Home » Articles posted by Manesh Patel, M.D. (Page 8)
Author Archives: Manesh Patel, M.D.
Duke Heart Pulse for week ending Feb 27th 2022
Highlights of the week:
Thank you, Residents & Fellows
On behalf of the Duke Heart Leadership team and faculty across the Divisions of Cardiology and Cardiovascular and Thoracic Surgery, we thank each and every one of our trainees – our surgery residents and all fellows — we hope you know how much we value and appreciate the work you do, your dedication to patient care, and the fact that you chose to spend your training years here with us in Durham, NC.
These are not easy years for anyone who chooses to embark on a career in surgery or medicine – but we hope you find your time here fulfilling, enriching, fun and inspiring. This week happens to be GME Appreciation Week, but your work matters today and every day, and it will matter for years to come. Thank you for the many ways in which you inspire each of us and for being part of the Duke Heart family!
Voting for USNWR ‘Best Hospitals’ Now Open in Doximity
 The survey period for U.S. News & World Report’s ‘Best Hospitals’ is now open in Doximity. We encourage all those who are eligible to vote in the survey of “Best Hospitals for Cardiology and Heart Surgery” to consider casting a vote for Duke’s hospitals – this is a great way to support our efforts in leading the country in patient care, innovation, research and the education of future specialists.
The survey period for U.S. News & World Report’s ‘Best Hospitals’ is now open in Doximity. We encourage all those who are eligible to vote in the survey of “Best Hospitals for Cardiology and Heart Surgery” to consider casting a vote for Duke’s hospitals – this is a great way to support our efforts in leading the country in patient care, innovation, research and the education of future specialists.
Reminder: paper surveys have been discontinued. The only way to vote in the survey is online via Doximity.
If you have not yet claimed your profile on this platform, you can do so at any time during the voting period.
- Go to Doximity.com
- Enter your first and last name on the home screen
- Click on the ‘Find My Profile’ button
A survey will display in your profile until you vote or the survey closes on March 25, 2022.
Circulate! 2022 Recognizes Duke Efforts
 Members of the Duke Heart team were recently celebrated by our Vascular Cures partners at Circulate!, their annual gala held to celebrate the work done throughout the year by patient advocates, industry members and researchers, all of whom are dedicated to improving the care of patients with vascular disease.
Members of the Duke Heart team were recently celebrated by our Vascular Cures partners at Circulate!, their annual gala held to celebrate the work done throughout the year by patient advocates, industry members and researchers, all of whom are dedicated to improving the care of patients with vascular disease.
According to Megan Patterson, chief executive officer of Vascular Cures, all proceeds from the gala support national education and awareness initiatives that help at-risk populations, patients, and their caregivers. This year’s gala was held virtually on Feb. 3.
Some of the work done through Duke in support of Vascular Cures and honored this year include the following:
Chronic Limb-Threatening Ischemia (CLTI) Research
Manesh Patel, MD and E. Hope Weissler, MD, a resident in our Vascular Surgery Integrated Residency Program,  are members of the Vascular Cures Chronic Limb-Threatening Ischemia (CLTI) Working Group for Patient Engagement, an initiative to promote and facilitate CLTI patient engagement in research. Patel and Weissler comprise half the team responsible for organizing this working group. This initiative is designed to build capacity to engage CLTI patients in research as advisors and participants, so that study results align with the needs of patients. It also works to prioritize the kinds of research that are most important to patients. Ultimately, the goal of this work is to create new knowledge and treatments that more closely align with CLTI patient needs and improve health outcomes in this population.
are members of the Vascular Cures Chronic Limb-Threatening Ischemia (CLTI) Working Group for Patient Engagement, an initiative to promote and facilitate CLTI patient engagement in research. Patel and Weissler comprise half the team responsible for organizing this working group. This initiative is designed to build capacity to engage CLTI patients in research as advisors and participants, so that study results align with the needs of patients. It also works to prioritize the kinds of research that are most important to patients. Ultimately, the goal of this work is to create new knowledge and treatments that more closely align with CLTI patient needs and improve health outcomes in this population.
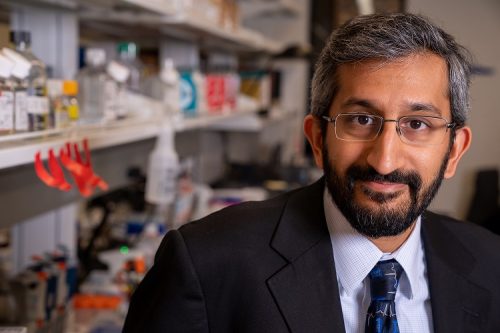
Kevin Southerland, MD, assistant professor of vascular surgery, is the 2021 Wylie Scholar Award recipient for his  project Transcriptional Dynamics and Heterogeneity of Macrophages in Chronic Limb Threatening Ischemia. The award is given annually by the Vascular Cures Foundation and the Society for Vascular Surgery Foundation. Chronic limb-threatening ischemia (CLTI) is the most severe manifestation of peripheral arterial disease. Patients with CLTI are at high risk for limb loss and death. A significant number of CLTI patients suffer limb loss despite successful restoration of arterial flow. Novel approaches to treat CLTI remain an unmet clinical need. The goal of Dr. Southerland’s work is to understand the communication signals between the various cell types in the ischemic limb. He is particularly interested in how macrophages interact with muscle stem cells. He believes that understanding these mechanisms will be the groundwork for the development of new therapies for CLTI patients.
project Transcriptional Dynamics and Heterogeneity of Macrophages in Chronic Limb Threatening Ischemia. The award is given annually by the Vascular Cures Foundation and the Society for Vascular Surgery Foundation. Chronic limb-threatening ischemia (CLTI) is the most severe manifestation of peripheral arterial disease. Patients with CLTI are at high risk for limb loss and death. A significant number of CLTI patients suffer limb loss despite successful restoration of arterial flow. Novel approaches to treat CLTI remain an unmet clinical need. The goal of Dr. Southerland’s work is to understand the communication signals between the various cell types in the ischemic limb. He is particularly interested in how macrophages interact with muscle stem cells. He believes that understanding these mechanisms will be the groundwork for the development of new therapies for CLTI patients.
Patient Reported Outcome Measures in Peripheral Artery Disease (PAD)
Patel and Jennifer Rymer, MD have been instrumental in facilitating the Vascular Cures Working Group on

Patient-Reported Outcome Measures in PAD, which resulted in the recently published (23 Dec 2021) review article in Circulation: Cardiovascular Interventions, “Patient-Reported Outcome Measures in Symptomatic, Non-Limb Threatening Peripheral Artery Disease: A State-of-the-Art Review”.
The Circulate! gala includes the announcement of the recipient of the Ron Stoney Vascular Hero Award which is given annually to an outstanding care provider and/or researcher who goes above and beyond to advocate for patients. Stoney, a surgeon and professor emeritus at UCSF, co-founded Vascular Cures in 1982 to “save and improve the lives of those living with vascular diseases outside the heart.”
This year’s honoree was Manesh Patel, MD.

“Dr. Patel received this award not just because of the incredible support he has provided Vascular Cures as an advisor, but his persistent and passionate commitment to improving vascular health for patients through research and other national initiatives with organizations like the American Heart Association,” says Patterson. “He is a visionary and is always inspiring us to do more and do it better so that more people can have happy healthy lives.”
Congratulations to Hope, Jenn, Kevin and Manesh – well deserved recognition for the work you are doing!
Kelsey Appointed to CAAHEP’s JRC on Education in CV Technology

Congratulations to Anita M. Kelsey, MD, MBA! Kelsey has been appointed as Commissioner for the Joint Review Committee on Education in Cardiovascular Technology (JRC) by the Commission on Accreditation of Allied Health Education Programs (CAAHEP). CAAHEP is the largest programmatic accreditor of the health sciences professions.
Originally established in 1976 by the American Medical Association as the Committee on Allied Health Education and Accreditation (CAHEA) with our own Joseph Kisslo, MD and Kitty B. (Filly) Kisslo (who was then at Stanford) as founding JRC members who led the way in defining the standards of cardiac sonography.
CAAHEP reviews and accredits more than 2100 individual education programs across 32 health science occupations. CAAHEP-accredited programs are assessed on an ongoing basis to ensure they meet the standards and guidelines of each profession.
Duke’s Cardiac Ultrasound Certificate Program received CAAHEP accreditation in 2021. We are proud to be accredited by this organization that upholds the highest standards of quality, outcomes-based education. We are equally as proud of Dr. Kelsey for her new role.
Congratulations Dr. Kelsey, for your work to ensure quality allied health education here at Duke and, now, across the U.S. as part of CAAHEP. Way to go!
Newest HF Collaboratory Members Include Three from Duke Heart
Congratulations to cardiology fellows Vanessa Blumer and Shahzeb Khan, and to former cardiology fellow Jordan Pomeroy! Blumer, Khan and Pomeroy were each asked to join the Heart Failure Collaboratory (HFC), and all were welcomed as new members last week during a quarterly meeting of the HFC’s Drugs and Devices Working Group.
Excellent additions to the Collaboratory!


Paul Farmer, MD & Dzau Distinguished Lecture in Global Health
We were shocked and deeply saddened this week by the passing of Duke alumnus and trustee emeritus Dr. Paul Farmer, who — along with Dr. Agnes Binagwaho, vice chancellor of the University of Global Health Equity in Rwanda — delivered the annual Victor J. Dzau Distinguished Lecture in Global Health on Jan. 26, 2022.
For those who were unable to attend that event (held via Zoom), we share the following article by our colleagues at Duke Global Health Institute. The article includes a link to the lecture: https://globalhealth.duke.edu/news/never-try-save-people-without-them-participating.
Reaction to his passing was swift and widespread. A compilation of moving tributes, including several from members of our Duke Heart team, can be found here: https://globalhealth.duke.edu/news/dghi-reacts-death-dr-paul-farmer
Duke Today’s memorial piece about Farmer is available here: https://duke.is/jmxq6.
ICYMI: Genomic & Precision Medicine Forum
Duke Heart’s Bill Kraus was guest speaker at the Genomic & Precision Medicine Forum sponsored by the Duke Center for Applied Genomics & Precision Medicine on Thursday, Feb. 24. His lecture, “Components of Personalized Lifestyle Medicine with a Focus on Physical Activity” can be viewed here.
Great job, Bill!
Participants in Duke’s PROMOTE Study Hope to Improve Care for Type 2 Diabetes
Joining Duke’s diabetes study in Kannapolis at the N.C. Research Campus was part of Susan Wagner’s commitment to improving the health of her community.
“I have diabetes, and it’s somewhat under control. But I wanted to provide Duke with statistical data that they will need to build a model to address the issues of diabetes in Cabarrus County,” said Wagner, of Concord.
Retired from manufacturing, Wagner, 68, participates in several Duke Clinical and Translational Science Institute (CTSI) studies in Kannapolis, including the PROMOTE study. PROMOTE will assess whether a test product can improve insulin sensitivity in people with Type 2 diabetes.
The study seeks more people like Wagner, who are between the ages of 18 and 70 and are under the care of a healthcare professional for management of their disease.
“This study fit into the bigger picture for me,” she said. “I don’t know if I am getting the placebo or the product, but diabetics in Cabarrus County need data to improve their health.”
Study participation lasts about 15 weeks with six appointments in either Kannapolis or Durham. Participants are randomly assigned to receive either the test product or placebo.
 The PROMOTE team in Kannapolis, led by Duke cardiologist Dr. Kristin Newby, recently expanded the study to a new Duke research facility in Durham. Launched in October 2020, Duke Research at Pickett Road encourages community participation and diversity in clinical research by providing a convenient and comfortable site for study participants and researchers.
The PROMOTE team in Kannapolis, led by Duke cardiologist Dr. Kristin Newby, recently expanded the study to a new Duke research facility in Durham. Launched in October 2020, Duke Research at Pickett Road encourages community participation and diversity in clinical research by providing a convenient and comfortable site for study participants and researchers.
“We are grateful to our study participants for their contributions to answering important healthcare questions,” Newby said. “Diabetes mellitus is such a challenging disease that affects almost every system in the body and can lead to a number of major long-term health consequences. Research into ways to improve management of diabetes is critical to reduce the burden of illness resulting from diabetes mellitus. To this end, we are excited to work with the community to conduct studies like PROMOTE.”
Wagner, who has had Type 2 diabetes since 1995, began focusing on diet and exercise when she took a class at Cabarrus Health Alliance and began reading labels, counting steps, and keeping a daily food log.
As her focus on health grew, Wagner began volunteering at Green Leaf Farms in the garden. She now eats mostly food that she has helped grow, and she’s enjoying relatively good health.
“This is not something that happened overnight,” Wagner said. “Part of this evolution was to join the PROMOTE study, as well as doing things like getting enough sleep and eating correct portions. It’s about expanding your toolbox.”
Like Wagner, Rosa Dorantes has Type 2 diabetes and participates in several Duke studies in Kannapolis. She 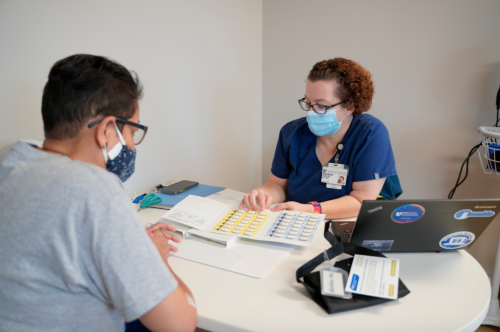 joined PROMOTE after returning home to Granite Quarry from Mexico, where she had cared for a loved one who eventually passed away from complications due to diabetes.
joined PROMOTE after returning home to Granite Quarry from Mexico, where she had cared for a loved one who eventually passed away from complications due to diabetes.
Her family history of diabetes, and witnessing the devastating effects of the disease if untreated, motivated Dorantes to begin participating in clinical research seven years ago.
“I never thought that I would be a research participant, but it is important to me to help other people by helping researchers find new medicines,” said Dorantes, 56. “People are suffering.”
Dorantes, who works for her daughter’s diaper service in Charlotte, said she has improved her health by eating well and staying active. When her PROMOTE appointments are complete, she plans to keep enrolling in new studies.
“We are regular people,” she said. “For me to be able to do something like this, to perhaps save a life or help find a new medicine to help people, I can say I did something good during my journey.”
People who want to learn whether they qualify for PROMOTE can call 704-273-5456, email mailto:TransPop@duke.edu or visit duketranspop.org/promote. Compensation is provided for completed study activities.
To learn more about the Duke CTSI clinical research facility in Kannapolis, visit https://ctsi.duke.edu/research-support/duke-kannapolis. To learn more about Duke CTSI, visit ctsi.duke.edu.
COVID-19 Updates
The COVID-19 Employee Hotline hours are changing to reflect recent utilization trends. Beginning March 1, the hotline will be available during these times:
- Monday — Friday: 8 a.m. to 5 p.m.
- Saturday — Sunday: 8 a.m. to 12 p.m.
The phone number for the hotline is 919-385-0429 (option 1).
All the latest Clinical Operations updates related to COVID can be found at https://covid-19.dukehealth.org.
Upcoming Events & Opportunities
Cardiology Grand Rounds
March 1: Toward Allograft Longevity: Leveraging Multiomic Approaches to Understand Biomarkers and Biology of Heart Transplant Outcomes with Lauren Truby. 5 p.m. via Webex.
Duke Research & Innovation Virtual Conference
March 3 & March 4: The Evolving Role of Universities in the American Innovation System
 Duke Research & Innovation is proud to co-sponsor The Evolving Role of Universities in the American Innovation System, a two-day virtual conference discussing the role of university research in the U.S. innovation ecosystem.
Duke Research & Innovation is proud to co-sponsor The Evolving Role of Universities in the American Innovation System, a two-day virtual conference discussing the role of university research in the U.S. innovation ecosystem.
Hosted by the Center for Innovation Policy at Duke Law, this conference aims to outline a new framework for America’s universities in the context of the country’s long-term competitive future and features five presidents from five major universities, including Duke’s very own President Price.
The conference kicks off next Thursday, March 3rd and is open to everyone. Registration is required.
Upcoming Duke Heart CME
April 23: Duke Sports Cardiology & Sudden Death in Athletes Symposium with course directors Jim Daubert and Bill Kraus. Virtual. For information or to register, contact Christy Darnell christy.darnell@duke.edu or 919-880-8686.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
February 17 — Christopher Granger
HCPLive
Multifaceted Therapy Interventions Suggested for Patients with Diabetes, ASCVD
https://duke.is/nerg3
February 17 — Kristin Newby
WBTV.com (Charlotte, NC)
Participants in Duke’s PROMOTE study in Kannapolis hope to improve care for Type 2 diabetes
https://duke.is/bxx9c
February 19 — Kristin Newby
Independent Tribune
Participants in Duke’s PROMOTE study hope to improve care for Type 2 diabetes
https://duke.is/2cnjj
February 19 — Christopher Granger
Medscape
Full-press Therapy Rare in Diabetes With ASCVD
https://duke.is/48mqn
February 22 — Duke Health
Advisory Board
Update: The ‘Best Employers’ in health care, according to Forbes
https://duke.is/95myg
February 24 — Duke University
Forbes.com
Johns Hopkins Tops List Of Leading Universities For NIH Funding In 2021
https://duke.is/4ggpc
February 28 — Allan Kirk
The New Yorker
The Medical Miracle of a Pig’s Heart in a Human Body
https://duke.is/9phm8
Division of Cardiology Publications Indexed in PubMed February 17-23, 2022
Bodkin N, Ross M, McClain MT, Ko ER, Woods CW, Ginsburg GS, Henao R, Tsalik EL. Systematic comparison of published host gene expression signatures for bacterial/viral discrimination. Genome Med 2022;14(1):18. PM: 35184750.
Fanaroff AC, Lopes RD. The role of triple antithrombotic therapy in patients with atrial fibrillation undergoing percutaneous coronary intervention. Prog Cardiovasc Dis 2021;69:11-17. PM: 34883097.
Fanaroff AC, Vora AN, Lopes RD. Non-vitamin K antagonist oral anticoagulants in patients with valvular heart disease. Eur Heart J Suppl 2022;24(Suppl A):A19-A31. PM: 35185406.
Kam W, Holmes DN, Hernandez AF, Saver JL, Fonarow GC, Smith EE, Bhatt DL, Schwamm LH, Reeves MJ, Matsouaka RA, Khan YM, Unverdorben M, Birmingham MC, Lyden PD, Asimos AW, Altschul D, Schoonover TL, Jumaa MA, Nomura JT, Suri MFK, Moore SA, Lafranchise EF. Association of Recent Use of Non-Vitamin K Antagonist Oral Anticoagulants With Intracranial Hemorrhage Among Patients With Acute Ischemic Stroke Treated With Alteplase. JAMA 2022;327(8):760-771. PM: 35143601.
Lam CSP, Ramasundarahettige C, Branch KRH, Sattar N, Rosenstock J, Pratley R, Del Prato S, Lopes RD, Niemoeller E, Khurmi NS, Baek S, Gerstein HC. Efpeglenatide and Clinical Outcomes With and Without Concomitant Sodium-Glucose Cotransporter-2 Inhibition Use in Type 2 Diabetes: Exploratory Analysis of the AMPLITUDE-O Trial. Circulation 2022;145(8):565-574. PM: 34775781.
Lau ES, Binek A, Parker SJ, Shah SH, Zanni MV, Van Eyk JE, Ho JE. Sexual Dimorphism in Cardiovascular Biomarkers: Clinical and Research Implications. Circ Res 2022;130(4):578-592. PM: 35175850.
Nelson AJ, O’Brien EC, Kaltenbach LA, Green JB, Lopes RD, Morse CG, Al-Khalidi HR, Aroda VR, Cavender MA, Gaynor T, Kirk JK, Lingvay I, Magwire ML, McGuire DK, Pak J, Pop-Busui R, Richardson CR, Senyucel C, Kelsey MD, Pagidipati NJ, Granger CB. Use of Lipid-, Blood Pressure-, and Glucose-Lowering Pharmacotherapy in Patients With Type 2 Diabetes and Atherosclerotic Cardiovascular Disease. JAMA Netw Open 2022;5(2):e2148030. PM: 35175345.
Pasquali SK, Thibault D, Hall M, Chiswell K, Romano JC, Gaynor JW, Shahian DM, Jacobs ML, Gaies MG, O’Brien SM, Norton EC, Hill KD, Cowper PA, Shah SS, Mayer JE, Jacobs JP. Evolving Cost-Quality Relationship in Pediatric Heart Surgery. Ann Thorac Surg 2022;113(3):866-873. PM: 34116004.
Peters AE, Mentz RJ, DeWald TA, Greene SJ. An evaluation of torsemide in patients with heart failure and renal disease. Expert Rev Cardiovasc Ther 2022;20(1):5-11. PM: 34936522.
Russo JJ, Yan AT, Pocock SJ, Brieger D, Owen R, Sundell KA, Bagai A, Granger CB, Cohen MG, Yasuda S, Nicolau JC, Brandrup-Wognsen G, Westermann D, Simon T, Goodman SG. Determinants of long-term dual antiplatelet therapy use in post myocardial infarction patients: Insights from the TIGRIS registry. J Cardiol 2022;79(4):522-529. PM: 34857432.
Utz PJ, Jain MK, Cheung VG, Kobilka BK, Lefkowitz R, Yamada T, Dzau VJ. Translating science to medicine: The case for physician-scientists. Sci Transl Med 2022;14(632):eabg7852. PM: 35171650.
Welsh RC, Dehghani P, Lopes R, Wojdyla DM, Aronson R, Granger CB, Windecker S, Vora AN, Vinereanu D, Halvorsen S, Parkhomenko A, Mehran R, Alexander JH, Goodman S. Impact of prior oral anticoagulant use and outcomes on patients from secondary analysis in the AUGUSTUS trial. Open Heart 2022;9(1):e001892. PM: 35172988.
Wilson RJ, Lyons SP, Koves TR, Bryson VG, Zhang H, Li T, Crown SB, Ding JD, Grimsrud PA, Rosenberg PB, Muoio DM. Disruption of STIM1-mediated Ca sensing and energy metabolism in adult skeletal muscle compromises exercise tolerance, proteostasis, and lean mass. Mol Metab 2022;57:101429. PM: 34979330.
Wu JH, Zhang L, Nepliouev I, Brian L, Huang T, Snow KP, Schickling BM, Hauser ER, Miller FJ, Freedman NJ, Stiber JA. Drebrin attenuates atherosclerosis by limiting smooth muscle cell transdifferentiation. Cardiovasc Res 2022;118(3):772-784. PM: 33914863.
Zeitler EP, Poole JE, Albert CM, Al-Khatib SM, Ali-Ahmed F, Birgersdotter-Green U, Cha YM, Chung MK, Curtis AB, Hurwitz JL, Lampert R, Sandhu RK, Shaik F, Sullivan E, Tamirisa KP, Santos Volgman A, Wright JM, Russo AM. Arrhythmias in Female Patients: Incidence, Presentation and Management. Circ Res 2022;130(4):474-495. PM: 35175839
Duke Heart Pulse Week ending February 20th 2022
Highlights of the week:
Califf Confirmed as Commissioner for the FDA
 Robert M. Califf, MD, Duke University adjunct professor of medicine (cardiology) and former director of the Duke Clinical Research Institute (DCRI), has been confirmed as commissioner for the U.S. Food and Drug Administration following a vote by the Senate on Tuesday, Feb. 15. Califf’s appointment to the position will mark his second time heading the agency, which he also led during the final year of former President Barack Obama’s administration.
Robert M. Califf, MD, Duke University adjunct professor of medicine (cardiology) and former director of the Duke Clinical Research Institute (DCRI), has been confirmed as commissioner for the U.S. Food and Drug Administration following a vote by the Senate on Tuesday, Feb. 15. Califf’s appointment to the position will mark his second time heading the agency, which he also led during the final year of former President Barack Obama’s administration.
Califf was nominated to the post by President Joe Biden in November of 2021. His confirmation was hailed by his colleagues in the world of clinical research and academic medicine.
“Dr. Califf is the ideal choice to lead the FDA at this critical time,” said Mary E. Klotman, MD, dean of the Duke University School of Medicine. “He brings extraordinary experience and wisdom. I’m so appreciative of his willingness to serve our country again.”
“There’s no question that Rob Califf is the perfect fit for this job at this moment,” said Duke cardiologist and current executive director of the DCRI Adrian Hernandez, MD, a longtime colleague of Califf’s. “He has the background, the skills, the knowledge, and the personal integrity to lead the FDA at a critically important time.”
The nomination also garnered swift support from six former FDA Commissioners, who in a joint letter to the Senate confirmation committee praised Califf’s “lifelong commitment to leadership in promoting public health and advancing clinical science” and noted that his previous experience as commissioner would allow him to be uniquely well prepared to be “effective from day one.”
Califf’s new tenure at the FDA is likely to be marked by what many of his supporters consider one of his key strengths: a combination of enthusiasm and expertise applied to the task of developing scientific evidence that can be used to create better therapies and guide more informed decision-making by clinicians and patients.
That enthusiasm has long been a hallmark of Califf’s work at Duke, where he established a global reputation as an innovative and highly knowledgeable expert in clinical trials, particularly large, complex, and logistically challenging international studies.
“Rob has been a major force in establishing Duke as a leader in clinical and translational research on the world stage,” said A. Eugene Washington, MD, chancellor for health affairs at Duke University and president and CEO of Duke University Health System. “His exceptional leadership and unwavering commitment to evidence-based medicine and to the health and welfare of patients have driven us to higher levels of excellence and impact. His contributions have no doubt improved the lives of millions here and around the world, making Rob uniquely qualified to take on this pivotal role during these unprecedented times.”
Califf’s history at Duke stretches back to his undergraduate years in the early 1970s, when he majored in psychology. He went on to earn his medical degree from Duke, and aside from three years of residency in internal medicine at the University of California, San Francisco, Califf spent his entire career as cardiologist, researcher and senior leader at Duke until leaving in 2015 to assume the posts of deputy commissioner and later commissioner at the FDA.
During his medical training at Duke, Califf was mentored by Dr. Eugene Stead, Jr., a cardiologist and chair of Duke’s Department of Medicine. An early pioneer in the use of computer technology, Stead influenced Califf’s focus on gathering and analyzing data on patient outcomes. Stead’s mentorship would ignite Califf’s lifelong interest in the potential for combining computer technology with clinical data to answer important questions about medicine and patient care. That passion would ultimately lead to the creation of the Duke Clinical Research Institute, one of the world’s leading academic clinical research organizations. As the founding director of the DCRI, Califf oversaw and in many cases personally led numerous pivotal trials in cardiology and other medical specialties.
Despite the demands of his career in clinical research, throughout his decades at Duke, Califf continued to see patients as a working cardiologist. He distinguished himself as a teacher and mentor, helping to shape a new generation of physicians and clinical researchers.
After stepping down from his leadership post at the DCRI in 2006, Califf served as vice chancellor for clinical and translational research at Duke before moving to the FDA. Shortly afterward, Obama nominated him as commissioner and the Senate confirmed him in early 2016. Califf’s time at the helm of FDA was marked by efforts to update the agency’s approach to evaluating scientific evidence about the safety and effectiveness of medical products. In particular, this included developing a framework for incorporating new sources of data, including information gathered from sources such as electronic health records and administrative databases.
After leaving the FDA in early 2017, Califf returned briefly to Duke to create and lead Duke Forge, a university center for health data science, before transitioning in 2019 to a leadership role as senior adviser at Verily Life Sciences, a Google-affiliated company focused on health data. He will step down from that role to assume his new position as FDA chief.
“It’s hard for me to think of anyone who would be better prepared to lead the FDA, given the scope of Rob’s experience in patient care, research, and policy,” said Amy Abernethy, MD, PhD, president of Verily’s clinical research business and a former Duke professor of medicine who served as principal deputy commissioner and acting chief information officer at the FDA from February 2019 to April 2021. “And the fact that he’s led the FDA effectively before means that he’ll be able to get to work immediately on the most pressing issues on the agency’s to-do list. There’s no question that Rob will be prepared to hit the ground running.”
ADAPTABLE Team Selected for CR Forum Achievement Award
The Clinical Research (CR) Forum, a nonprofit organization dedicated to promoting understanding and support for clinical research and its impact on health and health care, has selected the ADAPTABLE study as a Top 10 Clinical Research Achievement Awardee for 2022. The awards recognize outstanding achievements in clinical research from across the U.S., identifying major advances in the biomedical field resulting from the nation’s investment in health and welfare.
The CR Forum will honor the ADAPTABLE research team on April 19 at a ceremony to be held at the Hyatt Regency McCormick Place in Chicago. The team will then present at Translational Science 2022 and meet with members of the U.S. Congress to promote the importance of funding for clinical research.
The CR Forum will present this award to Duke interventional cardiologist Schuyler Jones, MD, ADAPTABLE’s

principal investigator, member of the Duke Clinical Research Institute and the lead author of the results paper, which was simultaneously published in the New England Journal of Medicine and presented at the 70th annual American College of Cardiology Scientific Session & Expo.
A pragmatic, open-label, patient-centered, randomized clinical trial, ADAPTABLE sought to determine the safest and most effective dose of aspirin for patients with existing cardiovascular disease. Despite aspirin being used as a secondary prevention method for nearly three decades, this question had not been studied previously.
Beginning in 2016, ADAPTABLE randomized 15,076 people with existing cardiovascular disease to receive either baby aspirin (81 mg) or regular strength aspirin (325 mg). Ultimately, investigators found no significant difference in either protective effects or bleeding risk between the two doses. However, the patients in the group taking the lower dose were less likely to switch doses mid-study; furthermore, that group’s patients were slightly less likely to discontinue aspirin completely.
Congratulations, Schuyler and team!
Early Exercise Interventions Used from Duke Trial to Decrease Cardiovascular Disease
With 2022 underway and the pandemic continuing, health and prevention of disease continues to be of the upmost importance. Physical activity has been shown to not only improve health, but help prevent the onset of many disorders – including cardiovascular disease.
 Duke cardiologist William Kraus, MD, the Richard and Pat Johnson University Distinguished Professor at Duke University School of Medicine, a researcher and affiliated faculty for the Duke Center for Applied Genomics & Precision Medicine (CAGPM), is studying exercise effects in individuals ranging from healthy to those at-risk of disease and those with disease, such as coronary heart disease.
Duke cardiologist William Kraus, MD, the Richard and Pat Johnson University Distinguished Professor at Duke University School of Medicine, a researcher and affiliated faculty for the Duke Center for Applied Genomics & Precision Medicine (CAGPM), is studying exercise effects in individuals ranging from healthy to those at-risk of disease and those with disease, such as coronary heart disease.
For the last 35 years, the Kraus laboratory particularly focuses on increased physical activity as the means by which to prevent premature cardiovascular death. Kraus’ well-known randomized exercise trials – STRRIDE (Studies of a Targeted Risk Reduction Intervention through Defined Exercise) are being used to investigate genetic predictors associated with individuals dropping out from or adherence to an exercise intervention. Postdoc Katherine Collins, PhD, is a research assistant in the Kraus Lab part of this endeavor, through the CAGPM T32 fellowship.
Specifically, Kraus Lab is currently working on a project using data from the STRRIDE trial to undertake the project, “Molecular Predictors of Dropout from and Adherence to Lifestyle Interventions.” The team has identified multiple variants within an array of genes associated with an individual’s ability to adhere to — or lack of ability to adhere to (i.e. dropout) — the STRRIDE exercise interventions. During her fellowship, Dr. Collins’ goal is to validate findings Kraus and his team have made to identify genetic variants associated with dropout and adherence to the randomized exercise trials. The team has investigated potential mediators of the genetic association with intervention dropout. During Collins’ time as a T32 fellow, she has been a valuable contributor to the project, bringing biospecimens from a 12-month behavioral weight loss randomized trial and utilizing data from the 2-year caloric restriction dietary intervention – CALERIE™ (Comprehensive Assessment of Long-term Effects of Reducing Intake of Energy) trial to further investigate Dr. Kraus’ initial findings.
“The CAGPM T32 fellowship has provided me hands-on experience, under the mentorship of Dr. Kraus, in human clinical trials, bio-banking, developing human samples into bio-molecular data, and human translational research as a whole,” said Collins. “This fellowship has helped me establish a foundation for my future research endeavors around precision medicine approaches in exercise and lifestyle interventions.”
These findings will help guide future interventions and help identify those individuals who may be most at-risk or prone to dropout or have poor adherence to exercise. The overarching goal of this investigation is to develop a personalized medicine approach for exercise, giving interventionists the ability to target at-risk individuals early in the invention process, pushing them past the key dropout phase—the initial 2 months—of the exercise intervention.
“We know physical activity is good and anything is better than none and more is better than less,” said Kraus. “However, the responses to physical activity and exercise are individually different, partly mediated by genetic factors. The tendency to engage in and maintain regular physical activity patterns are mediated by a combination of personality and genetic factors.”
Lack of physical activity is an ongoing public health concern. This is contributing to heart disease, even for people that have no risk factors, while also increasing the rates of obesity, diabetes, high blood pressure, and more.
“Outside of communicable diseases, cardiovascular disease remains the number one cause of premature death in the US and the World,” said Kraus. “The spectrum of cardiometabolic risk factors—hypertension, abnormal blood lipids and diabetes—are, separately and combined, the major non-lifestyle risk factor contributors to cardiovascular risk. Smoking, the lack of physical activity, and poor diets are the major lifestyle-related risk factors which also contribute to worsening hypertension, lipids and diabetes.”
Studies like these ultimately aim to help individuals maintain active lifestyles long-term.
Many of these issues will be addressed during the Genomic & Precision Medicine Forum being held February 24, where Kraus will be presenting on “Components of Personalized Lifestyle Medicine with a Focus on Physical Activity.” Learn more and register to attend the virtual talk on Zoom.
Kudos to Spates!
Cardiology fellow Toi Spates presented an excellent grand rounds this past week on the management of pregnancy and heart disease. Further, she did an interview on a related topic with CBS-17 (WNCN), see link below under “news”.
Nicely done!

COVID-19 Updates
All the latest Clinical Operations updates related to COVID can be found at https://covid-19.dukehealth.org.
Upcoming Events & Opportunities
Cardiology Grand Rounds
March 1: Lipoprotein (a): Unveiling the Mysterious Biomarker. Presenter will be Nishant Shah. 5 p.m. via Webex. Link will be sent via email.
Duke Genomic & Precision Medicine Forum Series
February 24: Guest will be William E. Kraus, MD speaking on Components of Personalized Lifestyle Medicine with a Focus on Physical Activity. Noon – 1 p.m. via Zoom. Sponsored by Duke Center for Applied Genomics & Precision Medicine. Registration is required; event is free. To learn more and to register, please visit: https://bit.ly/3ouqDiK.
Upcoming Duke Heart CME
April 23: Duke Sports Cardiology & Sudden Death in Athletes Symposium with course directors Jim Daubert and Bill Kraus. Virtual. For information or to register, contact Christy Darnell christy.darnell@duke.edu or 919-880-8686.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
February 11 — Tracy Wang
The Science Times
Gestational Diabetes Linked to Chronic Cardiovascular Outcome Later in Life
https://duke.is/cwaa8
February 11 — Duke University Health System
Becker’s Hospital Review
48 hospitals on Forbes’ list of best employers
https://duke.is/wz8ez
February 13 — Stuart Russell
WPTF AM-640/Podcast
Aging Matters: Heart Failure 101
https://duke.is/4w5w4
February 15 — Toi Spates
WNCN CBS-17
Most women giving birth in the US have poor heart health before pregnancy
https://duke.is/9zj9w
February 17 — Adrian Hernandez
WNCN CBS-17
Duke doctors testing whether more ivermectin for twice as long will work against COVID-19
https://duke.is/wxmgt
Division of Cardiology Publications Indexed in PubMed February 10-16, 2022
Bhasin S, Lincoff AM, Basaria S, Bauer DC, Boden WE, Cunningham GR, Davey D, Dubcenco E, Fukumoto S, Garcia M, Granger CB, Kalahasti V, Khera M, Miller MG, Mitchell LM, O’Leary MP, Pencina KM, Snyder PJ, Thompson IM, Travison TG, Wolski K, Nissen SE. Effects of long-term testosterone treatment on cardiovascular outcomes in men with hypogonadism: Rationale and design of the TRAVERSE study. Am Heart J 2022;245:41-50. PM: 34871580.
Bhatt DL, Lopes RD, Harrington RA. Diagnosis and Treatment of Acute Coronary Syndromes: A Review. JAMA 2022;327(7):662-675. PM: 35166796.
Bloomfield GS, Weir IR, Ribaudo HJ, Fitch KV, Fichtenbaum CJ, Moran LE, Bedimo R, de Filippi C, Morse CG, Piccini J, Zanni MV, Lu MT, Hoffmann U, Grinspoon SK, Douglas PS. Prevalence and Correlates of Electrocardiographic Abnormalities in Adults With HIV: Insights From the Randomized Trial to Prevent Vascular Events in HIV (REPRIEVE). J Acquir Immune Defic Syndr 2022;89(3):349-359. PM: 35147583.
Bozkurt B, Hill JA, Al-Khatib SM. Sixth Annual Go Red for Women Issue. Circulation 2022;145(7):489-490. PM: 35157526.
Cardoso R, Ternes CMP, Justino GB, Fernandes A, Rocha AV, Knijnik L, d’Avila A, Lopes RD. Non-Vitamin K Antagonists Versus Warfarin in Patients with Atrial Fibrillation and Bioprosthetic Valves: A Systematic Review and Meta-Analysis. Am J Med 2022;135(2):228-234. PM: 34634252.
Carnicelli AP, Blumer V, Genovese L, Gage A, Agarwal R, Lakdawala NK, Bohula E, Katz JN. The Road Not Yet Traveled: Distinction in Critical Care Cardiology through the Advanced Heart Failure and Transplant Cardiology Training Pathway. J Card Fail 2022;28(2):339-342. PM: 35148880.
Carnicelli AP, Clare RM, Hofmann P, Chiswell K, DeVore AD, Vemulapalli S, Felker GM, Kelsey AM, DeWald TA, Sarocco P, Mentz RJ. Clinical trajectory of patients with a worsening heart failure event and reduced ventricular ejection fraction. Am Heart J 2022;245:110-116. PM: 34932997.
Chan PS, Spertus JA, Kennedy K, Nallamothu BK, Starks MA, Girotra S. In-Hospital Cardiac Arrest Survival in the United States During and After the Initial Novel Coronavirus Disease 2019 Pandemic Surge. Circ Cardiovasc Qual Outcomes 2022;15(2):e008420. PM: 35098727.
Chew DS, Li Y, Zeitouni M, Whellan DJ, Kitzman D, Mentz RJ, Duncan P, Pastva AM, Reeves GR, Nelson MB, Chen H, Reed SD. Economic Outcomes of Rehabilitation Therapy in Older Patients With Acute Heart Failure in the REHAB-HF Trial: A Secondary Analysis of a Randomized Clinical Trial. JAMA Cardiol 2022;7(2):140-148. PM: 34817542.
Chew DS, Li Z, Steinberg BA, O’Brien EC, Pritchard J, Bunch TJ, Mark DB, Patel MR, Nabutovsky Y, Greiner MA, Piccini JP. Arrhythmic Burden and the Risk of Cardiovascular Outcomes in Patients With Paroxysmal Atrial Fibrillation and Cardiac Implanted Electronic Devices. Circ Arrhythm Electrophysiol 2022;15(2):e010304. PM: 35089799.
Chiarito M, Baber U, Cao D, Sharma SK, Dangas G, Angiolillo DJ, Briguori C, Cohen DJ, Dudek D, Džavík V, Escaned J, Gil R, Hamm CW, Henry T, Huber K, Kastrati A, Kaul U, Kornowski R, Krucoff M, Kunadian V, Mehta SR, Moliterno D, Ohman EM, Oldroyd K, Sarde. Ticagrelor Monotherapy After PCI in High-Risk Patients With Prior MI: A Prespecified TWILIGHT Substudy. JACC Cardiovasc Interv 2022;15(3):282-293. PM: 35033468.
Echouffo-Tcheugui JB, Mwasongwe SE, Musani SK, Hall ME, Correa A, Hernandez AF, Golden SH, Mentz RJ, Bertoni AG. Dysglycemia and incident heart failure among blacks: The jackson heart study. Am Heart J 2022;245:1-9. PM: 34808103.
Ekerstad N, Javadzadeh D, Alexander KP, Bergström O, Eurenius L, Fredrikson M, Gudnadottir G, Held C, Ängerud KH, Jahjah R, Jernberg T, Mattsson E, Melander K, Mellbin L, Ohlsson M, Ravn-Fischer A, Svennberg L, Yndigegn T, Alfredsson J. Clinical Frailty Scale classes are independently associated with 6-month mortality for patients after acute myocardial infarction. Eur Heart J Acute Cardiovasc Care 2022;11(2):89-98. PM: 34905049.
Fordyce CB, Giugliano RP, Cannon CP, Roe MT, Sharma A, Page C, White JA, Lokhnygina Y, Braunwald E, Blazing MA. Cardiovascular Events and Long-Term Risk of Sudden Death Among Stabilized Patients After Acute Coronary Syndrome: Insights From IMPROVE-IT. J Am Heart Assoc 2022;11(4):e022733. PM: 35112882.
Fulda ES, Fitch KV, Overton ET, Zanni MV, Aberg JA, Currier JS, Lu MT, Malvestutto C, Fichtenbaum CJ, Martinez E, Umbleja T, Douglas PS, Ribaudo HJ, Grinspoon SK. COVID-19 Vaccination Rates in a Global HIV Cohort. J Infect Dis 2022;225(4):603-607. PM: 34794178.
Gibson CM, Mack MJ, Lee VT, Schneider DJ, Sellke FW, Ohman EM, Thourani VH, Doros G, Kroger H, Cutlip DE, Deliargyris EN. Rationale and design of the safe and timely antithrombotic removal – ticagrelor (STAR-T) trial: A prospective, multi-center, double-blind, randomized controlled trial evaluating reductions in postoperative bleeding with intraoperative removal of ticagrelor. Am Heart J 2022;245:19-28. PM: 34736855.
Granger BB, Tulsky JA, Kaufman BG, Clare RM, Anstrom K, Mark DB, Johnson KA, Patel CB, Fiuzat M, Steinhauser K, O’Connor C, Rogers JG, Mentz RJ. Polypharmacy in Palliative Care for Advanced Heart Failure: The PAL-HF Experience. J Card Fail 2022;28(2):334-338. PM: 34628013.
Gutierrez JA, Christian RT, Aday AW, Gu L, Schulteis RD, Shihai L, Petrini M, Sun AY, Swaminathan RV, Katzenberger DR, Banerjee S, Rao SV. Electronic alerts to initiate anticoagulation dialogue in patients with atrial fibrillation. Am Heart J 2022;245:29-40. PM: 34808105.
Harrington J, Felker GM. Leveraging Multiple Biomarkers to Assess Risk of Acute Heart Failure: Is More Better? J Card Fail 2022;28(2):234-236. PM: 34952784.
Harrington J, Gouda P, Ezekowitz J, Mentz RJ. Exploring the pragmatic-explanatory spectrum across cardiovascular clinical trials. Contemp Clin Trials 2022;113:106646. PM: 34863929.
Hirji SA, Sabatino ME, Minhas AMK, Okoh AK, Fudim M, Vaduganathan M, Khan MS. Contemporary Nationwide Heart Transplantation and Left Ventricular Assist Device Outcomes in Patients with Histories of Bariatric Surgery. J Card Fail 2022;28(2):330-333. PM: 34509598.
Lala A, Mentz RJ. Heart Month – A Historical Look and Simple “Walk” of Acknowledgement in the Present. J Card Fail 2022;28(2):169-170. PM: 35148879.
Mac Grory B, Ohman EM, Feng W, Xian Y, Yaghi S, Kamel H, Reznik ME. Advances in the management of cardioembolic stroke associated with patent foramen ovale. BMJ 2022;376:e063161. PM: 35140114.
Megaly M, Buda K, Alaswad K, Brilakis ES, Dupont A, Naidu S, Ohman M, Napp LC, O’Neill W, Basir MB. Comparative Analysis of Patient Characteristics in Cardiogenic Shock Studies: Differences Between Trials and Registries. JACC Cardiovasc Interv 2022;15(3):297-304. PM: 35144785.
Nanna MG, Vemulapalli S, Fordyce CB, Mark DB, Patel MR, Al-Khalidi HR, Kelsey M, Martinez B, Yow E, Mullen S, Stone GW, Ben-Yehuda O, Udelson JE, Rogers C, Douglas PS. The prospective randomized trial of the optimal evaluation of cardiac symptoms and revascularization: Rationale and design of the PRECISE trial. Am Heart J 2022;245:136-148. PM: 34953768.
Nathan AS, Yang L, Yang N, Eberly LA, Khatana SAM, Dayoub EJ, Vemulapalli S, Julien H, Cohen DJ, Nallamothu BK, Baron SJ, Desai ND, Szeto WY, Herrmann HC, Groeneveld PW, Giri J, Fanaroff AC. Racial, Ethnic, and Socioeconomic Disparities in Access to Transcatheter Aortic Valve Replacement Within Major Metropolitan Areas. JAMA Cardiol 2022;7(2):150-157. PM: 34787635.
Piccini JP, Ahlsson A, Dorian P, Gillinov MA, Kowey PR, Mack MJ, Milano CA, Perrault LP, Steinberg JS, Waldron NH, Adams LM, Bharucha DB, Brin MF, Ferguson WG, Benussi S. Design and Rationale of a Phase 2 Study of NeurOtoxin (Botulinum Toxin Type A) for the PreVention of Post-Operative Atrial Fibrillation – The NOVA Study. Am Heart J 2022;245:51-59. PM: 34687654.
Rao VN, Kelsey MD, Blazing MA, Pagidipati NJ, Fortin TA, Fudim M. Unexplained Dyspnea on Exertion: The Difference the Right Test Can Make. Circ Heart Fail 2022;15(2):e008982. PM: 35038884.
Sheehy S, Fonarow GC, Holmes DN, Lewis WR, Matsouaka RA, Piccini JP, Zhi L, Bhatt DL. Seasonal Variation of Atrial Fibrillation Admission and Quality of Care in the United States. J Am Heart Assoc 2022;11(4):e023110. PM: 35156386.
Ullal AJ, Holmes DN, Lytle BL, Matsouaka RA, Sheng S, Desai NR, Curtis AB, Fang MC, McCabe PJ, Fonarow GC, Russo AM, Lewis WR, Heidenreich PA, Piccini JP, Turakhia MP, Perino AC. Achievement and quality measure attainment in patients hospitalized with atrial fibrillation: Results from The Get With The Guidelines – Atrial Fibrillation (GWTG-AFIB) registry. Am Heart J 2022;245:90-99. PM: 34932998.
Vaduganathan M, Fonarow GC, Greene SJ, Devore AD, Albert NM, Duffy CI, Hill CL, Patterson JH, Spertus JA, Thomas LE, Williams FB, Hernandez AF, Butler J. Treatment Persistence of Renin-Angiotensin-Aldosterone-System Inhibitors Over Time in Heart Failure with Reduced Ejection Fraction. J Card Fail 202;28(2):191-201. PM: 34428591.
Vemulapalli S, Kerr MSD, Roberts GJ, Prillinger JB, Meduri CU, McCarthy P. Tricuspid valve disease prevalence and the impact of tricuspid valve surgery on cardiovascular events and hospital resource use in medicare beneficiaries. Am Heart J 2022;245:100-109. PM: 34932999.
Weissler EH, Ford CB, Narcisse DI, Lippmann SJ, Smerek MM, Greiner MA, Hardy NC, O’Brien B, Sullivan RC, Brock AJ, Long C, Curtis LH, Patel MR, Jones WS. Clinician Specialty, Access to Care, and Outcomes Among Patients with Peripheral Artery Disease. Am J Med 2022;135(2):219-227. PM: 34627781.
Duke Heart Pulse week ending February 13th 2022
Shah Named Director of Duke Kannapolis Research
 The Duke Clinical and Translational Science Institute (CTSI) this week announced Svati Shah, MD, MHS, professor of medicine in cardiology at Duke, as the new director of Duke Kannapolis Research. In this role, she will direct all activities and projects based at the Duke CTSI clinical research facility in Kannapolis, including ongoing leadership of the Duke Project Baseline initiative — a collaboration with Verily Life Sciences — and assuming leadership of the MURDOCK Study and all associated programs.
The Duke Clinical and Translational Science Institute (CTSI) this week announced Svati Shah, MD, MHS, professor of medicine in cardiology at Duke, as the new director of Duke Kannapolis Research. In this role, she will direct all activities and projects based at the Duke CTSI clinical research facility in Kannapolis, including ongoing leadership of the Duke Project Baseline initiative — a collaboration with Verily Life Sciences — and assuming leadership of the MURDOCK Study and all associated programs.
Shah is an Associate Dean for Genomics in the Duke University School of Medicine, where she is also Director of the Precision Genomics Collaboratory, Director of the Adult Cardiovascular Genetics Clinic, and the Vice-Chief of Translational Research in the Division of Cardiology.
Shah is a physician scientist and practicing cardiologist who sees patients and families with cardiovascular genetic disorders. She earned a Master of Health Science degree in epidemiology from Johns Hopkins School of Public Health and a master’s degree in Medical Genomics from Duke University, and she completed a research fellowship in genetic epidemiology at the Duke Center for Human Genetics.
Her research laboratory focuses on the molecular epidemiology of cardiometabolic diseases, using integrated omics technologies including genomics and metabolomics, to identify novel biomarkers and mechanisms of disease pathogenesis.
Shah brings a wealth of experience to her new role as Director of Duke Kannapolis Research, including her internationally recognized expertise in omics, precision medicine, and population health. Her leadership will move Duke Kannapolis forward with a renewed vision in these areas while leveraging a number of partnerships both internal and external to Duke, as well as the vital partnership with our community in Kannapolis and Cabarrus County.
Congratulations, Svati!!
Rajagopal Elected to ASCI
 The American Society for Clinical Investigation (ASCI) this week announced the election of 95 new members for 2022. Among them, Sudarshan Rajagopal, MD, PhD, associate professor of medicine in cardiology at Duke and member of the Duke Cardiovascular Research Center.
The American Society for Clinical Investigation (ASCI) this week announced the election of 95 new members for 2022. Among them, Sudarshan Rajagopal, MD, PhD, associate professor of medicine in cardiology at Duke and member of the Duke Cardiovascular Research Center.
ASCI’s new members come from 46 different institutions and represent excellence across the breadth of academic medicine. They will be officially inducted into the Society at the ASCI Dinner and New Member Induction Ceremony on April 8, 2022, as part of the AAP/ASCI/APSA Joint Meeting planned for April 8-10 at the Swissotel Chicago.
For the 2022 membership nomination cycle, the Council considered 227 nominations and recommended 95 nominees for election.
Congratulations, Sudar. Well deserved!
USNWR Ratings vs Outcomes Data Presented at STS 2022
 Congratulations to Oliver K. Jawitz, MD, MHS, a Duke General Surgery resident and clinical research fellow with Duke Clinical Research Institute for presenting his team’s work at the 58th Annual Meeting of the Society of Thoracic Surgeons, which was held virtually Jan. 29-30. Jawitz presented Comparing Consumer-Directed Hospital Rankings with Society of Thoracic Surgeons (STS) Adult Cardiac Surgery Database Outcomes during a plenary session on Jan. 29.
Congratulations to Oliver K. Jawitz, MD, MHS, a Duke General Surgery resident and clinical research fellow with Duke Clinical Research Institute for presenting his team’s work at the 58th Annual Meeting of the Society of Thoracic Surgeons, which was held virtually Jan. 29-30. Jawitz presented Comparing Consumer-Directed Hospital Rankings with Society of Thoracic Surgeons (STS) Adult Cardiac Surgery Database Outcomes during a plenary session on Jan. 29.
Annual hospital rankings – particularly those issued by USNWR – typically make a big splash in the news upon release, but there has been relatively little work done to explore how the rankings compare with actual patient outcomes in any specialty, according to Jawitz. His team designed a study to examine whether the rankings would correlate in a meaningful way with outcomes in adult cardiac surgery patients.
Jawitz and his team compared annual U.S. News & World Report (USNWR) rankings with risk-adjusted mortality/morbidity data from the STS Adult Cardiac Surgery Database. In total, 524,393 patients undergoing CABG or CABG with a valve procedure from 149 hospitals (65 of which were consistently ranked in the top 100 hospitals during the 5-year period examined by the team) were included in the data.
USNWR rankings rely on a complicated methodology that appears to be rigorous but is not fully transparent, says Jawitz. USNWR publishes their methodology, but it changes each year.
In the team’s preliminary dive into the data, Jawitz says he was surprised to see the impact that shifts in USNWR rankings can have on hospitals. “A one spot change in ranking from year to year has been correlated with a one-percent change in revenue and patient volume, which is significant.”
What was not surprising to him or to his team was their primary finding: that the USNWR ratings for cardiology and heart surgery programs do not correlate in any meaningful way with risk-adjusted outcomes data from the STS database.
“This was not a ground-breaking finding, to be perfectly honest,” Jawitz says. “However, what was surprising is that we found absolutely no correlation – not even a signal of correlation — between rankings and outcomes. Given the impact rankings can have can have on patient choices and, frankly, on hospital revenue and the resources that some institutions have dedicated toward trying to lift their USNWR ranking over time, we think it’s an important step to study how these rating systems compare to actual outcome measures for various specialties.”
From the standpoint of heart surgery, the gold standard is the STS database and the public reporting of STS Star Ratings.
“US News and World Report rankings can tell consumers a lot of things, but they don’t tell them enough information about surgical outcomes,” says Peter K. Smith, Mary and Deryl Hart Distinguished Professor of Surgery and former chief, Duke Division of Cardiovascular and Thoracic Surgery. “This particular ranking system combines surgery measures with cardiology measures for heart programs across the U.S., so for patients seeking information about surgical outcomes that information is obscured.
“The primary message here for consumers is that rankings should be used with caution because the differences in rankings of heart programs at U.S. hospitals don’t necessarily relate to differences in surgical outcomes across those same programs,” Smith adds. “Instead – and particularly for patients in need of heart surgery – they really need to look at the public reporting done by the STS and use that information as part of their decision-making process.”
Jawitz concurs.
“We’re really fortunate in the CT surgery world to have the STS database. The STS tracks procedures that have been incredibly well studied for decades; they have risk models and calculators and the ability to hone in on which groups really are performing well and which have some room for improvement,” Jawitz says.
“At the end of the day, the record of surgical outcomes are what should be most important to heart surgery patients – getting your procedure done safely with minimal morbidity and being able to go home to your family is what should matter most. This type of measure appears to be getting lost with high-profile ranking systems such as USNWR.”
Jawitz believes future studies should look at consumer-directed ranking systems in a rigorous and statistically sound way and suggest better ways for such rankings to map better to what matters most to patients as well as to the clinical community.
“Healthcare is a difficult enough system to navigate as it is,” he adds. “I would strongly encourage consumers who are seeking guidance toward programs to consult professional societies that publish risk-adjusted data for the area in which they need care. Relying more on those types of sources than on hospital rankings would probably be of great benefit to them.”
Jawitz and team expect to publish their findings later this year.
Great job, Oliver and team!
Also at STS 2022:
 Congratulations to Christopher Jensen, MD, MHS, a general surgery resident,
Congratulations to Christopher Jensen, MD, MHS, a general surgery resident,  for his on-demand presentation, Cardiovascular Mechanism of Donor Brain Death and Heart Recipient Survival and to Fabian Jimenez Contreras for his on-demand presentation Progression of Aortic Valve Insufficiency During Fully Magnetically Levitated Centrifugal Versus Axial Flow Left Ventricular Assist Device (LVAD) Support that were part of STS’s 58th Annual Meeting. Jimenez Contreras, a 4th year medical student at Duke, is planning a career in cardiothoracic surgery. This was his first presentation at STS
for his on-demand presentation, Cardiovascular Mechanism of Donor Brain Death and Heart Recipient Survival and to Fabian Jimenez Contreras for his on-demand presentation Progression of Aortic Valve Insufficiency During Fully Magnetically Levitated Centrifugal Versus Axial Flow Left Ventricular Assist Device (LVAD) Support that were part of STS’s 58th Annual Meeting. Jimenez Contreras, a 4th year medical student at Duke, is planning a career in cardiothoracic surgery. This was his first presentation at STS
Well done!
Heart Month Celebration Continues!
In celebration of Heart month, the Duke Heart leadership team distributed heart-shaped cookies to team members this week.
Dr. Manesh Patel, Dr. Ed Chen, Jill Engel and the entire leadership team thanks everyone for their dedication to excellent patient care, safety and awareness as we continue to celebrate Heart Month. We hope our team members will take time to reflect on the amazing things each of them and the entire Duke Heart team have achieved over the last year. We are so fortunate to have each and every team member – we could not provide the excellent care that we do without every single one of you. Thank you!
Duke Cardiac Ultrasound Students Named ASE Scholarship Award Winners
Two students in Duke’s Cardiac Ultrasound Certificate Program have won American Society of Echocardiography (ASE) Foundation student scholarships.
 Nick Medlock has received the Waggoner Award and Daisy Chang has received the Katanick Award.
Nick Medlock has received the Waggoner Award and Daisy Chang has received the Katanick Award.
The Katanick award is given to the highest ranking student sonographer candidate nominated for ASEF scholarship awards. This award was established in 2016 and was named to honor the legacy of Sandy Katanick, RN, RVT, CAE, who retired as CEO of the Intersocietal Accreditation Commission after more than 25 years of service to the field.
This is the first year that Duke has been eligible to nominate students; only programs that are nationally accredited can nominate students. Duke’s program received accreditation in 2021.
The awards will be given to Medlock and Chang at the annual ASE meeting in June in Seattle, WA. They will each receive $1,000 and support for travel.
Congratulations to Nick and Daisy! And… hat tip to the Cardiac Ultrasound Program – your efforts are making this one of the best recognized programs in the country!
ICYMI: JCF Ignite! Featured in Medpage Today
This past week, there was a terrific piece in Medpage Today (link below, in “news”) that speaks to a new feature in the Journal of Cardiac Failure.
“At JCF, we’ve been thinking, how can we meet contemporary demands to facilitate conversation, inclusion and excitement in academic publishing? We communicate in new ways,” says Rob Mentz, associate professor of medicine in cardiology and editor-in-chief of the Journal of Cardiac Failure. “JCF Ignite! is one such initiative intended to favorably transform our field. This new section is designed to serve as a platform for very concise and rigorous reports on a novel (potentially provocative) concept, analysis, insight or data presentation. The goal is to enable authors to disseminate worthwhile material in an exceptionally timely manner to enhance impactful discourse and consider paradigm shifts in the care of patients with heart failure.”
Congrats to Mentz and the team at JCF!
Duke Schools of Medicine and Nursing Rank in Top 5 for NIH Research Funding
The medical and nursing schools at Duke University both rank in the top five nationally for research funding received from the National Institutes of Health (NIH), according to the Blue Ridge Institute for Medical Research.
Duke University School of Medicine was awarded more than $608 million in federal funding from the NIH in 2021, ranking third nationally among academic medical centers, up from 10th last year.
“The amount of research funding awarded to Duke scientists by the NIH is a key measure of excellence across all of our missions,” said Mary E. Klotman, MD, dean of Duke University School of Medicine. “These rankings reflect the hard work, dedication and innovation of our outstanding faculty and research staff, and their commitment and contributions to scientific discovery and advancing care for our patients.”
The Blue Ridge ranking — an annual, independent analysis of NIH research funds to colleges and universities — places Duke University School of Nursing at fifth in the nation, up from 8th last year, garnering $8.5 million from the NIH.
“Duke School of Nursing’s growth in research funding reflects the dedication of our faculty and their commitment to improving the health of real people, families, and communities,” said Vincent Guilamo-Ramos, PhD, dean of Duke University School of Nursing and vice chancellor of nursing affairs at Duke University. “They are shaping innovative health interventions and solutions; developing and testing technology that improves health outcomes; and designing nurse-led models of health care that truly are the future of nursing.”
At the medical school, two basic science departments and eight clinical science departments were ranked among the top 10 in the country:
#1 for Pediatrics
#1 for Surgery
#2 for Orthopedics
#5 for Neurosurgery
#6 for Internal Medicine
#8 for Anesthesiology
#9 for Genetics
#9 for Otolaryngology
#10 for Pharmacology
#10 for Ophthalmology
The NIH is the largest public funder of biomedical research in the world, investing more than $41 billion a year to advance research aimed at improving health.
COVID-19 Updates
Final Reminder: All Duke University Health System (DUHS) and Private Diagnostic Clinic (PDC) team members, regardless of work location, are required to receive and provide documentation of a completed COVID-19 booster vaccination by 10 a.m. on Tuesday, Feb. 15, 2022, or within 28 days of their eligibility under CDC and state guidelines. More details are available in this email that was sent to all staff on Tuesday, Dec. 28.
All the latest Clinical Operations updates related to COVID can be found at https://covid-19.dukehealth.org.
Upcoming Events & Opportunities
Duke Genomic & Precision Medicine Forum Series
February 24: Guest will be William E. Kraus, MD speaking on Components of Personalized Lifestyle Medicine with a Focus on Physical Activity. Noon – 1 p.m. via Zoom. Sponsored by Duke Center for Applied Genomics & Precision Medicine. Registration is required; event is free. To learn more and to register, please visit: https://bit.ly/3ouqDiK.
Upcoming Duke Heart CME
April 23: Duke Sports Cardiology & Sudden Death in Athletes Symposium with course directors Jim Daubert and Bill Kraus. Virtual. For information or to register, contact Christy Darnell christy.darnell@duke.edu or 919-880-8686.
Seeking Applicants: Chan Zuckerberg Science Diversity Leadership Award
The Chan Zuckerberg Initiative (CZI) and the National Academies of Sciences, Engineering, and Medicine invite applications for the new Science Diversity Leadership program, which will support projects led by excellent biomedical researchers who—through their outreach, mentoring, and teaching—have a record of promoting diversity, equity and inclusion in their scientific fields.
Each grant recipient will be awarded a total of $1.15 million over five years, with the first two cohorts of grantees selected in 2022 and 2023. Investigators leading the grantees’ projects will use funds to support research programs and outreach, mentoring, and teaching activities. The principal investigator must lead an independent research laboratory in a university, medical school, or nonprofit research institution in the U.S. or a U.S. territory and have started their first independent laboratory no earlier than January 1, 2012. Learn more and apply. Applications close May 19, 2022.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
February 9 — Rob Mentz
Medpage Today
Do You Know How Many Great Ideas and Findings Never Get Published?
https://www.medpagetoday.com/opinion/revolutionandrevelation/97089
February 10 — Duke University & Health System
Forbes
America’s Best Large Employers
https://www.forbes.com/lists/best-large-employers/?sh=3369e30e7b66
Division of Cardiology Publications Indexed in PubMed February 3-9, 2022
Becker F, Dakin HA, Reed SD, Li Y, Leal J, Gustavson SM, Wittbrodt E, Hernandez AF, Gray AM, Holman RR. Lifetime cost-effectiveness simulation of once-weekly exenatide in type 2 diabetes: A cost-utility analysis based on the EXSCEL trial. Diabetes Res Clin Pract 2022 Jan;183:109152. PM: 34813910.
Bloomfield GS, Alenezi F, Chiswell K, Dunning A, Okeke NL, Velazquez EJ. Progression of cardiac structure and function in people with human immunodeficiency virus. Echocardiography 2022 Feb;39(2):268-277. PM: 35048419.
Coniglio AC, Segar MW, Loungani RS, Savla JJ, Grodin JL, Fox ER, Garg S, de Lemos JA, Berry JD, Drazner MH, Shah S, Hall ME, Shah A, Khan SS, Mentz RJ, Pandey A. Transthyretin V142I Genetic Variant and Cardiac Remodeling, Injury, and Heart Failure Risk in Black Adults. JACC Heart Fail 2022 Feb;10(2):129-138. PM: 35115086.
Fiuzat M, Hamo CE, Butler J, Abraham WT, DeFilippis EM, Fonarow GC, Lindenfeld J, Mentz RJ, Psotka MA, Solomon SD, Teerlink JR, Vaduganathan M, Vardeny O, McMurray JJV, O’Connor CM. Optimal Background Pharmacological Therapy for Heart Failure Patients in Clinical Trials: JACC Review Topic of the Week. J Am Coll Cardiol 2022 Feb 8;79(5):504-510. PM: 35115106.
Gilchrist SC, Hall JL, Khandelwal A, Hidalgo B, Aggarwal B, Kinzy C, Mallya P, Conners K, Stevens LM, Alger HM, Mehta L, Wexler L, Mega JL, Hernandez A, Hayes SN, Mieres JH, Jessup M, Roger VL. Research Goes Red: Early Experience With a Participant-Centric Registry. Circ Res 2022 Feb 4;130(3):343-351. PM: 35113661.
Harskamp RE, Fanaroff AC, Lopes RD, Wojdyla DM, Goodman SG, Thomas LE, Aronson R, Windecker S, Mehran R, Granger CB, Alexander JH. Antithrombotic Therapy in Patients With Atrial Fibrillation After Acute Coronary Syndromes or Percutaneous Intervention. J Am Coll Cardiol 2022 Feb 8;79(5):417-427. PM: 35115097.
King HA, Doernberg SB, Grover K, Miller J, Oakes M, Wang TW, McFatrich M, Ruffin F, Staman K, Lane HG, Rader A, Sund Z, Bosworth HB, Reeve BB, Fowler VG, Holland TL. Patients’ Experiences With and Gram-Negative Bacterial Bloodstream Infections: Results From Cognitive Interviews to Inform Assessment of Health-Related Quality of Life. Open Forum Infect Dis 2021 Dec 8;9(2):ofab622. PM: 35106313.
Loring Z, Bahnson TD. Is there a mortality benefit of atrial fibrillation ablation? J Cardiovasc Electrophysiol 2022 Feb;33(2):194-196. PM: 34911158.
Quintanilha JCF, Liu Y, Etheridge AS, Yazdani A, Kindler HL, Kelly WK, Nixon AB, Innocenti F. Plasma levels of angiopoietin-2, VEGF-A, and VCAM-1 as markers of bevacizumab-induced hypertension: CALGB 80303 and 90401 (Alliance). Angiogenesis 2022 Feb;25(1):47-55. PM: 34028627.
Redfors B, Simonato M, Chen S, Vincent F, Zhang Z, Thiele H, Eitel I, Patel MR, Ohman EM, Maehara A, Ben-Yehuda O, Stone GW. Ambient temperature and infarct size, microvascular obstruction, left ventricular function and clinical outcomes after ST-segment elevation myocardial infarction. Coron Artery Dis 2022 Mar 1;33(2):81-90. PM: 34569991.
Salah HM, Al’Aref SJ, Khan MS, Al-Hawwas M, Vallurupalli S, Mehta JL, Mounsey JP, Greene SJ, McGuire DK, Lopes RD, Fudim MEfficacy and safety of sodium-glucose cotransporter 2 inhibitors initiation in patients with acute heart failure, with and without type 2 diabetes: a systematic review and meta-analysis. Cardiovasc Diabetol 2022 Feb 5;21(1):20. PM:35123480
Tobin RS, Samsky MD, Kuchibhatla M, O’Connor CM, Fiuzat M, Warraich HJ, Anstrom KJ, Granger BB, Mark DB, Tulsky JA, Rogers JG, Mentz RJ, Johnson KS Race Differences in Quality of Life following a Palliative Care Intervention in Patients with Advanced Heart Failure: Insights from the Palliative Care in Heart Failure Trial.J Palliat Med 2022 Feb;25(2):296-300. PM:34851740
Toro C, Temkin N, Barber J, Manley G, Jain S, Ohnuma T, Komisarow J, Foreman B, Korley FK, Vavilala MS, Laskowitz DT, Mathew JP, Hernandez A, Sampson J, James ML, Goldstein BA, Markowitz AJ, Krishnamoorthy V, Association of Vasopressor Choice with Clinical and Functional Outcomes Following Moderate to Severe Traumatic Brain Injury: A TRACK-TBI Study. Neurocrit Care 2022 Feb;36(1):180-191.PM:34341913
Duke Heart Week Ending February 6th 2022
Highlights of the week:
National Wear Red Day
Kudos to all team members for sporting red on National Wear Red Day, Friday, Feb. 4. We remain so grateful to each of you for the work you’re doing to provide the very best care possible for our patients, for the work you do to continue to lift one another up during very stressful and challenging circumstances, and helping to increase awareness of cardiovascular disease overall. Great job! Please continue to share photos with Pulse – we’ll happily share them all month long as we celebrate Heart month!
Shown here are members of our Heart Leadership team (Heart leadership team members and administrative assistants); our VAD team (L to R: Kevin Cox, Catherine Shuford, Helen Barnes, Laura Blue, Pernestaline McAllister and Dakota Bentz); Two generations of Kelsey’s: faculty member Anita Kelsey, MD and cardiology fellow Michelle Kelsey, MD; Duke Heart administrative assistant Caleb Smith; Jill Engel & Terri Fortin; Cath lab sporting some red! (Clockwise from top L: Terri Fortin, and the sporty shoes of Larry Jackson, Jill Engel & Manesh Patel); several of our amazing WICs (L-R: Anita Kelsey, Jessie Duran, Toi Spates, Brittany Zwischenberger, and Nkiru Osude).
Looking good, everyone!!! More photos to come next week…







Heart Highlights: Duke Electrophysiology
It was another incredible year in Duke Heart with impressive accomplishments across the board. We are pleased to share with you just a few of the highlights from the past year from our Duke Electrophysiology team:
In calendar year 2021, (despite several waves of the COVID pandemic) Duke EP clinicians performed:
- 6316 in person device interrogations
9% increase from 2020
- 16,603 remote device interrogations
12% increase from 2020
- 1103 device implants at Duke University Hospital
No change from 2020
- 1078 EP study/ablation procedures at Duke University Hospital
10% increase from 2020
- Includes 545 AF ablations
12% increase from 2020
- Includes 138 VT ablations at Duke University Hospital
5% increase from 2020
- 54 left atrial appendage closure procedures at Duke University Hospital
- 127 lead extraction procedures within the Duke Heart network, including 34 at Wake Med-Heart Care Plus
6% increase from 2020
Duke EP welcomed several new members this year, including Daniel J. Friedman, MD, a former Duke cardiology and EP fellow who rejoined us after serving on the faculty at Yale School of Medicine; Laura Webb, PA-C, MPAS and Chrystal Foster, RNFA, FNP-C, MSN.
Team members engaged in a number of volunteer efforts, including Bill Cockfield, who served as a Covid-19 community vaccinator at the Karsh Alumni Center and Kelly Valencia, who did similarly at Duke Raleigh’s first “Pop Up” Covid-19 vaccine clinic.
Camille Frazier-Mills and Tristram Bahnson were appointed to editorial boards – Frazier-Mills to Circulation: Arrhythmia and Electrophysiology and Bahnson to Heart Rhythm O2. Multiple EP faculty members – including Bahnson, Frazier-Mills, James Daubert, Don Hegland, Larry Jackson, Kevin Jackson, Jason Koontz, Jon Piccini and Al Sun are chapter authors in the most recent edition of the popular EKG textbook Marriott’s Practical Electrocardiography (13th edition).
Notable awards this past year include:
- Brenda Smith who received the prestigious Wilma Minniear Award for Excellence in Nursing Mentorship, part of Duke’s Friends of Nursing Excellence awards;
- Kevin Thomas received the Excellence in Professionalism Award from Duke School of Medicine – the award recognizes a faculty member who exemplifies professionalism and personifies Duke’s guiding principles of respect, trustworthiness, diversity, teamwork, and learning.
Research accomplishments include:
- 108 peer-reviewed publications for 2021!
- Larry Jackson received a K-Award from the NIH’s National Heart, Lung, and Blood Institute for his project, Shared Decision-Making to Reduce Racial Disparities in Oral Anticoagulation Use in Patients with Non-Valvular Atrial Fibrillation.
- Enrollment of the first patient in the nationwide DEFINE AFIB trial, an app-based research study that will assess atrial fibrillation burden and its impact on patient outcomes, quality of life, and healthcare utilization. Jon Piccini, MD is chair of the DEFINE AFib Steering Committee.
- Sean Pokorney, MD and team on June 14th implanted the first Extravascular Implantable Cardioverter Defibrillator (EV ICD) in the Carolinas as part of the Medtronic EV ICD Pivotal Study.
- Several presentations at the European Society of Cardiology Congress, including Micra Coverage with Evidence Development (CED) Study Two Year Follow-up Results, the largest evaluation of leadless pacemakers to date, presented by Jon Piccini, MD.
- In September Drs. Al Sun and Jason Koontz conducted the first-in-man utilization of the Ventrax ventricular access sheath that was designed in collaboration with Merit Medical. The system is designed with an integrated pigtail dilator to allow seamless transition from femoral access directly to crossing the aortic valve. The sheath is FDA approved and there are ongoing efforts to test the sheath in a small trial evaluating the benefit of avoiding using an ablation catheter to cross the valve as well as the additional support of a long sheath in the LV.
- The National Institutes of Health awarded Joseph Mathew, MD, chair of Duke Anesthesiology, Jerry Reves, MD, professor of anesthesiology, and Jon Piccini, MD, MHS a $3,739,083 R01 grant for their project titled, Neurocognition and Greater Maintenance of Sinus Rhythm in AF (NOGGIN AF). Drs. Mathew, Piccini, and the Duke EP Team will test the hypothesis that restoration of sinus rhythm with catheter ablation vs drug therapy leads to less long-term neurologic damage and dysfunction due to improved cerebral blood flow and lower risk for additional ischemic injury.
Congrats to the entire Duke EP team – we know even more was accomplished than we could include here this week – what a terrific year you’ve had; there is a lot to celebrate!
ICYMI: Blumer Piece Featured by ACC
Duke Cardiology fellow Vanessa Blumer, MD, has a terrific piece in the American College of Cardiology’s Cardiology Magazine: Training Pathways for Critical Care Cardiology: The Intersection with Advanced Heart Failure. Great job!

Machovec Receives DCHC Impact Award
Duke Cardiac Anesthesiologist Kelly Machovec, MD, MPH, has been awarded the Pediatric and Congenital Heart Center (PCHC) Impact Award for the exceptional impact she has had on clinical practice around hemostasis, on both a local and
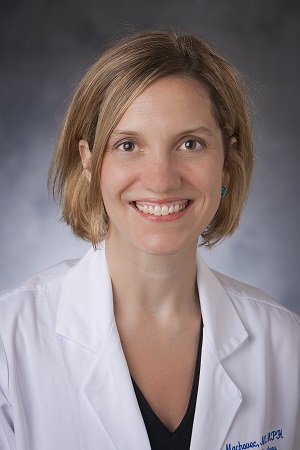
national level.
“I am grateful for the recognition and so proud to be part of the amazing PCHC team,” says Machovec, associate professor of anesthesiology. “Being a pediatric cardiac anesthesiologist is the best job in the world.”
The Pediatric and Congenital Heart Center Impact Award is an annual accolade that is decided by the voting of peers. Machovec’s colleague, Dr. Warwick Ames, presented her the award on January 26 at the PCHC yearly retreat. As he describes, “her impact is palpable everywhere in the Duke Children’s Heart Center.” Machovec is credited for discontinuing preoperative blood testing to avoid children having painful, unnecessary blood draws in the preoperative clinic, which revolutionized the way blood products are ordered for children with congenital heart disease at Duke. She also wrote the handbook of coagulation management for children coming off cardiopulmonary bypass. This led to her founding the Hemostasis Interest Group, a committee within the Congenital Cardiac Anesthesia Society, described as “a forum where some of the sharpest brains in pediatric anesthesia meet to share knowledge and expertise.”
“Kelly has had a special impact on each of us and is fully deserving of this award. I am proud to call her a dear friend and colleague and congratulate her on receiving this award,” adds Ames.
Machovec completed a fellowship in pediatric anesthesiology at Duke University before joining Duke Anesthesiology faculty in 2013 where she is a member of the Pediatric Anesthesiology Division. Machovec’s impact is also recognized outside of Duke. As a mark of her influence, she is an advocate for basic science cancer research; to-date, Machovec has raised $48,000 for the Dana-Farber Cancer Institute as part of her participation in the 2022 Boston Marathon.
Flags Lowered in Memory of Jones
University flags were lowered on Monday, Jan. 31, 2022 in memory of Robert “Bob” H. Jones, MD, Professor Emeritus of Surgery, who died on Jan. 26. We thank all who shared their thoughts of him with Pulse. A reminder that his obituary can be found here and that a memorial service will be held at 11:00 a.m. on March 5th at the Cole Mill Road Church of Christ, 1617 Cole Mill Rd, Durham, NC 27705.
COVID-19 Updates
All the latest Clinical Operations updates related to COVID can be found at https://covid-19.dukehealth.org.
Reminder: All Duke University Health System (DUHS) and Private Diagnostic Clinic (PDC) team members, regardless of work location, are required to receive and provide documentation of a completed COVID-19 booster vaccination by 10 a.m. on Tuesday, Feb. 15, 2022, or within 28 days of their eligibility under CDC and state guidelines. More details are available in this email that was sent to all staff on Tuesday, Dec. 28.
Upcoming Events & Opportunities
Cardiology Grand Rounds
February 8: No CGR today.
February 10: Topic TBA. Our guest will be AAMC President, Dr. David Skorton.
February 15: Topic TBA. Presenter will be Toi Spates.
Duke Genomic & Precision Medicine Forum Series
February 24: Guest will be William E. Kraus, MD speaking on Components of Personalized Lifestyle Medicine with a Focus on Physical Activity. Noon – 1 p.m. via Zoom. Sponsored by Duke Center for Applied Genomics & Precision Medicine. Registration is required; event is free. To learn more and to register, please visit: https://bit.ly/3ouqDiK.
Upcoming Duke Heart CME
April 23: Duke Sports Cardiology & Sudden Death in Athletes Symposium with course directors Jim Daubert and Bill Kraus. Virtual. For information or to register, contact Christy Darnell christy.darnell@duke.edu or 919-880-8686.
Seeking Applicants: Chan Zuckerberg Science Diversity Leadership Award
The Chan Zuckerberg Initiative (CZI) and the National Academies of Sciences, Engineering, and Medicine invite applications for the new Science Diversity Leadership program, which will support projects led by excellent biomedical researchers who—through their outreach, mentoring, and teaching—have a record of promoting diversity, equity and inclusion in their scientific fields.
Each grant recipient will be awarded a total of $1.15 million over five years, with the first two cohorts of grantees selected in 2022 and 2023. Investigators leading the grantees’ projects will use funds to support research programs and outreach, mentoring, and teaching activities. The principal investigator must lead an independent research laboratory in a university, medical school, or nonprofit research institution in the U.S. or a U.S. territory and have started their first independent laboratory no earlier than January 1, 2012. Learn more and apply. Applications close May 19, 2022.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
January 27 — Christopher Granger
Healio/Cardiology
Early referral for ablation may be needed for certain patients with AF
https://duke.is/gb3gw
January 31 — Midge Bowers
NPschools.com
Day in the Life of a Cardiology NP – Two Experts Share Their Perspectives
https://duke.is/vxj3b
February 1 — L. Kristin Newby
MCG magazine/Augusta University
https://duke.is/m2enw
February 2 — John Haney
Fierce Biotech
Paragonix’s lung transport system completes 4,700-mile, cross-country transplant
https://duke.is/8rb6a
February 2 — Duke University Hospital (Lung Tx program)
Becker’s Hospital Review
10 hospitals performing high volumes of lung transplants
https://duke.is/2d5z7
February 3 — Adam DeVore
WSOCtv.com (Charlotte)
‘Saved my life’: Harrisburg man is first in North America with artificial heart
https://bit.ly/3rw2pGQ
February 4 — Svati Shah
CBS17.com (Raleigh)
National Wear Red Day seeks to raise awareness among women about heart disease
https://bit.ly/34mF3uf
Division of Cardiology Publications Indexed in PubMed January 27-February 2, 2022
Al-Khatib SM, Link MS. Perplexing Results From the PRAETORIAN Trial: Revisiting the Debate About the Value of Antitachycardia Pacing. Circulation 2022;145(5):330-332. PM: 35100016.
Carnicelli AP, Hong H, Connolly SJ, Eikelboom J, Giugliano RP, Morrow DA, Patel MR, Wallentin L, Alexander JH, Cecilia Bahit M, Benz AP, Bohula EA, Chao TF, Dyal L, Ezekowitz M, A A Fox K, Gencer B, Halperin JL, Hijazi Z, Hohnloser SH, Hua K, Hylek E, et al. Direct Oral Anticoagulants Versus Warfarin in Patients With Atrial Fibrillation: Patient-Level Network Meta-Analyses of Randomized Clinical Trials With Interaction Testing by Age and Sex. Circulation 2022;145(4):242-255. PM: 34985309.
Chandra A, Skali H, Claggett B, Solomon SD, Rossi JS, Russell SD, Matsushita K, Kitzman DW, Konety SH, Mosley TH, Chang PP, Shah AM. Race- and Gender-Based Differences in Cardiac Structure and Function and Risk of Heart Failure. J Am Coll Cardiol 2022;79(4):355-368. PM: 35086658.
Chau KH, Chen S, Crowley A, Redfors B, Li D, Hahn RT, Douglas PS, Alu MC, Finn MT, Kodali S, Jaber WA, Rodriguez L, Thourani VH, Pibarot P, Leon MB. Paravalvular regurgitation after transcatheter aortic valve replacement in intermediate-risk patients: a pooled PARTNER 2 study. EuroIntervention 2022;17(13):1053-1060. PM: 34483095.
Collins KA, Ross LM, Piner LW, Fos LB, Slentz CA, Bateman LA, Willis LH, Bales CW, Siegler IC, Wolever RQ, Huffman KM, Kraus WE. Amount and intensity effects of exercise training alone versus a combined diet and exercise lifestyle intervention on health-related quality of life in the STRRIDE-PD randomized trial. BMJ Open Diabetes Res Care 2022;10(1):e002584. PM: 35086944.
DeVore AD, Hill CL, Thomas LE, Albert NM, Butler J, Patterson JH, Hernandez AF, Williams FB, Shen X, Spertus JA, Fonarow GC. Identifying patients at increased risk for poor outcomes from heart failure with reduced ejection fraction: the PROMPT-HF risk model. ESC Heart Fail 2022;9(1):178-185. PM: 34791838.
El-Chami MF, Garweg C, Iacopino S, Al-Samadi F, Martinez-Sande JL, Tondo C, Johansen JB, Prat XV, Piccini JP, Cha YM, Grubman E, Bordachar P, Roberts PR, Soejima K, Stromberg K, Fagan DH, Clementy N. Leadless pacemaker implant, anticoagulation status, and outcomes: Results from the Micra Transcatheter Pacing System Post-Approval Registry. Heart Rhythm 2022;19(2):228-234. PM: 34757189.
Ezekowitz JA, Alemayehu W, Rathwell S, Grant AD, Fiuzat M, Whellan DJ, Ahmad T, Adams K, Piña IL, Cooper LS, Januzzi JL, Leifer ES, Mark D, O’Connor CM, Felker GM. The influence of comorbidities on achieving an N-terminal pro-b-type natriuretic peptide target: a secondary analysis of the GUIDE-IT trial. ESC Heart Fail 2022;9(1):77-86. PM: 34784657.
Govsyeyev N, Nehler MR, Low Wang CC, Kavanagh S, Hiatt WR, Long C, Jones WS, Fowkes FGR, Berger JS, Baumgartner I, Patel MR, Goodney PP, Beckman JA, Katona BG, Mahaffey KW, Blomster J, Norgren L, Bonaca MP. Etiology and outcomes of amputation in patients with peripheral artery disease in the EUCLID trial. J Vasc Surg 2022;75(2):660-670. PM: 34597783.
Greene SJ, Butler J, Fonarow GC. In-hospital initiation of quadruple medical therapy for heart failure: making the post-discharge vulnerable phase far less vulnerable. Eur J Heart Fail 2022;24(1):227-229. PM: 34779112.
Gupta K, Girotra S, Nallamothu BK, Kennedy K, Starks MA, Chan PS. Impact of the three COVID-19 surges in 2020 on in-hospital cardiac arrest survival in the United States. Resuscitation 2022;170:134-140. PM: 34838661.
Katz DH, Tahir UA, Bick AG, Pampana A, Ngo D, Benson MD, Yu Z, Robbins JM, Chen ZZ, Cruz DE, Deng S, Farrell L, Sinha S, Schmaier AA, Shen D, Gao Y, Hall ME, Correa A, Tracy RP, Durda P, Taylor KD, Liu Y, Johnson WC, Guo X, Yao J, Ida Chen YD, et al. Whole Genome Sequence Analysis of the Plasma Proteome in Black Adults Provides Novel Insights Into Cardiovascular Disease. Circulation 2022;145(5):357-370. PM: 34814699.
Kittipibul V, Fudim M. Tackling Inflammation in Heart Failure With Preserved Ejection Fraction: Resurrection of Vagus Nerve Stimulation? J Am Heart Assoc 2022;11(3):e024481. PM: 35023352.
Mac Grory B, Piccini JP, Yaghi S, Poli S, De Havenon A, Rostanski SK, Weiss M, Xian Y, Johnston SC, Feng W. Hyperglycemia, Risk of Subsequent Stroke, and Efficacy of Dual Antiplatelet Therapy: A Post Hoc Analysis of the POINT Trial. J Am Heart Assoc 2022;11(3):e023223. PM: 35043692.
Narins CR, Aktas MK, Chen AY, McNitt S, Ling FS, Younis A, Zareba W, Daubert JP, Huang DT, Rosero S, Kutyifa V, Goldenberg I. Arrhythmic and Mortality Outcomes Among Ischemic Versus Nonischemic Cardiomyopathy Patients Receiving Primary ICD Therapy. JACC Clin Electrophysiol 2022;8(1):1-11. PM: 34454875.
Ngeno GTK, Barasa F, Kamano J, Kwobah E, Wambui C, Binanay C, Egger JR, Kussin PS, Thielman NM, Bloomfield GS. Feasibility of Cardiac Rehabilitation Models in Kenya. Ann Glob Health 2022;88(1):7. PM: 35087707.
Norgren L, North R, Baumgartner I, Berger JS, Blomster JI, Hiatt WR, Jones WS, Katona BG, Mahaffey KW, Mulder H, Patel MR, Rockhold FW, Fowkes FGR. World regional differences in outcomes for patients with peripheral artery disease: Insights from the EUCLID trial. Vasc Med 2022;27(1):21-29. PM: 34516308.
Oliver CE, Patel H, Hong J, Carter J, Kraus WE, Huffman KM, Truskey GA. Tissue engineered skeletal muscle model of rheumatoid arthritis using human primary skeletal muscle cells. J Tissue Eng Regen Med 2022;16(2):128-139. PM: 34781416.
Oster ME, Shay DK, Su JR, Gee J, Creech CB, Broder KR, Edwards K, Soslow JH, Dendy JM, Schlaudecker E, Lang SM, Barnett ED, Ruberg FL, Smith MJ, Campbell MJ, Lopes RD, Sperling LS, Baumblatt JA, Thompson DL, Marquez PL, Strid P, Woo J, Pugsley R, Reagan-S. Myocarditis Cases Reported After mRNA-Based COVID-19 Vaccination in the US From December 2020 to August 2021. JAMA 2022;327(4):331-340. PM: 35076665.
Smith ID, Ross LM, Gabaldon JR, Holdgate N, Pieper CF, Ning TC, Kraus WE, Huffman KM. The Relation of Accelerometer-Measured Physical Activity and Serum Uric Acid Using the National Health and Nutrition Survey (NHANES) 2003-2004. Front Sports Act Living 2022;3:775398. PM: 35098119.
Tsai S, Liu Y, Alaiti MA, Gutierrez JA, Brilakis ES, Banerjee S. No benefit of vorapaxar on walking performance in patients with intermittent claudication. Vasc Med 2022;27(1):33-38. PM: 34609939.
Wang H, Kurniansyah N, Cade BE, Goodman MO, Chen H, Gottlieb DJ, Gharib SA, Purcell SM, Lin X, Saxena R, Zhu X, Durda P, Tracy R, Liu Y, Taylor KD, Johnson WC, Gabriel S, Smith JD, Aguet F, Ardlie K, Blackwell T, Reiner AP, Rotter JI, Rich SS. Upregulated heme biosynthesis increases obstructive sleep apnea severity: a pathway-based Mendelian randomization study. Sci Rep 2022;12(1):1472. PM: 35087136.
Wharton JM, Piccini JP, Koren A, Huse S, Ronk CJ. Comparative Safety and Effectiveness of Sotalol Versus Dronedarone After Catheter Ablation for Atrial Fibrillation. J Am Heart Assoc 2022;11(3):e020506. PM: 35060388.
Woldu B, Temu TM, Kirui N, Christopher B, Ndege S, Post WS, Kamano J, Bloomfield GS. Diastolic dysfunction in people with HIV without known cardiovascular risk factors in Western Kenya. Open Heart 2022;9(1):e001814. PM: 35064055.
Duke Heart Pulse week ending January 30th 2022
Updates of the week:
In Memoriam: Robert H. Jones, MD, Professor Emeritus of Surgery
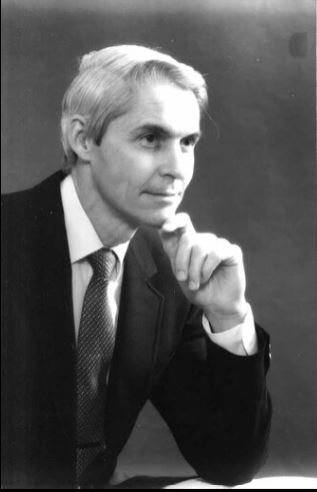 It is with great sadness that we inform you of the passing of Robert “Bob” H. Jones, MD, Professor Emeritus of Surgery, on January 26, 2022. Dr. Jones was the Mary and Deryl Hart Distinguished Professor of Surgery and a prolific cardiothoracic surgeon and clinical investigator until his retirement in 2014. We have lost a treasured member of the Duke community, but his legacy will live on.
It is with great sadness that we inform you of the passing of Robert “Bob” H. Jones, MD, Professor Emeritus of Surgery, on January 26, 2022. Dr. Jones was the Mary and Deryl Hart Distinguished Professor of Surgery and a prolific cardiothoracic surgeon and clinical investigator until his retirement in 2014. We have lost a treasured member of the Duke community, but his legacy will live on.
Dr. Jones received his medical degree from Johns Hopkins University in 1965, and became one of the first Duke University surgical residents taught by Dr. David C. Sabiston, Jr. His residency was interrupted by military service when Dr. Jones served as a Captain in the Air Force. He then completed his residency and joined the Duke Department of Surgery as an Assistant Professor in 1975.
Dr. Jones’ career at Duke spanned 40 years as a cardiac surgeon, clinical investigator, resident educator, and an agent of change in the provision of cardiac care here at Duke and around the world. Beginning as a Howard Hughes Investigator, he made several seminal contributions in the field of lung scanning and nuclear cardiology imaging. His major interest was in the treatment of patients with coronary artery disease, where he was instrumental in the employment of patient data from the Duke Cardiovascular Disease Databank and the Duke Cardiac Research Institute to develop evidence that has guided surgeons and cardiologists through decades of change. From this platform, he obtained NIH funding for the STICH trial, which compared medical therapy to surgical therapy for coronary artery disease. This trial ultimately enrolled over 2,000 patients worldwide, following them for a decade, and publishing outcomes in more than 50 manuscripts to date.
As his academic career flourished, he was selected as the inaugural recipient of the Mary and Deryl Hart Distinguished Professorship, created to honor the founder of Duke’s Department of Surgery. As a professor, Dr. Jones was an accomplished surgeon performing thousands of Coronary Artery Bypass operations and training scores of surgical residents. He emphasized the integration of science and clinical decision making within everyday practice.
Professorship, created to honor the founder of Duke’s Department of Surgery. As a professor, Dr. Jones was an accomplished surgeon performing thousands of Coronary Artery Bypass operations and training scores of surgical residents. He emphasized the integration of science and clinical decision making within everyday practice.
Dr. Jones published more than 250 manuscripts that have provided the evidence base used in that everyday practice. His research also focused on harmonizing the roles of surgeons and cardiologists in order to strengthen collaboration between specialties.
Dr. Jones co-founded the Heart Center in 1989 as the first service line within Duke Hospital and promoted joint research and joint clinical practice. This directly led to the concept of Heart Team decision making that is now embodied in all national and international guidelines for the treatment of coronary disease.
Dr. Jones’ legacy is embodied in the thousands of recipients of his generous teaching and mentorship in the clinical, research, and administrative communities. This legacy is best summed up by the inscription on his retirement gift: “Physician, Surgeon, Scholar, Mentor, Leader…and so much more!”
A memorial service will be held at 11:00 am on March 5th at the Cole Mill Road Church of Christ, 1617 Cole Mill Rd, Durham, NC 27705. A full obituary can be found here.
Upon Dr. Jones’ retirement, Duke’s Medical Alumni Association honored him and other retiring faculty at a reception and dinner. The Association produced a video to honor him that evening; it can be viewed here: https://www.youtube.com/watch?v=j6-NK9RUfhA.
We extend our deep condolences to his family, friends, his mentees and former colleagues throughout the world. We know he will be missed.
We wanted to share some thoughts and reminiscences with you:
From Jerry Reves, MD, Dean Emeritus, Distinguished Professor Medical University of South Carolina and former faculty member, Duke Anesthesiology
“Bob was a colleague and good friend. The quality I most admired was his honesty that was always informed by his intelligence and innovation. He had pioneered the surgical component of the Duke Databank and learned very early how the preoperative cardiac catherization data could be used to predict surgical outcome. This was truly innovative, but once in a conversation we were having in relation to various surgeons reporting mortality data after coronary bypass surgery, he said: “I can make my mortality whatever I want.” He had learned by looking at the Duke Databank that if you operated only on patients with very good ventricular function and little coronary disease that the mortality approached zero. However, if you operated on patients with poor ventricular function and a lot of coronary disease the mortality approached 5 percent. So his comment was not boastful, it was an honest, scientifically precise statement that surgical results were almost solely dependent on the preoperative condition of his patient. If a surgeon wanted great results he/she would not operate on sick patients. Bob continued to take all patients and I admired him for that.
 Bob, Tom Bashore and I were asked to design a Heart Center for Duke. This request came from Drs. Greenfield and Sabiston. We visited three places — Mayo Clinic, Texas Heart, and Cleveland Clinic — and studied University of Alabama Birmingham and Emory. The three of us, especially with Bob’s enthusiasm agreed that we could build a unique Heart Center at Duke that featured superb clinical care and innovative research. We designed a heart center that integrated Cardiology, Cardiac Surgery and Cardiac Anesthesia. The model was accepted, and the rest is history. It would not have happened without Bob Jones representing cardiac surgery!
Bob, Tom Bashore and I were asked to design a Heart Center for Duke. This request came from Drs. Greenfield and Sabiston. We visited three places — Mayo Clinic, Texas Heart, and Cleveland Clinic — and studied University of Alabama Birmingham and Emory. The three of us, especially with Bob’s enthusiasm agreed that we could build a unique Heart Center at Duke that featured superb clinical care and innovative research. We designed a heart center that integrated Cardiology, Cardiac Surgery and Cardiac Anesthesia. The model was accepted, and the rest is history. It would not have happened without Bob Jones representing cardiac surgery!
Bob Jones was the “go to” surgeon if you or your patient needed coronary bypass surgery, the most frequently performed operation in the formative days of the Duke Heart Center. He was consistent, competent, and available. In the high stakes, sometimes stressful cardiac surgical operating room, where everyone had to work in a professional, communicative, and collaborative fashion, there was no better team player to be with than Dr. Jones.”
From Tom Bashore, Duke Professor of Medicine in Cardiology:
“My first memory of Bob Jones was when one of my patients commented that they thought he was such a nice man — they were not sure if he was the chaplain or their heart surgeon. With his head of white hair and broad grin of white teeth, Bob put everyone at ease. He was kind, but he was innovative, and he was willing to try novel things in the OR. What many might not know is that in the late 1970s, he was also one of the first people working in nuclear cardiology at Duke. Using a “first-pass” technique, for the first time one could view images of the heart chambers contracting and relaxing as the radionuclide traversed through the heart. The spatial resolution was lousy though, and I remember Bob’s hearty laugh the first time he presented his data where the end-systolic image of the heart came down to a single square red pixel. Rather than being alarmed, Bob was the kind of person that could see the humor in that and was not at all deterred by such stuff. He obviously moved on to other areas as his career took off in other directions. When he, Jerry Reves, and I went around the country visiting Heart Centers (in the hope of forming one here at Duke), he traveled with only a tiny satchel bag and never a suitcase (he bragged about that). Despite that, he always looked the best dressed of all of us, and with his smooth style he was certainly the best looking and best talker among us, no matter what the situation. And that aura about him never changed throughout his whole career. He will always be remembered for not only being an outstanding physician and surgeon but for being a wonderful and warm human being. There have been few like him at Duke, and I daresay in medicine.”
From Carmelo A. Milano, MD, Professor of Surgery and chief, Section of Adult Cardiac Surgery at Duke:
“Dr. Jones developed and ran the influential STICH trial. This was a large international trial that demonstrated the benefits of CABG surgery for patients with reduced heart function and heart failure. The results of this trial changed the way we practice heart surgery today.”
From Peter K. Smith, Mary and Deryl Hart Distinguished Professor of Surgery and former chief, Duke Division of Cardiovascular and Thoracic Surgery:
“Bob Jones influenced me in so many ways. I did a couple of hundred coronary operations with him; I took care of maybe 500-600 patients of his, maybe more. I interacted with him every day, and learned something every day. He essentially took me under his wing in the research area, and made a huge difference in my research capabilities and my ability to get grants. He was a pretty amazing guy and he was driven to contribute. He was very goal-oriented with a very strong desire to bring cardiology and surgery together in a meaningful way, which he was able to do at Duke — which led to a real blossoming of both cardiology and cardiothoracic surgery here as the Duke Heart Center. He was very forward-thinking — not only was the creation of a true ‘Heart Center’ good for Duke, it was good for our patients. This was happening at a time when cardiologists were transitioning from being ‘diagnosticians’ toward cardiologists as ‘treating specialists.’ And that transition period was very interesting because we were pretty co-dependent in the early days. Percutaneous interventions were quite hazardous in the beginning and required close collaboration with surgeons. As percutaneous intervention became much less “risky” it became potentially more competitive, but the evidence-base was poor. So all the decisions really had to be made either individually by cardiologists or individually by surgeons or jointly between the two — and it became much more frequent that we did this jointly at Duke, with due credit to Dr. Jones who recognized where this transition was going to go. It could have been polarizing or it could be harmonizing. He stressed the latter.
Interestingly, his academic career in professional societies was primarily through the American College of Cardiology, and not with a surgical society. He served as chair of their Board of Governors for time and was a trustee for a time as well. With academic surgeons, they’re typically more involved with a surgical society such as AATS, but Bob put his time and commitment toward the ACC which speaks a great deal to his desire for collaboration.”
From Chris O’Connor, MD, President, Inova Heart and Vascular Institute and former division chief, Duke Cardiology:
“As a surgeon, Bob Jones was thought of as ‘the cardiologist’s surgeon’ – he was so collaborative with us. When I was a junior attending in the intensive care unit at Duke we would have these difficult cases that would often get turned down by his surgical colleagues. We would always call him and he would talk with us and talk with the patient – he was very good with patient interactions. He would take on high-risk cases that needed to be done because he understood the evidence from the Duke Databank, and most importantly, he understood the needs of the patient and valued the recommendations of the cardiologists.
As an investigator, he had this unique mindset which was rich in his understanding of quantitative science and data and it just fit the philosophy of the Duke Databank and the DCRI. He was completely committed to the philosophy of quantitative clinical research. He worked closely with Kerry Lee and the biostatisticians at DCRI — he was also a consultant to the New York State Cardiothoracic Surgery database. He was a superb clinical investigator. The capstone of his career was his work with Eric Velazquez on the STICH trial, a 15-year endeavor that really changed the way we think of surgery and the management of heart failure forever. It’s an enduring body of work that will last forever, in my opinion, not just the STICH trial but all the follow-up trials to that. He was so passionate about it — and it would have never been completed if it wasn’t for Bob Jones leading that effort; it was just so hard to do that trial. He dedicated the latter part of his career entirely to that effort.
STICH took an enormous amount of education and awareness, which Bob led globally. He leveraged some deep relationships with his colleagues in Poland, which he had developed over 30-40 years. It was through those relationships in particular, that they were able to complete the trial. Only 25 percent of the patients enrolled were in the United States.
The other thing to know about Bob is, early in his career, he did some very important investigations looking at how nuclear scans can be used to detect heart disease. And for many, many years, people outside of Duke thought he was a nuclear cardiologist, not a surgeon, because of his publications in that area.
Bob was just a prince of a person. He was deeply spiritual and he brought that connectivity to his care of patients and his interactions with people, and I thought he was a terrific professional colleague. He could be hard-headed and firm, but in the end, he really loved his professional colleagues. He loved his family and he really loved his patients. He was an outstanding cardiothoracic surgeon, outstanding clinical investigator, and outstanding person.”
From Manesh Patel, MD, professor of medicine and chief, Division of Cardiology:
As a fellow, faculty member, and clinical researcher at the DCRI, we looked towards Bob Jones as the standard bearer for the cardiothoracic surgical group. He was a clinician who many of us got to interact with for patient care, for clinical research, and most importantly as a mentor for both cardiologists and surgeons. He was kind, consistent and would be direct and firm about how we considered research and patient care, and in the end was a key driving force inmproving the way we cared for patients. In the cardiology world, his work with Eric Velazquez on the STITCH trial will be one of his key legacies in addition to the Duke Heart Center and people that practice here.
Cardio-Onc Program Named Center of Excellence by ICO Society
We learned this week that our Duke Cardio-Oncology program is among the first to achieve Center of Excellence gold status designation by the International Cardio-Oncology Society. It is one of only nineteen programs world-wide to receive the Center of Excellence rating. In the inaugural effort, 15 programs received gold designation and 4 received silver. To learn more about the ICO Society and the COE rating, please visit: https://ic-os.org/excellence-certification/. The official presentation was made during a virtual event held January 27.
Congratulations to Michel Khouri, Susan Dent and their incredible team!
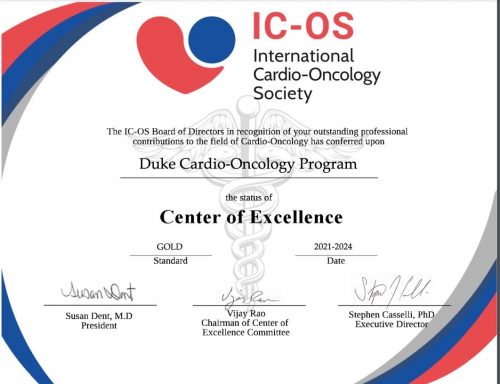
Shah Named to NC Chapter of ACC

Nishant Shaw, assistant professor of medicine in cardiology has been elected to the Leadership Board of the North Carolina chapter of the American College of Cardiology as a Councilor. He will serve a three-year term starting in March. Councilors to the chapter are responsible for serving as a member of the Nominating Committee; serving as an advocate for his/her region in the areas of education and advocacy; communicating Chapter business to members of his/her region and reporting back to the Chapter, as well as participating in approving the annual Chapter budget.
Shah will serve alongside fellow Councilor Adam DeVore and cardiology fellow Vanessa Blumer, who serves as the ACC FIT Liaison.
Congratulations, Nishant! Well-deserved and certainly this team will represent us well.
Shout-out to Rymer & PWIM Planning Team

Congratulations to Jenn Rymer and the planning team for the Program for Women in Internal Medicine (PWIM). They held a terrific online session this week that featured Pam Douglas, Leslie Curtis and  April Salama discussing how they got their start in medicine and launched superb careers in research. Rymer moderated an engaging and informative discussion. Great job to all!
April Salama discussing how they got their start in medicine and launched superb careers in research. Rymer moderated an engaging and informative discussion. Great job to all!
Byler Named Clinical Lead 3100 Effective March 14th
 We are excited to share that Hannah Byler will be joining the 3100 leadership team as a Clinical Lead effective Monday, March 14, 2022. Hannah began her nursing career on 3100 in March 2019. She earned her Associates in Nursing at Wake Technical Community College in 2018 and her Bachelor of Science in Nursing at University of North Carolina Wilmington in 2021. Hannah holds a variety of roles on 3100 including preceptor, charge nurse, MOVEs champion, Time to Pace class instructor, and has recently advanced to CNIII.
We are excited to share that Hannah Byler will be joining the 3100 leadership team as a Clinical Lead effective Monday, March 14, 2022. Hannah began her nursing career on 3100 in March 2019. She earned her Associates in Nursing at Wake Technical Community College in 2018 and her Bachelor of Science in Nursing at University of North Carolina Wilmington in 2021. Hannah holds a variety of roles on 3100 including preceptor, charge nurse, MOVEs champion, Time to Pace class instructor, and has recently advanced to CNIII.
Congratulations, Hannah!
CVRC Post-Holiday Morale Booster!
The Duke Cardiovascular Research Center team was able to help celebrate their team members last week with a post-holiday pick-me-up.
Their leadership team ordered team hats and distributed almost a hundred in total. CVRC faculty and staff could pick between the  baseball cap style worn by Cheryl Woodard and Maria Price Rapoza or and the beanie ski hat style worn by Howard Rockman. The hats were originally intended as a holiday gift for CVRC faculty and staff, but due to pandemic-related manufacturing issues they weren’t ready in time for the holidays, so the team used them to liven up the last Wednesday in January instead (a day when everyone needed a bit of cheer and a morale boost!).
baseball cap style worn by Cheryl Woodard and Maria Price Rapoza or and the beanie ski hat style worn by Howard Rockman. The hats were originally intended as a holiday gift for CVRC faculty and staff, but due to pandemic-related manufacturing issues they weren’t ready in time for the holidays, so the team used them to liven up the last Wednesday in January instead (a day when everyone needed a bit of cheer and a morale boost!).
Great idea and perfect timing with the recent cold weather!

Shout-out to CDU Team
Congratulations to the Cardiac Diagnostic Unit for completing a successful Intersocietal Accreditation Commission audit for Adult Echo, Adult Stress Echo, and Adult Transesophageal Echo! Thank you to everyone who worked through the process, and thanks to the entire team for maintaining the Duke Standards even during the accreditation “off season”. We are so proud of the work you do for our cardiac patients every day!
Great job, everyone!
It’s Duke Research Week 2022
January 31 – February 4: Duke Research Week 2022. Join us virtually for a week-long celebration of research underway at Duke! There is an excellent lineup of faculty lectures, panel discussions, “flash talks” with graduate students, trainees and postdoctoral fellows, and guest presenters for the Robert J. Lefkowitz, MD, Distinguished Lecture and Daubechies Lecture.
Check out the full agenda here: https://dukeresearchweek.vfairs.com/en/#distinguishedlectures
Duke Heart Family Grows Again!
Congratulations to newly minted grandfather, Richie Palma! His family welcomed twin boys two weeks ago. Owen Scott Horvath and Finn Lucas Horvath were born to Richie’s daughter Chloe and her husband Andrew. The family lives in Lafayette, CA. Richie reports that everyone is healthy and doing great!


National Wear Red Day
Friday, Feb. 4: National Wear Red Day. Help increase awareness of the impact cardiovascular disease has on all of us — wear red on Friday, Feb. 4! Please consider taking photos of your teams and sending them to us so that we can share them in Pulse throughout the month of February.
ICYMI: STAT First Opinion Piece By Galanos, et al.
Our Duke Palliative Care colleague, Tony Galanos, has co-authored an opinion piece that ran this week in STAT (Jan. 24, 2022). His co-authors are faculty members at UCSF. We think it’s worth a read: We all need help working through grief and hardship.
COVID-19 Updates
All the latest Clinical Operations updates related to COVID can be found at https://covid-19.dukehealth.org.
Duke Health’s Adopt-A-Unit is a matchmaking program that enables teams to actively support units continuing to fight on the frontlines of COVID through efforts such as meals, expressions of gratitude or other well-being support. If you are a leader interested in adopting a unit, please complete this smartsheet form. Once your information is received, a program member will be in touch to connect you with a unit in need that fits your budget and timeline. If you’d like to donate to our Healthcare Worker Unit Support fund, click here for details. Questions? Contact caring@duke.edu.
Reminder: All Duke University Health System (DUHS) and Private Diagnostic Clinic (PDC) team members, regardless of work location, are required to receive and provide documentation of a completed COVID-19 booster vaccination by 10 a.m. on Tuesday, Feb. 15, 2022, or within 28 days of their eligibility under CDC and state guidelines. More details are available in this email that was sent to all staff on Tuesday, Dec. 28.
Upcoming Events & Opportunities
Cardiology Grand Rounds
February 1: No CGR today.
February 8: No CGR today.
February 10: Topic TBA. Our guest will be AAMC President, Dr. David Skorton.
February 15: Topic TBA. Presenter will be Toi Spates.
Upcoming Duke Heart CME
April 23: Duke Sports Cardiology & Sudden Death in Athletes Symposium with course directors Jim Daubert and Bill Kraus. Virtual. For information or to register, contact Christy Darnell christy.darnell@duke.edu or 919-880-8686.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
January 21 — Adrian Hernandez
WebMD
Ivermectin as Potential COVID-19 Treatment Gets Studied at Duke University
https://duke.is/4rj8r
January 24 — Adrian Hernandez
Lakeland Ledger (FL)
Lakeland Regional joins national study to see if ivermectin is effective against COVID-19
https://duke.is/98db9
January 24 — Adrian Hernandez
Medscape
Ivermectin as Potential COVID-19 Treatment Gets Studied at Duke University
https://duke.is/jfanc
January 25 — G. Chad Hughes
Endovascular Today
STS and AATS Publish New Practice Guideline for Type B Aortic Dissection
https://duke.is/gn86g
January 25 — G. Chad Hughes
Vascular Specialist
https://duke.is/v99z8
January 25 — Andrew Wang
tctMD
Differing Advice for Infective Endocarditis Surgery Stems From Evidence Gaps
https://duke.is/z767z
January 25 — G. Chad Hughes
Cardiovascular Business
A fresh look at managing patients with type B aortic dissection
https://duke.is/nja47
January 26 — Derek Chew and Duke Clinical Research Institute
tctMD
CABG Provides ‘Good Value’ in Ischemic Cardiomyopathy
https://duke.is/b48ru
Duke Heart Pulse week ending January 23rd 2022
Highlights of the week:
Duke Health Welcomes Craig Albanese as Executive VP & COO
 Please join us in welcoming Craig Albanese, MD, MBA, to Duke University Health System! In October, Duke Health named Albanese, a seasoned health care executive and distinguished academic pediatric surgeon, as our next executive vice president and chief operating officer. He succeeds William Fulkerson, MD, who held the executive vice president position since 2010. Fulkerson stepped down from the role at the end of the 2021. Albanese began his new role on Monday, Jan. 17.
Please join us in welcoming Craig Albanese, MD, MBA, to Duke University Health System! In October, Duke Health named Albanese, a seasoned health care executive and distinguished academic pediatric surgeon, as our next executive vice president and chief operating officer. He succeeds William Fulkerson, MD, who held the executive vice president position since 2010. Fulkerson stepped down from the role at the end of the 2021. Albanese began his new role on Monday, Jan. 17.
As executive vice president, Albanese will serve as the senior leader overseeing the timely execution of DUHS goals and strategic priorities. He will work with other clinical enterprise leaders to deliver outstanding outcomes and care across Duke’s network, from the hospital to ambulatory clinics to care in homes and the community. He will also bring new insights to manage the organization’s COVID pandemic response, to support the health system’s faculty and staff and to further advance the clinical enterprise strategic plan.
Albanese was previously with NewYork-Presbyterian Hospital, where he served as senior vice president and chief medical officer of the $9.2 billion, 10-hospital academic health system.
Please click here to view a video released this week where he introduces himself to the Duke team: https://duke.is/57vus
Welcome to Duke, Dr. Albanese!
Endress Named Clinical Lead 3300 Effective Jan. 31st
 We are pleased to share that Gerald Endress, a clinical nurse on 3300, has been named Clinical Lead. Endress has worked on 3300 since July 2016 when he began as a new graduate RN. Gerald graduated from Durham Tech Community College and then received his BSN from Western Governors University. Gerald holds several leadership roles here at Duke including Charge Nurse, Preceptor, Responsiveness/Purposeful Rounding Project Manager, and is a member of the DUH Pain team and 3300 Scheduling committee. Endress holds an MS in Exercise Physiology from Old Dominion University and served for many years as the Fitness Director of the former Duke Diet & Fitness Center (now the Duke Lifestyle and Weight Management Center).
We are pleased to share that Gerald Endress, a clinical nurse on 3300, has been named Clinical Lead. Endress has worked on 3300 since July 2016 when he began as a new graduate RN. Gerald graduated from Durham Tech Community College and then received his BSN from Western Governors University. Gerald holds several leadership roles here at Duke including Charge Nurse, Preceptor, Responsiveness/Purposeful Rounding Project Manager, and is a member of the DUH Pain team and 3300 Scheduling committee. Endress holds an MS in Exercise Physiology from Old Dominion University and served for many years as the Fitness Director of the former Duke Diet & Fitness Center (now the Duke Lifestyle and Weight Management Center).
Gerald and his husband, Scott, have been married for five years and live in Raleigh. He is well-known for his great sense of humor. His new role as Clinical Lead is effective January 31st.
Congratulations, Gerald!
First Subject Enrolled in PATCHWORK
 Congratulations to Clinical Cardiac Electrophysiology fellow Zak Loring and his research team – they have enrolled their first patient in the PATCHWORK trial. This study follows the NIH Small Business Innovation Research (SBIR) grant on which Loring serves as PI: Non-invasive hemodynamic sensor patch for remote, early detection and prevention of heart failure with left bundle branch block. The team is targeting any patients who are referred for an echo who do not have complex congenital heart disease and are not actively being paced. If you have any questions about the study or wish to refer a patient, please contact Zak Loring, Melissa Lefevre or Danielle Wilson via email.
Congratulations to Clinical Cardiac Electrophysiology fellow Zak Loring and his research team – they have enrolled their first patient in the PATCHWORK trial. This study follows the NIH Small Business Innovation Research (SBIR) grant on which Loring serves as PI: Non-invasive hemodynamic sensor patch for remote, early detection and prevention of heart failure with left bundle branch block. The team is targeting any patients who are referred for an echo who do not have complex congenital heart disease and are not actively being paced. If you have any questions about the study or wish to refer a patient, please contact Zak Loring, Melissa Lefevre or Danielle Wilson via email.
Cardiac MRI-DN Wins Performance Award
 Congratulations to the Duke Heart Cardiac MRI-DN team – they earned the Patient Experience Monthly Performance Award for Outpatient Test & Treatment (OP T&T) Response to Concerns/Complaints Most Improved from Prior Quarter. Increased Top-Box score from July 2021 – September 2021 to October 2021 – December 2021.
Congratulations to the Duke Heart Cardiac MRI-DN team – they earned the Patient Experience Monthly Performance Award for Outpatient Test & Treatment (OP T&T) Response to Concerns/Complaints Most Improved from Prior Quarter. Increased Top-Box score from July 2021 – September 2021 to October 2021 – December 2021.
Some of the comments received by the team include:
- “Staff was great”
- “So sweet and great with my son. Absolutely loved them.”
- “Everyone was wonderful. We’re all very appreciative.”
Congratulations and keep up the great work!
Duke MLK Observances Continue
 Thursday, Jan. 27: It Starts with Me: Shifting Priorities to Create the Beloved Community. 11-11:45 a.m. via Zoom.
Thursday, Jan. 27: It Starts with Me: Shifting Priorities to Create the Beloved Community. 11-11:45 a.m. via Zoom.
Dr. King once said, “Our lives begin to end the day we become silent about things that matter.” At Duke Health we are putting actions behind these words as we raise our voices together to create a community that is stronger, healthier and more just. While our 2022 celebrations look different from years past, here’s how you can honor Dr. King’s legacy and further his selfless dream:
- Participate in the Jan. 27 Virtual Event. Click here to join “It Starts with Me: Shifting Priorities to Create the Beloved Community,” from 11 – 11:45 a.m. on Thursday, Jan. 27. The keynote speaker will be Damon Tweedy, MD, JD, Associate Professor of Psychiatry and Behavioral Sciences, Duke University School of Medicine, and author of “Black Man in a White Coat: A Doctor’s Reflections on Race and Medicine.” View the flyer and share as appropriate. Download the Zoom background.
- Consider volunteering. Check out opportunities available in the community via MLK service events or Activate Good.
COVID-19 Update
Consider joining the next Duke Health Leadership Town Hall tomorrow, January 24, to ask questions and hear updates on our COVID response, testing, and Omicron. The Zoom event can be accessed here.
Duke Health’s Adopt-A-Unit is a matchmaking program that enables teams to actively support units continuing to fight on the frontlines of COVID through efforts such as meals, expressions of gratitude or other well-being support. If you are a leader interested in adopting a unit, please complete this smartsheet form. Once your information is received, a program member will be in touch to connect you with a unit in need that fits your budget and timeline. If you’d like to donate to our Healthcare Worker Unit Support fund, click here for details. Questions? Contact caring@duke.edu.
Reminder: All Duke University Health System (DUHS) and Private Diagnostic Clinic (PDC) team members, regardless of work location, are required to receive and provide documentation of a completed COVID-19 booster vaccination by 10 a.m. on Tuesday, Feb. 15, 2022, or within 28 days of their eligibility under CDC and state guidelines. More details are available in this email that was sent to all staff on Tuesday, Dec. 28.
All the latest Clinical Operations updates related to COVID can be found at https://covid-19.dukehealth.org.
Upcoming Events & Opportunities
Cardiology Grand Rounds
January 25: End of Life in Heart Failure with Carmelo Milano, Chet Patel and Tony Galanos. 5 p.m., Webex.
February 1: Topic TBA. Presenter will be Caitlin Drescher.
February 10: Topic TBA. Our guest will be AAMC President, Dr. David Skorton.
February 15: Topic TBA. Presenter will be Toi Spates.
THIS WEEK: Dzau Distinguished Lecture in Global Health
Wednesday, Jan. 26: Restoring Global Solidarity on the Road to Pandemic Recovery — A Conversation with Dr. Agnes Binagwaho and Dr. Paul Farmer. Noon – 1:30 p.m., Zoom. Registration required: https://bit.ly/3tbw7SM.
Global health crises require global responses. But in the effort to control COVID-19, rising tides of nationalism have threatened collective action and deepened health inequities for many countries. In the face of these challenges to global health solidarity, the Duke Global Health Institute presents a probing discussion with two of the world’s preeminent global health experts – Dr. Agnes Binagwaho and Dr. Paul Farmer – on how the world failed to cooperate to fight the pandemic and how to chart a new vision to achieve health equity.
This interactive webinar will span two continents, with our featured speakers appearing at the University of Global Health Equity in Butaro, Rwanda. Dr. Gavin Yamey, professor of the practice of global health and public policy, will moderate the conversation from Duke, fielding questions from the online audience. Attendees will join using Zoom webinar, space permitting.
Call for Applicants: 2022 AAMC Early-Career Women Seminar
The Department of Medicine and Program for Women in Internal Medicine (PWIM) are pleased to announce sponsorship for one faculty member to attend the in-person AAMC Early-Career Women Seminar on July 19-22, 2022. This popular and highly interactive seminar provides women at the assistant professor level with foundational leadership knowledge and skills to help achieve career goals and thrive as successful leaders in academic medicine and science. If interested in being considered for sponsorship, please send an email to Kimberly Dorman (kimberly.dorman@duke.edu) by January 31, 2022. Members of the office of the Vice-Chair for Faculty Development and Diversity (Drs. Laura Svetkey and Daniella Zipkin) will select one faculty member to nominate to attend and will notify the applicant by email.
Duke Research Week 2022
January 31 – February 4: Registration is now open for Duke Research Week 2022. Join us virtually for a week-long celebration of research underway at Duke! There is an excellent lineup of faculty lectures, panel discussions, “flash talks” with graduate students, trainees and postdoctoral fellows, and guest presenters for the Robert J. Lefkowitz, MD, Distinguished Lecture and Daubechies Lecture. Check out the full agenda here: https://dukeresearchweek.vfairs.com/en/#distinguishedlectures
National Wear Red Day
Friday, Feb. 4: National Wear Red Day. Help increase awareness of the impact cardiovascular disease has on all of us — wear red on Friday, Feb. 4! We would love to have individual and team photos of you sporting your awareness gear to share in Pulse!!
Kisslo Spring Courses Announced
The 2022 Echo Techs Anatomic & Computer Dissections Course will be held on Saturday, Feb. 5 (Basic) and Saturday, Feb. 12 (Intermediate) for fellows, echo techs and attendings.
Registration is required. Seats fill fast and space is limited. Boxed breakfast/lunch will be provided (as allowed per Covid restrictions). If you would like more information or want to register, please email Dawne Smith. A calendar invitation to confirm registration will be sent to you or you may be added to a waitlist if the sessions are filled. First time participants are given priority. Please let her know if you have taken the course before. If you register and your plans change, please cancel as soon as possible by declining the calendar invite or contacting Dawne so that the open seat can be offered to someone on the waitlist.
The Basic Course on Feb. 5 will take place in the Duke South Amphitheater located across from the Duke South cafeteria entrance. The Intermediate Course on Feb. 12 will take place in the Main Lecture Hall in the Searle Center. Directions for access will be provided closer to the course date. Questions? Dawne can be reached at 919-668-1524 or dawne.t.smith@duke.edu.
Newly Announced CME
April 23: Duke Sports Cardiology & Sudden Death in Athletes Symposium with course directors Jim Daubert and Bill Kraus. Virtual. For information or to register, contact Christy Darnell christy.darnell@duke.edu or 919-880-8686.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
January 17 — Manesh Patel and Marat Fudim
HCP Live
7 FDA Drug Decisions To Watch Through July 2022
https://duke.is/jk9uj
January 18 — Sana Al-Khatib
Medscape
Subclinical Atrial Disease: A Window to Prevent AF and HF?
https://www.medscape.com/viewarticle/966784
January 19 — Duke University Health System
Kiss 95.1 FM
25 of the Best Employers to Work For in North Carolina
https://duke.is/yn9b5
January 20 — Adrian Hernandez
News & Observer
Ivermectin’s potential to treat COVID gets a serious look in Duke University study
https://duke.is/r9dxy###
Division of Cardiology Publications Indexed in PubMed January 13-19, 2022
Assimon MM, Pun PH, Wang LC, Al-Khatib SM, Brookhart MA, Weber DJ, Winkelmayer WC, Flythe JE. Analysis of Respiratory Fluoroquinolones and the Risk of Sudden Cardiac Death Among Patients Receiving Hemodialysis. JAMA Cardiol 2022;7(1):75-83. PM: 34668928.
Berger JS, Kornblith LZ, Gong MN, Reynolds HR, Cushman M, Cheng Y, McVerry BJ, Kim KS, Lopes RD, Atassi B, Berry S, Bochicchio G, de Oliveira Antunes M, Farkouh ME, Greenstein Y, Hade EM, Hudock K, Hyzy R, Khatri P, Kindzelski A, Kirwan BA, Baumann Kreuzi. Effect of P2Y12 Inhibitors on Survival Free of Organ Support Among Non-Critically Ill Hospitalized Patients With COVID-19: A Randomized Clinical Trial. JAMA 2022;327(3):227-236. PM: 35040887.
Cavender MA, Harrington RA, Stone GW, Steg PG, Gibson CM, Hamm CW, Price MJ, Lopes RD, Leonardi S, Deliargyris EN, Prats J, Mahaffey KW, White HD, Bhatt DL. Ischemic Events Occur Early in Patients Undergoing Percutaneous Coronary Intervention and Are Reduced With Cangrelor: Findings From CHAMPION PHOENIX. Circ Cardiovasc Interv 2022;15(1):e010390. PM: 34915723.
Doll JA, Nelson AJ, Kaltenbach LA, Wojdyla D, Waldo SW, Rao SV, Wang TY. Percutaneous Coronary Intervention Operator Profiles and Associations With In-Hospital Mortality. Circ Cardiovasc Interv 2022;15(1):e010909. PM: 34847693.
Felker GM, Solomon SD, Claggett B, Diaz R, McMurray JJV, Metra M, Anand I, Crespo-Leiro MG, Dahlström U, Goncalvesova E, Howlett JG, MacDonald P, Parkhomenko A, Tomcsányi J, Abbasi SA, Heitner SB, Hucko T, Kupfer S, Malik FI, Teerlink JR. Assessment of Omecamtiv Mecarbil for the Treatment of Patients With Severe Heart Failure: A Post Hoc Analysis of Data From the GALACTIC-HF Randomized Clinical Trial. JAMA Cardiol 2022;7(1):26-34. PM: 34643642.
Gandhi S, Garratt KN, Li S, Wang TY, Bhatt DL, Davis LL, Zeitouni M, Kontos MC. Ten-Year Trends in Patient Characteristics, Treatments, and Outcomes in Myocardial Infarction From National Cardiovascular Data Registry Chest Pain-MI Registry. Circ Cardiovasc Qual Outcomes 2022;15(1):e008112. PM: 35041478.
Haghighat L, Reinhardt SW, Saly DL, Lu D, Matsouaka RA, Wang TY, Desai NR. Comfort Measures Only in Myocardial Infarction: Prevalence of This Status, Change Over Time, and Predictors From a Nationwide Study. Circ Cardiovasc Qual Outcomes 2022;15(1):e007610. PM: 35041476.
Huffman KM, Parker DC, Bhapkar M, Racette SB, Martin CK, Redman LM, Das SK, Connelly MA, Pieper CF, Orenduff M, Ross LM, Ramaker ME, Dorling JL, Rosen CJ, Shalaurova I, Otvos JD, Kraus VB, Kraus WE. Calorie restriction improves lipid-related emerging cardiometabolic risk factors in healthy adults without obesity: Distinct influences of BMI and sex from CALERIE™ a multicentre, phase 2, randomised controlled trial. EClinicalMedicine 2022;43:101261. PM: 35028547.
Li C, Qu L, Matz AJ, Murphy PA, Liu Y, Manichaikul AW, Aguiar D, Rich SS, Herrington DM, Vu D, Johnson WC, Rotter JI, Post WS, Vella AT, Rodriguez-Oquendo A, Zhou B. AtheroSpectrum Reveals Novel Macrophage Foam Cell Gene Signatures Associated With Atherosclerotic Cardiovascular Disease Risk. Circulation 2022;145(3):206-218. PM: 34913723.
Lima FV, Manandhar P, Wojdyla D, Wang T, Aronow HD, Kadiyala V, Weissler EH, Madan N, Gilchrist IC, Grines C, Abbott JD. Percutaneous Coronary Intervention Following Diagnostic Angiography by Noninterventional Versus Interventional Cardiologists: Insights From the CathPCI Registry. Circ Cardiovasc Interv 2022;15(1):e011086. PM: 34933569.
Lopez-Sendon JL, Cyr DD, Mark DB, Bangalore S, Huang Z, White HD, Alexander KP, Li J, Nair RG, Demkow M, Peteiro J, Wander GS, Demchenko EA, Gamma R, Gadkari M, Poh KK, Nageh T, Stone PH, Keltai M, Sidhu M, Newman JD, Boden WE, Reynolds HR, Chaitman BR. Effects of initial invasive vs. initial conservative treatment strategies on recurrent and total cardiovascular events in the ISCHEMIA trial. Eur Heart J 2022;43(2):148-149. PM: 34514494.
Mann DL, Givertz MM, Vader JM, Starling RC, Shah P, McNulty SE, Anstrom KJ, Margulies KB, Kiernan MS, Mahr C, Gupta D, Redfield MM, Lala A, Lewis GD, DeVore AD, Desvigne-Nickens P, Hernandez AF, Braunwald E. Effect of Treatment With Sacubitril/Valsartan in Patients With Advanced Heart Failure and Reduced Ejection Fraction: A Randomized Clinical Trial. JAMA Cardiol 2022;7(1):17-25. PM: 34730769.
Newby LK. A new biomarker of acute coronary ischaemia: from bench to bedside? Eur Heart J 2022;43(2):164-166. PM: 34791138.
Nørgaard BL, Gaur S, Fairbairn TA, Douglas PS, Jensen JM, Patel MR, Ihdayhid AR, Ko BSH, Sellers SL, Weir-McCall J, Matsuo H, Sand NPR, Øvrehus KA, Rogers C, Mullen S, Nieman K, Parner E, Leipsic J, Abdulla J. Prognostic value of coronary computed tomography angiographic derived fractional flow reserve: a systematic review and meta-analysis. Heart 2022;108(3):194-202. PM: 34686567.
Reed SD, Yang JC, Rickert T, Johnson FR, Gonzalez JM, Mentz RJ, Krucoff MW, Vemulapalli S, Adamson PB, Gebben DJ, Rincon-Gonzalez L, Saha A, Schaber D, Stein KM, Tarver ME, Bruhn-Ding D. Quantifying Benefit-Risk Preferences for Heart Failure Devices: A Stated-Preference Study. Circ Heart Fail 2022;15(1):e008797. PM: 34937393.
Rymer JA, Li S, Pun PH, Thomas L, Wang TY. Racial Disparities in Invasive Management for Patients With Acute Myocardial Infarction With Chronic Kidney Disease. Circ Cardiovasc Interv 2022;15(1):e011171. PM: 34915722.
Rymer JA, Narcisse D, Cosiano M, Tanaka J, McDermott MM, Treat-Jacobson DJ, Conte MS, Tuttle B, Patel MR, Smolderen KG. Patient-Reported Outcome Measures in Symptomatic, Non-Limb-Threatening Peripheral Artery Disease: A State-of-the-Art Review. Circ Cardiovasc Interv 2022;15(1):e011320. PM: 34937395.
Takagi H, Leipsic JA, McNamara N, Martin I, Fairbairn TA, Akasaka T, Nørgaard BL, Berman DS, Chinnaiyan K, Hurwitz-Koweek LM, Pontone G, Kawasaki T, Rønnow Sand NP, Jensen JM, Amano T, Poon M, Øvrehus KA, Sonck J, Rabbat MG, Mullen S, De Bruyne B, et al. Trans-lesional fractional flow reserve gradient as derived from coronary CT improves patient management: ADVANCE registry. J Cardiovasc Comput Tomogr 2022;16(1):19-26. PM: 34518113.
Timmons JA, Anighoro A, Brogan RJ, Stahl J, Wahlestedt C, Farquhar DG, Taylor-King J, Volmar CH, Kraus WE, Phillips SM. A human-based multi-gene signature enables quantitative drug repurposing for metabolic disease. Elife 2022;11:10.7554/eLife.68832. PM: 35037854.
Vora AN, Swaminathan RV. Posting Another Win for Intravascular Imaging: Moving Away From Angiography-Only Percutaneous Coronary Intervention Toward a More Comprehensive Approach. Circ Cardiovasc Interv 2022;15(1):e011670. PM: 35041451.
Wang H, Noordam R, Cade BE, Schwander K, Winkler TW, Lee J, Sung YJ, Bentley AR, Manning AK, Aschard H, Kilpeläinen TO, Ilkov M, Brown MR, Horimoto AR, Richard M, Bartz TM, Vojinovic D, Lim E, Nierenberg JL, Liu Y, Chitrala K, Rankinen T, Musani SK, et al. Multi-ancestry genome-wide gene-sleep interactions identify novel loci for blood pressure. Mol Psychiatry 2021;26(11):6293-6304. PM: 33859359.
Yancy CW, Hernandez AF, Fonarow GC. Identifying Treatments for Stage C2 Heart Failure. JAMA Cardiol 2022;7(1):34-35. PM: 34643645.
Duke Heart Pulse – Week Ending January 16th 2022
Chief’s message:
Hopefully you all will get a moment this weekend to enjoy the North Carolina “Snow.” As we reflect on MLK day, we remember the non-violent protests and consistent work of Dr. King to advocate and fight for justice and civil rights for all. I am including some of his words below to consider in our upcoming days of action and service.
“Of all the forms of inequality, injustice in healthcare is the most shocking and inhumane.”
“Life’s most persistent and urgent question is, ‘What are you doing for others?”
“The time is always right to do what is right.”
Rounding this last week in the CICU, I was again reminded by the tremendous dedication of our fellows, residents, nurses, respiratory therapists, pharmacists, APPs, faculty, and countless other staff that are continually working as teams to help care for our patients and each other. Thank you all for the unwavering dedication, professionalism, and clinical expertise.
Highlights of the week:
Rymer, Greene Selected for 2022 LEADER Program

Duke Heart faculty members Jennifer Rymer and Stephen Greene are among 36 Duke
physician scientists selected to the 2022 cohort for Duke’s course on Leadership Development for Researchers (LEADER). The faculty development program is an interactive 5-month series designed for junior faculty who are leading research teams. The leadership course is designed to help build critical skills for leading teams, such as conflict management, effective mentorship, negotiation skills, leading with emotional intelligence and balancing competing priorities.
Congratulations, Jenn and Steve!
7E Earns Beacon Award for Excellence
We are excited to share that our Duke Heart Cardiac Intensive Care Unit (ICU) has received a Beacon Award for Excellence from the American Association of Critical-Care Nurses (AACN)!
This national award recognizes caregivers in units whose consistent and systematic approach to evidence-based care optimizes patient outcomes. Units that receive this national recognition serve as role models to others across the country on their journey to excellent patient and family care. The application reviewers noted the unit’s strong sense of collaboration amongst teams to drive patient outcomes and improve quality of care.
Beacon Awards are national awards recognizing nursing excellence and speak to the caliber of nursing provided on the unit. A team must apply for consideration and must meet clearly defined criteria across five categories: leadership structures and systems; appropriate staffing and staff engagement; effective communication, knowledge management and learning development; evidence-based practice and processes; and outcome measurements.
Only 20 Cardiac ICUs in the U.S. currently hold this designation. We are incredibly proud of 7 East!
Congratulations and way to go, team!!!
![]()

![]()
Kudos to Eleazu!
Kristin Newby shared a terrific note with us that she received this week about cardiology fellow Ijeoma Eleazu:
“Hi Dr. Newby,
I wanted to write a quick message singling out Dr. Eleazu for special praise. Our team had a difficult night last night, not only  because of challenges in patient care, but also with the additional stress on everyone, largely because of Covid. Despite the multiple codes and many other challenges, Dr. Eleazu was a true leader, providing a steady and reassuring hand throughout. She demonstrated unflappability despite the increased stress and difficulties in patient care. For the housestaff, she was a tremendous advocate, stepping up when we needed input or a voice of support. Throughout it all, she continue to teach, challenging us to rise the occasion by allowing us to formulate our own plans rather than dictating.
because of challenges in patient care, but also with the additional stress on everyone, largely because of Covid. Despite the multiple codes and many other challenges, Dr. Eleazu was a true leader, providing a steady and reassuring hand throughout. She demonstrated unflappability despite the increased stress and difficulties in patient care. For the housestaff, she was a tremendous advocate, stepping up when we needed input or a voice of support. Throughout it all, she continue to teach, challenging us to rise the occasion by allowing us to formulate our own plans rather than dictating.
I am thankful for her leadership and exemplary performance and wanted to make sure it was recognized.
Best regards, Hubie Haywood”
Great work, Ijeoma!
Kudos to Whitney Bakimli!
One of our excellent Cardiothoracic Surgery Step-down Unit nurses, Whitney Bakimli, has received a Great Catch from Duke University Hospital leadership!
Whitney noticed two identical orders for Lasix for a patient. While the total dose was not unusual, she was concerned that it might be too high for this particular patient. Whitney contacted the provider and learned that the order was mistakenly duplicated.
Great job, Whitney!
MLK Commemoration 2022
This year’s Martin Luther King, Jr. keynote address will take place at 3 p.m. today (Sunday, Jan. 16). How Long Must We Wait: Striving For the Beloved Community will be given by historian and social activist, Keeanga-Yamahtta Taylor. The event, originally planned to occur in Duke Chapel, has been moved to a virtual event that will be live streamed due to the pending winter storm. There are several community service opportunities scheduled this week in honor of MLK Day. We encourage you to check them out. Information about both the keynote address and service opportunities are available on the Duke MLK Commemoration website (https://mlk.duke.edu).

COVID-19 Update
As of Friday, Jan. 14, Duke Health has moved from Tier 2 (Limited Access) to Tier 3 (Restricted Access) of our visitation guidelines. The transition was made based on recommendations from the CDC and our infectious disease experts due to the increased COVID infection rates in our community and among team members.
Documentation regarding visitation restrictions as well as the latest Clinical Operations updates regarding COVID-19 and links to the most recent DUHS Leadership Virtual Town Hall recordings can be found here: https://covid-19.dukehealth.org.
Reminder: All Duke University Health System (DUHS) and Private Diagnostic Clinic (PDC) team members, regardless of work location, are required to receive and provide documentation of a completed COVID-19 booster vaccination by 10 a.m. on Tuesday, Feb. 1, 2022, or within 28 days of their eligibility under CDC and state guidelines. More details are available in this email that was sent to all staff on Tuesday, Dec. 28.
Critical Need for Blood Donations
 On Tuesday, the American Red Cross announced a national blood crisis – the worst shortage in more than 10 years. If you’d like to donate, there are several upcoming blood drives scheduled to take place in The Great Hall at Trent Semans Center:
On Tuesday, the American Red Cross announced a national blood crisis – the worst shortage in more than 10 years. If you’d like to donate, there are several upcoming blood drives scheduled to take place in The Great Hall at Trent Semans Center:
- Thursday, Jan. 20 from 11 a.m. to 4 p.m.
- Tuesday, Feb. 1 from 9 a.m. to 3 p.m.
- Tuesday, Feb. 15 from 9 a.m. to 3 p.m
The best way to locate a drive in your area and to schedule a donation is by visiting: https://www.redcrossblood.org/.
ICYMI: Durham County Offering Boosters to Ages 12-15, Third Doses to Ages 5-11; Pfizer Booster Waiting Period Reduced to Five Months
As of Monday, January 10, the Durham County Department of Public Health expanded COVID-19 vaccination eligibility at its vaccination clinic. They will offer booster doses of Pfizer COVID-19 vaccines for all people ages 12-15, and third doses of Pfizer vaccines for children ages 5-11 who are moderately to severely immunocompromised. Additionally, booster vaccinations will now be available for all people 12 and older five months after they complete a primary Pfizer vaccination series, reducing the waiting period from its previous length of six months. To learn more, visit: https://bit.ly/3qsa4Fm.
Upcoming Events & Opportunities
Cardiology Grand Rounds
January 18: The Ultimate ‘Anti-Racism Statement’ Medicine Can Make is to Diversify its Ranks with Quinn Capers, IV of the University of Texas Southwestern Medical Center. 5 p.m. via Webex.
January 20: Road to Heart Transplantation: Challenges, Opportunities, New Frontiers with Mary Keebler, University of Pittsburgh Medical Center. 5 p.m., Webex.
January 25: Palliative Care Grand Rounds with Carmelo Milano, Chet Patel and Tony Galanos. Time and location TBA.
February 1: Topic TBA. Presenter will be Caitlin Drescher.
February 10: Topic TBA. Our guest will be AAMC President, Dr. David Skorton.
February 15: Topic TBA. Presenter will be Toi Spates.
Dzau Distinguished Lecture in Global Health
Wednesday, Jan. 26: Restoring Global Solidarity on the Road to Pandemic Recovery — A Conversation with Dr. Agnes Binagwaho and Dr. Paul Farmer. Noon – 1:30 p.m., Zoom. Registration required: https://bit.ly/3tbw7SM.
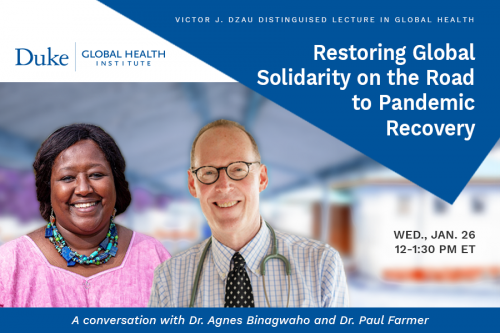 Global health crises require global responses. But in the effort to control COVID-19, rising tides of nationalism have threatened collective action and deepened health inequities for many countries. In the face of these challenges to global health solidarity, the Duke Global Health Institute presents a probing discussion with two of the world’s preeminent global health experts – Dr. Agnes Binagwaho and Dr. Paul Farmer – on how the world failed to cooperate to fight the pandemic and how to chart a new vision to achieve health equity.
Global health crises require global responses. But in the effort to control COVID-19, rising tides of nationalism have threatened collective action and deepened health inequities for many countries. In the face of these challenges to global health solidarity, the Duke Global Health Institute presents a probing discussion with two of the world’s preeminent global health experts – Dr. Agnes Binagwaho and Dr. Paul Farmer – on how the world failed to cooperate to fight the pandemic and how to chart a new vision to achieve health equity.
This interactive webinar will span two continents, with our featured speakers appearing at the University of Global Health Equity in Butaro, Rwanda. Dr. Gavin Yamey, professor of the practice of global health and public policy, will moderate the conversation from Duke, fielding questions from the online audience. Attendees will join using Zoom webinar, space permitting.
Call for Applicants: 2022 AAMC Early-Career Women Seminar
The Department of Medicine and Program for Women in Internal Medicine (PWIM) are pleased to announce sponsorship for one faculty member to attend the in-person AAMC Early-Career Women Seminar on July 19-22, 2022. This popular and highly interactive seminar provides women at the assistant professor level with foundational leadership knowledge and skills to help achieve career goals and thrive as successful leaders in academic medicine and science. If interested in being considered for sponsorship, please send an email to Kimberly Dorman (kimberly.dorman@duke.edu) by January 31, 2022. Members of the office of the Vice-Chair for Faculty Development and Diversity (Drs. Laura Svetkey and Daniella Zipkin) will select one faculty member to nominate to attend and will notify the applicant by email.
Duke Research Week 2022
January 31 – February 4: Registration is now open for Duke Research Week 2022. Join us virtually for a week-long celebration of research underway at Duke! There is an excellent lineup of faculty lectures, panel discussions, “flash talks” with graduate students, trainees and postdoctoral fellows, and guest presenters for the Robert J. Lefkowitz, MD, Distinguished Lecture and Daubechies Lecture. Check out the full agenda here: https://dukeresearchweek.vfairs.com/en/#distinguishedlectures
National Wear Red Day
Friday, Feb. 4: National Wear Red Day. Help increase awareness of the impact cardiovascular disease has on all of us — wear red on Friday, Feb. 4! We would love to have individual and team photos of you sporting your awareness gear to share in Pulse!!
Kisslo Spring Courses Announced
The 2022 Echo Techs Anatomic & Computer Dissections Course will be held on Saturday, Feb. 5 (Basic) and Saturday, Feb. 12 (Intermediate) for fellows, echo techs and attendings.
Registration is required. Seats fill fast and space is limited. Boxed breakfast/lunch will be provided (as allowed per Covid restrictions). If you would like more information or want to register, please email Dawne Smith. A calendar invitation to confirm registration will be sent to you or you may be added to a waitlist if the sessions are filled. First time participants are given priority. Please let her know if you have taken the course before. If you register and your plans change, please cancel as soon as possible by declining the calendar invite or contacting Dawne so that the open seat can be offered to someone on the waitlist.
The Basic Course on Feb. 5 will take place in the Duke South Amphitheater located across from the Duke South cafeteria entrance. The Intermediate Course on Feb. 12 will take place in the Main Lecture Hall in the Searle Center. Directions for access will be provided closer to the course date. Questions? Dawne can be reached at 919-668-1524 or dawne.t.smith@duke.edu.
Newly Announced CME
April 23: Duke Sports Cardiology & Sudden Death in Athletes Symposium with course directors Jim Daubert and Bill Kraus. Virtual. For information or to register, contact Christy Darnell christy.darnell@duke.edu or 919-880-8686.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
January 7 — Robert McGarrah
The Washington Post
https://duke.is/gmcqy
January 8 — Duke University Hospital (Carmat)
Healio/Cardiology
Most read in HF of 2021: Empagliflozin for HFpEF, COVID-19-related myocarditis and more
https://duke.is/gmcqy
January 12 — Maitreya Thakkar
Healio/Cardiology
New perspectives on CV risk assessment of prospective kidney recipients, donors
https://duke.is/6738f
Division of Cardiology Publications Indexed in PubMed January 6-12, 2022
Bishawi M, Milano C, Gaca J, Carr K, Wang A, Glower DD. The outcome of mitral repair for degenerative versus ischemic mitral regurgitation using a single complete ring. J Card Surg 2022;37(2):290-296. PM: 34665478.
Califf RM, Wong C, Doraiswamy PM, Hong DS, Miller DP, Mega JL. Biological and clinical correlates of the patient health questionnaire-9: exploratory cross-sectional analyses of the baseline health study. BMJ Open 2022;12(1):e054741. PM: 34983769.
Devore AD, Schlendorf KH. HCV Positive Allograft Use in Heart Transplant: A Silver Lining to an Epidemic. J Card Fail 2022;28(1):42-43. PM: 34628017.
Fox KAA, Virdone S, Bassand JP, Camm AJ, Goto S, Goldhaber SZ, Haas S, Kayani G, Koretsune Y, Misselwitz F, Oh S, Piccini JP, Parkhomenko A, Sawhney JPS, Stepinska J, Turpie AGG, Verheugt FWA, Kakkar AK. Do baseline characteristics and treatments account for geographical disparities in the outcomes of patients with newly diagnosed atrial fibrillation? The prospective GARFIELD-AF registry. BMJ Open 2022;12(1):e049933. PM: 34996784.
Friedman DJ, Overmann JA, Fish JM, Gaeta SA, Tranter JH, Thao R, Piccini JP. Continuous and discontinuous radiofrequency energy delivery on the atrial free wall: Lesion transmurality, width, and biophysical characteristics. Heart Rhythm O2 2021;2(6Part A):635-641. PM: 34988509.
Lala A, Mentz RJ. The JCF Reviewer Mentorship Program. J Card Fail 2022;28(1):1-2. PM: 35000756.
Lam KY, Reardon MJ, Yakubov SJ, Modine T, Fremes S, Tonino PAL, Tan ME, Gleason TG, Harrison JK, Hughes GC, Oh JK, Head SJ, Huang J, Deeb GM. Surgical Sutureless and Sutured Aortic Valve Replacement in Low-risk Patients. Ann Thorac Surg 2022;113(2):616-622. PM: 33794164.
Oshunbade AA, Lirette ST, Windham BG, Shafi T, Hamid A, Gbadamosi SO, Tin A, Yimer WK, Tibuakuu M, Clark D, Kamimura D, Lutz EA, Mentz RJ, Fox ER, Butler J, Butler KR, Garovic VD, Turner ST, Mosley TH, Hall ME. Hypertensive Diseases in Pregnancy and Kidney Function Later in Life: The Genetic Epidemiology Network of Arteriopathy (GENOA) Study. Mayo Clin Proc 2022;97(1):78-87. PM: 34565606.
Packer DL, Mark DB, Lee KL. CABANA: underpowered and with detrimental protocol changes: is ‘ablation salvation’?-Reply by the authors of the CABANA trial. Europace 2022;24(1):3. PM: 34792125.
Patel MR, Jeremias A, Maehara A, Matsumura M, Zhang Z, Schneider J, Tang K, Talwar S, Marques K, Shammas NW, Gruberg L, Seto A, Samady H, Sharp ASP, Ali ZA, Mintz G, Davies J, Stone GW. 1-Year Outcomes of Blinded Physiological Assessment of Residual Ischemia After Successful PCI: DEFINE PCI Trial. JACC Cardiovasc Interv 2022;15(1):52-61. PM: 34991824.
Rao VN, Obeid MJ, Rigiroli F, Russell SD, Patel CB, Molinger J, Gupta RT, Agarwal R, Fudim M. Pericardial Adipose Tissue Volume and Left Ventricular Assist Device-Associated Outcomes. J Card Fail 2022;28(1):149-153. PM: 34274515.
Rasmussen PV, Pallisgaard JL, Hansen ML, Gislason GH, Torp-Pedersen C, Ruwald M, Alexander KP, Lopes RD, Al-Khatib SM, Dalgaard F. Treatment of older patients with atrial fibrillation by morbidity burden. Eur Heart J Qual Care Clin Outcomes 2022;8(1):23-30. PM: 32857834.
Rimbach R, Yamada Y, Sagayama H, Ainslie PN, Anderson LF, Anderson LJ, Arab L, Baddou I, Bedu-Addo K, Blaak EE, Blanc S, Bonomi AG, Bouten CVC, Bovet P, Buchowski MS, Butte NF, Camps SGJA, Close GL, Cooper JA, Das SK, Dugas LR, Ekelund U, Entringer S. Total energy expenditure is repeatable in adults but not associated with short-term changes in body composition. Nat Commun 2022;13(1):99. PM: 35013190.
Sharma A, Zheng Y, Ezekowitz JA, Westerhout CM, Udell JA, Goodman SG, Armstrong PW, Buse JB, Green JB, Josse RG, Kaufman KD, McGuire DK, Ambrosio G, Chuang LM, Lopes RD, Peterson ED, Holman RR. Cluster Analysis of Cardiovascular Phenotypes in Patients With Type 2 Diabetes and Established Atherosclerotic Cardiovascular Disease: A Potential Approach to Precision Medicine. Diabetes Care 2022;45(1):204-212. PM: 34716214.
Steinberg BA, Zhang M, Bensch J, Lyons A, Bunch TJ, Piccini JP, Siu A, Spertus JA, Stehlik J, Wohlfahrt P, Greene T, Hess R, Fang JC. Quantifying the Impact of Atrial Fibrillation on Heart Failure-Related Patient-Reported Outcomes in the Utah mEVAL Program. J Card Fail 2022;28(1):13-20. PM: 34324927.
Tamirisa KP, Al-Khatib SM, Mohanty S, Han JK, Natale A, Gupta D, Russo AM, Al-Ahmad A, Gillis AM, Thomas KL. Racial and Ethnic Differences in the Management of Atrial Fibrillation. CJC Open 2021;3(12 Suppl):S137-S148. PM: 34993443.
Tanawuttiwat T, Stebbins A, Marquis-Gravel G, Vemulapalli S, Kosinski AS, Cheng A. Use of Direct Oral Anticoagulant and Outcomes in Patients With Atrial Fibrillation after Transcatheter Aortic Valve Replacement: Insights From the STS/ACC TVT Registry. J Am Heart Assoc 2022;11(1):e023561. PM: 34970918.
Tcheng JE, Nguyen MV, Brann HW, Clarke PA, Pfeiffer M, Pleasants JR, Shelton GW, Kelly JF. The Medical Device Unique Device Identifier as the Single Source of Truth in Healthcare Enterprises – Roadmap for Implementation of the Clinically Integrated Supply Chain. Med Devices (Auckl) 2021;14:459-467. PM: 34992475.
Wang P, Castellani CA, Yao J, Huan T, Bielak LF, Zhao W, Haessler J, Joehanes R, Sun X, Guo X, Longchamps RJ, Manson JE, Grove ML, Bressler J, Taylor KD, Lappalainen T, Kasela S, Van Den Berg DJ, Hou L, Reiner A, Liu Y, Boerwinkle E, Smith JA, Peyser PA. Epigenome-wide association study of mitochondrial genome copy number. Hum Mol Genet 2021;31(2):309-319. PM: 34415308.
Warraich HJ, Kitzman DW, Nelson MB, Mentz RJ, Rosenberg PB, Lev Y, Whellan DJ. Older Patients With Acute Decompensated Heart Failure Who Live Alone: An Analysis From the REHAB-HF Trial. J Card Fail 2022;28(1):161-163. PM: 34147611.
Duke Heart Pulse week ending January 9th 2022
Chief’s message:
Hope you all had some time with family and had a happy new year. We know the upcoming weeks and months will be challenging to all of us, including many of our colleagues, staff, faculty and fellows in healthcare. We appreciate the continued diligence across the Heart Center in helping care for our patients and each other.
Highlights of the week:
Kudos Across Duke Heart & to Center of Excellence Staff!
The latest surge in COVID-19 infections has posed great challenges across all areas of Duke Heart and we recognize how stressful this has been to each member of our team and to our colleagues across the Health System. We appreciate the flexibility our entire team is showing and your willingness to support one another. THANK YOU for all that you’re doing.
The Duke Heart Leadership team has check-ins throughout the day to monitor and assess needs during this rapidly changing situation. If you are in need of resources, supplies or other support please do not hesitate to reach out to us. We will do everything we can to get you what you need as soon as possible.
The leadership team for Duke Heart is deeply grateful for all efforts across the Heart Center as we respond to the current surge in infections and the impact that is having on staffing levels. We especially want to thank Joe Kelly, Melissa Williams and the full Center of Excellence team for stepping up, saying ‘yes’, and mobilizing their team to help.
After a big increase in the number of Duke Health employees who have been out sick with COVID, nurses across the health system — including a number of nurses from the Duke Heart Center of Excellence — who do not work directly in patient care settings are assisting with efforts to return employees to work. They have been making calls to employees and screening them for suitability to return to work. They are collaborating closely with the Employee Occupational Health and Wellness (EOHW) team to apply the latest recommendations on reducing the risk of infectious spread in the workplace. Employees with active symptoms which are not improving are being re-assigned to an EOHW case manager.
Again, thank you for all that you’re doing. We will continue to support one another and our patients and we will get through this, together. Keep up the outstanding work!
Heart Transplants Hit 116 for Year; Further Reduction in Wait Times Noted
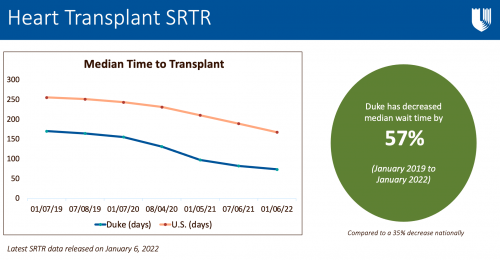 Our Duke Heart Transplant team completed a remarkable 116 heart transplants in 2021 and the latest Scientific Registry of Transplant Recipients (SRTR) report — released on Thursday, January 6 — shows excellent outcomes as well as a reduction in our median wait times.
Our Duke Heart Transplant team completed a remarkable 116 heart transplants in 2021 and the latest Scientific Registry of Transplant Recipients (SRTR) report — released on Thursday, January 6 — shows excellent outcomes as well as a reduction in our median wait times.
“We continue to have year over year growth and this past year was our highest ever at 116 total heart transplants,” says Adam DeVore, medical director, Duke Heart Transplantation Program. “Our wait times have been the lowest in the southeast for a while and a lot of that is due to the DCD program and changes around that. We have also seen an increase in referrals from other transplant centers throughout the region, which we attribute to our ability to get patients transplanted faster as well as good outcomes.”
Based on data reported to SRTR from October 2018 through December 31, 2021, Duke’s median wait time has decreased by 57 percent.
“Our highest ever volume, with continued excellent results, reflects the amazing work by the entire team, says Jacob Schroder, MD, surgical director, Duke Heart Transplantation Program and Co-Director, Cardiothoracic Surgical Intensive Care Unit. “We continue to be leaders, and innovators, in advanced heart failure therapies, not only in the U.S. but the world. 116 is just the beginning.”
DeVore says it’s important to recognize that these results are not just the result of the transplant program, but the efforts of all members across Duke Heart Center.
“The transplant program itself is a huge team made up of people from surgery, anesthesia and cardiology and the latest data demonstrates the hard work of our team across those areas,” DeVore added. “However, this is also very much a celebration of the Heart Center. These patients go to the Echo lab, they get MRIs, they go to the Catheterization lab, they sometimes come into the Health System because they need an EP procedure… and then maybe at some point they need a transplant. So, not only is this great news for the heart transplant program, but it’s a reflection of the work done across Duke Heart.”
We could not have said it better. Impressive work, across the board. Congratulations, team!
Bryner Named Assistant Program Director, CT Surgery Residency Program
 We are pleased to share that Ben Bryner has been named the new assistant program director of our Cardiothoracic Surgery Residency Program.
We are pleased to share that Ben Bryner has been named the new assistant program director of our Cardiothoracic Surgery Residency Program.
In a note to the cardiothoracic faculty in December, Dr. Edward P. Chen, chief of the division, commented: “During his time on faculty, Dr. Bryner has proven to be a tireless educator committed to providing our resident learners with a rich and comprehensive training experience. We look forward to his leadership in our training program as well as his development of creative and innovative methods to further advance and improve upon our education mission. Dr. Bryner will continue the tradition of excellence in this role established by his predecessor, Dr. Brittany Zwischenberger. I would also like to express my sincere gratitude to Dr. Zwischenberger for her devoted service to our residency program over the last several years.”
Congrats, Ben!
Gutierrez Selected for ACC Emerging Faculty Leadership Academy

Duke Heart
Congratulations to Tony Gutierrez! He was recently notified of his selection from a competitive group of candidates to participate
in the 2022 American College of Cardiology’s Rick Nishimura, MD, MACC and Patrick T. O’Gara, MD, MACC Emerging Faculty Leadership Academy. The leadership course will be held May 1-3 at Heart House in Washington, DC.
Well deserved!
Snider Named President-Elect of AmSECT
Duke Heart perfusionist William Scott Snider has been named President-Elect of the American Society of Extracorporeal Technology (AmSECT) Board of Directors. The term begins in April. Snider currently serves on the Board as Treasurer. He also chairs AmSECT’s Perfusion Without Borders subcommittee.
We asked him recently about his experiences with AmSECT and his commitment to volunteering:
“Like a lot of society volunteers, I became a member of AmSECT as a student and watched from a distance for a long time — not really understanding all that a professional society can mean or the long history behind it and the many volunteers who spend hours upon hours of time in the pursuit of professional excellence within our profession,” Snider says. “As I have become more involved over the years, I have gained a better appreciation for all of these things and am very grateful for all that has been done to grow our field and keep it strong. I volunteer because it’s very exciting to me to be a small part of that big vision.
“My path in AmSECT and my career at Duke began at almost the same time, and each have rewarded me in very similar ways. Each day I’m humbled by the quality of character of each of the nurses, doctors and allied health professionals that I work with. The vision statement of Duke, ‘to educate and discover,’ is very similar to the mission statement of AmSECT. For more than 50 years, they have been driven by a goal to support our workforce as they support their patients. It’s a vision that’s shared by everyone who dedicates their life to healthcare. What makes it so gratifying is doing it together, as a team. If there was one thing that I could share about why I value both AmSECT and Duke, it would be because of the truly remarkable, conscientious, professional, motivated people that I’ve met along the way. They continue to inspire me, and I’m so fortunate to be a part of it all.”
Congratulations, Scott!
Kisslo Spring Courses Announced
The 2022 spring session dates of the echocardiography course led by Joe Kisslo have been released. The Echo Techs Anatomic & Computer Dissections Course will be held on Saturday, Feb. 5 (Basic) and Saturday, Feb. 12 (Intermediate) for fellows, echo techs and attendings.
Registration is required. Seats fill fast and space is limited. Boxed breakfast/lunch will be provided (as allowed per Covid restrictions). If you would like more information or want to register, please email Dawne Smith. A calendar invitation to confirm registration will be sent to you or you may be added to a waitlist if the sessions are filled. First time participants are given priority. Please let her know if you have taken the course before. If you register and your plans change, please cancel as soon as possible by declining the calendar invite or contacting Dawne so that the open seat can be offered to someone on the waitlist.
The Basic Course on Feb. 5 will take place in the Duke South Amphitheater located across from the Duke South cafeteria entrance. The Intermediate Course on Feb. 12 will take place in the Main Lecture Hall in the Searle Center. Directions for access will be provided closer to the course date. Questions? Dawne can be reached at 919-668-1524 or dawne.t.smith@duke.edu.
Coston & Team Place in Top 4, NurseHack4Health
 Congratulations to Kimberly Coston, one of our amazing nurses on 3300, and to her ‘Knightingale‘ team members for placing among the top four teams in the November NurseHack4Health hackathon sponsored by Johnson & Johnson. Coston collaborated with the other healthcare professionals on her team (located throughout the world) and worked on a project to combat nursing burnout.
Congratulations to Kimberly Coston, one of our amazing nurses on 3300, and to her ‘Knightingale‘ team members for placing among the top four teams in the November NurseHack4Health hackathon sponsored by Johnson & Johnson. Coston collaborated with the other healthcare professionals on her team (located throughout the world) and worked on a project to combat nursing burnout.
Team Knightingale
Project title: Solving for nurse burnout, which has been exacerbated by COVID-19, with cloud-based software for hospitals and facilities to assess, reaffirm and reset nurses’ mental health.
Track: Diversity in Practice and Care
Team Members: Ryan Etzel, Layne Price, Sharonda Davis, Pak Chau, Rachel Harper, Kimberly Coston, Rob McKenna and Rashna Batliwala
“We are so proud to have Kimberly on our 3300 team!” says Courtney Stierwalt, clinical lead RN for 3300.
Designed to give nurses the unique opportunity to create solutions for challenges that directly impact them and their profession, the weekend-long virtual hackathon was themed “building a sustainable nursing workforce of the future” and was a direct response to the urgent need to recruit and retain a diverse nursing workforce as a nursing shortage accelerates around the country. Nursing turnover is reaching nearly 20 percent per year, leading to a risk of decreased stability and quality in patient care and increasing health system costs.
Over the course of 48 hours, a diverse audience of innovators, including registered nurses, physicians, academics, nursing students, developers and design experts from 38 states and over 40 countries came together to focus on developing solutions for long-standing foundational challenges in the nursing workforce.
Nicely done, Kimberly!
Kudos to all Cardiology Fellows!
We were sent a wonderful note by Anna Lisa Chamis ahead of the holidays – it was sent to the entire team of cardiology fellows from Jacob Schroder.
“I just wanted to write you all a note expressing my gratitude for the amazing job you guys do on a daily basis.
Year in, year out, the CV fellow group is hands down the best in the hospital. For most other specialties, I often skip the trainees and go straight for attending-to-attending communication. Cardiology is different, though. Most of the time, I see the CV fellows as more of an ally and equal and will seek them out first. Not to mention, for our trainees, the cardiology fellows are a huge resource. I still remember being the surgical intern covering 31/3300. Dan Bensimon, a fellow at that time, was the person I called constantly for CV issues. Saved my life. And I know for my wife, Vanessa, that person was one Chet Patel (!) and she felt the same way.
Being a fellow is often a daunting and thankless job. But…
- Keep doing what you are doing, you have a significant role in how well our patients do
- Call any time day or night
- Come visit any time in the OR, especially when you are bored, curious, or want to see how we deal with one of your patients!
Happy New Year!!! 2022 is going to be off the hook.” — JNS
“Thank you so much for taking the time to write this thoughtful feedback about and to the cardiology fellows. Our cardiology fellows (and faculty!) are truly lucky to learn from and collaborate with the best CT surgeons anywhere. #ilovedukeheart” — Anna Lisa
The Duke Heart team is truly special — please keep that gratitude flowing! Sharing with one another how much you appreciate and value your teammates is important, especially during these challenging times. We love sharing your uplifting notes and kudos in Pulse. Keep up the great work, everyone!
Kudos to the Duke Electrophysiology Team
We received a warm note from a grateful patient family member during the holiday season. They wrote:
“Hi Dr. Piccini, Our family is deeply grateful for your care of our beloved family member over the weekend. You inspired a great deal of confidence regarding his care plan, which greatly reduced his stress while hospitalized. Being an ever proud Frenchman, he was very pleased about your experiences with and fond feelings for France. Thanks to you and your team, he will be returning home in better condition than he left. We would like to wish you and your family un Joyeux Noel!” – grateful family member (names withheld to maintain confidentiality)
And this related note to the team from Diane Sauro, “Thank you all for the exceptional work you do every day. We appreciate all you do for your patients and the team.” — Diane
Great work, Jon and team!
Kudos to Kesler!
A grateful patient took some extra time last month to speak with James Mills and send a follow-up note about Autumn Kesler, nurse practitioner, via MyChart:
“When you hired Autumn you hit a grand slam completely out of the park! She is great!” – grateful patient
According to Cheri Wills, Health Center Administrator for Duke Cardiology of Raleigh, “Autumn has only been with our clinic since March 2021 and fit in immediately. She is wonderful in so many ways and we are fortunate to have her as part of our team.”
Way to go, Autumn!
Heart Services Holiday Open House
The Heart Services Leadership team held a holiday open house on Wednesday, Dec. 22 on the 8th floor of the HAFS building. A good time was had by all – thank you to those of you who were able to stop by and celebrate the season with us!


COVID-19 Update
You can quickly access the latest Clinical Operations updates regarding COVID-19 as well as the most recent DUHS Leadership Virtual Town Hall recordings here: https://covid-19.dukehealth.org.
Reminder: All Duke University Health System (DUHS) and Private Diagnostic Clinic (PDC) team members, regardless of work location, are required to receive and provide documentation of a completed COVID-19 booster vaccination by 10 a.m. on Tuesday, Feb. 15, 2022, or within 28 days of their eligibility under CDC and state guidelines. More details are available in this email that was sent to all staff on Tuesday, Dec. 28.
Upcoming Events & Opportunities
Cardiology Grand Rounds
January 11: Telehealth to Improve Functional Status and Quality of Life in Veterans with Peripheral Artery Disease with Tony Gutierrez. 5 p.m. via Webex.
January 18: The Ultimate ‘Anti-Racism Statement’ Medicine Can Make is to Diversify its Ranks with Quinn Capers, IV of the University of Texas Southwestern Medical Center. 5 p.m. via Webex.
MLK Commemoration 2022
 Sunday, Jan. 16: How Long Must We Wait: Striving For the Beloved Community. The 2022 MLK keynote address will be given by historian and social activist, Keeanga-Yamahtta Taylor on Sunday, Jan. 16 at 3 p.m. at Duke Chapel. [UPDATE (1/14/22): This even will be virtual due to weather.] In addition, several community service opportunities are scheduled for the week of MLK Day. You can find more information about the main ceremony and service opportunities on the Duke MLK Commemoration website (https://mlk.duke.edu/). The Commemoration Service is free and open to the public. In accordance with Duke University COVID-19 mitigation policies, all guests must wear a mask at all times when indoors regardless of vaccination status. Parking will be available to all guests at the Bryan Center Garage free of charge.
Sunday, Jan. 16: How Long Must We Wait: Striving For the Beloved Community. The 2022 MLK keynote address will be given by historian and social activist, Keeanga-Yamahtta Taylor on Sunday, Jan. 16 at 3 p.m. at Duke Chapel. [UPDATE (1/14/22): This even will be virtual due to weather.] In addition, several community service opportunities are scheduled for the week of MLK Day. You can find more information about the main ceremony and service opportunities on the Duke MLK Commemoration website (https://mlk.duke.edu/). The Commemoration Service is free and open to the public. In accordance with Duke University COVID-19 mitigation policies, all guests must wear a mask at all times when indoors regardless of vaccination status. Parking will be available to all guests at the Bryan Center Garage free of charge.

Dzau Distinguished Lecture in Global Health
Wednesday, Jan. 26: Restoring Global Solidarity on the Road to Pandemic Recovery — A Conversation with Dr. Agnes Binagwaho and Dr. Paul Farmer. Noon – 1:30 p.m., Zoom. Registration required: https://bit.ly/3tbw7SM.
 Global health crises require global responses. But in the effort to control COVID-19, rising tides of nationalism have threatened collective action and deepened health inequities for many countries. In the face of these challenges to global health solidarity, the Duke Global Health Institute presents a probing discussion with two of the world’s preeminent global health experts – Dr. Agnes Binagwaho and Dr. Paul Farmer – on how the world failed to cooperate to fight the pandemic and how to chart a new vision to achieve health equity.
Global health crises require global responses. But in the effort to control COVID-19, rising tides of nationalism have threatened collective action and deepened health inequities for many countries. In the face of these challenges to global health solidarity, the Duke Global Health Institute presents a probing discussion with two of the world’s preeminent global health experts – Dr. Agnes Binagwaho and Dr. Paul Farmer – on how the world failed to cooperate to fight the pandemic and how to chart a new vision to achieve health equity.
This interactive webinar will span two continents, with our featured speakers appearing at the University of Global Health Equity in Butaro, Rwanda. Dr. Gavin Yamey, professor of the practice of global health and public policy, will moderate the conversation from Duke, fielding questions from the online audience. Attendees will join using Zoom webinar, space permitting.
Duke Well-Being Ambassador Virtual Course
January 11 – March 15: The Well-being Essentials for Learning Life-Balance (WELL-B) weekly webinar series begins January 11, 2022 at 3 p.m. EST. For only one hour a week for 10 weeks (with an optional 11th week for sharing content with colleagues), healthcare workers can learn about the science and practice of well-being from Dr. Bryan Sexton, Dr. Carrie Adair, and Dr. Kyle Rehder. These strategies can enhance your well-being, and through sharing, the well-being of your co-workers. Available to all Duke Health employees and those outside of Duke as well. More information: bit.ly/dukewellb. Offered by the Duke Center for Healthcare Safety and Quality.
Call for Applicants: 2022 AAMC Early-Career Women Seminar
The Department of Medicine and Program for Women in Internal Medicine (PWIM) are pleased to announce sponsorship for one faculty member to attend the in-person AAMC Early-Career Women Seminar on July 19-22, 2022. This popular and highly interactive seminar provides women at the assistant professor level with foundational leadership knowledge and skills to help achieve career goals and thrive as successful leaders in academic medicine and science. If interested in being considered for sponsorship, please send an email to Kimberly Dorman (kimberly.dorman@duke.edu) by January 31, 2022. Members of the office of the Vice-Chair for Faculty Development and Diversity (Drs. Laura Svetkey and Daniella Zipkin) will select one faculty member to nominate to attend and will notify the applicant by email.
Duke Research Week 2022
January 31 – February 4: Registration is now open for Duke Research Week 2022. Join us virtually for a week-long celebration of research underway at Duke! There is an excellent lineup of faculty lectures, panel discussions, “flash talks” with graduate students, trainees and postdoctoral fellows, and guest presenters for the Robert J. Lefkowitz, MD, Distinguished Lecture and Daubechies Lecture. Check out the full agenda here: https://dukeresearchweek.vfairs.com/en/#distinguishedlectures
National Wear Red Day
Friday, Feb. 4: National Wear Red Day. Help increase awareness of the impact cardiovascular disease has on all of us — wear red on Friday, Feb. 4! We would love to have individual and team photos of you sporting your awareness gear to share in Pulse!!
Newly Announced CME
April 23: Duke Sports Cardiology & Sudden Death in Athletes Symposium with course directors Jim Daubert and Bill Kraus. Virtual. For information or to register, contact Christy Darnell christy.darnell@duke.edu or 919-880-8686.
Postponed: Evening with Heart Benefitting Marfan
Due to the latest COVID surge, An Evening with Heart to benefit the Marfan Foundation has been postponed to Thursday, May 5. Location remains the same: The Maxwell in Raleigh, NC. The event will include a silent auction, cocktails, heavy hors d’oeuvres and entertainment. Proceeds will benefit The Marfan Foundation. For information please visit: https://bit.ly/3cHIBYD.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
December 19 — Svati Shah
Healio/Cardiology Today
AHA to fund research on long-term impact of COVID-19 on heart, brain health
https://bit.ly/33686Sa
December 22 — Manesh Patel
Medscape
Apixaban: The ‘Anticoagulant of Choice’ for AF
https://www.medscape.com/viewarticle/965390#vp_1
December 22 — Manesh Patel
tctMD
Correction Issued for Controversial Study Linking COVID-19 Vaccines to ACS Risk
https://bit.ly/3F8NQfR
December 26 — Harry Severance
ACEP eNow
Top 5 Articles of 2021: How the COVID-19 mRNA Vaccines Work, and Some Current Concerns
https://bit.ly/3zNl9nK
December 27 — Jennifer Rymer
Healio/Cardiology Today
Racial gap remains in invasive management for patients with MI with chronic kidney disease
https://bit.ly/3FaYzqa
December 30 — Sana Al-Khatib
Healio/Cardiology
The Take Home: AHA Scientific Sessions
https://bit.ly/3f2P5CL
December 30 — Tristram Bahnson
Healio/Cardiology Today
Catheter ablation outcomes in patients with AF vary by age: CABANA
https://bit.ly/3F7vITG
December 31 — Jennifer Rymer and Manesh Patel
HCP Live
The Best from AHA & TCT 2021 with Jennifer Rymer, MD
https://bit.ly/3F5xS65
Division of Cardiology Publications Indexed in PubMed December 16-22, 2021
Boakye E, Kwapong YA, Obisesan O, Ogunwole SM, Hays AG, Nasir K, Blumenthal RS, Douglas PS, Blaha MJ, Hong X, Creanga AA, Wang X, Sharma G. Nativity-Related Disparities in Preeclampsia and Cardiovascular Disease Risk Among a Racially Diverse Cohort of US Women. JAMA Netw Open 2021;4(12):e2139564. PM: 34928357.
Carnicelli AP, Owen R, Pocock SJ, Brieger DB, Yasuda S, Nicolau JC, Goodman SG, Cohen MG, Simon T, Westermann D, Hedman K, Andersson Sundell K, Granger CB. Atrial fibrillation and clinical outcomes 1 to 3 years after myocardial infarction. Open Heart 2021;8(2):e001726. PM: 34911791.
Fanaroff AC, Li S, Marquis-Gravel G, Giri J, Lopes RD, Piccini JP, Wang TY. Atrial Fibrillation and Coronary Artery Disease: A Long-Term Perspective on the Need for Combined Antithrombotic Therapy. Circ Cardiovasc Interv 2021;14(12):e011232. PM: 34932388.
Franklin JM, Platt R, Dreyer NA, London AJ, Simon GE, Watanabe JH, Horberg M, Hernandez A, Califf RM. When Can Nonrandomized Studies Support Valid Inference Regarding Effectiveness or Safety of New Medical Treatments? Clin Pharmacol Ther 2022;111(1):108-115. PM: 33826756.
Friedman DJ, Emerek K, Sørensen PL, Graff C, Loring Z, Jackson KP, Polcwiartek C, Singh JP, Kisslo J, Søgaard P, Atwater BD. Relationship Between Electrical and Mechanical Dyssynchrony and Outcomes Among Patients Undergoing Cardiac Resynchronization Therapy. Circ Arrhythm Electrophysiol 2021;14(12):e010217. PM: 34843407.
Fudim M, Wojdyla DM, Alexander JH, Goodman SG, Mehran R, Windecker S, Aronson R, Vinereanu D, Halvorsen S, Bahit MC, Granger CB, Lopes RD. Efficacy and Safety of Antithrombotic Therapy in Patients With Atrial Fibrillation, Recent Acute Coronary Syndrome, or Percutaneous Coronary Intervention and a History of Heart Failure: Insights From the AUGUSTUS Trial. J Am Heart Assoc 2021 Dec 21;10(24):e023143. PM: 34873913.
Fuery MA, Chouairi F, Natov P, Bhinder J, Rose Chiravuri M, Wilson L, Clark KA, Reinhardt SW, Mullan C, Miller PE, Davis RP, Rogers JG, Patel CB, Sen S, Geirsson A, Anwer M, Desai N, Ahmad T. Trends and Outcomes of Cardiac Transplantation in the Lowest Urgency Candidates. J Am Heart Assoc 2021;10(24):e023662. PM: 34743559.
Greene SJ, Butler J, Fonarow GC. Contextualizing Risk Among Patients With Heart Failure. JAMA 2021;326(22):2261-2262. PM: 34779819.
Hegde SM, Lester SJ, Solomon SD, Michels M, Elliott PM, Nagueh SF, Choudhury L, Zemanek D, Zwas DR, Jacoby D, Wang A, Ho CY, Li W, Sehnert AJ, Olivotto I, Abraham TP. Effect of Mavacamten on Echocardiographic Features in Symptomatic Patients With Obstructive Hypertrophic Cardiomyopathy. J Am Coll Cardiol 2021;78(25):2518-2532. PM: 34915982.
Kolupoti A, Fudim M, Pandey A, Kucharska-Newton A, Hall ME, Vaduganathan M, Mentz RJ, Caughey MC. Temporal Trends and Prognosis of Physical Examination Findings in Patients With Acute Decompensated Heart Failure: The ARIC Study Community Surveillance. Circ Heart Fail 2021;14(12):e008403. PM: 34702047.
Lunsford-Avery JR, Engelhard MM, Navar AM, Kollins SH. Author Correction: Validation of the Sleep Regularity Index in Older Adults and Associations with Cardiometabolic Risk. Sci Rep 2021;11(1):24398. PM: 34916542.
Lunyera J, Diamantidis CJ, Bosworth HB, Patel UD, Bain J, Muehlbauer MJ, Ilkayeva O, Nguyen M, Sharma B, Ma JZ, Shah SH, Scialla JJ. Urine tricarboxylic acid cycle signatures of early-stage diabetic kidney disease. Metabolomics 2021;18(1):5. PM: 34928443.
Marquis-Gravel G, Hammill BG, Mulder H, Roe MT, Robertson HR, Wruck LM, Sharlow A, Harris DF, Pohlman FW, Hernandez AF, Jones WS. Validation of Cardiovascular End Points Ascertainment Leveraging Multisource Electronic Health Records Harmonized Into a Common Data Model in the ADAPTABLE Randomized Clinical Trial. Circ Cardiovasc Qual Outcomes 2021;14(12):e008190. PM: 34886680.
Murray EM, Whellan DJ, Chen H, Bertoni AG, Duncan P, Pastva AM, Kitzman DW, Mentz RJ. Physical Rehabilitation in Older Patients Hospitalized with Acute Heart Failure and Diabetes: Insights from REHAB-HF. Am J Med 2022;135(1):82-90. PM: 34516959.
Ross M, Henao R, Burke TW, Ko ER, McClain MT, Ginsburg GS, Woods CW, Tsalik EL. A comparison of host response strategies to distinguish bacterial and viral infection. PLoS One 2021;16(12):e0261385. PM: 34905580.
Simon GE, Bindman AB, Dreyer NA, Platt R, Watanabe JH, Horberg M, Hernandez A, Califf RM. When Can We Trust Real-World Data To Evaluate New Medical Treatments? Clin Pharmacol Ther 2022;111(1):24-29. PM: 33932030.
Simon GE, Platt R, Watanabe JH, Bindman AB, John London A, Horberg M, Hernandez A, Califf RM. When Can We Rely on Real-World Evidence to Evaluate New Medical Treatments? Clin Pharmacol Ther 2022;111(1):30-34. PM: 33895994.
Singh AK, Carroll K, McMurray JJV, Solomon S, Jha V, Johansen KL, Lopes RD, Macdougall IC, Obrador GT, Waikar SS, Wanner C, Wheeler DC, Więcek A, Blackorby A, Cizman B, Cobitz AR, Davies R, DiMino TL, Kler L, Meadowcroft AM, Taft L, Perkovic V. Daprodustat for the Treatment of Anemia in Patients Not Undergoing Dialysis. N Engl J Med 2021;385(25):2313-2324. PM: 34739196.
Singh AK, Carroll K, Perkovic V, Solomon S, Jha V, Johansen KL, Lopes RD, Macdougall IC, Obrador GT, Waikar SS, Wanner C, Wheeler DC, Więcek A, Blackorby A, Cizman B, Cobitz AR, Davies R, Dole J, Kler L, Meadowcroft AM, Zhu X, McMurray JJV. Daprodustat for the Treatment of Anemia in Patients Undergoing Dialysis. N Engl J Med 2021;385(25):2325-2335. PM: 34739194.
Watanabe JH, Simon GE, Horberg M, Platt R, Hernandez A, Califf RM. When Are Treatment Blinding and Treatment Standardization Necessary in Real-World Clinical Trials? Clin Pharmacol Ther 2022;111(1):116-121. PM: 33829639.
Division of Cardiology Publications Indexed in PubMed Dec 23, 2021-Jan 5, 2022
Ariss RW, Minhas AMK, Issa R, Ahuja KR, Patel MM, Eltahawy EA, Michos ED, Fudim M, Nazir S. Demographic and Regional Trends of Mortality in Patients With Acute Myocardial Infarction in the United States, 1999 to 2019. Am J Cardiol 2022;164:7-13. PM: 34857365.
Bekfani T, Hamadanchi A, Ijuin S, Bekhite M, Nisser J, Derlien S, Westphal J, Bogoviku J, Morris DA, Fudim M, Braun-Dullaeus RC, Möbius-Winkler S, Schulze PC. Relation of left atrial function with exercise capacity and muscle endurance in patients with heart failure. ESC Heart Fail 2021;8(6):4528-4538. PM: 34726343.
Breathett KK, Xu H, Sweitzer NK, Calhoun E, Matsouaka RA, Yancy CW, Fonarow GC, DeVore AD, Bhatt DL, Peterson PN. Is the affordable care act medicaid expansion associated with receipt of heart failure guideline-directed medical therapy by race and ethnicity? Am Heart J 2022;244:135-148. PM: 34813771.
Chew DS, Li Z, Steinberg BA, O’Brien E, Pritchard J, Bunch TJ, Mark DB, Patel MR, Nabutovsky Y, Greiner MA, Piccini JP. Association between economic and arrhythmic burden of paroxysmal atrial fibrillation in patients with cardiac implanted electronic devices. Am Heart J 2022;244:116-124. PM: 34800369.
Do WL, Nguyen S, Yao J, Guo X, Whitsel EA, Demerath E, Rotter JI, Rich SS, Lange L, Ding J, Van Den Berg D, Liu Y, Justice AE, Guan W, Horvath S, Assimes TL, Bhatti P, Jordahl K, Shadyab A, Valencia CI, Stein AD, Smith A, Staimez LR, Conneely K, Narayan K. Associations between DNA methylation and BMI vary by metabolic health status: a potential link to disparate cardiovascular outcomes. Clin Epigenetics 2021;13(1):230. PM: 34937574.
Fudim M, Borges-Neto S. Utility of diastolic dyssynchrony in the setting of cardiac resynchronization therapy. J Nucl Cardiol 2021;28(6):2644-2646. PM: 31512196.
Gaudino M, Di Franco A, Alexander JH, Bakaeen F, Egorova N, Kurlansky P, Boening A, Chikwe J, Demetres M, Devereaux PJ, Diegeler A, Dimagli A, Flather M, Hameed I, Lamy A, Lawton JS, Reents W, Robinson NB, Audisio K, Rahouma M, Serruys PW, Hara H, Taggart et al. Sex differences in outcomes after coronary artery bypass grafting: a pooled analysis of individual patient data. Eur Heart J 2021;43(1):18-28. PM: 34338767.
Goldstein SA, Krasuski RA. Pulmonary Hypertension in Adults with Congenital Heart Disease. Cardiol Clin 2022;40(1):55-67. PM: 34809917.
Huang MN, D’Anniballe VM, Gunn MD. Monocytes as a Cellular Vaccine Platform to Induce Antitumor Immunity. Methods Mol Biol 2022;2410:627-647. PM: 34914073.
Krasuski RA. Pulmonary Hypertension. Cardiol Clin 2022;40(1):xi-xii. PM: 34809921.
Pagidipati NJ, Phelan M, Page C, Clowse M, Henao R, Peterson ED, Goldstein BA. The importance of weight stabilization amongst those with overweight or obesity: Results from a large health care system. Prev Med Rep 2021;24:101615. PM: 34976671.
Duke Heart Pulse – Week Ending December 19th 2021
Chief’s message:
Dear Duke Heart Faculty, Staff, Fellows, Residents, and Community.

As 2021 comes to an end, we take time to reflect on the amazing accomplishments, resiliency, and teamwork of our entire Duke Heart community. In another difficult year, we were again privileged to be able to provide healthcare to our community, to be able to lean on each other in challenging times, and to be able to celebrate joint successes. Importantly we cherish our ability to continue to be with each other through these difficult times, frequently centering on our mission to train the next generation of heart leaders while we work to discover and deliver heart health.
So, on behalf of the Duke Heart Leadership team, we offer our heartfelt wishes of joy and health to you and your loved ones. More than ever, we recognize life is precious and hope that the season brings you peace — happiness, and warmth that comes from shared moments spent with friends and family.
Happy Holidays and Best Wishes in the upcoming year!
Highlights of the week:
Pediatric Team Receives SVRF Funding
 We learned this week that Andrew Landstrom, MD, PhD, and his colleagues have been awarded a 2021 Single Ventricle Research Fund award. The funding was announced publicly on Wednesday, Dec. 15 by Additional Ventures. Landstrom will receive $660,000 ($220K for three years) to study single ventricle heart disease in the laboratory; his project is titled, “Leveraging induced pluripotent stem cells to define the developmental drivers of hypoplastic left heart syndrome.” Landstrom will serve as principal investigator; Drs. Nick Andersen and Joe Turek will serve as co-investigators.
We learned this week that Andrew Landstrom, MD, PhD, and his colleagues have been awarded a 2021 Single Ventricle Research Fund award. The funding was announced publicly on Wednesday, Dec. 15 by Additional Ventures. Landstrom will receive $660,000 ($220K for three years) to study single ventricle heart disease in the laboratory; his project is titled, “Leveraging induced pluripotent stem cells to define the developmental drivers of hypoplastic left heart syndrome.” Landstrom will serve as principal investigator; Drs. Nick Andersen and Joe Turek will serve as co-investigators.


The grant is particularly notable because it represents the first major funding award for the Single Ventricle Care and Research Program (SVCRP) launched in 2019 and housed within Duke’s Pediatric and Congenital Heart Center. The SVCRP is dedicated to the care of children born with single ventricle heart disease and improving their survival and quality of life. Their multi-disciplinary team is dedicated to the longitudinal care of these patients, from fetal life through adulthood. The program is led by Nick Andersen, surgical director; Andrew McCrary, cardiology director, and Veera Allareddy, medical director.
Congratulations to all!!!
Lee Completes EP Fellowship; Will Return to Military Service
 Joshua Lee, DO, a fellow in the Duke Clinical Cardiac Electrophysiology Fellowship program, is completing his training with us this month and then heading back to San Antonio, TX. There, he will complete his military service with the U.S. Army and put his new skillset to work caring for patients at Brooke Army Medical Center, a 400-bed hospital situated at Fort Sam Houston.
Joshua Lee, DO, a fellow in the Duke Clinical Cardiac Electrophysiology Fellowship program, is completing his training with us this month and then heading back to San Antonio, TX. There, he will complete his military service with the U.S. Army and put his new skillset to work caring for patients at Brooke Army Medical Center, a 400-bed hospital situated at Fort Sam Houston.
Lee joined the EP fellowship in July 2019, spending the bulk of his time at Duke training during the COVID-19 pandemic. He says he chose the Duke program in part based on overall reputation, but also because he had known a former Duke EP fellow serving in the U.S. Army who had raved about their training here.
“When I first came to interview, I immediately sensed the collegiality between the EP attendings, as well as between the fellows and the attendings,” Lee says. “I knew I’d pick up excellent skills and knowledge here, but I also felt that I’d be joining a supportive, encouraging team who would provide great mentorship.”
He says that beyond the supportive environment, one of the things that really stood out to him was the emphasis on the importance of teamwork.
“Patient care is not just about offering a knowledgeable team of physicians,” Lee states. “It’s a holistic partnership involving EP technicians, EP staff, cardiologists, surgeons and general medicine – it’s all about teamwork. This has really been emphasized during my years here at Duke and it’s very similar to my work in the Army where you have a core group of people working together. You really develop a strong bond with others on your team.”
Electrophysiology began to intrigue Lee while he was practicing as a general cardiologist in San Antonio. During that time, he encountered a cardiac sarcoid patient with a recurrent ventricular tachycardia (VT). An electrophysiologist on the team performed a procedure and afterward the patient was shown to have no signs of VT and felt a lot better.
“It’s amazing how procedures, skills and knowledge are always improving in the EP field,” adds Lee. “Medicine is lifelong learning. I now have some great tools and resources that I’ve picked up during my time here at Duke and I am excited to keep learning more.”
Lee has four more years of commitment to fulfill with the Army and is looking forward to assisting in the training of general cardiology fellows when he gets back to Brooke Army Medical Center.
“It is very bittersweet to leave Duke, and while I feel sad about that, I am so excited to move on to another adventure,” Lee says. “I am so thankful to the many people that I have worked with here, especially the small group of EP attendings who work with our fellowship program. Everyone has been so easy to work with and it has been really fun. I felt happy every day to be here.”
It’s clear that Lee made just as big an impact on the EP team as they did on him.
“We are really grateful to have had Josh in our EP fellowship program during the trying and difficult times of the COVID pandemic,” said Jonathan Piccini, MD, associate professor of medicine and director of Duke Electrophysiology. “He has inspired all of us with his eternal optimism, refreshing smile, and the kindness he extends to everyone. He always goes the extra mile for every single one of his patients. We know the San Antonio area and military will be very fortunate to have Lt. Colonel Lee taking care of them and keeping their hearts in rhythm. We salute you Dr. Lee and thank you for your service to Duke, our country, and the US Armed Forces!”
Congratulations, Josh! We look forward to tracking your career and wish you all the best.
Duke Heart Network Welcomes Kotyra as new Senior Director
Duke Network Services is happy to introduce Lisa Kotyra, RN, MSBA, ACNP, as the new Senior Director of the Duke Heart Network.

Lisa comes to Duke Network Services after practicing in the Advanced Heart Failure Program at the University of Rochester Medical Center (URMC) as a Senior Nurse Practitioner and the Program Administrator. Lisa had been with Advanced Heart Failure since 2004 and has experience managing one of the largest VAD centers in the US (behind Duke). Additionally, Lisa’s role included oversight of both CMS and the Joint Commission regulatory processes for Advanced Heart Failure and VAD. Throughout her career, Lisa has cared for cardiovascular patients, including time spent as a nurse practitioner in the URMC Cardiothoracic ICU and in a private, community cardiology practice in both inpatient and outpatient roles. Lisa has been a longstanding member of the American Association of Critical Care Nurses (AACN) and the American College of Cardiology (ACC); most recently serving as the NY State representative for the national ACC CV Team.
Lisa received her Bachelor of Science in Nursing from State University of New York at Binghamton. She received her Masters of Science in Nursing (Acute Care NP Program/Critical Care) from the University of Rochester and her Masters of Science in Business Administration from the Simon Business School at the University of Rochester.
Lisa enjoys paddle boarding, hiking and traveling with family — perfect for our NC landscape. She is married with three children – one of whom is 26, and twins who are 19.
Please give her a warm welcome when you are able to do so!
Outing with Califf
Saturday, December 11, brought a fun outing with Rob Califf – Duke and UNC cardiologists Kristin Newby, Sid Smith (UNC), Magnus Ohman and Chris Granger spent the day out on the links helping to “prep” Califf for his FDA Commissioner Senate hearing, which was held on Tuesday, Dec. 14.
For more on the hearing, please visit: https://www.pbs.org/newshour/politics/watch-live-senate-hearing-on-the-nomination-of-robert-califf-as-commissioner-of-fda.

Ginsburg Celebrated, Pre-Departure for NIH
The team at Duke’s Center for Applied Genomics & Precision Medicine (CAGPM) gathered this week to honor Geoff Ginsburg in his final days as Center director. Ginsburg, a faculty member in our division of cardiology, is leaving Duke to take on the role of Chief Medical and Scientific Officer for the National Institutes of Health (NIH) All of Us Research Program starting next month. In a recent message to the CAGPM, he said, “Transitions are great opportunities for everyone. I am extremely confident in this team, in your future growth and successes, and that Duke CAGPM will continue to be at the forefront of genomics and precision medicine.”
We wish him all the best in his exciting new role and look forward to staying in touch!

Kudos to Ouyang
We received some terrific feedback from a patient recently on behalf of Wendy Chian Ouyang, one of our terrific nurse practitioners.
The patient’s note states: “Wen a gentle spirit, she is. Dr. Glower picked a great lady, caring, kind and a loving spirit. Super attentive.”
Thank you for the care and the compassion you show to all of the patients you provide care for, Wendy! We are very happy that you joined our team. – Diane Sauro, MSN, ANP, NEA-BC, Director-Advanced Practice, Duke Heart Center
Way to go, Wendy!

ICYMI: Final Tributes – Duke Univ & Health System Passings, 2021
We lost several members of our Duke Heart family in 2021. The University published a full list of all staff, faculty and retirees who passed away this past year, through November. To access that publication, please visit: https://bit.ly/3J3zBfB.
Happy Holidays & Reminder from the Pulse!
We wish each of you a calm, peaceful and joy-filled holiday season. Duke Heart Pulse will not be published on Dec. 26 or Jan. 2. We’ll be back on Sunday, Jan. 9. Be safe and healthy out there and we’ll see you in the New Year!
Upcoming Events & Opportunities
Duke Well-Being Ambassador Virtual Course
January 11 – March 15: The Well-being Essentials for Learning Life-Balance (WELL-B) weekly webinar series begins January 11, 2022 at 3 p.m. EST. For only one hour a week for 10 weeks (with an optional 11th week for sharing content with colleagues), healthcare workers can learn about the science and practice of well-being from Dr. Bryan Sexton, Dr. Carrie Adair, and Dr. Kyle Rehder. These strategies can enhance your well-being, and through sharing, the well-being of your co-workers. Available to all Duke Health employees and those outside of Duke as well. More information: bit.ly/dukewellb. Offered by the Duke Center for Healthcare Safety and Quality.
Duke Research Week 2022
January 31 – February 4: Registration is now open for Duke Research Week 2022. Join us virtually for a week-long celebration of research underway at Duke! There is an excellent lineup of faculty lectures, panel discussions, “flash talks” with graduate students, trainees and postdoctoral fellows, and guest presenters for the Robert J. Lefkowitz, MD, Distinguished Lecture and Daubechies Lecture. Check out the full agenda here: https://dukeresearchweek.vfairs.com/en/#distinguishedlectures

Save the Date: Wear Your Red
Friday, Feb. 4: National Wear Red Day. Seriously team, put this one on the calendar! It’s never too early to start thinking of what you can wear on National Wear Red Day — red running shoes? Heart socks? The perfect red top or sweater? A cool red tie? What about that AHA gear you picked up at the last in-person Sessions? Stock up, plan ahead and have plenty of attire to wear throughout heart month to help promote cardiovascular disease awareness — and YES — we would love to have individual and team photos to share in Pulse!!
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion. Note: Pulse is taking a break for the holidays (Dec. 26, Jan. 2). We’ll return on Jan. 9, 2022!
Duke Heart in the News:
December 13 — Manesh Patel
tctMD
World-wise: As In-Person Meetings Resume, Global Voices Hope to Be Heard
https://duke.is/g4tz7
December 14 — Stephen Greene
Medscape
Metformin Benefits Patients Hospitalized for Heart Failure
https://duke.is/w6c3p
December 15 — Svati Shah
Associated Press
$10 million invested to study long-term impact of COVID-19 on heart and brain health
https://duke.is/vdmnw
December 15 — Svati Shah
dicardiology.com
AHA Funds Research on Underlying Causes and Therapies for Cardiovascular Impacts of Long COVID
https://duke.is/ze76a
December 15 — Sunil Rao
Healio/Cardiology Today
DES systems to facilitate transradial PCI receive FDA approval
https://duke.is/mgxbq
December 15 — Rajesh Swaminathan
tctMD
Discharge Safe as Early as a Day After Primary PCI for STEMI
https://duke.is/85yyr
Duke Heart Pulse 12-12-2021
Highlights of the week:
Latest DUH Adult Cardiac Surgery Program STS Ratings
 We learned this week that our Adult Cardiac Surgery program has earned 3-star quality ratings for all ranked categories from the Society of Thoracic Surgeons (STS). The 3-star ratings were earned for isolated coronary artery bypass grafting (CABG) procedures; isolated aortic valve replacement (AVR) surgery; for AVR + CABG, and for isolated mitral valve replacement and repair (MVRR) surgery.
We learned this week that our Adult Cardiac Surgery program has earned 3-star quality ratings for all ranked categories from the Society of Thoracic Surgeons (STS). The 3-star ratings were earned for isolated coronary artery bypass grafting (CABG) procedures; isolated aortic valve replacement (AVR) surgery; for AVR + CABG, and for isolated mitral valve replacement and repair (MVRR) surgery.
The Duke University Hospital STS Risk Adjusted Harvest 3 report includes analyzed results for the 3-year period spanning July 2018 to June 2021.
The STS star rating system is one of the most sophisticated and highly regarded overall measures of quality in health care, rating the benchmarked outcomes of cardiothoracic surgery programs in the U.S. The star rating is calculated using a combination of quality measures for specific procedures performed by an STS Adult Cardiac Surgery Database (ACSD) participant.
Established in 1989 as an initiative for quality improvement and patient safety among cardiothoracic surgeons, the STS ACSD houses more than 6.5 million surgical records and gathers information from more than 3,800 participating physicians, including surgeons and anesthesiologists from more than 90 percent of groups that perform heart surgery in the U.S. The Database includes three other components: the Congenital Heart Surgery Database (CHSD), the General Thoracic Surgery Database (GTSD), and the mechanical circulatory support database (Intermacs). Duke has participated in the STS National Database since its inception.
This achievement is the result of the effort the entire Duke Heart team puts in every day — across the board – our nurses, residents, fellows, CT surgeons, anesthesiologists, ICU teams, cardiologists, pharmacy leaders, cardiac rehabilitation team and all those who support them. Congratulations!
CVRC Announces Annual Mandel Awards
The Duke Cardiovascular Research Center (CVRC) has recently announced their annual Mandel Awards. The Mandel Funding Program Review Committee made three awards in the Seed program, one award in the Fellow program, and one in the Scholar program. We are pleased to share the projects and scholars receiving funding for the 2022 project period which begins January 1.
Mandel Scholar Award
Ravi Karra, MD

Project: Correction of LMNA Cardiomyopathy by Cardioediting
Dilated cardiomyopathies (DCM) due to genetic mutations are common and more likely to progress to end stage heart failure compared to other types of DCM. Here, we propose the development of a system to treat genetic DCM by correcting the causal mutation, using LMNA DCM as an example. We will develop tools to genetically edit LMNA mutations and develop an ultrasound-based method to deliver these tools to the heart. These experiments can establish “cardioediting” as a potential treatment of heritable DCM.
Mandel Fellow Award
 Pavitra Murali, PhD, mentored by Sudha Shenoy, PhD
Pavitra Murali, PhD, mentored by Sudha Shenoy, PhD
Project: Trafficking of Angiotensin Receptors into autophagosomes and its impact on
β-arrestin-dependent signaling
Drugs that bind to the extracellular domains of cell-surface G protein-coupled receptors (GPCRs) are used to treat a variety of cardiovascular diseases including hypertension. Activated GPCRs trigger a signal transduction cascade that produces physiological responses including contraction/relaxation of smooth muscle cells lining arteries. GPCRs, which are bound by drugs at the plasma membrane, rapidly internalize into the cell into intracellular vesicles called endosomes and subsequently traffic into highly acidic vesicles called lysosomes where the GPCR protein is degraded into small peptides. This degradation ensures the long-term desensitization or dampening of signaling and subsiding of the physiological action. We have found that internalized angiotensin type II receptor (AT1R) localizes into a distinct population of vesicles called autophagosomes, which is an unexpected phenomenon because the pathway that invokes formation of autophagosomes called autophagy is known only for recycling organelles and protein catabolism during cell starvation. Since agonist Ang II provokes autophagy trafficking of the AT1R, we believe that this sub-cellular localization may have putative roles in defining AT1R signaling and physiologic effects. The AT1R is an essential target for drugs used to treat many forms of cardiovascular diseases including hypertension; recent evidence reveals that the AT1R mediates its physiologic effects through both G protein and β-arrestin-dependent pathways. In this proposal, I will study how the autophagy trafficking of the AT1R is regulated, and determine the relevance of this trafficking pathway to AT1R signal transduction. The proposed studies will uncover hitherto unknown molecular mechanisms in AT1R trafficking and signaling and might provide new therapeutic angles to treat high blood pressure and cardiovascular disease.
Mandel Seed Awards
Neil Freedman, MD and Christopher Holley, MD, PhD

Project: Atherogenic Mechanisms of Small Nucleolar RNAs
Atherosclerosis fundamentally involves oxidation, a chemical process that is critical for
normal cell function. When oxidation is excessive, it deranges the chemical structure of lipids and proteins and thereby adversely affects their function. The pathogenesis of atherosclerosis initiates with oxidation of the cholesterol-rich low-density lipoprotein particles, and perpetuates with excessive oxidative cell signaling—termed “oxidative stress”—in the inner layers of the artery. This project aims to attenuate excessive oxidative signaling through a novel regulatory mechanism involving particular RNA molecules known as small nucleolar RNAs, or “snoRNAs”, which are expressed throughout the body’s cells. We have found a group of four snoRNAs that augment cellular oxidative stress (Rpl13a-snoRNAs); they appear to do so by facilitating the modification of various messenger RNAs with 2’-O-methylation—a modification that reduces the translation of the messenger RNA into protein.
With previous support from the Mandel Foundation, we found that genetic deficiency of these snoRNAs in Apoe-/- mice reduces arterial levels of reactive oxygen species and attenuates atherosclerosis. Furthermore, we found that snoRNA deficiency in smooth muscle cells dramatically increases the expression of a mitochondrial protein (COX4i2) that reduces mitochondrial production of reactive oxygen species. Therefore, we hypothesize that snoRNAs augment the level of reactive oxygen species in vascular cells by methylating the messenger RNA encoding COX4i2 and thereby reducing the cellular level of COX4i2 protein.
The Mandel Seed Grant will allow us to continue our snoRNA atherosclerosis studies until we can secure NIH funding. Specifically, this new application seeks to achieve the following aims: (1) to determine whether antagonizing snoRNA function with antisense oligonucleotides reduces atherosclerosis in low-density lipoprotein receptor-deficient (Ldlr-/-) mice, and thereby to determine whether snoRNAs can be targeted therapeutically, and (2) to determine in vascular smooth muscle cells and macrophages whether the pre-mRNA encoding COX4i2 is a target of snoRNA-guided methylation, and thereby to elucidate molecular mechanisms underlying the effects of snoRNAs on cellular oxidative stress. Completing these aims will advance our work toward publishing our first manuscript and obtaining NIH support for our ongoing investigations into the anti-atherogenic therapeutic potential of snoRNA-targeted strategies.
Christopher Kontos, MD
Project: Regulation of endothelial metabolism by the Tie1 receptor tyrosine kinase
In the presence of oxygen, cells typically generate energy by breaking down glucose through glycolysis, and then the byproduct, pyruvate, is used by mitochondria to generate ATP through aerobic respiration. Under anaerobic conditions lacking oxygen, cells are unable to utilize mitochondrial respiration, and after glycolysis, pyruvate gets converted to lactate, which is then shuttled out of the cell. Although oxidative metabolism is more efficient than anaerobic glycolytic metabolism in terms of energy production, some cells paradoxically utilize glycolysis as their main form of energy production even in the presence of oxygen.
This phenomenon of “aerobic glycolysis”, was first described by Dr. Otto Warburg (also known as the “Warburg Effect”) in cancer cells. Interestingly, aerobic glycolysis occurs not only in aberrant cancer cells, but it is the primary metabolic pathway that endothelial cells lining the vasculature use to generate energy. Alterations in endothelial cell metabolism are a hallmark of their activation, which occurs during new blood vessel growth and inflammation, and while this activation may be helpful in some contexts, e.g., growth of new blood vessels in response to exercise, the activation of endothelial cells in large arteries can be harmful and lead to atherosclerosis and high blood pressure. When endothelial cells are activated, their metabolism changes to increase their rate of glycolysis, but how they do this is not completely understood.
We hypothesize that the endothelial receptor tyrosine kinase Tie1, which is increased in activated endothelial cells, is partially responsible for altering the metabolism of these activated endothelial cells, and that blocking Tie1’s role in this metabolic shift may help prevent vascular dysfunction and subsequent cardiovascular disease.
Huanghe Yang, PhD
 Project: Demystify flow-activated chloride conductance in endothelium and its role in hypertension
Project: Demystify flow-activated chloride conductance in endothelium and its role in hypertension
Mechanical forces are fundamental in cardiovascular health and disease. Lining the interior surface of blood vessels, the endothelium constantly senses blood flow-induced shear and stretch forces and converts these mechanical stimuli into biochemical signals. Endothelial mechanotransduction is therefore central for both acute vasoregulation and chronic vascular remodeling; and malfunction of endothelial mechanotransduction contributes to cardiovascular diseases including hypertension and atherosclerosis. Mechanosensitive ion channels (MSCs) are the primary mechanotransducers in the endothelium. The endothelial MSCs, including the recently discovered mechanosensitive PIEZO1 calcium permeable channel, have been extensively investigated. Nevertheless, the molecular identity and pathophysiological role of an endothelial flow-activated chloride conductance (FACC) still remain elusive.
Our preliminary results showed that the FACC is significantly upregulated in angiotensin II (Ang II)-treated endothelial cells in vitro, highlighting the urgency to uncover its molecular identity and contribution in hypertension. With this Seed Grant, we aim to acquire critical preliminary results to strengthen our hypothesis that the functional coupling between Piezo1 mechanosensitive calcium channel and TMEM16A calcium-activated chloride channel (CaCC) gives rise to the FACC and enhanced endothelial FACC contributes to hypertension. I anticipate to utilize this opportunity to establish collaborations with CVRC investigators and submit an NIH R01 to further understand FACC in endothelial biology and diseases.
Congratulations to all Mandel funding recipients – we look forward to learning more about your work!
ICYMI: 2021 ACC/AHA/SCAI Guideline for Coronary Artery Revascularization
Congratulations to Brittany Zwischenberger and Sunil Rao, two members of the writing team for the latest Guidelines for Coronary Artery Revascularization which were co-published online in the Journal of the American College of Cardiology and in Circulation on Thursday. ACC/AHA Joint committee members from Duke include: Sana Al-Khatib, Adrian Hernandez, W. Schuyler Jones, and Dan Mark.

Congratulations to Helen Barnes!
Duke Heart’s leadership team wishes to congratulate Helen Barnes who graduated yesterday from University of Mount Olive with a Bachelor of Science degree in Business Administration in Healthcare Management.
“Helen is a great asset who is always willing to partner on new projects with a ready smile and kind words,” said Laura Blue, DNP, VAD Program Team Lead. “I am so proud of her for pursuing her dream of getting her degree and I think she is a great role model for others who wish to pursue their education. Helen was a big supporter of mine when I was working on my doctorate. When she came to me and let me know she felt she could achieve this, I wanted to support her as much as she had supported me. I am really excited for her.”
Barnes, a dedicated member of the Duke family since 1999, has functioned as an administrative assistant with the Duke’s Ventricular Assist Device program for 11 years. Helen partnered with leadership to develop and successfully lead her final project, “Optimizing Incoming Communication in a Multidisciplinary Subspecialty Clinic.”
Congratulations, Helen!
Hofmeister Lands Emerging Leaders Grant
Karl Hofmeister, a 2021 graduate of Duke’s Cardiac Ultrasound Certificate program, has been selected by the Society of Diagnostic Medical Sonography (SDMS) Foundation for their 2022 Emerging Leaders Grant Recipient Program. Hofmeister’s cohort will participate virtually in a variety of leadership education opportunities that are designed to engage them in meaningful dialogue and projects related to the future of the profession and leadership volunteerism.
Hofmeister was the first recipient of our Cardiac Ultrasound Certificate program’s inaugural outstanding student award, which is now named after Joseph Kisslo, MD.
The Emerging Leaders program will culminate with one participant being selected to receive a grant to attend the Fall SDMS and SDMS Foundation Board of Directors Meetings, Liaison Meetings, and the 2022 SDMS Annual Conference.
Congratulations, Karl!
Upcoming Events & Opportunities
SI4R Training Workshop
December 14: Stepping in 4-Respect (SI4R) Workshop for Duke Division of Cardiology. 5-7 p.m. Zoom (Details in email from Kim Dorman)
As part of the Department of Medicine Civility Champion initiatives, a 2-hr zoom workshop for all faculty, staff, and trainees throughout all DOM divisions has been developed. Civility Champions are trained faculty, fellows, and chief residents who provide informal support in response to incidents of bias, harassment, or other unprofessional behaviors, and to help those affected understand their options for intervention and reporting. People generally come to Civility Champions after the fact, and the Champions debrief their experiences every quarter.
The workshop that Drs. John Duronville, Jane Gagliardi, Anita Kelsey, Camille Frazier-Mills, Daniella Zipkin, Laura Previll, and Sophia Weinmann will be presenting to the Cardiology clinical faculty is entitled Stepping In 4-Respect. It is being offered twice and is a new component of these civility efforts designed to teach faculty the skills needed to step in (be an “upstander”) in the moment, with a particular focus on race-, ethnicity- and gender-based incidents. This workshop is supported by Dr. Kathleen Cooney, Chair of the DOM, and will be provided to each division’s faculty over the coming months.
Please be sure to attend the workshop on Dec. 14 if you missed the one on Nov. 30. Additional details about registration, the structure and goals of the workshop appeared in the email invitation.
Duke Well-Being Ambassador Virtual Course
January 11 – March 15: The Well-being Essentials for Learning Life-Balance (WELL-B) weekly webinar series begins January 11, 2022 at 3 p.m. EST. For only one hour a week for 10 weeks, healthcare workers can learn about the science and practice of well-being from Dr. Bryan Sexton, Dr. Carrie Adair, and Dr. Kyle Rehder. These strategies can enhance your well-being, and through sharing, the well-being of your co-workers. Available to all Duke Health employees and those outside of Duke as well. More information: bit.ly/dukewellb. Offered by the Duke Center for Healthcare Safety and Quality.
Duke Research Week 2022
January 31 – February 4: Registration is now open for Duke Research Week 2022. Join us virtually for a week-long celebration of research underway at Duke! There is an excellent lineup of faculty lectures, panel discussions, “flash talks” with graduate students, trainees and postdoctoral fellows, and guest presenters for the Robert J. Lefkowitz, MD, Distinguished Lecture and Daubechies Lecture. Check out the full agenda here: https://dukeresearchweek.vfairs.com/en/#distinguishedlectures

Save the Date: Wear Your Red
Friday, Feb. 4: National Wear Red Day. Seriously team, put this one on the calendar! It’s never too early to start thinking of what you can wear on National Wear Red Day — red running shoes? Heart socks? The perfect red top or sweater? A cool red tie? What about that AHA gear you picked up at the last in-person Sessions? Stock up, plan ahead and have plenty of attire to wear throughout heart month to help promote cardiovascular disease awareness — and YES — we would love to have individual and team photos to share in Pulse!!
Save the Date: Support the Marfan Foundation
February 11: An Evening with Heart to benefit The Marfan Foundation. 7-10 p.m. at The Maxwell in Raleigh, NC. A Valentine’s Day weekend event with silent auction, cocktails, heavy hors d’oeuvres and entertainment. Cocktail attire. Tickets required. For information, visit: https://bit.ly/3cHIBYD.
The Duke Center for Aortic Disease, led by cardiovascular surgeon Chad Hughes, works closely with Marfan patients, their family members and the Marfan Foundation. We are the only location in NC offering access to comprehensive aortic surgical interventions as well as coordinated cardiovascular care and genetic counseling for patients with Marfan syndrome and other connective tissue disorders such as Loeys-Dietz. If you’re interested in learning more about the work being done at Duke or would like to partner or otherwise get involved, please contact Dr. Hughes or Melissa Merrill Burkett, ACNP.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion. Note: Pulse will be taking a break for the holidays from Dec. 26 through Jan. 2; we’ll return on Jan. 9, 2022!
Duke Heart in the News:
December 3 — E. Hope Weissler and W. Schuyler Jones
tctMD
Statins Underprescribed in PAD Before and After Interventions
https://duke.is/722jz
December 7 — E. Hope Weissler and W. Schuyler Jones
Physician’s Weekly
PAD: Statin Prescribing After Revascularization Still Low
https://duke.is/mmhc7
December 8 — Amanda Coniglio
NIH
Rare gene mutation in some Black Americans may allow earlier screening of heart failure
https://bit.ly/3IGG8N5
December 9 — Duke University Hospital
Becker’s Hospital Review
https://bit.ly/3lVQ77f
December 9 — Amanda Coniglio
Clinicalomics
Mutation Linked to Heart Failure in People of African Descent
https://bit.ly/3EKmCNf
Division of Cardiology Publications Indexed in PubMed December 2-8, 2021
Becher PM, Schrage B, Benson L, Fudim M, Corovic Cabrera C, Dahlström U, Rosano GMC, Jankowska EA, Anker SD, Lund LH, Savarese G. Phenotyping heart failure patients for iron deficiency and use of intravenous iron therapy: data from the Swedish Heart Failure Registry. Eur J Heart Fail 2021:10.1002/ejhf.2338. PM: 34476878.
Bernstein E, Wang TY. Point-of-Care Ultrasonography: Visually Satisfying Medicine or Evidence-Based Medicine? JAMA Intern Med 2021:10.1001/jamainternmed.2021.5831. PM: 34633409.
Carnicelli AP, Li Z, Greiner MA, Lippmann SJ, Greene SJ, Mentz RJ, Hardy NC, Blumer V, Shen X, Yancy CW, Peterson PN, Allen LA, Fonarow GC, O’Brien EC. Sacubitril/Valsartan Adherence and Postdischarge Outcomes Among Patients Hospitalized for Heart Failure With Reduced Ejection Fraction. JACC Heart Fail 2021;9(12):876-886. PM: 34509408.
Del Rosario M, Guduguntla V, Wang TY. Nonfatal Myocardial Infarction-Poor Surrogate for Mortality. JAMA Intern Med 2021:10.1001/jamainternmed.2021.5713. PM: 34694340.
Escaned J, Cao D, Baber U, Nicolas J, Sartori S, Zhang Z, Dangas G, Angiolillo DJ, Briguori C, Cohen DJ, Collier T, Dudek D, Gibson M, Gil R, Huber K, Kaul U, Kornowski R, Krucoff MW, Kunadian V, Mehta S, Moliterno DJ, Ohman EM, Oldroyd KG, Sardella G, et al. Ticagrelor monotherapy in patients at high bleeding risk undergoing percutaneous coronary intervention: TWILIGHT-HBR. Eur Heart J 2021;42(45):4624-4634. PM: 34662382.
Hess CN, Debus ES, Nehler MR, Anand SS, Patel MR, Szarek M, Capell WH, Hsia J, Beckman JA, Brodmann M, Diaz R, Habertheuer P, Leeper NJ, Powell RJ, Sillesen H, Muehlhofer E, Berkowitz SD, Haskell LP, Bauersachs RM, Bonaca MP. Reduction in Acute Limb Ischemia with Rivaroxaban versus Placebo in Peripheral Artery Disease after Lower Extremity Revascularization: Insights from VOYAGER PAD. Circulation 2021:10.1161/CIRCULATIONAHA.121.055146. PM: 34637332.
Hsia J, Kavanagh ST, Hopley CW, Baumgartner I, Berger JS, Fowkes GR, Jones WS, Mahaffey KW, Norgren L, Patel MR, Rockhold F, Blomster J, Katona BG, Hiatt WR, Bonaca MP. Impact of chronic kidney disease on hemoglobin among patients with peripheral artery disease treated with P2Y inhibitors: Insights from the EUCLID trial. Vasc Med 2021;26(6):608-612. PM: 34082620.
Ma Z, Viswanathan G, Sellig M, Jassal C, Choi I, Garikipati A, Xiong X, Nazo N, Rajagopal S. β-Arrestin-Mediated Angiotensin II Type 1 Receptor Activation Promotes Pulmonary Vascular Remodeling in Pulmonary Hypertension. JACC Basic Transl Sci 2021;6(11):854-869. PM: 34869949.
Mack M, Carroll JD, Thourani V, Vemulapalli S, Squiers J, Manandhar P, Deeb GM, Batchelor W, Herrmann HC, Cohen DJ, Hanzel G, Gleason T, Kirtane A, Desai N, Guibone K, Hardy K, Michaels J, DiMaio JM, Christensen B, Fitzgerald S, Krohn C, Brindis RG, et al. Transcatheter Mitral Valve Therapy in the United States: A Report From the STS-ACC TVT Registry. J Am Coll Cardiol 2021;78(23):2326-2353. PM: 34711430.
Manolio TA, Bult CJ, Chisholm RL, Deverka PA, Ginsburg GS, Goldrich M, Jarvik GP, Mensah GA, Ramos EM, Relling MV, Roden DM, Rowley R, Williams MS, Green ED. Genomic medicine year in review: 2021. Am J Hum Genet 2021;108(12):2210-2214. PM: 34861172.
Matsue Y, Sama IE, Postmus D, Metra M, Greenberg BH, Cotter G, Davison BA, Felker GM, Filippatos G, Pang P, Ponikowski P, Severin T, Gimpelewicz C, Voors AA, Teerlink JR. Association of Early Blood Pressure Decrease and Renal Function With Prognosis in Acute Heart Failure. JACC Heart Fail 2021;9(12):890-903. PM: 34627724.
Salah HM, Pandey A, Soloveva A, Abdelmalek MF, Diehl AM, Moylan CA, Wegermann K, Rao VN, Hernandez AF, Tedford RJ, Parikh KS, Mentz RJ, McGarrah RW, Fudim M. Relationship of Nonalcoholic Fatty Liver Disease and Heart Failure With Preserved Ejection Fraction. JACC Basic Transl Sci 2021;6(11):918-932. PM: 34869957.
Salisbury AC, Safley DM, Kennedy KF, Bhardwaj B, Aronow HD, Jones WS, Feldman DN, Secemsky E, Tsai TT, Attaran RR, Spertus JA. Development and validation of a predictive model for bleeding after peripheral vascular intervention: A report from the National Cardiovascular Data Registry Peripheral Vascular Interventions Registry. Catheter Cardiovasc Interv 2021;98(7):1363-1372. PM: 34569709.
Samsky MD, Mentz RJ, Stebbins A, Lokhnygina Y, Aday AW, Pagidipati NJ, Jones WS, Katona BG, Patel MR, Holman RR, Hernandez AF, Gutierrez JA. Polyvascular disease and increased risk of cardiovascular events in patients with type 2 diabetes: Insights from the EXSCEL trial. Atherosclerosis 2021;338:1-6. PM: 34741929.
Stefanini GG, Briguori C, Cao D, Baber U, Sartori S, Zhang Z, Dangas G, Angiolillo DJ, Mehta S, Cohen DJ, Collier T, Dudek D, Escaned J, Gibson CM, Gil R, Huber K, Kaul U, Kornowski R, Krucoff MW, Kunadian V, Moliterno DJ, Ohman EM, Oldroyd KG, Sardella G. Ticagrelor monotherapy in patients with chronic kidney disease undergoing percutaneous coronary intervention: TWILIGHT-CKD. Eur Heart J 2021;42(45):4683-4693. PM: 34423374.
Weissler EH, Jones WS. Who Will Own the Responsibility to Prescribe Statins? Tragedy of the Commons. JAMA Netw Open 2021;4(12):e2137605. PM: 34860247.
Recent Comments