Duke Heart Pulse – November 27th 2022
Chief’s message:
Thanksgiving is a time where we get to spend time hopefully recharging and in the presence of friends and family contemplating the people and things we are grateful for in our lives. It is also a time of traditions with the familiarity of food, family, and often sporting events. This year I was again able to be a referee in the annual Thanksgiving day Turkey Bowl played between the medicine residents representing the VA Hospital and Duke Hospital (VA Jets vs. Duke Marines). This annual flag football game has been a tradition for nearly 50 years  (Harvey Cohen – pictured helping with the Coin Toss in the Turkey Hat is checking on the actual first game (1973 or 1974). As every year, the goal is the have a good time, avoid all injuries, and identify a winner for bragging rights over the next year. Additionally, the game allows families in town, dogs, kids, and others to come and see our tradition. Over the last 10-15 years the game has gotten much more serious (wrist bands with plays), set plays, positions, and variety of tactics to help conduct a good game. In 2020 it was a softball game and is now back to flag football. Despite the world cup, Duke Basketball, NFL and College games, this is one of the more entertaining and generally close events of the Thanksgiving weekend
(Harvey Cohen – pictured helping with the Coin Toss in the Turkey Hat is checking on the actual first game (1973 or 1974). As every year, the goal is the have a good time, avoid all injuries, and identify a winner for bragging rights over the next year. Additionally, the game allows families in town, dogs, kids, and others to come and see our tradition. Over the last 10-15 years the game has gotten much more serious (wrist bands with plays), set plays, positions, and variety of tactics to help conduct a good game. In 2020 it was a softball game and is now back to flag football. Despite the world cup, Duke Basketball, NFL and College games, this is one of the more entertaining and generally close events of the Thanksgiving weekend  activities. This year it reminded me of the special place we have in Academic Medical Centers – in the ability to interact and train the next generation of leaders, residents, fellows, and junior faculty that quickly become the day to day fabric of Duke. Many of the sideline cheering squads, referees, team coaches (Dr. G) and others have been part of or have influenced generations of residents playing in these games. The last few years of pandemic, consolidation and strains on our health systems have worked to put tremendous stress on our faculty, residents, fellows and staff. These times of interreacting outside the hospital, getting to do things not directly related to our day to day activities serve as important moments for our teams to be together and appreciate each other. Hopefully, we will continue to find venues for these types of activities with each other. Oh, and as to the outcome of the game: 14-14 Tie on a last second Hail Mary touchdown from the VA to end the game as the clock ran out.
activities. This year it reminded me of the special place we have in Academic Medical Centers – in the ability to interact and train the next generation of leaders, residents, fellows, and junior faculty that quickly become the day to day fabric of Duke. Many of the sideline cheering squads, referees, team coaches (Dr. G) and others have been part of or have influenced generations of residents playing in these games. The last few years of pandemic, consolidation and strains on our health systems have worked to put tremendous stress on our faculty, residents, fellows and staff. These times of interreacting outside the hospital, getting to do things not directly related to our day to day activities serve as important moments for our teams to be together and appreciate each other. Hopefully, we will continue to find venues for these types of activities with each other. Oh, and as to the outcome of the game: 14-14 Tie on a last second Hail Mary touchdown from the VA to end the game as the clock ran out.


Importantly, we are also grateful during this time and the upcoming holidays for our staff and faculty/fellows/residents that help care for our patients in the hospital. In this version of the pulse you will some photos below of our staff and others seen around town.
Highlights of the week:
Chet Patel Accepts New Role as Associate Vice Chair, Strategic Physician Relations
 Congratulations to Chet Patel, MD! He will soon serve as associate vice chair for strategic physician relations for the Duke Department of Medicine. The announcement was made on Wednesday, Nov. 23 by Dr. Kathleen Cooney, chair, Department of Medicine. Her statement reads:
Congratulations to Chet Patel, MD! He will soon serve as associate vice chair for strategic physician relations for the Duke Department of Medicine. The announcement was made on Wednesday, Nov. 23 by Dr. Kathleen Cooney, chair, Department of Medicine. Her statement reads:
“Over the past five years, the Department of Medicine has been working coordinately with Duke University Health System and the PDC to extend our clinical practice into Wake County and other strategic areas. This work is very different from our usual clinical operations/quality management and requires strategic thinking as well as close collaboration with internal and external groups. I am pleased to announce that Chet Patel, MD, our current Vice Chair of Clinical Affairs, has accepted a new leadership position within the Department of Medicine as Associate Vice Chair, Strategic Physician Relations.
Dr. Patel’s new responsibilities will include supporting the implementation of the clinical strategic plan for the Department with a focus on internal and external partnerships. He will represent the Department of Medicine in agreements with external entities by coordinating efforts with the DUHS strategic planning office. He will also focus on facilitating communication to physicians about specialty services and procedures provided at DUHS while streamlining those efforts. In this role he will report to the Vice Chair for Clinical Affairs.
Dr. Patel will transition to this new role once a new Vice Chair for Clinical Affairs has been selected. A search to fill the Vice Chair role will begin on Monday, November 21 led by David D’Alessio, MD, chief, Endocrinology, Metabolism, and Nutrition. Candidates interested in the role of Vice Chair for Clinical Affairs are asked to email a brief letter of intent and an updated CV to emelia.dunston@duke.edu by Wednesday, December 21.
View the job description, duties and responsibilities here. Additional position details will also be sent in a subsequent email message for those interested in the role.”
We are excited for you, Chet!
Tong, Zwischenberger Featured in WTS Oracle
Duke Heart’s Betty Tong, MD and Brittany Zwischenberger, MD are featured in the latest issue of Oracle, an annual magazine produced by Women in Thoracic Surgery. The article is about Lise Tchouta, a 4th year General Surgery resident at Columbia University Medical Center and recent recipient of the Brigid Scanlan Traveling Mentorship Award. Tchouta chose to spend four weeks at Duke under the mentorship of Tong and Zwischenberger; the article speaks to the importance of mentorship and increasing the number of women in the field.
It’s a terrific piece in a powerful edition of Oracle. Well worth the read (p. 22)!
Both Allan Kirk, MD and Edward P. Chen, MD chimed in on the piece.
“Congratulations on such a wonderful story,” said Kirk. “Thanks for projecting the progressive side of Duke CT Surgery and helping move us to a better future.”
“Great job Betty and Brittany in attracting future female CT surgeons to Duke, Chen added.”
The importance of mentors can never be overstated. Way to go!
Loring Awarded Pilot Study Grant

Zak Loring, MD has been awarded a Durham VA Health Services Research & Development ADAPT COIN pilot study grant for his proposal Improving Disparities in Atrial Fibrillation Care Through ECG-based Machine Learning Risk Models. This is a 1-year preliminary project award worth $50,000 aimed at enhancing healthcare equity.
We also learned that Loring has passed his boards. Great news all around, Zak! Congratulations!!!
In Gratitude to Our Many Teams!
We hope each of you enjoyed the holiday. Thank you to all of our many team members who cared for patients on our units over the holiday weekend. We hope you’ve had some time to decompress and relax! We’ve had an amazing year of accomplishments. Thank you for all that you do.








Reminder: ORA Holiday Deadlines
The Office of Research Administration (ORA) will operate with a reduced staff during the holiday season to allow team members time to recharge. To help ORA respond as timely as possible to your needs, please plan in advance based on the following:
Picture of the Week
Seen in the Cameron Crazie section of the Duke Basketball game

Last two weeks of December
For any transactions with due dates between December 19 – January 2, please have submitted in ready-form to ORA by Thursday, December 15 to ensure there is adequate time and staffing to respond to your needs.
Please note: the next NIH SBIR/STTR deadline is Jan. 5, 2023, and the internal deadline is 8 a.m. on Dec. 28, 2022. Because this deadline falls in the last two weeks in December when ORA will be operating with reduced staff and because these award mechanisms are usually complex and require careful institutional coordination before submission:
- Please complete Intent to Submit for all planned SBIR/STTR applications no later than Dec. 5, 2022; and
- Please plan to route a submission-ready application no later than Dec. 15, 2022; if more time is needed, please submit a late waiver request so that ORA can plan for appropriate coverage to support these applications.
For anything submitted in the last two weeks of December that can wait until after the holiday break, ORA will be back up to speed with a full team on Jan. 3, 2023 and will look forward to managing all pending issues at that time.
Additional Reminders:
- It is vital that we all remain vigilant with masking, hand hygiene, PPE, and other safe behaviors to prevent the spread of infection. Please pay special attention to the proper wearing and securing of gowns and be mindful of PPE compliance. Thank you for all you do to keep everyone safe and healthy.
Upcoming Events & Opportunities
Cardiology Grand Rounds
November 29: No CGR this week.
CME & Other Events
Call for abstracts: 2023 Duke Health Quality and Safety Conference
The virtual poster submission period for the 2023 Duke Health Quality and Safety Conference is now open. The deadline for submission is Wednesday, Dec. 14. The 2023 Conference will be held the weeks of March 13 and 20, with an in-person event on Thursday, March 23.
For more information and to submit your abstract, please click here.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
November 8 — Pamela Douglas
Cardiovascular Business
VIDEO: PRECISE trial shows cardiac CT with FFR-CT significantly improves patient outcomes
https://duke.is/9mu94
November 9 — Manesh Patel
Everyday Health
Dietary Supplements Don’t Lower ‘Bad’ Cholesterol, Study Finds
https://duke.is/b9nq6
November 9 — W. Schuyler Jones
Medpage Today
Surgery Bests Endovascular Therapy for Most Limb-Threatening Ischemia Patients
https://duke.is/cfvgf
November 10 — Neha Pagidipati
Medscape
Remote Care May Help Curb High Blood Pressure, High Cholesterol
https://duke.is/5cnhr
November 10 — Robert Mentz
Pharmacy Pratice News
No Efficacy Difference Between 2 Common Loop Diuretics
https://duke.is/nyw3x
November 10 — Renato Lopes
Medscape
No Benefit of Rivaroxaban in COVID Outpatients: PREVENT-HD
https://duke.is/r6wzq
November 11 — Jennifer Rymer
tctMD
Cangrelor After Ticagrelor Pretreatment in ACS Might Be OK: SWAP-5
https://duke.is/8buun
November 11 — Kevin Hill (pediatric cardiology)
EMJ
Methylprednisolone in Infants Undergoing Cardiopulmonary Bypass Surgery
https://duke.is/phvjj
November 11 — Kevin Hill
tctMD
STRESS Shows ‘Borderline Results’ for Methylprednisolone in Infant Cardiac Surgery
https://duke.is/gkspc
November 11 — Neha Pagidipati
Patient Care
https://duke.is/65dnu
November 14 — Jennifer Li and Kevin Hill (peds cardiology)
Diagnostic and Interventional Cardiology
Largest Randomized Trial Evaluates Steroids for Infant Heart Surgery
https://duke.is/mvvtt
November 14 — Renato Lopes
Healio/Cardiology Today
Trial does not support routine antithrombotic use in ill outpatients with COVID-19
https://duke.is/7mrd3
November 14 — Manesh Patel
tctMD
Drug Preconditioning Before CABG, Valve Surgery Shows Promise: START
https://duke.is/v3sss
November 15 — Christopher Granger
tctMD
Many STEMI Patients Not Treated Within National Time Goals
https://duke.is/gwwct
November 17– Duke Clinical Research Institute
Practical Cardiology
Almost 1 in 3 High-Risk AFib Patients Not Receiving Anticoagulation
https://duke.is/9augu
November 17 — Jonathan Piccini
Healio/Cardiology Today
Botulinum toxin injection does not prevent postoperative AF: NOVA
https://duke.is/2pk25
November 18 — Jonathan Piccini
Medscape
Neurotoxin to Avert Postoperative AF: Patient Selection Clues in NOVA
https://duke.is/4svy7
November 21 — Josef Turek and the Sinnamon family
KFVS-CBS12 Cape Girardeau (MO)
18-month old medical miracle from world’s first heart-thymus procedure
https://duke.is/p4n3a
November 21 — Manesh Patel
Parallax by Ankur Kalra
EP 80: AHA’s Scientific Sessions: Science, Innovation and Community With Dr Manesh Patel
https://duke.is/6jwkw
November 22 – Stephen Greene
Healio/Cardiology Today
Low household income may predict higher risk for 30-day HF readmission
https://duke.is/5knzk
November 23 — Jonathan Piccini
Medscape
Factor Xa Inhibitors Tied to Interstitial Lung Disease in AF
https://duke.is/rtw5h
Duke Heart Pulse November 20th 2022
Highlights of the week:
Happy Thanksgiving to All!
On behalf of the entire Duke Heart leadership team, we wish you and your loved ones a happy Thanksgiving. During this time of reflection on our many personal blessings, we also give thanks for the incredible team we have here in Duke Heart. Together, we have persevered through some big challenges over the last several years, and also accomplished a great deal. We have a lot to be proud of. Thank you for all that you do — each member of our team makes a difference. Warm wishes to you and we hope you have some time to spend with your family, friends, and loved ones.
CVRC Announces Research Staff Appreciation Awardees
Each year, the Duke Cardiovascular Research Center (CVRC) presents research staff appreciation awards to members of their team who have made an exceptional contribution to their team. Due to the pandemic, the CVRC was unable to formally celebrate as a group last year due to the pandemic, so this year was extra special! We are excited to share with you their awardees for both 2021 and 2022. The CVRC awards were made on Nov. 9.
 The 2021 awardee is Xinhe Yin of the Holley Lab, nominated by Dr. Chris Holley with support from colleague Brittany Elliott, PhD. In their summary, Holley and Elliott shared the following:
The 2021 awardee is Xinhe Yin of the Holley Lab, nominated by Dr. Chris Holley with support from colleague Brittany Elliott, PhD. In their summary, Holley and Elliott shared the following:
“Xinhe is a valuable member of the Holley Lab and CVRC. This is evidenced by her ever-growing knowledge base of technical expertise, the efforts she makes to care about and help the scientific endeavors in the CVRC succeed, and by being a good citizen of the CVRC by going above and beyond to maintain instrumentation within the shared CVRC resource. Xinhe brings multiple areas of expertise to the lab. First, she is an expert in managing our mouse colony, including breeding, genotyping, and tissue collection. Second, she performs a significant amount of cell culture for the laboratory, maintaining a wide variety of human, mouse, and rat cell lines, including many CRISPR-modified clonal lines. Third, she has developed the necessary expertise to prepare samples for our UPLC-MS/MS method that quantifies RNA modifications. Fourth, she has developed expertise with the Seahorse platform, which has allowed her to supervise this instrument for the CVRC. Her technical expertise contributes to every project in the lab!
“Xinhe also serves as our lab manager, taking responsibility for safety protocols, inspections, maintaining lab equipment and supplies, and ensuring that successful transitions as lab members join then eventually leave the lab. She is the primary contact for many collaborations, coordinating animal and material transfers. She serves as an emergency contact for the animal colony and the remote monitoring of our freezers. One of the things that I really respect about Xinhe is that when she sees something that seems wrong, or she doesn’t understand something, she asks about it instead of ignoring it.”
 The 2022 awardee is Longquan Xu of the Rockman Lab, nominated by Dr. Howard Rockman with support from colleague Darion Rapoza, PhD. In their nomination, Rockman and Rapoza shared:
The 2022 awardee is Longquan Xu of the Rockman Lab, nominated by Dr. Howard Rockman with support from colleague Darion Rapoza, PhD. In their nomination, Rockman and Rapoza shared:
“Longquan Xu is a highly skilled small animal cardiac microsurgeon and echocardiographer in the CVRC Cardiovascular Physiology Core. He is by far one of the most conscientious technicians we have ever had the pleasure of working with. His technical expertise is exemplary. He is the go-to person in the CVRC Core for performing cardiac surgeries and the precision analyses of B mode 2D echocardiograms. He is totally dedicated to excellence and precision in performing noninvasive and invasive hemodynamic studies. When there is time available in his schedule, and on his own initiative, he will practice surgeries to hone newly acquired skills or to keep his procedural skills sharp and at the highest level of competency. Moreover, he is willing to learn new techniques and will practice new procedures until he has achieved perfection. He is always eager to be helpful. He is a supportive teacher, flexible, and always cooperative in sharing the workload to keep the core’s performance at its best for the PIs and their research programs. From COVID precautions to barrier facility protocols, he rigorously complies with guidelines and assists other in doing so as well, because, in his words, “It matters.”
Congratulations to Xinhe and Longquan!
To be eligible for a CVRC Research Staff Award, an individual must be employed by the Duke School of Medicine and must meet all of the following criteria:
- Technicians, Lab Research Analysts, Project Leaders, or any staff member who provides exemplary support in the conduct of basic or translational research within the CVRC.
- Current role provides technical expertise to support basic or translational research program(s) in a manner which strengthens the research mission of the CVRC.
- At least 5 years of continuous service in a research role in the CVRC.
- Demonstrated record of excellent performance and good citizenship.
Not Eligible: Faculty or staff members who have primary investigator status, research fellows, research associates and senior research associates, post-doctoral fellows and graduate students, administrative professionals.
Harper Recognized for Years of Service to Duke Heart
 Our long-time colleague, Monica Harper, will be retiring on November 30, 2022 after more than 39 years of service at Duke. Monica has worked in the Heart Center since 1990 in varying roles including staff nurse, assistant head nurse, and — since 2000 — as 7300 Nurse Manager of Operations. Throughout her time with our team she served on many task forces and committees.
Our long-time colleague, Monica Harper, will be retiring on November 30, 2022 after more than 39 years of service at Duke. Monica has worked in the Heart Center since 1990 in varying roles including staff nurse, assistant head nurse, and — since 2000 — as 7300 Nurse Manager of Operations. Throughout her time with our team she served on many task forces and committees.
Monica is known for her calm and humble demeanor, her approachability, fair and consistent practice, and patient and staff advocacy. It came as a surprise to no one when she was named a recipient of the highly esteemed Duke Friends of Nursing Leadership Award.
On behalf of the entire Duke Heart Center Leadership team, we thank Monica for her loyalty and dedication to our patients, the faculty and staff of Duke Heart, and to Duke University Hospital.
She will certainly be missed. Please join us in wishing her well in her retirement!
National Nurse Practitioner Week, Nov. 13-19
In recognition of the Nurse Practitioner profession and the many contributions they make to Duke Health and the health of the nation. Did you know there are more than 355,000 certified NPs in the U.S. caring for patients of all ages? We are deeply grateful for the efforts and contributions these vital Duke Heart team members make each and every day.
As highly skilled team members and healthcare leaders, NPs provide exceptional patient care in virtually all health care specialties and settings. NPs are pivotal in the health care delivery of Duke Heart and Duke Health, serving in critical roles throughout clinical care, education, health administration, leadership, and research.
We hope all of our amazing Duke NPs had a great week!
High Five to Harris-Holloway!
Sandra Harris-Holloway, CCP, LP, Associate Chief, Adult Services Manager for Perfusion Services at Duke University Hospital  received a High Five on Nov. 7.
received a High Five on Nov. 7.
“Sandra has an office close to a patient care area. She noticed a patient who was frequently sitting by the windows outside her office to get sunlight. Sandra partnered with the care team and advocated for administrative approval for the patient to go outside. During a time of restrictions, Sandra advocated for this patient’s mental health and wellbeing by going above and beyond her duties.”
We know this made a big difference for this patient. Way to go, Sandra!
Duke Heart Family Expands by One!
We are excited to share the happy news that Nishant Shah and Nikita Goel welcomed their son, Asher Jayden Shah, on November 17. Mom and baby are doing well, and big sister Amara is excited to have a little brother!
He’s adorable and we can’t wait to meet him in person. Welcome to the Duke Heart family, Asher. Congratulations to the Shah family!

ICYMI: Krasuski Featured Guest on CardioNerds
Rich Krasuski was recently a featured guest on the popular podcast, CardioNerds. A link to episode 242 appears here ACHD: Atrial Septal Defects with Dr. Richard Krasuski.
Nicely done, Rich!

ORA Holiday Deadlines
The Office of Research Administration (ORA) will operate with a reduced staff during the holiday season to allow team members time to recharge. During this period, please plan as far in advance as possible.
To help ORA respond as timely as possible to your needs, please plan in advance based on the following:
Thanksgiving Day and the Friday After
If you need something processed BEFORE the Thanksgiving holiday, please have it submitted in ready-form to ORA by Thursday, November 17. Otherwise, if it can wait, ORA will process the following week (beginning November 28).
Last two weeks of December
For any transactions with due dates between December 19 – January 2, please have submitted in ready-form to ORA by Thursday, December 15 to ensure there is adequate time and staffing to respond to your needs.
Please note: the next NIH SBIR/STTR deadline is Jan. 5, 2023, and the internal deadline is 8 a.m. on Dec. 28, 2022. Because this deadline falls in the last two weeks in December when ORA will be operating with reduced staff and because these award mechanisms are usually complex and require careful institutional coordination before submission:
- Please complete Intent to Submit for all planned SBIR/STTR applications no later than Dec. 5, 2022; and
- Please plan to route a submission-ready application no later than Dec. 15, 2022; if more time is needed, please submit a late waiver request so that ORA can plan for appropriate coverage to support these applications.
For anything submitted in the last two weeks of December that can wait until after the holiday break, ORA will be back up to speed with a full team on Jan. 3, 2023 and will look forward to managing all pending issues at that time.
This has been another year of tremendous growth in research at Duke. The Office of Research Administration thanks you for your continued partnership in support of Duke’s research mission and they send warm holiday wishes to all!
Additional Reminders:
- It is vital that we remain vigilant with masking, hand hygiene, PPE, and other safe behaviors to prevent the spread of infection. Please pay special attention to the proper wearing and securing of gowns and be mindful of PPE compliance. Thank you for all you do to keep everyone safe and healthy.
- November is American Diabetes Month, Pulmonary Hypertension Awareness Month, and National COPD Awareness Month. Thanks for all you do to help patients with these conditions!
- November 13-19 National Nurse Practitioner Week.

Upcoming Events & Opportunities
Cardiology Grand Rounds
November 22: Calcium Modification in Percutaneous Coronary Intervention with Ali Corley. 5 p.m., Webex.
CME & Other Events
Call for abstracts: 2023 Duke Health Quality and Safety Conference
The virtual poster submission period for the 2023 Duke Health Quality and Safety Conference is now open. The deadline for submission is Wednesday, Dec. 14. The 2023 Conference will be held the weeks of March 13 and 20, with an in-person event on Thursday, March 23.
For more information and to submit your abstract, please click here.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News: Our news coverage will return Nov. 27.
Duke Heart Pulse November 13th 2022
Highlights of the week:
Veterans Day Weekend
We hope you’re all enjoying the weekend. With more than 1200 veterans on our extended team throughout DUHS, and so many of our Duke Heart team members caring for veterans at the Durham VAMC, we thank all those who have served in the U.S. military. Whether their service occurred during a time of war or time of peace, and regardless their length of service, we will always be indebted to veterans and their families for all they’ve given to the U.S.
Celebrating Tracy Wang, MD

It’s hard to believe, but Tracy Wang’s last official day with us at Duke was Monday, Nov. 7. As we mentioned in Pulse several weeks ago, Wang is headed to the Patient Centered Outcomes Research Institute (PCORI) to serve as their Chief of Comparative Effectiveness Research.
We had the opportunity to speak with Tracy about her time at Duke, what she has valued most, and what she’s looking forward to with her new position.
“The skills and experience that I’ve acquired over the last 20 years or so at Duke is one of the beauties about being a faculty member at Duke. We have the freedom to pick and choose what kind of questions we want to answer,” Wang said. “I believe it’s one of the most grounding aspects of what we do. Many of us are clinicians in addition to researchers, and we try to answer questions that are really meaningful to clinical care. I’ll very much draw on that as I think about the future of research in my new role. I’ve had so many amazing mentors and role models here and I’ve had the pleasure of working with so many statistical and methodological experts as well. I have a solid grounding in knowing good science, recognizing it, and being able to think about ways in we could affect change within the field. There is so much innovation happening at Duke. The sentiment here is very much about progress — not doing the same thing over and over again. We’re always learning and innovating – we want to know how we can do something better the next time. This spirit of innovation, I think, is really key to any leader within a research field. We’re not trying to do the same thing every day, we’re trying to continuously improve how we think about the conduct of research. These are important aspects of Duke that have shaped both my experience and who I am as a clinician scientist.”
A lot of what PCORI is trying to do, according to Wang, is take a look at therapies that are already approved, and try to figure out which therapies best serve patient needs.
“One of the key missions PCORI has is to stay very patient-focused,” Wang said. “We need to have a finger on the pulse of what patients and patient stakeholders feel are important questions to answer. It’s also about making sure that we’re good stewards of the funding and ensuring that the type of science we fund is impactful and done in as efficient a manner as possible. I’ll also help guide how to think about investing in research, so that strategically we make the best use of the resources we have.”
Wang says her time at Duke has prepared her well for the role at PCORI.
“Duke is one of the most collaborative and creative leaders within clinical research,” she added. “It’s our spirit of collaboration and innovation that sets us apart from many other research entities out there. And, I think, we broadly recognize that even though there’s a lot of excellence within our group at Duke, we can always learn from others. We know that when we work with others, we are in a much better position to get the job done and to shape the future of medicine. This is definitely one of the strengths of being at Duke and one of the grounding characteristics of our faculty here. This is the type of spirit that I would like to hopefully extend to other groups out there through “the sauce,” if you will, that PCORI provides in trying to get all the players in the field to be able to collaborate and form partnerships more effectively so that we can be more innovative about our methods.
“What I’m looking forward to at PCORI is having the ability to really scale out this process on a more national and international scale. So rather than thinking about individual projects, I’ll be thinking about a whole portfolio of comparative effectiveness research that we can and should be doing.
“As much as I love what I do at Duke, this is what really attracted me to PCORI. I’ll have an opportunity to really have some influence on clinical research – from the type of research being done, to how it can be done, to how we can disseminate the results more effectively. How do we go back to our roots – to what patients need and want? Being able to work on these questions on a much more national scale is what really appealed to me.”
Wang received the 2022 Outstanding Lifetime Achievement Award from the American Heart Association’s Council on Quality of Care and Outcomes Research (QCOR) last May. The award was presented to her during the QCOR Scientific Sessions held in Reston, VA. A tribute video was created specifically for her QCOR award and it’s worth checking out if you didn’t get a chance to see it back in May. A link to it can be found here.
While a lifetime achievement award from QCOR is an incredible honor, Wang says she considers her greatest achievement to be the success of her mentees.
“I am most proud of the talent that I’ve hopefully coached along. One of the things I’m really going to miss about Duke is the really incredible folks here that are in various phases of their career, especially those who are at earlier stages. I really enjoy working with these amazing young minds! To be able to stop and think about what they’re interested in and help them work towards something that is satisfying for them, to help them grow skills that will be helpful to them as time goes on, and then watching them far surpass me in terms of where they’ve gone and what they’ve done. I’ve mentored almost 40 individuals since I started on faculty in 2008. it’s kind of nice to be able to work alongside some of the people I’ve helped train and have them ‘show me up’ on a daily basis. It makes me extraordinarily happy when they do that! It’s also nice to see mentees that have left Duke and gone on to flourish at other places. Bar none, that’s the achievement I am most proud of.
Over the course of her many years at Duke, a large number of people have had the opportunity to work with and learn from Tracy. We reached out to several of them for thoughts on her and her lasting legacy. Here is what they had to say:
“Tracy is an amazing cardiologist, investigator, colleague, and person. She has tremendous insight into tough clinical research issues and usually finds the simplest and most effective solutions. She is always willing to help colleagues without seeking credit. A fantastic mentor to many, I will truly miss her no-nonsense good humor, humility and zest. Tracy is a treasure so I hope she remains part of our Duke family while surely being hugely successful in shaping the nation’s outcomes research agenda at PCORI.” — Pamela S. Douglas, MD
“It is impossible to outline all the ways that Tracy has mentored me through the years. She met with me as an intern, and I began working with her at that time. She has given me so many opportunities, from learning how to work with industry to running analyses and projects independently. Her advice through the years has been invaluable. She was instrumental in helping me transition from a fellow to a faculty member. Tracy has mentored countless fellows and early career faculty at both Duke and more widespread through her significant work with the AHA. Her impact on health outcomes research at the DCRI is widespread and is one of the most talented people I have ever worked with in her ability to formulate scientific questions and develop the appropriate methodology to answer those questions. She has successfully mentored me through two career development awards and many other successful grant applications. She quickly turned from a mentor to a close friend. I will miss her so much, but can’t wait to see what she will accomplish through her work at PCORI.” — Jenn Rymer, MD
“Tracy is a great clinician, researcher and teacher that we rarely see. While many could have focused on themselves, Tracy wasn’t in that mold. She constantly had a string of mentees advancing their careers in a “pay it forward” manner. Beyond that she is a great friend to many. Just as she has had an impact on Duke and DCRI, it will be great to see how she has an impact on PCORI and the nation’s portfolio of comparative effectiveness research. We certainly need better answers and all of us will benefit from her leadership there shaping the questions and delivering clear answers with high-quality research.” — Adrian Hernandez, MD
Shown here are photos from a farewell celebration for Tracy that was held on the patio at Tobacco Road Sports Cafe in Durham on Oct. 6.
She summed up her feelings about leaving with a Chinese saying:
長江後浪推前浪,世上新人隨舊人
Chang jiang hou lang tui qian lang shi shang xin ren suay jiu ren
“Translated, this means ‘Just as the waves of the Yangtze River behind drive on those ahead, so does each new generation replace the old one,’” she added. “While leaving is bittersweet for me and many others, I remain optimistic and excited about the future of Duke as the next generation at Duke has so much talent and potential.”
You will be missed here at Duke, Tracy! We are extremely proud of you and happy that you’re not going far — you’ll always be a part of the Duke Heart family.


Scientific Sessions Wrap-Up
The 2022 American Heart Association Scientific Sessions concluded earlier this past week, yet our celebration of the great work you’ve done continues:
AHA.22 LBCT: Chest Pain Patients Benefit from Precision Diagnostic Testing Approach
A study comparing two approaches for diagnosing heart disease found that a risk analysis strategy is superior to the usual approach of immediately performing functional tests or catheterization for low- to intermediate-risk patients with new-onset chest pain.
Presented Nov. 6 at the American Heart Association’s 2022 Scientific Sessions, the study bolsters a risk-analysis strategy that either defers testing among low-risk patients, or uses coronary computed tomography angiography (CTA), a CT scan with a contrast agent to assess for blockages.
The risk analysis approach has been outlined in guidelines and is championed as a means of reducing often unnecessary and costly tests. It has never been tested rigorously in a randomized trial, however, and its clinical application has lagged without definitive evidence of its effectiveness compared to various functional stress tests.
“New onset chest pain is a common clinical problem that involves a lot of testing, work and expense,” said study lead Pamela S. Douglas, MD, the Ursula Geller Professor of Research in Cardiovascular Diseases at Duke University School of Medicine and a member of the Duke Clinical Research Institute.
“Our study provides evidence that, among low-risk patients, the tests will likely be negative for coronary artery disease and patients will go on to do well,” Douglas said. “As a result, we should be deferring testing in these low-risk people.”
Douglas and colleagues enrolled more than 2,100 patients across the U.S. and Europe with new-onset chest pain in the PRECISE clinical trial. Participants’ average age was 58, with roughly equal numbers of men and women.
Half of the patients were randomly assigned to receive usual testing — including stress echocardiogram, nuclear stress test, stress MRI or catheterization — which physicians selected at their discretion.
The other half of participants were randomized to the precision strategy, which uses a pre-test probability assessment to guide next steps, including deferred testing or CTA, with selective use of image analysis software to determine the significance of any blockages.
Within both groups, about 21% of symptomatic patients were assessed to be at low risk of heart disease. Of these low-risk patients in the usual testing group, 86% underwent some sort of test, compared to 37% in the precision strategy group.
The primary focus was whether, within a year, there were any differences between the two diagnostic approaches for any combination of the following outcomes: deaths from any cause, nonfatal myocardial infarction, or catheterizations that did not show blockages and may have been unnecessary.
The researchers found that the precision strategy substantially reduced the incidence of the composite endpoint compared to the usual stress testing approaches.
To provide a full picture of clinical value, the investigators balanced this demonstrated effectiveness with examination of any safety concerns. There were no differences in death or the composite of death and myocardial infarction, but there was a small, non-significant difference in nonfatal myocardial infarction in the precision group.
“In stable, symptomatic patients with suspected heart disease who physicians feel require testing, a precision strategy incorporating a set of actions based on guideline recommendations, will improve outcomes compared to usual testing,” Douglas said.
In addition to Douglas, study authors include Michael G. Nanna, Michelle D. Kelsey, Eric Yow, Daniel B. Mark, Manesh R. Patel, Campbell Rogers, James E. Udelson, Christopher B. Fordyce, Nick Curzen, Gianluca Pontone, Pál Maurovich-Horvat, Bernard De Bruyne, John P. Greenwood, Victor Marinescu, Jonathon Leipsic, Gregg W. Stone, Ori Ben-Yehuda, Colin Berry, Shea E. Hogan, Bjorn Redfors, Ziad A. Ali, Robert A. Byrne, Christopher M. Kramer, Robert W. Yeh, Beth Martinez, Sarah Mullen, Whitney Huey, Kevin J. Anstrom, Hussein R. Al-Khalidi, and Sreekanth Vemulapalli, for the PRECISE Investigators.
The study received funding from HeartFlow, a medical technology company.
AHA.22: Additional Presenters and Session Moderators
Jonathan Piccini presented results from the phase-2, dose-ranging NOVA study. The team found no significant differences in the rate of postoperative atrial fibrillation (POAF) in cardiac surgery patients who received either 125U or 250U doses of botulinum toxin type A (AGN-151607) compared with placebo. Piccini noted that subgroup analyses suggested a lower rate of POAF and rehospitalization in patients undergoing isolated CABG and in patients older than 65 years who received 125U of AGN-151607. He added that the mechanism of AFib suppression with botulinum toxin may be related to both direct autonomic influences and decreased inflammation.
 Cardiovascular surgeon Brittany Zwischenberger presented several sets of findings across Sessions including “Keep the Guidelines for Radial Artery Grafts in CABG Surgery” during the Consensus and Controversies: Debating the 2021 ACC/AHA/SCAI Guidelines for Coronary Revascularization session held Saturday, Nov. 5, and “Highlights and Controversies from 2021 Guidelines on Coronary Artery Revascularization” during the Update on 2022 Cardiovascular Clinical Guidelines session held on Monday, Nov. 7. Zwischenberger also served as session moderator for New Insights – Cardiac Surgery held Sunday, Nov. 6.
Cardiovascular surgeon Brittany Zwischenberger presented several sets of findings across Sessions including “Keep the Guidelines for Radial Artery Grafts in CABG Surgery” during the Consensus and Controversies: Debating the 2021 ACC/AHA/SCAI Guidelines for Coronary Revascularization session held Saturday, Nov. 5, and “Highlights and Controversies from 2021 Guidelines on Coronary Artery Revascularization” during the Update on 2022 Cardiovascular Clinical Guidelines session held on Monday, Nov. 7. Zwischenberger also served as session moderator for New Insights – Cardiac Surgery held Sunday, Nov. 6.
New Duke Heart faculty member Senthil Selvaraj is senior author on findings presented on Monday at AHA. His team’s study was simultaneously published in JACC: Basic to Translational Science. Their paper is “Metabolomic Signatures of Myocardial Glucose Uptake on Fluorine-18 Fluorodeoxyglucose Positron Emission Tomography.” Co-authors include Svati H. Shah, Mahesh K. Vidula, Daniel P. Kelly, Zoltan Arany, Kenneth B. Margulies, Thomas P. Cappola, and Paco E. Bravo.
Finally, Manesh Patel and Kelly Arps were the featured guests in a Twitter Spaces held Tuesday, Nov. 8 on Twitter. Patel and Arps did a recap of some of the most notable findings presented at Scientific Sessions. The event was recorded, but a link has not yet been made available. Once it is, we’ll post it here in Pulse.
Our team received a great deal of news coverage this year. Please visit the News section below to check it out. We truly had an outstanding presence at Sessions this year. We look forward to 2023!
Mark Serves as Guest Lecturer for AKUPI-NCD
Dan Mark, MD, was invited to discuss landmark studies in cardiovascular disease at a research certification course held recently as part of the Aga Khan University Pakistan Initiative for Non-Communicable Diseases (AKUPI-NCD) Research Training Program. The course audience consisted of aspiring and early career researchers from across Pakistan.
AKUPI-NCD was created to address a critical gap in the response to the NCD epidemic. The Aga Khan University partnered with Duke University to design a comprehensive, integrated, multi-disciplinary training program to prepare the next generation of leaders in NCD research. The program, focused on cardiovascular and cerebrovascular diseases and their shared risk factors, is funded by a research training grant by the U.S. National Institutes of Health via the Fogarty International Center.
Great work!

Huber Presents CGR
We welcomed Kurt Huber for Cardiology Grand Rounds on Tuesday evening, Nov. 8. His talk was entitled, “The Paradigm Shift of DAPT after ACS.” Huber is vice-dean of research at Sigmund Freud University for Medicine in Vienna, Austria, and chair of acute and interventional cardiology at the Wilhelminenspital.
Thanks to all who joined us!


Future Relocation of DN 7100 for Renovations
The Duke North 100 Tower is in the process of being renovated. Eventually, Duke University Hospital unit 7100 will be relocated to allow for renovations which will occur sometime after the start of the year. Once we receive additional information as to the timeline and where 7100 is relocating, updates will be provided.
Shout-out to 7W & 3300!
Our teams on 7W and 3300 received a kudos at DUH on Nov. 8 for achieving 100% compliance for hand hygiene and PPE use. Way to go!
Thanksgiving Edition of Pulse
In this season of gratitude, who or what within Duke Heart (or beyond) are you particularly grateful for this year? We are offering a way to acknowledge those who’ve been a big support or help to you over the past year. Send your shout-outs and kudos to Tracey Koepke by Tuesday, November 22 and we’ll include them in our Thanksgiving issue of Pulse on Sunday, Nov. 27. We look forward to shout-outs and gratitude galore!
Additionally, as we move into the holiday season, please let us know if your team or unit within Duke Heart will be doing anything special to celebrate — perhaps you’ll be adopting a family in need? Hosting a food drive? If you’d like others to join your effort, or if you would just like to showcase what you’ll be doing (or what you did) in Pulse, let us know! We’ll issue the newsletter through December 18th, then we’ll be taking our annual break for two weeks. Pulse will resume on Sunday, Jan. 8, 2023. As always, email your items to tracey.koepke@duke.edu.
Webex User Accounts Decommission Notice
Duke Health is decommissioning Webex User Accounts effective Wednesday, Feb. 1, 2023, and will shift to Zoom for conferencing and collaboration needs. This decision was based on a significant decline in Webex usage and will allow for consolidation of technology support. Current Webex users can use this three-month window to explore Zoom, which offers a user-friendly experience for conferencing needs.
Webex user accounts will be decommissioned and Webex Recordings will no longer be available. Duke Health recommends downloading Webex recordings prior to Feb 1. 2023.
While Webex will remain available until February, Webex users are encouraged to start using Zoom as soon as possible to ensure a smooth transition. Duke Health will still have the ability to join a Webex Meeting as a “GUEST”.
Note: Cisco Webex Rooms/Devices will NOT be impacted. Cisco Webex Rooms/Devices will remain registered to the Cisco Webex Control Hub (Cloud)
If you have questions or concerns, visit the IT Portal and click on Create a New Request in the Popular Items section to open a request, or contact the Duke Health Service Desk at 919-684-2243.
Duke Angel Network is now Duke Capital Partners
On Wednesday, Nov. 9, Duke Angel Network rolled out a new name and website.
Duke Capital Partners is the early-stage venture investing arm of Duke University, helping to connect Duke alumni investors with Duke-affiliated early-stage companies. Duke Capital Partners provides capital and expertise to help Duke start-ups, and features one of Duke’s most innovative experiential learning opportunities for students. As one of the largest and oldest university investment entities of its kind, Duke Capital Partners consistently places among the top five in North America.
It is hoped that faculty, students, and alumni will find Duke Capital Partners to be an exciting new way to engage with the university and its entrepreneurial community.
Link for Real Talk with Craig Albanese
If you missed last week’s Real Talk with Craig Albanese, MD, MBA, Executive Vice President and Chief Operating Officer of Duke University Health System, please click here to learn more about how the expertise and dedication of our financial care counselors have allowed DUHS to provide more than $141 million in direct financial assistance to patients every year. The incredible work this team does every day makes a huge difference to our patients and their families.
CulturePulse 2022 — Be Heard
The Culture Pulse survey link will remain open through Nov. 16; CulturePulse is a way for team members to share their feedback about what’s going well and what could be improved at Duke Health. Please participate and encourage your team members to do so as well. You will receive automatic reminders about the survey until you complete it or it closes. This is a great opportunity for all of us to have our voices heard.
This Week: Matters of Grief Symposium 2022
The Duke Health Office of Culture and Well-being is offering a Grief Symposium 2022 on Tues., Nov. 15 and a panel discussion on Wed., Nov. 16. Please consider joining for one or more events (most are virtual) in which they and participants will explore the many aspects of grief, including common grief reactions, how to support those who are grieving, professional grief, grief around loss of function or role, disenfranchised grief, rituals that may help us in the grieving process, and how to turn grief into positive action. Register here (please use your Duke e-mail to complete your registration).
- Grief Symposium: Tues., Nov. 15, noon-2 p.m.
- Grief Panel Discussion: Wed., Nov. 16, 1-2 p.m.
- Small Group Interactive Activities including Somatic Body Work, Narrative Writing, Mandala Art, and Restorative Circles for Personal Grief, Pet Grief, and Gun Violence: Wed-Fri, Nov. 16-18.
To learn more, please visit: https://cultureandwellbeing.dukehealth.org/grief-toolkit-symposium. A link to last year’s symposium is available on that page.
Reminder! ORA Holiday Deadlines
The Office of Research Administration (ORA) will operate with reduced staff during the holiday season. Please plan in advance based on the following:
Thanksgiving Day and the Friday After
If you need something processed BEFORE the Thanksgiving holiday, please have it submitted in ready-form to ORA by Thursday, November 17. Otherwise, if it can wait, ORA will process the following week (beginning November 28).
Last two weeks of December
For any transactions with due dates between December 19 – January 2, please have submitted in ready-form to ORA by Thursday, December 15 to ensure there is adequate time and staffing to respond to your needs.
Please note: the next NIH SBIR/STTR deadline is Jan. 5, 2023, and the internal deadline is 8 a.m. on Dec. 28, 2022. Because this deadline falls in the last two weeks in December when ORA will be operating with reduced staff and because these award mechanisms are usually complex and require careful institutional coordination before submission:
- Please complete Intent to Submit for all planned SBIR/STTR applications no later than Dec. 5, 2022; and
- Please plan to route a submission-ready application no later than Dec. 15, 2022; if more time is needed, please submit a late waiver request so that ORA can plan for appropriate coverage to support these applications.
ORA will be back up to speed with a full team on Jan. 3, 2023 and will look forward to managing all pending issues at that time.
Additional Reminders:
- It is vital that we remain vigilant with masking, hand hygiene, PPE, and other safe behaviors to prevent the spread of infection. Please pay special attention to the proper wearing and securing of gowns and be mindful of PPE compliance. Thank you for all you do to keep everyone safe and healthy.
- November is American Diabetes Month, Pulmonary Hypertension Awareness Month, and National COPD Awareness Month. Thanks for all you do to help patients with these conditions!
- The deadline for staff flu vaccinations is Tuesday, Nov. 15 at 10 a.m. Vaccination sites for faculty and staff can be found here: https://flu.duke.edu/vaccination/employees/
Upcoming Events & Opportunities
Cardiology Grand Rounds
November 15: AHA Recap with Manesh Patel, L. Kristin Newby, Robert Mentz and Pamela Douglas. 5 p.m., Webex only. https://duke.is/pqv6g.
November 22: Fellow presentation with Ali Corley. 5 p.m., Webex. Watch your email for the link.
CME & Other Events
November 14: Prostate Cancer & CVD Symposium, Webinar 4. Final of a four-part webinar series. Collaboration between the International Cardio-Oncology Society & Duke Heart. Noon, Eastern. Free. To register visit https://duke.is/ptjbs.
Call for abstracts: 2023 Duke Health Quality and Safety Conference
The virtual poster submission period for the 2023 Duke Health Quality and Safety Conference is now open. The deadline for submission is Wednesday, Dec. 14. The 2023 Conference will be held the weeks of March 13 and 20, with an in-person event on Thursday, March 23.
For more information and to submit your abstract, please click here.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
November 5 — Betty Tong
WNCN CBS-17
Health experts urge screening for lung cancer for early detection
https://duke.is/5dz6a
November 5 — Robert Mentz
Medpage Today
Furosemide Holds Up to Newer, Stronger Loop Diuretic During HF Hospitalization
https://duke.is/n3qy8
*also carried by 3 additional outlets
November 5 — Robert Mentz
tctMD
TRANSFORM-HF: Torsemide No Better Than Furosemide for Hospitalized HF
https://duke.is/pmzgz
*also carried by 11 additional industry & scientific outlets
November 5 — Robert Mentz and Manesh Patel
Healio/Cardiology
Loop diuretic choice does not reduce all-cause death in HF: TRANSFORM-HF
https://duke.is/9zbfd
*also carried by Newsbreezer
November 5 — Robert Mentz
Medscape
No Survival Advantage for Either Torsemide or Furosemide in HF: TRANSFORM-HF
https://duke.is/24psp
*also carried by 4 additional industry & scientific outlets
November 5 — Manesh Patel
tctMD
Pemafibrate Fails to Lower CVD Risk in Patients With High Triglycerides: PROMINENT
https://duke.is/z5fg9
November 5 — Robert Mentz
Archynetys.com
Furosemide tolerates new, a lot more potent loop diuretics in hospitalized heart failure
https://duke.is/gvfdh
November 5 — Robert Mentz
ACC.org
Torsemide Comparison With Furosemide for Management of Heart Failure – TRANSFORM-HF
https://duke.is/vecc9
November 6 — Robert Mentz
News-Medical.net
Two heart failure therapies prove to be nearly identical in reducing death
https://duke.is/m9q9m
*also carried by 2 additional industry & scientific outlets
November 6 — Robert Mentz
Pharmacy Times
Trial Finds No Benefit with Torsemide Versus Furosemide in Heart Failure
https://duke.is/4we3g
November 6 — Kevin Hill
Medpage Today
Definitive Answer on Steroids for Infant Heart Surgery Falls Short
https://duke.is/w2pny
*also carried by 4 additional outlets
November 6 — Kevin Hill
Healio/Cardiology Today
Methylprednisolone does not reduce odds of poor outcomes in infant heart surgery
https://duke.is/6tpe6
November 6 — Kevin Hill
AHA Newsroom
Steroids during surgery may not be helpful for infants having heart bypass
https://duke.is/puftb
November 6 — Pamela Douglas
tctMD
PRECISE CT-Based Strategy Allows Clinicians to ‘Do Less’ for Stable Chest Pain
https://duke.is/5ye8w
November 6 — Pamela Douglas
Healio/Cardiology
Precision testing strategy strongly benefits stable patients with suspected CAD
https://duke.is/nschn
*also carried by Knowledgia News
November 6 — Pamela Douglas
Postsus (Spain)
Los pacientes con dolor torácico se benefician del enfoque de pruebas diagnósticas de precisión
https://duke.is/baes8
*also carried by 9 additional industry & scientific outlets
November 6 — Pamela Douglas
HeartFlow
https://duke.is/4cq2c
*also carried by 38 additional industry & scientific outlets
November 6 — Pamela Douglas
News-Medical.net
New risk analysis strategy benefits chest pain patients compared to the usual testing approach
https://duke.is/9vzcg
November 6 — Pamela Douglas
AHA Newsroom
Personalized evaluation for chest pain effective, may eliminate unnecessary testing
https://duke.is/j3zkj
*also carried by 7 additional industry & scientific outlets
November 6 — Pamela Douglas
CRTOnline.org
https://duke.is/gm23p
November 6 — Manesh Patel
Healio/Cardiology
VIDEO: Takeaways from AHA 2022 with Manesh R. Patel
https://duke.is/bcc6t
November 6 — Pamela Douglas
Applied Radiology
Risk-Analysis Strategy Best Approach for New-Onset Chest Pain Patients
https://duke.is/ygzbu
November 7 — Stephen Greene
Biospace.com
Cytokinetics Presents New Data at the American Heart Association Scientific Sessions 2022
https://duke.is/vwpyr
*also carried by 4 additional industry & scientific outlets
November 7 — Pamela Douglas
Cardiovascular Business
AI-powered CCTA outperforms usual care when evaluating stable chest pain
https://duke.is/rbcv4
*also carried by Roxx Cloud
November 7 — Stephen Greene
AJMC
Dr Stephen J. Greene: New VICTORIA Trial Data Show Benefit to Vericiguat In-Hospital Initiation
https://duke.is/n67n5
November 7 — Robert Mentz
Medical Dialogues
Torsemide Does Not Confer Any Survival Benefit Over Furosemide in HF: TRANSFORM HF Trial
https://duke.is/zxe4e
November 7 — Jonathan Piccini
tctMD
Botulinum Toxin Injections No Help for Postoperative AF: NOVA
https://duke.is/chpzs
November 7 — Manesh Patel
U.S. News & World Report
Experimental Pill May Be New Way to Control Cholesterol
https://duke.is/wdf73
*also carried by 249 additional outlets including by HealthDay, United Press International and in Chicago, Houston & Philadelphia
November 7 — Vishal Rao
tctMD
New Tool Assesses Risk in Acute HF Then Suggests Next Steps, Cutting Later Events
https://duke.is/jbq87
November 7 — Duke University (PRECISE study)
Spectrum News Carolinas
Strategy for diagnostic testing benefits chest pain patients
https://duke.is/rkexa
(*clip begins @ 11:00:25)
November 7 — Kevin Hill
Medscape
Steroids Fail to Deliver Clear Benefits in Infant Heart Surgery
https://duke.is/5qbuq
November 7 — Pamela Douglas
MDedge
Precision CAD testing shows 70% cut in composite risk at 1 year
https://duke.is/vm6jx
November 8 — Robert Mentz
UPI
Switching diuretics may not make a difference in treating heart failure
https://duke.is/z6sc6
November 8 — Robert Mentz
U.S.News & World Report
Study Compares 2 Common Diuretics Used in Heart Failure
https://duke.is/8duxp
November 8 — Pamela Douglas
Medpage Today
Precision Medicine Strategy Reduced Testing in Patients With Chest Pain
https://duke.is/cc68r
November 8 — Renato Lopes
Medpage Today
Anticoagulation Again Flops for Outpatient COVID-19
https://duke.is/6kdnc
November 9 — Jonathan Piccini
Medpage Today
Can Botox for the Heart Ward Off Afib After Cardiac Surgery?
November 11 — Vishal Rao
Healio/Cardiology
In-hospital peer-to-peer consult may improve guideline-directed therapy in HFrEF
Division of Cardiology Publications Indexed in PubMed October 27 – November 9, 2022
Adamson C, Kondo T, Jhund PS, de Boer RA, Cabrera Honorio JW, Claggett B, Desai AS, Alcocer Gamba MA, Al Habeeb W, Hernandez AF, Inzucchi SE, Kosiborod MN, Lam CSP, Langkilde AM, Lindholm D, Bachus E, Litwin SE, Martinez F, Petersson M, Shah SJ, Vaduganathan M, Nguyen Vinh P, Wilderäng U, Solomon SD, McMurray JJV. Dapagliflozin for heart failure according to body mass index: the DELIVER trial. Eur Heart J 2022 Nov 1;43(41):4406-4417. PM: 36029309.
Batra G, Lindbäck J, Becker RC, Harrington RA, Held C, James SK, Kempf T, Lopes RD, Mahaffey KW, Steg PG, Storey RF, Swahn E, Wollert KC, Siegbahn A, Wallentin L. Biomarker-Based Prediction of Recurrent Ischemic Events in Patients With Acute Coronary Syndromes. J Am Coll Cardiol 2022 Nov 1;80(18):1735- 1747. PM: 36302586.
Blumenthal JA, Smith PJ, Jiang W, Hinderliter A, Watkins LL, Hoffman BM, Kraus WE, Mabe S, Liao L, Davidson J, Sherwood A. Exercise and Escitalopram in the Treatment of Anxiety in Patients with Coronary Heart Disease: One Year Follow- Up of the UNWIND Randomized Clinical Trial. J Cardiovasc Dev Dis 2022 Sep 22;9(10):320. PM: 36286272.
Butler J, Anker SD, Lund LH, Coats AJS, Filippatos G, Siddiqi TJ, Friede T, Fabien V, Kosiborod M, Metra M, Piña IL, Pinto F, Rossignol P, van der Meer P, Bahit C, Belohlavek J, Böhm M, Brugts JJ, Cleland JGF, Ezekowitz J, Bayes-Genis A, Gotsman I, Goudev A, Khintibidze I, Lindenfeld J, Mentz RJ, Merkely B, Montes EC, Mullens W, Nicolau JC, Parkhomenko A, Ponikowski P, Seferovic PM, Senni M, Shlyakhto E, Cohen-Solal A, Szecsödy P, Jensen K, Dorigotti F, Weir MR, Pitt B. Patiromer for the management of hyperkalemia in heart failure with reduced ejection fraction: the DIAMOND trial. Eur Heart J 2022 Nov 1;43(41):4362-4373. PM: 35900838.
Butt JH, Kondo T, Jhund PS, Comin-Colet J, de Boer RA, Desai AS, Hernandez AF, Inzucchi SE, Janssens SP, Kosiborod MN, Lam CSP, Langkilde AM, Lindholm D, Martinez F, Petersson M, Shah SJ, Thierer J, Vaduganathan M, Verma S, Wilderäng U, Claggett BC, Solomon SD, McMurray JJV. Atrial Fibrillation and Dapagliflozin Efficacy in Patients With Preserved or Mildly Reduced Ejection Fraction. J Am Coll Cardiol 2022 Nov 1;80(18):1705- 1717. PM: 36041668.
Campbell MM, Benjamin DK, Mann TK, Fist A, Blakemore A, Diaz KS, Kim H, Edwards LJ, Rak Z, Brookhart MA, Moore Z, Tilson EC, Kalu I, Boutzoukas AE, Moorthy GS, Uthappa D, Scott Z, Weber DJ, Shane AL, Bryant KA, Zimmerman KO. Test-to-Stay After SARS-CoV-2 Exposure: A Mitigation Strategy for Optionally Masked K-12 Schools. Pediatrics 2022 Nov 1;150(5):e2022058200. PM: 35971240.
Diamond J, DeVore AD. New Strategies to Prevent Rehospitalizations for Heart Failure. Curr Treat Options Cardiovasc Med 2022;24(12):199-212. PM: 36164396.
Dunbar TK, Olsen MK, Yang H, Kennedy D, Jackson LR, Thomas KL, Alkon A, Prose NS, Pollak KI. Characteristics Associated with Burnout among Cardiologists in an Academic Medical Setting: Baseline Survey Results from a Communication Coaching RCT. Behav Sci (Basel) 2022 Sep 27;12(10):362. PM: 36285931.
Fitch KV, McCallum SA, Erlandson KM, Overton ET, Zanni MV, Fichtenbaum C, Aberg JA, Fulda ES, Kileel EM, Moran LE, Bloomfield GS, Novak RM, Pérez-Frontera S, Abrams-Downey A, Pierone G, Kumarasamy N, Ruxrungtham K, Mngqibisa R, Douglas PS, Ribaudo HJ, Grinspoon SK. Diet in a global cohort of adults with HIV at low-to- moderate traditional cardiovascular disease risk. AIDS 2022 Nov 15;36(14):1997-2003. PM: 35876637.
Freedman NJ. From Colon to Aortic Aneurysm: Trek of the Treg. JACC Basic Transl Sci 2022 Sep 26;7(9):948- 950. PM: 36317127.
Fudim M, Shahid I, Emani S, Klein L, Dupuy- McCauley KL, Zieroth S, Mentz RJ. Evaluation and Treatment of Central Sleep Apnea in Patients with Heart Failure. Curr Probl Cardiol 2022 Dec;47(12):101364. PM: 35995244.
Gargiulo G, Giacoppo D, Jolly SS, Cairns J, Le May M, Bernat I, Romagnoli E, Rao SV, van Leeuwen MAH, Mehta SR, Bertrand OF, Wells GA, Meijers TA, Siontis GCM, Esposito G, Windecker S, Jüni P, Valgimigli M. Effects on Mortality and Major Bleeding of Radial Versus Femoral Artery Access for Coronary Angiography or Percutaneous Coronary Intervention: Meta-Analysis of Individual Patient Data From 7 Multicenter Randomized Clinical Trials. Circulation 2022 Nov;146(18):1329-1343. PM: 36036610.
Metkus TS, Baird-Zars VM, Alfonso CE, Alviar CL, Barnett CF, Barsness GW, Berg DD, Bertic M, Bohula EA, Burke J, Burstein B, Chaudhry SP, Cooper HA, Daniels LB, Fordyce CB, Ghafghazi S, Goldfarb M, Katz JN, Keeley EC, Keller NM, Kenigsberg B, Kontos MC, Kwon Y, Lawler PR, Leibner E, Liu S, Menon V, Miller PE, Newby LK, O’Brien CG, Papolos AI, Pierce MJ, Prasad R, Pisani B, Potter BJ, Roswell RO, Sinha SS, Shah KS, Smith TD, Snell RJ, So D, Solomon MA, Ternus BW, Teuteberg JJ, van Diepen S, Zakaria S, Morrow DA. Critical Care Cardiology Trials Network (CCCTN): a cohort profile. Eur Heart J Qual Care Clin Outcomes 2022 Oct 26;8(7):703-708. PM: 36029517.
Minhas AMK, Jain V, Maqsood MH, Pandey A, Khan SS, Fudim M, Fonarow GC, Butler J, Khan MS. Non-Alcoholic Fatty Liver Disease, Heart Failure, and Long-Term Mortality: Insights From the National Health and Nutrition Examination Survey. Curr Probl Cardiol 2022 Dec;47(12):101333. PM: 35901855.
Myhre PL, Prescott MF, Claggett B, Felker GM, Butler J, Piña IL, Maisel AS, Williamson KM, Ward JH, Solomon SD, Januzzi JL. Comparative Effect of Angiotensin Receptor Neprilysin Inhibition on B-type Natriuretic Peptide Levels Measured by Three Different Assays: The PROVE-HF Study. Clin Chem 2022 Nov 3;68(11):1391-1398. PM: 36103292.
Park DY, Hanna JM, Kadian S, Kadian M, Jones WS, Damluji AA, Kochar A, Curtis JP, Nanna MG. In-hospital outcomes and readmission in older adults treated with percutaneous coronary intervention for stable ischemic heart disease. J Geriatr Cardiol 2022 Sep 28;19(9):631-642. PM: 36284680.
Salah HM, Verma S, Santos-Gallego CG, Bhatt AS, Vaduganathan M, Khan MS, Lopes RD, Al’Aref SJ, McGuire DK, Fudim M. Sodium-Glucose Cotransporter 2 Inhibitors and Cardiac Remodeling. J Cardiovasc Transl Res 2022 Oct;15(5):944-956. PM: 35290593.
Siddiqi TJ, Ahmed A, Greene SJ, Shahid I, Usman MS, Oshunbade A, Alkhouli M, Hall ME, Murad MH, Khera R, Jain V, Van Spall HGC, Khan MS. Performance of current risk stratification models for predicting mortality in patients with heart failure: a systematic review and meta-analysis. Eur J Prev Cardiol 2022 Nov 8;29(15):2027-2048. PM: 35919956.
Siddiqi TJ, Khan Minhas AM, Greene SJ, Van Spall HGC, Khan SS, Pandey A, Mentz RJ, Fonarow GC, Butler J, Khan MS. Trends in Heart Failure-Related Mortality Among Older Adults in the United States From 1999-2019. JACC Heart Fail 2022 Nov;10(11):851-859. PM: 36328654.
Srinivasan ES, Wang TY, Rapoport A, Erickson MM, Abd-El-Barr MM, Shaffrey CI, Than KD. Minimally invasive lateral retroperitoneal transpsoas approach for lumbar corpectomy and fusion with posterior instrumentation. Neurosurg Focus Video 2022 Jul 1;7(1):V7. PM: 36284723.
Tomaszewski WH, Waibl-Polania J, Chakraborty M, Perera J, Ratiu J, Miggelbrink A, McDonnell DP, Khasraw M, Ashley DM, Fecci PE, Racioppi L, Sanchez-Perez L, Gunn MD, Sampson JH. Neuronal CaMKK2 promotes immunosuppression and checkpoint blockade resistance in glioblastoma. Nat Commun 2022 Oct 29;13(1):6483. PM: 36309495.
Vaduganathan M, Claggett BL, Jhund P, de Boer RA, Hernandez AF, Inzucchi SE, Kosiborod MN, Lam CSP, Martinez F, Shah SJ, Desai AS, Lindholm D, Petersson M, Langkilde AM, McMurray JJV, Solomon SD. Estimated Long-Term Benefit of Dapagliflozin in Patients With Heart Failure. J Am Coll Cardiol 2022 Nov 8;80(19):1775-1784. PM: 36041669.
Vaios EJ, Batich KA, Buckley AF, Dunn-Pirio A, Patel MP, Kirkpatrick JP, Goudar R, Peters KB. Addendum: Resolution of radiation necrosis with bevacizumab following radiation therapy for primary CNS lymphoma. Oncotarget 2022 Oct 20;13:1165. PM: 36289014.
White EJ, Susman SJ, Bouffler A, Leahy JC, Griffin SM, Christenson R, Newby LK, Gordee A, Kuchibhatla M, Limkakeng AT. Predictors of Stress-Delta High-Sensitivity Troponin T in Emergency Department Patients Undergoing Stress Testing. Cureus 2022 Sep 26;14(9):e29601. PM: 36321030.
Yazdi D, Patel S, Ozonat K, Fudim M, Smith S, Centen C. Feasibility of a Cardiac Scale in Measuring Blood Pressure. J Cardiovasc Transl Res 2022 Oct;15(5):1212-1214. PM: 35396626.
Duke Heart Pulse – November 6th 2022
Chief’s message:
This weekend is the kickoff of the American Heart Association Scientific Sessions 2022 in person with a virtual component in Chicago. The meeting has gotten off to a great start with many presentations of science from Duke Faculty and Fellows, opportunities to connect and see people in person, and in general get to participate and see science (much of which is not related to COVID). The meeting also highlights for us the amazing colleagues, connections, and people that we have had through the years as part of the Duke Fellowship, Faculty, and research and clinical collaborations. It is humbling to be the Chair for this years AHA Scientific Sessions. I was reminded as well about our mission and responsibility in the opening session for the AHA that included two US Surgeons General (Jerome Adams and Regina Benjamin), FDA Director Rob Califf, and AHA president Michelle Albert and World Heart Federation president Fausto Pinto. These scientific session meetings and even our own meetings at Duke with our faculty and fellows to discuss clinical care and science have highlighted how energizing and reinvigorating in person engagement is for us all.


Highlights of the week:
Scientific Sessions Kicks Off in Chicago!
So many of our team members throughout Duke Heart and the Duke Clinical Research Institute have been preparing for the 2022 American Heart Association’s Scientific Sessions and it’s finally here. We’ll have coverage this weekend and next to showcase as much of it as we can.
We are extremely proud of all the work – from the research done at (and in partnership with) Duke that will be presented during Sessions, to the effort that has gone into planning this event at the national level, to the work done to organize our annual presence in the Exhibit Hall – it takes a lot of planning and effort by a lot of people. On behalf of the Duke Heart leadership team, thank you.
We kick off our coverage this weekend with two of our late-breaking clinical trial presentations and close out with two award winners.
We hope those of you who have traveled to be in Chicago this weekend are having a great time. Once again, congratulations to all, and thank you for all that you do!
AHA.22 LBCT: Comparative Study of Two Heart Failure Drugs Finds No Difference in Outcomes
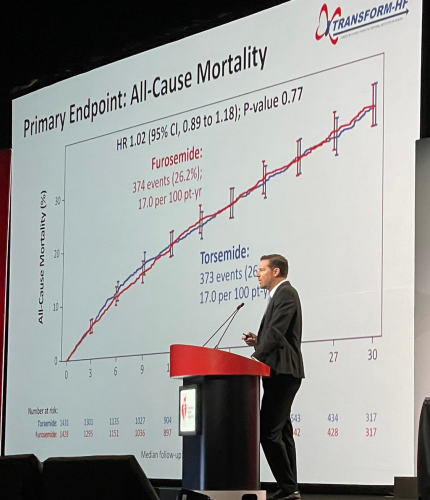 In a head-to-head comparison of two so-called ‘water pills’ that keep fluid from building up in patients with heart failure, the therapies proved nearly identical in reducing deaths, according to a large study led by Duke Health researchers.
In a head-to-head comparison of two so-called ‘water pills’ that keep fluid from building up in patients with heart failure, the therapies proved nearly identical in reducing deaths, according to a large study led by Duke Health researchers.
The study compared the diuretics torsemide and furosemide that were prescribed to patients with heart failure starting in the hospital setting. While prior data suggested a potential reduction in deaths among patients taking torsemide, the current study found no such benefit, providing clarity for both doctors and patients.
“Given that the two different therapies provide the same effect on outcomes, we shouldn’t spend time switching patients from one to the other, and instead concentrate on giving the right dose and adjusting other therapies that have been proven to have long-term benefits,” said cardiologist Robert J. Mentz, MD, chief of the heart failure section in the Division of Cardiology at Duke University School of Medicine and member of the Duke Clinical Research Institute.
Mentz was lead author of the study, called TRANSFORM-HF and funded by the National Heart, Lung and Blood Institute. He presented the findings as a late-breaking clinical trial yesterday at the American Heart Association’s 2022 Scientific Sessions in Chicago.
The study was designed as a direct comparison of loop diuretics, which are commonly prescribed to reduce the fluid buildup that causes swelling and breathing difficulties in patients with heart failure.
Mentz and colleagues enrolled more than 2,800 patients hospitalized with heart failure. Participants were randomly assigned to receive either torsemide or furosemide, and doctors determined the dosing. The study group was diverse, with women comprising 37% of participants and Black patients comprising 34%.
The main question was whether torsemide reduced patient deaths due to any cause over long-term follow-up (average of more than 17 months). The researchers found that death occurred in 373 of 1,431 study participants (26.1%) in the torsemide group and 374 of 1,428 patients (26.2%) in the furosemide group.
A secondary outcomes analysis looked at deaths or hospitalizations within 12 months, and again found little difference, with death or hospitalization occurring in 677 patients (47.3%) in the torsemide group and 704 patients (49.3%) in the furosemide group.
“This study has immediate clinical applications,” Mentz said. “Doctors spend a lot of time considering whether they will change from one diuretic to another, but there is no difference between the two for outcomes. This provides much-needed clarity. The insights from TRANSFORM-HF add to the evidence base that should help us improve patient care.”
In addition to Mentz, study authors include Kevin J. Anstrom, Eric L. Eisenstein, Shelly Sapp, Stephen J. Greene, Shelby Morgan, Jeffrey M. Testani, Amanda H. Harrington, Vandana Sachdev, Fassil Ketema, Dong-Yun Kim, Patrice Desvigne-Nickens, Bertram Pitt, and Eric J. Velazquez.
Congratulations to all TRANSFORM-HF team members – nicely done!
AHA.22 LBCT: Largest Randomized Trial Evaluates Steroids for Infant Heart Surgery
For more than four decades, doctors have been split on whether giving steroids during a pediatric open-heart surgery could be helpful for post-operative recovery. A new study is providing a bit more clarity, suggesting there are some benefits for certain kinds of patients.
Led by Duke Health researchers, the study was the largest trial designed to resolve the long-standing issue. More than 1,200 infants with heart disease were enrolled at 24 U.S. centers, with roughly half randomly assigned to receive steroids prior to heart surgeries, and the other half randomized to receive a placebo.
The main focus was whether prophylactic steroid use reduced any of more than a dozen complications, including death and heart transplant, compared to a placebo.
In the primary analysis, the researchers found no differences in the two groups, but steroid use was associated with elevated blood-sugar levels that required insulin therapy in some cases. Results showed 19% of participants using steroids required insulin therapy, compared to 8% in the placebo group. However, like many trials, the results were more nuanced and secondary analyses showed that some children might benefit.
The findings appear Nov. 6 in the New England Journal of Medicine and were presented this morning at the AHA’s 2022 Scientific Sessions.
Lead author of the study, Kevin Hill, MD, a member of the DCRI and chief of the Division of Pediatric Cardiology at Duke University School of Medicine, described the nuances of the study. Secondary results suggested that patients with less complex cases might be the ones who do better with steroids.
“Steroids reduce inflammation, and their benefit may be highest in children undergoing less complex procedures where inflammation is manageable,” Hill said. “But when you have the most complicated patients with severe inflammation affecting multiple organ systems, using steroids is like throwing a glass of water on a forest fire, and they seem to have less impact.”
Jennifer S. Li, MD, is the senior author of the paper and a professor in the departments of Pediatrics and Medicine at Duke. She says there’s a need for further study.
“We need to hone in on the patients who can actually benefit most from steroid use and develop a targeted approach to using this medicine, so that we maximize its benefit and minimize adverse effects,” Li said.
The DCRI performed the trial administration, data management and statistical analyses. The study was performed as a “trial within a registry” leveraging the infrastructure of the Society of Thoracic Surgeons Congenital Heart Surgery Database to conduct a low cost, pragmatic trial.
In addition to Hill and Li, study authors include, Prince J. Kannankeril, Jeffrey P. Jacobs, H. Scott Baldwin, Marshall L. Jacobs, Sean M. O’Brien, David P. Bichel, Eric M. Graham, Brian Blasiole, Ashraf Resheidat, Adil S. Husain, S. Ram Kumar, Jerry L. Kirchner, Dianne S. Gallup, Joseph W. Turek, Mark Bleiweis, Bret Mettler, Alexis Benscoter, Eric Wald, Tara Karamlou, Andrew H. Van Bergen, David Overman, Pirooz Eghtesady, Ryan Butts, John S. Kim, John P. Scott, Brett R. Anderson, Michael F. Swartz, Patrick I. McConnell, David F. Vener, and the STRESS Network Investigators.
Well done, team! Congratulations!
AHA.22: Presenters and Session Moderators
Between today and yesterday there were 35 Abstract Poster Session presentations by Duke Heart team members including Stephen Greene, Shahzeb Khan, Michelle Kelsey, Caitlin Drescher, Josephine Harrington, Michael Cosiano, Anand Shah, Jenn Rymer, Nishant Shah, and Conrad Hodgkinson – just to name a few.
Cardiology fellow Michael Cosiano presented “Comparing Patient Reported Outcomes and New York Heart Association Class Among Patients Hospitalized for Heart Failure” during abstract poster sessions on Saturday. He is lead author on the paper that was simultaneously published in Circulation: Heart Failure. His co-authors include Andrew Vista, Jie-lena Sun, Brooke Alhanti, Josephine Harrington, Adrian Hernandez, Robert Mentz, Stephen Greene, et al. This paper earned Cosiano recognition as a Circulation: Heart Failure (Circ HF) “Emerging Investigator.” Circ HF editors will feature his work as part of their series highlighting young investigators—defined as individuals less than ten years out of training—in the fields of heart failure, mechanical circulatory support, cardiac transplantation, and pulmonary hypertension. Additionally, this paper will be the focus of an upcoming Twitter journal club sponsored by Circ HF. Way to go, Michael!
Internal Medicine resident Anand Shah presented findings on the study, “In-Hospital Virtual Peer-to-Peer Consultation to Improve Guideline-Directed Medical Therapy for Heart Failure: A Pilot Randomized Trial” which was a Duke Heart Failure team and hospitalist-led pilot program on multidisciplinary care for hospitalized patients with heart failure. The presentation was done during a poster session held yesterday. The study findings were published online earlier this week in Circulation: Heart Failure. ICYMI, Vishal Rao was interviewed by TCTMD about the team’s findings. The TCTMD article was published earlier this week and appears in our News section below. (This was Rao’s first phone interview related to his research and he did a great job explaining the work done by the team. Great job, Vishal!). Other authors on the study include Jamie McDermott, Stephanie Barnes, Evan Murray, Michelle Kelsey, Stephen Greene, Marat Fudim, Adam Devore, Mike Blazing, Cara O’Brien, and Rob Mentz.
Findings from the study, “Adoption of Sacubitril/Valsartan in Patients with Heart Failure with Mildly Reduced or Preserved Ejection Fraction: The AHA Get With the Guidelines – Heart Failure Registry,” were presented during a poster session yesterday by Duke internal medicine resident Jacob Pierce. His co-authors include Zhen Li, Melissa Greiner, Steven Lippmann, Natalie Chantelle Hardy, Robert Mentz, Emily O’Brien, and Stephen Greene. The team’s findings were simultaneously published in Circulation: Heart Failure.
Cardiology fellow Jessie Duran presented “Abnormal Exercise Electrocardiography With Normal Stress Echocardiography is Associated With Increased Subclinical Coronary Atherosclerosis: Insights From the Project Baseline Health Study” yesterday during an oral session. Duran highlighted residual cardiovascular risk in a group of patients with positive ECG but negative stress echo. Well done!
Additionally, plenty of our Duke team members served as moderators for sessions throughout the day Saturday. They included: Andrew Landstrom, Larry Jackson, Sreekanth Vemulapalli, Manesh Patel, Neha Pagidipati, Jennifer Rymer, Jason Katz, Bradi Granger, Adrian Hernandez, Howard Rockman, Emily O’Brien, L. Kristen Newby and Rob Mentz.
We have an outstanding presence at Sessions this year! Great work everyone.
AHA.22: Douglas, Shah Honored with Council Awards
 We’re incredibly proud of Duke Heart team members Pamela Douglas, MD, and Svati Shah, MD. Both received awards last night during separate events at the AHA Scientific Sessions.
We’re incredibly proud of Duke Heart team members Pamela Douglas, MD, and Svati Shah, MD. Both received awards last night during separate events at the AHA Scientific Sessions.
Douglas was selected to receive the James B. Herrick Award for Outstanding Achievement in Clinical Cardiology by the AHA’s Council on Clinical Cardiology. Douglas delivered the James B. Herrick Lecture as part of the AHA’s Council Named Lecture Series held during Sessions. The series features lectures from some of today’s foremost clinicians and researchers as well as those with a lifetime of

contributions to the field of cardiovascular disease. Congratulations, Pam!
Shah was selected to receive the Genomic and Precision Medicine Mentoring Award by the AHA’s Council on Genomic and Precision Medicine. It was presented to her last night during the Council’s annual reception held this year in the Field Ballroom at the Hyatt Regency McCormick Place. Congratulations, Svati!
Frazier-Mills to Co-Lead ABC EP Committee

We are excited to share that electrophysiologist Camille Frazier-Mills, MD has been named co-chair of the Association of Black Cardiologists (ABC) Electrophysiology Committee. Her appointment is effective immediately and ends in April, 2024.
Congratulations, Camille! This is a tremendous honor!
CPR Performed by Duke Team Saves In-flight Passenger
 Duke Heart CVSSU team member Kaitlyn Allen and her husband, Justin Allen, MD, a Duke hospitalist, were recently in Utah so that Justin could compete in the 2022 Half Ironman World Championship race held Oct. 29 in St. George. On Tuesday, Nov. 1 while flying home toward RDU, a medical emergency was declared approximately 40 minutes into their three-hour flight. Both were nearby when a flight attendant yelled for an AED; Kaitlyn saw a passenger lying on her back in the middle of the aisle in the cabin ahead of her.
Duke Heart CVSSU team member Kaitlyn Allen and her husband, Justin Allen, MD, a Duke hospitalist, were recently in Utah so that Justin could compete in the 2022 Half Ironman World Championship race held Oct. 29 in St. George. On Tuesday, Nov. 1 while flying home toward RDU, a medical emergency was declared approximately 40 minutes into their three-hour flight. Both were nearby when a flight attendant yelled for an AED; Kaitlyn saw a passenger lying on her back in the middle of the aisle in the cabin ahead of her.
She and Justin immediately ran to the passenger’s aid. When they arrived, another passenger – a pediatric physician assistant – was maintaining the passenger’s airway, but neither Kaitlyn nor the PA could feel a pulse. Kaitlyn immediately started chest compressions while Justin took over the airway and prepared the AED. After the second round of compressions, the patient began moving her arms and became responsive. The team then applied oxygen, the AED, and took a set of vitals. Another passenger who happened to be a medical ICU nurse provided a glucometer and a pulse oximeter. With the passenger’s vitals stable, Justin cleared the patient’s cervical spine and she was able to sit upright, and eventually get back into a seat.
Kaitlyn communicated directly with the pilot about the situation. Ultimately the passenger arrived in stable condition and upon landing was handed off to paramedics for further evaluation.
This was not the first time the Allen’s have been in an emergency situation together. The two worked together at Lakeland Health in St. Joseph, MI (Kaitlyn’s hometown) during Justin’s internal medicine residency. There, they worked together during rapid responses and code blues. Kaitlyn and Justin concur that it was their previous experiences that allowed them to operate as a cohesive unit during this in-flight emergency. Even in less-than-ideal conditions on a fully booked flight at 29,000 feet with limited medical equipment, they worked together quickly and professionally to save a fellow passenger’s life.
Great teamwork and use of CPR!
Shout-out to D’Amico, Antonia
We received a great message this week regarding a patient compliment for Tommy D’Amico and Scott Antonia:
“My experience in the hospital was excellent. All the personnel treated me extremely well. I am eternally appreciative to Dr. D’Amico and the dream team at Duke University Hospital. All the services of the hospital are excellent. My operation was a success & I am already recovered. My appreciation to Dr. D’Amico & Dr. Scott Antonia for all that they did for me. Thanks.” — a grateful patient (name withheld for privacy)
“Tommy and Scott, I was just delighted to read this lovely compliment about you both on our Patient Satisfaction Survey. Thank you for your excellence and compassion. You clearly made a difference in this patient’s life. Very best wishes, Lisa” — Lisa Clark Pickett, Chief Medical Officer, Duke University Hospital
Nice work!
Halloween Pics
The week started off with fun Halloween celebrations — check out this pumpkin carved by cardiology fellow Ilia Shadrin! That’s the Shadrin family dressed as The Incredibles, and Dennis Narcisse with his twin boys as dinosaurs. So adorable!
We love the holiday spirit shown by our Duke Heritage Cardiology team in Wake County. Your ‘Boo Crew’ t-shirts are awesome. What a great way to show your enthusiasm while providing amazing care to our patients. Great work!
Thank you to all who shared your holiday pics with us for Pulse. We love getting your submissions – please keep them coming.



Samuel L. Katz, doctor who helped develop measles vaccine, dies at 95
 We were saddened this week to learn of the passing of our long-time Duke Health colleague, Dr. Sam Katz. A luminary in the field of infectious diseases and pediatrics, Katz was a beloved team member at Duke. His work has impacted millions although few of them may realize it. Our deepest sympathy to his family, friends, and colleagues throughout the world.
We were saddened this week to learn of the passing of our long-time Duke Health colleague, Dr. Sam Katz. A luminary in the field of infectious diseases and pediatrics, Katz was a beloved team member at Duke. His work has impacted millions although few of them may realize it. Our deepest sympathy to his family, friends, and colleagues throughout the world.
Remembering Samuel L. Katz, MD
Samuel L. Katz, MD, died on Monday, October 31, 2022.
Dr. Katz was a world-renowned virologist, pediatrician, and chair emeritus and Wilburt C. Davison Professor Emeritus of Pediatrics at Duke University School of Medicine. He was an honors graduate of Dartmouth College and Harvard Medical School. After a medical internship at Beth Israel Hospital, he completed pediatrics residency training at the Massachusetts General Hospital and the Boston Children’s Hospital, followed by a research fellowship in virology and infectious diseases.
Dr. Katz then became a staff member at Children’s Hospital working with Nobel Laureate John F. Enders for the next 12 years researching viruses — specifically measles, a disease that at the time killed more than five to six million children each year globally. During this time, Drs. Katz and Enders developed an attenuated measles virus vaccine.
In 1960, David Morley, MD, a British physician working in Nigeria, where the effects of measles were far more severe than they were in the United States, contacted Dr. Katz. Together, they inoculated Nigerian children with the new vaccine, with successful results. Not long after, the vaccine was tested in national clinical trials, approved by the Food and Drug Administration in 1963, and is now used throughout the world.
In addition to the development of the measles vaccine, Dr. Katz worked extensively on a range of other vaccines, including vaccinia (used as smallpox vaccine), polio, rubella, influenza, pertussis (whooping cough), Haemophilus influenzae b conjugates, and HIV.
In 1968, Dr. Katz was appointed chair of the Duke Department of Pediatrics, where he served for 22 years. In addition to mentoring two decades of students and residents, he established an exchange program with Oxford University and provided training for an annual succession of residents from the American University of Beirut. Throughout his tenure he displayed genuine interest in his patients, faculty, and trainees, actively encouraging female and minority physicians and seeking to diversify the faculty.
“As he did for so many others, Dr. Katz had a profound influence on my career,” said School of Medicine Dean Mary E. Klotman, MD. “His commitment, passion, and warmth were infectious. Duke School of Medicine, Pediatrics, and the world are all the better because of him.”
“Dr. Katz has been a stellar role model for all of us, as a clinician, as a teacher, as an investigator, and as an advocate for children,” said Department of Pediatrics Chair Ann M. Reed, MD. “He set a high bar, advancing medicine in ways that have improved children’s health around the world–he is truly one of the outstanding pediatric investigators of our times.”
In addition to seeing patients and supporting faculty, Dr. Katz expanded his role as an advocate for vaccination. Experiencing firsthand the ways in which disease affects children living in resource-poor countries contributed to Dr. Katz’s lifelong advocacy, within the United States, and around the world. He chaired the Committee on Infectious Diseases of the American Academy of Pediatrics (AAP), the Advisory Committee on Immunization Practices (ACIP) of the Centers for Disease Control (CDC), the Vaccine Priorities Study of the Institute of Medicine (IOM), and several World Health Organization (WHO) vaccine and HIV panels. He served on the National Institutes of Health (NIH) Committee for AIDS Vaccines and co-chaired the India-U.S. Vaccine Action Program and the National Network for Immunization Information. In addition, he served as chair of the Public Policy Council of the Infectious Diseases Society of America (IDSA), co-chaired IDSA’s Vaccine Initiative, and worked on behalf of UNICEF and the American Red Cross.
Dr. Katz earned numerous accolades throughout his career, including the inaugural Joseph St. Geme, Jr. Leadership Award in 1988, the 2003 Albert B. Sabin Gold Medal awarded by the Sabin Vaccine Institute, and the 2015 Maxwell Finland Award for Scientific Achievement for his contributions to vaccine discoveries during his career.
Please see link to The Washington Post news brief about his death in our News section below.
Reminder: Voting Day is Tuesday, Nov. 8
Election Day is Tuesday, Nov. 8 and a list of polling locations can be found here. Visit the State Board of Elections website or vote.duke.edu for additional information. Please vote!!!
On Thursday, Nov. 10 from Noon – 1 p.m., the Duke State Relations team and Duke Health’s Government Relations team are offering a post-election briefing to discuss the outcomes of the 2022 Election, how it will impact Duke Health, and provide a preview of the 2023 legislative sessions in Raleigh and Washington, DC. This event will be moderated by Dev Sangvai, MD, interim president, Duke Regional Hospital. To participate via Zoom, visit https://duke.is/2eq4k.

CulturePulse 2022 — Be Heard
All Duke Health team members were emailed a link to the 2022 CulturePulse survey on Wednesday, Nov. 2. The brief survey is confidential, mobile-friendly, and simple to complete.
The survey link will remain open through Nov. 16; you can also find it via the QR code you’ll see on digital signage and printed flyers around Duke.
CulturePulse is a way for team members to share their feedback about what’s going well and what could be improved at Duke Health. Please participate and encourage your team members to do so as well. You will receive automatic reminders about the survey until you complete it or it closes. This is a great opportunity for all of us to have our voices heard.

ORA Holiday Deadlines
The Office of Research Administration (ORA) will operate with reduced staff during the holiday season to allow team members time to recharge. During this period, please plan as far in advance as possible.
To help ORA respond as timely as possible to your needs, please plan in advance based on the following:
Thanksgiving Day and the Friday After
If you need something processed BEFORE the Thanksgiving holiday, please have it submitted in ready-form to ORA by Thursday, November 17. Otherwise, if it can wait, ORA will process it the following week (beginning November 28).
Last two weeks of December
For any transactions with due dates between December 19 – January 2, please have them submitted in ready-form to ORA by Thursday, December 15 to ensure there is adequate time and staffing to respond to your needs.
Please note: the next NIH SBIR/STTR deadline is Jan. 5, 2023, and the internal deadline is 8 a.m. on Dec. 28, 2022. Because this deadline falls in the last two weeks in December when ORA will be operating with reduced staff and because these award mechanisms are usually complex and require careful institutional coordination before submission:
- Please complete Intent to Submit for all planned SBIR/STTR applications no later than Dec. 5, 2022; and
- Please plan to route a submission-ready application no later than Dec. 15, 2022; if more time is needed, please submit a late waiver request so that ORA can plan for appropriate coverage to support these applications.
For anything submitted in the last two weeks of December that can wait until after the holiday break, ORA will be back up to speed with a full team on Jan. 3, 2023 and will look forward to managing all pending issues at that time.
This has been another year of tremendous growth in research at Duke. The Office of Research Administration thanks you for your continued partnership in support of Duke’s research mission and they send warm holiday wishes to all!
Matters of Grief: Grief Symposium 2022
The Duke Health Office of Culture and Well-being is offering Grief Symposium 2022 on Tues., Nov. 15 and a panel discussion on Wed., Nov. 16. Please consider joining for one or more events (most are virtual) in which they and participants will explore the many aspects of grief, including common grief reactions, how to support those who are grieving, professional grief, grief around loss of function or role, disenfranchised grief, rituals that may help us in the grieving process, and how to turn grief into positive action. Register here (please use your Duke e-mail to complete your registration).
- Grief Symposium: Tues., Nov. 15, noon-2 p.m.
- Grief Panel Discussion: Wed., Nov. 16, 1-2 p.m.
- Small Group Interactive Activities: Wed-Fri, 11/16-11/18. These will include: Somatic Body Work, Narrative Writing, Mandala Art, and Restorative Circles: Personal Grief, Pet Grief, and Gun Violence.
To learn more, please visit: https://cultureandwellbeing.dukehealth.org/grief-toolkit-symposium. A link to last year’s symposium is available on that page.
Additional Reminders:
- It is vital that we remain vigilant with masking, hand hygiene, PPE, and other safe behaviors to prevent the spread of infection. Please pay special attention to the proper wearing and securing of gowns and be mindful of PPE compliance. Thank you for all you do to keep everyone safe and healthy.
- November is American Diabetes Month, Pulmonary Hypertension Awareness Month, and National COPD Awareness Month. Thanks for all you do to help patients with these conditions!
- The deadline for staff flu vaccinations is Tuesday, Nov. 15 at 10 a.m. Vaccination sites for faculty and staff can be found here: https://flu.duke.edu/vaccination/employees/
Upcoming Events & Opportunities
Cardiology Grand Rounds
November 8: Topic, presenter TBD. Watch your email for the Zoom link!
CME & Other Events
November 8: Election Day. Please vote!
November 8: DOM Research Quality Town Hall. Topic: 2023 NIH Data Management and Sharing Policy. 12-1 p.m. via Zoom. Register here. You must register to receive the Zoom link for the event.
November 14: Prostate Cancer & CVD Symposium, Webinar 4. Final of a four-part webinar series. Collaboration between the International Cardio-Oncology Society & Duke Heart. Noon, Eastern. Free. To register visit https://duke.is/ptjbs.
Call for abstracts: 2023 Duke Health Quality and Safety Conference
The virtual poster submission period for the 2023 Duke Health Quality and Safety Conference is now open. The deadline for submission is Wednesday, Dec. 14. The 2023 Conference will be held the weeks of March 13 and 20, with an in-person event on Thursday, March 23.
For more information and to submit your abstract, please click here.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
October 27 — Duke Clinical Research Institute
Reuters
U.S. government to test Pfizer’s Paxlovid for long COVID
https://duke.is/7nbtf
October 28 — Duke Health
CBS17.com
450+ turn out for Duke Health event to help caregivers in Durham
https://duke.is/g9zvx
October 28 — Joseph Turek and the Sinnamon family
KALB-TV (Alexandria, LA)
Health headlines: First-of-its-kind heart and thymus surgery proves successful
https://duke.is/ga2km
October 28 — Duke Health
Becker’s Hospital Review
https://duke.is/vfeed
October 28 — Duke Clinical Research Institute
MSN/Washington Examiner
NIH to use Pfizer’s Paxlovid to study causes of long COVID
https://duke.is/m6t8h
October 31 — Jonathan Piccini
Patientcareonline.com
https://duke.is/8cpbk
October 31 — Joseph Turek and the Sinnamon family
WFMZ-TV (Allentown, PA)
Doctors pioneer a heart transplant technique involving another life-saving procedure
https://duke.is/2hzxe
November 2 — Betty Tong
WNCN-CBS17.com
November is Lung Cancer Awareness Month; Duke doctor recommends screening
https://duke.is/zq27k
November 3 — Samuel Katz (pediatrics)
The Washington Post
Samuel L. Katz, doctor who helped develop measles vaccine, dies at 95
https://duke.is/mrcde
Recent Comments