Duke Heart Pulse week ending January 30th 2022
Updates of the week:
In Memoriam: Robert H. Jones, MD, Professor Emeritus of Surgery
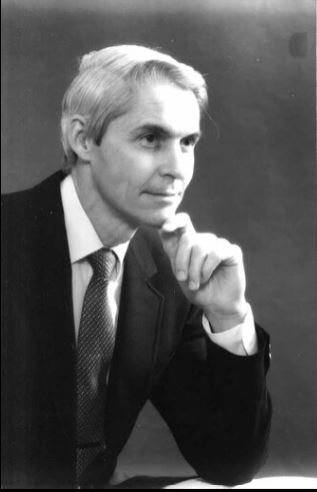 It is with great sadness that we inform you of the passing of Robert “Bob” H. Jones, MD, Professor Emeritus of Surgery, on January 26, 2022. Dr. Jones was the Mary and Deryl Hart Distinguished Professor of Surgery and a prolific cardiothoracic surgeon and clinical investigator until his retirement in 2014. We have lost a treasured member of the Duke community, but his legacy will live on.
It is with great sadness that we inform you of the passing of Robert “Bob” H. Jones, MD, Professor Emeritus of Surgery, on January 26, 2022. Dr. Jones was the Mary and Deryl Hart Distinguished Professor of Surgery and a prolific cardiothoracic surgeon and clinical investigator until his retirement in 2014. We have lost a treasured member of the Duke community, but his legacy will live on.
Dr. Jones received his medical degree from Johns Hopkins University in 1965, and became one of the first Duke University surgical residents taught by Dr. David C. Sabiston, Jr. His residency was interrupted by military service when Dr. Jones served as a Captain in the Air Force. He then completed his residency and joined the Duke Department of Surgery as an Assistant Professor in 1975.
Dr. Jones’ career at Duke spanned 40 years as a cardiac surgeon, clinical investigator, resident educator, and an agent of change in the provision of cardiac care here at Duke and around the world. Beginning as a Howard Hughes Investigator, he made several seminal contributions in the field of lung scanning and nuclear cardiology imaging. His major interest was in the treatment of patients with coronary artery disease, where he was instrumental in the employment of patient data from the Duke Cardiovascular Disease Databank and the Duke Cardiac Research Institute to develop evidence that has guided surgeons and cardiologists through decades of change. From this platform, he obtained NIH funding for the STICH trial, which compared medical therapy to surgical therapy for coronary artery disease. This trial ultimately enrolled over 2,000 patients worldwide, following them for a decade, and publishing outcomes in more than 50 manuscripts to date.
As his academic career flourished, he was selected as the inaugural recipient of the Mary and Deryl Hart Distinguished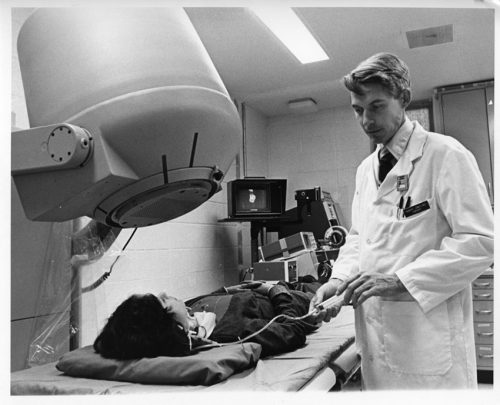 Professorship, created to honor the founder of Duke’s Department of Surgery. As a professor, Dr. Jones was an accomplished surgeon performing thousands of Coronary Artery Bypass operations and training scores of surgical residents. He emphasized the integration of science and clinical decision making within everyday practice.
Professorship, created to honor the founder of Duke’s Department of Surgery. As a professor, Dr. Jones was an accomplished surgeon performing thousands of Coronary Artery Bypass operations and training scores of surgical residents. He emphasized the integration of science and clinical decision making within everyday practice.
Dr. Jones published more than 250 manuscripts that have provided the evidence base used in that everyday practice. His research also focused on harmonizing the roles of surgeons and cardiologists in order to strengthen collaboration between specialties.
Dr. Jones co-founded the Heart Center in 1989 as the first service line within Duke Hospital and promoted joint research and joint clinical practice. This directly led to the concept of Heart Team decision making that is now embodied in all national and international guidelines for the treatment of coronary disease.
Dr. Jones’ legacy is embodied in the thousands of recipients of his generous teaching and mentorship in the clinical, research, and administrative communities. This legacy is best summed up by the inscription on his retirement gift: “Physician, Surgeon, Scholar, Mentor, Leader…and so much more!”
A memorial service will be held at 11:00 am on March 5th at the Cole Mill Road Church of Christ, 1617 Cole Mill Rd, Durham, NC 27705. A full obituary can be found here.
Upon Dr. Jones’ retirement, Duke’s Medical Alumni Association honored him and other retiring faculty at a reception and dinner. The Association produced a video to honor him that evening; it can be viewed here: https://www.youtube.com/watch?v=j6-NK9RUfhA.
We extend our deep condolences to his family, friends, his mentees and former colleagues throughout the world. We know he will be missed.
We wanted to share some thoughts and reminiscences with you:
From Jerry Reves, MD, Dean Emeritus, Distinguished Professor Medical University of South Carolina and former faculty member, Duke Anesthesiology
“Bob was a colleague and good friend. The quality I most admired was his honesty that was always informed by his intelligence and innovation. He had pioneered the surgical component of the Duke Databank and learned very early how the preoperative cardiac catherization data could be used to predict surgical outcome. This was truly innovative, but once in a conversation we were having in relation to various surgeons reporting mortality data after coronary bypass surgery, he said: “I can make my mortality whatever I want.” He had learned by looking at the Duke Databank that if you operated only on patients with very good ventricular function and little coronary disease that the mortality approached zero. However, if you operated on patients with poor ventricular function and a lot of coronary disease the mortality approached 5 percent. So his comment was not boastful, it was an honest, scientifically precise statement that surgical results were almost solely dependent on the preoperative condition of his patient. If a surgeon wanted great results he/she would not operate on sick patients. Bob continued to take all patients and I admired him for that.
 Bob, Tom Bashore and I were asked to design a Heart Center for Duke. This request came from Drs. Greenfield and Sabiston. We visited three places — Mayo Clinic, Texas Heart, and Cleveland Clinic — and studied University of Alabama Birmingham and Emory. The three of us, especially with Bob’s enthusiasm agreed that we could build a unique Heart Center at Duke that featured superb clinical care and innovative research. We designed a heart center that integrated Cardiology, Cardiac Surgery and Cardiac Anesthesia. The model was accepted, and the rest is history. It would not have happened without Bob Jones representing cardiac surgery!
Bob, Tom Bashore and I were asked to design a Heart Center for Duke. This request came from Drs. Greenfield and Sabiston. We visited three places — Mayo Clinic, Texas Heart, and Cleveland Clinic — and studied University of Alabama Birmingham and Emory. The three of us, especially with Bob’s enthusiasm agreed that we could build a unique Heart Center at Duke that featured superb clinical care and innovative research. We designed a heart center that integrated Cardiology, Cardiac Surgery and Cardiac Anesthesia. The model was accepted, and the rest is history. It would not have happened without Bob Jones representing cardiac surgery!
Bob Jones was the “go to” surgeon if you or your patient needed coronary bypass surgery, the most frequently performed operation in the formative days of the Duke Heart Center. He was consistent, competent, and available. In the high stakes, sometimes stressful cardiac surgical operating room, where everyone had to work in a professional, communicative, and collaborative fashion, there was no better team player to be with than Dr. Jones.”
From Tom Bashore, Duke Professor of Medicine in Cardiology:
“My first memory of Bob Jones was when one of my patients commented that they thought he was such a nice man — they were not sure if he was the chaplain or their heart surgeon. With his head of white hair and broad grin of white teeth, Bob put everyone at ease. He was kind, but he was innovative, and he was willing to try novel things in the OR. What many might not know is that in the late 1970s, he was also one of the first people working in nuclear cardiology at Duke. Using a “first-pass” technique, for the first time one could view images of the heart chambers contracting and relaxing as the radionuclide traversed through the heart. The spatial resolution was lousy though, and I remember Bob’s hearty laugh the first time he presented his data where the end-systolic image of the heart came down to a single square red pixel. Rather than being alarmed, Bob was the kind of person that could see the humor in that and was not at all deterred by such stuff. He obviously moved on to other areas as his career took off in other directions. When he, Jerry Reves, and I went around the country visiting Heart Centers (in the hope of forming one here at Duke), he traveled with only a tiny satchel bag and never a suitcase (he bragged about that). Despite that, he always looked the best dressed of all of us, and with his smooth style he was certainly the best looking and best talker among us, no matter what the situation. And that aura about him never changed throughout his whole career. He will always be remembered for not only being an outstanding physician and surgeon but for being a wonderful and warm human being. There have been few like him at Duke, and I daresay in medicine.”
From Carmelo A. Milano, MD, Professor of Surgery and chief, Section of Adult Cardiac Surgery at Duke:
“Dr. Jones developed and ran the influential STICH trial. This was a large international trial that demonstrated the benefits of CABG surgery for patients with reduced heart function and heart failure. The results of this trial changed the way we practice heart surgery today.”
From Peter K. Smith, Mary and Deryl Hart Distinguished Professor of Surgery and former chief, Duke Division of Cardiovascular and Thoracic Surgery:
“Bob Jones influenced me in so many ways. I did a couple of hundred coronary operations with him; I took care of maybe 500-600 patients of his, maybe more. I interacted with him every day, and learned something every day. He essentially took me under his wing in the research area, and made a huge difference in my research capabilities and my ability to get grants. He was a pretty amazing guy and he was driven to contribute. He was very goal-oriented with a very strong desire to bring cardiology and surgery together in a meaningful way, which he was able to do at Duke — which led to a real blossoming of both cardiology and cardiothoracic surgery here as the Duke Heart Center. He was very forward-thinking — not only was the creation of a true ‘Heart Center’ good for Duke, it was good for our patients. This was happening at a time when cardiologists were transitioning from being ‘diagnosticians’ toward cardiologists as ‘treating specialists.’ And that transition period was very interesting because we were pretty co-dependent in the early days. Percutaneous interventions were quite hazardous in the beginning and required close collaboration with surgeons. As percutaneous intervention became much less “risky” it became potentially more competitive, but the evidence-base was poor. So all the decisions really had to be made either individually by cardiologists or individually by surgeons or jointly between the two — and it became much more frequent that we did this jointly at Duke, with due credit to Dr. Jones who recognized where this transition was going to go. It could have been polarizing or it could be harmonizing. He stressed the latter.
Interestingly, his academic career in professional societies was primarily through the American College of Cardiology, and not with a surgical society. He served as chair of their Board of Governors for time and was a trustee for a time as well. With academic surgeons, they’re typically more involved with a surgical society such as AATS, but Bob put his time and commitment toward the ACC which speaks a great deal to his desire for collaboration.”
From Chris O’Connor, MD, President, Inova Heart and Vascular Institute and former division chief, Duke Cardiology:
“As a surgeon, Bob Jones was thought of as ‘the cardiologist’s surgeon’ – he was so collaborative with us. When I was a junior attending in the intensive care unit at Duke we would have these difficult cases that would often get turned down by his surgical colleagues. We would always call him and he would talk with us and talk with the patient – he was very good with patient interactions. He would take on high-risk cases that needed to be done because he understood the evidence from the Duke Databank, and most importantly, he understood the needs of the patient and valued the recommendations of the cardiologists.
As an investigator, he had this unique mindset which was rich in his understanding of quantitative science and data and it just fit the philosophy of the Duke Databank and the DCRI. He was completely committed to the philosophy of quantitative clinical research. He worked closely with Kerry Lee and the biostatisticians at DCRI — he was also a consultant to the New York State Cardiothoracic Surgery database. He was a superb clinical investigator. The capstone of his career was his work with Eric Velazquez on the STICH trial, a 15-year endeavor that really changed the way we think of surgery and the management of heart failure forever. It’s an enduring body of work that will last forever, in my opinion, not just the STICH trial but all the follow-up trials to that. He was so passionate about it — and it would have never been completed if it wasn’t for Bob Jones leading that effort; it was just so hard to do that trial. He dedicated the latter part of his career entirely to that effort.
STICH took an enormous amount of education and awareness, which Bob led globally. He leveraged some deep relationships with his colleagues in Poland, which he had developed over 30-40 years. It was through those relationships in particular, that they were able to complete the trial. Only 25 percent of the patients enrolled were in the United States.
The other thing to know about Bob is, early in his career, he did some very important investigations looking at how nuclear scans can be used to detect heart disease. And for many, many years, people outside of Duke thought he was a nuclear cardiologist, not a surgeon, because of his publications in that area.
Bob was just a prince of a person. He was deeply spiritual and he brought that connectivity to his care of patients and his interactions with people, and I thought he was a terrific professional colleague. He could be hard-headed and firm, but in the end, he really loved his professional colleagues. He loved his family and he really loved his patients. He was an outstanding cardiothoracic surgeon, outstanding clinical investigator, and outstanding person.”
From Manesh Patel, MD, professor of medicine and chief, Division of Cardiology:
As a fellow, faculty member, and clinical researcher at the DCRI, we looked towards Bob Jones as the standard bearer for the cardiothoracic surgical group. He was a clinician who many of us got to interact with for patient care, for clinical research, and most importantly as a mentor for both cardiologists and surgeons. He was kind, consistent and would be direct and firm about how we considered research and patient care, and in the end was a key driving force inmproving the way we cared for patients. In the cardiology world, his work with Eric Velazquez on the STITCH trial will be one of his key legacies in addition to the Duke Heart Center and people that practice here.
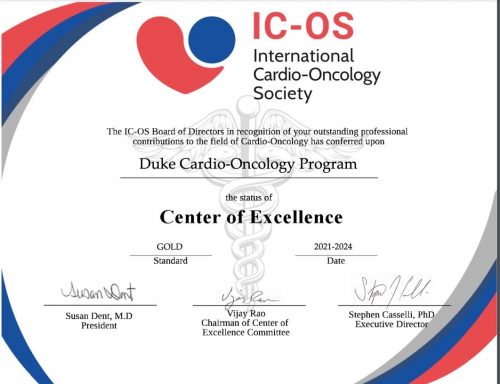
Cardio-Onc Program Named Center of Excellence by ICO Society
We learned this week that our Duke Cardio-Oncology program is among the first to achieve Center of Excellence gold status designation by the International Cardio-Oncology Society. It is one of only nineteen programs world-wide to receive the Center of Excellence rating. In the inaugural effort, 15 programs received gold designation and 4 received silver. To learn more about the ICO Society and the COE rating, please visit: https://ic-os.org/excellence-certification/. The official presentation was made during a virtual event held January 27.
Congratulations to Michel Khouri, Susan Dent and their incredible team!
Shah Named to NC Chapter of ACC

Nishant Shaw, assistant professor of medicine in cardiology has been elected to the Leadership Board of the North Carolina chapter of the American College of Cardiology as a Councilor. He will serve a three-year term starting in March. Councilors to the chapter are responsible for serving as a member of the Nominating Committee; serving as an advocate for his/her region in the areas of education and advocacy; communicating Chapter business to members of his/her region and reporting back to the Chapter, as well as participating in approving the annual Chapter budget.
Shah will serve alongside fellow Councilor Adam DeVore and cardiology fellow Vanessa Blumer, who serves as the ACC FIT Liaison.
Congratulations, Nishant! Well-deserved and certainly this team will represent us well.
Shout-out to Rymer & PWIM Planning Team

Congratulations to Jenn Rymer and the planning team for the Program for Women in Internal Medicine (PWIM). They held a terrific online session this week that featured Pam Douglas, Leslie Curtis and  April Salama discussing how they got their start in medicine and launched superb careers in research. Rymer moderated an engaging and informative discussion. Great job to all!
April Salama discussing how they got their start in medicine and launched superb careers in research. Rymer moderated an engaging and informative discussion. Great job to all!
Byler Named Clinical Lead 3100 Effective March 14th
 We are excited to share that Hannah Byler will be joining the 3100 leadership team as a Clinical Lead effective Monday, March 14, 2022. Hannah began her nursing career on 3100 in March 2019. She earned her Associates in Nursing at Wake Technical Community College in 2018 and her Bachelor of Science in Nursing at University of North Carolina Wilmington in 2021. Hannah holds a variety of roles on 3100 including preceptor, charge nurse, MOVEs champion, Time to Pace class instructor, and has recently advanced to CNIII.
We are excited to share that Hannah Byler will be joining the 3100 leadership team as a Clinical Lead effective Monday, March 14, 2022. Hannah began her nursing career on 3100 in March 2019. She earned her Associates in Nursing at Wake Technical Community College in 2018 and her Bachelor of Science in Nursing at University of North Carolina Wilmington in 2021. Hannah holds a variety of roles on 3100 including preceptor, charge nurse, MOVEs champion, Time to Pace class instructor, and has recently advanced to CNIII.
Congratulations, Hannah!
CVRC Post-Holiday Morale Booster!
The Duke Cardiovascular Research Center team was able to help celebrate their team members last week with a post-holiday pick-me-up.
Their leadership team ordered team hats and distributed almost a hundred in total. CVRC faculty and staff could pick between the  baseball cap style worn by Cheryl Woodard and Maria Price Rapoza or and the beanie ski hat style worn by Howard Rockman. The hats were originally intended as a holiday gift for CVRC faculty and staff, but due to pandemic-related manufacturing issues they weren’t ready in time for the holidays, so the team used them to liven up the last Wednesday in January instead (a day when everyone needed a bit of cheer and a morale boost!).
baseball cap style worn by Cheryl Woodard and Maria Price Rapoza or and the beanie ski hat style worn by Howard Rockman. The hats were originally intended as a holiday gift for CVRC faculty and staff, but due to pandemic-related manufacturing issues they weren’t ready in time for the holidays, so the team used them to liven up the last Wednesday in January instead (a day when everyone needed a bit of cheer and a morale boost!).
Great idea and perfect timing with the recent cold weather!

Shout-out to CDU Team
Congratulations to the Cardiac Diagnostic Unit for completing a successful Intersocietal Accreditation Commission audit for Adult Echo, Adult Stress Echo, and Adult Transesophageal Echo! Thank you to everyone who worked through the process, and thanks to the entire team for maintaining the Duke Standards even during the accreditation “off season”. We are so proud of the work you do for our cardiac patients every day!
Great job, everyone!
It’s Duke Research Week 2022
January 31 – February 4: Duke Research Week 2022. Join us virtually for a week-long celebration of research underway at Duke! There is an excellent lineup of faculty lectures, panel discussions, “flash talks” with graduate students, trainees and postdoctoral fellows, and guest presenters for the Robert J. Lefkowitz, MD, Distinguished Lecture and Daubechies Lecture.
Check out the full agenda here: https://dukeresearchweek.vfairs.com/en/#distinguishedlectures
Duke Heart Family Grows Again!
Congratulations to newly minted grandfather, Richie Palma! His family welcomed twin boys two weeks ago. Owen Scott Horvath and Finn Lucas Horvath were born to Richie’s daughter Chloe and her husband Andrew. The family lives in Lafayette, CA. Richie reports that everyone is healthy and doing great!


National Wear Red Day
Friday, Feb. 4: National Wear Red Day. Help increase awareness of the impact cardiovascular disease has on all of us — wear red on Friday, Feb. 4! Please consider taking photos of your teams and sending them to us so that we can share them in Pulse throughout the month of February.
ICYMI: STAT First Opinion Piece By Galanos, et al.
Our Duke Palliative Care colleague, Tony Galanos, has co-authored an opinion piece that ran this week in STAT (Jan. 24, 2022). His co-authors are faculty members at UCSF. We think it’s worth a read: We all need help working through grief and hardship.
COVID-19 Updates
All the latest Clinical Operations updates related to COVID can be found at https://covid-19.dukehealth.org.
Duke Health’s Adopt-A-Unit is a matchmaking program that enables teams to actively support units continuing to fight on the frontlines of COVID through efforts such as meals, expressions of gratitude or other well-being support. If you are a leader interested in adopting a unit, please complete this smartsheet form. Once your information is received, a program member will be in touch to connect you with a unit in need that fits your budget and timeline. If you’d like to donate to our Healthcare Worker Unit Support fund, click here for details. Questions? Contact caring@duke.edu.
Reminder: All Duke University Health System (DUHS) and Private Diagnostic Clinic (PDC) team members, regardless of work location, are required to receive and provide documentation of a completed COVID-19 booster vaccination by 10 a.m. on Tuesday, Feb. 15, 2022, or within 28 days of their eligibility under CDC and state guidelines. More details are available in this email that was sent to all staff on Tuesday, Dec. 28.
Upcoming Events & Opportunities
Cardiology Grand Rounds
February 1: No CGR today.
February 8: No CGR today.
February 10: Topic TBA. Our guest will be AAMC President, Dr. David Skorton.
February 15: Topic TBA. Presenter will be Toi Spates.
Upcoming Duke Heart CME
April 23: Duke Sports Cardiology & Sudden Death in Athletes Symposium with course directors Jim Daubert and Bill Kraus. Virtual. For information or to register, contact Christy Darnell christy.darnell@duke.edu or 919-880-8686.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
January 21 — Adrian Hernandez
WebMD
Ivermectin as Potential COVID-19 Treatment Gets Studied at Duke University
https://duke.is/4rj8r
January 24 — Adrian Hernandez
Lakeland Ledger (FL)
Lakeland Regional joins national study to see if ivermectin is effective against COVID-19
https://duke.is/98db9
January 24 — Adrian Hernandez
Medscape
Ivermectin as Potential COVID-19 Treatment Gets Studied at Duke University
https://duke.is/jfanc
January 25 — G. Chad Hughes
Endovascular Today
STS and AATS Publish New Practice Guideline for Type B Aortic Dissection
https://duke.is/gn86g
January 25 — G. Chad Hughes
Vascular Specialist
https://duke.is/v99z8
January 25 — Andrew Wang
tctMD
Differing Advice for Infective Endocarditis Surgery Stems From Evidence Gaps
https://duke.is/z767z
January 25 — G. Chad Hughes
Cardiovascular Business
A fresh look at managing patients with type B aortic dissection
https://duke.is/nja47
January 26 — Derek Chew and Duke Clinical Research Institute
tctMD
CABG Provides ‘Good Value’ in Ischemic Cardiomyopathy
https://duke.is/b48ru
Duke Heart Pulse week ending January 23rd 2022
Highlights of the week:
Duke Health Welcomes Craig Albanese as Executive VP & COO
 Please join us in welcoming Craig Albanese, MD, MBA, to Duke University Health System! In October, Duke Health named Albanese, a seasoned health care executive and distinguished academic pediatric surgeon, as our next executive vice president and chief operating officer. He succeeds William Fulkerson, MD, who held the executive vice president position since 2010. Fulkerson stepped down from the role at the end of the 2021. Albanese began his new role on Monday, Jan. 17.
Please join us in welcoming Craig Albanese, MD, MBA, to Duke University Health System! In October, Duke Health named Albanese, a seasoned health care executive and distinguished academic pediatric surgeon, as our next executive vice president and chief operating officer. He succeeds William Fulkerson, MD, who held the executive vice president position since 2010. Fulkerson stepped down from the role at the end of the 2021. Albanese began his new role on Monday, Jan. 17.
As executive vice president, Albanese will serve as the senior leader overseeing the timely execution of DUHS goals and strategic priorities. He will work with other clinical enterprise leaders to deliver outstanding outcomes and care across Duke’s network, from the hospital to ambulatory clinics to care in homes and the community. He will also bring new insights to manage the organization’s COVID pandemic response, to support the health system’s faculty and staff and to further advance the clinical enterprise strategic plan.
Albanese was previously with NewYork-Presbyterian Hospital, where he served as senior vice president and chief medical officer of the $9.2 billion, 10-hospital academic health system.
Please click here to view a video released this week where he introduces himself to the Duke team: https://duke.is/57vus
Welcome to Duke, Dr. Albanese!
Endress Named Clinical Lead 3300 Effective Jan. 31st
 We are pleased to share that Gerald Endress, a clinical nurse on 3300, has been named Clinical Lead. Endress has worked on 3300 since July 2016 when he began as a new graduate RN. Gerald graduated from Durham Tech Community College and then received his BSN from Western Governors University. Gerald holds several leadership roles here at Duke including Charge Nurse, Preceptor, Responsiveness/Purposeful Rounding Project Manager, and is a member of the DUH Pain team and 3300 Scheduling committee. Endress holds an MS in Exercise Physiology from Old Dominion University and served for many years as the Fitness Director of the former Duke Diet & Fitness Center (now the Duke Lifestyle and Weight Management Center).
We are pleased to share that Gerald Endress, a clinical nurse on 3300, has been named Clinical Lead. Endress has worked on 3300 since July 2016 when he began as a new graduate RN. Gerald graduated from Durham Tech Community College and then received his BSN from Western Governors University. Gerald holds several leadership roles here at Duke including Charge Nurse, Preceptor, Responsiveness/Purposeful Rounding Project Manager, and is a member of the DUH Pain team and 3300 Scheduling committee. Endress holds an MS in Exercise Physiology from Old Dominion University and served for many years as the Fitness Director of the former Duke Diet & Fitness Center (now the Duke Lifestyle and Weight Management Center).
Gerald and his husband, Scott, have been married for five years and live in Raleigh. He is well-known for his great sense of humor. His new role as Clinical Lead is effective January 31st.
Congratulations, Gerald!
First Subject Enrolled in PATCHWORK
 Congratulations to Clinical Cardiac Electrophysiology fellow Zak Loring and his research team – they have enrolled their first patient in the PATCHWORK trial. This study follows the NIH Small Business Innovation Research (SBIR) grant on which Loring serves as PI: Non-invasive hemodynamic sensor patch for remote, early detection and prevention of heart failure with left bundle branch block. The team is targeting any patients who are referred for an echo who do not have complex congenital heart disease and are not actively being paced. If you have any questions about the study or wish to refer a patient, please contact Zak Loring, Melissa Lefevre or Danielle Wilson via email.
Congratulations to Clinical Cardiac Electrophysiology fellow Zak Loring and his research team – they have enrolled their first patient in the PATCHWORK trial. This study follows the NIH Small Business Innovation Research (SBIR) grant on which Loring serves as PI: Non-invasive hemodynamic sensor patch for remote, early detection and prevention of heart failure with left bundle branch block. The team is targeting any patients who are referred for an echo who do not have complex congenital heart disease and are not actively being paced. If you have any questions about the study or wish to refer a patient, please contact Zak Loring, Melissa Lefevre or Danielle Wilson via email.
Cardiac MRI-DN Wins Performance Award
 Congratulations to the Duke Heart Cardiac MRI-DN team – they earned the Patient Experience Monthly Performance Award for Outpatient Test & Treatment (OP T&T) Response to Concerns/Complaints Most Improved from Prior Quarter. Increased Top-Box score from July 2021 – September 2021 to October 2021 – December 2021.
Congratulations to the Duke Heart Cardiac MRI-DN team – they earned the Patient Experience Monthly Performance Award for Outpatient Test & Treatment (OP T&T) Response to Concerns/Complaints Most Improved from Prior Quarter. Increased Top-Box score from July 2021 – September 2021 to October 2021 – December 2021.
Some of the comments received by the team include:
- “Staff was great”
- “So sweet and great with my son. Absolutely loved them.”
- “Everyone was wonderful. We’re all very appreciative.”
Congratulations and keep up the great work!
Duke MLK Observances Continue
 Thursday, Jan. 27: It Starts with Me: Shifting Priorities to Create the Beloved Community. 11-11:45 a.m. via Zoom.
Thursday, Jan. 27: It Starts with Me: Shifting Priorities to Create the Beloved Community. 11-11:45 a.m. via Zoom.
Dr. King once said, “Our lives begin to end the day we become silent about things that matter.” At Duke Health we are putting actions behind these words as we raise our voices together to create a community that is stronger, healthier and more just. While our 2022 celebrations look different from years past, here’s how you can honor Dr. King’s legacy and further his selfless dream:
- Participate in the Jan. 27 Virtual Event. Click here to join “It Starts with Me: Shifting Priorities to Create the Beloved Community,” from 11 – 11:45 a.m. on Thursday, Jan. 27. The keynote speaker will be Damon Tweedy, MD, JD, Associate Professor of Psychiatry and Behavioral Sciences, Duke University School of Medicine, and author of “Black Man in a White Coat: A Doctor’s Reflections on Race and Medicine.” View the flyer and share as appropriate. Download the Zoom background.
- Consider volunteering. Check out opportunities available in the community via MLK service events or Activate Good.
COVID-19 Update
Consider joining the next Duke Health Leadership Town Hall tomorrow, January 24, to ask questions and hear updates on our COVID response, testing, and Omicron. The Zoom event can be accessed here.
Duke Health’s Adopt-A-Unit is a matchmaking program that enables teams to actively support units continuing to fight on the frontlines of COVID through efforts such as meals, expressions of gratitude or other well-being support. If you are a leader interested in adopting a unit, please complete this smartsheet form. Once your information is received, a program member will be in touch to connect you with a unit in need that fits your budget and timeline. If you’d like to donate to our Healthcare Worker Unit Support fund, click here for details. Questions? Contact caring@duke.edu.
Reminder: All Duke University Health System (DUHS) and Private Diagnostic Clinic (PDC) team members, regardless of work location, are required to receive and provide documentation of a completed COVID-19 booster vaccination by 10 a.m. on Tuesday, Feb. 15, 2022, or within 28 days of their eligibility under CDC and state guidelines. More details are available in this email that was sent to all staff on Tuesday, Dec. 28.
All the latest Clinical Operations updates related to COVID can be found at https://covid-19.dukehealth.org.
Upcoming Events & Opportunities
Cardiology Grand Rounds
January 25: End of Life in Heart Failure with Carmelo Milano, Chet Patel and Tony Galanos. 5 p.m., Webex.
February 1: Topic TBA. Presenter will be Caitlin Drescher.
February 10: Topic TBA. Our guest will be AAMC President, Dr. David Skorton.
February 15: Topic TBA. Presenter will be Toi Spates.
THIS WEEK: Dzau Distinguished Lecture in Global Health
Wednesday, Jan. 26: Restoring Global Solidarity on the Road to Pandemic Recovery — A Conversation with Dr. Agnes Binagwaho and Dr. Paul Farmer. Noon – 1:30 p.m., Zoom. Registration required: https://bit.ly/3tbw7SM.
Global health crises require global responses. But in the effort to control COVID-19, rising tides of nationalism have threatened collective action and deepened health inequities for many countries. In the face of these challenges to global health solidarity, the Duke Global Health Institute presents a probing discussion with two of the world’s preeminent global health experts – Dr. Agnes Binagwaho and Dr. Paul Farmer – on how the world failed to cooperate to fight the pandemic and how to chart a new vision to achieve health equity.
This interactive webinar will span two continents, with our featured speakers appearing at the University of Global Health Equity in Butaro, Rwanda. Dr. Gavin Yamey, professor of the practice of global health and public policy, will moderate the conversation from Duke, fielding questions from the online audience. Attendees will join using Zoom webinar, space permitting.
Call for Applicants: 2022 AAMC Early-Career Women Seminar
The Department of Medicine and Program for Women in Internal Medicine (PWIM) are pleased to announce sponsorship for one faculty member to attend the in-person AAMC Early-Career Women Seminar on July 19-22, 2022. This popular and highly interactive seminar provides women at the assistant professor level with foundational leadership knowledge and skills to help achieve career goals and thrive as successful leaders in academic medicine and science. If interested in being considered for sponsorship, please send an email to Kimberly Dorman (kimberly.dorman@duke.edu) by January 31, 2022. Members of the office of the Vice-Chair for Faculty Development and Diversity (Drs. Laura Svetkey and Daniella Zipkin) will select one faculty member to nominate to attend and will notify the applicant by email.
Duke Research Week 2022
January 31 – February 4: Registration is now open for Duke Research Week 2022. Join us virtually for a week-long celebration of research underway at Duke! There is an excellent lineup of faculty lectures, panel discussions, “flash talks” with graduate students, trainees and postdoctoral fellows, and guest presenters for the Robert J. Lefkowitz, MD, Distinguished Lecture and Daubechies Lecture. Check out the full agenda here: https://dukeresearchweek.vfairs.com/en/#distinguishedlectures
National Wear Red Day
Friday, Feb. 4: National Wear Red Day. Help increase awareness of the impact cardiovascular disease has on all of us — wear red on Friday, Feb. 4! We would love to have individual and team photos of you sporting your awareness gear to share in Pulse!!
Kisslo Spring Courses Announced
The 2022 Echo Techs Anatomic & Computer Dissections Course will be held on Saturday, Feb. 5 (Basic) and Saturday, Feb. 12 (Intermediate) for fellows, echo techs and attendings.
Registration is required. Seats fill fast and space is limited. Boxed breakfast/lunch will be provided (as allowed per Covid restrictions). If you would like more information or want to register, please email Dawne Smith. A calendar invitation to confirm registration will be sent to you or you may be added to a waitlist if the sessions are filled. First time participants are given priority. Please let her know if you have taken the course before. If you register and your plans change, please cancel as soon as possible by declining the calendar invite or contacting Dawne so that the open seat can be offered to someone on the waitlist.
The Basic Course on Feb. 5 will take place in the Duke South Amphitheater located across from the Duke South cafeteria entrance. The Intermediate Course on Feb. 12 will take place in the Main Lecture Hall in the Searle Center. Directions for access will be provided closer to the course date. Questions? Dawne can be reached at 919-668-1524 or dawne.t.smith@duke.edu.
Newly Announced CME
April 23: Duke Sports Cardiology & Sudden Death in Athletes Symposium with course directors Jim Daubert and Bill Kraus. Virtual. For information or to register, contact Christy Darnell christy.darnell@duke.edu or 919-880-8686.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
January 17 — Manesh Patel and Marat Fudim
HCP Live
7 FDA Drug Decisions To Watch Through July 2022
https://duke.is/jk9uj
January 18 — Sana Al-Khatib
Medscape
Subclinical Atrial Disease: A Window to Prevent AF and HF?
https://www.medscape.com/viewarticle/966784
January 19 — Duke University Health System
Kiss 95.1 FM
25 of the Best Employers to Work For in North Carolina
https://duke.is/yn9b5
January 20 — Adrian Hernandez
News & Observer
Ivermectin’s potential to treat COVID gets a serious look in Duke University study
https://duke.is/r9dxy###
Division of Cardiology Publications Indexed in PubMed January 13-19, 2022
Assimon MM, Pun PH, Wang LC, Al-Khatib SM, Brookhart MA, Weber DJ, Winkelmayer WC, Flythe JE. Analysis of Respiratory Fluoroquinolones and the Risk of Sudden Cardiac Death Among Patients Receiving Hemodialysis. JAMA Cardiol 2022;7(1):75-83. PM: 34668928.
Berger JS, Kornblith LZ, Gong MN, Reynolds HR, Cushman M, Cheng Y, McVerry BJ, Kim KS, Lopes RD, Atassi B, Berry S, Bochicchio G, de Oliveira Antunes M, Farkouh ME, Greenstein Y, Hade EM, Hudock K, Hyzy R, Khatri P, Kindzelski A, Kirwan BA, Baumann Kreuzi. Effect of P2Y12 Inhibitors on Survival Free of Organ Support Among Non-Critically Ill Hospitalized Patients With COVID-19: A Randomized Clinical Trial. JAMA 2022;327(3):227-236. PM: 35040887.
Cavender MA, Harrington RA, Stone GW, Steg PG, Gibson CM, Hamm CW, Price MJ, Lopes RD, Leonardi S, Deliargyris EN, Prats J, Mahaffey KW, White HD, Bhatt DL. Ischemic Events Occur Early in Patients Undergoing Percutaneous Coronary Intervention and Are Reduced With Cangrelor: Findings From CHAMPION PHOENIX. Circ Cardiovasc Interv 2022;15(1):e010390. PM: 34915723.
Doll JA, Nelson AJ, Kaltenbach LA, Wojdyla D, Waldo SW, Rao SV, Wang TY. Percutaneous Coronary Intervention Operator Profiles and Associations With In-Hospital Mortality. Circ Cardiovasc Interv 2022;15(1):e010909. PM: 34847693.
Felker GM, Solomon SD, Claggett B, Diaz R, McMurray JJV, Metra M, Anand I, Crespo-Leiro MG, Dahlström U, Goncalvesova E, Howlett JG, MacDonald P, Parkhomenko A, Tomcsányi J, Abbasi SA, Heitner SB, Hucko T, Kupfer S, Malik FI, Teerlink JR. Assessment of Omecamtiv Mecarbil for the Treatment of Patients With Severe Heart Failure: A Post Hoc Analysis of Data From the GALACTIC-HF Randomized Clinical Trial. JAMA Cardiol 2022;7(1):26-34. PM: 34643642.
Gandhi S, Garratt KN, Li S, Wang TY, Bhatt DL, Davis LL, Zeitouni M, Kontos MC. Ten-Year Trends in Patient Characteristics, Treatments, and Outcomes in Myocardial Infarction From National Cardiovascular Data Registry Chest Pain-MI Registry. Circ Cardiovasc Qual Outcomes 2022;15(1):e008112. PM: 35041478.
Haghighat L, Reinhardt SW, Saly DL, Lu D, Matsouaka RA, Wang TY, Desai NR. Comfort Measures Only in Myocardial Infarction: Prevalence of This Status, Change Over Time, and Predictors From a Nationwide Study. Circ Cardiovasc Qual Outcomes 2022;15(1):e007610. PM: 35041476.
Huffman KM, Parker DC, Bhapkar M, Racette SB, Martin CK, Redman LM, Das SK, Connelly MA, Pieper CF, Orenduff M, Ross LM, Ramaker ME, Dorling JL, Rosen CJ, Shalaurova I, Otvos JD, Kraus VB, Kraus WE. Calorie restriction improves lipid-related emerging cardiometabolic risk factors in healthy adults without obesity: Distinct influences of BMI and sex from CALERIE™ a multicentre, phase 2, randomised controlled trial. EClinicalMedicine 2022;43:101261. PM: 35028547.
Li C, Qu L, Matz AJ, Murphy PA, Liu Y, Manichaikul AW, Aguiar D, Rich SS, Herrington DM, Vu D, Johnson WC, Rotter JI, Post WS, Vella AT, Rodriguez-Oquendo A, Zhou B. AtheroSpectrum Reveals Novel Macrophage Foam Cell Gene Signatures Associated With Atherosclerotic Cardiovascular Disease Risk. Circulation 2022;145(3):206-218. PM: 34913723.
Lima FV, Manandhar P, Wojdyla D, Wang T, Aronow HD, Kadiyala V, Weissler EH, Madan N, Gilchrist IC, Grines C, Abbott JD. Percutaneous Coronary Intervention Following Diagnostic Angiography by Noninterventional Versus Interventional Cardiologists: Insights From the CathPCI Registry. Circ Cardiovasc Interv 2022;15(1):e011086. PM: 34933569.
Lopez-Sendon JL, Cyr DD, Mark DB, Bangalore S, Huang Z, White HD, Alexander KP, Li J, Nair RG, Demkow M, Peteiro J, Wander GS, Demchenko EA, Gamma R, Gadkari M, Poh KK, Nageh T, Stone PH, Keltai M, Sidhu M, Newman JD, Boden WE, Reynolds HR, Chaitman BR. Effects of initial invasive vs. initial conservative treatment strategies on recurrent and total cardiovascular events in the ISCHEMIA trial. Eur Heart J 2022;43(2):148-149. PM: 34514494.
Mann DL, Givertz MM, Vader JM, Starling RC, Shah P, McNulty SE, Anstrom KJ, Margulies KB, Kiernan MS, Mahr C, Gupta D, Redfield MM, Lala A, Lewis GD, DeVore AD, Desvigne-Nickens P, Hernandez AF, Braunwald E. Effect of Treatment With Sacubitril/Valsartan in Patients With Advanced Heart Failure and Reduced Ejection Fraction: A Randomized Clinical Trial. JAMA Cardiol 2022;7(1):17-25. PM: 34730769.
Newby LK. A new biomarker of acute coronary ischaemia: from bench to bedside? Eur Heart J 2022;43(2):164-166. PM: 34791138.
Nørgaard BL, Gaur S, Fairbairn TA, Douglas PS, Jensen JM, Patel MR, Ihdayhid AR, Ko BSH, Sellers SL, Weir-McCall J, Matsuo H, Sand NPR, Øvrehus KA, Rogers C, Mullen S, Nieman K, Parner E, Leipsic J, Abdulla J. Prognostic value of coronary computed tomography angiographic derived fractional flow reserve: a systematic review and meta-analysis. Heart 2022;108(3):194-202. PM: 34686567.
Reed SD, Yang JC, Rickert T, Johnson FR, Gonzalez JM, Mentz RJ, Krucoff MW, Vemulapalli S, Adamson PB, Gebben DJ, Rincon-Gonzalez L, Saha A, Schaber D, Stein KM, Tarver ME, Bruhn-Ding D. Quantifying Benefit-Risk Preferences for Heart Failure Devices: A Stated-Preference Study. Circ Heart Fail 2022;15(1):e008797. PM: 34937393.
Rymer JA, Li S, Pun PH, Thomas L, Wang TY. Racial Disparities in Invasive Management for Patients With Acute Myocardial Infarction With Chronic Kidney Disease. Circ Cardiovasc Interv 2022;15(1):e011171. PM: 34915722.
Rymer JA, Narcisse D, Cosiano M, Tanaka J, McDermott MM, Treat-Jacobson DJ, Conte MS, Tuttle B, Patel MR, Smolderen KG. Patient-Reported Outcome Measures in Symptomatic, Non-Limb-Threatening Peripheral Artery Disease: A State-of-the-Art Review. Circ Cardiovasc Interv 2022;15(1):e011320. PM: 34937395.
Takagi H, Leipsic JA, McNamara N, Martin I, Fairbairn TA, Akasaka T, Nørgaard BL, Berman DS, Chinnaiyan K, Hurwitz-Koweek LM, Pontone G, Kawasaki T, Rønnow Sand NP, Jensen JM, Amano T, Poon M, Øvrehus KA, Sonck J, Rabbat MG, Mullen S, De Bruyne B, et al. Trans-lesional fractional flow reserve gradient as derived from coronary CT improves patient management: ADVANCE registry. J Cardiovasc Comput Tomogr 2022;16(1):19-26. PM: 34518113.
Timmons JA, Anighoro A, Brogan RJ, Stahl J, Wahlestedt C, Farquhar DG, Taylor-King J, Volmar CH, Kraus WE, Phillips SM. A human-based multi-gene signature enables quantitative drug repurposing for metabolic disease. Elife 2022;11:10.7554/eLife.68832. PM: 35037854.
Vora AN, Swaminathan RV. Posting Another Win for Intravascular Imaging: Moving Away From Angiography-Only Percutaneous Coronary Intervention Toward a More Comprehensive Approach. Circ Cardiovasc Interv 2022;15(1):e011670. PM: 35041451.
Wang H, Noordam R, Cade BE, Schwander K, Winkler TW, Lee J, Sung YJ, Bentley AR, Manning AK, Aschard H, Kilpeläinen TO, Ilkov M, Brown MR, Horimoto AR, Richard M, Bartz TM, Vojinovic D, Lim E, Nierenberg JL, Liu Y, Chitrala K, Rankinen T, Musani SK, et al. Multi-ancestry genome-wide gene-sleep interactions identify novel loci for blood pressure. Mol Psychiatry 2021;26(11):6293-6304. PM: 33859359.
Yancy CW, Hernandez AF, Fonarow GC. Identifying Treatments for Stage C2 Heart Failure. JAMA Cardiol 2022;7(1):34-35. PM: 34643645.
Duke Heart Pulse – Week Ending January 16th 2022
Chief’s message:
Hopefully you all will get a moment this weekend to enjoy the North Carolina “Snow.” As we reflect on MLK day, we remember the non-violent protests and consistent work of Dr. King to advocate and fight for justice and civil rights for all. I am including some of his words below to consider in our upcoming days of action and service.
“Of all the forms of inequality, injustice in healthcare is the most shocking and inhumane.”
“Life’s most persistent and urgent question is, ‘What are you doing for others?”
“The time is always right to do what is right.”
Rounding this last week in the CICU, I was again reminded by the tremendous dedication of our fellows, residents, nurses, respiratory therapists, pharmacists, APPs, faculty, and countless other staff that are continually working as teams to help care for our patients and each other. Thank you all for the unwavering dedication, professionalism, and clinical expertise.
Highlights of the week:
Rymer, Greene Selected for 2022 LEADER Program

Duke Heart faculty members Jennifer Rymer and Stephen Greene are among 36 Duke
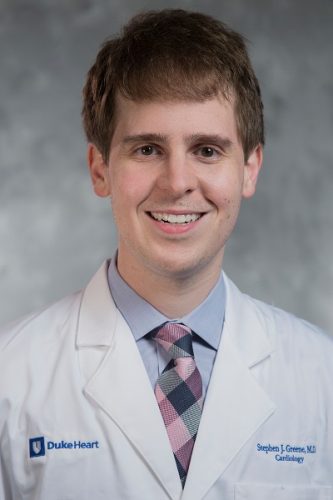
physician scientists selected to the 2022 cohort for Duke’s course on Leadership Development for Researchers (LEADER). The faculty development program is an interactive 5-month series designed for junior faculty who are leading research teams. The leadership course is designed to help build critical skills for leading teams, such as conflict management, effective mentorship, negotiation skills, leading with emotional intelligence and balancing competing priorities.
Congratulations, Jenn and Steve!
7E Earns Beacon Award for Excellence
We are excited to share that our Duke Heart Cardiac Intensive Care Unit (ICU) has received a Beacon Award for Excellence from the American Association of Critical-Care Nurses (AACN)!
This national award recognizes caregivers in units whose consistent and systematic approach to evidence-based care optimizes patient outcomes. Units that receive this national recognition serve as role models to others across the country on their journey to excellent patient and family care. The application reviewers noted the unit’s strong sense of collaboration amongst teams to drive patient outcomes and improve quality of care.
Beacon Awards are national awards recognizing nursing excellence and speak to the caliber of nursing provided on the unit. A team must apply for consideration and must meet clearly defined criteria across five categories: leadership structures and systems; appropriate staffing and staff engagement; effective communication, knowledge management and learning development; evidence-based practice and processes; and outcome measurements.
Only 20 Cardiac ICUs in the U.S. currently hold this designation. We are incredibly proud of 7 East!
Congratulations and way to go, team!!!
![]()

![]()
Kudos to Eleazu!
Kristin Newby shared a terrific note with us that she received this week about cardiology fellow Ijeoma Eleazu:
“Hi Dr. Newby,
I wanted to write a quick message singling out Dr. Eleazu for special praise. Our team had a difficult night last night, not only  because of challenges in patient care, but also with the additional stress on everyone, largely because of Covid. Despite the multiple codes and many other challenges, Dr. Eleazu was a true leader, providing a steady and reassuring hand throughout. She demonstrated unflappability despite the increased stress and difficulties in patient care. For the housestaff, she was a tremendous advocate, stepping up when we needed input or a voice of support. Throughout it all, she continue to teach, challenging us to rise the occasion by allowing us to formulate our own plans rather than dictating.
because of challenges in patient care, but also with the additional stress on everyone, largely because of Covid. Despite the multiple codes and many other challenges, Dr. Eleazu was a true leader, providing a steady and reassuring hand throughout. She demonstrated unflappability despite the increased stress and difficulties in patient care. For the housestaff, she was a tremendous advocate, stepping up when we needed input or a voice of support. Throughout it all, she continue to teach, challenging us to rise the occasion by allowing us to formulate our own plans rather than dictating.
I am thankful for her leadership and exemplary performance and wanted to make sure it was recognized.
Best regards, Hubie Haywood”
Great work, Ijeoma!
Kudos to Whitney Bakimli!
One of our excellent Cardiothoracic Surgery Step-down Unit nurses, Whitney Bakimli, has received a Great Catch from Duke University Hospital leadership!
Whitney noticed two identical orders for Lasix for a patient. While the total dose was not unusual, she was concerned that it might be too high for this particular patient. Whitney contacted the provider and learned that the order was mistakenly duplicated.
Great job, Whitney!
MLK Commemoration 2022
This year’s Martin Luther King, Jr. keynote address will take place at 3 p.m. today (Sunday, Jan. 16). How Long Must We Wait: Striving For the Beloved Community will be given by historian and social activist, Keeanga-Yamahtta Taylor. The event, originally planned to occur in Duke Chapel, has been moved to a virtual event that will be live streamed due to the pending winter storm. There are several community service opportunities scheduled this week in honor of MLK Day. We encourage you to check them out. Information about both the keynote address and service opportunities are available on the Duke MLK Commemoration website (https://mlk.duke.edu).

COVID-19 Update
As of Friday, Jan. 14, Duke Health has moved from Tier 2 (Limited Access) to Tier 3 (Restricted Access) of our visitation guidelines. The transition was made based on recommendations from the CDC and our infectious disease experts due to the increased COVID infection rates in our community and among team members.
Documentation regarding visitation restrictions as well as the latest Clinical Operations updates regarding COVID-19 and links to the most recent DUHS Leadership Virtual Town Hall recordings can be found here: https://covid-19.dukehealth.org.
Reminder: All Duke University Health System (DUHS) and Private Diagnostic Clinic (PDC) team members, regardless of work location, are required to receive and provide documentation of a completed COVID-19 booster vaccination by 10 a.m. on Tuesday, Feb. 1, 2022, or within 28 days of their eligibility under CDC and state guidelines. More details are available in this email that was sent to all staff on Tuesday, Dec. 28.
Critical Need for Blood Donations
 On Tuesday, the American Red Cross announced a national blood crisis – the worst shortage in more than 10 years. If you’d like to donate, there are several upcoming blood drives scheduled to take place in The Great Hall at Trent Semans Center:
On Tuesday, the American Red Cross announced a national blood crisis – the worst shortage in more than 10 years. If you’d like to donate, there are several upcoming blood drives scheduled to take place in The Great Hall at Trent Semans Center:
- Thursday, Jan. 20 from 11 a.m. to 4 p.m.
- Tuesday, Feb. 1 from 9 a.m. to 3 p.m.
- Tuesday, Feb. 15 from 9 a.m. to 3 p.m
The best way to locate a drive in your area and to schedule a donation is by visiting: https://www.redcrossblood.org/.
ICYMI: Durham County Offering Boosters to Ages 12-15, Third Doses to Ages 5-11; Pfizer Booster Waiting Period Reduced to Five Months
As of Monday, January 10, the Durham County Department of Public Health expanded COVID-19 vaccination eligibility at its vaccination clinic. They will offer booster doses of Pfizer COVID-19 vaccines for all people ages 12-15, and third doses of Pfizer vaccines for children ages 5-11 who are moderately to severely immunocompromised. Additionally, booster vaccinations will now be available for all people 12 and older five months after they complete a primary Pfizer vaccination series, reducing the waiting period from its previous length of six months. To learn more, visit: https://bit.ly/3qsa4Fm.
Upcoming Events & Opportunities
Cardiology Grand Rounds
January 18: The Ultimate ‘Anti-Racism Statement’ Medicine Can Make is to Diversify its Ranks with Quinn Capers, IV of the University of Texas Southwestern Medical Center. 5 p.m. via Webex.
January 20: Road to Heart Transplantation: Challenges, Opportunities, New Frontiers with Mary Keebler, University of Pittsburgh Medical Center. 5 p.m., Webex.
January 25: Palliative Care Grand Rounds with Carmelo Milano, Chet Patel and Tony Galanos. Time and location TBA.
February 1: Topic TBA. Presenter will be Caitlin Drescher.
February 10: Topic TBA. Our guest will be AAMC President, Dr. David Skorton.
February 15: Topic TBA. Presenter will be Toi Spates.
Dzau Distinguished Lecture in Global Health
Wednesday, Jan. 26: Restoring Global Solidarity on the Road to Pandemic Recovery — A Conversation with Dr. Agnes Binagwaho and Dr. Paul Farmer. Noon – 1:30 p.m., Zoom. Registration required: https://bit.ly/3tbw7SM.
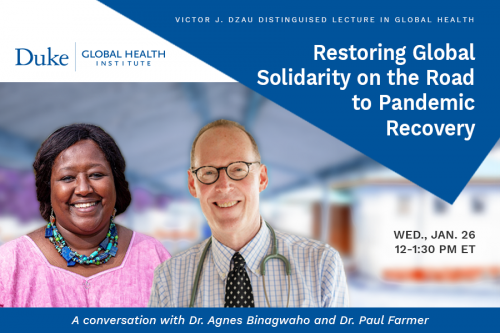 Global health crises require global responses. But in the effort to control COVID-19, rising tides of nationalism have threatened collective action and deepened health inequities for many countries. In the face of these challenges to global health solidarity, the Duke Global Health Institute presents a probing discussion with two of the world’s preeminent global health experts – Dr. Agnes Binagwaho and Dr. Paul Farmer – on how the world failed to cooperate to fight the pandemic and how to chart a new vision to achieve health equity.
Global health crises require global responses. But in the effort to control COVID-19, rising tides of nationalism have threatened collective action and deepened health inequities for many countries. In the face of these challenges to global health solidarity, the Duke Global Health Institute presents a probing discussion with two of the world’s preeminent global health experts – Dr. Agnes Binagwaho and Dr. Paul Farmer – on how the world failed to cooperate to fight the pandemic and how to chart a new vision to achieve health equity.
This interactive webinar will span two continents, with our featured speakers appearing at the University of Global Health Equity in Butaro, Rwanda. Dr. Gavin Yamey, professor of the practice of global health and public policy, will moderate the conversation from Duke, fielding questions from the online audience. Attendees will join using Zoom webinar, space permitting.
Call for Applicants: 2022 AAMC Early-Career Women Seminar
The Department of Medicine and Program for Women in Internal Medicine (PWIM) are pleased to announce sponsorship for one faculty member to attend the in-person AAMC Early-Career Women Seminar on July 19-22, 2022. This popular and highly interactive seminar provides women at the assistant professor level with foundational leadership knowledge and skills to help achieve career goals and thrive as successful leaders in academic medicine and science. If interested in being considered for sponsorship, please send an email to Kimberly Dorman (kimberly.dorman@duke.edu) by January 31, 2022. Members of the office of the Vice-Chair for Faculty Development and Diversity (Drs. Laura Svetkey and Daniella Zipkin) will select one faculty member to nominate to attend and will notify the applicant by email.
Duke Research Week 2022
January 31 – February 4: Registration is now open for Duke Research Week 2022. Join us virtually for a week-long celebration of research underway at Duke! There is an excellent lineup of faculty lectures, panel discussions, “flash talks” with graduate students, trainees and postdoctoral fellows, and guest presenters for the Robert J. Lefkowitz, MD, Distinguished Lecture and Daubechies Lecture. Check out the full agenda here: https://dukeresearchweek.vfairs.com/en/#distinguishedlectures
National Wear Red Day
Friday, Feb. 4: National Wear Red Day. Help increase awareness of the impact cardiovascular disease has on all of us — wear red on Friday, Feb. 4! We would love to have individual and team photos of you sporting your awareness gear to share in Pulse!!
Kisslo Spring Courses Announced
The 2022 Echo Techs Anatomic & Computer Dissections Course will be held on Saturday, Feb. 5 (Basic) and Saturday, Feb. 12 (Intermediate) for fellows, echo techs and attendings.
Registration is required. Seats fill fast and space is limited. Boxed breakfast/lunch will be provided (as allowed per Covid restrictions). If you would like more information or want to register, please email Dawne Smith. A calendar invitation to confirm registration will be sent to you or you may be added to a waitlist if the sessions are filled. First time participants are given priority. Please let her know if you have taken the course before. If you register and your plans change, please cancel as soon as possible by declining the calendar invite or contacting Dawne so that the open seat can be offered to someone on the waitlist.
The Basic Course on Feb. 5 will take place in the Duke South Amphitheater located across from the Duke South cafeteria entrance. The Intermediate Course on Feb. 12 will take place in the Main Lecture Hall in the Searle Center. Directions for access will be provided closer to the course date. Questions? Dawne can be reached at 919-668-1524 or dawne.t.smith@duke.edu.
Newly Announced CME
April 23: Duke Sports Cardiology & Sudden Death in Athletes Symposium with course directors Jim Daubert and Bill Kraus. Virtual. For information or to register, contact Christy Darnell christy.darnell@duke.edu or 919-880-8686.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
January 7 — Robert McGarrah
The Washington Post
https://duke.is/gmcqy
January 8 — Duke University Hospital (Carmat)
Healio/Cardiology
Most read in HF of 2021: Empagliflozin for HFpEF, COVID-19-related myocarditis and more
https://duke.is/gmcqy
January 12 — Maitreya Thakkar
Healio/Cardiology
New perspectives on CV risk assessment of prospective kidney recipients, donors
https://duke.is/6738f
Division of Cardiology Publications Indexed in PubMed January 6-12, 2022
Bishawi M, Milano C, Gaca J, Carr K, Wang A, Glower DD. The outcome of mitral repair for degenerative versus ischemic mitral regurgitation using a single complete ring. J Card Surg 2022;37(2):290-296. PM: 34665478.
Califf RM, Wong C, Doraiswamy PM, Hong DS, Miller DP, Mega JL. Biological and clinical correlates of the patient health questionnaire-9: exploratory cross-sectional analyses of the baseline health study. BMJ Open 2022;12(1):e054741. PM: 34983769.
Devore AD, Schlendorf KH. HCV Positive Allograft Use in Heart Transplant: A Silver Lining to an Epidemic. J Card Fail 2022;28(1):42-43. PM: 34628017.
Fox KAA, Virdone S, Bassand JP, Camm AJ, Goto S, Goldhaber SZ, Haas S, Kayani G, Koretsune Y, Misselwitz F, Oh S, Piccini JP, Parkhomenko A, Sawhney JPS, Stepinska J, Turpie AGG, Verheugt FWA, Kakkar AK. Do baseline characteristics and treatments account for geographical disparities in the outcomes of patients with newly diagnosed atrial fibrillation? The prospective GARFIELD-AF registry. BMJ Open 2022;12(1):e049933. PM: 34996784.
Friedman DJ, Overmann JA, Fish JM, Gaeta SA, Tranter JH, Thao R, Piccini JP. Continuous and discontinuous radiofrequency energy delivery on the atrial free wall: Lesion transmurality, width, and biophysical characteristics. Heart Rhythm O2 2021;2(6Part A):635-641. PM: 34988509.
Lala A, Mentz RJ. The JCF Reviewer Mentorship Program. J Card Fail 2022;28(1):1-2. PM: 35000756.
Lam KY, Reardon MJ, Yakubov SJ, Modine T, Fremes S, Tonino PAL, Tan ME, Gleason TG, Harrison JK, Hughes GC, Oh JK, Head SJ, Huang J, Deeb GM. Surgical Sutureless and Sutured Aortic Valve Replacement in Low-risk Patients. Ann Thorac Surg 2022;113(2):616-622. PM: 33794164.
Oshunbade AA, Lirette ST, Windham BG, Shafi T, Hamid A, Gbadamosi SO, Tin A, Yimer WK, Tibuakuu M, Clark D, Kamimura D, Lutz EA, Mentz RJ, Fox ER, Butler J, Butler KR, Garovic VD, Turner ST, Mosley TH, Hall ME. Hypertensive Diseases in Pregnancy and Kidney Function Later in Life: The Genetic Epidemiology Network of Arteriopathy (GENOA) Study. Mayo Clin Proc 2022;97(1):78-87. PM: 34565606.
Packer DL, Mark DB, Lee KL. CABANA: underpowered and with detrimental protocol changes: is ‘ablation salvation’?-Reply by the authors of the CABANA trial. Europace 2022;24(1):3. PM: 34792125.
Patel MR, Jeremias A, Maehara A, Matsumura M, Zhang Z, Schneider J, Tang K, Talwar S, Marques K, Shammas NW, Gruberg L, Seto A, Samady H, Sharp ASP, Ali ZA, Mintz G, Davies J, Stone GW. 1-Year Outcomes of Blinded Physiological Assessment of Residual Ischemia After Successful PCI: DEFINE PCI Trial. JACC Cardiovasc Interv 2022;15(1):52-61. PM: 34991824.
Rao VN, Obeid MJ, Rigiroli F, Russell SD, Patel CB, Molinger J, Gupta RT, Agarwal R, Fudim M. Pericardial Adipose Tissue Volume and Left Ventricular Assist Device-Associated Outcomes. J Card Fail 2022;28(1):149-153. PM: 34274515.
Rasmussen PV, Pallisgaard JL, Hansen ML, Gislason GH, Torp-Pedersen C, Ruwald M, Alexander KP, Lopes RD, Al-Khatib SM, Dalgaard F. Treatment of older patients with atrial fibrillation by morbidity burden. Eur Heart J Qual Care Clin Outcomes 2022;8(1):23-30. PM: 32857834.
Rimbach R, Yamada Y, Sagayama H, Ainslie PN, Anderson LF, Anderson LJ, Arab L, Baddou I, Bedu-Addo K, Blaak EE, Blanc S, Bonomi AG, Bouten CVC, Bovet P, Buchowski MS, Butte NF, Camps SGJA, Close GL, Cooper JA, Das SK, Dugas LR, Ekelund U, Entringer S. Total energy expenditure is repeatable in adults but not associated with short-term changes in body composition. Nat Commun 2022;13(1):99. PM: 35013190.
Sharma A, Zheng Y, Ezekowitz JA, Westerhout CM, Udell JA, Goodman SG, Armstrong PW, Buse JB, Green JB, Josse RG, Kaufman KD, McGuire DK, Ambrosio G, Chuang LM, Lopes RD, Peterson ED, Holman RR. Cluster Analysis of Cardiovascular Phenotypes in Patients With Type 2 Diabetes and Established Atherosclerotic Cardiovascular Disease: A Potential Approach to Precision Medicine. Diabetes Care 2022;45(1):204-212. PM: 34716214.
Steinberg BA, Zhang M, Bensch J, Lyons A, Bunch TJ, Piccini JP, Siu A, Spertus JA, Stehlik J, Wohlfahrt P, Greene T, Hess R, Fang JC. Quantifying the Impact of Atrial Fibrillation on Heart Failure-Related Patient-Reported Outcomes in the Utah mEVAL Program. J Card Fail 2022;28(1):13-20. PM: 34324927.
Tamirisa KP, Al-Khatib SM, Mohanty S, Han JK, Natale A, Gupta D, Russo AM, Al-Ahmad A, Gillis AM, Thomas KL. Racial and Ethnic Differences in the Management of Atrial Fibrillation. CJC Open 2021;3(12 Suppl):S137-S148. PM: 34993443.
Tanawuttiwat T, Stebbins A, Marquis-Gravel G, Vemulapalli S, Kosinski AS, Cheng A. Use of Direct Oral Anticoagulant and Outcomes in Patients With Atrial Fibrillation after Transcatheter Aortic Valve Replacement: Insights From the STS/ACC TVT Registry. J Am Heart Assoc 2022;11(1):e023561. PM: 34970918.
Tcheng JE, Nguyen MV, Brann HW, Clarke PA, Pfeiffer M, Pleasants JR, Shelton GW, Kelly JF. The Medical Device Unique Device Identifier as the Single Source of Truth in Healthcare Enterprises – Roadmap for Implementation of the Clinically Integrated Supply Chain. Med Devices (Auckl) 2021;14:459-467. PM: 34992475.
Wang P, Castellani CA, Yao J, Huan T, Bielak LF, Zhao W, Haessler J, Joehanes R, Sun X, Guo X, Longchamps RJ, Manson JE, Grove ML, Bressler J, Taylor KD, Lappalainen T, Kasela S, Van Den Berg DJ, Hou L, Reiner A, Liu Y, Boerwinkle E, Smith JA, Peyser PA. Epigenome-wide association study of mitochondrial genome copy number. Hum Mol Genet 2021;31(2):309-319. PM: 34415308.
Warraich HJ, Kitzman DW, Nelson MB, Mentz RJ, Rosenberg PB, Lev Y, Whellan DJ. Older Patients With Acute Decompensated Heart Failure Who Live Alone: An Analysis From the REHAB-HF Trial. J Card Fail 2022;28(1):161-163. PM: 34147611.
Duke Heart Pulse week ending January 9th 2022
Chief’s message:
Hope you all had some time with family and had a happy new year. We know the upcoming weeks and months will be challenging to all of us, including many of our colleagues, staff, faculty and fellows in healthcare. We appreciate the continued diligence across the Heart Center in helping care for our patients and each other.
Highlights of the week:
Kudos Across Duke Heart & to Center of Excellence Staff!
The latest surge in COVID-19 infections has posed great challenges across all areas of Duke Heart and we recognize how stressful this has been to each member of our team and to our colleagues across the Health System. We appreciate the flexibility our entire team is showing and your willingness to support one another. THANK YOU for all that you’re doing.
The Duke Heart Leadership team has check-ins throughout the day to monitor and assess needs during this rapidly changing situation. If you are in need of resources, supplies or other support please do not hesitate to reach out to us. We will do everything we can to get you what you need as soon as possible.
The leadership team for Duke Heart is deeply grateful for all efforts across the Heart Center as we respond to the current surge in infections and the impact that is having on staffing levels. We especially want to thank Joe Kelly, Melissa Williams and the full Center of Excellence team for stepping up, saying ‘yes’, and mobilizing their team to help.
After a big increase in the number of Duke Health employees who have been out sick with COVID, nurses across the health system — including a number of nurses from the Duke Heart Center of Excellence — who do not work directly in patient care settings are assisting with efforts to return employees to work. They have been making calls to employees and screening them for suitability to return to work. They are collaborating closely with the Employee Occupational Health and Wellness (EOHW) team to apply the latest recommendations on reducing the risk of infectious spread in the workplace. Employees with active symptoms which are not improving are being re-assigned to an EOHW case manager.
Again, thank you for all that you’re doing. We will continue to support one another and our patients and we will get through this, together. Keep up the outstanding work!
Heart Transplants Hit 116 for Year; Further Reduction in Wait Times Noted
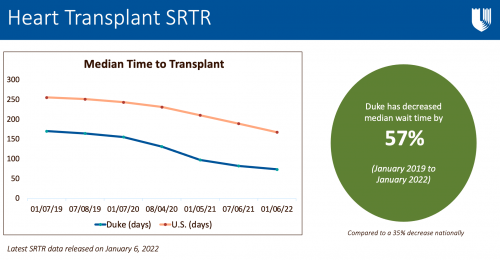 Our Duke Heart Transplant team completed a remarkable 116 heart transplants in 2021 and the latest Scientific Registry of Transplant Recipients (SRTR) report — released on Thursday, January 6 — shows excellent outcomes as well as a reduction in our median wait times.
Our Duke Heart Transplant team completed a remarkable 116 heart transplants in 2021 and the latest Scientific Registry of Transplant Recipients (SRTR) report — released on Thursday, January 6 — shows excellent outcomes as well as a reduction in our median wait times.
“We continue to have year over year growth and this past year was our highest ever at 116 total heart transplants,” says Adam DeVore, medical director, Duke Heart Transplantation Program. “Our wait times have been the lowest in the southeast for a while and a lot of that is due to the DCD program and changes around that. We have also seen an increase in referrals from other transplant centers throughout the region, which we attribute to our ability to get patients transplanted faster as well as good outcomes.”
Based on data reported to SRTR from October 2018 through December 31, 2021, Duke’s median wait time has decreased by 57 percent.
“Our highest ever volume, with continued excellent results, reflects the amazing work by the entire team, says Jacob Schroder, MD, surgical director, Duke Heart Transplantation Program and Co-Director, Cardiothoracic Surgical Intensive Care Unit. “We continue to be leaders, and innovators, in advanced heart failure therapies, not only in the U.S. but the world. 116 is just the beginning.”
DeVore says it’s important to recognize that these results are not just the result of the transplant program, but the efforts of all members across Duke Heart Center.
“The transplant program itself is a huge team made up of people from surgery, anesthesia and cardiology and the latest data demonstrates the hard work of our team across those areas,” DeVore added. “However, this is also very much a celebration of the Heart Center. These patients go to the Echo lab, they get MRIs, they go to the Catheterization lab, they sometimes come into the Health System because they need an EP procedure… and then maybe at some point they need a transplant. So, not only is this great news for the heart transplant program, but it’s a reflection of the work done across Duke Heart.”
We could not have said it better. Impressive work, across the board. Congratulations, team!
Bryner Named Assistant Program Director, CT Surgery Residency Program
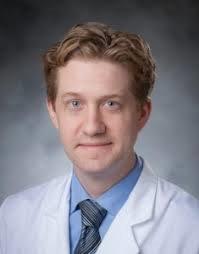 We are pleased to share that Ben Bryner has been named the new assistant program director of our Cardiothoracic Surgery Residency Program.
We are pleased to share that Ben Bryner has been named the new assistant program director of our Cardiothoracic Surgery Residency Program.
In a note to the cardiothoracic faculty in December, Dr. Edward P. Chen, chief of the division, commented: “During his time on faculty, Dr. Bryner has proven to be a tireless educator committed to providing our resident learners with a rich and comprehensive training experience. We look forward to his leadership in our training program as well as his development of creative and innovative methods to further advance and improve upon our education mission. Dr. Bryner will continue the tradition of excellence in this role established by his predecessor, Dr. Brittany Zwischenberger. I would also like to express my sincere gratitude to Dr. Zwischenberger for her devoted service to our residency program over the last several years.”
Congrats, Ben!
Gutierrez Selected for ACC Emerging Faculty Leadership Academy

Duke Heart
Congratulations to Tony Gutierrez! He was recently notified of his selection from a competitive group of candidates to participate
in the 2022 American College of Cardiology’s Rick Nishimura, MD, MACC and Patrick T. O’Gara, MD, MACC Emerging Faculty Leadership Academy. The leadership course will be held May 1-3 at Heart House in Washington, DC.
Well deserved!
Snider Named President-Elect of AmSECT
Duke Heart perfusionist William Scott Snider has been named President-Elect of the American Society of Extracorporeal Technology (AmSECT) Board of Directors. The term begins in April. Snider currently serves on the Board as Treasurer. He also chairs AmSECT’s Perfusion Without Borders subcommittee.
We asked him recently about his experiences with AmSECT and his commitment to volunteering:
“Like a lot of society volunteers, I became a member of AmSECT as a student and watched from a distance for a long time — not really understanding all that a professional society can mean or the long history behind it and the many volunteers who spend hours upon hours of time in the pursuit of professional excellence within our profession,” Snider says. “As I have become more involved over the years, I have gained a better appreciation for all of these things and am very grateful for all that has been done to grow our field and keep it strong. I volunteer because it’s very exciting to me to be a small part of that big vision.
“My path in AmSECT and my career at Duke began at almost the same time, and each have rewarded me in very similar ways. Each day I’m humbled by the quality of character of each of the nurses, doctors and allied health professionals that I work with. The vision statement of Duke, ‘to educate and discover,’ is very similar to the mission statement of AmSECT. For more than 50 years, they have been driven by a goal to support our workforce as they support their patients. It’s a vision that’s shared by everyone who dedicates their life to healthcare. What makes it so gratifying is doing it together, as a team. If there was one thing that I could share about why I value both AmSECT and Duke, it would be because of the truly remarkable, conscientious, professional, motivated people that I’ve met along the way. They continue to inspire me, and I’m so fortunate to be a part of it all.”
Congratulations, Scott!
Kisslo Spring Courses Announced
The 2022 spring session dates of the echocardiography course led by Joe Kisslo have been released. The Echo Techs Anatomic & Computer Dissections Course will be held on Saturday, Feb. 5 (Basic) and Saturday, Feb. 12 (Intermediate) for fellows, echo techs and attendings.
Registration is required. Seats fill fast and space is limited. Boxed breakfast/lunch will be provided (as allowed per Covid restrictions). If you would like more information or want to register, please email Dawne Smith. A calendar invitation to confirm registration will be sent to you or you may be added to a waitlist if the sessions are filled. First time participants are given priority. Please let her know if you have taken the course before. If you register and your plans change, please cancel as soon as possible by declining the calendar invite or contacting Dawne so that the open seat can be offered to someone on the waitlist.
The Basic Course on Feb. 5 will take place in the Duke South Amphitheater located across from the Duke South cafeteria entrance. The Intermediate Course on Feb. 12 will take place in the Main Lecture Hall in the Searle Center. Directions for access will be provided closer to the course date. Questions? Dawne can be reached at 919-668-1524 or dawne.t.smith@duke.edu.
Coston & Team Place in Top 4, NurseHack4Health
 Congratulations to Kimberly Coston, one of our amazing nurses on 3300, and to her ‘Knightingale‘ team members for placing among the top four teams in the November NurseHack4Health hackathon sponsored by Johnson & Johnson. Coston collaborated with the other healthcare professionals on her team (located throughout the world) and worked on a project to combat nursing burnout.
Congratulations to Kimberly Coston, one of our amazing nurses on 3300, and to her ‘Knightingale‘ team members for placing among the top four teams in the November NurseHack4Health hackathon sponsored by Johnson & Johnson. Coston collaborated with the other healthcare professionals on her team (located throughout the world) and worked on a project to combat nursing burnout.
Team Knightingale
Project title: Solving for nurse burnout, which has been exacerbated by COVID-19, with cloud-based software for hospitals and facilities to assess, reaffirm and reset nurses’ mental health.
Track: Diversity in Practice and Care
Team Members: Ryan Etzel, Layne Price, Sharonda Davis, Pak Chau, Rachel Harper, Kimberly Coston, Rob McKenna and Rashna Batliwala
“We are so proud to have Kimberly on our 3300 team!” says Courtney Stierwalt, clinical lead RN for 3300.
Designed to give nurses the unique opportunity to create solutions for challenges that directly impact them and their profession, the weekend-long virtual hackathon was themed “building a sustainable nursing workforce of the future” and was a direct response to the urgent need to recruit and retain a diverse nursing workforce as a nursing shortage accelerates around the country. Nursing turnover is reaching nearly 20 percent per year, leading to a risk of decreased stability and quality in patient care and increasing health system costs.
Over the course of 48 hours, a diverse audience of innovators, including registered nurses, physicians, academics, nursing students, developers and design experts from 38 states and over 40 countries came together to focus on developing solutions for long-standing foundational challenges in the nursing workforce.
Nicely done, Kimberly!
Kudos to all Cardiology Fellows!
We were sent a wonderful note by Anna Lisa Chamis ahead of the holidays – it was sent to the entire team of cardiology fellows from Jacob Schroder.
“I just wanted to write you all a note expressing my gratitude for the amazing job you guys do on a daily basis.
Year in, year out, the CV fellow group is hands down the best in the hospital. For most other specialties, I often skip the trainees and go straight for attending-to-attending communication. Cardiology is different, though. Most of the time, I see the CV fellows as more of an ally and equal and will seek them out first. Not to mention, for our trainees, the cardiology fellows are a huge resource. I still remember being the surgical intern covering 31/3300. Dan Bensimon, a fellow at that time, was the person I called constantly for CV issues. Saved my life. And I know for my wife, Vanessa, that person was one Chet Patel (!) and she felt the same way.
Being a fellow is often a daunting and thankless job. But…
- Keep doing what you are doing, you have a significant role in how well our patients do
- Call any time day or night
- Come visit any time in the OR, especially when you are bored, curious, or want to see how we deal with one of your patients!
Happy New Year!!! 2022 is going to be off the hook.” — JNS
“Thank you so much for taking the time to write this thoughtful feedback about and to the cardiology fellows. Our cardiology fellows (and faculty!) are truly lucky to learn from and collaborate with the best CT surgeons anywhere. #ilovedukeheart” — Anna Lisa
The Duke Heart team is truly special — please keep that gratitude flowing! Sharing with one another how much you appreciate and value your teammates is important, especially during these challenging times. We love sharing your uplifting notes and kudos in Pulse. Keep up the great work, everyone!
Kudos to the Duke Electrophysiology Team
We received a warm note from a grateful patient family member during the holiday season. They wrote:
“Hi Dr. Piccini, Our family is deeply grateful for your care of our beloved family member over the weekend. You inspired a great deal of confidence regarding his care plan, which greatly reduced his stress while hospitalized. Being an ever proud Frenchman, he was very pleased about your experiences with and fond feelings for France. Thanks to you and your team, he will be returning home in better condition than he left. We would like to wish you and your family un Joyeux Noel!” – grateful family member (names withheld to maintain confidentiality)
And this related note to the team from Diane Sauro, “Thank you all for the exceptional work you do every day. We appreciate all you do for your patients and the team.” — Diane
Great work, Jon and team!
Kudos to Kesler!
A grateful patient took some extra time last month to speak with James Mills and send a follow-up note about Autumn Kesler, nurse practitioner, via MyChart:
“When you hired Autumn you hit a grand slam completely out of the park! She is great!” – grateful patient
According to Cheri Wills, Health Center Administrator for Duke Cardiology of Raleigh, “Autumn has only been with our clinic since March 2021 and fit in immediately. She is wonderful in so many ways and we are fortunate to have her as part of our team.”
Way to go, Autumn!
Heart Services Holiday Open House
The Heart Services Leadership team held a holiday open house on Wednesday, Dec. 22 on the 8th floor of the HAFS building. A good time was had by all – thank you to those of you who were able to stop by and celebrate the season with us!


COVID-19 Update
You can quickly access the latest Clinical Operations updates regarding COVID-19 as well as the most recent DUHS Leadership Virtual Town Hall recordings here: https://covid-19.dukehealth.org.
Reminder: All Duke University Health System (DUHS) and Private Diagnostic Clinic (PDC) team members, regardless of work location, are required to receive and provide documentation of a completed COVID-19 booster vaccination by 10 a.m. on Tuesday, Feb. 15, 2022, or within 28 days of their eligibility under CDC and state guidelines. More details are available in this email that was sent to all staff on Tuesday, Dec. 28.
Upcoming Events & Opportunities
Cardiology Grand Rounds
January 11: Telehealth to Improve Functional Status and Quality of Life in Veterans with Peripheral Artery Disease with Tony Gutierrez. 5 p.m. via Webex.
January 18: The Ultimate ‘Anti-Racism Statement’ Medicine Can Make is to Diversify its Ranks with Quinn Capers, IV of the University of Texas Southwestern Medical Center. 5 p.m. via Webex.
MLK Commemoration 2022
 Sunday, Jan. 16: How Long Must We Wait: Striving For the Beloved Community. The 2022 MLK keynote address will be given by historian and social activist, Keeanga-Yamahtta Taylor on Sunday, Jan. 16 at 3 p.m. at Duke Chapel. [UPDATE (1/14/22): This even will be virtual due to weather.] In addition, several community service opportunities are scheduled for the week of MLK Day. You can find more information about the main ceremony and service opportunities on the Duke MLK Commemoration website (https://mlk.duke.edu/). The Commemoration Service is free and open to the public. In accordance with Duke University COVID-19 mitigation policies, all guests must wear a mask at all times when indoors regardless of vaccination status. Parking will be available to all guests at the Bryan Center Garage free of charge.
Sunday, Jan. 16: How Long Must We Wait: Striving For the Beloved Community. The 2022 MLK keynote address will be given by historian and social activist, Keeanga-Yamahtta Taylor on Sunday, Jan. 16 at 3 p.m. at Duke Chapel. [UPDATE (1/14/22): This even will be virtual due to weather.] In addition, several community service opportunities are scheduled for the week of MLK Day. You can find more information about the main ceremony and service opportunities on the Duke MLK Commemoration website (https://mlk.duke.edu/). The Commemoration Service is free and open to the public. In accordance with Duke University COVID-19 mitigation policies, all guests must wear a mask at all times when indoors regardless of vaccination status. Parking will be available to all guests at the Bryan Center Garage free of charge.

Dzau Distinguished Lecture in Global Health
Wednesday, Jan. 26: Restoring Global Solidarity on the Road to Pandemic Recovery — A Conversation with Dr. Agnes Binagwaho and Dr. Paul Farmer. Noon – 1:30 p.m., Zoom. Registration required: https://bit.ly/3tbw7SM.
 Global health crises require global responses. But in the effort to control COVID-19, rising tides of nationalism have threatened collective action and deepened health inequities for many countries. In the face of these challenges to global health solidarity, the Duke Global Health Institute presents a probing discussion with two of the world’s preeminent global health experts – Dr. Agnes Binagwaho and Dr. Paul Farmer – on how the world failed to cooperate to fight the pandemic and how to chart a new vision to achieve health equity.
Global health crises require global responses. But in the effort to control COVID-19, rising tides of nationalism have threatened collective action and deepened health inequities for many countries. In the face of these challenges to global health solidarity, the Duke Global Health Institute presents a probing discussion with two of the world’s preeminent global health experts – Dr. Agnes Binagwaho and Dr. Paul Farmer – on how the world failed to cooperate to fight the pandemic and how to chart a new vision to achieve health equity.
This interactive webinar will span two continents, with our featured speakers appearing at the University of Global Health Equity in Butaro, Rwanda. Dr. Gavin Yamey, professor of the practice of global health and public policy, will moderate the conversation from Duke, fielding questions from the online audience. Attendees will join using Zoom webinar, space permitting.
Duke Well-Being Ambassador Virtual Course
January 11 – March 15: The Well-being Essentials for Learning Life-Balance (WELL-B) weekly webinar series begins January 11, 2022 at 3 p.m. EST. For only one hour a week for 10 weeks (with an optional 11th week for sharing content with colleagues), healthcare workers can learn about the science and practice of well-being from Dr. Bryan Sexton, Dr. Carrie Adair, and Dr. Kyle Rehder. These strategies can enhance your well-being, and through sharing, the well-being of your co-workers. Available to all Duke Health employees and those outside of Duke as well. More information: bit.ly/dukewellb. Offered by the Duke Center for Healthcare Safety and Quality.
Call for Applicants: 2022 AAMC Early-Career Women Seminar
The Department of Medicine and Program for Women in Internal Medicine (PWIM) are pleased to announce sponsorship for one faculty member to attend the in-person AAMC Early-Career Women Seminar on July 19-22, 2022. This popular and highly interactive seminar provides women at the assistant professor level with foundational leadership knowledge and skills to help achieve career goals and thrive as successful leaders in academic medicine and science. If interested in being considered for sponsorship, please send an email to Kimberly Dorman (kimberly.dorman@duke.edu) by January 31, 2022. Members of the office of the Vice-Chair for Faculty Development and Diversity (Drs. Laura Svetkey and Daniella Zipkin) will select one faculty member to nominate to attend and will notify the applicant by email.
Duke Research Week 2022
January 31 – February 4: Registration is now open for Duke Research Week 2022. Join us virtually for a week-long celebration of research underway at Duke! There is an excellent lineup of faculty lectures, panel discussions, “flash talks” with graduate students, trainees and postdoctoral fellows, and guest presenters for the Robert J. Lefkowitz, MD, Distinguished Lecture and Daubechies Lecture. Check out the full agenda here: https://dukeresearchweek.vfairs.com/en/#distinguishedlectures
National Wear Red Day
Friday, Feb. 4: National Wear Red Day. Help increase awareness of the impact cardiovascular disease has on all of us — wear red on Friday, Feb. 4! We would love to have individual and team photos of you sporting your awareness gear to share in Pulse!!
Newly Announced CME
April 23: Duke Sports Cardiology & Sudden Death in Athletes Symposium with course directors Jim Daubert and Bill Kraus. Virtual. For information or to register, contact Christy Darnell christy.darnell@duke.edu or 919-880-8686.
Postponed: Evening with Heart Benefitting Marfan
Due to the latest COVID surge, An Evening with Heart to benefit the Marfan Foundation has been postponed to Thursday, May 5. Location remains the same: The Maxwell in Raleigh, NC. The event will include a silent auction, cocktails, heavy hors d’oeuvres and entertainment. Proceeds will benefit The Marfan Foundation. For information please visit: https://bit.ly/3cHIBYD.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
December 19 — Svati Shah
Healio/Cardiology Today
AHA to fund research on long-term impact of COVID-19 on heart, brain health
https://bit.ly/33686Sa
December 22 — Manesh Patel
Medscape
Apixaban: The ‘Anticoagulant of Choice’ for AF
https://www.medscape.com/viewarticle/965390#vp_1
December 22 — Manesh Patel
tctMD
Correction Issued for Controversial Study Linking COVID-19 Vaccines to ACS Risk
https://bit.ly/3F8NQfR
December 26 — Harry Severance
ACEP eNow
Top 5 Articles of 2021: How the COVID-19 mRNA Vaccines Work, and Some Current Concerns
https://bit.ly/3zNl9nK
December 27 — Jennifer Rymer
Healio/Cardiology Today
Racial gap remains in invasive management for patients with MI with chronic kidney disease
https://bit.ly/3FaYzqa
December 30 — Sana Al-Khatib
Healio/Cardiology
The Take Home: AHA Scientific Sessions
https://bit.ly/3f2P5CL
December 30 — Tristram Bahnson
Healio/Cardiology Today
Catheter ablation outcomes in patients with AF vary by age: CABANA
https://bit.ly/3F7vITG
December 31 — Jennifer Rymer and Manesh Patel
HCP Live
The Best from AHA & TCT 2021 with Jennifer Rymer, MD
https://bit.ly/3F5xS65
Division of Cardiology Publications Indexed in PubMed December 16-22, 2021
Boakye E, Kwapong YA, Obisesan O, Ogunwole SM, Hays AG, Nasir K, Blumenthal RS, Douglas PS, Blaha MJ, Hong X, Creanga AA, Wang X, Sharma G. Nativity-Related Disparities in Preeclampsia and Cardiovascular Disease Risk Among a Racially Diverse Cohort of US Women. JAMA Netw Open 2021;4(12):e2139564. PM: 34928357.
Carnicelli AP, Owen R, Pocock SJ, Brieger DB, Yasuda S, Nicolau JC, Goodman SG, Cohen MG, Simon T, Westermann D, Hedman K, Andersson Sundell K, Granger CB. Atrial fibrillation and clinical outcomes 1 to 3 years after myocardial infarction. Open Heart 2021;8(2):e001726. PM: 34911791.
Fanaroff AC, Li S, Marquis-Gravel G, Giri J, Lopes RD, Piccini JP, Wang TY. Atrial Fibrillation and Coronary Artery Disease: A Long-Term Perspective on the Need for Combined Antithrombotic Therapy. Circ Cardiovasc Interv 2021;14(12):e011232. PM: 34932388.
Franklin JM, Platt R, Dreyer NA, London AJ, Simon GE, Watanabe JH, Horberg M, Hernandez A, Califf RM. When Can Nonrandomized Studies Support Valid Inference Regarding Effectiveness or Safety of New Medical Treatments? Clin Pharmacol Ther 2022;111(1):108-115. PM: 33826756.
Friedman DJ, Emerek K, Sørensen PL, Graff C, Loring Z, Jackson KP, Polcwiartek C, Singh JP, Kisslo J, Søgaard P, Atwater BD. Relationship Between Electrical and Mechanical Dyssynchrony and Outcomes Among Patients Undergoing Cardiac Resynchronization Therapy. Circ Arrhythm Electrophysiol 2021;14(12):e010217. PM: 34843407.
Fudim M, Wojdyla DM, Alexander JH, Goodman SG, Mehran R, Windecker S, Aronson R, Vinereanu D, Halvorsen S, Bahit MC, Granger CB, Lopes RD. Efficacy and Safety of Antithrombotic Therapy in Patients With Atrial Fibrillation, Recent Acute Coronary Syndrome, or Percutaneous Coronary Intervention and a History of Heart Failure: Insights From the AUGUSTUS Trial. J Am Heart Assoc 2021 Dec 21;10(24):e023143. PM: 34873913.
Fuery MA, Chouairi F, Natov P, Bhinder J, Rose Chiravuri M, Wilson L, Clark KA, Reinhardt SW, Mullan C, Miller PE, Davis RP, Rogers JG, Patel CB, Sen S, Geirsson A, Anwer M, Desai N, Ahmad T. Trends and Outcomes of Cardiac Transplantation in the Lowest Urgency Candidates. J Am Heart Assoc 2021;10(24):e023662. PM: 34743559.
Greene SJ, Butler J, Fonarow GC. Contextualizing Risk Among Patients With Heart Failure. JAMA 2021;326(22):2261-2262. PM: 34779819.
Hegde SM, Lester SJ, Solomon SD, Michels M, Elliott PM, Nagueh SF, Choudhury L, Zemanek D, Zwas DR, Jacoby D, Wang A, Ho CY, Li W, Sehnert AJ, Olivotto I, Abraham TP. Effect of Mavacamten on Echocardiographic Features in Symptomatic Patients With Obstructive Hypertrophic Cardiomyopathy. J Am Coll Cardiol 2021;78(25):2518-2532. PM: 34915982.
Kolupoti A, Fudim M, Pandey A, Kucharska-Newton A, Hall ME, Vaduganathan M, Mentz RJ, Caughey MC. Temporal Trends and Prognosis of Physical Examination Findings in Patients With Acute Decompensated Heart Failure: The ARIC Study Community Surveillance. Circ Heart Fail 2021;14(12):e008403. PM: 34702047.
Lunsford-Avery JR, Engelhard MM, Navar AM, Kollins SH. Author Correction: Validation of the Sleep Regularity Index in Older Adults and Associations with Cardiometabolic Risk. Sci Rep 2021;11(1):24398. PM: 34916542.
Lunyera J, Diamantidis CJ, Bosworth HB, Patel UD, Bain J, Muehlbauer MJ, Ilkayeva O, Nguyen M, Sharma B, Ma JZ, Shah SH, Scialla JJ. Urine tricarboxylic acid cycle signatures of early-stage diabetic kidney disease. Metabolomics 2021;18(1):5. PM: 34928443.
Marquis-Gravel G, Hammill BG, Mulder H, Roe MT, Robertson HR, Wruck LM, Sharlow A, Harris DF, Pohlman FW, Hernandez AF, Jones WS. Validation of Cardiovascular End Points Ascertainment Leveraging Multisource Electronic Health Records Harmonized Into a Common Data Model in the ADAPTABLE Randomized Clinical Trial. Circ Cardiovasc Qual Outcomes 2021;14(12):e008190. PM: 34886680.
Murray EM, Whellan DJ, Chen H, Bertoni AG, Duncan P, Pastva AM, Kitzman DW, Mentz RJ. Physical Rehabilitation in Older Patients Hospitalized with Acute Heart Failure and Diabetes: Insights from REHAB-HF. Am J Med 2022;135(1):82-90. PM: 34516959.
Ross M, Henao R, Burke TW, Ko ER, McClain MT, Ginsburg GS, Woods CW, Tsalik EL. A comparison of host response strategies to distinguish bacterial and viral infection. PLoS One 2021;16(12):e0261385. PM: 34905580.
Simon GE, Bindman AB, Dreyer NA, Platt R, Watanabe JH, Horberg M, Hernandez A, Califf RM. When Can We Trust Real-World Data To Evaluate New Medical Treatments? Clin Pharmacol Ther 2022;111(1):24-29. PM: 33932030.
Simon GE, Platt R, Watanabe JH, Bindman AB, John London A, Horberg M, Hernandez A, Califf RM. When Can We Rely on Real-World Evidence to Evaluate New Medical Treatments? Clin Pharmacol Ther 2022;111(1):30-34. PM: 33895994.
Singh AK, Carroll K, McMurray JJV, Solomon S, Jha V, Johansen KL, Lopes RD, Macdougall IC, Obrador GT, Waikar SS, Wanner C, Wheeler DC, Więcek A, Blackorby A, Cizman B, Cobitz AR, Davies R, DiMino TL, Kler L, Meadowcroft AM, Taft L, Perkovic V. Daprodustat for the Treatment of Anemia in Patients Not Undergoing Dialysis. N Engl J Med 2021;385(25):2313-2324. PM: 34739196.
Singh AK, Carroll K, Perkovic V, Solomon S, Jha V, Johansen KL, Lopes RD, Macdougall IC, Obrador GT, Waikar SS, Wanner C, Wheeler DC, Więcek A, Blackorby A, Cizman B, Cobitz AR, Davies R, Dole J, Kler L, Meadowcroft AM, Zhu X, McMurray JJV. Daprodustat for the Treatment of Anemia in Patients Undergoing Dialysis. N Engl J Med 2021;385(25):2325-2335. PM: 34739194.
Watanabe JH, Simon GE, Horberg M, Platt R, Hernandez A, Califf RM. When Are Treatment Blinding and Treatment Standardization Necessary in Real-World Clinical Trials? Clin Pharmacol Ther 2022;111(1):116-121. PM: 33829639.
Division of Cardiology Publications Indexed in PubMed Dec 23, 2021-Jan 5, 2022
Ariss RW, Minhas AMK, Issa R, Ahuja KR, Patel MM, Eltahawy EA, Michos ED, Fudim M, Nazir S. Demographic and Regional Trends of Mortality in Patients With Acute Myocardial Infarction in the United States, 1999 to 2019. Am J Cardiol 2022;164:7-13. PM: 34857365.
Bekfani T, Hamadanchi A, Ijuin S, Bekhite M, Nisser J, Derlien S, Westphal J, Bogoviku J, Morris DA, Fudim M, Braun-Dullaeus RC, Möbius-Winkler S, Schulze PC. Relation of left atrial function with exercise capacity and muscle endurance in patients with heart failure. ESC Heart Fail 2021;8(6):4528-4538. PM: 34726343.
Breathett KK, Xu H, Sweitzer NK, Calhoun E, Matsouaka RA, Yancy CW, Fonarow GC, DeVore AD, Bhatt DL, Peterson PN. Is the affordable care act medicaid expansion associated with receipt of heart failure guideline-directed medical therapy by race and ethnicity? Am Heart J 2022;244:135-148. PM: 34813771.
Chew DS, Li Z, Steinberg BA, O’Brien E, Pritchard J, Bunch TJ, Mark DB, Patel MR, Nabutovsky Y, Greiner MA, Piccini JP. Association between economic and arrhythmic burden of paroxysmal atrial fibrillation in patients with cardiac implanted electronic devices. Am Heart J 2022;244:116-124. PM: 34800369.
Do WL, Nguyen S, Yao J, Guo X, Whitsel EA, Demerath E, Rotter JI, Rich SS, Lange L, Ding J, Van Den Berg D, Liu Y, Justice AE, Guan W, Horvath S, Assimes TL, Bhatti P, Jordahl K, Shadyab A, Valencia CI, Stein AD, Smith A, Staimez LR, Conneely K, Narayan K. Associations between DNA methylation and BMI vary by metabolic health status: a potential link to disparate cardiovascular outcomes. Clin Epigenetics 2021;13(1):230. PM: 34937574.
Fudim M, Borges-Neto S. Utility of diastolic dyssynchrony in the setting of cardiac resynchronization therapy. J Nucl Cardiol 2021;28(6):2644-2646. PM: 31512196.
Gaudino M, Di Franco A, Alexander JH, Bakaeen F, Egorova N, Kurlansky P, Boening A, Chikwe J, Demetres M, Devereaux PJ, Diegeler A, Dimagli A, Flather M, Hameed I, Lamy A, Lawton JS, Reents W, Robinson NB, Audisio K, Rahouma M, Serruys PW, Hara H, Taggart et al. Sex differences in outcomes after coronary artery bypass grafting: a pooled analysis of individual patient data. Eur Heart J 2021;43(1):18-28. PM: 34338767.
Goldstein SA, Krasuski RA. Pulmonary Hypertension in Adults with Congenital Heart Disease. Cardiol Clin 2022;40(1):55-67. PM: 34809917.
Huang MN, D’Anniballe VM, Gunn MD. Monocytes as a Cellular Vaccine Platform to Induce Antitumor Immunity. Methods Mol Biol 2022;2410:627-647. PM: 34914073.
Krasuski RA. Pulmonary Hypertension. Cardiol Clin 2022;40(1):xi-xii. PM: 34809921.
Pagidipati NJ, Phelan M, Page C, Clowse M, Henao R, Peterson ED, Goldstein BA. The importance of weight stabilization amongst those with overweight or obesity: Results from a large health care system. Prev Med Rep 2021;24:101615. PM: 34976671.
Recent Comments