sacrifice.
DeShantra Kelly, CCP, and Heather Keck, CCP have passed both the Perfusion Basic Science Examination (PBSE) and the Clinical Applications in Perfusion Examination (CAPE). They are now designated by the American Board of Cardiovascular Perfusion as Certified Clinical Perfusionists (CCP). We are so proud of them – this accomplishment is the culmination of many years of hard work and sacrifice.
Kudos also to the Pediatric Perfusion Team. They have successfully rolled out new state of the art technology in cardiopulmonary bypass this week. New Quantum pediatric heart-lung machines with Viper technology made by Spectrum Medical came online this past week – they are equipped with enhanced digitization, safety monitoring and best practice alerts. Spectrum customized the software with our Duke team to fit our specific needs and goals. This software enables the Duke team to continue to customize and design best practices alerts to optimize the care of our patients.
After many, many months of design, coordination, and simulation the team successfully pumped their first case with these heart lung machines on Wednesday, November 10th — a neonatal arterial switch operation.
Pictured here some of the members of the pediatric perfusion team: Amy Evans, Rachel Gambino, Felicia Shugars, Greg Smigla, and Travis Siffring.
Great work, everyone!!!

Shout-out to Hernandez
A shout-out to Adrian Hernandez who volunteered his entire Sunday last weekend (November 7) to help give COVID vaccines to kids at Durham Academy and throughout the broader Durham community.
Our hat tip comes from Jenn Rymer: “I got my son vaccinated and was so thankful to do so, and saw a lot of other Duke parents getting their kids vaccinated. I really appreciated people like Adrian being there to hopefully get our world back to a normal place!”
Nicely done, Adrian!
ICYMI: Code Blue & Duke’s Chaplain Service
A new peer-reviewed journal article is out in the American Journal of Critical Care: “A Descriptive Study of Chaplains’ Code Blue Responses” (https://doi.org/10.4037/ajcc2021854) by co-authors Callie Tennyson, John Oliver (chaplain services) and Karen Joost (pediatrics, palliative care), all of Duke. Background: Family presence during resuscitation is the compassionate practice of allowing a patient’s family to witness treatment for cardiac or respiratory arrest (code blue event) when appropriate. Offering family presence during resuscitation as an interprofessional practice is consistent with patient- and family-centered care. In many institutions, the role of family facilitator is not formalized and may be performed by various staff members. At the large academic institution of this study, the family facilitator is a member of the chaplain staff.
Congrats, Callie, John and Karen!
Duke Heart Family Halloween Fun
Many thanks to Jamie Jollis for collecting some really adorable photos of our Duke Heart team family members to share with Pulse. We hope everyone had an enjoyable Halloween!



Upcoming Events & Opportunities
Cardiology Grand Rounds
We will not hold Cardiology Grand Rounds this week.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged.
Duke Heart in the News:
November 5 — Edward Chen
tctMD
TAVI Edges Out Surgery in 2-Year Costs for Low-risk Patients: PARTNER 3
https://bit.ly/3qBHWjE
November 5 — Jennifer Rymer
Medpage Today
Surgical Scores Shine for Prognostication in No-Option PCI — Surgeons, Not So Much
https://bit.ly/3c6YyaB
November 8 — Manesh Patel
tctMD
AHA 2021 Tackles AF Triggers, Watchful Waiting in AS, Data Overload, and More
https://bit.ly/3FfpjX1
November 8 — Manesh Patel
Medscape
AHA 2021 Puts Scientific Dialogue, Health Equity Center Stage
https://wb.md/31WtKYm
November 9 — Geoffrey Ginsburg
Triangle Business Journal
Duke professor leaving to join NIH for ‘once in a lifetime opportunity’
https://bit.ly/3wIdxRR
November 9 — Mitchell Krucoff
tctMD
Cardiogenic Shock: SCAI Categories Get a Rethink as Research Rolls On
https://bit.ly/3n9YtJD
November 9 — Jennifer Rymer
MDEdge
At 5 years, iFR found as effective and safe as FFR for guiding PCI intervention
https://bit.ly/30pwtsS
November 10 — Pamela Douglas
Radiology Today
Heart CT Shows Slight Benefit Over Stress Tests
https://bit.ly/3HhxcwR
November 10 — Pamela Douglas
tctMD
Debating ISCHEMIA: Do the Results Apply to CABG, Too?
https://bit.ly/3CfQ3V7
November 12 — Robert Califf
Associate Press*
Biden picks ex-FDA chief Robert Califf to again lead agency
https://bit.ly/3FcAG1W
*story appears in dozens of news outlets across the U.S.
November 12 — Robert Califf
Politico
Biden nominates Califf as FDA chief
https://politi.co/3FizFoK
Division of Cardiology Publications Indexed in PubMed November 4-10, 2021
Berntorp K, Persson J, Koul SM, Patel MR, Christiansen EH, Gudmundsdottir I, Yndigegn T, Omerovic E, Erlinge D, Fröbert O, Götberg M. Instantaneous wave-free ratio compared with fractional flow reserve in PCI: A cost-minimization analysis. Int J Cardiol 2021;344:54-59. PM: 34600977.
Blumenthal JA, Smith PJ, Jiang W, Hinderliter A, Watkins LL, Hoffman BM, Kraus WE, Liao L, Davidson J, Sherwood A. Effect of Exercise, Escitalopram, or Placebo on Anxiety in Patients With Coronary Heart Disease: The Understanding the Benefits of Exercise and Escitalopram in Anxious Patients With Coronary Heart Disease (UNWIND) Randomized Clinical Trial. JAMA Psychiatry 2021;78(11):1270-1278. PM: 34406354.
Chouairi F, Miller PE, Guha A, Clarke JR, Reinhardt SW, Ahmad T, Freeman JV, Desai NR, Friedman DJ. Cannabis use disorder among atrial fibrillation admissions, 2008-2018. Pacing Clin Electrophysiol 2021;44(11):1934-1938. PM: 34506639.
Darden D, Duong T, Du C, Munir MB, Han FT, Reeves R, Saw J, Zeitler EP, Al-Khatib SM, Russo AM, Minges KE, Curtis JP, Freeman JV, Hsu JC. Sex Differences in Procedural Outcomes Among Patients Undergoing Left Atrial Appendage Occlusion: Insights From the NCDR LAAO Registry. JAMA Cardiol 2021;6(11):1275-1284. PM: 34379072.
Dupre ME, Farmer HR, Xu H, Navar AM, Nanna MG, George LK, Peterson ED. The Cumulative Impact of Chronic Stressors on Risks of Myocardial Infarction in US Older Adults. Psychosom Med 2021;83(9):987-994. PM: 34297011.
Feng KY, O’Connor CM, Clare R, Alhanti B, Piña IL, Kraus WE, Whellan DJ, Mentz RJ. Greater Pain Severity Is Associated with Worse Outcomes in Patients with Heart Failure. J Cardiovasc Transl Res 2021;14(5):984-991. PM: 33564986.
Grubb AF, Greene SJ, Fudim M, Dewald T, Mentz RJ. Drugs of Abuse and Heart Failure. J Card Fail 2021;27(11):1260-1275. PM: 34133967.
Hein AM, Scialla JJ, Sun JL, Greene SJ, Shaw LK, Chiswell K, Pun PH, Mentz RJ. Estimated Glomerular Filtration Rate Variability in Patients With Heart Failure and Chronic Kidney Disease. J Card Fail 2021;27(11):1175-1184. PM: 33971291.
Klem I, Cavalier JS. Vasodilator Stress Magnetic Resonance Imaging in Patients With Prior Myocardial Infarction. JACC Cardiovasc Imaging 2021;14(11):2152-2154. PM: 34147445.
Kumar N, Xu H, Garg N, Pandey A, Matsouaka RA, Field ME, Turakhia MP, Piccini JP, Lewis WR, Fonarow GC. Patient characteristics, care patterns, and outcomes of atrial fibrillation associated hospitalizations in patients with chronic kidney disease and end-stage renal disease. Am Heart J 2021;242:45-60. PM: 34216572.
Lala A, Mentz RJ. Following Our Hearts: Prioritizing Self-care and Wellness. J Card Fail 2021;27(11):1163-1164. PM: 34749927.
Naidu SS, Baron SJ, Eng MH, Sathanandam SK, Zidar DA, Feldman DN, Ing FF, Latif F, Lim MJ, Henry TD, Rao SV, Dangas GD, Hermiller JB, Daggubati R, Shah B, Ang L, Aronow HD, Banerjee S, Box LC, Caputo RP, Cohen MG, Coylewright M, Duffy PL, Goldsweig AM, et al. Hot topics in interventional cardiology: Proceedings from the society for cardiovascular angiography and interventions (SCAI) 2021 think tank. Catheter Cardiovasc Interv 2021;98(5):904-913. PM: 34398509.
Nathan SD, Waxman A, Rajagopal S, Case A, Johri S, DuBrock H, De La Zerda DJ, Sahay S, King C, Melendres-Groves L, Smith P, Shen E, Edwards LD, Nelsen A, Tapson VF. Inhaled treprostinil and forced vital capacity in patients with interstitial lung disease and associated pulmonary hypertension: a post-hoc analysis of the INCREASE study. Lancet Respir Med 2021;9(11):1266-1274. PM: 34214475.
Ramacciotti E, Agati LB, Calderaro D, Volpiani GG, de Oliveira CCC, Aguiar VCR, Rodrigues E, Sobreira ML, Joviliano EE, Dusilek C, Itinose K, Dedivitis RA, Cortina AS, Sanches SMV, de Moraes NF, Tierno PFGMM, de Oliveira ALML, Tachibana A, Chate RC, et al. Medically Ill hospitalized Patients for COVID-19 THrombosis Extended ProphyLaxis with rivaroxaban ThErapy: Rationale and Design of the MICHELLE Trial. Am Heart J 2021;242:115-122. PM: 34480880.
Samsky MD, Morrow DA, Proudfoot AG, Hochman JS, Thiele H, Rao SV. Cardiogenic Shock After Acute Myocardial Infarction: A Review. JAMA 2021;326(18):1840-1850. PM: 34751704.
Shi H, Ossip DJ, Mayo NL, Lopez DA, Block RC, Post WS, Bertoni AG, Ding J, Chen S, Yan C, Xie Z, Hoeschele I, Liu Y, Li D. Role of DNA methylation on the association between physical activity and cardiovascular diseases: results from the longitudinal multi-ethnic study of atherosclerosis (MESA) cohort. BMC Genomics 2021;22(1):790. PM: 34732130.
Sofer T, Kurniansyah N, Aguet F, Ardlie K, Durda P, Nickerson DA, Smith JD, Liu Y, Gharib SA, Redline S, Rich SS, Rotter JI, Taylor KD. Benchmarking association analyses of continuous exposures with RNA-seq in observational studies. Brief Bioinform 2021;22(6):bbab194. PM: 34015820.
Sun D, Richard M, Musani SK, Sung YJ, Winkler TW, Schwander K, Chai JF, Guo X, Kilpeläinen TO, Vojinovic D, Aschard H, Bartz TM, Bielak LF, Brown MR, Chitrala K, Hartwig FP, Horimoto ARVR, Liu Y, Manning AK, Noordam R, Smith AV, Harris SE, Kühnel B, et al. Multi-Ancestry Genome-wide Association Study Accounting for Gene-Psychosocial Factor Interactions Identifies Novel Loci for Blood Pressure Traits. HGG Adv 2021;2(1):100013. PM: 34734193.
Taron J, Foldyna B, Mayrhofer T, Osborne MT, Meyersohn N, Bittner DO, Puchner SB, Emami H, Lu MT, Ferencik M, Pagidipati NJ, Douglas PS, Hoffmann U. Risk Stratification With the Use of Coronary Computed Tomographic Angiography in Patients With Nonobstructive Coronary Artery Disease. JACC Cardiovasc Imaging 2021;14(11):2186-2195. PM: 33865792.
Vemulapalli S, Stebbins A, Jones WS, Gutierrez JA, Patel MR, Dolor RJ, Pellikka PA, Alhanti B, Hoffmann U, Douglas PS. Cardiovascular risk and outcomes in symptomatic patients with suspected coronary artery disease and non coronary vascular disease: A report from the PROMISE trial. Am Heart J 2021;242:82-91. PM: 34384742.
Weissler EH, Ford CB, Patel MR, Goodney P, Clark A, Long C, Jones WS. Younger patients with chronic limb threatening ischemia face more frequent amputations. Am Heart J 2021;242:6-14. PM: 34371002.
Westerterp KR, Yamada Y, Sagayama H, Ainslie PN, Andersen LF, Anderson LJ, Arab L, Baddou I, Bedu-Addo K, Blaak EE, Blanc S, Bonomi AG, Bouten CVC, Bovet P, Buchowski MS, Butte NF, Camps SGJA, Close GL, Cooper JA, Das SK, Cooper R, Dugas LR, Ekelund U, et al. Physical activity and fat-free mass during growth and in later life. Am J Clin Nutr 2021;114(5):1583-1589. PM: 34477824.
Duke Heart Week ending November 7th 2021
Highlights of the week:
Ginsburg named Chief Medical & Scientific Officer, NIH All of Us Research Program
 Geoffrey S. Ginsburg, MD, PhD, a professor of medicine in cardiology, a professor in pathology, biostatistics and bioinformatics, a professor of biomedical engineering, and a professor in Duke’s School of Nursing, will leave Duke to assume the role of Chief Medical and Scientific Officer for the National Institutes of Health (NIH) All of Us Research Program, effective January 2022. Dual announcements were made on Nov. 3 by the NIH and Duke School of Medicine.
Geoffrey S. Ginsburg, MD, PhD, a professor of medicine in cardiology, a professor in pathology, biostatistics and bioinformatics, a professor of biomedical engineering, and a professor in Duke’s School of Nursing, will leave Duke to assume the role of Chief Medical and Scientific Officer for the National Institutes of Health (NIH) All of Us Research Program, effective January 2022. Dual announcements were made on Nov. 3 by the NIH and Duke School of Medicine.
In his new role, Ginsburg will have the opportunity to build out the research agenda for All of Us and to engage research scientists across all 27 institutes of the NIH as well as the research community across the U.S. and internationally.
“As I reflect on what I’ve been doing across most of my career both at Millennium Pharmaceuticals in the late 1990s and early 2000s and then at Duke for the last 17 years, this opportunity with All of Us is the capstone for everything I’ve been thinking about,” says Ginsburg. “In the U.S., this platform is second to none in terms of the ability to carry out the research agenda for precision medicine. It encompasses an amazing set of resources that has the potential to really change how we practice medicine, how we do research, and it brings to fruition my particular focus on individualized care, health, and population health.”
Originally announced as the Precision Medicine Initiative cohort program in 2015 by former U.S. President Barack Obama, the name was later changed to the All of Us Research Program, which aims to gather data from at least one million diverse people aged 18 and up who reside in the U.S. as a means of accelerating biomedical research and improving health. The data repository is expected to permit researchers to “take into account individual differences in lifestyle, socioeconomic factors, environment, and biologic characteristics in order to advance precision diagnosis, prevention, and treatment,” according to a 2019 special report in the New England Journal of Medicine.
All of Us is enrolling participants from a network of more than 340 recruitments sites. According to the All of Us research website more than 429,000 participants have joined the program and more than 329,000 have contributed biospecimens to the repository, with more than 80 percent of those participants hailing from groups that have been historically underrepresented in biomedical research. The first 80,000 whole genome sequences will be released by the end of the year.
“A visionary leader in genomics and precision medicine, Dr. Ginsburg has been instrumental in Duke’s work to advance this still emerging field of science, foster important collaborations, and improve human health,” said Mary E. Klotman, MD, Dean, Duke University School of Medicine.
Indeed, Ginsburg has been a transformative leader for Duke University and the School of Medicine for 17 years. He is the founding director of the Center for Applied Genomics & Precision Medicine (CAGPM) and also founding director of MEDx, a partnership between Duke’s Schools of Medicine and Engineering, which is designed to stimulate collaboration and innovation. During his tenure at Duke, Ginsburg has pioneered translational genomics, the development of novel diagnostics, and precision medicine. With a strong commitment to interdisciplinary science and innovation, he has led projects to develop predictive models for common complex diseases using high dimensional genomic data and developed partnerships with engineering colleagues to develop novel point of care sensors.
“Dr. Ginsburg’s achievements at Duke are numerous, and they all center around genetic science and entrepreneurship fueled by innovation and collaboration,” says Kathleen Cooney, MD, chair, Duke Department of Medicine. “Geoff has made an enormous difference here as founder of both the Center for Applied Genomics & Precision Medicine and MEDx. His ability to identify and build partnerships across the Duke enterprise with the Pratt School of Engineering, Duke Heart, and many, many others has been a driving force behind our leadership in precision medicine.”
An internationally recognized expert in genomics and personalized medicine, Ginsburg has authored or co-authored more than 300 peer-reviewed publications. His research has been supported by the NIH, the Department of Defense, National Aeronautics and Space Administration (NASA), the Defense Advanced Research Projects Agency (DARPA), the Gates Foundation, and others. Throughout his career, he has demonstrated a strong commitment to interdisciplinary science and innovation, with work spanning oncology, infectious diseases, cardiovascular disease and metabolic disorders. He is a founding co-chair of the International HundredK+ Cohorts Consortium, and founder and president of the Global Genomic Medicine Collaborative (G2MC), a not-for-profit organization aimed at creating international partnerships to advance the implementation of precision medicine.
Ginsburg has served on a number of advisory councils for the NIH including the National Heart, Lung and Blood Institute’s (NHLBI) Board of External Experts (2007-2016), the National Advisory Council for Human Genome Research (2009-2011), the External Advisory Committee of the Pharmacogenomics Research Network (2010-2013), the National Center to Accelerate Translational Science (NCATS) Advisory Council (2012-2017), the NHLBI External Advisory Board for Precision Medicine Initiative (2015-2016), and most recently on the Advisory Committee to the Director of the NIH (2016-2020), and the Genomic Medicine Working Group for the National Human Genome Research Institute (2011 to present). He has held leadership roles as the Chair of the NIH CTSA Translational Steering Committee and as Vice Chair of the Cures Acceleration Network Advisory Board.
Ginsburg will step down from both of his directorship roles at Duke in late December. He will remain on faculty at Duke as an adjunct professor in the School of Medicine. The Center for Applied Genomics will continue to grow and succeed at Duke thanks to the team Ginsburg has grown over the years. Dr. Cooney will serve as interim center director to ensure a smooth and orderly transition once a new director is named. Dean Klotman, Provost Sally Kornbluth, and Jerome Lynch, who was recently named dean of Duke’s Pratt School of Engineering, will work together to plan the future direction of MEDx.
We are so excited for Geoff and this incredible career opportunity for him at the NIH! He has done an outstanding job at Duke and he will be deeply missed. Please join us in congratulating him on this exciting next step in his accomplished career!
Celebrating Nurse Practitioner Week 2021
It’s Nurse Practitioner (NP) Week, November 7-13. Please join us in helping to celebrate our many nurse  practitioners throughout Duke Heart and Duke Health. They are a vital part of all Duke care teams and an invaluable resource to our patients and their loved ones.
practitioners throughout Duke Heart and Duke Health. They are a vital part of all Duke care teams and an invaluable resource to our patients and their loved ones.
NP Week recognizes the contributions NPs make to the health of patients nationwide. These health care professionals practice in clinics, hospitals, emergency rooms, urgent care centers, nursing homes and private practices across the country — wherever patients are in need. They’ve done an exceptional job in all areas of Duke Heart throughout the COVID-19 pandemic.
Did you know there are more than 325,000 NPs licensed in the U.S.? According to the American Association of Nurse Practitioners, 81 percent of full time NPs see Medicare patients and 78.7 percent see Medicaid patients; 42.5 percent hold hospital privileges. NPs assess patients, order and interpret tests, make diagnoses and provide treatment, including prescribing medications. As clinicians who blend clinical expertise with an added emphasis on disease prevention and health management, NPs are critical members of health care teams across the U.S.
Please join us in thanking and celebrating our Duke Heart Nurse Practitioners!
Positive Top Line Results from U.S. Randomized OCS DCD Heart Trial Announced
TransMedics Group, Inc., announced this week positive topline results from its OCS Donation After Circulatory death (DCD) Heart Trial, which was designed as the first and only randomized trial to compare post-transplant clinical outcomes between hearts transplanted from DCD donors that were resuscitated and assessed on their OCS Heart System and standard criteria donation after brain death (DBD) heart transplants that were preserved using cold storage in the U.S.
The primary goal of the study was to assess the effectiveness and safety of OCS Heart technology to expand the heart donor pool with hearts from DCD donors. Heart transplant candidates were randomized 3:1 into two groups: DCD Heart Possible (DCD) or DBD cold stored hearts (Control). The trial protocol compared the post-transplant outcomes from recipients of DCD hearts preserved on OCS (DCD) to all those who received standard criteria DBD hearts preserved with cold storage (DBD Control).
The OCS DCD Heart trial achieved its primary clinical objectives by meeting the primary
effectiveness endpoint of 6 month patient survival post-transplant which was 95 percent for OCS DCD arm vs. 89 percent for the Control cold storage DBD arm. Even when the outcomes were adjusted for all risk factors between the two groups the results were 94 percent for OCS and 90 percent for Control (non-inferiority p<0.0001), according to the statement released by TransMedics on Nov. 3.
Of 101 DCD donor hearts that were perfused and assessed on OCS Heart technology, 90 were successfully transplanted resulting in a utilization rate of 89 percent. Long-term follow-up is ongoing and the final results are expected to be presented at the International Society for Heart and Lung Transplantion 42nd annual meeting and scientific sessions in April 2022 in Boston.
The OCS Heart System was approved by the U.S. Food and Drug Administration (FDA) for its
DBD heart indication in September 2021. According to TransMedics, the DCD trial results will be submitted shortly to the FDA in a premarket approval supplement to support the approval for the OCS DCD heart indication.

“The OCS DCD Heart Trial provides objective randomized evidence showing high utilization and
excellent short-term clinical outcomes using hearts that historically were never considered for
transplants in the U.S.,” said Jacob Schroder, MD, surgical director of heart transplantation at
Duke University Health System and the principal investigator for the OCS DCD Heart Trial. “The
more widespread use of DCD hearts for transplantation is the biggest thing to happen since the
beginning of heart transplantation.”
Duke was the first U.S. site to enroll a patient into the TransMedics OCS DCD Heart Trial. Schroder led a Duke Heart transplant team in the first DCD heart transplant in the U.S. on Dec. 2, 2019 at Duke University Hospital. Duke was the lead enroller in the trial.
Al-Khatib, Daubert Listed as Top Scholars, Sudden Cardiac Death
Sana Al-Khatib and Jim Daubert, electrophysiologists with Duke Heart, have been listed by Expertscape in

 the top 1 percent of sudden cardiac death experts contributing peer-reviewed journal articles to the scientific literature over the past 10 years. Al-Khatib is ranked as the top contributor, globally.
the top 1 percent of sudden cardiac death experts contributing peer-reviewed journal articles to the scientific literature over the past 10 years. Al-Khatib is ranked as the top contributor, globally.
Expertscape is an online tool geared toward consumers seeking information regarding the most knowledgeable experts in various biomedical research fields. According to their website, Expertscape bases its rankings by mining available scientific publications via online search engines such as PubMed.
Congrats, Sana and Jim!
13th Annual Pulmonary Hypertension Symposium Held
The 13th Annual North Carolina Research Triangle Pulmonary Hypertension Symposium was held on Friday, Nov. 5. Course directors H. James Ford of UNC School of Medicine and Duke Heart’s Terry Fortin pulled together a terrific program for more than 240 attendees. In addition to Fortin, Duke presenters included Kishan Parikh, Sudarshan Rajagopal and Jordan Whitson. The event was held online and presented by Duke Health and UNC School of Medicine.

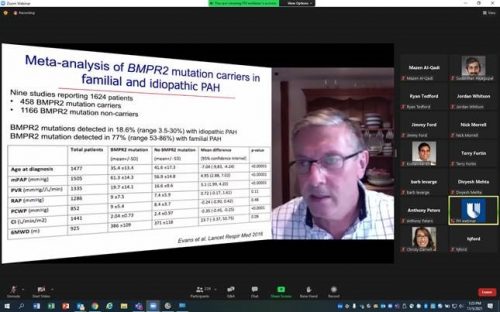
Katz Opens NYU Critical Care Cardiology Symposium
Jason Katz served as a co-course director of the first NYU Langone Critical Care Cardiology Symposium held virtually on Friday, Nov. 5. He kicked off session 1 of the symposium with his presentation, Why Do We Need This Conference? A Journey Through the Evolution of Critical Care Cardiology. The symposium, more than seven years in the making, was a resounding success with more than 850 registrants from over 28 countries. Katz not only helped plan the event, he also served as a moderator for several sessions and pledged to cover costs for any Duke cardiology fellow wishing to attend. Katz’s fellow co-course directors included Carlos L. Alviar, Samuel Bernard, James Horowitz and Eugene Yuriditsky, all of the NYU Grossman School of Medicine, and Christopher Barnett of the University of California, San Francisco.
The NYU Langone Critical Care Cardiology Symposium became the first dedicated Cardiac Critical Care conference to take place in the U.S. Way to go, Jason!
Duke Heart at TCT2021
TCT2021, the Transcatheter Cardiovascular Therapeutics 2021 conference was held Nov. 4-6 as a hybrid event based in Orlando and online. Duke had a strong presence with the following moderators and discussants: Pamela Douglas, Sunil Rao, Jennifer Rymer, Mitch Krucoff, Rob Califf, Sreekanth Vemulapalli, Vishal Rao, Marat Fudim, Christopher Granger and Renato Lopes. Poster presentations included Duke cardiology fellow Zach Wegermann. Jenn Rymer is quoted in several news stories, be sure to check out our News section, below.
BTW, TCT2021 content is on demand and free for one year. Great job, everyone!


Flores Rosario Presents at ACC NC-Chile Case Conference
Karen Flores Rosario, a Duke cardiology 2nd year fellow, was chosen to give an international conference presentation on behalf of the North Carolina chapter of the American College of Cardiology and the Chilean Society of Cardiology and Cardiovascular Surgery (SOCHICAR). The webinar, Clinical Cases from ACC North Carolina and SOCHICAR was held Oct. 25. Flores Rosario presented a brilliant case of lamin cardiomyopathy and did an exceptional job. The discussion was co-moderated by Drs. Adam DeVore and Richard Krasuski.
Well done, Karen!
Upcoming Events & Opportunities
Cardiology Grand Rounds
November 9: Case Conference – Lessons Learned in Peri-Operative LVAD Care with Amanda Coniglio. 5 p.m. Webex.
Request for Nominations: Samuel DuBois Cook Society Awards

The Samuel DuBois Cook Society invites nominations of individuals from every sector of the Duke Community: staff, administrators, and students — undergraduate, graduate or professional.
Founded to be an instrument of social engagement and change, the Cook Society seeks to recognize members of the Duke community who reflect in their work or in their academic pursuits, the objectives to which Dr. Cook dedicated his professional life — social justice, mentoring, the University’s relationship to the black community, and his vision of the “beloved community,” seeking to improve relations among persons of all backgrounds.
Nominations are due November 8, 2021, and winners will be notified in the first week of December.
Awards will be presented during the annual Cook Society Awards Ceremony on February 22, 2022, at the Washington Duke Inn & Golf Club.
In evaluating nominees, the committee seeks members of the Duke community who:
- Actively nurture a sense of community and belonging for Black people.
- Commit to translate the promise and potential of Black people at Duke into fulfillment and actuality
- Foster positive and constructive interpersonal and intergroup relations within both Duke University’s and Durham’s Black communities
- Cultivate positive relations between Black people and other ethnic, racial, and national groups on the basis of an enlightened appreciation and knowledge of our historic interdependence
To learn more/make a nomination please click here.
Request for Nominations: Raymond Gavins Distinguished Faculty Award
The Samuel DuBois Cook Society invites nominations of faculty whose teaching, mentoring, research, publishing, and engagement with faculty, students and staff have helped to improve relations among people of all backgrounds at Duke and beyond.
Nominations are due November 8, 2021, and winners will be notified in the first week of December. Awards will be presented during the annual Cook Society Awards Dinner on February 22, 2022, at the Washington Duke Inn & Golf Club.
In evaluating nominees, the committee seeks faculty who:
- Actively nurture a sense of community and belonging for Black people.
- Commit to translate the promise and potential of Black people at Duke into fulfillment and actuality
- Foster positive and constructive interpersonal and intergroup relations within both Duke University’s and Durham’s Black communities
- Cultivate positive relations between Black people and other ethnic, racial, and national groups on the basis of an enlightened appreciation and knowledge of our historic interdependence
To learn more/make a nomination please click here.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged.
Duke Heart in the News:
October 28 — Duke University Hospital
The Fox Magazine
11 Six Reasons To Relocate To North Carolina: A Useful Guide
https://bit.ly/3nSuXHf
October 29 — Duke University Hospital/Cardiology
Cardiovascular Business
Learning from the best: The world’s top 20 universities for cardiology
https://bit.ly/3BPCDPP
November 1 — Joseph Turek
Science
Skin, nerve transplants from genetically modified pigs could help humans, but organs are a way off
https://bit.ly/3mChFiP
November 2 — Robert Califf and Haider Warraich
STAT
I’ve worked with Robert Califf. He is the leader the FDA needs
https://bit.ly/3CHJHiz
November 4 — Jennifer Rymer
tctMD
Good Early Outcomes With PCI in Complex Patients Unsuited to Surgery: OPTIMUM
https://bit.ly/3D6RHdj
November 4 — Jennifer Rymer
tctMD
OCT Guidance Cuts Stent Use in STEMI Without Plaque Rupture: EROSION III
https://bit.ly/3CVQsNY
Division of Cardiology Publications Indexed in PubMed Oct. 28-Nov. 3, 2021
Breitbart P, Koch A, Schmidt M, Magedanz A, Lindhoff-Last E, Voigtländer T, Schmermund A, Mehta RH, Eggebrecht H. Clinical and cardiac magnetic resonance findings in post-COVID patients referred for suspected myocarditis. Clin Res Cardiol 2021;110(11):1832-1840. PM: 34448040.
Cho SM, Floden D, Wallace K, Hiivala N, Joseph S, Teuteberg J, Rogers JG, Pagani FD, Mokadam N, Tirschwell D, Li S, Starling RC, Mahr C, Uchino K. Long-Term Neurocognitive Outcome in Patients With Continuous Flow Left Ventricular Assist Device. JACC Heart Fail 2021;9(11):839-851. PM: 34509403.
Dorling JL, Belsky DW, Racette SB, Das SK, Ravussin E, Redman LM, Höchsmann C, Huffman KM, Kraus WE, Kobor MS, MacIsaac JL, Lin DTS, Corcoran DL, Martin CK. Association between the FTO rs9939609 single nucleotide polymorphism and dietary adherence during a 2-year caloric restriction intervention: Exploratory analyses from CALERIE™ phase 2. Exp Gerontol 2021;155:111555. PM: 34543722.
Duan KI, Helfrich CD, Rao SV, Neely EL, Sulc CA, Naranjo D, Wong ES. Cost analysis of a coaching intervention to increase use of transradial percutaneous coronary intervention. Implement Sci Commun 2021;2(1):123. PM: 34706775.
Ezekowitz JA, Zheng Y, Cohen-Solal A, Melenovský V, Escobedo J, Butler J, Hernandez AF, Lam CSP, O’Connor CM, Pieske B, Ponikowski P, Voors AA, deFilippi C, Westerhout CM, McMullan C, Roessig L, Armstrong PW. Hemoglobin and Clinical Outcomes in the Vericiguat Global Study in Patients With Heart Failure and Reduced Ejection Fraction (VICTORIA). Circulation 2021;144(18):1489-1499. PM: 34432985.
Friedland A, Hernandez AF, Anstrom KJ, Chen-Lim ML, Cohen LW, Currier JS, Forrest CB, Fraser R, Fraulo E, George A, Handberg E, Jackman J, Koellhoffer J, Lawrence D, Leverty R, McAdams P, McCourt B, Mickley B, Naqvi SH, O’Brien EC, Olson R, Prater C, et al. Design of the Healthcare Worker Exposure Response and Outcomes (HERO) research platform. Contemp Clin Trials 2021;109:106525. PM: 34371163.
Hess CN, Patel MR, Bauersachs RM, Anand SS, Debus ES, Nehler MR, Fanelli F, Yeh RW, Secemsky EA, Beckman JA, Mauri L, Govsyeyev N, Capell WH, Brackin T, Berkowitz SD, Muehlhofer E, Haskell LP, Hiatt WR, Bonaca MP. Safety and Effectiveness of Paclitaxel Drug-Coated Devices in Peripheral Artery Revascularization: Insights From VOYAGER PAD. J Am Coll Cardiol 2021;78(18):1768-1778. PM: 34711335.
Karnam S, Maddala R, Stiber JA, Rao PV. Drebrin, an actin-binding protein, is required for lens morphogenesis and growth. Dev Dyn 2021;250(11):1600-1617. PM: 33896079.
Koontz BF, Levine E, McSherry F, Niedzwiecki D, Sutton L, Dale T, Streicher M, Rushing C, Owen L, Kraus WE, Bennett G, Pollak KI. Increasing physical activity in Cancer Survivors through a Text-messaging Exercise motivation Program (ICanSTEP). Support Care Cancer 2021;29(12):7339-7349. PM: 34050402.
Miller PE, Mullan CW, Chouairi F, Sen S, Clark KA, Reinhardt S, Fuery M, Anwer M, Geirsson A, Formica R, Rogers JG, Desai NR, Ahmad T. Mechanical ventilation at the time of heart transplantation and associations with clinical outcomes. Eur Heart J Acute Cardiovasc Care 2021;10(8):843-851. PM: 34389855.
Noyd DH, Berkman A, Howell C, Power S, Kreissman SG, Landstrom AP, Khouri M, Oeffinger KC, Kibbe WA. Leveraging Clinical Informatics Tools to Extract Cumulative Anthracycline Exposure, Measure Cardiovascular Outcomes, and Assess Guideline Adherence for Children With Cancer. JCO Clin Cancer Inform 2021;5:1062-1075. PM: 34714665.
Ohman EM. The Evolving Post-PCI Antithrombotic Therapies. N Engl J Med 2021;385(18):1712-1714. PM: 34449186.
Oyediran IO, Prattipati S, Sakita FM, Kweka GL, Tarimo TG, Peterson T, Loring Z, Limkakeng AT, Bloomfield GS, Hertz JT. The prevalence, management, and thirty-day outcomes of symptomatic atrial fibrillation in a Tanzanian emergency department. Afr J Emerg Med 2021;11(4):404-409. PM: 34703731.
Shenker RF, Hong JC, Eclov N, Fairchild A, Patel P, Niedzwiecki D, Palta M. Survey of Healthcare Providers Utilization and Perception of Telehealth On-Treatment Visits During COVID-19 Pandemic. Int J Radiat Oncol Biol Phys 2021;111(3S):S112. PM: 34700417.
Duke Heart Pulse week ending 10-31-2021
Albanese Named EVP, COO of DUHS Effective Jan. 17
 Craig Albanese, a seasoned health care executive and distinguished academic pediatric surgeon, has been named executive vice president and chief operating officer of Duke University Health System (DUHS).
Craig Albanese, a seasoned health care executive and distinguished academic pediatric surgeon, has been named executive vice president and chief operating officer of Duke University Health System (DUHS).
Albanese comes to DUHS from New York-Presbyterian Hospital, where he’s currently group senior vice president and chief medical officer of the $9.2 billion, 10-hospital academic health system. He will start his new role at Duke on Jan. 17, 2022.
“Dr. Albanese is a passionate and collaborative executive with deep experience in leading cutting-edge academic health systems such as ours in becoming the best place to work, delivering highest-quality patient care, and helping to advance our other missions, including research, education and community health,” said A. Eugene Washington, MD, chancellor for health affairs and DUHS president and CEO.
“Given his impressive achievements and commitment to our values, I am confident that Duke University Health System will begin a new era of excellence and impact under his leadership,” Washington said.
As executive vice president, Albanese will serve as the senior leader overseeing the timely execution of DUHS goals and strategic priorities. He will work with other clinical enterprise leaders to deliver outstanding outcomes and care across Duke’s network, from the hospital to ambulatory clinics to care in homes and the community. He will also bring new insights to manage the organization’s COVID pandemic response, to support the health system’s faculty and staff and to further advance the clinical enterprise strategic plan.
“I am honored to accept this position and to join the Duke family,” Albanese said. “I look forward to growing Duke’s footprint in the community and building upon the existing quality improvement work that contributes to Duke’s reputation as a world-class health system.”
Albanese succeeds William Fulkerson, MD, who held the executive vice president position since 2010 and announced he would step down at the end of the year.
In his current role at NYP, Albanese is responsible for the chief medical officers and all eight service lines, including oversight for enterprise clinical standardization, network integration and medical affairs. He also oversees quality, safety, and infection prevention and control for the enterprise.
His more than 25 years of health care management experience includes overseeing the redesign of service line strategy at NYP to drive integration and single standards of care across 10 hospitals and two medical schools, Columbia Vagelos College of Physicians and Surgeons and the Weill Cornell Medical College.
He also served as the COO of New York-Presbyterian’s Morgan Stanley Children’s Hospital and the Sloane Hospital for Women, which is located within the Children’s Hospital.
Prior to NYP, Albanese held senior leadership roles at Stanford University and Stanford Health Care. A respected surgeon-scientist and clinical investigator, he co-directed the team that pioneered in-utero fetal surgery.
Albanese received his medical degree from SUNY Health Science Center in Brooklyn and was a resident and chief resident in general surgery at Mount Sinai Medical Center. He completed pediatric general surgery and critical care research fellowships at Children’s Hospital of Pittsburgh. Albanese also holds a Master’s in Business Administration from the Leavey School of Business at Santa Clara University.
“Dr. Albanese is a seasoned health care leader who possesses a collaborative management style and is committed to the same core ideals we value here at Duke,” said Duke University President Vincent E. Price.
Jackson Receives K Award
 Congratulations to Duke electrophysiologist Larry R. Jackson, MD, assistant professor of medicine in cardiology! He has received notification of a K-award from the National Institutes of Health’s National Heart, Lung, and Blood Institute for his project, Shared Decision-Making to Reduce Racial Disparities in Oral Anticoagulation Use in Patients with Non-Valvular Atrial Fibrillation.
Congratulations to Duke electrophysiologist Larry R. Jackson, MD, assistant professor of medicine in cardiology! He has received notification of a K-award from the National Institutes of Health’s National Heart, Lung, and Blood Institute for his project, Shared Decision-Making to Reduce Racial Disparities in Oral Anticoagulation Use in Patients with Non-Valvular Atrial Fibrillation.
Jackson, a faculty member at Duke since 2016, says this award “will allow him finalize the skill set that will lead him toward independence as a physician scientist with a research program focused on addressing racial differences and abnormal heart rhythm care.”
We look forward to sharing more about this important project as it gets underway.
Thanking Respiratory Therapists
Duke Heart’s leadership team took time to recognize our Respiratory Care Team this week during Respiratory Care Week by thanking each of them for their professional accomplishments and contributions over the last year.
“We recognize that the past 18 months has been filled with challenges like we have not seen before and that each of you have stepped up to support our patients, their loves ones and the entire Duke Health team. We have all seen the amazing outcomes and even miracles that have positively impacted patients and families due to the contributions made by each of you. Duke Respiratory Therapists are recognized as the best in the country because of the amazing things that each of you make possible for our patients each and every day (and night). The number of lives you touch is immeasurable as you set the bar for others in your profession.
Please take time to reflect on and celebrate your personal and team successes during the 2021 Respiratory Therapy Week. We thank you for everything you have done and continue to do for Duke Health patients.”
Shown in photo collage are some celebratory shots of our Respiratory Care Team members. We think you’re awesome – thank you for all you do!

Adams Named Nurse Manager for 7700 Effective Nov. 1
The Duke Heart Leadership team is pleased to announce Katherine Adams as the new 7700 Nurse Manager, effective November 1, 2021. Adams has been a Duke Heart Nurse since September 2015 after obtaining her BSN at Liberty University. She has served as a Clinical Team Lead for Cardiology Step-Down since June 2019, including units 7100 and 7700.
Adams has been instrumental in the opening and establishing of 7700 as a new Cardiology Step-Down Unit since it opened in December 2020. She has helped 7700 grow through her mentorship of new team members, leadership of committees and assisting in various champion roles as the staff have developed experience and embraced various leadership roles of their own. We are looking forward to all that she has planned for the future of 7700.
Please join us in congratulating Katherine on her new role!
Shout-Out to Haney
We received a patient compliment on behalf of Jack Haney this week — passed along to us by Lisa Clark Pickett, Chief Medical Officer for Duke University Hospital.
“Jack, While reading comments on our Patient Satisfaction Survey, I found another wonderful compliment about you and your team!
Thank you for giving me such great care. The nurses and staff were amazing! Dr. Haney did a great job!
Thank you so much for your dedication, excellence, and positive spirit!” – Lisa Clark Pickett
Mother and Daughter Receive Organ Transplants at Duke One Month Apart
 Tyra Ingram, 19, of Laurinburg, NC was born with more than one congenital heart defect and needed three major heart surgeries and a pacemaker before she was five years old. She underwent a heart transplant at Duke in 2021, but the family couldn’t relax just yet. Within weeks of Tyra’s transplant, her mother, Teyanna, received a kidney transplant at Duke. Now, months later, mom and daughter are feeling great, going on family vacations again, and looking forward to a healthy future.
Tyra Ingram, 19, of Laurinburg, NC was born with more than one congenital heart defect and needed three major heart surgeries and a pacemaker before she was five years old. She underwent a heart transplant at Duke in 2021, but the family couldn’t relax just yet. Within weeks of Tyra’s transplant, her mother, Teyanna, received a kidney transplant at Duke. Now, months later, mom and daughter are feeling great, going on family vacations again, and looking forward to a healthy future.
A Journey Not for the Faint of Heart
Tyra was born with several heart defects, including congenitally corrected transposition of the great arteries (also called L-transposition of the great arteries, or L-TGA). This rare defect caused two of Tyra’s four heart chambers to be switched, one of which was too small to function properly. By the time she was in kindergarten, Tyra had undergone a series of complex heart surgeries at Duke University Hospital. She had a pulmonary artery band surgery at two months old, a bidirectional Glenn procedure at 14 months old, and a Fontan surgery with a pacemaker placement when she was four. As she grew, Tyra struggled to keep up with other kids.
“I was the worrywart,” Teyanna, now 41, said. “I’d see her trying to run, and I would tell her not to. I’d be like, ‘No, baby. You might need to sit down. You look tired.’”
Kidney Failure Complicates Things
In June 2019, Teyanna was diagnosed with kidney failure due to complications from diabetes. She started dialysis, which required four-hour treatments, three times a week. Within a few months, Teyanna’s doctors suggested she be evaluated for a kidney transplant. She was added to the national waitlist.
Two Organ Transplants Within One Month
Two years later, in February 2021, Tyra started having trouble breathing while she was a student at North Carolina Central University. “I called my grandma. They were like, ‘let’s call the doctor,’” Tyra said.
Michael Carboni, MD, Tyra’s Duke pediatric cardiologist since she was five years old, knew that she needed advanced therapy or a heart transplant. About two weeks after Tyra was put on the transplant waitlist, a heart became available.
“She had a really complicated surgery because of her complex congenital heart disease. But the transplant went really well, and she thrived afterward,” said Duke transplant cardiologist Adam DeVore, MD, MHS, who was part of her care team.
Just a few weeks later, Teyanna got the call that a kidney was available for her and she underwent the transplant. Six weeks later, her kidney transplant surgeon Kadiyala Ravindra, MBBS, was pleased with her progress. “She was really sick prior to her transplant,” he said. “It’s gratifying to see how well she’s done.”
Figuring Out What’s Next
Both Teyanna and Tyra are getting stronger every day. “I can walk a lot more without getting tired,” Tyra said.
“My experience was great. Some of my Duke nurses were the same ones who took care of Tyra, so they remembered me. They would ask how she was doing,” Teyanna said. “It felt like a second home.”
According to Dr. Carboni, Duke has the resources and collaborative expertise to help people like Tyra and Teyanna Ingram. “We can do the same for others like them,” he said.
Upcoming Events & Opportunities
Cardiology Grand Rounds
November 2: Coronary Microvascular Dysfunction with Jessica Duran. 5 p.m. Webex.
November 9: Case Conference – Lessons Learned in Peri-Operative LVAD Care with Amanda Coniglio. 5 p.m. Webex.
Upcoming Duke Heart CME
November 5: 13th Annual NC Research Triangle Pulmonary Hypertension Symposium. Course directors are H. James Ford (UNC) and Terry Fortin. 8:30 a.m. to 4:20 p.m. Morning case-based workshops have been cancelled due to Covid. Afternoon portion will be held via Zoom. For more information and to register, please visit: https://bit.ly/3DrZwuv.
Request for Nominations: Samuel DuBois Cook Society Award
The Samuel DuBois Cook Society invites nominations of individuals from every sector of the Duke Community: staff, administrators, and students — undergraduate, graduate or professional.
Founded to be an instrument of social engagement and change, the Cook Society seeks to recognize members of the Duke community who reflect in their work or in their academic pursuits, the objectives to which Dr. Cook dedicated his professional life — social justice, mentoring, the University’s relationship to the black community, and his vision of the “beloved community,” seeking to improve relations among persons of all backgrounds.
Nominations are due November 8, 2021, and winners will be notified in the first week of December.
Awards will be presented during the annual Cook Society Awards Ceremony on February 22, 2022, at the Washington Duke Inn & Golf Club.
In evaluating nominees, the committee seeks members of the Duke community who:
- Actively nurture a sense of community and belonging for Black people.
- Commit to translate the promise and potential of Black people at Duke into fulfillment and actuality
- Foster positive and constructive interpersonal and intergroup relations within both Duke University’s and Durham’s Black communities
- Cultivate positive relations between Black people and other ethnic, racial, and national groups on the basis of an enlightened appreciation and knowledge of our historic interdependence
To learn more/make a nomination please click here.
Request for Nominations: Raymond Gavins Distinguished Faculty Award
The Samuel DuBois Cook Society invites nominations of faculty whose teaching, mentoring, research, publishing, and engagement with faculty, students and staff have helped to improve relations among people of all backgrounds at Duke and beyond.
Nominations are due November 8, 2021, and winners will be notified in the first week of December. Awards will be presented during the annual Cook Society Awards Dinner on February 22, 2022, at the Washington Duke Inn & Golf Club.
In evaluating nominees, the committee seeks faculty who:
- Actively nurture a sense of community and belonging for Black people.
- Commit to translate the promise and potential of Black people at Duke into fulfillment and actuality
- Foster positive and constructive interpersonal and intergroup relations within both Duke University’s and Durham’s Black communities
- Cultivate positive relations between Black people and other ethnic, racial, and national groups on the basis of an enlightened appreciation and knowledge of our historic interdependence
To learn more/make a nomination please click here.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged.
Duke Heart in the News:
October 18 — Kevin Thomas
Cardiovascular Business
Exploring reports of discrimination, burnout and job satisfaction among US cardiologists
https://duke.is/yzge9
October 18 — Kevin Thomas
tctMD
ACC Survey Reveals Racial/Ethnic Gaps but Also Job Satisfaction
https://duke.is/jwuar
October 18 — Kevin Thomas
Medscape
Survey Spotlights Double-Edged Sword for Minority Cardiologists
https://www.medscape.com/viewarticle/961101
October 20 — Kevin Thomas
HealthDay
Many Minority, Women Cardiologists Face Discrimination
https://duke.is/vmsrp
October 20 — Joseph Turek
Medscape
US Surgeons Successfully Test Pig Kidney Transplant in Human Patient
https://www.medscape.com/viewarticle/961240?src
October 20 — Manesh Patel
Healio/Cardiology
For patients with HFpEF, medical therapy options now abound
https://duke.is/wxumz
October 20 — Kevin Thomas
Cardiovascular News
Ethnic and racial minority cardiologists face professional discrimination and exclusion
https://duke.is/cerq8
October 21 — Kevin Thomas
Becker’s Hospital Review
Discrimination in the cardiology field: 5 survey findings
https://duke.is/b8n9g
October 22 — Robert Califf
Politico
Biden meets with top FDA candidate
https://duke.is/n4wwc
October 25 — Sunil Rao
tctMD
OPTIMIZE: 2-Year DES Data Affirm Need for Meaningful MI Definitions
https://duke.is/zjrvh
October 26 — Adrian Hernandez
Fox13 Memphis
Woman says controversial COVID-19 treatment Ivermectin saved her life
https://duke.is/mhuks
October 26 — Jonathan Piccini
AHA Newsroom
New heart clinical trial to shine light on early atrial fibrillation treatment
https://duke.is/8ag33
October 26 — G. Michael Felker
Cardiology Today
GALACTIC-HF: Omecamtiv mecarbil effective in patients with severe HF
https://duke.is/ccsyt
October 28 — Andrew Almond (Respiratory Therapy)
ABC11/WTVD (Raleigh/Durham)
Raleigh man credits Duke respiratory therapists for saving him from COVID-19
https://duke.is/wvrwn
Division of Cardiology Publications Indexed in PubMed October 14-27, 2021
Ageno W, Lopes RD, Goldin M, Yusen RD, Albers GW, Elliott GC, Halperin JL, Hiatt WR, Maynard G, Steg PG, Weitz JI, Suh E, Lu W, Barnathan ES, Raskob GE, Spyropoulos AC. Rivaroxaban for extended thromboprophylaxis in acutely ill medical patients 75 years of age or older. J Thromb Haemost 2021;19(11):2772-2780. PM: 34314574.
Arps K, Piccini JP, Yapejian R, Leguire R, Smith B, Al-Khatib SM, Bahnson TD, Daubert JP, Hegland DD, Jackson KP, Jackson LR, Lewis RK, Pokorney SD, Sun AY, Thomas KL, Frazier-Mills C. Optimizing mechanically sensed atrial tracking in patients with atrioventricular-synchronous leadless pacemakers: A single-center experience. Heart Rhythm O2 2021;2(5):455-462. PM: 34667960.
Barnett AS, Bahnson TD. Recurrent atrial fibrillation after pulmonary vein isolation: Box it or not? Heart Rhythm O2 2021;2(5):498-499. PM: 34667965.
Bossone E, Cademartiri F, AlSergani H, Chianese S, Mehta R, Capone V, Ruotolo C, Tarrar IH, Frangiosa A, Vriz O, Maffei V, Annunziata R, Galzerano D, Ranieri B, Sepe C, Salzano A, Cocchia R, Majolo M, Russo G, Longo G, Muto M, Fedelini P, Esposito C, et al. Preoperative Assessment and Management of Cardiovascular Risk in Patients Undergoing Non-Cardiac Surgery: Implementing a Systematic Stepwise Approach during the COVID-19 Pandemic Era. J Cardiovasc Dev Dis 2021;8(10):126. PM: 34677195.
Bracamonte-Baran W, Gilotra NA, Won T, Rodriguez KM, Talor MV, Oh BC, Griffin J, Wittstein I, Sharma K, Skinner J, Johns RA, Russell SD, Anders RA, Zhu Q, Halushka MK, Brandacher G, Čiháková D. Endothelial Stromal PD-L1 (Programmed Death Ligand 1) Modulates CD8 T-Cell Infiltration After Heart Transplantation. Circ Heart Fail 2021;14(10):e007982. PM: 34555935.
Careau V, Halsey LG, Pontzer H, Ainslie PN, Andersen LF, Anderson LJ, Arab L, Baddou I, Bedu-Addo K, Blaak EE, Blanc S, Bonomi AG, Bouten CVC, Buchowski MS, Butte NF, Camps SGJA, Close GL, Cooper JA, Das SK, Cooper R, Dugas LR, Eaton SD, Ekelund U, et al. Energy compensation and adiposity in humans. Curr Biol 2021;31(20):4659-4666. PM: 34453886.
Edmonston DL, Matsouaka R, Shah SH, Rajagopal S, Wolf M. Noninvasive Risk Score to Screen for Pulmonary Hypertension With Elevated Pulmonary Vascular Resistance in Diseases of Chronic Volume Overload. Am J Cardiol 2021;159:113-120. PM: 34497006.
Gautam N, Saluja P, Fudim M, Jambhekar K, Pandey T, Al’Aref S. A Late Presentation of COVID-19 Vaccine-Induced Myocarditis. Cureus 2021;13(9):e17890. PM: 34660088.
Gelijns AC, Moskowitz AJ, O’Gara PT, Giustino G, Mack MJ, Mancini DM, Bagiella E, Hung J, Ailawadi G, Leon MB, Acker MA, Alexander JH, Dickert NW, Taddei-Peters WC, Miller MA. Transcatheter mitral valve repair for functional mitral regurgitation: Evaluating the evidence. J Thorac Cardiovasc Surg 2021;162(5):1504-1511. PM: 32359794.
Gutierrez JA, Patel MR. Crossing Peripheral Chronic Total Occlusions: More Tolls and More Questions. J Am Heart Assoc 2021;10(20):e023423. PM: 34612087.
Holder TA, Gutierrez JA, Aday AW. Medical Management of Peripheral Artery Disease. Cardiol Clin 2021;39(4):471-482. PM: 34686260.
Jackson LR, Ugowe F. Epidemiology and Outcomes Associated with PR Prolongation. Card Electrophysiol Clin 2021;13(4):661-669. PM: 34689893.
Kuno T, Claessen B, Cao D, Chandiramani R, Guedeney P, Sorrentino S, Krucoff M, Kozuma K, Ge J, Seth A, Makkar R, Bangalore S, Bhatt DL, Angiolillo DJ, Saito S, Neumann FJ, Hermiller J, Rau V, Ruster K, Wang J, Valgimigli M, Mehran R. Impact of renal function in high bleeding risk patients undergoing percutaneous coronary intervention: a patient-level stratified analysis from four post-approval studies. J Thromb Thrombolysis 2021;52(2):419-428. PM: 33709255.
Lopes RD, Higano CS, Slovin SF, Nelson AJ, Bigelow R, Sørensen PS, Melloni C, Goodman SG, Evans CP, Nilsson J, Bhatt DL, Clarke NW, Olesen TK, Doyle-Olsen BT, Kristensen H, Arney L, Roe MT, Alexander JH. Cardiovascular Safety of Degarelix Versus Leuprolide in Patients With Prostate Cancer: The Primary Results of the PRONOUNCE Randomized Trial. Circulation 2021;144(16):1295-1307. PM: 34459214.
Martinez Campos C, Tsai K, Courtney DG, Bogerd HP, Holley CL, Cullen BR. Mapping of pseudouridine residues on cellular and viral transcripts using a novel antibody-based technique. RNA 2021;27(11):1400-1411. PM: 34376564.
Pani B, Ahn S, Rambarat PK, Vege S, Kahsai AW, Liu A, Valan BN, Staus DP, Costa T, Lefkowitz RJ. Unique Positive Cooperativity Between the -Arrestin-Biased -Blocker Carvedilol and a Small Molecule Positive Allosteric Modulator of the 2-Adrenergic Receptor. Mol Pharmacol 2021;100(5):513-525. PM: 34580163.
Perino AC, Gummidipundi SE, Lee J, Hedlin H, Garcia A, Ferris T, Balasubramanian V, Gardner RM, Cheung L, Hung G, Granger CB, Kowey P, Rumsfeld JS, Russo AM, True Hills M, Talati N, Nag D, Tsay D, Desai S, Desai M, Mahaffey KW, Turakhia MP, Perez MV. Arrhythmias Other Than Atrial Fibrillation in Those With an Irregular Pulse Detected With a Smartwatch: Findings From the Apple Heart Study. Circ Arrhythm Electrophysiol 2021;14(10):e010063. PM: 34565178.
Polcwiartek C, Loewenstein D, Friedman DJ, Johansson KG, Graff C, Sørensen PL, Nielsen RE, Kragholm K, Torp-Pedersen C, Søgaard P, Jensen SE, Jackson KP, Atwater BD. Clinical Heart Failure Among Patients With and Without Severe Mental Illness and the Association With Long-Term Outcomes. Circ Heart Fail 2021;14(10):e008364. PM: 34587762.
Sheikh FH, Ravichandran AK, Goldstein DJ, Agarwal R, Ransom J, Bansal A, Kim G, Cleveland JC, Uriel N, Sheridan BC, Chomsky D, Patel SR, Dirckx N, Franke A, Mehra MR. Impact of Race on Clinical Outcomes After Implantation With a Fully Magnetically Levitated Left Ventricular Assist Device: An Analysis From the MOMENTUM 3 Trial. Circ Heart Fail 2021;14(10):e008360. PM: 34525837.
Siddiqi TJ, Arshad MS, Sreenivasan J, Blumer V, Almani MU, Usman MS, Kolawole JO, Fudim M, Hernandez GA, Khan MS. Readmissions in Patients With Heart Failure and Mental Health Disorders (from a National Database). Am J Cardiol 2021;159:142-143. PM: 34493385.
Siegbahn A, Lindbäck J, Hijazi Z, Åberg M, Alexander JH, Eikelboom JW, Lopes RD, Pol T, Oldgren J, Granger CB, Yusuf S, Wallentin L. Multiplex protein screening of biomarkers associated with major bleeding in patients with atrial fibrillation treated with oral anticoagulation. J Thromb Haemost 2021;19(11):2726-2737. PM: 34390530.
Starks MA, Jackson LR, Hellkamp A, Al-Khatib SM, Mark DB, Thomas KL, Nichol G, Lee KL, Davidson-Ray L, Poole J, Anderson J, Johnson G, Bardy GH. Outcomes for patients with anterior myocardial infarction and prior cardiac arrest in the home automated external defibrillator trial (HAT). Resuscitation 2021;168:75-83. PM: 34500022.
Thomas KL, Mehta LS, Rzeszut AK, Lewis SJ, Duvernoy CS, Douglas PS. Perspectives of Racially and Ethnically Diverse U.S. Cardiologists: Insights From the ACC Professional Life Survey. J Am Coll Cardiol 2021;78(17):1746-1750. PM: 34674820.
Tran AT, Fonarow G\C, Arnold SV, Jones PG, Thomas LE, Hill CL, DeVore AD, Butler J, Albert NM, Spertus JA. Risk Adjustment Model for Preserved Health Status in Patients With Heart Failure and Reduced Ejection Fraction: The CHAMP-HF Registry. Circ Cardiovasc Qual Outcomes 2021;14(10):e008072. PM: 34615366.
Yoon S, Goh H, Fung SM, Tang S, Matchar D, Ginsburg GS, Orlando LA, Ngeow J, Wu RR. Experience and Perceptions of a Family Health History Risk Assessment Tool among Multi-Ethnic Asian Breast Cancer Patients. J Pers Med 2021;11(10):1046. PM: 34683187.
Krantz MJ, Debus SE, Hsia J, Patel MR, Anand SS, Nehler MR, Hess CN, Capell WH, Bracken T, Szarek M, Mátyás L, Krievins DK, Nault P, Stefanov S, Haskell LP, Berkowitz SD, Muehlhofer E, Hiatt WR, Bauersachs RM, Bonaca MP. Low-dose rivaroxaban plus aspirin in older patients with peripheral artery disease undergoing acute limb revascularization: insights from the VOYAGER PAD trial. Eur Heart J 2021 Oct 14;42(39):4040-4048. PM: 34430972.
Duke Heart Week Ending 10-24-2021
Updates from the week:
Passing: Robert W. Anderson, MD, Professor of Surgery
It is with great sadness that we inform you of the passing of Robert W. Anderson, Professor of Surgery and former Chair of the Department of Surgery, on October 19, 2021.
 Dr. Anderson served as chair of Duke Department of Surgery from 1994–2003. An accomplished cardiothoracic surgeon with additional training in business administration, Dr. Anderson successfully led a department that had been seeded as the epitome of traditional surgical education and training, research, and clinical excellence by his predecessor Dr. David C. Sabiston, Jr. Dr. Anderson’s leadership as chair solidified Duke Surgery’s stature as a world-class institution and fortified its continued dedication to a tripartite mission of clinical, educational, and investigational achievement.
Dr. Anderson served as chair of Duke Department of Surgery from 1994–2003. An accomplished cardiothoracic surgeon with additional training in business administration, Dr. Anderson successfully led a department that had been seeded as the epitome of traditional surgical education and training, research, and clinical excellence by his predecessor Dr. David C. Sabiston, Jr. Dr. Anderson’s leadership as chair solidified Duke Surgery’s stature as a world-class institution and fortified its continued dedication to a tripartite mission of clinical, educational, and investigational achievement.
Dr. Anderson’s surgical career spanned more than five decades, beginning with his surgical training at Duke University in 1967. After his residency, Dr. Anderson was appointed as Assistant Professor of Surgery at Duke. A true surgeon–scientist committed to both clinical care and investigative discovery, Dr. Anderson launched his clinical practice while also serving as Director of the CORE Cardiovascular Research Laboratory at Duke University Medical Center until 1977.
“Dr. Anderson was one of my most important mentors and a close friend,” said Peter K. Smith, MD, Mary and Deryl Hart Professor of Surgery in the division of cardiovascular and thoracic surgery at Duke. “I was lucky to meet him on my first day of medical school, and he was instrumental in my decision to become a thoracic surgeon. I worked in his lab during my third year of medical school, forming lasting relationships with him, his family and with his close friend and confidant Walter Wolfe. I cherish all the connections thus made with Bob at the center, and all returned full circle when he returned to become the Chairman of Surgery. To his enormous credit, he was singularly responsible for the critical transition from Dr. Sabiston’s leadership to a more modern, diverse department built to thrive in the 21st century. I do not believe that anyone else could have done a better job, and I will miss his larger than life presence every day.”
Strong leadership was the defining characteristic of Dr. Anderson’s career. He served as Chief of Cardiovascular and Thoracic Surgery at University of Minnesota Hospitals from 1979–1984, and held the same role at Evanston-Northwestern Hospital in Illinois from 1984–1986. He then served a dual-leadership role as Chair of the Department of Surgery at Evanston Hospital from 1986–1994, while concurrently serving as Chief of Cardiothoracic Surgery at Northwestern Memorial Hospital in Chicago from 1990–1994.
Prior to his surgical career, Dr. Anderson served in the military as Captain of the U.S. Army at the 3rd Surgical Hospital in Vietnam, and Director of the Trauma Research Unit at Walter Reed Army Medical Center. He received the Army Commendation Medal and Vietnam Service Medal for his service.
Our thoughts go out to the family and many friends of Dr. Anderson. He will be remembered as a skilled clinician, an accomplished investigator, and a respected leader, mentor, and colleague.
Information about memorial services will be shared as his family makes it available.
Program Partnership between AKU and Duke Receives 1.2 Million in NIH Funding
 A training program designed by researchers at Aga Khan University (AKU) in partnership with researchers at Duke University has been awarded a research training grant of $1.2 million over five years by the National Institutes of Health. The training program is designed to address a critical gap in response to a growing world-wide epidemic of non-communicable diseases (NCDs) such as cardiovascular and cerebrovascular disease. The NIH’s Fogarty International Center will administer the grant.
A training program designed by researchers at Aga Khan University (AKU) in partnership with researchers at Duke University has been awarded a research training grant of $1.2 million over five years by the National Institutes of Health. The training program is designed to address a critical gap in response to a growing world-wide epidemic of non-communicable diseases (NCDs) such as cardiovascular and cerebrovascular disease. The NIH’s Fogarty International Center will administer the grant.
Aga Khan University, located in Karachi, Pakistan, is situated in an area of the world with a pressing need to develop a cohort of trained researchers who can contribute to the understanding of NCD prevalence and risk factors as well as develop and test safe, effective, and low-cost solutions to them.
“This grant brings together research and intellectual expertise from two major institutions across the world with the shared vision of enhancing research capacity to tackle NCDs in Pakistan. This can be achieved as we keep equity and our drive for data at the core of our strategy. I look forward to working with our team at AKU and my long term colleagues at Duke to fulfill the goals of the Aga Khan University – Pakistan Initiative for NCDs program,” said Dr. Zainab Samad, Ibn-e-Sina endowed professor and chair of the Department of Medicine at the AKU, project director and contact principal investigator (PI) of this project. Samad is a cardiologist and adjunct associate professor of medicine in the Duke Division of Cardiology.
vision of enhancing research capacity to tackle NCDs in Pakistan. This can be achieved as we keep equity and our drive for data at the core of our strategy. I look forward to working with our team at AKU and my long term colleagues at Duke to fulfill the goals of the Aga Khan University – Pakistan Initiative for NCDs program,” said Dr. Zainab Samad, Ibn-e-Sina endowed professor and chair of the Department of Medicine at the AKU, project director and contact principal investigator (PI) of this project. Samad is a cardiologist and adjunct associate professor of medicine in the Duke Division of Cardiology.
The epidemic of NCDs presents an extraordinary crisis world-wide. Over three quarters of all NCD related deaths and 82 percent of premature NCD related deaths occur in low-and middle-income countries like Pakistan, where locally relevant and high-quality research data is scarce. According to the World Health Organization, nearly 50 percent of deaths in Pakistan are from NCDs, creating barriers to development goals including poverty reduction, human security, economic stability and health equity. The most prevalent NCDs are cardiovascular diseases, an area the comprehensive, integrated, multi-disciplinary research training program will focus on.
The training program leverages AKU and the AKU Institute for Global Health and Development’s extensive development network platform and infrastructure at its flagship site in Pakistan. The aim is to build sustainable research capacity, and develop a pool of Pakistani experts in cardio-cerebrovascular disease surveillance and implementation science who will provide the vision and leadership necessary to produce high-quality research of relevance to tackle NCDs in Pakistan and other low-and middle-income countries. This is in line with the Fogarty International Center’s mission of supporting and facilitating global health research conducted by U.S. and international investigators, building partnerships between health research institutions in the U.S. and abroad, and training the next generation of scientists to address global health needs.
 “This award is another milestone signaling the incredibly valuable collaboration between our mutual institutions. We are excited to join this effort as meaningful collaborators, researchers, and mentors. I am humbled to have the opportunity to lead collaborators from Duke University to assist Dr. Samad and her team to deliver on this important goal, and anticipate much success that will lead to improved health and lives saved,” said Dr. Gerald S. Bloomfield, associate professor of medicine in cardiology at Duke and associate research professor of global health at the Duke Global Health Institute. Bloomfield will serve as a PI on this project.
“This award is another milestone signaling the incredibly valuable collaboration between our mutual institutions. We are excited to join this effort as meaningful collaborators, researchers, and mentors. I am humbled to have the opportunity to lead collaborators from Duke University to assist Dr. Samad and her team to deliver on this important goal, and anticipate much success that will lead to improved health and lives saved,” said Dr. Gerald S. Bloomfield, associate professor of medicine in cardiology at Duke and associate research professor of global health at the Duke Global Health Institute. Bloomfield will serve as a PI on this project.
A large part of the grant will include research training that leverages digital information technology—with an opportunity to work with AKU’s Clinical and Translational Research Incubator (CITRIC) Health Data Science Center. Additional PIs based at AKU include Drs. Aysha Almas and Ayeesha Kamal.
Congratulations to all those at Duke and AKU involved in this important work!
Shout-Out to Dixson!
We received a terrific note this week regarding Jeff Dixson, a cardiology fellow.
Dear Dr. Crowley,
I am writing to recognize Dr. Jeff Dixson, who volunteered several hours of his time yesterday to teach our first-year medical students basic cardiac ultrasound. The students clearly loved learning from Dr. Dixson, and have been raving about the experience!
Thank you for sharing your gifted educators with our medical students!
Julian
Julian Hertz, MD, MScGH
Assistant Professor of Surgery & Global Health
Course Director, Longitudinal Point-of-care Ultrasound Curriculum
Duke University School of Medicine
Well done, Jeff!!!
Respiratory Care Week 2021: Oct. 24-31
Please join us in thanking and celebrating all respiratory therapists at Duke and elsewhere! Today is the start of Respiratory Care Week 2021. To mark the occasion, the Duke Heart respiratory care team has received a special message from Duke men’s basketball coach, Mike Krzyzewski.

October is Medical Ultrasound Awareness Month
Please join us in celebrating Medical Ultrasound Awareness Month (MUAM) throughout the month of October. MUAM is  held annually to raise awareness of the role diagnostic medical sonographers play in the medical community and to educate the public about medical ultrasound and its many uses in healthcare. We want to celebrate all Medical Sonographers with a special shout-out to our Duke Heart Center vascular and cardiac sonographers. We are grateful for the positive impact our sonography team has on the care of our patients.
held annually to raise awareness of the role diagnostic medical sonographers play in the medical community and to educate the public about medical ultrasound and its many uses in healthcare. We want to celebrate all Medical Sonographers with a special shout-out to our Duke Heart Center vascular and cardiac sonographers. We are grateful for the positive impact our sonography team has on the care of our patients.
Cardiac and vascular sonographers are the eyes of the providers by assessing important cardiovascular findings such as ejection fraction, valvular regurgitation, valvular stenosis, flow limiting lesions, and dangerous thrombus formation. Many diagnoses would fail to be identified without the skills and expertise of cardiovascular sonographers.
The history of cardiovascular sonography runs deep at Duke Health, starting with the first phased array ultrasound development, live 3D scanning, and the most recent developments in high speed ultrasound. This is thanks to many years of collaboration between the Cardiac Diagnostic Unit and Biomedical Engineering program, pioneered by colleagues and friends Joseph Kisslo, MD and Olaf Von Ram, PhD.
A heartfelt thank you to all of the medical sonographers throughout Duke Health!
Upcoming Events & Opportunities
Cardiology Grand Rounds
October 26: Sleep Disordered Breathing and Cardiovascular Disease with Jonathan Piccini, Marat Fudim and Andrew Spector. 5 p.m. Webex.
November 2: Coronary Microvascular Dysfunction with Jessica Duran. 5 p.m. Webex.
November 9: Case Conference – Lessons Learned in Peri-Operative LVAD Care with Amanda Coniglio. 5 p.m. Webex.
Upcoming Duke Heart CME
November 5: 13th Annual NC Research Triangle Pulmonary Hypertension Symposium. Course directors are H. James Ford (UNC) and Terry Fortin. 8:30 a.m. to 4:20 p.m. Morning case-based workshops have been cancelled due to Covid. Afternoon portion will be held via Zoom. For more information and to register, please visit: https://bit.ly/3DrZwuv.
Child Educational Rights Webinar
October 27: Heart Heroes Webinar. The American Heart Association- Southeast invites parents to join a FREE webinar to learn how to be their child’s best advocate in school. This webinar will be a great opportunity for parents to learn when, why & how to get involved in creating the best school environment for their child. Special needs, education plans and meetings at the school are just a few important discoveries parents can make in shaping their child’s learning experiences. Guest speaker: Lorilynn V. Bowie, EdD, Behavior Resource Teacher. Families of children with a congenital heart defect may find the information particularly helpful. Seminar is free, but registration is required: https://bit.ly/3vE1Yug.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged.
Duke Heart in the News:
October 15 — Jonathan Piccini
Medscape
Half-Dose DOACs Cut Bleeding, Thrombus Risk Post-Watchman LAA Closure
https://www.medscape.com/viewarticle/960974
Duke Heart Week ending October 17th 2021
Highlights of the week:
Friede & Nafissi at NCYIF 2021
Kevin Friede and Navid Nafissi presented their work at the 17th Annual Northwestern Cardiovascular Young Investigator’s Forum this weekend in Chicago. Friede presented his abstract, A Gene Expression Signature Reflective of Exposure to Antiplatelet Therapy is Associated with Bleeding. Mentor: Deepak Voora. Nafissi presented his abstract, Integration of Electronic Health Records with Genetics in Monogenic Electrophysiologic Disorders. Mentor: Svati Shah.

Both presentations were well received. Congratulations to Nafissi who was awarded 3rd place in the Basic Science category during the awards ceremony on Saturday evening, Oct. 16.


The event was presented by Northwestern University Feinberg School of Medicine and Creative Educational Concepts, Inc., and supported by an independent educational grant from AstraZeneca.
Nicely done, Kevin and Navid!!!
Latest by Tcheng is Hot Off the Press!

Congratulations to James Tcheng and his co-authors at the University of Nebraska Medical Center and University of Nebraska-Omaha for their newly published article “A Roadmap to a More Useful and Usable Electronic Health Record” in Cardiovascular Digital Health Journal:
Windle JR, Windle TA, Shamavu KY, Nelson QM, Clarke MA, Fruhling AL,Tcheng JE, A Roadmap to a More Useful and Usable Electronic Health Record, Cardiovascular DigitalHealth Journal (2021), doi: https://doi.org/10.1016/j.cvdhj.2021.09.007
Kudos to TRANSFORM-HF Team!
Congratulations to Tracy DeWald, Kim Biever and the entire Duke TRANSFORM-HF team for reaching 200 participants enrolled in the TRANSFORM-HF study. The team was notified this week that the Duke site is the highest enroller in TRANSFORM to date and is, so far, the only site to reach 200 participants. Way to go!!

Daubert Member of Championship Hockey Team
Fun fact: Duke Electrophysiologist James Daubert stays active by playing in a couple of local hockey leagues. He and his teammates in the ‘Summer Over-40 league’ recently won their league championship!
Daubert says his team includes a rather interesting cast of characters — professors, restaurant owners, recording studio owner-managers, business owners and at least one electrophysiologist… He adds that, for a team of players over 40, “the level of sportsmanship is pretty good although good natured competition for sure.”
His team had made it to the final game in the past two seasons, but had lost to their arch rivals, the “green” team both times. This season, however, Daubert’s “blue” team prevailed.
Congratulations, Jim!!!

Upcoming Events & Opportunities
Cardiology Grand Rounds
October 19: New Approaches to the Mitral Valve, with Jeff Gaca. 5 p.m. Webex.
October 20: Special Grand Rounds from Jonathan Lindner on Advanced Imaging and Cardiovascular Drug Development
October 26: Sleep Disordered Breathing and Cardiovascular Disease with Jonathan Piccini, Marat Fudim and Andrew Spector. 5 p.m. Webex.
November 2: Coronary Microvascular Dysfunction with Jessica Duran. 5 p.m. Webex.
Upcoming Duke Heart CME
November 5: 13th Annual NC Research Triangle Pulmonary Hypertension Symposium. Course directors are H. James Ford (UNC) and Terry Fortin. 8:30 a.m. to 4:20 p.m. Morning case-based workshops have been cancelled due to Covid. Afternoon portion will be held via Zoom. For more information and to register, please visit: https://bit.ly/3DrZwuv.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged.
Duke Heart in the News:
October issue– Division of Cardiology
Newsweek
World’s Best Specialized Hospitals 2021
https://www.newsweek.com/worlds-best-specialized-hospitals-2021
October 11 — William Kraus
Physician’s Weekly
Pandemic Intensifies Push for Home-Based Cardiac Care
https://duke.is/p4gs6
October 11 — Jacob Schroder
The Brunswick Beacon
Shallotte heart recipient one step closer to coming home
https://duke.is/cfsc8
October 12 — Mitch Krucoff
tctMD
Conversations in Cardiology: Do You Use Antibiotics in the Cath Lab?
https://duke.is/g3n65
October 13 — G. Michael Felker
tctMD
HF Care Didn’t Suffer as Clinicians Turned to Telehealth in COVID-19
https://duke.is/nyusc
October 13 — G. Michael Felker
HCPLive
Omecamtiv Mecarbil May Reduce Time To Event in Patients with Severe Heart Failure
https://duke.is/b9gdg
October 14 — Robert Califf
CBSNews.com*
Robert Califf is the leading contender for FDA commissioner
https://duke.is/6znt4
*story appears in dozens of news outlets
October 14 — Robert Califf
The Hill*
Biden likely to tap Robert Califf to return as FDA head
https://duke.is/phhxw
October 14 — Robert Califf
WSJ.com
Biden Weighs Nominating Former FDA Commissioner Robert Califf to Lead Agency Again
https://duke.is/r6u8b
October 15 — G. Michael Felker
Medpage Today
Analysis Makes Stronger Case for Omecamtiv Mecarbil in Severe HF
https://duke.is/5cgb7
Division of Cardiology Publications Indexed in PubMed Oct 4-13, 2021
Andonian BJ, Hardy N, Bendelac A, Polys N, Kraus WE. Making Cardiopulmonary Exercise Testing Interpretable for Clinicians. Curr Sports Med Rep 2021;20(10):545-552. PM: 34622820.
Blumenthal JA, Hinderliter AL, Smith PJ, Mabe S, Watkins LL, Craighead L, Ingle K, Tyson C, Lin PH, Kraus WE, Liao L, Sherwood A. Effects of Lifestyle Modification on Patients With Resistant Hypertension: Results of the TRIUMPH Randomized Clinical Trial. Circulation 2021;144(15):1212-1226. PM: 34565172.
Bossard M, Gao P, Boden W, Steg G, Tanguay JF, Joyner C, Granger CB, Kastrati A, Faxon D, Budaj A, Pais P, Di Pasquale G, Valentin V, Flather M, Moccetti T, Yusuf S, Mehta SR. Antiplatelet therapy in patients with myocardial infarction without obstructive coronary artery disease. Heart 2021;107(21):1739-1747. PM: 33504513.
Butala NM, Secemsky E, Kazi DS, Song Y, Strom JB, Faridi KF, Brennan JM, Elmariah S, Shen C, Yeh RW. Applicability of Transcatheter Aortic Valve Replacement Trials to Real-World Clinical Practice: Findings From EXTEND-CoreValve. JACC Cardiovasc Interv 2021;14(19):2112-2123. PM: 34620389.
Camp J, Glaubitz L, Filla T, Kaasch AJ, Fuchs F, Scarborough M, Kim HB, Tilley R, Liao CH, Edgeworth J, Nsutebu E, López-Cortés LE, Morata L, Llewelyn M, Fowler VG, Thwaites G, Seifert H, Kern WV, Kuss O, Rieg S. Impact of Immunosuppressive Agents on Clinical Manifestations and Outcome of Staphylococcus aureus Bloodstream Infection: A Propensity Score-Matched Analysis in 2 Large, Prospectively Evaluated Cohorts. Clin Infect Dis 2021;73(7):1239-1247. PM: 33914861.
Carnicelli AP, Hellkamp AS, Mahaffey KW, Singer DE, Breithardt G, Halperin JL, Hankey GJ, Piccini JP, Becker RC, Nessel CC, Berkowitz SD, Fox KAA, Califf RM, Patel MR. Termination Based on Event Accrual in Per Protocol Versus Intention to Treat in the ROCKET AF Trial. J Am Heart Assoc 2021;10(19):e022485. PM: 34569249.
Chunawala ZS, Fudim M, Arora S, Qamar A, Vaduganathan M, Mentz RJ, Pandey A, Caughey MC. Clinical and Echocardiographic Characteristics of Patients Hospitalized With Acute Versus Chronic Heart Failure With Preserved Ejection Fraction (From the ARIC Study). Am J Cardiol 2021;158:59-65. PM: 34474908.
Curzen N, Nicholas Z, Stuart B, Wilding S, Hill K, Shambrook J, Eminton Z, Ball D, Barrett C, Johnson L, Nuttall J, Fox K, Connolly D, O’Kane P, Hobson A, Chauhan A, Uren N, Mccann G, Berry C, Carter J, Roobottom C, Mamas M, Rajani R, Ford I, Douglas P. Fractional flow reserve derived from computed tomography coronary angiography in the assessment and management of stable chest pain: the FORECAST randomized trial. Eur Heart J 2021;42(37):3844-3852. PM: 34269376.
Debus ES, Nehler MR, Govsyeyev N, Bauersachs RM, Anand SS, Patel MR, Fanelli F, Capell WH, Brackin T, Hinterreiter F, Krievins D, Nault P, Piffaretti G, Svetlikov A, Jaeger N, Hess CN, Sillesen HH, Conte M, Mills J, Muehlhofer E, Haskell LP, Berkowitz SD. Effect of Rivaroxaban and Aspirin in Patients With Peripheral Artery Disease Undergoing Surgical Revascularization: Insights From the VOYAGER PAD Trial. Circulation 2021;144(14):1104-1116. PM: 34380322.
Eisenstein EL, Zozus MN, Terry SF, Davidson-Ray L, Anstrom KJ. Ascertaining Nonfatal Endpoints in Clinical Trials: Central Adjudication Versus Patient Insurance Claims. Ther Innov Regul Sci 2021;55(6):1250-1257. PM: 34228318.
Flumignan RL, Trevisani VF, Lopes RD, Baptista-Silva JC, Flumignan CD, Nakano LC. Ultrasound guidance for arterial (other than femoral) catheterisation in adults. Cochrane Database Syst Rev 2021;10:CD013585. PM: 34637140.
Gardner RS, Capodilupo RC, Ahmed R, Stolen CM, An Q, Averina V, Hernandez AF, Boehmer JP. Multiparameter diagnostic sensor measurements in heart failure patients presenting with SARS-CoV-2 infection. ESC Heart Fail 2021;8(5):4026-4036. PM: 34184428.
Ginsburg G, Penny M, Feero WG, Miller M, Addie S, Beachy SH. The National Academies’ Roundtable on Genomics and Precision Health: Where we have been and where we are heading. Am J Hum Genet 2021;108(10):1817-1822. PM: 34626581.
Greene SJ, Butler J. Investigator-Reported Versus Adjudicated Clinical Events: 2 Versions of the Truth? J Am Coll Cardiol 2021;78(15):1538-1540. PM: 34620411.
Johnson JN, Mandell JG, Christopher A, Olivieri LJ, Loke YH, Campbell MJ, Darty S, Kim HW, Clark DE, Frischhertz BP, Fish FA, Bailey AL, Mikolaj MB, Hughes SG, Oneugbu A, Chung J, Burdowski J, Marfatia R, Bi X, Craft J, Umairi RA, Kindi FA, Williams JL. Society for Cardiovascular Magnetic Resonance 2020 Case of the Week series. J Cardiovasc Magn Reson 2021;23(1):108. PM: 34629101.
Jones RC, Creutzfeldt CJ, Cox CE, Haines KL, Hough CL, Vavilala MS, Williamson T, Hernandez A, Raghunathan K, Bartz R, Fuller M, Krishnamoorthy V. Racial and Ethnic Differences in Health Care Utilization Following Severe Acute Brain Injury in the United States. J Intensive Care Med 2021;36(11):1258-1263. PM: 32912070.
Kim HJ, Snyder LD, Adegunsoye A, Neely ML, Bender S, White ES, Conoscenti CS, Strek ME. Hospitalizations in patients with idiopathic pulmonary fibrosis. Respir Res 2021;22(1):257. PM: 34592998.
Kim HW, Jenista ER, Wendell DC, Azevedo CF, Campbell MJ, Darty SN, Parker MA, Kim RJ. Patients With Acute Myocarditis Following mRNA COVID-19 Vaccination. JAMA Cardiol 2021;6(10):1196-1201. PM: 34185046.
Levy KD, Blake K, Fletcher-Hoppe C, Franciosi J, Goto D, Hicks JK, Holmes AM, Kanuri SH, Madden EB, Musty MD, Orlando L, Pratt VM, Ramos M, Wu R, Ginsburg GS. Correction: Opportunities to implement a sustainable genomic medicine program: lessons learned from the IGNITE Network. Genet Med 2021;23(10):2020. PM: 33288881.
Lopes RD, de Barros E Silva PGM, Furtado RHM, Alexander JH, Berwanger O. Age-adjusted D-dimer cutoffs to guide anticoagulation in COVID-19 – Authors’ reply. Lancet 2021;398(10308):1304. PM: 34627488.
Mentz RJ, Whellan DJ, Reeves GR, Pastva AM, Duncan P, Upadhya B, Nelson MB, Chen H, Reed SD, Rosenberg PB, Bertoni AG, O’Connor CM, Kitzman DW. Rehabilitation Intervention in Older Patients With Acute Heart Failure With Preserved Versus Reduced Ejection Fraction. JACC Heart Fail 2021;9(10):747-757. PM: 34246602.
Mirza KK, Szymanski MK, Schmidt T, de Jonge N, Brahmbhatt DH, Billia F, Hsu S, MacGowan GA, Jakovljevic DG, Agostoni P, Trombara F, Jorde U, Rochlani Y, Vandersmissen K, Reiss N, Russell SD, Meyns B, Gustafsson F. Prognostic Value of Peak Oxygen Uptake in Patients Supported With Left Ventricular Assist Devices (PRO-VAD). JACC Heart Fail 2021;9(10):758-767. PM: 34391745.
O’Neill BP, Grines C, Moses JW, Ohman EM, Lansky A, Popma J, Kapur NK, Schreiber T, Mannino S, O’Neill WW, Medjamia AM, Mahmud E. Outcomes of bailout percutaneous ventricular assist device versus prophylactic strategy in patients undergoing nonemergent percutaneous coronary intervention. Catheter Cardiovasc Interv 2021;98(4):E501-E512. PM: 34051033.
Oyama K, Giugliano RP, Blazing MA, Park JG, Tershakovec AM, Sabatine MS, Cannon CP, Braunwald E. Baseline Low-Density Lipoprotein Cholesterol and Clinical Outcomes of Combining Ezetimibe With Statin Therapy in IMPROVE-IT. J Am Coll Cardiol 2021;78(15):1499-1507. PM: 34620406.
Piccini JP, El-Chami M, Wherry K, Crossley GH, Kowal RC, Stromberg K, Longacre C, Hinnenthal J, Bockstedt L. Contemporaneous Comparison of Outcomes Among Patients Implanted With a Leadless vs Transvenous Single-Chamber Ventricular Pacemaker. JAMA Cardiol 2021;6(10):1187-1195. PM: 34319383.
Povsic TJ, Henry TD, Ohman EM, Pepine CJ, Crystal RG, Rosengart TK, Reinhardt RR, Dittrich HC, Traverse JH, Answini GA, Mokadam NA. Epicardial delivery of XC001 gene therapy for refractory angina coronary treatment (The EXACT Trial): Rationale, design, and clinical considerations. Am Heart J 2021;241:38-49. PM: 34224684.
Sharma A, Januzzi JL, Suchindran S, Coles A, Hoffmann U, Ferencik M, Patel MR, Ginsburg GS, Douglas PS. Utility of High-Sensitivity Troponin Among Stable Patients With Chest Pain Undergoing Stress Imaging (from PROMISE). Am J Cardiol 2021;158:148-149. PM: 34454709.
Sullivan AE, Nanna MG, Wang TY, Bhatt DL, Angiolillo DJ, Mehran R, Banerjee S, Cantrell S, Jones WS, Rymer JA, Washam JB, Rao SV, Ohman EM. Bridging Antiplatelet Therapy After Percutaneous Coronary Intervention: JACC Review Topic of the Week. J Am Coll Cardiol 2021;78(15):1550-1563. PM: 34620413.
Temu TM, Macharia P, Mtui J, Mwangi M, Ngungi PW, Wanjalla C, Bloomfield GS, Farquhar C, Nyanjau L, Gathecha GK, Kibachio J. Obesity and risk for hypertension and diabetes among Kenyan adults: Results from a national survey. Medicine (Baltimore) 2021;100(40):e27484. PM: 34622879.
Wang L, Wang E, Prado Balcazar J, Wu Z, Xiang K, Wang Y, Huang Q, Negrete M, Chen KY, Li W, Fu Y, Dohlman A, Mines R, Zhang L, Kobayashi Y, Chen T, Shi G, Shen JP, Kopetz S, Tata PR, Moreno V, Gersbach C, Crawford G, Hsu D, Huang E, Bu P, Shen X. Chromatin Remodeling of Colorectal Cancer Liver Metastasis is Mediated by an HGF-PU.1-DPP4 Axis. Adv Sci (Weinh) 2021;8(19):e2004673. PM: 34378358.
White PJ, McGarrah RW, Herman MA, Bain JR, Shah SH, Newgard CB. Insulin action, type 2 diabetes, and branched-chain amino acids: A two-way street. Mol Metab 2021;52:101261. PM: 34044180
Recent Comments