Home » 2021 (Page 3)
Yearly Archives: 2021
Duke Heart Pulse week ending July25th 2021
Highlights of the week:
Duke CTS among Top 20 for TSF Funding
The Thoracic Surgery Foundation (TSF) this week announced its “Top 20” Institutional Honor Roll for 2021. Duke University’s Cardiovascular & Thoracic surgical team ranked at #18 with a total of $365,000 in grant funding received.
TSF, which is the charitable arm of The Society of Thoracic Surgeons (STS), provides awards for cardiothoracic surgery research, education, leadership, and surgical outreach in underserved patients. So far in 2021, the Foundation has distributed $861,870 in awards and scholarships. The Foundation plans to award additional grants later in the year.
“Pursuit of the academic mission is deeply entrenched throughout the fabric of this institution,” said Edward P. Chen, MD, chief of Duke’s Division of Cardiovascular and Thoracic Surgery. “Being in the TSF Top 20 Institutional Honor Roll is reflective of not only our Division’s longstanding commitment to scientific discovery and academic development, but is also a testament to the longevity of this commitment.”
The TSF “Top 20” most funded institutions since 1993 are:
#1 University of Pittsburgh
#2 University of Pennsylvania
#3 Washington University
#4 University of California San Francisco
#5 Johns Hopkins Hospital
#6 University of Virginia
#7 University of Washington
#8 Tie – University of California Los Angeles
#8 Tie – Stanford University
#10 University of Michigan
#11 Massachusetts General Hospital
#12 Brigham and Women’s Hospital
#13 University of Toronto
#14 University of Colorado
#15 Baylor College of Medicine
#16 Medical College of Wisconsin
#17 University of Cincinnati
#18 Duke University
#19 Roswell Park Cancer Center
#20 Northwestern Memorial Hospital
“We congratulate each of these institutions for achieving TSF Top 20 Honor Roll status. This status signals the strength of their cardiothoracic surgery programs, faculty, and staff,” said TSF President Joseph E. Bavaria, MD. “Each TSF funding application is thoroughly analyzed and scored by rigorous peer review, without bias or conflict of interest. The TSF Research Committee is composed of more than 46 appointed surgeon-scientist leaders who are actively practicing at medical institutions across the U.S. and Canada. The contributions of award recipients at these Top 20 institutions to cardiothoracic surgery and our patients is significant.”
The Foundation’s 2022 Award cycle launched on July 1, 2021. TSF welcomes applications from qualified cardiothoracic surgeons and residents, employed at any institution with a cardiothoracic surgery program. Award offerings and applications can be accessed at www.thoracicsurgeryfoundation.org/awards. The deadline for most TSF Award applications is September 15, 2021.
Congratulations to all members of our Division of Cardiovascular and Thoracic Surgery on this great accomplishment!
Blumer Selected as Laennec Finalist
 Vanessa Blumer, MD, has been selected by the American Heart Association’s Council on Clinical Cardiology (CLCD) as a finalist for the 2021 Laennec Fellow in Training (FIT) Clinician Award Competition!
Vanessa Blumer, MD, has been selected by the American Heart Association’s Council on Clinical Cardiology (CLCD) as a finalist for the 2021 Laennec Fellow in Training (FIT) Clinician Award Competition!
The Laennec FIT Clinician Award recognizes the importance of clinical acumen, inductive analytic skills, and teaching ability in future academic cardiologists; it is a highly competitive award category.
Blumer, a third year fellow in our cardiovascular disease fellowship program, will present her abstract, A Challenging Case of Endocarditis — Multi-Disciplinary Approach is an Achievable Chimera during the Laennec FIT Award Competition Session at the upcoming AHA Scientific Sessions scheduled for November 13-15, 2021, in Boston, MA.
Outstanding! Congratulations, Vanessa!
Kudos to Yankey!
This week, we received the following note regarding excellent care and attention provided by Sipa Yankey and team to a patient and their family members at the Durham VAMC.
and their family members at the Durham VAMC.
“Dr. Rao,
This email is to let you know my husband’s comments concerning Doctor Yankey’s diagnosis and treatment for him in Durham VA hospital.
[He] has not been feeling well for some time now and I had been trying to get him to a heart doctor. Once he visited the VA in Salisbury to see Doctor Card, she immediately scheduled him to be seen and treated in Durham. Once we arrived at Durham VA we could see the great care offered to all veterans. The staff is so very professional and caring, especially Doctor Yankey. He installed a stent in the LAD in [my husband’s] heart which was 99 percent blocked. He SAVED his life! And he was so calm as he explained, in detail, what he had to do to correct his problem. He had a nurse by the name of Kim, not sure of last name, but she was excellent also and very detailed on explaining what all the steps would be to give comfort to my wife and daughters. She took the time to answer questions as also Doctor Yankey did to our daughter that is a registered nurse. Kim has a husband that also worked in one of the areas that called to check on him when he arrived home. What great staff and so caring.
We realize you may not always get appreciation shown for your staff. We feel it is important to let you know that with God’s help and the great knowledge and skills that Doctor Yankey has is what saved [my husband]’s life.
Doctor Yankey diagnosed and operated on [my husband] and did an excellent job! How do you thank someone that saves your life?
Again, we both wanted to show appreciation for the care and expert skills that you provide to our veterans who protect our country.
Thank you.” — Name withheld to protect patient privacy
Way to go, Sipa!
Duke Raleigh Hospital Names New President
 Barbara Griffith, MD, will be returning to Duke Health to become president of Duke Raleigh Hospital.
Barbara Griffith, MD, will be returning to Duke Health to become president of Duke Raleigh Hospital.
Griffith, who currently serves as president and chief executive officer of Woman’s Hospital in Baton Rouge, La., had previously been at Duke Regional Hospital as Chief Medical Officer and president and chief financial officer of Durham Emergency Physicians, the medical practice within Duke Regional Hospital’s emergency department.
“Duke Health and North Carolina have always been home,” Griffith said. “It is such a privilege to join the amazing team at Duke Raleigh Hospital when it is growing its footprint in Wake County and opening a beautiful new bed tower, the South Pavilion. I am thrilled that I will soon be a part of it.”
Griffith received her medical degree at the University of North Carolina at Chapel Hill. She is board certified in emergency medicine and has received training in executive health care education at the Wharton School of Business.
“Dr. Griffith joins us at a critical time when the health system is growing to deliver care to the many thousands of patients who seek out the quality care that we provide,” said William J. Fulkerson, Jr., MD, executive vice president of Duke University Health System. “Her experience as a leader in safety and quality and as a highly regarded physician whom our providers and staff trust make her a remarkable fit for this role.”
During the year-long recruitment process, Leigh Bleecker served as interim president of Duke Raleigh Hospital and will return to her role as chief financial officer.
REMINDER: Change Passwords to Comply with New Policy
Duke Health users and sponsored guests must update passwords as soon as possible, but will not be required to change passwords in the future – unless you want to update it or your password is compromised.
The new password policy removes the requirement to update passwords every 180 days and requires passwords to be at least 12 characters (special characters and numbers are no longer required); however, including special characters creates a stronger password. In addition, the option to update passwords using CTRL+ALT+DEL is no longer available.
Team members can update their passwords now, but will receive a notice from DHTS via email that requires passwords to be changed by a deadline. Please visit the OIT Account Self Service Portal and create a new NetID password that doesn’t expire.
Tip: If working remotely (at a non-Duke site) users should connect to the Duke Virtual Private Network (VPN) before updating passwords (see page 29 of the Technology Toolkit for more information about the VPN). Passwords can be updated without connecting to the VPN, but passwords are synced across all your Duke log-ins faster if connected to the VPN.
Visit https://security.duke.edu/news-alerts/new-password-policy to review the password policy FAQ.
Attention Omnicell Users
Due to Omnicell’s password policy, Duke Health employees that use Omnicell, with the exception of Duke Raleigh Hospital employees, must keep passwords to 15 characters or less; Duke Raleigh Hospital employees must keep passwords to a maximum of 30 characters.
We are working with Omnicell to upgrade their password policy to remove restrictions across Duke Health. Check the password policy information page for updates.
Contact the Duke Health Service Desk at (919) 684-2243 for technical support.
If you have not yet updated your passcode to fit this policy, please do so as soon as possible. Thank you!
Upcoming Events/Opportunities
Conversations with Colleagues expands offerings
The Conversations with Colleagues program has changed the way we talk with one another about tough topics like COVID-19 and racial justice. Now the team is adding two additional timely topics to the mix, as well as opening up another cohort of their highly popular extended series that takes a deeper dive into racial justice. Deeper Dive and Returning to the Workplace are open to all Duke Health team members, while The Social Side of Medicine is for clinical professionals and PFAC members. Learn more and sign up below.
Racial Justice: Deeper Dive
This six-week transformative experience explores the origins of systemic racism and helps participants understand their own implicit biases and what they can do to have a positive impact on our local community. The curriculum includes mixed media to engage all learning styles. Because this is a cohort-based experience based on building relationships, we ask that attendees commit to all six weeks of the series. You will select a day and time that works for you and will be expected to attend all six sessions on that set day. Sign up for a cohort to start in August:
Wednesdays from 8-9am
https://duke.zoom.us/meeting/register/tJYtfu2oqDIpHtMLUx6L2EZim8Ldd1RjOiaC
Fridays from 12-1pm
https://duke.zoom.us/meeting/register/tJwvceyvqz4qHdLjVhx-HDSt6_Aj835UDN_1
New Topic: Returning to the Workplace
Many teams are transitioning back to the office after a long period of working from home. As with any change, this transition can invoke a flurry of different emotions. Your CwC friends are here to talk through this transition with you. Please join us at any of the sessions listed below. Sign up here: https://bit.ly/dukecwc
Wednesday 8/11 8 a.m.
Wednesday 8/11 12 noon
Friday 8/13 at 12 noon
For Clinical Professionals and PFAC Council Members: The Social Side of Medicine
Patient and Family Engagement (PFE) and Conversations with Colleagues are excited to offer a different kind of conversation. We invite clinical professionals of all disciplines and Patient and Family Advisors (PFAs) who serve on one of Duke Health’s 10 Patient and Family Advisory Councils to come together and discuss the “Social Side of Medicine.” During this guided, hour-long conversation, we will explore communication between patients and clinical professionals, how we can build stronger partnerships, and how we can continually improve the quality and delivery of care. Sign up here: https://bit.ly/dukecwc
Wednesday 7/28, 6pm
Friday 7/30, 12 noon
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged.
Duke Heart in the News:
July 19 — Duke University Hospital
Healio
Top in cardiology: Next-generation artificial heart, methamphetamine-related heart failure
http://duke.is/Mn3FSY
July 20 — Carmelo Milano
Interesting Engineering
First Total Artificial Heart Successfully Transplanted In the US
http://duke.is/bSLrGq
July 20 — Carmelo Milano
Republic World
French Prosthetics Company Carmat Makes First-ever Commercial Sale Of Artificial Heart
http://duke.is/kiGytc
July 20 — Robert Califf
Infection Control Today
COVID-19 Isn’t Done with Us Yet, Medical Experts Warn
http://duke.is/VbDuxR
July 20 — Duke University Hospital
QMED New Product News
First US Implant of Carmat’s Total Artificial Heart Performed at Duke
http://duke.is/mCRfT6
*story carried in 17 other news outlets
July 20 — Stephen Greene and Muhammad Shahzeb Khan
Healio/Cardiology Today
Lung ultrasound in ED to manage acute HF confers no benefit vs. usual care
http://duke.is/gm8Ebz
July 20 — Carmelo Milano
Home Healthcare Business News
Duke implants first new generation artificial heart in North America
https://www.dotmed.com/news/story/55378
July 21 — Carmelo Milano and Jacob Schroder
Insider.com
http://duke.is/kabNC6
July 21 — Duke University Hospital
WTRF.com (Wheeling, WV)
U.S patient gets first total artificial heart implant
http://duke.is/nId6CE
July 21 — Carmelo Milano and Jacob Schroder
Plastics Today
Transatlantic Milestones for Carmat’s Total Artificial Heart
Division of Cardiology Publications Indexed in PubMed July 15-21, 2021
Amin AP, Rao SV, Seto AH, Thangam M, Bach RG, Pancholy S, Gilchrist IC, Kaul P, Shah B, Cohen MG, Gluckman TJ, Bortnick A, DeVries JT, Kulkarni H, Masoudi FA. Transradial Access for High-Risk Percutaneous Coronary Intervention: Implications of the Risk-Treatment Paradox. Circ Cardiovasc Interv. 2021;14(7):e009328. PM: 34253050.
Biering-Sørensen T, Minamisawa M, Liu J, Claggett B, Papolos AI, Felker GM, McMurray JJV, Legg JC, Malik FI, Honarpour N, Kurtz CE, Teerlink JR, Solomon SD. The effect of the cardiac myosin activator, omecamtiv mecarbil, on right ventricular structure and function in chronic systolic heart failure (COSMIC-HF). Eur J Heart Fail 2021;23(6):1052-1056. PM: 33826209.
Desai ND, O’Brien SM, Cohen DJ, Carroll J, Vemulapalli S, Arnold SV, Forrest JK, Thourani VH, Kirtane AJ, O’Neil B, Manandhar P, Shahian DM, Badhwar V, Bavaria JE. Composite Metric for Benchmarking Site Performance in Transcatheter Aortic Valve Replacement: Results From the STS/ACC TVT Registry. Circulation 2021;144(3):186-194. PM: 33947202.
Gilotra NA, Pamboukian SV, Mountis M, Robinson SW, Kittleson M, Shah KB, Forde-McLean RC, Haas DC, Horstmanshof DA, Jorde UP, Russell SD, Taddei-Peters WC, Jeffries N, Khalatbari S, Spino CA, Richards B, Yosef M, Mann DL, Stewart GC, Aaronson KD, Grady KL. Caregiver Health-Related Quality of Life, Burden, and Patient Outcomes in Ambulatory Advanced Heart Failure: A Report From REVIVAL. J Am Heart Assoc 2021;10(14):e019901. PM: 34250813.
Giroux NS, Ding S, McClain MT, Burke TW, Petzold E, Chung HA, Palomino GR, Wang E, Xi R, Bose S, Rotstein T, Nicholson BP, Chen T, Henao R, Sempowski GD, Denny TN, Ko ER, Ginsburg GS, Kraft BD, Tsalik EL, Woods CW, Shen X. Chromatin remodeling in peripheral blood cells reflects COVID-19 symptom severity. bioRxiv 2020:2020.12.04.412155. PM: 33300002.
Goldsweig AM, Povsic TJ. Complex Percutaneous Coronary Intervention: Discrete Entity or Just Another Subgroup to Analyze? Circ Cardiovasc Interv 2021;14(7):e010891. PM: 34130479.
Haga SB, Mills R, Moaddeb J, Liu Y, Voora D. Delivery of Pharmacogenetic Testing with or without Medication Therapy Management in a Community Pharmacy Setting. Pharmgenomics Pers Med 2021;14:785-796. PM: 34276225.
Hiatt WR, Hess CN, Bonaca MP, Kavanagh S, Patel MR, Baumgartner I, Berger JS, Blomster JI, Jones WS, Katona BG, Mahaffey KW, Norgren L, Rockhold FW, Fowkes FGR. Ankle-Brachial Index for Risk Stratification in Patients With Symptomatic Peripheral Artery Disease With and Without Prior Lower Extremity Revascularization: Observations From the EUCLID Trial. Circ Cardiovasc Interv 2021;14(7):e009871. PM: 34253048.
Jering KS, Claggett B, Pfeffer MA, Granger C, Køber L, Lewis EF, Maggioni AP, Mann D, McMurray JJV, Rouleau JL, Solomon SD, Steg PG, van der Meer P, Wernsing M, Carter K, Guo W, Zhou Y, Lefkowitz M, Gong J, Wang Y, Merkely B, Macin SM, Shah U, Nicolau JC, Braunwald E. Prospective ARNI vs. ACE inhibitor trial to DetermIne Superiority in reducing heart failure Events after Myocardial Infarction (PARADISE-MI): design and baseline characteristics. Eur J Heart Fail 2021;23(6):1040-1048. PM: 33847047.
Khan MS, Fonarow GC, Greene SJ. Sodium-glucose co-transporter 2 inhibitors for heart failure: clinical trial efficacy and clinical practice effectiveness. Eur J Heart Fail 2021;23(6):1023-1025. PM: 33779013.
Khan MS, Sreenivasan J, Shahid I, Bhinder J, Fudim M, Greene SJ, Butler J. Trends in Substance Abuse Disorders Among Patients Hospitalized for Heart Failure in the United States. Circ Heart Fail 2021;14(7):e008147. PM: 34233481.
Kitzman DW, Whellan DJ, Duncan P, Pastva AM, Mentz RJ, Reeves GR, Nelson MB, Chen H, Upadhya B, Reed SD, Espeland MA, Hewston L, O’Connor CM. Physical Rehabilitation for Older Patients Hospitalized for Heart Failure. N Engl J Med 2021;385(3):203-216. PM: 33999544.
Kochar A, Summers MB, Benziger CP, Marquis- Gravel G, DeWalt DA, Pepine CJ, Gupta K, Bradley SM, Dodson JA, Lampert BC, Robertson H, Polonsky TS, Jones WS, Effron MB. Clinician engagement in the ADAPTABLE (Aspirin Dosing: A Patient-centric Trial Assessing Benefits and Long-Term Effectiveness) trial. Clin Trials 2021;18(4):449-456. PM: 33541120.
Matos JD, McIlvaine S, Grau-Sepulveda M, Jawitz OK, Brennan JM, Khabbaz KR, Sellke FW, Yeh R, Zimetbaum P. Anticoagulation and amiodarone for new atrial fibrillation after coronary artery bypass grafting: Prescription patterns and 30-day outcomes in the United States and Canada. J Thorac Cardiovasc Surg 2021;162(2):616-624. PM: 32197901.
O’Brien EC, Raman SR, Ellis A, Hammill BG, Berdan LG, Rorick T, Janmohamed S, Lampron Z, Hernandez AF, Curtis LH. The use of electronic health records for recruitment in clinical trials: a mixed methods analysis of the Harmony Outcomes Electronic Health Record Ancillary Study. Trials 2021;22(1):465. PM: 34281607.
Rao VN, Bush CG, Mongraw-Chaffin M, Hall ME, Clark D, Fudim M, Correa A, Hammill BG, O’Brien E, Min YI, Mentz RJ. Regional Adiposity and Risk of Heart Failure and Mortality: The Jackson Heart Study. J Am Heart Assoc 2021;10(14):e020920. PM: 34238024.
Roe MT, Patrick-Lake B, von Eschenbach AC. Post-COVID-19 Syndrome: Leveraging the Patient Perspective and Technological Innovations to Enable the Delineation of Effective Treatments. Drugs 2021;81(10):1235-1237. PM: 34132992.
Duke Heart Pulse Week ending 7-18-2021
Highlights of the week:
New Generation Artificial Heart Implanted in Patient at Duke – First in U.S.

A surgical team at Duke University Hospital, led by Drs. Jacob Schroder and Carmelo Milano, successfully implanted a new-generation artificial heart in a 39-year-old man with heart failure, becoming the first center in North America to perform the procedure.


The artificial heart was developed by CARMAT and has been studied in Europe, where it is approved for use. Last year, the company received FDA approval to begin studies in the U.S. to potentially enroll 10 patients with end-stage bi-ventricular heart failure. The study will evaluate whether the artificial heart is a viable option as a life-saving step before transplant.
“We are encouraged that our patient is doing so well after the procedure Monday,” said Milano, a transplant surgeon and the principal investigator of the device study at Duke. “As we evaluate this device, we are both excited and hopeful that patients who otherwise have few to no options could have a lifeline.”
The Duke patient, Matthew Moore, is from Shallotte, N.C., and was referred to Duke in June after a sudden, unexpected diagnosis of heart failure. Moore and his wife, Rachel, recently adopted their two-year-old foster son, Marshall, and arrived at Duke expecting only to undergo heart bypass surgery.
As Moore’s condition quickly deteriorated, however, traditional options, including transplant, became too risky. Meanwhile, Duke was among just three transplant centers in the United States selected to join the device study, and the procedure team received specialized training to prepare for the implant surgery.
“As a nurse, I understand how important it is to bring these advancements forward,” Rachel Moore said. “Both Matthew and I are so grateful that we’ve been provided an opportunity to participate in something that has the potential to have an impact on so many lives. We are just taking it day-by-day and hope everything continues to progress well.”
The artificial heart developed by CARMAT is an implantable prosthetic that includes biological valves derived from bovine tissue. It operates on an external power supply.
If the device receives FDA approval, it would provide a bridge to transplant for patients whose hearts require assistance to pump blood through both chambers. Current technology – notably a left-ventricular assist device (LVAD) — supports just one chamber.
“Because of the shortages of donor hearts, many patients die while waiting for a heart transplant,” said Schroder, a transplant surgeon who led the implant procedure. “We are hopeful for new options to help these patients, many like Mr. Moore who have devastating disease and cannot otherwise be considered for a transplant.”
Manesh Patel, M.D., chief of the Division of Cardiology in Duke’s Department of Medicine, said the heart care program at Duke has fostered a culture of innovation over decades, aimed at improving care for patients.
“Our goal is to both deliver the best health care and to play a role in discovering it,” Patel said. “Innovation is essential for this. Patients locally and nationally are seen by our heart transplant team for care they may not get elsewhere. The key is the culture of innovation and the teamwork between our cardiac surgeons, heart failure cardiologists, nurses and all the heart center staff that care for our patients.”

Dr. Jason Katz, co-director of Duke’s Mechanical Circulatory Support Program and co-PI on the CARMAT trial agrees, “This is another example of multidisciplinary collaborative innovation for our advanced heart failure patients and speaks to how important innovation of patient care is to the entire team. It’s the first of what I hope will be many innovative options for this high risk patient population.”
Clinical research nurse coordinator for the trial, Frank Benedetti added, “A million things had to happen over the past several weeks, but all the pieces fell in line. When I got the call that the patient was out of the OR and had done well, I teared up with joy. It was such a proud moment to see all of our hard work come together and really pay off for this patient – I am so proud of our whole team.”
“The successful implant of the CARMAT artificial heart represents the latest in a long list of accomplishments by the Duke heart transplant team aimed at further expanding the treatment options available for patients with end-stage cardiac disease,” said Edward P. Chen, M.D., chief of the Division of Cardiovascular and Thoracic Surgery in Duke’s Department of Surgery.
Many thanks to our cardiothoracic surgical team led by Drs. Jacob Schroder and Carmelo Milano; to our Cardiac

Anesthesiology team members, Drs. Sharon McCartney, Alina Nicoara, Meredith Whitacre and Mihai Podgoreanu; all of our VAD coordinators, Laura Blue, Kevin Cox, Catherine Shuford, Dakota Bentz; our perfusion team; the entire nursing staff of the CTICU and clinical stepdown unit teams, including the Advance Practice Providers who are getting very familiar with a device that no other APP team in the U.S. is familiar with; and our Clinical Research Team, especially our clinical research nurse coordinator Frank Benedetti, “who was asked to do a lot on a very short timeline and came through with flying colors,” said Katz. We also thank the CICU who help care for the patient during his course of illness and kept him stable and supported to get to the CT surgical team.
Benedetti acknowledged the help of dozens of people including Robyn Osborne, laboratory manager at Substrate Services Core Research Support team in the Department of Surgery; Susan Churchill with the Multi-Dimensional Image Processing Laboratory in Duke Radiology, Brian Gore with Duke University Hospital Clinical Engineering; Diane Pinder, a fellow clinical research nurse coordinator, and Clancy Leahy, research project manager with SOCR.
A Duke press conference to discuss the device was held on Thursday afternoon. A link to the recording can be found here: https://youtu.be/GAI22Y6ksjo.
Shout-out to Barba & Team!
We received a recognition note this past week from Diane Sauro, director – Advanced Practice, for Ashley Barba and members of the patient care team.
“Ashley, see below comment from report I received from Patient Visitor Relations. The awesome, compassionate care you provide to your patients does not go unnoticed. You are a role model to your team. Thank you for everything you do for Heart patients and your team.” —Diane
“Patient complimented Dezarae, Sonya, Taylor, Kaitlyn, Samantha, Ashley and Kat. Patient stated, “They were outstanding nurses!!! They were always attentive and very responsive. They listened to me and answered all of my questions in ways that I could understand. Most importantly they always treated me as a person and not just a patient!”
Great job, everyone!
Upcoming Events/Opportunities
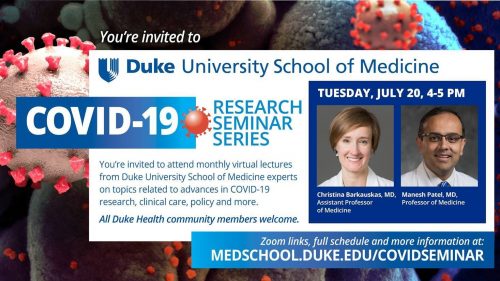
July 20: COVID-19 Research Seminar Series featuring Christina Barkauskas and Manesh Patel. 4-5 p.m. Zoom. Sponsored by Duke University School of Medicine.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged.
Duke Heart in the News:
July 9 — Duke Clinical Research Institute
Becker’s Health IT
8 hospitals, health systems that launched innovation centers in 2021
https://bit.ly/3Bea92R
July 14 — Duke University Medical Center
Rev Cycle Intelligence
Study Raises Concerns About Gender Pay Gap in Healthcare
https://bit.ly/3BgtnoE
July 15 — Carmelo Milano and Jacob Schroder
WRAL/NBC-5
Adoptive father of 2-year-old becomes first patient to get artificial heart at Duke
https://bit.ly/3BhwQTJ
July 15 — Duke University Hospital
Nuevo Periodico
La empresa francesa Carmat realiza la primera implantación humana de su corazón artificial total
https://bit.ly/3rhlIln
July 15 — Carmelo Milano and Jacob Schroder
Healio/Cardiology Today
First North American patient implanted with next-generation total artificial heart
https://bit.ly/2Ui58G6
July 15 — Carmelo Milano and Jacob Schroder
Yahoo News/Business Wire
CARMAT Announces the First Human Implant of Its Total Artificial Heart in the United States
https://yhoo.it/3rgQURE
July 15 — Duke University Hospital
The Sun
First US-based artificial heart implant for French firm
https://bit.ly/3rpRxsf
July 15 —Carmelo Milano and Jacob Schroder
Health Tech World
CARMAT bioprosthetic heart implanted
https://bit.ly/3Bf0HfG
July 15 — Adrian Hernandez and W. Schuyler Jones
Healio/Cardiology Today
ADAPTABLE points to solutions about aspirin dose, conduct of pragmatic trials
https://bit.ly/3kuhntA
Duke Heart Week Ending July 11th 2021
Highlights of the week:
EXACT Trial Launched; New Gene Therapy Option for Refractory Angina, CAD Patients
EXACT, a first-in-human clinical trial examining the safety and efficacy of using an adenoviral vector to more efficiently deliver human vascular endothelial growth factor (VEGF) directly into the myocardium with the goal of stimulating angiogenesis in patients suffering from refractory angina due to advanced coronary artery disease (CAD), has launched at Duke. Investigators on the trial include E. Magnus Ohman, Thomas Povsic (serving as site and national PI) and cardiothoracic surgeon Adam Williams.



The first treatment at Duke was performed by Williams on June 23.
“This is a very exciting time – this trial is the first of its kind,” said Williams. “It has the potential to change the landscape for patients with refractory angina by providing a new therapy that has the potential to stimulate the body to grow new blood vessels in the heart.”
Patients with refractory angina due to advanced CAD are often referred to as ‘no-option’ patients, according to Ohman.
When patients are first diagnosed with CAD, the treatment approach typically involves lifestyle changes along with medications and, as the disease progresses, interventions such as angioplasty or coronary artery bypass grafting can be performed to improve blood flow throughout the heart. As CAD becomes more severe, however, medications may not be as effective and patients eventually exhaust all options for revascularization. Patients with refractory angina due to CAD have typically had prior interventions to open vessels in the heart, but can continue to experience pain or pressure in their chest due to the diffuse nature of their disease. This is an experience that can be severely debilitating, occurring on a daily basis, significantly limiting their quality of life.
“At this point, Ohman says, “there are very few options and we have been working on trying to figure out more ways to help these patients. This trial represents a significant new option for them.”
Other EXACT trial sites enrolling patients are located in OH, MN, GA and FL.
“Treatments for patients such as these are desperately needed and this is a new option offered here at Duke that is not available elsewhere in this region,” says Povsic. “This option represents a novel approach from conventional revascularization or medical therapy, and aims to address the fundamental deficit of microvascular dysfunction and lack of blood flow to the myocardium.”
According to Williams, most gene therapy trials that have been done in humans use an adeno-associated virus, but EXACT is using an adenoviral vector to deliver VEGF directly into the myocardium. This is done, he says, through a very small, minimally invasive incision to reach the heart tissue. Under direct vision, the surgeon then injects areas of the heart muscle that are known to be ischemic with the goal of stimulating new blood vessel development in that area.
Adenovirus, Williams says, has a quick onset of action – it begins within a couple of days – and after a couple of weeks, it stops expressing the VEGF. The team expects it will take 1 to 2 months post-therapy to start seeing a noticeable difference in the heart tissue.
Importantly, the team will evaluate enrolled patients using positron emission tomography (PET) scans over the course of a year. The scans will provide critical objective data as to whether the intervention is leading to increased blood supply to the ischemic areas.
The team is happy to evaluate any patients who have ongoing angina (chest pain due to coronary artery disease) for inclusion in this or other potential trials. To learn more about the EXACT Trial criteria, please visit: https://clinicaltrials.gov/ct2/show/NCT04125732. To make a referral or discuss a possible patient with a member of the team, please contact the offices of either Dr. Povsic, 919-684-1284, or Dr. Ohman, 919-681-2069, or email Dr. Povsic directly at thomas.povsic@duke.edu.
Pokorney & Duke EP Enroll 1st Patient for Extravascular ICD Trial

Congratulations to electrophysiologist Sean Pokorney and the Duke EP team – they recently became an enrolling site for the Medtronic Extravascular Implantable Cardioverter Defibrillator (EV ICD) Pivotal Study. Pokorney and team did their first implant of the investigational device on Monday, June 14th.
The clinical trial is designed to determine the safety and efficacy of using Medtronic’s investigational EV ICD system to treat patients who are at increased risk of dangerous ventricular rhythms – patients who are at increased risk for sudden cardiac death, who have an ejection fraction of 35 percent or less.
Traditional ICDs are implanted under the skin below the patient’s collarbone with electrode wires (“leads”) placed transvenously, meaning the wires are placed through a vein and into the heart, where they are attached directly into the heart muscle. The location of the leads directly inside blood vessels and heart tissue can increase the risk of blood stream infections in patients.
The EV ICD utilizes extravascular placement, meaning the leads are not placed inside the blood vessels, which eliminates the risk of blood stream infections. The device is the same size as traditional ICDs with a wire that is designed to be placed underneath the sternum and close to the heart without the need for transvenous positioning, according to Pokorney.
“This allows the device to both pace the heart and shock the heart out of ventricular tachycardia,” said Pokorney.
The EV ICD Pivotal Study is a worldwide clinical trial with 50 sites, 23 of which are based in the U.S. Duke is the only enrolling site between Washington, DC and Jacksonville, FL. To learn more about eligibility criteria, please visit: https://clinicaltrials.gov/ct2/show/NCT04060680.
Shout-out to Lindgren!
We received a recognition note this past week about Allison Lindgren, a cardiology PA on 7700. The note was sent to Rio Landa and Faith Williams by Katherine Adams, a clinical team lead for 7700, the cardiology stepdown unit at Duke University Hospital.
“Hi Rio & Faith, I wanted to take a moment to recognize Allison Lindgren. The nursing staff on 7700 submitted a recognition form for Allison for the quality care and team work that she provided from 6/21-6/23/2021. The staff members wrote this on the recognition form:
“Thank you for being someone who we can rely on. You are a great person to work with and we are so lucky to have you as a colleague”
Allison – thank you so much for all of your excellent work on the unit! We really appreciate you!” — Katherine
Way to go, Allison!
ICYMI: Duke Raleigh Hospital Opens New South Pavilion Bed Tower
Duke Raleigh Hospital celebrated the opening of its South Pavilion on Thursday, July 8, with move-in for patients expected to begin on Monday, July 12.
The nearly $196 million dollar project – which includes renovations to the hospital’s existing bed tower — is Duke Health’s largest investment in Wake County to date. The South Pavilion features 92 single-occupancy patient rooms, nine state-of-the-art operating suites and a new kitchen and café for patients and visitors.
“The newly completed South Pavilion adds space, not just for innovative care, but more room for families to be involved in the healing process during their stay,” said Leigh Bleecker, Duke Raleigh Hospital interim president. “This expansion brings us to 256 available beds in our facility — 186 licensed inpatient beds, plus 70 beds for observation and outpatient procedures. This total includes 28 ICU beds — an increase from the 15 we have today.”
The six-story South Pavilion compliments the hospital’s existing North Pavilion, which will be undergoing renovations in August to expand surgical areas, enhance the chapel and create a new corridor to link the two patient towers.
Construction on the new, 210,200-square-foot South Pavilion building began in 2018 and was designed to enhance patient and visitor experiences during their stays. Patient rooms include separate sitting areas for families, and new waiting rooms on inpatient floors overlooking Wake Forest Road.
Additionally, the new building incorporates art throughout, with a large, open lobby displaying work from local artists. The expanded café includes seating for nearly 200 guests and a menu featuring varied cuisines. An outdoor courtyard with dining areas, a tranquility garden and walking paths provides patients and visitors an opportunity to enjoy fresh air and sunshine.
With the new building and renovations in the North Pavilion, Duke Raleigh Hospital will have a new unified front entrance off Wake Forest Road in 2022.
“The building projects at Duke Raleigh Hospital – including construction of the South Pavilion bed tower and the upcoming renovations to the North Pavilion – represent the strength of our commitment to Wake County and the communities we serve,” said William Fulkerson, MD, executive vice president of Duke University Health System. “These projects are designed with careful attention to meeting the health and wellness needs of our patients, visitors and staff — both now and into the future.”
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged.
Duke Heart in the News:
July 6 — Christopher Granger, Tracy Wang and Manesh Patel
HCP Live
Christopher Granger, MD: Antithrombotic Therapy in Patients with Atrial Fibrillation
https://bit.ly/3qYo0FH
July 6 — Kevin Thomas
Medscape
CABANA: Ablation Bests Drugs for AF in Racial/Ethnic Minorities
https://www.medscape.com/viewarticle/954248
July 7 — Kevin Thomas
Physician’s Weekly
Catheter Ablation May Be Better Option for Non-White AFib Patients
https://bit.ly/2UAk8yQ
July 7 — Stephen Greene and Mohammad Shahzeb Khan
Medpage Today
HF Care in the ED Languishes Despite Congestion-Driven Treatment Strategy
https://www.medpagetoday.com/cardiology/chf/93460
July 7 — Manesh Patel
HCP Live
Manesh Patel, MD: New Therapies for Cardiovascular Risk Management
https://bit.ly/3dXCzEs
July 7 — Schuyler Jones and Tracy Wang
HCP Live
Schuyler Jones, MD: Identifying High Risk Patients for CAD/PAD
https://bit.ly/3woSjXj
July 7 — Kevin Thomas
Reuters Health/MD Alert
Ablation bests drug therapy for minorities with afib in North America
https://bit.ly/3e1RnSC
July 8 — Derek Chew and Duke Clinical Research Institute
Medscape
IV Iron Cost-Effective, Maybe Even Cost-Saving in HF With Iron Deficiency
https://www.medscape.com/viewarticle/954455
July 8 — Kevin Thomas
HealthDay News
Catheter Ablation Improves A-Fib Outcomes in Racial/Ethnic Minorities
https://bit.ly/3AGFgUF
Duke Heart Week – July 4th 2021
Highlights of the week:
Welcome New Cardiology Fellows
This week, we welcomed 10 cardiology fellows to the Duke Cardiovascular Disease fellowship. They are all incredibly talented and have accomplished so much already. We are excited to work with them, get to know them, and watch their careers unfold!
Shown L-R are: Sara Coles; Willard Applefield; Manasi Tannu; Ijeoma Eleazu; Nkiru “Kiki” Osude; Balim Senman; Ilya Shadrin; Lonnie Sullivan; M. Shahzeb Khan, and V. Mark Kittipibul.

Please give them a warm welcome when you see them!
Cardiovascular & Thoracic Surgery Residents, Fellows Celebrated
Congratulations to our incredible residents and fellows who wrapped up their training with us in May:
- Hai Viet-Nguyen Salfity, MD, MPH, Thoracic Surgery Residency Program. She is headed to the University of Cincinnati Medical School, Cincinnati, OH.
- Robert Patrick Davis, MD, Thoracic Surgery Residency Program. He is heading to Yale in New Haven, CT.
- Charles Wojnarski, MD, Thoracic Surgery Residency Program. He is heading to Virginia Mason Hospital in Seattle, WA.
- Eriberto Michel, MD, Thoracic Transplant and Advanced Cardiac Surgery Fellowship. He is headed to Massachusetts General Hospital in Boston, MA.
- John M. Trahanas, MD, Advanced Aortic and Endovascular Surgery Fellowship. He is headed to Vanderbilt Medical School of Medicine in Nashville, TN.
Shown L-R are: E. Michel; J. Trahanas; H. Salfity (front); R. Patrick Davis (rear) and C. Wojnarski; with B. Zwischenberger, associate program director; J. Haney, program director; E. Chen, division chief; B. Tong, associate program director; and P. Smith, former division chief.

We are so excited for you! Best wishes as you embark on the next phase of your careers.
Rao Appointed VISN 6 Cardiology Lead
 We are pleased to share that Sunil V. Rao, professor of medicine in cardiology at Duke and section chief of cardiology at the Durham Veterans Affairs Medical Center, has been appointed as the Cardiology Lead for the VA’s Virtual Integrated Service Network (VISN) 6!
We are pleased to share that Sunil V. Rao, professor of medicine in cardiology at Duke and section chief of cardiology at the Durham Veterans Affairs Medical Center, has been appointed as the Cardiology Lead for the VA’s Virtual Integrated Service Network (VISN) 6!
The Veterans Health Administration is the largest integrated health care system in the U.S. and is comprised of 18 VISNs. VISN 6 is the VA’s Mid-Atlantic Health Care Network, which includes 7 inpatient Veterans Affairs Medical Centers, 7 VA outpatient clinics, and 30 Community-based outpatient clinics in North Carolina and Virginia.
“It is an honor to do this work and it’s a natural progression of the work that all of us at the VA have been doing,” says Rao. “We’ve got a great team at the Durham VA and everyone is interested in increasing the level of care we’re providing.”
Cardiovascular care is a big proportion of the care the VA delivers both on an inpatient and outpatient basis, according to Rao. Because there are a lot of complexities within the scope of cardiovascular services provided, there had become a need to have someone who could serve in a coordinating role in order to improve care delivery to veterans across the VISN.
Rao credits his team at the VA and the strong partnership with Duke as the academic partner for the Durham VAMC, for their ability to provide extraordinary care to veterans.
“We’ve been able to develop treatment pathways – frequently in coordination with Duke –particularly as it relates to the things that the VA just can’t offer, like transplantation and advanced heart care therapies,” says Rao. “To serve as the cardiology lead for the VISN, for me, this is a chance to bring the work that our team at the VA has done and introduce it to a broader audience and try and make cardiology care around the entire VISN more efficient and to increase access to care for veterans.”
According to Rao, he and others within the VISN will be working to identify and address gaps in care for cardiology patients. Their goal is for patients in VISN 6 to get access to the top notch care they need in the places nearest them, and, when necessary, to more efficiently coordinate care with sites in Durham, Richmond or Asheville in the event that more advanced care is needed.
“I think for all of us, it’s really an honor to be able to serve people who have served their country and that is what keeps us dedicated to the VA,” says Rao. “I’m looking forward to seeing how we can elevate the level of care within the VA system both in NC and Virginia. I’m really looking forward to working with the entire team at the VISN level to try and do that.”
Congratulations, Sunil!
Piccini and Duke EP Launch DEFINE AFib Trial with Medtronic
Congratulations to Jon Piccini and the Duke EP team for enrolling one of the first two patients into the DEFINE AFib clinical  trial, a research study funded by Medtronic. Using data collected from Medtronic’s LINQ family of insertable cardiac monitors (ICMs), the study aims to address unanswered questions around atrial fibrillation (AF) burden and its impact on patient outcomes, quality of life, and healthcare utilization. This is the first app-based research study for Medtronic.
trial, a research study funded by Medtronic. Using data collected from Medtronic’s LINQ family of insertable cardiac monitors (ICMs), the study aims to address unanswered questions around atrial fibrillation (AF) burden and its impact on patient outcomes, quality of life, and healthcare utilization. This is the first app-based research study for Medtronic.
Piccini enrolled Duke’s first patient on June 21. A second patient was enrolled the same day at Florida Electrophysiology Associates in Atlantis, FL.
DEFINE AFib will be conducted remotely through the new Medtronic Discovery App in coordination with U.S. sites that will collectively enroll approximately 5,000 patients. Study participants will include patients age 22 or older who have a history of AF, an iPhone device (iOS version 13 or higher), and one of the LINQ family of ICMs, among other criteria. The study will incorporate both device data and patient-reported data derived from scheduled patient surveys and the HealthKit — coupled with electronic health record information about medications and previous cardiac procedures — to provide comprehensive, actionable insights. Through a machine learning approach, aggregated study data will be leveraged to enable improved AF management in the future.
“When it comes to managing atrial fibrillation, there is not a ‘one-size-fits-all’ approach, and the hope is that DEFINE AFib may give us the tools to help personalize AF management based on a patient’s individual health profile and physiology,” said Piccini, associate professor of medicine and director of electrophysiology at Duke, who is also chair of the DEFINE AFib Steering Committee. “DEFINE AFib will harness the power of digital health to make fundamental discoveries about how we can manage atrial fibrillation better in each and every one of our patients.”
Congratulations, Jon and team!
Shout-out to DeVore & Karra
We received the following note this week from our anesthesiology colleague Yuriy Bronshteyn:
“Hi, I’m an intensivist-anesthesiologist here at Duke and wanted to recognize two of your faculty for their dedication and patient-centric care:
- Adam DeVore
- Ravi Karra

Last week, a patient who lives 4+ hours away came to our anesthesia pre-op clinic anticipating surgery the next day for a slow-growing cancer. Unfortunately, her EKG showed some concerning findings so her surgeon asked that the cancer surgery by postponed pending a cardiology evaluation. The patient was distraught and asked only that her cardiology workup happen at Duke the next day since she was already staying at a local hotel overnight and that she would have difficulty returning to Duke later. At 5:30 p.m., Dr. DeVore – while wrapping up a busy clinic day – personally scoured the cardiology schedules and found a slot for the patient the next day with Dr. Karra. Dr. Karra then generously agreed to see the patient and proceeded to take excellent care of her.
Dr. DeVore and Dr. Karra went above and beyond to help a patient who was at risk of falling through the cracks of the healthcare system. And at a time when the patient was dealing with the emotional consequences of a cancelled cancer surgery. It is acts like this that make Duke an exceptional place to work and receive care.
Thank you to Dr. DeVore and Dr. Karra!” — Yuriy
We agree! Nicely done, Adam and Ravi!
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged.
Duke Heart in the News:
June 29 — L. Kristin Newby
Mirage News
https://bit.ly/3hkTL7K
June 29 — Raymond Kim
Diagnostic Imaging
Cardiac MRI Picks Up Myocarditis in Patients Fully Vaccinated for COVID-19
https://bit.ly/2TwVv5S
June 30 — Susan Dent (medical oncology)
Health Day
https://bit.ly/3hvnoDs
June 30 — Keisha Bentley-Edwards (internal medicine)
Triangle Tribune
‘Denomination matters’ in Black-focused faith-based health programs
https://bit.ly/3qRO3i4
July 1 — Han Kim
Physician’s Weekly
Covid-19: New Reports of Vaccine Linked Myocarditis
https://bit.ly/2V40Thk
Division of Cardiology Publications Indexed in PubMed June 24-30, 2021
Curtis LH, Hoffman MN, Califf RM, Hammill BG. Life expectancy and voting patterns in the 2020 U.S. presidential election. SSM Popul Health 2021;15:100840. PM: 34169139.
Hamo CE, Abdelmoneim SS, Han SY, Chandy E, Muntean C, Khan SA, Sunkesula P, Meykler M, Ramachandran V, Rosenberg E, Klem I, Sacchi TJ, Heitner JF. OUTpatient intravenous LASix Trial in reducing hospitalization for acute decompensated heart failure (OUTLAST). PLoS One 2021;16(6):e0253014. PM: 34170908.
Hoffmann U, Lu MT, Foldyna B, Zanni MV, Karady J, Taron J, Zhai BK, Burdo T, Fitch KV, Kileel EM, Williams K, Fichtenbaum CJ, Overton ET, Malvestutto C, Aberg J, Currier J, Sponseller CA, Melbourne K, Floris-Moore M, Van Dam C, Keefer MC, Koletar SL, et al. Assessment of Coronary Artery Disease With Computed Tomography Angiography and Inflammatory and Immune Activation Biomarkers Among Adults With HIV Eligible for Primary Cardiovascular Prevention. JAMA Netw Open 2021;4(6):e2114923. PM: 34185068.
Lopes RD, de Barros E Silva PGM, Furtado RHM, Macedo AVS, Ramacciotti E, Damini LP, Bronhara B, Cavalcanti AB, Rosa RG, Azevedo LCP, Veiga VC, Machado FR, Ritt LE, Martins PA, Alexander JH, Avezum A, Berwanger O, et al. Randomized clinical trial to evaluate a routine full anticoagulation Strategy in Patients with Coronavirus Infection (SARS-CoV2) admitted to hospital: Rationale and design of the ACTION (AntiCoagulaTlon cOroNavirus)-Coalition IV trial. Am Heart J 2021;238:1-11. PM: 33891907.
Malian HM, Smith PJ, Hoffman B, Jiang W, Ammerman K, Kraus WE, Hinderliter A, Sherwood A, Blumenthal JA. Effects of Acute Exercise on Anxiety Ratings in Patients With Coronary Heart Disease and Elevated Anxiety. J Cardiopulm Rehabil Prev 2021;41(4):277-281. PM: 34158457.
Singh H, Mehta RH, O’Neill W, Kapur NK, Lalonde T, Ohman M, Ghiu I, Chen-Hsing Y, Dutcheshen K, Schreiber T, Rosman H, Kaki A. Clinical features and outcomes in patients with cardiogenic shock complicating acute myocardial infarction: early vs recent experience with impella. Am Heart J 2021;238:66-74. PM: 33848505.
Vogel RF, Delewi R, Angiolillo DJ, Wilschut JM, Lemmert ME, Diletti R, van Vliet R, van der Waarden NWPL, Nuis RJ, Paradies V, Alexopoulos D, Zijlstra F, Montalescot G, Krucoff MW, van Mieghem NM, Smits PC, Vlachojannis GJ. Pharmacodynamic Effects of Pre-Hospital Administered Crushed Prasugrel in Patients With ST-Segment Elevation Myocardial Infarction. JACC Cardiovasc Interv 2021;14(12):1323-1333. PM: 34167672.
Duke Heart Week ending June 27th 2021
Chief’s message: Changing residents and fellows
Each year in July, the change of the Academic Calendar we say good bye to our graduating fellows and residents and welcome in our newly starting residents and fellows. This upcoming week holds that excitement on the clinical wards as we go into July 4th. I have always found the transition to be both bittersweet – saying by to some that have spent somewhere between 4-9 years at Duke, while embracing the excitement of teaching and workin with the next generation of medicine and cardiovascular medicine leaders. The end of the Academic year also allows for reflection on our accomplishments, and we continue that series with an update from our Interventional Labs by Schuyler Jones this week.
Highlights of the week:
Heart Highlights: Duke Interventional Cardiology
We are pleased to offer an update on our Interventional Cardiology team from Schuyler Jones as we continue to celebrate the accomplishments our team has made over the past year:
The Duke Interventional Cardiology team has continued to stay busy as we work to fulfill the tripartite mission, support Duke University Health System, and take care of ourselves, our patients, and our partners. COVID-19 was an especially challenging time in the Cath Lab, as reports from all over the world made us think differently about how we deliver care to patients with heart disease. We held true to our beliefs that we should not change how we approach patient care, and we worked diligently with our operational and nursing teams to ensure that we all had the appropriate personal protective equipment and created adjunctive processes that ensured the safety of our patients, staff, fellows, and faculty. Special thanks to Anna Mall (Clinical Lead) for her work with donning and doffing practice, training of staff, and overall coordination of care during the pandemic – there was a period when Anna was on call to come in for emergency procedures almost every night.
The Interventional Cardiology Fellowship is the life blood of our Cath Lab, and this year, the four fellows – Adam Banks, Jaidip Chakravartti, Angela Lowenstern, and Michael Nanna – really rose to the challenge. Maintaining an affable and steady approach, this team worked together to take care of some of the sickest patients in the hospital. They learned, they taught, and they did it as a team, and honestly, we couldn’t be more proud of this group as they all finish their training and move on to start their careers.
- Adam will be moving to Albuquerque, New Mexico where he will be doing coronary and structural interventional procedures alongside former Duke fellow, Sharif Halim.
- Jaidip will be starting his practice in Portland, Maine where he will be a coronary and peripheral interventionalist in a practice with former Dukie, Ed Sze.
- Angela is moving to Nashville, Tennessee where she will join the Vanderbilt University faculty and perform coronary and structural interventions.
- Finally, Mike will be moving back to New Haven, Connecticut where he did his residency and joining the Yale University faculty to focus on research and perform coronary and peripheral interventions.


Huge congratulations to this outstanding group!
More so than most sections, our faculty and fellows are highly dependent on our nurses and staff members in the Cath Lab to stay up-to-date on devices and procedures, provide critical care services to patients needing urgent or emergent procedures, and to work in an environment that is both complex and (at times) extremely stressful. Our fearless leaders—Elizabeth Watts, Tara Bass, and Anna Mall—helped run the Cath Lab and Cardiovascular Short Stay Unit masterfully and they have maintained full staffing during this difficult year. This partnership has remained strong, and while we know that our fellows and staff will transition frequently, having a solid leadership team makes a huge difference and we appreciate their work and all the work of our nurses, techs, and other staff members. We also want to recognize the efforts of our APP colleagues who evaluate and treat our patients in the CVSSU and on the cardiology ward – we’re excited to continue this partnership with Paige Rossman and Tiffany McEwen, among others.
Our site-based research team, including Stephanie Newbold, Mary Beth Summers, Jennifer Andrews, Jessica Ashworth, Inneke (Nikki) Johnson, Chris Pruitt, Krista Camuglia, and Cynthia Pierce have continued to do great work. Like many of our groups within the Heart Center Clinical Research Unit, our team worked from home during a large part of the last academic year. We are gearing up to resume full-time, in-person recruitment for studies involving TAVR, HOCM, coronary stents, acute coronary syndrome, and heart failure hemodynamics and new devices. Great work everyone.
We have 24 faculty members who take care of patients and do procedures in the Duke University Cath Lab, and we have two new faculty members that I would like to highlight:
- Jennifer Rymer – Jenn joined our faculty after completing residency, chief residency, cardiology fellowship (and being chief fellow), and interventional cardiology fellowship at Duke. She splits her time between seeing patients and doing coronary/vascular procedures at Duke Hospital and Mariah Parham Hospital and doing clinical research at the DCRI. Her enthusiasm for cardiology and work product are truly impressive, and we are incredibly happy to have her on our Cath Lab faculty. Jenn is one of five international winners of the women as one escalator award for your early career contributions to the field. Winners are awarded $50,000 in support of an approved research project, participation in networking events, and attend quarterly online research mentorship meetings with field leaders and previous Escalator Award winners.
- Marat Fudim – Marat’s primary appointment is within Heart Failure, but his focus on hemodynamics and new devices has led to him spending some of his time in the Cath Lab. We expect Marat to continue to expand the hemodynamic investigation of patients with suspected or confirmed heart failure and focus on early phase device and diagnostic modalities. Marat was awarded the 2021 Zipes Award from the American College of Cardiology at this year’s Scientific Sessions. His zest for new knowledge and to try new things (including devices and procedures) are exciting, and we’re happy to partner with him in the Cath Lab.
As an interventional cardiology faculty, we have continued to improve our delivery and coordination of care, fellow education, and research opportunities. Some examples include:
- Duke Heart Team: As a group, we consistently meet every Tuesday morning at 6:30am (in-person and webex) to review patient care decisions and angiograms; this meeting has served as an example of the close partnership we have in Duke Heart among cardiologists, interventional cardiologists, and cardiac surgeons.
- Duke TAVR Team: This team meets every Friday morning at 6:30am (typically in-person) to review imaging tests (echos, CTAs, angiograms) and discuss the most appropriate management for high-risk patients with aortic valve disease, concomitant coronary disease, and other valvular problems. TAVR procedures continue to be done in the hybrid OR and multiple Duke Heart partners offer this service including cardiologists (Kevin Harrison, Todd Kiefer, and Andrew Wang) and cardiac surgeons (Chad Hughes, Jeff Gaca, Adam Williams, and Ryan Plichta). This team has performed >250 TAVR procedures over the last year. Special thanks to Edana Christy (valve coordinator), Lynne Koweek (chest radiology), and our Cath Lab and OR staff for the excellent work and collaboration.
- Chronic total occlusions: Izzy Othman has continued to offer and perform complex procedures to recanalize chronic total occlusions of the coronary arteries. Typically, ischemia/viability testing is used to determine the appropriateness for these higher risk procedures, and Izzy has been able to draw referrals from our Duke Heart practices and from all over the state. Great work, Izzy!
- MitraClip: Andrew Wang continues to develop and expand the MitraClip program at Duke, using data that he and others collected and published from the COAPT study and registry. Andrew performs these procedures with the help of our Echo/TEE partners and Duke Anesthesia, and he has availability on most Tuesdays to coordinate and complete these procedures.
- Coronary/peripheral revascularization: As I describe below, the expansion of coronary and peripheral revascularization continues in the community and this has meant that we do fewer coronary interventions in Duke North Hospital. But that also means that our faculty members take on more complex and high-risk procedures for patients with multivessel CAD, more challenging anatomy, cardiogenic shock, and other conditions – and our Heart Team approach is one that we’re very proud of. Our group of vascular interventionalists (Manesh Patel, Larry Crawford, Tony Gutierrez, Jenn Rymer, Raj Swaminathan, Raj Swamy, Schuyler Jones) also continue to be active and often collaborate with our Vascular Surgery partners who do procedures alongside us in the Duke Cath Lab (Kevin Southerland, Chandler Long, Mitch Cox, Zach Williams).
- Adult Congential: Rich Krasuski has developed a niche for complex congenital procedures, as well as for ASD/PFO closures and pulmonary angioplasty for CTEPH.
- Quality improvement work: As he has done for the past few decades, Jimmy Tcheng has led our quality improvement efforts in the Cath Lab. Partnering with multiple hospitals (including many Duke Lifepoint hospitals), Jimmy leads M&M conferences, cine reviews, and QI projects in many states and most of North Carolina.
- Diagnostic fellow education: Tom Bashore continues to teach our diagnostic and interventional fellows about hemodynamics, radiation safety, and other aspects of diagnostic catheterization. I don’t know what we’ll do when Bashore retires, but I have a feeling that our group including Todd Kiefer, Mike Sketch, and Tom Gehrig will step in to fill that gap.
- Our faculty members continue to do great work at Duke University Hospital, but I would be remiss not to mention the great interventional cardiology work at other centers including Duke Regional (Matt Brennan, Stew Jones, Mike Komada), Duke Raleigh (James Mills, Mark Leithe), Alamance Regional (Dwayne Callwood, Alex Parachos, Ken Fath, Bruce Kowalski), Sovah Danville (Bosh Zakhary, Kevin Lingle, Brian Zagol, David Kotlaba), Lumberton (Bill Herzog), Sanford/Central Carolina Hospital (Rajiv Swamy), Wake Med Cary (Manesh Patel, Izzy Othman, Tom Gehrig), Henderson/Mariah Parham Hospital (Syd Short, Jennifer Rymer, Tony Gutierrez, Manesh Patel, Rajesh Swaminathan, Schuyler Jones), and the Durham VA Medical Center (Sunil Rao, Rajesh Swaminathan, Tony Gutierrez, Tom Povsic, Mitch Krucoff).
On the research side, a number of faculty have led important clinical trial and outcomes research projects. To my best count, the faculty have published 250 manuscripts (collectively) over the past 12 months in high-impact journals including New England Journal of Medicine, Lancet, Circulation, Journal of the American College of Cardiology, European Heart Journal, and JAMA Cardiology. Impressively, 75% of our faculty have published this year, with many publications involving multiple members of the Duke Cath Lab team. I have highlighted a few – the first 6 publications represent studies where we enrolled patients at Duke and our faculty had key leadership roles and/or were included on the main/subsequent publications:
- Rivaroxaban in Peripheral Artery Disease after Revascularization. Bonaca MP, Bauersachs RM, Anand SS, Debus ES, Nehler MR, Patel MR, Fanelli F, Capell WH, Diao L, Jaeger N, Hess CN, Pap AF, Kittelson JM, Gudz I, Mátyás L, Krievins DK, Diaz R, Brodmann M, Muehlhofer E, Haskell LP, Berkowitz SD, Hiatt WR. N Engl J Med. 2020;382(21):1994-2004. PMID: 32222135
- Intracoronary ALLogeneic heart STem cells to Achieve myocardial Regeneration (ALLSTAR): a randomized, placebo-controlled, double-blinded trial. Makkar RR, Kereiakes DJ, Aguirre F, Kowalchuk G, Chakravarty T, Malliaras K, Francis GS, Povsic TJ, Schatz R, Traverse JH, Pogoda JM, Smith RR, Marbán L, Ascheim DD, Ostovaneh MR, Lima JAC, DeMaria A, Marbán E, Henry TD. Eur Heart J. 2020;41(36):3451-3458. PMID: 32749459
- Mavacamten for treatment of symptomatic obstructive hypertrophic cardiomyopathy (EXPLORER-HCM): a randomised, double-blind, placebo-controlled, phase 3 trial. Olivotto I, Oreziak A, Barriales-Villa R, Abraham TP, Masri A, Garcia-Pavia P, Saberi S, Lakdawala NK, Wheeler MT, Owens A, Kubanek M, Wojakowski W, Jensen MK, Gimeno-Blanes J, Afshar K, Myers J, Hegde SM, Solomon SD, Sehnert AJ, Zhang D, Li W, Bhattacharya M, Edelberg JM, Waldman CB, Lester SJ, Wang A, Ho CY, Jacoby D; EXPLORER-HCM study investigators. Lancet. 2020;396(10253):759-769. PMID: 32871100
- Five-Year Clinical and Quality of Life Outcomes From the CoreValve US Pivotal Extreme Risk Trial. Arnold SV, Petrossian G, Reardon MJ, Kleiman NS, Yakubov SJ, Wang K, Hermiller J Jr, Harrison JK, Deeb GM, Huang J, Cohen DJ; US CoreValve Investigators. Circ Cardiovasc Interv. 2021 (online ahead of print). PMID: 34092091
- Splanchnic Nerve Block for Chronic Heart Failure. Fudim M, Boortz-Marx RL, Ganesh A, DeVore AD, Patel CB, Rogers JG, Coburn A, Johnson I, Paul A, Coyne BJ, Rao SV, Gutierrez JA, Kiefer TL, Kong DF, Green CL, Jones WS, Felker GM, Hernandez AF, Patel MR. JACC Heart Fail. 2020;8(9):742-752. PMID: 32535123
- Comparative Effectiveness of Aspirin Dosing in Cardiovascular Disease. Jones WS, Mulder H, Wruck LM, Pencina MJ, Kripalani S, Muñoz D, Crenshaw DL, Effron MB, Re RN, Gupta K, Anderson RD, Pepine CJ, Handberg EM, Manning BR, Jain SK, Girotra S, Riley D, DeWalt DA, Whittle J, Goldberg YH, Roger VL, Hess R, Benziger CP, Farrehi P, Zhou L, Ford DE, Haynes K, VanWormer JJ, Knowlton KU, Kraschnewski JL, Polonsky TS, Fintel DJ, Ahmad FS, McClay JC, Campbell JR, Bell DS, Fonarow GC, Bradley SM, Paranjape A, Roe MT, Robertson HR, Curtis LH, Sharlow AG, Berdan LG, Hammill BG, Harris DF, Qualls LG, Marquis-Gravel G, Modrow MF, Marcus GM, Carton TW, Nauman E, Waitman LR, Kho AN, Shenkman EA, McTigue KM, Kaushal R, Masoudi FA, Antman EM, Davidson DR, Edgley K, Merritt JG, Brown LS, Zemon DN, McCormick TE 3rd, Alikhaani JD, Gregoire KC, Rothman RL, Harrington RA, Hernandez AF; ADAPTABLE Team. N Engl J Med. 2021;384(21):1981-1990. PMID: 33999548
- In-Hospital Outcomes and Discharge Medication Use Among Patients With Critical Limb Ischemia Versus Claudication. Rymer JA, Kennedy KF, Lowenstern AM, Secemsky EA, Tsai TT, Aronow HD, Prasad A, Gray B, Armstrong EJ, Rosenfield K, Shishehbor MH, Jones WS. J Am Coll Cardiol. 2020 Feb 18;75(6):704-706. PMID: 32057381
- Survival and Causes of Death Among Veterans With Lower Extremity Revascularization With Paclitaxel-Coated Devices: Insights From the Veterans Health Administration. Gutierrez JA, Rao SV, Jones WS, Secemsky EA, Aday AW, Gu L, Schulteis RD, Krucoff MW, White R, Armstrong EJ, Banerjee S, Tsai S, Patel MR, Swaminathan RV. J Am Heart Assoc. 2021;10(4):e018149. PMID: 33554613
- Characteristics and Outcomes of Patients With History of CABG Undergoing Cardiac Catheterization Via the Radial Versus Femoral Approach. Manly DA, Karrowni W, Rymer JA, Kaltenbach LA, Swaminathan RV, Messenger JC, Abbott JD, Seto A, Panetta C, Brilakis E, Nikolakopoulos I, Gilchrist IC, Kaul P, Dakik H, Rao SV. JACC Cardiovasc Interv. 2021;14(8):907-916. PMID: 33812824
Overall, we’re incredibly proud of the work we do in the Duke Interventional Cardiology section, and we are excited to expand our services throughout North Carolina. Really excellent work everyone!
Year-End Celebration for Interventional & Structural Heart Fellowship Programs
Our graduating structural heart fellow and three interventional fellows were celebrated in downtown Durham on Thursday evening at The Roof restaurant at The Durham hotel. Congratulations to Angela Lowenstern, who completed the Structural Heart Disease Fellowship Training program; and to Adam Banks, Jaidip Chakravartti and Mike Nanna who have completed the Interventional Cardiology Fellowship Training program. (See additional highlights from Schuyler Jones, above)
The Warren S. and Gloria R. Newman Fellowship in Cardiology award established in Honor of Robert H. “Jess” Peter, MD, was awarded to Adam Banks. Congratulations, Adam!
Best wishes to each of them as they embark on their new positions! Congratulations!





McDermott Earns DNP at Hopkins
Congratulations to Jaime McDermott, cardiology nurse practitioner, for completing her Doctor of Nursing Practice degree with Johns Hopkins University School of Nursing in May. Her DNP capstone project, Improving Advanced Practice Provider Knowledge and Screening of Medication Adherence in Cardiovascular Patients received the JHU Doctor of Nursing Practice Executive Track program award for greatest clinical impact!
Johns Hopkins University School of Nursing in May. Her DNP capstone project, Improving Advanced Practice Provider Knowledge and Screening of Medication Adherence in Cardiovascular Patients received the JHU Doctor of Nursing Practice Executive Track program award for greatest clinical impact!
McDermott began the JHU program in 2017 before relocating to Durham, NC for a nursing position at Duke Heart in 2018. She took time off from the program to settle into her new role here at Duke before rejoining the program in January 2020.
She worked closely with Jill Engel and Bradi Granger – both of whom hold DNP degrees — to map out a doctoral capstone project. In September of 2020, Jaime successfully designed a medication adherence screening tool and an educational program for APPs. When the project wrapped up two months later, data showed that by having the APPs use the screening tool in the electronic health record, screening for medication adherence increased from 3.7% to over 73%.
“Jaime is such a tremendous cardiology APP provider and Duke Heart team member,” says Jill Engel, associate vice president of Duke Heart Services. “Her capstone project exemplified what a QI DNP capstone project should look like. She was masterful in her execution and positively impacted Duke Heart patients and the provider team. Dr. Bradi Granger was a tremendous asset, as always, in the academic partnership with the Johns Hopkins faculty. People like Jaime and Bradi make Duke Heart the great place it is.”
Congratulations Dr. McDermott!
PHASeR Team Earns FHIT Award

Congratulations to Deepak Voora and his research team! Voora leads the Pharmacogenomics program at the VA called PHarmacogenomics Action for Cancer Survivorship (PHASeR) — and they just won a 2021 Federal Health IT Award!
Awardees were celebrated this past week during the 7th Annual FedHealthIT Innovation Awards, an event that recognizes and honors the Federal Health technology and consulting community by celebrating the programs nominated and selected by their peers for driving innovation and results across the Department of Veterans Affairs, Military Health, Health and Human Services, and Centers for Medicare & Medicaid Services.
PHASeR is a clinical program bringing preemptive pharmacogenetic testing to up to 250,000 Veterans across the VA system. Congratulations, Deepak!
Patient Compliment for Heart Valve Replacement Team & Support Staff
We received a note this week from Lisa Clark Pickett, Chief Medical Officer for Duke University Hospital with a compliment for some of our Duke Heart team members:
“Good Morning, I was just delighted to read this lovely compliment about your team on our Patient Satisfaction survey. I wanted to share so that you can enjoy the good words and convey to your team at huddle, etc.! Best wishes, Lisa
“During my week’s visit, I was impressed by the entire staff of the hospital, from the doctors and nurses to the food service, sanitation, and other support groups. Everyone I encountered was friendly, helpful, respectful, caring, professional, and inspired confidence that my decision to go to Duke University Hospital for my heart valve repair surgery was the correct choice.” — Name withheld for privacy
Great job, team!
Kudos to Pena!
I just wanted to give a shout out to Heather Pena who just obtained official certification in patient safety (CPPS). Kudos to her and all the work she does in support of the Heart Center. She is a great asset to Heart Services and the DUH SSA group, always sharing great insights and best practices. It is always a pleasure working with Heather and I am excited she reached this achievement. — Submitted by Kara Lyven, MBA, CPPS, Executive Director, Patient Safety, Duke University Hospital
Congratulations, Heather!!
Duke Health: Change Passwords; New Policy
Good news, Duke has updated its password policy! Why is this good news? Duke Health users and sponsored guests must update passwords as soon as possible, but will not be required to change passwords in the future – unless you want to update or your password is compromised.
The new password policy removes the requirement to update passwords every 180 days and requires passwords to be at least 12 characters (special characters and numbers are no longer required); however, including special characters creates a stronger password. In addition, the option to update passwords using CTRL+ALT+DEL is no longer available.
Team members can update their passwords now, but will receive a notice from DHTS via email that requires passwords to be changed by a deadline. Please visit the OIT Account Self Service Portal and create a new NetID password that doesn’t expire.
Tip: If working remotely (at a non-Duke site) users should connect to the Duke Virtual Private Network (VPN) before updating passwords (see page 29 of the Technology Toolkit for more information about the VPN). Passwords can be updated without connecting to the VPN, but passwords are synced across all your Duke log-ins faster if connected to the VPN.
Visit https://security.duke.edu/news-alerts/new-password-policy to review the password policy FAQ.
Attention Omnicell Users
Due to Omnicell’s password policy, Duke Health employees that use Omnicell, with the exception of Duke Raleigh Hospital employees, must keep passwords to 15 characters or less; Duke Raleigh Hospital employees must keep passwords to a maximum of 30 characters.
We are working with Omnicell to upgrade their password policy to remove restrictions across Duke Health. Check the password policy information page for updates.
Contact the Duke Health Service Desk at (919) 684-2243 for technical support.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged.
Duke Heart in the News:
June 10 — Harry Severance
VN Express
Seven-day quarantine for fully vaccinated foreigners feasible: experts
https://bit.ly/3d1ZEp3
June 16 — Christopher Granger and Sean Pokorney
Physician’s Weekly
DOAC Reversal Agents Tied to High Bleeding Risk
https://bit.ly/3gM5MTk
June 18 — Michael Carboni (pediatric cardiology)
WSOC-TV (Charlotte)
CDC investigating possible link between mRNA COVID-19 vaccines and heart inflammation
https://bit.ly/3wQYTa8
June 18 — Manesh Patel
tctMD
Unseen and Unheard: In the Cath Lab, Anti-racism Efforts Fall Short
https://bit.ly/3wTKavc
June 22 — Myra Ellis
Physician’s Weekly
New Protocol Aims for Early Extubation in Cardiac Surgery Patients
https://bit.ly/35JwnLM
June 22 — Manesh Patel
WNCN/CBS17.com
https://bit.ly/3wUQd2t
June 23 — Renato Lopes
Medscape
No Benefit to Therapeutic Oral Anticoagulation in COVID-19 Hospitalizations
https://www.medscape.com/viewarticle/953573?src=
June 24 — Sunil Rao
Medscape
Could the Surgisphere Lancet and NEJM Retractions Debacle Happen Again?
https://www.medscape.com/viewarticle/953653
Division of Cardiology Publications Indexed in PubMed June 19-23, 2021
Boshara A, Patel A, Alasaad M, Dutcheshen KJ, LaLonde TA, Schreiber TL, Mehta RH, Kaki A, Rosman HS. Cardiogenic Shock Complicating Acute Myocardial Infarction Treated With Percutaneous Coronary Intervention Supported by Impella: Implications of Advanced Age and Refractory Shock on Outcomes. Crit Care Explor 2021;3(6):e0447. PM: 34136823.
de Boer RA, Aboumsallem JP, Bracun V, Leedy D, Cheng R, Patel S, Rayan D, Zaharova S, Rymer J, Kwan JM, Levenson J, Ronco C, Thavendiranathan P, Brown SA. A new classification of cardio-oncology syndromes. Cardiooncology 2021;7(1):24. PM: 34154667.
Dungan JR, Qin X, Hurdle M, Haynes CS, Hauser ER, Kraus WE. Genome-Wide Variants Associated With Longitudinal Survival Outcomes Among Individuals With Coronary Artery Disease. Front Genet 2021;12:661497. PM: 34140969.
Granger CB, Pokorney SD. Preventing and Managing Bleeding With Anticoagulation for Atrial Fibrillation. J Am Coll Cardiol 2021;77(24):3002-3004. PM: 34140102.
Hess CN, Cannon CP, Beckman JA, Goodney PP, Patel MR, Hiatt WR, Mues KE, Orroth KK, Shannon E, Bonaca MP. Effectiveness of Blood Lipid Management in Patients With Peripheral Artery Disease. J Am Coll Cardiol 2021;77(24):3016-3027. PM: 34140105.
Lowenstern A, Li S, Navar AM, Virani SS, Roger VL, Robinson JG, Goldberg AC, Kampman W, Peterson ED, Wang TY. Patient perceptions and use of non-statin lipid lowering therapy among patients with or at risk for atherosclerotic cardiovascular disease: Insights from the PALM registry. Clin Cardiol 2021;44(6):863-870. PM: 34008247.
Meyersohn NM, Mayrhofer T, Corey KE, Bittner DO, Staziaki PV, Szilveszter B, Hallett T, Lu MT, Puchner SB, Simon TG, Foldyna B, Voora D, Ginsburg GS, Douglas PS, Hoffmann U, Ferencik M. Association of Hepatic Steatosis With Major Adverse Cardiovascular Events, Independent of Coronary Artery Disease. Clin Gastroenterol Hepatol 2021;19(7):1480-1488. PM: 32707340.
Nachun D, Lu AT, Bick AG, Natarajan P, Weinstock J, Szeto MD, Kathiresan S, Abecasis G, Taylor KD, Guo X, Tracy R, Durda P, Liu Y, Johnson C, Rich SS, Van Den Berg D, Laurie C, Blackwell T, Papanicolaou GJ, Correa A, Raffield LM, Johnson AD, Murabito J, et al. Clonal hematopoiesis associated with epigenetic aging and clinical outcomes. Aging Cell 2021;20(6):e13366. PM: 34050697.
Serfas JD, Thibault D, Andersen ND, Chiswell K, Jacobs JP, Jacobs ML, Krasuski RA, Lodge AJ, Turek JW, Hill KD. The Evolving Surgical Burden of Fontan Failure: An Analysis of The Society of Thoracic Surgeons Congenital Heart Surgery Database. Ann Thorac Surg 2021;112(1):179-187. PM: 32763267.
Slawsky E, Ward-Caviness CK, Neas L, Devlin RB, Cascio WE, Russell AG, Huang R, Kraus WE, Hauser E, Diaz-Sanchez D, Weaver AM. Evaluation of PM air pollution sources and cardiovascular health. Environ Epidemiol 2021;5(3):e157. PM: 34131618.
Smith LR, Darty SN, Jenista ER, Gamoneda GL, Wendell DC, Azevedo CF, Parker MA, Kim RJ, Kim HW. ECG-gated MR angiography provides better reproducibility for standard aortic measurements. Eur Radiol 2021;31(7):5087-5095. PM: 33409772.
Duke Heart June 20th 2021 – Father’s Day Weekend
Chief’s message:
The end of the academic year is highlighted by fellowship graduation ceremonies, time with family and friends, and this weekend we had the additional benefit of having Father’s Day. We are blessed at Duke Heart with the lifeblood of our program, the fellowship training program. We have the privilege of training the next generation of cardiovascular leaders with an amazing group of fellows, and that was on display at our year end get together. Chris and Bradi Granger kindly shared their home/farm in Bahama, NC for the festivities. You will find the pictures and updates below of all the amazing faculty and fellow awards. Additionally, hopefully all of you got sometime this weekend to celebrate father’s day.
Highlights of the week:
Year-End Celebration for General Cardiology Fellowship Programs
On Friday evening, we gathered (together, in-person, for the first time in far too long!) to celebrate five of our  fellows who are completing their training with us and those who are completing one program and transferring into their next fellowship. The general cardiology fellowship year-end dinner, held at the home of Drs. Chris and Bradi Granger and hosted by fellowship program director Anna Lisa Crowley, honored fellows from the Cardiovascular Disease, Advanced Training in Cardiology, and Clinical Investigator Pathway – Cardiovascular Disease fellowship programs. The casual affair featured a BBQ dinner, an awards program and presentation, the annual Fellows video, live music performed by Tony & Ashli Carnicelli and Rob Mentz, MCNA$TY, some free ranging chickens and a dog named Tilley.
fellows who are completing their training with us and those who are completing one program and transferring into their next fellowship. The general cardiology fellowship year-end dinner, held at the home of Drs. Chris and Bradi Granger and hosted by fellowship program director Anna Lisa Crowley, honored fellows from the Cardiovascular Disease, Advanced Training in Cardiology, and Clinical Investigator Pathway – Cardiovascular Disease fellowship programs. The casual affair featured a BBQ dinner, an awards program and presentation, the annual Fellows video, live music performed by Tony & Ashli Carnicelli and Rob Mentz, MCNA$TY, some free ranging chickens and a dog named Tilley.





Congratulations to:
- Rahul Loungani, completing the Advanced Heart Failure and Transplant Cardiology program. He has accepted a position with Piedmont Hospital in Atlanta.
- Hirak Shah, completing the Advanced Heart Failure and Transplant Cardiology program. He has accepted a position with the University of Kansas in Kansas City.
- Angela Lowenstern, our Structural Heart Fellow, is completing the Advanced Training in Cardiology program. She has accepted a position with Vanderbilt University in Nashville.
- Gedion Titus Ng’eno, completing the Advanced Training in Cardiology program. He will join the Duke faculty.
- Jordan Pomeroy, completing the Clinical Investigator Pathway – Cardiovascular Disease program. He has accepted a position with the Food and Drug Administration in Silver Spring.
The following fellows are completing one of the general cardiology fellowship programs on June 30 and transitioning to another. They are:
Amanda Coniglio, completing Advanced Heart Failure and Transplant Cardiology training and returning to the Cardiovascular Disease program for her third year. She will serve as Duke’s chief cardiology fellow for 2021-2022.
Caitlin Dresher, Michelle Kelsey, Navid Nafissi, Vishal Rao, and Lauren Truby are completing the Cardiovascular Disease program and moving into Advanced clinical and research training in the Cardiology fellowship.
Kevin Friede, Zachary Wegermann and George Sipa Yankey are completing the Advanced Training in Cardiology program and moving into Interventional Cardiology fellowship.
Anthony Carnicelli and Marc Samsky are completing the Advanced Training in Cardiology program and moving into Advanced Heart Failure and Transplant Cardiology fellowship.
Jeffrey Dixson will return to the Cardiovascular Disease fellowship program on July 1 to complete his third year. He will complete the Non-pulmonary Critical Care Medicine fellowship on June 30.
Christopher Wrobel will take a one year break from the Cardiovascular Disease program to complete the Advanced Heart Failure and Transplant Cardiology fellowship, starting July 1.
John Serfas is completing the Adult Congenital Heart Disease fellowship and moving into the Advanced Training in Cardiology program as the Structural Heart Fellow.
As is our custom at year-end, we presented the following annual awards, which are selected by the cardiology faculty:
- The Cassell-Saperstein Award recognizes a cardiology fellow who most demonstrates a commitment to teaching and passion for clinical education. Our recipient this year is George Sipa Adjay Yankey, Jr.
- The Brandt and Belinda Louie Award recognizes a cardiology fellow who demonstrates a commitment to excellence in all three missions of Duke Heart (clinical, education, and research). Our recipient this year is Kevin Friede.
- The Joseph G. Greenfield Scholar in Cardiology Award recognizes a fellow demonstrating dedication and contribution to research. Our recipient this year is Lauren Truby.

The following annual awards, selected by the fellows, were also presented:
- The Walter J. Floyd Award is presented to a fellow who demonstrates most outstanding clinical skills and acumen. Our recipient this year is Vishal Rao.
- The Bashore Faculty Teaching Award is presented to a faculty member demonstrating dedication and excellence in teaching. Our recipient this year is Jason Katz.

- The Fellow Mentorship Award is presented to a faculty member demonstrating dedication and excellence in mentoring fellows’ careers. Our recipient this year is Adam DeVore.
- The Outstanding Service Award is presented to a hospital staff member who demonstrates dedication to and excellence in fellow education. Our recipient this year is Richard Palma.
Congratulations to all awardees and — once again to Rahul, Hirak, Angela, Titus and Jordan — all the best as you transition into the next phase of your careers! Many thanks to all who joined us for a joy- and music-filled evening — special thanks to the fellows for their annual video presentation, to the Grangers for a beautiful venue; to Anna Lisa Crowley, Manesh Patel and Amanda Coniglio for a truly wonderful event, welcoming remarks and presentation. Great job, everyone!
Wofford Heading to Atrium Health

Brian M. Wofford, Vice President of Heart Operations in Durham County, has accepted a position at Atrium Health as the VP of Clinical Integration. His last day at Duke will be June 22. Brian has been on the Duke Heart team for four years and has spent 11 years overall at Duke. He is well-known for his excellent communication skills, ability to network and provide mentorship.
Brian came to Duke in 2010 as an Administrative Fellow and has supported key operational and strategic projects as an Administrative Manager for Strategic Operations including leading the Facility Transition Planning Team for the Duke Medical Pavilion. Brian’s other roles at Duke University Hospital include Administrative Director of Strategic Operations, Administrative Director for Perioperative Ambulatory Services, Interim VP of Emergency Services and Patient Flow and VP of Medical, Surgical and Critical Care Services.
In his most recent role as VP of Heart Services for Durham County, Brian provided support for the expansion of Respiratory Care Services to a system model, partnered with the operational teams and faculty on key construction projects, and co-created the Heart Patient and Family Advisory Council. Brian played a key role as a trainer for other leaders and team members in the Duke Quality System Commit to Zero Harm journey and served as the Operations Sections Co-Chief for the DUH COVID-19 Command Center.
Brian is a talented leader who focuses on relationship building and growing new leaders as demonstrated by the numerous Duke Administrative fellows he has mentored over the years. We very much appreciate Brian’s leadership and commitment to Duke University Hospital and Duke Heart and his strong commitment to excellence, safety and quality.
Please join us in congratulating Brian and thanking him for his tremendous contributions during his time with us!
Frazier-Mills Appointed to Editorial Board

Congratulations to Camille Frazier-Mills from our Electrophysiology team – she has been appointed to the Editorial Board of the journal Circulation: Arrhythmia and Electrophysiology. She joins fellow faculty members Sana Al-Khatib, Jim Daubert, Jon Piccini and Kevin L. Thomas who also serve on the editorial board.
Congratulations, Camille!
Southerland Named Wylie Scholar for 2021
Kevin Southerland, MD, an assistant professor of vascular surgery who has been working in the Duke

Cardiovascular Research Center under the mentorship of Dr. Chris Kontos, was mentioned earlier this month in the Pulse after he was awarded a Strong Start Award from the School of Medicine. We are pleased to share that Southerland is this year’s winner of the prestigious Wylie Scholar Award from the Vascular Cures Foundation and the Society for Vascular Surgery Foundation.
The Wylie Scholar Award is given to only one vascular surgeon-scientist each year, and the prize’s previous winners since it was first awarded in 1996 have gone on to become many of the top academic vascular surgeon-scientists in North America. The award is for his project “Transcriptional Dynamics and Heterogeneity of Macrophages in Chronic Limb Threatening Ischemia.” Like the Strong Start Award, the three-year Wylie Scholar Award will provide support for Kevin’s work to understand the mechanisms of critical limb threatening ischemia (CLTI).
Kevin is also supported by a KL2 award from the Duke CTSA, and he is co-investigator on an NIH U01 award with his collaborator Yarui Diao in the Department of Cell Biology. Kevin’s work has focused on single cell transcriptomic and genomic data in clinical and preclinical models to elucidate mechanisms for tissue loss in limb ischemia.
Congratulations, Kevin!!
Bonadonna Named to AmSECT Board of Directors
 We learned this week that Desiree Bonadonna, chief of Perfusion Services, has been appointed to the American Society of Extracorporeal Technology (AmSECT) Board of Directors as the Extracorporeal Life Support Organization (ELSO) Liaison. The position places her on the ELSO Steering Committee, as well.
We learned this week that Desiree Bonadonna, chief of Perfusion Services, has been appointed to the American Society of Extracorporeal Technology (AmSECT) Board of Directors as the Extracorporeal Life Support Organization (ELSO) Liaison. The position places her on the ELSO Steering Committee, as well.
The role of the ELSO Liaison is to promote the science of Extracorporeal Life Support in the perfusion community by maintaining an active role in the collaborative efforts of both AmSECT and ELSO. The position, which requires clinical experience in providing extracorporeal life support to neonatal, pediatric and adult patients, is seen as integral in establishing and maintaining all levels of communication across the steering committee, leaders of ELSO and the Board of Directors of AmSECT.
The role is effective July 1. Congratulations, Desiree!
Duke Heart APPs Support MSN Students
Several of our ambulatory APP members shared their knowledge and skills with MSN students from the Duke School of Nursing over the past week during the Nurse Practitioner Intensive.
Michelle Johnson, NP-C discussed cases of Adults with Congenital Heart Disease and Mike Strub, PA-C did a live demonstration of cardiac ultrasound and shared his knowledge of Point of Care Cardiac Ultrasound with students across the country via Zoom. Allen Stephens, PA-C discussed EKG interpretation and Kevin Cox, NP-C facilitated discussions on Initiating Home Inotropes and Caring for an LVAD in the outpatient setting.
Great work, everyone! Hat tip to Midge Bowers for sharing this update with us!
Cardiology Faculty Members Participate in AAHFN
This week, the American Association of Heart Failure Nurses (AAHFN) held its 17th Annual Meeting, including a pre-meeting Mechanical Circulatory Support (MCS) Bootcamp and Pharmacology workshop this week. The AAHFN thanks Stu Russell, Jason Katz and Marat Fudim for sharing their expertise with the audience.
Thank you to Stephanie Barnes, Clinical Director for Advanced Heart Failure Services, for sharing this with Pulse!
ICYMI: Rauch Foundation Makes Historic Gift for Financial Aid
A family foundation established by the late Dudley Rauch, AB’63, has pledged $30 million to establish an endowment for need-based financial aid for medical students in the Duke University School of Medicine.
The gift by the Rauch Family Foundation is the single largest commitment for financial aid ever made to the School of Medicine.
School of Medicine Dean Mary E. Klotman said the Rauch Family Foundation’s generosity will ease the financial burden on generations of medical students at Duke. The gift will help open the path to a career in medicine to more students from diverse backgrounds, and enhance Duke’s ability to compete for the highest caliber of incoming students.
To read the full story, please see: https://bit.ly/3iMhpMF.
Upcoming Opportunities/Save the Date:
Cardiovascular Risk Management: State of the Science Summit
June 23: — Institutional Perspectives in Cardiology: Cardiovascular Risk Management webinar with Manesh Patel, Schuyler Jones, Tracy Wang and Christopher Granger. 7 to 8:30 p.m. EST. Virtual. Registration is free. They’ll cover:
- CAD/PAD: Identifying Risk & Summary of Recent Clinical Trials
- Extended Thromboprophylaxis: What Do We Know About Scoring, Risk and Contemporary Trials?
- Atrial Fibrillation: What Have We Learned About NOACs in Special Populations?
- Putting This All Together: Treatment Pyramid
To learn more, please visit: HCPLive Institutional Perspectives in Cardiology.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged.
Duke Heart in the News:
June 11 — Sunil Rao and Zachary Wegermann
MDEdge/Cardiology
First risk score to predict bleeding risk after TAVR
https://bit.ly/3iWpVZN
June 14 — Christopher Granger and Sean Pokorney
Medpage Today
DOAC Antidotes No Panacea for Fatal Bleeds
https://www.medpagetoday.com/cardiology/prevention/93096
June 14 — Christopher Granger and Sean Pokorney
Medscape
Reversal Agents Curb DOAC-related Bleeding but Deaths Still High
https://www.medscape.com/viewarticle/953045#vp_2
June 17 — Vanessa Blumer
Univision NC/WUVC 40
“Fue un héroe”: padre muere ahogado luego de rescatar a su hijo
(Story is about a drowning/water safety & importance of CPR)
https://bit.ly/35Aem2o
Division of Cardiology Publications Indexed in PubMed June 10-18, 2021
Arnold SV, Petrossian G, Reardon MJ, Kleiman NS, Yakubov SJ, Wang K, Hermiller J, Harrison JK, Deeb GM, Huang J, Cohen DJ. Five-Year Clinical and Quality of Life Outcomes From the CoreValve US Pivotal Extreme Risk Trial. Circ Cardiovasc Interv 2021;14(6):e010258. PM: 34092091.
Coles TM, Hernandez AF, Reeve BB, Cook K, Edwards MC, Boutin M, Bush E, Degboe A, Roessig L, Rudolph A, McNulty P, Patel N, Kay-Mugford T, Vernon M, Woloschak M, Buchele G, Spertus JA, Roe MT, Bury D, Weinfurt K. Enabling patient-reported outcome measures in clinical trials, exemplified by cardiovascular trials. Health Qual Life Outcomes 2021;19(1):164. PM: 34120618.
Friedman DJ, Emerek K, Sørensen PL, Zeitler EP, Goldstein SA, Al-Khatib SM, Søgaard P, Graff C, Atwater BD. Sex differences in left ventricular electrical dyssynchrony and outcomes with cardiac resynchronization therapy. Heart Rhythm O2 2020;1(4):243-249. PM: 34113878.
Friedman DJ, Field ME, Rahman M, Goldstein L, Sha Q, Sidharth M, Khanna R, Piccini JP. Catheter ablation and healthcare utilization and cost among patients with paroxysmal versus persistent atrial fibrillation. Heart Rhythm O2 2020;2(1):28-36. PM: 34113902.
Lam CSP, Giczewska A, Sliwa K, Edelmann F, Refsgaard J, Bocchi E, Ezekowitz JA, Hernandez AF, O’Connor CM, Roessig L, Patel MJ, Pieske B, Anstrom KJ, Armstrong PW. Clinical Outcomes and Response to Vericiguat According to Index Heart Failure Event: Insights From the VICTORIA Trial. JAMA Cardiol 2021;6(6):706-712. PM: 33185650.
Lopes RD, de Barros E Silva PGM, Furtado RHM, Macedo AVS, Bronhara B, Damiani LP, Barbosa LM, de Aveiro Morata J, Ramacciotti E, de Aquino Martins P, de Oliveira AL, Nunes VS, Ritt LEF, Rocha AT, Tramujas L, Santos SV, Diaz DRA, Viana LS, Melro LMG, et al. Therapeutic versus prophylactic anticoagulation for patients admitted to hospital with COVID-19 and elevated D-dimer concentration (ACTION): an open-label, multicentre, randomised, controlled trial. Lancet 2021;397(10291):2253-2263. PM: 34097856.
Murphy SP, Prescott MF, Maisel AS, Butler J, Piña IL, Felker GM, Ward JH, Williamson KM, Camacho A, Kandanelly RR, Solomon SD, Januzzi JL. Association Between Angiotensin Receptor-Neprilysin Inhibition, Cardiovascular Biomarkers, and Cardiac Remodeling in Heart Failure With Reduced Ejection Fraction. Circ Heart Fail 2021;14(6):e008410. PM: 33998243.
Nagaraja V, Rao SV, George S, Mamas M, Nolan J. Evidence-based arterial access site practice in patients with acute coronary syndromes: Has SAFARI-STEMI changed the landscape? Catheter Cardiovasc Interv 2021;97(7):1417-1421. PM: 33837993.
Patel D, Kumar A, Black-Maier E, Morgan RL, Trulock K, Wilner B, Nemer D, Donnellan E, Tarakji KG, Cantillon DJ, Varma N, Saba SF, Al-Khatib SM, Wilkoff BL, Rickard JW. Cardiac Resynchronization Therapy With or Without Defibrillation in Patients With Nonischemic Cardiomyopathy: A Systematic Review and Meta-Analysis. Circ Arrhythm Electrophysiol 2021;14(6):e008991. PM: 33999647.
Piccini JP, Braegelmann KM, Simma S, Koneru JN, Ellenbogen KA. Risk of atrioesophageal fistula with cryoballoon ablation of atrial fibrillation. Heart Rhythm O2 2020 May 28;1(3):173-179. PM: 34113871.
Rao SV, Wegermann ZK. Quo Vadis, Bleeding Risk Models? JACC Cardiovasc Interv 2021 Jun 14;14(11):1207-1208. PM: 34112455.
Rodriguez F, Solomon N, de Lemos JA, Das SR, Morrow DA, Bradley SM, Elkind MSV, Williams JH, Holmes D, Matsouaka RA, Gupta D, Gluckman TJ, Abdalla M, Albert MA, Yancy CW, Wang TY. Racial and Ethnic Differences in Presentation and Outcomes for Patients Hospitalized With COVID-19: Findings From the American Heart Association’s COVID-19 Cardiovascular Disease Registry. Circulation 2021 Jun 15;143(24):2332-2342. PM: 33200953.
Samsky MD, Hellkamp A, Hiatt WR, Fowkes FGR, Baumgartner I, Berger JS, Katona BG, Mahaffey KW, Norgren L, Blomster JI, Rockhold FW, DeVore AD, Patel MR, Jones WS. Association of Heart Failure With Outcomes Among Patients With Peripheral Artery Disease: Insights From EUCLID. J Am Heart Assoc 2021 Jun 15;10(12):e018684. PM: 34056910.
Segar MW, Jaeger BC, Patel KV, Nambi V, Ndumele CE, Correa A, Butler J, Chandra A, Ayers C, Rao S, Lewis AA, Raffield LM, Rodriguez CJ, Michos ED, Ballantyne CM, Hall ME, Mentz RJ, de Lemos JA, Pandey A. Development and Validation of Machine Learning-Based Race-Specific Models to Predict 10-Year Risk of Heart Failure: A Multicohort Analysis. Circulation 2021 Jun 15;143(24):2370-2383. PM: 33845593.
Sutton NR, Banerjee S, Cooper MM, Arbab-Zadeh A, Kim J, Arain MA, Rao SV, Blumenthal RS. Coronary Artery Disease Evaluation and Management Considerations for High Risk Occupations: Commercial Vehicle Drivers and Pilots. Circ Cardiovasc Interv 2021 Jun;14(6):e009950. PM: 34092098.
Wang A, Truong T, Black-Maier E, Green C, Campbell KB, Barnett AS, Febre J, Loring Z, Al-Khatib SM, Atwater BD, Daubert JP, Frazier-Mills C, Hegland DD, Jackson KP, Jackson LR, Koontz JI, Lewis RK, Pokorney SD, Sun AY, Thomas KL, Bahnson TD, Piccini JP. Catheter ablation of atrial fibrillation in patients with diabetes mellitus. Heart Rhythm O2 2020 May 12;1(3):180-188. PM: 34113872.
Duke Heart Week ending June 13th 2021
Highlights of the week:
Kisslo to Receive ASE Award for Outstanding Achievement

Joseph Kisslo, professor of medicine in cardiology, will receive the American Society of Echocardiography’s (ASE) Outstanding Achievement in Perioperative Echocardiography Award next weekend at the ASE 2021 Scientific Sessions Virtual Experience. Kisslo, who served as the fourth president of ASE (1983-1984), is the first cardiologist to be recognized with the award. His recorded presentation regarding the award will be shown during the ASE Virtual Gala on Sunday, June 20.
The Outstanding Achievement in Perioperative Echocardiography Award recognizes an individual who has made significant clinical, research or educational contributions to the development of the field of perioperative echocardiography. The awardee is chosen by the ASE Council on Perioperative Echocardiography.
Kisslo was the first to use phased array ultrasound imaging in the human body and the first to describe most of the disease for which the technique is now commonplace. Not only has his work shaped the field of echocardiography, it helped establish Duke Heart as one of the premier cardiovascular treatment centers in the world.
We asked Dr. Kisslo’s colleagues to submit their perspective on his work at Duke and what it has meant to them. We received a tremendous response. Without a doubt, Dr. Kisslo is among our most beloved faculty members. Here is what they shared:
“Dr. Kisslo was inclusive even before the term was invented. He elevates people around him, his colleagues, anesthesiologists, sonographers. He is a friend and a teacher, and one of the founding fathers of perioperative echocardiography. Without him, our professional landscape would be different. Thank you!” — Alina Nicoara, MD
“Dr. Joe Kisslo is recognized worldwide for his formative work in the field of echocardiography. His impact on cardiac ultrasound imaging stems from his unique ability to forge lasting collaborative relationships between clinical cardiology, cardiac anesthesia and engineering at Duke resulting in meaningful contributions including phased array ultrasound imaging, Doppler color flow imaging, and transesophageal imaging. He has been honored worldwide for his contributions to the field. I consider myself overwhelming lucky to have been one of his students and colleagues.” – Anita Kelsey, MD
“Dr. Kisslo is a legend in the field of Cardiac Ultrasound. He has been a leader and dedicated professor that has shared his wealth of knowledge and experience with the world. Learning from him has been an honor and a gift that I will cherish and apply to my students.” — Richard A. Palma, Director of the Duke Cardiac Ultrasound Certificate Program
“I feel so privileged to have the opportunity to learn from Dr. Kisslo going over cases almost daily. Thanks to Dr. Kisslo, I will always remember to calculate LV strain patterns at the onset of the QRS complex!! It’s not every day that you get to learn from not only an expert in your field but one of the few who revolutionized the entire world of cardiac ultrasound!” – Sarah H., sonographer
“Vince Lombardi may have said, ‘Perfection is not attainable. But if we chase perfection, we can catch excellence.’ Dr. Kisslo has lived this adage throughout his career, and has taught all of us to not settle for mediocrity. He inspires me to work harder, not to settle for mediocrity, and therefore I believe that I am a better person, both professionally and personally.” – Jean Woolard, sonographer
“Thank you for your pioneering efforts in the field of Perioperative Echocardiography. You were the first to advocate for and actually demonstrate how collaboration between cardiology, cardiac anesthesiology, and cardiac surgery would actually improve the care of our patients. And what a difference that pioneering spirit has made to the field of cardiac anesthesiology and to the generations (including me) that learned from you not just about echocardiography but also of excellence, innovation, and passionate curiosity. Congratulations on this well-deserved award, Doctor, Professor, Reverend Kisslo!” — Joseph Mathew, MD
“Dr. Joseph Kisslo is a true pioneer in the field of echocardiography. While most are familiar with his contributions to the development of the technology and its use in cardiovascular care, few may be aware of his profound influence in the operating room. In the early days of perioperative echo, Joe made countless trips to the operating room to collaborate with surgeons and anesthesiologists and demonstrate the value of echo in patients undergoing cardiac surgery. Whether it was using a TEE probe with a sterile sheath for epicardial echo in pediatric cardiac surgery, or pioneering the use of TEE in adult patients, Joe had a huge impact on an entire generation of cardiac anesthesiologists. He helped us see the immediate results of heart surgery, something we had never envisioned before. As a result, the field developed and Duke has been a leader in perioperative echo ever since, including at ASE, a society he helped create in the mid ’70s. His staunch support of perioperative echo led to the first anesthesiologist leading ASE as president in 2019. I will forever be grateful for his support. Congratulations on this award, Joe!” – Madhav Swaminathan, MD
“When I was in school and at my first job out of state, I was always curious about the clinical impact that the operator dependence of echo has on a patient’s care. During Hi-5, Joe is passionate and a huge advocate for the ongoing training and education of sonographers. He not only advocates for us to think as a sonographer but also as a clinician and about the clinical implications our echo will have on a patient’s care. This has made me much more diligent and helps me think critically about the role that I play in helping answer a clinical question. Through the education and training that Joe provides, I have learned so much in my short time here. I now know what sets our lab, sonographers, and echoes apart from other institutions. What makes for a good echo is not just the latest and greatest machine, but the sonographer that is able to think critically and use the appropriate tools to answer a clinical question. I have no regrets and have zero disappointments in making the move from Arizona. Thanks to Joe and his involvement, the opportunity to work at Duke has lived up to all of my expectations of what it would be like to work at a world renowned institution. Joe has made me proud to be a sonographer here at Duke and I appreciate all that he does.” – Eddy Sandoval, sonographer
“Dr. Kisslo has made a career out of educating all of us in cardiology. Treating us all as brother, sisters, children and grandchildren he never misses a chance to mentor us all. The passion he shows and the high expectations to which he holds us are on the forefront each and every day, making us all better professionals. I am so thankful for the left and right SVC ladder, making 3D “Jelly Beans” and after-hours adult congenital training. Heart dissections and 3D training with experts that I have had the pleasure of working side by side with are unique and valuable opportunities. Joe, thanks so much for pushing us all to be great.” — One of your children of Echo
“Dr. Kisslo, from the moment we sat in his office in 1984 asking if he would help two ignorant cardiac anesthesiologists learn about transesophageal echocardiography, has been continuously supportive of everyone involved in the use of TEE at Duke.
When our first book about TEE was published in 1987, Joe’s foreword included this prescient remark concerning the use of TEE in cardiac anesthesia: “…likely to redefine the requisite fund of knowledge and skills necessary for the practice of cardiovascular anesthesiology in the future.”
Joe’s history with the development of phased array echo transducers is the reason we got hold of HP color flow Doppler probes so early in the game.
His willingness to come to the OR to help with any questions, and his willingness to allow his expert echocardiographers, Kitty Kisslo and David Adams, to help with our education enabled our TEE skills to develop and engendered confidence amongst anesthesiologists and cardiac surgeons.
Cardiologists, not generally used to inserting gastroscope-like echo probes into awake patients, used to come along to the OR induction rooms for assistance in looking for left atrial thrombi and vegetations associated with infectious endocarditis. They were thrilled with the quality of images obtained with the esophageal window.
There again, Joe’s leadership resulted in advances in cardiology practice. His has been a remarkable career, and so many of us lucky to have learned from him.” — Fiona and Norbert (Drs. Norbert de Bruijn and Fiona Clements, now retired)
“It’s hard to put together what to say about Dr. Kisslo because one feels they’ll fall short. He’s a mentor, innovator, father figure, teacher, someone who makes you want to be the best person you can be. I find myself quoting him almost daily at work, especially as I’m educating others. His hunger for knowledge and understanding is contagious. He’s one of the most supportive individuals I’ve ever met. There’s always a challenge he puts forward for us to meet, but it drives us to excel. Thank you Joe for your continual support, we all are better in our careers from it.” — Alicia Armour, Health Center Administrator, Triangle Heart Associates
“‘We are in the relentless pursuit of perfection,’ Dr. Kisslo has instilled this in all of us that have had the privilege of being his students, echo disciples, and friends. Joe has more determination than anyone I have ever met, when many of us would have given up, he just keeps going. He will be there for you in any way he can, both professionally as well as personally. When my mom was diagnosed with cancer, Joe was my first call “who should she see?” and when in the cross-roads of professional decisions, Joe was there to bounce ideas off of (and give me the hard truths). Most importantly, he taught us the 4th of the 3 Rules of Echo: ‘Talk to each other.’” — Ashlee Davis, Chief Technologist, CDU
“I am thrilled to see Dr. Kisslo recognized for his never-ending dedication to the field of Echocardiography. I have so much respect for the time and effort that Dr. Kisslo invests in educating sonographers, physicians, engineering students, and many more at Duke and across the world. His passion for the field of echo is contagious. He makes me want to be better at what I do and made me realize that I can contribute to the advancement and future of echo. Working closely with Dr. Kisslo has emphatically impacted my life both personally and professionally.” – Batina Kight, sonographer
Congratulations, Dr. Kisslo!
Swaminathan to Deliver Edler Lecture

Congratulations to our colleague Madhav Swaminathan, cardiac anesthesiologist and immediate past president of the American Society of Echocardiography (ASE)! He has been selected to deliver the Edler Lecture next weekend at ASE 2021 Scientific Sessions Virtual Experience. The title of his presentation is Echo, Equity, and Empowerment: A Framework for the Future. The annual Edler Lecture honors the founder of echocardiography, Dr. Inge Edler; it was created in 1990.
Shout-out to EKG Support Unit, Daubert & Kraus
A wonderful shout-out to our Duke Heart EKG Support Unit & Diagnostics teams – including Terri DeMuro, Kim Starkey, Duke LifeFlight Event Medicine, Jim Daubert and Bill Kraus!
Hap Zarzour, of Duke Athletics wrote to us in thanks of our annual support of their freshman football player physicals, which were held on Monday, June 7 at Yoh Football Center:
“Thank you everyone for all of your help during freshman football physicals. Things went perfectly, we were able to get all the testing completed as well as an ECHO that afternoon. Amazing. Your hard work and support is so appreciated. I’m so proud of our resources at Duke that enable us to provide care for our athletes and staff, and Duke Cardiology is at the top of the list.” – Robert “Hap” Zarzour, Executive Director of Athletic Medicine
“Kudos to the Duke Heart team for their outstanding commitment and performance once again!”– Jill Engel, Associate Vice President – Heart Services
Shout-out to Team Members on 7700
Rio Landa wrote in earlier this week with a shout-out to team members on 7700. Great work, everyone!
“Big thank you to Brooke, Callie, Dr. Dennis Abraham, and Dr. Jamie Jollis for their help with a sick patient on 7700 last weekend.” – Rio Landa, co-team leader of Cardiology APPs
Patient Compliments from Satisfaction Surveys
Many thanks to Lisa Clark Pickett, Chief Medical Officer, Duke University Hospital for sharing the following two great notes with us!
In the first, Pickett shared, “While reading comments on our Patient Satisfaction Survey I was delighted to read this high compliment of the excellent care provided by your team. Thank you for such outstanding teamwork and care!:
“The various teams of Doctors headed up my Drs. Wang and Milano and the stent placement team were outstanding and worked closely together to solve my blocked arteries without having to resort to open heart surgery. The nurses on floors 3 and 7 were also outstanding especially on floor three. Please give them all my heartfelt thanks!” – Name withheld for confidentiality
Nicely done, Andrew Wang, Carmelo Milano and Floors 3 & 7 Nursing teams!
Her second note stated, “While reading comments on our Patient Satisfaction Survey, I was delighted to read this lovely one about your team. Please share with the wonderful nurses, as their last names were not included. Thank you all for providing such excellent and compassionate care!:
“All of the nurses were exceptional in their card during my stay. Nurse JT in CCU was a great guy to have during a time that I did feel uncomfortable due to the fact that I never stayed in a hospital. Dr. Crawford is excellent as my Cardiologist for my Cath Lab Dr. Jollis was superb in giving me insight into my heart issues. Dr Bloomfield did a noteworthy job in giving me the information on my future Open Heart Surgery. Nurse Andreas and the rest of the RN Staff were exceptional in making sure that I was comfortable and helped me with all my needs during my stay. Duke Cardiology is most definitely a first-class operation that genuinely cares about their patients.” – Name withheld for confidentiality
Great work, Larry Crawford, Jamie Jollis, Gerry Bloomfield & Care teams!
Virtual Town Hall, June 14
A virtual Town Hall, Planning for the Future of Duke Health’s Clinical Enterprise will be held Monday, June 14 from 5-6 p.m. The event is open to all members of the Duke Health community. Panelists will include Eugene Washington, William Fulkerson, Mary Klotman, Thomas Owens, Theodore Pappas and John Sampson. Erica Taylor will moderate. You may submit questions in advance to DHPG@duke.edu. A recording of the town hall will be posted on dukehealthplanning.duke.edu by close of business the following day. To join the Zoom, please click here: Join the Zoom.
Note: Access to the webinar requires authenticated access with your NetID and password. If prompted to sign in, please select to ‘Sign in with SSO’ and enter ‘duke’ when prompted for the company domain. You will be directed to log in with your NetID and password.
Scholars Tip: Global Scholarship
Do you want your research and expertise to appear on the Duke in the World map? It’s as easy as updating your Scholars@Duke profile to reflect your global scholarship! Any global scholarship from your profile is automatically added to the map for others to explore.
Duke scholars represent more than 150 countries with their research, expertise, service, and teaching. Sharing your global scholarship is a great way to connect with other experts who share interest in a particular region.
How to indicate your Global Scholarship:
Make sure your device is connected to the internet, then follow these steps:
- Type duke.edu in your computer’s browser address bar.
- Click Edit My Profile under Update
- Log in using your NetID and password, and then click Manage Your Profile.
- Select Global Scholarship from the Scholarly Output section of the Profile Manager.
- Follow the instructions in the How to Edit box to designate a specific state, country, or continent that you’ve impacted with your work.
- Click Save to update your profile or click Cancel to discard any changes.
Remember to update your Community Outreach
Often, your Global Scholarship involves some form of community outreach, which might include activities such as field work or advocacy. If this applies to you, be sure to indicate these activities in the Outreach and Engaged Scholarship section of your Scholars profile.
Upcoming Opportunities/Save the Date:
Virtual PMWC: Precision Medicine in the Era of a Pandemic Recovery
 June 14-18 – Precision World Medicine Conference. Registration is free and open to all. https://www.pmwcintl.com/covid/
June 14-18 – Precision World Medicine Conference. Registration is free and open to all. https://www.pmwcintl.com/covid/
Duke University Chancellor Emeritus Dr. Ralph Snyderman will lead a panel discussion on Personalized, Proactive Value-Based Care: Emerging New Models.
The confluence of the growth of chronic diseases, the impact of COVID, the emergence of new technologies, and the impact of value-based reimbursement are driving major innovations and changes in care delivery. Proactive, personalized, precision, population-based and digitally supported care is emerging and heralding new approaches to health care. This session will capture the elements of these changes and the dynamics of the forces that are driving them. Perspective from care innovators, large providers and payers will be discussed by the following key opinion leaders:
- Patrick Conway, CEO of Care Solutions, Optum
- Jaewon Ryu, President and Chief Executive Officer, Geisinger
- Rodney Hochman, President & CEO, Providence St. Joseph Health
- Marc Harrison, President and CEO, Intermountain Healthcare
HCPLive State of the Science Summit
June 23: — Institutional Perspectives in Cardiology: Cardiovascular Risk Management webinar with Manesh Patel, Schuyler Jones, Tracy Wang and Christopher Granger. 7 to 8:30 p.m. EST. Virtual. Registration is free. They’ll cover:
- CAD/PAD: Identifying Risk & Summary of Recent Clinical Trials
- Extended Thromboprophylaxis: What Do We Know About Scoring, Risk and Contemporary Trials?
- Atrial Fibrillation: What Have We Learned About NOACs in Special Populations?
- Putting This All Together: Treatment Pyramid
To learn more, please visit: HCPLive Institutional Perspectives in Cardiology.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged.
Duke Heart in the News:
June 4 — Cameron Wolfe
CBS17.com
Heart reaction in 7 teenagers probed as possible rare Pfizer vaccine link
https://bit.ly/3xfo0U2
June 6 — Marc Samsky
Healio/Cardiology Today
Among patients with PAD, those with HF at higher risk for poor outcomes
https://bit.ly/2TWe57o
June 7 — Christopher Granger
WECT News (Wilmington, NC)
Brunswick County EMS to participate in Duke University study
https://bit.ly/3pKgHkG
June 7 — Sunil Rao
Medscape
First Risk Score to Predict Bleeding Risk After TAVR
https://www.medscape.com/viewarticle/952580#vp_1
Division of Cardiology Publications Indexed in PubMed June 3-9, 2021
Butala NM, Makkar R, Secemsky EA, Gallup D, Marquis-Gravel G, Kosinski AS, Vemulapalli S, Valle JA, Bradley SM, Chakravarty T, Yeh RW, Cohen DJ. Cerebral Embolic Protection and Outcomes of Transcatheter Aortic Valve Replacement: Results From the Transcatheter Valve Therapy Registry. Circulation 2021;143(23):2229-2240. PM: 33619968.
Dal-Ré R, Mentz RJ, Rosendaal FR. Thoughtful selection and use of scientific terms in clinical research: the case of ‘pragmatic’ trials. J Investig Med 2021;69(5):1056-1058. PM: 33753535.
Dong R, Leung C, Naert MN, Naanyu V, Kiptoo P, Matelong W, Matini E, Orango V, Bloomfield GS, Edelman D, Fuster V, Manyara S, Menya D, Pastakia SD, Valente T, Kamano J, Horowitz CR, Vedanthan R. Chronic disease stigma, skepticism of the health system, and socio-economic fragility: Qualitative assessment of factors impacting receptiveness to group medical visits and microfinance for non-communicable disease care in rural Kenya. PLoS One 2021;16(6):e0248496. PM: 34097700.
Elliott BA, Holley CL. Assessing 2′-O-Methylation of mRNA Using Quantitative PCR. Methods Mol Biol 2021;2298:171-184. PM: 34085245.
Felker GM, Butler J, Januzzi JL, Desai AS, McMurray JJV, Solomon SD. Probabilistic Readjudication of Heart Failure Hospitalization Events in the PARAGON-HF Study. Circulation 2021;143(23):2316-2318. PM: 34097449.
Kaufman BG, Granger BB, Sun JL, Sanders G, Taylor DH, Mark DB, Warraich H, Fiuzat M, Steinhauser K, Tulsky JA, Rogers JG, O’Connor C, Mentz RJ. The Cost-Effectiveness of Palliative Care: Insights from the PAL-HF Trial. J Card Fail 2021;27(6):662-669. PM: 33731305.
Kennedy DL, Olsen MK, Yang H, Gao X, Alkon A, Prose NS, Dunbar K, Jackson LR, Pollak KI. Communication Coaching in Cardiology (CCC): A study protocol and methodological challenges and solutions of a randomized controlled trial in outpatient cardiology clinics. Contemp Clin Trials 2021;105:106389. PM: 33798730.
Lala A, Mentz RJ. Remembering the Calling – Where Patients and Caregivers Are Front and Center. J Card Fail 2021;27(6):621. PM: 34088378.
Mullan CW, Chouairi F, Sen S, Mori M, Clark KAA, Reinhardt SW, Miller PE, Fuery MA, Jacoby D, Maulion C, Anwer M, Geirsson A, Mulligan D, Formica R, Rogers JG, Desai NR, Ahmad T. Changes in Use of Left Ventricular Assist Devices as Bridge to Transplantation With New Heart Allocation Policy. JACC Heart Fail 2021;9(6):420-429. PM: 33714748.
Perez AL, Grodin JL, Chaikijurajai T, Wu Y, Hernandez AF, Butler J, Metra M, Felker GM, Voors AA, McMurray JJ, Armstrong PW, O’Connor C, Starling RC, Tang WHW. Interleukin-6 and Outcomes in Acute Heart Failure: An ASCEND-HF Substudy. J Card Fail 2021;27(6):670-676. PM: 33497809.
Pfeiffer CT, Wang J, Paulo JA, Jiang X, Gygi SP, Rockman HA. Mapping Angiotensin II Type 1 Receptor-Biased Signaling Using Proximity Labeling and Proteomics Identifies Diverse Actions of Biased Agonists. J Proteome Res 2021;20(6):3256-3267. PM: 33950683.
Rao SV. Real-World Data on the Intravascular Microaxial Left Ventricular Flow Pump (Impella) in High-Risk Patients. Korean Circ J 2021;51(6):487-494. PM: 34085421.
Duke Heart Week ending June 6th 2021
Highlights of the week:
Milano Delivers Inaugural Cohn Lectureship at Tufts

Duke heart surgeon Carmelo Milano, MD, delivered the inaugural American Association of Thoracic Surgery (AATS) Lawrence H. Cohn Visiting Lectureship of Cardiac Surgery at Tufts Medical Center on May 27. Milano’s talk, Heart Transplantation Utilizing Donors after Circulatory Death, was held via Zoom. The Tufts team was unanimously chosen as the inaugural recipient of the AATS/AATS Foundation lectureship award.
The lectureship was established to honor the memory of the late Dr. Lawrence H. Cohn, former president of AATS and a highly-esteemed cardiovascular surgeon who spent the majority of his career in Boston. Cohn died in 2016 at the age of 78. He was the former chief of the Division of Cardiac Surgery at Brigham and Women’s Hospital and held the Virginia and James Hubbard Chair in Cardiac Surgery at Harvard Medical School. Across his career, Cohn performed more than 11,500 cardiac surgical operations and was world-renowned in the field of valve repair and replacement surgery and minimally invasive heart surgery. He was a member of the team that completed the first heart transplant in New England in 1984.
Cohn died in 2016 at the age of 78. He was the former chief of the Division of Cardiac Surgery at Brigham and Women’s Hospital and held the Virginia and James Hubbard Chair in Cardiac Surgery at Harvard Medical School. Across his career, Cohn performed more than 11,500 cardiac surgical operations and was world-renowned in the field of valve repair and replacement surgery and minimally invasive heart surgery. He was a member of the team that completed the first heart transplant in New England in 1984.
“In a nutshell, Dr. Cohn was the consummate academic cardiac surgeon leader and trainer of academic surgeons,” said Frederick Y. Chen, MD, PhD, chief of the Division of Cardiac Surgery at Tufts University School of Medicine and a mentee of Cohn’s. “He wanted to train surgeons who would change and move the field forward.”
The American Association of Thoracic Surgery and AATS Foundation opened applications a year ago to apply for the Cohn Lectureship. As part of the application process, the Tufts team identified Milano as their choice of lecturer if they were to win the award.
Earlier this year, Tufts was approved to begin use of the technology that makes DCD heart transplantation possible. They were eager to hear directly from a surgeon with a high level of expertise in DCD who is also a leader within AATS.
“When I surveyed the field, I felt there really is no other surgeon with the expertise of Dr. Milano in the U.S. who performs DCD transplants,” added Chen. “Moreover, I’ve known about Dr. Milano for a very long time. He, too, is a consummate academic cardiac surgeon. He has an R01; he operates, and he’s a teacher – so he really is the traditional triple threat surgeon. We felt, as an internationally known senior AATS member and a highly-regarded educator and mentor, that he would be a great fit for this.”
As part of the lectureship, the Tufts team held a tribute to Dr. Cohn and a meet-and-greet so that all members of their cardiovascular and thoracic surgery teams, including PAs, perfusionists, and anesthesiologists, as well as members of leadership and their administration could participate. The tribute and lecture were attended by family members of the late Dr. Cohn.
McGarrah, Southerland Receive Strong Start awards


Congratulations to Rob McGarrah, assistant professor of medicine in cardiology, researcher in the Cardiovascular Research Center (CVRC) and member of the Duke Molecular Physiology Institute; and to Kevin Southerland, assistant professor of surgery in the division of vascular and endovascular surgery, who has done considerable research in the CVRC lab of Christopher Kontos. They are two of six physician scientists in the Duke School of Medicine who were selected to receive Strong Start Awards.
McGarrah’s research has made strides in answering the question of how a disease in the liver can affect a distant organ like the heart. He and his collaborators have found that obesity turns off a certain metabolism pathway in the liver, leading to non-alcoholic fatty liver disease and also increasing the levels of specific amino acids (building blocks of proteins) in the blood. When these amino acids are delivered to the heart, they cause the heart to store more fat, which is unhealthy, and to make more protein, which can cause unhealthy heart muscle thickening. This liver-heart cross talk might explain why non-alcoholic fatty liver disease causes abnormal heart function.
The overall goal of the Kontos lab is to understand how blood vessels grow and remodel in response to both pathological and physiological stimuli as well as how they maintain normal tissue function, a process known as vascular homeostasis. The work that Dr. Southerland did in the Kontos lab focused specifically on how genetics influence muscle injury following ischemia in a mouse model.
The Strong Start Award program is designed to nurture the careers of junior, laboratory-based physician-scientists at Duke. By offering substantive mentoring and financial resources, the award supports junior faculty during a critical period of their career — the transition to research independence. Each award is for $75,000 per year, renewable up to three consecutive years ($225,000 total). The funds are to be used at the discretion of the individual recipient to support their research program.
Congratulations Rob and Kevin!
Katz, Arps & Sullivan Receive Year-End Medicine Awards



Congratulations to Jason Katz; third-year cardiology fellow Kelly Arps; and incoming fellow Lonnie Sullivan! Katz was awarded the Internal Medicine residency program’s Eugene Stead Faculty Teaching Award given to the faculty who best exemplifies the principles of teach from Dr. Steads time at Duke; Arps received the Fellow Teaching Award and Sullivan received the Haskell Schiff Award for Excellence, which is peer-selected and given to the house staff member who best represents the ideal of the program. The awards, presented annually by Duke’s Internal Medicine Chief Residents, were presented on Friday, June 4 during Medicine Grand Rounds. We are so proud of you!
McKee Retiring from Heart Center Communications
 Vickie McKee, a transitional care nurse with Heart Center Communications, will retire from Duke University Health System at the end of June. She has been working at Duke for 43 years. A certified Basic Life Support Instructor and Heart Failure Nurse, McKee was one of the first recipients of Duke’s Friends of Nursing Award, receiving it in 1989 and again in 1999. She has co-authored several poster presentations related to heart failure, and shepherded a number of projects to advance education for patients, including iPad Technology for Heart Failure Education that involved a collaboration between the Duke Transitional Nursing Institute and DCRI/Duke Center for Learning Health Care. Another such project was Heart at Home, Transition in Care where she assisted in the development of a DVD used to educate heart failure patients transitioning from the hospital to home and back to clinic.
Vickie McKee, a transitional care nurse with Heart Center Communications, will retire from Duke University Health System at the end of June. She has been working at Duke for 43 years. A certified Basic Life Support Instructor and Heart Failure Nurse, McKee was one of the first recipients of Duke’s Friends of Nursing Award, receiving it in 1989 and again in 1999. She has co-authored several poster presentations related to heart failure, and shepherded a number of projects to advance education for patients, including iPad Technology for Heart Failure Education that involved a collaboration between the Duke Transitional Nursing Institute and DCRI/Duke Center for Learning Health Care. Another such project was Heart at Home, Transition in Care where she assisted in the development of a DVD used to educate heart failure patients transitioning from the hospital to home and back to clinic.
Vickie’s last official day with us will be Wednesday, June 30. Please offer her your warm congratulations this month. We know she will be missed!
Members of the HCC team shared these thoughts with us:
“I was thrilled when Vickie joined the Heart Center Communications team as a cardiology transitional care nurse, where we provide our inpatient cardiology patients with post discharge follow up telephone calls. She has brought a wealth of cardiac nursing knowledge and skill to our team, and it has been an honor to work with Vickie and to learn from her. She has served in many nursing roles during her years here at Duke, and each of these roles have played a part in the nursing expertise that she has brought to our team. I have seen her provide such genuine and exemplary care to her patients; she has truly had a positive impact on so many lives. I am so proud to call her my friend and colleague, and I wish her all the best as she enters into the next chapter in her life. I will miss her!” — Cheryl Swartz, Cardiology Transitional Care Nurse, HCC
“Vickie is a great nurse, coworker, and friend. She is compassionate with patients and their families. I wish her the best in this next phase of her life.” — Ruth B. Cavales, Transitional Care Nurse, HCC
“Vickie’s compassion and experience will be greatly missed.” — Michael Blazing, Medical Director; Greg Shelton, Administrative Director; and Gina Nesmith, Nurse Program Manager; HCC.
Wegermann Closes Out CGR
 Zach Wegermann was the closer for the 2020-21 Cardiology Grand Rounds season on Tuesday, June 1. Wegermann presented research that utilized several different registries to gain insights on various questions related to interventional cardiology. His work showed that patients receiving MitraClip had larger improvements in quality of life outcomes, as measured by Kansas City Cardiomyopathy Questionnaire (KCCQ) scores, when they had lower baseline KCCQ score prior to the procedure. Another project highlighted that intraoperative TEE during CABG frequently reveals worse-than-expected valvular disease, leading to unplanned valve repair or replacement. Notably, there is wide variance across centers in the usage of intraoperative TEE for CABG, raising the question of whether a more standardized approach is needed. The lecture was not recorded for potential PHI reasons, but we are sure that Dr. Wegermann would be happy to field any follow-up questions. You can read the published results here.
Zach Wegermann was the closer for the 2020-21 Cardiology Grand Rounds season on Tuesday, June 1. Wegermann presented research that utilized several different registries to gain insights on various questions related to interventional cardiology. His work showed that patients receiving MitraClip had larger improvements in quality of life outcomes, as measured by Kansas City Cardiomyopathy Questionnaire (KCCQ) scores, when they had lower baseline KCCQ score prior to the procedure. Another project highlighted that intraoperative TEE during CABG frequently reveals worse-than-expected valvular disease, leading to unplanned valve repair or replacement. Notably, there is wide variance across centers in the usage of intraoperative TEE for CABG, raising the question of whether a more standardized approach is needed. The lecture was not recorded for potential PHI reasons, but we are sure that Dr. Wegermann would be happy to field any follow-up questions. You can read the published results here.
Looking forward, CGR will be on summer break until September 14, when we will kick off the 2021-22 academic year with Dr. Robert Lefkowitz as our guest speaker.
Krasuski Grand Rounds Presentation, Mass General
Rich Krasuski, director of our Adult Congenital Heart Disease Center, was the guest presenter for Cardiology Grand Rounds at Mass General Hospital (MGH) on June 2. A recorded presentation of his talk, The Complexities of Managing Pulmonary Hypertension in Congenital Heart Disease, can be found here; a pre-grand rounds interview with Krasuski, conducted by Mostafa Al-Alusi, a first-year cardiovascular disease fellow at MGH, can be found here.
Fast Track Extubation Article in AACN
 Congratulations to our 7W research team, including Myra Ellis, Heather Pena, Allen Cadavero, Debra Farrell, Mollie Kettle, Alexandra Kaatz, Tonda Thomas, Bradi Granger and Kamrouz Ghadami! Their article, Reducing Intubation Time in Adult Cardiothoracic Surgery Patients With a Fast-track Extubation Protocol is the cover article in the June 2021 issue of Critical Care Nurse (CCN), one of the journals of the American Association of Critical-Care Nurses. The publication is available online and can be found here. Be sure to check out the associated article appearing in HealthLeaders below in “Duke Heart in the News.”
Congratulations to our 7W research team, including Myra Ellis, Heather Pena, Allen Cadavero, Debra Farrell, Mollie Kettle, Alexandra Kaatz, Tonda Thomas, Bradi Granger and Kamrouz Ghadami! Their article, Reducing Intubation Time in Adult Cardiothoracic Surgery Patients With a Fast-track Extubation Protocol is the cover article in the June 2021 issue of Critical Care Nurse (CCN), one of the journals of the American Association of Critical-Care Nurses. The publication is available online and can be found here. Be sure to check out the associated article appearing in HealthLeaders below in “Duke Heart in the News.”
Heart Center Leadership Council Spring Meeting Held
The Heart Center Leadership Council held their spring meeting on Friday, May 21 via Zoom. The Council has welcomed four new members over the past year: Kathy Finley, Brad Branch, Chuck Swoboda and Dennis Wicker.
Manesh Patel and Edward Chen, co-directors of Duke Heart Center, provided a general overview of our programs, an update on our latest research and how the pandemic impacted us. The Council then heard a great presentation on the Heart Transplant program from Jacob Schroder and Chet Patel, who covered major milestones from across the past year.
Some comments from the meeting:
“I just wanted to say how blessed I think we are to have Duke and Duke Heart in our neighborhood as well as southeast United States. I am impressed and proud of what is being done — thank you!” — Robb Teer, member, Heart Center Leadership Council
“So impressed by the energy, innovation and courage it takes to do things differently.” Donna Childress, member, Heart Center Leadership Council
The HCLC will meet again in October.
Duke Health Closes COVID-19 Command Centers
At the beginning of the COVID-19 pandemic, Duke established Hospital Incident Command Structure (HICS) command centers that allowed for close monitoring and quick adjustments to every part of our operations across the health system. Due to the significant decrease in the spread of infection, Duke has closed all COVID-19 command centers as of June 1. DUHS leadership will continue to monitor COVID-19 and keep safe practices in place. However, the command center closures represent the end of Duke Health’s official emergency response efforts.
COVID Hotline Hours as of June 1
As of June 1, the COVID hotline hours of operation for patients, Duke employees and students are as follows:
Employee Hotline: 8 a.m. – 6 p.m., daily. For urgent after-hours concerns, call the Blood and Body Fluids Hotline at 919-684-8115.
Vaccine Hotline: 8 a.m. – 6 p.m., Monday – Saturday.
Patient Hotline: 8 a.m. – 6 p.m., Monday – Saturday. There will remain an option to reach Nurse Triage from 6 p.m. – 8 p.m. and Sundays from 8 a.m. – 8 p.m. for symptomatic and exposed patients.
Student Hotline: 8 a.m. – 8 p.m. daily.
Asymptomatic Testing Hotline: 8 a.m. – 5 p.m., Monday – Saturday.
Scholars Tip: Showcase Your Presentations
Did you know your Scholars@Duke profile has a spot for all of your important invited talks and keynotes? Your Scholars profile is the ultimate tool to demonstrate your contributions to the Duke community and enable discovery of your work. Be sure to list any notable presentations (conferences, lectures, interviews, invited talks, keynotes, etc.) you want others to notice.
How to display notable appearances on your Scholars profile
Make sure your device is connected to the internet, then follow these steps:
- Type scholars.duke.edu in your computer’s browser address bar.
- Click Edit My Profile under Update
- Log in using your NetID and password, and then click Manage Your Profile.
- Select Global Scholarship from the Scholarly Output section of the Profile Manager.
- Scroll down to the Professional Activities section, expand the Recognition heading, then click Presentations & Appearances.
- Click Add and complete the required fields to describe your presentation and provide a link to any related materials, then click save. Repeat this step for every presentation you wish to display on your profile.
Information contained in your Scholars@Duke profile feeds into other websites at Duke, so it’s good to keep your Scholars profile as up to date as possible.
Upcoming Opportunities/Save the Date:
Virtual PMWC: Precision Medicine in the Era of a Pandemic Recovery
June 14-18 – Precision World Medicine Conference. Registration is free and open to all. https://www.pmwcintl.com/covid/
 Duke University Chancellor Emeritus Dr. Ralph Snyderman will lead a panel discussion on Personalized, Proactive Value-Based Care: Emerging New Models.
Duke University Chancellor Emeritus Dr. Ralph Snyderman will lead a panel discussion on Personalized, Proactive Value-Based Care: Emerging New Models.
The confluence of the growth of chronic diseases, the impact of COVID, the emergence of new technologies, and the impact of value-based reimbursement are driving major innovations and changes in care delivery. Proactive, personalized, precision, population-based and digitally supported care is emerging and heralding new approaches to health care. This session will capture the elements of these changes and the dynamics of the forces that are driving them. Perspective from care innovators, large providers and payers will be discussed by the following key opinion leaders:
- Patrick Conway, CEO of Care Solutions, Optum
- Jaewon Ryu, President and Chief Executive Officer, Geisinger
- Rodney Hochman, President & CEO, Providence St. Joseph Health
- Marc Harrison, President and CEO, Intermountain Healthcare
HCPLive State of the Science Summit
June 23: — Institutional Perspectives in Cardiology: Cardiovascular Risk Management webinar with Manesh Patel, Schuyler Jones, Tracy Wang and Christopher Granger. 7 to 8:30 p.m. EST. Virtual. Registration is free. They’ll cover:
- CAD/PAD: Identifying Risk & Summary of Recent Clinical Trials
- Extended Thromboprophylaxis: What Do We Know About Scoring, Risk and Contemporary Trials?
- Atrial Fibrillation: What Have We Learned About NOACs in Special Populations?
- Putting This All Together: Treatment Pyramid
To learn more, please visit: HCPLive Institutional Perspectives in Cardiology.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged.
Duke Heart in the News:
May 26 — Manesh Patel
Weather.com/TWC India
Individuals Advised to Look Out for Symptoms of Heart Problems After COVID-19 Vaccine Shot
https://bit.ly/3g1Uv0M
May 27 — W. Schuyler Jones
TheDoctorWillSeeYouNow.com
Aspirin for Heart Disease? Less May Be More
https://www.thedoctorwillseeyounow.com/content/heart/art6404.html
May 27 — Manesh Patel
PennLive.com/Patriot News
CDC investigates a potential link between COVID-19 vaccines and heart problem seen in young people
https://bit.ly/3wSA650
May 30 — Harry Severance
CNBC.com
Covid has made it harder to be a health-care worker. Now, many are thinking of quitting
https://cnb.cx/34Hmwpk
*carried by 26 other news outlets
May 31 — Daniel Mark
PhysiciansWeekly.com
Dapagliflozin Is Cost-Effective in HFrEF, But Is It Affordable?
https://bit.ly/2RlEbzO
June 3 — Daniel Mark and Derek Chew
MDEdge.com
Dapagliflozin’s cost-effectiveness ‘intermediate’ for HFrEF
https://bit.ly/3vVI90V
June 3 — Myra Ellis
HealthLeaders
Nursing Researchers Safely Decrease Ventilation Time for Cardiac Surgery Patients
https://bit.ly/2Sc2xfx
Division of Cardiology Publications Indexed in PubMed May 27-June 2, 2021
Bernstein RA, Kamel H, Granger CB, Piccini JP, Sethi PP, Katz JM, Vives CA, Ziegler PD, Franco NC, Schwamm LH. Effect of Long-term Continuous Cardiac Monitoring vs Usual Care on Detection of Atrial Fibrillation in Patients With Stroke Attributed to Large- or Small-Vessel Disease: The STROKE-AF Randomized Clinical Trial. JAMA 2021;325(21):2169-2177. PM: 34061145.
Bihlmeyer NA, Kwee LC, Clish CB, Deik AA, Gerszten RE, Pagidipati NJ, Laferrère B, Svetkey LP, Newgard CB, Kraus WE, Shah SH. Metabolomic profiling identifies complex lipid species and amino acid analogues associated with response to weight loss interventions. PLoS One 2021;16(5):e0240764. PM: 34043632.
Chow C, Mentz RJ, Greene SJ. Update on the Impact of Comorbidities on the Efficacy and Safety of Heart Failure Medications. Curr Heart Fail Rep 2021;18(3):132-143. PM: 33835396.
Garza MY, Rutherford MW, Adagarla B, Eisenstein E, Kumar KR, Zimmerman KO, Topaloglu U, Zozus M. Evaluating Site-Level Implementations of the HL7 FHIR Standard to Support eSource Data Exchange in Clinical Research. Stud Health Technol Inform 2021;281:397-401. PM:
34042773
Gutierrez JA, Samsky MD, Schulteis RD, Gu L, Swaminathan RV, Aday AW, Rao SV. Venous thromboembolism among patients hospitalized with COVID-19 at Veterans Health Administration Hospitals. Am Heart J 2021;237:1-4. PM: 33745899.
Jones WS, Mulder H, Wruck LM, Pencina MJ, Kripalani S, Muñoz D, Crenshaw DL, Effron MB, Re RN, Gupta K, Anderson RD, Pepine CJ, Handberg EM, Manning BR, Jain SK, Girotra S, Riley D, DeWalt DA, Whittle J, Goldberg YH, Roger VL, Hess R, Benziger CP, Farrehi, et al. Comparative Effectiveness of Aspirin Dosing in Cardiovascular Disease. N Engl J Med 2021;384(21):1981-1990. PM: 33999548.
Lowenstern A, Sheridan P, Wang TY, Boero I, Vemulapalli S, Thourani VH, Leon MB, Peterson ED, Brennan JM. Sex disparities in patients with symptomatic severe aortic stenosis. Am Heart J 2021;237:116-126. PM: 33722584.
Mentz RJ, Pulungan Z, Kim S, Yang M, Teigland C, Hilkert R, Djatche LM. Quality outcomes, healthcare resource utilization and costs in Medicare patients with chronic heart failure with reduced ejection fraction with and without a worsening event. J Med Econ 2021;24(1):698-705. PM: 33900874.
Pagidipati NJ, Svetkey LP. Time for a Renewed Focus on the DASH-Low Sodium Diet. J Am Coll Cardiol 2021;77(21):2635-2637. PM: 34045019.
Rymer JA, Webb L, McCall D, Hills MT, Wang TY. Differences in Preferences Between Clinicians and Patients for the Use and Dosing of Direct Oral Anticoagulants for Atrial Fibrillation. J Am Heart Assoc 2021;10(11):e020697. PM: 33998252.
Sliwa K, Singh K, Raspail L, Ojji D, Lam CSP, Thienemann F, Ge J, Banerjee A, Newby LK, Ribeiro ALP, Gidding S, Pinto F, Perel P, Prabhakaran D. The World Heart Federation Global Study on COVID-19 and Cardiovascular Disease. Glob Heart 2021;16(1):22. PM: 34040935.
Southwell BG, Wood JL, Navar AM. Función de los profesionales de la salud de rectificar la información errónea que tienen los pacientes más allá de corregir los hechos. Rev Panam Salud Publica 2021;45:e60. PM: 34035798.
Turakhia M, Sundaram V, Smith SN, Ding V, Michael Ho P, Kowey PR, Piccini JP, Foody J, Birmingham MC, Ianus J, Rajmane A, Mahaffey KW, et al. Efficacy of a centralized, blended electronic, and human intervention to improve direct oral anticoagulant adherence: Smartphones to improve rivaroxaban ADHEREnce in atrial fibrillation (SmartADHERE) a randomized clinical trial. Am Heart J 2021;237:68-78. PM: 33676886.
Duke Heart Updates – May 30th 2021
Chief’s message: Memorial Day Weekend
It’s a traditional start to the summer, Memorial Day weekend with the Indianapolis 500 and many end of the academic year festivities coming up including graduating medical school students, residents going to fellowships or jobs, and fellows finishing to start their careers as cardiologists. Some of the weekend is also spent remembering the tremendous sacrifices of the women and men in the armed services that allow us the freedoms that we have today. This Memorial Day, we reflect on their sacrifice and the debt we owe our fallen service members and their families.
It would also be hard not to remember our ongoing battle with the COVID-19 pandemic where one year ago today we were trying to keep the COVID related deaths under 100,000 and thinking of ways in which we could continue to safely care for our patients and each other. One year has made a tremendous difference, and we are blessed to have kept our fellows, faculty, and staff healthy with continued focus on serving our local community and the broader missions of academic discovery and training. So, as our health system, faculty, and school are working to determine an aligned way forward in which we can better meet the needs of our community, our clinical and academic missions, I am encouraged by the resiliency and teamwork of all of you at Duke Heart. Together we are stronger and the mission to improve Heart Health remains our true north. You will see in the updates this week that we have kept pushing to develop new ways to educate, innovate, and care for our patients.
Highlights of the week:
 Cardiac Ultrasound Certificate Program Receives CAAHEP Accreditation
Cardiac Ultrasound Certificate Program Receives CAAHEP Accreditation
Congratulations to our Duke Cardiac Ultrasound Certificate Program team led by Richie Palma and Anita Kelsey! They have been granted initial accreditation by the Board of Directors of the Commission on Accreditation of Allied Health Education Programs (CAAHEP). The CAAHEP Board acted upon the accreditation recommendation of the Joint Review Committee on Education in Cardiovascular Technology (JRC-CVT). The decision was made during the CAAHEP board meeting held May 21.
Through the accreditation process, which includes a thorough review of the program, curriculum, resources, faculty and staff, as well as a site visit, the Duke program was determined to be in substantial compliance with the nationally-approved Standards and Guidelines for educational programs. The CAAHEP Standards by which the program was measured has been developed primarily by Cardiovascular Technology professionals, are approved by each profession’s sponsoring organizations, and are intended to reflect required knowledge and skills that a person needs to be able to successfully function within the Cardiovascular Technology profession. CAAHEP Standards focus on quality outcomes, assuring that educational programs are preparing competent Cardiovascular Technology professionals.
CAAHEP accredits more than 2,200 educational programs that prepare health professionals in 32 different disciplines. Accreditation is a critical step in a process that is meant to protect the public and ensure a supply of qualified health care professionals. For more information about CAAHEP and accreditation, visit www.caahep.org.
The Duke Cardiac Ultrasound Certificate Program will graduate its first class in August. The team will be adding a six-month pediatric training program this fall.
Cath Team Performs Duke’s 1st Coronary Angiogram Using Transmedics System
 Congratulations to Jennifer Rymer, Angela Lowenstern, Robyn Strong, Meghan Ronn, Michaela Fahn and Shawna Walker (not pictured) – the team completed Duke’s first coronary angiogram using the Transmedics Organ Care System (OCS) to assess the coronary arteries of a donor heart in the catheterization lab.
Congratulations to Jennifer Rymer, Angela Lowenstern, Robyn Strong, Meghan Ronn, Michaela Fahn and Shawna Walker (not pictured) – the team completed Duke’s first coronary angiogram using the Transmedics Organ Care System (OCS) to assess the coronary arteries of a donor heart in the catheterization lab.
“We now have one of the largest experiences with the Transmedics OCS in the world, but have not – until this week—had to assess the coronary arteries of the donor heart once it was on the device,” said Chet Patel. “We had discussed the need for doing this on a few occasions in the past, but this was the first time we had to complete one.”
Very few such procedures have been done worldwide among medical centers currently using the Transmedics OCS, according to Patel. Congratulations, team!
Chen Named to JTCVS Editorial Board; Klapper, Andersen Earn Ed Board Awards
Congratulations to Edward P. Chen, chief of the division of Cardiovascular and Thoracic Surgery – he has been named to the editorial board of the Journal of Thoracic and Cardiovascular Surgery (JTCVS). He joins a number of Duke colleagues there, including Tom D’Amico, Nick Andersen, Don Glower, Matt Hartwig, Jacob Klapper, Jerrold Levy, Andrew Lodge, Betty Tong and Joe Turek.
“For me, this is a tremendous honor. JTCVS is arguably the leading CT surgery journal in North America and to be asked to serve in this capacity is a tremendous privilege,” said Chen. “Getting a manuscript accepted into this journal has always been recognized as very difficult and I hope to continue to uphold these high publication standards as a member of the Editorial Board. I am extremely pleased that we have such robust representation of our Duke CT faculty on this Board which is reflective of the emphasis we put on discovery and academic pursuits in our Division.”
Congratulations also to Jacob Klapper and Nick Andersen who were both recognized by the JTCVS with 2021 Editorial Board Awards – which are based on overall average ratings as a reviewer. The average is calculated from the number of papers that reviewers accept for review, the percentage of those completed on time, and the number of reviews that score higher than 70%. “I find reviewing the papers a vital part of continuing to read and assess the medical literature critically as well an opportunity to gain new and valuable insights into my field,” said Klapper.
Excellent work!
Bishawi, Randles Honored with Novim AJN Award
 Muath Bishawi, a cardiothoracic surgery resident in our Integrated Thoracic Surgery Residency Program, and Amanda Randles, the Alfred Winborne and Victoria Stover Mordecai Assistant Professor of Biomedical Sciences at Duke, have been honored by Novim with an Alexandra Jane Noble Award. AJN awards are given for innovations contributing to world health, social impact, increasing awareness and new discovery. The awards, now in their fourth year, honor efforts to communicate complex topics in innovative, engaging ways to stimulate higher awareness of scientific issues, particularly in young adults.
Muath Bishawi, a cardiothoracic surgery resident in our Integrated Thoracic Surgery Residency Program, and Amanda Randles, the Alfred Winborne and Victoria Stover Mordecai Assistant Professor of Biomedical Sciences at Duke, have been honored by Novim with an Alexandra Jane Noble Award. AJN awards are given for innovations contributing to world health, social impact, increasing awareness and new discovery. The awards, now in their fourth year, honor efforts to communicate complex topics in innovative, engaging ways to stimulate higher awareness of scientific issues, particularly in young adults.
Bishawi and Randles were given the 2021 Science Inspiration Award; the colleagues made fundamental contributions to engineering with their split ventilator prototype. With ventilators in high demand during the COVID-19 pandemic, Dr. Randles and Dr. Bishawi created a ventilator splitter and resistor system (VSRS) which enables one ventilator to support two or more patients. A full article about their ventilator system can be found here. Don’t miss this Microsoft Inspire video about the computational models used in development: https://www.youtube.com/watch?v=B55viclEWLc&t=640s
A full listing of all 2021 Novim awardees can be found here. The awards, announced earlier this year, were presented on Wednesday, May 26.
Congratulations, Muath! We are so proud of you!
UPDATE: Risk Capture & HCC Coding: CV Disease
Clinical providers, please review this updated PowerPoint we have sent from Drs. Momen Wahidi and Dev Sangvai on the importance of Risk Adjustment Factor (RAF) documentation. Please take time to review slides 12-18 that highlight documentation tips with patients for the following cardiovascular related conditions: Specified Heart Arrhythmias, Vascular Disease, Angina Pectoris, and Opportunities in Cardiovascular Disease. For additional information, please contact: Momen Wahidi. Thank you!
All Three Duke Hospitals among Top Performing for Treatment of MI
 Congratulations to our teams at Duke Raleigh Hospital, Duke University Hospital and Duke Regional Hospital – all three hospitals are recipients of the American College of Cardiology’s NCDR Chest Pain ̶ MI Registry Platinum Performance Achievement Award for 2021. Only 212 hospitals nationwide have received the honor.
Congratulations to our teams at Duke Raleigh Hospital, Duke University Hospital and Duke Regional Hospital – all three hospitals are recipients of the American College of Cardiology’s NCDR Chest Pain ̶ MI Registry Platinum Performance Achievement Award for 2021. Only 212 hospitals nationwide have received the honor.
To receive the Chest Pain ̶ MI Registry Platinum Performance Achievement Award, hospitals must demonstrate sustained achievement in the Chest Pain ̶ MI Registry for two consecutive years (2019 and 2020), and perform at the highest level for specific performance measures. Full participation in the registry engages hospitals in a robust quality improvement process using data to drive improvements in adherence to guideline recommendations and overall quality of care provided to heart attack patients.
This award is evidence of the hard work and commitment it takes to deliver the highest quality in cardiovascular care to transform heart health. Congratulations to all involved in our Chest Pain – MI Registry!
AACN NTI Poster Presentation
 Congratulations to members of the Duke Cardiac Catheterization Lab! They had a poster presentation at the American Association of Critical Care Nurses 2021 National Teaching Institute & Critical Care Exposition. Their poster, Improving Adoption of Evidenced-Based Chlorohexidine Skin Prep Prior to Cardiac Catheterization, authored by Robyn Strong and Cassidy Johnson, demonstrated results of how the cath lab team worked together to improve scrub time, scrub technique and prep dry time to >95% compliance. Great job, everyone!
Congratulations to members of the Duke Cardiac Catheterization Lab! They had a poster presentation at the American Association of Critical Care Nurses 2021 National Teaching Institute & Critical Care Exposition. Their poster, Improving Adoption of Evidenced-Based Chlorohexidine Skin Prep Prior to Cardiac Catheterization, authored by Robyn Strong and Cassidy Johnson, demonstrated results of how the cath lab team worked together to improve scrub time, scrub technique and prep dry time to >95% compliance. Great job, everyone!
High Five: Clinic 2F/2G
Our 2F/2G Duke South Clinic team was nominated for a “high five” recently by Carolyn Lekavich. In her nomination, she wrote, “I want to recognize the exceptional team that we have at 2F/2G. I can’t say enough about the exceptional care, compassion, and humanistic style that the entire team provides, every day, for our patients and each other!”
Nicely done, team!
COVID-19 Updates:
All the latest official DUHS information regarding coronavirus/COVID-19 response at the following locations:
Upcoming Opportunities/Save the Date:
Virtual PMWC: Precision Medicine in the Era of a Pandemic Recovery
June 14-18 – Precision World Medicine Conference. Registration is free and open to all. https://www.pmwcintl.com/covid/
Duke University Chancellor Emeritus Dr. Ralph Snyderman will lead a panel discussion on Personalized, Proactive Value-Based Care: Emerging New Models.
The confluence of the growth of chronic diseases, the impact of COVID, the emergence of new technologies, and the impact of value-based reimbursement are driving major innovations and changes in care delivery. Proactive, personalized, precision, population-based and digitally supported care is emerging and heralding new approaches to health care. This session will capture the elements of these changes and the dynamics of the forces that are driving them. Perspective from care innovators, large providers and payers will be discussed by the following key opinion leaders:
- Patrick Conway, CEO of Care Solutions, Optum
- Jaewon Ryu, President and Chief Executive Officer, Geisinger
- Rodney Hochman, President & CEO, Providence St. Joseph Health
- Marc Harrison, President and CEO, Intermountain Healthcare
HCPLive State of the Science Summit
June 23: — Institutional Perspectives in Cardiology: Cardiovascular Risk Management webinar with Manesh Patel, Schuyler Jones, Tracy Wang and Christopher Granger. 7 to 8:30 p.m. EST. Virtual. Registration is free. They’ll cover:
- CAD/PAD: Identifying Risk & Summary of Recent Clinical Trials
- Extended Thromboprophylaxis: What Do We Know About Scoring, Risk and Contemporary Trials?
- Atrial Fibrillation: What Have We Learned About NOACs in Special Populations?
- Putting This All Together: Treatment Pyramid
To learn more, please visit: HCPLive Institutional Perspectives in Cardiology.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged.
Duke Heart in the News:
May 18 — Harry Severance, Jr.
ACEPNow.com
Unintended Consequences of Vaccine “Passports”
https://bit.ly/34j3fds
May 21 — Harry Severance, Jr.
CNBC/Travel
Unvaccinated Americans are less worried about traveling than vaccinated Americans are, study says
https://cnb.cx/3ugD95v
May 21 — Sunil Rao
tctMD
Transradial PCI Bests Femoral Access in Complex Cases: COLOR
https://bit.ly/3hXAJ98
May 24 — Manesh Patel
NBCNews.com
CDC looking into possible link between heart problem and Covid vaccines in young people
https://nbcnews.to/3voTsi7
May 25 — W. Schuyler Jones
WebMD
‘Baby’ Aspirin As Effective As High-Dose for Heart
https://wb.md/3fNmcdB
Division of Cardiology Publications Indexed in PubMed May 20-26, 2021
Aktaş MK, Younis A, Zareba W, Kutyifa V, Klein H, Daubert JP, Estes M, McNitt S, Polonsky B, Goldenberg I. Survival After Implantable Cardioverter-Defibrillator Shocks. J Am Coll Cardiol 2021;77(20):2453-2462. PM: 34016257.
Barnett AS, Kiefer T, Kim HW, Mitchell M, Jackson KP, Piccini JP, Koontz JI, Sun AY. Ablation of Ventricular Tachycardia Storm With Coronary Venous Ethanol. JACC Clin Electrophysiol 2021;7(5):682-683. PM: 34016399.
Chiamvimonvat N, Frazier-Mills C, Shen ST, Avari Silva JN, Wan EY. Sex and Race Disparities in Presumed Sudden Cardiac Death: One Size Does Not Fit All. Circ Arrhythm Electrophysiol 2021;14(5):e010053. PM: 33993706.
Chouairi F, Pacor J, Miller PE, Fuery MA, Caraballo C, Sen S, Leifer ES, Felker GM, Fiuzat M, O’Connor CM, Januzzi JL, Friedman DJ, Desai NR, Ahmad T, Freeman JV. Effects of Atrial Fibrillation on Heart Failure Outcomes and NT-proBNP Levels in the GUIDE-IT Trial. Mayo Clin Proc Innov Qual Outcomes 2021;5(2):447-455. PM: 33997640.
Chrispin J, Frazier-Mills C, Sogade F, Wan EY, Clair WK. Pandemic Highlights Disparities in Health Care. Circ Arrhythm Electrophysiol 2021;14(5):e009908. PM: 33993701.
Forrest CB, Xu H, Thomas LE, Webb LE, Cohen LW, Carey TS, Chuang CH, Daraiseh NM, Kaushal R, McClay JC, Modave F, Nauman E, Todd JV, Wallia A, Bruno C, Hernandez AF, O’Brien EC. Impact of the Early Phase of the COVID-19 Pandemic on US Healthcare Workers: Results from the HERO Registry. J Gen Intern Med 2021;36(5):1319-1326. PM: 33694071.
Gargiulo G, Cannon CP, Gibson CM, Lopes RD, Vranckx P, Valgimigli M. The multiplication of loaves and fishes approach: a critic to double anti-thrombotics or to double number of ischaemic events? Eur Heart J Cardiovasc Pharmacother 2021;7(3):e29-e30. PM: 33340322.
Huang HI, Jewell ML, Youssef N, Huang MN, Hauser ER, Fee BE, Rudemiller NP, Privratsky JR, Zhang JJ, Reyes EY, Wang D, Taylor GA, Gunn MD, Ko DC, Cook DN, Chandramohan V, Crowley SD, Hammer GE. Th17 Immunity in the Colon Is Controlled by Two Novel Subsets of Colon-Specific Mononuclear Phagocytes. Front Immunol 2021;12:661290. PM: 33995384.
Lopes RD, Alexander KP, Hochman JS, Maron DJ. Response by Lopes et al to Letter Regarding Article, “Initial Invasive Versus Conservative Management of Stable Ischemic Heart Disease Patients With a History of Heart Failure or Left Ventricular Dysfunction: Insights From the ISCHEMIA Trial”. Circulation 2021;143(20):e961-e962. PM: 33999666.
Mentz RJ, Ambrosy AP, Ezekowitz JA, Lewis GD, Butler J, Wong YW, De Pasquale CG, Troughton RW, O’Meara E, Rockhold FW, Garg J, Samsky MD, Leloudis D, Dugan M, Mundy LM, Hernandez AF. Randomized Placebo-Controlled Trial of Ferric Carboxymaltose in Heart Failure With Iron Deficiency: Rationale and Design. Circ Heart Fail 2021;14(5):e008100. PM: 34003690.
Nelson AJ, Pagidipati NJ, Granger CB. The SAMSON trial: using a placebo to improve medication tolerability. Eur Heart J Cardiovasc Pharmacother 2021;7(3):e13. PM: 33638980.
Ohman EM, Zwischenberger BA, Thiele H. Left Ventricular Support for the Management of Cardiogenic Shock: Sooner May Be Better. JACC Cardiovasc Interv 2021;14(10):1120-1122. PM: 34016409.
Patel PA, Green CL, Lokhnygina Y, Christensen J, Milano CA, Rogers JG, Patel CB, Koweek LM, Daubert MA. Cardiac computed tomography improves the identification of cardiomechanical complications among patients with suspected left ventricular assist device malfunction. J Cardiovasc Comput Tomogr 2021;15(3):260-267. PM: 32891544.
Tai A, Ambrosy AP, Fudim M. Making the case for sacubitril/valsartan in patients with heart failure with a preserved ejection fraction. Eur Heart J Cardiovasc Pharmacother 2021;7(3):e5-e6. PM: 33537712.
Teerlink JR, Felker GM, McMurray JJV. Omecamtiv Mecarbil in Systolic Heart Failure. Reply. N Engl J Med 2021;384(20):1967-1968. PM: 34010541.
Wang L, Balmat TJ, Antonia AL, Constantine FJ, Henao R, Burke TW, Ingham A, McClain MT, Tsalik EL, Ko ER, Ginsburg GS, DeLong MR, Shen X, Woods CW, Hauser ER, Ko DC. An atlas connecting shared genetic architecture of human diseases and molecular phenotypes provides insight into COVID-19 susceptibility. Genome Med 2021;13(1):83. PM: 34001247.
Yoneshiro T, Kataoka N, Walejko JM, Ikeda K, Brown Z, Yoneshiro M, Crown SB, Osawa T, Sakai J, McGarrah RW, White PJ, Nakamura K, Kajimura S. Metabolic flexibility via mitochondrial BCAA carrier SLC25A44 is required for optimal fever. Elife 2021;10:10.7554/eLife.66865. PM: 33944778.
Younis A, Goldberger JJ, Kutyifa V, Zareba W, Polonsky B, Klein H, Aktas MK, Huang D, Daubert J, Estes M, Cannom D, McNitt S, Stein K, Goldenberg I. Predicted benefit of an implantable cardioverter-defibrillator: the MADIT-ICD benefit score. Eur Heart J 2021;42(17):1676-1684. PM: 33417692.
Duke Heart Week ending May 23rd 2021
Highlights of the week:
Duke Highlights, ACC 2021 – part 2!
We closed out ACC.21 earlier this week with lots of great presentations, including:
 Melissa Daubert had a poster presentation: Impact of Postpartum BP Screening on Clinical Outcomes in Women with Hypertensive Disorders of Pregnancy
Melissa Daubert had a poster presentation: Impact of Postpartum BP Screening on Clinical Outcomes in Women with Hypertensive Disorders of Pregnancy
Key findings:
- Early postpartum BP screening was performed in a minority of women with HDP, but was associated with greater detection of CV risk factors and CV disease.
- Over 1/3 of women with HDP developed ≥ 1 new CV risk factor within 5 years of delivery.
- Further study is needed to optimize preventive Figure 2 CV care in high-risk women with HDP.
Adam DeVore presented Effect of a Hospital and Post-discharge Quality Improvement Intervention on Clinical Outcomes and  Quality of Care for Patients With Heart Failure With Reduced Ejection Fraction on behalf of the CONNECT-HF investigators and committees. Their conclusion: “In this cluster-randomized trial of hospitals treating patients after a hospitalization for HFrEF, a hospital and post-discharge quality improvement intervention that focused on clinician education and audit and feedback of HF quality of care did not meaningfully improve HF outcomes or care above current quality improvement efforts.”
Quality of Care for Patients With Heart Failure With Reduced Ejection Fraction on behalf of the CONNECT-HF investigators and committees. Their conclusion: “In this cluster-randomized trial of hospitals treating patients after a hospitalization for HFrEF, a hospital and post-discharge quality improvement intervention that focused on clinician education and audit and feedback of HF quality of care did not meaningfully improve HF outcomes or care above current quality improvement efforts.”
Clinical implications:
- Major gaps in guideline-directed care remain
- Low rates of ACEI/ARB/ARNI, evidence-based beta-blocker, and MRA
- New approaches are needed to improve care above current quality improvement efforts for patients with HFrEF
- HF rehospitalization or death: 39% over 12 months of follow-up
- Fragmented nature of HF care in the US apparent during the study
 Renato Lopes presented The Coalition ACTION Trial, a Randomized Clinical Trial To Evaluate a Routine Full Anticoagulation Strategy In Patients With Coronavirus Infection (SARS-CoV-2) Admitted To Hospital. The presentation received a good amount of news coverage (see below). Lopes and colleagues conducted the ACTION trial to determine whether a therapeutic anticoagulation strategy based on rivaroxaban improved outcomes in patients with elevated D-dimer levels hospitalized with COVID-19 compared with a prophylactic anticoagulation strategy.
Renato Lopes presented The Coalition ACTION Trial, a Randomized Clinical Trial To Evaluate a Routine Full Anticoagulation Strategy In Patients With Coronavirus Infection (SARS-CoV-2) Admitted To Hospital. The presentation received a good amount of news coverage (see below). Lopes and colleagues conducted the ACTION trial to determine whether a therapeutic anticoagulation strategy based on rivaroxaban improved outcomes in patients with elevated D-dimer levels hospitalized with COVID-19 compared with a prophylactic anticoagulation strategy.
Neha Pagidipati presented Caring for Women With Familial Hypercholesterolemia Through Pregnancy during the Applying the Guidelines for Lipid Management in Special Populations session.
Guidelines for Lipid Management in Special Populations session.
Key findings:
- As screening for FH increases, clinicians will increasingly encounter women with FH who become pregnant
- Lipids normally increase in pregnancy; in FH, the absolute increase is greater
- Pregnancy is not associated with risks to mothers with FH, however may be associated with risks to fetus
- Statins are NOT recommended during pregnancy
- Need more studies on what the risks actually are
- Colsevelam is approved during pregnancy, but use is limited by side-effects
- This area is woefully understudied — need more data to drive evidence-based practice for both mothers and their children
 J.D. Serfas, a fellow in our Adult Congenital Heart Disease Program, served on the ACC.21 planning committee for the Adult Congenital and Pediatric Cardiology section and primarily designed the section, “Controversies in Interventional and Surgical Management of Congenital Heart Disease.”
J.D. Serfas, a fellow in our Adult Congenital Heart Disease Program, served on the ACC.21 planning committee for the Adult Congenital and Pediatric Cardiology section and primarily designed the section, “Controversies in Interventional and Surgical Management of Congenital Heart Disease.”
Serfas was involved in the planning of several Fellows-in-Training sessions, and helped facilitate the FIT Mix-and-Mingle and Fellows-in-Training Networking Events. He also co-designed and co-moderated the session Art with Heart: Tales of Creativity in Cardiology, a podcast-style session that included conversations with Doug Zipes, Suzie Brown Sacks, Nazanin Moghbeli, and Kedar Sankholkar, all of whom have integrated careers in the arts or entertainment with active cardiology careers.
Serfas presented the case of a patient with d-transposition of the great arteries after atrial switch repair with advanced heart failure requiring LVAD support in the session “Challenges of Transplantation in Congenital Heart Disease Patients: Ethics, Listing Strategy & MCS.”
Additionally, he had a poster presentation: Racial and Ethnic Disparities in Location of Death Among Adult Congenital Heart Disease Patients.
Key findings:
- Minority patients with ACHD are less likely to die at home or with hospice and more likely to die in a hospitalized setting than non-Hispanic White patients, and that structured programs to address these racial disparities in end-of-life care in ACHD are needed.
 Olivia Dong, a post-doctoral research fellow working with Deepak Voora, earned first place in the ACC.21 Young Investigator Competition in Outcomes Research. She presented, One-year cost-effectiveness of CYP2C19-guided P2Y12 inhibitors de-escalation and escalation in Veterans undergoing percutaneous coronary intervention.
Olivia Dong, a post-doctoral research fellow working with Deepak Voora, earned first place in the ACC.21 Young Investigator Competition in Outcomes Research. She presented, One-year cost-effectiveness of CYP2C19-guided P2Y12 inhibitors de-escalation and escalation in Veterans undergoing percutaneous coronary intervention.
Key takeaway:
- In Veterans with acute coronary syndromes who have undergone percutaneous coronary intervention, CYP2C19-guided P2Y12 inhibitor selection can improve cardiovascular outcomes and lower costs for the Veterans Health Administration within 12 months of implementation.
“I’m very grateful I had the opportunity to share this research at the ACC.21 conference,” said Dong. “This achievement would not have been possible without the unwavering support from my primary mentor, Dr. Deepak Voora, and my amazing research collaborators– Dr. Kevin Friede (Duke Cardiology Fellow), and Dr. Catherine Chanfreau-Coffinier (Veterans Affairs PHASER Data Core Director).”
Dong is currently completing a post-doctoral T32 NHGRI fellowship in genomic medicine research through the Duke Center for Applied Genomics and Precision Medicine and the Durham VA Health Care System. She will graduate in June. Well done, Olivia – congratulations!
Congratulations to all faculty and fellows who participated in ACC.21 this year – you’re doing remarkable work!
Shout-out to Respiratory Care Services
We were delighted and not at all surprised to learn of the generosity of our Respiratory Care Services team, led by Charlotte Reikofski, in helping support Duke Health by preparing supplies for India. The team gathered resuscitators, oxygen masks, filters and more for shipment to New Delhi – an effort spearheaded by anesthesiologist Madhav Swaminathan, clinical director of CT Anesthesia and Critical Care Medicine.
To read more about the effort, please visit: Duke Health Sends Supplies to India to Assist with Covid-19 Crisis.
Way to go, Respiratory Care team!!!
Moments to Movement – May 25th
Recently, Chancellor Washington shared an update with all Duke Health staff regarding the upcoming anniversary of our Moments to Movement initiative. Locations across Duke Health are planning time for all to stand together in observance of this important day and reflect upon our progress and prepare us for the work to come. Here are a few ways you can participate in the Stand for Peace this week.
Across Duke Health, many of us will take a one-day pause from non-essential meetings to allow our faculty and staff extra space and time to have conversation or to participate in one of the planned observances.
Stand for Peace: 7 a.m. – 9 a.m. and 2 p.m. – 4 p.m.; Duke Medicine Circle (grassy area in front of Duke South Clinics). This event is for all Duke Health faculty, staff and students working on campus; Create individual signs for display; sign the Duke Health Anti-racism Pledge
M2M Virtual Tea for the Soul: 7 a.m., 10 a.m., and 2 p.m., via Zoom. Guided reflection, relaxation for all Duke Health faculty, staff and students; each session will last 15 minutes. Participants are encouraged to bring their own tea. Click here to join. Hosted by Chaplain Services.
Revisiting Black Man in a White Coat: 3:00 p.m. – 3:45 p.m.; Register or read more here. All are invited to join Chancellor A. Eugene Washington and Associate Professor Damon Tweedy for a special conversation as they revisit Black Man In A White Coat — Tweedy’s 2015 bestselling book examining the difficult and often contradictory terrain of race and medicine.
Collective Breath for Justice: 4 p.m. – 4:45 p.m.; via Zoom. The Duke School of Medicine Office of Diversity & Inclusion will lead a virtual event to reflect, connect and share in a collective breath for justice. It will include a nine minute and 29 second silent vigil. Join here.
Senior leadership for Duke University Hospital and DUHS are committed to supporting everyone who wants to participate in one of these events. They ask that you please coordinate with your manager so that as many team members as possible are able to join in these activities while maintaining patient safety.
Thank you for everything you do every day to care for our communities. We are proud of each of you for your commitment to eliminating health disparities and standing against racial inequality and injustice.
COVID-19 Updates:
All the latest official DUHS information regarding coronavirus/COVID-19 response at the following locations:
Upcoming Opportunities/Save the Date:
 Virtual PMWC: Precision Medicine in the Era of a Pandemic Recovery
Virtual PMWC: Precision Medicine in the Era of a Pandemic Recovery
June 14-18 – Precision World Medicine Conference. Registration is free and open to all. https://www.pmwcintl.com/covid/
Duke University Chancellor Emeritus Dr. Ralph Snyderman will lead a panel discussion on Personalized, Proactive Value-Based Care: Emerging New Models.
The confluence of the growth of chronic diseases, the impact of COVID, the emergence of new technologies, and the impact of value-based reimbursement are driving major innovations and changes in care delivery. Proactive, personalized, precision, population-based and digitally supported care is emerging and heralding new approaches to health care. This session will capture the elements of these changes and the dynamics of the forces that are driving them. Perspective from care innovators, large providers and payers will be discussed by the following key opinion leaders:
- Patrick Conway, CEO of Care Solutions, Optum
- Jaewon Ryu, President and Chief Executive Officer, Geisinger
- Rodney Hochman, President & CEO, Providence St. Joseph Health
- Marc Harrison, President and CEO, Intermountain Healthcare
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged.
Duke Heart in the News:
May 15 — W. Schuyler Jones
Associated Press
Heart study: Low- and regular-dose aspirin safe, effective
https://bit.ly/3bARUtt
*story carried by 425 news outlets
May 15 — W. Schuyler Jones
Medpage Today
Baby Aspirin on Par With Full Dose to Prevent Repeat Heart Events
https://bit.ly/3wgN2BE
May 15 — W. Schuyler Jones
tctMD
High- and Low-Dose Aspirin Equivalent in ASCVD: ADAPTABLE
May 17 — Renato Lopes
tctMD
ACTION: Full-Dose Rivaroxaban Doesn’t Help in Hospitalized COVID-19
https://www.tctmd.com/news/action-full-dose-rivaroxaban-doesnt-help-hospitalized-covid-19
May 17 — W. Schuyler Jones
HealthDay
ACC: 81-mg, 325-mg Aspirin Similarly Effective in ASCVD
https://bit.ly/3yklkFV
May 17 — Renato Lopes
Healio/Cardiology
ACTION: Rivaroxaban-based anticoagulation strategy fails to improve outcomes in COVID-19
https://bit.ly/2S421QC
May 17 — Adam DeVore
Medpage Today
Stubborn Gaps in Heart Failure Persist Despite Clinician Education, Feedback
https://bit.ly/3hBG7yT
May 17 — Adam DeVore
Healio/Cardiology
Hospital, post-discharge quality improvement intervention failed to improve HFrEF outcomes
https://bit.ly/3u3TSbU
May 17 — Manesh Patel and W. Schuyler Jones
HCPLive
VOYAGER PAD with Manesh Patel, MD, and Schuyler Jones, MD
https://bit.ly/3fu7QP9
May 18 — W. Schuyler Jones
WNDU-NBC-16 (South Bend, IN)
Study finds low-dose and regular-dose aspirin perform the same for heart health
https://bit.ly/3eVWTqG
*carried by 17 additional news outlets
May 18 — W. Schuyler Jones and Renato Lopes
Medical Dialogues
Study Cautions Against Use of Oral Anticoagulants in Admitted COVID Patients, ACC 2021
https://bit.ly/3foK86M
May 18 — Adam DeVore
AJMC
Hospital Quality Program for Heart Failure Patients Fails to Improve Outcomes
https://bit.ly/3wgCVg0
May 18 — W. Schuyler Jones
USNews.com
Low- or High-Dose, Aspirin Brings Similar Protection Against Heart Disease: Study
https://bit.ly/3bGIuMT
May 18 — Renato Lopes
HCP Live
Rivaroxaban Linked to Increased Bleeding Among Hospitalized COVID-19 Patients
https://bit.ly/3u6M9tD
May 18 — Manesh Patel
Medium.com
The Extra Extra Life Conversations, Part Two
https://bit.ly/3hDFQLH
Division of Cardiology Publications Indexed in PubMed May 6–19, 2021
Caughey MC, Vaduganathan M, Arora S, Qamar A, Mentz RJ, Chang PP, Yancy CW, Russell SD, Shah SJ, Rosamond WD, Pandey A. Racial Differences and Temporal Obesity Trends in Heart Failure with Preserved Ejection Fraction. J Am Geriatr Soc 2021;69(5):1309-1318. PM: 33401338.
Daubert MA, Yow E, Barnhart HX, Piña IL, Ahmad T, Leifer E, Cooper L, Desvigne-Nickens P, Fiuzat M, Adams K, Ezekowitz J, Whellan DJ, Januzzi JL, O’Connor CM, Felker GM. Differences in NT-proBNP Response and Prognosis in Men and Women With Heart Failure With Reduced Ejection Fraction. J Am Heart Assoc 2021:e019712. PM: 33955231.
Gaeta S, Bahnson TD, Henriquez C. High-Resolution Measurement of Local Activation Time Differences From Bipolar Electrogram Amplitude. Front Physiol 2021;12:653645. PM: 33967825.
Greene SJ, Butler J, Spertus JA, Hellkamp AS, Vaduganathan M, DeVore AD, Albert NM, Duffy CI, Patterson JH, Thomas L, Williams FB, Hernandez AF, Fonarow GC. Comparison of New York Heart Association Class and Patient-Reported Outcomes for Heart Failure With Reduced Ejection Fraction. JAMA Cardiol 2021;6(5):522-531. PM: 33760037.
Greene SJ, Mentz RJ, Limkakeng AT, Irons T, Truong T, Green CL, Nowak C, Blumer V, Pang PS. Comparison of Dyspnea Measurement Instruments in Acute Heart Failure: The DYSPNEA-AHF Pilot Study. J Card Fail 2021;27(5):607-609. PM: 33091609.
Harris Walker G, Gonzalez-Guarda R, Yang Q, Shah S, Prvu Bettger J. Socio-ecological perspective on factors influencing acute recovery of younger stroke survivors: A mixed methods study. J Adv Nurs 2021:10.1111/jan.14778. PM: 33650219.
Hurst JH, Liu Y, Maxson PJ, Permar SR, Boulware LE, Goldstein BA. Development of an electronic health records datamart to support clinical and population health research. J Clin Transl Sci 2020;5(1):e13. PM: 33948239.
Kelsey MD, Granger CB. LOW-HARM score predicted mortality in patients hospitalized with COVID-19 in Mexico. Ann Intern Med 2021:10.7326/ACPJ202105180-059. PM: 33939489.
Lala A, Mentz RJ. Reaping from Reciprocity: the Mentor-Mentee Relationship. J Card Fail 2021;27(5):507-508. PM: 33962740.
Lopes RD, Thomas L, Di Fusco M, Keshishian A, Luo X, Li X, Masseria C, Friend K, Mardekian J, Pan X, Yuce H, Jones WS. Clinical and Economic Outcomes Among Nonvalvular Atrial Fibrillation Patients With Coronary Artery Disease and/or Peripheral Artery Disease. Am J Cardiol 2021;148:69-77. PM: 33667438.
Mann DL, Felker GM. Mechanisms and Models in Heart Failure: A Translational Approach. Circ Res 2021;128(10):1435-1450. PM: 33983832.
Parikh PB, Bhatt DL, Bhasin V, Anker SD, Skopicki HA, Claessen BE, Fonarow GC, Hernandez AF, Mehran R, Petrie MC, Butler J. Impact of Percutaneous Coronary Intervention on Outcomes in Patients With Heart Failure: JACC State-of-the-Art Review. J Am Coll Cardiol 2021;77(19):2432-2447. PM: 33985688.
Peri-Okonny PA, Wang J, Gosch KL, Patel MR, Shishehbor MH, Safley DL, Abbott JD, Aronow HD, Mena-Hurtado C, Jelani QU, Tang Y, Bunte M, Labrosciano C, Beltrame JF, Spertus JA, Smolderen KG. Establishing Thresholds for Minimal Clinically Important Differences for the Peripheral Artery Disease Questionnaire. Circ Cardiovasc Qual Outcomes 2021:120007232. PM: 33947205.
Povsic TJ, Sanz-Ruiz R, Climent AM, Bolli R, Taylor DA, Gersh BJ, Menasché P, Perin EC, Pompilio G, Atsma DE, Badimon L, DeMaria AN, Hare JM, Henry TD, Janssens S, Kastrup J, Torella D, Traverse JH, Willerson JT, Fernández-Avilés F. Reparative cell therapy for the heart: critical internal appraisal of the field in response to recent controversies. ESC Heart Fail 2021;8(3):2306-2309. PM: 33652498.
Prado GM, Mahfoud F, Lopes RD, Moreira DAR, Staico R, Damiani LP, Ukena C, Armaganijan LV. Renal denervation for the treatment of ventricular arrhythmias: A systematic review and meta-analysis. J Cardiovasc Electrophysiol 2021;32(5):1430-1439. PM: 33724602.
Rao VN, Kelsey MD, Kelsey AM, Russell SD, Mentz RJ, Patel MR, Fudim M. Acute cardiovascular hospitalizations and illness severity before and during the COVID-19 pandemic. Clin Cardiol 2021;44(5):656-664. PM: 33682157.
Rettmann ME, Holmes Iii DR, Monahan KH, Breen JF, Bahnson TD, Mark D, Poole J, Ellis AM, Silverstein A, Al-Khalidi HR, Lee KL, Robb RA, Packer DL. Treatment-Related Changes in Left Atrial Structure in Atrial Fibrillation: Findings from the CABANA Imaging Substudy. Circ Arrhythm Electrophysiol 2021:10.1161/CIRCEP.120.008540. PM: 33848199.
Sharma G, Douglas PS, Hayes SN, Mehran R, Rzeszut A, Harrington RA, Poppas A, Walsh MN, Singh T, Parekh R, Blumenthal RS, Mehta LS. Global Prevalence and Impact of Hostility, Discrimination, and Harassment in the Cardiology Workplace. J Am Coll Cardiol 2021;77(19):2398-2409. PM: 33985685.
Sun H, Hodgkinson CP, Pratt RE, Dzau VJ. CRISPR/Cas9 Mediated Deletion of the Angiotensinogen Gene Reduces Hypertension: A Potential for Cure? Hypertension 2021;77(6):1990-2000. PM: 33813849.
Recent Comments