Updates of the week:
In Memoriam: Robert H. Jones, MD, Professor Emeritus of Surgery
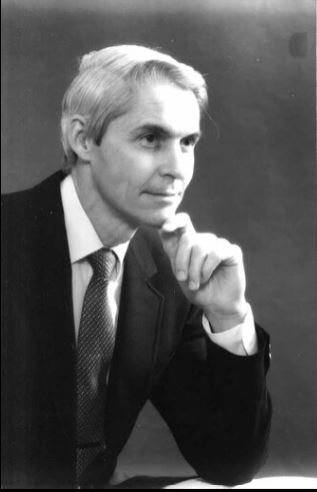 It is with great sadness that we inform you of the passing of Robert “Bob” H. Jones, MD, Professor Emeritus of Surgery, on January 26, 2022. Dr. Jones was the Mary and Deryl Hart Distinguished Professor of Surgery and a prolific cardiothoracic surgeon and clinical investigator until his retirement in 2014. We have lost a treasured member of the Duke community, but his legacy will live on.
It is with great sadness that we inform you of the passing of Robert “Bob” H. Jones, MD, Professor Emeritus of Surgery, on January 26, 2022. Dr. Jones was the Mary and Deryl Hart Distinguished Professor of Surgery and a prolific cardiothoracic surgeon and clinical investigator until his retirement in 2014. We have lost a treasured member of the Duke community, but his legacy will live on.
Dr. Jones received his medical degree from Johns Hopkins University in 1965, and became one of the first Duke University surgical residents taught by Dr. David C. Sabiston, Jr. His residency was interrupted by military service when Dr. Jones served as a Captain in the Air Force. He then completed his residency and joined the Duke Department of Surgery as an Assistant Professor in 1975.
Dr. Jones’ career at Duke spanned 40 years as a cardiac surgeon, clinical investigator, resident educator, and an agent of change in the provision of cardiac care here at Duke and around the world. Beginning as a Howard Hughes Investigator, he made several seminal contributions in the field of lung scanning and nuclear cardiology imaging. His major interest was in the treatment of patients with coronary artery disease, where he was instrumental in the employment of patient data from the Duke Cardiovascular Disease Databank and the Duke Cardiac Research Institute to develop evidence that has guided surgeons and cardiologists through decades of change. From this platform, he obtained NIH funding for the STICH trial, which compared medical therapy to surgical therapy for coronary artery disease. This trial ultimately enrolled over 2,000 patients worldwide, following them for a decade, and publishing outcomes in more than 50 manuscripts to date.
As his academic career flourished, he was selected as the inaugural recipient of the Mary and Deryl Hart Distinguished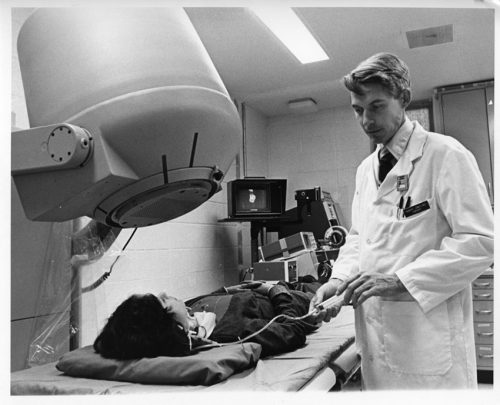 Professorship, created to honor the founder of Duke’s Department of Surgery. As a professor, Dr. Jones was an accomplished surgeon performing thousands of Coronary Artery Bypass operations and training scores of surgical residents. He emphasized the integration of science and clinical decision making within everyday practice.
Professorship, created to honor the founder of Duke’s Department of Surgery. As a professor, Dr. Jones was an accomplished surgeon performing thousands of Coronary Artery Bypass operations and training scores of surgical residents. He emphasized the integration of science and clinical decision making within everyday practice.
Dr. Jones published more than 250 manuscripts that have provided the evidence base used in that everyday practice. His research also focused on harmonizing the roles of surgeons and cardiologists in order to strengthen collaboration between specialties.
Dr. Jones co-founded the Heart Center in 1989 as the first service line within Duke Hospital and promoted joint research and joint clinical practice. This directly led to the concept of Heart Team decision making that is now embodied in all national and international guidelines for the treatment of coronary disease.
Dr. Jones’ legacy is embodied in the thousands of recipients of his generous teaching and mentorship in the clinical, research, and administrative communities. This legacy is best summed up by the inscription on his retirement gift: “Physician, Surgeon, Scholar, Mentor, Leader…and so much more!”
A memorial service will be held at 11:00 am on March 5th at the Cole Mill Road Church of Christ, 1617 Cole Mill Rd, Durham, NC 27705. A full obituary can be found here.
Upon Dr. Jones’ retirement, Duke’s Medical Alumni Association honored him and other retiring faculty at a reception and dinner. The Association produced a video to honor him that evening; it can be viewed here: https://www.youtube.com/watch?v=j6-NK9RUfhA.
We extend our deep condolences to his family, friends, his mentees and former colleagues throughout the world. We know he will be missed.
We wanted to share some thoughts and reminiscences with you:
From Jerry Reves, MD, Dean Emeritus, Distinguished Professor Medical University of South Carolina and former faculty member, Duke Anesthesiology
“Bob was a colleague and good friend. The quality I most admired was his honesty that was always informed by his intelligence and innovation. He had pioneered the surgical component of the Duke Databank and learned very early how the preoperative cardiac catherization data could be used to predict surgical outcome. This was truly innovative, but once in a conversation we were having in relation to various surgeons reporting mortality data after coronary bypass surgery, he said: “I can make my mortality whatever I want.” He had learned by looking at the Duke Databank that if you operated only on patients with very good ventricular function and little coronary disease that the mortality approached zero. However, if you operated on patients with poor ventricular function and a lot of coronary disease the mortality approached 5 percent. So his comment was not boastful, it was an honest, scientifically precise statement that surgical results were almost solely dependent on the preoperative condition of his patient. If a surgeon wanted great results he/she would not operate on sick patients. Bob continued to take all patients and I admired him for that.
 Bob, Tom Bashore and I were asked to design a Heart Center for Duke. This request came from Drs. Greenfield and Sabiston. We visited three places — Mayo Clinic, Texas Heart, and Cleveland Clinic — and studied University of Alabama Birmingham and Emory. The three of us, especially with Bob’s enthusiasm agreed that we could build a unique Heart Center at Duke that featured superb clinical care and innovative research. We designed a heart center that integrated Cardiology, Cardiac Surgery and Cardiac Anesthesia. The model was accepted, and the rest is history. It would not have happened without Bob Jones representing cardiac surgery!
Bob, Tom Bashore and I were asked to design a Heart Center for Duke. This request came from Drs. Greenfield and Sabiston. We visited three places — Mayo Clinic, Texas Heart, and Cleveland Clinic — and studied University of Alabama Birmingham and Emory. The three of us, especially with Bob’s enthusiasm agreed that we could build a unique Heart Center at Duke that featured superb clinical care and innovative research. We designed a heart center that integrated Cardiology, Cardiac Surgery and Cardiac Anesthesia. The model was accepted, and the rest is history. It would not have happened without Bob Jones representing cardiac surgery!
Bob Jones was the “go to” surgeon if you or your patient needed coronary bypass surgery, the most frequently performed operation in the formative days of the Duke Heart Center. He was consistent, competent, and available. In the high stakes, sometimes stressful cardiac surgical operating room, where everyone had to work in a professional, communicative, and collaborative fashion, there was no better team player to be with than Dr. Jones.”
From Tom Bashore, Duke Professor of Medicine in Cardiology:
“My first memory of Bob Jones was when one of my patients commented that they thought he was such a nice man — they were not sure if he was the chaplain or their heart surgeon. With his head of white hair and broad grin of white teeth, Bob put everyone at ease. He was kind, but he was innovative, and he was willing to try novel things in the OR. What many might not know is that in the late 1970s, he was also one of the first people working in nuclear cardiology at Duke. Using a “first-pass” technique, for the first time one could view images of the heart chambers contracting and relaxing as the radionuclide traversed through the heart. The spatial resolution was lousy though, and I remember Bob’s hearty laugh the first time he presented his data where the end-systolic image of the heart came down to a single square red pixel. Rather than being alarmed, Bob was the kind of person that could see the humor in that and was not at all deterred by such stuff. He obviously moved on to other areas as his career took off in other directions. When he, Jerry Reves, and I went around the country visiting Heart Centers (in the hope of forming one here at Duke), he traveled with only a tiny satchel bag and never a suitcase (he bragged about that). Despite that, he always looked the best dressed of all of us, and with his smooth style he was certainly the best looking and best talker among us, no matter what the situation. And that aura about him never changed throughout his whole career. He will always be remembered for not only being an outstanding physician and surgeon but for being a wonderful and warm human being. There have been few like him at Duke, and I daresay in medicine.”
From Carmelo A. Milano, MD, Professor of Surgery and chief, Section of Adult Cardiac Surgery at Duke:
“Dr. Jones developed and ran the influential STICH trial. This was a large international trial that demonstrated the benefits of CABG surgery for patients with reduced heart function and heart failure. The results of this trial changed the way we practice heart surgery today.”
From Peter K. Smith, Mary and Deryl Hart Distinguished Professor of Surgery and former chief, Duke Division of Cardiovascular and Thoracic Surgery:
“Bob Jones influenced me in so many ways. I did a couple of hundred coronary operations with him; I took care of maybe 500-600 patients of his, maybe more. I interacted with him every day, and learned something every day. He essentially took me under his wing in the research area, and made a huge difference in my research capabilities and my ability to get grants. He was a pretty amazing guy and he was driven to contribute. He was very goal-oriented with a very strong desire to bring cardiology and surgery together in a meaningful way, which he was able to do at Duke — which led to a real blossoming of both cardiology and cardiothoracic surgery here as the Duke Heart Center. He was very forward-thinking — not only was the creation of a true ‘Heart Center’ good for Duke, it was good for our patients. This was happening at a time when cardiologists were transitioning from being ‘diagnosticians’ toward cardiologists as ‘treating specialists.’ And that transition period was very interesting because we were pretty co-dependent in the early days. Percutaneous interventions were quite hazardous in the beginning and required close collaboration with surgeons. As percutaneous intervention became much less “risky” it became potentially more competitive, but the evidence-base was poor. So all the decisions really had to be made either individually by cardiologists or individually by surgeons or jointly between the two — and it became much more frequent that we did this jointly at Duke, with due credit to Dr. Jones who recognized where this transition was going to go. It could have been polarizing or it could be harmonizing. He stressed the latter.
Interestingly, his academic career in professional societies was primarily through the American College of Cardiology, and not with a surgical society. He served as chair of their Board of Governors for time and was a trustee for a time as well. With academic surgeons, they’re typically more involved with a surgical society such as AATS, but Bob put his time and commitment toward the ACC which speaks a great deal to his desire for collaboration.”
From Chris O’Connor, MD, President, Inova Heart and Vascular Institute and former division chief, Duke Cardiology:
“As a surgeon, Bob Jones was thought of as ‘the cardiologist’s surgeon’ – he was so collaborative with us. When I was a junior attending in the intensive care unit at Duke we would have these difficult cases that would often get turned down by his surgical colleagues. We would always call him and he would talk with us and talk with the patient – he was very good with patient interactions. He would take on high-risk cases that needed to be done because he understood the evidence from the Duke Databank, and most importantly, he understood the needs of the patient and valued the recommendations of the cardiologists.
As an investigator, he had this unique mindset which was rich in his understanding of quantitative science and data and it just fit the philosophy of the Duke Databank and the DCRI. He was completely committed to the philosophy of quantitative clinical research. He worked closely with Kerry Lee and the biostatisticians at DCRI — he was also a consultant to the New York State Cardiothoracic Surgery database. He was a superb clinical investigator. The capstone of his career was his work with Eric Velazquez on the STICH trial, a 15-year endeavor that really changed the way we think of surgery and the management of heart failure forever. It’s an enduring body of work that will last forever, in my opinion, not just the STICH trial but all the follow-up trials to that. He was so passionate about it — and it would have never been completed if it wasn’t for Bob Jones leading that effort; it was just so hard to do that trial. He dedicated the latter part of his career entirely to that effort.
STICH took an enormous amount of education and awareness, which Bob led globally. He leveraged some deep relationships with his colleagues in Poland, which he had developed over 30-40 years. It was through those relationships in particular, that they were able to complete the trial. Only 25 percent of the patients enrolled were in the United States.
The other thing to know about Bob is, early in his career, he did some very important investigations looking at how nuclear scans can be used to detect heart disease. And for many, many years, people outside of Duke thought he was a nuclear cardiologist, not a surgeon, because of his publications in that area.
Bob was just a prince of a person. He was deeply spiritual and he brought that connectivity to his care of patients and his interactions with people, and I thought he was a terrific professional colleague. He could be hard-headed and firm, but in the end, he really loved his professional colleagues. He loved his family and he really loved his patients. He was an outstanding cardiothoracic surgeon, outstanding clinical investigator, and outstanding person.”
From Manesh Patel, MD, professor of medicine and chief, Division of Cardiology:
As a fellow, faculty member, and clinical researcher at the DCRI, we looked towards Bob Jones as the standard bearer for the cardiothoracic surgical group. He was a clinician who many of us got to interact with for patient care, for clinical research, and most importantly as a mentor for both cardiologists and surgeons. He was kind, consistent and would be direct and firm about how we considered research and patient care, and in the end was a key driving force inmproving the way we cared for patients. In the cardiology world, his work with Eric Velazquez on the STITCH trial will be one of his key legacies in addition to the Duke Heart Center and people that practice here.
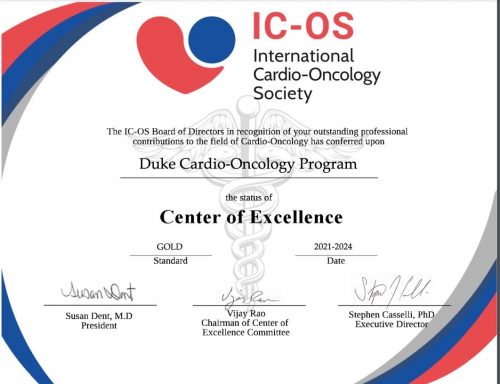
Cardio-Onc Program Named Center of Excellence by ICO Society
We learned this week that our Duke Cardio-Oncology program is among the first to achieve Center of Excellence gold status designation by the International Cardio-Oncology Society. It is one of only nineteen programs world-wide to receive the Center of Excellence rating. In the inaugural effort, 15 programs received gold designation and 4 received silver. To learn more about the ICO Society and the COE rating, please visit: https://ic-os.org/excellence-certification/. The official presentation was made during a virtual event held January 27.
Congratulations to Michel Khouri, Susan Dent and their incredible team!
Shah Named to NC Chapter of ACC

Nishant Shaw, assistant professor of medicine in cardiology has been elected to the Leadership Board of the North Carolina chapter of the American College of Cardiology as a Councilor. He will serve a three-year term starting in March. Councilors to the chapter are responsible for serving as a member of the Nominating Committee; serving as an advocate for his/her region in the areas of education and advocacy; communicating Chapter business to members of his/her region and reporting back to the Chapter, as well as participating in approving the annual Chapter budget.
Shah will serve alongside fellow Councilor Adam DeVore and cardiology fellow Vanessa Blumer, who serves as the ACC FIT Liaison.
Congratulations, Nishant! Well-deserved and certainly this team will represent us well.
Shout-out to Rymer & PWIM Planning Team

Congratulations to Jenn Rymer and the planning team for the Program for Women in Internal Medicine (PWIM). They held a terrific online session this week that featured Pam Douglas, Leslie Curtis and  April Salama discussing how they got their start in medicine and launched superb careers in research. Rymer moderated an engaging and informative discussion. Great job to all!
April Salama discussing how they got their start in medicine and launched superb careers in research. Rymer moderated an engaging and informative discussion. Great job to all!
Byler Named Clinical Lead 3100 Effective March 14th
 We are excited to share that Hannah Byler will be joining the 3100 leadership team as a Clinical Lead effective Monday, March 14, 2022. Hannah began her nursing career on 3100 in March 2019. She earned her Associates in Nursing at Wake Technical Community College in 2018 and her Bachelor of Science in Nursing at University of North Carolina Wilmington in 2021. Hannah holds a variety of roles on 3100 including preceptor, charge nurse, MOVEs champion, Time to Pace class instructor, and has recently advanced to CNIII.
We are excited to share that Hannah Byler will be joining the 3100 leadership team as a Clinical Lead effective Monday, March 14, 2022. Hannah began her nursing career on 3100 in March 2019. She earned her Associates in Nursing at Wake Technical Community College in 2018 and her Bachelor of Science in Nursing at University of North Carolina Wilmington in 2021. Hannah holds a variety of roles on 3100 including preceptor, charge nurse, MOVEs champion, Time to Pace class instructor, and has recently advanced to CNIII.
Congratulations, Hannah!
CVRC Post-Holiday Morale Booster!
The Duke Cardiovascular Research Center team was able to help celebrate their team members last week with a post-holiday pick-me-up.
Their leadership team ordered team hats and distributed almost a hundred in total. CVRC faculty and staff could pick between the  baseball cap style worn by Cheryl Woodard and Maria Price Rapoza or and the beanie ski hat style worn by Howard Rockman. The hats were originally intended as a holiday gift for CVRC faculty and staff, but due to pandemic-related manufacturing issues they weren’t ready in time for the holidays, so the team used them to liven up the last Wednesday in January instead (a day when everyone needed a bit of cheer and a morale boost!).
baseball cap style worn by Cheryl Woodard and Maria Price Rapoza or and the beanie ski hat style worn by Howard Rockman. The hats were originally intended as a holiday gift for CVRC faculty and staff, but due to pandemic-related manufacturing issues they weren’t ready in time for the holidays, so the team used them to liven up the last Wednesday in January instead (a day when everyone needed a bit of cheer and a morale boost!).
Great idea and perfect timing with the recent cold weather!

Shout-out to CDU Team
Congratulations to the Cardiac Diagnostic Unit for completing a successful Intersocietal Accreditation Commission audit for Adult Echo, Adult Stress Echo, and Adult Transesophageal Echo! Thank you to everyone who worked through the process, and thanks to the entire team for maintaining the Duke Standards even during the accreditation “off season”. We are so proud of the work you do for our cardiac patients every day!
Great job, everyone!
It’s Duke Research Week 2022
January 31 – February 4: Duke Research Week 2022. Join us virtually for a week-long celebration of research underway at Duke! There is an excellent lineup of faculty lectures, panel discussions, “flash talks” with graduate students, trainees and postdoctoral fellows, and guest presenters for the Robert J. Lefkowitz, MD, Distinguished Lecture and Daubechies Lecture.
Check out the full agenda here: https://dukeresearchweek.vfairs.com/en/#distinguishedlectures
Duke Heart Family Grows Again!
Congratulations to newly minted grandfather, Richie Palma! His family welcomed twin boys two weeks ago. Owen Scott Horvath and Finn Lucas Horvath were born to Richie’s daughter Chloe and her husband Andrew. The family lives in Lafayette, CA. Richie reports that everyone is healthy and doing great!


National Wear Red Day
Friday, Feb. 4: National Wear Red Day. Help increase awareness of the impact cardiovascular disease has on all of us — wear red on Friday, Feb. 4! Please consider taking photos of your teams and sending them to us so that we can share them in Pulse throughout the month of February.
ICYMI: STAT First Opinion Piece By Galanos, et al.
Our Duke Palliative Care colleague, Tony Galanos, has co-authored an opinion piece that ran this week in STAT (Jan. 24, 2022). His co-authors are faculty members at UCSF. We think it’s worth a read: We all need help working through grief and hardship.
COVID-19 Updates
All the latest Clinical Operations updates related to COVID can be found at https://covid-19.dukehealth.org.
Duke Health’s Adopt-A-Unit is a matchmaking program that enables teams to actively support units continuing to fight on the frontlines of COVID through efforts such as meals, expressions of gratitude or other well-being support. If you are a leader interested in adopting a unit, please complete this smartsheet form. Once your information is received, a program member will be in touch to connect you with a unit in need that fits your budget and timeline. If you’d like to donate to our Healthcare Worker Unit Support fund, click here for details. Questions? Contact caring@duke.edu.
Reminder: All Duke University Health System (DUHS) and Private Diagnostic Clinic (PDC) team members, regardless of work location, are required to receive and provide documentation of a completed COVID-19 booster vaccination by 10 a.m. on Tuesday, Feb. 15, 2022, or within 28 days of their eligibility under CDC and state guidelines. More details are available in this email that was sent to all staff on Tuesday, Dec. 28.
Upcoming Events & Opportunities
Cardiology Grand Rounds
February 1: No CGR today.
February 8: No CGR today.
February 10: Topic TBA. Our guest will be AAMC President, Dr. David Skorton.
February 15: Topic TBA. Presenter will be Toi Spates.
Upcoming Duke Heart CME
April 23: Duke Sports Cardiology & Sudden Death in Athletes Symposium with course directors Jim Daubert and Bill Kraus. Virtual. For information or to register, contact Christy Darnell christy.darnell@duke.edu or 919-880-8686.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
January 21 — Adrian Hernandez
WebMD
Ivermectin as Potential COVID-19 Treatment Gets Studied at Duke University
https://duke.is/4rj8r
January 24 — Adrian Hernandez
Lakeland Ledger (FL)
Lakeland Regional joins national study to see if ivermectin is effective against COVID-19
https://duke.is/98db9
January 24 — Adrian Hernandez
Medscape
Ivermectin as Potential COVID-19 Treatment Gets Studied at Duke University
https://duke.is/jfanc
January 25 — G. Chad Hughes
Endovascular Today
STS and AATS Publish New Practice Guideline for Type B Aortic Dissection
https://duke.is/gn86g
January 25 — G. Chad Hughes
Vascular Specialist
https://duke.is/v99z8
January 25 — Andrew Wang
tctMD
Differing Advice for Infective Endocarditis Surgery Stems From Evidence Gaps
https://duke.is/z767z
January 25 — G. Chad Hughes
Cardiovascular Business
A fresh look at managing patients with type B aortic dissection
https://duke.is/nja47
January 26 — Derek Chew and Duke Clinical Research Institute
tctMD
CABG Provides ‘Good Value’ in Ischemic Cardiomyopathy
https://duke.is/b48ru
Recent Comments