Home » 2022
Yearly Archives: 2022
Duke Heart Pulse week ending December 18th 2022
Highlights of the week:
Duke Heart Welcomes Two New Family Members
What better way to kick off holiday celebrations than by celebrating two new Duke Heart family members? That’s what we’re doing this week!
Congratulations to Joey Harrington and Thomas Rose on the birth of their son, Harry Rose, on Dec. 9. He weighed in at 7 lbs, 15 oz.


And congratulations to Dennis & Sara Lynne Narcisse who welcomed their third child, Leo Lane, on Dec. 14. “Mom and baby are doing well and his older twin brothers, Tripp and Henry, are anxiously awaiting to meet him at home!”

They are gorgeous and we are so happy for both families!
SCMR Publishes First Training Recs for CMR Techs
The Society for Cardiovascular Magnetic Resonance (SCMR) has recently issued their first framework to define the knowledge, experience and skills required for a technologist to be competent in cardiovascular magnetic resonance (CMR) imaging. The international team of authors include three members of Duke’s Cardiovascular MRI team: Raymond Kim, MD; Stephen Darty, BSRS, RT-N, MR, and Elizabeth Jenista, PhD.
In drawing up their recommendations, the authors sought to address the following:

-
-
- Significant regional variations in CMR service delivery.
-
- The need for competent and well-trained CMR technologists, as they are fundamental to the success of CMR programs. The current limited availability of CMR technologists is a challenge for CMR adoption more widely into clinical care.
- Guidelines and/or formal education in CMR imaging for magnetic resonance (MR) technologists are neither widely available nor standardized worldwide.
The SCMR recommendations were published Dec. 5, 2022 in the Journal of Cardiovascular Magnetic Resonance.
This is a terrific accomplishment for our Duke authors and speaks to our team’s dedication to advancing the use of CMR. Well done and congratulations!
Bloomfield Presents at AKUPI-NCD Research Symposium
Gerald S. Bloomfield, MD, MPH was invited to speak on Research Methodology Experience in Non-Communicable Diseases as part of the Aga Khan University Pakistan Initiative for Non-Communicable Diseases (AKUPI-NCD) Research Symposium: Landscape of Research in Pakistan. The symposium represents the first nation-wide initiative to bring together researchers from multiple disciplines and backgrounds focused on NCDs, from across Pakistan as well as international partners. This event was held in Karachi, Pakistan, Dec. 5-6, 2022.


AKUPI-NCD was created to address a critical gap in the response to the NCD epidemic. The Aga Khan University partnered with Duke University to design a comprehensive, integrated, multi-disciplinary training program to prepare the next generation of leaders in NCD research. The program, focused on cardiovascular and cerebrovascular diseases and their shared risk factors, is funded by a research training grant by the U.S. National Institutes of Health via the Fogarty International Center.
AKUPI-NCD is led by principal investigator (PI) Dr. Zainab Samad, the Ibn-e-Sina endowed Professor and chair of the Dept. of Medicine at Aga Khan University in Karachi. Additional PIs include Drs. Aysha Almas (AKU), Ayeesha Kamal (AKU) and Gerald Bloomfield.
Pictured here are Gerald Bloomfield, Zainab Samad, Adil Haider, Dean of the AKU School of Medicine, and a number of NCD researchers from across Pakistan at the Symposium Dinner event. Participants were gifted a Topi hat and Ajarak shawl/scarf.
Dr. Samad also shows off her selfie skills with Dr. Adil Haider (AKU Dean, SOM) and Gerald Bloomfield on the AKU campus in Karachi.
Great work!

Loring Invited to PACE Editorial Board
Congratulations to Zak Loring! He has been invited to serve on the Pacing and Clinical Electrophysiology (PACE) Editorial Board. His term will run three years.
“This is pretty impressive for an assistant professor who joined our faculty less than six months ago,” said Jon Piccini, Director, Cardiac Electrophysiology.
We concur! This is great news, Zak!
Ngeno Selected for 2023 LEADER Cohort
The School of Medicine Office for Faculty recently announced their 2023 LEADER participants.
 The Leadership Development for Researchers (LEADER) Program is designed for junior faculty who are leading a research group and driving their own research agenda. The course provides insight into leadership and team building as well as direction on how to develop and manage a scientific laboratory or research program, how to improve productivity, and how to harness creativity and innovation. The program was developed to bridge the gap between the scientific expertise that led individuals to a career in academic medicine, and the management skills that will be required to succeed as the leaders of small business units.
The Leadership Development for Researchers (LEADER) Program is designed for junior faculty who are leading a research group and driving their own research agenda. The course provides insight into leadership and team building as well as direction on how to develop and manage a scientific laboratory or research program, how to improve productivity, and how to harness creativity and innovation. The program was developed to bridge the gap between the scientific expertise that led individuals to a career in academic medicine, and the management skills that will be required to succeed as the leaders of small business units.
Among the 23 members of the cohort is our very own Gedion Ngeno. Congratulations, Titus!!!
Shout-out to STEMI Team
A big shout-out to our STEMI team, especially Larry Crawford, Caitlyn Dresher, Nadia, Gordon, Rebecca, and Brad — who were recently involved in the care of a patient who was brought to us shortly after collapsing during a Duke men’s basketball game. The family is deeply appreciative for the great care their loved one received.
We have an incredible STEMI team and together, we do amazing things for our community and visitors to our area. Way to go!
Wang Celebrated During CGR
 Thanks to everyone who joined us via Webex on Tuesday evening to celebrate Tracy Wang, MD. It was great to revisit the work she has done over the years, and to hear about it through the comments of several mentees and colleagues who know her best!
Thanks to everyone who joined us via Webex on Tuesday evening to celebrate Tracy Wang, MD. It was great to revisit the work she has done over the years, and to hear about it through the comments of several mentees and colleagues who know her best!
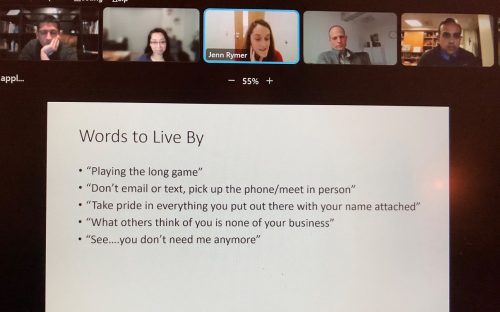
Former mentees Jake Doll and Jenn Rymer started off the hour. Doll gave us some background on how the ARTEMIS trial got its name and we learned that no detail is too small for Wang. Among the many things he and Rymer learned under Wang is that clarity is the highest virtue – and anything worth writing is worth writing well. Rymer shared her gratitude for Wang’s guidance along with some ‘words to live by’ which are included in the image here.
Pam Douglas, Jason Katz, Manesh Patel, Adrian Hernandez, Terry Fortin, Kristin Newby, Nishant Shah, and Mitch Krucoff each contributed across the evening, which culminated in comments from Wang, who thanked all of us for 20 years of fun, friendship, and life-changing moments.
It was a fitting and well-deserved tribute to Wang and her legacy at Duke. Great job, Nishant and Jenn for planning this special session of Grand Rounds!
Some Pictures from the week:
Holiday Party pics and Matt Brennan helping clean up at the THA office after a “near miss’ with some Soda.



Additional Reminders:
- Thank you for all you do to keep everyone safe and healthy. Please remain vigilant with masking, hand hygiene, PPE, and other safe behaviors to prevent the spread of infection. Please pay special attention to the proper wearing and securing of gowns and be mindful of PPE compliance.
- Pulse is taking a break for two weeks and will return on Jan. 8, 2023. Enjoy the holidays!
Upcoming Events & Opportunities
Cardiology Grand Rounds
Dec. 20: TTR Amyloidosis: Recognizing that it’s Not Uncommon with Dr. Michel Khouri. Webex.
Dec. 27: No CGR this week. Happy holidays!
Jan. 10: Our guest speaker will be Dr. Larry Jackson. Zoom. 5 p.m.
CME & Other Events
Dec. 19: PDC Annual Member Meeting. 5:30-6:30 p.m. Zoom.
The meeting will be recorded and posted the following day. Submit questions to: PDC-President@dm.duke.edu. Agenda items will include:
- Financial Year In Review
- Review of Retirement Portfolio Performance from CAPTRUST
- The Path Forward for 2023: Duke Health Integrated Practice
- Anticipated Member Asset Distribution Plan
February is Heart Month
Feb. 3: National Wear Red Day. We encourage everyone to wear red on Friday, Feb. 3 to show our support for heart health overall, but especially to support women and cardiovascular disease awareness.

Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
December 6 — Nishant Shah
Healio/Cardiology
Bromocriptine appears to drop BP, improve arterial stiffness in teens with type 1 diabetes
https://duke.is/zrkjq
December 12 — Duke Health/Duke Heart
Becker’s Hospital Review
28 moves from top US heart centers in 2022
https://duke.is/8gk7k
December 13 — Christopher O’Connor
Medpage Today
Omecamtiv Mecarbil Not Ready for Prime Time, FDA Advisors Say
https://duke.is/gqd2m
December 14 — Joseph Turek & the Sinnamon family
WAFB-BTR (CBS News 9/Baton Rouge, LA)
Heart transplant makes medical history
(*clip begins @ 05:49:43)
https://duke.is/23j6e
December 14 — Pamela Douglas
tctMD
Bullying in Cardiology: Has More Diversity Led to Backlash?
Division of Cardiology Publications Indexed in PubMed December 8-13, 2022
Abtan J, Bhatt DL, Elbez Y, Ducrocq G, Goto S, Smith SC, Ohman EM, Eagle KA, Fox K, Harrington RA, Leiter LA, Mehta SR, Simon T, Petrov I, Sinnaeve PR, Pais P, Lev E, Bueno H, Wilson P, Steg PG. External applicability of the Effect of ticagrelor on Health Outcomes in diabEtes Mellitus patients Intervention Study (THEMIS) trial: An analysis of patients with diabetes and coronary artery disease in the REduction of Atherothrombosis for Continued Health (REACH) registry. Int J Cardiol 2023 Jan 1;370:51-57. PM: 36270493.
Butler J, Usman MS, Anstrom KJ, Blaustein RO, Bonaca MP, Ezekowitz JA, Freitas C, Lam CSP, Lewis EF, Lindenfeld J, McMullan CJ, Mentz RJ, O’Connor C, Rosano GMC, Saldarriaga CI, Senni M, Udelson J, Voors AA, Zannad F. Soluble guanylate cyclase stimulators in patients with heart failure with reduced ejection fraction across the risk spectrum. Eur J Heart Fail 2022 Nov;24(11):2029-2036. PM: 36250238.
Chunawala ZS, Qamar A, Arora S, Pandey A, Fudim M, Vaduganathan M, Mentz RJ, Bhatt DL, Caughey MC. Prognostic significance of obstructive coronary artery disease in patients admitted with acute decompensated heart failure: the ARIC study community surveillance. Eur J Heart Fail 2022 Nov;24(11):2140-2149. PM: 35851711.
Friedman DJ, Pierre D, Wang Y, Gambone L, Koutras C, Segawa C, Farb A, Vemulapalli S, Varosy PD, Masoudi FA, Lansky A, Curtis JP, Freeman JV. Development and validation of an automated algorithm for end point adjudication for a large U.S. national registry. Am Heart J 2022 Dec;254:102-111. PM: 36007567.
Greene SJ, Goto D, Wang D, Hilkert R, Lautsch D, Fonarow GC. Outpatient versus inpatient intravenous diuretic therapy for heart failure in the United States. Eur J Heart Fail 2022 Nov;24(11):2199-2202. PM: 36334074.
Kaolawanich Y, Azevedo CF, Kim HW, Jenista ER, Wendell DC, Chen EL, Parker MA, Judd RM, Kim RJ. Native T1 Mapping for the Diagnosis of Myocardial Fibrosis in Patients With Chronic Myocardial Infarction. JACC Cardiovasc Imaging 2022Dec;15(12):2069-2079. PM: 36481075.
Kapur NK, Kim RJ, Moses JW, Stone GW, Udelson JE, Ben-Yehuda O, Redfors B, Issever MO, Josephy N, Polak SJ, O’Neill WW. Primary left ventricular unloading with delayed reperfusion in patients with anterior ST-elevation myocardial infarction: Rationale and design of the STEMI-DTU randomized pivotal trial. Am Heart J 2022 Dec;254:122-132. PM: 36058253.
Kester KM, Hatton J, Kelly J, Carroll M, Lindsay M, Jordan N, Fuchs MA, Patel MR, Engel J, Granger B. Moving nursing innovation to prime time through the use of creative partnerships. Nurs Outlook 2022 ;70(6):820-826. PM: 36154773.
Longo de Oliveira ALM, de Oliveira Pereira RF, Agati LB, Ribeiro CM, Kawamura Suguiura GY, Cioni CH, Bermudez M, Pirani MB, Caffaro RA, Castelli V, Resende Aguiar VC, Volpiani GG, Paschoa A, Scarlatelli Macedo AV, de Barros E Silva PGM, de Campos Guerra JC, Fareed J, Lopes RD, Ramacciotti E. Rivaroxaban Versus Enoxaparin for Thromboprophylaxis After major Gynecological Cancer Surgery: The VALERIA Trial : Venous thromboembolism prophylxis after gynecoogical plvic cancer surgery with varoxaban versus enoxparin (VALERIA trial). Clin Appl Thromb Hemost 2022;28:10760296221132556. PM: 36474344.
Mori M, Mark DB, Khera R, Lin H, Jones P, Huang C, Lu Y, Geirsson A, Velazquez EJ, Spertus JA, Krumholz HM. Identifying quality of life outcome patterns to inform treatment choices in ischemic cardiomyopathy. Am Heart J 2022 Dec;254:12-22. PM: 35932911.
Murray EM, Greene SJ, Rao VN, Sun JL, Alhanti BA, Blumer V, Butler J, Ahmad T, Mentz RJ. Machine learning to define phenotypes and outcomes of patients hospitalized for heart failure with preserved ejection fraction: Findings from ASCEND-HF. Am Heart J 2022 Dec;254:112-121. PM: 36007566.
Nardin M, Pivato CA, Cao D, Sartori S, Zhang Z, Vogel B, Nicolas J, Chiarito M, Qiu H, Chandrasekhar J, Spirito A, Abizaid A, Christiansen EH, Colombo A, de Winter RJ, Haude M, Jakobsen L, Jensen LO, Krucoff MW, Landmesser U, Saito S, Suryapranata H, De Luca G, Dangas G, Mehran R. The mega COMBO collaboration: An individual patient data pooled analysis of patients undergoing PCI with COMBO stent. Int J Cardiol 2023 Jan 1;370:149-155. PM: 36270496.
Nelson AJ, Inohara T, Rao SV, Kaltenbach LA, Wojdyla D, Wang TY. Comparing the Classification of Percutaneous Coronary Interventions Using the 2012 and 2017 Appropriate Use Criteria: Insights From 245,196 Patients in the NCDR CathPCI Registry. Am Heart J 2023 Jan;255:117-124. PM: 36220357.
Rosario KF, Brezitski K, Arps K, Milne M, Doss J, Karra R. Cardiac Sarcoidosis: Current Approaches to Diagnosis and Management. Curr Allergy Asthma Rep 2022 Dec;22(12):171-182. PM: 36308680.
Rymer JA, Kirtane AJ, Farb A, Malone M, Jaff MR, Seward K, Stephens D, Barakat MK, Krucoff MW. One-Year Follow-Up of Vascular Intervention Trials Disrupted by the COVID-19 Pandemic: A Use-Case landscape. Cardiovasc Revasc Med 2022 Dec;45:67-73. PM: 35953406.
Schwartz FR, Daubert MA, Molvin L, Ramirez-Giraldo JC, Samei E, Marin D, Tailor TD. Coronary Artery Calcium Evaluation Using New Generation Photon-counting Computed Tomography Yields Lower Radiation Dose Compared With Standard Computed Tomography. J Thorac Imaging 2023 Jan 1;38(1):44-45. PM: 36490311.
Duke Heart Pulse – December 11th 2022
Highlights of the week:
Gutierrez Named Durham VA Cath Lab Director
Antonio Gutierrez, MD, has been named Cardiac Catheterization Lab Director at the Durham Veterans Affairs Medical Center (VAMC). The position was effective as of Dec. 1.

Gutierrez is a nationally-recognized academic interventional cardiologist specializing in the management of coronary and peripheral arterial disease. He is the recipient of a highly prestigious VA Career Development Award, which provides five years of protected federal research funding and support. During this time, Gutierrez is focusing on the development and implementation of a virtual, home-based, supervised exercise therapy program for Veterans with peripheral arterial disease.
Gutierrez currently serves on the editorial board of Circulation: Cardiovascular Interventions. He has consistently shown excellent leadership skills, having previously served as a Duke Chief Resident, received the 2018 CRT Young Leadership Award, and participated in the 2021 ACC Emerging Faculty Leadership Academy.
He completed internship and residency training at Duke; cardiology and vascular medicine fellowships at Brigham & Women’s Hospital, and interventional fellowship at Duke prior to joining the Duke and Durham VA faculty in 2017. Gutierrez is taking over this role from Rajesh Swaminathan, MD, who will now focus on leadership responsibilities as Section Chief and with Regional VISN-6, the VA Mid-Atlantic Health Care Network.
In this new role, Dr. Gutierrez will build on VAMC Cath lab innovation, focus on Cath lab staff education, and continue to expand the robust site-based research program.
Congratulations, Tony!
This week: CGR Celebrates Tracy Wang, MD
Be sure to join us on Tuesday evening, Dec. 13 at 5 p.m. via Webex. We’ll celebrate Tracy Wang, MD, who is now serving as Chief of Comparative Effectiveness Research at the Patient Centered Outcomes Research Institute (PCORI).

Shout-out to 7W, 6E Team Members
A big shout-out this week to members of our Duke Heart team. We received the following message from Lisa Clark Pickett, Chief Medical Officer, Duke University Hospital, in follow-up to a patient compliment.
“Greetings, Heart Team!
We received this glowing compliment about the Heart Team and our awesome (general surgery) resident, Holly Lewis! Thank you all for your commitment to excellence, compassion, and efficiency! I was so impressed! I hope that you will share this, personally, with the heart nurses, as I do not have their last names listed to allow me to thank them in this email!
You are all living out Duke Values so visibly, and for that I am most thankful.
Best wishes to you all for a lovely holiday season.” –Lisa
“Excellent care from admission to discharge. Everyone was courteous and professional, from admitting, Pre-op, OR, ICU, nursing, and the physicians. In 7 West, Darby and Gil, and on 6 East, Brooke, Leah, Marjorie, Amanda, Scott, Taylor Q, Demetria were all fantastic. Extra special thanks to Nurses David and Lena who took care of me for 3 days! They were incredible and I really appreciated how comfortable they made my stay. Also want to thank Dr. Holly Lewis for expediting my discharge. She personally walked me down to X-ray twice to help get my chest tube out ASAP!” — a grateful patient (name withheld for privacy)
“Outstanding, team! Thanks so much!” — Chantal Howard, Chief Nursing & Patient Care Services Officer, Duke University Hospital
You all continue to make a great impression on our patients — keep up the excellent work!
Ulrich Departing DUHS at Year End
The upcoming departure of Kate Ulrich was shared earlier this week in a Leadership Update. The announcement was made by Mary Ann Fuchs, Vice President of Patient Care and System Chief Nurse Executive and Clif Flintom, Service Line Vice President of Perioperative Services for Duke  University Health System
University Health System
“Dear Colleagues,
With mixed feelings, we announce that Kate Ulrich, MS, BSN, RN, NEA-BC, is leaving her position as assistant vice president of Perioperative Nursing at DUHS to take a leadership role at Tampa General Hospital in Tampa, Florida. In her new role, Kate will serve as senior vice president of perioperative services at Tampa General Hospital, a 1,040-bed hospital and one of the largest hospitals in Florida.
Kate has been at DUHS since 2011 and has held positions with increasing levels of responsibility, including her current role as the first AVP for DUHS Perioperative Nursing. Kate is proud of being a strong advocate of the nursing profession and advancing nursing practice across perioperative services. Her advocacy for nursing has influenced perioperative practice standards across DUHS, improving the quality and safety of patient care.
She begins her new position in mid-January and will remain at DUHS until Dec. 31. Tara Walczak-Daege, DNP, RN, NE-BC, CNOR, associate chief nursing officer, Duke Raleigh Hospital, will cover Kate’s role until a permanent replacement is found.
Kate is known as an advocate for patients and leaves behind a legacy of always putting the patient first. She and her team of more than 700 staff provided clinical and administrative operations that supported over 79,000 surgeries and procedures in the most recently completed fiscal year across DUHS’s surgical platforms, ambulatory surgery centers and peri-anesthesia care units.
Kate has been a tremendous leader as Perioperative Services has transformed from a single-entity service line to a health system service line encompassing acute care and ambulatory surgery platforms across multiple campuses. We are grateful for the many contributions she has made to DUHS nursing and Perioperative Services.
Please join us in congratulating Kate on this exciting new phase of her career and thank her for all she has done to serve our patients and teams.”
Kate has been an important partner to the Duke Heart team – especially our surgical teams– and a wonderful colleague. We wish her all the best!
Reminder: ORA Holiday Deadlines
The Office of Research Administration (ORA) will operate with a reduced staff during the holiday season to allow team members time to recharge. To help ORA respond as timely as possible to your needs, please plan in advance based on the following:
Last two weeks of December
For any transactions with due dates between December 19 – January 2, please have submitted in ready-form to ORA by Thursday, December 15 to ensure there is adequate time and staffing to respond to your needs.
Please note: the next NIH SBIR/STTR deadline is Jan. 5, 2023, and the internal deadline is 8 a.m. on Dec. 28, 2022. Because this deadline falls in the last two weeks in December when ORA will be operating with reduced staff and because these award mechanisms are usually complex and require careful institutional coordination before submission:
- Please complete Intent to Submit for all planned SBIR/STTR applications no later than Dec. 5, 2022; and
- Please plan to route a submission-ready application no later than Dec. 15, 2022; if more time is needed, please submit a late waiver request so that ORA can plan for appropriate coverage to support these applications.
For anything submitted in the last two weeks of December that can wait until after the holiday break, ORA will be back up to speed with a full team on Jan. 3, 2023 and will look forward to managing all pending issues at that time.
Additional Reminders:
- We’re seeing improvements with PPE throughout DUH – great job! It is vital that we all remain vigilant with masking, hand hygiene, PPE, and other safe behaviors to prevent the spread of infection. Please pay special attention to the proper wearing and securing of gowns and be mindful of PPE compliance. Thank you for all you do to keep everyone safe and healthy.
- Next week will be our final Pulse of 2022! We’ll break for two weeks and return on Jan. 8, 2023!
Upcoming Events & Opportunities
Cardiology Grand Rounds
Dec. 13: Celebration for Dr. Tracy Wang. 5 p.m. Webex.
Dec. 20: Our featured speaker will be Dr. Michel Khouri. Webex.
Dec. 27: No CGR this week.
CME & Other Events
Dec. 19: PDC Annual Member Meeting. 5:30-6:30 p.m. Zoom.
The meeting will be recorded and posted the following day. Submit questions to: PDC-President@dm.duke.edu. Agenda items will include:
- Financial Year In Review
- Review of Retirement Portfolio Performance from CAPTRUST
- The Path Forward for 2023: Duke Health Integrated Practice
- Anticipated Member Asset Distribution Plan
Call for abstracts: 2023 Duke Health Quality and Safety Conference
The virtual poster submission period for the 2023 Duke Health Quality and Safety Conference is now open. The deadline for submission is Wednesday, Dec. 14. The 2023 Conference will be held the weeks of March 13 and 20, with an in-person event on Thursday, March 23.
For more information and to submit your abstract, please click here.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
November 27 — Soderblom family
Monroe (NC) Enquirer Journal
Monroe ‘miracle’ baby receives rare partial heart transplant
https://duke.is/9wkrp
December 5 — Amy Berkman (pediatrics)
Health Thoroughfare
Young Cancer Survivors See Higher Risk of Cardiovascular Disease
https://duke.is/vr9vt
December 5 — Amy Berkman
Medicalxpress.com
https://duke.is/zb6bn
December 5 — Amy Berkman
HealthDay
CVD Risk Increased for Adolescent, Young Adult Cancer Survivors
https://duke.is/8fvqb
December 7 — Duke Health
Becker’s Hospital Review
42 cardiology firsts in 2022 (see 14, 36)
https://duke.is/4y84j
December 8 — Pamela Douglas
Fox News
Bullies in white coats? ‘Too many’ health care workers experience toxic workplaces, studies show
https://duke.is/nu9sq
December 8 — Richard Krasuski
ABC News
Doctors should ask heart patients if they take supplements to manage heart failure
https://duke.is/bf6ar
December 8 — Pamela Douglas
New York Post
Health care workers treating each other ‘disrespectfully’ on the rise
https://duke.is/2jkfn
December 8 — Stephen Greene
tctMD
Sequencing HF Meds? Most Doctors Stick to Old Habits, Survey Says
https://duke.is/g4wq8
December 8 — Manesh Patel
Medpage Today
TAVR at 20: How Much Longer Will Medicare Mandate a Registry?
https://duke.is/vsdwc
Duke Heart Pulse – December 4th 2022
Chief’s message: Welcome to our New Cardiology Fellows and Ongoing Work to do around Heart Disease.
As we approach the final month of the year, this week we were excited to welcome our next fellowship class to Duke. These are the next generation of leaders that will help us continue to discover and deliver heart health. We were also excited to have some end of year meetings with the CVCT (CardioVascular Clinical Trials) conference with several Duke Faculty and Fellows presenting. Lots more work to do to ensure our evidence generation system improves to include more patients, work faster to get answer to patients and groups that need it the most. It was again great to see some rising stars around the country in clinical research and heart from leaders like Dr. Califf from the FDA.

We also have had the start of the BacktoHeart22 Cardiology conference which is a Hybrid Medscape conference (in-person and Virtual) summarizing the years lessons in CV medicine. This conference led by Bob Harrington and Fatima Rodriquez from Stanford and feature several interactive sessions. The conference started this AM with a powerful survivor story from Bob Harper (Fitness Expert and Host of the Biggest Loser) who shared his near fatal Acute Heart Attack story. He shared that bystander CPR and cardiac rehab after angioplasty and stent for his AMI saved his life. He also shared the work he is doing to increase awareness around Lp(a) levels.

So through all our challenges and work to ensure access to healthcare, as the year comes to an end we are reminded about the significant work we still have to do to bend the curve on cardiovascular death and disability around the world and in our local communities.
Highlights of the week:
Incoming Cardiology Fellows Announced
We are excited to share with you the new members of our cardiology fellowship class starting in July, 2023. They are:
Jawan Abdulrahim 
Residency: Duke
Medical School: UAB
Aubrie Carroll
Residency: Duke
Medical School: University of Virginia
Jonathan Hanna
Residency: Yale
Medical School: Yale
Seamus Hughes
Residency: UTSW
Medical School:
John Hopkins
Damarcus Ingram
Residency: Duke
Medical School: Drexel
Ivan Nenadic Wood
Residency: Michigan
Medical School: Mayo
Josh Rushakoff
Residency: Cedars Sinai
Medical School: UC San Francisco
Husam Salah
Residency: Arkansas
Medical School: Jordan University
Aarti Thakkar
Residency: John Hopkins
Medical School: Duke
Eric Xie
Residency: Johns Hopkins
Medical School: John Hopkins
Anna Lisa Chamis would like to especially thank Manesh Patel, Camille Frazier Mills, Neha Pagidipati, Chris Holley, Rob Mentz and Chris Wrobel along with the fellowship recruitment committee, faculty interviewers and all the fellows for their time and efforts to recruit this amazing incoming class. In addition, Anna Lisa would like to thank Kayla Humphreys and Brianna Small for effectively and efficiently managing the administrative aspect of this virtual recruitment season.
We look forward to welcoming this outstanding team of fellows in July. Great job, everyone!
Shout-out: Outstanding Week for Duke EP Team
A big shout-out this week to Duke’s EP team. Way to go!
“I just wanted to recognize everyone on the invasive labs team (including Cath & CVSSU) for orchestrating the most number of cases completed in a single day ever by the DUH EP Lab! Thank you for the Herculean effort by our incredible team,” Shawn Johnson, Assistant Nurse Manager, Adult Electrophysiology Lab.
On Dec. 1, the team completed 17 cases, including four Outpatient Tilt, seven Outpatient Devices, four Outpatient Ablations, one Inpatient Device, and 1 Inpatient Ablation.
“Sometimes we do special things and they go unnoticed. This should not. While the number of cases itself is not necessarily important, the cooperation, collaboration, and commitment required of the whole team to accomplish this milestone is truly impressive,” said Jonathan Piccini, MD, director of Cardiac Electrophysiology. “Thank you for your leadership and thanks to every member of the team that enabled this to happen – particularly on a day in which we were understaffed and short-handed. Our patients get the best because we have the best team.”
“Dr. Piccini said it so well. Kudos and thanks to the EP team for their tremendous dedication and talent, added Jill Engel, DNP, Service Line Vice President for Duke Heart. “We appreciate everything you do and are fortunate to have each of you on team Duke Heart!”
Scientific Sessions Twitter Space Link Now Available
As we mentioned previously in Pulse, Manesh Patel and Kelly Arps were the featured guests in a Twitter Space held Tuesday, Nov. 8 on Twitter. Patel and Arps did a recap of some of the most notable findings presented at Scientific Sessions. That link was made available to us this week. To check it out, please visit: https://duke.is/jq953.
Pickett Leaving as DUH CMO; Becoming Hospice & Palliative Care Fellow
Earlier this week we learned that Duke University Hospital Chief Medical Officer Lisa Pickett, MD will leave her role in 2023. She has been accepted into the Duke Hospice and Palliative Care Fellowship program. The announcement was made earlier this week by Tom Owens and Mary Martin:
It is with mixed emotions that we share the news that Dr. Lisa Pickett, FACS, has been accepted into the Duke Hospice and Palliative Care Fellowship program, beginning in July 2023. In pursuit of this next phase of her career, Lisa will step back from her current role as Chief Medical Officer for Duke University Hospital. The transition will take place in Spring 2023, and we will share more details as they are confirmed.
 So many of us at Duke University Hospital, and across the entire Duke community, have been touched by Lisa’s compassionate care and servant leadership. As the hospital’s first female Chief Medical Officer, Lisa has shaped the role of hospital physicians at Duke and has supported our teams through more than ten years of transformational change.
So many of us at Duke University Hospital, and across the entire Duke community, have been touched by Lisa’s compassionate care and servant leadership. As the hospital’s first female Chief Medical Officer, Lisa has shaped the role of hospital physicians at Duke and has supported our teams through more than ten years of transformational change.
As a member of the DUH Senior Leadership team, Lisa has helped develop the Health System Disruptive Patient and Visitor Policy, coordinated patient moves for both DMP and DCT, and worked to create an environment of gratitude and appreciation among our teams.
Throughout her career, Lisa’s passion for caring for our patients and families during their most difficult care journeys has always been evident. This will serve her very well in this next professional opportunity.
Lisa will join the Palliative Care Fellow class in July and so will continue her time with our Duke family. For those who may not know, Lisa began her career at Duke as an Intern and then a Resident in General Surgery in 1994. She subsequently completed a Fellowship in Critical Care and joined our faculty where she currently serves as Assistant Professor of Surgery and Critical Care.
Lisa also worked at Duke Regional Hospital, where she helped build a general surgery program and a 24/7 Critical Care service. She served as Chief Medical Officer at DRH for three years before beginning her current role as Duke University Hospital Chief Medical Officer in 2012.
We will share our plans for identifying our next Chief Medical Officer in the coming weeks. For now, please join us as we congratulate Lisa on this exciting new phase of her career and thank her for all she has done as a leader in our hospital and throughout the Duke community. Thank you, Lisa!
Reminder: ORA Holiday Deadlines
The Office of Research Administration (ORA) will operate with a reduced staff during the holiday season to allow team members time to recharge. To help ORA respond as timely as possible to your needs, please plan in advance based on the following:
Last two weeks of December
For any transactions with due dates between December 19 – January 2, please have submitted in ready-form to ORA by Thursday, December 15 to ensure there is adequate time and staffing to respond to your needs.
Please note: the next NIH SBIR/STTR deadline is Jan. 5, 2023, and the internal deadline is 8 a.m. on Dec. 28, 2022. Because this deadline falls in the last two weeks in December when ORA will be operating with reduced staff and because these award mechanisms are usually complex and require careful institutional coordination before submission:
- Please complete Intent to Submit for all planned SBIR/STTR applications no later than Dec. 5, 2022; and
- Please plan to route a submission-ready application no later than Dec. 15, 2022; if more time is needed, please submit a late waiver request so that ORA can plan for appropriate coverage to support these applications.
For anything submitted in the last two weeks of December that can wait until after the holiday break, ORA will be back up to speed with a full team on Jan. 3, 2023 and will look forward to managing all pending issues at that time.
Additional Reminders:
- We’re seeing improvements with PPE throughout DUH – great job! It is vital that we all remain vigilant with masking, hand hygiene, PPE, and other safe behaviors to prevent the spread of infection. Please pay special attention to the proper wearing and securing of gowns and be mindful of PPE compliance. Thank you for all you do to keep everyone safe and healthy.
Upcoming Events & Opportunities
Cardiology Grand Rounds
Dec. 6: No CGR this week.
Dec. 13: Celebration for Dr. Tracy Wang. 5 p.m. Webex.
Dec. 20: Our featured speaker will be Dr. Michel Khouri. Webex.
Dec. 27: No CGR this week.
CME & Other Events
Dec. 19: PDC Annual Member Meeting. 5:30-6:30 p.m. Zoom.
The meeting will be recorded and posted the following day. Submit questions to: PDC-President@dm.duke.edu. Agenda items will include:
- Financial Year In Review
- Review of Retirement Portfolio Performance from CAPTRUST
- The Path Forward for 2023: Duke Health Integrated Practice
- Anticipated Member Asset Distribution Plan
Call for abstracts: 2023 Duke Health Quality and Safety Conference
The virtual poster submission period for the 2023 Duke Health Quality and Safety Conference is now open. The deadline for submission is Wednesday, Dec. 14. The 2023 Conference will be held the weeks of March 13 and 20, with an in-person event on Thursday, March 23.
For more information and to submit your abstract, please click here.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
November 23 — Pamela Douglas
Healio
Health care industry struggles to keep pace with ‘tectonic shift’ in paid family leave
https://duke.is/najvu
November 23 — Ravi Karra and Navid Nafissi
Medscape
Test for ‘Concealed Cardiomyopathy’ After Sudden Unexplained Death
https://duke.is/btdbj
November 29 — Wayne Feng (neurology/Duke Stroke Center)
Neurology Live
Expanding the Capabilities of Treating Neuromuscular Poststroke Symptoms: Wayne Feng, MD, FAHA
https://duke.is/4rktq
Division of Cardiology Publications Indexed in PubMed November 19-30, 2022
Berwanger O, Pfeffer M, Claggett B, Jering KS, Maggioni AP, Steg PG, Mehran R, Lewis EF, Zhou Y, van der Meer P, De Pasquale C, Merkely B, Filippatos G, McMurray JJV, Granger CB, Solomon SD, Braunwald E. Sacubitril/valsartan versus ramipril for patients with acute myocardial infarction: win-ratio analysis of the PARADISE-MI trial. Eur J Heart Fail 2022 Oct;24(10):1918-1927. PM: 36054480.
Bonafiglia JT, Swinton PA, Ross R, Johannsen NM, Martin CK, Church TS, Slentz CA, Ross LM, Kraus WE, Walsh JJ, Kenny GP, Goldfield GS, Prud’homme D, Sigal RJ, Earnest CP, Gurd BJ. Interindividual Differences in Trainability and Moderators of Cardiorespiratory Fitness, Waist Circumference, and Body Mass Responses: A Large-Scale Individual Participant Data Meta-analysis. Sports Med 2022 Dec;52(12):2837-2851. PM: 35781787.
Brown LC, Halabi S, Somarelli JA, Humeniuk M, Wu Y, Oyekunle T, Howard L, Huang J, Anand M, Davies C, Patel P, Staats J, Weinhold KJ, Harrison MR, Zhang T, George DJ, Armstrong AJ. A phase 2 trial of avelumab in men with aggressive- variant or neuroendocrine prostate cancer. Prostate Cancer Prostatic Dis 2022 Apr;25(4):762-769. PM: 35292724.
Capodanno D, Baber U, Bhatt DL, Collet JP, Dangas G, Franchi F, Gibson CM, Gwon HC, Kastrati A, Kimura T, Lemos PA, Lopes RD, Mehran R, O’Donoghue ML, Rao SV, Rollini F, Serruys PW, Steg PG, Storey RF, Valgimigli M, Vranckx P, Watanabe H, Windecker S, Angiolillo DJ. P2Y inhibitor monotherapy in patients undergoing percutaneous coronary intervention. Nat Rev Cardiol 2022 Dec;19(12):829-844. PM: 35697777.
Chanfreau-Coffinier C, Tuteja S, Hull LE, MacDonald S, Efimova O, Bates J, Voora D, Oslin DW, DuVall SL, Lynch JA. Drug-drug-gene interaction risk among opioid users in the U.S. Department of Veterans Affairs. Pain 2022 Dec 1;163(12):2390-2397. PM: 35319502.
Doberne JW, Maisonave Y, DeVore A, Guinn N, Schroder JN. Bloodless HeartMate 3 explantation and orthotopic heart transplant in a heart failure patient refusing blood products. J Heart Lung Transplant 2022 Dec;41(12):1859-1860. PM: 36115786.
Fiorino C, Liu Y, Henao R, Ko ER, Burke TW, Ginsburg GS, McClain MT, Woods CW, Tsalik EL. Host Gene Expression to Predict Sepsis Progression. Crit Care Med 2022 Dec 1;50(12):1748-1756. PM: 36178298.
Greene SJ, Fonarow GC, Butler J. Sodium-glucose cotransporter 2 inhibitors for heart failure with mildly reduced or preserved ejection fraction: time to deliver implementation. Eur J Heart Fail 2022 Oct;24(10):1902-1905. PM: 36097872.
Inzucchi SE, Claggett BL, Vaduganathan M, Desai AS, Jhund PS, de Boer RA, Hernandez AF, Kosiborod MN, Lam CSP, Martinez F, Shah SJ, Verma S, Han Y, Kerr Saraiva JF, Bengtsson O, Petersson M, Langkilde AM, McMurray JJV, Solomon SD. Efficacy and safety of dapagliflozin in patients with heart failure with mildly reduced or preserved ejection fraction by baseline glycaemic status (DELIVER): a subgroup analysis from an international, multicentre, double-blind, randomised, placebo-controlled trial. Lancet Diabetes Endocrinol 2022 Dec;10(12):869-881. PM: 36372069.
Januzzi JL, Omar AMS, Liu Y, Murphy S, Butler J, Felker GM, Piña IL, Ward J, Solomon S, Contreras J. Association Between Sacubitril/Valsartan Initiation and Mitral Regurgitation Severity in Heart Failure With Reduced Ejection Fraction: The PROVE-HF Study. Circulation 2022 Nov 22;146(21):1638-1640. PM: 36183276.
Jollis JG, Granger CB, Zègre-Hemsey JK, Henry TD, Goyal A, Tamis-Holland JE, Roettig ML, Ali MJ, French WJ, Poudel R, Zhao J, Stone RH, Jacobs AK. Treatment Time and In-Hospital Mortality Among Patients With ST-Segment Elevation Myocardial Infarction, 2018-2021. JAMA 2022 Nov 22;328(20):2033-2040. PM: 36335474.
Karády J, Ferencik M, Mayrhofer T, Meyersohn NM, Bittner DO, Staziaki PV, Szilveszter B, Hallett TR, Lu MT, Puchner SB, Simon TG, Foldyna B, Ginsburg GS, McGarrah RW, Voora D, Shah SH, Douglas PS, Hoffmann U, Corey KE. Risk factors for cardiovascular disease among individuals with hepatic steatosis. Hepatol Commun 2022 Dec;6(12):3406-3420. PM: 36281983.
Karra R, Nafissi NA. Expanding the Molecular Autopsy to Uncover Occult Cardiomyopathy: Concealed to Revealed. J Am Coll Cardiol 2022 Nov 29;80(22):2069-2071. PM: 36423991.
Kern MJ, Cox D, Fearon W, Johnson N, Klein L, Krucoff M, Moses J, Naidu SS, Pinto D, Ramee S, Teirstein P, Yeung A. Is FFR dead? A conversation in cardiology. Catheter Cardiovasc Interv 2022Nov;100(6):1045-1050. PM: 36273434.
Liang J, Wang H, Cade BE, Kurniansyah N, He KY, Lee J, Sands SA, A Brody J, Chen H, Gottlieb DJ, Evans DS, Guo X, Gharib SA, Hale L, Hillman DR, Lutsey PL, Mukherjee S, Ochs-Balcom HM, Palmer LJ, Purcell S, Saxena R, Patel SR, Stone KL, Tranah GJ, Boerwinkle E, Lin X, Liu Y, et al. Targeted Genome Sequencing Identifies Multiple Rare Variants in Caveolin-1 Associated with Obstructive Sleep Apnea. Am J Respir Crit Care Med 2022 Nov15;206(10):1271-1280. PM: 35822943.
Long C, Tcheng JE, Marinac-Dabic D, Iorga A, Krucoff M, Fisher D. Developing minimum core data structure for the obesity devices Coordinated Registry Network (CRN). BMJ Surg Interv Health Technol 2022 Nov11;4(Suppl 1):e000118. PM: 36393892.
Navar AM, Fine LJ, Ambrosius WT, Brown A, Douglas PS, Johnson K, Khera AV, Lloyd-Jones D, Michos ED, Mujahid M, Muñoz D, Nasir K, Redmond N, Ridker PM, Robinson J, Schopfer D, Tate DF, Lewis CE. Earlier treatment in adults with high lifetime risk of cardiovascular diseases: What prevention trials are feasible and could change clinical practice? Report of a National Heart, Lung, and Blood Institute (NHLBI) Workshop. Am J Prev Cardiol 2022 Nov 13;12:100430. PM: 36439649.
Navar AM, Kolkailah AA, Overton R, Shah NP, Rousseau JF, Flaker GC, Pignone MP, Peterson ED. Trends in Oral Anticoagulant Use Among 436 864 Patients With Atrial Fibrillation in Community Practice, 2011 to 2020. J Am Heart Assoc 2022 Nov15;11(22):e026723. PM: 36346063.
Orvin NJ, Beavers JC, Russell SD. Acute Diuretic-Sparing Effects of Sacubitril-Valsartan: Staying in the Loop. J Pharm Pract 2022 Dec;35(6):859-863. PM: 33882753.
Ostrominski JW, Vaduganathan M, Claggett BL, de Boer RA, Desai AS, Dobreanu D, Hernandez AF, Inzucchi SE, Jhund PS, Kosiborod M, Lam CSP, Langkilde AM, Lindholm D, Martinez FA, O’Meara E, Petersson M, Shah SJ, Thierer J, McMurray JJV, Solomon SD. Dapagliflozin and New York Heart Association functional class in heart failure with mildly reduced or preserved ejection fraction: the DELIVER trial. Eur J Heart Fail 2022 Oct;24(10):1892-1901. PM: 36054231.
Patel D, Vatterott P, Piccini J, Epstein LM, Hakmi S, Syed I, Koweek LM, Bolen M, Schoenhagen P, Tarakji KG, Francis N, Shao M, Wilkoff BL. Prospective Evaluation of the Correlation Between Gated Cardiac Computed Tomography Detected Vascular Fibrosis and Ease of Transvenous Lead Extraction. Circ Arrhythm Electrophysiol 2022Nov;15(11):e010779. PM: 36306341.
Prabhakaran D, Singh K, Kondal D, Raspail L, Mohan B, Kato T, Sarrafzadegan N, Talukder SH, Akter S, Amin MR, Goma F, Gomez-Mesa J, Ntusi N, Inofomoh F, Deora S, Philippov E, Svarovskaya A, Konradi A, Puentes A, Ogah OS, Stanetic B, Issa A, Thienemann F, Juzar D, Zaidel E, et al. Correction: Cardiovascular Risk Factors and Clinical Outcomes among Patients Hospitalized with COVID-19: Findings from the World Heart Federation COVID-19 Study. Glob Heart 2022 Oct 31;17(1):79. PM: 36382154.
Rao VN, Mentz RJ, Coniglio AC, Kelsey MD, Fudim M, Fonarow GC, Matsouaka RA, DeVore AD, Caughey MC. Neighborhood Socioeconomic Disadvantage and Hospitalized Heart Failure Outcomes in the American Heart Association Get With The Guidelines-Heart Failure Registry. Circ Heart Fail 2022 Nov;15(11):e009353. PM: 36378758.
Regan JA, Truby LK, Tahir UA, Katz DH, Nguyen M, Kwee LC, Deng S, Wilson JG, Mentz RJ, Kraus WE, Hernandez AF, Gerszten RE, Peterson ED, Holman RR, Shah SH. Protein biomarkers of cardiac remodeling and inflammation associated with HFpEF and incident events. Sci Rep 2022 Nov 22;12(1):20072. PM: 36418363.
Reid HW, Parente V, Gupta MD, Hantzmon S, Olsen MK, Yang H, Jackson LR, Johnson KS, Pollak KI. Examining the relationship between clinician communication and patient participatory behaviors in cardiology encounters. Patient Educ Couns 2022 Dec;105(12):3473- 3478. PM: 36137906.
Scherba JC, Karra R, Turek JW, Bursac N. Toward improved understanding of cardiac development and congenital heart disease: The advent of cardiac organoids. J Thorac Cardiovasc Surg 2022 Dec;164(6):2013-2018. PM: 35307217.
Sedrakyan A, Marinac-Dabic D, Campbell B, Aryal S, Baird CE, Goodney P, Cronenwett JL, Beck AW, Paxton EW, Hu J, Brindis R, Baskin K, Cowley T, Levy J, Liebeskind DS, Poulose BK, Rardin CR, Resnic FS, Tcheng J, Fisher B, Viviano C, Devlin V, Sheldon M, Eldrup-Jorgensen J, et al. Advancing the Real-World Evidence for Medical Devices through Coordinated Registry Networks. BMJ Surg Interv Health Technol 2022 Nov 11;4(Suppl 1):e000123. PM: 36393894.
Selvaraj S, Seidelmann SB, Soni M, Bhattaru A, Margulies KB, Shah SH, Dugyala S, Qian C, Pryma DA, Arany Z, Kelly DP, Chirinos JA, Bravo PE. Comprehensive nutrient consumption estimation and metabolic profiling during ketogenic diet and relationship with myocardial glucose uptake on FDG-PET. Eur Heart J Cardiovasc Imaging 2022 Nov17;23(12):1690-1697. PM: 35366303.
Simard T, Vemulapalli S, Jung RG, Vekstein A, Stebbins A, Holmes DR, Czarnecki A, Hibbert B, Alkhouli M. Transcatheter Edge-to-Edge Mitral Valve Repair in Patients With Severe Mitral Regurgitation and Cardiogenic Shock. J Am Coll Cardiol 2022 Nov 29;80(22):2072- 2084. PM: 36126766.
Toro C, Ohnuma T, Komisarow J, Vavilala MS, Laskowitz DT, James ML, Mathew JP, Hernandez AF, Goldstein BA, Sampson JH, Krishnamoorthy V. Early Vasopressor Utilization Strategies and Outcomes in Critically Ill Patients With Severe Traumatic Brain Injury. Anesth Analg 2022 Dec 1;135(6):1245-1252. PM: 35203085.
Winther S, Schmidt SE, Foldyna B, Mayrhofer T, Rasmussen LD, Dahl JN, Hoffmann U, Douglas PS, Knuuti J, Bøttcher M. Coronary Calcium Scoring Improves Risk Prediction in Patients With Suspected Obstructive Coronary Artery Disease. J Am Coll Cardiol 2022 Nov 22;80(21):1965- 1977. PM: 36396197.
Yamada Y, Zhang X, Henderson MET, Sagayama H, Pontzer H, Watanabe D, Yoshida T, Kimura M, Ainslie PN, Andersen LF, Anderson LJ, Arab L, Baddou I, Bedu-Addo K, Blaak EE, Blanc S, Bonomi AG, Bouten CVC, Bovet P, Buchowski MS, Butte NF, Camps SG, Close GL, Cooper JA, Cooper R, Das S. Variation in human water turnover associated with environmental and lifestyle factors. Science 2022 Nov 25;378(6622):909-915. PM: 36423296.
Duke Heart Pulse – November 27th 2022
Chief’s message:
Thanksgiving is a time where we get to spend time hopefully recharging and in the presence of friends and family contemplating the people and things we are grateful for in our lives. It is also a time of traditions with the familiarity of food, family, and often sporting events. This year I was again able to be a referee in the annual Thanksgiving day Turkey Bowl played between the medicine residents representing the VA Hospital and Duke Hospital (VA Jets vs. Duke Marines). This annual flag football game has been a tradition for nearly 50 years  (Harvey Cohen – pictured helping with the Coin Toss in the Turkey Hat is checking on the actual first game (1973 or 1974). As every year, the goal is the have a good time, avoid all injuries, and identify a winner for bragging rights over the next year. Additionally, the game allows families in town, dogs, kids, and others to come and see our tradition. Over the last 10-15 years the game has gotten much more serious (wrist bands with plays), set plays, positions, and variety of tactics to help conduct a good game. In 2020 it was a softball game and is now back to flag football. Despite the world cup, Duke Basketball, NFL and College games, this is one of the more entertaining and generally close events of the Thanksgiving weekend
(Harvey Cohen – pictured helping with the Coin Toss in the Turkey Hat is checking on the actual first game (1973 or 1974). As every year, the goal is the have a good time, avoid all injuries, and identify a winner for bragging rights over the next year. Additionally, the game allows families in town, dogs, kids, and others to come and see our tradition. Over the last 10-15 years the game has gotten much more serious (wrist bands with plays), set plays, positions, and variety of tactics to help conduct a good game. In 2020 it was a softball game and is now back to flag football. Despite the world cup, Duke Basketball, NFL and College games, this is one of the more entertaining and generally close events of the Thanksgiving weekend  activities. This year it reminded me of the special place we have in Academic Medical Centers – in the ability to interact and train the next generation of leaders, residents, fellows, and junior faculty that quickly become the day to day fabric of Duke. Many of the sideline cheering squads, referees, team coaches (Dr. G) and others have been part of or have influenced generations of residents playing in these games. The last few years of pandemic, consolidation and strains on our health systems have worked to put tremendous stress on our faculty, residents, fellows and staff. These times of interreacting outside the hospital, getting to do things not directly related to our day to day activities serve as important moments for our teams to be together and appreciate each other. Hopefully, we will continue to find venues for these types of activities with each other. Oh, and as to the outcome of the game: 14-14 Tie on a last second Hail Mary touchdown from the VA to end the game as the clock ran out.
activities. This year it reminded me of the special place we have in Academic Medical Centers – in the ability to interact and train the next generation of leaders, residents, fellows, and junior faculty that quickly become the day to day fabric of Duke. Many of the sideline cheering squads, referees, team coaches (Dr. G) and others have been part of or have influenced generations of residents playing in these games. The last few years of pandemic, consolidation and strains on our health systems have worked to put tremendous stress on our faculty, residents, fellows and staff. These times of interreacting outside the hospital, getting to do things not directly related to our day to day activities serve as important moments for our teams to be together and appreciate each other. Hopefully, we will continue to find venues for these types of activities with each other. Oh, and as to the outcome of the game: 14-14 Tie on a last second Hail Mary touchdown from the VA to end the game as the clock ran out.


Importantly, we are also grateful during this time and the upcoming holidays for our staff and faculty/fellows/residents that help care for our patients in the hospital. In this version of the pulse you will some photos below of our staff and others seen around town.
Highlights of the week:
Chet Patel Accepts New Role as Associate Vice Chair, Strategic Physician Relations
 Congratulations to Chet Patel, MD! He will soon serve as associate vice chair for strategic physician relations for the Duke Department of Medicine. The announcement was made on Wednesday, Nov. 23 by Dr. Kathleen Cooney, chair, Department of Medicine. Her statement reads:
Congratulations to Chet Patel, MD! He will soon serve as associate vice chair for strategic physician relations for the Duke Department of Medicine. The announcement was made on Wednesday, Nov. 23 by Dr. Kathleen Cooney, chair, Department of Medicine. Her statement reads:
“Over the past five years, the Department of Medicine has been working coordinately with Duke University Health System and the PDC to extend our clinical practice into Wake County and other strategic areas. This work is very different from our usual clinical operations/quality management and requires strategic thinking as well as close collaboration with internal and external groups. I am pleased to announce that Chet Patel, MD, our current Vice Chair of Clinical Affairs, has accepted a new leadership position within the Department of Medicine as Associate Vice Chair, Strategic Physician Relations.
Dr. Patel’s new responsibilities will include supporting the implementation of the clinical strategic plan for the Department with a focus on internal and external partnerships. He will represent the Department of Medicine in agreements with external entities by coordinating efforts with the DUHS strategic planning office. He will also focus on facilitating communication to physicians about specialty services and procedures provided at DUHS while streamlining those efforts. In this role he will report to the Vice Chair for Clinical Affairs.
Dr. Patel will transition to this new role once a new Vice Chair for Clinical Affairs has been selected. A search to fill the Vice Chair role will begin on Monday, November 21 led by David D’Alessio, MD, chief, Endocrinology, Metabolism, and Nutrition. Candidates interested in the role of Vice Chair for Clinical Affairs are asked to email a brief letter of intent and an updated CV to emelia.dunston@duke.edu by Wednesday, December 21.
View the job description, duties and responsibilities here. Additional position details will also be sent in a subsequent email message for those interested in the role.”
We are excited for you, Chet!
Tong, Zwischenberger Featured in WTS Oracle
Duke Heart’s Betty Tong, MD and Brittany Zwischenberger, MD are featured in the latest issue of Oracle, an annual magazine produced by Women in Thoracic Surgery. The article is about Lise Tchouta, a 4th year General Surgery resident at Columbia University Medical Center and recent recipient of the Brigid Scanlan Traveling Mentorship Award. Tchouta chose to spend four weeks at Duke under the mentorship of Tong and Zwischenberger; the article speaks to the importance of mentorship and increasing the number of women in the field.
It’s a terrific piece in a powerful edition of Oracle. Well worth the read (p. 22)!
Both Allan Kirk, MD and Edward P. Chen, MD chimed in on the piece.
“Congratulations on such a wonderful story,” said Kirk. “Thanks for projecting the progressive side of Duke CT Surgery and helping move us to a better future.”
“Great job Betty and Brittany in attracting future female CT surgeons to Duke, Chen added.”
The importance of mentors can never be overstated. Way to go!
Loring Awarded Pilot Study Grant

Zak Loring, MD has been awarded a Durham VA Health Services Research & Development ADAPT COIN pilot study grant for his proposal Improving Disparities in Atrial Fibrillation Care Through ECG-based Machine Learning Risk Models. This is a 1-year preliminary project award worth $50,000 aimed at enhancing healthcare equity.
We also learned that Loring has passed his boards. Great news all around, Zak! Congratulations!!!
In Gratitude to Our Many Teams!
We hope each of you enjoyed the holiday. Thank you to all of our many team members who cared for patients on our units over the holiday weekend. We hope you’ve had some time to decompress and relax! We’ve had an amazing year of accomplishments. Thank you for all that you do.








Reminder: ORA Holiday Deadlines
The Office of Research Administration (ORA) will operate with a reduced staff during the holiday season to allow team members time to recharge. To help ORA respond as timely as possible to your needs, please plan in advance based on the following:
Picture of the Week
Seen in the Cameron Crazie section of the Duke Basketball game

Last two weeks of December
For any transactions with due dates between December 19 – January 2, please have submitted in ready-form to ORA by Thursday, December 15 to ensure there is adequate time and staffing to respond to your needs.
Please note: the next NIH SBIR/STTR deadline is Jan. 5, 2023, and the internal deadline is 8 a.m. on Dec. 28, 2022. Because this deadline falls in the last two weeks in December when ORA will be operating with reduced staff and because these award mechanisms are usually complex and require careful institutional coordination before submission:
- Please complete Intent to Submit for all planned SBIR/STTR applications no later than Dec. 5, 2022; and
- Please plan to route a submission-ready application no later than Dec. 15, 2022; if more time is needed, please submit a late waiver request so that ORA can plan for appropriate coverage to support these applications.
For anything submitted in the last two weeks of December that can wait until after the holiday break, ORA will be back up to speed with a full team on Jan. 3, 2023 and will look forward to managing all pending issues at that time.
Additional Reminders:
- It is vital that we all remain vigilant with masking, hand hygiene, PPE, and other safe behaviors to prevent the spread of infection. Please pay special attention to the proper wearing and securing of gowns and be mindful of PPE compliance. Thank you for all you do to keep everyone safe and healthy.
Upcoming Events & Opportunities
Cardiology Grand Rounds
November 29: No CGR this week.
CME & Other Events
Call for abstracts: 2023 Duke Health Quality and Safety Conference
The virtual poster submission period for the 2023 Duke Health Quality and Safety Conference is now open. The deadline for submission is Wednesday, Dec. 14. The 2023 Conference will be held the weeks of March 13 and 20, with an in-person event on Thursday, March 23.
For more information and to submit your abstract, please click here.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
November 8 — Pamela Douglas
Cardiovascular Business
VIDEO: PRECISE trial shows cardiac CT with FFR-CT significantly improves patient outcomes
https://duke.is/9mu94
November 9 — Manesh Patel
Everyday Health
Dietary Supplements Don’t Lower ‘Bad’ Cholesterol, Study Finds
https://duke.is/b9nq6
November 9 — W. Schuyler Jones
Medpage Today
Surgery Bests Endovascular Therapy for Most Limb-Threatening Ischemia Patients
https://duke.is/cfvgf
November 10 — Neha Pagidipati
Medscape
Remote Care May Help Curb High Blood Pressure, High Cholesterol
https://duke.is/5cnhr
November 10 — Robert Mentz
Pharmacy Pratice News
No Efficacy Difference Between 2 Common Loop Diuretics
https://duke.is/nyw3x
November 10 — Renato Lopes
Medscape
No Benefit of Rivaroxaban in COVID Outpatients: PREVENT-HD
https://duke.is/r6wzq
November 11 — Jennifer Rymer
tctMD
Cangrelor After Ticagrelor Pretreatment in ACS Might Be OK: SWAP-5
https://duke.is/8buun
November 11 — Kevin Hill (pediatric cardiology)
EMJ
Methylprednisolone in Infants Undergoing Cardiopulmonary Bypass Surgery
https://duke.is/phvjj
November 11 — Kevin Hill
tctMD
STRESS Shows ‘Borderline Results’ for Methylprednisolone in Infant Cardiac Surgery
https://duke.is/gkspc
November 11 — Neha Pagidipati
Patient Care
https://duke.is/65dnu
November 14 — Jennifer Li and Kevin Hill (peds cardiology)
Diagnostic and Interventional Cardiology
Largest Randomized Trial Evaluates Steroids for Infant Heart Surgery
https://duke.is/mvvtt
November 14 — Renato Lopes
Healio/Cardiology Today
Trial does not support routine antithrombotic use in ill outpatients with COVID-19
https://duke.is/7mrd3
November 14 — Manesh Patel
tctMD
Drug Preconditioning Before CABG, Valve Surgery Shows Promise: START
https://duke.is/v3sss
November 15 — Christopher Granger
tctMD
Many STEMI Patients Not Treated Within National Time Goals
https://duke.is/gwwct
November 17– Duke Clinical Research Institute
Practical Cardiology
Almost 1 in 3 High-Risk AFib Patients Not Receiving Anticoagulation
https://duke.is/9augu
November 17 — Jonathan Piccini
Healio/Cardiology Today
Botulinum toxin injection does not prevent postoperative AF: NOVA
https://duke.is/2pk25
November 18 — Jonathan Piccini
Medscape
Neurotoxin to Avert Postoperative AF: Patient Selection Clues in NOVA
https://duke.is/4svy7
November 21 — Josef Turek and the Sinnamon family
KFVS-CBS12 Cape Girardeau (MO)
18-month old medical miracle from world’s first heart-thymus procedure
https://duke.is/p4n3a
November 21 — Manesh Patel
Parallax by Ankur Kalra
EP 80: AHA’s Scientific Sessions: Science, Innovation and Community With Dr Manesh Patel
https://duke.is/6jwkw
November 22 – Stephen Greene
Healio/Cardiology Today
Low household income may predict higher risk for 30-day HF readmission
https://duke.is/5knzk
November 23 — Jonathan Piccini
Medscape
Factor Xa Inhibitors Tied to Interstitial Lung Disease in AF
https://duke.is/rtw5h
Duke Heart Pulse November 20th 2022
Highlights of the week:
Happy Thanksgiving to All!
On behalf of the entire Duke Heart leadership team, we wish you and your loved ones a happy Thanksgiving. During this time of reflection on our many personal blessings, we also give thanks for the incredible team we have here in Duke Heart. Together, we have persevered through some big challenges over the last several years, and also accomplished a great deal. We have a lot to be proud of. Thank you for all that you do — each member of our team makes a difference. Warm wishes to you and we hope you have some time to spend with your family, friends, and loved ones.
CVRC Announces Research Staff Appreciation Awardees
Each year, the Duke Cardiovascular Research Center (CVRC) presents research staff appreciation awards to members of their team who have made an exceptional contribution to their team. Due to the pandemic, the CVRC was unable to formally celebrate as a group last year due to the pandemic, so this year was extra special! We are excited to share with you their awardees for both 2021 and 2022. The CVRC awards were made on Nov. 9.
 The 2021 awardee is Xinhe Yin of the Holley Lab, nominated by Dr. Chris Holley with support from colleague Brittany Elliott, PhD. In their summary, Holley and Elliott shared the following:
The 2021 awardee is Xinhe Yin of the Holley Lab, nominated by Dr. Chris Holley with support from colleague Brittany Elliott, PhD. In their summary, Holley and Elliott shared the following:
“Xinhe is a valuable member of the Holley Lab and CVRC. This is evidenced by her ever-growing knowledge base of technical expertise, the efforts she makes to care about and help the scientific endeavors in the CVRC succeed, and by being a good citizen of the CVRC by going above and beyond to maintain instrumentation within the shared CVRC resource. Xinhe brings multiple areas of expertise to the lab. First, she is an expert in managing our mouse colony, including breeding, genotyping, and tissue collection. Second, she performs a significant amount of cell culture for the laboratory, maintaining a wide variety of human, mouse, and rat cell lines, including many CRISPR-modified clonal lines. Third, she has developed the necessary expertise to prepare samples for our UPLC-MS/MS method that quantifies RNA modifications. Fourth, she has developed expertise with the Seahorse platform, which has allowed her to supervise this instrument for the CVRC. Her technical expertise contributes to every project in the lab!
“Xinhe also serves as our lab manager, taking responsibility for safety protocols, inspections, maintaining lab equipment and supplies, and ensuring that successful transitions as lab members join then eventually leave the lab. She is the primary contact for many collaborations, coordinating animal and material transfers. She serves as an emergency contact for the animal colony and the remote monitoring of our freezers. One of the things that I really respect about Xinhe is that when she sees something that seems wrong, or she doesn’t understand something, she asks about it instead of ignoring it.”
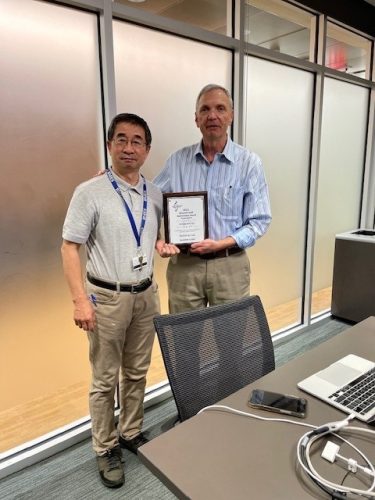 The 2022 awardee is Longquan Xu of the Rockman Lab, nominated by Dr. Howard Rockman with support from colleague Darion Rapoza, PhD. In their nomination, Rockman and Rapoza shared:
The 2022 awardee is Longquan Xu of the Rockman Lab, nominated by Dr. Howard Rockman with support from colleague Darion Rapoza, PhD. In their nomination, Rockman and Rapoza shared:
“Longquan Xu is a highly skilled small animal cardiac microsurgeon and echocardiographer in the CVRC Cardiovascular Physiology Core. He is by far one of the most conscientious technicians we have ever had the pleasure of working with. His technical expertise is exemplary. He is the go-to person in the CVRC Core for performing cardiac surgeries and the precision analyses of B mode 2D echocardiograms. He is totally dedicated to excellence and precision in performing noninvasive and invasive hemodynamic studies. When there is time available in his schedule, and on his own initiative, he will practice surgeries to hone newly acquired skills or to keep his procedural skills sharp and at the highest level of competency. Moreover, he is willing to learn new techniques and will practice new procedures until he has achieved perfection. He is always eager to be helpful. He is a supportive teacher, flexible, and always cooperative in sharing the workload to keep the core’s performance at its best for the PIs and their research programs. From COVID precautions to barrier facility protocols, he rigorously complies with guidelines and assists other in doing so as well, because, in his words, “It matters.”
Congratulations to Xinhe and Longquan!
To be eligible for a CVRC Research Staff Award, an individual must be employed by the Duke School of Medicine and must meet all of the following criteria:
- Technicians, Lab Research Analysts, Project Leaders, or any staff member who provides exemplary support in the conduct of basic or translational research within the CVRC.
- Current role provides technical expertise to support basic or translational research program(s) in a manner which strengthens the research mission of the CVRC.
- At least 5 years of continuous service in a research role in the CVRC.
- Demonstrated record of excellent performance and good citizenship.
Not Eligible: Faculty or staff members who have primary investigator status, research fellows, research associates and senior research associates, post-doctoral fellows and graduate students, administrative professionals.
Harper Recognized for Years of Service to Duke Heart
 Our long-time colleague, Monica Harper, will be retiring on November 30, 2022 after more than 39 years of service at Duke. Monica has worked in the Heart Center since 1990 in varying roles including staff nurse, assistant head nurse, and — since 2000 — as 7300 Nurse Manager of Operations. Throughout her time with our team she served on many task forces and committees.
Our long-time colleague, Monica Harper, will be retiring on November 30, 2022 after more than 39 years of service at Duke. Monica has worked in the Heart Center since 1990 in varying roles including staff nurse, assistant head nurse, and — since 2000 — as 7300 Nurse Manager of Operations. Throughout her time with our team she served on many task forces and committees.
Monica is known for her calm and humble demeanor, her approachability, fair and consistent practice, and patient and staff advocacy. It came as a surprise to no one when she was named a recipient of the highly esteemed Duke Friends of Nursing Leadership Award.
On behalf of the entire Duke Heart Center Leadership team, we thank Monica for her loyalty and dedication to our patients, the faculty and staff of Duke Heart, and to Duke University Hospital.
She will certainly be missed. Please join us in wishing her well in her retirement!
National Nurse Practitioner Week, Nov. 13-19
In recognition of the Nurse Practitioner profession and the many contributions they make to Duke Health and the health of the nation. Did you know there are more than 355,000 certified NPs in the U.S. caring for patients of all ages? We are deeply grateful for the efforts and contributions these vital Duke Heart team members make each and every day.
As highly skilled team members and healthcare leaders, NPs provide exceptional patient care in virtually all health care specialties and settings. NPs are pivotal in the health care delivery of Duke Heart and Duke Health, serving in critical roles throughout clinical care, education, health administration, leadership, and research.
We hope all of our amazing Duke NPs had a great week!
High Five to Harris-Holloway!
Sandra Harris-Holloway, CCP, LP, Associate Chief, Adult Services Manager for Perfusion Services at Duke University Hospital  received a High Five on Nov. 7.
received a High Five on Nov. 7.
“Sandra has an office close to a patient care area. She noticed a patient who was frequently sitting by the windows outside her office to get sunlight. Sandra partnered with the care team and advocated for administrative approval for the patient to go outside. During a time of restrictions, Sandra advocated for this patient’s mental health and wellbeing by going above and beyond her duties.”
We know this made a big difference for this patient. Way to go, Sandra!
Duke Heart Family Expands by One!
We are excited to share the happy news that Nishant Shah and Nikita Goel welcomed their son, Asher Jayden Shah, on November 17. Mom and baby are doing well, and big sister Amara is excited to have a little brother!
He’s adorable and we can’t wait to meet him in person. Welcome to the Duke Heart family, Asher. Congratulations to the Shah family!

ICYMI: Krasuski Featured Guest on CardioNerds
Rich Krasuski was recently a featured guest on the popular podcast, CardioNerds. A link to episode 242 appears here ACHD: Atrial Septal Defects with Dr. Richard Krasuski.
Nicely done, Rich!

ORA Holiday Deadlines
The Office of Research Administration (ORA) will operate with a reduced staff during the holiday season to allow team members time to recharge. During this period, please plan as far in advance as possible.
To help ORA respond as timely as possible to your needs, please plan in advance based on the following:
Thanksgiving Day and the Friday After
If you need something processed BEFORE the Thanksgiving holiday, please have it submitted in ready-form to ORA by Thursday, November 17. Otherwise, if it can wait, ORA will process the following week (beginning November 28).
Last two weeks of December
For any transactions with due dates between December 19 – January 2, please have submitted in ready-form to ORA by Thursday, December 15 to ensure there is adequate time and staffing to respond to your needs.
Please note: the next NIH SBIR/STTR deadline is Jan. 5, 2023, and the internal deadline is 8 a.m. on Dec. 28, 2022. Because this deadline falls in the last two weeks in December when ORA will be operating with reduced staff and because these award mechanisms are usually complex and require careful institutional coordination before submission:
- Please complete Intent to Submit for all planned SBIR/STTR applications no later than Dec. 5, 2022; and
- Please plan to route a submission-ready application no later than Dec. 15, 2022; if more time is needed, please submit a late waiver request so that ORA can plan for appropriate coverage to support these applications.
For anything submitted in the last two weeks of December that can wait until after the holiday break, ORA will be back up to speed with a full team on Jan. 3, 2023 and will look forward to managing all pending issues at that time.
This has been another year of tremendous growth in research at Duke. The Office of Research Administration thanks you for your continued partnership in support of Duke’s research mission and they send warm holiday wishes to all!
Additional Reminders:
- It is vital that we remain vigilant with masking, hand hygiene, PPE, and other safe behaviors to prevent the spread of infection. Please pay special attention to the proper wearing and securing of gowns and be mindful of PPE compliance. Thank you for all you do to keep everyone safe and healthy.
- November is American Diabetes Month, Pulmonary Hypertension Awareness Month, and National COPD Awareness Month. Thanks for all you do to help patients with these conditions!
- November 13-19 National Nurse Practitioner Week.

Upcoming Events & Opportunities
Cardiology Grand Rounds
November 22: Calcium Modification in Percutaneous Coronary Intervention with Ali Corley. 5 p.m., Webex.
CME & Other Events
Call for abstracts: 2023 Duke Health Quality and Safety Conference
The virtual poster submission period for the 2023 Duke Health Quality and Safety Conference is now open. The deadline for submission is Wednesday, Dec. 14. The 2023 Conference will be held the weeks of March 13 and 20, with an in-person event on Thursday, March 23.
For more information and to submit your abstract, please click here.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News: Our news coverage will return Nov. 27.
Duke Heart Pulse November 13th 2022
Highlights of the week:
Veterans Day Weekend
We hope you’re all enjoying the weekend. With more than 1200 veterans on our extended team throughout DUHS, and so many of our Duke Heart team members caring for veterans at the Durham VAMC, we thank all those who have served in the U.S. military. Whether their service occurred during a time of war or time of peace, and regardless their length of service, we will always be indebted to veterans and their families for all they’ve given to the U.S.
Celebrating Tracy Wang, MD

It’s hard to believe, but Tracy Wang’s last official day with us at Duke was Monday, Nov. 7. As we mentioned in Pulse several weeks ago, Wang is headed to the Patient Centered Outcomes Research Institute (PCORI) to serve as their Chief of Comparative Effectiveness Research.
We had the opportunity to speak with Tracy about her time at Duke, what she has valued most, and what she’s looking forward to with her new position.
“The skills and experience that I’ve acquired over the last 20 years or so at Duke is one of the beauties about being a faculty member at Duke. We have the freedom to pick and choose what kind of questions we want to answer,” Wang said. “I believe it’s one of the most grounding aspects of what we do. Many of us are clinicians in addition to researchers, and we try to answer questions that are really meaningful to clinical care. I’ll very much draw on that as I think about the future of research in my new role. I’ve had so many amazing mentors and role models here and I’ve had the pleasure of working with so many statistical and methodological experts as well. I have a solid grounding in knowing good science, recognizing it, and being able to think about ways in we could affect change within the field. There is so much innovation happening at Duke. The sentiment here is very much about progress — not doing the same thing over and over again. We’re always learning and innovating – we want to know how we can do something better the next time. This spirit of innovation, I think, is really key to any leader within a research field. We’re not trying to do the same thing every day, we’re trying to continuously improve how we think about the conduct of research. These are important aspects of Duke that have shaped both my experience and who I am as a clinician scientist.”
A lot of what PCORI is trying to do, according to Wang, is take a look at therapies that are already approved, and try to figure out which therapies best serve patient needs.
“One of the key missions PCORI has is to stay very patient-focused,” Wang said. “We need to have a finger on the pulse of what patients and patient stakeholders feel are important questions to answer. It’s also about making sure that we’re good stewards of the funding and ensuring that the type of science we fund is impactful and done in as efficient a manner as possible. I’ll also help guide how to think about investing in research, so that strategically we make the best use of the resources we have.”
Wang says her time at Duke has prepared her well for the role at PCORI.
“Duke is one of the most collaborative and creative leaders within clinical research,” she added. “It’s our spirit of collaboration and innovation that sets us apart from many other research entities out there. And, I think, we broadly recognize that even though there’s a lot of excellence within our group at Duke, we can always learn from others. We know that when we work with others, we are in a much better position to get the job done and to shape the future of medicine. This is definitely one of the strengths of being at Duke and one of the grounding characteristics of our faculty here. This is the type of spirit that I would like to hopefully extend to other groups out there through “the sauce,” if you will, that PCORI provides in trying to get all the players in the field to be able to collaborate and form partnerships more effectively so that we can be more innovative about our methods.
“What I’m looking forward to at PCORI is having the ability to really scale out this process on a more national and international scale. So rather than thinking about individual projects, I’ll be thinking about a whole portfolio of comparative effectiveness research that we can and should be doing.
“As much as I love what I do at Duke, this is what really attracted me to PCORI. I’ll have an opportunity to really have some influence on clinical research – from the type of research being done, to how it can be done, to how we can disseminate the results more effectively. How do we go back to our roots – to what patients need and want? Being able to work on these questions on a much more national scale is what really appealed to me.”
Wang received the 2022 Outstanding Lifetime Achievement Award from the American Heart Association’s Council on Quality of Care and Outcomes Research (QCOR) last May. The award was presented to her during the QCOR Scientific Sessions held in Reston, VA. A tribute video was created specifically for her QCOR award and it’s worth checking out if you didn’t get a chance to see it back in May. A link to it can be found here.
While a lifetime achievement award from QCOR is an incredible honor, Wang says she considers her greatest achievement to be the success of her mentees.
“I am most proud of the talent that I’ve hopefully coached along. One of the things I’m really going to miss about Duke is the really incredible folks here that are in various phases of their career, especially those who are at earlier stages. I really enjoy working with these amazing young minds! To be able to stop and think about what they’re interested in and help them work towards something that is satisfying for them, to help them grow skills that will be helpful to them as time goes on, and then watching them far surpass me in terms of where they’ve gone and what they’ve done. I’ve mentored almost 40 individuals since I started on faculty in 2008. it’s kind of nice to be able to work alongside some of the people I’ve helped train and have them ‘show me up’ on a daily basis. It makes me extraordinarily happy when they do that! It’s also nice to see mentees that have left Duke and gone on to flourish at other places. Bar none, that’s the achievement I am most proud of.
Over the course of her many years at Duke, a large number of people have had the opportunity to work with and learn from Tracy. We reached out to several of them for thoughts on her and her lasting legacy. Here is what they had to say:
“Tracy is an amazing cardiologist, investigator, colleague, and person. She has tremendous insight into tough clinical research issues and usually finds the simplest and most effective solutions. She is always willing to help colleagues without seeking credit. A fantastic mentor to many, I will truly miss her no-nonsense good humor, humility and zest. Tracy is a treasure so I hope she remains part of our Duke family while surely being hugely successful in shaping the nation’s outcomes research agenda at PCORI.” — Pamela S. Douglas, MD
“It is impossible to outline all the ways that Tracy has mentored me through the years. She met with me as an intern, and I began working with her at that time. She has given me so many opportunities, from learning how to work with industry to running analyses and projects independently. Her advice through the years has been invaluable. She was instrumental in helping me transition from a fellow to a faculty member. Tracy has mentored countless fellows and early career faculty at both Duke and more widespread through her significant work with the AHA. Her impact on health outcomes research at the DCRI is widespread and is one of the most talented people I have ever worked with in her ability to formulate scientific questions and develop the appropriate methodology to answer those questions. She has successfully mentored me through two career development awards and many other successful grant applications. She quickly turned from a mentor to a close friend. I will miss her so much, but can’t wait to see what she will accomplish through her work at PCORI.” — Jenn Rymer, MD
“Tracy is a great clinician, researcher and teacher that we rarely see. While many could have focused on themselves, Tracy wasn’t in that mold. She constantly had a string of mentees advancing their careers in a “pay it forward” manner. Beyond that she is a great friend to many. Just as she has had an impact on Duke and DCRI, it will be great to see how she has an impact on PCORI and the nation’s portfolio of comparative effectiveness research. We certainly need better answers and all of us will benefit from her leadership there shaping the questions and delivering clear answers with high-quality research.” — Adrian Hernandez, MD
Shown here are photos from a farewell celebration for Tracy that was held on the patio at Tobacco Road Sports Cafe in Durham on Oct. 6.
She summed up her feelings about leaving with a Chinese saying:
長江後浪推前浪,世上新人隨舊人
Chang jiang hou lang tui qian lang shi shang xin ren suay jiu ren
“Translated, this means ‘Just as the waves of the Yangtze River behind drive on those ahead, so does each new generation replace the old one,’” she added. “While leaving is bittersweet for me and many others, I remain optimistic and excited about the future of Duke as the next generation at Duke has so much talent and potential.”
You will be missed here at Duke, Tracy! We are extremely proud of you and happy that you’re not going far — you’ll always be a part of the Duke Heart family.


Scientific Sessions Wrap-Up
The 2022 American Heart Association Scientific Sessions concluded earlier this past week, yet our celebration of the great work you’ve done continues:
AHA.22 LBCT: Chest Pain Patients Benefit from Precision Diagnostic Testing Approach
A study comparing two approaches for diagnosing heart disease found that a risk analysis strategy is superior to the usual approach of immediately performing functional tests or catheterization for low- to intermediate-risk patients with new-onset chest pain.
Presented Nov. 6 at the American Heart Association’s 2022 Scientific Sessions, the study bolsters a risk-analysis strategy that either defers testing among low-risk patients, or uses coronary computed tomography angiography (CTA), a CT scan with a contrast agent to assess for blockages.
The risk analysis approach has been outlined in guidelines and is championed as a means of reducing often unnecessary and costly tests. It has never been tested rigorously in a randomized trial, however, and its clinical application has lagged without definitive evidence of its effectiveness compared to various functional stress tests.
“New onset chest pain is a common clinical problem that involves a lot of testing, work and expense,” said study lead Pamela S. Douglas, MD, the Ursula Geller Professor of Research in Cardiovascular Diseases at Duke University School of Medicine and a member of the Duke Clinical Research Institute.
“Our study provides evidence that, among low-risk patients, the tests will likely be negative for coronary artery disease and patients will go on to do well,” Douglas said. “As a result, we should be deferring testing in these low-risk people.”
Douglas and colleagues enrolled more than 2,100 patients across the U.S. and Europe with new-onset chest pain in the PRECISE clinical trial. Participants’ average age was 58, with roughly equal numbers of men and women.
Half of the patients were randomly assigned to receive usual testing — including stress echocardiogram, nuclear stress test, stress MRI or catheterization — which physicians selected at their discretion.
The other half of participants were randomized to the precision strategy, which uses a pre-test probability assessment to guide next steps, including deferred testing or CTA, with selective use of image analysis software to determine the significance of any blockages.
Within both groups, about 21% of symptomatic patients were assessed to be at low risk of heart disease. Of these low-risk patients in the usual testing group, 86% underwent some sort of test, compared to 37% in the precision strategy group.
The primary focus was whether, within a year, there were any differences between the two diagnostic approaches for any combination of the following outcomes: deaths from any cause, nonfatal myocardial infarction, or catheterizations that did not show blockages and may have been unnecessary.
The researchers found that the precision strategy substantially reduced the incidence of the composite endpoint compared to the usual stress testing approaches.
To provide a full picture of clinical value, the investigators balanced this demonstrated effectiveness with examination of any safety concerns. There were no differences in death or the composite of death and myocardial infarction, but there was a small, non-significant difference in nonfatal myocardial infarction in the precision group.
“In stable, symptomatic patients with suspected heart disease who physicians feel require testing, a precision strategy incorporating a set of actions based on guideline recommendations, will improve outcomes compared to usual testing,” Douglas said.
In addition to Douglas, study authors include Michael G. Nanna, Michelle D. Kelsey, Eric Yow, Daniel B. Mark, Manesh R. Patel, Campbell Rogers, James E. Udelson, Christopher B. Fordyce, Nick Curzen, Gianluca Pontone, Pál Maurovich-Horvat, Bernard De Bruyne, John P. Greenwood, Victor Marinescu, Jonathon Leipsic, Gregg W. Stone, Ori Ben-Yehuda, Colin Berry, Shea E. Hogan, Bjorn Redfors, Ziad A. Ali, Robert A. Byrne, Christopher M. Kramer, Robert W. Yeh, Beth Martinez, Sarah Mullen, Whitney Huey, Kevin J. Anstrom, Hussein R. Al-Khalidi, and Sreekanth Vemulapalli, for the PRECISE Investigators.
The study received funding from HeartFlow, a medical technology company.
AHA.22: Additional Presenters and Session Moderators
Jonathan Piccini presented results from the phase-2, dose-ranging NOVA study. The team found no significant differences in the rate of postoperative atrial fibrillation (POAF) in cardiac surgery patients who received either 125U or 250U doses of botulinum toxin type A (AGN-151607) compared with placebo. Piccini noted that subgroup analyses suggested a lower rate of POAF and rehospitalization in patients undergoing isolated CABG and in patients older than 65 years who received 125U of AGN-151607. He added that the mechanism of AFib suppression with botulinum toxin may be related to both direct autonomic influences and decreased inflammation.
 Cardiovascular surgeon Brittany Zwischenberger presented several sets of findings across Sessions including “Keep the Guidelines for Radial Artery Grafts in CABG Surgery” during the Consensus and Controversies: Debating the 2021 ACC/AHA/SCAI Guidelines for Coronary Revascularization session held Saturday, Nov. 5, and “Highlights and Controversies from 2021 Guidelines on Coronary Artery Revascularization” during the Update on 2022 Cardiovascular Clinical Guidelines session held on Monday, Nov. 7. Zwischenberger also served as session moderator for New Insights – Cardiac Surgery held Sunday, Nov. 6.
Cardiovascular surgeon Brittany Zwischenberger presented several sets of findings across Sessions including “Keep the Guidelines for Radial Artery Grafts in CABG Surgery” during the Consensus and Controversies: Debating the 2021 ACC/AHA/SCAI Guidelines for Coronary Revascularization session held Saturday, Nov. 5, and “Highlights and Controversies from 2021 Guidelines on Coronary Artery Revascularization” during the Update on 2022 Cardiovascular Clinical Guidelines session held on Monday, Nov. 7. Zwischenberger also served as session moderator for New Insights – Cardiac Surgery held Sunday, Nov. 6.
New Duke Heart faculty member Senthil Selvaraj is senior author on findings presented on Monday at AHA. His team’s study was simultaneously published in JACC: Basic to Translational Science. Their paper is “Metabolomic Signatures of Myocardial Glucose Uptake on Fluorine-18 Fluorodeoxyglucose Positron Emission Tomography.” Co-authors include Svati H. Shah, Mahesh K. Vidula, Daniel P. Kelly, Zoltan Arany, Kenneth B. Margulies, Thomas P. Cappola, and Paco E. Bravo.
Finally, Manesh Patel and Kelly Arps were the featured guests in a Twitter Spaces held Tuesday, Nov. 8 on Twitter. Patel and Arps did a recap of some of the most notable findings presented at Scientific Sessions. The event was recorded, but a link has not yet been made available. Once it is, we’ll post it here in Pulse.
Our team received a great deal of news coverage this year. Please visit the News section below to check it out. We truly had an outstanding presence at Sessions this year. We look forward to 2023!
Mark Serves as Guest Lecturer for AKUPI-NCD
Dan Mark, MD, was invited to discuss landmark studies in cardiovascular disease at a research certification course held recently as part of the Aga Khan University Pakistan Initiative for Non-Communicable Diseases (AKUPI-NCD) Research Training Program. The course audience consisted of aspiring and early career researchers from across Pakistan.
AKUPI-NCD was created to address a critical gap in the response to the NCD epidemic. The Aga Khan University partnered with Duke University to design a comprehensive, integrated, multi-disciplinary training program to prepare the next generation of leaders in NCD research. The program, focused on cardiovascular and cerebrovascular diseases and their shared risk factors, is funded by a research training grant by the U.S. National Institutes of Health via the Fogarty International Center.
Great work!

Huber Presents CGR
We welcomed Kurt Huber for Cardiology Grand Rounds on Tuesday evening, Nov. 8. His talk was entitled, “The Paradigm Shift of DAPT after ACS.” Huber is vice-dean of research at Sigmund Freud University for Medicine in Vienna, Austria, and chair of acute and interventional cardiology at the Wilhelminenspital.
Thanks to all who joined us!


Future Relocation of DN 7100 for Renovations
The Duke North 100 Tower is in the process of being renovated. Eventually, Duke University Hospital unit 7100 will be relocated to allow for renovations which will occur sometime after the start of the year. Once we receive additional information as to the timeline and where 7100 is relocating, updates will be provided.
Shout-out to 7W & 3300!
Our teams on 7W and 3300 received a kudos at DUH on Nov. 8 for achieving 100% compliance for hand hygiene and PPE use. Way to go!
Thanksgiving Edition of Pulse
In this season of gratitude, who or what within Duke Heart (or beyond) are you particularly grateful for this year? We are offering a way to acknowledge those who’ve been a big support or help to you over the past year. Send your shout-outs and kudos to Tracey Koepke by Tuesday, November 22 and we’ll include them in our Thanksgiving issue of Pulse on Sunday, Nov. 27. We look forward to shout-outs and gratitude galore!
Additionally, as we move into the holiday season, please let us know if your team or unit within Duke Heart will be doing anything special to celebrate — perhaps you’ll be adopting a family in need? Hosting a food drive? If you’d like others to join your effort, or if you would just like to showcase what you’ll be doing (or what you did) in Pulse, let us know! We’ll issue the newsletter through December 18th, then we’ll be taking our annual break for two weeks. Pulse will resume on Sunday, Jan. 8, 2023. As always, email your items to tracey.koepke@duke.edu.
Webex User Accounts Decommission Notice
Duke Health is decommissioning Webex User Accounts effective Wednesday, Feb. 1, 2023, and will shift to Zoom for conferencing and collaboration needs. This decision was based on a significant decline in Webex usage and will allow for consolidation of technology support. Current Webex users can use this three-month window to explore Zoom, which offers a user-friendly experience for conferencing needs.
Webex user accounts will be decommissioned and Webex Recordings will no longer be available. Duke Health recommends downloading Webex recordings prior to Feb 1. 2023.
While Webex will remain available until February, Webex users are encouraged to start using Zoom as soon as possible to ensure a smooth transition. Duke Health will still have the ability to join a Webex Meeting as a “GUEST”.
Note: Cisco Webex Rooms/Devices will NOT be impacted. Cisco Webex Rooms/Devices will remain registered to the Cisco Webex Control Hub (Cloud)
If you have questions or concerns, visit the IT Portal and click on Create a New Request in the Popular Items section to open a request, or contact the Duke Health Service Desk at 919-684-2243.
Duke Angel Network is now Duke Capital Partners
On Wednesday, Nov. 9, Duke Angel Network rolled out a new name and website.
Duke Capital Partners is the early-stage venture investing arm of Duke University, helping to connect Duke alumni investors with Duke-affiliated early-stage companies. Duke Capital Partners provides capital and expertise to help Duke start-ups, and features one of Duke’s most innovative experiential learning opportunities for students. As one of the largest and oldest university investment entities of its kind, Duke Capital Partners consistently places among the top five in North America.
It is hoped that faculty, students, and alumni will find Duke Capital Partners to be an exciting new way to engage with the university and its entrepreneurial community.
Link for Real Talk with Craig Albanese
If you missed last week’s Real Talk with Craig Albanese, MD, MBA, Executive Vice President and Chief Operating Officer of Duke University Health System, please click here to learn more about how the expertise and dedication of our financial care counselors have allowed DUHS to provide more than $141 million in direct financial assistance to patients every year. The incredible work this team does every day makes a huge difference to our patients and their families.
CulturePulse 2022 — Be Heard
The Culture Pulse survey link will remain open through Nov. 16; CulturePulse is a way for team members to share their feedback about what’s going well and what could be improved at Duke Health. Please participate and encourage your team members to do so as well. You will receive automatic reminders about the survey until you complete it or it closes. This is a great opportunity for all of us to have our voices heard.
This Week: Matters of Grief Symposium 2022
The Duke Health Office of Culture and Well-being is offering a Grief Symposium 2022 on Tues., Nov. 15 and a panel discussion on Wed., Nov. 16. Please consider joining for one or more events (most are virtual) in which they and participants will explore the many aspects of grief, including common grief reactions, how to support those who are grieving, professional grief, grief around loss of function or role, disenfranchised grief, rituals that may help us in the grieving process, and how to turn grief into positive action. Register here (please use your Duke e-mail to complete your registration).
- Grief Symposium: Tues., Nov. 15, noon-2 p.m.
- Grief Panel Discussion: Wed., Nov. 16, 1-2 p.m.
- Small Group Interactive Activities including Somatic Body Work, Narrative Writing, Mandala Art, and Restorative Circles for Personal Grief, Pet Grief, and Gun Violence: Wed-Fri, Nov. 16-18.
To learn more, please visit: https://cultureandwellbeing.dukehealth.org/grief-toolkit-symposium. A link to last year’s symposium is available on that page.
Reminder! ORA Holiday Deadlines
The Office of Research Administration (ORA) will operate with reduced staff during the holiday season. Please plan in advance based on the following:
Thanksgiving Day and the Friday After
If you need something processed BEFORE the Thanksgiving holiday, please have it submitted in ready-form to ORA by Thursday, November 17. Otherwise, if it can wait, ORA will process the following week (beginning November 28).
Last two weeks of December
For any transactions with due dates between December 19 – January 2, please have submitted in ready-form to ORA by Thursday, December 15 to ensure there is adequate time and staffing to respond to your needs.
Please note: the next NIH SBIR/STTR deadline is Jan. 5, 2023, and the internal deadline is 8 a.m. on Dec. 28, 2022. Because this deadline falls in the last two weeks in December when ORA will be operating with reduced staff and because these award mechanisms are usually complex and require careful institutional coordination before submission:
- Please complete Intent to Submit for all planned SBIR/STTR applications no later than Dec. 5, 2022; and
- Please plan to route a submission-ready application no later than Dec. 15, 2022; if more time is needed, please submit a late waiver request so that ORA can plan for appropriate coverage to support these applications.
ORA will be back up to speed with a full team on Jan. 3, 2023 and will look forward to managing all pending issues at that time.
Additional Reminders:
- It is vital that we remain vigilant with masking, hand hygiene, PPE, and other safe behaviors to prevent the spread of infection. Please pay special attention to the proper wearing and securing of gowns and be mindful of PPE compliance. Thank you for all you do to keep everyone safe and healthy.
- November is American Diabetes Month, Pulmonary Hypertension Awareness Month, and National COPD Awareness Month. Thanks for all you do to help patients with these conditions!
- The deadline for staff flu vaccinations is Tuesday, Nov. 15 at 10 a.m. Vaccination sites for faculty and staff can be found here: https://flu.duke.edu/vaccination/employees/
Upcoming Events & Opportunities
Cardiology Grand Rounds
November 15: AHA Recap with Manesh Patel, L. Kristin Newby, Robert Mentz and Pamela Douglas. 5 p.m., Webex only. https://duke.is/pqv6g.
November 22: Fellow presentation with Ali Corley. 5 p.m., Webex. Watch your email for the link.
CME & Other Events
November 14: Prostate Cancer & CVD Symposium, Webinar 4. Final of a four-part webinar series. Collaboration between the International Cardio-Oncology Society & Duke Heart. Noon, Eastern. Free. To register visit https://duke.is/ptjbs.
Call for abstracts: 2023 Duke Health Quality and Safety Conference
The virtual poster submission period for the 2023 Duke Health Quality and Safety Conference is now open. The deadline for submission is Wednesday, Dec. 14. The 2023 Conference will be held the weeks of March 13 and 20, with an in-person event on Thursday, March 23.
For more information and to submit your abstract, please click here.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
November 5 — Betty Tong
WNCN CBS-17
Health experts urge screening for lung cancer for early detection
https://duke.is/5dz6a
November 5 — Robert Mentz
Medpage Today
Furosemide Holds Up to Newer, Stronger Loop Diuretic During HF Hospitalization
https://duke.is/n3qy8
*also carried by 3 additional outlets
November 5 — Robert Mentz
tctMD
TRANSFORM-HF: Torsemide No Better Than Furosemide for Hospitalized HF
https://duke.is/pmzgz
*also carried by 11 additional industry & scientific outlets
November 5 — Robert Mentz and Manesh Patel
Healio/Cardiology
Loop diuretic choice does not reduce all-cause death in HF: TRANSFORM-HF
https://duke.is/9zbfd
*also carried by Newsbreezer
November 5 — Robert Mentz
Medscape
No Survival Advantage for Either Torsemide or Furosemide in HF: TRANSFORM-HF
https://duke.is/24psp
*also carried by 4 additional industry & scientific outlets
November 5 — Manesh Patel
tctMD
Pemafibrate Fails to Lower CVD Risk in Patients With High Triglycerides: PROMINENT
https://duke.is/z5fg9
November 5 — Robert Mentz
Archynetys.com
Furosemide tolerates new, a lot more potent loop diuretics in hospitalized heart failure
https://duke.is/gvfdh
November 5 — Robert Mentz
ACC.org
Torsemide Comparison With Furosemide for Management of Heart Failure – TRANSFORM-HF
https://duke.is/vecc9
November 6 — Robert Mentz
News-Medical.net
Two heart failure therapies prove to be nearly identical in reducing death
https://duke.is/m9q9m
*also carried by 2 additional industry & scientific outlets
November 6 — Robert Mentz
Pharmacy Times
Trial Finds No Benefit with Torsemide Versus Furosemide in Heart Failure
https://duke.is/4we3g
November 6 — Kevin Hill
Medpage Today
Definitive Answer on Steroids for Infant Heart Surgery Falls Short
https://duke.is/w2pny
*also carried by 4 additional outlets
November 6 — Kevin Hill
Healio/Cardiology Today
Methylprednisolone does not reduce odds of poor outcomes in infant heart surgery
https://duke.is/6tpe6
November 6 — Kevin Hill
AHA Newsroom
Steroids during surgery may not be helpful for infants having heart bypass
https://duke.is/puftb
November 6 — Pamela Douglas
tctMD
PRECISE CT-Based Strategy Allows Clinicians to ‘Do Less’ for Stable Chest Pain
https://duke.is/5ye8w
November 6 — Pamela Douglas
Healio/Cardiology
Precision testing strategy strongly benefits stable patients with suspected CAD
https://duke.is/nschn
*also carried by Knowledgia News
November 6 — Pamela Douglas
Postsus (Spain)
Los pacientes con dolor torácico se benefician del enfoque de pruebas diagnósticas de precisión
https://duke.is/baes8
*also carried by 9 additional industry & scientific outlets
November 6 — Pamela Douglas
HeartFlow
https://duke.is/4cq2c
*also carried by 38 additional industry & scientific outlets
November 6 — Pamela Douglas
News-Medical.net
New risk analysis strategy benefits chest pain patients compared to the usual testing approach
https://duke.is/9vzcg
November 6 — Pamela Douglas
AHA Newsroom
Personalized evaluation for chest pain effective, may eliminate unnecessary testing
https://duke.is/j3zkj
*also carried by 7 additional industry & scientific outlets
November 6 — Pamela Douglas
CRTOnline.org
https://duke.is/gm23p
November 6 — Manesh Patel
Healio/Cardiology
VIDEO: Takeaways from AHA 2022 with Manesh R. Patel
https://duke.is/bcc6t
November 6 — Pamela Douglas
Applied Radiology
Risk-Analysis Strategy Best Approach for New-Onset Chest Pain Patients
https://duke.is/ygzbu
November 7 — Stephen Greene
Biospace.com
Cytokinetics Presents New Data at the American Heart Association Scientific Sessions 2022
https://duke.is/vwpyr
*also carried by 4 additional industry & scientific outlets
November 7 — Pamela Douglas
Cardiovascular Business
AI-powered CCTA outperforms usual care when evaluating stable chest pain
https://duke.is/rbcv4
*also carried by Roxx Cloud
November 7 — Stephen Greene
AJMC
Dr Stephen J. Greene: New VICTORIA Trial Data Show Benefit to Vericiguat In-Hospital Initiation
https://duke.is/n67n5
November 7 — Robert Mentz
Medical Dialogues
Torsemide Does Not Confer Any Survival Benefit Over Furosemide in HF: TRANSFORM HF Trial
https://duke.is/zxe4e
November 7 — Jonathan Piccini
tctMD
Botulinum Toxin Injections No Help for Postoperative AF: NOVA
https://duke.is/chpzs
November 7 — Manesh Patel
U.S. News & World Report
Experimental Pill May Be New Way to Control Cholesterol
https://duke.is/wdf73
*also carried by 249 additional outlets including by HealthDay, United Press International and in Chicago, Houston & Philadelphia
November 7 — Vishal Rao
tctMD
New Tool Assesses Risk in Acute HF Then Suggests Next Steps, Cutting Later Events
https://duke.is/jbq87
November 7 — Duke University (PRECISE study)
Spectrum News Carolinas
Strategy for diagnostic testing benefits chest pain patients
https://duke.is/rkexa
(*clip begins @ 11:00:25)
November 7 — Kevin Hill
Medscape
Steroids Fail to Deliver Clear Benefits in Infant Heart Surgery
https://duke.is/5qbuq
November 7 — Pamela Douglas
MDedge
Precision CAD testing shows 70% cut in composite risk at 1 year
https://duke.is/vm6jx
November 8 — Robert Mentz
UPI
Switching diuretics may not make a difference in treating heart failure
https://duke.is/z6sc6
November 8 — Robert Mentz
U.S.News & World Report
Study Compares 2 Common Diuretics Used in Heart Failure
https://duke.is/8duxp
November 8 — Pamela Douglas
Medpage Today
Precision Medicine Strategy Reduced Testing in Patients With Chest Pain
https://duke.is/cc68r
November 8 — Renato Lopes
Medpage Today
Anticoagulation Again Flops for Outpatient COVID-19
https://duke.is/6kdnc
November 9 — Jonathan Piccini
Medpage Today
Can Botox for the Heart Ward Off Afib After Cardiac Surgery?
November 11 — Vishal Rao
Healio/Cardiology
In-hospital peer-to-peer consult may improve guideline-directed therapy in HFrEF
Division of Cardiology Publications Indexed in PubMed October 27 – November 9, 2022
Adamson C, Kondo T, Jhund PS, de Boer RA, Cabrera Honorio JW, Claggett B, Desai AS, Alcocer Gamba MA, Al Habeeb W, Hernandez AF, Inzucchi SE, Kosiborod MN, Lam CSP, Langkilde AM, Lindholm D, Bachus E, Litwin SE, Martinez F, Petersson M, Shah SJ, Vaduganathan M, Nguyen Vinh P, Wilderäng U, Solomon SD, McMurray JJV. Dapagliflozin for heart failure according to body mass index: the DELIVER trial. Eur Heart J 2022 Nov 1;43(41):4406-4417. PM: 36029309.
Batra G, Lindbäck J, Becker RC, Harrington RA, Held C, James SK, Kempf T, Lopes RD, Mahaffey KW, Steg PG, Storey RF, Swahn E, Wollert KC, Siegbahn A, Wallentin L. Biomarker-Based Prediction of Recurrent Ischemic Events in Patients With Acute Coronary Syndromes. J Am Coll Cardiol 2022 Nov 1;80(18):1735- 1747. PM: 36302586.
Blumenthal JA, Smith PJ, Jiang W, Hinderliter A, Watkins LL, Hoffman BM, Kraus WE, Mabe S, Liao L, Davidson J, Sherwood A. Exercise and Escitalopram in the Treatment of Anxiety in Patients with Coronary Heart Disease: One Year Follow- Up of the UNWIND Randomized Clinical Trial. J Cardiovasc Dev Dis 2022 Sep 22;9(10):320. PM: 36286272.
Butler J, Anker SD, Lund LH, Coats AJS, Filippatos G, Siddiqi TJ, Friede T, Fabien V, Kosiborod M, Metra M, Piña IL, Pinto F, Rossignol P, van der Meer P, Bahit C, Belohlavek J, Böhm M, Brugts JJ, Cleland JGF, Ezekowitz J, Bayes-Genis A, Gotsman I, Goudev A, Khintibidze I, Lindenfeld J, Mentz RJ, Merkely B, Montes EC, Mullens W, Nicolau JC, Parkhomenko A, Ponikowski P, Seferovic PM, Senni M, Shlyakhto E, Cohen-Solal A, Szecsödy P, Jensen K, Dorigotti F, Weir MR, Pitt B. Patiromer for the management of hyperkalemia in heart failure with reduced ejection fraction: the DIAMOND trial. Eur Heart J 2022 Nov 1;43(41):4362-4373. PM: 35900838.
Butt JH, Kondo T, Jhund PS, Comin-Colet J, de Boer RA, Desai AS, Hernandez AF, Inzucchi SE, Janssens SP, Kosiborod MN, Lam CSP, Langkilde AM, Lindholm D, Martinez F, Petersson M, Shah SJ, Thierer J, Vaduganathan M, Verma S, Wilderäng U, Claggett BC, Solomon SD, McMurray JJV. Atrial Fibrillation and Dapagliflozin Efficacy in Patients With Preserved or Mildly Reduced Ejection Fraction. J Am Coll Cardiol 2022 Nov 1;80(18):1705- 1717. PM: 36041668.
Campbell MM, Benjamin DK, Mann TK, Fist A, Blakemore A, Diaz KS, Kim H, Edwards LJ, Rak Z, Brookhart MA, Moore Z, Tilson EC, Kalu I, Boutzoukas AE, Moorthy GS, Uthappa D, Scott Z, Weber DJ, Shane AL, Bryant KA, Zimmerman KO. Test-to-Stay After SARS-CoV-2 Exposure: A Mitigation Strategy for Optionally Masked K-12 Schools. Pediatrics 2022 Nov 1;150(5):e2022058200. PM: 35971240.
Diamond J, DeVore AD. New Strategies to Prevent Rehospitalizations for Heart Failure. Curr Treat Options Cardiovasc Med 2022;24(12):199-212. PM: 36164396.
Dunbar TK, Olsen MK, Yang H, Kennedy D, Jackson LR, Thomas KL, Alkon A, Prose NS, Pollak KI. Characteristics Associated with Burnout among Cardiologists in an Academic Medical Setting: Baseline Survey Results from a Communication Coaching RCT. Behav Sci (Basel) 2022 Sep 27;12(10):362. PM: 36285931.
Fitch KV, McCallum SA, Erlandson KM, Overton ET, Zanni MV, Fichtenbaum C, Aberg JA, Fulda ES, Kileel EM, Moran LE, Bloomfield GS, Novak RM, Pérez-Frontera S, Abrams-Downey A, Pierone G, Kumarasamy N, Ruxrungtham K, Mngqibisa R, Douglas PS, Ribaudo HJ, Grinspoon SK. Diet in a global cohort of adults with HIV at low-to- moderate traditional cardiovascular disease risk. AIDS 2022 Nov 15;36(14):1997-2003. PM: 35876637.
Freedman NJ. From Colon to Aortic Aneurysm: Trek of the Treg. JACC Basic Transl Sci 2022 Sep 26;7(9):948- 950. PM: 36317127.
Fudim M, Shahid I, Emani S, Klein L, Dupuy- McCauley KL, Zieroth S, Mentz RJ. Evaluation and Treatment of Central Sleep Apnea in Patients with Heart Failure. Curr Probl Cardiol 2022 Dec;47(12):101364. PM: 35995244.
Gargiulo G, Giacoppo D, Jolly SS, Cairns J, Le May M, Bernat I, Romagnoli E, Rao SV, van Leeuwen MAH, Mehta SR, Bertrand OF, Wells GA, Meijers TA, Siontis GCM, Esposito G, Windecker S, Jüni P, Valgimigli M. Effects on Mortality and Major Bleeding of Radial Versus Femoral Artery Access for Coronary Angiography or Percutaneous Coronary Intervention: Meta-Analysis of Individual Patient Data From 7 Multicenter Randomized Clinical Trials. Circulation 2022 Nov;146(18):1329-1343. PM: 36036610.
Metkus TS, Baird-Zars VM, Alfonso CE, Alviar CL, Barnett CF, Barsness GW, Berg DD, Bertic M, Bohula EA, Burke J, Burstein B, Chaudhry SP, Cooper HA, Daniels LB, Fordyce CB, Ghafghazi S, Goldfarb M, Katz JN, Keeley EC, Keller NM, Kenigsberg B, Kontos MC, Kwon Y, Lawler PR, Leibner E, Liu S, Menon V, Miller PE, Newby LK, O’Brien CG, Papolos AI, Pierce MJ, Prasad R, Pisani B, Potter BJ, Roswell RO, Sinha SS, Shah KS, Smith TD, Snell RJ, So D, Solomon MA, Ternus BW, Teuteberg JJ, van Diepen S, Zakaria S, Morrow DA. Critical Care Cardiology Trials Network (CCCTN): a cohort profile. Eur Heart J Qual Care Clin Outcomes 2022 Oct 26;8(7):703-708. PM: 36029517.
Minhas AMK, Jain V, Maqsood MH, Pandey A, Khan SS, Fudim M, Fonarow GC, Butler J, Khan MS. Non-Alcoholic Fatty Liver Disease, Heart Failure, and Long-Term Mortality: Insights From the National Health and Nutrition Examination Survey. Curr Probl Cardiol 2022 Dec;47(12):101333. PM: 35901855.
Myhre PL, Prescott MF, Claggett B, Felker GM, Butler J, Piña IL, Maisel AS, Williamson KM, Ward JH, Solomon SD, Januzzi JL. Comparative Effect of Angiotensin Receptor Neprilysin Inhibition on B-type Natriuretic Peptide Levels Measured by Three Different Assays: The PROVE-HF Study. Clin Chem 2022 Nov 3;68(11):1391-1398. PM: 36103292.
Park DY, Hanna JM, Kadian S, Kadian M, Jones WS, Damluji AA, Kochar A, Curtis JP, Nanna MG. In-hospital outcomes and readmission in older adults treated with percutaneous coronary intervention for stable ischemic heart disease. J Geriatr Cardiol 2022 Sep 28;19(9):631-642. PM: 36284680.
Salah HM, Verma S, Santos-Gallego CG, Bhatt AS, Vaduganathan M, Khan MS, Lopes RD, Al’Aref SJ, McGuire DK, Fudim M. Sodium-Glucose Cotransporter 2 Inhibitors and Cardiac Remodeling. J Cardiovasc Transl Res 2022 Oct;15(5):944-956. PM: 35290593.
Siddiqi TJ, Ahmed A, Greene SJ, Shahid I, Usman MS, Oshunbade A, Alkhouli M, Hall ME, Murad MH, Khera R, Jain V, Van Spall HGC, Khan MS. Performance of current risk stratification models for predicting mortality in patients with heart failure: a systematic review and meta-analysis. Eur J Prev Cardiol 2022 Nov 8;29(15):2027-2048. PM: 35919956.
Siddiqi TJ, Khan Minhas AM, Greene SJ, Van Spall HGC, Khan SS, Pandey A, Mentz RJ, Fonarow GC, Butler J, Khan MS. Trends in Heart Failure-Related Mortality Among Older Adults in the United States From 1999-2019. JACC Heart Fail 2022 Nov;10(11):851-859. PM: 36328654.
Srinivasan ES, Wang TY, Rapoport A, Erickson MM, Abd-El-Barr MM, Shaffrey CI, Than KD. Minimally invasive lateral retroperitoneal transpsoas approach for lumbar corpectomy and fusion with posterior instrumentation. Neurosurg Focus Video 2022 Jul 1;7(1):V7. PM: 36284723.
Tomaszewski WH, Waibl-Polania J, Chakraborty M, Perera J, Ratiu J, Miggelbrink A, McDonnell DP, Khasraw M, Ashley DM, Fecci PE, Racioppi L, Sanchez-Perez L, Gunn MD, Sampson JH. Neuronal CaMKK2 promotes immunosuppression and checkpoint blockade resistance in glioblastoma. Nat Commun 2022 Oct 29;13(1):6483. PM: 36309495.
Vaduganathan M, Claggett BL, Jhund P, de Boer RA, Hernandez AF, Inzucchi SE, Kosiborod MN, Lam CSP, Martinez F, Shah SJ, Desai AS, Lindholm D, Petersson M, Langkilde AM, McMurray JJV, Solomon SD. Estimated Long-Term Benefit of Dapagliflozin in Patients With Heart Failure. J Am Coll Cardiol 2022 Nov 8;80(19):1775-1784. PM: 36041669.
Vaios EJ, Batich KA, Buckley AF, Dunn-Pirio A, Patel MP, Kirkpatrick JP, Goudar R, Peters KB. Addendum: Resolution of radiation necrosis with bevacizumab following radiation therapy for primary CNS lymphoma. Oncotarget 2022 Oct 20;13:1165. PM: 36289014.
White EJ, Susman SJ, Bouffler A, Leahy JC, Griffin SM, Christenson R, Newby LK, Gordee A, Kuchibhatla M, Limkakeng AT. Predictors of Stress-Delta High-Sensitivity Troponin T in Emergency Department Patients Undergoing Stress Testing. Cureus 2022 Sep 26;14(9):e29601. PM: 36321030.
Yazdi D, Patel S, Ozonat K, Fudim M, Smith S, Centen C. Feasibility of a Cardiac Scale in Measuring Blood Pressure. J Cardiovasc Transl Res 2022 Oct;15(5):1212-1214. PM: 35396626.
Duke Heart Pulse – November 6th 2022
Chief’s message:
This weekend is the kickoff of the American Heart Association Scientific Sessions 2022 in person with a virtual component in Chicago. The meeting has gotten off to a great start with many presentations of science from Duke Faculty and Fellows, opportunities to connect and see people in person, and in general get to participate and see science (much of which is not related to COVID). The meeting also highlights for us the amazing colleagues, connections, and people that we have had through the years as part of the Duke Fellowship, Faculty, and research and clinical collaborations. It is humbling to be the Chair for this years AHA Scientific Sessions. I was reminded as well about our mission and responsibility in the opening session for the AHA that included two US Surgeons General (Jerome Adams and Regina Benjamin), FDA Director Rob Califf, and AHA president Michelle Albert and World Heart Federation president Fausto Pinto. These scientific session meetings and even our own meetings at Duke with our faculty and fellows to discuss clinical care and science have highlighted how energizing and reinvigorating in person engagement is for us all.


Highlights of the week:
Scientific Sessions Kicks Off in Chicago!
So many of our team members throughout Duke Heart and the Duke Clinical Research Institute have been preparing for the 2022 American Heart Association’s Scientific Sessions and it’s finally here. We’ll have coverage this weekend and next to showcase as much of it as we can.
We are extremely proud of all the work – from the research done at (and in partnership with) Duke that will be presented during Sessions, to the effort that has gone into planning this event at the national level, to the work done to organize our annual presence in the Exhibit Hall – it takes a lot of planning and effort by a lot of people. On behalf of the Duke Heart leadership team, thank you.
We kick off our coverage this weekend with two of our late-breaking clinical trial presentations and close out with two award winners.
We hope those of you who have traveled to be in Chicago this weekend are having a great time. Once again, congratulations to all, and thank you for all that you do!
AHA.22 LBCT: Comparative Study of Two Heart Failure Drugs Finds No Difference in Outcomes
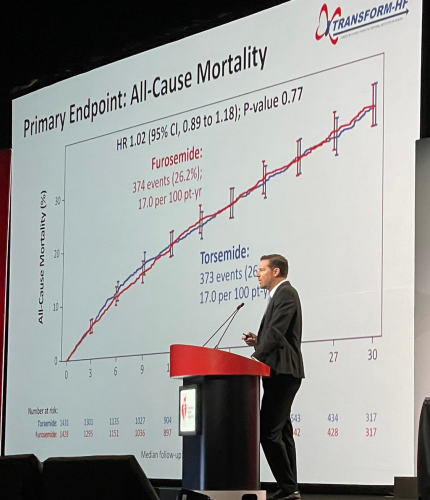 In a head-to-head comparison of two so-called ‘water pills’ that keep fluid from building up in patients with heart failure, the therapies proved nearly identical in reducing deaths, according to a large study led by Duke Health researchers.
In a head-to-head comparison of two so-called ‘water pills’ that keep fluid from building up in patients with heart failure, the therapies proved nearly identical in reducing deaths, according to a large study led by Duke Health researchers.
The study compared the diuretics torsemide and furosemide that were prescribed to patients with heart failure starting in the hospital setting. While prior data suggested a potential reduction in deaths among patients taking torsemide, the current study found no such benefit, providing clarity for both doctors and patients.
“Given that the two different therapies provide the same effect on outcomes, we shouldn’t spend time switching patients from one to the other, and instead concentrate on giving the right dose and adjusting other therapies that have been proven to have long-term benefits,” said cardiologist Robert J. Mentz, MD, chief of the heart failure section in the Division of Cardiology at Duke University School of Medicine and member of the Duke Clinical Research Institute.
Mentz was lead author of the study, called TRANSFORM-HF and funded by the National Heart, Lung and Blood Institute. He presented the findings as a late-breaking clinical trial yesterday at the American Heart Association’s 2022 Scientific Sessions in Chicago.
The study was designed as a direct comparison of loop diuretics, which are commonly prescribed to reduce the fluid buildup that causes swelling and breathing difficulties in patients with heart failure.
Mentz and colleagues enrolled more than 2,800 patients hospitalized with heart failure. Participants were randomly assigned to receive either torsemide or furosemide, and doctors determined the dosing. The study group was diverse, with women comprising 37% of participants and Black patients comprising 34%.
The main question was whether torsemide reduced patient deaths due to any cause over long-term follow-up (average of more than 17 months). The researchers found that death occurred in 373 of 1,431 study participants (26.1%) in the torsemide group and 374 of 1,428 patients (26.2%) in the furosemide group.
A secondary outcomes analysis looked at deaths or hospitalizations within 12 months, and again found little difference, with death or hospitalization occurring in 677 patients (47.3%) in the torsemide group and 704 patients (49.3%) in the furosemide group.
“This study has immediate clinical applications,” Mentz said. “Doctors spend a lot of time considering whether they will change from one diuretic to another, but there is no difference between the two for outcomes. This provides much-needed clarity. The insights from TRANSFORM-HF add to the evidence base that should help us improve patient care.”
In addition to Mentz, study authors include Kevin J. Anstrom, Eric L. Eisenstein, Shelly Sapp, Stephen J. Greene, Shelby Morgan, Jeffrey M. Testani, Amanda H. Harrington, Vandana Sachdev, Fassil Ketema, Dong-Yun Kim, Patrice Desvigne-Nickens, Bertram Pitt, and Eric J. Velazquez.
Congratulations to all TRANSFORM-HF team members – nicely done!
AHA.22 LBCT: Largest Randomized Trial Evaluates Steroids for Infant Heart Surgery
For more than four decades, doctors have been split on whether giving steroids during a pediatric open-heart surgery could be helpful for post-operative recovery. A new study is providing a bit more clarity, suggesting there are some benefits for certain kinds of patients.
Led by Duke Health researchers, the study was the largest trial designed to resolve the long-standing issue. More than 1,200 infants with heart disease were enrolled at 24 U.S. centers, with roughly half randomly assigned to receive steroids prior to heart surgeries, and the other half randomized to receive a placebo.
The main focus was whether prophylactic steroid use reduced any of more than a dozen complications, including death and heart transplant, compared to a placebo.
In the primary analysis, the researchers found no differences in the two groups, but steroid use was associated with elevated blood-sugar levels that required insulin therapy in some cases. Results showed 19% of participants using steroids required insulin therapy, compared to 8% in the placebo group. However, like many trials, the results were more nuanced and secondary analyses showed that some children might benefit.
The findings appear Nov. 6 in the New England Journal of Medicine and were presented this morning at the AHA’s 2022 Scientific Sessions.
Lead author of the study, Kevin Hill, MD, a member of the DCRI and chief of the Division of Pediatric Cardiology at Duke University School of Medicine, described the nuances of the study. Secondary results suggested that patients with less complex cases might be the ones who do better with steroids.
“Steroids reduce inflammation, and their benefit may be highest in children undergoing less complex procedures where inflammation is manageable,” Hill said. “But when you have the most complicated patients with severe inflammation affecting multiple organ systems, using steroids is like throwing a glass of water on a forest fire, and they seem to have less impact.”
Jennifer S. Li, MD, is the senior author of the paper and a professor in the departments of Pediatrics and Medicine at Duke. She says there’s a need for further study.
“We need to hone in on the patients who can actually benefit most from steroid use and develop a targeted approach to using this medicine, so that we maximize its benefit and minimize adverse effects,” Li said.
The DCRI performed the trial administration, data management and statistical analyses. The study was performed as a “trial within a registry” leveraging the infrastructure of the Society of Thoracic Surgeons Congenital Heart Surgery Database to conduct a low cost, pragmatic trial.
In addition to Hill and Li, study authors include, Prince J. Kannankeril, Jeffrey P. Jacobs, H. Scott Baldwin, Marshall L. Jacobs, Sean M. O’Brien, David P. Bichel, Eric M. Graham, Brian Blasiole, Ashraf Resheidat, Adil S. Husain, S. Ram Kumar, Jerry L. Kirchner, Dianne S. Gallup, Joseph W. Turek, Mark Bleiweis, Bret Mettler, Alexis Benscoter, Eric Wald, Tara Karamlou, Andrew H. Van Bergen, David Overman, Pirooz Eghtesady, Ryan Butts, John S. Kim, John P. Scott, Brett R. Anderson, Michael F. Swartz, Patrick I. McConnell, David F. Vener, and the STRESS Network Investigators.
Well done, team! Congratulations!
AHA.22: Presenters and Session Moderators
Between today and yesterday there were 35 Abstract Poster Session presentations by Duke Heart team members including Stephen Greene, Shahzeb Khan, Michelle Kelsey, Caitlin Drescher, Josephine Harrington, Michael Cosiano, Anand Shah, Jenn Rymer, Nishant Shah, and Conrad Hodgkinson – just to name a few.
Cardiology fellow Michael Cosiano presented “Comparing Patient Reported Outcomes and New York Heart Association Class Among Patients Hospitalized for Heart Failure” during abstract poster sessions on Saturday. He is lead author on the paper that was simultaneously published in Circulation: Heart Failure. His co-authors include Andrew Vista, Jie-lena Sun, Brooke Alhanti, Josephine Harrington, Adrian Hernandez, Robert Mentz, Stephen Greene, et al. This paper earned Cosiano recognition as a Circulation: Heart Failure (Circ HF) “Emerging Investigator.” Circ HF editors will feature his work as part of their series highlighting young investigators—defined as individuals less than ten years out of training—in the fields of heart failure, mechanical circulatory support, cardiac transplantation, and pulmonary hypertension. Additionally, this paper will be the focus of an upcoming Twitter journal club sponsored by Circ HF. Way to go, Michael!
Internal Medicine resident Anand Shah presented findings on the study, “In-Hospital Virtual Peer-to-Peer Consultation to Improve Guideline-Directed Medical Therapy for Heart Failure: A Pilot Randomized Trial” which was a Duke Heart Failure team and hospitalist-led pilot program on multidisciplinary care for hospitalized patients with heart failure. The presentation was done during a poster session held yesterday. The study findings were published online earlier this week in Circulation: Heart Failure. ICYMI, Vishal Rao was interviewed by TCTMD about the team’s findings. The TCTMD article was published earlier this week and appears in our News section below. (This was Rao’s first phone interview related to his research and he did a great job explaining the work done by the team. Great job, Vishal!). Other authors on the study include Jamie McDermott, Stephanie Barnes, Evan Murray, Michelle Kelsey, Stephen Greene, Marat Fudim, Adam Devore, Mike Blazing, Cara O’Brien, and Rob Mentz.
Findings from the study, “Adoption of Sacubitril/Valsartan in Patients with Heart Failure with Mildly Reduced or Preserved Ejection Fraction: The AHA Get With the Guidelines – Heart Failure Registry,” were presented during a poster session yesterday by Duke internal medicine resident Jacob Pierce. His co-authors include Zhen Li, Melissa Greiner, Steven Lippmann, Natalie Chantelle Hardy, Robert Mentz, Emily O’Brien, and Stephen Greene. The team’s findings were simultaneously published in Circulation: Heart Failure.
Cardiology fellow Jessie Duran presented “Abnormal Exercise Electrocardiography With Normal Stress Echocardiography is Associated With Increased Subclinical Coronary Atherosclerosis: Insights From the Project Baseline Health Study” yesterday during an oral session. Duran highlighted residual cardiovascular risk in a group of patients with positive ECG but negative stress echo. Well done!
Additionally, plenty of our Duke team members served as moderators for sessions throughout the day Saturday. They included: Andrew Landstrom, Larry Jackson, Sreekanth Vemulapalli, Manesh Patel, Neha Pagidipati, Jennifer Rymer, Jason Katz, Bradi Granger, Adrian Hernandez, Howard Rockman, Emily O’Brien, L. Kristen Newby and Rob Mentz.
We have an outstanding presence at Sessions this year! Great work everyone.
AHA.22: Douglas, Shah Honored with Council Awards
 We’re incredibly proud of Duke Heart team members Pamela Douglas, MD, and Svati Shah, MD. Both received awards last night during separate events at the AHA Scientific Sessions.
We’re incredibly proud of Duke Heart team members Pamela Douglas, MD, and Svati Shah, MD. Both received awards last night during separate events at the AHA Scientific Sessions.
Douglas was selected to receive the James B. Herrick Award for Outstanding Achievement in Clinical Cardiology by the AHA’s Council on Clinical Cardiology. Douglas delivered the James B. Herrick Lecture as part of the AHA’s Council Named Lecture Series held during Sessions. The series features lectures from some of today’s foremost clinicians and researchers as well as those with a lifetime of

contributions to the field of cardiovascular disease. Congratulations, Pam!
Shah was selected to receive the Genomic and Precision Medicine Mentoring Award by the AHA’s Council on Genomic and Precision Medicine. It was presented to her last night during the Council’s annual reception held this year in the Field Ballroom at the Hyatt Regency McCormick Place. Congratulations, Svati!
Frazier-Mills to Co-Lead ABC EP Committee

We are excited to share that electrophysiologist Camille Frazier-Mills, MD has been named co-chair of the Association of Black Cardiologists (ABC) Electrophysiology Committee. Her appointment is effective immediately and ends in April, 2024.
Congratulations, Camille! This is a tremendous honor!
CPR Performed by Duke Team Saves In-flight Passenger
 Duke Heart CVSSU team member Kaitlyn Allen and her husband, Justin Allen, MD, a Duke hospitalist, were recently in Utah so that Justin could compete in the 2022 Half Ironman World Championship race held Oct. 29 in St. George. On Tuesday, Nov. 1 while flying home toward RDU, a medical emergency was declared approximately 40 minutes into their three-hour flight. Both were nearby when a flight attendant yelled for an AED; Kaitlyn saw a passenger lying on her back in the middle of the aisle in the cabin ahead of her.
Duke Heart CVSSU team member Kaitlyn Allen and her husband, Justin Allen, MD, a Duke hospitalist, were recently in Utah so that Justin could compete in the 2022 Half Ironman World Championship race held Oct. 29 in St. George. On Tuesday, Nov. 1 while flying home toward RDU, a medical emergency was declared approximately 40 minutes into their three-hour flight. Both were nearby when a flight attendant yelled for an AED; Kaitlyn saw a passenger lying on her back in the middle of the aisle in the cabin ahead of her.
She and Justin immediately ran to the passenger’s aid. When they arrived, another passenger – a pediatric physician assistant – was maintaining the passenger’s airway, but neither Kaitlyn nor the PA could feel a pulse. Kaitlyn immediately started chest compressions while Justin took over the airway and prepared the AED. After the second round of compressions, the patient began moving her arms and became responsive. The team then applied oxygen, the AED, and took a set of vitals. Another passenger who happened to be a medical ICU nurse provided a glucometer and a pulse oximeter. With the passenger’s vitals stable, Justin cleared the patient’s cervical spine and she was able to sit upright, and eventually get back into a seat.
Kaitlyn communicated directly with the pilot about the situation. Ultimately the passenger arrived in stable condition and upon landing was handed off to paramedics for further evaluation.
This was not the first time the Allen’s have been in an emergency situation together. The two worked together at Lakeland Health in St. Joseph, MI (Kaitlyn’s hometown) during Justin’s internal medicine residency. There, they worked together during rapid responses and code blues. Kaitlyn and Justin concur that it was their previous experiences that allowed them to operate as a cohesive unit during this in-flight emergency. Even in less-than-ideal conditions on a fully booked flight at 29,000 feet with limited medical equipment, they worked together quickly and professionally to save a fellow passenger’s life.
Great teamwork and use of CPR!
Shout-out to D’Amico, Antonia
We received a great message this week regarding a patient compliment for Tommy D’Amico and Scott Antonia:
“My experience in the hospital was excellent. All the personnel treated me extremely well. I am eternally appreciative to Dr. D’Amico and the dream team at Duke University Hospital. All the services of the hospital are excellent. My operation was a success & I am already recovered. My appreciation to Dr. D’Amico & Dr. Scott Antonia for all that they did for me. Thanks.” — a grateful patient (name withheld for privacy)
“Tommy and Scott, I was just delighted to read this lovely compliment about you both on our Patient Satisfaction Survey. Thank you for your excellence and compassion. You clearly made a difference in this patient’s life. Very best wishes, Lisa” — Lisa Clark Pickett, Chief Medical Officer, Duke University Hospital
Nice work!
Halloween Pics
The week started off with fun Halloween celebrations — check out this pumpkin carved by cardiology fellow Ilia Shadrin! That’s the Shadrin family dressed as The Incredibles, and Dennis Narcisse with his twin boys as dinosaurs. So adorable!
We love the holiday spirit shown by our Duke Heritage Cardiology team in Wake County. Your ‘Boo Crew’ t-shirts are awesome. What a great way to show your enthusiasm while providing amazing care to our patients. Great work!
Thank you to all who shared your holiday pics with us for Pulse. We love getting your submissions – please keep them coming.



Samuel L. Katz, doctor who helped develop measles vaccine, dies at 95
 We were saddened this week to learn of the passing of our long-time Duke Health colleague, Dr. Sam Katz. A luminary in the field of infectious diseases and pediatrics, Katz was a beloved team member at Duke. His work has impacted millions although few of them may realize it. Our deepest sympathy to his family, friends, and colleagues throughout the world.
We were saddened this week to learn of the passing of our long-time Duke Health colleague, Dr. Sam Katz. A luminary in the field of infectious diseases and pediatrics, Katz was a beloved team member at Duke. His work has impacted millions although few of them may realize it. Our deepest sympathy to his family, friends, and colleagues throughout the world.
Remembering Samuel L. Katz, MD
Samuel L. Katz, MD, died on Monday, October 31, 2022.
Dr. Katz was a world-renowned virologist, pediatrician, and chair emeritus and Wilburt C. Davison Professor Emeritus of Pediatrics at Duke University School of Medicine. He was an honors graduate of Dartmouth College and Harvard Medical School. After a medical internship at Beth Israel Hospital, he completed pediatrics residency training at the Massachusetts General Hospital and the Boston Children’s Hospital, followed by a research fellowship in virology and infectious diseases.
Dr. Katz then became a staff member at Children’s Hospital working with Nobel Laureate John F. Enders for the next 12 years researching viruses — specifically measles, a disease that at the time killed more than five to six million children each year globally. During this time, Drs. Katz and Enders developed an attenuated measles virus vaccine.
In 1960, David Morley, MD, a British physician working in Nigeria, where the effects of measles were far more severe than they were in the United States, contacted Dr. Katz. Together, they inoculated Nigerian children with the new vaccine, with successful results. Not long after, the vaccine was tested in national clinical trials, approved by the Food and Drug Administration in 1963, and is now used throughout the world.
In addition to the development of the measles vaccine, Dr. Katz worked extensively on a range of other vaccines, including vaccinia (used as smallpox vaccine), polio, rubella, influenza, pertussis (whooping cough), Haemophilus influenzae b conjugates, and HIV.
In 1968, Dr. Katz was appointed chair of the Duke Department of Pediatrics, where he served for 22 years. In addition to mentoring two decades of students and residents, he established an exchange program with Oxford University and provided training for an annual succession of residents from the American University of Beirut. Throughout his tenure he displayed genuine interest in his patients, faculty, and trainees, actively encouraging female and minority physicians and seeking to diversify the faculty.
“As he did for so many others, Dr. Katz had a profound influence on my career,” said School of Medicine Dean Mary E. Klotman, MD. “His commitment, passion, and warmth were infectious. Duke School of Medicine, Pediatrics, and the world are all the better because of him.”
“Dr. Katz has been a stellar role model for all of us, as a clinician, as a teacher, as an investigator, and as an advocate for children,” said Department of Pediatrics Chair Ann M. Reed, MD. “He set a high bar, advancing medicine in ways that have improved children’s health around the world–he is truly one of the outstanding pediatric investigators of our times.”
In addition to seeing patients and supporting faculty, Dr. Katz expanded his role as an advocate for vaccination. Experiencing firsthand the ways in which disease affects children living in resource-poor countries contributed to Dr. Katz’s lifelong advocacy, within the United States, and around the world. He chaired the Committee on Infectious Diseases of the American Academy of Pediatrics (AAP), the Advisory Committee on Immunization Practices (ACIP) of the Centers for Disease Control (CDC), the Vaccine Priorities Study of the Institute of Medicine (IOM), and several World Health Organization (WHO) vaccine and HIV panels. He served on the National Institutes of Health (NIH) Committee for AIDS Vaccines and co-chaired the India-U.S. Vaccine Action Program and the National Network for Immunization Information. In addition, he served as chair of the Public Policy Council of the Infectious Diseases Society of America (IDSA), co-chaired IDSA’s Vaccine Initiative, and worked on behalf of UNICEF and the American Red Cross.
Dr. Katz earned numerous accolades throughout his career, including the inaugural Joseph St. Geme, Jr. Leadership Award in 1988, the 2003 Albert B. Sabin Gold Medal awarded by the Sabin Vaccine Institute, and the 2015 Maxwell Finland Award for Scientific Achievement for his contributions to vaccine discoveries during his career.
Please see link to The Washington Post news brief about his death in our News section below.
Reminder: Voting Day is Tuesday, Nov. 8
Election Day is Tuesday, Nov. 8 and a list of polling locations can be found here. Visit the State Board of Elections website or vote.duke.edu for additional information. Please vote!!!
On Thursday, Nov. 10 from Noon – 1 p.m., the Duke State Relations team and Duke Health’s Government Relations team are offering a post-election briefing to discuss the outcomes of the 2022 Election, how it will impact Duke Health, and provide a preview of the 2023 legislative sessions in Raleigh and Washington, DC. This event will be moderated by Dev Sangvai, MD, interim president, Duke Regional Hospital. To participate via Zoom, visit https://duke.is/2eq4k.

CulturePulse 2022 — Be Heard
All Duke Health team members were emailed a link to the 2022 CulturePulse survey on Wednesday, Nov. 2. The brief survey is confidential, mobile-friendly, and simple to complete.
The survey link will remain open through Nov. 16; you can also find it via the QR code you’ll see on digital signage and printed flyers around Duke.
CulturePulse is a way for team members to share their feedback about what’s going well and what could be improved at Duke Health. Please participate and encourage your team members to do so as well. You will receive automatic reminders about the survey until you complete it or it closes. This is a great opportunity for all of us to have our voices heard.

ORA Holiday Deadlines
The Office of Research Administration (ORA) will operate with reduced staff during the holiday season to allow team members time to recharge. During this period, please plan as far in advance as possible.
To help ORA respond as timely as possible to your needs, please plan in advance based on the following:
Thanksgiving Day and the Friday After
If you need something processed BEFORE the Thanksgiving holiday, please have it submitted in ready-form to ORA by Thursday, November 17. Otherwise, if it can wait, ORA will process it the following week (beginning November 28).
Last two weeks of December
For any transactions with due dates between December 19 – January 2, please have them submitted in ready-form to ORA by Thursday, December 15 to ensure there is adequate time and staffing to respond to your needs.
Please note: the next NIH SBIR/STTR deadline is Jan. 5, 2023, and the internal deadline is 8 a.m. on Dec. 28, 2022. Because this deadline falls in the last two weeks in December when ORA will be operating with reduced staff and because these award mechanisms are usually complex and require careful institutional coordination before submission:
- Please complete Intent to Submit for all planned SBIR/STTR applications no later than Dec. 5, 2022; and
- Please plan to route a submission-ready application no later than Dec. 15, 2022; if more time is needed, please submit a late waiver request so that ORA can plan for appropriate coverage to support these applications.
For anything submitted in the last two weeks of December that can wait until after the holiday break, ORA will be back up to speed with a full team on Jan. 3, 2023 and will look forward to managing all pending issues at that time.
This has been another year of tremendous growth in research at Duke. The Office of Research Administration thanks you for your continued partnership in support of Duke’s research mission and they send warm holiday wishes to all!
Matters of Grief: Grief Symposium 2022
The Duke Health Office of Culture and Well-being is offering Grief Symposium 2022 on Tues., Nov. 15 and a panel discussion on Wed., Nov. 16. Please consider joining for one or more events (most are virtual) in which they and participants will explore the many aspects of grief, including common grief reactions, how to support those who are grieving, professional grief, grief around loss of function or role, disenfranchised grief, rituals that may help us in the grieving process, and how to turn grief into positive action. Register here (please use your Duke e-mail to complete your registration).
- Grief Symposium: Tues., Nov. 15, noon-2 p.m.
- Grief Panel Discussion: Wed., Nov. 16, 1-2 p.m.
- Small Group Interactive Activities: Wed-Fri, 11/16-11/18. These will include: Somatic Body Work, Narrative Writing, Mandala Art, and Restorative Circles: Personal Grief, Pet Grief, and Gun Violence.
To learn more, please visit: https://cultureandwellbeing.dukehealth.org/grief-toolkit-symposium. A link to last year’s symposium is available on that page.
Additional Reminders:
- It is vital that we remain vigilant with masking, hand hygiene, PPE, and other safe behaviors to prevent the spread of infection. Please pay special attention to the proper wearing and securing of gowns and be mindful of PPE compliance. Thank you for all you do to keep everyone safe and healthy.
- November is American Diabetes Month, Pulmonary Hypertension Awareness Month, and National COPD Awareness Month. Thanks for all you do to help patients with these conditions!
- The deadline for staff flu vaccinations is Tuesday, Nov. 15 at 10 a.m. Vaccination sites for faculty and staff can be found here: https://flu.duke.edu/vaccination/employees/
Upcoming Events & Opportunities
Cardiology Grand Rounds
November 8: Topic, presenter TBD. Watch your email for the Zoom link!
CME & Other Events
November 8: Election Day. Please vote!
November 8: DOM Research Quality Town Hall. Topic: 2023 NIH Data Management and Sharing Policy. 12-1 p.m. via Zoom. Register here. You must register to receive the Zoom link for the event.
November 14: Prostate Cancer & CVD Symposium, Webinar 4. Final of a four-part webinar series. Collaboration between the International Cardio-Oncology Society & Duke Heart. Noon, Eastern. Free. To register visit https://duke.is/ptjbs.
Call for abstracts: 2023 Duke Health Quality and Safety Conference
The virtual poster submission period for the 2023 Duke Health Quality and Safety Conference is now open. The deadline for submission is Wednesday, Dec. 14. The 2023 Conference will be held the weeks of March 13 and 20, with an in-person event on Thursday, March 23.
For more information and to submit your abstract, please click here.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
October 27 — Duke Clinical Research Institute
Reuters
U.S. government to test Pfizer’s Paxlovid for long COVID
https://duke.is/7nbtf
October 28 — Duke Health
CBS17.com
450+ turn out for Duke Health event to help caregivers in Durham
https://duke.is/g9zvx
October 28 — Joseph Turek and the Sinnamon family
KALB-TV (Alexandria, LA)
Health headlines: First-of-its-kind heart and thymus surgery proves successful
https://duke.is/ga2km
October 28 — Duke Health
Becker’s Hospital Review
https://duke.is/vfeed
October 28 — Duke Clinical Research Institute
MSN/Washington Examiner
NIH to use Pfizer’s Paxlovid to study causes of long COVID
https://duke.is/m6t8h
October 31 — Jonathan Piccini
Patientcareonline.com
https://duke.is/8cpbk
October 31 — Joseph Turek and the Sinnamon family
WFMZ-TV (Allentown, PA)
Doctors pioneer a heart transplant technique involving another life-saving procedure
https://duke.is/2hzxe
November 2 — Betty Tong
WNCN-CBS17.com
November is Lung Cancer Awareness Month; Duke doctor recommends screening
https://duke.is/zq27k
November 3 — Samuel Katz (pediatrics)
The Washington Post
Samuel L. Katz, doctor who helped develop measles vaccine, dies at 95
https://duke.is/mrcde
Duke Heart Pulse – October 30th 2022
Updates of the week:
Chancellor Washington to Leave Leadership Roles June 30
Most of you have heard the news regarding Dr. Washington’s decision to step down from his roles at Duke University and Duke University Health System. In case you missed his formal message to the Duke Health team, which was issued on Wednesday, Oct. 26, we are reprinting it here.
Dear Colleagues,

Since April 2015, I have had the great honor and privilege to serve as your Chancellor for Health Affairs at Duke University and President and CEO of the Duke University Health System. Now in my eighth year, I have decided I will step down from these roles at the end of this academic year, June 30, 2023. A formal announcement about my decision and transition plans will be forthcoming from President Vincent Price today.
Serving with you in these leadership roles has unquestionably been the best professional experience I have enjoyed in my life. Words really cannot adequately convey the emotions I am feeling at this time as I share this decision with you. Suffice it to say that I am currently overwhelmed with a sense of heartfelt gratitude.
From that first spring in Durham when you so warmly welcomed Marie and me to the Duke community, all the way up to today, I have felt your unwavering support and been emboldened by it. Your tremendous talent, creativity, deep sense of caring, dedication, and can-do attitude have bolstered and empowered my leadership tenure. Together, we have indeed advanced health, as we have elevated our excellence and amplified Duke Health’s impact locally and globally. And, because of you, Duke Health is strongly positioned to continue thriving — innovating and leading in the decades ahead. I am very proud of our extraordinary accomplishments, and I am confident in a bright future for us all as we continue to distinguish Duke Health as a leader among the very top academic health systems in the world.
Most importantly, I want to thank you! Thank you for all you have given to me. Thank you for all you have given to each other, our patients and their loved ones, and our communities.
For those of you who are wondering why now, my decision is principally driven by my desire to devote more attention to my personal life. Last month, I turned 72 years-of-age. Young! Earlier this month, Marie and I celebrated 40 years of marriage, and we are thrilled about spending more time together. And as some of you know, we have a new granddaughter. I imagine that this personal renewal will be invigorating.
At the same time, I also believe that institutional renewal is good. In fact, in dynamic industries and organizations such as ours with rapid, dramatic change afoot, renewal is a constant imperative. We have an exceptionally strong team across Duke Health, and continued renewal at the top will only enhance the remarkable achievements and significant contributions we are already making.
Looking ahead over the next eight-plus months, please know that I am still all-in with you as we continue to advance Duke Health: Onward. Upward. Beyond. You can count on me to sprint right up to the hand-off of my leadership baton next June. My excitement and energy today are as high as when I arrived in April 2015.
With deep gratitude and admiration,
Eugene Washington, MD
Chancellor for Health Affairs, Duke University
President and CEO, Duke University Health System
Welcoming Newest Faculty Members
We are pleased to have a number of new faculty members on the Duke Heart team. Earlier this summer Zak Loring and Michelle Kelsey joined the faculty as assistant professors of medicine in cardiology after the completion of their fellowship training. Ziv Beckerman also joined our team in July as a faculty member in the division of cardiovascular and thoracic surgery. Since then, we’ve added four additional team members: Bharathi Upadhya, Senthil Selvaraj, Girish Kalra and Deepa Upadhyaya.
This week we’re highlighting Bharathi Upadhya.
Upadhya Joins Duke Heart Team

Bharathi Upadhya, MD, officially joined the Duke Heart team on Aug. 22 as associate professor of medicine in cardiology. She is the newest member of our adult congenital heart disease team and will see patients at Duke Cardiology Arringdon.
Upadhya says she is most excited about joining the Duke Heart team because of the professional growth and learning opportunities available here. With congenital heart disease patients living longer, the field of care is growing and offers great opportunity, especially at a large and varied program like Duke. She says she enjoys treating patients with challenging conditions such as chromosomal abnormalities and muscular dystrophy.
“These patients really need attentive care, which I enjoy providing,” said Upadhya. “Initially, this was not an area of interest for me, but when I learned more about the association of these chromosomal issues to cardiovascular defects, I became quite dedicated to this area. I am equally fascinated by the hemodynamics of congenital heart disease.”
She is particularly enthusiastic about working with and learning from Tom Bashore and Rich Krasuski, she says. “There is no end to learning and growing, no matter how old you get it should never stop.”
“I most enjoy the long-lasting relationships that can be built with patients, especially those with congenital heart disease,” she adds. “I typically become their primary care provider and I do everything I can for them. They come to feel like family or lifelong friends to me.”
Born in Karnataka, India, Upadhya earned her MBBS at Mysore Medical College followed by residency training at Vijaya Nagar Institute of Medical Science — both in India. In the U.S., she completed residency at Wake Forest University School of Medicine (WFUSOM), and a fellowship in cardiology at Penn State Hershey Medical Center.
“My father’s dream for me was to become a doctor. He really wanted me to help people and saw that I would be good at it,” Upadhya says. “I specifically chose cardiology due to our family history. My mom’s eldest sister died due to heart disease back in India. At that time, we didn’t have as much access to treatment options or support. I believe her death could have been prevented and this is what drove my interest toward cardiology.”
Her parents, she adds, are her greatest mentors. “All that I am is because of them,” says Upadhya. “When I came to the U.S. for fellowship, my mom and dad came here from India. My mom, who could not even speak English, came and stayed for two years just to help me. They have sacrificed greatly for me and I am so thankful to them.”
fellowship, my mom and dad came here from India. My mom, who could not even speak English, came and stayed for two years just to help me. They have sacrificed greatly for me and I am so thankful to them.”
Prior to coming to Duke, she was associate professor of medicine in cardiology at WFUSOM, where she joined the faculty in 2010. While at Wake Forest Baptist Health, she helped launch a congenital heart program in partnership with pediatric cardiologist Derek Williams, MD. She earned numerous awards for teaching excellence and was the Arnold P. Gold Foundation’s 2017 recipient of the Leonard Tow Humanism Award. She currently serves as an ad hoc reviewer for more than a dozen journals and is a member-at-large for the American Society of Echocardiography’s membership committee.
Upadhya is a clinical investigator with board certification in Cardiovascular Medicine, Echocardiography, Nuclear Cardiology, and Adult Congenital Heart Disease. Her research has spanned a wide range of topics in cardiovascular medicine including medical imaging-related projects and cardiac rehabilitation, heart failure with preserved ejection fraction, exercise physiology, and aging.
Bharathi’s husband, Sudarshan Upadhya, PhD, MBA, is co-founder of Aestas Pharma, Inc., based here in Durham. They have two children. Their son is a senior at Duke University, and their daughter is in the 6th grade. Outside of medicine, Bharathi has learned Bharatanatyam, a classical dance of India. She has a strong interest in music and is a trained vocalist of Hindustani classical music. She is currently learning a different form of classical Indian music with her daughter.
We are so pleased to have Bharathi on the Duke Heart team! Please give her a warm welcome, if you have not yet had the opportunity to do so.
Caregiving Conference Held Oct. 28
The Duke Caregiver Community Event was held Friday, Oct. 28 at the Sheraton Imperial Hotel in Durham. Nishant Shah, Laura Blue and Stephanie Barnes served as speakers for the event. Dakota Bentz and Henry Delgado Alvia were wellness clinic volunteers. There was a fantastic turnout with over 500 attendees.
Thanks to those from Duke Heart who participated!

CulturePulse 2022 is Coming This Week — Be Heard
All Duke Health team members will receive information about and a link to the 2022 CulturePulse survey on Wednesday, Nov. 2. The brief survey is confidential, mobile-friendly, and simple to complete. Questions will cover your sense of belonging, safety, and well-being, as well as the strength of your teams and management. The goal is to maintain what’s going well and adjust what could be better.
The survey link will remain open through Nov. 16; you can also find it via the QR code you’ll see on digital signage and printed flyers around Duke.
CulturePulse is a way for team members to share their feedback about what’s going well and what could be improved at Duke Health. Please participate and encourage your team members to do so as well. This is a great opportunity for all of us to have our voices heard.
NIH Data Management and Sharing Policy
The National Institutes of Health (NIH) will require all grants submitted on or after Jan. 25, 2023 to include a Data Management and Sharing Policy. As part of this policy, all new NIH funding mechanisms that produce research data will need to document a two page Data Management and Sharing Plan (DMSP), which will be considered a term and condition of the award. This plan needs to be submitted when applying for funding. Researchers should plan and budget for the management and sharing of data.
To assist faculty in the DOM in meeting this requirement, there will be a DOM Research Quality Town Hall, led by the Duke Office of Scientific Integrity, on Nov. 8, 2022 from 12-1 p.m.
The Town Hall will cover resources at Duke to help faculty meet this requirement. RCR200 credit will be given for those attending the full one-hour meeting. The meeting will be recorded for those unable to attend, but RCR credit is only available for those who attend the live meeting.
To attend this Town Hall and submit your questions regarding the NIH DMSP, please register at the following link: Town Hall on Data Management and Sharing Policy.
ICYMI: Anti-Ableist Advocacy: Lunsford Aims to Change the Conversation Around Disability
He didn’t always have an awareness of it or a word for it, but Christopher Lunsford, MD, was affected by ableism throughout his  life. It affected how he coped with the challenges that came with being hard of hearing since birth and having a speech impediment. It wasn’t always easy to make his way in a world that focuses mostly on the experiences of people who can hear and speak clearly.
life. It affected how he coped with the challenges that came with being hard of hearing since birth and having a speech impediment. It wasn’t always easy to make his way in a world that focuses mostly on the experiences of people who can hear and speak clearly.
Going on rounds during medical school proved especially difficult. The noisy nature of hospitals with multiple people speaking at once — sometimes in masks — made it extremely hard for Lunsford to know what his attending physicians, patients, and classmates were saying. He said he found himself working twice as hard just to keep up. He did ask for and receive accommodations, but it was a cumbersome process, and ultimately, the accommodations were not helpful. He simply chose to “grin and bear” it.
Now he realizes the pressure to minimize his issues was due to ableism. He also has come to understand that not only is it okay to ask for accommodation, but it’s also important to look at changing systems that lead to inequitable learning environments and patient care settings.
“Rounds is possibly the worst possible way for a person who is hard of hearing to learn,” said Lunsford, an assistant professor in the Department of Orthopaedic Surgery as well as the Department of Pediatrics. “The number one ‘coping skill’ that I was given was to minimize the challenge and to make it go away just by ignoring the negative impacts of it. I did not even process it as a systematic failure. At the time, I thought I should have never complained in the first place: ‘I’ll be fine, I’ll figure it out.’ I now process it differently in the hope that it helps make me a better advocate.”
This feature story from Duke SOM’s Magnify continues here. It’s worth reading.
Call for abstracts: 2023 Duke Health Quality and Safety Conference
The virtual poster submission period for the 2023 Duke Health Quality and Safety Conference is now open. The deadline for submission is Wednesday, Dec. 14. The 2023 Conference will be held the weeks of March 13 and 20, with an in-person event on Thursday, March 23.
For more information and to submit your abstract, please click here.
Reminder: Early Voting, 2022 Election
The one-stop early voting period in North Carolina opened on Thursday, Oct. 20 and runs through Saturday, Nov. 5. During early voting, voters may cast a ballot at any early voting site in their county and would-be voters may same-day register and vote. Durham residents have the opportunity to vote at Duke University’s early voting site on campus in Karsh Alumni Center (2080 Duke University Rd, Durham, NC 27708). Multiple early voting sites are available in Durham, Wake, Orange, Person, and Alamance counties. Early voting locations in each county can be found on the NC State Board of Elections website.
Voters who choose to vote by mail may request an absentee ballot until Tuesday, Nov. 1 at 5 p.m. All absentee ballots must be postmarked by 5 p.m. on Election Day and received by Nov. 14 at 5 p.m. Voters who have already requested an absentee ballot may drop it off at any early voting site in-person, either for themselves or a close relative. Absentee ballots may also be returned to the local board of elections office or a designated drop-off site by 5 p.m. on Election Day. Voters can make sure their absentee ballot was received by using Ballottrax, an absentee ballot tracking site operated by the State Board of Elections.
Election Day is Tuesday, Nov. 8 and a list of polling locations can be found here. Visit the State Board of Elections website or vote.duke.edu for additional information. For those of you going to AHA this upcoming weekend, be sure to get out and vote as the meeting is close to election day. The early voting areas in Durham have the weight times on line.

Additional Reminders:
- November is American Diabetes Month and National COPD Awareness Month.
- The DUHS annual flu vaccination campaign is underway. The deadline for staff vaccinations is Tuesday, Nov. 15 at 10 a.m. Vaccination sites for faculty and staff can be found here: https://flu.duke.edu/vaccination/employees/
Upcoming Events & Opportunities
Cardiology Grand Rounds
November 1: No CGR this week.
CME & Other Events
November 4: 14th Annual NC Research Triangle Pulmonary Hypertension Symposium. 7 a.m.-4 p.m. This will be an in-person event at the Durham Convention Center. Registration required. To learn more and register, visit: https://duke.is/jag2b
November 5: Duke Annual Reception at AHA.22. Grand Horizon C, Marriott Marquis Chicago. 5:30 – 8:30 p.m. Questions? Contact Elizabeth Evans or Willette Wilkins.
November 8: Election Day. Please vote!
November 8: DOM Research Quality Town Hall. Topic: 2023 NIH Data Management and Sharing Policy. 12-1 p.m. via Zoom. Register here. You must register to receive the Zoom link for the event.
November 14: Prostate Cancer & CVD Symposium, Webinar 4. Final of a four-part webinar series. Collaboration between the International Cardio-Oncology Society & Duke Heart. Noon, Eastern. Free. To register visit https://duke.is/ptjbs.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
October 20 — Adrian Hernandez and Susanna Naggie
U.S. News & World Report
Study Debunks Use of Antidepressant Luvox as COVID Treatment
https://duke.is/6mc7p
October 24 — Duke Clinical Research Institute
Becker’s Hospital Review
Ivermectin doesn’t accelerate COVID-19 recovery, study suggests
https://duke.is/45qj9
October 24 — Duke University (DCRI)
CNBC
https://duke.is/9hz2e
October 25 — Marat Fudim
mHealth Intelligence
How Wearables Can Enhance Cardiac Care, Boost Patient Engagement
https://duke.is/2vzug
October 25 — Anne Ford (obstetrics/gynecology)
verywellhealth.com
Are Hot Flashes Bad for Your Heart?
Division of Cardiology Publications Indexed in PubMed October 21-26, 2022
Assimon MM, Pun PH, Al-Khatib SM, Brookhart MA, Gaynes BN, Winkelmayer WC, Flythe JE. The modifying effect of the serum-to-dialysate potassium gradient on the cardiovascular safety of SSRIs in the hemodialysis population: a pharmacoepidemiologic study. Nephrol Dial Transplant 2022 Oct 19;37(11):2241-2252. PM: 35793567.
Assimon MM, Pun PH, Wang L, Al-Khatib SM, Brookhart MA, Weber DJ, Winkelmayer WC, Flythe JE. Letter to the editor. Kidney Int 2022 Nov;102(5):1191-1192. PM: 36272744.
Bose S, Yao H, Huang Q, Whitaker R, Kontos CD, Previs RA, Shen X. Using genetically encoded fluorescent biosensors to interrogate ovarian cancer metabolism. J Ovarian Res 2022 Oct 20;15(1):114. PM: 36266675.
Damluji AA, Tehrani B, Sinha SS, Samsky MD, Henry TD, Thiele H, West NEJ, Senatore FF, Truesdell AG, Dangas GD, Smilowitz NR, Amin AP, deVore AD, Moazami N, Cigarroa JE, Rao SV, Krucoff MW, Morrow DA, Gilchrist IC. Position Statement on Vascular Access Safety for Percutaneous Devices in AMI Complicated by Cardiogenic Shock. JACC Cardiovasc Interv 2022 Oct 24;15(20):2003-2019. PM: 36265932.
Naggie S, Boulware DR, Lindsell CJ, Stewart TG, Gentile N, Collins S, McCarthy MW, Jayaweera D, Castro M, Sulkowski M, McTigue K, Thicklin F, Felker GM, Ginde AA, Bramante CT, Slandzicki AJ, Gabriel A, Shah NS, Lenert LA, Dunsmore SE, Adam SJ, DeLong A, Hanna G, Remaly A, Wilder R, Wilson S, Shenkman E, Hernandez AF. Effect of Ivermectin vs Placebo on Time to Sustained Recovery in Outpatients With Mild to Moderate COVID- 19: A Randomized Clinical Trial. JAMA 2022 Oct 25;328(16):1595-1603. PM: 36269852.
Perkovic V, Blackorby A, Cizman B, Carroll K, Cobitz AR, Davies R, DiMino TL, Jha V, Johansen KL, Lopes RD, Kler L, Macdougall IC, McMurray JJV, Meadowcroft AM, Obrador GT, Solomon S, Taft L, Wanner C, Waikar SS, Wheeler DC, Wiecek A, Singh AK. The ASCEND-ND trial: study design and participant characteristics. Nephrol Dial Transplant 2022 Oct 19;37(11):2157-2170. PM: 34865143.
Salah HM, Goldberg LR, Molinger J, Felker GM, Applefeld W, Rassaf T, Tedford RJ, Mirro M, Cleland JGF, Fudim M. Diaphragmatic Function in Cardiovascular Disease: JACC Review Topic of the Week. J Am Coll Cardiol 2022 Oct 25;80(17):1647- 1659. PM: 36265961.
Shahid RA, Vigna SR, Huang MN, Gunn MD, Liddle RA. Nicotinic stimulation of splenic T cells is protective in endoscopic retrograde cholangiopancreatography- induced acute pancreatitis in mice. Am J Physiol Gastrointest Liver Physiol 2022 Nov 1;323(5):G420-G427. PM: 36126221.
Wand AL, Russell SD, Gilotra NA. Ambulatory Management of Worsening Heart Failure: Current Strategies and Future Directions. Heart Int 2021 Jun 7;15(1):49-53. PM: 36277316.
Wendell D, Jenista E, Kim HW, Chen EL, Azevedo CF, Kaolawanich Y, Alenezi F, Rehwald W, Darty S, Parker M, Kim RJ. Assessment of papillary muscle infarction with dark-blood delayed enhancement cardiac MRI in canines and humans. Radiology 2022 Nov;305(2):329-338. PM: 35880980.
Duke Heart Pulse – October 23 2022: Highlights and Updates
Chief’s message:
It is a busy time of year for all of our teams at Duke Heart. This week there are faculty and fellows working on Capital Hill to  discuss the importance of supporting Heart Health. One of our fellows NKiru Osude was a member of the American College of Cardiology group (representing North Carolina) who met with members of congress to discuss the impact of health care disparities, access to care, and the importance of covering services and care for people with heart disease or people as risk for heart disease. She is seen here taking a selfie with the whole group.
discuss the importance of supporting Heart Health. One of our fellows NKiru Osude was a member of the American College of Cardiology group (representing North Carolina) who met with members of congress to discuss the impact of health care disparities, access to care, and the importance of covering services and care for people with heart disease or people as risk for heart disease. She is seen here taking a selfie with the whole group.
As you will see in the stories below, members of Duke Heart continue to work hard to perform research to identify ways to have our community and patients have health, from first responders in cardiac arrest research, the genetics of cardiac arrest, helping with a national cardiogenic shock registry, to studying treatments for COVID, and holding symposiums on pulmonary hypertension. The research and clinical care work at Duke Heart remain vibrant.
 This time of year also has our community in full swing for a variety of fall celebrations and traditions. Halloween for the kids will be next week, we had the NC state fair this week (you can see – still some work to be done for our community’s food choices), and the upcoming American Heart Association Scientific Sessions in early November where we will have several scientific presentations from Faculty and Fellows.
This time of year also has our community in full swing for a variety of fall celebrations and traditions. Halloween for the kids will be next week, we had the NC state fair this week (you can see – still some work to be done for our community’s food choices), and the upcoming American Heart Association Scientific Sessions in early November where we will have several scientific presentations from Faculty and Fellows.
For some of us this weekend also was important as the start of the celebration of Diwali. Diwali is traditionally held on the darkest night of the new moon in Autumn, and celebrates the victory of light over darkness, knowledge over ignorance, good over evil, hope over despair. In many homes it is marked by cleaning and setting up decorations, symbols, and of course many lights. Kids and families celebrate with songs, dances, and all sorts of treats. My daughter was able to perform in a traditional dance at the local temple, and we were fortunate enough to have her grandparents present. After several years of challenges to our communities, health care systems, and scientific communities, we hope whether you celebrate Diwali or not, you have some time over the fall to spend with family and loved ones. You will see in this version of the Pulse there is much to be thankful for, and many who are working to spread light, knowledge, and health in our Duke Heart Community.
evil, hope over despair. In many homes it is marked by cleaning and setting up decorations, symbols, and of course many lights. Kids and families celebrate with songs, dances, and all sorts of treats. My daughter was able to perform in a traditional dance at the local temple, and we were fortunate enough to have her grandparents present. After several years of challenges to our communities, health care systems, and scientific communities, we hope whether you celebrate Diwali or not, you have some time over the fall to spend with family and loved ones. You will see in this version of the Pulse there is much to be thankful for, and many who are working to spread light, knowledge, and health in our Duke Heart Community.
Highlights of the week:
Duke Heart Teams with NC First Responders on Cardiac Arrest Trial
Duke Heart researchers are teaming up with North Carolina emergency care personnel—EMS, fire, police, 911 dispatch and community members—across the state in a pragmatic cluster-randomized trial that will test community interventions to improve survival for out of hospital cardiac arrest (OHCA), a leading cause of death in the U.S.
survival for out of hospital cardiac arrest (OHCA), a leading cause of death in the U.S.
There are more than 400,000 out of hospital cardiac arrests a year in the U.S. with a survival rate of less than 10%. Despite 30 years of efforts by health care professionals, there is scant evidence that cardiac arrest survival odds have substantially improved. Duke researchers are focused on changing that.
The RAndomized Cluster Evaluation of Cardiac ARrest Systems (RACE-CARS) trial covers a geographic area of 62 counties involving eight million residents and expects to enroll 20,000 cardiac arrest patients over a four-year period. It is one of the first U.S. registry-based trials, such that all eligible patients are included and data are efficiently collected in routine care, an approach that has been used with great success in large, efficient clinical trials in Europe. The trial is being conducted by Duke Clinical Research Institute (DCRI) with a $15 million grant from the National Institutes of Health (NIH).
“We’ve leveraged a highly efficient clinical trial design methodology to be able to address a major public health concern in an ambitious project to test community interventions to improve survival from cardiac arrest,” says the trial’s principal investigator, Christopher Granger, MD, professor of medicine in cardiology and director of the Cardiac Care Unit at Duke. “If we’re successful, this will provide compelling evidence to guide how care is provided around the country and around the world to improve survival from cardiac arrest.”
For the trial, 62 counties were randomly assigned to intervention or control groups. Interventions are focused on community CPR and AED treatment, 911 dispatch performance, and first responder treatment for OHCA. The goal is to have more patients with cardiac arrest treated with bystander CPR and early defibrillation. Intervention counties are working closely with the trial team to carry out and evaluate trial interventions while the control groups will continue to provide their usual care.
and AED treatment, 911 dispatch performance, and first responder treatment for OHCA. The goal is to have more patients with cardiac arrest treated with bystander CPR and early defibrillation. Intervention counties are working closely with the trial team to carry out and evaluate trial interventions while the control groups will continue to provide their usual care.
The data collection phase began in July for the trial, which runs from July 1, 2020 through June 30, 2027, and uses the pre-existing Cardiac Arrest Registry to Enhance Survival (CARES) registry for patient enrollment, a platform previously implemented in North Carolina by the RACE CARS team. CARES collects data from 911 dispatch centers, EMS agencies, and hospitals and links that information in a single record.
 In laying the trial groundwork, researchers in the last two years have surveyed current practices at the counties, reviewed care metrics in each county, created site actions plans and held in-person site visits to provide improved outcome guidance, focusing on activities that will shorten the treatment time to CPR and defibrillation during the first 10 minutes of the cardiac arrest. Each county randomized to the intervention strategy has worked with RACE-CARS investigators to develop a customized intervention strategy that is tailored to each individual agency’s unique needs and resources, and customized training plans for each level of the prehospital chain of survival. (Story continues here)
In laying the trial groundwork, researchers in the last two years have surveyed current practices at the counties, reviewed care metrics in each county, created site actions plans and held in-person site visits to provide improved outcome guidance, focusing on activities that will shorten the treatment time to CPR and defibrillation during the first 10 minutes of the cardiac arrest. Each county randomized to the intervention strategy has worked with RACE-CARS investigators to develop a customized intervention strategy that is tailored to each individual agency’s unique needs and resources, and customized training plans for each level of the prehospital chain of survival. (Story continues here)
In addition to Granger, the RACE-CARS team includes Dan Mark, Lisa Monk, Monique Starks, Sana Al-Khatib, Hayden Bosworth, Hussein Al-Khalidi, Kimberly Ward, Steve Vendeventer and James Jollis. Congratulations to all on this important work!
Determining Genetic Causes for Sudden Cardiac Death
People commonly associate heart attacks with clogged arteries, fatty diets, high cholesterol, and plaque buildup in the heart. And while all those things can cause sudden cardiac death, they are not the only culprit; gene mutations can also be to blame.
Certain genetic variants can cause irregular heart rhythms, called arrhythmias, and can affect how well the heart is able to pump

blood to the rest of the body. Otherwise healthy individuals with these genetic variants can fall victim to arrhythmias that are often fatal.
Duke researchers investigated 55 genes responsible for various arrhythmia-related disorders to understand how common these
variants are and the risks they pose. Results were published in Circulation: Genomics and Precision Medicine on September 22.
The team, led by Svati Shah, MD, professor of medicine in cardiology, integrated electronic health records with whole exome sequencing data collected from 8,574 people in the Catheterization Genetics (CATHGEN) cohort, a group that had undergone cardiac catheterization at Duke University Medical Center from 2001 through 2011.
 “We took an in-depth look at the entire diagnostic spectrum, from electrocardiograms to cardiac MRIs, as well as medical charts for history of syncope, arrhythmias, and all the other ways these types of conditions could manifest,” said Navid Nafissi, MD, lead author and a Duke cardiac electrophysiology fellow.
“We took an in-depth look at the entire diagnostic spectrum, from electrocardiograms to cardiac MRIs, as well as medical charts for history of syncope, arrhythmias, and all the other ways these types of conditions could manifest,” said Navid Nafissi, MD, lead author and a Duke cardiac electrophysiology fellow.
The researchers wanted to know whether patients’ symptoms met diagnostic criteria for these conditions and if there was any evidence of sub-diagnoses that might have been missed because they did not meet full diagnostic criteria.
One in 108 people in this cohort carried a pathogenic or likely pathogenic variant in arrhythmia-related genes, which means these variants may be more common in the general population than researchers initially thought.
How severe the genetic variants are, though, varies greatly. The likelihood that a particular variant might cause health problems can range from zero to as high as 83%. Issues might include dilated cardiomyopathy, which causes the heart’s ventricles to thin, stretch out, and grow larger; or hypertrophic cardiomyopathy, which causes the heart muscle to gather scar tissue and thicken. Both these disorders make it harder for the heart to pump blood to the rest of the body. Variants can also cause disorders like long QT syndrome and Brugada syndrome that cause fast, chaotic heartbeats. All of these disorders can lead to sudden death in otherwise healthy people.
“These are people who just die suddenly — without any warning signs,” Nafissi said. “Sometimes there’s no clear manifestations of cardiac disease, even in autopsy.” The heart might look completely healthy: no cholesterol build up, and sometimes no signs of scar tissue from hypertrophic cardiomyopathy or thinning ventricles from dilated cardiomyopathy.
When there is no clear reason as to why a person had a sudden cardiac death, genetic testing can help determine what happened. “Sometimes you can find a causative genetic variant in these cases,” Nafissi said, “which can allow for tailored management and cascade screening of family members.”
Current standards of care still take a reactive approach to this problem. If someone goes into sudden cardiac arrest, health care and emergency workers address the crisis and try to save the patient — but what if there was a better, more proactive approach?
Nafissi hopes this research takes researchers one step closer to utilizing genetic testing earlier to identify those who have genetic variants that could put them at increased risk of sudden cardiac arrest. But, Nafissi clarifies, “Not everyone who carries a variant will go on to have a cardiac event.”
The trick will be identifying those at highest risk and determining the appropriate preventive interventions, such as an implantable cardioverter-defibrillator or something less invasive, like lifestyle modifications or medications. “There are multiple ways that this research could lead to saving lives,” Nafissi said.
Duke Team to help Co-Lead Newly Established Cardiogenic Shock Registry
The American Heart Association (AHA) has established the world’s first professional society shock registry as part of the Get With The Guidelines registries network. Mitch Krucoff, MD, professor of medicine in cardiology at Duke will serve as co-chair of the registry along with Dr. David Morrow, director of the Levine Cardiac Intensive Care Unit at Brigham and Women’s Hospital  and professor of medicine at Harvard.
and professor of medicine at Harvard.
The creation of this new registry is the direct result of work done by the Cardiac Safety Research Consortium Think Tank on cardiogenic shock, according to Krucoff.
Cardiogenic shock—a life threatening condition when a person’s heart can’t pump enough blood to meet the needs of the body—is most often caused by serious heart attack or advanced heart failure. Historically, data related to cardiogenic shock have been limited, inconsistent and challenging to interpret. As a result, varying treatment recommendations exist around best  practices.
practices.
The new registry will help researchers, clinicians and regulators to better understand the clinical symptoms of shock types, treatment patterns and outcomes. The registry will provide a foundation for working toward improving the quality and consistency of care in patients in U.S. hospitals with cardiogenic shock symptoms. This effort has had many of our current and past Duke Faculty and fellows involved including Mark Samsky, Magnus Ohman, Joseph Rogers, and Sunil Rao.
“To understand how to improve care for cardiogenic shock patients, we first need a clearer view of the landscape of existing treatment practices for cardiogenic shock in U.S.-based acute care settings,” said Krucoff. “No organization is better positioned to advance this critical public health question than the AHA, with already established networks of sites entering data on heart failure, acute cardiac syndromes, cardiac arrest and COVID—all of which involve patients at risk of progressing to cardiogenic shock.”
The Cardiogenic Shock Registry builds on more than 20 years of quality improvement and registry experience rooted in the AHA’s Get With The Guidelines platform. Data from the registry will help inform the larger medical community on how best to treat cardiogenic shock.
“The new Cardiogenic Shock Registry will leverage the unparalleled reach of the AHA in a unique collaboration between academic clinicians and researchers, federal agencies and funding supporters’ experts to provide high-quality evidence and promote best practices for the treatment of patients with cardiogenic shock,” said Morrow.
Krucoff and Morrow both serve as volunteer experts for the AHA. The AHA’s Precision Medicine Platform, a secure cloud-computing platform, will be used to facilitate the research.
ICYMI: Boulware Named Dean of WFU School of Medicine
 Ebony Boulware, MD, MPH, Director of the Duke Clinical and Translational Science Institute (CTSI), Vice Dean for Translational Science in the School of Medicine, and Associate Vice Chancellor for Translational Research at Duke University, has accepted the role of Dean of the Wake Forest University School of Medicine. She will begin her new role in January 2023. Dr. Boulware will also serve as the Vice Chief Academic Officer and Chief Science Officer at Atrium Health. She will step down from her positions at Duke on December 31, 2022, as she makes her transition to this exciting leadership opportunity.
Ebony Boulware, MD, MPH, Director of the Duke Clinical and Translational Science Institute (CTSI), Vice Dean for Translational Science in the School of Medicine, and Associate Vice Chancellor for Translational Research at Duke University, has accepted the role of Dean of the Wake Forest University School of Medicine. She will begin her new role in January 2023. Dr. Boulware will also serve as the Vice Chief Academic Officer and Chief Science Officer at Atrium Health. She will step down from her positions at Duke on December 31, 2022, as she makes her transition to this exciting leadership opportunity.
The announcement was made on Monday by Kathleen Cooney, MD, chair of the Duke Department of Medicine and Mary E. Klotman, MD, Dean, Duke University School of Medicine.
Boulware, the Nanaline H. Duke University Distinguished Professor in the Department of Medicine, joined the Duke faculty in 2013 as Chief of the Division of General Internal Medicine in the Department of Medicine and has served as Director of CTSI and Vice Dean for Translational Science since 2016. She has spent most of her academic career investigating how to improve health care and health outcomes for individuals and populations with chronic kidney disease, hypertension, and other chronic diseases, particularly focusing on minoritized populations. In her roles at Duke, she has been instrumental in accelerating the translation of research to clinical care, and she is a national leader in addressing the causes and effects of racial and ethnic health and health care inequities.
The SOM and DOM will work with the Division of General Internal Medicine to create a transitional leadership plan as they prepare to launch a national search for a new Division Chief.
“Dr. Boulware has been a dedicated and innovative leader, and we want to thank her for her service and commitment to the School of Medicine,” said Cooney and Klotman in their statement. “She made significant contributions to the Department of Medicine in her role as Division Chief and generously mentored many faculty members within and outside of the Division. Her passion for addressing health inequities and improving our approach to diversity, equity, and inclusion has profoundly strengthened our department. We know you will join us in congratulating Dr. Boulware.”
Personally, Ebony has been a leader across so many areas a Duke – she will be missed. We are excited for her and will look forward to continuing to collaborate on making NC a healthier state! Congratulations – Ebony!
Nicholls, Chen Join Duke Heart APP Team
Please join us in welcoming two new APPs to our Duke Heart team!
First, we are welcoming Stephanie Nicholls, a nurse practitioner, back to our team. She will be working at South Durham Clinic with Michael Blazing, and at Duke Cardiology Arringdon. Nicholls is originally from a small town in Maine and moved to NC in 2013 to work at Duke. She was initially in the CTICU and then went on to serve as a heart transplant coordinator. She met her husband at Duke and they now have two children — Emma, 3, and Luke, 1. She lives in Durham and can typically be found chasing children around The Museum of Life and Science. She enjoys the great restaurant scene in Durham and going to the beach. She has always enjoyed being a part of the vibrant Duke community and is excited to join her new team.
Karina Chen, a physician assistant, will be at Duke Cardiology Arringdon working with Cary Ward and the DHP group. Chen grew up in southeastern Michigan and attended Fordham University for her bachelor’s degree in biology. She spent some time working as an EMT and CNA before moving to Boston for PA school at Massachusetts College of Pharmacy and Health Science. After graduating, she worked at Brigham and Women’s Hospital in Pulmonary Vascular Medicine with a focus on caring for patients with pulmonary hypertension. She and her husband moved to NC in order to escape the freezing Boston winters, as well as to be closer to her parents who are now living in SC. They are enjoying trying new restaurants in the Triangle area and exploring hiking trails with their corgi, Gimli. She is excited to join the Duke Heart team.
Please welcome Stephanie and Karina to our team!
Shout-out to CT OR Team
Our cardiothoracic team managed a particularly difficult surgical case on Wednesday — a big shout-out to our incredible and dedicated multidisciplinary team! Together, they rallied, showed incredible teamwork, and the patient is doing well.
“I especially want to express my gratitude for Reeni, who scrubbed in and stayed way late to see this through to completion.” – Jacob Schroder
Congrats to all. Well done!
Duke Heart Construction Update
Construction on Cardiac Catheterization Lab 1 is due for completion by Nov. 7 with inspections taking place Nov. 7-11. The team plans to conduct their first case in Cath 1 on the afternoon of Nov. 14. A team from Philips will be present for support as well as training from Nov. 14-17. If you have any questions please contact Elizabeth Watts.
Arges Focused on Raising Vital Funds for MSA
Many of you know that Kristine Arges, RN, BSN, CCRC, left Duke Heart earlier this year after 31 years on the team. Arges is on disability leave after receiving a diagnosis of Multiple Systems Atrophy-Cerebellar (MSA), a rare, incurable neurodegenerative disease that can rapidly progress.
Due to elusive symptoms that appeared over time and seemed unrelated to each other, she went several years before being diagnosed. The disease has progressed fast, and she is now walker- and wheelchair-dependent. After her diagnosis, she began reading up on MSA and says she was shocked to find there are few treatment options and little research being done. She reached out to Mayo Clinic after learning about the work of Dr. Wolfgang Singer, an associate professor of neurology who has completed phase-one research showing that disease progression of MSA could be slowed through the infusion of autologous mesenchymal stem cells. The research looks promising. Arges qualified for the study and enrolled; she is three months in and has completed two infusions of either stem cells or placebo, 2:1.
Having grown up in Manhattan, she earned her BSN at Columbia School of Nursing and quickly found work in a neuro-surgical stepdown at Columbia-Presbyterian. Two years later, she was ready to leave New York City behind her and chose Durham, NC as her next home.
Arges applied at Duke Hospital where there was a need for nurses on 3200; she started on the unit in 1991. Once she made the switch to cardiology care she never looked back. Arges says she developed her sea legs in the ACU and then joined the heart failure research group under Chris O’Connor, MD. There, she eventually coordinated the PRAISE 1 & 2 studies, noting that O’Connor always inspired a healthy sense of competition – and that he and she, ‘Chris and Kris,’ were always vying to be the top enrollers. Kris went on to coordinate many trials in the HF group such as BEST, OPTIME, and CHARM to name just a few.

Pictured here with longtime friend Stephanie Kerr, RN, MSN, at a party celebrating the successful conclusion of the PRAISE 1 trial.
She joined Duke’s Cardiac Diagnostic Unit in 2003 and conducted imaging trials with many of ‘the greats’ in Duke Cardiology, including Jamie Jollis, Joe Kisslo, Zainab Samad, Jerry Bloomfield, Pam Douglas, Eric Velazquez, Michel Khouri, Sreek Vemulapalli and, of course, Fawaz Alenezi. Kris became a “lifer” in the CDU and spent the remainder of her career there. She wore many hats in the CDU – as a stress-nurse one day per week, and as an intermediary for study coordinators in various disciplines who needed tests done on their research patients.
In the “old days,” she says, there wasn’t a system in place to help sonographers know which images to acquire. With the trend in clinical trials to monitor cardiac safety, more and more studies required echocardiograms on study patients. In addition to organizing a system of imaging instructions for what came to be more than 100 research clinical trials, she coordinated contrast perfusion studies in ultrasound; helped manage core lab work at the Duke Clinical Research Institute; and in the lab, she coordinated amyloid studies – including the ATTRACT trial (which became Tafamidis), served as the REMIT nurse working with Wei Jiang, MD for several years, and coordinated a number of studies with the Biomedical Engineering group.
In her last ten years at Duke, she served as lead CRC of Cardiac Imaging. She shared this role with Michele Parker in MRI. Kris’s research group was multi-disciplinary — a microcosm of life in the CDU– consisting of exercise physiologists, sonographers, nurses, clerical assistants, and students.
“Perhaps the thing I loved most about my job was the ever-present variety of people, patients, and disciplines,” said Arges. “Never was there ever a dull moment. The CDU was the place to be.”
Arges and others are working to raise funds to ensure that all 70 patients currently enrolled in the clinical trial can receive compassionate use of stem cells upon completion of Phase 2. All patients involved “have everything to lose if funds are not raised to buy them time until a new treatment or cure is found,” Arges says.
Saddened to have left her role at Duke, Arges is resolved to keep fighting as long as she can. She thinks fondly of her time at Duke Heart, misses her former co-workers, and wishes all of us a belated and fond farewell.
Arges is open about her life with MSA and wants to raise awareness of this poorly recognized disease. She has created a ‘legacy page’ which lives on the Defeat MSA Alliance website where you can learn more about MSA as well as donate. Kris says that she would be honored if you considered supporting her and others with this condition.

Kris is shown here with members of her Duke research group. L-R are: Alicia Armour, Melissa LeFevre, Arges, Jennifer Tomfohr and Danielle Wilson).
You are missed, Kris!
Early Voting in NC, on Duke Campus: 2022 Election
The one-stop early voting period in North Carolina opened on Thursday, Oct. 20, and runs through Saturday, Nov. 5. During early voting, voters may cast a ballot at any early voting site in their county and would-be voters may same-day register and vote. Durham residents have the opportunity to vote at Duke University’s early voting site on campus in Karsh Alumni Center (2080 Duke University Rd, Durham, NC 27708). Multiple early voting sites are available in Durham, Wake, Orange, Person, and Alamance counties. Early voting locations in each county can be found on the NC State Board of Elections website.
 Voters who choose to vote by mail may request an absentee ballot until Tuesday, Nov. 1 at 5 p.m. All absentee ballots must be postmarked by 5 p.m. on Election Day and received by Nov. 14 at 5 p.m. Voters who have already requested an absentee ballot may drop it off at any early voting site in-person, either for themselves or a close relative. Absentee ballots may also be returned to the local board of elections office or a designated drop-off site by 5 p.m. on Election Day. Voters can make sure their absentee ballot was received by using Ballottrax, an absentee ballot tracking site operated by the State Board of Elections.
Voters who choose to vote by mail may request an absentee ballot until Tuesday, Nov. 1 at 5 p.m. All absentee ballots must be postmarked by 5 p.m. on Election Day and received by Nov. 14 at 5 p.m. Voters who have already requested an absentee ballot may drop it off at any early voting site in-person, either for themselves or a close relative. Absentee ballots may also be returned to the local board of elections office or a designated drop-off site by 5 p.m. on Election Day. Voters can make sure their absentee ballot was received by using Ballottrax, an absentee ballot tracking site operated by the State Board of Elections.
Election Day is Tuesday, Nov. 8 and a list of polling locations can be found here. Visit the State Board of Elections website or vote.duke.edu for additional information.
Additional Reminders:
- October 23-29 is Respiratory Care Week. Please send some love their way this week!

- DukeALERT testing was performed this week. Please make sure you’re familiar with the several ways in which you would be informed in the event of an emergency. You can find great information on the Duke Emergency Management Website as well as the DUHS Preparedness and Response Center.
- October is Medical Ultrasound Awareness Month – thank a sonographer!
- Open Enrollment is now open through Oct. 28. This is your opportunity to review your medical, dental, vision, and reimbursement account benefit elections and make any changes necessary to ensure your choices continue to meet your needs. You should have received a copy of the annual Open Enrollment Guide in the mail from Duke HR.
- The DUHS annual flu vaccination campaign is underway. The deadline for staff vaccinations is Tuesday, Nov. 15 at 10 a.m. Vaccination sites for faculty and staff can be found here: https://flu.duke.edu/vaccination/employees/
Upcoming Events & Opportunities
Cardiology Grand Rounds
October 25: No CGR this week.
CME & Other Events
October 17-28: Open Enrollment period for 2023 for all Duke faculty and staff.
October 28: Duke Caregiver Community Event, in-person conference. Details here: https://duke.is/nzbcp.
November 4: 14th Annual NC Research Triangle Pulmonary Hypertension Symposium. 7 a.m.-4 p.m. This will be an in-person event at the Durham Convention Center. Registration required. To learn more and register, visit: https://duke.is/jag2b
November 5: Duke Annual Reception at AHA.22. Grand Horizon C, Marriott Marquis Chicago. 5:30 – 8:30 p.m. Questions? Contact Elizabeth Evans or Willette Wilkins.
November 14: Prostate Cancer & CVD Symposium, Webinar 4. Final of a four-part webinar series. Collaboration between the International Cardio-Oncology Society & Duke Heart. Noon, Eastern. Free. To register visit https://duke.is/ptjbs.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
October 14 — Mark Sendak (DIHI)
The Medical Futurist
The 8 Most Reassuring Examples of Using A.I. In Healthcare
https://duke.is/gg32v
October 17 — Joseph Turek and the Sinnamon family
WAFF TV-48 (Huntsville, AL)
World’s first heart & thymus transplant
https://duke.is/v3jh2
*clip begins @ 12:24:34
October 18 — Duke Health
Becker’s Hospital Review
10,000 patients out of network in Duke-UnitedHealthcare dispute
https://duke.is/bca28
October 19 — Shahzeb Khan, G. Michael Felker & Marat Fudim
Medscape/JACC HF
Are we Getting any Closer to Understanding Congestion?
https://duke.is/ch3hc
October 19 — Adrian Hernandez & Susanna Naggie
CBS-17 WNCN/cbs17.com (Raleigh)
COVID debate semi-settled: Antidepressant does not work as treatment
https://duke.is/wa9sg
October 20 — Adrian Hernandez & Susanna Naggie
HealthDay News/U.S. News & World Report
Study Debunks Use of Antidepressant Luvox as COVID Treatment
https://duke.is/jp5pj
Duke Heart Pulse October 16th 2022
Wang to become Chief of Comparative Effectiveness Research at PCORI

Tracy Wang, MD, professor of medicine in cardiology at Duke and Director of Health Services & Outcomes Research at the Duke Clinical Research Institute, has accepted an exciting new role as Chief of Comparative Effectiveness Research at the Patient Centered Outcomes Research Institute (PCORI). Her last day at Duke will be Nov. 7.
“After almost 20 years at Duke, I have made the difficult decision to pursue a totally different career pathway at PCORI in Washington, DC,” Wang wrote in a message to colleagues. “As many of you know, it’s been a true privilege to train here at Duke, and my time as faculty has continued to offer learning opportunities every day as I work alongside amazing colleagues and friends.
“Here, we have a unique environment that allows us to contribute to medicine by taking care of some of the sickest patients out there, by taking on meaningful and impactful scientific research, and by growing the next generation of cardiologists and researchers. It has been a true honor to serve here and, from the bottom of my heart, I thank you for all your support, collegiality, and friendship over the years.”
Tracy has been an inspiration to generations of cardiology fellows and faculty and has won numerous mentoring awards. She has been tireless in her pursuit of improving quality of our care and has been a consummate collaborator and leader in our Division. The ability to shape the national landscape of comparative effectiveness research through PCORI seems like the a position built for someone with her skills, passion, and desire to improve health through clinical science. Tracy is a world-class physician researcher who will undoubtedly bring critical thinking and common sense solutions that will have immediate impact on all of those around her.
Personally, it is bittersweet to have her leave our Duke Heart team and the DCRI, but we are excited for this next stage of her career and we look forward to continued collaboration and friendship with her over the coming years.
Congratulations, Tracy!
Gehling Joins Duke Development; Will Support Duke Heart
Please join us in welcoming William Gehling to Duke Heart! Gehling is the new Director of Development for Heart and Lung in the office of Duke Health Development and Alumni Affairs. He began his position in late August and has spent the last  month acclimating to DUHS.
month acclimating to DUHS.
William relocated here from New York, where he most recently served as a director of development at Stony Brook Medicine supporting their Department of Surgery as well as Stony Brook Children’s. He has prior experience with fundraising and alumni relations at the Center for Reproductive Rights, Weill Cornell Medicine, NYU Langone Health, and New York-Presbyterian.
Gehling says he looked at the chance to work for Duke Health as an opportunity to reconnect with his roots.
“My family is still here in North Carolina, so it’s nice to be able to be closer to them,” he said. “I really love academic medicine fundraising and the opportunity to support Duke Heart is special to me because my father had care here. Dr. Milano was his provider and I can really attest to the amazing care that was provided to our family. It’s nice to go full circle and give back to support a program that supported us as a family.
“Overall, I’m excited to support the tripartite mission. I know the faculty here are just really incredible. They have a vision they are trying to execute and that’s where my job comes in. I can’t do the medical work or the discovery work that they’re doing, but I can help find the right donor to support their efforts. I know that every time I’m raising funds, another family is going to be provided for and that’s really special.”
Originally from the greater Charlotte area, William holds a bachelor’s degree from NC State University. He enjoys running and has completed two New York City marathons.
Welcome to Duke Heart, William!
Notable Efforts & Recent Happenings
Camille Frazier-Mills and Sana Al-Khatib served as program faculty for the Women in Electrophysiology summit held at the Sofitel Chicago Magnificent Mile in Chicago Oct. 13-15.

Tommy D’Amico served as a member of the program committee for the AATS International
Thoracic Surgical Oncology Summit held in NYC Sept. 30-Oct. 1
Jason Katz served as a course director for the 2nd Annual NYU Langone Critical Care Cardiology Symposium held in NYC Oct. 13-14.

The Duke Cardio-Oncology 2022 conference Cardio-Oncology in the Era of Precision Medicine was held at the J.B. Duke Hotel & Conference Center in Durham on Friday, Oct. 14. Michel Khouri and Susan Dent co-led the program. The conference was very well attended and we continue to be excited about this growing area of research and improved care for patients. Khouri presented “Risk Identification and Management Strategies of Cardiotoxicities” and Nishant Shah presented “Identifying Cardiometabolic Risk and Preventive Cardiology Strategies.”



Congratulations to all – great job!
Celebrating Sonographers
October is Medical Ultrasound Awareness Month, and we would like to take a moment to thank all of the sonographers throughout Duke Heart for their hard work and dedication to the field of Cardiovascular Ultrasound. Our Duke Heart Center patients benefit from your expertise, careful attention to detail, and thoughtful care. We are grateful to work alongside each of you!
throughout Duke Heart for their hard work and dedication to the field of Cardiovascular Ultrasound. Our Duke Heart Center patients benefit from your expertise, careful attention to detail, and thoughtful care. We are grateful to work alongside each of you!
Speaking of sonographers… we’re excited about a newly published book with submissions by several of our team members. Please see our next story.
New Congenital Echocardiography Guide Now Available
A new reference guide for congenital echocardiography is now available. The first edition of Congenital Echocardiographer’s  Pocket Reference was authored by Richie Palma, Director of the Duke Cardiac Ultrasound Certificate Program, and Melissa Wasserman, Supervisor of Echo Lab Satellite Operations at
Pocket Reference was authored by Richie Palma, Director of the Duke Cardiac Ultrasound Certificate Program, and Melissa Wasserman, Supervisor of Echo Lab Satellite Operations at Children’s Hospital of Philadelphia. The book includes contributions from 33 of the top sonographers in the U.S., including Duke’s own Colin Dunbar, Tracy Ralston, Ashlee Davis and Jon Owensby. Gregory Tatum, MD, Medical Director of Duke Children’s Specialty Clinic of Greensboro and Director of Quality and Education for the Duke Pediatric Echocardiography Lab, wrote the forward and served as editor.
Children’s Hospital of Philadelphia. The book includes contributions from 33 of the top sonographers in the U.S., including Duke’s own Colin Dunbar, Tracy Ralston, Ashlee Davis and Jon Owensby. Gregory Tatum, MD, Medical Director of Duke Children’s Specialty Clinic of Greensboro and Director of Quality and Education for the Duke Pediatric Echocardiography Lab, wrote the forward and served as editor.
The book has 32 chapters and offers access to hundreds of videos and diagrams. Tatum says it’s “the perfect book for someone who is beginning their career in echocardiography, as well as someone who wants to refresh on topics within congenital heart disease. Palma and Wasserman have created an invaluable reference resource for all learners and practitioners of congenital echocardiography.”
The book, published this summer, is currently available only through the Arizona Heart Foundation.
Congratulations to all involved!
Shout-out to Senman
 Congratulations to second year fellow Balim Senman — she was the only cardiology trainee invited to participate in and lead a session at the 2nd annual NYU Langone Critical Care Cardiology Symposium held Oct. 13-14 in NYC. Senman co-moderated an incredible breakout discussion on the impact of “Social Media in Critical Care Cardiology Education, Research and Professional Advancement.”
Congratulations to second year fellow Balim Senman — she was the only cardiology trainee invited to participate in and lead a session at the 2nd annual NYU Langone Critical Care Cardiology Symposium held Oct. 13-14 in NYC. Senman co-moderated an incredible breakout discussion on the impact of “Social Media in Critical Care Cardiology Education, Research and Professional Advancement.”
Great job, Balim!
Kudos to Kosovec
Congratulations to Juliann Kosovec, a resident in Duke’s General Surgery Residency Program — she and her co-authors won the best poster award at the AATS’s International Thoracic Surgical Oncology Summit held Sept. 30-Oct. 1 at the Sheraton New York Times Square in NYC. Their abstract, Redefining Quality Metrics in cN2M0 Non-Small Cell Lung Cancer, can be found here.
Way to go, Juliann!
Shout-out to Rao
Congratulations to Advanced Heart Failure and Transplant Cardiology fellow Vishal Rao – he has been named a top reviewer to the Journal of Cardiac Failure (JCF).
 In a letter sent to Manesh Patel from the journal’s Editor-in-Chief Robert Mentz and Deputy Editor Anu Lala-Trinidade, they stated, “Of a large pool of expert reviewers, Dr. Rao stood out for being timely and providing insightful comments that contributed meaningfully to the improvement of manuscripts and publication decision processes. We recognize the numerous demands on Dr. Rao’s time and are especially grateful for the time and effort that goes into providing high-quality impactful reviews. Dr. Rao was acknowledged publicly at the JCF reception at the HFSA Annual Scientific Meeting on October 2, 2022, for his contributions. We look forward to Dr. Rao’s further work with the JCF family.”
In a letter sent to Manesh Patel from the journal’s Editor-in-Chief Robert Mentz and Deputy Editor Anu Lala-Trinidade, they stated, “Of a large pool of expert reviewers, Dr. Rao stood out for being timely and providing insightful comments that contributed meaningfully to the improvement of manuscripts and publication decision processes. We recognize the numerous demands on Dr. Rao’s time and are especially grateful for the time and effort that goes into providing high-quality impactful reviews. Dr. Rao was acknowledged publicly at the JCF reception at the HFSA Annual Scientific Meeting on October 2, 2022, for his contributions. We look forward to Dr. Rao’s further work with the JCF family.”
Well deserved, Vishal!
Duke Team Attends AMPATH Global Gathering
The AMPATH Global Gathering was held last weekend in Indianapolis and Duke was well represented. The team celebrated advancing our commitment to global health and in particular, our relationship with Moi Teaching and Referral Hospital (MTRH) in El Doret, Kenya. AMPATH (Academic Model Providing Access to Healthcare) is a partnership between MTRH and a consortium of North American institutions led by Indiana University.

AMPATH began working in western Kenya in 1988 and has been most widely known for its work addressing HIV/AIDS. Duke joined the AMPATH consortium in 2009 with support from a National Heart, Lung, and Blood Institute (NHLBI) grant to create a cardiovascular and pulmonary disease Center of Excellence. The Cardiovascular Center of Excellence partnership has been a joint effort led by the Hubert-Yeargan Center for Global Health (HYC), the Duke Clinical Research Institute (DCRI) and Duke Heart, with initial leadership from Duke faculty members Eric Velazquez (now at Yale) and Gerald Bloomfield.
Clinical educational efforts have been led by John Lawrence, adjunct assistant professor of medicine in cardiology at Duke. Lawrence has, since the earliest years, has spent four to eight months a year in Kenya helping to establish a clinical cardiovascular service including a robust outpatient clinic, inpatient teaching service, opening a new 10-bed cardiac care unit and leading the development of a Cardiovascular Fellowship Training Program at Moi University with the support of HYC.
HYC is led by Executive Director Chris Woods, Executive Director Nathan Thielman and Director of Operations Cynthia Binanay, who has led the Kenya Operations with HYC since 2006. Since 2009, the cardiovascular efforts have been supported by expanding partnerships within Duke, with other AMPATH institutions, and the DUCCS alumni network.
Duke Heart has been a consistent partner and supporter of the Cardiovascular COE since its inception. Numerous physicians, nurses and echocardiographers have rotated there for educational and consultative activities. Duke trainees have rotated at MTRH as part of the Global Health Residency Pathway, and many have been mentored by Bloomfield as Fogarty Global Health Fellows, Doris Duke Clinical Scholars and junior faculty at Duke with ongoing support from Duke Heart for global health efforts.
Pictured here (left to right) are some members of the partnership who attended the Global Gathering last weekend: Gerald Bloomfield, Cory Miller, Nick Nguyen, Titus Ngeno, Felix Barasa (Head, Cardiology Unit at MTRH), Wilson Sugut (Head, Department of Medicine at MTRH), Duke hospitalist Rebecca Lumsden, Andrew McCrary, Lauren McCrary, Cynthia Binanay, Tara Holder (former Duke IM resident, current ICC fellow at Vanderbilt), Rob Nealy (UT Austin, Cardiothoracic Surgery); Shanti Nulu (UT Austin, Cardiology), Dale Lawrence, and John Lawrence.
Bloomfield, Ngeno, Lawrence and others have been pillars leading the development of clinical programs and research with our colleagues at MTRH. They’ve done incredible work in El Doret and we look forward to all they will continue to accomplish.
Photo of the Week
Magnus Ohman, adjunct professor of medicine in cardiology, met recently with long-time Duke Heart supporters Mr. and Mrs. Albert “Lynn” Williams over lunch at the Washington Duke Inn.
 Ohman said, “We had a wonderful meeting and we spoke about their philanthropy supporting the lecture in Cardiovascular Genetics. He and his wife shared how meaningful it was for them to support this and to see all the outstanding scientists that have spoken at these lectures over the years. They also commented on how cardiovascular genetics are now moving to the forefront in several areas of cardiology.”
Ohman said, “We had a wonderful meeting and we spoke about their philanthropy supporting the lecture in Cardiovascular Genetics. He and his wife shared how meaningful it was for them to support this and to see all the outstanding scientists that have spoken at these lectures over the years. They also commented on how cardiovascular genetics are now moving to the forefront in several areas of cardiology.”
Having fostered numerous relationships with Duke Heart donors, grateful patients and the Duke Health development teams over many years, Ohman enjoys maintaining these connections.
“Philanthropy is so rewarding, as it is so meaningful to a donor and so important for the academic aspects of medicine that otherwise would not be possible,” Ohman added. “It’s a true win-win situation.”
Additional Reminders:
- October is Medical Ultrasound Awareness Month – thank a sonographer!
- National Physician Assistant Week was celebrated Oct. 6-12. We are so grateful for the incredible work our PAs do throughout Duke Heart and throughout the Health System. Thank you!
- Open Enrollment starts tomorrow and runs Oct. 17-28. This is your opportunity to review your medical, dental, vision, and reimbursement account benefit elections and make any changes necessary to ensure your choices continue to meet your needs. You should have received a copy of the annual Open Enrollment Guide in the mail from Duke HR.
- The DUHS annual flu vaccination campaign is underway. The deadline for staff vaccinations is Tuesday, Nov. 15 at 10 a.m. Vaccination sites for faculty and staff can be found here: https://flu.duke.edu/vaccination/employees/
- Duke Health has launched our first comprehensive Team Member Referral Program. Team members at Duke University Health System and Duke University who refer qualified candidates for any posted clinical or non-clinical positions at https://careers.dukehealth.org/ may be eligible for a monetary bonus and prizes. To learn more, visit: https://duke.is/2sjkv
Upcoming Events & Opportunities
Cardiology Grand Rounds
October 18: PRECIDENT D Study at Duke with Schuyler Jones. 5 p.m. Webex. This event will be online only.
CME & Other Events
October 17-28: Open Enrollment period for 2023 for all Duke faculty and staff.
October 28: Duke Caregiver Community Event, in-person conference. Details here: https://duke.is/nzbcp.
November 4: 14th Annual NC Research Triangle Pulmonary Hypertension Symposium. 7 a.m.-4 p.m. This will be an in-person event at the Durham Convention Center. Registration required. To learn more and register, visit: https://duke.is/jag2b
November 5: Duke Annual Reception at AHA.22. Marriott Marquis Chicago. 5:30 – 8:30 p.m. Questions? Contact Elizabeth Evans or Willette Wilkins.
November 14: Prostate Cancer & CVD Symposium, Webinar 4. Final of a four-part webinar series. Collaboration between the International Cardio-Oncology Society & Duke Heart. Noon, Eastern. Free. To register visit https://duke.is/ptjbs.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
October 7 — Joseph Turek and the Sinnamon family
WILX 10 News (Lansing, MI)
Your Health: History-making patient is thriving
https://duke.is/zbkkx
October 7 — Adrian Hernandez
The Daily Progress
UVa Health leads statewide COVID-19 clinical trial
https://duke.is/mk59u
October 7 — Senthil Selvaraj
Medscape
Dapagliflozin DELIVERs Regardless of Systolic BP in HF With Preserved EF
https://duke.is/8qjzj
October 10 — Michael Pencina
Healthcare Innovation
With Focus on Equity, Coalition for Health AI Readies Framework Release
https://duke.is/j8bcn
October 10 — Joseph Turek and the Sinnamon family
WDAM (Hattiesburg-Laurel, MS)
https://duke.is/rujdc
*clip starts at 5:17:05
October 12 — G. Michael Felker
Medical Dialogues
Sacubitril/Valsartan May Reduce Mitral Regurgitation in HFrEF, Eliminating Need for Interventions
https://duke.is/bj9fr
October 12 — Harry Severance
Medpage Today
Isn’t It a Seller’s Market for Healthcare Professionals?
https://duke.is/czagj
October 13 — Tommy D’Amico
rtve.es (Spain)
Diego González Rivas, el cirujano que ha operado en más países en la historia de la medicina
https://duke.is/ws8wp
Division of Cardiology Publications Indexed in PubMed October 7-12, 2022
Coats AJS, Abraham WT, Zile MR, Lindenfeld JA, Weaver FA, Fudim M, Bauersachs J, Duval S, Galle E, Zannad F. Baroreflex activation therapy with the Barostim™ device in patients with heart failure with reduced ejection fraction: a patient level meta-analysis of randomized controlled trials. Eur J Heart Fail 2022 Sep;24(9):1665-1673. PM: 35713888.
Garus M, Zdanowicz A, Fudim M, Zymliński R, Niewiński P, Paleczny B, Rosiek-Biegus M, Iwanek G, Ponikowski P, Biegus J. Clinical determinants and prognostic significance of hypocapnia in acute heart failure. Sci Rep 2022 Oct 7;12(1):16889. PM: 36207364.
Heffron SP, Windheim J, Barrett TJ, Voora D, Berger JS. Platelet inhibition by low-dose aspirin is not influenced by body mass or weight. Platelets 2022 Nov 17;33(8):1208-1213. PM: 35768902.
Jones MM, McElroy LM, Mirreh M, Fuller M, Schroeder R, Ghadimi K, DeVore A, Patel CB, Black-Maier E, Bartz R, Thomas K. The impact of race on utilization of durable left ventricular assist device therapy in patients with advanced heart failure. J Card Surg 2022 Nov;37(11):3586-3594. PM: 36124416.
Kunadian V, Baber U, Pivato CA, Cao D, Dangas G, Sartori S, Zhang Z, Angiolillo DJ, Briguori C, Cohen DJ, Collier T, Dudek D, Gibson M, Gil R, Huber K, Kaul U, Kornowski R, Krucoff MW, Dehghani P, Mehta S, Moliterno DJ, Ohman EM, Escaned J, Sardella G, Sharma SK, Shlofmitz R, Weisz G, Witzenbichler B, Džavík V, Gurbel P, Hamm CW, Henry T, Kastrati A, Marx SO, Oldroyd K, Steg PG, Pocock S, Mehran R. Bleeding and Ischemic Outcomes With Ticagrelor Monotherapy According to Body Mass Index. JACC Cardiovasc Interv 2022 Oct 10;15(19):1948-1960. PM: 36202563.
Morris K, Weston K, Davy A, Silva S, Goode V, Pereira K, Brysiewicz P, Bruce J, Clarke D. Identification of risk factors for postoperative pulmonary complications in general surgery patients in a low-middle income country. PLoS One 2022 Oct 11;17(10):e0274749. PM: 36219615.
Nelson AJ, Harrington JL, Kolkailah AA, Pagidipati NJ, McGuire DK. Sodium-Glucose Cotransporter-2 Inhibitors: Impact on Atherosclerosis and Atherosclerotic Cardiovascular Disease Events. Heart Fail Clin 2022 Oct;18(4):597-607. PM: 36216489.
Peters AE, DeVore AD. Pharmacologic Therapy for Heart Failure with Preserved Ejection Fraction. Cardiol Clin 2022 Nov;40(4):473-489. PM: 36210132.
Pineda AM, Wang A. New Pacemaker Implantation After Alcohol Septal Ablation: How Sharp Is the Double-Edged Sword? JACC Cardiovasc Interv 2022 Oct 10;15(19):1918-1920. PM: 36202560.
Salah HM, Fudim M. Sodium-glucose Cotransporter 2 Inhibitors and Nonalcoholic Fatty Liver Disease. Heart Fail Clin 2022 Oct;18(4):625-634. PM: 36216491.
Salah HM, Fudim M. Tolerability and safety barriers to sodium-glucose cotransporter 2 inhibitor initiation in heart failure with reduced ejection fraction. Eur J Heart Fail 2022 Sep;24(9):1633-1635. PM: 35867845.
Salah HM, Levin AP, Fudim M. Device Therapy for Heart Failure with Preserved Ejection Fraction. Cardiol Clin 2022 Nov;40(4):507-515. PM: 36210134.
Senni M, Alemayehu WG, Sim D, Edelmann F, Butler J, Ezekowitz J, Hernandez AF, Lam CSP, O’Connor CM, Pieske B, Ponikowski P, Roessig L, Voors AA, Westerhout CM, McMullan C, Armstrong PW. Efficacy and safety of vericiguat in patients with heart failure with reduced ejection fraction treated with sacubitril/valsartan: insights from the VICTORIA trial. Eur J Heart Fail 2022 Sep;24(9):1614-1622. PM: 35791083.
Recent Comments