Duke Heart Week Ending June 5th 2022
Chief’s message:
In Memoriam: Robb Kociol, MD, former Cardiology Fellow
It is with great sadness that we share the news of the passing of Robb Kociol, MD, a 2011 graduate of our  cardiology fellowship program.
cardiology fellowship program.
A native of the San Francisco Bay area, Kociol came to Duke for fellowship from Brigham and Women’s Hospital. He was noted during fellowship for being caring, fun, smart, and often self-deprecating. He was passionate about advanced heart failure care and after training at Duke, returned to Boston and the Beth Israel Deaconess Medical Center as a faculty member. He eventually became the director of their Transplant Program. Over the last few years, he transitioned to pharma – initially at Boehringer Ingelheim before going to Cytokinetics where he partnered with Duke faculty and company leadership for the omecamtiv mecarbil work.
He is survived by his wife Kristin, their two young daughters, and his parents.
Robb was a friend, gentle and thoughtful, and will be missed by all of us that knew him and by the larger cardiovascular community. His passing, like many of the events over the last few years, reminds us how precious life is and the bonds we have with each other.
At this time, service details have not been announced. We will remain in contact with the family to get details around his service, and ensure that the Duke community works to find any ways that we can support them.
As a start, below is a gofundme site that has been started to support his family.
|
We are raising money for the Kociol family after the unexpected passing of Robb. Th… Colleen Donovan needs your support for Kociol Family Memorial Fund
gofund.me
|
We asked several Duke Heart team members to share their thoughts on Robb with us. Here is what they wrote:
From Adrian Hernandez, MD:
“Robb came to Duke as a cardiology fellow with the triple aim of excellence in clinical care, research, and education. He achieved all of this plus more. What we learned from Robb is there is a 4th aim- excellence in humanity. He cared about people- friends, family, and others. It showed every day.
As we’ve learned about Robb’s passing, I know it brings up so many fond memories of him. Some of my best experiences have been with and because of Robb. At the beginning of his fellowship, I remember when he first met with me and asked if I could be his mentor in his own quirky style. Along the way, I had the privilege to see things differently through his eyes when he had decisions to make, opportunities to consider and difficult times to confront. Each time our conversation turned to what was best for the family and the people around him. He also had plenty of amusing stories to share in his self-deprecating way.
Just one example of his impact comes from several years ago when I had the pleasure of visiting Beth Israel-Deaconess Medical Center. Robb had just started the advanced heart failure program with ventricular assist devices, and it was clearly on its way to success. Every fellow noted how much of an impact Robb had on the place, their lives, and the lives of others. I heard stories from the fellows about Robb and the amount of time he spent with them and the patients selflessly ensuring their success. He led by example and all the fellows wanted to be like Robb. He relentlessly dedicated himself to every patient for the best outcome possible whether on ECMO or getting a VAD or making a tough decision at the end of life. He also wanted everyone to learn together and advance the field. He was so committed and loved it. That was Robb—committed to others. I was thankful Robb had ignored my advice on starting a VAD program- “Don’t do it. It’s impossibly hard, especially in Boston!” His reply, “I know, but its family.”
From Ravi Karra, MD:
“Robb was the best. He was brilliant and led by modeling excellence with humility and a quirky charm that was infectious. No one left a chat, text, or email from Robb without a smile on their face. Robb was always dedicated to serving patients and taking care of his family. Robb loved doctoring more than anyone I have ever met, and Robb was a great doctor. As a new attending, he built up the heart transplant program at the BI, caring for his patients as soon as the cross-clamp came off. He absolutely adored his wife, Kristin, and his girls, Sophia and Olivia. When catching up with Robb, he always gushed about what his girls were up to and always expressed his deep appreciation and love for Kristin. His sudden passing has been heart-breaking. My family has been privileged to know and grow with the Kociol’s – we sorely miss our dear friend.”
From Robert Mentz, MD:
“Robb lived an inspiring life. An exceptional clinician and researcher, he was a role model for many interested in improving care for patients with heart failure. He excelled during his training at Duke and the DCRI. Brilliant, hardworking and engaging, he helped lead a number of foundational projects in outcomes research and trials. Having trailed him at Brigham and Women’s Hospital and Duke, I became used to being referred to as “Robb” – though his shoes would be impossible to fill. He paved the way for many of us and was a thoughtful mentor and friend.
Following his training, he returned to Boston where he went on to lead and expand the advanced heart failure program at Beth Israel. He worked so incredibly hard to provide the best possible care for his patients. He had a remarkable career as a clinician investigator but perhaps even more inspiring was his life as a husband, father and friend. He faced both personal and family health issues with grit, courage and resiliency. It was shocking to hear of his passing and our thoughts go out to his wife and kids in particular. May they find some peace in knowing the tremendous impact he has had on so many of his colleagues and patients’ lives.
We will explore the best ways to support his family and remember his legacy within the walls of Duke and beyond. Back in 2016, he published a thoughtful piece about the need to be a well-rounded clinician – his words extend beyond clinical medicine and truly reflect the well-rounded and caring man he was – he will be missed.”
From Jason Katz, MD:
“Robb was a brilliant cardiologist, but most importantly he was a compassionate, caring, and beautiful human being. He had overcome so many obstacles over the last several years, and yet remained steadfast to the important things in life – his family, friends, and his passion for innovation. I am glad I had the chance to speak with him just a few weeks ago and was able to tell him how lucky we all felt to work with him. He represented the Duke family in such amazing ways.”
Highlights of the week:
Jill Engel named Service Line VP, Heart & Vascular Services
 Jill Engel, RN, DNP, FNP, ACNP, ANP, NEA-BC, FAANP, has been named Service Line Vice President – Heart & Vascular Services, Duke University Health System (DUHS), effective July 1, 2022. She holds a wealth of experience and expertise for our organization and was promoted to the role after an extensive and very competitive national search.
Jill Engel, RN, DNP, FNP, ACNP, ANP, NEA-BC, FAANP, has been named Service Line Vice President – Heart & Vascular Services, Duke University Health System (DUHS), effective July 1, 2022. She holds a wealth of experience and expertise for our organization and was promoted to the role after an extensive and very competitive national search.
Jill is a health care leader specializing in operational care redesign and strategic planning; programmatic design, development and financial planning; and a strong track record of recruiting, retaining, coaching and mentoring diverse and highly functional teams.
As an accomplished Advanced Practice Provider (APP) and nursing leader with an expertise and passion for advancing the mission of the heart and vascular service line, Jill served as interim Service Line VP – Heart & Vascular Services, DUHS, for nearly 18 months. During this time, Jill demonstrated her capabilities to strategically collaborate with physicians and colleagues, improve operational effectiveness and develop people. Prior to this interim role, Jill served as the nursing leader for the heart and vascular service line.
Additionally, she has served since 2020 as Academic Program Advisory Board member for Duke University School of Nursing and the Duke University School of Medicine (School of Cardiac Sonography).
The announcement was made on Thursday, June 2 by Craig Albanese, MD, executive vice president and chief operating officer for DUHS.
Personally, I will just add that Jill’s has been a great partner to work with and we are inspired by her ability to understand the issues that our clinical teams face in our day to day activities, her drive to improve patient care, and her ability to communicate broadly to our teams.
Please join us in congratulating Jill on her new executive leadership role!
Duke CTSI Announces MURDOCK Biorepository Initiative for Investigators
The Duke Clinical and Translational Science Institute (CTSI) has announced a new opportunity for Duke investigators to obtain biospecimens from the MURDOCK Study for research. The MURDOCK study is a landmark longitudinal cohort of more than 12,000 diverse participants linked to clinical data and up to 14 years of outcomes data.
investigators to obtain biospecimens from the MURDOCK Study for research. The MURDOCK study is a landmark longitudinal cohort of more than 12,000 diverse participants linked to clinical data and up to 14 years of outcomes data.
The MURDOCK Biorepository Transformation Initiative, led by the Duke Kannapolis Research group, will work with Duke investigators to convert samples into rich molecular datasets by facilitating access to these samples.
To make the MURDOCK samples easier to access, researchers will only incur costs for biospecimen retrieval and shipment.
“Through this science-forward initiative, we are making thousands of biospecimens and associated clinical and outcome data available to all Duke researchers,” said Svati Shah, MD, MHS, professor of medicine, associate dean for genomics, and director of Duke Kannapolis Research. “We are thrilled for the opportunity to share this powerful resource with more Duke collaborators, and we are incredibly grateful to the greater than 12,000 participants who contributed to one of the most unique biorepositories of its kind.”
The broad phenotypes included in the community-based MURDOCK cohort provide an excellent opportunity to study many different diseases and longitudinal outcomes, as well as serving as matched controls.
To read the full story, please visit: https://duke.is/2627y

Call for Heart Walk Captains, Walkers
Duke Health will once again participate in the Triangle Heart Walk and Dr. Rick Shannon has put out the call for team captains and walkers. Shannon is serving as the 2022 Heart Walk Campaign Chair.
The Heart Walk is the American Heart Association’s (AHA) premiere fundraising event that brings communities across the U.S. together to celebrate progress in the fight against heart disease and stroke, which remain the No. 1 and No. 5 leading causes of death in adult Americans.
In this year of renewal, we especially want to dedicate our efforts in remembrance of those members of the Duke family who have lost their lives or that of a loved one to heart disease and redouble our efforts to prevent these tragic losses.
After two years, the Triangle Heart Walk is planned as an in-person event this fall (date will be announced this summer). Our Duke Health theme is “We’re back—and together, we’re stronger than ever!” This will be a great opportunity to gather and celebrate one another and our efforts to reinvigorate heart-healthy lifestyles as well as raise lifesaving funds for the AHA.
We have set a goal of recruiting 350 team captains and 3,500 walkers to represent Duke Health, with a fundraising target of $350,000. Achieving this would make 2022 our most successful Heart Walk ever – and we can do this, together! Please consider becoming a team captain or committing to join a Duke Heart Walk team.
Registering as a team captain or walker is quick and easy.
- Visit https://www2.heart.org/site/TR/HeartWalk/GSA-GreaterSoutheastAffiliate?pg=entry&fr_id=7037
- Select the “Create new team” or the “Join a Team” button. Then complete the registration page.
- Personalize your page with a photo and send emails inviting others (co-workers, friends and family) to join the team and donate to your fundraiser.
If you have any questions, you can contact Sangeetha Menon, Development Director for the Triangle American Heart Association via email (sangeetha.menon@heart.org). She can help you get started.
Blumer Presents Final CGR of Season
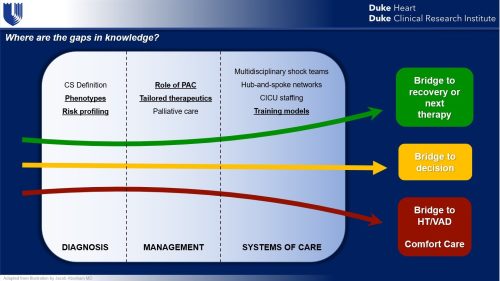
Vanessa Blumer, MD, cardiology fellow, presented our final cardiology grand rounds of the season on Tuesday evening, May 31. Her topic was “Heart Failure Cardiogenic Shock and the Golden Circle.” Vanessa walked us through her “why” for this area of research and provided the current evidence around detection, management, and the working group on cardiogenic shock. Great job!

Duke Heart Team Heads to Honduras
A team from Duke Heart, comprised of cardiothoracic surgeons, anesthesiologists, perfusionists, nurses, an engineer, a medical student and a surgery resident have left on a medical mission trip to Honduras. The team, part of an effort known as Duke Heart for Honduras, is headed to the country of approximately 10 million people which has almost no cardiac surgery practitioners or facilities, and a very high incidence of rheumatic valvular heart disease. The team will be in Honduras through June 12 to perform cardiac surgery at Honduras Medical Center in the capital city of Tegucigalpa. This is the second trip for Duke Heart for Honduras. The first trip was in 2019.

COVID-19 Update
All the latest Clinical Operations updates related to COVID can be found at https://covid-19.dukehealth.org. Patient-facing resources on DukeHealth.org can be found here: https://www.dukehealth.org/covid-19-update/resources. Duke University maintains a resource page as well, which can be accessed here: https://coronavirus.duke.edu/updates/for-staff.
Upcoming Events & Opportunities
Cardiology Grand Rounds
Cardiology Grand Rounds has concluded and will resume in September. Thanks for joining us – 2021-2022 has been a great year of presentations!
Duke-Stanford Cardiovascular Research Symposium
June 27 & 28. The Duke-Stanford Cardiovascular Research Symposium returns to Durham this year and is offered as a hybrid event. This symposium is sponsored by the Edna and Fred L. Mandel, Jr. Foundation.
offered as a hybrid event. This symposium is sponsored by the Edna and Fred L. Mandel, Jr. Foundation.
Registration required. In person: Great Hall, Mary Duke Biddle Trent Semans Center, Durham, NC. For those who wish to attend virtually, the event will offer live-streaming. The link will be emailed prior to the program. Registrants who choose the virtual live-streamed webinar option will be able to obtain CE credit for the course. For more information, contact Christy Darnell.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Division of Cardiology Publications Indexed in PubMed May 26 – June 1, 2022
Erickson ML, Wang W, Counts J, Redman LM, Parker D, Huebner JL, Dunn J, Kraus WE. Field-Based Assessments of Behavioral Patterns During Shiftwork in Police Academy Trainees Using Wearable Technology. J Biol Rhythms 2022 Jun;37(3):260-271. PM: 35416084.
Généreux P, Kirtane AJ, Kandzari DE, Armstrong EJ, Krucoff MW, Redfors B, Ben-Yehuda O, Lerew DR, Ali ZA, Maehara A, O’Neill WW, Stone GW. Randomized evaluation of vessel preparation with orbital atherectomy prior to drug-eluting stent implantation in severely calcified coronary artery lesions: Design and rationale of the ECLIPSE trial. Am Heart J 2022 Jul;249:1-11. PM: 35288105.
Jones WS, Wruck LM, Harrington RA, Hernandez AF. Iterative approaches to the use of electronic health records data for large pragmatic studies. Contemp Clin Trials 2022 Jun;117:106789. PM: 35545204.
Macedo AVS, de Barros E Silva PGM, de Paula TC, Moll-Bernardes RJ, Mendonça Dos Santos T, Mazza L, Feldman A, Arruda GDAS, de Albuquerque DC, de Sousa AS, de Souza OF, Gibson CM, Granger CB, Alexander JH, Lopes RD. Discontinuing vs continuing ACEIs and ARBs in hospitalized patients with COVID-19 according to disease severity: Insights from the BRACE CORONA trial. Am Heart J 2022 Jul;249:86-97. PM: 35405099.
Petek BJ, Moulson N, Drezner JA, Harmon KG, Kliethermes SA, Churchill TW, Patel MR, Baggish AL. Cardiovascular Outcomes in Collegiate Athletes After SARS-CoV-2 Infection: 1-Year Follow-Up From the Outcomes Registry for Cardiac Conditions in Athletes. Circulation 2022 May 31;145(22):1690-1692. PM: 35545946.
Pfeiffer CT, Paulo JA, Gygi SP, Rockman HA. Proximity labeling for investigating protein-protein interactions. Methods Cell Biol 2022 ;169:237-266. PM: 35623704.
Pokorney SD, Cocoros N, Al-Khalidi HR, Haynes K, Li S, Al-Khatib SM, Corrigan-Curay J, Driscoll MR, Garcia C, Calvert SB, Harkins T, Jin R, Knecht D, Levenson M, Lin ND, Martin D, McCall D, McMahill-Walraven C, Nair V, Parlett L, Petrone A, Temple R, Zhan. Effect of Mailing Educational Material to Patients With Atrial Fibrillation and Their Clinicians on Use of Oral Anticoagulants: A Randomized Clinical Trial. JAMA Netw Open 2022 May 2;5(5):e2214321. PM: 35639381.
Reading Turchioe M, Volodarskiy A, Pathak J, Wright DN, Tcheng JE, Slotwiner D. Systematic review of current natural language processing methods and applications in cardiology. Heart 2022 May 25;108(12):909-916. PM: 34711662.
Sandhu RK, Seiler A, Johnson CJ, Bunch TJ, Deering TF, Deneke T, Kirchhof P, Natale A, Piccini JP, Russo AM, Hills MT, Varosy PD, Araia A, Smith AM, Freeman J. Heart Rhythm Society Atrial Fibrillation Centers of Excellence Study: A survey analysis of stakeholder practices, needs, and barriers. Heart Rhythm 2022 Jun;19(6):1039-1048. PM: 35428582.
Shavadia JS, Alemayehu W, deFilippi C, Westerhout CM, Tromp J, Granger CB, Armstrong PW, van Diepen S. Novel multi-marker proteomics in phenotypically matched patients with ST-segment myocardial infarction: association with clinical outcomes. J Thromb Thrombolysis 2022 May;53(4):841-850. PM: 34708315.
Singer DE, Atlas SJ, Go AS, Lopes RD, Lubitz SA, McManus DD, Revkin JH, Mills D, Crosson LA, Lenane JC, Aronson RS. ReducinG stroke by screening for UndiAgnosed atRial fibrillation in elderly inDividuals (GUARD-AF): Rationale and design of the GUARD-AF randomized trial of screening for atrial fibrillation with a 14-day patch-based continuous ECG monitor. Am Heart J 2022 Jul;249:76-85. PM: 35472303.
Udell JA, Lu D, Bagai A, Dodson JA, Desai NR, Fonarow GC, Goyal A, Garratt KN, Lucas J, Weintraub WS, Forman DE, Roe MT, Alexander KP. Preexisting frailty and outcomes in older patients with acute myocardial infarction. Am Heart J 2022 Jul;249:34-44. PM: 35339451.
Duke Heart Pulse – week ending May 29th 2022
Memorial Day
This has been a difficult week for our country as we continue to struggle with the pattern of senseless gun violence and the safety of our communities. On behalf of the Duke Heart Leadership team, we’d like to wish all of you a very safe and peaceful Memorial Day weekend. As our nation takes time to remember all those who have been lost while serving in the U.S. military, we hope you’re able to spend some time in self-care, in reflection, and hopefully in the company of those most dear to you. Thank you for all that you do to make Duke Heart one of the very best places to work and care for others.
Duke Execs Kick-off Heart Walk Season
Cardiologist Rick Shannon, MD, Chief Quality Officer for Duke Health, is serving as the Triangle-area campaign chair for the 2022 Triangle Heart Walk. He recently hosted two Heart Walk kick-off events for senior leaders across Duke University Health System. The first was held May 12 at Duke University Hospital and the second was held on Thursday morning at Duke Raleigh.
Duke Heart’s leadership team shared highlights and successes of our ongoing partnership with the American Heart Association (AHA) both locally and nationally, as well as personal accounts of why supporting fundraising efforts like the Heart Walk are important. Cardiovascular disease and stroke have impacted most members of our team in some way — and hearing team members share their “why” stories and our efforts toward research, care and prevention was deeply inspiring.
We’re looking forward to a successful Heart Walk this fall–be on the lookout for more information. We’d like to make this our biggest and most successful year, ever! The date of the walk will be announced this summer.
Speaking of our AHA partnership, congratulations to our colleagues in the Duke Stroke Center! Two of their teams from Duke Raleigh Hospital participated in the Triangle CycleNation event held by the AHA on May 17 at Coastal Credit Union Midtown Park at North Hills in Raleigh. The teams raised funds to help fight stroke and increase awareness around stroke prevention and warning signs. Good work!




Highlights: AATS 2022
The American Association for Thoracic Surgery (AATS) 102nd annual meeting took place the weekend of May 14-17 in Boston.
Duke highlights included:
Presentations by thoracic surgeons Betty Tong and Matt Hartwig – they were each recognized during AATS 2022 with separate news briefs in the AATS Daily News on Monday, May 16 .

Tong was highlighted for her AATS presentation, “Lung Cancer Screening in 2022” which she gave on Saturday, May 14. Tong discussed study findings that demonstrate roughly five percent of screen-eligible patients are getting low-dose computed tomography (LDCT) scans of their chest to screen for lung cancer. Fairly recently, the U.S. Preventative Services Taskforce expanded screening guidelines that make an even larger number of patients screen-eligible, but Tong says, “only time will tell if more people get LDCT scans.” In her interview with AATS Daily News, Tong stated, “Adherence to screening guidelines and follow-up is suboptimal right now.” She discussed accessibility, budget constraints, socio-economic issues and general misconceptions about lung cancer screenings as issues that all contribute to low screening rates. See story on p. 4: https://duke.is/855sp.
Hartwig was highlighted to preview his presentation on proposals for an AATS

consensus document, “The Use of Mechanical Circulatory Support (MCS) for Lung Transplantation” which took place on Monday, May 16. “The AATS believes it’s important to provide the latest
guidance on how to best use modern MCS to benefit our patients before, during, and after lung transplantation,” Hartwig says in the piece. “Establishing an expert consensus document would be the most appropriate way to meet our needs.” See story on p. 6: https://duke.is/855sp.
Jacob Schroder presented the AATS consensus statement on DCD heart transplantation,

“Cardiac Transplantation Utilizing Donors Following Circulatory Death” on Saturday evening, May 15. The consensus statement will soon be published in the Journal of Thoracic and Cardiovascular Surgery; Schroder and Carmelo Milano are the first and senior authors.
Early EXACT Trial Findings Presented as AATS Late Breaker
The Epicardial Delivery of XC001 Gene Therapy for Refractory Angina Coronary Treatment (EXACT) trial is a first-in-human clinical trial examining the safety and efficacy of using an adenoviral vector to more efficiently deliver human vascular endothelial growth factor (VEGF) directly into the myocardium with the goal of stimulating angiogenesis in patients suffering from refractory angina due to advanced coronary artery disease (CAD). Readers may recall the trial launched at Duke last summer when study investigator and cardiothoracic surgeon Adam Williams  performed the first procedure on one of our Duke study participants.
performed the first procedure on one of our Duke study participants.
The preliminary findings in a small sample size of participants suggests a dose-response across several efficacy variables and supports continued investigation in the Phase 2 portion of the trial. Early clinical trial results were presented at AATS by Nahush Mokadam of Ohio State’s Wexner Medical Center, one of the site investigators, on Sunday, May 15.
Additional Duke investigators on the trial include: Tom Povsic, Duke site and national PI, and executive committee member E. Magnus Ohman, who Povsic credits with getting  this study to Duke.
this study to Duke.
- Related EXACT news: Povsic presented the 6-month follow up data “Preliminary Safety, Tolerability and Efficacy of Direct Epicardial Administration of Encoberminogene Rezmadenovec (XC001) to Ischemic Myocardium in Patients with Refractory Angina: Six Month Phase 1 Data for the EXACT Trial” at the American Society of Gene and Cell Therapy

Magnus Ohman in Boston on May 18th.
Additional Duke presenters at AATS included faculty members: Thomas D’Amico, Jacob Klapper, David Harpole, Edward Chen and Chad Hughes, as well as the following members of Duke’s general surgery residency program: Vignesh Raman, Christopher Jensen, Kristen Rhodin and Samuel Kesseli.
Impressive work! Congratulations to all!
NCDR Announces 2022 Chest Pain-MI Awards
 We are excited to share our latest performance achievement awards for the American College of Cardiology’s Chest Pain-MI Registry. This week we were notified by the National Cardiovascular Data Registry (NCRD) of our latest ratings across all three hospitals.
We are excited to share our latest performance achievement awards for the American College of Cardiology’s Chest Pain-MI Registry. This week we were notified by the National Cardiovascular Data Registry (NCRD) of our latest ratings across all three hospitals.
- Duke Regional Hospital: Silver
- Duke Raleigh Hospital: Platinum
- Duke University Hospital: Platinum
More than 2,400 hospitals and over 8,500 outpatient providers worldwide participate in one or more of the ACC’s ten registries, such as Chest Pain-MI, forming a comprehensive network of cardiovascular care providers committed to ensuring evidence-based cardiovascular care, improving patient outcomes and lowering health care costs.
The Chest Pain-MI Registry is the most trusted source for outcomes-based, continuous quality improvement, according to the ACC. It is the go-to registry for hospitals and health systems applying ACC and American Heart Association clinical guideline recommendations.
Congratulations to all!
Shout-out to Haney & Ashley!
We received a terrific note this week from Lisa Clark Pickett, Chief Medical Officer for Duke University Hospital, regarding team members Jack Haney and Ciarra Ashley and wanted to share it with you. Pickett wrote:
“Good Morning, Jack and Ciarra,
While reading comments on our Patient Satisfaction Survey I was just delighted to read this lovely compliment about you and your team. Thank you for your continual dedication to patients, professionalism, and excellence!”
The survey note read: “Dr. Haney and his medical team were awesome! Nurses on the 6 East Floor were very attentive to my needs & took excellent care of me. This was the BEST hospital stay for me.” – a grateful patient
Great job!

Kudos to Loriaux, Pagidipati!
We’re also sharing some warm compliments we received regarding cardiology fellow Dan Loriaux and faculty member Neha Pagidipati via Duke Health’s StarCard feedback system.

 “Dr. Pagidipati is an exceptional doctor. Dr. Dan Loriaux, fellow at Duke, is a remarkable young man. If he continues with cardiology, there is no one better to add to the Duke team. Both (Dan and Neha) are uniquely gifted,” the patient wrote (names are withheld in StarCard).
“Dr. Pagidipati is an exceptional doctor. Dr. Dan Loriaux, fellow at Duke, is a remarkable young man. If he continues with cardiology, there is no one better to add to the Duke team. Both (Dan and Neha) are uniquely gifted,” the patient wrote (names are withheld in StarCard).
Another wrote, “Excellent, compassionate care by Dr. Pagidipati. None better.”
Well done!
Latorre Nominated For Daisy Award
Amanda Latorre, one of our wonderful nurses on 7100, was recently nominated for a Daisy Award for providing compassionate care. She received the nomination from a patient’s daughter. The daughter had been present with her mother for the duration of the hospitalization as she was hesitant to leave and miss out on important information. Amanda put the daughter’s mind at ease with her excellent bedside manner and strong communication skills which allowed the daughter to leave for a night of good rest. Amanda also provided the patient with fresh toiletries and a moisturizing foot massage.
Thank you, Amanda, for the exceptional care you continue to provide for our Heart patients!

COVID-19 Update
All the latest Clinical Operations updates related to COVID can be found at https://covid-19.dukehealth.org. Patient-facing resources on DukeHealth.org can be found here: https://www.dukehealth.org/covid-19-update/resources. Duke University maintains a resource page as well, which can be accessed here: https://coronavirus.duke.edu/updates/for-staff.
Upcoming Events & Opportunities
Cardiology Grand Rounds
May 31: Heart Failure Cardiogenic Shock and the Golden Circle with Vanessa Blumer. 5 p.m., Webex.
Duke-Stanford Cardiovascular Research Symposium
June 27 & 28. The Duke-Stanford Cardiovascular Research Symposium returns to Durham this year and is offered as a hybrid event. This symposium is sponsored by the Edna and Fred L. Mandel, Jr. Foundation.
Registration required. In person: Great Hall, Mary Duke Biddle Trent Semans Center, Durham, NC. For those who wish to attend virtually, the event will offer live-streaming. The link will be emailed prior to the program. Registrants who choose the virtual live-streamed webinar option will be able to obtain CE credit for the course. For more information, contact Christy Darnell.

Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
May 20 — Richard Shannon
Axios
Red states aren’t prepared for a post-Roe baby boom
https://duke.is/v4vqs
May 23 — Jennifer Rymer
tctMD
DISRUPT PAD III: Lithotripsy Prep Linked to Better PAD Patency at 1 Year
https://duke.is/ycwfv
May 24 — Sunil Rao
Healio
SCAI president discusses results of the DIPRA trial
https://duke.is/5n3s8
May 24 — Marat Fudim
Medscape
Paradigm-Challenging Heart Failure Treatment Strategy Hopeful in Early Trial
https://duke.is/jze4f
Division of Cardiology Publications Indexed in PubMed May 19-25, 2022
Bier EA, Alenezi F, Lu J, Wang Z, Mammarappallil JG, O’Sullivan-Murphy B, Erkanli A, Driehuys B, Rajagopal S. Noninvasive diagnosis of pulmonary hypertension with hyperpolarised Xe magnetic resonance imaging and spectroscopy. ERJ Open Res 2022 May 16;8(2):00035-2022. PM:35586448.
DeVore AD, Hellkamp AS, Thomas L, Albert NM, Butler J, Patterson JH, Spertus JA, Williams FB, Shen X, Hernandez AF, Fonarow GC. The association of improvement in left ventricular ejection fraction with outcomes in patients with heart failure with reduced ejection fraction: data from CHAMP-HF. Eur J Heart Fail 2022 May;24(5):762-770. PM: 35293088.
Jawitz OK, Lawton JS, Thibault D, O’Brien S, Higgins RSD, Schena S, Vemulapalli S, Thomas KL, Zwischenberger BA. Sex Differences in Coronary Artery Bypass Grafting Techniques: A Society of Thoracic Surgeons Database Analysis. Ann Thorac Surg 2022 Jun;113(6):1979-1988. PM: 34280377.
Kelsey MD, Patrick-Lake B, Abdulai R, Broedl UC, Brown A, Cohn E, Curtis LH, Komelasky C, Mbagwu M, Mensah GA, Mentz RJ, Nyaku A, Omokaro SO, Sewards J, Whitlock K, Zhang X, Bloomfield GS. Inclusion and diversity in clinical trials: Actionable steps to drive lasting change. Contemp Clin Trials 2022 May;116:106740. PM: 35364292.
Kwapong YA, Boakye E, Obisesan OH, Shah LM, Ogunwole SM, Hays AG, Blumenthal RS, Creanga AA, Blaha MJ, Cainzos-Achirica M, Nasir K, Douglas PS, Wang X, Sharma G. Nativity-Related Disparities in Preterm Birth and Cardiovascular Risk in a Multiracial U.S. Cohort. Am J Prev Med 2022 Jun;62(6):885-894. PM: 35597568.
O’Brien EC, Sugarman J, Weinfurt KP, Larson EB, Heagerty PJ, Hernandez AF, Curtis LH. The impact of COVID-19 on pragmatic clinical trials: lessons learned from the NIH Health Care Systems Research Collaboratory. Trials 2022 May 21;23(1):424. PM: 35597988.
Rosenberg P. VDAC2 as a novel target for heart failure: Ca at the sarcomere, mitochondria and SR. Cell Calcium 2022 Jun;104:102586. PM: 35429733.
Saldarriaga C, Atar D, Stebbins A, Lewis BS, Abidin IZ, Blaustein RO, Butler J, Ezekowitz JA, Hernandez AF, Lam CSP, O’Connor CM, Pieske B, Ponikowski P, Roessig L, Voors AA, Anstrom KJ, Armstrong PW. Vericiguat in patients with coronary artery disease and heart failure with reduced ejection fraction. Eur J Heart Fail 2022 May;24(5):782-790. PM: 35239245.
Sata SS, Spratt SE, Edmonston DL, Pagidipati N. Clinical progress note: Indications for and management of sodium-glucose cotransporter-2 (SGLT-2) inhibitors in hospitalized patients. J Hosp Med 2022 May;17(5):360-363. PM: 35535917.
Schocken DD. Registry Evidence for Modulation of the Acute Ischemic Heart Disease Pathway: Statins Prevent Heart Failure? J Am Coll Cardiol 2022 May 24;79(20):2034-2036. PM: 35589165.
Stacey RB, Hall ME, Leaverton PE, Schocken DD, Zgibor J. Relation of glycemic status with unrecognized MI and the subsequent risk of mortality: The Jackson Heart Study. Am J Prev Cardiol 2022 May 10;11:100348. PM: 35600110.
Udell JA, Jones WS, Petrie MC, Harrington J, Anker SD, Bhatt DL, Hernandez AF, Butler J. Sodium Glucose Cotransporter-2 Inhibition for Acute Myocardial Infarction: JACC Review Topic of the Week. J Am Coll Cardiol 2022 May 24;79(20):2058-2068. PM: 35589167.
Duke Heart Pulse week ending May 22nd 2022
Highlights of the week:
Rao Named President of SCAI
 Sunil Rao, MD, professor of medicine in cardiology at Duke and section chief of cardiology at the Durham VA Health System, assumed the office of president of the Society for Cardiovascular Angiography & Interventions (SCAI) on Saturday evening during the SCAI 2022 Scientific Sessions being held May 19-22 in Atlanta, GA. He gave the presidential address.
Sunil Rao, MD, professor of medicine in cardiology at Duke and section chief of cardiology at the Durham VA Health System, assumed the office of president of the Society for Cardiovascular Angiography & Interventions (SCAI) on Saturday evening during the SCAI 2022 Scientific Sessions being held May 19-22 in Atlanta, GA. He gave the presidential address.
Rao graduated summa cum laude from Miami University in Oxford, OH, and magna cum laude from The Ohio State University College of Medicine where he won the David Saylor Memorial Award for cardiology research. He completed a residency in internal medicine and fellowships in cardiology and interventional cardiology at Duke University Medical Center. After his training, he joined the faculty at Duke University Medical Center as an assistant professor of medicine and rose to become professor of medicine in 2017. In 2005, he became the director of the catheterization laboratories at the Durham VA Medical Center, and in 2014, he was appointed chief of cardiology at the Durham VA. Rao has won several awards as an attending physician including the W. Proctor Harvey Award from the American College of Cardiology (2011), and the Duke Cardiology Fellows’ Mentoring Award (2013, 2018), and the DCRI Robert M. Califf MD Award for Fellow Mentoring (2020).
As the VA’s chief of cardiology, Rao has overseen the expansion of the faculty to increase patient access, start new clinical programs, and leverage VA research funding. New clinical programs include a structural heart disease service, a same-day discharge after PCI program, and a transradial PCI program. Under his leadership, the Durham VA is the leading transradial PCI center in the VA system nationally.
In September, Rao will begin a new role as director of interventional cardiology for the NYU Langone Health System in New York. At the national level, Rao serves as Editor-in-Chief of Circulation: Cardiovascular Interventions and is a former chair of the SCAI Quality Improvement Committee and was the program chair for the SCAI 2019 Scientific Sessions.
“It is a tremendous honor to lead SCAI during the next year as we continue to make meaningful progress towards the organization’s priorities outlined in our strategic plan, as well as empower and educate our members who are the leaders of interventional cardiology,” Rao stated. “I look forward to working with our members in the year ahead to improve patient outcomes.”
Congratulations, Sunil!
Additional SCAI Highlights: 
We had several current and former faculty and fellows present and moderate at SCAI. Raj Swaminathan was part of the SCAI program committee and former fellow Amit Vora (now at UPMC) was inducted into the Emerging Leader Mentorship program Congratulations, Raj and Amit!
Jennifer Rymer had two invited oral presentations: Managing bleeding in high risk ACS and Diversifying the Vascular Workforce and panel on cardiogenic shock. Great work, Jenn!

DCRI Fellows Graduation Reception Held
After three years without a formal Duke Clinical Research Institute (DCRI) Fellows’ Graduation Reception, the DCRI team was able to get together in person at the University Club in Durham on Tuesday evening, May 17. There, the team celebrated the accomplishments of nine graduating fellows and wholeheartedly thanked all the mentors and DCRI faculty and staff who supported them.
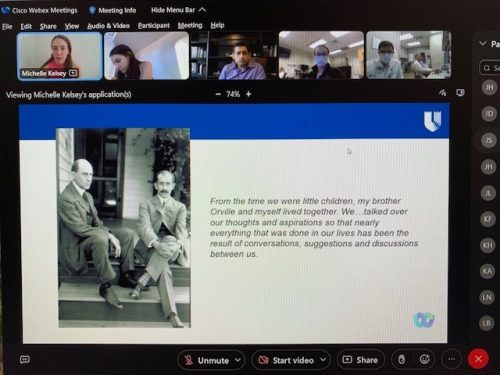
Graduating trainees from the Heart Center included: Drs. Michelle Kelsey, Andrew Vekstein, Vishal Rao, Vanessa Blumer, and Kelly Arps. The event was attended by several DCRI members/cardiology faculty including Drs. Adrian Hernandez, Manesh Patel, Michael Felker, and Robert Mentz. Several individuals were awarded as follows:
- The DCRI Fellows’ Citizenship Award was given to Andrew Vekstein, MD, resident in the CT Surgery Integrated Thoracic Surgery Residency Program. Mentor: John Alexander.
 The Robert A. Harrington Excellence in Fellowship Award was given to Michelle D. Kelsey, MD. Begun in 2012, this award is designed to recognize a graduating DCRI research fellow who has contributed the most to the DCRI fellowship during his/her tenure and who has demonstrated excellence in academic accomplishments, in participation in clinical research operations, and in peer-to-peer mentoring. Fellows considered for this award are expected to have demonstrated the following key attributes during their DCRI tenure: a passionate pursuit of innovative clinical research, humility, inclusiveness, loyalty to colleagues, consensus-building, and selflessness. All graduating DCRI research fellows are eligible for this award.
The Robert A. Harrington Excellence in Fellowship Award was given to Michelle D. Kelsey, MD. Begun in 2012, this award is designed to recognize a graduating DCRI research fellow who has contributed the most to the DCRI fellowship during his/her tenure and who has demonstrated excellence in academic accomplishments, in participation in clinical research operations, and in peer-to-peer mentoring. Fellows considered for this award are expected to have demonstrated the following key attributes during their DCRI tenure: a passionate pursuit of innovative clinical research, humility, inclusiveness, loyalty to colleagues, consensus-building, and selflessness. All graduating DCRI research fellows are eligible for this award.- The Eric D. Peterson Manuscript Award was given to Vishal N. Rao, MD. Rao won the Peterson award for his JACC
 paper In-Hospital Initiation of Sodium-Glucose Cotransporter-2 Inhibitors for Heart Failure With Reduced Ejection Fraction. This award recognizes a DCRI fellow whose writing excellence is demonstrated in at least one impactful and novel medical article. Through this award, the fellowship program recognizes Dr. Eric D. Peterson, a former DCRI Director, and his contributions to the DCRI fellowship program.
paper In-Hospital Initiation of Sodium-Glucose Cotransporter-2 Inhibitors for Heart Failure With Reduced Ejection Fraction. This award recognizes a DCRI fellow whose writing excellence is demonstrated in at least one impactful and novel medical article. Through this award, the fellowship program recognizes Dr. Eric D. Peterson, a former DCRI Director, and his contributions to the DCRI fellowship program.
In commenting on the event, Sana Al-Khatib, MD, DCRI Fellowship Program Director said, “Congratulations to all the graduating fellows! It was truly wonderful to have the opportunity to celebrate them and to thank everyone who supported them in person. We are very proud of the amazing accomplishments of our trainees and look forward to seeing how they will shape the future and make a difference for patients and the world. We appreciate the tremendous commitment of our faculty and staff who work tirelessly to support our mission to train the next generations.”
Congratulations, Michelle, Andrew, Vishal, Vanessa & Kelly! You are all amazing!



Fudim Presents LBCT at Heart Failure 2022
Marat Fudim, MD, MHS, presented data from the REBALANCE-HF trial this morning (May 22) as part of late-breakers at the Heart Failure 2022 & World Congress on Acute Heart Failure, the annual congress of the Heart Failure Association of the European Society of Cardiology, being held this weekend in Madrid (May 21-24).

The REBALANCE-HF trial is examining the safety and efficacy of a splanchic nerve ablation in patients with heart failure with preserved ejection fraction (HFpEF). Fudim reported on the first 18 patients with HFpEF to have been enrolled into the roll-in, open-label arm of the study. The findings were simultaneously published in the European Journal of Heart Failure.
The preliminary open-label results support the safety and efficacy of splanchnic ablation for volume management (SAVM) in HFpEF. The findings require confirmation in the ongoing randomized, sham-controlled portion of the trial.
In addition to Fudim, Manesh Patel is a co-author. Additional authors from other institutions include Peter S. Fail, Sheldon E. Litwin, Tamaz Shaburishvili, Parag Goyal, Scott Hummel, Barry A. Borlaug, Rajeev C. Mohan, Ravi B. Patel, Sumeet S. Mitter, Liviu Klein, Krishna Rocha-Singh, Vivek Y. Reddy, Daniel Burkhoff and Sanjiv J. Shah.
Congratulations, Marat!
Milano Named Beard Distinguished Professor

Congratulations to Carmelo Milano, MD, professor of surgery in the Division of Cardiovascular and Thoracic Surgery. He has been named the Joseph W. and Dorothy W. Beard Distinguished Professor of Experimental Surgery effective July 1.
Distinguished professorships are awarded to faculty who have demonstrated extraordinary scholarship in advancing science and improving human health. Milano is one of 16 faculty members in the Duke School of Medicine to be awarded a distinguished professorship this year. David Harpole is another; his distinguished professorship was mentioned in a Pulse post last month. The SOM officially announced all professorship on May 19.
To read about each of the 2022 distinguished professorships, please visit: https://medschool.duke.edu/news/meet-school-medicines-2022-distinguished-professors.
Congratulations, Carmelo!
Kelsey on CV Prevention at CGR
Michelle Kelsey presented an engaging cardiology grand rounds on Tuesday, May 17. In CV Prevention: Taking Flight, Kelsey discussed a range of factors impacting cardiovascular disease prevention, including BP guideline variance and too few specialists available to efficiently monitor the 34.2 million people with type 2 diabetes. She stressed the importance of teamwork, comparing it to that of the Wright brothers’ whose partnership made the first successful aircraft flight possible.
Great presentation, Michelle!
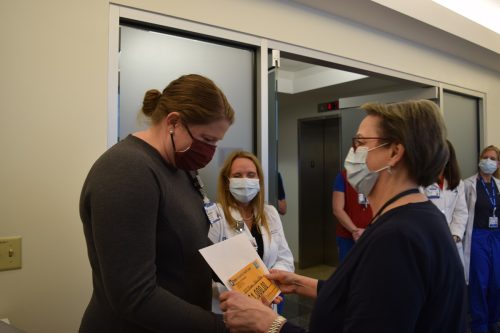
2022 FON Excellence Award Winners Celebrated
The 33rd Duke Friends of Nursing (FON) Annual Gala was held last weekend at the Durham Convention Center. Thirty-seven Duke nurses were recognized with Excellence Awards; all 216 nominees and the contributions of Duke nurses across Duke University Health System were celebrated. Each winner was recognized individually with a Friends of Nursing pin, a certificate, an engraved trophy, and a $1,000 education stipend. To watch a replay of the entire celebration from last weekend, click here.
The following Duke Heart team members were recognized with Excellence Awards:
- Ciarra Ashley
- Jo Nocito
- Gilbert Thomas Rutledge
- Diane M. Sauro
- Dustin Tart
- Mutya Valente
- Melissa Williams
FON was launched in 1988 thanks to the vision of Martha White Blalock and Dan S. Blalock Jr., grateful patients who sought a way to thank the nurses who were caring for them during Martha’s hospitalization at Duke. Following Martha’s death, Dan collaborated with others to establish the Friends of Nursing program. He remained closely involved until his passing in 2017. Through the Daniel S. Blalock Jr. Charitable Foundation, Dan continues to make a difference at Duke.
During the 2022 nomination cycle, FON received nominations across all settings of care, with many nurses receiving multiple submissions. The nominations came from patients and their loved ones, and from other nurses and interprofessional colleagues.
“My sincere thanks to those who nominated a colleague,” said Mary Ann Fuchs, vice president of patient care and system chief nurse executive for Duke University Health System. “When you take the time to submit a nomination, you enhance the person’s sense of purpose and well-being, and you help to build a supportive work culture.”
Friends of Nursing nominations are open year-round. To learn more or to nominate a colleague, please visit: https://dukefriendsofnursing.org/nominate-a-nurse.
Congratulations, Ciarra, Jo, Gilbert, Diane, Dustin, Mutya and Melissa! We are so happy for you!






ICYMI: CardioNerds launches AF Series with Arps as Co-Chair
 Our friends at CardioNerds have launched a new series on Atrial Fibrillation. Duke cardiology fellow Kelly Arps co-chairs the series with Colin Blumenthal, a fellow at the University of Pennsylvania. The series launched this week with episode #208, featuring Larry Jackson.
Our friends at CardioNerds have launched a new series on Atrial Fibrillation. Duke cardiology fellow Kelly Arps co-chairs the series with Colin Blumenthal, a fellow at the University of Pennsylvania. The series launched this week with episode #208, featuring Larry Jackson.  Arps and Blumenthal were joined by Dinu-Valentin Balanescu, rising internal medicine chief resident at Beaumont Hospital, to interview Jackson. The topic is Atrial Fibrillation: Epidemiology, Health Equity, & The Double Paradox with Dr. Larry Jackson. Not to be missed – this will be a terrific series!
Arps and Blumenthal were joined by Dinu-Valentin Balanescu, rising internal medicine chief resident at Beaumont Hospital, to interview Jackson. The topic is Atrial Fibrillation: Epidemiology, Health Equity, & The Double Paradox with Dr. Larry Jackson. Not to be missed – this will be a terrific series!
Great job, Kelly and Larry!
COVID-19 Update
All the latest Clinical Operations updates related to COVID can be found at https://covid-19.dukehealth.org. Patient-facing resources on DukeHealth.org can be found here: https://www.dukehealth.org/covid-19-update/resources. Duke University maintains a resource page as well, which can be accessed here: https://coronavirus.duke.edu/updates/for-staff.
Upcoming Events & Opportunities
Cardiology Grand Rounds
May 24: Global Cardiovascular Health in the Peri-Pandemic Era with Mark Huffman of Washington University School of Medicine. 5 p.m. Webex.
May 31: Heart Failure Cardiogenic Shock and the Golden Circle with Vanessa Blumer. 5 p.m., Webex. (Link not yet available.)
Duke-Stanford Cardiovascular Research Symposium
 June 27 & 28. The Duke-Stanford Cardiovascular Research Symposium returns to Durham this year and is offered as a hybrid event. This symposium is sponsored by the Edna and Fred L. Mandel, Jr. Foundation.
June 27 & 28. The Duke-Stanford Cardiovascular Research Symposium returns to Durham this year and is offered as a hybrid event. This symposium is sponsored by the Edna and Fred L. Mandel, Jr. Foundation.
Registration required. In person: Great Hall, Mary Duke Biddle Trent Semans Center, Durham, NC. For those who wish to attend virtually, the event will offer live-streaming. The link will be emailed prior to the program. Registrants who choose the virtual live-streamed webinar option will be able to obtain CE credit for the course. For more information, contact Christy Darnell.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
May 12 — Duke Heart
El Heraldo (Honduras)
Brigada regresa al país para aliviar corazones de personas sin recursos
https://duke.is/jtkus
May 15 — Robert Mentz
CBS Mornings
Spirituality can improve outcomes for patients with heart failure (*clip begins @ 01:52:52)
https://duke.is/ykwk3
May 17 — Salim Idriss
Applied Clinical Trials
The Need For Pediatric Clinical Trials and Data
https://duke.is/468ja
May 19 — Sunil Rao
Medpage Today
Distal Radial Artery PCI Access Doesn’t Hurt the Hand
https://duke.is/gw6wg
May 20 — Kelly Arps and Larry Jackson
CardioNerds (#208)
Atrial Fibrillation: Epidemiology, Health Equity, & The Double Paradox with Dr. Larry Jackson
Division of Cardiology Publications Indexed in PubMed May 12-18, 2022
Asher WB, Terry DS, Gregorio GGA, Kahsai AW, Borgia A, Xie B, Modak A, Zhu Y, Jang W, Govindaraju A, Huang LY, Inoue A, Lambert NA, Gurevich VV, Shi L, Lefkowitz RJ, Blanchard SC, Javitch JA. GPCR-mediated β-arrestin activation deconvoluted with single-molecule precision. Cell 2022 May 12;185(10):1661-1675.e16. PM: 35483373.
Bhatt AS, Fonarow GC, Greene SJ. Prioritizing prevention of de novo and worsening chronic heart failure. Eur J Heart Fail 2022 Apr;24(4):653-656. PM: 35218135.
Campbell MM, Benjamin DK, Mann T, Fist A, Kim H, Edwards L, Rak Z, Brookhart MA, Anstrom K, Moore Z, Tilson EC, Kalu IC, Boutzoukas AE, Moorthy GS, Uthappa D, Scott Z, Weber DJ, Shane AL, Bryant KA, Zimmerman KO. Test-to-Stay After Exposure to SARS-CoV-2 in K-12 Schools. Pediatrics 2022 May 1;149(5):e2021056045. PM: 35437593.
DeFilippis EM, Blumer V, Mentz RJ, Agarwal R, Haythe JH, Kittleson M. In-Hospital Outcomes in Pregnancy After Heart Transplantation. Am J Cardiol 2022 Jun 1;172:68-72. PM: 35331474.
Eiger DS, Smith J, Shi T, Stepniewski TM, Honeycutt C, Boldizsar N, Gardner J, Tsai CF, Nicora C, Moghieb A, Kawakami K, Choi I, Smith R, Inoue A, Selent J, Jacobs J, Rajagopal S. Phosphorylation barcode ensembles encoded by biased CXCR3 agonists direct non-redundant chemokine signaling. FASEB J 2022 May;36 Suppl 1:10.1096/fasebj.2022.36.S1.0R486. PM: 35554623.
Fordyce CB, Hill CL, Mark DB, Alhanti B, Pellikka PA, Hoffmann U, Patel MR, Douglas PS. Physician judgement in predicting obstructive coronary artery disease and adverse events in chest pain patients. Heart 2022 May 12;108(11):860-867. PM: 35110385.
Gardner J, Eiger D, Boldizsar N, Honeycutt CC, Kirchner S, Hicks C, Choi I, Zheng K, Warman A, Smith J, Zhang J, Rajagopal S. Location Bias Contributes to Functionally Selective Responses of Biased CXCR3 Agonists to Regulate Inflammation. FASEB J 2022 May;36 Suppl 1:10.1096/fasebj.2022.36.S1.0R865. PM: 35555971.
Harrington J, Tseliou E, Shah S, Shah KS. Paying Homage to the Power of Proteomics: Insights Into Obesity and Heart Failure From the HOMAGE Trial. J Card Fail 2022 May;28(5):787-788. PM: 35304349.
Hicks CN, Eiger D, Gardner J, Boldizsar N, Honeycutt C, Choi I, Rajagopal S. Location Bias of G Protein-Coupled Receptor Kinases Promotes Biased Signaling at CXCR3. FASEB J 2022 May;36 Suppl 1:10.1096/fasebj.2022.36.S1.R2182. PM: 35554028.
Kohlmann T, Lee C, Rajagopal S. Determining the Requirements for Gαi:β-arrestin Complex Formation at G Protein-Coupled Receptors. FASEB J 2022 May;36 Suppl 1:10.1096/fasebj.2022.36.S1.R5812. PM: 35554641.
Krychtiuk KA, Granger CB. In older persons at risk for dementia, a multidomain approach reduced stroke and transient ischemic attack. Ann Intern Med 2022 May;175(5):JC55. PM: 35500268.
Krychtiuk KA, Newby LK. Moderna COVID-19 vaccine was linked to myocarditis or myopericarditis at 28 d (4.2 events/100 000 persons). Ann Intern Med 2022 May;175(5):JC58. PM: 35500266.
Lala A, Lopes RD, Mentz RJ. International Collaborations in Heart Failure: JCF in Latin America. J Card Fail 2022 May;28(5):695-696. PM: 35559918.
Lee C, Kohlmann T, Xiong X, Rajagopal S. Regulation of Endothelial Cell function by Integration of Gαi and β-arrestin signaling at Atypical Chemokine Receptor 3. FASEB J 2022 May;36 Suppl 1:10.1096/fasebj.2022.36.S1.R6324. PM: 35554058.
Lewis GD, Docherty KF, Voors AA, Cohen-Solal A, Metra M, Whellan DJ, Ezekowitz JA, Ponikowski P, Böhm M, Teerlink JR, Heitner SB, Kupfer S, Malik FI, Meng L, Felker GM. Developments in Exercise Capacity Assessment in Heart Failure Clinical Trials and the Rationale for the Design of METEORIC-HF. Circ Heart Fail 2022 May;15(5):e008970. PM: 35236099.
Li A, Liu S, Huang R, Ahn S, Lefkowitz RJ. Loss of Biased Signaling Specificity of the Angiotensin II Type 1 Receptor in Overexpressed Systems. FASEB J 2022 May;36 Suppl 1:10.1096/fasebj.2022.36.S1.R2797. PM: 35555965.
Lowenstern A, Alexander KP, Pagidipati NJ, Hill CL, Pellikka PA, Cooper LS, Alhanti B, Hoffmann U, Mark DB, Douglas PS. Presenting Symptoms in Patients Undergoing Coronary Artery Disease Evaluation: Association With Noninvasive Test Results and Clinical Outcomes in the PROMISE Trial. Circ Cardiovasc Qual Outcomes 2022 May;15(5):e008298. PM: 35369715.
Minhas AMK, Ijaz SH, Jamal S, Dani SS, Khan MS, Greene SJ, Fudim M, Warraich HJ, Shapiro MD, Virani SS, Nasir K, Khan SU. Trends in Characteristics and Outcomes in Primary Heart Failure Hospitalizations Among Older Population in the United States, 2004 to 2018. Circ Heart Fail 2022 May;15(5):e008943. PM: 35078346.
Mullens W, Martens P, Testani JM, Tang WHW, Skouri H, Verbrugge FH, Fudim M, Iacoviello M, Franke J, Flammer AJ, Palazzuoli A, Barragan PM, Thum T, Marcos MC, Miró Ò, Rossignol P, Metra M, Lassus J, Orso F, Jankowska EA, Chioncel O, Milicic D, Hill L et al. Renal effects of guideline-directed medical therapies in heart failure: a consensus document from the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail 2022 Apr;24(4):603-619. PM: 35239201.
Patel JN, Abramov D, Fudim M, Okwuosa IS, Rabkin DG, Chung JS. The heart transplant allocation change attenuates but does not eliminate blood group O waitlist outcome disadvantage. Clin Transplant 2022 May;36(5):e14620. PM: 35213753.
Pham U, Chundi A, Rajagopal S. Distinct Spatial Conformations and Trafficking Patterns of β-arrestin Isoforms in AT1R Signaling. FASEB J 2022 May;36 Suppl 1:10.1096/fasebj.2022.36.S1.L7742. PM: 35559563.
Price MJ, Valderrábano M, Zimmerman S, Friedman DJ, Kar S, Curtis JP, Masoudi FA, Freeman JV. Periprocedural Pericardial Effusion Complicating Transcatheter Left Atrial Appendage Occlusion: A Report From the NCDR LAAO Registry. Circ Cardiovasc Interv 2022 May;15(5):e011718. PM: 35369701.
Razaghizad A, Oulousian E, Randhawa VK, Ferreira JP, Brophy JM, Greene SJ, Guida J, Felker GM, Fudim M, Tsoukas M, Peters TM, Mavrakanas TA, Giannetti N, Ezekowitz J, Sharma A. Clinical Prediction Models for Heart Failure Hospitalization in Type 2 Diabetes: A Systematic Review and Meta-Analysis. J Am Heart Assoc 2022 May 17;11(10):e024833. PM: 35574959.
Remillard TC, Cronley AC, Pilch NA, Dubay DA, Willner IR, Houston BA, Jackson GR, Inampudi C, Ramu B, Kilic A, Fudim M, Wright SP, Hajj ME, Tedford RJ. Hemodynamic and Clinical Determinants of Left Atrial Enlargement in Liver Transplant Candidates. Am J Cardiol 2022 Jun 1;172:121-129. PM: 35341576.
Van Belle E, Patel M, Davies J. Fractional Flow Reserve-Guided PCI as Compared with Coronary Bypass Surgery. N Engl J Med 2022 May 12;386(19):1863-1864. PM: 35544399.
Yaranov DM, Jefferies JL, Silver MA, Burkhoff D, Rao VN, Fudim M. Discordance of Pressure and Volume: Potential Implications for Pressure-Guided Remote Monitoring in Heart Failure. J Card Fail 2022 May;28(5):870-872. PM: 35158025.
Zeitouni M, Marquis-Gravel G, Smilowitz NR, Zakroysky P, Wojdyla DM, Amit AP, Rao SV, Wang TY. Prophylactic Mechanical Circulatory Support Use in Elective Percutaneous Coronary Intervention for Patients With Stable Coronary Artery Disease. Circ Cardiovasc Interv 2022 May;15(5):e011534. PM: 35580202.
Zhang Y, Kontos CD, Annex BH, Popel AS. Endothelial Regulation of Microvascular Growth and Stability by Ang-Tie and VEGF Signaling Pathways: A Mechanistic Computational Systems Biology Model. FASEB J 2022 May;36 Suppl 1:10.1096/fasebj.2022.36.S1.R2072. PM: 35560284.
Zhu H, Yin X, Holley CL, Meyer KD. Improved Methods for Deamination-Based mA Detection. Front Cell Dev Biol 2022 Apr 27;10:888279. PM: 35573664.
Duke Heart Pulse – week ending May 15th 2022
Highlights of the week:
Wang Receives Lifetime Achievement Award at QCOR22
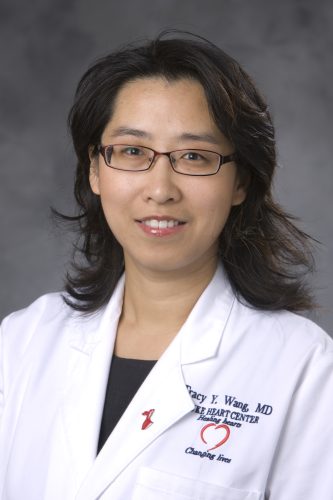
Congratulations to Tracy Y. Wang, MD, professor of medicine in cardiology, director of Health Services & Outcomes Research, and Duke Clinical Research Institute member, has received the American Heart Association’s Council on Quality of Care and Outcomes Research (QCOR) 2022 Outstanding Lifetime Achievement Award! The award was presented earlier this weekend during the QCOR Scientific Sessions (May 13-14) in Reston, VA. Wang gave the keynote address.
The QCOR lifetime achievement award is presented to a QCOR council member for their significant long-term contributions to outcomes research and the improvement of cardiovascular care. Candidates are selected annually by QCOR’s nominating committee and the winner is selected by their leadership committee.
“Well, I guess this award makes me officially old now,” said Wang ahead of the award presentation. “Duke has such a unique environment that has allowed me to explore my interests and grow in delightfully unexpected ways. I’ve benefited from incredible mentorship, and am rejuvenated daily working alongside creative younger minds who want to make a difference in how we take care of patients.”
She received a number of accolades on Twitter, including:
“There’s no smarter researcher, more supportive mentor, or better human being in cardiology.” – Alex Fanaroff, MD, former Duke cardiology fellow.
“She is a brilliant physician scientist, and more importantly a truly wonderful person. Well deserved. Just wondering what she’ll do with the second half of her life???” — Women as One
“Exceptional clinician, researcher, educator, leader, sponsor, mentor, and friend.” — Vanessa Blumer, MD, Duke cardiology fellow.
“Such a well-deserved honor. Had to travel to Reston VA to see her IRL!”– Rob Mentz, MD
In addition to Wang, a number of current and former Duke faculty and fellows presented at QCOR including Emily O’Brien, Lesley Curtis, Alex Fanaroff, Mike Nanna, Jenn Rymer, Ajar Kochar, Rob Mentz, Vanessa Blumer, and Stephen Greene.
A perspective piece by Wang – “Mentorship and the Leaky Pipeline in Academic Cardiology” — was published in Circulation: Cardiovascular Quality and Outcomes during her award speech on Friday. A link to it can be found here: https://duke.is/yy65w.
Congratulations, Tracy! We are so proud of you – way to go!


Update: High-Sensitivity Troponin I (hsTnI), Effective 5/17 at DUH
Beginning May 17, 2022, High-Sensitivity Troponin I (hsTnI) will replace the current High-Sensitivity Troponin T test at Duke University Hospital. There will be no fundamental changes to the hsTn algorithm, results/interpretations reporting, or ordering. The hsTnI numerical thresholds are nearly identical to those for hsTnT, and the interpretations and disposition guidance that go with them will be available as currently and are unchanged.
Additional information is available through the following links:
High Sensitivity Troponin I for Providers: https://intranet.dh.duke.edu/sites/MaestroCare/Maestro%20Care%20Training%20Supplements/High%20Sensitivity%20Troponin%20I%20for%20Providers.pdf
Troponin I Smarttext tipsheet (PPT): https://intranet.dh.duke.edu/sites/MaestroCare/Maestro%20Care%20Training%20Supplements/Troponin%20I%20Smarttext%20tipsheet.pptx?d=wb2ba5706a7da4939bd620ddc971b5d21
SOM Faculty Awards Dinner Honors 2020-2022 Awardees
The Duke School of Medicine annual faculty awards dinner was held this week at the Sarah Duke Gardens. A number of Duke Heart faculty members were in attendance, including Cary Ward, Carmelo Milano and Manesh Patel – our 2022 awardees. Due to the pandemic, the awards dinner had not been held in person for two years. Awardees for 2020 or 2021 were invited to join the festivities. A recap of our current and past awardees:


- Ward and Milano were co-winners of the 2022 Palumbo award which recognizes dedication to compassionate patient care and excellence in the teaching and mentoring of young physicians.
- Manesh Patel received the 2022 Career Mentoring Award in Clinical Research/Population Health.
- 2021: Kevin Thomas was the recipient of the Excellence in Professionalism Award, which recognizes the importance of promoting ethical and professional behavior in our community.
- 2021: Robert Mentz received the Early Career Research Mentoring Award in Clinical/Population Health Science.
- 2021: Terry Fortin received the Master Clinician/Teacher Award, which honors individuals with superlative accomplishment and service in the areas of clinical care and teaching
- 2020: Larry Crawford received the Excellence in Professionalism Award. As noted above, the award is given to a faculty member that exemplifies ethical and professional behavior in our community. Recipients represent Duke’s guiding principles of respect, trustworthiness, diversity, teamwork, and learning.
- 2020: Mike Sketch received the Leonard Tow Humanism in Medicine Award.
- 2020: Tracy Wang received the Early Career Mentoring Award in Clinical/Population Health Science.
We are so proud of each one of you. Congratulations!





2022 AATS Underway in Boston
The American Association for Thoracic Surgery’s 102nd annual meeting is underway in Boston (May 14-17) and we’re giving a shout-out to all Duke team members in attendance!

A very special congratulations to Jeff Gaca, MD and Jacob Klapper, MD – both surgeons were elected to AATS and officially inducted this weekend. Such great news! Founded in 1917, the American Association for Thoracic Surgery (AATS), is comprised of more than 1,500 of the world’s foremost cardiothoracic surgeons from 46 countries. We are excited for both of them.
We’ll have coverage of key Duke presentations next weekend.

Arlene Martin Departs Fellowship Program
We are saddened to have said goodbye to one of our long-term Duke Heart team members this week. Arlene Martin, our wonderful GME program coordinator for the Cardiovascular Disease fellowship, the Advanced Training in Cardiology fellowship, and the Clinical Investigator Pathway-Cardiovascular Disease fellowship has left Duke in order to focus on family needs. Her last day with us was May 11.
Arlene has worked closely with the fellowship program for more than a decade — and it’s hard to imagine the fellowship program without her. She has done an incredible job for us and for our fellows!
From Anna Lisa Chamis, MD, current program director:
“Arlene has diligently served as program coordinator for multiple Division of Cardiology fellowships since 2011. During that time, she supported 9 program directors and ~140 trainees. Notably, she helped launch 2 new ACGME fellowship programs at Duke and spearheaded the initial site accreditation for those programs. Arlene also worked tirelessly to help us apply for grants/ external funding to support our fellowship programs, assisting in the acquisition of $2.3 million in salary and benefits for our fellowship programs during her tenure. Not surprisingly, she was awarded the 2015-2016 Fellows’ staff service award. Personally, Arlene has taught me so much about the administrative regulations and policies surrounding our programs, and I am grateful to have benefitted from her vast knowledge and experience.”
From Andrew Wang, MD:
“Arlene actually began her work at Duke as my administrative assistant, but helped with tasks for the previous program coordinator too. When the program coordinator role became available, she expressed her interest, applied, and was clearly the most qualified candidate (even with little knowledge of ACGME requirements at that time). In nearly 10 years of working with her as our program coordinator, she was dedicated to improving our program as well as the experience and environment for our fellows. She made important and lasting improvements in our fellowship program. She brought our program from the “paper chart” era to the electronic era. She took on new responsibilities and learned new skills, including grant-writing to support our fellows, with rapid adeptness and competency. In all of her work, she demonstrates a strong sense of ownership, conscientiousness, timeliness, and high quality. I wish her the best in her future endeavors and thank her for her support and contributions to our fellowship program.”
From Svati Shah, MD:
“Arlene has done an incredible job as the Cardiology Fellowship Program Director! I had the honor of being an Associate Program Director with Arlene for many years. She has balanced the intense responsibilities of this job beautifully. She did so much work quietly behind the scenes to make sure we had a robust (and compliant!) fellowship. I am so grateful for how much she taught me and helped me grow as an APD. She will be greatly missed.”
From Amanda Coniglio, MD, (outgoing chief cardiology fellow)
“Arlene has always gone above and beyond to make sure the fellows and program were supported. She has paid meticulous attention to detail and has always been quick to help when needed. She will be greatly missed!”
From Christopher Wrobel, MD (incoming chief cardiology fellow):
“Arlene has been an invaluable asset to the fellowship. She has superhuman organizational prowess that I hope to have a fraction of some day. She has always been understanding of my (occasional) lapses, and gently guided me on the road to full compliance. I know I and all of the other fellows will remain greatly indebted to Arlene for all of her work over the years. We will miss you greatly Arlene!”
She truly has been a behind-the-scenes person helping make “all the things” happen. Thank you so much for all you’ve done for us, Arlene! We wish you all the best!
ICYMI: Frazier-Mills Interviewed by HeartRhythm TV
Camille Frazier-Mills, MD appears in a recent episode of the Women in EP – Mentorship Series on HeartRhythm TV (YouTube). The topic last weekend was Heart Rhythm Society DEI Council: Inclusion Series, Closing the Sex Gap. She was interviewed along with Annabelle Volgman of Rush University Medical Center. Among other factors, Frazier Mills says early exposure and mentorship are key to getting more women to specialize in electrophysiology. This is definitely worth watching! Check it out here: https://duke.is/ru8mb.
D’Amico Named Associate Editor, Annals of Surgery
 Congratulations to Thomas D’Amico, MD, the Gary Hock Endowed Professor of Surgery and Chief, Section of General Thoracic Surgery in the Division of Cardiovascular and Thoracic Surgery. He was recently named associate editor for thoracic surgery for the journal Annals of Surgery. D’Amico is currently serving a two-year term as medical director of the AATS.
Congratulations to Thomas D’Amico, MD, the Gary Hock Endowed Professor of Surgery and Chief, Section of General Thoracic Surgery in the Division of Cardiovascular and Thoracic Surgery. He was recently named associate editor for thoracic surgery for the journal Annals of Surgery. D’Amico is currently serving a two-year term as medical director of the AATS.
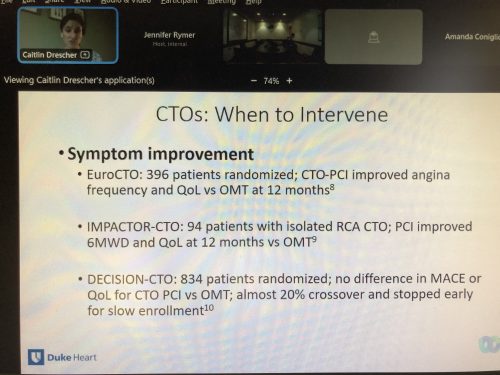
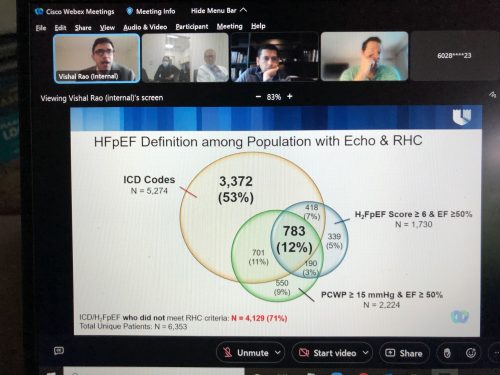
Dresher & Rao Presented CGR
We had two terrific cardiology grand rounds presentations this past week. On Tuesday, cardiology fellow Caitlin Dresher presented on coronary CTOs and cardiac MRI, and on Thursday, cardiology fellow Vishal Rao presented on gaps in care delivery and phenotyping across the spectrum of heart failure along with strategies for improvement. Nicely done!
Nurses Week 2022: Our 1st Daisy Award!
We want to close out Nurses Week with another round of thanks to all our terrific Duke Heart nurses! We hope you enjoyed some of the special events that were held to celebrate you this past week. Shown here are Duke Heart CVSSU RNs enjoying mid-morning Coffee Cart with Mary Lindsay and Joe Kelly!

In other great news this week, we learned that Zac Snell, RN on 6East has received the first DAISY Award for the Heart Center! The awards are given by the Daisy Foundation, which is an international foundation that was formed in November 1999 by the family of J. Patrick Barnes, a patient who passed away due to complications of Idiopathic Thrombocytopenic Purpura (ITP). The nursing care that Patrick received when hospitalized profoundly touched his family; they launched the Foundation in his memory. Nurses who demonstrate extraordinary and compassionate care are nominated by patients and family members.
Zac is pictured below with 6E team members, Heart Center leadership, and leadership from DUH. Great job, Zac! Well done.
The week culminated with the annual Friends of Nursing Gala, which was held last night. We will have coverage of all Duke Heart winners and photos next weekend!

COVID-19 Update
All the latest Clinical Operations updates related to COVID can be found at https://covid-19.dukehealth.org. Patient-facing resources on DukeHealth.org can be found here: https://www.dukehealth.org/covid-19-update/resources. Duke University maintains a resource page as well, which can be accessed here: https://coronavirus.duke.edu/updates/for-staff.
Upcoming Events & Opportunities
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
May 10 — Duke Hospital, Duke Regional, Duke Raleigh
Newsobserver.com
NC claims top spot for nation’s safest hospitals. See how Triangle hospitals rank
https://duke.is/n7dts
May 10 — Richard Shannon and Beverly Gray
CBS17.com
Duke Health doctors worry about abortion ban impacts
https://duke.is/5pv96
May 12 — Michelle Kelsey
CBS17.com/WNCN
How you brew coffee could impact your cholesterol, research shows
https://duke.is/bjdvy
Division of Cardiology Publications Indexed in PubMed April 28 – May 11, 2022
Ahmed F, Abid M, Maniya T, Usman MS, Fudim M.Incidence and prognosis of COVID-19 amongst heart transplant recipients: a systematic review and meta-analysis. Eur J Prev Cardiol 2022;29(6):e224-e226. PM: 34757386.
Alenezi F, Covington TA, Mukherjee M, Mathai SC, Yu PB, Rajagopal S. Novel Approaches to Imaging the Pulmonary Vasculature and Right Heart. Circ Res 2022;130(9):1445-1465. PM: 35482838.
Anand SS, Hiatt W, Dyal L, Bauersachs R, Berkowitz SD, Branch KRH, Debus S, Fox KAA, Liang Y, Muehlhofer E, Nehler M, Haskell LP, Patel M, Szarek M, Yusuf S, Eikelboom J, Bonaca MP. Low-dose rivaroxaban and aspirin among patients with peripheral artery disease: a meta-analysis of the COMPASS and VOYAGER trials. Eur J Prev Cardiol 2022;29(5):e181-e189. PM: 34463737.
Andonian BJ, Koss A, Koves TR, Hauser ER, Hubal MJ, Pober DM, Lord JM, MacIver NJ, St Clair EW, Muoio DM, Kraus WE, Bartlett DB, Huffman KM. Rheumatoid arthritis T cell and muscle oxidative metabolism associate with exercise-induced changes in cardiorespiratory fitness. Sci Rep 2022;12(1):7450. PM: 35523821.
Assimon MM, Pun PH, Al-Khatib SM, Brookhart MA, Gaynes BN, Winkelmayer WC, Flythe JE. Proton pump inhibitors may enhance the risk of citalopram- and escitalopram-associated sudden cardiac death among patients receiving hemodialysis. Pharmacoepidemiol Drug Saf 2022;31(6):670-679. PM: 35285107.
Bachour K, Dodge SE, Kearing S, Douglas PS, Wong S, Coylewright M. Predicting When Women Will Achieve Equitable Representation in Four Specialties: The WHEN Study. Am J Med 2022;135(5):650-653. PM: 35134367.
Baggish AL, Chang CJ, Drezner JA, Harmon KG, Kraus WE, Matuszak J, Wasfy MM. ACSM-AMSSM Call to Action: Adapting Preparticipation Cardiovascular Screening to the COVID-19 Pandemic. Curr Sports Med Rep 2022;21(5):159-162. PM: 35522440.
Bernstein E, Wang TY. Point-of-Care Ultrasonography: Clearly More Than a Pretty Picture-Reply. JAMA Intern Med 2022;182(5):568. PM: 35285852.
Blankstein R, Shaw LJ, Gulati M, Atalay MK, Bax J, Calnon DA, Dyke CK, Ferencik M, Heitner JF, Henry TD, Hung J, Knuuti J, Lindner JR, Phillips LM, Raman SV, Rao SV, Rybicki FJ, Saraste A, Stainback RF, Thompson RC, Williamson E, Nieman K, Tremmel JA, et al. Implications of the 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Chest Pain Guideline for Cardiovascular Imaging: A Multisociety Viewpoint. JACC Cardiovasc Imaging 2022;15(5):912-926. PM: 35512960.
De Caterina R, Patti G, Westerbergh J, Horowitz J, Ezekowitz JA, Lewis BS, Lopes RD, McMurray JJV, Atar D, Bahit MC, Keltai M, López-Sendón JL, Ruzyllo W, Granger CB, Alexander JH, Wallentin L. Heterogeneity of diabetes as a risk factor for major adverse cardiovascular events in anticoagulated patients with atrial fibrillation: an analysis of the ARISTOTLE trial. Eur Heart J Cardiovasc Pharmacother 2022;8(3):227-235. PM: 33367487.
Frankel DS, Dechert-Crooks BE, Campbell K, DeSimone CV, Etheridge S, Harvey M, Lampert R, Nayak HM, Saliba WI, Shea J, Thomas J, Zado E, Daubert JP. 2021 HRS Educational Framework for Clinical Cardiac Electrophysiology. Heart Rhythm O2 2022 Apr 15;3(2):120-132. PM: 35496459.
Freeman JV, Higgins AY, Wang Y, Du C, Friedman DJ, Daimee UA, Minges KE, Pereira L, Goldsweig AM, Price MJ, Reddy VY, Gibson D, Doshi SK, Varosy PD, Masoudi FA, Curtis JP. Antithrombotic Therapy After Left Atrial Appendage Occlusion in Patients With Atrial Fibrillation. J Am Coll Cardiol 2022;79(18):1785-1798. PM: 35512858.
Friedman DJ, Du C, Wang Y, Agarwal V, Varosy PD, Masoudi FA, Holmes DR, Reddy VY, Price MJ, Curtis JP, Freeman JV. Patient-Level Analysis of Watchman Left Atrial Appendage Occlusion in Practice Versus Clinical Trials. JACC Cardiovasc Interv 2022;15(9):950-961. PM: 35512918.
Fudim M, Kaye DM, Borlaug BA, Shah SJ, Rich S, Kapur NK, Costanzo MR, Brener MI, Sunagawa K, Burkhoff D. Venous Tone and Stressed Blood Volume in Heart Failure: JACC Review Topic of the Week. J Am Coll Cardiol 2022;79(18):1858-1869. PM: 35512865.
Goldberg LR, Jorbenadze A, Shaburishvilli T, Mirro MJ, Fudim M, Zuber M, Stämpfli SF, Tanner FC, Erne P, Cleland JG. Synchronized diaphragmatic stimulation: a case report of a novel extra-cardiac intervention for chronic heart failure. ESC Heart Fail 2022;9(3):1677-1681. PM: 35297198.
Harskamp RE, Lucassen WAM, Lopes RD, Himmelreich JCL, Parati G, Weert HCPMV. Risk of stroke and bleeding in relation to hypertension in anticoagulated patients with atrial fibrillation: a meta-analysis of randomised controlled trials. Acta Cardiol 2022;77(3):191-195. PM: 33685380.
Jain V, Minhas AMK, Khan SU, Greene SJ, Pandey A, Van Spall HGC, Fonarow GC, Mentz RJ, Butler J, Khan MS. Trends in HF Hospitalizations Among Young Adults in the United States From 2004 to 2018. JACC Heart Fail 2022;10(5):350-362. PM: 35483798.
Jimenez Contreras F, Mendiola Pla M, Schroder J, Bryner B, Agarwal R, Russell SD, Mirza J, Daneshmand MA, Milano C. Progression of aortic valve insufficiency during centrifugal versus axial flow left ventricular assist device support. Eur J Cardiothorac Surg 2022;61(5):1188-1196. PM: 35167677.
Kelsey MD, Nelson AJ, Green JB, Granger CB, Peterson ED, McGuire DK, Pagidipati NJ. Guidelines for Cardiovascular Risk Reduction in Patients With Type 2 Diabetes: JACC Guideline Comparison. J Am Coll Cardiol 2022;79(18):1849-1857. PM: 35512864.
Malenka DJ, Bhatt DL, Bradley SM, Shahian DM, Draoui J, Segawa CA, Koutras C, Abbott JD, Blankenship JC, Vincent R, Windle J, Tsai TT, Curtis J, Roe M, Masoudi FA. The National Cardiovascular Data Registry Data Quality Program 2020: JACC State-of-the-Art Review. J Am Coll Cardiol 2022;79(17):1704-1712. PM: 35483759.
Manichaikul A, Lin H, Kang C, Yang C, Rich SS, Taylor KD, Guo X, Rotter JI, Craig Johnson W, Cornell E, Tracy RP, Peter Durda J, Liu Y, Vasan RS, Adrienne Cupples L, Gerszten RE, Clish CB, Jain D, Conomos MP, Blackwell T, Papanicolaou GJ, Rodriguez A. Lymphocyte activation gene-3-associated protein networks are associated with HDL-cholesterol and mortality in the Trans-omics for Precision Medicine program. Commun Biol 2022;5(1):362. PM: 35501457.
Muiruri C, Corneli A, Cooper L, Dombeck C, Gray S, Longenecker CT, Meissner EG, Okeke NL, Pettit AC, Swezey T, Vicini J, Bloomfield GS. Perspectives of HIV specialists and cardiologists on the specialty referral process for people living with HIV: a qualitative descriptive study. BMC Health Serv Res 2022;22(1):623. PM: 35534889.
Narcisse DI, Katzenberger DR, Gutierrez JA. Contemporary Medical Therapies for Patients with Peripheral Artery Disease and Concomitant Type 2 Diabetes Mellitus: a Review of Current Evidence. Curr Cardiol Rep 2022;24(5):567-576. PM: 35201560.
Nelson AJ, Haynes K, Shambhu S, Eapen Z, Cziraky MJ, Nanna MG, Calvert SB, Gallagher K, Pagidipati NJ, Granger CB . High-Intensity Statin Use Among Patients With Atherosclerosis in the U.S. J Am Coll Cardiol 2022;79(18):1802-1813. PM: 35512860.
Piccini JP, Arps K. Sacubitril/Valsartan Therapy for AF and HFpEF: Is the Glass Half Empty or Half Full? JACC Heart Fail 2022;10(5):347-349. PM: 35483797.
Roselli C, Yu M, Nauffal V, Georges A, Yang Q, Love K, Weng LC, Delling FN, Maurya SR, Schrölkamp M, Tfelt-Hansen J, Hagège A, Jeunemaitre X, Debette S, Amouyel P, Guan W, Muehlschlegel JD, Body SC, Shah S, Samad Z, Kyryachenko S, Haynes C, Rienstra M, et al. Genome-wide association study reveals novel genetic loci: a new polygenic risk score for mitral valve prolapse. Eur Heart J 2022;43(17):1668-1680. PM: 35245370.
Rymer JA, Gutierrez JA. Challenges in Peripheral Artery Disease Clinical Trial Implementation and Design. Can J Cardiol 2022;38(5):699-702. PM: 35074414.
Salah HM, Levin AP, Fudim M. Updates from the American Heart Association Scientific Sessions: cardiovascular pharmacotherapy. Eur Heart J Cardiovasc Pharmacother 2022;8(3):E4-E6. PM: 34864960.
Selvaraj S, Margulies KB, Dugyala S, Schubert E, Tierney A, Arany Z, Pryma DA, Shah SH, Rame JE, Kelly DP, Bravo PE. Comparison of Exogenous Ketone Administration Versus Dietary Carbohydrate Restriction on Myocardial Glucose Suppression: A Crossover Clinical Trial. J Nucl Med 2022;63(5):770-776. PM: 34675108.
Sidhu MS, Alexander KP, Huang Z, O’Brien SM, Chaitman BR, Stone GW, Newman JD, Boden WE, Maggioni AP, Steg PG, Ferguson TB, Demkow M, Peteiro J, Wander GS, Phaneuf DC, De Belder MA, Doerr R, Alexanderson-Rosas E, Polanczyk CA, Henriksen PA, Conway DSG, et al. Causes of cardiovascular and noncardiovascular death in the ISCHEMIA trial. Am Heart J 2022;248:72-83. PM: 35149037.
Smith PJ, Sherwood A, Hinderliter AL, Mabe S, Tyson C, Avorgbedor F, Watkins LL, Lin PH, Kraus WE, Blumenthal JA. Cerebrovascular Function, Vascular Risk, and Lifestyle Patterns in Resistant Hypertension. J Alzheimers Dis 2022;87(1):345-357. PM: 35275539.
Spertus JA, Mack MJ, Ohman EM. Improving the National Cardiovascular Data Registry’s Value to Elevate the Quality of Cardiovascular Care. J Am Coll Cardiol 2022;79(17):1713-1716. PM: 35483760.
Spitzer E, Fanaroff AC, Gibson CM, Seltzer J, McFadden E, Ali M, Wilson M, Menon V, Mehran R, Held C, Mahaffey KW, Lopes RD. Independence of clinical events committees: A consensus statement from clinical research organizations. Am Heart J 2022;248:120-129. PM: 35296411.
Tanaka A, Hebert AM, Smith-Washington A, Hoffstaetter T, Goldenberg R, Vemulapalli S, Del Río-Solá L, Arnaoutakis GJ, Mussa F, Ota T. Knowledge gaps in surgical management for aortic dissection. Semin Vasc Surg 2022;35(1):35-42. PM: 35501039.
Verma S, Rathwell S, Fremes S, Zheng Y, Mehta R, Lopes RD, Alexander JH, Goodman SG, Diepen SV. Associated factors and clinical outcomes in mechanical circulatory support use in patients undergoing high risk on-pump cardiac surgery: Insights from the LEVO-CTS trial. Am Heart J 2022;248:35-41. PM: 35263653.
Wang A, Fosbøl EL. Current recommendations and uncertainties for surgical treatment of infective endocarditis: a comparison of American and European cardiovascular guidelines. Eur Heart J 2022;43(17):1617-1625. PM: 35029274.
Wegermann ZK, Mack MJ, Arnold SV, Thompson CA, Ryan M, Gunnarsson C, Strong S, Cohen DJ, Alexander KP, Brennan JM. Anxiety and Depression Following Aortic Valve Replacement. J Am Heart Assoc 2022;11(9):e024377. PM: 35470691.
Wilson BS, Tucci DL, Moses DA, Chang EF, Young NM, Zeng FG, Lesica NA, Bur AM, Kavookjian H, Mussatto C, Penn J, Goodwin S, Kraft S, Wang G, Cohen JM, Ginsburg GS, Dawson G, Francis HW. Harnessing the Power of Artificial Intelligence in Otolaryngology and the Communication Sciences. J Assoc Res Otolaryngol 2022;23(3):319-349. PM: 35441936.
Duke Heart Pulse – Week Ending May 8th 2022 – Mother’s Day
Chief’s message:
Mother’s Day and appreciating the Moms in our Lives!
Mother’s Day around Duke and UNC is also noted for college, medical school, and post-graduate degree graduations. It is a good tradition allowing family’s to relish an important milestone and provide the opportunity to consider the influence mothers have on our lives.We hope that you all got to spend some time with the ones you love appreciate all the moms out in the Duke Heart community and the lessons of love, kindness, and selfless devotion they have on us all. Mothers come in many iterations – to those we are blessed to have among us, and those who have passed before us — we hope this has been a wonderful weekend for all!
Highlights of the Week.
Harrington gives Medicine Grand Rounds as Joseph C. Greenfield Visiting Professor
We welcomed Robert Harrington, chair of the Department of Medicine at Stanford, back to campus this week as the Joseph C. Greenfield Visiting Professor. His lecture, Cardiovascular Medicine as a Data Science was presented during Medicine Grand Rounds on Friday. It was great to see so many residents, faculty and fellows that could attend. Bob Harrington was able to provide an amazing over-arching view of not only how medicine has become a data science field, but more importantly providing many examples of how clinicians and data scientists are interacting to do clinical research, engage patients, and deliver care. It was a fun to have Bob revisit the cath lab, the clinical wards, work with our residents and fellows to discuss how we can continue to improve medicine. The innovation on getting data science and information at the point of care at Stanford Medicine was quite impressive.

Nafissi Grand Rounds Presentations
Navid Nafissi gave an excellent presentation this week during Cardiology Grand Rounds on Tuesday evening. His topic was “Precision Medicine in Arrhythmias: Not Your Daddy’s Long QT”. In keeping with the data science theme – Navid highlighted how our understanding of arrhythmias and the genetic and clinical correlates is exploding requiring a broad set of skills for clinicians in this area.
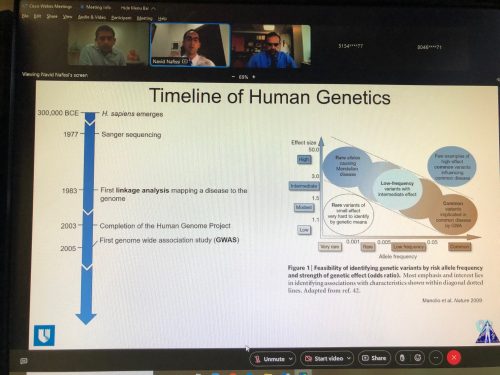
Nurses Week 2022
It’s Nurses Week, 2022 (May 6-12)! On behalf of Duke Heart, we would like to recognize each of our nurses for their professiona l accomplishments and contributions in caring for Duke Heart patients over the past year. This year continues to be challenging with the ongoing COVID pandemic and more patients than ever in need of the highly specialized care that only the Duke Heart team can provide.
l accomplishments and contributions in caring for Duke Heart patients over the past year. This year continues to be challenging with the ongoing COVID pandemic and more patients than ever in need of the highly specialized care that only the Duke Heart team can provide.
Duke Heart Nurses are foundational to Duke’s ability to provide best-in-class heart care. Each of our nurses have been a part of many firsts in the U.S. and at Duke. These firsts include caring for patients and partnering with our cardiology and cardiac surgery providers in landmark clinical trials including the TransMedics DCD trials and the implant of the first-in-U.S. Carmat total artificial heart last summer. At Duke University Hospital, Duke Heart Nurses supported bed and tower expansion, growth of CICU and cardiology beds and grew the emergency response teams including the addition of a Behavioral Response team. Our outpatient teams continued to support our patients and families using new technologies and approaches, including enhanced telehealth and mobile cardiac rehabilitation. None of these accomplishments would be possible without the amazing care across our outpatient, rehabilitation, procedural, and diagnostic teams and the inpatient cardiology and surgical units.
In the midst of a busy clinical year, each of them continued to show tremendous compassion for not only Duke patients and families but also each other and our community. The Duke Heart Nursing team possesses unmatched talent, dedication and teamwork that exemplifies living the Duke Values.
Kudos and Thank you!
Celebrating Perfusionists!
 Our Duke Perfusion team, one of the largest in the country, has a scope of practice inclusive of cardiopulmonary bypass, extracorporeal support, mechanical circulatory support, and autotransfusion for adult and pediatric patients. Areas of expertise include major aortic surgery, advanced heart failure, heart and lung transplantation, minimally invasive and robotic surgery, blood conservation, surgical oncology, and complex congenital surgery. Our team has been involved in multiple groundbreaking innovations including Transmedics OCS heart procurements, cutting-edge mechanical support and laboratory research. Duke perfusionists are nationally recognized leaders in the field and serve as clinical instructors for four perfusion schools.
Our Duke Perfusion team, one of the largest in the country, has a scope of practice inclusive of cardiopulmonary bypass, extracorporeal support, mechanical circulatory support, and autotransfusion for adult and pediatric patients. Areas of expertise include major aortic surgery, advanced heart failure, heart and lung transplantation, minimally invasive and robotic surgery, blood conservation, surgical oncology, and complex congenital surgery. Our team has been involved in multiple groundbreaking innovations including Transmedics OCS heart procurements, cutting-edge mechanical support and laboratory research. Duke perfusionists are nationally recognized leaders in the field and serve as clinical instructors for four perfusion schools.
The Duke Perfusion team is devoted to our community and engages in multiple outreach and service initiatives each year. To celebrate Perfusion Week (May 1-7), the team volunteered with Habitat Build.
An outstanding group in any year, this team has put in an incredible effort during the pandemic and we are extremely proud of them. Great job!!!

Kudos to Hughes & Burkett
 We received the following note this week via Press Ganey in regard to care provided to a patient by
We received the following note this week via Press Ganey in regard to care provided to a patient by
Chad Hughes and Melissa Burkett:
“I would like to comment on Dr. Hughes first, then his assistant Melissa. I doubt anything I say hasn’t been said before about Dr. Hughes or Melissa, but perhaps substantiates comments made by others. I found both of these professionals to be world class. Dr. Hughes reminds me of a military special operator or fighter pilot I have met and worked with in my career. I know the personality well. Dr. Hughes is laser focused, precise, and highly motivated. He’s EXACTLY what you would want in a surgeon. The bonus is he puts you at ease immediately. Perhaps it’s his demeanor or level of confidence, but make no mistake you know when talking with him he knows his craft very well. He’s obviously highly trained and skilled. I would venture to guess if medicine had not called him, he would have been a Green Beret, Navy SEAL, or fighter pilot. And if you were going into an operation, you would want him on your TEAM. He’s on point, and will get the job done better than probably 99.9% of surgeons in the world (that’s my after-action report). Generally, you cannot help but like the guy. And his assistant, Melissa, who must work a crazy schedule, always manages to follow up with every question or concern you may have. I am not sure what anyone would expect or want in a medical care TEAM. Perhaps Dr. Hughes and Melissa are the special forces of Duke Medical.” — A grateful patient, name withheld for confidentiality
“THANK YOU for the great things you are doing for our patients every day!” — Jamie Hilton, Nurse Manager, Operations
Well done, Chad & Melissa!

ACC Leadership Academy Held
The ACC Emerging Faculty Leadership Academy was held May 1-3 at Heart House in Washington, DC. Four invited participants had ties to Duke Heart. Here they are together, shown L-R are: Tony Gutierrez, Lauren Cooper, cardiology fellow from 2012-2016; Kristen Campbell, clinical pharmacist with Duke EP, and Kelly Schlendorf, advanced heart failure fellow, 2011 – 2012. Congrats to all of you and a hat tip to Kristen Campbell for the photo!

Tannu Recognized by ASE Foundation
 We are pleased to share that Manasi Tannu, a first-year cardiology fellow, has been recognized by the ASE Foundation with a Top Investigator Travel Grant.
We are pleased to share that Manasi Tannu, a first-year cardiology fellow, has been recognized by the ASE Foundation with a Top Investigator Travel Grant.
We received a message from Fawaz Alenezi this week that read, “Our Duke echo lab abstracts that are led by our phenomenal fellow Manasi Tannu have been recognized as the ASE Foundation Top Investigators and will receive $1000 to support travel to attend the ASE meeting. The selected abstracts are:
- Echocardiography based estimation of pulmonary vascular resistance and outcomes in patients with pulmonary hypertension.
- Prognostic value of right ventricular-pulmonary artery coupling in patients with pulmonary hypertension.
The ASE Foundation is the philanthropic arm of the American Society of Echocardiography. Each year, the ASE Foundation works with the ASE Scientific Sessions Abstract Chairs to identify meritorious early career abstract presenters. The selected presenters are recognized as the ASE Foundation Top Investigators and each receives a travel grant in the amount of $1,000 (U.S. currency) to support their travel to attend the ASE meeting and present their accepted abstract(s).
In the announcement letter to Tannu, Andrea M. Van Hoever, Deputy Director of the ASE Foundation wrote, “Young investigators such as yourself are the scientific heart and future of ASE’s annual meeting. We are honored to be able to support your attendance and look forward to seeing you in Seattle.”
Way to go, Manasi!
COVID-19 Update
All the latest Clinical Operations updates related to COVID can be found at https://covid-19.dukehealth.org. Patient-facing resources on DukeHealth.org can be found here: https://www.dukehealth.org/covid-19-update/resources. Duke University maintains a resource page as well, which can be accessed here: https://coronavirus.duke.edu/updates/for-staff.
Upcoming Events & Opportunities
Cardiology Grand Rounds
May 10: Coronary CTOs and Cardiac MRI: The Duke Experience with Caitlin Dresher. 5 p.m., Webex.
May 12: Mind the Gaps: Novel Strategies for Care Delivery and Phenotyping Across the Spectrum of Heart Failure with Vishal Rao. 5 p.m., Webex link coming soon.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
April 28 — Manesh Patel
Healio/Cardiology
Asundexian confers lower bleeding rates vs. apixaban for stroke prevention in AF
https://duke.is/wjqbn
April 29 — Manesh Patel
HCP Live
Overview of Polyvascular Disease and Coronary Artery Disease
https://duke.is/pu7nq
April 29 — Jonathan Piccini
Cardiac Rhythm News
New data from STROKE AF trial shared at HRS 2022
https://duke.is/r8t5u
May 1 — Jonathan Piccini
Cardiovascular Business
STROKE AF study shows insertable cardiac monitors detect 4 times more AFib than Holter monitoring
https://duke.is/6tmma
May 1 — James Daubert
MedpageToday
Menstrual Cycles Point to Link Between Sex Hormones and Long QT
https://duke.is/5yp7j
May 1 — Joseph Turek
WCBS-NY (Radio)
Breakthrough could mean end of anti-rejection drugs for transplant patients
https://duke.is/nhtkd
May 2 — Sana Al-Khatib
Medscape
Apple Watch ECG App, Still Experimental, Reveals Asymptomatic Low LVEF
https://duke.is/cnyvt
May 3 — Daniel Friedman
tctMD
NCDR Analyses Offer Insights Into First-Generation Watchman Outcomes
https://duke.is/yqt4m
May 5 — Sana Al-Khatib
Healio
Apple Watch app, using AI, identifies left ventricular dysfunction
https://duke.is/pfkp6
May 5 — Sana Al-Khatib
Medscape (en español)
https://duke.is/rg6xf
Duke Heart Pulse – week ending May 1st 2022
Chief’s message:
Hope everyone had a good week and some time for rest. This was a busy week for Duke Heart with the Heart Rhythm Society (HRS) national meeting with several faculty and fellow presentations, the International Society for Heart & Lung Transplantation (ISHLT) 42nd Annual Meeting and Scientific Sessions in Boston with several important presentations from our Duke Heart Faculty and fellows including several clinical practice changing studies, the first in-person Heart Center Leadership Council meeting to review our progress in three years, and the Duke ACTIV-3 clinical research team, led by our own Peter K. Smith, MD — the team was presented with a Duke University Presidential Award. This all happened while we kept working hard to provide our patients the best opportunity for heart care – something that was again evident this weekend on the wards and in the cath lab. Our Heart Center Leadership council Chair – Bob Keegan wanted to make sure that on behalf of the Heart Center Leadership council we include a tremendous thanks to all employees across Duke Heart on their behalf of the council in this weekend’s issue of Pulse. Appreciate the support Bob!
Hopefully as we approach the end of the academic year we will have an opportunity to celebrate our fellows, faculty and staff at some of our end of year events.
Highlights of the week:
ACTIV-3, Global Efforts, Transplant Nurses & Perfusion Week
We have so much to celebrate! First, happy May Day, traditionally the halfway point between the spring equinox and the summer solstice, according to the Farmer’s Almanac. With spring well underway here in NC, today also kicks off Perfusion Week 2022, May 1-7, so be sure to thank our amazing perfusionists when you see them!
Several cardiologists and their global efforts were featured in a new Magnify article out this week; our ACTIV-3 team received the prized Duke University Presidential Award (see below), we wrapped up Patient Experience Week (April 25-29), National Donate Life month (April) and Transplant Nurses Week runs through tomorrow, May 2. Duke is blessed with one of the best transplant teams in the world, and our nurses are a big part of that! We especially thank the nurses supporting our lung and heart transplant surgical teams and all those caring for our transplant patients pre- and post-surgery. We could not do this without you!
Speaking of transplant teams…
Duke Heart Shines at ISHLT 2022
The International Society for Heart & Lung Transplantation (ISHLT) 42nd Annual Meeting and Scientific Sessions were held April 27-30 in Boston.
ICYMI, the U.S. Food and Drug Administration this week granted premarket approval to TransMedics for its OCS Heart System for use with organs from donors after circulatory death (DCD). The TransMedics OCS Heart System is now approved with the extended clinical indication for ex vivo reanimation, functional monitoring, and beating-heart preservation of DCD hearts. This indication is based on the results of the OCS DCD Heart Trial and the associated Continued Access Protocol (EXPAND trial) which were presented by Jacob Schroder, MD, on Friday, April 29 at ISHLT.

“The FDA’s approval of the OCS for DCD donor hearts is the natural progression from the prior approval of the device for extended criteria brain dead donors, supported by the excellent results from the U.S. DCD trial,” said Schroder, surgical director of heart transplantation at Duke University Health System and the principal investigator for the OCS DCD Heart Trial. “The use of OCS is actively expanding the donor pool, as I expected. It is time we stop considering heart transplant as a severely supply limited resource. With OCS we will be able to expand access to this life saving therapy to more end-stage heart failure patients.”
Schroder presented clinical trial results on Friday morning. The multicenter, randomized, U.S. Donation after Circulatory Death (DCD) trial utilized direct procurement and perfusion (DPP) with the Organ Care System (OCS). In this trial, patients awaiting heart transplantation were randomized in a three to one manner to a donation after circulatory death (DCD) eligible arm versus donation after brain death (DBD) only. Inclusion and exclusion criteria were pre-established both with regards to the recipient and donor characteristics but also with regards to the DCD management; for example, a functional warm ischemia time less than 30 minutes was defined and served as part of the trial protocol. This resulted in comparison of 80 DCD transplants versus 86 DBD cases, which were treated as randomized and per protocol. The DCD transplant cohort displayed significantly younger donor and recipient age. Furthermore, duration of wait list time was less for the DCD cohort. The primary effectiveness endpoint was patient survival at 6 months and did not differ between the two groups (95% DCD versus 89% DBD). Overall patient and graft survival at 2 years was significantly better in the DCD cohort (93%) versus the DBD control (83%). The incidence of moderate or severe LV or RV PGD was greater for the DCD group (22.5%) versus the DBD (9.5%).
This U.S. DCD trial was the first of its kind in that a randomized control group, deemed as DCD ineligible, was utilized and there were predetermined inclusion and exclusion criteria. The team concludes that despite higher rates of primary graft dysfunction, heart transplantation with DCD achieves intermediate survival outcomes equivalent to those achieved with DBD. Of note: Duke was the first and leading enroller in the trial.
In a note from Schroder to members of leadership this weekend, he reflected on the work:
“I am heading back from ISHLT in Boston after presenting the 2-year EXPAND heart and US DCD trials yesterday. Both ground breaking trials with results that have moved the needle in heart transplant. The DCD trial is probably the most meaningful thing to happen in heart transplant in the U.S. in many decades.
Now we, and anyone who is even remotely familiar with either trial, knows THAT THESE WERE REALLY DUKE TRIALS. We, as a team, made this happen out of sheer collective willpower.
Each and every team member should feel really great about this. Not only about the patients we helped along the way. But the countless more that will be helped in the future from our hard work.
I thank you all from the bottom of my heart for your efforts to continue to get the absolute best for Duke patients. And a special thanks to Sarah Casalinova who, for 6 years, has been the cornerstone to everything we have done with OCS.”
These results – the clinical trial findings, the FDA approval, the ISHLT presentations, and lives saved — stem from an incredible effort put forth over many years by members of this team. Their commitment to advanced heart failure patients with extremely limited options as well as their dedication to one another is truly inspiring. Congratulations!
And there is even more to celebrate from ISHLT:
 Duke Cardiology fellow Lauren Truby gave an excellent oral scientific presentation on “Proteomic profiling of cold storage preservation solution to identify signatures of primary graft dysfunction following heart transplantation.” This work helped to identify a set of novel biomarkers associated with primary graft dysfunction following heart transplantation; she also gave an excellent talk entitled, “Bridge to transplant with durable left ventricular assist device is associated with primary graft dysfunction: a report from the International Consortium on Primary Graft Dysfunction” and gave an invited presentation entitled “The rise of the machines: PGD risk scoring systems in the MCS bridge-to-transplant populations.” In summary: her work is helping to identify important clinical and biochemical risk factors for the development of primary graft dysfunction after heart transplantation.
Duke Cardiology fellow Lauren Truby gave an excellent oral scientific presentation on “Proteomic profiling of cold storage preservation solution to identify signatures of primary graft dysfunction following heart transplantation.” This work helped to identify a set of novel biomarkers associated with primary graft dysfunction following heart transplantation; she also gave an excellent talk entitled, “Bridge to transplant with durable left ventricular assist device is associated with primary graft dysfunction: a report from the International Consortium on Primary Graft Dysfunction” and gave an invited presentation entitled “The rise of the machines: PGD risk scoring systems in the MCS bridge-to-transplant populations.” In summary: her work is helping to identify important clinical and biochemical risk factors for the development of primary graft dysfunction after heart transplantation.
Way to go, Lauren!
 Duke cardiology fellow Vanessa Blumer was the only fellow invited to participate in and present during the first-ever, multi-national, ISHLT-endorsed Shock Consensus Conference. The focus was on identifying key areas of consensus for the care of patients with non-ischemic cardiogenic shock. She was asked to present a talk entitled, “How to proceed? Tools to quantify non-AMI cardiogenic shock severity and establish goals for treatment.”
Duke cardiology fellow Vanessa Blumer was the only fellow invited to participate in and present during the first-ever, multi-national, ISHLT-endorsed Shock Consensus Conference. The focus was on identifying key areas of consensus for the care of patients with non-ischemic cardiogenic shock. She was asked to present a talk entitled, “How to proceed? Tools to quantify non-AMI cardiogenic shock severity and establish goals for treatment.”
In summary: her contribution will hopefully lead to several consensus documents helping to identify priority areas for investigation focusing on the care of patients with cardiogenic shock unrelated to acute myocardial infarction.
ICYMI, Vanessa is co-author on a new perspectives piece Women Empowering Women in Heart Transplantation and Mechanical Circulatory Support that appears online (article in-press) in the Journal of Cardiac Failure.
Nicely done, Vanessa!
Chet Patel chaired a session entitled “Will you be mine? Choosing donors and recipients for heart transplantation” – Way to represent Duke Heart, Chet!
 Integrated thoracic surgery resident Julie Doberne presented on heart transplant in HIV-positive recipients and compared results with other solid organ transplants in same population. In a post to Twitter she credited Chet Patel and Carmelo Milano for being instrumental in the research and stated that HIV is no longer a death sentence.
Integrated thoracic surgery resident Julie Doberne presented on heart transplant in HIV-positive recipients and compared results with other solid organ transplants in same population. In a post to Twitter she credited Chet Patel and Carmelo Milano for being instrumental in the research and stated that HIV is no longer a death sentence.
Great work, Julie!
Comments from team members related to work presented at ISHLT include:
- “I’m extremely proud of all team member efforts leading the care of patients with cardiogenic shock, mechanical circulatory support, and heart transplantation.” – Jason Katz, Duke’s Director of Cardiovascular Critical Care; Co-Director, Duke Mechanical Circulatory Support Program, and Co-Director, Duke Cardiac Intensive Care Unit
- “Every day I am so thankful to have trained in HF at Duke but I’m especially proud today” – Amanda Coniglio via Twitter regarding Schroder presentations.
- “This is what it’s all about. JNS and our surgical team are the most fantastic surgeons out there-tireless, brilliant, committed, bringing real change to the field.” — Richa Agarwal via Twitter during Schroder presentations.
Heart Rhythm Society 2022, San Francisco
On the west coast this weekend, many of our Duke Heart faculty and fellows are attending and presenting during the Heart Rhythm Society 2022 annual meeting (April 29-May 1) in San Francisco.
 Earlier today, Jon Piccini presented 4-fold Higher Rate Of Atrial Fibrillation Detection After Stroke Of Presumed Known Etiology With Continuous Versus Intermittent Monitoring: Results From The Stroke AF Study:
Earlier today, Jon Piccini presented 4-fold Higher Rate Of Atrial Fibrillation Detection After Stroke Of Presumed Known Etiology With Continuous Versus Intermittent Monitoring: Results From The Stroke AF Study:
Despite progress in the prevention of stroke, it remains the fifth most common cause of death in the U.S. Atrial fibrillation increases the risk of stroke five-fold and is a common cause of stroke, especially in older individuals. Stroke often leads to permanent disability or death and identifying the cause of a stroke is an important step in preventing future or recurrent stroke.
Prior work has shown that between 20 and 30% of patients with stroke of undetermined cause (often referred to as cryptogenic stroke) have atrial fibrillation. Thus, patients with stroke of undetermined cause often undergo intensified heart rhythm monitoring in order to diagnose (and treat) atrial fibrillation as a potential cause of stroke. However, a recent analysis from the STROKE AF study suggests that looking for atrial fibrillation may be very important in patients whose stroke was not caused by atrial fibrillation and how we look for atrial fibrillation has important implications for providers and patients.
The STROKE AF study compared heart rhythm monitoring with an implantable cardiac monitor (ICM) versus standard approaches to intermittent heart rhythm monitoring in patients with stroke attributed to large artery atherosclerosis or small vessel occlusion. In patients whose stroke did not appear to be due to an abnormal heart rhythm, the study found that 1 in 8 patients had atrial fibrillation detected by an ICM by 12 months.
At today’s Heart Rhythm Society annual meeting, Piccini and colleagues reported on an additional analysis of the STROKE AF data.
In their analysis, they examined how the type of heart rhythm monitoring may impact the ability of monitoring to identify atrial fibrillation in these patients. As one might expect, they said, when comparing continuous monitoring with an ICM versus intermittent heart rhythm monitoring, continuous monitoring identified more instances of atrial fibrillation. However, and perhaps more importantly, even the most aggressive intermittent monitoring strategy would have missed 77% of patients with episodes of atrial fibrillation lasting an hour or more.
According to Piccini and team, these findings are important because after someone experiences a stroke, an important goal of care is to avoid another episode of stroke, no matter what caused the first. Individuals who have atrial fibrillation and a history of stroke have a Class I guideline recommendation for oral anticoagulation to prevent future stroke. The results from the STROKE AF investigators suggests that even with the most aggressive forms of intermittent monitoring, a large proportion of patients with atrial fibrillation would not be diagnosed and may go untreated.
“Traditionally, we have focused our efforts with AF screening in persons who had no clear cause of their stroke,” Dr. Jonathan Piccini, director of cardiac electrophysiology at Duke emphasized. “STROKE AF highlights the importance of diagnosing atrial fibrillation even in persons whose stroke appeared to be due to atherosclerosis or small vessel ischemia. Moreover, these data add to the growing evidence that highlight the importance of continuous cardiac monitoring in some patients who are at-risk for atrial fibrillation, regardless of what may have caused their first stroke.”
Great work, Jon!
Additional presentations during HRS included:
Duke cardiology fellow Kelly Arps presented Use Of Ripple Mapping To Enhance Localization And Ablation Of Outflow Tract  Premature Ventricular Contractions on Friday as well as a poster presentation Temporal Relationship Of Atrial Arrhythmias With The Diagnosis Of Cardiac Sarcoidosis.
Premature Ventricular Contractions on Friday as well as a poster presentation Temporal Relationship Of Atrial Arrhythmias With The Diagnosis Of Cardiac Sarcoidosis.
Jon Piccini presented Bridging the Gap in Guideline-driven Care for CIED Infections – We Must Do Better and Understanding the Clinical Utility of Anti-Tachycardia Pacing.
Marat Fudim presented Barostim: Patient Identification and Real World Experience during a session on Friday and Splanchnic Nerve Block in Heart Failure: Rationale and Clinical Application on Saturday.
Kevin Thomas co-chaired the Saturday session on Disparities or Differences in ICD/CRTD Utilization and earlier today co-chaired a session with Sana Al-Khatib on Racial and Ethnic Disparities in Clinical Electrophysiology.
Al-Khatib also served as a session commentator for Artificial Intelligence To Identify Left Ventricular Dysfunction From An Apple  Watch ECG: A Prospective, Decentralized International Pragmatic Study and presented Clinical Trials: Where does the Evidence Lie for Prevention of Pacing Induced Cardiomyopathy?
Watch ECG: A Prospective, Decentralized International Pragmatic Study and presented Clinical Trials: Where does the Evidence Lie for Prevention of Pacing Induced Cardiomyopathy?
Jim Daubert presented ICDs are No Longer Indicated for Primary Prevention in Patients with Non-ischemic Cardiomyopathy
Sean Pokorney presented Successes and Failures in Rhythm Control: Is it Time for a Hybrid Approach to Cardioversion, Ablation and AADs?
Impressive work by our Duke EP team. Way to go!!
ACTIV-3 Research Team Celebrated with Presidential Award
We are pleased to celebrate the Duke ACTIV-3 clinical research team, led by Peter K. Smith, MD — the team was presented with a Duke University Presidential Award for their continuing efforts in COVID-19 research on Wednesday, April 27 during a ceremony at Page Auditorium.

When Duke decided to halt all unnecessary clinical research activity at the start of the pandemic, Smith, the site PI for the Cardiothoracic Surgery Network (CTSN), recognized that the CTSN could be redirected for COVID-19 clinical trials due to how they were structured as well as their prior experience in the study of stem cells. The NIH quickly selected the CTSN to serve as one of four research platforms for the government’s unified response to COVID-19 – becoming the ACTIV-3 network. By mid-April 2020, Smith had not only gathered experts from throughout Duke Health to serve on the Duke-based ACTIV-3 clinical research team, the team had drafted the first clinical trial protocol using stem cell therapy for COVID-19 ICU patients.
With unprecedented speed and efficiency – the team created new infrastructure and established new systems to conduct COVID-19 research. Team members screened and consented patients 24/7/365, with staff working overtime, putting themselves and their families at potential risk at a time when very little was known about the virus. Multidisciplinary team capabilities were expanded, including pulmonary critical care physicians, infectious disease specialists, residents, and expansion from 4 to 32 clinical research staff dedicated to the project. Data and biospecimens were collected with an efficiency that far surpassed any that had previously been achieved in a clinical trial setting.
After completing the first stem cell study, the team then successfully helped to complete accrual to 5 other monoclonal antibody studies, one of which was recently published in the New England Journal of Medicine. The ACTIV-3 team currently has 2 other studies which are actively enrolling, including studies with new classes of promising therapeutics for the most critically ill patients. Almost 40% of patients enrolled at Duke have been African American, providing proportional representation of those most affected by COVID-19 in our community, which is something the ACTIV-3 team is especially proud of.

“We often don’t do a good job of enrolling the full breadth of our Duke patient population into clinical trials — meaning geographically, racially, ethnically and from a socio-economic standpoint, said Tom Holland, MD, a faculty member in infectious diseases. “The fact that we presented this to everybody, and we were willing to do the kinds of things to go to where patients were for follow up, for labs and visits to make it so that any patient who wanted to enroll, and was able to do so, could. We truly enrolled a population that looks a whole lot like the general population that we’ve taken care of for COVID.”
In 18 months, the ACTIV-3 international network enrolled more than 3000 patients across 139 sites, 422 of which have been accrued from Duke as the leading enrolling site, earning a special commendation from the Director of the NIH.
“This remarkable achievement is a testament to the commitment and dedication of the ACTIV-3 team which has shown single-minded purpose to save the lives of current and future patients most critically affected by the pandemic by enrolling them to clinical trials. We nominate the ACTIV-3 team for their courage and for serving as an inspiring example of what can be achieved through extraordinary teamwork,” states the team’s nomination letter.
“The surgery research group was very generous with their resources, making sure that we had clinical research coordinators and nurses to help get this going,” added Christina Barkauskas, MD, Duke faculty member in Pulmonary and Critical Care Medicine. “From the beginning we had a robust team that was willing to work hard, especially at the beginning of the pandemic when we felt like we had something different, novel and special to offer these patients – we wanted to give them the best chance we could, so we offered it to as many patients as we possibly could.”
nurses to help get this going,” added Christina Barkauskas, MD, Duke faculty member in Pulmonary and Critical Care Medicine. “From the beginning we had a robust team that was willing to work hard, especially at the beginning of the pandemic when we felt like we had something different, novel and special to offer these patients – we wanted to give them the best chance we could, so we offered it to as many patients as we possibly could.”
Speaking to Smith’s leadership of the ACTIV-3 team, Holland and Barkauskas were equally effusive.
“It was really fun to be able to experience his commitment to a project and to a mission and a scientific question — he has pretty remarkable drive,” Barkauskas said. “We knew what we wanted to do, and he would be persistent in finding a way to make it happen, and I think we all appreciated his constant presence to support the team. We screened patients every single day for two years. And getting this award is a nice testament to how hard we worked and how committed we all were. Sometimes it just feels good to get a little bit of recognition, even though we already felt good about what we were doing.”
Holland concurred, “Peter has been our captain and driving force for ACTIV-3 the whole time. He tends to deflect credit for this, but around the clock he was keeping an eye on who was coming into the hospital and who might be eligible for our trials. He was on every one of the calls multiple times a day to review what was going on. We would not have been able to keep up the pace of enrollment or maintain the motivation and vision to keep going as quickly as we did without his passion or his vision.”
Leading and working with the ACTIV-3 team has been refreshing, Smith says. “Seeing the capability of a multidisciplinary team that includes surgeons, experts from infectious disease, critical care, and the hospitalist program come together in this way has been exhilarating. This team created a potent research engine and it broke down a lot of the silos that can prevent certain kinds of research from thriving. I’m optimistic that we can branch out and potentially replicate this for further disease states.”
We are thrilled for the ACTIV-3 team – congratulations to all. The Presidential Award is well-deserved!
HCLC Sends Kudos to Duke Heart Team
The Spring Meeting of the Duke Heart Center Leadership Council (HCLC) took place on Friday, April 29 at the J.B. Duke Hotel & Conference Center in Durham.
The HCLC is led by Bob Keegan, who serves as Chair. The group heard overall highlights and updates from Manesh Patel and Ed Chen, co-directors of Duke Heart. Patel and Chen led a panel discussion, Focus on Discovery Science and Innovation with presentations by Chris Holley, Jennifer Rymer, Sreekanth Vemulapalli and Brittany Zwischenberger. Jill Engel presented an update on the efforts of our nursing and hospital-based teams during the pandemic as well as an update on cardiac nursing research.
The HCLC was truly impressed with the efforts reported on — particularly the care and dedication each and every Duke Heart team member exhibited during the pandemic.
Keegan and the HCLC requested that we specifically include a tremendous thanks to all employees across Duke Heart on their behalf in this weekend’s issue of Pulse. They asked us to send their profuse thanks for the incredible care we gave to patients coming to Duke Heart during the pandemic, for the advances we have been able to make despite the extreme challenges we faced because of the pandemic, the dedication all of us have shown by sticking together and standing by Duke Health, and for the care each of us takes in our respective positions — be they administrative, educational, research-focused, at the bench or at the bedside, they thank all of us for our work.
GREAT JOB, EVERYONE!
Shout-out to Duke Heart Administrative Professionals
A huge shout-out to our Duke Heart Administrative Professionals — they are some of the unsung heroes of healthcare, working behind the scenes to manage schedules, patient inquiries, appointments, paperwork — all “the things” (countless, really) that need doing to keep our faculty, fellows and other staff members organized and productive. Administrative Professionals Day was Wednesday, April 27, but it’s never too late to acknowledge their efforts and celebrate all they do.
Shout out to Holley

Our Ventricular Assist Device team wrote to us this week to recognize Chris Holley, MD, for the great rounding attending experience for their team during Patient Experience Week. Holley, often recognized for his research efforts as part of the Duke Cardiovascular Research Center, demonstrated his clinical excellence this week while leading the VAD clinical team for the LVAD service.
Comments from inpatient and outpatient APPs, fellows, pharmacists, nurses and patients recognize “his thoughtful attention and thorough evaluation of each issue with timely teaching moments for our fellows and other clinicians. His conversations with each patient and clinician on primary, outpatient and consult services represents the wisdom and kindness we hoped to inspire this week. Thanks Dr. Holley!”
Great job, Chris!
Duke Heart Global Efforts Celebrated in Magnify
Three of our terrific Duke Heart faculty members, Gerald Bloomfield, Waseem Akhter and Titus Ng’eno are featured in the current issue of Magnify, the Duke University School of Medicine magazine. The article, ‘A Pandemic in Slow Motion’: Duke Cardiologists Call for a New Approach to Prevent a Looming Global Crisis in Heart Health is a great way to learn more about the important work they are doing to advance access to cardiovascular care across the world. Inspiring!
Chen Featured in STS Podcast
Dr. Edward P. Chen, chief of the division of Cardiovascular and Thoracic Surgery is the featured guest in The Society of Thoracic Surgeons April 28 podcast (#133: Same Surgeon, Different Light: Dr. Ed Chen).
This is well worth a listen. Well done!
In Passing: Marc Caron, PhD, Professor of Cell Biology, Neurobiology and Medicine
We were saddened earlier this week by the passing of our long-time Duke colleague, Marc Caron, PhD, James B. Duke Professor of Cell Biology, Professor of Neurobiology and Professor of Medicine in Cardiology. Dr. Caron, 75, also was a member of the Duke Cancer Institute and Duke Institute for Brain Sciences.
of the Duke Cancer Institute and Duke Institute for Brain Sciences.
In a joint message from Mary Klotman, MD, Dean, Duke School of Medicine and Scott Soderling, PhD, Chair of the department of Cell Biology, they wrote:
An authoritative and prolific scientist, Dr. Caron spent all but two of his 47-year career at Duke. He studied the mechanisms of action and regulation of hormones and neurotransmitters and how they might underlie brain and behavior disorders such as schizophrenia, Parkinson’s disease, attention-deficit hyperactivity disorder, mood disorders and addiction. Among his many achievements, Dr. Caron and his colleagues engineered and characterized a large number of genetically modified mouse models to analyze the foundations of these various brain disorders. In a groundbreaking study, his team identified a novel mode of signaling for the brain’s dopamine D2 receptors, which are principal targets of antipsychotic medications. Dr. Caron also contributed to the discovery of how receptor signaling is regulated by kinases and arrestins, and he defined the molecular signals for their endocytosis and recycling as functional entities. His genetic gain and loss-of-function models provided evidence for the importance of GPCR regulation through kinases and arrestins and identified one of the first in vivo examples of G protein- versus arrestin-mediated GPCR signaling. Dr. Caron mentored many trainees, and followed them through their own careers with encouragement and advice.
Among his many honors, Dr. Caron was an investigator of the Howard Hughes Medical Institute from 1992 to 2004, a member of the American Academy of Arts & Sciences and a fellow of the American Association for the Advancement of Science. In 2005, he received the Julius Axelrod Award from the American Society for Pharmacology and Experimental Therapeutics. Dr. Caron authored more than 650 publications and served as editor or editorial board member of several leading journals including the Journal of Clinical Investigation.
Dr. Caron received his BSc in Chemistry from Laval University and his PhD from the University of Miami. He completed a postdoctoral fellowship at Duke University. He joined the faculty of Laval University School of Medicine as an assistant professor in 1975, and then returned to join Duke’s faculty in 1977.
His funeral mass was held yesterday at Immaculate Conception Catholic Church in Durham. An online obituary can be found here.
Our deep condolences go out to Dr. Caron’s family, friends and his colleagues throughout the world.
COVID-19 Update
All the latest Clinical Operations updates related to COVID can be found at https://covid-19.dukehealth.org. Patient-facing resources on DukeHealth.org can be found here: https://www.dukehealth.org/covid-19-update/resources. Duke University maintains a resource page as well, which can be accessed here: https://coronavirus.duke.edu/updates/for-staff.
Upcoming Events & Opportunities
Cardiology Grand Rounds
May 3: Precision Medicine in Arrhythmias: Not Your Daddy’s Long QT with Navid Nafissi. 5 p.m. Webex.
May 10: Coronary CTOs and Cardiac MRI: The Duke Experience with Caitlin Dresher. 5 p.m., Webex.
MDEpiNet Spring 2022 Virtual Mini-Think Tank
May 5: MDEpiNet Spring 2022 Virtual Mini-Think Tank. Noon – 5:30 p.m., ET
MDEpiNet Predictable And SuStainable Implementation Of National CardioVascular Registries (PASSION CVR) Registry-Supported Prospective Clinical Trials
Join and invite your colleagues to join for updates from, and dialogues across our Registry-supported Prospective Trials Working Groups:
- Data Governance & Access
- Operational Roles & Responsibilities
- Global Regulatory Acceptance
- Use Cases:
- Aortic Intervention
- Heart Valves
- Mechanical Circulatory Support
- Peripheral Arterial Intervention
Registration now open: https://duke.qualtrics.com/jfe/form/SV_2f6JBD6WfaF9jBc.
Evening with Heart Raleigh
An Evening with Heart Raleigh, which has been rescheduled from earlier this year, will benefit Marfan families as well as those with Loeys-Dietz (LDS), Vascular Ehlers-Danlos (VEDS), and related conditions.
May 5, 2022
The Maxwell
7-10 p.m.
Cocktail attire
Tickets for the event include open bar, taco bar, heavy appetizers, dessert, silent auction, DJ, and a fun photo booth. For those unable to attend in person but who would like to participate, the silent auction items can be bid on online from anywhere. Lots of cool items have been donated so far! For tickets, more information or silent auction viewing and bidding, please visit: https://marfan.ejoinme.org/raleigh22.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
April 25 — Stuart Knechtle (transplant surgery)
CBS17.com
NC mom, daughter share organ transplant journey during National Donate Life Month
https://duke.is/m4tqy
April 26 — Gerald Bloomfield
Poz.com
More Cardiac Abnormalities Seen in People Living With HIV
https://duke.is/2byb2
April 27 — Duke University Health System
Becker’s Hospital Review
36 hospitals on Forbes list of best employers for diversity
https://duke.is/gyqpy
April 27 — Joe Turek
CBS News/CBS Mornings
First-of-its-kind heart transplant in infant could possibly prevent organ rejection
https://duke.is/zfek5
April 28 — Manesh Patel
Healio/Cardiology
Asundexian confers lower bleeding rates vs. apixaban for stroke prevention in AF
Division of Cardiology Publications Indexed in PubMed April 21-27, 2022
Ani C, Shavlik D, Knutsen S, Abudayyeh I, Banta J, O’Brien E, Mentz RJ, Bertoni AG, Fraser G. Glycemic status, non-traditional risk and left ventricular structure and function in the Jackson Heart Study. BMC Cardiovasc Disord 2022 Apr 21;22(1):186. PM: 35448969.
Berkowitz SD, Bauersachs RM, Szarek M, Nehler MR, Debus ES, Patel MR, Anand SS, Capell WH, Hess CN, Hsia J, Leeper NJ, Brasil D, Mátyás L, Diaz R, Brodmann M, Muehlhofer E, Haskell LP, Bonaca MP. Prevention of arterial and venous thrombotic events in symptomatic peripheral arterial disease patients after lower extremity revascularization in the VOYAGER PAD trial: Dual anticoagulant/antiplatelet regimen vs antiplatelet therapy alone. J Thromb Haemost 2022 May;20(5):1193-1205. PM: 35170216.
Coniglio AC, Mentz RJ. Sleep Breathing Disorders in Heart Failure. Cardiol Clin 2022 May;40(2):183-189. PM: 35465892.
Cooper-DeHoff RM, Niemi M, Ramsey LB, Luzum JA, Tarkiainen EK, Straka RJ, Gong L, Tuteja S, Wilke RA, Wadelius M, Larson EA, Roden DM, Klein TE, Yee SW, Krauss RM, Turner RM, Palaniappan L, Gaedigk A, Giacomini KM, Caudle KE, Voora D. The Clinical Pharmacogenetics Implementation Consortium Guideline for SLCO1B1, ABCG2, and CYP2C9 genotypes and Statin-Associated Musculoskeletal Symptoms. Clin Pharmacol Ther 2022 May;111(5):1007-1021. PM: 35152405.
Goodney P, Shah S, Hu YD, Suckow B, Kinlay S, Armstrong DG, Geraghty P, Patterson M, Menard M, Patel MR, Conte MS. A systematic review of patient-reported outcome measures patients with chronic limb-threatening ischemia. J Vasc Surg 2022 May;75(5):1762-1775. PM: 35085747.
Greene SJ, Tan X, Yeh YC, Bernauer M, Zaidi O, Yang M, Butler J. Factors associated with non-use and sub-target dosing of medical therapy for heart failure with reduced ejection fraction. Heart Fail Rev 2022 May;27(3):741-753. PM: 33471236.
Mark DB, Spertus JA, Bigelow R, Anderson S, Daniels MR, Anstrom KJ, Baloch KN, Cohen DJ, Held C, Goodman SG, Bangalore S, Cyr D, Reynolds HR, Alexander KP, Rosenberg Y, Stone GW, Maron DJ, Hochman JS. Comprehensive Quality-of-Life Outcomes With Invasive Versus Conservative Management of Chronic Coronary Disease in ISCHEMIA. Circulation 2022 Apr 26;145(17):1294-1307. PM: 35259918.
Minhas AMK, Salah HM, Khan MS, Rao VN, Tedford RJ, Reddy YNV, Caughey MC, Savarese G, Greene SJ, Michos ED, Fudim M. Most Common Causes of Hospitalization Associated with Inpatient Mortality in the United States Between 2005-2018. Am J Med Sci 2022 May;363(5):459-461. PM: 35090870.
Simonato M, Vemulapalli S, Ben-Yehuda O, Wu C, Wood L, Popma J, Feldman T, Krohn C, Hardy KM, Guibone K, Christensen B, Alu MC, Chen S, Ng VG, Chau KH, Shahim B, Vincent F, MacMahon J, James S, Mack M, Leon MB, Thourani VH, Carroll J, Krucoff M. Minimum Core Data Elements for Evaluation of TAVR: A Scientific Statement by PASSION CV, HVC, and TVT Registry. Ann Thorac Surg 2022 May;113(5):1730-1742. PM: 35367049.
Singh AK, Blackorby A, Cizman B, Carroll K, Cobitz AR, Davies R, Jha V, Johansen KL, Lopes RD, Kler L, Macdougall IC, McMurray JJV, Meadowcroft AM, Obrador GT, Perkovic V, Solomon S, Wanner C, Waikar SS, Wheeler DC, Wiecek A. Study design and baseline characteristics of patients on dialysis in the ASCEND-D trial. Nephrol Dial Transplant 2022 Apr 25;37(5):960-972. PM: 33744933.
Smilowitz NR, Cornwell M, Offerman EJ, Rockman CB, Shah SH, Newman JD, Ruggles K, Voora D, Berger JS. Risk factors, transcriptomics, and outcomes of myocardial injury following lower extremity revascularization. Sci Rep 2022 Apr 25;12(1):6718. PM: 35468922.
Voora D, Baye J, McDermaid A, Narayana Gowda S, Wilke RA, Nicole Myrmoe A, Hajek C, Larson EA. SLCO1B1*5 Allele Is Associated With Atorvastatin Discontinuation and Adverse Muscle Symptoms in the Context of Routine Care. Clin Pharmacol Ther 2022 May;111(5):1075-1083. PM: 35034348.
White HD, Schwartz GG, Szarek M, Bhatt DL, Bittner VA, Chiang CE, Diaz R, Goodman SG, Jukema JW, Loy M, Pagidipati N, Pordy R, Ristić AD, Zeiher AM, Wojdyla DM, Steg PG. Alirocumab after acute coronary syndrome in patients with a history of heart failure. Eur Heart J 2022 Apr 19;43(16):1554-1565. PM: 34922353.
Duke Heart Pulse – Updates from the week ending April 24th 2022
Sunil Rao, MD to take New Role Leading Interventional Cardiology at NYU Langone
It is bittersweet that we announce that Sunil Rao has accepted the position of Director of Interventional Cardiology for the NYU Langone Health System where he will work to facilitate coordination, program development, uniform quality standards, operational efficiency, financial goals and best practices across the NYULH System Cardiac Catheterization Laboratories.
We are extremely excited for Sunil and thrilled that he will be taking on this important leadership opportunity to continue to innovate the care of patients undergoing invasive procedures, and certain his impact and skill will be immediately felt across the NYU Langone cath labs.
He will be missed at Duke where he has been a friend, trusted colleague, mentor, teacher, and consummate interventionalist over the last 26 years. Sunil came to Duke after completing medical school at The Ohio State University and did his medical residency and cardiology, and interventional fellowship at Duke. Since coming on Faculty, he has been a north star for our invasive labs – studying, teaching, and ushering in radial procedures, best cath practices, and playing an instrumental role in how we think about and train the next generation of leaders in cardiology. His impact can be seen based on the number of fellows, trainees, and colleagues that look to work with him. He has been the repeatedly been the recipient of fellowship mentorship and teaching awards. Academically, he is an internationally recognized clinical investigator involved in many of the seminal trials in interventional cardiology around management of patients undergoing invasive procedures, including devices, access site, and treatment strategies.
He is also the current Chief of Cardiology at the Durham VA where is has helped transform the cardiovascular care of our veterans while supporting the faculty. He is currently the editor of Circulation Cardiovascular Interventions and will be the President of the Society for Cardiovascular Angiography and Intervention (SCAI) in May 2022. He is the true triple threat.
Personally, what I will miss most is the camaraderie, fun, and drive for excellence that Sunil brought to Duke every day.
Reflecting on his time at Duke, Sunil said, “Duke has been my home for 26 years and I consider the Cardiology division my family. The mentorship, collaborations, and friendships over the years have been integral to my personal and professional life. Although I will be leaving Duke, Duke will always be part of who I am. It’s really been a privilege to be part of Duke Heart.”
Congratulations Sunil – you will certainly be missed and we look forward to collaborating in the future.
Duncan Recognized for 36 Years of Service in Heart
Lisa Duncan will be retiring on May 2, 2022 after more than 36 years of service. Lisa has worked in the Heart Center since 1987  in varying roles including professional nursing assistant, nursing assistant, staff nurse, assistant head nurse and, since the 1990’s, as 7100 Nurse Manager of Operations. Throughout her time at Duke, she served on many task forces and committees.
in varying roles including professional nursing assistant, nursing assistant, staff nurse, assistant head nurse and, since the 1990’s, as 7100 Nurse Manager of Operations. Throughout her time at Duke, she served on many task forces and committees.
She received the highly esteemed Mary Ann Peter Friends of Nursing Award for excellence. Lisa is known for her approachability, fair and consistent practice, and patient/staff advocacy.
On behalf of the entire Duke Heart Center Leadership team, we thank Lisa for her loyalty and dedication to our patients, the faculty and staff of Duke Heart, as well as to Duke University Hospital.
Please join us in wishing her well in her retirement!
Heart Transplant Team Celebrates Donate Life Month
April is Donate Life Month and members of our heart transplant team were overjoyed to celebrate in person this year by attending the NC Gift of Life Gala which was held Thursday, April 21 at the Prestonwood Country Club in Cary. There, they enjoyed interacting as a team, bidding on artwork by local artists, hearing from organ recipients, and enjoying the delicious dinner and the silent auction.
The theme of the Gala this year was the HeART of the Matter, marking the use of the red heart on NC state drivers’ licenses for all those who promise to give the gift of life by becoming an organ donor. The team asks if you are not a registered organ donor, please consider becoming one!

Shown here are (L to R): Rotunda Kearney, Melissa Shreve, Tia Thompson, Emily Schneidewind, Sam Murari, Kris Barnes, Cathy Alligood and Sonia Leon.
Rotunda is a program specialist for the heart transplant team. Sonia and Sam are pre-heart transplant coordinators. Tia, Emily, Melissa, Kris and Cathy are post-heart transplant coordinators.
Special thanks to Chet Patel and Adam DeVore for giving their team the opportunity to attend and represent Duke Heart Transplant.
NC Organ Donation Fast Fact: In 2019, when North Carolina Governor Roy Cooper signed into law SB 210 Organ and Tissue Donation/Heart Heroes, it brought North Carolina into parity with the rest of the nation by including tissue for transplantation along with organs and eyes when one says “Yes” to donation at the DMV. Today, anyone who says “Yes” to donation at the NCDMV will be making a legal first-person authorization to become an organ, eye, and tissue donor upon death. Those who had the heart symbol placed on their drivers’ license or ID card before October 1, 2019 must take an extra step to add tissue donation to their registry status by visiting DonateLifeNC.org. Changes to your donor registration status can be made at any time by visiting the same site.

Shout-Out to Duke’s HF Guidelines Contributors
A big shout-out to Duke Heart team members who served as authors, reviewers or ACC/AHA/HFSA Joint Committee Members for the recently published 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. We are deeply grateful for the effort each of you have put into this effort – your work helps educate others and saves lives. Well done, Adrian Hernandez, Carmelo Milano, Sana Al-Khatib, Schuyler Jones and Dan Mark!
Kudos to Senman!
We are always pleased to hear about the great work our fellows are doing. This week, we heard about Balim Senman from  Corey Fry, our APP Team Lead in the Cardiac Intensive Care Unit via a note to Anna Lisa Chamis:
Corey Fry, our APP Team Lead in the Cardiac Intensive Care Unit via a note to Anna Lisa Chamis:
“I’d like to take a moment to recognize Dr. Balim Senman for the exceptional work she’s doing in CICU. Dr. Senman has been a leader, communicator, and positive source of support in CICU through the changes we’ve faced as a team over the past year.
“The CICU runs smoothly when Dr. Senman is working …and APP’s feel supported and heard. Her solution-based focus has made her a valuable partner in addressing workflow processes with the APP group… I appreciate her input and feedback. She’s an exceptional fellow with a bright future and I’m glad to have opportunity to work with her.”
Nicely done, Balim!!
Kudos to Lin!
Shu Lin was recently commended by Andrea Carpenter, president of the Thoracic Surgery Directors Association (TSDA) and Matthew Romano, the In-Training Exam Cardiac Subcommittee Chair of the TSDA, for his contributions to the TSDA’s 2022 In-Training Exam and for his work as a member of the ITE Cardiac Subcommittee. Great work Shu! Thank you for representing Duke Heart!

Cybersecurity Advisory Alert
A critical message was issued to all employees on Thursday by Jeff Ferranti, MD, chief digital officer and senior vice president for DUHS and Randy Arvay, PhD, chief information security officer for DUHS.
Due to the Russian invasion of Ukraine, the U.S. Department of Health & Human Services Health Sector Cybersecurity Coordination Center and Health-ISAC has issued a joint advisory for credible cybersecurity threats to U.S. critical infrastructure sectors.
Duke Health has been responsive and continues to expand our defense strategies. Initial actions prioritized leveraging our strong vendor partnerships and intelligence feeds to monitor for indicators of threats. But, we still need all Duke Health employees to remain vigilant and assist in protecting our systems and resources.
How to Safeguard Against Cyber Threats
We have seen an increase in suspicious email, phone calls, and text messaging to Duke staff, including some that have spoofed/faked prominent Duke leader names.
At this time, we feel that it is important to remind all staff of key steps that you can take, including:
- Staying vigilant around the potential for social engineering and phishing via email, phone (vishing), text (smishing) and social media. Do not click links or attachments or give out personal or sensitive information. Always independently verify that requests are coming from a known, trusted source.
- Using strong, unique passwords and multi-factor authentication (MFA) on all accounts. Duke offers a free password manager to all staff (oit.duke.edu/what-we-do/services/1password) and encourages staff to set their MFA preference to “Always” (idms-mfa.oit.duke.edu).
- Patching/Updating all software and running current Antivirus on personal devices.
- Avoiding use of free or untrusted Wi-Fi.
- Report all suspicious emails using ReportPhish in Outlook or other concerning activity or by contacting security@duke.edu.
Each of us, working together, can do our part to ensure the safety of our patients, their loved ones and each other.
Thank you for your continued vigilance!
NC Walk for Victory Raises $50K
Duke Heart was very proud to serve as the presenting sponsor of the NC Walk for Victory held yesterday at Laurel Hills Park in  Raleigh. The NC Walk for Victory raises much needed funding to support patients with Marfan syndrome, Loeys-Dietz, VEDS and related conditions. We had a really great day – and the teams exceeded their $50K fundraising goal — a testament to their dedication to research, programming and services offered by the Marfan Foundation
Raleigh. The NC Walk for Victory raises much needed funding to support patients with Marfan syndrome, Loeys-Dietz, VEDS and related conditions. We had a really great day – and the teams exceeded their $50K fundraising goal — a testament to their dedication to research, programming and services offered by the Marfan Foundation
Chad Hughes served as the medical director for the event. Hughes, Melissa Burkett and their team have done an incredible job of welcoming more patients and their families to Duke and providing access to treatment and support not readily available elsewhere. Great job!
Thanks to all who donated and walked to support our patients and their families!

Sports Cardiology & Sudden Death in Athletes CME
The Duke Sports Cardiology & Sudden Death in Athletes Symposium was held yesterday, April 23 with course directors Jim Daubert and Bill Kraus. The virtual event drew just over 160 registrants. Guest speakers included Duke faculty members Igor Klem, Howard Rockman, Jeff Bytomski, Hap Zarzour, Al Sun and Kenzie Johnston along with Aaron Baggish (Mass General) and Norbert Guettler (Central Military Hospital, Koblenz, Germany). Shout-out to Christy Darnell for terrific planning! The CME was free to attend; enduring material can be accessed for up to two years by registering and obtaining the link. To do so, please visit https://duke.is/gkffw.
directors Jim Daubert and Bill Kraus. The virtual event drew just over 160 registrants. Guest speakers included Duke faculty members Igor Klem, Howard Rockman, Jeff Bytomski, Hap Zarzour, Al Sun and Kenzie Johnston along with Aaron Baggish (Mass General) and Norbert Guettler (Central Military Hospital, Koblenz, Germany). Shout-out to Christy Darnell for terrific planning! The CME was free to attend; enduring material can be accessed for up to two years by registering and obtaining the link. To do so, please visit https://duke.is/gkffw.
Reves Lecture
Mark F. Newman, MD, Executive Vice President of Health Affairs at the University of Kentucky, former president of the Duke PDC and former chair of Duke Anesthesiology delivered Cardiology Grand Rounds on Tuesday evening and the Reves Lecture/Anesthesiology Grand Rounds on Wednesday morning. It was great to have Mark back on campus! (Pictured are Joe Mathew and Newman.) If you were unable to attend the Reves Lecture, it can be viewed here: https://dukemed.mediasite.com/Mediasite/Play/bd690445bc724c8488afab4226b6891a1d. Note, the main presentation begins approximately 17 minutes into the video.

COVID-19 Update
All the latest Clinical Operations updates related to COVID can be found at https://covid-19.dukehealth.org. Patient-facing resources on DukeHealth.org can be found here: https://www.dukehealth.org/covid-19-update/resources. Duke University maintains a resource page as well, which can be accessed here: https://coronavirus.duke.edu/updates/for-staff.
Upcoming Events & Opportunities
Cardiology Grand Rounds
April 26: Clinicopathologic Conference with Francis Ugowe. 5 p.m. via Webex.
May 3: Topic TBA with Navid Nafissi. Details forthcoming.
May 10: Topic TBA with Caitlin Dresher. Details forthcoming.
MDEpiNet Spring 2022 Virtual Mini-Think Tank
May 5: MDEpiNet Spring 2022 Virtual Mini-Think Tank. Noon – 5:30 p.m., ET
MDEpiNet Predictable And SuStainable Implementation Of National CardioVascular Registries (PASSION CVR) Registry-Supported Prospective Clinical Trials
Join and invite your colleagues to join for updates from, and dialogues across our Registry-supported Prospective Trials Working Groups:
- Data Governance & Access
- Operational Roles & Responsibilities
- Global Regulatory Acceptance
- Use Cases:
- Aortic Intervention
- Heart Valves
- Mechanical Circulatory Support
- Peripheral Arterial Intervention
Registration now open: https://duke.qualtrics.com/jfe/form/SV_2f6JBD6WfaF9jBc.
Evening with Heart Raleigh
An Evening with Heart Raleigh, which has been rescheduled from earlier this year, will benefit Marfan families as well as those with Loeys-Dietz (LDS), Vascular Ehlers-Danlos (VEDS), and related conditions.
May 5, 2022
The Maxwell
7-10 p.m.
Cocktail attire
Tickets for the event include open bar, taco bar, heavy appetizers, dessert, silent auction, DJ, and a fun photo booth. For those unable to attend in person but who would like to participate, the silent auction items can be bid on online from anywhere. Lots of cool items have been donated so far! For tickets, more information or silent auction viewing and bidding, please visit: https://marfan.ejoinme.org/raleigh22.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
April 15 — Richard Shannon
WNCN, CBS-17
Annual campaign aims to improve maternal health outcomes for Black women
https://duke.is/zwp56
April 15 — Jonathan Piccini
DotMed/HealthCareBusiness News
Patients with infected cardiac implants should have them removed
https://duke.is/nmm2j
April 16 — Robert Mentz
Healio/Cardiology Today
Editors of HF journal question use of the word ‘candidate’
https://duke.is/b67cp
April 21 — Kevin Oeffinger (Duke Cancer Institute)
Healio/Hematology-Oncology
Cardiovascular care of pediatric cancer survivors: Mitigating a lifelong risk
https://duke.is/whpd9
April 22 — Sean Pokorney
Cardiology Advisor
ACC: Infected CV Implantable Electronic Devices Often Not Removed
https://duke.is/jvyyc
Duke Heart Pulse week ending April 17th 2022
Chief’s message:
This weekend hopefully you all got some time to spend with family around Easter, Ramadan, Passover, or just to get time spend together. The last few years have taught all of use to ensure we enjoy the moments with friends and family to recharge. Personally, we want to thank the Duke Heart teams that have continued to pull together for our patients and each other in the ever changing world of health care.
Highlights of the week:
Shout-out to Duke Heart teams
A tremendous shout-out to Duke Heart team members throughout our clinical care areas, in particular to our interventional teams. As many of you know, the EP and Cath Labs were tremendously busy this past week!

According to Anna Mall, cases in the cath lab began to spike on Friday, April 8 with a record setting 38 cases completed. She added that on Monday alone, 44% of cases were PCI, including four STEMI. Tuesday, the trend continued with 32 cases and multiple STEMI activations. Volume hadn’t waned toward the end of the week — the teams continued to see busy outpatient and inpatient case volumes.
“Special thanks to the cath lab staff, fellows and faculty for the amazing teamwork handling incredibly busy days – all with a smile!!” — Anna Mall
The interventional teams really pulled together to establish unique work flows in order to manage this uptick in patient cases, according to Jill Engel, associate VP, Duke Heart.
We’d like to add a special shout-out to Andrew Wang, MD, who has been exceptional with morning bed flow call. Across the board, we thank all cardiologists and nursing teams for helping manage bed capacity and patient care. This has been a truly busy time for everyone and Duke Heart leadership appreciates the way everyone has pulled together to help.
THANK YOU! We appreciate all that you and your teams are doing to take great care of our patients and to keep everyone safe. Great job, everyone!!!
Wrobel Named Chief Cardiology Fellow
We are pleased to share the wonderful news that our Duke Cardiology fellows have selected Dr. Christopher Wrobel as their 2022-2023 Chief Cardiology Fellow. The announcement was made earlier this week by fellowship director Anna Lisa Chamis, MD.

Wrobel was born and raised in Valparaiso, IN. He obtained a BS in chemistry from Duke in 2009. After teaching high school chemistry in New Orleans for two years, he returned to Indiana for medical school. There he met his wife, Dr. Heather Wolfe. Wrobel completed his internal medicine residency at University of Texas Southwestern (UTSW) in 2018. He worked as a hospitalist for one year at UTSW before returning to Duke for cardiology fellowship.
He will complete his Advanced Heart Failure and Transplant Cardiology fellowship in June. Heather and Chris are expecting their first child later this month. In his spare time, Chris enjoys traveling, moonlighting as an amateur restaurant critic, exploring Old World wine, and irrationally supporting his favorite sports teams.
Wrobel will transition to his new role in June. (Photo shows Drs. Chris and Heather Wrobel.)
Please join us in congratulating Chris and welcoming him to his new role!
Thank-you to Coniglio!
Please join us in thanking Dr. Amanda Coniglio for serving as the Cardiology fellowship Chief Fellow this past year. She has worked tirelessly to advocate for the fellows. In a message to the team this week, Dr. Anna Lisa Chamis shared the following:
“Dr. Coniglio’s impact on our fellowship program has been substantial! In particular, she started a bi-monthly fellows’ Critical Care conference, sent weekly educational and informational summaries to all the fellows with references and championed the return to in-person gatherings – in addition to the routine Chief Fellow responsibilities.

Coniglio will be joining the advanced heart failure team at Rochester General Hospital after graduation.” Amanda is shown here with her husband, Dr. Andrew Coniglio.
When asked about her experience this year, Dr. Coniglio said, “I am incredibly grateful for the opportunity to have served as chief this past year and am hopeful that the initiation of CICU case conferences and weekly conference summaries have been an educational resource to all. Congratulations and best wishes to Dr. Wrobel on being elected as chief!”
Coniglio will transition the Chief Fellow role to Dr. Chris Wrobel during June.
Great job, Amanda!
Patel Receives SOM Faculty Award
Manesh Patel, MD, professor of medicine and chief of the Division of Cardiology, has been selected to receive the School of Medicine’s Career Mentoring Award in Clinical Research – Population Health. Patel commented that he was “Humbled for the opportunity to work with some of the best colleagues, fellows, and faculty in cardiovascular medicine. Also appreciative of those that have supported, mentored and taught me including Bob Harrington, Rob Califf, Pam Douglas, Chris O’Connor and many others.”
Chen Inducted to ASA
Congratulations to Edward P. Chen, MD, chief of the Division of Cardiovascular and Thoracic Surgery! Chen was inducted into the American Surgical Association during their 142nd annual meeting held April 7-9 in Chicago at the Chicago Marriott Downtown Magnificent Mile.
Way to go!
Shah to Lead ASPC Group
Congratulations to Nishant Shah! He has been selected to serve a 1-year term as Chair of the Fellow-in-Training and Early Career Working Group of the American Society for Preventive Cardiology.
Mark Newman to Deliver Reves Lecture
This week, Dr. Mark F. Newman, Executive Vice President of Health Affairs at the University of Kentucky, former president of the Duke PDC and former chair of Duke Anesthesiology, will deliver Cardiology Grand Rounds and the Reves Lecture. Both events promise to be excellent and both are listed in the event section below. Not to be missed!
COVID-19 Update
Second Booster Shot Available for Eligible Faculty, Staff and Students
Duke is now offering second booster shots of the COVID-19 vaccine for eligible faculty, staff and students over the age of 50, as well as anyone who is considered severely immunocompromised to increase their protection against severe disease.
Following approval by the U.S. Food and Drug Administration and the Centers for Disease Control and Prevention last week, Duke will offer the Pfizer vaccine as a second booster shot for those who have had their first booster shot at least four months ago. The second booster shot is not currently required for Duke students, faculty or staff, but it is offered as an option for those who are eligible.
Second booster shots are available by appointment or walk-in at the Duke Medical Pavilion in Conference Room 2w91, Duke Clinic 1J, Duke Regional Hospital and Duke Raleigh Hospital. For more information or to schedule an appointment, visit the Duke COVID Vaccine website. Eligible faculty, staff and students are also encouraged to consider vaccination options at local pharmacies or their healthcare provider.
All the latest Clinical Operations updates related to COVID can be found at https://covid-19.dukehealth.org. Patient-facing resources on DukeHealth.org can be found here: https://www.dukehealth.org/covid-19-update/resources. Duke University maintains a resource page as well, which can be accessed here: https://coronavirus.duke.edu/updates/for-staff.
Upcoming Events & Opportunities
Cardiology Grand Rounds
April 19: Treating the Epidemic after the Pandemic with Mark Newman, University of Kentucky. 5 p.m., DN 2002 or online via Webex.
Reves Lecture/Anesthesiology Grand Rounds
April 20: Reves Lecture: Creating Alignment for a Healthier State with Mark Newman, University of Kentucky. 7 a.m., DN 2001 or online via Webex. (Link will not be available until 4/18)
Dr. Mark Newman currently serves as Executive Vice President of Health Affairs at the University of Kentucky. The Reves Visiting Professorship and Lecture is supported by the philanthropic efforts of our donors in honor of Jerry Reves, MD, former chair of Duke Anesthesiology.
Note: seating for the in-person lectures on April 19 & 20 will be limited to half the room capacity due to COVID protocols.
Duke Heart CME
April 23: Duke Sports Cardiology & Sudden Death in Athletes Symposium with course directors Jim Daubert and Bill Kraus. Virtual. For information or to register, please visit: https://duke.is/gkffw. If you have additional questions, please contact Christy Darnell christy.darnell@duke.edu or 919-880-8686.
MDEpiNet Spring 2022 Virtual Mini-Think Tank
May 5: MDEpiNet Spring 2022 Virtual Mini-Think Tank. Noon – 5:30 p.m., ET
MDEpiNet Predictable And SuStainable Implementation Of National CardioVascular Registries (PASSION CVR) Registry-Supported Prospective Clinical Trials
Join and invite your colleagues to join for updates from, and dialogues across our Registry-supported Prospective Trials Working Groups:
- Data Governance & Access
- Operational Roles & Responsibilities
- Global Regulatory Acceptance
- Use Cases:
- Aortic Intervention
- Heart Valves
- Mechanical Circulatory Support
- Peripheral Arterial Intervention
Registration now open: https://duke.qualtrics.com/jfe/form/SV_2f6JBD6WfaF9jBc.
Marfan NC Walk for Victory, April 23
The North Carolina Walk for Victory to support Marfan patients and their families will take place on Saturday, April 23, 2022 from Noon to 3 p.m. at Laurel Hills Park on Edwards Mill Road in Raleigh.
Duke Heart is proud to serve as the presenting sponsor and we are excited for Chad Hughes, MD to serve as medical chair for the walk.
Please help us support all Marfan families as well as those with Loeys-Dietz (LDS), Vascular Ehlers-Danlos (VEDS), and related conditions. Donate or come join us at the event! Parking is easy to access and free.
Walk for Victory is The Marfan Foundation’s global walk program. The event is low-key, fun and family-oriented. To learn more or to register for this event, please visit: https://give.marfan.org/event/2022-north-carolina-walk-for-victory/e353032.
To learn more about The Marfan Foundation, please visit marfan.org.
Evening with Heart Raleigh
May 5, 2022
The Maxwell
7-10 p.m.
Cocktail attire
(This event was rescheduled from earlier in the year.) For those unable to attend in person but who would like to participate, the silent auction items can be bid on online from anywhere. Lots of cool items have been donated so far! Tickets for the event include open bar, taco bar, heavy appetizers, dessert, silent auction, DJ, and a fun photo booth. Proceeds benefit The Loeyz-Dietz and Marfan Foundation. For tickets, more information or silent auction viewing and bidding, please visit: https://marfan.ejoinme.org/raleigh22.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
April 8 — G. Michael Felker
tctMD
METEORIC-HF: Omecamtiv Mecarbil Doesn’t Boost Exercise Capacity in HFrEF
https://duke.is/v4q88
April 8 — Sean Pokorney
U.S. News & World Report
Few People Get Infected Heart Devices Removed, Despite Benefit
https://duke.is/z8zbz
*this story was carried by 10 additional news outlets including UPI, HealthDay and MSN News
April 10 — Mark Sendak and Cara O’Brien (DIHI)
The Wall St. Journal
How Hospitals Are Using AI to Save Lives
https://duke.is/mucf7
April 11 — Sean Pokorney
Cardiovascular Business
VIDEO: Lowering mortality rates from infected EP implantable cardiac devices
https://duke.is/jypq3
April 11 — Jonathan Piccini
Healio/Cardiology
Fitbit receives FDA clearance for algorithm to detect AF
https://duke.is/ywqnc
April 11 — Sean Pokorney
HealthDay
ACC: Infected CV Implantable Electronic Devices Often Not Removed
https://duke.is/rfc5n
April 12 — Christopher Granger
tctMD
Managing AF Patients Undergoing PCI—Some Lingering Questions
https://duke.is/zmez8
April 12 — Duke University (CIED ACC LBCT)
Becker’s Hospital Review
https://duke.is/6vcuk
Duke Heart Pulse week ending April 10th 2022
Highlights of the week:
ACC.22: Looking Back
There were so many excellent presentations across ACC – great job, everyone! Sana Al-Khatib submitted the following thoughts to us regarding the outstanding presentations by our cardiology fellows:
It was very uplifting to connect with friends and colleagues at ACC22 and learn about the latest scientific discoveries that will benefit our patients. To me, the main highlight of the meeting was our fellows’ strong presence and participation.
 Vishal Rao gave a very informative and interesting presentation on intravascular blood volume analysis and hemodynamic measures of vascular compliance in patients hospitalized with heart failure. Kelly Arps did a great job presenting novel data on time to relapse after weaning immune suppressive therapy in cardiac sarcoidosis. Vanessa Blumer gave a very engaging and insightful presentation on whether a PA catheter is needed for the cardiogenic shock patient (to which my answer is always ‘yes ’; my view on this has not changed since my fellowship ). Josephine Harrington did an excellent job presenting powerful data on NOAC use in patients with atrial fibrillation and reduced renal function in the COMBINE-AF database (the largest analysis on this topic to date). Anthony Peters gave a very important and clinically relevant presentation on decongestion, quality of life and outcomes among patients hospitalized for HFrEF versus HFpEF. Michelle Kelsey masterfully facilitated a discussion on managing the patient with obesity, new onset diabetes, and a family history of CV disease. Both Josephine and Vanessa did a great job moderating poster sessions.
Vishal Rao gave a very informative and interesting presentation on intravascular blood volume analysis and hemodynamic measures of vascular compliance in patients hospitalized with heart failure. Kelly Arps did a great job presenting novel data on time to relapse after weaning immune suppressive therapy in cardiac sarcoidosis. Vanessa Blumer gave a very engaging and insightful presentation on whether a PA catheter is needed for the cardiogenic shock patient (to which my answer is always ‘yes ’; my view on this has not changed since my fellowship ). Josephine Harrington did an excellent job presenting powerful data on NOAC use in patients with atrial fibrillation and reduced renal function in the COMBINE-AF database (the largest analysis on this topic to date). Anthony Peters gave a very important and clinically relevant presentation on decongestion, quality of life and outcomes among patients hospitalized for HFrEF versus HFpEF. Michelle Kelsey masterfully facilitated a discussion on managing the patient with obesity, new onset diabetes, and a family history of CV disease. Both Josephine and Vanessa did a great job moderating poster sessions.
Seeing our fellows share their research findings and knowledge on a national stage was incredibly  rewarding. Indeed, having the opportunity to work with superb trainees is one of the best aspects of our work at Duke. Kudos to our fellows and the faculty mentoring them!
rewarding. Indeed, having the opportunity to work with superb trainees is one of the best aspects of our work at Duke. Kudos to our fellows and the faculty mentoring them!
We agree, Sana! Our trainees are superb and we are so proud of them!
Additionally, Schuyler Jones let us know that the VALOR HCM team presented positive trial results on Saturday at ACC. Duke was the 6th highest enrolling site and Kim Biever was one of the CRCs recognized on the enrollment ranking. Great job, Kim and to Duke’s VALOR HCM team!
We also learned that Midge Bowers led Cardio-OB simulations at ACC. Way to go!



Our late-breaker teams received quite a bit of news coverage this week. Check it out below in our news section.
Mentz Recognized with Master CardioNerd Award

We were thrilled to learn this week that Robert Mentz was selected for the Master CardioNerd Award by the CardioNerds team.
“It is with the utmost respect, gratitude, and privilege that we offer you the Master CardioNerd Award. This honor is awarded to a faculty who ‘supports the mission to democratize cardiovascular education.’
The CardioNerds Clinical Trials Network is a major credit to your mentorship, innovation, and vision. We are hopeful that the lessons from this program will be applicable to other subspecialties as we learn how best to enhance trial enrollment that is both efficient and equitable as well as nurture careers in clinical research.
We are also very excited to produce the Decipher the Guidelines Series for the 2022 HF Guidelines with yourself and Dr. Anu Lala as Series Mentors.
CardioNerds is just a 28-month old toddler. Your constant support, mentorship, and encouragement has helped us mature into the platform it is today. We are eternally grateful and will continue benefiting from your inspiration as we look beyond our terrible twos.”
The message was signed by CardioNerds co-founders Amit Goyal, MD, cardiovascular fellow at the Cleveland Clinic and Daniel Ambinder, MD, interventional/structural cardiology fellow at Johns Hopkins.
The video is a must-see: https://twitter.com/i/status/1512374750114459654
Congratulations, Rob!!!
Rymer, Greene Receive AHA Career Development Awards

Congratulations to Jennifer Rymer, MD and Stephen Greene, MD! Both have

been notified that they’ll be receiving Career Development Awards from the American Heart Association.
Rymer’s project title is Implementation of a Medication Adherence Instrument Among Patients with Symptomatic Peripheral Artery Disease after PVI. Her mentors include: Tracy Wang, Schuyler Jones, Hayden Bosworth, Sharron Docherty, and Manesh Patel. Her funding is for three years, effective April 1.
Greene’s project title is Use and Effectiveness of Outpatient Intravenous Diuretic Therapy as Treatment of Worsening Heart Failure. He will study the clinical and economic implications of treating select patients with worsening heart failure using an outpatient IV diuretic strategy, as compared with a traditional strategy centered on hospitalization. His mentors include G. Michael Felker, Adrian Hernandez, Brad Hammill, Javed Butler of the University of Mississippi Medical Center, and Greg Fonarow at UCLA. Funding is for three years, effective April 1.
Such great news! Congratulations!
Kudos to Glower
We received the following note regarding Donald Glower, MD:

“Good Afternoon, I had the opportunity to spend time this afternoon with a patient who was being discharged from 3300 after valve surgery by Dr. Glower. He was effusive in his praise for his team. He noted that Dr. Glower communicated well and rounded on him, personally, often 2 times/day. He felt lucky to have had the very best for his surgery. He noted that his nurses, especially all in the ICU (whose names he could not recall) and Connie on 3300 were outstanding. He also called out by name Valerie, who kindly took his food order and was so professional and caring. He feels like he has a new lease on life and is grateful for your care. Thank you all for the part you have played and please forward this to those whose last names I do not have. Very best wishes, Lisa”
Lisa Clark Pickett MD FACS
Assistant Professor of Surgery and Medicine, Duke University & Chief Medical Officer, Duke University Hospital
Great work, Don!
Harpole Named Geller Distinguished Professor
We are pleased to share with you that thoracic surgeon David H. Harpole, Jr., MD, professor of surgery in the Division of Cardiovascular and Thoracic Surgery, will be named the George Barth Geller Distinguished Professor for Research in Cancer effective July 1, 2022.
Wonderful news, David! Congratulations!!
Kudos to Carlisle
 We received the following note regarding cardiology fellow Matt Carlisle:
We received the following note regarding cardiology fellow Matt Carlisle:
“Dr. Matt Carlisle came to see a rapidly decompensating patient in the Emergency Department recently. He had just began his shift when he received a phone call from the ED Cardiology Consult provider about an unstable patient. He came immediately to bedside to assess the patient. Ultimately, he placed an urgent temporary pacemaker in the patient. Dr. Matt Carlisle is always attentive to patient needs, and is super kind and helpful to his coworkers.” — Jordan Hausladen, Advanced Practice Provider, Division of Cardiology
Way to go, Matt!
Duke Sonographers Attend NCUS
The North Carolina Ultrasound Society’s 42nd annual Spring Symposium was held last weekend in Wilmington, NC. Congratulations to the Duke Heart CDU and Duke Cardiac Ultrasound Program for representing Duke at the conference this year!
Cardiac Sonographer Jon Owensby gave the Saturday morning lecture on Aortic Stenosis Evaluation and cardiac sonographer Jayne Leypoldt gave the Sunday morning lecture on Mitral Regurgitation; student Courtney Snyder entered the Scientific Exhibit competition, winning 3rd place for a stellar exhibit on Pericardiocentesis!
We have an incredible and active sonography team within Duke Heart! Great job!



Duke Heart Network Visit to Frey Regional
Members of the Duke Heart Network and Duke Heart leadership team received a warm welcome at Frey Regional during a site visit held on March 21.
Shown L-R are: Jill Engel, Katie Troxler, Desiree Bonadonna, Lisa Kotyra, Trevor Krawchuk, Dr. Edward P. Chen, Dr. Brett Starr (CT surgeon at Frey) and Pam Peaks.

Palma Appointed Commissioner for CAAHEP
Richard Palma, program director of the Duke Cardiac Ultrasound Certificate Program, has been  appointed as a commissioner for the Commission on Accreditation of Allied Health Education Programs (CAAHEP) representing Hospital/VA Based Educational Institutions.
appointed as a commissioner for the Commission on Accreditation of Allied Health Education Programs (CAAHEP) representing Hospital/VA Based Educational Institutions.
His 3-year term began late last month. Congratulations, Richie!
Join the NC Walk for Victory, April 23 – Support Marfan!
We are looking forward to the upcoming NC Walk for Victory in support of the Marfan Foundation and the many families they help. The walk is coming up on Saturday, April 23. Event details are below, under “events”. We have 125 registered participants with seven new families joining the walking teams from 2021. Please consider joining us! To learn more, visit: https://duke.is/phzdy.
COVID-19 Updates
Second Booster Shot Available for Eligible Faculty, Staff and Students
Duke is now offering second booster shots of the COVID-19 vaccine for eligible faculty, staff and students over the age of 50, as well as anyone who is considered severely immunocompromised to increase their protection against severe disease.
Following approval by the U.S. Food and Drug Administration and the Centers for Disease Control and Prevention last week, Duke will offer the Pfizer vaccine as a second booster shot for those who have had their first booster shot at least four months ago. The second booster shot is not currently required for Duke students, faculty or staff, but it is offered as an option for those who are eligible.
Second booster shots are available by appointment or walk-in at the Duke Medical Pavilion in Conference Room 2w91, Duke Clinic 1J, Duke Regional Hospital and Duke Raleigh Hospital. For more information or to schedule an appointment, visit the Duke COVID Vaccine website. Eligible faculty, staff and students are also encouraged to consider vaccination options at local pharmacies or their healthcare provider.
All the latest Clinical Operations updates related to COVID can be found at https://covid-19.dukehealth.org. Patient-facing resources on DukeHealth.org can be found here: https://www.dukehealth.org/covid-19-update/resources. Duke University maintains a resource page as well, which can be accessed here: https://coronavirus.duke.edu/updates/for-staff.
Upcoming Events & Opportunities
Cardiology Grand Rounds
April 19: Treating the Epidemic after the Pandemic with Mark Newman (University of Kentucky). 5 p.m. In-person, DN2002. Online link coming soon.
April 20: Alignment for a Healthier State (Reves Lecture) with Mark Newman (University of Kentucky). 7 a.m. In-person, DN 2001. Online link coming soon.
Dr. Mark Newman currently serves as Executive Vice President of Health Affairs at the University of Kentucky. The Reves Visiting Professorship and Lecture is supported by the philanthropic efforts of our donors in honor of Jerry Reves, MD, former chair of Duke Anesthesiology and a co-founder of Duke Heart Center. Note: seating for the in-person lectures will be limited to half the room capacity due to COVID protocols.
Duke Heart CME
April 23: Duke Sports Cardiology & Sudden Death in Athletes Symposium with course directors Jim Daubert and Bill Kraus. Virtual. For information or to register, please visit: https://duke.is/gkffw. If you have additional questions, please contact Christy Darnell christy.darnell@duke.edu or 919-880-8686.
Marfan NC Walk for Victory, April 23
The North Carolina Walk for Victory to support Marfan patients and their families will take place on Saturday, April 23, 2022 from Noon to 3 p.m. at Laurel Hills Park on Edwards Mill Road in Raleigh.
Duke Heart is proud to serve as the presenting sponsor and we are excited for Chad Hughes, MD to serve as medical chair for the walk.
Please help us support all Marfan families as well as those with Loeys-Dietz (LDS), Vascular Ehlers-Danlos (VEDS), and related conditions. Donate or come join us at the event! Parking is easy to access and free.
Walk for Victory is The Marfan Foundation’s global walk program. The event is low-key, fun and family-oriented. To learn more or to register for this event, please visit: https://give.marfan.org/event/2022-north-carolina-walk-for-victory/e353032.
To learn more about The Marfan Foundation, please visit marfan.org.
MDEpiNet Spring 2022 Virtual Mini-Think Tank
May 5: MDEpiNet Spring 2022 Virtual Mini-Think Tank. Noon – 5:30 p.m., ET
MDEpiNet Predictable And SuStainable Implementation Of National CardioVascular Registries (PASSION CVR) Registry-Supported Prospective Clinical Trials
Join and invite your colleagues to join for updates from, and dialogues across our Registry-supported Prospective Trials Working Groups:
- Data Governance & Access
- Operational Roles & Responsibilities
- Global Regulatory Acceptance
- Use Cases:
- Aortic Intervention
- Heart Valves
- Mechanical Circulatory Support
- Peripheral Arterial Intervention
Registration now open: https://duke.qualtrics.com/jfe/form/SV_2f6JBD6WfaF9jBc.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
March 31 — Harold Koenig (psychiatry) and Rachel Tobin (internal medicine)
Medscape
Spiritual Interventions Improve QOL, Outcomes in HF
https://duke.is/mq7ba
April 3 — Sean Pokorney and Jonathan Piccini
Cardiac Rhythm News
ACC.22: Analysis shows low rate of device removal in case of CIED infection
https://duke.is/rttj3
April 4 — Robert Mentz
CBS News*
https://duke.is/b6cpq
*carried by 152 additional news outlets
April 4 — Manesh Patel and Jonathan Piccini
News-Medical.net
New type of anti-clotting drug reduces bleeding incidents among patients with atrial fibrillation
https://duke.is/c5puu
April 4 — Stephen Greene
Practical Cardiology
Q&A on SODIUM-HF and Impact of Salt Restriction, with Stephen Greene, MD
https://duke.is/5kpcc
April 4 — Sean Pokorney
News-Medical.net
Just 18% of patients have their infected heart devices removed, even though removal is recommended
https://duke.is/w7f3j
April 4 — Sean Pokorney and Jonathan Piccini
Cardiology Today
Most patients with implantable device infections do not receive extraction
https://duke.is/6jtwe
April 4 — Sean Pokorney
tctMD
Most Infected Cardiac Implanted Electronic Devices Not Removed Fast Enough
https://duke.is/p4p5m
April 4 — Sean Pokorney
Modern Healthcare
Doctors aren’t removing infected heart implants, resulting in patient deaths, study finds
https://duke.is/4szqk
April 4 — G. Michael Felker
News-Medical.net
Experimental heart failure drug has little impact on exercise tolerance
https://duke.is/jrq7t
April 4 — G. Michael Felker
Cardiovascular Business
Cholesterol medications, flu shots and heart failure: Day 2 at ACC.22
https://duke.is/ybzsn
April 4 — Manesh Patel
Endpoints News
Running behind Bristol Myers and J&J, Bayer inches forward in the next-gen blood thinner race
https://duke.is/9ecn2
April 5 — Sean Pokorney and Jonathan Piccini
Medtech Dive
Nearly 80% of patients with infection following cardiac implant not treated appropriately: study
https://duke.is/2ycax
April 5 — Stephen Greene
Practical Cardiology
Don’t Miss a Beat: ACC.22 Recap of DIAMOND, SODIUM-HF, and PROMPT-HF
https://duke.is/gwet6
April 5 — Sean Pokorney
ScienceBlog.com
Few Patients Have Infected Heart Devices Removed Despite Lifesaving Benefits
https://duke.is/v3qrf
April 6 — Manesh Patel
Medscape
Less Bleeding With Factor XI Inhibitor Anticoagulant? PACIFIC-AF
https://duke.is/7mz84
April 6 — G. Michael Felker
Medical Dialogues
Omecamtiv Mecarbil Has Little Impact on Exercise Tolerance in HF Patient: METEORIC-HF Trial
https://duke.is/mv7y6
April 6 — Sean Pokorney
MDEdge.com
Extraction of infected implanted cardiac devices rare, despite guidelines
https://duke.is/65qs2
April 7 — Sean Pokorney
Medscape
Extraction of Infected Implanted Cardiac Devices Rare, Despite Guidelines
https://duke.is/8pcgb
Division of Cardiology Publications Indexed in PubMed March 31 – April 6, 2022
Avezum Á, Oliveira GBF, Oliveira H, Lucchetta RC, Pereira VFA, Dabarian AL, D O Vieira R, Silva DV, Kormann APM, Tognon AP, De Gasperi R, Hernandes ME, Feitosa ADM, Piscopo A, Souza AS, Miguel CH, Nogueira VO, Minelli C, Magalhães CC, Morejon KML, Bicudo et al. Hydroxychloroquine versus placebo in the treatment of non-hospitalised patients with COVID-19 (COPE – Coalition V): A double-blind, multicentre, randomised, controlled trial. Lancet Reg Health Am 2022 Jul;11:100243. PM: 35378952.
Bishawi M, Lee FH, Abraham DM, Glass C, Blocker SJ, Cox DJ, Brown ZD, Rockman HA, Mao L, Slaba TC, Dewhirst MW, Truskey GA, Bowles DE. Late onset cardiovascular dysfunction in adult mice resulting from galactic cosmic ray exposure. iScience 2022 Mar 16;25(4):104086. PM: 35378858.
Coylewright M, Dodge SE, Bachour K, Hossain S, Zeitler EP, Kearing S, Douglas PS, Holmes D, Reddy VY, Nair D. Women in procedural leadership roles in cardiology: The Women In Local Leadership (WILL) observational study. Heart Rhythm 2022 Apr;19(4):623-629. PM: 34923161.
Dong OM, Poonnen PJ, Winski D, Reed SD, Vashistha V, Bates J, Kelley MJ, Voora D. Cost-Effectiveness of Tumor Genomic Profiling to Guide First-Line Targeted Therapy Selection in Patients With Metastatic Lung Adenocarcinoma. Value Health 2022 Apr;25(4):582-594. PM: 35365302.
Dzau VJ, Ellaissi WF, Krishnan KRR, Balatbat CA. How Academic Health Systems Can Be Ready for the Next Pandemic. Acad Med 2022 Apr 1;97(4):479-483. PM: 34966030.
Khan MS, Segar MW, Usman MS, Singh S, Greene SJ, Fonarow GC, Anker SD, Felker GM, Januzzi JL, Butler J, Pandey A. Frailty, Guideline-Directed Medical Therapy, and Outcomes in HFrEF: From the GUIDE-IT Trial. JACC Heart Fail 2022 Apr;10(4):266-275. PM: 35361446.
Martin CK, Höchsmann C, Dorling JL, Bhapkar M, Pieper CF, Racette SB, Das SK, Redman LM, Kraus WE, Ravussin E. Challenges in defining successful adherence to calorie restriction goals in humans: Results from CALERIE™ 2. Exp Gerontol 2022 Jun 1;162:111757. PM: 35240264.
Morrill J, Qirko K, Kelly J, Ambrosy A, Toro B, Smith T, Wysham N, Fudim M, Swaminathan S. A Machine Learning Methodology for Identification and Triage of Heart Failure Exacerbations. J Cardiovasc Transl Res 2022 Feb;15(1):103-115. PM: 34453676.
Rao VN, Fudim M, Wang J. Beyond the Anatomy of Renal Nerves: Functional Diversity of Renal Nerves. J Cardiovasc Transl Res 2022 Feb;15(1):27-28. PM: 35212975.
Tobin RS, Cosiano MF, O’Connor CM, Fiuzat M, Granger BB, Rogers JG, Tulsky JA, Steinhauser KE, Mentz RJ. Spirituality in Patients With Heart Failure. JACC Heart Fail 2022 Apr;10(4):217-226. PM: 35361439.
Vinson AJ, Singh S, Chadban S, Cherney D, Gaber O, Gill JS, Helgeson E, Herzog CA, Jardine M, Jha V, Kasiske BL, Mannon RB, Michos ED, Mottl AK, Newby K, Roy-Chaudhury P, Sawinski D, Sharif A, Sridhar VS, Tuttle KR, Vock DM, Matas A. Premature Death in Kidney Transplant Recipients: The Time for Trials is Now. J Am Soc Nephrol 2022 Apr;33(4):665-673. PM: 35292438.
Xiong X, Nazo N, Revoori R, Rajagopal S, Sparks MA. G protein- and -arrestin Signaling Profiles of Endothelin Derivatives at the Type A Endothelin Receptor. Kidney360 2021 May 17;2(7):1124-1131. PM: 35368349.
Xu H, Granger BB, Drake CD, Peterson ED, Dupre ME. Effectiveness of Telemedicine Visits in Reducing 30-Day Readmissions Among Patients With Heart Failure During the COVID-19 Pandemic. J Am Heart Assoc 2022 Apr 5;11(7):e023935. PM: 35229656.
Duke Heart week ending April 3rd 2022
Chief’s message:
Living in the Moment:
If anything, the last few years have taught us how fragile our usual way life is and how much things can change quickly. This week’s Pulse is notable for the fact that the American College of Cardiology conference has been going on both virtually but also in-person this weekend. The conference has had vaccination confirmation and masking, but still has quite a bit of great science and clinical sessions that our fellows and faculty have worked to present. You will see some of it here and more over the upcoming months. More importantly has been the ability to see people (not on zoom) and exchange ideas and just be back together has been important. The weekend of course has also had the ups and downs (depending on your shades of blue) around the Final Four. The outcome of the game, despite not being favorable for the Duke side of the world, has also underscored the refrain from the pandemic to Coach K of living in the moment. The ability to appreciate your colleagues, friends, and most importantly family. As we continue to go through the changes in our healthcare environment, the unknown around virus resurgences or getting back to life, we hope you all have time to spend with loved ones. The conference this week has highlighted for Duke Cardiology the value of our colleagues, alumni, fellows, and friend near and far. More than ever – it has also provided an opportunity to enjoy and live in the moment for our group.


Highlights of the week:
ACC.22: Few Patients Have Infected Heart Devices Removed Despite Lifesaving Benefits
Medicare patients whose implantable heart devices became infected were less likely to die from the complication if they had the hardware removed compared to patients who only received antibiotics, according to the largest study on the topic, led by the Duke Clinical Research Institute.
The study showed that just 18 percent of patients with device infections underwent surgeries to have their pacemakers or defibrillators removed, even though removal is recommended by all leading medical society treatment guidelines. There is a 43-percent lower risk of death in these patients if guidelines are followed.
The findings, reported earlier today as a late-breaker presentation at the 2022 American College of Cardiology Scientific Sessions, highlight that cardiac device infection is a major public health issue, and there are large gaps in guideline adherence.
“This is an important message about a persistent gap in care: These devices should be removed when an

infection occurs, and their removal saves lives,” said lead author Sean D. Pokorney, MD, an electrophysiologist and cardiologist in the Department of Medicine at Duke University School of Medicine. Pokorney is also a member of the Duke Clinical Research Institute.
Pokorney and colleagues launched the study in 2021, using Medicare data for nearly 1.1 million patients who received cardiac implantable electronic devices, or CIEDs, between 2006 and 2019.
Of those study patients, 11,619 (about 1 percent) developed infections a year or more after implantation. Only 13 percent of the patients had the device removed within six days of infection, and an additional 5 percent had them removed from day 7 to 30.
The vast majority — nearly 82 percent — were treated solely with antibiotics, despite numerous earlier studies showing antibiotics fail to wipe out infections involving CIEDs.
Those earlier studies led to a 2017 consensus of leading health organizations to recommend removal of CIEDs when a definitive infection is identified.
In the current study, the researchers found that removing the devices had a clear survival benefit. The death rate for those who did not have their devices removed was 32.4 percent in the year after an infection was diagnosed, compared with a rate of 18.5 percent among patients who underwent extraction within six days and 23.2 percent for patients who had extractions on days 7 to 30.
“Any extraction was associated with lower mortality when compared to no extraction, but the highest benefit was to those who had devices removed within six days of an infection,” Pokorney said. “This speaks to the importance of putting systems in place to identify these patients and get them quickly and appropriately treated, because delays in care result in higher mortality.”
The Duke Clinical Research Institute, with funding from Philips and leadership from Pokorney and Christopher B. Granger, MD, is acting on this data and launching a quality improvement demonstration project to address the gap in care for CIED infection patients within three health care systems in the US.
In addition to Pokorney, study authors include Lindsay Zepel, Melissa A. Greiner, Eric Black-Maier, Robert K. Lewis, Donald D. Hegland, Christopher B. Granger, Laurence M. Epstein, Roger G. Carrillo, Bruce L. Wilkoff, Chantelle Hardy and Jonathan P. Piccini.
The study received funding support from Philips, which markets devices used in CIED extraction procedures. The funder had no role in the design, implementation or publication of the study. Six study authors — Pokorney, Lewis, Epstein, Carillo, Wilkoff, and Piccini — reported ties to the company; a full disclosure is provided in the study manuscript.
ACC.22: Investigational Anti-Clotting Drug Reduces Bleeding Risk Among AF Patients
A new type of anti-clotting drug caused fewer bleeding incidents among patients with atrial fibrillation than the commonly prescribed apixaban, according to results from a head-to-head comparison of the two.
The study, led by cardiologists at Duke, was reported today as a late-breaking presentation at the 2022 American College of Cardiology Scientific Sessions being held in Washington, DC. The results were simultaneously published in the journal The Lancet.
“Anti-clotting therapy is a lifesaver for people who develop atrial fibrillation, which can increase the risk of stroke by five-fold,” said presenter and senior author Manesh Patel, MD, chief of the Division of Cardiology at Duke University School of Medicine and member of the Duke Clinical Research Institute. “But a serious complication associated with anti-clotting therapies is bleeding, leading many patients to reduce or stop taking their medications. As a result, there is great interest in alternatives that reduce this risk.”
Asundexian is a new class of anti-clotting drug that is under investigation. It works by inhibiting a blood protein called Factor XI, which contributes to the development of blood clots but is not involved in the process of healing blood vessels.
In the PACIFIC-AF trial — a phase 2 study funded by Bayer AG, which manufactures the investigative therapy — the researchers focused on bleeding outcomes arising from two different doses among patients with atrial fibrillation.
Both doses of asundexian taken once daily, 20 mg and 50 mg, were tested in comparison to similar dosages of apixaban, which is one of several commonly prescribed anti-clotting therapies that affect a different blood clotting protein.
The trial included 755 patients with an average age of about 74 years old. At both doses, patients who took asundexian had a 67-percent lower risk of bleeding compared to patients taking apixaban.
“Reducing bleeding risks for atrial fibrillation patients is encouraging,” said lead author Jonathan Piccini, MD, clinical cardiac electrophysiologist at Duke. “One in four people will develop atrial fibrillation — it’s the leading cause of heart arrhythmia and is a risk factor for stroke — so it’s important that we have safe and effective therapies. We’re eager to see the research move into phase 3 studies.”
MD, clinical cardiac electrophysiologist at Duke. “One in four people will develop atrial fibrillation — it’s the leading cause of heart arrhythmia and is a risk factor for stroke — so it’s important that we have safe and effective therapies. We’re eager to see the research move into phase 3 studies.”
In addition to Piccini and Patel, study authors include Valeria Caso, Stuart J. Connolly, Keith A.A. Fox, Jonas Oldgren, W. Schuyler Jones, Diana A. Gorog, Václav Durdil, Thomas Viethen, Christoph Neumann, Hardi Mundl, on behalf of the PACIFIC-AF Investigators.

ACC.22: Investigational Drug for Heart Failure has Little Impact on Exercise Tolerance
Heart failure patients taking the investigational drug omecamtiv mecarbil, which has been previously shown to improve long-term outcomes, see little impact on their ability to exercise compared to a placebo, according to a study supported by Duke Clinical Research Institute (DCRI).
The study was designed to test whether the new therapy — a selective cardiac myosin activator — could yield improvements in overall exercise capacity for patients with heart failure. Therapies that help heart failure patients better tolerate exercise remains an unmet need.
The findings were reported today as a late-breaking presentation at the 2022 American College of Cardiology Scientific Sessions. Circulation: Heart Failure published the study design in March 2022.
“We are fortunate to have a lot of medications in heart failure that can help patients live longer or stay out of the hospital — all very important goals,” said Duke cardiologist Michael Felker, MD, study co-chair and a member of DCRI.
“However, exercise tolerance is the main symptom patients with heart failure have,” Felker said. “They get tired or out of breath very easily. This is a major impediment for their quality of life. Unfortunately, many of the guideline-directed drugs that improve survival don’t improve exercise tolerance.”
The research study, called the Multicenter Exercise Tolerance Evaluation of Omecamtiv Mecarbil Related to Increased Contractility in Heart Failure (METEORIC-HF), recruited patients across 64 sites in nine countries. It included 276 adult heart failure patients with reduced ejection fraction; they were randomly assigned to receive the study medication or a placebo. The results were blinded to the investigators, the study sponsor, and the participants.
As its primary outcome, METEORIC-HF sought to examine the changes omecamtiv mecarbil had on peak oxygen uptake during cardiopulmonary exercise over a 20-week period. Secondary outcome measurements included assessing overall exercise capacity, ventilator efficiency, and daily activity.
“We found in the trial that even though omecamtiv mecarbil was safe and well-tolerated, it did not improve exercise tolerance over placebo,” Felker said. “I think what that tells us is finding interventions that can improve people’s exercise tolerance is still an unsolved/unmet need for our patients with heart failure. What our trial has done is helped better define what this medication does and doesn’t do.”
During the METEORIC-HF trial, study authors for the Global Approach to Lowering Adverse Cardiac Outcomes Through Improving Contractility in Heart Failure (GALACTIC-HF) trial published their own results. That trial examined outcomes between omecamtiv mecarbil and a placebo in a broad population of over 8,000 symptomatic patients. GALACTIC-HF found that omecamtiv mecarbil decreased the rate of heart failure or death from cardiovascular causes.
Felker and Gregory Lewis, MD, at Massachusetts General Hospital, co-chaired the study.
In addition to Felker and Lewis, study authors include Kieran Docherty, Adriaan Voors, Alain Cohen-Solal, Marco Metra, David Whellan, Justin Ezekowitz, Piotr Ponikowski, Michael Böhm, John Teerlink, Stephen Heitner, Stuart Kupfer, Fady Malik, and Lisa Meng.
Impressive work by all! Please note: We will have additional coverage from ACC.22 next weekend. Stay tuned! Please consider submitting photos from your ACC experience as well as information related to your presentation for inclusion in Pulse; please email your submissions to Tracey Koepke by EOB Wednesday, 4/6. Thank you!
Rymer to Host Post-ACC.22 Twitter Space
Duke Heart is collaborating with Med-IQ to conduct a Twitter Space ‘live’ on Wednesday, April 6 at 6:30 p.m. Join interventional cardiologist Dr. Jennifer Rymer for a recap of highlights from the ACC! Rymer will lead a free-flowing discussion highlighting data presented during the 2022 ACC Scientific Sessions and provide expert insight on the trials. You can follow Jenn on Twitter @jennifer_rymer. You can also follow Med-IQ (@MedIQCME).
When: Wednesday, April 6 at 6:30 p.m. ET
Where: https://twitter.com/i/spaces/1vAxRkbplgqKl
If you’re not familiar with Twitter, all you’ll need to do is visit the Twitter Space at https://twitter.com/i/spaces/1vAxRkbplgqKl and drop in. You DO NOT need a Twitter account just to listen in (simply click the link to join). You only need a Twitter account if you’d like to request to “speak” during the Twitter Space event.
If you can’t join the live space, Med-IQ will have the recording on their Facebook page (https://www.facebook.com/MedIQCME) later next week.
We’re looking forward to this and hope you’ll join us!
Karra & Team Score Grant Funding to Explore Sarcoidosis
 Congratulations to Ravi Karra, MD, MHS, and team — they were recently notified that their project, Epithelioid Mechanisms of Sarcoidosis, has been selected for award funding by the Ann Theodore Foundation Breakthrough Sarcoidosis Initiative, supported by the Ann Theodore Foundation.
Congratulations to Ravi Karra, MD, MHS, and team — they were recently notified that their project, Epithelioid Mechanisms of Sarcoidosis, has been selected for award funding by the Ann Theodore Foundation Breakthrough Sarcoidosis Initiative, supported by the Ann Theodore Foundation.
Sarcoidosis is a systemic disease defined by the presence of granulomas provoked by an unknown trigger. Although central to sarcoidosis, granulomas also occur in other diseases where they serve to contain bacteria or foreign materials. In prior work on infectious granulomas, David Tobin, PhD, an associate professor of Molecular Genetics and Microbiology at Duke and his team have determined that epithelioid cells, found in the granuloma interior, are responsible for the barrier function of the granuloma. Interfering with macrophage epithelioid transformation can loosen the granuloma and allow for inflammatory cells to clear the infection. Karra – who is partnering with Tobin on this project — and team hypothesize that specific targeting of epithelioid cells in sarcoidosis might similarly improve treatment responses. However, before such treatments can be developed, the biology of epithelioid cells in sarcoidosis needs to be better understood.
The goal of the Epithelioid Mechanisms of Sarcoidosis project is to identify key pathways and events that lead to the emergence of epithelioid cells. Their first aim is to use spatial RNA sequencing to profile granuloma formation following the Kveim test, the only system available to induce and follow sarcoid granulomas over time in humans. Their experiments will illuminate where and when signaling pathways are activated in different cell types during granuloma formation and provide a better understanding of how epithelioid cells form in sarcoidosis. Their second aim is to profile changes in DNA and RNA of individual circulating cells. They believe their work will identify why patients with sarcoidosis develop epithelioid cells in response to a trigger, while individuals without sarcoidosis do not.
The team hopes their project can lead to new therapeutic targets for treating sarcoidosis and new diagnostic tests for identifying sarcoidosis.
Duke Heart launched a multidisciplinary sarcoid clinic about one year ago, which has seen regular growth over time. According to Karra, the team has treated 50 sarcoid patients in the past year and are now seeing 2-3 new patients for evaluation each week and that a number of our cardiology fellows have been involved in the work, including Kelly Arps, MD, who will be presenting on arrhythmia concerns related to sarcoid during our next Cardiology Grand Rounds on Tuesday, April 5 (Webex link included in events listing, below).
Congratulations to Ravi and our sarcoid team — this is excellent news!
Shout-out to Barnes, Dimsdale!
The North Carolina Nurses Association held its annual Nurse Practitioner Spring Symposium in Asheville, NC from March 20-23. Presenters from Duke Heart included Stephanie Barnes and Allison Dimsdale.
Way to go!!!


In Memoriam: Kelly Ann Machovec, MD, MPH, Peds Cardiac Anesthesiologist
It is with deep sadness that we share the news of the passing of our colleague, Kelly Ann Machovec, MD, MPH, a pediatric cardiac anesthesiologist and team member with the Duke Pediatric and Congenital Heart Center. She passed away on March 30 at the age of 43.
She will be remembered as an exceptional academician and physician who dedicated her career to improving the lives of children undergoing cardiothoracic or vascular surgery, and for her special impact that was palpable to her colleagues and patients throughout the Duke Children’s Heart Center.
Originally from Baltimore, Maryland, Machovec received her Master of Public Health degree in 2005 and her Doctor of Medicine degree in 2006, both at the University of North Carolina. She went on to complete a residency in anesthesiology at Drexel University College of Medicine in Philadelphia and a fellowship in pediatric anesthesiology at Duke University School of Medicine. In 2013, Dr. Machovec joined Duke Anesthesiology faculty as an assistant professor of anesthesiology; she was appointed an associate professor of anesthesiology in 2019. She was an accomplished pediatric anesthesiologist whose research primarily focused on the hemostasis management of children following open heart surgery performed on cardiopulmonary bypass.
Earlier this year she received the Duke Pediatric and Congenital Heart Center Impact Award, recognizing her exceptional impact on the clinical practice around hemostasis, on both local and national levels. She was a fierce advocate for child-centered health care policies and always questioned the status quo. For example, she led the charge to discontinue preoperative blood testing in children to prevent them from having unnecessary painful blood draws in the preoperative clinic.
Dr. Machovec’s excellence and research led to her invitation to write the book chapter on “Anesthesia for Pediatric Cardiac Surgery” in Miller’s Anesthesia textbook. In 2015, she co-founded the Hemostasis Interest Group, a committee within the Congenital Cardiac Anesthesia Society which she served on for six years as committee chair, member and mentor; she also served as an at-large member on the Board of Directors of the Congenital Cardiac Anesthesia Society. Dr. Machovec was a passionate educator, serving as chair of the Clinical Competency Committee for Duke’s Pediatric Anesthesiology Fellowship and as a question writer and committee member for the American Board of Anesthesiology’s Pediatric Maintenance of Certification.
In addition to being an outstanding clinician and a dedicated educator, she was recognized with the high honor of the Leonard Tow Humanism in Medicine Award at the Duke University School of Medicine in March of this year. Recipients of this distinguished award are recognized as exemplars of humanism in the care of their patients, their compassionate delivery of care and respectfulness given to their patients and health care colleagues, as well as for their clinical excellence.
Beyond her career, Dr. Machovec advocated and raised funds for basic science research. From 2013-2017, she also advocated for pediatric health care on a global scale by taking part in medical missions in India, the Philippines and Haiti for Operation Smile, which helps children with cleft lip and cleft palate, and Gift of Life International, which provides lifesaving cardiac treatment to children in need from developing countries.
When introduced by Dr. Edmund Jooste prior to her delivery of Duke Anesthesiology Grand Rounds last year, Dr. Machovec was described as having “the determination of Ruth Bader Ginsberg, the curiosity of Marie Curie and fierceness of Wonder Woman” and these are the qualities that her work family loved and admired in her. She was also described as funny, strong-willed and energetic, and a dedicated team member who will be deeply missed by her pediatric anesthesiology colleagues and all of her interprofessional friends and colleagues within Duke Anesthesiology and the Pediatric Heart Center.
To preserve Dr. Machovec’s legacy at Duke, the Department of Anesthesiology has formally established the Kelly Machovec Humanism Award. The recipient of this annual departmental award will exemplify grace and compassion in their delivery of patient-centered care, reverence for patients, their loved ones and colleagues, ethical principles, and a continuous commitment to clinical excellence.
Most importantly, Dr. Machovec’s legacy will live on through her family. She was a dedicated and loving wife to her husband, Scott Matthews, and proud mother to her three young daughters, Vivienne, Eva and Caroline. Her loved ones will remember her as an engaged, talented and powerful woman with unwavering passion and optimism, who loved spending time with her family and friends, running, practicing yoga, reading, and baking.
A Celebration of Life will be held on Monday, April 11 from 5:00 – 8:00 p.m. at the Rigmor House, 5501 NC Highway 54, in Chapel Hill. All are welcome to attend. The family kindly requests that if you do plan to attend, please respond via this link for catering purposes.
We extend our deep condolences to Dr. Machovec’s family, friends and colleagues. Duke flags were lowered on Friday in honor of her life and legacy. They will remain lowered through Monday. At the request of her family, in lieu of flowers, memorial gifts may be made in her name to the Dana-Farber Cancer Institute.
COVID-19 Updates
All the latest Clinical Operations updates related to COVID can be found at https://covid-19.dukehealth.org.
Upcoming Events & Opportunities
Cardiology Grand Rounds
April 5: Cardiac Sarcoidosis: Updates and Contemporary Challenges with Kelly Arps. 5 p.m. via Webex.
Duke Heart CME
April 23: Duke Sports Cardiology & Sudden Death in Athletes Symposium with course directors Jim Daubert and Bill Kraus. Virtual. For information or to register, contact Christy Darnell christy.darnell@duke.edu or 919-880-8686.
Marfan NC Walk for Victory, April 23
The North Carolina Walk for Victory to support Marfan patients and their families will take place on Saturday, April 23, 2022 from Noon to 3 p.m. at Laurel Hills Park on Edwards Mill Road in Raleigh. Duke Heart is proud to serve as the presenting sponsor and we are excited for Chad Hughes, MD to serve as medical chair for the walk.
Please help us support all Marfan families as well as those with Loeys-Dietz (LDS), Vascular Ehlers-Danlos (VEDS), and related conditions. Donate or come join us!
Walk for Victory is The Marfan Foundation’s global walk program. The event is low-key, fun and family-oriented. To learn more or to register for this event, please visit: https://give.marfan.org/event/2022-north-carolina-walk-for-victory/e353032.
To learn more about The Marfan Foundation, please visit marfan.org.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
March 17 — Pamela Douglas
Medscape
ACC Looks to Build Inclusive, Bully-Free Cardiology Workplaces
https://duke.is/zrp29
March 19 — Adrian Hernandez
The Western Journal
https://duke.is/v2tjr
March 22 – Joseph Turek, Mary Louise Markert and Allan Kirk
Medical News Today
Novel heart-thymus transplant technique may spell end of lifelong drugs
https://duke.is/ydzhp
March 24 — Nishant Shah
Cardiology Advisor
Mean Monthly BP Increased Among US Adults During COVID-19
https://duke.is/j7q7j
March 27 — Renato Lopes
Healio/Cardiology Today
Alirocumab does not impact AF risk after ACS
https://duke.is/wffkg
March 29 — Duke University/Duke Health
Becker’s Hospital Review
Best medical schools for 2023: US News
https://duke.is/ckpuc
March 29 — Duke University/Duke Health
Becker’s Hospital Review
10 best nursing schools for master’s and DNPs, as ranked by US News
https://duke.is/bgcp8
March 30 — Joseph Turek
Nation (Kenya)
New procedure gives hope to transplant patients
https://duke.is/nb7bn
March 31 — Sunil Rao
Cardiovascular News
SCAI aims to minimise risks in medical proctoring of new techniques and technologies
https://duke.is/5jcmw
Division of Cardiology Publications Indexed in PubMed March 17-23, 2022
Blumer V, Parsons JB, Anderson DR, Bloomfield GS, Ward C. Hemophagocytic Lymphohistiocytosis Associated With Endocarditis: A Case Years in the Making. Circulation 2022 Mar 22;145(12):934-939. PM: 35312382.
Dangas G, Baber U, Sharma S, Giustino G, Sartori S, Nicolas J, Goel R, Mehta S, Cohen D, Angiolillo DJ, Zhang Z, Camaj A, Cao D, Briguori C, Dudek D, Escaned J, Huber K, Collier T, Kornowski R, Kunadian V, Moliterno DJ, Ohman EM, Weisz G, Gil R, Krucoff M. Safety and efficacy of ticagrelor monotherapy according to drug-eluting stent type: the TWILIGHT-STENT study. EuroIntervention 2022 Mar 18;17(16):1330-1339. PM: 34881696.
El-Chami MF, Bockstedt L, Longacre C, Higuera L, Stromberg K, Crossley G, Kowal RC, Piccini JP. Leadless vs. transvenous single-chamber ventricular pacing in the Micra CED study: 2-year follow-up. Eur Heart J 2022 Mar 21;43(12):1207-1215. PM: 34788416.
Fagundes A, Berg DD, Bohula EA, Baird-Zars VM, Barnett CF, Carnicelli AP, Chaudhry SP, Guo J, Keeley EC, Kenigsberg BB, Menon V, Miller PE, Newby LK, van Diepen S, Morrow DA, Katz JN. End-of-life care in the cardiac intensive care unit: a contemporary view from the Critical Care Cardiology Trials Network (CCCTN) Registry. Eur Heart J Acute Cardiovasc Care 2022 Mar 16;11(3):190-197. PM: 34986236.
Friedman DJ, Qin L, Parzynski C, Heist EK, Russo AM, Ranasinghe I, Zeitler EP, Minges KE, Akar JG, Freeman JV, Curtis JP, Al-Khatib SM. Longitudinal Outcomes of Subcutaneous or Transvenous Implantable Cardioverter-Defibrillators in Older Patients. J Am Coll Cardiol 2022 Mar 22;79(11):1050-1059. PM: 35300816.
Gallagher EJ, Rockey DC, Kontos CD, Vyas JM, Brass LF, Hu PJ, Isales CM, Ajijola OA, Rathmell WK, Conlin PR, Baiocchi RA, Kazmierczak BI, Akabas MH, Williams CS. Pearls of wisdom for aspiring physician-scientist residency applicants and program directors. JCI Insight 2022 Mar 22;7(6):10.1172/jci.insight.158467. PM: 35315364.
Gulati M, Korn RM, Wood MJ, Sarma A, Douglas PS, Singh T, Merz NB, Lee J, Mehran R, Andrews OA, Williams JC. Childbearing Among Women Cardiologists: The Interface of Experience, Impact, and the Law. J Am Coll Cardiol 2022 Mar 22;79(11):1076-1087. PM: 35300820.
Haeusler KG, Eichner FA, Heuschmann PU, Fiebach JB, Engelhorn T, Blank B, Callans D, Elvan A, Grimaldi M, Hansen J, Hindricks G, Al-Khalidi HR, Mont L, Nielsen JC, Piccini JP, Schotten U, Themistoclakis S, Vijgen J, Di Biase L, Kirchhof P. MRI-Detected Brain Lesions and Cognitive Function in Patients With Atrial Fibrillation Undergoing Left Atrial Catheter Ablation in the Randomized AXAFA-AFNET 5 Trial. Circulation 2022 Mar 22;145(12):906-915. PM: 35135308.
Mansour M, Radaideh Q, Alaiwah MN, Alnimer Y, Devabhaktuni SR, Dhar G, Vallurupalli S, Michos ED, Newby DE, Williams MC, Fudim M, Al’Aref SJ. Major adverse cardiac events in symptomatic women with non-obstructive CAD on coronary CTA: pooled analysis from PROMISE and SCOT-HEART. Int J Cardiovasc Imaging 2022 Mar;38(3):683-693. PM: 34628593.
Parker DC, Wan M, Lohman K, Hou L, Nguyen AT, Ding J, Bertoni A, Shea S, Burke GL, Jacobs DR, Post W, Corcoran D, Hoeschele I, Parks JS, Liu Y. Monocyte miRNAs Are Associated With Type 2 Diabetes. Diabetes 2022 Apr 1;71(4):853-861. PM: 35073575.
Pinsker BL, Serfas JD, Krasuski RA. Burden and Impact of Arrhythmias in Repaired Tetralogy of Fallot. Curr Cardiol Rep 2022 Mar;24(3):225-234. PM: 35138576.
Salah HM, Minhas AMK, Khan MS, Khan SU, Ambrosy AP, Blumer V, Vaduganathan M, Greene SJ, Pandey A, Fudim M. Trends and characteristics of hospitalizations for heart failure in the United States from 2004 to 2018. ESC Heart Fail 2022 Apr;9(2):947-952. PM: 35098700.
Usman MS, Khan MS, Fonarow GC, Greene SJ, Friede T, Vaduganathan M, Filippatos G, Coats AJS, Anker SD, Butler J. Robustness of outcomes in trials evaluating sodium-glucose co-transporter 2 inhibitors for heart failure. ESC Heart Fail 2022 Apr;9(2):885-893. PM: 35029056.
Voors AA, Angermann CE, Teerlink JR, Collins SP, Kosiborod M, Biegus J, Ferreira JP, Nassif ME, Psotka MA, Tromp J, Borleffs CJW, Ma C, Comin-Colet J, Fu M, Janssens SP, Kiss RG, Mentz RJ, Sakata Y, Schirmer H, Schou M, Schulze PC, Spinarova L, Volterrani. The SGLT2 inhibitor empagliflozin in patients hospitalized for acute heart failure: a multinational randomized trial. Nat Med 2022 Mar;28(3):568-574. PM: 35228754.
Zheng K, Smith JS, Eiger DS, Warman A, Choi I, Honeycutt CC, Boldizsar N, Gundry JN, Pack TF, Inoue A, Caron MG, Rajagopal S. Biased agonists of the chemokine receptor CXCR3 differentially signal through Gα:β-arrestin complexes. Sci Signal 2022 Mar 22;15(726):eabg5203. PM: 35316095.
Division of Cardiology Publications Indexed in PubMed March24-30, 2022
Alexander JH. Equipoise in Clinical Trials: Enough Uncertainty in Whose Opinion? Circulation 2022 Mar 29;145(13):943-945. PM: 35344405.
Elgendy IY, Wegermann ZK, Li S, Mahtta D, Grau-Sepulveda M, Smilowitz NR, Gulati M, Garratt KN, Wang TY, Jneid H. Sex Differences in Management and Outcomes of Acute Myocardial Infarction Patients Presenting With Cardiogenic Shock. JACC Cardiovasc Interv 2022 Mar 28;15(6):642-652. PM: 35331456.
Komisarow JM, Toro C, Curley J, Mills B, Cho C, Simo GM, Vavilala MS, Laskowitz DT, James ML, Mathew JP, Hernandez A, Sampson J, Ohnuma T, Krishnamoorthy V. Utilization of Brain Tissue Oxygenation Monitoring and Association with Mortality Following Severe Traumatic Brain Injury. Neurocrit Care 2022 Apr;36(2):350-356. PM: 34845596.
Rao SV. RESPONSE: Navigating the Transition From Fellowship to Early Career: “Sink or Swim” to “Lifting All Boats”. J Am Coll Cardiol 2022 Mar 29;79(12):1218-1219. PM: 35331418.
Xian Y, Xu H, Smith EE, Saver JL, Reeves MJ, Bhatt DL, Hernandez AF, Peterson ED, Schwamm LH, Fonarow GC. Achieving More Rapid Door-to-Needle Times and Improved Outcomes in Acute Ischemic Stroke in a Nationwide Quality Improvement Intervention. Stroke 2022 Apr;53(4):1328-1338. PM: 34802250.
