Chief’s message:
This weekend is the kickoff of the American Heart Association Scientific Sessions 2022 in person with a virtual component in Chicago. The meeting has gotten off to a great start with many presentations of science from Duke Faculty and Fellows, opportunities to connect and see people in person, and in general get to participate and see science (much of which is not related to COVID). The meeting also highlights for us the amazing colleagues, connections, and people that we have had through the years as part of the Duke Fellowship, Faculty, and research and clinical collaborations. It is humbling to be the Chair for this years AHA Scientific Sessions. I was reminded as well about our mission and responsibility in the opening session for the AHA that included two US Surgeons General (Jerome Adams and Regina Benjamin), FDA Director Rob Califf, and AHA president Michelle Albert and World Heart Federation president Fausto Pinto. These scientific session meetings and even our own meetings at Duke with our faculty and fellows to discuss clinical care and science have highlighted how energizing and reinvigorating in person engagement is for us all.


Highlights of the week:
Scientific Sessions Kicks Off in Chicago!
So many of our team members throughout Duke Heart and the Duke Clinical Research Institute have been preparing for the 2022 American Heart Association’s Scientific Sessions and it’s finally here. We’ll have coverage this weekend and next to showcase as much of it as we can.
We are extremely proud of all the work – from the research done at (and in partnership with) Duke that will be presented during Sessions, to the effort that has gone into planning this event at the national level, to the work done to organize our annual presence in the Exhibit Hall – it takes a lot of planning and effort by a lot of people. On behalf of the Duke Heart leadership team, thank you.
We kick off our coverage this weekend with two of our late-breaking clinical trial presentations and close out with two award winners.
We hope those of you who have traveled to be in Chicago this weekend are having a great time. Once again, congratulations to all, and thank you for all that you do!
AHA.22 LBCT: Comparative Study of Two Heart Failure Drugs Finds No Difference in Outcomes
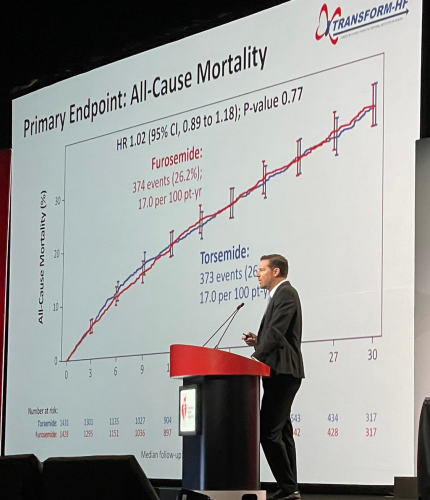 In a head-to-head comparison of two so-called ‘water pills’ that keep fluid from building up in patients with heart failure, the therapies proved nearly identical in reducing deaths, according to a large study led by Duke Health researchers.
In a head-to-head comparison of two so-called ‘water pills’ that keep fluid from building up in patients with heart failure, the therapies proved nearly identical in reducing deaths, according to a large study led by Duke Health researchers.
The study compared the diuretics torsemide and furosemide that were prescribed to patients with heart failure starting in the hospital setting. While prior data suggested a potential reduction in deaths among patients taking torsemide, the current study found no such benefit, providing clarity for both doctors and patients.
“Given that the two different therapies provide the same effect on outcomes, we shouldn’t spend time switching patients from one to the other, and instead concentrate on giving the right dose and adjusting other therapies that have been proven to have long-term benefits,” said cardiologist Robert J. Mentz, MD, chief of the heart failure section in the Division of Cardiology at Duke University School of Medicine and member of the Duke Clinical Research Institute.
Mentz was lead author of the study, called TRANSFORM-HF and funded by the National Heart, Lung and Blood Institute. He presented the findings as a late-breaking clinical trial yesterday at the American Heart Association’s 2022 Scientific Sessions in Chicago.
The study was designed as a direct comparison of loop diuretics, which are commonly prescribed to reduce the fluid buildup that causes swelling and breathing difficulties in patients with heart failure.
Mentz and colleagues enrolled more than 2,800 patients hospitalized with heart failure. Participants were randomly assigned to receive either torsemide or furosemide, and doctors determined the dosing. The study group was diverse, with women comprising 37% of participants and Black patients comprising 34%.
The main question was whether torsemide reduced patient deaths due to any cause over long-term follow-up (average of more than 17 months). The researchers found that death occurred in 373 of 1,431 study participants (26.1%) in the torsemide group and 374 of 1,428 patients (26.2%) in the furosemide group.
A secondary outcomes analysis looked at deaths or hospitalizations within 12 months, and again found little difference, with death or hospitalization occurring in 677 patients (47.3%) in the torsemide group and 704 patients (49.3%) in the furosemide group.
“This study has immediate clinical applications,” Mentz said. “Doctors spend a lot of time considering whether they will change from one diuretic to another, but there is no difference between the two for outcomes. This provides much-needed clarity. The insights from TRANSFORM-HF add to the evidence base that should help us improve patient care.”
In addition to Mentz, study authors include Kevin J. Anstrom, Eric L. Eisenstein, Shelly Sapp, Stephen J. Greene, Shelby Morgan, Jeffrey M. Testani, Amanda H. Harrington, Vandana Sachdev, Fassil Ketema, Dong-Yun Kim, Patrice Desvigne-Nickens, Bertram Pitt, and Eric J. Velazquez.
Congratulations to all TRANSFORM-HF team members – nicely done!
AHA.22 LBCT: Largest Randomized Trial Evaluates Steroids for Infant Heart Surgery
For more than four decades, doctors have been split on whether giving steroids during a pediatric open-heart surgery could be helpful for post-operative recovery. A new study is providing a bit more clarity, suggesting there are some benefits for certain kinds of patients.
Led by Duke Health researchers, the study was the largest trial designed to resolve the long-standing issue. More than 1,200 infants with heart disease were enrolled at 24 U.S. centers, with roughly half randomly assigned to receive steroids prior to heart surgeries, and the other half randomized to receive a placebo.
The main focus was whether prophylactic steroid use reduced any of more than a dozen complications, including death and heart transplant, compared to a placebo.
In the primary analysis, the researchers found no differences in the two groups, but steroid use was associated with elevated blood-sugar levels that required insulin therapy in some cases. Results showed 19% of participants using steroids required insulin therapy, compared to 8% in the placebo group. However, like many trials, the results were more nuanced and secondary analyses showed that some children might benefit.
The findings appear Nov. 6 in the New England Journal of Medicine and were presented this morning at the AHA’s 2022 Scientific Sessions.
Lead author of the study, Kevin Hill, MD, a member of the DCRI and chief of the Division of Pediatric Cardiology at Duke University School of Medicine, described the nuances of the study. Secondary results suggested that patients with less complex cases might be the ones who do better with steroids.
“Steroids reduce inflammation, and their benefit may be highest in children undergoing less complex procedures where inflammation is manageable,” Hill said. “But when you have the most complicated patients with severe inflammation affecting multiple organ systems, using steroids is like throwing a glass of water on a forest fire, and they seem to have less impact.”
Jennifer S. Li, MD, is the senior author of the paper and a professor in the departments of Pediatrics and Medicine at Duke. She says there’s a need for further study.
“We need to hone in on the patients who can actually benefit most from steroid use and develop a targeted approach to using this medicine, so that we maximize its benefit and minimize adverse effects,” Li said.
The DCRI performed the trial administration, data management and statistical analyses. The study was performed as a “trial within a registry” leveraging the infrastructure of the Society of Thoracic Surgeons Congenital Heart Surgery Database to conduct a low cost, pragmatic trial.
In addition to Hill and Li, study authors include, Prince J. Kannankeril, Jeffrey P. Jacobs, H. Scott Baldwin, Marshall L. Jacobs, Sean M. O’Brien, David P. Bichel, Eric M. Graham, Brian Blasiole, Ashraf Resheidat, Adil S. Husain, S. Ram Kumar, Jerry L. Kirchner, Dianne S. Gallup, Joseph W. Turek, Mark Bleiweis, Bret Mettler, Alexis Benscoter, Eric Wald, Tara Karamlou, Andrew H. Van Bergen, David Overman, Pirooz Eghtesady, Ryan Butts, John S. Kim, John P. Scott, Brett R. Anderson, Michael F. Swartz, Patrick I. McConnell, David F. Vener, and the STRESS Network Investigators.
Well done, team! Congratulations!
AHA.22: Presenters and Session Moderators
Between today and yesterday there were 35 Abstract Poster Session presentations by Duke Heart team members including Stephen Greene, Shahzeb Khan, Michelle Kelsey, Caitlin Drescher, Josephine Harrington, Michael Cosiano, Anand Shah, Jenn Rymer, Nishant Shah, and Conrad Hodgkinson – just to name a few.
Cardiology fellow Michael Cosiano presented “Comparing Patient Reported Outcomes and New York Heart Association Class Among Patients Hospitalized for Heart Failure” during abstract poster sessions on Saturday. He is lead author on the paper that was simultaneously published in Circulation: Heart Failure. His co-authors include Andrew Vista, Jie-lena Sun, Brooke Alhanti, Josephine Harrington, Adrian Hernandez, Robert Mentz, Stephen Greene, et al. This paper earned Cosiano recognition as a Circulation: Heart Failure (Circ HF) “Emerging Investigator.” Circ HF editors will feature his work as part of their series highlighting young investigators—defined as individuals less than ten years out of training—in the fields of heart failure, mechanical circulatory support, cardiac transplantation, and pulmonary hypertension. Additionally, this paper will be the focus of an upcoming Twitter journal club sponsored by Circ HF. Way to go, Michael!
Internal Medicine resident Anand Shah presented findings on the study, “In-Hospital Virtual Peer-to-Peer Consultation to Improve Guideline-Directed Medical Therapy for Heart Failure: A Pilot Randomized Trial” which was a Duke Heart Failure team and hospitalist-led pilot program on multidisciplinary care for hospitalized patients with heart failure. The presentation was done during a poster session held yesterday. The study findings were published online earlier this week in Circulation: Heart Failure. ICYMI, Vishal Rao was interviewed by TCTMD about the team’s findings. The TCTMD article was published earlier this week and appears in our News section below. (This was Rao’s first phone interview related to his research and he did a great job explaining the work done by the team. Great job, Vishal!). Other authors on the study include Jamie McDermott, Stephanie Barnes, Evan Murray, Michelle Kelsey, Stephen Greene, Marat Fudim, Adam Devore, Mike Blazing, Cara O’Brien, and Rob Mentz.
Findings from the study, “Adoption of Sacubitril/Valsartan in Patients with Heart Failure with Mildly Reduced or Preserved Ejection Fraction: The AHA Get With the Guidelines – Heart Failure Registry,” were presented during a poster session yesterday by Duke internal medicine resident Jacob Pierce. His co-authors include Zhen Li, Melissa Greiner, Steven Lippmann, Natalie Chantelle Hardy, Robert Mentz, Emily O’Brien, and Stephen Greene. The team’s findings were simultaneously published in Circulation: Heart Failure.
Cardiology fellow Jessie Duran presented “Abnormal Exercise Electrocardiography With Normal Stress Echocardiography is Associated With Increased Subclinical Coronary Atherosclerosis: Insights From the Project Baseline Health Study” yesterday during an oral session. Duran highlighted residual cardiovascular risk in a group of patients with positive ECG but negative stress echo. Well done!
Additionally, plenty of our Duke team members served as moderators for sessions throughout the day Saturday. They included: Andrew Landstrom, Larry Jackson, Sreekanth Vemulapalli, Manesh Patel, Neha Pagidipati, Jennifer Rymer, Jason Katz, Bradi Granger, Adrian Hernandez, Howard Rockman, Emily O’Brien, L. Kristen Newby and Rob Mentz.
We have an outstanding presence at Sessions this year! Great work everyone.
AHA.22: Douglas, Shah Honored with Council Awards
 We’re incredibly proud of Duke Heart team members Pamela Douglas, MD, and Svati Shah, MD. Both received awards last night during separate events at the AHA Scientific Sessions.
We’re incredibly proud of Duke Heart team members Pamela Douglas, MD, and Svati Shah, MD. Both received awards last night during separate events at the AHA Scientific Sessions.
Douglas was selected to receive the James B. Herrick Award for Outstanding Achievement in Clinical Cardiology by the AHA’s Council on Clinical Cardiology. Douglas delivered the James B. Herrick Lecture as part of the AHA’s Council Named Lecture Series held during Sessions. The series features lectures from some of today’s foremost clinicians and researchers as well as those with a lifetime of

contributions to the field of cardiovascular disease. Congratulations, Pam!
Shah was selected to receive the Genomic and Precision Medicine Mentoring Award by the AHA’s Council on Genomic and Precision Medicine. It was presented to her last night during the Council’s annual reception held this year in the Field Ballroom at the Hyatt Regency McCormick Place. Congratulations, Svati!
Frazier-Mills to Co-Lead ABC EP Committee

We are excited to share that electrophysiologist Camille Frazier-Mills, MD has been named co-chair of the Association of Black Cardiologists (ABC) Electrophysiology Committee. Her appointment is effective immediately and ends in April, 2024.
Congratulations, Camille! This is a tremendous honor!
CPR Performed by Duke Team Saves In-flight Passenger
 Duke Heart CVSSU team member Kaitlyn Allen and her husband, Justin Allen, MD, a Duke hospitalist, were recently in Utah so that Justin could compete in the 2022 Half Ironman World Championship race held Oct. 29 in St. George. On Tuesday, Nov. 1 while flying home toward RDU, a medical emergency was declared approximately 40 minutes into their three-hour flight. Both were nearby when a flight attendant yelled for an AED; Kaitlyn saw a passenger lying on her back in the middle of the aisle in the cabin ahead of her.
Duke Heart CVSSU team member Kaitlyn Allen and her husband, Justin Allen, MD, a Duke hospitalist, were recently in Utah so that Justin could compete in the 2022 Half Ironman World Championship race held Oct. 29 in St. George. On Tuesday, Nov. 1 while flying home toward RDU, a medical emergency was declared approximately 40 minutes into their three-hour flight. Both were nearby when a flight attendant yelled for an AED; Kaitlyn saw a passenger lying on her back in the middle of the aisle in the cabin ahead of her.
She and Justin immediately ran to the passenger’s aid. When they arrived, another passenger – a pediatric physician assistant – was maintaining the passenger’s airway, but neither Kaitlyn nor the PA could feel a pulse. Kaitlyn immediately started chest compressions while Justin took over the airway and prepared the AED. After the second round of compressions, the patient began moving her arms and became responsive. The team then applied oxygen, the AED, and took a set of vitals. Another passenger who happened to be a medical ICU nurse provided a glucometer and a pulse oximeter. With the passenger’s vitals stable, Justin cleared the patient’s cervical spine and she was able to sit upright, and eventually get back into a seat.
Kaitlyn communicated directly with the pilot about the situation. Ultimately the passenger arrived in stable condition and upon landing was handed off to paramedics for further evaluation.
This was not the first time the Allen’s have been in an emergency situation together. The two worked together at Lakeland Health in St. Joseph, MI (Kaitlyn’s hometown) during Justin’s internal medicine residency. There, they worked together during rapid responses and code blues. Kaitlyn and Justin concur that it was their previous experiences that allowed them to operate as a cohesive unit during this in-flight emergency. Even in less-than-ideal conditions on a fully booked flight at 29,000 feet with limited medical equipment, they worked together quickly and professionally to save a fellow passenger’s life.
Great teamwork and use of CPR!
Shout-out to D’Amico, Antonia
We received a great message this week regarding a patient compliment for Tommy D’Amico and Scott Antonia:
“My experience in the hospital was excellent. All the personnel treated me extremely well. I am eternally appreciative to Dr. D’Amico and the dream team at Duke University Hospital. All the services of the hospital are excellent. My operation was a success & I am already recovered. My appreciation to Dr. D’Amico & Dr. Scott Antonia for all that they did for me. Thanks.” — a grateful patient (name withheld for privacy)
“Tommy and Scott, I was just delighted to read this lovely compliment about you both on our Patient Satisfaction Survey. Thank you for your excellence and compassion. You clearly made a difference in this patient’s life. Very best wishes, Lisa” — Lisa Clark Pickett, Chief Medical Officer, Duke University Hospital
Nice work!
Halloween Pics
The week started off with fun Halloween celebrations — check out this pumpkin carved by cardiology fellow Ilia Shadrin! That’s the Shadrin family dressed as The Incredibles, and Dennis Narcisse with his twin boys as dinosaurs. So adorable!
We love the holiday spirit shown by our Duke Heritage Cardiology team in Wake County. Your ‘Boo Crew’ t-shirts are awesome. What a great way to show your enthusiasm while providing amazing care to our patients. Great work!
Thank you to all who shared your holiday pics with us for Pulse. We love getting your submissions – please keep them coming.



Samuel L. Katz, doctor who helped develop measles vaccine, dies at 95
 We were saddened this week to learn of the passing of our long-time Duke Health colleague, Dr. Sam Katz. A luminary in the field of infectious diseases and pediatrics, Katz was a beloved team member at Duke. His work has impacted millions although few of them may realize it. Our deepest sympathy to his family, friends, and colleagues throughout the world.
We were saddened this week to learn of the passing of our long-time Duke Health colleague, Dr. Sam Katz. A luminary in the field of infectious diseases and pediatrics, Katz was a beloved team member at Duke. His work has impacted millions although few of them may realize it. Our deepest sympathy to his family, friends, and colleagues throughout the world.
Remembering Samuel L. Katz, MD
Samuel L. Katz, MD, died on Monday, October 31, 2022.
Dr. Katz was a world-renowned virologist, pediatrician, and chair emeritus and Wilburt C. Davison Professor Emeritus of Pediatrics at Duke University School of Medicine. He was an honors graduate of Dartmouth College and Harvard Medical School. After a medical internship at Beth Israel Hospital, he completed pediatrics residency training at the Massachusetts General Hospital and the Boston Children’s Hospital, followed by a research fellowship in virology and infectious diseases.
Dr. Katz then became a staff member at Children’s Hospital working with Nobel Laureate John F. Enders for the next 12 years researching viruses — specifically measles, a disease that at the time killed more than five to six million children each year globally. During this time, Drs. Katz and Enders developed an attenuated measles virus vaccine.
In 1960, David Morley, MD, a British physician working in Nigeria, where the effects of measles were far more severe than they were in the United States, contacted Dr. Katz. Together, they inoculated Nigerian children with the new vaccine, with successful results. Not long after, the vaccine was tested in national clinical trials, approved by the Food and Drug Administration in 1963, and is now used throughout the world.
In addition to the development of the measles vaccine, Dr. Katz worked extensively on a range of other vaccines, including vaccinia (used as smallpox vaccine), polio, rubella, influenza, pertussis (whooping cough), Haemophilus influenzae b conjugates, and HIV.
In 1968, Dr. Katz was appointed chair of the Duke Department of Pediatrics, where he served for 22 years. In addition to mentoring two decades of students and residents, he established an exchange program with Oxford University and provided training for an annual succession of residents from the American University of Beirut. Throughout his tenure he displayed genuine interest in his patients, faculty, and trainees, actively encouraging female and minority physicians and seeking to diversify the faculty.
“As he did for so many others, Dr. Katz had a profound influence on my career,” said School of Medicine Dean Mary E. Klotman, MD. “His commitment, passion, and warmth were infectious. Duke School of Medicine, Pediatrics, and the world are all the better because of him.”
“Dr. Katz has been a stellar role model for all of us, as a clinician, as a teacher, as an investigator, and as an advocate for children,” said Department of Pediatrics Chair Ann M. Reed, MD. “He set a high bar, advancing medicine in ways that have improved children’s health around the world–he is truly one of the outstanding pediatric investigators of our times.”
In addition to seeing patients and supporting faculty, Dr. Katz expanded his role as an advocate for vaccination. Experiencing firsthand the ways in which disease affects children living in resource-poor countries contributed to Dr. Katz’s lifelong advocacy, within the United States, and around the world. He chaired the Committee on Infectious Diseases of the American Academy of Pediatrics (AAP), the Advisory Committee on Immunization Practices (ACIP) of the Centers for Disease Control (CDC), the Vaccine Priorities Study of the Institute of Medicine (IOM), and several World Health Organization (WHO) vaccine and HIV panels. He served on the National Institutes of Health (NIH) Committee for AIDS Vaccines and co-chaired the India-U.S. Vaccine Action Program and the National Network for Immunization Information. In addition, he served as chair of the Public Policy Council of the Infectious Diseases Society of America (IDSA), co-chaired IDSA’s Vaccine Initiative, and worked on behalf of UNICEF and the American Red Cross.
Dr. Katz earned numerous accolades throughout his career, including the inaugural Joseph St. Geme, Jr. Leadership Award in 1988, the 2003 Albert B. Sabin Gold Medal awarded by the Sabin Vaccine Institute, and the 2015 Maxwell Finland Award for Scientific Achievement for his contributions to vaccine discoveries during his career.
Please see link to The Washington Post news brief about his death in our News section below.
Reminder: Voting Day is Tuesday, Nov. 8
Election Day is Tuesday, Nov. 8 and a list of polling locations can be found here. Visit the State Board of Elections website or vote.duke.edu for additional information. Please vote!!!
On Thursday, Nov. 10 from Noon – 1 p.m., the Duke State Relations team and Duke Health’s Government Relations team are offering a post-election briefing to discuss the outcomes of the 2022 Election, how it will impact Duke Health, and provide a preview of the 2023 legislative sessions in Raleigh and Washington, DC. This event will be moderated by Dev Sangvai, MD, interim president, Duke Regional Hospital. To participate via Zoom, visit https://duke.is/2eq4k.

CulturePulse 2022 — Be Heard
All Duke Health team members were emailed a link to the 2022 CulturePulse survey on Wednesday, Nov. 2. The brief survey is confidential, mobile-friendly, and simple to complete.
The survey link will remain open through Nov. 16; you can also find it via the QR code you’ll see on digital signage and printed flyers around Duke.
CulturePulse is a way for team members to share their feedback about what’s going well and what could be improved at Duke Health. Please participate and encourage your team members to do so as well. You will receive automatic reminders about the survey until you complete it or it closes. This is a great opportunity for all of us to have our voices heard.

ORA Holiday Deadlines
The Office of Research Administration (ORA) will operate with reduced staff during the holiday season to allow team members time to recharge. During this period, please plan as far in advance as possible.
To help ORA respond as timely as possible to your needs, please plan in advance based on the following:
Thanksgiving Day and the Friday After
If you need something processed BEFORE the Thanksgiving holiday, please have it submitted in ready-form to ORA by Thursday, November 17. Otherwise, if it can wait, ORA will process it the following week (beginning November 28).
Last two weeks of December
For any transactions with due dates between December 19 – January 2, please have them submitted in ready-form to ORA by Thursday, December 15 to ensure there is adequate time and staffing to respond to your needs.
Please note: the next NIH SBIR/STTR deadline is Jan. 5, 2023, and the internal deadline is 8 a.m. on Dec. 28, 2022. Because this deadline falls in the last two weeks in December when ORA will be operating with reduced staff and because these award mechanisms are usually complex and require careful institutional coordination before submission:
- Please complete Intent to Submit for all planned SBIR/STTR applications no later than Dec. 5, 2022; and
- Please plan to route a submission-ready application no later than Dec. 15, 2022; if more time is needed, please submit a late waiver request so that ORA can plan for appropriate coverage to support these applications.
For anything submitted in the last two weeks of December that can wait until after the holiday break, ORA will be back up to speed with a full team on Jan. 3, 2023 and will look forward to managing all pending issues at that time.
This has been another year of tremendous growth in research at Duke. The Office of Research Administration thanks you for your continued partnership in support of Duke’s research mission and they send warm holiday wishes to all!
Matters of Grief: Grief Symposium 2022
The Duke Health Office of Culture and Well-being is offering Grief Symposium 2022 on Tues., Nov. 15 and a panel discussion on Wed., Nov. 16. Please consider joining for one or more events (most are virtual) in which they and participants will explore the many aspects of grief, including common grief reactions, how to support those who are grieving, professional grief, grief around loss of function or role, disenfranchised grief, rituals that may help us in the grieving process, and how to turn grief into positive action. Register here (please use your Duke e-mail to complete your registration).
- Grief Symposium: Tues., Nov. 15, noon-2 p.m.
- Grief Panel Discussion: Wed., Nov. 16, 1-2 p.m.
- Small Group Interactive Activities: Wed-Fri, 11/16-11/18. These will include: Somatic Body Work, Narrative Writing, Mandala Art, and Restorative Circles: Personal Grief, Pet Grief, and Gun Violence.
To learn more, please visit: https://cultureandwellbeing.dukehealth.org/grief-toolkit-symposium. A link to last year’s symposium is available on that page.
Additional Reminders:
- It is vital that we remain vigilant with masking, hand hygiene, PPE, and other safe behaviors to prevent the spread of infection. Please pay special attention to the proper wearing and securing of gowns and be mindful of PPE compliance. Thank you for all you do to keep everyone safe and healthy.
- November is American Diabetes Month, Pulmonary Hypertension Awareness Month, and National COPD Awareness Month. Thanks for all you do to help patients with these conditions!
- The deadline for staff flu vaccinations is Tuesday, Nov. 15 at 10 a.m. Vaccination sites for faculty and staff can be found here: https://flu.duke.edu/vaccination/employees/
Upcoming Events & Opportunities
Cardiology Grand Rounds
November 8: Topic, presenter TBD. Watch your email for the Zoom link!
CME & Other Events
November 8: Election Day. Please vote!
November 8: DOM Research Quality Town Hall. Topic: 2023 NIH Data Management and Sharing Policy. 12-1 p.m. via Zoom. Register here. You must register to receive the Zoom link for the event.
November 14: Prostate Cancer & CVD Symposium, Webinar 4. Final of a four-part webinar series. Collaboration between the International Cardio-Oncology Society & Duke Heart. Noon, Eastern. Free. To register visit https://duke.is/ptjbs.
Call for abstracts: 2023 Duke Health Quality and Safety Conference
The virtual poster submission period for the 2023 Duke Health Quality and Safety Conference is now open. The deadline for submission is Wednesday, Dec. 14. The 2023 Conference will be held the weeks of March 13 and 20, with an in-person event on Thursday, March 23.
For more information and to submit your abstract, please click here.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
October 27 — Duke Clinical Research Institute
Reuters
U.S. government to test Pfizer’s Paxlovid for long COVID
https://duke.is/7nbtf
October 28 — Duke Health
CBS17.com
450+ turn out for Duke Health event to help caregivers in Durham
https://duke.is/g9zvx
October 28 — Joseph Turek and the Sinnamon family
KALB-TV (Alexandria, LA)
Health headlines: First-of-its-kind heart and thymus surgery proves successful
https://duke.is/ga2km
October 28 — Duke Health
Becker’s Hospital Review
https://duke.is/vfeed
October 28 — Duke Clinical Research Institute
MSN/Washington Examiner
NIH to use Pfizer’s Paxlovid to study causes of long COVID
https://duke.is/m6t8h
October 31 — Jonathan Piccini
Patientcareonline.com
https://duke.is/8cpbk
October 31 — Joseph Turek and the Sinnamon family
WFMZ-TV (Allentown, PA)
Doctors pioneer a heart transplant technique involving another life-saving procedure
https://duke.is/2hzxe
November 2 — Betty Tong
WNCN-CBS17.com
November is Lung Cancer Awareness Month; Duke doctor recommends screening
https://duke.is/zq27k
November 3 — Samuel Katz (pediatrics)
The Washington Post
Samuel L. Katz, doctor who helped develop measles vaccine, dies at 95
https://duke.is/mrcde
Recent Comments