Home » Articles posted by Manesh Patel, M.D.
Author Archives: Manesh Patel, M.D.
Duke Heart June 29th 2025 – Transitions, Partnerships and Summer Reading
Chief’s Message: This is the Moment – transitions, partnerships and lessons from summer reading.
This week we had another busy week at Duke Heart as we prepared for our new fellows and residents to join us while we continued our celebrations of the fellows finishing their training. Find some photos of our interventional fellow 
 graduation dinner here – where we are lucky to continue to train the next generation of cardiovascular leaders – in this case in the field of interventional cardiology. The dinner and celebration were a testament to our faculty and the leadership that helps train and support these fellows education. We are excited to see their next steps in their career.
graduation dinner here – where we are lucky to continue to train the next generation of cardiovascular leaders – in this case in the field of interventional cardiology. The dinner and celebration were a testament to our faculty and the leadership that helps train and support these fellows education. We are excited to see their next steps in their career.
Additionally, we welcomed colleagues from Red Cell Partners to help us consider and build the future of CV care and beyond as we work to imagine systems to bring data to life for our patients. We had a robust meeting with our health system leaders and the Red Cell to envision how we can work to bring AI and transformative access to therapies to  improve the workflow and operations of our practice and improve cardiovascular health of our community, state, and country. The speed of change in the way data and information will be brought to our clinicians is quite substantial and we are lucky to have the commitment of such an important partner and a health system looking to innovate. A photo from that meeting is included here. The next 12 months provide us with a clear moment and opportunity to help transform the CV health care and research enterprise as we lean in and learn how to better deliver CV care and discover the next therapies in a sustainable model. Over the coming weeks we hope to crystalize this opportunity and come back to our entire community to engage in working to innovate care and research.
improve the workflow and operations of our practice and improve cardiovascular health of our community, state, and country. The speed of change in the way data and information will be brought to our clinicians is quite substantial and we are lucky to have the commitment of such an important partner and a health system looking to innovate. A photo from that meeting is included here. The next 12 months provide us with a clear moment and opportunity to help transform the CV health care and research enterprise as we lean in and learn how to better deliver CV care and discover the next therapies in a sustainable model. Over the coming weeks we hope to crystalize this opportunity and come back to our entire community to engage in working to innovate care and research.
Dean Klotman also gave her state of the union speech this week for the school of medicine. As always it was impressive  how many in the school and health system have stepped up to meet these challenging times by increasing ways in which we collaborate, develop new ways to do research, and develop systems to support our trainees and faculty. The talk especially highlighted our administrative professionals and leaders that have helped moved the school, departments, and divisions quickly to meet this need. Perhaps most encouraging from the discussion was the numerous examples (with several in heart) of teams innovating and making an impact through discovery of new ways to do things to improve health.
how many in the school and health system have stepped up to meet these challenging times by increasing ways in which we collaborate, develop new ways to do research, and develop systems to support our trainees and faculty. The talk especially highlighted our administrative professionals and leaders that have helped moved the school, departments, and divisions quickly to meet this need. Perhaps most encouraging from the discussion was the numerous examples (with several in heart) of teams innovating and making an impact through discovery of new ways to do things to improve health.
Finally, I provide the next summer reading review – “Healing Children: A Surgeon’s Stories from the Frontiers of Pediatric Medicine” by Dr. Kurt Newman. I was lucky enough to meet Kurt as we kicked off our Made for This philanthropy campaign – and he was nice enough to give me a copy of his book. The lessons from the book, a compelling and quick read, seem even more timely this time of year.
 The book opens with Kurt sharing a story from 40 years ago working as a third year medical student in Nobel Prize winner and Duke Cardiology Faculty member Dr. Bob Lefkowitz’s lab. He shares how he felt a thyroid mass while looking in a microscope and knew that he had thyroid cancer – and through his care at Duke as a medical student – resolved to become a surgeon. He shares the stories of his care and observations as a patient going through the system then and as a physician caring for children for years to come.
The book opens with Kurt sharing a story from 40 years ago working as a third year medical student in Nobel Prize winner and Duke Cardiology Faculty member Dr. Bob Lefkowitz’s lab. He shares how he felt a thyroid mass while looking in a microscope and knew that he had thyroid cancer – and through his care at Duke as a medical student – resolved to become a surgeon. He shares the stories of his care and observations as a patient going through the system then and as a physician caring for children for years to come.
In fact, “Healing Children” is a compelling narrative that offers an insider’s perspective into the world of pediatric surgery from the viewpoint of Kurt – even questioning and sharing a heartfelt exploration of the challenges and triumphs in treating young patients and their families. It is both a memoir and a manifesto advocating for the importance of specialized pediatric care at many points throughout the book. Even more pertinent to our times, Kurt presents the strength of mentoring from Dr. Randolph early in his career, the lessons of system and quality improvement by looking standardize the operative care, and multiple stories and lessons on the strength of multi-disciplinary care in the outcomes of pediatric patients.
Through many of these narratives, he highlights the unique medical, emotional, and ethical challenges faced when treating children. He seamlessly weaves his personal experiences with broader discussions on healthcare policy and the need for dedicated pediatric resources. At a time that Duke and UNC are working to build the Children’s Hospital of North Carolina – this is a timely memoir on the work at Children’s National Hospital.
Key Themes:
The Unique Nature of Pediatric Care: Kurt Newman emphasizes that children are not just small adults; they require specialized care tailored to their physical and emotional development. He argues for the necessity of pediatric-trained surgeons and facilities, underscoring how such specialization leads to better outcomes.
The Emotional Impact of Pediatric Surgery: The book delves into the emotional roller coaster experienced by both families and healthcare providers. He shares poignant stories of hope, despair, and resilience, giving readers a glimpse into the human side of medicine.
Advocacy for Pediatric Healthcare: A significant portion of the book is dedicated to advocating for better healthcare policies and funding for pediatric research. He calls for systemic changes to ensure that children receive the best possible care, highlighting the disparities that exist in access to pediatric specialists.
The Interdisciplinary Nature of Pediatric Medicine: As noted through various anecdotes, he illustrates the collaborative nature of pediatric care, involving surgeons, nurses, therapists, and families. He stresses the importance of teamwork in achieving successful outcomes for young patients.
Impact of Philanthropy and Leadership. Dr. Newman shares how he learned from a key donor who had a child cared for by their team. He is pushed to move this vision forward and learns how to effect change and eventually become CEO and lead Children’s Hospital of Washington.
My Take Home Message:
This is an engaging and meaningful read to see and hear the stories of specific patients that Dr. Newman cared for and how it impacted his thoughts and actions to lead a multi-disciplinary team at Children’s Hospital of Washington. There are many analogies to the care we provide for cardiovascular patients – and his lessons on how to improve and move towards the community from a surgical center are quite relevant today. I personally found his voice, the stories, and ability to translate those to larger lessons in health care both impactful and important for our health care work today. If you get a chance – you can take a bit of time and hopefully find some meaning in this book from a past Duke Medical Student.
Duke Heart Pulse June 22nd 2025 – Summer Reading
Chief Message: Summer Reading Program
Hope you are all well. Our Duke Heart Pulse may look different over the next 3 -4 weeks.
The reason for this is that some of you may know that Tracey Koepke, communications director for Duke Heart, was diagnosed with breast cancer in November. She has an excellent care team at DCI, has done well through the first phase of her treatment, and is recovering from the next phase – a surgery. She has been amazing in supporting our teams – and we are supporting her and making sure she knows our thoughts are with her as she works to recover. She is comfortable with my sharing of this information – so keep her in your thoughts and if you get a chance send her a brief note.
While she is out of office (anticipated from till mid July), I have been thinking how to share more with our community. Given the summer time – my sense was to share detailed but concise reviews of things that I am reading – scientific and otherwise, a “summer reading list” if you will. The intention is to provide some thoughts and hopefully stir discussion amongst our community on topics of interest. This weekend I have been on call for our cath lab – so as with several cases and the energy of working with our teams and fellows near the end of their year of training – I wanted to share some thoughts on a book I recently read.
So first – the book that I wish to have you all consider is Super Agers by Eric Topol. As with everything Eric Topol does – it is a factual, easy to read, and informative book on some key themes that I believe will play a bigger role in all of medicine.
First, Eric Topol is a well known cardiologist (with many ties to Duke Faculty) and a history of working on some of our initial clinical trials in cardiovascular medicine, coronary revascularization – as I contemplate where we are with acute MI care this weekend and work with our team at Duke to carry out many of the lessons that Drs. Topol, Califf, Stack, Phillips, Granger, Ohman, Newby, Mark, and countless others have taught us. He is currently the founder and directly of the Scripps Research Translational Institute and still practices cardiology. He is also know as a digital health expert and broad thinker. He was previously also Director of the Cleveland Clinic Heart and Vascular Institute.
The concept for Super Agers he notes came from a study he performed on a cohort of 80 year old and above people with no medications and no signs of systemic disease. They did whole genome sequencing looking for the key genomics as their first hypothesis on what will be different for these people. And found that they are mostly healthy based on a serious of environmental and behavioral findings – and there was nothing in the genome sequences they could find to distinguish these peoples good aging.
These “Super Agers”—individuals who not only live longer but also maintain remarkable cognitive abilities, physical health, and emotional resilience well into their later years seem to have several findings. As noted – the answer is not in their genes. In fact, many had family members with many more clinical issues.
Fundamentally, Topal notes the big three (Cardiovascular disease, Cancer, and Neurodegenerative disease) are the keys to work on achieve Super Aging. In fact, he notes that all of these conditions often “inclubate” for 10- 20 years before clinically manifesting. Herein lies the greates opportunity with new science, technology – when added to routine daily behaviors.
Some Key Themes from the book:
- Defining Super Agers:
- Topol defines Super Agers as those who exhibit exceptional cognitive abilities and emotional well-being in their later years (above 80). They often outperform their peers in memory tests and maintain strong social connections.
- Biological and Environmental Factors:
- The book explores the interplay between genetics, lifestyle choices, and environmental influences on aging. Topol emphasizes the importance of diet, exercise, social interaction, and mental stimulation in promoting healthy aging.
- The Role of Technology:
- Topol is a strong advocate for the integration of technology in healthcare. He discusses how digital health tools, such as wearable devices and telemedicine, can empower individuals to take charge of their health and monitor their well-being.
- He highlights how the confluence of AI, omics, Lifestyle +plus (resistance / muscle training / diet / GLP-1), cells, and drugs and vaccines will lead to many more super agers.
- Neuroscience of Aging:
- The author examines advances in neuroscience that shed light on how the brain changes with age. He discusses neuroplasticity and the potential for the brain to adapt and grow, even in older adults.
- Real-life Examples:
- The book is enriched with stories of Super Agers and insights from researchers in the field of gerontology. Many of these story serve to help understand the work. Importantly – many of the chapters have great tables and all have references.
- Topol provides actionable recommendations for readers to enhance their cognitive and physical health. This includes adopting a Mediterranean diet, engaging in regular physical activity, maintaining social relationships, and pursuing lifelong learning.
Key Biologic Insights:
As is often the case with Eric Topol – he has summarized an amazing amount of information. He covers the GLP-1 and Gut-Brain axis, the biology of aging and three peaks for proteins that work to age, he covers gene editing and beyond, and ends with providing the overall impact of high computational biology and Agentic AI. These parts of the book provide what is likely the processes that we all will see explored to make breakthrough or continue those in diagnosis, immune reprogramming, and measures of biologic age. The book provides over 300 references.
My Take Home Message:
This is one of the next big frontiers for us to consider and conquer in how we move from caring for patients with existing and clinical disease to true prevention of cardiovascular, cancer, and neurodegenerative disease. Many of the process and underpinnings are similar, the technology and data for individual personalization are upon us. Hopefully we can all play a part in building trust in the scientific community and process to ensure these breakthrough reach all in our community.
The book is worth a read if you have the time and interest. Now for me – back to call with our great interventional fellow and team to ensure we can help those with urgent needs while we strive for a better world of prediction and care. Hope you all have a good week and I am open to any other summer reading suggestions from our Duke Heart Community.
Duke Heart Pulse: January 5th 2025
Chief’s Message:
Hopefully you all had some time over the holidays to get some time to reflect, relax, and come back rejuvenated to help us with our mission of improving the cardiovascular health of our community and country in 2025. Thanks to all of you that helped care for our patients and deal with unexpected challenges that our system faced with the brief ED closure.
Over the first few weeks of 2025 – we will spend a little time just highlighting a number of the amazing accomplishments and people we have in Duke Heart. Today we will highlight some of the people and awards over the last year. This is not an exhaustive list but one we thought would represent the accomplishments of so many. In the upcoming weeks we will highlight key research work with publications/findings and ongoing studies. Thank you all for the support and we look forward to continuing our work in 2025!
2024 Comes to a Close and 2025 Begins
2024 Began with a kick-off celebration of the Centennial for Duke University. The event included Duke Health faculty members Dr. Joseph Turek and Dr. Louise Markert who appeared as part of a special segment featuring the story of Easton Sinnamon, the now 3-year-old boy who received the world’s first combination heart transplant-thymus procedure here at Duke in 2021.
In January, we learned that St. Jude Children’s Research Hospital has invested nearly $13 million toward a new collaboration with researchers at Duke, Columbia, and Stanford Universities to expand the understanding of G-protein coupled receptors (GPCR), vital proteins that have been linked to more than 100 human diseases and disorders. The GPCR Collaborative is led by Scott Blanchard, PhD, and M. Madan Babu, PhD, of St. Jude’s. The two are partnering with Jonathan Javitch, MD, PhD, of Columbia University; Georgios Skiniotis, PhD, and Alice Ting, PhD, of Stanford University, and Robert J. Lefkowitz, MD, of Duke University School of Medicine and Duke Cardiovascular Research Center.
We had a number of faculty take on new roles and appointments in 2024, including:
Jacob N. Schroder, MD, was named Surgical Director for Advanced Heart Failure of Duke Health’s Heart and Vascular Service line and the Duke Division of Cardiovascular and Thoracic Surgery.
Jeffrey Gaca, MD, was appointed section chief for Adult Cardiac Surgery
Camille Frazier-Mills, MD was named Vice Chief for Clinical Services for Cardiology. Camille Frazier-Mills did an amazing job representing Duke Health as our Triangle Women of Impact nominee for 2024
Schuyler Jones, MD, director of Cardiac Catheterization Laboratories at Duke was named the Endowed Kent and Siri Rawson Director for Advanced Coronary Artery Disease in Duke Heart Center. Separately, he was also named director of our Invasive labs across Duke University Health System.
Chad Hughes, MD, Professor of Surgery, was appointed the inaugural Chief for the Section of Aortic Surgery, a new section housed jointly within the Divisions of Cardiothoracic Surgery and Vascular and Endovascular Surgery. Hughes will also serve as co-director, with vascular surgeon Chandler Long, MD, of the Duke Center for Aortic Disease.
Svati Shah, MD, MS, MHS, was named Vice Chief for Research in the Division of Cardiology. She currently also serves as the Associate Dean for Translational Research and Director of the Precision Genomics Collaboratory and Center for Precision Health. She was also named associate dean for translational research for Duke School of Medicine/
Anita Kelsey, MD was named Vice Chief for Faculty Affairs and Operations in Cardiology.
Jeffrey Keenan, MD, assistant professor of surgery at Duke, was named Surgical Director, Mechanical Circulatory Support.
Deepak Voora, MD, was appointed Executive Director for the Veterans Affairs National Pharmacogenomics Program.
Awards & Recognition
Thomas Bashore, MD, professor of medicine in cardiology, received the Triangle Business Journal’s 2024 Health Care Leadership Lifetime Achievement Award.
Adam Williams, MD received the Thoracic Surgery Foundation (TSF) Every Heartbeat Matters Award for medical outreach in Honduras via our Duke Heart for Honduras program.
Senthil Selvaraj, MD was been selected as a recipient of an American Society for Clinical Investigation (ASCI) 2024 Young Physician-Scientist Award (YPSA).
Kevin Cox was named to the 2024 Great 100 Nurses of North Carolina.
Duke cardiologist and rehabilitation specialist, William Kraus, MD, was selected as an American College of Sports Medicine (ACSM) Citation Award winner for 2024. The prestigious Citation Award recognizes distinguished individuals who have made significant contributions to sports medicine and/or to the exercise sciences.
Perfusionist Scott Snider Received the 2024 AmSECT Award of Excellence
Kevin Thomas, MD, professor of medicine in cardiology and vice dean for Diversity, Equity and Inclusion for Duke School of Medicine, was selected by the Heart Rhythm Society (HRS) to receive it’s 2024 James H. Youngblood Excellence in Leadership Award.
Pamela Douglas, MD, was one of four Department of Medicine faculty members to receive the 2024 Department of Medicine Career Achievement Award recognizing their extraordinary impact on one of the department’s three core missions: education, research, and clinical medicine.
Zak Loring, MD was awarded an AHA VISN 6 Career Development Award
Dennis Narcisse, MD, was selected for 2024 ACC Career Development Award
Duke’s Heart team received the Society of Critical Care Medicine’s (SCCM) “Family-Centered Care Innovation Award” for Duke University Hospital.
The Duke Perfusion team recently earned its second Pillar Award for Perfusion Excellence from the American Society of Extracorporeal Technology (AmSECT).
Duke’s Extracorporeal Membrane Oxygenation (ECMO) Specialist Team achieved – for the very first time — 100 percent ELSO Adult ECMO Practitioner Certification (E-AEC) for our experienced ECMO Specialists.
We earned a Mitral Valve Repair Reference Center Award for the fifth year in a row. Duke is one of only 22 mitral repair centers recognized by the Mitral Foundation as having the volume and outcomes needed to qualify for the honor.
The American Heart Association’s (AHA) Council on Quality of Care and Outcomes Research (QCOR) Council presented Adrian Hernandez, MD, with their Outstanding Lifetime Achievement Award during the AHA Scientific Sessions in November.
National Professional Society Leadership:
Below is a list of the national organizations in which our faculty serve on the national board or executive role
- American Association of Heart Failure Nurses: Steph Barnes – Board Director
- Heart Failure Society of America (HFSA) 2024-2025: Mike Felker as President
- Society of Cardiovascular Angiography and Intervention (SCAI) – Board Trustee: Raj Swaminathan
- Heart Rhythm Society (HRS): Board Trustee: Jon Piccini, Program Chair for Sessions: Sana Al Khatib
- American Heart Association (AHA): National Board: Svati Shah, Manesh Patel
- American Association for Thoracic Surgery (AATS): National board: Thomas A. D’Amico
School of Medicine Faculty awards:
The cardiovascular team was blessed to have several members recognized at the School of Medicine Faculty Awards for 2024.
- Adrian Hernandez, MD, professor of medicine in cardiology received an Excellence in Professionalism Award
- Christopher Holley, MD, PhD, associate professor of medicine in cardiology received a Research Mentoring Award
- Anita Kelsey, MD, MBA, professor of medicine in cardiology received the Master Clinician/Teacher Award
- Neha Pagidipati, MD, MPH, associate professor of medicine in cardiology received a Research Mentoring Award
- Madhav Swaminathan, MBBS, professor of anesthesiology, cardiothoracic anesthesiology/ critical care, received the Master Clinician/Teacher Award
- Annemarie Thompson, MD, professor of anesthesiology, pediatric cardiothoracic anesthesiology, received a Leonard Palumbo Jr., MD Faculty Achievement Award
Firsts & milestones
1st Barostim Device was implanted in January. Barostim is an implantable device now being used in heart failure patients with reduced ejection fraction.
In February we celebrated our record 161 heart transplants completed in 2023 and the 2000 Heart transplant milestone. Later that month, we implanted our 1500th Durable VAD.
In March, Duke became the first enroller for the Pulmonary Artery DenerVation Clinical Study Using the Gradient Denervation System in Heart Failure Patients with Pulmonary Hypertension Group 2 (PreVail-PH2 Study), an early feasibility, device study enrolling heart failure patients with pulmonary hypertension (PH).
Last summer, the Duke heart transplant team helped pioneer a new generation of Total Artificial Heart — A young Graham, NC, father became the second person in the world to receive a BiVACOR Total Artificial Heart (TAH) as a bridge to transplant, living with the device for 10 days before undergoing a heart transplant at Duke University Hospital.
Our first TriClip procedures were performed at DUH in September. The U.S. Food and Drug Administration approved the TriClip transcatheter edge-to-edge repair (TEER) system in April. The TriClip TEER procedure, performed in the cath lab, offers a minimally invasive approach designed to repair severe tricuspid regurgitation, or a leaky tricuspid valve, in patients with severe symptoms.
Forsyth County, NC became the first county in the state to sign on for a partnership with Duke for feasibility testing of AED drone delivery to cardiac arrest bystanders.
Philanthropic Success!
1.5M legacy gift from an anonymous family to support Duke Heart Transplant patients, and a gift from HCLC member Bob Keegan, who kicked off fundraising for the Duke Heart Precision and Innovation Collaboratory with a gift of $1.5 million toward the $10 million fundraising goal.
Additionally, NC Walk for Victory and AHA Triangle Heart Walk were both big successess and we look forward to supporting both events again this year
The cardiology fellows named Paula Rambarat, MD as chief cardiology fellow for 2024-2025.
We welcomed new family members: Rocky Matthew Davis, Patrick Tulp, Beck Allen Kusner, and Aspen Andreae.
We also mourned the passing of Aslan Turer, MD; Richard Everely “Rip” Waters, II, MD; Kristine Arges, RN; and HCLC member Scott Braswell.
And we wished Drs. Tom Bashore, Mike Sketch, Harry Phillips, and long-time team member Corey Miller all the best as they embarked on retirement.
We matched an incredible team of cardiology fellows for our incoming class of 2025!
Here’s to additional success and celebrations in the coming year!
Duke Heart Pulse – July 23rd 2023
Highlights of the week:
Pineda Rejoins Duke Heart Team Effective July 1
 We are pleased to welcome Andres M. Pineda Maldonado, MD, assistant professor of cardiology in the Duke Department of Medicine back to the Duke Heart team. He is an interventional cardiologist and structural heart disease specialist who started with us on July 1.
We are pleased to welcome Andres M. Pineda Maldonado, MD, assistant professor of cardiology in the Duke Department of Medicine back to the Duke Heart team. He is an interventional cardiologist and structural heart disease specialist who started with us on July 1.
Many of you may remember Dr. Pineda from his Structural Heart Disease fellowship training at Duke, which he completed in 2017.
Originally from Bogota, Colombia, Pineda completed his internship and residency in internal medicine at Mount Sinai Medical Center in 2012, where he also completed cardiology fellowship (2012-2015) and interventional cardiology fellowship training (2015-2016), prior to coming to Duke for training in structural heart disease.
Upon completion of his Duke fellowship in 2017, he joined the faculty of the University of Florida College of Medicine as assistant professor of medicine in the division of cardiology. At the University of Florida, Pineda served as Medical Director of the Cardiac Catheterization Laboratories for the University of Florida Health Cardiovascular Center in Jacksonville, FL for the past two years. He was also a member of the General Cardiology Fellowship Educational Committee, and a member of the STEMI and the Performance & Quality Improvement Committees for most of his time at Florida, and served as associate program director of their Interventional Cardiology Fellowship Program until his departure in June.
Pineda says he was always inclined toward the sciences, and while studying medicine knew he wanted to do something with procedures and imaging, so interventional cardiology was an obvious choice for him. He says he is pleased to rejoin Duke, saying “I like the team here, the hospital, and the overall area, which I enjoyed during my training. I wanted to join a bigger program for structural heart disease with more opportunities for research and career development.”
Please give Andres and his wife, Barbara Correal, and their children Federico and Santiago a very warm welcome when you meet them. Welcome back to Duke, Andres!
Great Catch, Skowronek & Taylor!
Two members of our Cardiopulmonary Rehab team earned a great catch award this week. Barbara Taylor, RT, recognized a patient was not feeling well and had a new symptom of dizziness during cardiac rehabilitation. She escalated her concern to Lisa Skowronek, RN, who assessed the patient and identified a dysrhythmia. On further assessment, they identified chest discomfort and assisted the patient with self-administration of prescribed nitroglycerine. The patient was transported via EMS to Duke Hospital, where she was admitted for treatment. Lisa and Barbara’s rapid assessment and intervention enabled the patient to receive necessary emergency care.
Way to go! Lisa and Barbara are the 5th and 6th cardiac rehab team members to earn ‘great catch’ awards so far in 2023. Nicely done – keep up the great work!

Kudos to Duke Heart’s “Triple J” Team!


Big kudos to John Lazzari, Jaime McDermott, and Jessica Shumate — collectively known as the APP “Triple J” team — for excellent work and support this week! In a note from Chris Holley, MD, we learned they knocked out eight discharges in one day for him. “That is definitely a record for me, and an incredible amount of work for the team,” he said, and added special kudos to Lazzari who covered all 17 VAD patients on service with Holley last weekend, and then participated in the discharge spree.
In response to Holley’s note, Diane Sauro and Stephanie Barnes added additional shout-out’s to acknowledge the team.

“Our Inpatient Heart APPs are awesome and do a fantastic job. Triple J team — great work. I know this weekend was challenging, but everyone stepped up to deliver the best care to the patients. Great work!” — Diane Sauro, MSN, Director, Advanced Practice
“Thank you for the note recognizing the Triple J team and their work on the Medicine VAD service. Jamie, Jessica and John: thank you all for doing it well and (I’m sure) doing it with a smile on your face. You rock!” — Stephanie Barnes, MSN, Clinical Director for Advanced Heart Failure Services
Nicely done, team! We love the opportunity to provide recognition to our team members — so please keep these terrific notes coming to Pulse!
NOTE: Pulse will not be published Aug. 6 or Aug. 13.
Pulse will be vacationing for a bit in August, as we hope many of you have done already. If not, we encourage you to find time for a break. Whether you find mountains to climb, hammocks to rest in, beaches to walk, or refreshing waters to float on or dip your toes in … where ever you might find yourself this summer, we hope you find much needed rest and rejuvenation!
We’ll break for the weekends of August 6 and 13, then return August 20. Please continue to send accolades and news to us.

Upcoming Events & Opportunities
CD Fellows Core Curriculum Conferences
July 26: Hypertension Guidelines with Michael Blazing. Noon, Zoom only.
July 28: LVAD Basics with Jason Katz. Noon, DN 2001.
Cardiology Grand Rounds is on hiatus for the summer. We’ll be back in the fall!
15th Annual NC RTP Pulmonary Hypertension Symposium
The 15th annual NC Research Triangle Pulmonary Hypertension Symposium will be held on Friday, November 17th at the Durham Convention Center. Faculty directors will be H. James Ford, MD, director of the PH program at UNC, and Terry Fortin, MD, co-director of the Pulmonary Vascular Disease Center at Duke.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
July 14 — Harry Severance
Becker’s ASC Review
What young physicians need to know
https://duke.is/6/zuvf
July 14 — Adam DeVore and Stuart Knechtle
Healio/Cardiology
Overhaul of ‘calcified’ US organ transplant system can expand donor pool, save lives
https://duke.is/p/sgb4
July 14 — Hayden Bosworth and Colleen Burke
tctMD
More Data Show Redlining’s Lasting Impact on CVD Risk
https://duke.is/r/jhx6
July 14 — Duke University
MedTech Intelligence
FDA Announces Center of Excellence in Regulatory Science Award Recipients
https://duke.is/5/44ub
July 18 — Duke Regional Hospital
Chief Healthcare Executive
Duke Regional Hospital named America’s most socially responsible hospital
https://duke.is/6/ggkx
July 18 — Sana Al-Khatib and Kevin Thomas
Circ/AHAjournals.org
https://duke.is/p/5mf6
July 19 — Dawn Coleman
Vascular Specialist
Crawford panel looks at opportunities to plug and extend vascular surgery workforce pipeline
https://duke.is/8/xrr5
July 20 — Kristin Newby
Heart.org
Warnings – and hope – from new heart disease treatment guidelines
https://duke.is/j/ugxj
July 20 — Kristin Newby
Newsroom/AHA
Symptom relief and healthy habits are top goals for treating chronic heart disease
https://duke.is/y/fmup
Duke Heart Pulse July 2nd 2023
Highlights of the week:
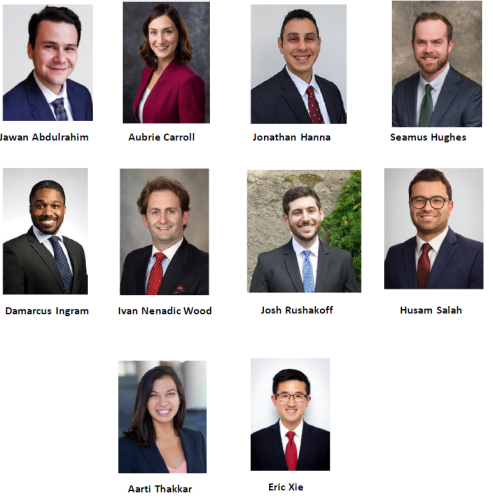
Welcome New Cardiology Fellows!
Each academic year starts with new fellows joining us — and is a reminder of the amazing people we have at Duke, and the impact we have on so much of the future of the field with our training program.
Our brand-new class of Cardiovascular Disease Fellows is listed below. Please give a warm welcome to the following individuals:
- Jawan Abdulrahim, joining us from Duke’s residency program
- Aubrie Carroll, Duke, joining us from Duke’s residency program
- Jonathan Hanna, joining us from Yale’s residency program
- Seamus Hughes, joining us from UT Southwestern’s residency program
- DaMarcus Ingram, joining us from Duke’s residency program
- Ivan Nenadic Wood, joining us from the University of Michigan’s residency program
- Josh Rushakoff, joining us from Cedars Sinai’s residency program
- Husam Salah, joining us from the University of Arkansas residency program
- Aarti Thakkar, joining us from the Johns Hopkins residency program
- Eric Xie, joining us from the Johns Hopkins residency program
Please also welcome our incoming Interventional Fellows:
- Todd Looney
- Sameer Prasada
And our incoming Structural Heart Disease Fellow:
- Ezequiel Munoz
We’re thrilled to have them joining us. Our new team started with us on Saturday. A huge THANK YOU to Bradi and Chris Granger who hosted the fellows’ welcome party at their home last night! The cardiovascular disease fellows have orientation and bootcamp activities this week and will start on their services Saturday, July 8.

Transition and Welcome to DHIP!
As we kick off July and a brand-new fiscal year, we’re also entering into a Health System milestone: the Duke Health Integrated Practice (DHIP) launched yesterday.
Our deep gratitude to all team members for their patience during this transition, and to those who have been closely involved in the planning and rolling-out of DHIP. This was not an easy effort. The future is indeed bright at DUHS, and we are blessed to be part of the great Duke Heart team!
Klotman Named Exec. VP for Health Affairs
In a message sent to all Duke University and Health System faculty and staff on Friday, Vincent Price, president of Duke  University, announced the appointment of Mary Klotman, MD, as Executive Vice President for Health Affairs, effective July 1.
University, announced the appointment of Mary Klotman, MD, as Executive Vice President for Health Affairs, effective July 1.
In this newly-created role, Klotman will report to Price and will serve as the university official providing strategic oversight of university academic health affairs, in close coordination and collaboration with the Provost, Executive Vice President, and CEO of Duke University Health System (DUHS). She will be the chief academic officer of Duke Health, responsible for strategic, academic, and budgetary oversight and authority for the School of Medicine and its affiliated academic institutes and programs, and will also oversee the Duke-NUS Medical School in Singapore and, with the Provost, oversee other relevant interdisciplinary centers including the Global Health Institute and the Margolis Center for Health Policy.
In this role, Klotman will continue to serve as Dean of the School of Medicine, a position she has held since 2017. In that capacity, she will report to the Provost; Vincent Guilamo-Ramos, Dean of the School of Nursing, will also report to the Provost.
In the announcement, Price stated, “Mary is an exceptional physician-scientist, leader, and colleague who is deeply committed to advancing biomedical science and human health through education, research, and patient care. As Dean, she has overseen advancements in research, teaching, and administration that have propelled the School of Medicine to new levels of national recognition and research activity. Under her leadership, the school has implemented significant new programs to advance diversity, equity, and inclusion; assure scientific integrity; and recruit, retain, and reward outstanding faculty. Mary is also a quadruple Duke alumna, having earned her undergraduate and medical degrees, and completed both her medical residency and fellowship, here at Duke.”
Klotman’s appointment follows a restructuring of the leadership model for Duke Health’s academic and clinical missions, which were previously consolidated under Gene Washington, MD, who served as Chancellor for Health Affairs of Duke University, and President and CEO of DUHS.
As part of the announcement of the transition in leadership, Price also recognized Dr. Washington’s many contributions, and thanked him for his distinguished service to Duke over the past eight years.
Under the new leadership structure, Klotman will oversee Duke Health’s academic mission, and Craig Albanese, who was named CEO of DUHS earlier this year, will oversee the clinical enterprise, reporting jointly to the DUHS Board of Directors and to President Price. The new leadership structure, Price stated, will help position Duke for success in the face of the challenging landscape for academic medical centers, including the changing healthcare marketplace, the need for more efficient and effective patient care models, and the ongoing imperative to support high quality medical research. The health system and university governing boards will regularly monitor the effectiveness of this new leadership structure.
Klotman and Albanese will work in close partnership to build deep alignment between Duke’s academic and clinical missions, and will establish shared goals and strategies, closely aligned organizational performance metrics, and other mechanisms to ensure effective connectivity and coordination across Duke Health. Each of them will be accountable for building a shared culture that capitalizes on the ways in which health science research and discovery and health delivery benefit each other, including agreed-upon goals and strategies that will be reflected in their individual performance assessments and incentives.
In the coming weeks the two will be in touch with the Duke Health community to provide more specific updates about how they will operationalize the new leadership structure, Price added.
Their partnership will be informed by the recommendations of a consultative committee that recently worked on behalf of the Office of the University President to seek expert input and advice regarding the new Duke Health leadership structure.
“I am grateful to the members of the consultative committee, as well as the individuals they interviewed, for their valuable perspectives and thoughtful guidance,” Price said. “I am confident that, with Mary joining my leadership team as Executive Vice President for Health Affairs, we will be well positioned to meet the challenges and realize the opportunities ahead, and I hope you will join me in congratulating her on her appointment.”
Congratulations, Dr. Klotman!
TAVR Procedures Added to DUH Cath Lab; Lead Extractions to EP Lab
Congratulations to our interventional teams! The first transcatheter aortic valve replacement (TAVR) procedure to be conducted in the Duke University Hospital Cath Lab occurred on Wednesday. We are incredibly excited to celebrate this milestone and all those who made it possible.
A multidisciplinary team of TAVR cardiologists and surgeons, cath lab nurses and CV invasive specialists, anesthesiologists and CRNAs, members of Duke Heart’s Center of Excellence, Cardiac Diagnostic staff, Cardiac OR and Cath schedulers, CVSSU and 7West nurses, Heart APPs and operational leaders met weekly for months to map and test workflows, and performed dry runs in preparation for this day, according to Jill Engel, VP for Duke Heart Services.
“It is a really exciting time for our patients that are presenting now for TAVR because with the addition of the procedural space in the cath labs being able to perform TAVR safely for them we’re able to get them in quicker, said Anna Mall, MSN, Assistant Nurse Manager, Adult Cardiac Cath Lab.
Mall says the Duke team had been seeing patient volume that exceeded the capacity of the current traditional TAVR process that is done in the OR. By adding the ability for the cath lab team to do these procedures on patients who are at low-risk for their TAVR procedure will allow patients to move through the care system faster, so they can get the care that they need quicker – which is important for this patient population.
“Although there may be other cath labs within NC with the capability to perform low-risk TAVRs, I think what sets Duke apart from other facilities is that now we have a greater ability to care for the patients that have complex needs and require the high-risk TAVR procedure in the OR, as well as the space for patients that are low-risk, as well,” Mall says. “We can be more all-encompassing now in our approach to ensuring that we’re able to care for any patient in need of TAVR in the most equitable way possible.”
To create a successful foundation for the discussions that began earlier this year, an interdisciplinary team of leaders was called together. By engaging different stakeholders from across the clinical space and the IT space, the team was able to get everyone on the same page to make sure that all of the processes for outpatient visits, the inpatient procedure, and transfer to the inpatient unit were all addressed.
“Major kudos to the entire Duke Heart Cath lab team for their tremendous effort as part of our commitment to expand services for patients. This initiative, led by Dr. Andrew Wang and Anna Mall, was masterfully planned and executed, said Engel. “This expansion of TAVR procedures to the Cath Lab demonstrates the tremendous skill and dedication of the entire team that makes Duke Heart a great place for our patients, families and staff.”
Great expertise from a talented multidisciplinary Duke Heart team is ensuring our patients can navigate cardiovascular care without major roadblocks.
“Our team was incredibly committed to getting this done for the patients. So much work went on behind the scenes to enhance how quickly patients can come for care to Duke. With this team and creating this process, the patients were completely at the center of everything that we did; everyone talked about ‘how can we improve care for the patients,’” Mall added.
“The process was amazing – the team was amazing – everyone working together to get this done. And then to see it in action this week and for it to go off so smoothly was an incredible testament to everyone’s contributions. The engagement of our teams is such a strong suit here at Duke Heart.”
Shown here are members of our cath lab recovery team, L-R: Mackenzie Sbashnig, Grace Eckler, Caroline Jenkins, and Anna Mall:

Great teamwork! L-R: J.D. Serfas, MD; Brad Cash, CVIS; Jeff Gaca, MD; Dylan Skiscim, RN; Todd Kiefer, MD; Gordon Pusateri, RN; Cassidy Johnson, RCIS; Wanda Cooley, CVIS; Seth Hanson, CRNA; Kevin Yardley, RN; Andrew Wang, MD; Crosby Culp, MD; Anna Mall, RN, and Miriam Nguyen, RN.

And, in another great example of multidisciplinary teamwork in Duke Heart, we’ve formally added laser lead extraction capability in the EP Labs at DUH.
Due to the increasing volume of patients we are seeing in need of laser lead extractions, we’ve developed a process to identify low-risk candidates in need of laser lead extraction through a partnership across our electrophysiology, CT surgery and cardiac anesthesiology teams. Together, they developed a protocol and policy to permit low-risk laser lead extractions to occur in the electrophysiology lab. Traditionally, laser lead extractions are done in the Hybrid OR with perfusion and CT surgery on standby, said Shawn Johnson, nurse manager for adult cath/EP and the Short Stay Unit. “This addition expands the EP lab’s ability to serve a broader patient base.”
To qualify as a low-risk patient case, the individual would require an infection as the primary indicator for the lead extraction; a prior sternotomy; an implant dwell-time of less than five years; no high-risk CT scan findings, and agreement between CT surgery and electrophysiology to proceed as a low-risk candidate.
Amazing job, everyone! Congratulations to all!
Graduating IC Fellows, Structural Fellow Celebrated!
Our Duke Interventional Cardiology Fellowship graduates and Structural Heart Fellowship grad were celebrated at our annual End-of-Year dinner for them on Thursday evening, June 29, at The Rooftop of the Durham Hotel in downtown Durham. It was another wonderful evening of accolades and reminiscing! We wish each of our fellows the best as they transition as follows:
- Caitlin Drescher, MD, who is entering into private practice with Prisma Health Carolina Cardiology Consultants.
- D. Serfas, MD, who is joining the faculty at the University of Kansas and Children’s Mercy Hospital in Kansas City.
- Doosup Shin, MD, who will enter research/advanced fellowship at Saint Francis Hospital in Roslyn, NY.
- Zachary Wegermann, MD, is joining the Duke Heart faculty. He was out of town and missed the dinner, unfortunately, but we celebrated him nonetheless!
Congratulations, Caitlin, J.D., Doosup, and Zach!

Barnes Inducted into AAHFN
Congratulations to Stephanie Barnes, MSN, AGPCNP-C, CHFN, PCCN, Clinical Director for Advanced Heart Failure Services here at Duke! She was inducted to the Board of the American Association of Heart Failure Nurses (AAHFN) during the annual meeting of the AAHFN held this weekend in Boston. Barnes has chaired the annual meeting for the past two years; she will serve a four-year term with the Board.
“She represents the best of Duke’s Heart Failure team,” said Robert Mentz, MD, section chief for Heart Failure. “She’s a national leader in HF and we’re proud of her leadership.”
Way to go, Stephanie!

Palma, Swaminathan Recognized at ASE
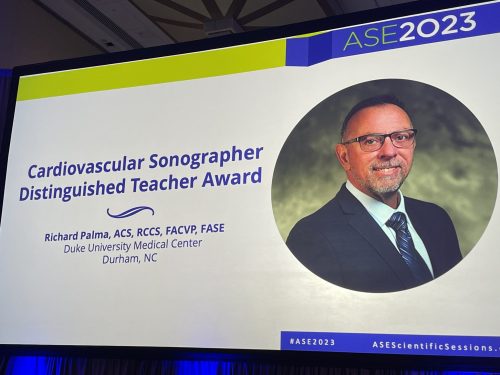 Congratulations to Richie Palma, Director of the Duke Cardiac
Congratulations to Richie Palma, Director of the Duke Cardiac

Ultrasound Certificate Program and Madhav Swaminathan, MD cardiothoracic anesthesiologist, for their well-deserved recognition at the 2023 American Society of Echocardiography Scientific Sessions, held June 23-26 in National Harbor, MD. Palma received ASE’s Cardiovascular Sonographer Distinguished Teacher Award, while Swaminathan received their Outstanding Achievement in Perioperative Echocardiography Award.
Congratulations! We’re so proud of you both and glad to have you on the Duke team!
Fox to Serve as Clinical Nurse Specialist, Effective July 3, 2023
Duke Heart is pleased to announce that Allison Fox, MSN, APRN, AGCNS-BC, PCCN will become Clinical Nurse Specialist  for the DUH Heart Stepdown Units, Cardiac Diagnostic Unit, and Cardiac MRI effective Monday, July 3. As Clinical Nurse Specialist, she will collaborate across Heart Services to identify patient care problems, implement approaches to these problems, and evaluate the effectiveness of the approaches.
for the DUH Heart Stepdown Units, Cardiac Diagnostic Unit, and Cardiac MRI effective Monday, July 3. As Clinical Nurse Specialist, she will collaborate across Heart Services to identify patient care problems, implement approaches to these problems, and evaluate the effectiveness of the approaches.
Allison joined the Duke Heart team in 2018 as a Clinical Nurse I on the DUH Cardiology Stepdown Unit, 7100. During her time at Duke, Allison advanced to a Clinical Nurse III, served as a preceptor, charge nurse, diabetes champion, Tikosyn champion, and on the Orientation Committee. In 2021, Allison transferred to the Adult Cardiac Electrophysiology Lab. Allison is also a member of Heart Rhythm Society (HRS), American Association of Critical Care Nurses (AACN), and the National Association of Clinical Nurse Specialists (NACNS). Allison serves on the graduate education committee of the NACNS.
Allison earned a Bachelor of Science in Nursing from George Mason University in 2018 and a Master of Science in Nursing- Adult Gerontology Clinical Nurse Specialist from East Carolina University in 2023. Her credentials include Progressive Care Certified Nurse and Adult Gerontology Clinical Nurse Specialist.
Please join us in congratulating and welcoming Allison to her new role!
Dial Named ANM for Adult Cath Lab
 We are pleased to announce Rebecca Dial, RN as the new Assistant Nurse Manager of the Adult Cath Lab here at Duke University Hospital. Rebecca has worked in the Cath Lab at DUH since 2020 and previously served as a Charge Nurse. Please welcome Rebecca to our HC Leadership Team!
We are pleased to announce Rebecca Dial, RN as the new Assistant Nurse Manager of the Adult Cath Lab here at Duke University Hospital. Rebecca has worked in the Cath Lab at DUH since 2020 and previously served as a Charge Nurse. Please welcome Rebecca to our HC Leadership Team!
Congrats, Rebecca!
Mall Named Clinical Nurse Specialist, Effective July 3, 2023
Duke Heart is pleased to announce that Anna Mall, MSN, APRN, ACCNS-AG, CCRN, CNL will become Clinical Nurse Specialist for the DUH Heart Center effective Monday, July 3, 2023. As Clinical Nurse Specialist, she will collaborate with Heart ICUs, Invasive Labs, CVSSU, and Patient Response Program to drive practice changes throughout the organization, and ensure the use of best practices and evidence-based care to achieve positive patient outcomes.
Heart ICUs, Invasive Labs, CVSSU, and Patient Response Program to drive practice changes throughout the organization, and ensure the use of best practices and evidence-based care to achieve positive patient outcomes.
Anna joined the Duke Heart team in 2014 as a Clinical Nurse III in the Adult Cardiac Cath Lab. She has served in the department as the Assistant Nurse Manager since 2019. She leads the department’s Cath Lab Nursing Research Group and serves as a Principal Investigator on several study teams. Anna is highly engaged in the American Association of Critical Care Nursing as a member of the Clinical Advisory Workgroup. She is also a member of the National Association of Clinical Nurse Specialists.
Anna earned a Diploma in Nursing from Watts School of Nursing in 2008 and a Master of Science in Nursing – Health Care Systems from UNC Chapel Hill in 2019. She then earned a Post-Masters Certificate – Adult-Gerontology Clinical Nurse Specialist from East Carolina University in May 2023.
Please join us in congratulating and welcoming Anna to her new role!
MURDOCK Samples Accelerate Heart Failure Discovery
 The ease and speed of obtaining samples and data from a groundbreaking community-based biorepository at Duke Kannapolis helped to accelerate a recent heart failure discovery by Duke researchers.
The ease and speed of obtaining samples and data from a groundbreaking community-based biorepository at Duke Kannapolis helped to accelerate a recent heart failure discovery by Duke researchers.
A Duke Pathology research team led by Salvatore Vincent Pizzo, MD, PhD used biospecimens and more than 13 years of corresponding data from 690 MURDOCK Study participants to determine that serum pro‐N‐cadherin is an early marker of heart failure. The discovery has the potential to identify patients who would benefit from intervention before they show signs of disease, as reported in the Journal of the American Heart Association.
The Duke Clinical and Translational Science Institute (CTSI) is making thousands of biospecimens and associated clinical outcomes data available to all Duke researchers through the MURDOCK Biorepository Transformation Initiative. Duke Kannapolis is part of the CTSI and directed by Svati H. Shah, MD, MHS.
With just a few clicks, a data exploration tool developed by CTSI enables Duke investigators to easily explore the 12,526-participant longitudinal cohort based in Kannapolis and encompassing Cabarrus County. The MURDOCK storefronts summarize data and samples at a glance.
“The demographics and outcomes of the participants over time is critical, and that is what sets MURDOCK apart from other biorepositories,” said Paul Ferrell, who manages Pizzo’s lab and quantified the new biomarker. “We would not have been able to correlate the biomarker with any meaning if we didn’t have that downstream outcome data.”
Tapping into the MURDOCK Biorepository
About a year ago, preliminary research indicated the protein could be a marker for heart failure. Pizzo’s team needed to expand their study and reached out to Duke Kannapolis, hoping to accelerate their research by tapping into the MURDOCK biorepository.
“Our goal was to understand the role of the biomarker effectively and rigorously without waiting a decade for a new, prospective study to accumulate years of data,” Pizzo said. “MURDOCK already had thousands of samples and years of follow-up, saving us an incredible amount of time while delivering the same level of rigorous data collection. The responsiveness of Duke Kannapolis saved us even more time.”
Total time from completing a brief interest form to the conclusion of the study was six months. By comparison, requesting and receiving samples from other biorepositories can take up to two years.
“MURDOCK has been the springboard,” said Kristi Oristian, the postdoctoral research consultant on the team. “We asked a question about the predictive nature of how something might work in the future, but we answered it using previously collected samples and data showing how health has changed over time, thanks to MURDOCK participants who had been completing annual follow-up for years.”
Next Steps
With the publication of the discovery, the research has drawn interest from collaborators and venture capitalists. The team’s next steps include repeating their initial findings in a different population, with additional techniques and a clinical approach.
Ultimately, they want to bring the biomarker to market and see it used in clinics and hospitals. The test for the biomarker is easy to administer and easy to understand, reducing the reliance on specialized equipment or expertise.
“Right now, there is no established community screening for heart failure,” Oristian said. “There are biomarkers that catch it at a later stage, but we are talking about detection well before people start to show symptoms.”
Duke Kannapolis provided Pizzo’s team with two cohorts from the MURDOCK Study. The participants all reported no heart failure when they enrolled in MURDOCK, and the two groups had very similar comorbidities and demographics. The participants who eventually suffered heart failure had the elevated biomarker. Those who never developed heart failure did not.
“It’s really important for us to see that against a background of common American comorbidities like high blood pressure and obesity, the biomarker was able to add additional predictive value to identify the folks who would develop heart failure,” Oristian said.
Providing More Evidence
Using such closely matched cohorts provided more evidence that the biomarker is an independent predictor of heart failure, Ferrell added.
“They have such a large amount of MURDOCK data and samples that they were able to match the cohort of people who did not develop heart failure with those who did,” Ferrell said. “That was a lot of the difficult work that Duke Kannapolis completed and then provided to us.”
The MURDOCK Biorepository Transformation Initiative makes thousands of biospecimens and associated clinical outcome data available to all Duke researchers. Investigators should complete this brief interest form as a first step toward.
Duke Statement Re: Affirmative Action Ruling
As you are aware, the U.S. Supreme Court struck down race-conscious admissions plans at Harvard and UNC-Chapel Hill, citing a 14th Amendment violation. The decision will undercut long-standing admissions policies at colleges and universities across the U.S. that use race as one of many factors in evaluating applicants.
In a statement released on Thursday afternoon, Vincent E. Price, president of Duke University, stated:
“Duke’s position continues to be that diversity is absolutely vital to our educational mission—everyone in our community, and the work they do, benefits from differing perspectives, opinions, and life experiences. We remain steadfastly committed to cultivating a racially and socially equitable Duke to the fullest extent permitted by the law. Over the coming weeks we will review the decision closely and determine what, if any, changes need to be made to our admission processes. We have already been planning for the many potential procedural implications. As this process unfolds, we remain committed to doing everything we can to foster a vibrant and diverse academic community.”
Shout-out to Clinic 2F/2G
A big shout-out to our team members in Clinic 2F/2G for taking time to support Pride Month at Duke Health! We have a diverse community throughout the Triangle and within Duke Health and Duke Heart – it takes all of us, together, to provide amazing care to our patients – thanks for having pride in each other.
Shown L-R are: Quivetta, Pat, Susan, Joey, Anna, Julie, Carolyn, Claire, Teressa, Chelsea, and Hannah of our 2F/2G care team.

Way to go!
Quick Reminders & Updates
“Real Talk” Year-in-Review: In the latest episode of the Real Talk video series, Craig Albanese, MD, MBA, Chief Executive Officer, DUHS, reflects on all that we’ve been through together. His message of gratitude highlights some of our greatest achievements and innovations over the past year. To view the recording, please visit: https://duke.is/m/jy94.
Upcoming Events & Opportunities
Cardiology Grand Rounds is on hiatus for the summer. We’ll be back in the fall!
Watch this space for dates and times of upcoming CD Fellows Core Curriculum Conferences starting next weekend.
Duke SOM Call for Applications: Restorative Justice Pilot Program
The Office for Faculty, in partnership with the Office of Equity, Diversity, and Inclusion, is now accepting applications for a pilot program that will provide training and support for implementation of Restorative Justice interventions in the School of Medicine. Restorative Justice (RJ) is an ethical framework that focuses on building community by living our shared values of respect, honesty, responsibility, empathy, and inclusivity. RJ has its roots in indigenous traditions, which uphold the belief that people are interconnected and that focus on the role of community. Restorative practices can create the environment necessary for building and sustaining relationships, maintaining shared accountability, repairing damage caused by harmful behaviors, and ultimately improving team culture.
About the program: Pilot participants will take part in an intensive RJ training program in fall 2023. Working with their teams and with support from experienced RJ practitioners, participants will develop and implement restorative interventions within their individual units in spring 2024. Participants will become part of a longitudinal learning community of individuals interested in exploring the use of restorative practices in the School of Medicine to shape culture and improve well-being. Participation will require significant time, including in-person classroom training sessions and asynchronous reading and reflection. There will be no charge to the participants or departments that participate. Participants will receive a stipend for participation and completion of activities.
Who should apply: Applications should come from groups of 2-4 faculty and staff from the same organizational unit (department, division, program, etc.) within the School of Medicine. All applicants must have the support of their manager/leader and be able to commit to attending all training dates in person (view dates).
Selection Criteria:
- Team members have a demonstrated commitment to improving institutional culture and climate within the unit, including diversity, equity and inclusion efforts.
- Team collectively has enough capacity, reach and local support to implement RJ practices within the unit.
- Potential ideas for the application of RJ within the organizational unit.
- Faculty and staff representation where possible
- Senior leadership support, including a statement confirming protected time for participants to attend all training sessions and participate in evaluation activities. The letter should confirm support for participants’ implementation efforts in the spring and address likely receptivity of the local unit to restorative interventions/mindset.The letter must be signed by the department chair or division chief for faculty applicants, and the manager(s) for staff applicants.
Evaluation:
Because this project is a pilot, program evaluators expect participants to provide feedback about their experience.
Complete program information and application details are available online: https://medschool.duke.edu/shifting-paradigm-restorative-justice-framework-workforce-well-being
Applications are due August 7.
Questions? Contact Jessica Schonberg, MEd, Director of Educational Programs in the Office for Faculty, at jessica.schonberg@duke.edu
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
June 23 — Adam DeVore
tctMD
Global Numbers Paint Grim Picture of GDMT Uptake, Costs, and HF Outcomes
https://duke.is/w/sp7g
June 23 — Adam DeVore
News & Observer
Duke researchers say new heart transplant method could expand donor pool by 30%
https://duke.is/j/8y8j
June 23 — Robert Mentz
Medpage Today
ARNI Again Shows Modest Benefits in HF With Mid-Range EF
https://duke.is/b/j768
June 25 — Jacob Schroder and Jason Banner
CBS Eye On America
Revolutionary technology is making more heart transplants possible
https://duke.is/n/nmnn
June 26 — Neha Pagidipati
AJMC
Coordinated Care Significantly Improves Treatment Quality for Patients With T2D, Heart Disease
https://duke.is/y/pqbp
June 27 — Lynne Koweek (Radiology)
Diagnostic and Interventional Cardiology
SCCT Issues New Expert Consensus, Provides Multi-society Update to Cardiac CT Medical Terminology
https://duke.is/r/ucxr
June 27 — Neha Pagidipati and Christopher Granger
Medpage Today
Protocol Optimizing Meds for T2D and CVD Pushed Beyond Cardiology Alone
https://duke.is/5/3eu9
June 27 — Neha Pagidipati
docwirenews
Multidisciplinary Approach Improves Care for Patients With Type 2 Diabetes, Heart Disease
https://duke.is/6/c4c6
June 28 — Nishant Shah
Healio/Cardiology
Ezetimibe did not increase diabetes risk in IMPROVE-IT substudy
https://duke.is/p/rt4b
June 30 — Duke/NUS CVMD Program
Lab & Life Scientist (AU)
Stem cell-based regenerative therapy to treat heart failure
https://duke.is/7/nfq5
Duke Heart Pulse June 25th 2023
Graduating Cardiology Fellows Celebrated!
Our Duke Cardiovascular Disease Fellowship graduates were celebrated at our annual End-of-Year dinner on Friday evening, June 23, at The Durham Hotel. We are blessed to have the cardiology fellows that we have, often matching 8-10 out of over 800 applicants. These are men and women with purpose and passion as evident by the graduation dinner. It was a terrific evening and we wish all of them the best as they transition as follows:
- J.D. Serfas, MD, is joining the faculty at the University of Kansas and Children’s Mercy Hospital in Kansas City.
- Matthew Carlisle, MD, will begin his fellowship in Clinical Cardiac Electrophysiology at Duke.
- Ali Corley, MD, will begin her fellowship in Interventional Cardiology at Duke.
- Jessica Duran, MD, will join the Multimodality Imaging & Women’s Cardiovascular Health faculty at Vanderbilt Health in Nashville.
- Karen Flores Rosario, MD, will begin her fellowship in Adult Heart Failure and Transplant Cardiology at Duke.
- Josephine Harrington, MD, will begin her fellowship in Adult Heart Failure and Transplant Cardiology here at Duke.
- Cara Hoke, MD, is joining Duke as an Imaging and Prevention faculty member in the Duke Raleigh practice.
- Anthony Peters, MD, will begin his fellowship in Adult Heart Failure and Transplant Cardiology here at Duke.
- Christopher Wrobel, MD, our chief fellow, is joining the Advanced Heart Failure and Transplant Cardiology faculty at UT Southwestern.

Per tradition, we recognized a number of faculty and fellows with annual awards during the dinner. We’re pleased to share the following:
The following awardees are selected by the current fellowship team:
- The 2023 Outstanding Service Award, awarded to a member (or members) of the hospital staff who demonstrate dedication and excellence in fellow education, goes to Brianna Small and Jeff Washam.


- The 2023 Bashore Faculty Teaching Award for a faculty member demonstrating dedication and excellence in teaching this year goes to Fawaz Alenezi, MD.

- The 2023 Fellow Mentorship Award for a faculty member demonstrating dedication and excellence in mentoring fellows’ careers goes to Svati Shah, MD.

The following awards are given in recognition of our fellows and are made possible by the generosity of donors to our training programs:
The Walter F. Floyd Award for Clinical Excellence goes to a fellow demonstrating the most outstanding skills and acumen. This year’s recipient is Daniel Loriaux, MD.
The Joseph G. Greenfield Award for Research Excellence goes to Josephine L. Harrington, MD.
The Cassell-Saperstein Award for Clinician-Educator Excellence goes to Cara Hoke, MD.
The Brandt and Belinda Louie Award for Excellence in all three missions goes to Matt Carlisle, MD.
Well earned! Congratulations to all of our graduates. Those of you leaving Duke will be missed – please stay in touch!
Duke’s MVRR Center Receives Recognition Award
Congratulations to Don Glower, Jeff Gaca, Andrew Wang, and our mitral valve and Center of Excellence teams! For the second year, our Mitral Valve Repair Reference Center has been notified by the Mitral Foundation (working in collaboration with the American Heart Association) that our application on behalf of Duke University Hospital again met all criteria to earn their 2023 recognition award.
The Award jointly recognizes centers in the U.S. which have a demonstrated record of superior clinical outcomes in degenerative mitral valve repair resulting from evidence-based guideline treatment. The Mitral Foundation’s Scientific Advisory Board, a multidisciplinary group of leaders including surgeons, cardiologists, and imagers from around the country, developed the criteria applied in the evaluation of candidate centers. Based on their review, our center has demonstrated that it continues to meet these high standards of quality care.
Great work, everyone!
Starks Awarded AHA Funding Via Rural PRO-CARE Health Network
A number of principal investigators, including Duke Heart cardiologist Dr. Monique Starks, were alerted this week by the American Heart Association that their innovative cardiovascular research projects have been awarded a portion of $20 million in funding via the Rural PRO-CARE Health Network, newly established by the AHA.

People who live in rural areas of the U.S. are 40% more likely to develop heart disease and have a 30% higher risk of stroke than people who live in urban areas, according to data reported in the 2020 Call to Action: Rural Health: A Presidential Advisory From the AHA and American Stroke Association. At least 20% of the U.S. population live in rural areas and these people face unique health challenges related to individual risk factors, social determinants of health and lack of access to health care. To address this issue, the AHA is funding a new $20 million scientific research initiative comprised of a network of special projects focused on advancing the understanding of the factors that impact health in rural America.
The Health Equity Research Network on Improving Access to Care and other Health Inequities in Rural America is part of the multi-pronged approach of the AHA’s ongoing work to improve health in rural America. Teams of scientists from Children’s Hospital Medical Center in Cincinnati, OH; Duke University School of Medicine in Durham, NC; Oregon Health & Science University in Portland; VA Palo Alto Health Care System in Palo Alto, CA.; and the University of Washington School of Medicine in Seattle will lead the community-engaged research projects. The University of Washington will also serve as the coordinating center for the network, leveraging expertise across network sites and nationally, to help train the next generation of rural health equity researchers, providing consultation and guidance, compiling data reports and coordinating the administration of the initiative.
“Along with higher rates of heart disease and stroke, people living in rural areas of the U.S. have a 20% higher death rate than people in metropolitan and urban areas and rural Americans live an average of three years fewer than their urban counterparts,” said Michelle A. Albert, MD, MPH, 2022-23 volunteer president of the AHA. “Rural populations have higher levels of obesity, diabetes and hypertension and higher rates of tobacco use – all factors that negatively impact heart and brain health. They have also been plagued by increasing prevalence of substance use disorders associated with opioids and methamphetamines. All of these risk factors contribute to poor health. In addition, higher rates of poverty, lower levels of education, lack of public transportation and shortages of health care facilities and providers contribute to the unique obstacles rural communities face in achieving good health. This new research initiative will explore innovative ways to address these challenges, as well as determine how tried-and-true methods can be used to make meaningful change.”
Reciprocal Innovations to Improve Cardiovascular Care in Rural America (Rural PRO-CARE) is the name of the overarching research network. The coordinating center will be managed by a team from the University of Washington School of Medicine, led by Chris Longenecker, MD
Starks’ project, Developing and Testing Drone-Delivered AEDs for Cardiac Arrests In Rural America, is one of five selected for funding. The others include:
- Implementation and Scale-up of the American Indian Structural Heart Disease Partnership (IN-STEP), led by Dr. Andrea Beaton, Children’s Hospital Medical Center in Cincinnati.
- Rural Community Peer Partnerships for Improving Methamphetamine-Associated Heart Failure Screening and Engagement, led by Dr. Todd Korthuis, of Oregon Health & Science University in Portland.
- Implementation and Evaluation of Pharmacist-Based Management of Chronic Heart Failure for Rural Veterans (PHARM-HF), led by Dr. Paul Heidenreich of the VA Palo Alto Health Care System in Palo Alto.
- GROW-RURAL: A Global to Rural Innovation Network to Adapt Evidence-Based Cardiovascular Interventions to Context led by Dr. Chris Longnecker of University of Washington School of Medicine in Seattle.
Congratulations, Monique!
Duke Children’s Ranked Top Children’s Hospital in NC, Peds Heart #2 in US!
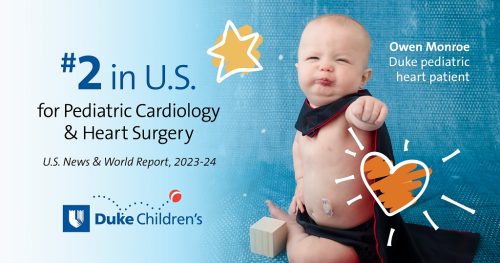 Congratulations to our Duke Children’s Hospital colleagues and especially our pediatric cardiology and pediatric cardiovascular and thoracic surgery teams! Duke Children’s Hospital has been ranked the top children’s hospital in NC by U.S. News & World Report in their annual pediatric rankings for 2023-2024.
Congratulations to our Duke Children’s Hospital colleagues and especially our pediatric cardiology and pediatric cardiovascular and thoracic surgery teams! Duke Children’s Hospital has been ranked the top children’s hospital in NC by U.S. News & World Report in their annual pediatric rankings for 2023-2024.
The ranking of every pediatric specialty improved this year, and all of our pediatric specialties ranked within the top 50 in the nation. We are especially excited for the recognition given to our pediatric heart team for being ranked second in the nation this year.
Congratulations to all for these outstanding pediatric specialty designations:
- Cancer – Ranked 26
- Cardiology & Heart Surgery – Ranked 2
- Diabetes & Endocrine – Ranked 32
- Gastroenterology & GI Surgery — Ranked 20
- Neonatal Care – Ranked 14
- Nephrology — Ranked 31
- Neurology & Neurosurgery – Ranked 45
- Orthopedics – Ranked 23
- Pulmonology – Ranked 23
- Urology – Ranked 19
These distinctions would not be possible without the remarkable work of our team members. Please take a moment today to pause and reflect on the positive difference you make in the lives of our patients and their families.
Way to go!
ICYMI: CMS Provider Enrollment and Revalidation Processes
ATTN PROVIDERS!! The following was distributed via email on Friday, June 23 from the PDC.
If you have recently received an email from CMS or if you receive an email from CMS in the future, you are required to take action in order to continue receiving payment from CMS. The email from CMS is not spam.
If you have not and do not receive an email from CMS in the future, no action is required.
As part of the Centers for Medicare and Medicaid Services (CMS) provider enrollment related to DHIP, enrollment updates and/or revalidation process, some providers may be required to login and complete a two-step process to ensure seamless billing and prescribing under CMS. The email will be sent from CMS (donotreply@cms.gov) with the subject “CMS I&A Connection Request – Action Required.”
This is a two-step process for you to take:
- If you have received or receive in the future an email from CMS (donotreply@cms.gov) with the subject “CMS I&A Connection Request – Action Required“, click the link and sign-in to the portal to approve surrogacy for the Enrollment Specialist to complete the enrollment update. You must approve surrogacy as soon as possible after receiving the email from CMS. By approving surrogacy, this gives the PRMO the authority to act on your behalf with PECOS.
- Once you approve the surrogacy request and the Enrollment Specialist has updated your enrollment record, you will receive a second email from CMS instructing you to login to PECOS and approve the application submission. You must approve the enrollment submission as soon as possible after receiving the email from CMS.
Failure to complete both steps will result in the provider being unenrolled in Medicare and could impact patient care. See the PDC email from 6/23 for an example for the CMS email.
Please note:
Your UserID/password for CMS and PECOS is the same UserID for updating your NPI information within NPPES.
There are additional links for “Forgot Password” and Forgot User ID” if needed:
- Forgot Password – https://nppes.cms.hhs.gov/IAWeb/forgotpassword.do
- Retrieve UserID – https://nppes.cms.hhs.gov/IAWeb/retrieveUserId.do
- Create a New UserID – https://nppes.cms.hhs.gov/IAWeb/register/startRegistration.do
Direct questions to:
Christina Blevins, Director of Provider Enrollment, at Christina.Blevins@duke.edu or to Kristen Mascoe, Manager of Provider Enrollment, at Kristen.Mascoe@duke.edu.
Thank you for your prompt attention to this important matter.
Quick Reminders & Updates
- DHIP Updates: The transition team released a Q&A via email on Friday, June 16 regarding Temporary Medical Leave. If you missed it, you can find all the information here, look under “Benefits Information.”
Upcoming Events & Opportunities
Cardiology Grand Rounds is on hiatus for the summer. We’ll be back in the fall!
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
June 9 — Harry Severance
KevinMD.com
AI-driven solutions for burnout, patient empathy, and worker shortage
https://duke.is/2/ut75
June 11 — Harry Severance
Medpage Today
A Manager’s Perspective on Healthcare Unionization
https://duke.is/z/hex2
June 12 — Harry Severance
Becker’s Hospital Review
Viewpoint: Why this hospital administrator is pro-union
https://duke.is/m/bm6y
June 15 — Duke Health & Jason Banner
Geo TV/Health
Hopes for dying patients awaiting heart donation get new lease on life
https://duke.is/yqsq3
June 15 — Carmelo Milano, Brandi Bottinger, and Alejandro Murillo-Berlioz
Fundahrse.org
https://duke.is/vgkwt
June 8 — Harry Severance
Becker’s ASC Review
Physicians are losing power. Here’s why. (Part 1)
https://duke.is/g/fpht
June 16 — Harry Severance
Becker’s ASC Review
How physician can become ‘captains of their own fates’ once more (Part 2)
https://duke.is/6/7ybw
June 16 — Adrian Hernandez
News & Observer
Biden picks Mandy Cohen, the architect of NC’s COVID-19 response, as CDC director
https://duke.is/n6j26
June 18 — Kelly Arps
Cardio Nerds
https://duke.is/c7ks4
June 19 — Jacob Schroder & Zachary Fitch
VOA News/Health & Lifestyle
Study: New Heart Transplant Method Could Save More Patients
https://duke.is/jb9y2
June 19 — Adam DeVore & Jacob Schroder
tctMD
Randomized Trial Supports Using Hearts Donated After Circulatory Death
https://duke.is/yg6gy
June 20 — James Tcheng
EHR Intelligence
ONC Project Taps FHIR to Extract Over 40% of Clinical Data Registry
https://duke.is/rkv3v
June 21 — Manesh Patel
tctMD
Medicare Data on AMICS Too Muddied for Firm Conclusions on Impella
https://duke.is/7/j66z
June 21 — Duke Children’s Hospital & Health Center
Becker’s Hospital Review
Top 20 children’s hospitals for cardiology, heart surgery
https://duke.is/m/n482
June 21 — Duke Children’s Hospital & Health Center
Triangle Business Journal
Duke Children’s Hospital named best in Southeast by U.S. News & World Report
https://duke.is/8/jtby
June 22 — Kelly Kester
Becker’s Hospital Review
Where have all the preceptors gone? Nurse leaders offer strategies to build a pipeline
https://duke.is/p/sqpa
Duke Heart Pulse June 18th 2023
Chief’s message:
Happy Father’s day to all the fathers and father figures throughout our Duke Heart teams. It is said it takes a village to raise our young, and we want to express our thanks to the fathers who provide love and support to so many. Hopefully you all will have a good day. Also, as we near the end of the Academic year, we will update the coming weeks with our graduating fellows and their future plans and impact on our cardiovascular program and cardiac-thoracic surgery group.
Also – we apologize as we are unable to insert the photos into the blog this week – we will include these in upcoming weeks.
Highlights of the week:
Celebrating Freedom & Juneteenth
Monday is Juneteenth, a federal holiday as of 2021. In honor of that, we are sharing the message issued last week by Chancellor Washington, as well as a short message from Dr. Fatima Zahara Syed.
“Freedom. Heritage. Remembrance. Reflection. Community. Our national holidays provide us with many opportunities to celebrate these fundamental values; and on June 19, we celebrate Juneteenth, the date that news of the Emancipation Proclamation finally made it to the formerly enslaved Black residents of Galveston, Texas — a full two years after the end of the Civil War. Juneteenth is one of our nation’s mileposts in an ongoing story of freedom and self-determination.
Juneteenth points to an essential truth at the core of our national story that freedom must be continually fought for. That is why the flag of Juneteenth is red, white and blue. Today, these colors remind us of our collective responsibility to live up to the beautiful pursuit of liberty and justice for all.
Here at Duke Health, we continue to work on behalf of diversity, equity, inclusion and belonging, because we believe that these ideals are the bedrock of a healthier society. While there is much more yet to achieve, both here at Duke and throughout our nation, we must also celebrate progress.
So this Juneteenth, I hope you will spend time with loved ones, volunteer in the community, and take time to reflect on the many twists and turns in our still unfolding story. In so doing, may we all feel inspired to keep pushing for progress in advancing our founding principles of freedom and equality.” — With appreciation and gratitude, A. Eugene Washington, MD, Chancellor for Health Affairs, Duke University.
“As we strive to foster an inclusive and equitable environment within our department and institution, it is essential that we take the time to reflect on the significance of this day and its relevance to the ongoing fight against systemic racism and social injustice,” said Fatima Zahara Syed, MD, associate professor of medicine in the division of General Internal Medicine and vice chief for Diversity, Equity, and Inclusion for Duke University School of Medicine. “Let us embrace Juneteenth as an opportunity to deepen our understanding, foster empathy, and reinforce our commitment to creating a diverse, inclusive, and equitable environment within our institution and beyond.”
Also worth checking out is this video clip from Duke’s Racial Equity Advisory Council: https://duke.is/vc6d5, which features Kim Hewitt, Duke University’s vice president for institutional equity, and Abbas Benmamoun, vice provost for faculty advancement giving their thoughts on the role of the Council and helping everyone feel welcome across Duke.
Patel Formally Recognized by AHA as Physician of the Year
In a virtual event held Wednesday evening, June 14, the American Heart Association formally acknowledged the recipients of their 2023 National Volunteer Awards – among them, Duke Heart’s Manesh Patel, MD, who received recognition as their Physician of the Year.
The event was hosted by Ray Vara, AHA’s Chairman of the Board, 2021-2023; Dr. Michelle Albert, AHA President; and Nancy Brown, AHA’s Chief Executive Officer. It was emceed by Sonia Azad, health and wellness reporter.
In total, 17 people and organizations were honored, and each honoree was introduced by a surprise special guest. For Manesh, his surprise presenter was Rob Califf, MD, cardiologist, Duke alum, and Commissioner of the Food and Drug Administration.
“One characteristic that I really cherish in Manesh is that he is a mentor,” Califf remarked. “If you look at the people that have come along behind him, he’s helped so many people, looked after them, advanced their careers, and they’ve gone on to do great things. I’ve always thought the best mark of a person in medicine is not the work of the person, but the work of all the people who came along afterwards – you really see what they can do.”
To see a recording of the event, you can watch it on YouTube by clicking here. The section specific to Dr. Patel begins at 1:21:30.
Congratulations to Manesh and his fellow honorees!
Graduating AHFTC Fellows Celebrated!
Our graduating Advanced Heart Failure & Transplant Cardiology fellows were celebrated at an End-of-Year dinner on Friday evening, June 16, at Hawthorne & Wood in Chapel Hill. We are excited for them as they each move into faculty positions! Jamie Diamond is heading to Emory Healthcare in Atlanta; Nima Moghaddam is joining our faculty at Duke, and Vishal Rao will head to MUSC Health.
Congratulations!!!
ICYMI: JCF Series Explores How Eroding Abortion Access Impacts the HF Community
The Journal of Cardiac Failure has launched a series that will explore the intersection of reproductive health and heart failure care following the loss of federal abortion protections in the US nearly a year ago. The series debuted this week with a perspective piece, Pregnancy and Left Ventricular Assist Devices in the Post Roe v Wade Era, co-authored by cardiology fellow Karen Flores Rosario, MD; Jerome Federspiel, MD, PhD; Stuart Russell, MD; Jonas Swartz, MD, MPh; Jason Katz, MD, MHS; Beverly Gray, MD; Stephanie Barnes, NP, and Richa Agarwal, MD.
The recurring feature was announced in a JCF Editor’s Page article by associate editor Nosheen Reza, MD, of the University of Pennsylvania; Editor-in-Chief Robert Mentz, MD, of Duke, and Deputy Editor Anu Lala, MD of the Icahn School of Medicine at Mount Sinai. Several other articles are planned over the coming months. To learn more, see the TCTMD article in our News section.
Shout-out to Shah!
Nishant Shah was quoted in USA Today last week – and received a highlight for that in The Duke Daily. Nicely done, Nishant! To see that news story and many others, see our ‘In the News’ section, below.
Kevin Shah Named CMO for Duke Primary Care
Dr. Tom Owens, executive vice president and chief operating officer for Duke University Health System announced on Monday that Kevin Shah, MD, MBA, has been named Chief Medical Officer for Duke Primary Care (DPC) and Vice President of Duke University Health System (DUHS), effective June 1, 2023.
In this new role, Dr. Shah will be the senior health system leader overseeing the DPC Network with responsibility for clinical quality and outcomes, operational excellence, and financial performance. In close partnership with DHIP and system executive leadership, Dr. Shah will oversee the strategic direction, growth, and deployment of primary and urgent care services across the health system. Dr. Shah will lead a high performing and diverse team of operational and clinical leaders, working collaboratively to prioritize quality and safety for our patients, as well as champion the effective recruitment, retention, and wellbeing of our providers.
Kevin has served as the Interim Chief Medical Officer for DPC since June 22, 2022. He joined the DPC network in 2015 and has served in numerous leadership roles, including Associate Chief Medical Officer for Innovation and Improvement and Associate Chief Medical Officer for Clinical Operations. In these roles, he was instrumental in helping DPC achieve strong clinical quality and operational success. Kevin has worked closely with multiple leaders across our specialty and our inpatient platforms and is regarded by his colleagues as a talented physician, leader and mentor. Dr. Shah is an Associate Professor in the Department of Medicine and continues to see patients at Duke Primary Care South Durham. In his new role, he will report to Dr. Owens.
Quick Reminders & Updates
- Masking is now optional. Duke Health went masking optional as of Tuesday, June 13. Masking is optional for patients, visitors, and team members in most circumstances. NOTE: Guidelines and exceptions are available in Sharepoint.
- DHIP Updates: The transition team released a Q&A via email on Friday, June 16 regarding Temporary Medical Leave. If you missed it, you can find all the information here, look under “Benefits Information.”
Upcoming Events & Opportunities
Cardiology Grand Rounds is on hiatus for the summer. We’ll be back in the fall!
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
June 7 — William Kraus
The Washington Post
Forget 10,000 steps. 7 surprising tips for step counters.
https://duke.is/y3wtu
June 8 — Jacob Schroder
U.S. News & World Report
New Approach to Transplants Could Boost Supply of Donor Hearts
https://duke.is/gykc8
June 8 — Duke University Hospital
Becker’s Hospital Review
This heart transplant method could increase the donor pool by 30%
https://duke.is/vk6sc
June 8 — Jacob Schroder
Washington Hispanic
Al parecer puede ser todo un éxito el nuevo método de trasplante de corazón
https://duke.is/zfsdg
June 8 — Jacob Schroder
Deseret News
‘Reanimated’ heart transplant method could save thousands of lives, increase donor hearts
https://duke.is/m4dt8
June 9 — Jacob Schroder
Medical Daily
‘Heart-In-A-Box’: Innovative Transplant Method Deemed Safe, Could Expand Donor Pool
https://duke.is/88vxz
June 10 — Jacob Schroder
Physician’s Weekly
Survival Noninferior With Heart Donated After Circulatory Death
https://duke.is/2e98g
June 10 — Jacob Schroder
Medical Dialogues
Hearts Donated After Circulatory Death Lead to Similar Survival as Donation After Brain Death: NEJM
https://duke.is/gu6bd
June 12 — Stephen Greene
HCPLive
TRANSFORM-HF Quality of Life Data Further Informs Diuretic Use in Heart Failure
https://duke.is/69jnp
June 12 — Nishant Shah
USA Today
Study reveals how alcohol has heart benefits. Why you should still sip with caution.
https://duke.is/pzd6h
June 12 — Neha Pagidipati
Healio
Risk for heart failure in women after pregnancy underrecognized
https://duke.is/rmkz9
June 13 — Jacob Schroder and Adam DeVore
Gizmodo
Major New Study Finds Way to Significantly Expand Heart Donor Pool
https://duke.is/5jw7e
June 13 — Stephen Greene
HCPLive
SGLT2 Inhibitor Prescription Rates Lag Behind in HFrEF, with Stephen Greene, MD
https://duke.is/nbk3b
June 14 — Jennifer Rymer
tctMD
Off-label DOAC Dosing Tied to Worse Adherence, More Discontinuation
https://duke.is/bgwf7
June 14 — Duke Heart for Honduras
Iconos magazine (Honduras)
Fundación Lady Lee apoya brigada cardiovascular Duke Heart for Honduras
https://duke.is/ckdgw
June 15 — Duke Heart for Honduras
La Tribuna
Banco Atlántida ofrece coctel a la brigada médica “Duke Heart for Honduras”
https://duke.is/wqvwa
June 15 — Michael Pencina
Health Tech
Reduce Healthcare Burnout Through Data-Driven Automation
https://duke.is/jh8cy
June 15 — Karen Flores Rosario and Robert Mentz
tctMD
Journal Series Explores How Eroding Abortion Access Impacts the HF Community
https://duke.is/ydk4s
Duke Heart Pulse June 11th 2023
Chief’s message:
Several highlights this week to demonstrate and again give pause to the amazing breadth of clinical, research and educational work that we do at Duke Heart. The work among our heart failure and transplant leaders and team to expand the donor pool by studying the use of hearts donated after circulatory death (DCD) was published this week in the NEJM. This work exemplifies the magic of health science that expands and informs heart care. This can only happen when there are the highest caliber clinicians and teams working to improve and study clinical care. We also have continued stories on the excellence of our faculty with Dr. Lefkowitz named one of the top 3 scientist worldwide by research.com. We also have excellence in teaching as recognized by our fellows and faculty, with Dr. Anita Kelsey winning the educational award in cardiology in the Department of Medicine. And finally service, as our multi-specialty team again goes to Honduras to support surgical cases, this time with ability to support pediatric cases with our world-class team. By any measure, our groups continue to have local and worldwide impact on the care of people with heart disease across the entire spectrum.
Highlights of the week:
New Heart Transplant Method May Grow Donor Pool 30%
Study finds new technique is equivalent to current standard of care
 For decades, doctors have used hearts donated after brain death as the standard of care for patients awaiting a heart transplant.
For decades, doctors have used hearts donated after brain death as the standard of care for patients awaiting a heart transplant.
A relatively new method of heart transplantation, which allows for the use of hearts donated after circulatory death (DCD), could expand the annual pool of available donor hearts by a projected 30%.
Traditionally, hearts could not be donated after cardiac death. The DCD method in the study uses a machine to keep the heart pumping, making it viable for donation, but also enabling the organ to travel further.
A study led by Duke Health physicians, appearing online June 7 in the New England Journal of Medicine, found that DCD hearts were equivalent to hearts procured through the current standard of care.
“This should eliminate any barriers for transplant centers to offer this to their patients because we now have objective, randomized data showing both types of hearts are equivalent,” said Jacob Schroder, MD, corresponding author and assistant professor in the Department of Surgery at the Duke University School of Medicine. Schroder is the surgical director of Duke’s Heart Transplantation Program.
The study enrolled 180 patients, with half receiving DCD hearts and the other half receiving brain death hearts. It compared risk-adjusted survival at six months and found a survival rate of 94% for those who received a DCD heart and 90% for those who received hearts donated after brain death.
Researchers also looked at serious adverse events 30 days after transplantation, with the mean number of such events at 0.2 for DCD and 0.1 for the standard donated hearts.
Duke Health helped pioneer the use of DCD in the United States, performing the country’s first DCD heart transplant and pediatric DCD heart transplant. The company that developed the technology to keep a DCD heart pumping during transit, TransMedics, sponsored this study.
Duke is now one of around twenty transplant centers in the country that provide DCD heart transplants. Researchers believe the validation from this study should galvanize other centers to consider adopting the method.
“We’ve remained committed to studying the viability of this method out of an aggressive desire to take care of and provide life-saving options for our patients,” said Chetan Patel, MD, study author and associate professor of cardiology in the Department of Medicine.
“Our goal has always been to expand the donor pool to offer heart transplantation to as many patients in need as possible, said Adam DeVore, MD, study author and associate professor of cardiology in the Department of Medicine. DeVore serves as medical director of Duke’s Heart Transplantation Program.
“By finishing and publishing the DCD Heart study, we offer a clear roadmap for other centers to adopt this practice as well,” DeVore said. “Duke has been lucky to be able offer this treatment option to patients since 2019. This has allowed us to offer transplant to more patients in need but also earlier in their disease course – before they become so sick they have difficulty recovering from the surgery. Our goal is to offer transplant to patients at the right time where they can undergo surgery and recover, and still thrive soon after.”
In addition to Schroder, Patel and DeVore, study authors include Benjamin S. Bryner, Sarah Casalinova, Ashish Shah, Jason W. Smith, Amy G. Fiedler, Mani Daneshmand, Scott Silvestry, Arnar Geirsson, Victor Pretorius, David L. Joyce, John Y. Um, Fardad Esmailian, Koji Takeda, Karol Mudy, Yasuhiro Shudo, Christopher T. Salerno, Si M. Pham, Daniel J. Goldstein, Jonathan Philpott, John Dunning, Lucian Lozonschi, Gregory S. Couper, Hari Reddy Mallidi, Michael M. Givertz, Duc Thinh Pham, Andrew W. Shaffer, Masashi Kai, Mohammed A. Quader, Tarek Absi, Tamer S. Attia, Bassam Shukrallah, Ben C. Sun, Maryjane Farr, Mandeep R. Mehra, Joren C. Madsen, Carmelo A. Milano, and David A. D’Alessandro.
Outstanding work – congratulations to the entire team!
Lefkowitz Again Ranked in Top 3 of Scientists Worldwide
 Research.com has released their annual rankings of the Top Scientists in the field of Biology and Biochemistry. Robert J. Lefkowitz, PhD, the Chancellor’s Distinguished Professor of Medicine, a professor of cardiology in the Duke Department of Medicine, and a principal investigator with the Duke Cardiovascular Research Center, currently ranks third in the world and second in the United States. He has also been recognized with Research.com’s Biology and Biochemistry Leader Award for 2023.
Research.com has released their annual rankings of the Top Scientists in the field of Biology and Biochemistry. Robert J. Lefkowitz, PhD, the Chancellor’s Distinguished Professor of Medicine, a professor of cardiology in the Duke Department of Medicine, and a principal investigator with the Duke Cardiovascular Research Center, currently ranks third in the world and second in the United States. He has also been recognized with Research.com’s Biology and Biochemistry Leader Award for 2023.
To see the full summary, please visit: https://research.com/careers/best-biology-and-biochemistry-scientists-2023-report.
Congratulations, Bob!!!
Duke Heart for Honduras – Third Time is the Charm!
More than 20 medical professionals representing Duke Heart and Duke Heart for Honduras are currently on their third trip to  the country – this time with the capability of providing surgical interventions to pediatric patients at Hospital Maria.
the country – this time with the capability of providing surgical interventions to pediatric patients at Hospital Maria.
For those yet unfamiliar with the program, Duke Heart for Honduras is an international cardiovascular surgical outreach partnership program between the Division of Cardiovascular and Thoracic Surgery at Duke and the Instituto Nacional Cardiopulmonar (INCP) in Tegucigalpa, Honduras. Hospital Maria, the pediatric hospital, is also located in Tegucigalpa.
The goal of the program is two-fold. First, the Duke team seeks to help improve survival rates and quality of life for Honduran adults, and now children, with acquired valvular heart disease (often due to rheumatic fever that resulted in rheumatic heart disease). The program was initiated in July 2019 when a surgical team traveled to Honduras and performed surgical procedures for the first time.
The team’s second goal is to provide education and training to local Honduran healthcare providers at all levels to help them better prevent and treat valvular heart disease in that region.
Such a terrific program. We look forward to hearing all about their trip when the team returns!
Cooney End-of-Year Review Focuses on People, Accomplishments, Resiliency
Closing out her fifth year as Chair of the Department of Medicine, Kathleen Cooney, MD, focused on the many  accomplishments of the members of the department on the frontlines as they continue to move us forward and advance our tripartite missions. In her End of the Year Review on Friday, June 2, Cooney noted that we are improving the health of our communities locally, regionally, nationally and abroad as a consequence. Cooney also noted the resiliency of the department’s faculty, trainees who achieved these goals while adapting to major change over the last year.
accomplishments of the members of the department on the frontlines as they continue to move us forward and advance our tripartite missions. In her End of the Year Review on Friday, June 2, Cooney noted that we are improving the health of our communities locally, regionally, nationally and abroad as a consequence. Cooney also noted the resiliency of the department’s faculty, trainees who achieved these goals while adapting to major change over the last year.
If you missed the event, a copy of the recording is available here.
Dr. Anita Kelsey was also awarded the Department of Medicine Excellence in Teaching award for Cardiology at the end of year Department Recognition Event. This award is provided to the Faculty with highest commitment and excellence to education in the Division of Cardiology. Congratulations Anita – well deserved.


CSRC Think Tank Meeting Held
The Cardiac Safety Research Consortium (CSRC) held their Think Tank meeting on June 7 in Washington, DC on the campus of the Food & Drug Administration (FDA). The event, CSRC Think Tank: Update on Regulatory Status of Hypertension, Biomarkers and Arrhythmia Monitoring in Clinical Trials was very well attended – despite the city having air quality not unlike that found in Beijing (see Canadian wildfires, impact on U.S.), according to Mitch Krucoff, MD. Krucoff, professor of cardiology in Duke’s Department of Medicine, is a member of the CSRC and principal investigator for the FDA-Duke Memo of Understanding founding the critical path Cardiac Safety Research Consortium (CSRC) PPP program.
of the Food & Drug Administration (FDA). The event, CSRC Think Tank: Update on Regulatory Status of Hypertension, Biomarkers and Arrhythmia Monitoring in Clinical Trials was very well attended – despite the city having air quality not unlike that found in Beijing (see Canadian wildfires, impact on U.S.), according to Mitch Krucoff, MD. Krucoff, professor of cardiology in Duke’s Department of Medicine, is a member of the CSRC and principal investigator for the FDA-Duke Memo of Understanding founding the critical path Cardiac Safety Research Consortium (CSRC) PPP program.
The event included professionals from FDA Regulatory, EU Regulatory, Japan PMDA, Cardiac Safety Consultants, Ltd., Eli Lilly, Richmond Pharmacology, and academic trialist experts on cardiogenic shock from the University of Connecticut, Stanford University, University of Pennsylvania, Cleveland Clinic, Mass General, DSI, Penn Medicine, and UCSF.
3200/2200 Great Catch Awards to Ameen & Haigh!
The 3200/2200 Cardiology Stepdown team at Duke University Hospital is very proud to recognize Melissa Ameen and Lakyn Haigh for receiving Great Catch Awards!
 Melissa Ameen, BSN, RN, PCCN, identified vital signs populating on the EMR for one of her patients that were very different from the patient’s trend. After investigating, she realized that the patient was admitted to a bedside monitor in another location in the hospital and that the vital signs were actually those of another patient, who was currently attached to that monitor. She caught the problem within 15 minutes, which prevented any of the incorrect vital signs from populating into her patient’s chart. This also ensured that the other patient’s vitals were correctly routed to that patient’s EMR, and that both care teams for the patients had the correct clinical information. Melissa is a Charge Nurse & Preceptor and has been a RN on 32/22 for 7.5 years. Great job, Melissa!
Melissa Ameen, BSN, RN, PCCN, identified vital signs populating on the EMR for one of her patients that were very different from the patient’s trend. After investigating, she realized that the patient was admitted to a bedside monitor in another location in the hospital and that the vital signs were actually those of another patient, who was currently attached to that monitor. She caught the problem within 15 minutes, which prevented any of the incorrect vital signs from populating into her patient’s chart. This also ensured that the other patient’s vitals were correctly routed to that patient’s EMR, and that both care teams for the patients had the correct clinical information. Melissa is a Charge Nurse & Preceptor and has been a RN on 32/22 for 7.5 years. Great job, Melissa!
Lakyn Haigh, RN, noticed that an IV medication was ordered to be administered IV push by drawing up four full vials of medication. Though the dose on the order was correct, the rate was not specified, and she recognized that this unusual administration method was not appropriate. She escalated her concerns twice, after which the formulation of the medication was changed to an IV bag. Lakyn’s willingness to escalate her concern led to a change to a safer and more appropriate administration method for the medication. Lakyn is a Travel RN who has worked on 32/22 for nearly one year. Nicely handled, Lakyn!
Thank you both for taking excellent care of our patients!
Quick Reminders & Updates
- Masking update. Beginning Tuesday, June 13, masking will be optional for patients, visitors, and team members in most circumstances. Guidelines and exceptions are available in Sharepoint.
- PG2 tunnel renovation is complete. New flooring was installed in the Duke University Hospital Parking Garage 2 lobby (tunnel level) throughout the walkway to Duke North. The work was completed last week, so the tunnel is once again fully open.
- DHIP Updates:
Town Hall Held
- On June 7th, DHIP Leadership hosted a community-wide Town Hall covering recent progress within the DHIP transition, Day 1 Expectations, a Training Overview, and Q&A. The recorded session can be found here.
Benefits
- The HR team is engaging in targeted follow-up with transitioning personnel who have not yet completed special enrollment or onboarding.
- Information regarding Duke Benefits is available on SharePoint.
- All benefits related questions can be sent to DHIPBenefits@Duke.edu.
- An email was distributed on 5/30 to all faculty eligible to enroll in benefits regarding an extension to the voluntary short term and long-term disability enrollment period through 6/23.
DHIP Trainings
- Please see the training site; you can register for upcoming trainings and view recorded sessions at PDC Intranet – Home (sharepoint.com)
Badges
- As a reminder, individuals who are DU and DUHS Leased with PDC on the bottom of their badge will be given new badges (rolling basis in July 2023) due to access constraints. DU/DUHS Leased individuals already have horizontal Duke badges which do not need to be replaced.
Reimbursements
- If possible, please submit all current reimbursement requests to PDC.AP@duke.edu by June 22nd for processing.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
May 28 — Jacob Schroder and Jason Banner
CBS News
New method revolutionizes heart transplants
https://duke.is/bpve5
**this story originally ran in Feb. 2023; it has been updated
May 30 — Stephen Greene
Healio/Cardiology
Early, rapid uptitration of HF therapies after discharge reduces death, readmission risk
https://duke.is/4fdpg
June issue — Geoffrey Ginsburg
Environmental Factor
Scientists talk precision medicine, environmental health at NC event
https://duke.is/cx9ry
June 1 — Adam DeVore
tctMD
Boosting GDMT and Improving Outcomes? No Mean Task After AHF
https://duke.is/5nvyd
June 2 — Harry Severance
KevinMD.com/Medpage Today
https://duke.is/w36vs
June 6 — Stephen Greene
tctMD
SGLT2i Still Underprescribed in HFrEF, New US Analysis Confirms
https://duke.is/jz6qb
June 6 — Sana Al-Khatib
Medscape
First-Line or BiV Backup? Conduction System Pacing for CRT in Heart Failure
https://duke.is/yhdm7
June 6 — Rob Mentz
AJMC.com
Combination of Sacubitril/Valsartan May Improve Heart Failure Outcomes
https://duke.is/v6k9w
June 7 — Jacob Schroder
Associated Press
Newer heart transplant method could allow more patients a chance at lifesaving surgery
https://duke.is/8td4m
*this story was carried by 490+ AP outlets including in ABC News, Medscape, and in New York, Los Angeles & Chicago
AP en español
EEUU: Ubican nueva alternativa para corazones donados
https://duke.is/wbwa2
En español via Telemundo:
Estudio: nuevo método quirúrgico podría expandir los trasplantes de corazón a miles de pacientes
https://duke.is/crksk
June 7 — Jacob Schroder
STATnews.com
Reanimated hearts donated after death work just as well for transplants, study finds
https://duke.is/maj2e
June 8 — Adam DeVore
Healio/Cardiology
Outcomes similar with heart donation after circulatory death vs. brain death
https://duke.is/6q9yx
June 9 — Jacob Schroder
CNN
https://duke.is/zcw5a
Duke Heart Pulse 6-4-2023
Chief’s message:
The Spring in North Carolina is notable for clear changing of seasons – with blooming dogwoods, graduations, and new fellows and faculty. We work every year to try to capture some of the amazing accomplishments of some many great cardiology and heart center team members including faculty, advanced practice providers, fellows, residents, and heart center nurses and staff. We will be doing this in the upcoming weeks. Hopefully taking a few moments to celebrate our accomplishments will help energize our teams as we continue to move forward to help improve the heart health of the triangle and below, improve knowledge, and train the next generation. As with all academic years, we also have shared some news of transitions from Duke and with Duke Cardiology Alumni. This week is no exception, as we are excited for Jason Katz as he moves to NYU and Bellevue, but also sad to see him leave us. Additionally, we share that our notable prior DCRI director and Duke Cardiology Alumni – Bob Harrington will become Dean of Weill Cornell Medicine and provost for medical affairs of Cornell University. We look forward to continuing to work with both of them and celebrating their successes in the future.
Highlights of the week:
Katz Departing for NYU Langone Health in November

As noted above, it is with bittersweet emotions, we announce that Jason Katz, MD, co-director of the Duke CICU and co-director of our Mechanical Circulatory Support (MCS) Program, will be departing Duke Health later this fall in order to take on several exciting new roles at NYU Langone Health System.
There, Katz will become professor of medicine and Associate Chief of Cardiology at Bellevue Hospital (the nation’s oldest public health institution), Director of Inpatient Cardiology at Bellevue, Associate Director of the Ventricular Assist Device Program, and Program Director for the NYU Langone Advanced Heart Failure & Transplant Cardiology Fellowship.
Katz has served as the Healthcare System Director of Cardiovascular Critical Care, Co-Director of the CICU, and Co-Director of the MCS Program. He has been influential in expanding and relocating the CICU, creating a CICU APP team, leading a multitude of educational efforts, expanding use of temporary MCS for cardiogenic shock, as well as a number of research endeavors. Katz’s efforts have helped improve the care of critically ill and mechanically-supported patients here at Duke and across the world.
“Above and beyond all of the important efforts noted above, he has been an ideal colleague and I feel fortunate to have him as a friend and mentor,” said Robert J. Mentz, section chief for Heart Failure at Duke. “He is a staunch patient advocate and has taught us all how to be better clinicians.”
In a statement shared with his section team, Mentz included a link to one of Katz’s recent Journal of Cardiac Failure articles – a perspective piece – and said he found it particularly impactful.
Jason represents the best of Duke in so many ways. He will be missed dearly across Duke Heart, and by all the teams with whom he has interacted and helped shape. We wish him all the best in this transition, and are happy to know that we will continue to collaborate across multiple fronts.
A gathering to celebrate Katz and his many successes here at Duke and beyond will be planned over the coming months. We wish him all the best as he joins the team at NYU Langone. Please join us in congratulating Jason on his new roles and in thanking him for all the work he has done on behalf of our patients, trainees, and our entire staff.
Congrats, Jason!
Alumni News: Harrington Heading to Weill Cornell Medicine
 Congratulations to Duke Heart alum Robert A. Harrington, MD, cardiologist and the Arthur L. Bloomfield Professor of Medicine and chair of the Department of Medicine at Stanford University. Harrington this week was named the Stephen and Suzanne Weiss Dean of Weill Cornell Medicine and provost for medical affairs of Cornell University. Harrington is the former Richard Sean Stack, M.D. Distinguished Professor at Duke and had served as Director of the Duke Clinical Research Institute.
Congratulations to Duke Heart alum Robert A. Harrington, MD, cardiologist and the Arthur L. Bloomfield Professor of Medicine and chair of the Department of Medicine at Stanford University. Harrington this week was named the Stephen and Suzanne Weiss Dean of Weill Cornell Medicine and provost for medical affairs of Cornell University. Harrington is the former Richard Sean Stack, M.D. Distinguished Professor at Duke and had served as Director of the Duke Clinical Research Institute.
The announcement was made on Thursday, June 1 by Cornell University president Martha E. Pollack. Harrington will begin his new position on Sept. 12.
Harrington, a member of the National Academy of Medicine, is a past president of the American Heart Association (AHA) and has most recently chaired Stanford’s Department of Medicine, a position he began in 2012.
“In addition to being an outstanding physician-scientist, Dr. Harrington is an energetic and proven leader, with a reputation for bringing people together to achieve shared objectives,” Pollack said. “I am looking forward to working closely with him as we continue to advance Weill Cornell Medicine’s mission as a world-class institution of patient care, scientific discovery and education of future health care leaders.”
Harrington, who grew up and attended college on the East Coast, is excited to be returning to his roots, although he terms the move as “bittersweet” after 11 years in Palo Alto, California.
“The opportunity to come to Weill Cornell Medicine was really extraordinary for us, professionally and as a family,” Harrington said. “I’m excited to help shape an already-excellent academic medical institution into its next version.”
Bob Harrington has mentored and had a tremendous impact on so many in medicine, and this new opportunity will undoubtedly allow a him to expand this impact and reach.
Congratulations, Bob! We’re excited to have you back East!
Women in Cardiology Update
The Duke Heart Women in Cardiology (WIC) group held their end-of-year event on Thursday evening, June 1 at the Washington Duke Inn.
There was a great turn-out for the event with fellows and faculty from all three hospitals across Duke University Health System in attendance – there was even a surprise appearance by Tracy Wang!
“It was wonderful to catch up and enjoy a fabulous spring night on the patio,” said Melissa Daubert, MD. “It was particularly great to see everyone in person with no masks!”
The group plans to continue offering WIC events at least twice per year. If you are not receiving updates about the WIC group or their upcoming events, please reach out to Dr. Daubert to be added to their distribution list.
Quite an amazing group of cardiologists. Great photo, WIC team!

Kudos to 3100 Team!
Kudos and special thanks to the DUH 3100 nursing staff, VAD medical team, and to Colby and Courtney from PT/OT for arranging for a long-term VAD patient to go outside and visit with his pup, ‘Colby Joe.’ Pictured are our patient, Dale*, along with Colby Joe, and Courtney and Colby with Colby Joe.
You can tell by Dale’s smile just how much he appreciated this special visit!
Great job, everyone! What a wonderful way to spread some joy by helping a patient get a bit of fresh air and some time with their beloved pet. *Name and photos used with permission.


Shout-out to Duke EP Team!
We received an outstanding note from an EP patient this week and wanted to share it with you. The patient had seen Drs. Jonathan Piccini and James Daubert, and received care from a number of EP team members while undergoing care at Duke University Hospital.
“I saw [the patient] yesterday in clinic, said Piccini. “He is doing great and he wanted me to share how much he appreciated each and every one of you and the care you delivered. Thanks for all you do for our patients!” — Best, Jon
The text of the letter is as follows, name withheld for privacy:
I am writing this letter to inform you of my superb care at Duke University Hospital 19-20 Jan 2023. I underwent a cardiac ablation led by Dr Jonathan Piccini, Director of Cardiac Electrophysiology. Dr Piccini was referred to me by my brother who Dr Piccini had helped several years ago with a heart arrhythmia problem.
I feel very fortunate to have had Dr Piccini and Dr James Daubert as my providers. Additionally, I would like to specifically thank some of the great members of their team to include Pre-Op: Joy Lombardi and Emily Tedesco; Afib Ablation: Stewart Capps; Post-Op: Jane Schultz, Emily Tedesco, Lauren Guy, Meredith Wilkinson, Isabella Grezzi, Grace Eckler, Mackensie Bashnig, Deanna Bagalawis, and Janice Febre. Please excuse any misspellings as I was trying to capture names while recovering.
I have been lucky to be a member of a number of high functioning teams during my professional life, and you certainly have one with Dr Piccini and his Electrophysiology superstars. I want to thank you and your medical team for an exceptional care experience. – grateful patient
Nicely done, team!
Great Catch, Aiken & Branson!
Janet Aiken, CNII and Michelle Branson, Clinical Exercise Physiologist from our Cardiopulmonary Rehab team, were concerned about a patient’s report of feeling unwell during warm-up for cardiac rehabilitation. The patient requested to go home, but they advocated for further work-up, which showed the patient to be going in and out of ventricular tachycardia. The patient was transported to the Duke Emergency Department via EMS, admitted as an inpatient, and discharged home several days later.
Way to go – truly a great catch!

This Week: DCRI Research Forum with John Scheyer
The Duke Clinical Research Institute team is excited to have rescheduled their Research Forum with special guest John Scheyer, head coach of the Duke Men’s Basketball program. Please join us on June 6, at 9 a.m. for the Forum, which will feature a fireside chat with Scheyer. This will be a virtual event; Scheyer will discuss his journey and the philosophy that keeps him focused on success — both his personal success and the success of his team. We’ll also address how his philosophy and resilience translates to healthcare and our approach to enhancing human health.
What: DCRI Research Forum: A Conversation with Duke Men’s Basketball Head Coach Jon Scheyer
When: Tuesday, June 6 from 9-10 a.m. ET
Zoom Link: DCRI Research Forum
Quick Reminders & Updates
- PG2 tunnel closure begins tomorrow, June 5. New flooring is being installed in the Duke University Hospital Parking Garage 2 lobby (tunnel level) throughout the walkway to Duke North. The work will take place between the hours of 8 p.m. and 5 a.m. on Monday, June 5 and Monday, June 12. Signage will be posted for awareness about the construction area.
Upcoming Events & Opportunities
Cardiac Safety Research Consortium Think Tank Meeting, June 7
The Cardiac Safety Research Consortium will hold a Think Tank meeting on June 7. The event, CSRC Think Tank: Update on Regulatory Status of Hypertension, Biomarkers and Arrhythmia Monitoring in Clinical Trials will be held at the FDA.
In Session 1, these leading industry professionals will speak on panels discussing:
- Regulations for ECG/QT
- The double-negative conundrum
- Alternative methods for assay sensitivity assessment in routine Phase 1 QT Studies
- Covid-19 and prolonged QT
In Session 2, we will discuss:
- Small increases in blood pressure and CV risk I
- Intermittent versus chronic use hypertension drugs
In Session 3, the meeting faculty will dive into:
- Biomarkers
In Session 4, the panelists will discuss hot topics in the field such as:
- Biologics/cardiomyopathy and vaccine development
- MACE
- Gene therapies
- Wearables
The event will include professionals from FDA Regulatory, Cardiac Safety Consultants, Ltd., Eli Lilly, Richmond Pharmacology, University of Connecticut, Stanford University, University of Pennsylvania, Cleveland Clinic, Clario, Mass General, DSI, Penn Medicine, and UCSF.
There is a registration fee for attendance, for academics it is $275. Registration and more information is available here: https://cardiac-safety.org/
The meeting will be held in person; a recording of the meeting and slide presentations will become available a month after the event occurs.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
News coverage will return next weekend!
Duke Heart Pulse May 28th 2023
Chief’s message:
Memorial Day message.
On this Memorial day weekend, we take time to ensure we stop and remember those who have served our country and sacrificed for the freedoms and life we enjoy. For those with the courage and calling to serve, we are thankful and blessed to have them as part of our community and country. For those who have had the ultimate sacrifice and lost a life in the service of our country, we remain forever grateful to them and their families.
As this weekend is also a time for many graduations and transitions, we hope that you get to spend some time with family and friends. We are also thankful for those of you in our Duke Heart community that are not in-hospital caring for patients and their loved ones.
We hope each of you has a safe and relaxing holiday weekend. Thank you for all you do.
Highlights of the Week
SCAI.23 Highlights
The Society for Cardiovascular Angiography & Interventions (SCAI) held its annual Scientific Sessions meeting from May 18-20 in Phoenix, AZ. A number of current and former Duke faculty helped shape the meeting.
 Outgoing SCAI president, Sunil Rao, MD (now with NYU Langone) gave the presidential address to a packed room. Rao received a standing ovation for highlighting a number of SCAI accomplishments during his term including securing a formal NRMP Match process for interventional cardiology fellowship applicants; initiating a new “Ready to Launch” program to introduce future under-represented minority and female medical students to the field of interventional cardiology; establishing the SCAI Early Career Research Grant program, and supporting numerous advocacy and government relation efforts. Congrats, Sunil on all your contributions to the interventional community!
Outgoing SCAI president, Sunil Rao, MD (now with NYU Langone) gave the presidential address to a packed room. Rao received a standing ovation for highlighting a number of SCAI accomplishments during his term including securing a formal NRMP Match process for interventional cardiology fellowship applicants; initiating a new “Ready to Launch” program to introduce future under-represented minority and female medical students to the field of interventional cardiology; establishing the SCAI Early Career Research Grant program, and supporting numerous advocacy and government relation efforts. Congrats, Sunil on all your contributions to the interventional community!
Raj Swaminathan, MD, current SCAI Board of Trustee member, presented primary results from his investigator-initiated national, multicenter ACCELERATION study evaluating the role of contrast FFR in physiologic assessment of intermediate coronary disease. He also participated in a number of events including presenting and serving as a panelist on a widely attended session on renal denervation.
 Tony Gutierrez, MD co-presented data with Marc Bonaca on a novel drug being evaluated in ischemia-reperfusion injury following PCI. Gutierrez also spoke about optimal access site considerations for aorto-iliac disease and served as a mentor for the inaugural Ready to Launch program.
Tony Gutierrez, MD co-presented data with Marc Bonaca on a novel drug being evaluated in ischemia-reperfusion injury following PCI. Gutierrez also spoke about optimal access site considerations for aorto-iliac disease and served as a mentor for the inaugural Ready to Launch program.
Jennifer Rymer, MD was recognized with one of SCAI’s top 30 in their 30s award! This prestigious award is given to  physicians who demonstrate professional excellence in their clinical practice. Rymer also gave a presentation on stent strategies for coronary bifurcations and mentored in the Ready to Launch program.
physicians who demonstrate professional excellence in their clinical practice. Rymer also gave a presentation on stent strategies for coronary bifurcations and mentored in the Ready to Launch program.
Raj Swamy, MD, an experienced interventionalist in the Duke Cath Lab who leads the Duke Lifepoint/CCH cardiology practice in Sanford, NC gave two invited talks on Imaging & AI and new scoring & non-compliant balloons for the treatment of complex, calcified lesions.
Amit Vora, MD, MPH (now with Yale) attended as a member of SCAI’s competitive 2-year Emerging Leader Mentorship (ELM) program. Recognized nationally as a leader in structural heart interventions, he served as a panelist on creative, advanced techniques in structural heart interventions and as a moderator in structural heart hemodynamic pearls.
Alexander Fanaroff, MD, MHS (now with U. Penn) was a recipient of one of SCAI’s Early Career Research Grants and presented his research on “Racial, Socioeconomic, and Geographic Disparities in the Management of PAD and CLI” as well as a featured science presentation on the “Development & Baseline Characteristics of a 1.13M-patient longitudinal cohort to assess CLTI quality of care.”

Strong work to all! We look forward to seeing a strong Duke presence at SCAI.24 in Long Beach, CA!

Friends of Nursing Gala & Duke Heart Winners
Duke’s Friends of Nursing held their 2023 Gala Celebration of Nursing Excellence on Saturday, May 20 at the Durham Convention Center. We’re pleased to celebrate all of the nurses who were nominated and those selected for awards this year, especially the eight winners from Duke Heart, which include:

Catie Dunn, RN received the 2023 Inez “Turk” James Award for Excellence in Nursing Practice. Catie is an RN and an assistant nurse manager for the DUH Patient Response Team. In her role she is responsible for the Behavioral Response Team and the Patient Response Team. This nominee is a powerful advocate for patients who are experiencing behavioral challenges. She strives to partner with the primary care team to identify the root cause of the behavior, rather than simply reacting to the behavior. Often, patients with behavioral challenges can be difficult to work with due to frequent refusal of care, sporadic communication, and caregiver discomfort. However, this nominee always remains unbiased and has an incredible ability to communicate calmly, concisely, and directly. Those who work with this nominee are proud to be her colleague due to her always ensuring that the patient is the focus and that each individual is treated with respect and dignity.
Ashley Frazier, RN, NMO received the 2023 Heart Center Award for Excellence in Cardiovascular Nursing in Recognition of Mary Ann Peter. She works on DUH 7100; Ashley is an exemplary model of a true, dedicated leader who is highly motivated to make a difference in the field of nursing. She promotes accountability, empowerment and team work as she analyze, investigates and obtain feedback to ensure service excellence will be provided.
Hope S. Miles, RN received the 2023 Nan & Hugh Cullman Heart Center Award for Excellence in Nursing Practice. Hope is an RN in the Duke Cardiopulmonary Lab at Duke University Hospital. She has more than 35 years of nursing experience, with 22 of those years serving the Duke community. She obtained her certification as a Certified Cardiac Rehabilitation Professional (CCRP) from the American Association of Cardiovascular and Pulmonary Rehab Profession Certification Commission (AACVPR) in 2017. Her nominator wrote, “Her kind and caring heart is evident to all in the way she approaches each and every interaction. She is always smiling and has a warm and approachable demeanor. She takes the time to listen to her patients and colleagues, making others feel instantly comfortable in her presence. She seeks to truly understand her patient’s reality and the trauma that they have been through using compassion and empathy to make a connection. Through active listening, she engages the patient to examine and set personal goals at the start of the program that are measurable and achievable. She endorses a ‘you can do it’ attitude which motivates the patient to make lifestyle changes and face the future with hope.
Adam Millard, RN received the 2023 Award for Excellence in Critical Care Nursing. Adam is an RN and assistant nurse manager and CNIII on 7W, our Cardiothoracic Intensive Care Unit (CTICU). He also has his CCRN certification. His nominator wrote, “This nominee strongly exemplifies Duke’s professional practice model through his commitment to patient care, performance improvement, and staff development, and multidisciplinary collaboration.” He oversees the quality improvement committee within the unit supporting prevention of hospital acquired infection (HAI), hospital acquired pressure injury (HAPI), patient falls, blood product wastage, and monitoring the unit based fast-track extubation practices. He has led efforts to establish an electronic rounding tool that captures multiple audits, which enables staff to audit efficiently and provide effective coaching where needed. Additionally, he supports unit team members overseeing equipment and medical supplies. Through this work, the unit has decreased null transactions resulting in decreased waste of supplies and improved finances. Moreover, he provides real time coaching at the bedside on a daily basis through his CL role.
Paige Romer, RN received the 2023 Ernestine Davis & Edward L. Cole Award for Excellence in Coronary Care Unit Nursing. Paige is currently applying for her CN3, is certified as a critical care nurse (CCRN) and is co-chair of the unit based healthy work environment committee. Her nominator wrote, “She supports the team in any way possible and always with a positive attitude. She really makes the unit a great place to work and her positivity and “can do” attitude is infectious. She’s currently in school and pursuing an advanced degree in nursing as family care practitioner. This nurse always strives to do the right thing and will hold others to the Duke and unit standards. I have often heard her giving constructive feedback to other nurses to ensure that we are providing the best care to our patients. She coaches in a way that is respectful and considerate, all while being understood clearly. I’ve over heard her helping family members understand the visitation policy and explains it in such a helpful way. She consistently makes sure that our patients’ needs are met, as well as the families’. This nurse makes herself approachable and often you’ll hear other nurses or physician ask her “what do you think?”
Amanda Rooney, RN received the 2023 Nan & Hugh Cullman Heart Center Award for Excellence in Nursing Practice. Her nominator wrote, “Amanda has been the gold standard of integrity. I have observed how she documents accordingly, how she speaks up and stands up for what is right, for implementing policy and protocols. She is consistent with what she says and what she does. Her great organizational skills, result-oriented mindset, proactiveness, promptness to act, and the most beautiful one is her positive attitude which is enormously contagious to the staff. She is the best cheer leader when the day is about to drown. You will know when she is around, aside from her charismatic patient greetings, the unit is in its tidiest and well-supplied state. Not to mention, her candy jar is always full and welcoming.”
Robert Stern, RN received the 2023 Fuchs Family Award for Excellence in Innovation. His nominator wrote, “This nominee is committed to the values of Duke nursing in his day-to-day practice. He is an innovator, who constantly strives to identify new challenges and implement solutions. This nominee is an active member on his home unit as well as an innovator in a multitude of initiatives throughout the hospital. He has a passion for health innovation and patient care. This nurse is certified with CCRN (Critical Care Certification). By achieving and maintain this certification, this nominee demonstrates his dedication to continuous learning and maintaining up-to-date Knowledge. Further this nominee is active in the professional organization American Association of Critical-Care Nurses through his sharing of learning at the organization’s national conference (National Teaching Institute).”
Shelley Thompson, RN received the 2023 Wilma Minniear Award for Excellence in Nursing Mentorship. Her nominator wrote, “She goes above and beyond patient care in ensuring that patients have everything they need prior to being discharged from the hospital. For example, on one occasion, a patient had difficulty with filling pill boxes at home which resulted in multiple hospital admissions. She called multiple pharmacies and found one that could provide blister packs instead, thereby reducing the stress and burden on the patient to ensure they could take all of their correct medications. This nurse is most giving of her time, both physically and emotionally. She contributes her time to volunteering through her home church and is recognized for the work she does in the volunteering space.
This nurse is a proud Duke Nurse who wears her Duke Nursing badge with pride. I recall many times when this nurse took extra time to sit with a patient and their family to share prognosis or explain the clinical situation. One patient, who will remain anonymous, was admitted to the hospital for end of life care. I had the pleasure to admit the patient where he promptly asked me, “How is my cousin ‘this nurse’ doing; can she come see me?” This nurse shared a similar name with this patient and the relationship they built of trust has stood out with me for many years. The patient’s family even voiced appreciation for this nurse as part of the patient’s memorial.”
Did you know? Duke Health is one of only a few (~6) organizations in the U.S. with an endowed program to support nursing? This is just one of the many reasons that Duke is a great place for nurses!
Congratulation to all winners across Duke Health – we are so proud of you and the work you do each day on behalf of our patients and team.
AACN NTI Conference Held
Last week, Duke Heart had a large representation at the American Association of Critical Care Nurses’ National Teaching Institute Conference held from May 22-24 in Philadelphia, PA. The AACN NTI is the largest conference in the United States held specifically for progressive and critical care nurses. We had 17 nurses representing several Duke Heart ICUs, stepdown units, and procedural areas. Our team delivered five podium and five poster presentations, with 13 different presenters.
The team disseminated their work on varying topics, including:
- Behavioral Response Team
- Appropriate Staffing
- Healthy Work Environment
- Onboarding and Orientation
- Leading with Science
- Electronic Debriefing Process
- CLABSI Reduction
- Delirium Prevention
- Patient Satisfaction in the ICU
- Ambulation of CRRT Patients
Several nurses from other healthcare organizations complimented the work ongoing at Duke Heart and even expressed interest in joining our teams! We received kudos on our outcomes related to clinical care, work environments, and interdisciplinary partnerships. Thank you to those who represented us at the conference, and to those who contributed to the work that was presented. Incredible job, all — way to go!



The Latest from Moi Teaching Hospital
Titus Ngeno traveled with Jerry Bloomfield, Chris Beyrer (the new director of Duke’s Global Health Institute), Wendy Omeara, John Lawrence, Cory Miller, Cynthia Binanay, and Gretchen Sanders to Moi Teaching Hospital in Eldoret, Kenya back in January. They held several training sessions on transesophageal echocardiography (TEE) and invasive hemodynamic monitoring. A catheterization lab and cardiac MRI are currently under construction there, and we’re looking forward to hearing more all about it from Andrew Wang, who will be visiting the space this summer! The Moi team now has a cardiac rehab space and they are working to set up CPET as well.



2023 Heart Walk Exec Kick-Off Held
The American Heart Association along with Drs. Rick Shannon and Manesh Patel hosted the Duke Health Executive Kick-off for the 2023 Triangle Heart Walk on Thursday, May 25. The breakfast event allowed the team to discuss the overall goals of the AHA, the need for team coaches and walkers for the fall event, as well as the many ways AHA funding comes back to Duke over time.
Stay tuned for information regarding the team captain and walker kick-off later this summer! Thanks to everyone who has been involved over the years with the American Heart Association and the Triangle Heart Walk.

Annual DOM End of Year Review: June 2
Department of Medicine (DOM) faculty and staff are invited to join Kathleen A. Cooney, MD, Chair, Department of Medicine and the George Barth Geller Distinguished Professor of Medicine, on Friday, June 2 at 8 a.m. for the annual DOM End of Year Review either in-person (Trent Semans Great Hall) or via Zoom. This event will take place during the regular time slot for Medicine Grand Rounds. Coffee/light breakfast will be provided at the Great Hall for those who choose to attend in person.
We look forward to celebrating and recognizing the numerous accomplishments across the department. If you plan to attend in person, please visit https://duke.is/p5p7y to RSVP by Thursday, May 25.
Thanks to all faculty who submitted accomplishments for the division of cardiology. Although it’s too late to be added to the DOM End of Year Review, we are still collecting items specifically for Duke Heart. If you haven’t yet submitted and would like to, send your list to Tracey Koepke.
DHIP Open Enrollment Deadline, May 28
As part of the transition to Duke Health Integrated Practice (DHIP), a special Open Enrollment for Duke Benefits** is currently underway through May 28.
Click here for resources and details – dhip.org/enroll
**Special enrollment does not apply to Duke-leased employees who already have access to Duke benefits. No changes or elections can be made during this time.
Quick Reminders & Updates
June 1-7 is National CPR & AED Awareness Week
The American Heart Association (AHA) is inviting all interested team members from Duke Heart and Duke Health to attend a virtual hands-only CPR awareness event on June 1st from 11 a.m. to Noon. Attendees will hear from a survivor, members of the local chapter of the American Heart Association, and learn about the importance of hands-only CPR and how to perform it.
Cardiac arrest is a leading cause of death throughout the world. Each year, more than 350,000 out-of-hospital cardiac arrests occur in the United States. Almost three out of four of those happen at home.
By attending this session, participants will increase their knowledge and awareness about Hands-Only CPR and learn how to act in the event of an emergency. By the end of the activity, employees will be aware of how and when to use Hands-Only CPR, what to do when calling 9-1-1, and specific ways to take action and get involved with our local AHA affiliate.
Event will be held via Microsoft Teams. June 1, 11 a.m. to Noon. https://duke.is/mr792. If you would like to receive a calendar invitation, please email Tracey Koepke.
New: Back-up Care Service for Duke Health Employees
In addition to a career filled with purpose and opportunity, at Duke Health we ensure that you are supported in both work and in life with a comprehensive benefits package that lets you plan your future. We are excited to add another incredible service to our Total Rewards Program that will give you and your family support during difficult times.
We have entered into a new partnership with Bright Horizons Family Solutions that will provide affordable back-up dependent care for you and your families. A high-level overview of this new service is provided below, and we encourage you to view this video that provides a more comprehensive description of the service.
Services provided:
- 10 annual days of back-up care at discounted rates using Bright Horizons’ network of caregivers who provide temporary care when you have a disruption in your regular care.
- Bright Horizons’ center-based care is $15 per child per day or $25 per family.
- Bright Horizons’ in-home care for both children and adults is priced at $6 per hour.
Please sign up for this service at the following link: https://hr.duke.edu/benefits/family/backup-care.
Once you complete the profile online, you will be able to make reservations as far out as 60 days in advance or as quickly as the same day care is needed.
Please note that all PDC employees joining the Duke Health Integrated Practice will be eligible for this service starting on July 1, 2023.
We are excited to offer this new service to you and your families so that you feel supported by our organization both as leaders in healthcare and leaders of your household.
Upcoming Events & Opportunities
DCRI Research Forum with John Scheyer
The Duke Clinical Research Institute team is excited to have rescheduled their Research Forum with special guest John Scheyer, head coach of the Duke Men’s Basketball program. Please join us on June 6, at 9 a.m. for the Forum, which will feature a fireside chat with Scheyer. This will be a virtual event; Scheyer will discuss his journey and the philosophy that keeps him focused on success — both his personal success and the success of his team. We’ll also address how his philosophy and resilience translates to healthcare and our approach to enhancing human health.
What: DCRI Research Forum: A Conversation with Duke Men’s Basketball Head Coach Jon Scheyer
When: Tuesday, June 6 from 9-10 a.m. ET
Zoom Link: DCRI Research Forum

Cardiac Safety Research Consortium Think Tank Meeting, June 7
The Cardiac Safety Research Consortium will hold a Think Tank meeting on June 7. The event, CSRC Think Tank: Update on Regulatory Status of Hypertension, Biomarkers and Arrhythmia Monitoring in Clinical Trials will be held at the FDA.
In Session 1, these leading industry professionals will speak on panels discussing:
- Regulations for ECG/QT
- The double-negative conundrum
- Alternative methods for assay sensitivity assessment in routine Phase 1 QT Studies
- Covid-19 and prolonged QT
In Session 2, we will discuss:
- Small increases in blood pressure and CV risk I
- Intermittent versus chronic use hypertension drugs
In Session 3, the meeting faculty will dive into:
- Biomarkers
In Session 4, the panelists will discuss hot topics in the field such as:
- Biologics/cardiomyopathy and vaccine development
- MACE
- Gene therapies
- Wearables
The event will include professionals from FDA Regulatory, Cardiac Safety Consultants, Ltd., Eli Lilly, Richmond Pharmacology, University of Connecticut, Stanford University, University of Pennsylvania, Cleveland Clinic, Clario, Mass General, DSI, Penn Medicine, and UCSF.
There is a registration fee for attendance, for academics it is $275. Registration and more information is available here: https://cardiac-safety.org/
The meeting will be held in person; a recording of the meeting and slide presentations will become available a month after the event occurs.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
May issue — William Kraus
Scientific American
You Don’t Really Need 10,000 Daily Steps to Stay Healthy
https://duke.is/yhwhy
May 19 — Robert Mentz and Stephen Greene
HCPLive
Don’t Miss a Beat: ESC Heart Failure Association Preview
https://duke.is/84kr8
May 22 — Robert Mentz
Korea Biomed
Will Entresto’s reimbursement be expanded to heart failure with ejection fraction above 40%?
https://duke.is/2d6ac
(scroll down)
May 22 — Robert Mentz
tctMD
More ARNI Insights Fortify Role in ‘Below Normal’ LVEF: PARAGLIDE-HF
https://duke.is/geseg
May 22 — Adrian Hernandez
The Washington Post
An exercise trial for long covid is being criticized by some patients
https://duke.is/6ydwj
May 22 — Robert Mentz
HCPLive
PARAGLIDE-HF Offers Further Insight into Sacubitril/Valsartan in Heart Failure with Elevated EF
https://duke.is/p9v9p
May 23 — Robert Mentz
DAIC
Sacubitril/Valsartan Shows Benefit in Heart Failure with Ejection Fraction Above 40%
https://duke.is/4fwqr
May 24 — W. Schuyler Jones
mmm-online.com
https://duke.is/5n6m9
May 24 — Jacob Schroder
Medical Stories
Heart Transplant: Strong Hearted
https://duke.is/nv9b6
May 25 — Jonathan Piccini
Medscape
Leadless Dual-Chamber Pacemaker Clears Early Safety, Performance Hurdles
https://duke.is/bp6pb
May 25 — Robert Mentz
Medscape
ARNI Bests ARB to Reduce NT-proBNP in Stabilized Preserved-EF HF
https://duke.is/cxvu4
May 26 — Stephen Greene
HCPLive
The Prospect of SGLT1/2i in Heart Failure: Cardiologists Await FDA Decision on Sotagliflozin
https://duke.is/j5k72
Recent Comments