Shah Named Director of Duke Kannapolis Research
 The Duke Clinical and Translational Science Institute (CTSI) this week announced Svati Shah, MD, MHS, professor of medicine in cardiology at Duke, as the new director of Duke Kannapolis Research. In this role, she will direct all activities and projects based at the Duke CTSI clinical research facility in Kannapolis, including ongoing leadership of the Duke Project Baseline initiative — a collaboration with Verily Life Sciences — and assuming leadership of the MURDOCK Study and all associated programs.
The Duke Clinical and Translational Science Institute (CTSI) this week announced Svati Shah, MD, MHS, professor of medicine in cardiology at Duke, as the new director of Duke Kannapolis Research. In this role, she will direct all activities and projects based at the Duke CTSI clinical research facility in Kannapolis, including ongoing leadership of the Duke Project Baseline initiative — a collaboration with Verily Life Sciences — and assuming leadership of the MURDOCK Study and all associated programs.
Shah is an Associate Dean for Genomics in the Duke University School of Medicine, where she is also Director of the Precision Genomics Collaboratory, Director of the Adult Cardiovascular Genetics Clinic, and the Vice-Chief of Translational Research in the Division of Cardiology.
Shah is a physician scientist and practicing cardiologist who sees patients and families with cardiovascular genetic disorders. She earned a Master of Health Science degree in epidemiology from Johns Hopkins School of Public Health and a master’s degree in Medical Genomics from Duke University, and she completed a research fellowship in genetic epidemiology at the Duke Center for Human Genetics.
Her research laboratory focuses on the molecular epidemiology of cardiometabolic diseases, using integrated omics technologies including genomics and metabolomics, to identify novel biomarkers and mechanisms of disease pathogenesis.
Shah brings a wealth of experience to her new role as Director of Duke Kannapolis Research, including her internationally recognized expertise in omics, precision medicine, and population health. Her leadership will move Duke Kannapolis forward with a renewed vision in these areas while leveraging a number of partnerships both internal and external to Duke, as well as the vital partnership with our community in Kannapolis and Cabarrus County.
Congratulations, Svati!!
Rajagopal Elected to ASCI
 The American Society for Clinical Investigation (ASCI) this week announced the election of 95 new members for 2022. Among them, Sudarshan Rajagopal, MD, PhD, associate professor of medicine in cardiology at Duke and member of the Duke Cardiovascular Research Center.
The American Society for Clinical Investigation (ASCI) this week announced the election of 95 new members for 2022. Among them, Sudarshan Rajagopal, MD, PhD, associate professor of medicine in cardiology at Duke and member of the Duke Cardiovascular Research Center.
ASCI’s new members come from 46 different institutions and represent excellence across the breadth of academic medicine. They will be officially inducted into the Society at the ASCI Dinner and New Member Induction Ceremony on April 8, 2022, as part of the AAP/ASCI/APSA Joint Meeting planned for April 8-10 at the Swissotel Chicago.
For the 2022 membership nomination cycle, the Council considered 227 nominations and recommended 95 nominees for election.
Congratulations, Sudar. Well deserved!
USNWR Ratings vs Outcomes Data Presented at STS 2022
 Congratulations to Oliver K. Jawitz, MD, MHS, a Duke General Surgery resident and clinical research fellow with Duke Clinical Research Institute for presenting his team’s work at the 58th Annual Meeting of the Society of Thoracic Surgeons, which was held virtually Jan. 29-30. Jawitz presented Comparing Consumer-Directed Hospital Rankings with Society of Thoracic Surgeons (STS) Adult Cardiac Surgery Database Outcomes during a plenary session on Jan. 29.
Congratulations to Oliver K. Jawitz, MD, MHS, a Duke General Surgery resident and clinical research fellow with Duke Clinical Research Institute for presenting his team’s work at the 58th Annual Meeting of the Society of Thoracic Surgeons, which was held virtually Jan. 29-30. Jawitz presented Comparing Consumer-Directed Hospital Rankings with Society of Thoracic Surgeons (STS) Adult Cardiac Surgery Database Outcomes during a plenary session on Jan. 29.
Annual hospital rankings – particularly those issued by USNWR – typically make a big splash in the news upon release, but there has been relatively little work done to explore how the rankings compare with actual patient outcomes in any specialty, according to Jawitz. His team designed a study to examine whether the rankings would correlate in a meaningful way with outcomes in adult cardiac surgery patients.
Jawitz and his team compared annual U.S. News & World Report (USNWR) rankings with risk-adjusted mortality/morbidity data from the STS Adult Cardiac Surgery Database. In total, 524,393 patients undergoing CABG or CABG with a valve procedure from 149 hospitals (65 of which were consistently ranked in the top 100 hospitals during the 5-year period examined by the team) were included in the data.
USNWR rankings rely on a complicated methodology that appears to be rigorous but is not fully transparent, says Jawitz. USNWR publishes their methodology, but it changes each year.
In the team’s preliminary dive into the data, Jawitz says he was surprised to see the impact that shifts in USNWR rankings can have on hospitals. “A one spot change in ranking from year to year has been correlated with a one-percent change in revenue and patient volume, which is significant.”
What was not surprising to him or to his team was their primary finding: that the USNWR ratings for cardiology and heart surgery programs do not correlate in any meaningful way with risk-adjusted outcomes data from the STS database.
“This was not a ground-breaking finding, to be perfectly honest,” Jawitz says. “However, what was surprising is that we found absolutely no correlation – not even a signal of correlation — between rankings and outcomes. Given the impact rankings can have can have on patient choices and, frankly, on hospital revenue and the resources that some institutions have dedicated toward trying to lift their USNWR ranking over time, we think it’s an important step to study how these rating systems compare to actual outcome measures for various specialties.”
From the standpoint of heart surgery, the gold standard is the STS database and the public reporting of STS Star Ratings.
“US News and World Report rankings can tell consumers a lot of things, but they don’t tell them enough information about surgical outcomes,” says Peter K. Smith, Mary and Deryl Hart Distinguished Professor of Surgery and former chief, Duke Division of Cardiovascular and Thoracic Surgery. “This particular ranking system combines surgery measures with cardiology measures for heart programs across the U.S., so for patients seeking information about surgical outcomes that information is obscured.
“The primary message here for consumers is that rankings should be used with caution because the differences in rankings of heart programs at U.S. hospitals don’t necessarily relate to differences in surgical outcomes across those same programs,” Smith adds. “Instead – and particularly for patients in need of heart surgery – they really need to look at the public reporting done by the STS and use that information as part of their decision-making process.”
Jawitz concurs.
“We’re really fortunate in the CT surgery world to have the STS database. The STS tracks procedures that have been incredibly well studied for decades; they have risk models and calculators and the ability to hone in on which groups really are performing well and which have some room for improvement,” Jawitz says.
“At the end of the day, the record of surgical outcomes are what should be most important to heart surgery patients – getting your procedure done safely with minimal morbidity and being able to go home to your family is what should matter most. This type of measure appears to be getting lost with high-profile ranking systems such as USNWR.”
Jawitz believes future studies should look at consumer-directed ranking systems in a rigorous and statistically sound way and suggest better ways for such rankings to map better to what matters most to patients as well as to the clinical community.
“Healthcare is a difficult enough system to navigate as it is,” he adds. “I would strongly encourage consumers who are seeking guidance toward programs to consult professional societies that publish risk-adjusted data for the area in which they need care. Relying more on those types of sources than on hospital rankings would probably be of great benefit to them.”
Jawitz and team expect to publish their findings later this year.
Great job, Oliver and team!
Also at STS 2022:
 Congratulations to Christopher Jensen, MD, MHS, a general surgery resident,
Congratulations to Christopher Jensen, MD, MHS, a general surgery resident,  for his on-demand presentation, Cardiovascular Mechanism of Donor Brain Death and Heart Recipient Survival and to Fabian Jimenez Contreras for his on-demand presentation Progression of Aortic Valve Insufficiency During Fully Magnetically Levitated Centrifugal Versus Axial Flow Left Ventricular Assist Device (LVAD) Support that were part of STS’s 58th Annual Meeting. Jimenez Contreras, a 4th year medical student at Duke, is planning a career in cardiothoracic surgery. This was his first presentation at STS
for his on-demand presentation, Cardiovascular Mechanism of Donor Brain Death and Heart Recipient Survival and to Fabian Jimenez Contreras for his on-demand presentation Progression of Aortic Valve Insufficiency During Fully Magnetically Levitated Centrifugal Versus Axial Flow Left Ventricular Assist Device (LVAD) Support that were part of STS’s 58th Annual Meeting. Jimenez Contreras, a 4th year medical student at Duke, is planning a career in cardiothoracic surgery. This was his first presentation at STS
Well done!
Heart Month Celebration Continues!
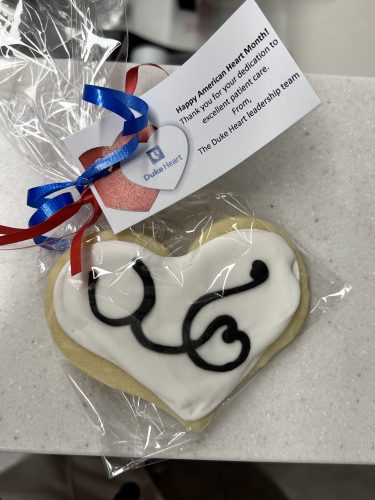
In celebration of Heart month, the Duke Heart leadership team distributed heart-shaped cookies to team members this week.
Dr. Manesh Patel, Dr. Ed Chen, Jill Engel and the entire leadership team thanks everyone for their dedication to excellent patient care, safety and awareness as we continue to celebrate Heart Month. We hope our team members will take time to reflect on the amazing things each of them and the entire Duke Heart team have achieved over the last year. We are so fortunate to have each and every team member – we could not provide the excellent care that we do without every single one of you. Thank you!
Duke Cardiac Ultrasound Students Named ASE Scholarship Award Winners
Two students in Duke’s Cardiac Ultrasound Certificate Program have won American Society of Echocardiography (ASE) Foundation student scholarships.
 Nick Medlock has received the Waggoner Award and Daisy Chang has received the Katanick Award.
Nick Medlock has received the Waggoner Award and Daisy Chang has received the Katanick Award.
The Katanick award is given to the highest ranking student sonographer candidate nominated for ASEF scholarship awards. This award was established in 2016 and was named to honor the legacy of Sandy Katanick, RN, RVT, CAE, who retired as CEO of the Intersocietal Accreditation Commission after more than 25 years of service to the field.
This is the first year that Duke has been eligible to nominate students; only programs that are nationally accredited can nominate students. Duke’s program received accreditation in 2021.
The awards will be given to Medlock and Chang at the annual ASE meeting in June in Seattle, WA. They will each receive $1,000 and support for travel.
Congratulations to Nick and Daisy! And… hat tip to the Cardiac Ultrasound Program – your efforts are making this one of the best recognized programs in the country!
ICYMI: JCF Ignite! Featured in Medpage Today
This past week, there was a terrific piece in Medpage Today (link below, in “news”) that speaks to a new feature in the Journal of Cardiac Failure.
“At JCF, we’ve been thinking, how can we meet contemporary demands to facilitate conversation, inclusion and excitement in academic publishing? We communicate in new ways,” says Rob Mentz, associate professor of medicine in cardiology and editor-in-chief of the Journal of Cardiac Failure. “JCF Ignite! is one such initiative intended to favorably transform our field. This new section is designed to serve as a platform for very concise and rigorous reports on a novel (potentially provocative) concept, analysis, insight or data presentation. The goal is to enable authors to disseminate worthwhile material in an exceptionally timely manner to enhance impactful discourse and consider paradigm shifts in the care of patients with heart failure.”
Congrats to Mentz and the team at JCF!
Duke Schools of Medicine and Nursing Rank in Top 5 for NIH Research Funding
The medical and nursing schools at Duke University both rank in the top five nationally for research funding received from the National Institutes of Health (NIH), according to the Blue Ridge Institute for Medical Research.
Duke University School of Medicine was awarded more than $608 million in federal funding from the NIH in 2021, ranking third nationally among academic medical centers, up from 10th last year.
“The amount of research funding awarded to Duke scientists by the NIH is a key measure of excellence across all of our missions,” said Mary E. Klotman, MD, dean of Duke University School of Medicine. “These rankings reflect the hard work, dedication and innovation of our outstanding faculty and research staff, and their commitment and contributions to scientific discovery and advancing care for our patients.”
The Blue Ridge ranking — an annual, independent analysis of NIH research funds to colleges and universities — places Duke University School of Nursing at fifth in the nation, up from 8th last year, garnering $8.5 million from the NIH.
“Duke School of Nursing’s growth in research funding reflects the dedication of our faculty and their commitment to improving the health of real people, families, and communities,” said Vincent Guilamo-Ramos, PhD, dean of Duke University School of Nursing and vice chancellor of nursing affairs at Duke University. “They are shaping innovative health interventions and solutions; developing and testing technology that improves health outcomes; and designing nurse-led models of health care that truly are the future of nursing.”
At the medical school, two basic science departments and eight clinical science departments were ranked among the top 10 in the country:
#1 for Pediatrics
#1 for Surgery
#2 for Orthopedics
#5 for Neurosurgery
#6 for Internal Medicine
#8 for Anesthesiology
#9 for Genetics
#9 for Otolaryngology
#10 for Pharmacology
#10 for Ophthalmology
The NIH is the largest public funder of biomedical research in the world, investing more than $41 billion a year to advance research aimed at improving health.
COVID-19 Updates
Final Reminder: All Duke University Health System (DUHS) and Private Diagnostic Clinic (PDC) team members, regardless of work location, are required to receive and provide documentation of a completed COVID-19 booster vaccination by 10 a.m. on Tuesday, Feb. 15, 2022, or within 28 days of their eligibility under CDC and state guidelines. More details are available in this email that was sent to all staff on Tuesday, Dec. 28.
All the latest Clinical Operations updates related to COVID can be found at https://covid-19.dukehealth.org.
Upcoming Events & Opportunities
Duke Genomic & Precision Medicine Forum Series
February 24: Guest will be William E. Kraus, MD speaking on Components of Personalized Lifestyle Medicine with a Focus on Physical Activity. Noon – 1 p.m. via Zoom. Sponsored by Duke Center for Applied Genomics & Precision Medicine. Registration is required; event is free. To learn more and to register, please visit: https://bit.ly/3ouqDiK.
Upcoming Duke Heart CME
April 23: Duke Sports Cardiology & Sudden Death in Athletes Symposium with course directors Jim Daubert and Bill Kraus. Virtual. For information or to register, contact Christy Darnell christy.darnell@duke.edu or 919-880-8686.
Seeking Applicants: Chan Zuckerberg Science Diversity Leadership Award
The Chan Zuckerberg Initiative (CZI) and the National Academies of Sciences, Engineering, and Medicine invite applications for the new Science Diversity Leadership program, which will support projects led by excellent biomedical researchers who—through their outreach, mentoring, and teaching—have a record of promoting diversity, equity and inclusion in their scientific fields.
Each grant recipient will be awarded a total of $1.15 million over five years, with the first two cohorts of grantees selected in 2022 and 2023. Investigators leading the grantees’ projects will use funds to support research programs and outreach, mentoring, and teaching activities. The principal investigator must lead an independent research laboratory in a university, medical school, or nonprofit research institution in the U.S. or a U.S. territory and have started their first independent laboratory no earlier than January 1, 2012. Learn more and apply. Applications close May 19, 2022.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
February 9 — Rob Mentz
Medpage Today
Do You Know How Many Great Ideas and Findings Never Get Published?
https://www.medpagetoday.com/opinion/revolutionandrevelation/97089
February 10 — Duke University & Health System
Forbes
America’s Best Large Employers
https://www.forbes.com/lists/best-large-employers/?sh=3369e30e7b66
Division of Cardiology Publications Indexed in PubMed February 3-9, 2022
Becker F, Dakin HA, Reed SD, Li Y, Leal J, Gustavson SM, Wittbrodt E, Hernandez AF, Gray AM, Holman RR. Lifetime cost-effectiveness simulation of once-weekly exenatide in type 2 diabetes: A cost-utility analysis based on the EXSCEL trial. Diabetes Res Clin Pract 2022 Jan;183:109152. PM: 34813910.
Bloomfield GS, Alenezi F, Chiswell K, Dunning A, Okeke NL, Velazquez EJ. Progression of cardiac structure and function in people with human immunodeficiency virus. Echocardiography 2022 Feb;39(2):268-277. PM: 35048419.
Coniglio AC, Segar MW, Loungani RS, Savla JJ, Grodin JL, Fox ER, Garg S, de Lemos JA, Berry JD, Drazner MH, Shah S, Hall ME, Shah A, Khan SS, Mentz RJ, Pandey A. Transthyretin V142I Genetic Variant and Cardiac Remodeling, Injury, and Heart Failure Risk in Black Adults. JACC Heart Fail 2022 Feb;10(2):129-138. PM: 35115086.
Fiuzat M, Hamo CE, Butler J, Abraham WT, DeFilippis EM, Fonarow GC, Lindenfeld J, Mentz RJ, Psotka MA, Solomon SD, Teerlink JR, Vaduganathan M, Vardeny O, McMurray JJV, O’Connor CM. Optimal Background Pharmacological Therapy for Heart Failure Patients in Clinical Trials: JACC Review Topic of the Week. J Am Coll Cardiol 2022 Feb 8;79(5):504-510. PM: 35115106.
Gilchrist SC, Hall JL, Khandelwal A, Hidalgo B, Aggarwal B, Kinzy C, Mallya P, Conners K, Stevens LM, Alger HM, Mehta L, Wexler L, Mega JL, Hernandez A, Hayes SN, Mieres JH, Jessup M, Roger VL. Research Goes Red: Early Experience With a Participant-Centric Registry. Circ Res 2022 Feb 4;130(3):343-351. PM: 35113661.
Harskamp RE, Fanaroff AC, Lopes RD, Wojdyla DM, Goodman SG, Thomas LE, Aronson R, Windecker S, Mehran R, Granger CB, Alexander JH. Antithrombotic Therapy in Patients With Atrial Fibrillation After Acute Coronary Syndromes or Percutaneous Intervention. J Am Coll Cardiol 2022 Feb 8;79(5):417-427. PM: 35115097.
King HA, Doernberg SB, Grover K, Miller J, Oakes M, Wang TW, McFatrich M, Ruffin F, Staman K, Lane HG, Rader A, Sund Z, Bosworth HB, Reeve BB, Fowler VG, Holland TL. Patients’ Experiences With and Gram-Negative Bacterial Bloodstream Infections: Results From Cognitive Interviews to Inform Assessment of Health-Related Quality of Life. Open Forum Infect Dis 2021 Dec 8;9(2):ofab622. PM: 35106313.
Loring Z, Bahnson TD. Is there a mortality benefit of atrial fibrillation ablation? J Cardiovasc Electrophysiol 2022 Feb;33(2):194-196. PM: 34911158.
Quintanilha JCF, Liu Y, Etheridge AS, Yazdani A, Kindler HL, Kelly WK, Nixon AB, Innocenti F. Plasma levels of angiopoietin-2, VEGF-A, and VCAM-1 as markers of bevacizumab-induced hypertension: CALGB 80303 and 90401 (Alliance). Angiogenesis 2022 Feb;25(1):47-55. PM: 34028627.
Redfors B, Simonato M, Chen S, Vincent F, Zhang Z, Thiele H, Eitel I, Patel MR, Ohman EM, Maehara A, Ben-Yehuda O, Stone GW. Ambient temperature and infarct size, microvascular obstruction, left ventricular function and clinical outcomes after ST-segment elevation myocardial infarction. Coron Artery Dis 2022 Mar 1;33(2):81-90. PM: 34569991.
Salah HM, Al’Aref SJ, Khan MS, Al-Hawwas M, Vallurupalli S, Mehta JL, Mounsey JP, Greene SJ, McGuire DK, Lopes RD, Fudim MEfficacy and safety of sodium-glucose cotransporter 2 inhibitors initiation in patients with acute heart failure, with and without type 2 diabetes: a systematic review and meta-analysis. Cardiovasc Diabetol 2022 Feb 5;21(1):20. PM:35123480
Tobin RS, Samsky MD, Kuchibhatla M, O’Connor CM, Fiuzat M, Warraich HJ, Anstrom KJ, Granger BB, Mark DB, Tulsky JA, Rogers JG, Mentz RJ, Johnson KS Race Differences in Quality of Life following a Palliative Care Intervention in Patients with Advanced Heart Failure: Insights from the Palliative Care in Heart Failure Trial.J Palliat Med 2022 Feb;25(2):296-300. PM:34851740
Toro C, Temkin N, Barber J, Manley G, Jain S, Ohnuma T, Komisarow J, Foreman B, Korley FK, Vavilala MS, Laskowitz DT, Mathew JP, Hernandez A, Sampson J, James ML, Goldstein BA, Markowitz AJ, Krishnamoorthy V, Association of Vasopressor Choice with Clinical and Functional Outcomes Following Moderate to Severe Traumatic Brain Injury: A TRACK-TBI Study. Neurocrit Care 2022 Feb;36(1):180-191.PM:34341913
Recent Comments