Home » Articles posted by Manesh Patel, M.D. (Page 5)
Author Archives: Manesh Patel, M.D.
Duke Heart Pulse Week ending September 25th 2022
Highlights of the week:
Triangle Heart Walk Held Today!
The American Heart Association Triangle Heart Walk was held today at PNC Arena. We had amazing weather and a really great turnout – it could not have been better! Thank you to all of you who have helped support us throughout our effort on behalf of DUHS. We had a sea of Duke Blue at the Walk. It was so much fun to see people in person, enjoying the weather and one another’s company. We appreciate our Heart Walk Chair Richard Shannon who helped organize the Duke Fundraising.Thanks to all who joined us!

As we’ve been saying, this annual Walk is a great opportunity to come together to celebrate one another, to represent Duke Health, and to reinvigorate the commitment we have for living a heart-healthy lifestyle. What we haven’t pointed out is that this is the largest sponsorship that Duke Health maintains annually. Not only does Duke have one of the biggest teams out there each year, but we often come in as a top organization for fundraising.
Most of you know that some of these funds come back to Duke in terms of research funding – and that is a great reason to fundraise! More importantly, patients and their family members are invited to the Walk every year. At every Heart Walk held nationally, there is always a “survivor’s” tent — and many of our cardiovascular, stroke and pulmonary patients and their family members come out to the walk to celebrate their lives with us. For them to see members of our Duke Heart team and the larger DUHS community out in force – walking to support them and the AHA — is incredibly important.




We are so appreciative of all those who helped with planning, those who served as team captains, and those who raised valuable funds. We are proud of the Duke Heart team each and every day – thanks for making this a great place for patients to receive some of the best cardiovascular care in the world and for making it a very special place to work.
In case you’re wondering, it is not too late to donate to DUHS’s Heart Walk teams. We have until the end of October to collect donations – and every dollar counts, so please consider!


Duran Receives CLCD Travel Grant for AHA Sci Sessions
Jessica Duran, MD has been awarded an AHA travel grant for the upcoming AHA Scientific Sessions 2022 in 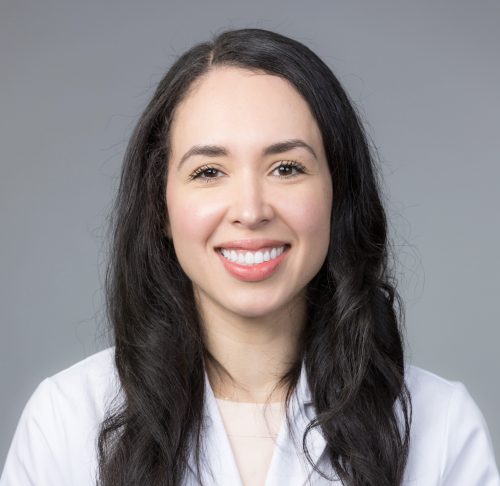 Chicago, IL where her abstract was accepted as an oral presentation entitled, Abnormal Exercise Electrocardiography with Normal Stress Echocardiography is Associated with Increased Subclinical Coronary Atherosclerosis: Insights From the Project Baseline Health Study.
Chicago, IL where her abstract was accepted as an oral presentation entitled, Abnormal Exercise Electrocardiography with Normal Stress Echocardiography is Associated with Increased Subclinical Coronary Atherosclerosis: Insights From the Project Baseline Health Study.
Duran has earned a 2022 Council on Clinical Cardiology (CLCD) Underrepresented Racial and Ethnic Groups Travel Grant. This award proudly supports the research efforts of early career investigators and trainees.
She will be acknowledged as a Travel Grant recipient at the CLCD dinner on Saturday, Nov. 5 at the Hyatt Regency McCormick.
Way to go, Jessie!
Fudim Delivers Cardiology Grand Rounds

Marat Fudim gave a terrific presentation on heart failure and pressure management on Tuesday evening. It was a great tour through our understanding of volume, pressure, and innovative therapies for patients with Heart Failure.
Still Time! Photography Fundraiser to Support Duke’s Heart Walk Effort!
Join Stephanie Barnes for a fall mini-photography session fundraiser in support of the American Heart Association Triangle Heart Walk and Team Got Heart. Several slots remain!
Dates: October 9 and 16, 2022 at Fearrington Village in Chapel Hill. Each session will be 15 minutes. Cost is $150, all of which goes to our fundraiser. Registration is required.
This is a great opportunity to get your holiday family portraits done ahead of Thanksgiving. Can be couples, just your kids, small families of 2-4, maybe even have your pets with you! You will receive full access and rights to all of your digital photos via a private web portal. Expect about 20 photos total.
Sign up here: https://www.signupgenius.com/go/409054DA9A623A2F49-photography1
EDS NOTE: Stephanie is a very talented photographer and this is a great price for a private photo shoot. This is an excellent opportunity to support the AHA Heart Walk by supporting our Got Heart team. You’ll get some beautiful photographs of people you love and they will make great gifts!
A big shout-out to Stephanie for donating her time and energy to this cause. If you have questions, please send an email to: Got Heart Fundraiser/Photoshoot. Sample photos shown here are used with client permission.
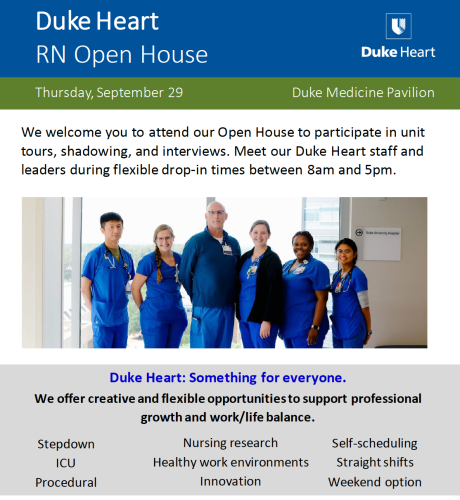
This week: Nursing Open House, Sept. 29
It’s nearly here! Duke Heart’s nursing team is hosting an open house on Thursday, Sept. 29 for new and experienced nurses as part of our recruitment efforts. The Open House will allow participants to take part in unit tours, shadowing and interviews.
Interested participants can meet our Duke Heart nursing staff and leaders anytime between 8 a.m. and 5 p.m. in Duke Medicine Pavilion. Greeters will be located at the front entrance (near valets) to meet attendees and direct them to the event throughout the day.
Please share this information with anyone you think might be a good candidate for us! They can register by scanning the QR code shown here.
Additional Reminders:
- The last week of September is the last week of Atrial Fibrillation Awareness month! Hug and thank an EP team member when you see them!
- The DUHS annual flu vaccination campaign is underway and will continue until mid-November. Vaccination sites for faculty and staff can be found here: https://flu.duke.edu/vaccination/employees/
- The Duke Health Integrated Practice (DHIP) Town Hall will be held this week — 7 a.m. on Wednesday, Sept. 28. This will be a Duke Health community-wide event. Questions you would like answered during the Town Hall can be sent ahead of time to DHIP@duke.edu.
- Open Enrollment is October 17-28. This is your opportunity to review your medical, dental, vision, and reimbursement account benefit elections and make any changes necessary to ensure your choices continue to meet your needs. Watch your email and home mail delivery for more information.
Upcoming Events & Opportunities
Cardiology Grand Rounds
September 27: Mortality & Morbidity with Jennifer Rymer and Nishant Shah. 5 p.m. Webex and in person (Duke North 2002)
October 4: Transcatheter Tricuspid Therapy with Paul Sorajja of the Minneapolis Heart Institute Foundation and Abbott Northwestern Hospital, Allina Health Minneapolis Heart Institute, Minneapolis. 7 a.m., Webex and in person (Duke North 2003)
CME & Other Events
September 28: DHIP Town Hall. 7 a.m. Links/location sent via email.
September 29: Nursing Open House. Duke Heart’s nursing team is hosting an Open House as part of recruitment efforts. 8 a.m. – 5 p.m., DMP. To register: https://duke.is/mhah5
October 14: Cardio-Oncology in the Era of Precision Medicine. Symposium to be held at the J.B. Duke Hotel, Durham, NC. Registration is open: https://bit.ly/CardioOnc22. Email Beth Tanner with questions: beth.tanner@duke.edu.
October 17-28: Open Enrollment period for 2023 for all Duke faculty members and staff.
October 28: Duke Caregiver Community Event, in-person conference. Details here: https://duke.is/nzbcp.
November 4: 14th Annual NC Research Triangle Pulmonary Hypertension Symposium. 7 a.m.-4 p.m. This will be an in-person event at the Durham Convention Center. Registration required. To learn more and register, visit: https://duke.is/jag2b
November 14: Prostate Cancer & CVD Symposium, Webinar 4. Final of a four-part webinar series. Collaboration between the International Cardio-Oncology Society & Duke Heart. Noon, Eastern. Free. To register visit https://duke.is/ptjbs.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
September 16 — Robert Keenan (rheumatology)
Rheumatology Advisor
Link Between Gout and Cardiovascular Events – An Interview With Robert Keenan, MD
https://duke.is/y4ya2
September 16 — Duke University Hospital
CBS17.com/WNCN
Duke Undiagnosed Diseases Network Center uncovers rare conditions, set to lose funding after 2024
https://duke.is/rsh4m
September 16 — Michael Carboni and Joseph Turek
Geo News/geo.tv
Doctors optimistic after world’s first partial heart transplant on newborn
https://duke.is/5e4rv
September 17 — Joseph Turek
WPTF News Radio 680
https://duke.is/nqh5u
September 18 — Owen Monroe (patient/HIPAA on file)
WKRC CBS-12/Cincinnati
https://duke.is/p647j
(*clip begins @06:53:28)
September 20 — Joseph Turek, Michael Carboni and Monroe family
Tribune News Service
Duke doctors perform world’s first partial heart transplant on NC newborn
https://duke.is/45gnq
September 21 — Wayneho Kam (neurology)
Medpage Today
Making Low-Dose tPA Work for Japanese DOAC Users With Ischemic Stroke
https://duke.is/9hmjr
September 21 — Duke Health
Becker’s Hospital Review
Duke: Healthcare worker burnout rose to 40% during pandemic
https://duke.is/2vmt3
September 22 — Brian Sexton
Public Radio East (Eastern NC)
Duke experts measure doctor and nurse burnout
https://duke.is/gb7uc
September 22 — Manesh Patel
WRAL/FOX 50
https://duke.is/vtxbn
(*clip begins @ 09:11:20)
Duke Heart Pulse – week ending September 18th 2022
Highlights of the week:
Swaminathan Named Section Chief of Cardiology, Durham VAMC
The Durham Veterans Affairs Medical Center (DVAMC) recently announced the appointment of Rajesh (Raj) Swaminathan, MD, FACC, FSCAI to the role of Section Chief of Cardiology, effective August 29, 2022.
 As the Durham VAMC Cath Lab Director, he has helped initiate and grow numerous clinical programs including CardioMEMS for advanced heart failure patients, novel therapies for treatment of calcified lesions and CTOs, and advanced coronary physiology and integrated/co-registered imaging platforms (IVUS/OCT) which are now utilized in >90% of PCIs at the VA. He has also been instrumental in piloting and innovating systems to reduce occupational hazards in the cath lab through robotic PCI and implementation of the new Rampart radiation shielding system allowing operators and staff to perform cardiac catheterizations without wearing lead.
As the Durham VAMC Cath Lab Director, he has helped initiate and grow numerous clinical programs including CardioMEMS for advanced heart failure patients, novel therapies for treatment of calcified lesions and CTOs, and advanced coronary physiology and integrated/co-registered imaging platforms (IVUS/OCT) which are now utilized in >90% of PCIs at the VA. He has also been instrumental in piloting and innovating systems to reduce occupational hazards in the cath lab through robotic PCI and implementation of the new Rampart radiation shielding system allowing operators and staff to perform cardiac catheterizations without wearing lead.
Raj has also strengthened the cardiology research portfolio at the VA and has ensured that the DVAMC has been a top enrolling site in numerous national, multicenter studies including ACCELERATION, ECLIPSE, OPTIMIZE, MINT, DISRUPT CAD III, and FUSION. A new trial, TARGET BP1, was recently launched to evaluate a novel renal denervation system for hypertension.
He has contributed in many ways to the VA’s clinical, research, and educational mission. He organized quarterly educational events for cardiology staff, hospital-wide general cardiology CME symposiums, delivers periodic lectures to residents and trainees, and serves on the DVAMC Radiation Safety Committee and the national VA-CART Research & Publications committee. Raj has been instrumental in developing pathways for same day discharge after PCI and teaching transradial techniques in VA hospitals around the country. Starting this year, he will serve as the VA’s VISN-6 Lead Cardiology consultant.
In addition, Raj is deeply involved in our cardiology professional societies and was recently elected to the Society for Cardiovascular Angiography & Interventions (SCAI) Board of Trustees. He also continues to support Duke University as past co-chair of the Duke Asian Alumni Alliance Board and is on the Board of Duke Triangle and the Duke Annual Fund Advisory Board.
“I am excited to continue building on the successful vision that Sunil Rao has fostered over many years of service to our Veterans, says Swaminathan. “I look forward to working with world-class physicians, APPs, and staff at the Durham VA as this is a pivotal time for Veteran care locally and nationally.
“Veterans have more opportunities to access care and many VAs are in the process of modernizing their facilities and expanding their services to areas of population growth,” he added. “I look forward to helping shape this next critical phase in Veteran care while continuing to work on pathways to optimize quality of care.”
Raj is a Duke alumnus (BS ’00, MD ‘04, HS ‘05). He completed his residency in Internal Medicine at Massachusetts General Hospital and was a research affiliate at the Harvard-MIT Health Sciences and Technology Center, where he studied coronary stent design and led preclinical studies which supported the initial FDA approval of the Xience V Everolimus Eluting coronary stent. He completed his general and interventional cardiology fellowships at New York Presbyterian Hospital-Weill Cornell Medical Center and continued as interventional faculty there before returning home to NC.
Congratulations, Raj!
Ken Morris Retiring from Durham VAMC
Hard as it may be to believe, Dr. Ken Morris has announced he will officially retire from the Durham Veterans Affairs Medical Center. His official end-date was still unknown at the time of our interview with Ken but is “imminent” and dependent upon the government processing of all paperwork. He’ll remain in the area and working with fellows one day a week.
When asked about his early years and what brought him to Duke, we learned the following:
“I was an intern resident and then chief medical resident at Ohio State, and then I came here in 1976 for my cardiology fellowship with the intent of returning to Ohio State to join the faculty. But then Joe Greenfield hired me. One can certainly argue that hiring me was an error, despite what a smart guy he was. Back then, he says, when you drove into Durham, the smell of tobacco curing in barns was everywhere.

“I didn’t figure I’d be tenurable here but I also figured that four or five years on the Duke faculty would look awfully good on a resume. I decided I wanted to be on the academic side of medicine — specifically cardiovascular medicine. I thought, “Okay, this will be good for me — I’ll learn a lot more things while I’m at Duke and then I can find some other place where they will love me. But it turned out that Joe loved me here, so I stayed.”

“I chose to become a cardiologist in the first month of my internship at Ohio State. I was rounding with an attending by the name of Dr. Charlie Wooley. He was an amazing clinical scientist and an amazing clinician at Ohio State. There were four of us – two students, a resident and me. The resident was a guy named Tom O’Dorisio who subsequently became a very important collaborator with a number of people here at Duke — he could teach a rat how to make an antibody to anything; there was me, and the two students were Jeff Crawford, who eventually became the director of the Duke Cancer Center and Willa Hsueh, who went on to become the president of the American Federation for Clinical Research (now the American Federation for Medical Research). The four of us were eager and hungry to learn and Wooley was this great attending who was very willing to feed us. By the end of that rotation I knew I wanted an academic career in cardiology. So that’s how it happened. Originally I planned to become a primary care internist in Elyria, Ohio.”
Morris has been involved in many things while at Duke, but his principal clinical responsibility was as an interventional cardiologist both at Duke and the Durham VAMC. He says he got into this area of cardiology when it was still at ‘ground zero’.
“Most people don’t remember this but Harry Phillips, Richard Stack and I were all over here at the VA trying to figure out coronary angioplasty. Not a lot of cases were being done on either side of the street — not until the TAMI trials (Thrombolysis and Angioplasty in Myocardial Infarction) started up at Duke and we had the helicopter and large clinical trials going on. I never had a clinic on the Duke side; I just did emergency angioplasty and I was in the cath lab over at Duke Hospital one day a week. I got involved in a lot of the VA clinical trials — COURAGE probably being the most important of all of those.”
Over the course of his career, he says he has enjoyed having the opportunity to study a variety of things.
“Fred Cobb, who was my immediate mentor at the VA, and Joe Greenfield were interested in coronary circulation. I went to the VA initially to spend a research year learning about coronary physiology, so I worked in the animal laboratory with them. I then worked to take what we learned there and move it to the human cath lab, which dovetailed nicely with interventional work.
“I then worked with a variety of forms of cardiac imaging to learn how to get physiologic information out of an image — not just anatomy, but physiologic information. I worked with a number of collaborators on that — most notable is probably Jack Cusma. It was a blast! I was privileged to live through what I consider the ‘glory days’ of myocardial infarction therapy and getting a better understanding of coronary physiology and ischemic heart disease. I mean, there were two decades — from 1985 to 2005 — where it was just one development after another where we took what we learned in the basic lab, applied them in the clinical arena and then demonstrated the life-saving value of what we were doing. It was really cool. And there are days like that ahead for people who are moving into the right areas today.”
Over his time at Duke, he says the fact that he’s been able to contribute to the education of a large number of fellows and faculty has been his biggest accomplishment.
“I have always loved what I do. The old adage, ‘Love what you do and you’ll never work a day in your life,’ has certainly been true for me.”
What will he do in retirement? Morris says his avocation is music — vocal music in a choir setting and percussion music. He plans to spend a lot more time engaged in these, and since Tom Bashore keeps trying to get him to go fishing with him, he may also get to do that, too. He and Bashore were in the same medical school class at Ohio State.
“I’ve enjoyed the friendship of my colleagues here for a long time. I hope the mythological “ideals” of Duke continue to remain a reality. The tripartite mission of taking care of patients, educating clinicians and conducting the best research should remain alive and well here — I hope it will. Change is inevitable, but if change is managed well and ideals are kept, change can still honor the foundation of what has been built here.
We asked some of Ken’s closest colleagues to share their thoughts with us. Here is what they said:
From Sunil Rao, MD:
“Ken Morris is a Durham VA institution. He took over the Cardiology Section from Joe Greenfield MD. Under Ken’s leadership, the Durham VA significantly expanded its clinical enterprise. He presided over the addition of key faculty and the modernization of the cardiac catheterization lab. He is the consummate clinician, always keeping the best interests of the veterans in mind. Ken’s reading of nuclear cardiology studies is legendary – his reads were always precise and accurate. I was lucky enough to be mentored by him and will always remember the question he asked me whenever I came to him with a clinical dilemma – “what is the goal of therapy?” It was his laser focus on what is best for the patient that made the Durham VA cardiology section the best in the country. He will be greatly missed, but we are hoping that he will continue to maintain a connection to the Durham VA and continue to work with Duke fellows.”
From Tom Bashore, MD:
“I have known Dr. Ken Morris since we were medical students in the same class at Ohio State 50 years ago this year. In those days Ken was known as a “free spirit,” and I suppose he still fits that description in some, pretty much modified, ways even today. After his chief residency at Ohio State, Ken came to Duke as a Cardiology Fellow and has remained here as a faculty member since; so, his retirement now is truly the end of a remarkable era for Duke and especially for the Durham VA. All the cardiology fellows and housestaff during that long period have benefited from his great sense of humor, hearty, unmistakable laugh, great teaching skills, and outstanding clinical judgement. Just as remarkable, he figured out how to actually get things done in the complicated and, at times, frustrating bureaucracy common to all VA Medical Centers. He taught generations of cardiology fellows how to correctly cath and perform coronary interventions, although he once had a cardiology fellow who just did not have it in the cath lab. Always quick with one-liners, I never forgot his comment on the fellow’s cath rotation review where he noted that “he should never enter anyone’s room with anything sharper than his elbows.” Where Ken will undoubtedly be missed the most from the fellows’ standpoint will be that he basically has been the major consistent teacher in our cardiovascular nuclear medicine program over these many years. We all wish him the very best in retirement, where I am sure he will continue singing (he has a great voice), fly fishing (he takes each grandkid when they turn 8 to Yellowstone) and spending more time with his ever-growing family. He leaves a sparkling legacy at the VA that will be impossible to fill.”
From Mark Donahue, MD:
“I met Ken Morris on the first day of my Duke Cardiology Fellowship July 1, 1999. In those days we were assigned in 6 month blocks for our Cath Lab rotation and I was going to be at the VA for 6 months. Ken was wearing a cath lab uniform designed by Krucoff. He looked like a barber from the 50s and acted like a character straight out of an episode of M*A*S*H. That 6th month block was invaluable for me and so when I had the opportunity to leave fellowship a few months early to join the VA faculty in 2003, I took it and have been there since. Ken’s father was a navigator on a B-17 in World War II flying numerous missions over Germany. When I started at the VA these WWII vets were everywhere and I came to realize that Ken really took care of each and every one of them like a family member. He has always been able to really relate to the veteran population and their trust in him was clear. The number of anecdotes and stories about Ken could fill a book; Sunil Rao and I may someday write one. Ken made no assumptions, always looked for the truth, put the patient first and above all made it fun. He is the single most important influence on my professional career and I will miss him.”
From Raj Swaminathan, MD:
“Dr. Ken Morris has served many roles at Duke and the VA including former Cath Lab Director and Chief of Cardiology. His early research in coronary physiology and myocardial perfusion laid the foundation for future invasive assessment and treatment of coronary lesions. He has taught numerous residents and fellows and has been a role model for staff and physicians. His contributions to Veteran care and shaping the positive culture at the VA is of immeasurable importance.”
It has been a pleasure working with you, Ken! We wish you all the best in retirement and we are thrilled for our fellows that you’ll continue to work with them.
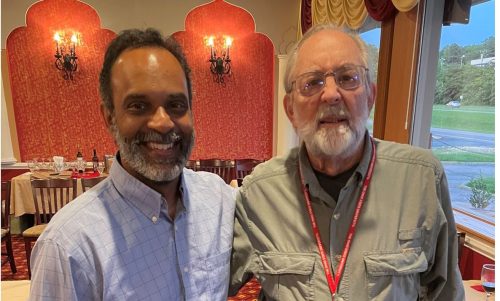
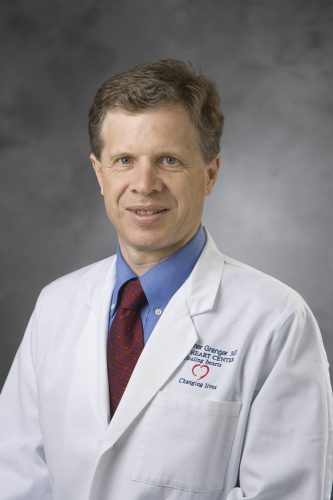
Gersh, Granger Deliver Cardiology, Medicine Grand Rounds
Chris Granger and special guest Bernard Gersh were our CGR presenters on Tuesday evening. They provided an excellent recap of ESC 2022, held Aug. 26-29 in Barcelona. Excellent discussion! Lots of great trials and commentary putting the studies in perspective. In short, more data for SGLT-2, surprising results around rheumatic heart disease and afib anticoagulation with DOACs, and some deeper dives needed to understand how to revascularize low EF patients when CABG is not an option.

Photography Fundraiser to Support AHA Team Got Heart!
 Join Stephanie Barnes for a fall mini-photography session fundraiser in support of the American Heart Association Triangle Heart Walk and Team Got Heart.
Join Stephanie Barnes for a fall mini-photography session fundraiser in support of the American Heart Association Triangle Heart Walk and Team Got Heart.
Dates: October 9 and 16, 2022 at Fearrington Village in Chapel Hill. Each session will be 15 minutes. Cost is $150, all of which goes to our fundraiser. Registration required.
This is a great opportunity to get your holiday family portraits done ahead of Thanksgiving. Can be couples, just your kids, small families of 2-4, maybe even with your pets! You will receive full access and rights to all of your digital photos via a private web portal. Expect about 20 photos total.
Sign up here: https://www.signupgenius.com/go/409054DA9A623A2F49-photography1
Editor Note: Stephanie is a very talented photographer and this is a great price for a private photo shoot. This is an excellent opportunity to support the AHA Heart Walk by supporting our Got Heart team. You’ll get some beautiful photographs of people you love and they will make great gifts!
A big shout-out to Stephanie for donating her time and energy to this cause. If you have questions, please send an email to: Got Heart Fundraiser/Photoshoot. Sample photos shown here are used with client permission.


Heart Walk is Next Weekend! Sunday, Sept. 25
One week remaining!! The American Heart Association Triangle Heart Walk is taking place next weekend on Sunday, September 25 at PNC Arena. Please plan to join us. Let’s make sure we have plenty of Duke Blue visible out there!
The annual Walk is a great opportunity to come together to celebrate one another, to represent Duke Health, and to reinvigorate the commitment we have for living a heart-healthy lifestyle. We are so appreciative of all of our team members who are taking time to plan for this event and raise funds.
Thank you to everyone who has already signed up to participate. It’s not too late! If you’d still like to register, visit the DUHS team page for the Walk and/or contact Sangeetha Menon from the AHA at sangeetha.menon@heart.org.
If you can’t join us in person, please consider a contribution of any amount to one (or more!) of the teams representing Duke Heart.
If you met the August 24 registration t-shirt deadline, you are eligible for a t-shirt. They will be available through your team captain this week, starting on Tuesday. Each team captain will be contacted via email to alert them where to go (and when) for pick-up. Walkers will need to get their shirt from their team captain.
If you missed the deadline for a shirt, please wear your favorite Duke Blue t-shirt or golf style shirt to the Heart Walk. You can even wear a shirt from a past Heart Walk. NOTE: T-shirts will NOT be distributed at the Walk.
Thank you! If you have questions, email Tracey Koepke.
Nursing Open House, Sept. 29
Coming up! Duke Heart’s nursing team is hosting an open house on Thursday, Sept. 29 for new and experienced nurses as part of our recruitment efforts. The Open House will allow participants to take part in unit tours, shadowing and interviews.
Interested participants can meet our Duke Heart nursing staff and leaders anytime between 8 a.m. and 5 p.m. in Duke Medicine Pavilion. Greeters will be located at the front entrance (near valets) to meet attendees and direct them to the event throughout the day.
Please share this information with anyone you think might be a good candidate for us! They can register by scanning the QR code shown here.

Congratulations to Tannu!
Congratulations to Manasi Tannu! Last weekend, Manasi was married to Alex Commanday, a first-year infectious disease fellow at UNC. They held a fusion ceremony in Charlotte, NC combining aspects of Hindu, Baha’i and Jewish wedding traditions. They had a three-day long weekend of wedding festivities with many performances, including a dance by Duke Cardiology fellows Mark Kittipibul, Nkiru Osude and former fellow Ijeoma Eleazu. It was a weekend to remember!
Congratulations and best wishes, Manasi and Alex. We are so happy for you!



Photos of the Week
More great photos captured on Twitter this week – our selection today is from the Mentz family – all of them sporting their Duke blue yesterday in Durham. We especially like the ‘Know Your Numbers’ shirt from last year’s Triangle Heart Walk. Way to go!!!
Saturday was both a home football game and employee appreciation day at Wallace Wade Stadium. The weather was gorgeous and we’re happy to report that the Blue Devils beat the NC A&T Aggies 49-20!
We hope all who were able to attend had a great time!
Additional Reminders:
- September is Atrial Fibrillation Awareness month!
- The DUHS annual flu vaccination campaign began on Thursday and will continue until mid-November. Vaccination sites for faculty and staff can be found here: https://flu.duke.edu/vaccination/employees/
- The Duke Health Integrated Practice (DHIP) Town Hall has been rescheduled for 7 a.m. on Wednesday, Sept. 28. This will be a Duke Health community-wide event. Questions you would like answered during the Town Hall can be sent ahead of time to DHIP@duke.edu.
- Open Enrollment is October 17-28. This is your opportunity to review your medical, dental, vision, and reimbursement account benefit elections and make any changes necessary to ensure your choices continue to meet your needs. Watch your email and home mail delivery for more information.
- Duke Health has closed its dedicated COVID Nurse Triage line for questions from patients, employees, students and families as of Sept. 1 due to the decrease in calls and a significant increase in community resources. The Duke Health COVID hotline for employees (919-385-0429) remains operational.
Upcoming Events & Opportunities
Cardiology Grand Rounds
September 20: Pressure and Volume Management in Heart Failure with Marat Fudim. 5 p.m. Webex only: https://duke.is/rr8x5.
CME & Other Events
September 20: Duke Caregiver Community Event, Virtual Sessions. Details here: https://duke.is/nzbcp.
September 22: Multimodality CV Imaging Conference. Topic: Mitral Regurgitation with Fawaz Alenezi. 12-1 p.m., Zoom: https://duke.is/58kut
September 25: Triangle Heart Walk. PNC Arena, Raleigh. Check-in and festivities start at 11 am. Walk begins at Noon. Join us!
September 28: DHIP Town Hall. 7 a.m. Links/location forthcoming. Watch your email.
September 29: Nursing Open House. Duke Heart’s nursing team is hosting an Open House as part of recruitment efforts. 8 a.m. – 5 p.m., DMP. To register: https://duke.is/mhah5
October 14: Cardio-Oncology in the Era of Precision Medicine. Symposium to be held at the J.B. Duke Hotel, Durham, NC. Registration is open: https://bit.ly/CardioOnc22. Email Beth Tanner with questions: beth.tanner@duke.edu.
October 17-28: Open Enrollment period for 2023 for all Duke faculty members and staff.
October 28: Duke Caregiver Community Event, in-person conference. Details here: https://duke.is/nzbcp.
November 4: 14th Annual NC Research Triangle Pulmonary Hypertension Symposium. 7 a.m.-4 p.m. This will be an in-person event at the Durham Convention Center. Registration required. To learn more and register, visit: https://duke.is/jag2b
November 14: Prostate Cancer & CVD Symposium, Webinar 4. Final of a four-part webinar series. Collaboration between the International Cardio-Oncology Society & Duke Heart. Noon, Eastern. Free. To register visit https://duke.is/ptjbs.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
September 1 — Harry Severance
Medpage Today’s Kevin MD
Monkeypox: Should the hospitality and transportation industries worry?
https://duke.is/y2j8q
September 9 — Shahzeb Khan
tctMD
Older Adults See Rebound in Rates of HF-Related Death: CDC Data
https://duke.is/r78tu
September 9 — Jonathan Piccini
HealthDay.com
COVID May Help Trigger A-Fib in Some Patients*
https://duke.is/5skuj
*also carried by 144 additional outlets including in Chicago, Dallas-Fort Worth, New York & U.S. News & World Report
September 9 — Jonathan Piccini
Newsmax Health
COVID Associated With Higher Risk for A-Fib
https://duke.is/n3b2d
September 12 — John Alexander
MIMS/Pharmacy
Asundexian + DAPT a treatment alternative for acute MI?
https://duke.is/8uan3
September 12 — Shahzeb Khan
Practical Cardiology
Heart Failure-Related Mortality Increasing Among Older Adults in US
https://duke.is/c835t
September 13 — Jonathan Piccini
Cardiac Rhythm News
Researchers find link between COVID-19 and new-onset AF
https://duke.is/wy97n
September 14 — Duke University Hospital
Becker’s ASC Review
World’s top 20 hospitals for cardiology
https://duke.is/4p3we
September 14 — Andrew Wang
Medpage Today
Aggressive Alcohol Septal Ablation for HCM Holds Up, Pacemakers Notwithstanding
https://duke.is/2j54d
September 14 — Joe Turek and Michael Carboni
Seattle Times
Doctors perform world’s first partial heart transplant on newborn
https://duke.is/9w95m
September 14 — Joe Turek and Michael Carboni
Cardiovascular Business
Cardiac surgeons perform the world’s first partial heart transplant
https://duke.is/g4jrf
September 15 — Sana Al-Khatib
Healio/Cardiology
VIDEO: Digital health meeting covered health equity, remote monitoring, more
https://duke.is/vs8ax
September 15 — Andrew Wang
tctMD
Pacemaker Doesn’t Harm Outcomes of Alcohol Septal Ablation for Obstructive HCM
https://duke.is/zakt6
September 15 — John Alexander
Medical Dialogues
Asundexian Promising Oral Anticoagulant in Post-Myocardial Infarction Patients
https://duke.is/mg2nb
September 15 — Joe Turek and Michael Carboni
dotmed.com
Duke Health performs world’s first partial heart transplant on newborn
https://duke.is/89a67
September 15 — Joe Turek and Michael Carboni
WWAYtv3.com (Cape Fear, NC)
UPDATE: Leland baby with believed to be first partial heart-transplant in world thriving
https://duke.is/wn97a
Duke Heart Pulse September 11th 2022
Chief Message:
We recognize and remember victims, family members, and survivors of 9-11-2001, and appreciate all of the people that work to ensure that our country and the world remain safe. Importantly, we hope that our country will continue to unite and remember the sacrifices and lives lost – many of which were remembered today at the ground zero ceremonies.
Highlights of the week:
Duke Health Performs World’s First Partial Heart Transplant
A team at Duke Health has performed what is believed to be the world’s first partial heart transplant, with the living arteries and valves from a freshly donated heart fused onto a patient’s existing heart.
The goal is to allow the valves to grow with the pediatric patient over time, increasing life expectancy. The team believes a similar approach could be used to place newly donated heart valves in countless other children with heart defects.
This animated video explains and illustrates the innovative procedure.
“This procedure potentially solves the problem of a growing valve,” said Joseph W. Turek, MD, PhD, Duke’s chief of pediatric cardiac surgery, who led the landmark surgery.
“If we can eliminate the need for multiple open-heart surgeries every time a child outgrows an old valve, we could be extending the life of that child by potentially decades or more,” Turek said.
The surgery was performed on 5-pound newborn, Owen Monroe. His family is from  Leland, NC, but he was born at Duke after his parents learned that he had a condition called truncus arteriosus, in which his two main heart arteries were fused together. Worse still, his one vessel was equipped with a leaky valve, making it unlikely he could survive the wait for a full heart transplant.
Leland, NC, but he was born at Duke after his parents learned that he had a condition called truncus arteriosus, in which his two main heart arteries were fused together. Worse still, his one vessel was equipped with a leaky valve, making it unlikely he could survive the wait for a full heart transplant.
Typically, children in situations like Owen’s would receive two preserved cadaver arteries with valves. But the implanted tissue used in this procedure doesn’t grow with the child’s own heart because it’s not living. Pediatric patients require multiple follow-up open heart surgeries to replace the valves with larger ones, dramatically limiting their life expectancy.

In the novel partial heart transplant, Turek and the Duke team — including fellow pediatric heart surgeon, Nicholas Andersen, MD and a large team of anesthesiologists, nurses, technicians and support staff — used living tissue and valves. The tissue was procured from a donor heart that had strong valves, but could not be used for full transplant due to the condition of the muscle.
The team’s effort to implant valves that could grow along with a patient appears to be a success. Owen is showing remarkable growth and improvements since undergoing the surgery on April 22, 2022, and his outlook remains strong.
“What’s particularly remarkable about this procedure, is that not only is this innovation something that can extend the lives of children, but it makes use of a donated heart that would otherwise not be transplantable,” said Michael Carboni, MD, an associate professor in the Department of Pediatrics at Duke University School of Medicine and Owen’s pediatric transplant  cardiologist.
cardiologist.
“The valves in this procedure come from a donor heart that had muscle tissue which was too weak to make it viable for full transplant but had strong valves that were well suited for Owen’s needs.” Carboni said. “This innovation amplifies the ways in which we can use the incredible gift of organ donation to save more lives.”
Experts at Duke are hopeful a similar approach could be used to treat common valve replacements in children, providing a one-time surgery to implant freshly donated tissue that could grow with the child.
“As harrowing of an experience as it was for our family, we knew from the beginning that Owen was in the best hands,” said Nick Monroe, Owen’s father. “Our greatest hope is that Owen’s success story will change the way organ donation and transplants are handled not only for congenital heart disease babies, but for all patients.”
Congratulations to the team and to Owen and his family!
To hear more about Owen’s story, please visit: https://duke.is/63jk7. There are links to news coverage in our News section, below.
President Price Applauds Research, Innovation at Duke Kannapolis Campus
Duke University President Vincent E. Price visited Duke’s clinical research office at the North Carolina Research Campus in Kannapolis on Thursday, Sept. 8. Duke Kannapolis demonstrates Duke’s commitment to advancing community health and improving lives across the state.
During roundtable discussions with Duke collaborators, local leaders, and study participants, Price spent his historic visit learning more about the unique research facility that has enrolled nearly 14,000 volunteers in dozens of studies using a successful community-engaged research model. Duke Kannapolis is a part of the Duke Clinical and Translational Science Institute (CTSI).
“Through community-based research and partnerships, Duke Kannapolis is on the forefront of population health research,” said Price, 10th president of Duke University and the first to visit Duke Kannapolis. “I am very grateful for the community leaders in Kannapolis and across the state who are strengthening Duke’s research and education missions to serve North Carolinians.”
Newly appointed Duke Kannapolis Director Svati H. Shah, MD, MHS, welcomed Price to Duke Kannapolis, which was founded in 2007 by Robert Califf, MD, Duke adjunct professor of medicine and commissioner of the U.S. Food and Drug Administration.
“I am so grateful for the time President Price gave us today to hear our story, see for himself the amazing work that’s happening here, and meet the extraordinary people who make this work a success,” she said. “Our partnership with our community in Kannapolis and Cabarrus County remains a vital and essential component of our success at Duke Kannapolis.”
Most Essential Component
Shah, who was recently tapped to lead Duke Kannapolis by CTSI Director L. Ebony Boulware, MD, MPH, shared her vision with Price to continue expanding work in omics, precision medicine, and population health with an increased focus on digital health, artificial intelligence, and genomic medicine to accelerate the translation of research to improved patient care.
While she builds new partnerships both within Duke and at the North Carolina Research Campus, Shah said the most important partner for Duke Kannapolis will remain the community itself.
“Our partnership with you, our community collaborators in Kannapolis and Cabarrus County, is the single most essential component of our success,” she told local leaders and study participants. “With your vision in reimagining the quality of life for your community, there is more for us to do and accomplish together.”
Community stakeholders at the event included representatives from the City of Kannapolis, City of Concord, Cabarrus Health Alliance, and El Puente Hispano, as well as participants in studies ranging from COVID-19 research to low back pain. Elected leaders included NC representative Kristin Baker.
The full story continues here: https://duke.is/wvjc3.
Skorton Delivers Cardiology, Medicine Grand Rounds
 We welcomed Dr. David J. Skorton, President and CEO of the Association of American Medical Colleges to Duke this past week as the Pamela S. Douglas, MD Visiting Scholar. Skorton gave Cardiology Grand Rounds in a special session held Thursday evening both in-person and online. His topic was ‘The Art and Science of Leadership’. A reception in the Doris Duke Center at Duke Gardens followed the presentation.
We welcomed Dr. David J. Skorton, President and CEO of the Association of American Medical Colleges to Duke this past week as the Pamela S. Douglas, MD Visiting Scholar. Skorton gave Cardiology Grand Rounds in a special session held Thursday evening both in-person and online. His topic was ‘The Art and Science of Leadership’. A reception in the Doris Duke Center at Duke Gardens followed the presentation.
He also delivered his presentation, ‘Advancing Diversity Equity and Inclusion in Academic Medicine: Its Critical Importance and the Role We All Must Play’ for Medicine Grand Rounds on Friday morning.
Skorton is a cardiologist specializing in congenital heart disease and cardiac imaging. We are deeply appreciative of the time he spent with us and are grateful to all who joined us!

Rymer Delivers Endocrinology Grand Rounds
Dr. Jennifer Rymer presented Endocrinology Grand Rounds on Friday afternoon, Sept. 9. Her topic was
Women’s cardiovascular health and disparities in the treatment of women with ASCVD.
Such an important topic — way to go, Jenn!
DHIP Town Hall Rescheduled to Sept. 28
The Duke Health Integrated Practice (DHIP) Town Hall has been rescheduled for 7 a.m. on Wednesday, Sept. 28. This will be a Duke Health community-wide event. Questions you would like answered during the Town Hall can be sent ahead of time to DHIP@duke.edu.
As we make progress in creating the Duke Health Integrated Practice (DHIP), the project team and subject-matter experts are answering your questions about our transition. For more questions and answers, see our recently updated FAQs at https://dhip.org/faqs.
Shiveler Named Assistant Nurse Manager, 3100, Effective Sept. 26
 Duke Heart is pleased to announce that Ally Shiveler, BSN, RN, CMSRN, CNIII will become Assistant Nurse Manager Operations for Duke University Hospital’s Cardiothoracic Stepdown Unit (3100) effective September 26th. Ally earned a Bachelor of Science in Nursing from the University of North Carolina, Wilmington in 2012. She joined Duke as a new graduate nurse on 4100 in July 2012.
Duke Heart is pleased to announce that Ally Shiveler, BSN, RN, CMSRN, CNIII will become Assistant Nurse Manager Operations for Duke University Hospital’s Cardiothoracic Stepdown Unit (3100) effective September 26th. Ally earned a Bachelor of Science in Nursing from the University of North Carolina, Wilmington in 2012. She joined Duke as a new graduate nurse on 4100 in July 2012.
During her time at Duke, Ally advanced on the clinical ladder by becoming a CNIII and has held a variety of roles on 4100 including Preceptor, Charge Nurse, Diabetes Management Champion, and POCT Trainer. Ally grew up in the Raleigh-Durham area and is excited to grow with this new opportunity in Duke Heart.
Please join us in congratulating and welcoming Ally to her new role!
Shout-out to Duke Transplant Teams & UNOS
The United Network for Organ Sharing (UNOS) on Friday shared that the U.S. has transplanted 1 million organs. As of the end of July, Duke had contributed 10,063 to that number!
A huge hat tip to all the donors and family members who have chosen to give the gift of life – without their trust and generosity, none of this would be possible.
A very special shout-out to the hundreds of team members across Duke who are part of the transplantation process: from the medical care of patients at the end of life, to those who provide care and solace to donor families, to those providing care to patients who need a transplant. This requires so many of us! To all who help and care for patients in need of listing; the counselors, financial experts and social workers, transplant and research coordinators; the perfusionists, respiratory therapists and imaging teams; transport teams, surgeons, anesthesiologists, nurses, techs and all those involved in the post-op care and follow-op of transplant patients.
We are so proud of your amazing teamwork each and every day. Exceptional work!!!
Photo of the Week
A great photo from Twitter this week of some of our incredible electrophysiology staff, courtesy of Jon Piccini! September is National Atrial Fibrillation (AFib) Awareness Month. Our Duke Electrophysiology team does an excellent job helping patients diagnosed with AFib, but also helps to build awareness all year long for this life threatening arrhythmia.

Did you know? In 2009, the Heart Rhythm Society and its partners worked to have the United States Senate officially designate September as National AFib Awareness Month. This was due to the growing prevalence of AFib and a desire to help the public become more familiar with the symptoms, warning signs, and available treatment options.
Nursing Open House, Sept. 29
Duke Heart’s nursing team is hosting an open house on Thursday, Sept. 29 for new and experienced nurses as part of our recruitment efforts. The Open House will allow for participants to take part in unit tours, shadowing and interviews.
Interested participants can meet our Duke Heart nursing staff and leaders anytime between 8 a.m. and 5 p.m. in Duke Medicine Pavilion. Greeters will be located at the front entrance (near valets) to meet attendees and direct them to the event throughout the day. Please share this information with anyone you think might be a good candidate for us! They can register by scanning the following QR code.

Heart Walk, 9/25; Kudos to Hitting with Heart Teams
Two weeks remaining!! We are excited for the upcoming American Heart Association Triangle Heart Walk scheduled for Sunday, September 25 at PNC Arena. Please plan to join us. Let’s make sure we have plenty of Duke Blue visible out there!
The annual Walk is a great opportunity to come together to celebrate one another, to represent Duke Health, and to reinvigorate the commitment we have for living a heart-healthy lifestyle. We are so appreciative of all of our team members who are taking time to plan for this event and raise funds, including DUH 7100!
KUDOS!
Kudos to all participants in the 6th annual “Hitting with Heart” softball tournament held Saturday, Aug. 27 at Valley Springs Park in Durham. The Healthy Work Environment committee from 7 West invited multiple departments from Duke University Hospital to participate in an all-day tournament to raise money for the American Heart Association’s Triangle Heart Walk.
They were finally able to have the tournament after being cancelled for the past two years due to Covid-19. This year’s tournament included nine teams. Groups represented included 7 West, CT Stepdown, 7100, Vascular IR, Clinical Engineering, DHTS-COO, Hospital Medicine, CT OR, and 6300.
All told, the tournament raised about $500 to benefit the AHA. Way to go!!!!


Interested?? Registering to participate in the Walk is easy. Visit the DUHS team page and/or contact Sangeetha Menon from the AHA at sangeetha.menon@heart.org for help getting started or with any questions.
Thank you to everyone who has already signed up to participate. If you can’t join us in person, please consider a contribution of any amount to one (or more!) of the teams representing Duke Heart.
We are getting closer to reaching our overall DUHS fundraising goal! Please help us get there. Support our Duke Heart teams!!! (Our teams can be found here: https://duke.is/6jpdp). Thank you!
Additional Reminders:
- September is Atrial Fibrillation Awareness month!
- Duke HR is hosting Financial Fitness Week THIS WEEK, 12-15. Staff and faculty can attend free virtual seminars to learn more about retirement planning, preparing budgets, handling investments, and more. Learn more/register here: https://duke.is/cc52s.
- The DUHS annual flu vaccination campaign begins on Thursday, September 15.
- Open Enrollment is October 17-28. This is your opportunity to review your medical, dental, vision, and reimbursement account benefit elections and make any changes necessary to ensure your choices continue to meet your needs. Watch your email and home mail delivery for more information.
- Duke Health has closed its dedicated COVID Nurse Triage line for questions from patients, employees, students and families as of Sept. 1 due to the decrease in calls and a significant increase in community resources. The Duke Health COVID hotline for employees (919-385-0429) remains operational.
Upcoming Events & Opportunities
Cardiology Grand Rounds
September 13: Guest speaker Bernard Gersh of Mayo Clinic, Rochester with Christopher Granger. 5 p.m. Webex only. (https://duke.is/pemrh)
CME & Other Events
September 12: Prostate Cancer & CVD Symposium — Collaborative Practice in Prostate Cancer: How is this actually done? Third webinar of a four-part series. Webinar series is a collaboration between the International Cardio-Oncology Society & Duke Heart. Noon, Eastern. Free. To learn more, please visit: https://duke.is/mbpte
September 12-15: Financial Fitness Week at Duke. Hosted by Duke HR. Register here: https://duke.is/cc52s.
September 16: MGR — Threatened Limbs at Duke: Multidisciplinary Care for a Multifaceted Problem with Katherine Neal and Kevin Southerland. Medicine Grand Rounds, DN 2002 or via Zoom.
September 25: Triangle Heart Walk. PNC Arena, Raleigh. Check-in and festivities start at 11 am. Walk begins at Noon. Join us!
September 28: DHIP Town Hall. 7 a.m. Links/location forthcoming. Watch your email.
September 29: Nursing Open House. Duke Heart’s nursing team is hosting an Open House as part of recruitment efforts. 8 a.m. – 5 p.m., DMP. To register: https://duke.is/mhah5
October 14: Cardio-Oncology in the Era of Precision Medicine. Symposium to be held at the J.B. Duke Hotel, Durham, NC. Registration is open: https://bit.ly/CardioOnc22. Email Beth Tanner with questions: beth.tanner@duke.edu.
October 17-28: Open Enrollment period for 2023 for all Duke faculty members and staff.
November 4: 14th Annual NC Research Triangle Pulmonary Hypertension Symposium. 7 a.m.-4 p.m. This will be an in-person event at the Durham Convention Center. Registration required. To learn more and register, visit: https://duke.is/jag2b
November 14: Prostate Cancer & CVD Symposium, Webinar 4. Final of a four-part webinar series. Collaboration between the International Cardio-Oncology Society & Duke Heart. Noon, Eastern. Free. Registration is not yet available. To learn more about the series, please visit: https://duke.is/mbpte.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
September 2 — Josephine Harrington
Medscape
Early Signal of Benefit for Empagliflozin in Acute MI: EMMY
https://duke.is/6b5b6
September 6 — John Alexander
Healio/Cardiology
Asundexian inhibits factor XIa activity with no excess bleeding risk after MI, stroke
https://duke.is/pgjpb
September 7 — Jonathan Piccini
AHA Newsroom
Study finds connection between COVID-19 and new-onset AFib
https://duke.is/4k8u4
September 8 — Joseph Turek
NBC Today Show
1st ever partial heart transplant saves 5-month-old: ‘Revolutionary’ for other kids
https://duke.is/n4b4n
*this story was carried on NBC affiliate stations nationally
September 8 — Michael Carboni and Joseph Turek
WRAL/NBC-5
Duke surgeon explains pioneering partial heart transplant
https://duke.is/9fkkw
Additional version:
WRAL/NBC-5
Newborn saved with first-of-its-kind heart transplant at Duke
https://duke.is/bv3r8
September 8 — Joseph Turek and Michael Carboni
WNCT/CBS (Greenville, NC)
Partial heart transplant at Duke
https://duke.is/yz89p
September 8 — Svati Shah, L. Ebony Boulware and Vincent E. Price
WBTV.com (Charlotte)
Duke University president visits Duke Kannapolis on Thursday
https://duke.is/cejac
September 8 — Michael Carboni and Joseph Turek
Healio/Cardiology
World’s first partial heart transplant completed in newborn with truncus arteriosus
https://duke.is/vm9qr
September 8 — Michael Carboni and Joseph Turek
Becker’s Hospital Review
Duke surgeons perform world’s 1st partial heart transplant
https://duke.is/zjjm9
September 9 — Jacob Schroder
USA Today
Organ transplant milestone: As US crosses 1 million mark, advances offer hope for millions more
https://duke.is/wxdeg
September 9 — Svati Shah, L. Ebony Boulware & Vincent E. Price
Salisbury Post
Duke University’s president visits clinical research office in Kannapolis
Division of Cardiology Publications Indexed in PubMed August 25–September 7, 2022
Barac YD, Toledano R, Jawitz OK, Schroder JN, Daneshmand MA, Patel CB, Aravot D, Milano CA. Right and left ventricular assist devices are an option for bridge to heart transplant. JTCVS Open 2022 Jan 22;9:146-159. PM: 36003474.
Frazier-Mills CG, Johnson LC, Xia Y, Rosemas SC, Franco NC, Pokorney SD. Syncope Recurrence and Downstream Diagnostic Testing after Insertable Cardiac Monitor Placement for Syncope. Diagnostics (Basel) 2022 Aug 16;12(8):1977. PM: 36010327.
Hernandez AF. Preface to theme issue on pragmatic and virtual trials: Progress and challenges. Contemp Clin Trials 2022 Aug;119:106816. PM: 35714912.
Lumsden RH, Pagidipati N. Management of cardiovascular risk factors during pregnancy. Heart 2022 Aug 25;108(18):1438-1444. PM: 35064047.
Minhas AMK, Sagheer S, Shekhar R, Sheikh AB, Nazir S, Ullah W, Khan MZ, Shahid I, Dani SS, Michos ED, Fudim M. Trends and Inpatient Outcomes of Primary Atrial Fibrillation Hospitalizations with Underlying Iron Deficiency Anemia: An Analysis of The National Inpatient Sample Database from 2004 -2018. Curr Probl Cardiol 2022 Oct;47(10):101001. PM: 34571106.
Mirowsky JE, Carraway MS, Dhingra R, Tong H, Neas L, Diaz-Sanchez D, Cascio WE, Case M, Crooks JL, Hauser ER, Dowdy ZE, Kraus WE, Devlin RB. Exposures to low-levels of fine particulate matter are associated with acute changes in heart rate variability, cardiac repolarization, and circulating blood lipids in coronary artery disease patients. Environ Res 2022 Nov;214(Pt 1):113768. PM: 35780850.
Moodie Z, Dintwe O, Sawant S, Grove D, Huang Y, Janes H, Heptinstall J, Omar FL, Cohen K, De Rosa SC, Zhang L, Yates NL, Sarzotti-Kelsoe M, Seaton KE, Laher F, Bekker LG, Malahleha M, Innes C, Kassim S, Naicker N, Govender V, Sebe M, Singh N, Kotze P, Lazarus E, Nchabeleng M, Ward AM, Brumskine W, Dubula T, Randhawa AK, Grunenberg N, Hural J, Kee JJ, Benkeser D, Jin Y, Carpp LN, Allen M, D’Souza P, Tartaglia J, DiazGranados CA, Koutsoukos M, Gilbert PB, Kublin JG, Corey L, Andersen-Nissen E, Gray GE, Tomaras GD, McElrath MJ. Analysis of the HIV Vaccine Trials Network 702 Phase 2b- 3 HIV-1 Vaccine Trial in South Africa Assessing RV144 Antibody and T-Cell Correlates of HIV-1 Acquisition Risk. J Infect Dis 2022 Aug 24;226(2):246-257. PM: 35758878.
Rao SJ, Douglas PS, Rzeszut A, Kwapong YA, Hayes SN, Poppas A, Mehta LS, Blumenthal RS, Sharma G. Global Differences in Parental Leave Policies and Satisfaction Among Cardiologists. Curr Probl Cardiol 2022 Oct;47(10):101299. PM: 35753397.
Stevens SR, Segar MW, Pandey A, Lokhnygina Y, Green JB, McGuire DK, Standl E, Peterson ED, Holman RR. Development and validation of a model to predict cardiovascular death, nonfatal myocardial infarction, or nonfatal stroke in patients with type 2 diabetes mellitus and established atherosclerotic cardiovascular disease. Cardiovasc Diabetol 2022 Aug 27;21(1):166. PM: 36030198.
Wixted D, Neighbors CE, Pieper CF, Wu A, Kingsbury C, Register H, Petzold E, Newby LK, Woods CW. Comparison of a Blood Self-Collection System with Routine Phlebotomy for SARS-CoV-2 Antibody Testing. Diagnostics (Basel) 2022 Jul 31;12(8):1857. PM: 36010206.
Armstrong PW, Zheng Y, Troughton RW, Lund LH, Zhang J, Lam CSP, Westerhout CM, Blaustein RO, Butler J, Hernandez AF, Roessig L, O’Connor CM, Voors AA, Ezekowitz JA. Sequential Evaluation of NT-proBNP in Heart Failure: Insights Into Clinical Outcomes and Efficacy of Vericiguat. JACC Heart Fail 2022 Sep;10(9):677-688. PM: 36049817.
Fiorito G, Pedron S, Ochoa-Rosales C, McCrory C, Polidoro S, Zhang Y, Dugué PA, Ratliff S, Zhao WN, McKay GJ, Costa G, Solinas MG, Harris KM, Tumino R, Grioni S, Ricceri F, Panico S, Brenner H, Schwettmann L, Waldenberger M, Matias-Garcia PR, Peters A, Hodge A, Giles GG, Schmitz LL, Levine M, Smith JA, Liu Y, Kee F, Young IS, McGuinness B, McKnight AJ, van Meurs J, Voortman T, Kenny RA, Vineis P, Carmeli C. The Role of Epigenetic Clocks in Explaining Educational Inequalities in Mortality: A Multicohort Study and Meta- analysis. J Gerontol A Biol Sci Med Sci 2022 Sep 1;77(9):1750-1759. PM: 35172329.
Gautam N, Ghanta SN, Clausen A, Saluja P, Sivakumar K, Dhar G, Chang Q, DeMazumder D, Rabbat MG, Greene SJ, Fudim M, Al’Aref SJ. Contemporary Applications of Machine Learning for Device Therapy in Heart Failure. JACC Heart Fail 2022 Sep;10(9):603-622. PM: 36049812.
Khan MS, Felker GM, Fudim M. Are We Getting Any Closer to Understanding Congestion? JACC Heart Fail 2022 Sep;10(9):633-636. PM: 36049814.
Spyropoulos AC, Lopes RD. Commentary on the 2021 ASH Guidelines on use of anticoagulation in patients with COVID-19 being discharged from the hospital. Blood Adv 2022 Sep 13;6(17):5045-5048. PM: 35245944.
Sun K, Corneli AL, Dombeck C, Swezey T, Rogers JL, Criscione-Schreiber LG, Sadun RE, Eudy AM, Doss J, Bosworth HB, Clowse MEB. Barriers to Taking Medications for Systemic Lupus Erythematosus: A Qualitative Study of Racial Minority Patients, Lupus Providers, and Clinic Staff. Arthritis Care Res (Hoboken) 2022 Sep;74(9):1459-1467. PM: 33662174.
Susman SJ, Bouffler A, Gordee A, Kuchibhatla M, Leahy JC, Griffin SM, Christenson RH, Newby LK, Limkakeng AT. Stress-Delta B-Type Natriuretic Peptide Does Not Exclude ACS in the ED. J Appl Lab Med 2022 Sep 1;7(5):1098-1107. PM: 35587711.
Duke Heart Week ending September 4th 2022
Chief’s message: 
Hope you all are having a restful weekend. You may be wondering what a photo of Harry Styles is doing at the start of the Pulse. I took my daughter (soon to be 16) to his concert in Madison Square Garden this weekend. Few things in life can make you feel as old as attending one of these concerts. Given all that is going on in the world, we definitely felt blessed to be able to go and it was fun as seeing her enjoy an event like this in the big city.
Highlights of the week:
Ward Appointed Associate Dean for Faculty Development
 Cary Ward, MD, associate professor of medicine in cardiology, has been appointed to the role of associate dean for faculty development in the Duke School of Medicine. In this role Ward will serve as the faculty lead for current and future School of Medicine faculty development programs including Leadership Development for Researchers (LEADER); Academic Leadership, Innovation, and Collaborative Engagement (ALICE); and the Duke Clinical Leadership Program (DCLP). She will partner with leaders in the Offices of Equity, Diversity, and Inclusion; Research Mentoring; APT; Professionalism; and others to maintain and grow a robust portfolio of programs that meet evolving faculty needs. Ward will also oversee the selection process for numerous School of Medicine faculty awards and the annual awards celebration to recognize and highlight the outstanding accomplishments of our faculty. Ward will report to the vice dean for faculty, Mara Becker, MD, who made the announcement on Wednesday, Aug. 31.
Cary Ward, MD, associate professor of medicine in cardiology, has been appointed to the role of associate dean for faculty development in the Duke School of Medicine. In this role Ward will serve as the faculty lead for current and future School of Medicine faculty development programs including Leadership Development for Researchers (LEADER); Academic Leadership, Innovation, and Collaborative Engagement (ALICE); and the Duke Clinical Leadership Program (DCLP). She will partner with leaders in the Offices of Equity, Diversity, and Inclusion; Research Mentoring; APT; Professionalism; and others to maintain and grow a robust portfolio of programs that meet evolving faculty needs. Ward will also oversee the selection process for numerous School of Medicine faculty awards and the annual awards celebration to recognize and highlight the outstanding accomplishments of our faculty. Ward will report to the vice dean for faculty, Mara Becker, MD, who made the announcement on Wednesday, Aug. 31.
Ward is an adult congenital and structural heart disease specialist, and serves as the program director for the Adult Congenital Heart Disease Fellowship and the director of the Cardio-Obstetrics Program. She received her MD from the University of Virginia, completed internal medicine residency at the University of Texas at Southwestern in Dallas, and was a cardiology fellow at Duke before joining the faculty in 2007. For the past eight years, she has led professional development activities for the Department of Medicine, first as director of credentialing and more recently as the associate vice chair for provider experience and development. She is the director of the ALICE leadership development program for mid-career women faculty and has served as the director of the Duke Clinical Leadership Program since 2018.
Ward is a 2022 recipient of the Leonard Palumbo Jr., MD Faculty Achievement Award, recognizing faculty who display dedication to compassionate patient care and excellence in the teaching and mentoring of young physicians.
Ward’s longstanding health system experience and leadership with several programs in the Office for Faculty make her uniquely positioned to strengthen and grow the portfolio of faculty development offerings at Duke. The expansion of the Office for Faculty reflects the school’s ongoing commitment to the continuous professional development of our faculty.
Congratulations, Cary! Well-deserved!
CGR, Douglas Visiting Scholar Program Welcomes Skorton, Sept. 8
We’re excited to welcome Dr. David J. Skorton, President and CEO of the Association of American Medical Colleges to Duke on Thursday, Sept. 8 as the Pamela S. Douglas, MD Visiting Scholar! Our Women in Cardiology and current ALICE members are invited to a meet & greet with Skorton at 4 p.m.; then, at 5 p.m., Skorton will deliver Cardiology Grand Rounds. His topic is ‘The Art and Science of Leadership’. A reception in the Doris Duke Center at Duke Gardens will immediately follow his presentation.
Skorton will deliver ‘Advancing Diversity Equity and Inclusion in Academic Medicine: Its Critical Importance and the Role We All Must Play’ for Medicine Grand Rounds on Friday, Sept. 9 at 8 a.m. MGR, 8-9 a.m., Duke North 2002 and via Zoom.
Prior to becoming President of the AAMC, Dr. Skorton, a cardiologist specializing in congenital heart disease and cardiac imaging, was also President of Cornell University (2006-2015) and the University of Iowa (2003-2006), as well as the 13th Secretary of the Smithsonian Institution (2015-2019). He has made profound contributions to government, higher education and academic medicine.
We look forward to his presentations!

Update from Samad, AKU : Flood in Pakistan
Many of you are aware that Pakistan has experienced devastating flooding. The country experienced prolonged heatwaves in April and May of this year, leading to glacial melt in the mountain region and an earlier-than-normal and heavier than normal monsoon season, which started in mid-June. It has been reported that at least one-third of Pakistan is under water; thousands of homes are destroyed and 33 million people have been displaced.
We reached out to adjunct cardiology faculty member Zainab Samad, MBBS, MHS, now the chair of the Dept. of Medicine at Aga Khan University in Karachi, to check in on how she and her team are doing. Here is what she shared:
“Thank you so much for asking about us. It is a disaster of unimaginable proportions-over a thousand have died, over 300,000 people have lost their homes. Millions internally displaced. We will realize the full scale in a few months as food insecurity from agricultural losses and livestock loss begins to set in. Pakistan is ground zero for climate change.
AKU is working through its own units and the Aga Khan Health Services to provide medical care to flood affectees. Those who wish to donate can do so through this link: https://duke.is/b7xj7. All my best to our Duke fam!”
We are thinking of you, Zainab and the entire country!
Photo credit: Bilawal Arbab/EPA, via Shutterstock and nytimes.com.

Cardiac Ultrasound Program Celebrates Graduates
We are pleased to announce the Duke Cardiac Ultrasound Certificate Program graduates for 2022! Their commencement was held Saturday, Aug. 27 in the Great Hall of the Trent Semans Center for Health Education. Graduates of our second class of program participants are: Leila Andrews, Daisy Chang, Haleigh Collins, Hannah Eldara, Kristina Mauro, Nicholas Medlock, Courtney Snyder, and Naomi Strauther.
Speakers at the event included program medical director, Anita Kelsey, MD, vice chief for non-cardiac invasive imaging; Richie Palma, program director, and Jill Engel, DNP, service line vice president for Duke Heart & Vascular.



Program graduate Naomi Strauther was named the Joseph Kisslo Outstanding Student for 2022.

Outstanding Service awards for clinical instructors were presented to Duke Heart team members Kathryne Nobles, Danny Rivera, and Eduardo Sandoval Murillo.
This program was a mere vision just three years ago. Since then, we’ve graduated 16 participants with a 100 percent board pass rate. Our entire class of 2022 scored in the top 3 percent of all those tested nationally on a test that has a less than 50 percent pass rate on the first try.
“This is a tremendous testament to Anita and Richie who fought through a number of challenges to get this school planned and launched, and then welcomed our first class during a pandemic,” said Manesh Patel, MD, chief of cardiology and co-director of Duke Heart Center. “It also speaks to their great work at recruiting and retaining excellent students.”
Duke University Health System hired three of eight program graduates in 2021 and seven of eight this year.
“The Duke Cardiac Ultrasound Program has quickly become a hiring pipeline for Duke Health and another source of immense pride for Duke School of Medicine, Duke Heart and Duke Health,” added Engel.
The program this year saw two of its class of 2022 members (Nick Medlock and Daisy Chang) receive American Society of Echocardiography (ASE) Awards, which were presented in June at ASE 2022 in Seattle. Medlock and Chang each won a competitive national award.
Shown here are the 2022 graduates (L-R): N. Strauther; H. Collins; L. Andrews; H. Eldara; K. Mauro; C. Snyder; N. Medlock, and D. Chang, along with program director Richie Palma.
Congratulations to all!

Shout-out to Gomez
The 7100 Cardiology Stepdown team would like to recognize Cindy Gomez for receiving a Daisy Award Nomination! Cindy was recognized by a patient’s daughter who felt at peace because Cindy was her mother’s nurse. Cindy spoke slowly and at an appropriate volume for the patient to clearly understand. Cindy also recognized that the patient was having difficulty swallowing pills, so she quickly intervened, providing the patient with crushed pills instead.
Thank you, Cindy, for living Duke’s values to the fullest and providing excellent patient-centered care. Way to go!

Photo of the Week
A great photo from Twitter this week of first-year cardiology fellows Aman Kansal and Andrew Andreae celebrating the end of their cath rotation. We’re glad they enjoyed it!

Duke Heart Nursing to Host Open House, Sept. 29
Duke Heart’s nursing team is hosting an open house on Thursday, Sept. 29 for new and experienced nurses as part of our recruitment efforts. The Open House will allow for participants to take part in unit tours, shadowing and interviews.
Interested participants can meet our Duke Heart nursing staff and leaders anytime between 8 a.m. and 5 p.m. in Duke Medicine Pavilion. Greeters will be located at the front entrance (near valets) to meet attendees and direct them to the event throughout the day. Please share this information with anyone you think might be a good candidate for us! They can register by scanning the following QR code.

Heart Walk: Sunday, Sept. 25
We are getting excited for the upcoming American Heart Association Triangle Heart Walk scheduled for Sunday, September 25 at PNC Arena. The annual Walk is a great opportunity to come together to celebrate one another, to represent Duke Health, and to reinvigorate the commitment we have for living a heart-healthy lifestyle. Incredibly, this event is only 3 weeks from today!
Please plan to join us. Let’s make sure we have plenty of Duke Blue visible at PNC Arena and that we outshine our friends from Carolina and Wake Med on September 25!
Registering is easy. Visit the DUHS team page and/or contact Sangeetha Menon from the AHA at sangeetha.menon@heart.org for help getting started or with any questions you might have about the Walk.
Thank you to everyone who has already signed up to participate. If you can’t join us in person, please consider a contribution of any amount to one (or more!) of the teams representing Duke Heart.
Help us meet our overall DUHS fundraising goals! Duke Heart’s teams can be found here: https://duke.is/6jpdp . Thank you!

Reminder: Flu Vaccine Campaign Launches Sept. 15
PDC and Duke University Health System (DUHS) require all healthcare workers to comply with our Healthcare Worker Flu Vaccination policy by either being vaccinated annually against the flu or receiving an approved exemption. Annual policy compliance is a condition of employment for all PDC and DUHS team members. Annual vaccination or policy compliance is also a condition of access to Duke Health facilities, including information systems, for those holding clinical privileges in a Duke Health facility and learners who wish to train in our facilities.
The DUHS annual flu vaccination campaign will begin on Thursday, September 15. In light of the COVID-19 pandemic, limited mass flu vaccination clinics will be available at each hospital and at select off-campus work locations.
Team members will have the opportunity to get vaccinated through any of the following means:
- Peer vaccination in clinical work areas will be available as in years past.
- West Campus of Duke University in Blue Devil Tower providing healthcare and university worker vaccinations by appointment on various dates throughout October.
- Entity-based vaccine clinics will be established; schedules will be posted and shared.
- Staff member’s primary care physician or at a local pharmacy.
Peer-to-Peer Vaccination
This year’s peer-to-peer initiative will be identical to last year. Although we will not be holding a vaccination drill, we do ask that you prepare to vaccinate your team members as early as possible. As always, we ask you to be thoughtful of any DUHS staff member who frequents your unit or work area. This may include EVS staff, patient transporters, or supply chain team members who will need to be vaccinated this year.
Please note these key dates for this flu vaccination season:
Thursday, September 15: Launch of Flu Vaccination Season
Tuesday, November 1: Deadline for applications for Medical or Religious Exemption should be submitted before this date. This will allow sufficient time for review and for communication of the review decision. Please note: Due to the availability of an egg-free formulation of the flu vaccine, egg allergy is not a reason for a medical exemption.
Tuesday, November 15, at 10 a.m.: Deadline for policy compliance through vaccination or granted medical or religious exemption.
We will be using an updated Duke VaxTrax QR, a digitized flu vaccination consent and health screening platform. You and your vaccinator will complete documentation of vaccination using this digital platform or, if you are vaccinated by your primary care provider or at a local pharmacy, you must submit evidence of vaccination to https://duke.is/vxsfu
If you have questions about the flu vaccine or its availability, please contact StopTheFlu@dm.duke.edu or EOHWflu@dm.duke.edu.
Thank you for your commitment to keeping our patients, each other and our community safe and healthy.
COVID-19 Update
Duke Health has closed its dedicated COVID Nurse Triage line for questions from patients, employees, students and families as of Sept. 1 due to the decrease in calls and a significant increase in community resources. The Duke Health COVID hotline for employees (919-385-0429) remains operational.
Please continue to practice safe COVID-19 protocols in your day-to-day interactions with others. Be particularly vigilant about masking, and avoid eating indoors in group settings. The health of our team members and our patients remains a priority as we continue to monitor the COVID-19 trends throughout our community.
Stay home if you are not feeling well. Employees who begin to experience any COVID-19 symptoms should report symptoms through the Duke SymMon app, which is available in both the Apple and Google app stores.
Donate blood if you’re able to. Click here for Duke-sponsored blood drives through the Red Cross. Patient-facing resources on DukeHealth.org can be found here: https://www.dukehealth.org/covid-19-update/resources. Duke University maintains a resource page as well, which can be accessed here: https://coronavirus.duke.edu/updates/for-staff.
Upcoming Events & Opportunities
Cardiology Grand Rounds
September 8: The Art and Science of Leadership with David Skorton, President and CEO of the Association of American Medical Colleges (AAMC). 5 p.m. in Duke North Room 2002 and via WebEx. Dr. Skorton is the Pamela S. Douglas, MD Visiting Scholar. A reception at Duke Gardens will be held immediately following this CGR presentation.
September 13: Guest speaker Bernard Gersh of Mayo Clinic, Rochester with Christopher Granger. 5 p.m. Webex only. (https://duke.is/pemrh)
CME & Other Events
September 9: ‘Advancing Diversity Equity and Inclusion in Academic Medicine: Its Critical Importance and the Role We All Must Play.’ Medicine Grand Rounds with David J. Skorton. 8-9 a.m., Duke North 2002 and via Zoom.
September 12: Prostate Cancer & CVD Symposium — Collaborative Practice in Prostate Cancer: How is this actually done? Third webinar of a four-part series. Webinar series is a collaboration between the International Cardio-Oncology Society & Duke Heart. Noon, Eastern. Free. To learn more, please visit: https://duke.is/mbpte
September 25: Triangle Heart Walk. PNC Arena, Raleigh. Check-in and festivities start at 11 am. Walk begins at Noon. Join us!
October 14: Cardio-Oncology in the Era of Precision Medicine. Symposium to be held at the J.B. Duke Hotel, Durham, NC. Registration is open: https://bit.ly/CardioOnc22. Email Beth Tanner with questions: beth.tanner@duke.edu.
November 4: 14th Annual NC Research Triangle Pulmonary Hypertension Symposium. 7 a.m.-4 p.m. Save the date! This will be an in-person event at the Durham Convention Center. Registration required. To learn more and register, visit: https://duke.is/jag2b
November 14: Prostate Cancer & CVD Symposium, Webinar 4. Final of a four-part webinar series. Collaboration between the International Cardio-Oncology Society & Duke Heart. Noon, Eastern. Free. Registration is not yet available. To learn more about the series, please visit: https://duke.is/mbpte.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
August 26 — Duke School of Medicine
Becker’s ASC Review
20 most diverse medical schools in the US: Report
https://duke.is/cvxge
August 27 — Michael Felker
Medpage Today
ADVOR Backs Add-On Acetazolamide for Cutting Congestion in Decompensated HF
https://duke.is/mcgpj
August 28 — Renato Lopes
MDEdge.com
Rivaroxaban outmatched by VKAs for AFib in rheumatic heart disease
https://duke.is/2a4kr
August 28 — John Alexander and Sunil Rao
tctMD
Factor XIa Inhibitors Show Potential for Safer Anticoagulation After MI, Stroke
https://duke.is/gtt39
August 29 — Manesh Patel
USNews.com
Biggest Study Yet Finds No Link Between Statins, Muscle Aches
https://duke.is/6gxhc
August 29 — Manesh Patel
tctMD
Only Very Small Risk of Muscle Symptoms With Statins: CTT Collaboration
https://duke.is/p5ysg
August 29 — Manesh Patel
HealthDay News
Biggest Study Yet Finds No Link Between Statins, Muscle Aches
https://duke.is/4qh28
August 29 — John Alexander
Medical Express
New oral anticoagulant shows promise in post-myocardial infarction patients
https://duke.is/564cz
August 30 — Manesh Patel
Medpage Today
P2Y12 Inhibitors May Be the Better Option for Secondary Prevention in CAD
https://duke.is/vnh6v
August 31 — Richard Shannon
Becker’s Hospital Review
11 clinical quality leaders on fall priorities
https://duke.is/z24j5
Duke Heart Pulse – Week ending August 28th 2022
Chief’s message: ESC Cardiology Meeting
This week the European Society of Cardiology meeting was held in Barcelona with several presentations from Duke Faculty. There were several presentations on late breaking trials and science including the presentation of the PACIFIC AMI study by John Alexander. Renato Lopes was the discussant of the INVICTUS study showing warfarin was superior in rhematic heart disease patients with atrial fibrillation. There were also several investigator and study meetings by Duke Heart Faculty and fellows. Below you will find a photo of Kelly Arps presenting some data on bleeding risk in patients with Atrial Fibrillation on DOACs. Additionally, Joey Harrington also had a presentation around the underdosing of these therapies, and Vishal Rao also had a poster presentation.


Also a photo of several of the faculty and fellows out with some past Duke residents and fellows who were at the meeting.

Highlights of the week:
Kudos to Flores Rosario, Decker and Gohman
We received a note this week from Anna Lisa Chamis regarding some outstanding care members of our team provided recently to a patient:
From Jeff Federspiel in Maternal-Fetal Medicine:
“I am so grateful to everyone who worked to coordinate keeping our patient safe. There are too many people to thank everyone individually, but I wanted to give a special thanks to the bedside team who stayed with our patient through delivery, monitoring and managing hemodynamics in real time and supporting her labor during what is always a difficult experience:
- Kelsey Decker and Natalie Gohman from the Duke Heart CTICU team
- Courtney Schultz from DBC
- Karen Flores Rosario from Duke Heart’s Advanced Heart Failure/Cardiology team
Richa Agarwal added the following comment: “Karen was involved in this emotionally challenging, complicated case. She was present bedside to help — really remarkable effort.”


We are proud of each of you — thank you for the teamwork and compassionate care you’re providing!
Kudos to Elliot
 First-year cardiology fellow David Elliott was commended this week in a note to Anna Lisa Chamis. She shared the following message she received from Chris Holley:
First-year cardiology fellow David Elliott was commended this week in a note to Anna Lisa Chamis. She shared the following message she received from Chris Holley:
“I just want to pass on this kudos about David Elliott: he is the first fellow I have ever seen do a personal review of a peripheral blood smear to check for schistocytes in working up hemolysis.”
Way to go the extra mile for your patient, David!
Shout-out to Shannon
 Rick Shannon, MD, chief quality officer for DUHS, cardiologist and area chair of the 2022 Triangle Heart Walk, along with leaders from the Triangle American Heart Association affiliate, hosted an informative health-related Town Hall for employees with Lenovo. Shannon presented the latest information on key health measures and tips for preventing and managing cardiovascular disease. Lenovo employees were able to ask questions during a Q&A session. The virtual event was held on Thursday, Aug. 25. Lenovo is hosting a team at the upcoming Heart Walk — we’re looking forward to seeing them there.
Rick Shannon, MD, chief quality officer for DUHS, cardiologist and area chair of the 2022 Triangle Heart Walk, along with leaders from the Triangle American Heart Association affiliate, hosted an informative health-related Town Hall for employees with Lenovo. Shannon presented the latest information on key health measures and tips for preventing and managing cardiovascular disease. Lenovo employees were able to ask questions during a Q&A session. The virtual event was held on Thursday, Aug. 25. Lenovo is hosting a team at the upcoming Heart Walk — we’re looking forward to seeing them there.
Great job sharing important health tips to our community, Rick!
Be Aware: Extortion Scam Targeting DEA Registrants
An extortion scam continues to target healthcare providers across the US. Please note this reminder:
The U.S. Department of Justice Drug Enforcement Administration (DEA) is aware that registrants are receiving telephone calls and emails by criminals identifying themselves as DEA employees or other law enforcement personnel. In an attempt to create the illusion that these criminals are DEA employees, they have masked their telephone number on caller id with a phone number for a legitimate DEA office. For example, these criminals have used the phone numbers for DEA’s Office of Congressional and Public Affairs and DEA’s 800 number which is used to provide direct support to DEA registrants.
Impersonating a federal agent is a violation of federal law. Registrants should be aware that no DEA agent will ever contact members of the public by telephone to demand money or any other form of payment or threaten to suspend a registrant’s DEA registration.
If you are contacted by a person purporting to work for DEA and seeking money or threatening to suspend your DEA registration, submit the information through “Extortion Scam Online Reporting” posted on the DEA Diversion Control Division’s website. For more information, please visit https://www.dea.gov/scam-alert.
Contact PDC Legal with further questions.
Coming Up: Influenza Vaccine Campaign
PDC and Duke University Health System (DUHS) require all healthcare workers to comply with our Healthcare Worker Flu Vaccination policy by either being vaccinated annually against the flu or receiving an approved exemption. Annual policy compliance is a condition of employment for all PDC and DUHS team members. Annual vaccination or policy compliance is also a condition of access to Duke Health facilities, including information systems, for those holding clinical privileges in a Duke Health facility and learners who wish to train in our facilities.
The DUHS annual flu vaccination campaign will begin on Thursday, September 15. In light of the COVID-19 pandemic, limited mass flu vaccination clinics will be available at each hospital and at select off-campus work locations.
Team members will have the opportunity to get vaccinated through any of the following means:
- Peer vaccination in clinical work areas will be available as in years past.
- West Campus of Duke University in Blue Devil Tower providing healthcare and university worker vaccinations by appointment on various dates throughout October.
- Entity-based vaccine clinics will be established; schedules will be posted and shared.
- Staff member’s primary care physician or at a local pharmacy.
Peer-to-Peer Vaccination
This year’s peer-to-peer initiative will be identical to last year. Although we will not be holding a vaccination drill, we do ask that you prepare to vaccinate your team members as early as possible. As always, we ask you to be thoughtful of any DUHS staff member who frequents your unit or work area. This may include EVS staff, patient transporters, or supply chain team members who will need to be vaccinated this year.
Please complete the following flu vaccination supply survey by close of business on Wednesday, August 31st if your work area will be participating in the peer vaccination program. https://duke.qualtrics.com/jfe/form/SV_cGCkAI3W8o8c8sK
Please note these key dates for this flu vaccination season:
Thursday, September 15: Launch of Flu Vaccination Season
Tuesday, November 1: Deadline for applications for Medical or Religious Exemption should be submitted before this date. This will allow sufficient time for review and for communication of the review decision. Please note: Due to the availability of an egg-free formulation of the flu vaccine, egg allergy is not a reason for a medical exemption.
Tuesday, November 15, at 10 a.m.: Deadline for policy compliance through vaccination or granted medical or religious exemption.
We will be using an updated Duke VaxTrax QR, a digitized flu vaccination consent and health screening platform. You and your vaccinator will complete documentation of vaccination using this digital platform or, if you are vaccinated by your primary care provider or at a local pharmacy, you must submit evidence of vaccination to https://duke.is/vxsfu
If you have questions about the flu vaccine or its availability, please contact StopTheFlu@dm.duke.edu or EOHWflu@dm.duke.edu.
Thank you for your commitment to keeping our patients, each other and our community safe and healthy.
Heart Walk: Sunday, Sept. 25
 We are getting excited for the upcoming Triangle Heart Walk scheduled for Sunday, September 25 at PNC Arena. The annual Walk is a great opportunity to come together to celebrate one another, to represent Duke Health, and to reinvigorate the commitment we have for living a heart-healthy lifestyle. Incredibly, this event is only one month away!
We are getting excited for the upcoming Triangle Heart Walk scheduled for Sunday, September 25 at PNC Arena. The annual Walk is a great opportunity to come together to celebrate one another, to represent Duke Health, and to reinvigorate the commitment we have for living a heart-healthy lifestyle. Incredibly, this event is only one month away!
We are in the final stretch and could use more help from across DUHS. Won’t you consider joining us? Let’s make sure we have plenty of Duke Blue visible at PNC Arena and that we outshine our friends from Carolina and Wake Med on September 25!
Registering is quick and easy.
- Visit TriangleHeartWalk.org
- Select the “Create new team” or the “Join a Team” button. Then complete the registration page.
- Personalize your page with a photo and send emails inviting others (colleagues, friends and family) to join the team and donate.
Contact Sangeetha Menon at sangeetha.menon@heart.org for help getting started or with any questions you might have about the Heart Walk.
Did you know?
As a part of the AHA’s Strategically Focused Research Network (SFRN), Duke principal investigator Svati Shah, MD received funding from the AHA from 2017-2021 to study microbiota related to molecular pathways in pediatric obesity. A subsequent publication highlighted novel metabolic pathways associated with heterogeneity in response to weight loss interventions, and related biomarkers which could be used in future studies of personalized approaches to weight loss interventions.
Our work to support the AHA Heart Walk comes back to us via grant funding for site PI’s.
Thank you to everyone who has already signed up to participate. If you can’t join us in person, please consider a contribution of any amount to one (or more!) of the nine teams representing Duke Heart.
Help us meet our overall DUHS fundraising goals! Duke Heart’s teams can be found here: https://duke.is/6jpdp
Photos of the Week
As noted – some of our faculty were in Barcelona this weekend for ESC Congress 2022. We’ve seen a number of posts on Twitter – (don’t forget to tag @DukeHeartCenter!) – we enjoyed this shot of Rob Mentz with Mike Felker, “looking like a celebrity that hates selfies with his fans.” Spot on!

COVID-19 Update
Please continue to practice safe COVID-19 protocols in your day-to-day interactions with others. Be particularly vigilant about masking, and avoid eating indoors in group settings. The health of our team members and our patients remains a priority as we continue to monitor the COVID-19 trends throughout our community.
Stay home if you are not feeling well. Employees who begin to experience any COVID-19 symptoms should report symptoms through the Duke SymMon app, which is available in both the Apple and Google app stores.
Donate blood if you’re able to. Click here for Duke-sponsored blood drives through the Red Cross.
All the latest Clinical Operations updates related to COVID can be found at https://covid-19.dukehealth.org. Patient-facing resources on DukeHealth.org can be found here: https://www.dukehealth.org/covid-19-update/resources. Duke University maintains a resource page as well, which can be accessed here: https://coronavirus.duke.edu/updates/for-staff.
Upcoming Events & Opportunities
Cardiology Grand Rounds
September 8: The Art and Science of Leadership with David Skorton, MD, President and CEO of the Association of American Medical Colleges (AAMC). 5 p.m. in Duke North Room 2002 and via WebEx.
CME & Other Events
September 12: Prostate Cancer & CVD Symposium. This is the third webinar of a four-part series. Collaboration between the International Cardio-Oncology Society & Duke Heart. Noon, Eastern. To learn more, please visit: https://duke.is/mbpte
September 25: Triangle Heart Walk. PNC Arena, Raleigh. Check-in and festivities start at 11 am. Walk begins at Noon. Join us!
October 14: Cardio-Oncology in the Era of Precision Medicine. Symposium to be held at the J.B. Duke Hotel, Durham, NC. Registration is open: https://bit.ly/CardioOnc22. Email Beth Tanner with questions: beth.tanner@duke.edu.
November 4: 14th Annual NC Research Triangle Pulmonary Hypertension Symposium. 7 a.m.-4 p.m. Save the date! This will be an in-person event at the Durham Convention Center. Registration required. To learn more and register, visit: https://duke.is/jag2b
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
August 19 — John Alexander and Manesh Patel
Geriatricarea
Bayer organiza un encuentro para mejorar el abordaje de los pacientes cardiovasculares complejos
https://duke.is/nwmkv
August 22 — Joe Turek and Louise Markert
RadioLab (NPR/PRI)
https://duke.is/547zd
August 23 — Jonathan Piccini
Medscape
Early AF Rhythm-Control Advantage Climbs With Comorbidity Burden: EAST-AFNET4
https://duke.is/b5735
August 24 — Michel Khouri and Stephen Greene
Practical Cardiology
https://duke.is/96ygs
Duke Heart Pulse – Week Ending August 21st 2022
Highlights of the week:
Celebrating Magnus Ohman

It is hard to believe, but Magnus Ohman’s last official day at Duke was August 5. Pulse readers know that we ran an extensive piece about him on Sunday, June 12 and that an in-person gathering was held on July 14th at the Washington Duke Inn.
Ohman has retired from clinical medicine and will now serve as vice-president of Global Development of Cardiometabolic Therapeutics for Amgen. We reached out to a number of our team members (current and former) for some reflections on Magnus and his time with us.
Here is what they shared:
From Pam Douglas:
“When I first came to Duke, Magnus had left to try his hand at being chief of cardiology at UNC. However his loyalty to Duke and his colleagues made him an easy ‘boomerang’ recruit. He took over our outpatient clinics—a difficult and often thankless job—but pulled off a major overhaul streamlining schedules, referrals and other aspects to make it much more patient and provider friendly.
Magnus’s own outpatient practice was remarkable. He thrived on clinical complexity and even set up a center for ‘end stage’ CAD, while also counting many luminaries and donors among his patients.
Never one to attract attention to himself, he quietly ran international trials and site based research, serving as a sought after mentor for many at DCRI and in the cath lab. I have always highly valued his wise counsel, perspective and insights, and will greatly miss his good cheer, intelligence, and can-do attitude! I’m sure that Amgen doesn’t yet know how amazing a gem they have recruited, but they will soon find out.”
From Kristin Newby:
“I first met Magnus when I was an intern on cardiology, during his first year of cardiology fellowship, and still remember many of the things he taught me! Years later, as I moved from the basic lab to clinical research as I came on faculty, Magnus was among several clinical research faculty who were instrumental in supporting my transition and providing enthusiastic mentorship and guidance throughout my career. We connected over biomarkers, especially through his seminal work on troponins as a prognostic marker, and I had the thrill of conducting with him one of the earliest studies of a multi-marker assessment tool for patients with chest pain (CHECKMATE) that was accepted for publication in Circulation as is, without any revisions! Through the years, I have watched him mentor numerous other fellows and early career faculty with the same enthusiasm and passion, and am especially proud of the role he has played in mentoring and sponsoring women fellows and early career faculty. These aspects, and his clinical presence, will certainly be missed at Duke, but I look forward to continuing our friendship and seeing him flourish in the next phase of his career. And, we still have a lot of golf to play—including bringing the William Harvey Trophy back to the US in 2024, through which Magnus has also been and a terrific friend and valued sponsor and mentor!”
From Jim Daubert:
“Magnus has been a frequent and treasured colleague of mine since returning to Duke in 2009. It was great reconnecting with him in clinical care after forging close bonds with him during our Fellowship some years ago! Over the last 13 years I have very much valued consulting on his uniquely challenging patients and soliciting his insights on especially gnarly coronary and other cases. I will truly miss interacting with him in the clinical realm. His wisdom, judgement and insight cannot be replaced. Fortunately, Amy and I will look to continuing our highly valued friendships with Magnus and Elspeth, not to mention going to Hurricanes games together!”
From Jennifer Rymer:
“It has been a true opportunity to get to work with Magnus from start to near finish on a large multi-site registry over the past two years. Magnus is extremely talented in collaborating with and building relationships with industry partners and external collaborators. He taught me so much about how to develop relationships with collaborators and run a registry, even when we were faced with challenges during COVID. His network runs deep, and always amazed me how he was able to stay in touch with colleagues and collaborators from projects years prior. I have valued his mentorship and appreciate that I had the privilege to work with someone who has done so much in CV research and for Duke. He has been an advocate for me from the beginning, and I know will continue to be a mentor even while at Amgen.”
From Mike Sketch:
“Magnus and I began our cardiology fellowship at Duke the same year, and it has truly been an honor to be his friend and colleague over the past 35 years. He has truly excelled in every aspect of his career and is so committed to our academic mission. He is so supportive of young faculty and wants to see others prosper and grow. He is always thinking outside the box and asking novel questions. Through his example, he has taught so many faculty and fellows how to think creatively. He is very highly respected both inside and outside of Duke. He has developed so many amazing relationships with external partners. He loves patient care, and his patients adore him. Finally, he beams with pride whenever he talks about his family, Elspeth and his three kids.
Magnus, you will be so missed!”
From Tracy Wang:
“Magnus’ career has changed so much for so many of us in medicine. One characteristic of his career I’ve always admired is that he’s not afraid to tackle the tough questions when they need to be answered. He just won’t take “no” for an answer, and many a time, has called up company CEOs to convince them to do the right thing scientifically. Another aspect I and many other others have enjoyed is his sincere interest and support of early careers. I don’t think there’s a recently Duke-trained interventional fellow out there who’s not received an invitation to write a paper with Magnus. He is a tireless advocate for his mentees, and a fervid supporter of supporter of women in cardiology. Magnus, we wish you all the best in the next phase of your career. Don’t forget us at Duke!”
From Chris Granger:
“As a fellow starting in 1989, I met Magnus as a bright, savvy, well spoken (and the accent helped as well), and personable fellow from Ireland who had worked with the Oxford University team — at the time, the most successful clinical trial group in the world. Moreover, Magnus was engaging and entertaining and fun. Life was richer when working with Magnus, as a member of a steering committee or on call for the clinical service. I, like many of us, was in awe and wanted to work with him and be with him. In fact, Magnus and I began to share a room at the major cardiology conferences as fellows because we could not afford to have our own rooms, and then kept doing it throughout our careers because we enjoyed it so much as friends as well as a way to keep up with what was going on at the meetings. He grew into one of the most successful and influential researchers and clinicians in the history of Duke cardiology. He has been recognized several times as one the most highly-cited researchers in all of Duke. He has led many important clinical trials. He served on FDA advisory panels. He was an important bridge between U.S. and European cardiology, being one the few people to serve on clinical practice guideline committees (including in leadership positions) on both sides of the Atlantic. Duke has been very fortunate to have Magnus who has been a terrific ambassador for Duke around the world. He is personal friends not only with those of us at Duke and those that he has trained, but also with many of the leaders of cardiology around the world. Like so many trained in the British Isles, Magnus is a world-class clinician and his patients love him. In short, Magnus has been a giant in his years working in the Heart Center. He has been a loyal, dedicated, beloved member of the Duke team. He will always be an important part of the Duke cardiology family.”
From Blue Dean:
“I did not have a chance to meet Magnus in person when I interviewed at Duke. Instead, he and I spoke by phone and I still remember our conversation. He didn’t ask about my experience; he asked about my children, my husband, and what we enjoyed doing as a family. He talked about the local community, Duke as a place to work, and what set the Duke Heart Center apart from peer institutions.
Shortly after my arrival, Chris O’Connor suggested that I work with Magnus as the point person for the Duke Heart Center’s development efforts. Little did I know that Magnus and I would spend the next eight years working together and in partnership with many faculty physicians to raise funds in support of the Duke Heart Center and Department of Medicine. We spent countless hours in the car crisscrossing North Carolina, Florida, California, and wherever else a donor visit might send us. I most often was the driver which caused me to jokingly referring to our arrangement as Driving Miss Daisy. I’m not sure Magnus appreciated being called Miss Daisy, but it was all in good fun!
And, we did have fun. Magnus is an excellent storyteller and a lover of music. He would keep me entertained (and awake) with both. During one of our trips to Florida, I lost my voice – completely lost my voice – and Magnus was quick to jump in and comfortably navigate the gift conversations on my behalf. Donors loved working with Magnus; they appreciated his enthusiasm and passion for Duke, as well as his commitment to excellent patient care.
I was very fortunate to work with Magnus and remain thankful for all he taught me. Fundraising, like so many professions, can be stressful. Magnus was always quick to lighten the mood with a good laugh and an appropriate story. And, on occasion, a really good bottle of wine!
Cheers to Magnus – here’s to a wonderful run and best wishes for great things to come!”
From Penny Hodgson:
“When Rob Califf invited me to take a job in 1992 editing the manuscripts that came out of the GUSTO trial, I had no idea what the job would turn into. One of the first faculty members to come say hello was Magnus Ohman. He was very supportive of the idea of having someone take his draft manuscript and polish it iteratively to the point of publication. And we did this over and over again, to the tune of more than 130 GUSTO manuscripts over the years; Magnus was likely a coauthor of at least a third of them.
As the Communications group grew, adding editors and graphic designers at first, Magnus welcomed them and put them to work. And he was unfailingly grateful and fun, making great suggestions for improving the slides and illustrations that were used to explain the results of our trials in print and in person.
I have two recollections about Magnus and the European Society of Cardiology meetings. One year he received a phone call from his daughter Elsa telling him that a hurricane was about to hit North Carolina and he needed to come home right away! He shared that story widely at that meeting.
The second remembrance is of being in Vienna the day following the end of the meeting and finding that Magnus was also there. We decided to see if we could get tickets to whatever was going on at the Vienna Symphony Hall, and we could. We had amazing seats with lots of legroom, and Magnus fell asleep before the end of the introduction. He woke up for the intermission and went immediately back to sleep afterwards. He agreed that the Russian pianist had been fabulous, although I’m not sure he heard a single note she played.”
From Bob Harrington:
“Hard to believe but I have now known Magnus for 33 years, since the time I arrived at Duke for my own fellowship. Magnus initially was some sort of very special “super fellow” from Ireland. We heard about him but didn’t see him much. I really got to know Magnus when I went to the Databank as a fellow and then for years had an office next to him and Chris Granger. We spent lots of late nights in the Databank then in the DCRI because none of us had a good internet connection at home. With Magnus, there was always loud rock music (yes, he is a Led Zeppelin fan) and great conversations about research and life. He taught me a lot about both! And talked me off more than a few ledges.
Traveling internationally with Magnus was always a memorable experience. First, he traveled in a suit jacket and tie, even on the overnight! Second, he was through immigration lines very quickly because he would use either his EU/Irish passport or his US one, whichever had the shorter line and so he was usually waiting for us. But he always had a car lined up and he always knew the best hotels in any European city. If you need travel advice, check with Magnus (but don’t ask or listen to Chris Granger, Magnus’ frequent roommate on the road).
Magnus is a creative thinker in research and the cath lab. That can get you in trouble, but Magnus always has a way of pulling himself out of those tricky situations. He’s been a terrific friend and colleague over these many years. And, he has a great wine cellar that he is always happy to share. I’m looking forward to seeing what he does in this next part of his professional journey and I’m definitely looking forward to greeting him more regularly on the left coast! Good luck Magnus.”
Magnus has certainly had an impact on so many of us as well as on Duke and the overall field of cardiology. He has touched most of the faculty and fellows during his time. He mentored many of us during both good and bad times. We will miss seeing him on campus, but we wish him all the best and look forward to many more stories and collaborations over the coming years!
Kudos to Cara Hoke
Anna Lisa Chamis shared a terrific note she received this week from Nishant Shah regarding cardiology fellow Cara Hoke:
“Hi Anna Lisa,
I wanted to let you know that Cara completed an elective on PAC this past week and did an outstanding job! We had a busy  service all week which she took the lead on. She was calm, collected, thoughtful, and well prepared. Her communication with other team members, consulting providers, patients, and families was very clear and she was always approachable/available for questions. Furthermore, her bedside manner was outstanding! Both patients and families felt very comfortable with her care. Cara would routinely review all the imaging on service herself including echos, cMRIs, nuclear studies, cath films before making her plans for the day. Her interpretations for the imaging studies would be spot even before the formal reads. Her assessments and plans were extremely well thought out and she also kept disposition/outpatient follow up plans always in the back of her mind as she led the service. The APPs on the PAC team also loved working with Cara and enjoyed learning from her on rounds. She really exemplified quality patient care, being an outstanding educator, as well as a superior team leader! Best, Nishant”
service all week which she took the lead on. She was calm, collected, thoughtful, and well prepared. Her communication with other team members, consulting providers, patients, and families was very clear and she was always approachable/available for questions. Furthermore, her bedside manner was outstanding! Both patients and families felt very comfortable with her care. Cara would routinely review all the imaging on service herself including echos, cMRIs, nuclear studies, cath films before making her plans for the day. Her interpretations for the imaging studies would be spot even before the formal reads. Her assessments and plans were extremely well thought out and she also kept disposition/outpatient follow up plans always in the back of her mind as she led the service. The APPs on the PAC team also loved working with Cara and enjoyed learning from her on rounds. She really exemplified quality patient care, being an outstanding educator, as well as a superior team leader! Best, Nishant”
Great work, Cara!!!
Shout-out to Duke Raleigh’s Heart Walk Team!
The team at Duke Raleigh Hospital held a Carnival Day that helped to raise $1600 in just three hours for their Heart Walk team. The funds raised will go to the American Heart Association. Way to go!
Note: Our own Sean Pokorney spent some time in the dunking booth that day – we’re not sure how many times he was dunked or how much was raised as a result, but what a team player!


Hot tip: Heart Walk T-Shirts
Speaking of the Heart Walk… tomorrow, we will be announcing to all DUHS employees that if you sign up by 5 p.m. on Wednesday, Aug. 24 as a walker (or team captain) for the upcoming Triangle Heart Walk you will receive a Duke team t-shirt. This is a hard deadline and you’re among the first to know!
If you can’t join us in person, please consider a contribution of any amount to one (or more!) of the nine teams representing Duke Heart. Help us meet our overall DUHS fundraising goals! Duke Heart’s teams can be found here: https://duke.is/6jpdp
Reminder: The Triangle Heart Walk is scheduled for Sunday, Sept. 25 at the PNC Arena.

Photos of the Week
It was a great week to be working in the CICU! Not one but two celebrations were held for cardiology fellow Willard Applefeld‘s birthday. Happy belated birthday!!


Also, a good week to be a member of the PWIM group – they gathered at Ponysaurus in Durham for some networking and camaraderie. Shout out to Jenn Rymer for her work with this amazing team of women!

COVID-19 Update
Please continue to practice safe COVID-19 protocols in your day-to-day interactions with others. Be particularly vigilant about masking, and avoid eating indoors in group settings. The health of our team members and our patients remains a priority as we continue to monitor the COVID-19 trends throughout our community.
Stay home if you are not feeling well. Employees who begin to experience any COVID-19 symptoms should report symptoms through the Duke SymMon app, which is available in both the Apple and Google app stores.
Donate blood if you’re able to. Click here for Duke-sponsored blood drives through the Red Cross.
All the latest Clinical Operations updates related to COVID can be found at https://covid-19.dukehealth.org. Patient-facing resources on DukeHealth.org can be found here: https://www.dukehealth.org/covid-19-update/resources. Duke University maintains a resource page as well, which can be accessed here: https://coronavirus.duke.edu/updates/for-staff.
Upcoming Events & Opportunities
Cardiology Grand Rounds
September 8: The Art and Science of Leadership with David Skorton, MD, President and CEO of the Association of American Medical Colleges (AAMC). 5 p.m. in Duke North Room 2002 and via WebEx.

CME & Other Events
September 12: Prostate Cancer & CVD Symposium. This is the third webinar of a four-part series. Collaboration between the International Cardio-Oncology Society & Duke Heart. Noon, Eastern. To learn more, please visit: https://duke.is/mbpte
September 25: Triangle Heart Walk. PNC Arena, Raleigh. Check-in and festivities start at 11 am. Walk begins at Noon. Join us!
October 14: Cardio-Oncology in the Era of Precision Medicine. Symposium to be held at the J.B. Duke Hotel, Durham, NC. Registration is open: https://bit.ly/CardioOnc22. Email Beth Tanner with questions: beth.tanner@duke.edu.
November 4: 14th Annual NC Research Triangle Pulmonary Hypertension Symposium. 7 a.m.-4 p.m. Save the date! This will be an in-person event at the Durham Convention Center. Registration required, but is not yet live. Stay tuned for updates.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
August 15 — Derek Chew
Health Day
Left Atrial Appendage Occlusion Favored for Some A-Fib Patients
https://duke.is/5ufpt
August 17 — Derek Chew and Jonathan Piccini
tctMD
Stroke, Bleeding Risks Key for Assessing Potential LAAO Benefit
https://
Division of Cardiology Publications Indexed in PubMed August 11-18, 2022
Allen LaPointe NM, Ali-Ahmed F, Dalgaard F, Kosinski AS, Sanders Schmidler G, Al-Khatib SM. Cardiac resynchronization therapy outcomes with left ventricular lead concordant with latest mechanical activation: A meta-analysis. Pacing Clin Electrophysiol 2022 Aug;45(8):930-939. PM: 35687711.
Altin SE, Gitto M, Secemsky EA, Rao SV, Hess CN. Sex-Based Differences in Periprocedural Complications Following Lower Extremity Peripheral Vascular Intervention. Circ Cardiovasc Interv 2022 Aug;15(8):e011768. PM: 35938403.
Attar R, Wu A, Wojdyla D, Jensen SE, Andell P, Mahaffey KW, Roe MT, James SK, Wallentin L, Vemulapalli S, Alexander JH, Lopes RD, Ohman EM, Hernandez AF, Patel MR, Jones WS. Outcomes After Acute Coronary Syndrome in Patients With Diabetes Mellitus and Peripheral Artery Disease (from the TRACER, TRILOGY-ACS, APPRAISE-2, and PLATO Clinical Trials). Am J Cardiol 2022 Sep 1;178:11-17. PM: 35835600.
Carlisle MA, Piccini JP, Fudim M. The interplay between autonomic tone and atrial arrhythmias. Clin Auton Res 2022 Aug;32(4):223-225. PM:35882685.
Chaitman BR, Cyr DD, Alexander KP, Pracoń R, Bainey KR, Mathew A, Acharya A, Kunichoff DF, Fleg JL, Lopes RD, Sidhu MS, Anthopolos R, Rockhold FW, Stone GW, Maron DJ, Hochman JS, Bangalore S. Cardiovascular and Renal Implications of Myocardial Infarction in the ISCHEMIA-CKD Trial. Circ Cardiovasc Interv 2022 Aug;15(8):e012103. PM: 35973009.
Chew DS, Li Y, Cowper PA, Anstrom KJ, Piccini JP, Poole JE, Daniels MR, Monahan KH, Davidson-Ray L, Bahnson TD, Al-Khalidi HR, Lee KL, Packer DL, Mark DB. Cost-Effectiveness of Catheter Ablation Versus Antiarrhythmic Drug Therapy in Atrial Fibrillation: The CABANA Randomized Clinical Trial. Circulation 2022 Aug 16;146(7):535-547. PM: 35726631.
Chunawala ZS, Qamar A, Arora S, Pandey A, Fudim M, Vaduganathan M, Bhatt DL, Mentz RJ, Caughey MC. Prevalence and Prognostic Significance of Polyvascular Disease in Patients Hospitalized With Acute Decompensated Heart Failure: The ARIC Study. J Card Fail 2022 Aug;28(8):1267-1277. PM: 35045321.
Denslow S, Wingert JR, Hanchate AD, Rote A, Westreich D, Sexton L, Cheng K, Curtis J, Jones WS, Lanou AJ, Halladay JR. Rural-urban outcome differences associated with COVID- 19 hospitalizations in North Carolina. PLoS One 2022 Aug 17;17(8):e0271755. PM: 35976813.
Dungan JR, Qin X, Gregory SG, Cooper-Dehoff R, Duarte JD, Qin H, Gulati M, Taylor JY, Pepine CJ, Hauser ER, Kraus WE. Sex-dimorphic gene effects on survival outcomes in people with coronary artery disease. Am Heart J Plus 2022 May;17:100152. PM: 35959094.
Fagundes A, Berg DD, Park JG, Baird-Zars VM, Newby LK, Barsness GW, Miller PE, van Diepen S, Katz JN, Phreaner N, Roswell RO, Menon V, Daniels LB, Morrow DA, Bohula EA. Patients With Acute Coronary Syndromes Admitted to Contemporary Cardiac Intensive Care Units: Insights From the CCCTN Registry. Circ Cardiovasc Qual Outcomes 2022 Aug;15(8):e008652. PM: 35862019.
Fordyce CB, Hill CL, Foldyna B, Douglas PS. Eligibility for Noninvasive Testing Based on the 2021 American Heart Association/American College of Cardiology Guideline for the Evaluation and Diagnosis of Stable Chest Pain: Implications From the PROMISE Trial. Circulation 2022 Aug 16;146(7):582-584. PM: 35969650
Fudim M, Fail PS, Litwin SE, Shaburishvili T, Goyal P, Hummel SL, Borlaug BA, Mohan RC, Patel RB, Mitter SS, Klein L, Rocha-Singh K, Patel MR, Reddy VY, Burkhoff D, Shah SJ. Endovascular ablation of the right greater splanchnic nerve in heart failure with preserved ejection fraction: early results of the REBALANCE-HF trial roll-in cohort. Eur J Heart Fail 2022 Aug;24(8):1410-1414. PM: 35598154.
Goldstein DJ, Puskas JD, Alexander JH, Chang HL, Gammie JS, Marks ME, Iribarne A, Vengrenyuk Y, Raymond S, Taylor BS, Yarden O, Orion E, Dagenais F, Ailawadi G, Chu MWA, DiMaio JM, Narula J, Moquete EG, O’Sullivan K, Williams JB, Crestanello JA, Jessup M, Rose EA, Scavo V, Acker MA, Gillinov M, Mack MJ, Gelijns AC, O’Gara PT, Moskowitz AJ, Bagiella E, Voisine P. External Support for Saphenous Vein Grafts in Coronary Artery Bypass Surgery: A Randomized Clinical Trial. JAMA Cardiol 2022 Aug 1;7(8):808-816. PM: 35675092.
Granger BB, Kaltenbach LA, Fonarow GC, Allen LA, Lanfear DE, Albert NM, Al-Khalidi HR, Butler J, Cooper LB, Dewald T, Felker GM, Heidenreich P, Kottam A, Lewis EF, Piña IL, Yancy CW, Granger CB, Hernandez AF, Devore AD. Health System-Level Performance in Prescribing Guideline-Directed Medical Therapy for Patients With Heart Failure With Reduced Ejection Fraction: Results From the CONNECT-HF Trial. J Card Fail 2022 Aug;28(8):1355-1361. PM: 35462033.
Greene SJ, Lautsch D, Yang L, Tan XI, Brady JE. Prognostic Interplay Between COVID-19 and Heart Failure With Reduced Ejection Fraction. J Card Fail 2022 Aug;28(8):1287-1297. PM: 35597512.
Hernandez AF, Albert NM, Allen LA, Ahmed R, Averina V, Boehmer JP, Cowie MR, Chien CV, Galvao M, Klein L, Kwan B, Lam CSP, Ruble SB, Stolen CM, Stein K. Multiple cArdiac seNsors for mAnaGEment of Heart Failure (MANAGE-HF) – Phase I Evaluation of the Integration and Safety of the HeartLogic Multisensor Algorithm in Patients With Heart Failure. J Card Fail 2022 Aug;28(8):1245-1254. PM: 35460884.
Kelsey MD, Newby LK. Recommendations for use of ezetimibe and/or PCSK9 inhibitors in patients with elevated LDL-C. Ann Intern Med 2022 Aug;175(8):JC86. PM: 35914252.
Lala A, Mentz RJ. Translating Nursing Partnerships in Clinical Care to Scientific Publishing. J Card Fail 2022 Aug;28(8):1243-1244. PM: 35961730.
Mentz RJ, Lautsch D, Pulungan Z, Kim S, Hilkert R, Teigland C, Yang M, Djatche L. Medication Trajectory and Treatment Patterns in Medicare Patients With Heart Failure and Reduced Ejection Fraction. J Card Fail 2022 Aug;28(8):1349-1354. PM: 34930657.
Moulson N, Petek BJ, Churchill TW, Drezner JA, Harmon KG, Kliethermes SA, Mellacheruvu P, Patel MR, Baggish AL. Cardiac Troponin Testing as a Component of Return to Play Cardiac Screening in Young Competitive Athletes Following SARS-CoV-2 Infection. J Am Heart Assoc 2022 Aug 16;11(16):e025369. PM: 35929475.
Stingl C, Dvergsten JA, Eng SWM, Yeung RSM, Fritzler MJ, Mason T, Crowson C, Voora D, Reed AM. Gene Expression Profiles of Treatment Response and Non-Response in Children With Juvenile Dermatomyositis. ACR Open Rheumatol 2022 Aug;4(8):671- 681. PM: 35616642.
Duke Heart Pulse August 14th 2022
Highlights of the week:
Celebrating Sunil Rao
 Please join us in wishing Sunil Rao, MD, professor of medicine in cardiology at Duke and section chief of cardiology at the Durham VA Medical Center all the best as he departs Durham and heads to NYU Langone Health System to serve as their director of interventional cardiology! He was recently celebrated by his team at the Durham VAMC. He has been the Chief of Cardiology at the VA since 2014. He initiated and grew the transradial catheterization program there and around the country. He also supported a number of VA programs including the Women’s Heart Health Program, Home-Based Cardiac Rehab, CardioMEMs, and robotic PCI (just to name a few). He has won numerous teaching and mentorship awards and supported successful VA Career Development Awards. He is leaving after 26 years at Duke and 18 years of VA service.
Please join us in wishing Sunil Rao, MD, professor of medicine in cardiology at Duke and section chief of cardiology at the Durham VA Medical Center all the best as he departs Durham and heads to NYU Langone Health System to serve as their director of interventional cardiology! He was recently celebrated by his team at the Durham VAMC. He has been the Chief of Cardiology at the VA since 2014. He initiated and grew the transradial catheterization program there and around the country. He also supported a number of VA programs including the Women’s Heart Health Program, Home-Based Cardiac Rehab, CardioMEMs, and robotic PCI (just to name a few). He has won numerous teaching and mentorship awards and supported successful VA Career Development Awards. He is leaving after 26 years at Duke and 18 years of VA service.
Sunil’s last official day at Duke and the VA was August 5. We had an opportunity to speak with him about his upcoming transition and his time at Duke. Here is some of what he shared with us:
“I did all my training at Duke and then joined the faculty in 2004. What I will remember most, obviously, are the people I’ve been fortunate enough to interact with during my time here. The people who mentored me, the fellows that I’ve interacted with, the junior faculty that I’ve worked with, the nurses, the nurse practitioners, the cath lab techs… Duke is a great place with incredible research and incredible clinical care, but at the end of the day, it’s the people that make the place. I feel really fortunate to have had the opportunity to work here,” he says. “When I was a medical student at Ohio State, the first two clinical rotations I did, the physicians that I interacted with had trained at Duke. When I was applying for residency programs, I knew that I wanted to be a cardiologist who had trained at Duke.
fortunate enough to interact with during my time here. The people who mentored me, the fellows that I’ve interacted with, the junior faculty that I’ve worked with, the nurses, the nurse practitioners, the cath lab techs… Duke is a great place with incredible research and incredible clinical care, but at the end of the day, it’s the people that make the place. I feel really fortunate to have had the opportunity to work here,” he says. “When I was a medical student at Ohio State, the first two clinical rotations I did, the physicians that I interacted with had trained at Duke. When I was applying for residency programs, I knew that I wanted to be a cardiologist who had trained at Duke.
“I consider myself one of the luckiest people in the world to have been able to train here and I feel really, really fortunate to have been able to work with all the people that I have while at Duke, and now to be able to take these lessons and apply them to my new position in New York.”
A big part of Sunil’s career has been his work at the Durham VAMC. He has been affiliated with the VA since completing his training 18 years ago.
“It is a huge privilege to be able to take care of veterans, I consider it an honor. The people that I’ve worked with at the VA have been phenomenal, too. They’ve always had the veterans best interests at heart and we’ve been able to do some really innovative things at the VA and develop, I think, what can only be described as really cutting-edge, innovative care. One of the things we’re very proud of is that the Durham VA recently achieved silver award quality status with the American Heart Association’s Get with the Guidelines registry. We are one of the few VAs that actually participate in that registry – and this was something that I felt was important for us to participate in, because I wanted to make sure that the quality of care that we delivered was not only on par with other VAs, but on par with or better than hospitals that we considered to be our peers, whether they were VA hospitals or not. This year, we had one of the highest ratings for quality of care for both acute coronary syndrome and stroke in the state of North Carolina. So we’re really proud of that. We’ve been laser-focused on delivering the highest quality of care to our veterans and creating opportunities for them to participate in innovative clinical research.”
We asked a number of Sunil’s colleagues for their reflections on his impact at Duke. Here is what they shared with us:
From Tom Povsic:
“It is rare to find people in academics with the complete skill set that Sunil possesses. Obviously, he has published extensively and was amongst the first to outline the detrimental impact bleeding has on outcomes in hospitalized patients and post-PCI. It’s hard to remember but most of the trials initially focused entirely on ischemic outcomes, with almost no attention paid to bleeding. But while many people publish, few then take the next step to transform care, and clearly one of the most effective strategies to mitigate bleeding is radial access. Sunil has been at the forefront of the transformation in PCI performance locally, nationally and internationally, and he did not stop there — changing the way we take care of patients based on sound clinical data to favor same-day discharge and, most recently, routine imaging to guide PCI. It’s amazing that one person has impacted care at the VA and Duke so much.
In addition, what I find truly astounding is how many people he knows by name. It’s impossible to go to a meeting with Sunil without him being constantly accosted by hordes of colleagues who want to speak with him, which just reflects his best attributes. And that is the type of person he is…deflecting attention from himself, promoting the interests of his colleagues and the many fellows and students he has mentored, and supporting group, rather than individual, efforts. We will miss his presence as a key thought leader, colleague and friend.”
From John Alexander:
“Sunil joined the Duke Cardiology faculty roughly 25 years ago and I have a hard time imagining Duke Cardiology without him. Sunil and I first met as cath lab fellows where he was identified early on by Jess Peter as the expert in cath-ing patients with extreme obesity. Sunil has always been a Master Educator with the knack for presenting complex topics simply. He was an early member of the Bleeding Mafia, revolutionizing the way we think about and measure bleeding as an adverse clinical outcome. Together with Mitch Krucoff and others, Sunil pioneered SAFE-PCI, the first Randomized Registry Trial leveraging the ACC’s NCDR Registry to collect data for a randomized trial comparing radial and femoral access in women undergoing coronary angiography and PCI. Sunil was the first interventional cardiologist at Duke to adopt Radial Access, seemingly training himself and then leading national training programs to train colleagues at Duke and elsewhere. Sunil has been and remains a Trusted Colleague. Sunil is now off to New York and NYU. Our loss is their gain. We can all look forward to seeing what Sunil does next. Wishing him all the best.”
From Tom Bashore:
“There have been few individuals that have come through the Duke program that have had a more positive impact than Sunil Rao. We often joked that he took the “golden pathway” to get here (both of us were graduates of Miami Ohio and Ohio State before coming to Duke). Sunil’s fantastic sense of humor, his incredibly caring instincts for others, his organizational skills and his impeccable clinical competence pushed his rapid rise through the system here. Those same characteristics were bound to eventually catch the eyes of folks nationally. It has been clear since early on that he would eventually be heavily recruited by others outside of Duke, and unfortunately for us, that time has now come. Though it really is a bummer to see Sunil move on, we can all take great pride in knowing he will be an outstanding representative of “all that is Duke” on the national stage.
And besides, if he doesn’t make it in the cardiology world in NYC, he has a real shot at a career in standup comedy there. And if that doesn’t work out, he is always welcome to come back “home” to Durham.”
From Mike Sketch:
“Sunil has the ideal academic pedigree being both a Buckeye and a Blue Devil!! He is an academic powerhouse at both Duke and worldwide… even without all his Twitter followers. What an amazing mentor he has been to so many fellows!
The most impressive thing about Sunil is his love and commitment to his wife, Carrie and to his four beautiful daughters! He will be so, so very missed.”
From Tony Gutierrez:
“Despite being the most technically gifted interventionalist I have ever worked with, Sunil’s greatest contribution to Duke these past 26 years is his relentless commitment towards mentoring young physician-scientists. Whether it’s learning how to draft a manuscript, perform a complex PCI, or navigating a difficult life moment, Sunil is the tiger dad every cardiology fellow needs to succeed. In the words of the great American hero RB, “Sunil is the best there is. Plain and simple.” Best of luck on your new endeavor.”
From Magnus Ohman:
“We both have had a great research career at Duke and it was so fitting that we were able to write our last editorial together and be published as we were both leaving Duke. Sunil has been an outstanding colleague.”
From Jenn Rymer:
“It’s hard to emphasize how much of an impact Sunil has had on both the faculty and fellows at Duke. He is one of those special people who always “elevate” those around him. I can remember during cath conferences or cine reviews that he would always highlight — in just minutes — a salient point about a case, and it made the process of learning from him a real privilege as a fellow and young faculty member. He is simultaneously a remarkably brilliant clinician, researcher and leader. As a fellow, he always took opportunities to introduce me to faculty outside of Duke at conferences and meetings, and is a real advocate for promoting Duke fellows for jobs and research opportunities. He is someone that I believe many young interventional cardiologists, like me, aspire to live up to. While we will all miss him here, I cannot wait to learn about the many successes that await him at NYU!”
From Rajesh Swaminathan:
“Sunil has been an amazing mentor, colleague, and friend. He has this unique ability to elevate the people around him in the most selfless way. He is particularly strong at mentoring fellows and early-career faculty. He supported my research and taught me the ins and outs of transradial interventions. Sunil has done an incredible job growing innovative programs at the VA. I’m glad that I will get to continue working with him through SCAI and societal committees and wish him all the best in the big city!”
And from Sean M. Wu, MD of Stanford, via Twitter:
“Congrats Sunil on your new leadership role @nyulangone. For just about my entire medical career I’ve associated you & @DukeMedSchool like PB&J. NYU is so fortunate to have you. I know you will do great things there in the coming year.”
We will miss your presence here with us at Duke, but you’ll always be part of our Duke Heart family. Best wishes, Sunil!
(Editor’s note: in the coming weeks, we’ll be recognizing Magnus Ohman as well as the recent retirement of Ken Morris.)
Fudim Receives DDCF Award

Congratulations to Marat Fudim, MD, MHS, assistant professor of medicine in cardiology at Duke for his selection as a 2022 recipient of a Doris Duke Charitable Foundation (DDCF) Clinical Scientist Development Award! This is an early-career development award that will support his project, “Role of the Splanchnic Vascular Compartment in Heart Failure with Preserved Ejection Fraction.”
Fudim has been working to understand the splanchnic nerve compartment’s role in heart failure for years. His team is now developing methods to simulate volume shifts, or volume distribution, so that they can better identify responders and non-responders ahead of time.
“We already know that not every medication or intervention can work for everybody,” he says. “We have seen the benefit of splanchnic nerve block in many people, but now we want to take a step back and ask how can we identify people who are more likely to be “volume shifters” versus “volume overloaders”? Who has the right physiology? Who will respond best?”
He says he doesn’t believe the situation is black and white, but that’s why he is eager to simulate volume distribution to see if there is an overlap between the phenotypes. Fudim hopes this will help lead to a better understanding of the contribution of volume redistribution to the average heart failure patient.
“It is a great honor for me to have been selected by the Doris Duke Charitable Foundation and I am especially appreciative in this time of very tight research funding,” Fudim said. “I believe this project will help bolster the entire field and that it will go beyond splanchnic nerve. It hopefully will help us get to the mechanism of how cardiac decompensation occurs.”
The DDCF announced their grant award recipients this week. Through the Clinical Scientist Development Awards, the foundation funds promising physician scientists whose projects have the potential to advance the prevention, diagnosis and treatment of human disease and to enable their transition to independent research careers.
A rigorous, multistage peer review process is done to evaluate each application on the significance, originality and research approach of their scientific proposals, and the research environment. According to the Foundation, a large share of this year’s recipients span a broad range of critical health issues and their grantees are diverse in representation, with 53 percent of the selected projects led by women and 23 percent by those identifying as Black or Hispanic/Latinx, which is critical for providing insights into the health concerns of a wide spectrum of the national population.
Duke interventional cardiologist Schuyler Jones, MD is a previous DDCF grant award recipient.
A list of additional 2022 grantees and their project titles can be found here: https://duke.is/vgcjj. Each recipient will receive a grant of $495,000 over three years which begins retroactively on July 1, 2022.
This is great news and well-deserved, Marat!
CMRI Team Granted IAC Accreditation
Our Duke Cardiac Magnetic Resonance Imaging (CMRI) program has achieved national accreditation for cardiovascular MRI and magnetic resonance angiogram (MRA) through the Intersocietal Accreditation Council (IAC). The application process includes a demanding clinical peer review that evaluates standards of care, safety criteria, and quality metrics of diagnostic images.
The awarded accreditation demonstrates the Duke Heart CMRI program’s commitment to the pursuit of excellence in its continuous quality improvements and documentation of safe, quality patient care in the field of MRI, setting the program apart from others.
Thank you to all team members who participated in the accreditation process with special thanks to Stephen Darty for preparing the submission.
Strong work, all!
Shout-out to Williams
Melissa Williams, clinical manager, Registry Team, in the Duke Heart Center of Excellence, has achieved the designation of  Certified Professional in Healthcare Quality (CPHQ).
Certified Professional in Healthcare Quality (CPHQ).
This is the only fully accredited credential in the field of healthcare quality. The CPHQ is accredited by the National Commission for Certifying Agencies which is the accrediting arm of the Institute for Credentialing Excellence.
Congratulations, Melissa — we are proud of you and so glad to have you on our team!

Celebrating an Engagement
Please join us in offering congratulations to Duke Heart cardiac sonographers Dallas Gardner and Eddy Sandoval on their recent engagement!
Eddy and Dallas met in the CDU and got engaged during a recent trip to the Outer Banks. Eddy popped the question on a private sunset cruise with a picture-perfect back drop. We are so happy for you, Dallas and Eddy!


Photo of the Week
Spotted on Twitter: Apparently our CICU has a sunshine committee that occasionally makes omelettes… We think that’s a great way to start the day and build camaraderie!

COVID-19 Update
Please continue to practice safe COVID-19 protocols in your day-to-day interactions with others. Be particularly vigilant about masking, and avoid eating indoors in group settings. The health of our team members and our patients remains a priority as we continue to monitor the COVID-19 trends throughout our community.
Stay home if you are not feeling well. Employees who begin to experience any COVID-19 symptoms should report symptoms through the Duke SymMon app, which is available in both the Apple and Google app stores.
Donate blood if you’re able to. Click here for Duke-sponsored blood drives through the Red Cross.
All the latest Clinical Operations updates related to COVID can be found at https://covid-19.dukehealth.org. Patient-facing resources on DukeHealth.org can be found here: https://www.dukehealth.org/covid-19-update/resources. Duke University maintains a resource page as well, which can be accessed here: https://coronavirus.duke.edu/updates/for-staff.
Upcoming Events & Opportunities
August 17: Duke GME DEI ‘First Look’. The Duke Office of Graduate Medical Education is holding a virtual DEI ‘First Look’ event for potential incoming residents and fellows. It’s specifically designed for underrepresented applicants and any applicant interested in DEI issues. Registration is required.
August 17: Duke Health Annual Blood Drive. 9:30 a.m. to 3 p.m., Searle Conference Center, Seeley G. Mudd Building. Appointments required. Please sign up at http://www.redcrossblood.org using sponsor code: Duke.
September 12: Prostate Cancer & CVD Symposium. This is the third webinar of a four-part series. Collaboration between the International Cardio-Oncology Society & Duke Heart. Noon, Eastern. To learn more, please visit: https://duke.is/mbpte
September 25: Triangle Heart Walk. PNC Arena, Raleigh. Check-in starts at 11 am. Walk begins at Noon. Join us!
October 14: Cardio-Oncology in the Era of Precision Medicine. Symposium to be held at the J.B. Duke Hotel, Durham, NC. Registration is open: https://bit.ly/CardioOnc22. Email Beth Tanner with questions: beth.tanner@duke.edu.
November 4: 14th Annual NC Research Triangle Pulmonary Hypertension Symposium. 7 a.m.-4 p.m. Save the date! This will be an in-person event at the Durham Convention Center. Registration required, but is not yet live. Stay tuned for updates.
Cardiology Grand Rounds
Cardiology Grand Rounds has concluded and will resume in September.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
August 5 — Harry Severance
Emergency Physicians Monthly
‘Burnout’ and the Healthcare Workplace
https://duke.is/n7q83
August 9 — Sunil Rao
Medpage Today
Potent DAPT After CABG Halves Vein Graft Failure
https://duke.is/bdzpc
August 9 — E. Magnus Ohman
Healio/Cardiology
Adding ticagrelor to aspirin reduces vein graft failure, increases bleeding after CABG
https://duke.is/42eun
August 10 — Pamela Douglas
Nature Reviews Cardiology
Implementing an anti-bullying culture in cardiology
PDF: https://duke.is/9rbk8
August 10 — Joe Turek and Louise Markert
ACC Expert Analysis
A Small Step For Heart Transplantation But a Huge Leap For Infant Heart Transplantation
https://duke.is/jkpzq
August 11 — J. Antonio Gutierrez
Time.com
What to Know About Peripheral Artery Disease—and Its Connection to Diabetes
Division of Cardiology Publications Indexed in PubMed July 21–August 10, 2022
Baksh SS, Hodgkinson CP. Conservation of miR combo based direct cardiac reprogramming. Biochem Biophys Rep 2022;31:101310. PM: 35860436.
Beller JP, Mehaffey JH, Wegermann ZK, Grau- Sepulveda M, O’Brien SM, Brennan JM, Thourani V, Badhwar V, Pagani FD, Ailawadi G, Yarboro LT, Teman NR. Strategies for Mechanical Right Ventricular Support During Left Ventricular Assist Device Implant. Ann Thorac Surg 2022;114(2):484-491. PM: 34843696.
Caruba T, Charles-Nelson A, Alexander JH, Mehta RH, Heringlake M, Toller W, Yavchitz A, Sabatier B, Chatellier G, Cholley B. Prophylactic levosimendan in patients with low ejection fraction undergoing coronary artery bypass grafting: A pooled analysis of two multicentre randomised controlled trials. Anaesth Crit Care Pain Med 2022;41(4):101107. PM: 35643391.
Cools F, Virdone S, Sawhney J, Lopes RD, Jacobson B, Arcelus JI, Hobbs FDR, Gibbs H, Himmelreich JCL, MacCallum P, Schellong S, Haas S, Turpie AGG, Ageno W, Rocha AT, Kayani G, Pieper K, Kakkar AK. Thromboprophylactic low-molecular-weight heparin versus standard of care in unvaccinated, at-risk outpatients with COVID-19 (ETHIC): an open-label, multicentre, randomised, controlled, phase 3b trial. Lancet Haematol 2022;9(8):e594-e604. PM: 35779560.
Czura CJ, Bikson M, Charvet L, Chen JDZ, Franke M, Fudim M, Grigsby E, Hamner S, Huston JM, Khodaparast N, Krames E, Simon BJ, Staats P, Vonck K. Neuromodulation Strategies to Reduce Inflammation and Improve Lung Complications in COVID-19 Patients. Front Neurol 2022;13:897124. PM: 35911909.
Domingo-Relloso A, Makhani K, Riffo-Campos AL, Tellez-Plaza M, Klein KO, Subedi P, Zhao J, Moon KA, Bozack AK, Haack K, Goessler W, Umans JG, Best LG, Zhang Y, Herreros-Martinez M, Glabonjat RA, Schilling K, Galvez-Fernandez M, Kent JW, Sanchez TR, Taylor KD, Johnson WC, et al. Arsenic Exposure, Blood DNA Methylation, and Cardiovascular Disease. Circ Res 2022;131(2):e51-e69. PM: 35658476.
Fanaroff AC, Wang TY. Risk Prediction in Percutaneous Coronary Intervention: Solving the Last Mile Problem. Circ Cardiovasc Interv 2022;15(7):e012262. PM: 35861801.
Friedman DJ, Tully AS, Zeitler EP. Subcutaneous and Transvenous ICDs: an Update on Contemporary Questions and Controversies. Curr Cardiol Rep 2022;24(8):947-958. PM: 35639275.
Goldstein SA, Pagidipati NJ. Hypertensive Disorders of Pregnancy and Heart Failure Risk. Curr Hypertens Rep 2022;24(7):205-213. PM: 35347569.
Harrington J, Felker GM, Mentz RJ. Catastrophic Disruptions in Clinical Trials. Circulation 2022;146(5):369-371. PM: 35914015.
Hogan SE, Nehler MR, Anand S, Patel MR, Debus S, Jackson MT, Buchanan C, King RW, Hess C, Muehlhofer E, Haskell LP, Bauersachs RM, Berkowitz SD, Hsia J, Bonaca MP. Improvement in walking impairment following surgical and endovascular revascularization: Insights from VOYAGER PAD. Vasc Med 2022;27(4):343-349. PM: 35467452.
Jensen AD, Østergaard L, Petersen JK, Graversen P, Butt JH, Bundgaard H, Moser C, Smerup MH, Modrau IS, Iversen K, Bruun NE, Torp-Pedersen C, Gislason G, Wang A, Ragnarsson S, Povlsen JA, Køber L, Fosbøl EL. Surgical treatment of patients with infective endocarditis: changes in temporal use, patient characteristics, and mortality-a nationwide study. BMC Cardiovasc Disord 2022;22(1):338. PM: 35906539.
Khan MS, Shahid I, Fonarow GC, Greene SJ. Classifying heart failure based on ejection fraction: imperfect but enduring. Eur J Heart Fail 2022;24(7):1154-1157. PM: 35239210.
Khouri MG, Greene SJ. Sodium-Glucose Co-Transporter-2 Inhibitor Therapy During Anthracycline Treatment: Is There a Role for Cardioprotection? JACC Heart Fail 2022;10(8):568-570. PM: 35902160.
Kosiborod MN, Angermann CE, Collins SP, Teerlink JR, Ponikowski P, Biegus J, Comin-Colet J, Ferreira JP, Mentz RJ, Nassif ME, Psotka MA, Tromp J, Brueckmann M, Blatchford JP, Salsali A, Voors AA. Effects of Empagliflozin on Symptoms, Physical Limitations, and Quality of Life in Patients Hospitalized for Acute Heart Failure: Results From the EMPULSE Trial. Circulation 2022;146(4):279-288. PM: 35377706.
Lamas GA, Anstrom KJ, Navas-Acien A, Boineau R, Kim H, Rosenberg Y, Stylianou M, Jones TLZ, Joubert BR, Santella RM, Escolar E, Aude YW, Fonseca V, Elliott T, Lewis EF, Farkouh ME, Nathan DM, Mon AC, Gosnell L, Newman JD, Mark DB. The trial to assess chelation therapy 2 (TACT2): Rationale and design. Am Heart J 2022;252:1-11. PM: 35598636.
Lee M, Huan T, McCartney DL, Chittoor G, de Vries M, Lahousse L, Nguyen JN, Brody JA, Castillo- Fernandez J, Terzikhan N, Qi C, Joehanes R, Min JL, Smilnak GJ, Shaw JR, Yang CX, Colicino E, Hoang TT, Bermingham ML, Xu H, Justice AE, Xu CJ, Rich SS, Cox SR, Vonk JM, Prokić I, et al. Pulmonary Function and Blood DNA Methylation: A Multiancestry Epigenome-Wide Association Meta- analysis. Am J Respir Crit Care Med 2022;206(3):321-336. PM: 35536696.
Lewis GD, Voors AA, Cohen-Solal A, Metra M, Whellan DJ, Ezekowitz JA, Böhm M, Teerlink JR, Docherty KF, Lopes RD, Divanji PH, Heitner SB, Kupfer S, Malik FI, Meng L, Wohltman A, Felker GM. Effect of Omecamtiv Mecarbil on Exercise Capacity in Chronic Heart Failure With Reduced Ejection Fraction: The METEORIC-HF Randomized Clinical Trial. JAMA 2022;328(3):259-269. PM: 35852527.
Li G, Zhang J, Van Spall HGC, Douglas PS, Wang Y, Sun X, Thabane L. Exploring ethnic representativeness in diabetes clinical trial enrolment from 2000 to 2020: a chronological survey. Diabetologia 2022;65(9):1461-1472. PM: 35705796.
Limkakeng AT, Rowlette LL, Hatch A, Nixon AB, Ilkayeva O, Corcoran D, Modliszewski J, Griffin SM, Ginsburg GS, Voora D. A precision medicine approach to stress testing using metabolomics and microribonucleic acids. Per Med 2022;19(4):287-297. PM: 35466688.
Loring Z, Holmqvist F, Sze E, Alenezi F, Campbell K, Koontz JI, Velazquez EJ, Atwater BD, Bahnson TD, Daubert JP Acute echocardiographic and hemodynamic response to his-bundle pacing in patients with first-degree atrioventricular block. Ann Noninvasive Electrocardiol 2022;27(4):e12954. PM: 35445488.
McIntyre WF, Wang J, Benz AP, Johnson L, Connolly SJ, Van Gelder IC, Lopes RD, Gold MR, Hohnloser SH, Lau CP, Israel CW, Wong JA, Conen D, Healey JS. Estimated incidence of previously undetected atrial fibrillation on a 14-day continuous electrocardiographic monitor and associated risk of stroke. Europace 2022;24(7):1058-1064. PM: 35061877.
Minhas AMK, Ijaz SH, Javed N, Sheikh AB, Jain V, Michos ED, Greene SJ, Fudim M, Warraich HJ, Shapiro MD, Al-Kindi SG, Sperling L, Virani SS. National trends and disparities in statin use for ischemic heart disease from 2006 to 2018: Insights from National Ambulatory Medical Care Survey. Am Heart J 2022;252:60-69. PM: 35644222.
Olsen C, Mandawat A, Sun JL, Triana T, Chiswell K, Karra R. Recovery of left ventricular function is associated with improved outcomes in LVAD recipients. J Heart Lung Transplant 2022;41(8):1055-1062. PM: 35410822.
Pandey A, Segar MW, Singh S, Reeves GR, O’Connor C, Piña I, Whellan D, Kraus WE, Mentz RJ, Kitzman DW. Frailty Status Modifies the Efficacy of Exercise Training Among Patients With Chronic Heart Failure and Reduced Ejection Fraction. Circulation 2022;146(2):80-90. PM: 35616018.
Petek BJ, Moulson N, Baggish AL, Kliethermes SA, Patel MR, Churchill TW, Harmon KG, Drezner JA, et al. Prevalence and clinical implications of persistent or exertional cardiopulmonary symptoms following SARS- CoV-2 infection in 3597 collegiate athletes: a study from the Outcomes Registry for Cardiac Conditions in Athletes (ORCCA). Br J Sports Med 2022;56(16):913-918. PM: 34725052.
Piccini JP, Cunnane R, Steffel J, El-Chami MF, Reynolds D, Roberts PR, Soejima K, Steinwender C, Garweg C, Chinitz L, Ellis CR, Stromberg K, Fagan DH, Mont L. Development and validation of a risk score for predicting pericardial effusion in patients undergoing leadless pacemaker implantation: experience with the Micra transcatheter pacemaker. Europace 2022;24(7):1119-1126. PM: 35025987.
Pohlman FW, Ford CB, Weissler EH, Smerek MM, Hardy NC, Narcisse DI, Lippmann SJ, Greiner MA, Long C, Rymer JA, Gutierrez JA, Patel MR, Jones WS. Impact of risk factor control on peripheral artery disease outcomes and health disparities. Vasc Med 2022;27(4):323-332. PM: 35387516.
Pokorney SD, Berchuck SI, Chiswell K, Sun JL, Thomas L, Jones WS, Patel MR, Piccini JP. Atrial branch coronary artery stenosis as a mechanism for atrial fibrillation. Heart Rhythm 2022;19(8):1237-1244. PM: 34958941
Pokorney SD, Granger CB. Evidence Builds for Catheter Ablation for Atrial Fibrillation and Heart Failure. Cardiovasc Res 2022;118(9):2112-2123. PM: 34358298
Polonsky TS, Khera A, Miedema MD, Schocken DD, Wilson PWF. Highlights in ASCVD Primary Prevention for 2021. J Am Heart Assoc 2022;11(13):e025973. PM: 35785971.
Vogel RF, Delewi R, Wilschut JM, Lemmert ME, Diletti R, van Vliet R, van der Waarden NWPL, Nuis RJ, Paradies V, Alexopoulos D, Zijlstra F, Montalescot G, Angiolillo DJ, Krucoff MW, Smits PC, Van Mieghem NM, Vlachojannis GJ. Pre-hospital treatment with crushed versus integral tablets of prasugrel in patients presenting with ST- Segment Elevation Myocardial Infarction-1-year follow- up results of the COMPARE CRUSH trial. Am Heart J 2022;252:26-30. PM: 35671829.
Wang TY. Mentorship and the Leaky Pipeline in Academic Cardiology. Circ Cardiovasc Qual Outcomes 2022;15(7):e009218. PM: 35562107.
Zhang X, Yamada Y, Sagayama H, Ainslie PN, Blaak EE, Buchowski MS, Close GL, Cooper JA, Das SK, Dugas LR, Gurven M, El Hamdouchi A, Hu S, Joonas N, Katzmarzyk P, Kraus WE, Kushner RF, Leonard WR, Martin CK, Meijer EP, Neuhouser ML, Ojiambo RM, Pitsiladis YP, Plasqui G, et al. Human total, basal and activity energy expenditures are independent of ambient environmental temperature. iScience 2022;25(8):104682. PM: 35865134
Ferencik M, Mayrhofer T, Lu MT, Bittner DO, Emami H, Puchner SB, Meyersohn NM, Ivanov AV, Adami EC, Voora D, Ginsburg GS, Januzzi JL, Douglas PS, Hoffmann U. Coronary Atherosclerosis, Cardiac Troponin, and Interleukin-6 in Patients With Chest Pain: The PROMISE Trial Results. JACC Cardiovasc Imaging 2022;15(8):1427-1438. PM: 35926901.
Grenier-Larouche T, Coulter Kwee L, Deleye Y, Leon-Mimila P, Walejko JM, McGarrah RW, Marceau S, Trahan S, Racine C, Carpentier AC, Lusis AJ, Ilkayeva O, Vohl MC, Huertas-Vazquez A, Tchernof A, Shah SH, Newgard CB, White PJ. Altered branched-chain α-keto acid metabolism is a feature of NAFLD in individuals with severe obesity. JCI Insight 2022;7(15):10.1172/jci.insight.159204. PM: 35797133.
Rao SV, Ohman EM. Balancing the Risks and Benefits of Antiplatelet Therapy After Coronary Artery Bypass Graft Surgery. JAMA 2022;328(6):532-533. PM: 35943481.
Rasmussen LD, Fordyce CB, Nissen L, Hill CL, Alhanti B, Hoffmann U, Udelson J, Bøttcher M, Douglas PS, Winther S. The PROMISE Minimal Risk Score Improves Risk Classification of Symptomatic Patients With Suspected CAD. JACC Cardiovasc Imaging 2022;15(8):1442-1454. PM: 35926903.
Salah HM, Minhas AMK, Khan MS, Pandey A, Michos ED, Mentz RJ, Fudim M. Causes of hospitalization in the USA between 2005 and 2018. Eur Heart J Open 2021;1(1):oeab001. PM: 35919090.
Toro C, Hatfield J, Temkin N, Barber J, Manley G, Ohnuma T, Komisarow J, Foreman B, Korley FK, Vavilala MS, Laskowitz DT, Mathew JP, Hernandez A, Sampson J, James ML, Raghunathan K, Goldstein BA, Markowitz AJ, Krishnamoorthy V. Risk Factors and Neurological Outcomes Associated With Circulatory Shock After Moderate-Severe Traumatic Brain Injury: A TRACK-TBI Study. Neurosurgery 2022;91(3):427-436. PM: 35593705.
Weissler EH, Mulder H, Rockhold FW, Baumgartner I, Norgren L, Blomster J, Katona BG, Fowkes FGR, Mahaffey K, Bonaca M, Patel MR, Jones WS. Understanding Study Drug Discontinuation Through EUCLID. Front Cardiovasc Med 2022;9:947645. PM: 35928933.
Duke Heart Pulse – August 7th 2022
Chief’s message:
We have been fortunate over the last several years to partner with the Joel Cornette Foundation and now a partnership with the  American Heart Association to better understand, study, and inform the care of young competitive athletes. The studies we have been looking to conduct evaluate the overlap between human physiology, performance, and cardiovascular risk. We aim to improve our understanding and to help our athletes make shared decisions around returning to play, preventing sudden cardiac events, and improving their performance. This week I was fortunate to attend and give some remarks at the Cornette Foundation fund raising event. It was great event in Cincinnati and we were fortunate to have several sports stars in attendance and supporting the work including: Charles Barkley, Carlos Boozer, Jay Williams, Brad Stevens, and several others. Thanks to all that work and support this work that Duke Heart has the opportunity be a part of and help lead.
American Heart Association to better understand, study, and inform the care of young competitive athletes. The studies we have been looking to conduct evaluate the overlap between human physiology, performance, and cardiovascular risk. We aim to improve our understanding and to help our athletes make shared decisions around returning to play, preventing sudden cardiac events, and improving their performance. This week I was fortunate to attend and give some remarks at the Cornette Foundation fund raising event. It was great event in Cincinnati and we were fortunate to have several sports stars in attendance and supporting the work including: Charles Barkley, Carlos Boozer, Jay Williams, Brad Stevens, and several others. Thanks to all that work and support this work that Duke Heart has the opportunity be a part of and help lead.
Highlights of the week:
Duke Surgery Announces New Division Chief of Vascular and Endovascular Surgery
 The Duke Department of Surgery this week announced the appointment of Dawn Marie Coleman, MD, FACS, to the role of Chief of the Division of Vascular and Endovascular Surgery.
The Duke Department of Surgery this week announced the appointment of Dawn Marie Coleman, MD, FACS, to the role of Chief of the Division of Vascular and Endovascular Surgery.
Coleman, a clinical professor of surgery and pediatrics, joins Duke from the University of Michigan in Ann Arbor where she served as co-director of the Pediatric Renovascular Hypertension Center as well as program director for the Integrated Vascular Surgery Residency and Fellowship at Michigan.
Her clinical and translational research interests encompass a unique pediatric vascular surgery practice, and her research leverages a multidisciplinary team to deeply phenotype patients with renovascular hypertension resulting from aorto-renal arterial dysplasia. She has made several high impact research contributions to this rare disease, and received major funding from the Taubman Institute, National Institutes of Health, Department of Defense, and the Patient-Centered Outcomes Research Institute. Dr. Coleman also leads an international pRVH patient-centered outcomes research collaborative.
Coleman serves as a lieutenant colonel in the U.S. Army Reserve, assigned to a Forward Resuscitative Surgical Team. She has deployed on three occasions to support forward operations in the Middle East.
“After a nationwide search, I am thrilled to welcome Dr. Coleman to Duke,” says Dr. Allan D. Kirk, Chair of the Department of Surgery. “She is a superb clinician, a skilled investigator, and an effective educator. However, I believe her towering strength is her humanistic approach toward leadership. Dr. Coleman’s rich, real world experience serves as a strong foundation for her executive intuition, and we are so fortunate to have her lead the growth of both the department and the Division of Vascular and Endovascular Surgery.”
Coleman obtained her Bachelor of Science degree in Biology from the University of Cincinnati, where she went on to obtain her Doctor of Medicine degree in 2003. She completed her general surgery residency at the University of Michigan Medical Center in 2010, and subsequently completed a fellowship in vascular surgery at Michigan in 2012. Upon completing her surgical training, Coleman joined the faculty as a clinical assistant professor in surgery at both the University of Michigan and the VA Ann Arbor Healthcare System.
Coleman holds leadership positions in several professional societies and associations, most recently having joined the Society of University Surgeons and the Excelsior Surgical Society. She is a dedicated surgeon educator and mentor, and is currently appointed as the President-Elect for the Association of Program Directors in Vascular Surgery. She has contributed review service to several peer-reviewed journals, and is currently a member of the editorial board for Vascular and Endovascular Surgery as well as Vascular Surgery Associate Editor for the Journal of Surgical Research.
“I am absolutely thrilled to join the extraordinary faculty and leadership of the Duke Department of Surgery,” says Dr. Coleman. “It’s an exciting time to join such a high performing team and renowned medical institution. I am beyond grateful for Dr. Shortell’s progressive divisional leadership to date, and the opportunity I have been granted by Dr. Kirk and Institutional Leadership to steward this division forward. Duke is renowned for being forward-thinking and at the forefront of surgical innovation, advancements in patient care, and dedication to research. I am certain that Duke Vascular and Endovascular Surgery will continue to excel and lead with clinical, educational, and academic excellence locally and nationally.”
Since 2005, Cynthia Shortell, MD, professor of surgery and Executive Vice Chair of the Department of Surgery, has skillfully led the Division of Vascular and Endovascular Surgery as Division Chief. Since 2006, she has also served as chief for the Section of Vascular Surgery at the Durham VA Medical Center; Director of Duke’s Center for Vascular Disease; Director for Duke’s Venous Center of Excellence; and Medical Director for Duke’s Vascular Non-Invasive Laboratory.
Shortell will continue her stewardship of the division as a faculty member and through her departmental leadership positions.
“I would like to thank Dr. Cynthia Shortell for her extraordinary leadership over the past 17 years in the division, to which she brought unparalleled dedication and enthusiasm,” says Dr. Kirk. “I am pleased that she will remain on our faculty at Duke Surgery as well as an integral piece of our department’s administration as Executive Vice Chair. I am excited to witness her continue to lead and develop our various educational programs.”
“I am delighted to welcome Dr. Coleman to her new role,” says Dr. Shortell. “She is exceptionally well qualified and has the strong leadership skills needed to take our division forward. I am committed to working closely with her to make the transition a smooth one.”
Coleman’s appointment as Chief of the Division of Vascular and Endovascular Surgery begins October 1, 2022.
We look forward to working with her!
HAV Pre-Clinical Work Presented at AHA BCVS
 Adam Williams, MD, Duke cardiothoracic surgeon, presented pre-clinical results of an off-the-shelf Human Acellular Vessel (HAV) in a nonhuman primate model of coronary artery bypass grafting at the American Heart Association’s Basic Cardiovascular Sciences (BCVS) 2022 annual scientific sessions held July 25-27 at the Hilton Chicago in Chicago, IL.
Adam Williams, MD, Duke cardiothoracic surgeon, presented pre-clinical results of an off-the-shelf Human Acellular Vessel (HAV) in a nonhuman primate model of coronary artery bypass grafting at the American Heart Association’s Basic Cardiovascular Sciences (BCVS) 2022 annual scientific sessions held July 25-27 at the Hilton Chicago in Chicago, IL.
The team demonstrated patent graphs at six months post-implantation and host repopulation of the HAV with vascular cells. Their results will be published in the September issue of Circulation Research.
Williams and his team are performing pre-clinical trials for HAV, a product of Humacyte, at Duke. Williams is serving as PI for the study. He is one of the lead surgeons along with Alan Kypson, MD from UNC Healthcare/Rex. Kypson is a former resident and fellow at Duke. Drs. Mihai Podgoreanu and Sharon McCarthy are Duke cardiothoracic anesthesiologists on the project team.
“This has been a great collaboration between Humacyte and Duke in an effort to bring novel therapies to the market,” says Williams.
Humacyte’s HAVs are engineered replacement vessels designed to be durable, infection-resistant and off-the-shelf to address long-standing limitations in vessel tissue repair and replacement. CABG surgery, which treats the blockage of the coronary arteries to restore blood flow to the heart, is performed more than 400,000 times annually in the United States, with over 765,000 annual CABG procedures globally. Humacyte is developing a small-diameter HAV as a potential alternative to existing vascular conduit substitutes during CABG surgery, particularly in obese or diabetic patients, where the risks of saphenous vein harvesting are substantial.
Laura Nicholson, MD, CEO of Humacyte is a former Duke faculty member.
Congratulations, Adam! We look forward to learning more about this great work!

New Cardiology Fellowship Program Coordinator Announced
 We are pleased to announce that Brianna Small has accepted our Cardiology Fellowship Program Coordinator position.
We are pleased to announce that Brianna Small has accepted our Cardiology Fellowship Program Coordinator position.
Brianna was born and raised in Hadley, PA, went to West Virginia University (WVU) and earned her Bachelor’s degree in Criminology and dual Master’s degrees in Social Work and Public Administration. She most recently worked with WVU faculty, staff, residents and fellows on wellness in her role as a graduate assistant at the internal employee assistance program.
Outside of work, Brianna enjoys kayaking, exercising, and shopping. Brianna said she is looking forward to joining our team because of the sense of community and to have the opportunity to work with fellows and assist them along their journey! She will join our team at the end of August.
Once her Duke contact information is established, we’ll share that with the team.
On behalf of Anna Lisa Chamis, we extend a huge THANK YOU to the program coordinator selection committee members for their hard work during the past 3+ months: Richa Agarwal, Chris Holley, Neha Pagidipati, Lisa Criscione Schreiber, Jill Rimmer and Lynsey Easley.
Please extend a warm welcome to Brianna when she arrives in a few weeks!
Call for Nominations: DHIP Strategic & Operational Committees
NOTE: Deadline is Tuesday, August 9 at 5 p.m.
The DHIP planning process is designed to ensure broad participation from physicians, other providers and staff to create the new clinical practice. There are seats designated for PDC members and staff on all key committees (click here for the total number of seats per Committee).
There are two levels of involvement for PDC members and staff: Committee Representative or Participant.
Committees
To be considered to serve as a PDC representative on the various DHIP Committees, please complete the form below. You may be nominated for only one Committee. Committee members should expect to spend 4-6 hours per week on Committee-related work, and will not be compensated for their time. Each Committee will have a designated staff lead, project manager and communications professional to support its work.
Participants
For physicians, other providers and staff who would like to stay apprised of the work of the Committees, but do not have the time to serve as a Committee representative, you may sign up to be a Participant to the Committee. Participants can offer direct input into the committee via elected liaisons, and will receive regular updates on the Committees’ work. There is no limit on the number of Committees on which you can be a Participant.
To be included as a Participant, please complete the form at the link below and indicate the Committees for which you would like to be a Participant. There is no limit on the number of Committees on which you can participate. Once the Participant groups have been formed, a separate process will be used to elect 2-3 PDC liaisons from within this population to serve on each Committee.
Strategic and Operational Transition Committees
(read: Committee descriptions and number of designated seats per entity here)
- Change Management and Culture (2 PDC positions)
- Diversity, Equity and Inclusion (2 PDC positions)
- PDC Team/Staff Transition (2 PDC positions)
- Advanced Practice Provider Transition (2 PDC positions)
- Community Practices (3 PDC positions)
- Funds Flow and Physician Compensation (2 PDC positions)
- New Hire Process (2 PDC positions)
Committee Eligibility
- Nominations are open to current PDC physicians, providers and staff with demonstrated experience in the subject area
- Nominees must submit a 250 word summary of their expertise
- Individuals may nominate themselves for only one Committee
Committee Selection Process
- The selection team includes the PDC Executive Committee, PDC CMO and ACMO for DEI.
- The selection team will base decisions on subject matter expertise, diversity, stakeholder perspective and leadership acumen.
- Nominees who are not selected will be added to the Participants group for the chosen Committee.
Send questions to PDC-President@dm.duke.edu
To access the Qualtrics nomination form click here.
DCRI selected as Coordinating Center for NIH RECOVER Long COVID Initiative
The Duke Clinical Research Institute (DCRI) has been named the Clinical Trials Data Coordinating Center for large-scale national research studies aimed at understanding and improving the treatment of long COVID.
As the data coordinating center, DCRI will partner with RTI International, the study’s Administrative Coordinating Center, to accelerate the clinical trial process, oversee the study’s program-wide infrastructure, establish a patient registry, and launch simultaneous prevention and therapeutic multi-intervention studies among adults and children.
The data coordinating center is part of the National Institutes of Health (NIH) Researching COVID to Enhance Recovery (RECOVER) initiative. In December 2020, Congress provided $1.15 billion in funding over four years for NIH to support research into the prolonged health consequences of SARS-CoV-2 infection.
RECOVER brings together patients, caregivers, clinicians, community leaders, and scientists from across the nation to understand, prevent, and treat long COVID. The initiative comprises multiple sub-awards to researchers at institutions across the country.
To read more, click here.
Ginsburg to Receive Leadership in Personalized Medicine Award
 We learned this week that the Personalized Medicine Coalition (PMC) will present its 17th Annual Award for Leadership in Personalized Medicine to Geoffrey S. Ginsburg, MD during the PMC summit Personalized Medicine and the Patient scheduled for Nov. 14-15, 2022, at the Hotel Commonwealth in Boston, MA. The award to Ginsburg will be presented on Nov. 15 by Jay Wohlgemuth, MD, chief medical officer and senior vice president of Quest Diagnostics. After accepting the award, Ginsburg, who now serves as the Chief Medical and Scientific Officer of the U.S. National Institutes of Health’s All of Us Research Program, will present on the future of personalized medicine and patient care from his new vantage point at the NIH. To learn more about the Summit, visit: https://pmandthepatient.org.
We learned this week that the Personalized Medicine Coalition (PMC) will present its 17th Annual Award for Leadership in Personalized Medicine to Geoffrey S. Ginsburg, MD during the PMC summit Personalized Medicine and the Patient scheduled for Nov. 14-15, 2022, at the Hotel Commonwealth in Boston, MA. The award to Ginsburg will be presented on Nov. 15 by Jay Wohlgemuth, MD, chief medical officer and senior vice president of Quest Diagnostics. After accepting the award, Ginsburg, who now serves as the Chief Medical and Scientific Officer of the U.S. National Institutes of Health’s All of Us Research Program, will present on the future of personalized medicine and patient care from his new vantage point at the NIH. To learn more about the Summit, visit: https://pmandthepatient.org.
Wonderful news, Geoff – congratulations!
Photos of the Week
A group of Duke CCU colleagues from across the decades — past and present — gathered at Local 22 on Saturday, July 30 to celebrate Karol Harshaw-Ellis and her years of service to Duke Cardiology. How many of these faces do you recognize?
Congratulations, Karol! So nice to see this group gather to celebrate you!


COVID-19 Update
Please continue to practice safe COVID-19 protocols in your day-to-day interactions with others. Be particularly vigilant about masking, and avoid eating indoors in group settings. The health of our team members and our patients remains a priority as we continue to monitor the COVID-19 trends throughout our community.
Stay home if you are not feeling well. Employees who begin to experience any COVID-19 symptoms should report symptoms through the Duke SymMon app, which is available in both the Apple and Google app stores.
Donate blood if you’re able to. Click here for Duke-sponsored blood drives through the Red Cross.
All the latest Clinical Operations updates related to COVID can be found at https://covid-19.dukehealth.org. Patient-facing resources on DukeHealth.org can be found here: https://www.dukehealth.org/covid-19-update/resources. Duke University maintains a resource page as well, which can be accessed here: https://coronavirus.duke.edu/updates/for-staff.
Upcoming Events & Opportunities
August 17: Duke GME DEI ‘First Look’. The Duke Office of Graduate Medical Education is holding a virtual DEI ‘First Look’ event for potential incoming residents and fellows. It’s specifically designed for underrepresented applicants and any applicant interested in DEI issues. Registration is required.
August 17: Duke Health Annual Blood Drive. 9:30 a.m. to 3 p.m., Searle Conference Center, Seeley G. Mudd Building. Appointments required. Please sign up at http://www.redcrossblood.org using sponsor code: Duke.
September 12: Prostate Cancer & CVD Symposium. This is the third webinar of a four-part series. Collaboration between the International Cardio-Oncology Society & Duke Heart. Noon, Eastern. To learn more, please visit: https://duke.is/mbpte
September 25: Triangle Heart Walk. PNC Arena, Raleigh. Check-in starts at 11 am. Walk begins at Noon. Join us!
October 14: Cardio-Oncology in the Era of Precision Medicine. Symposium to be held at the J.B. Duke Hotel, Durham, NC. Registration is open: https://bit.ly/CardioOnc22. Email Beth Tanner with questions: beth.tanner@duke.edu.
November 4: 14th Annual NC Research Triangle Pulmonary Hypertension Symposium. 7 a.m.-4 p.m. Save the date! This will be an in-person event at the Durham Convention Center. Registration required, but is not yet live. Stay tuned for updates.
Cardiology Grand Rounds
Cardiology Grand Rounds has concluded and will resume in September.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
July 25 — Jennifer Green (Endocrinology)
HCPLive.com
Advancing Insulin Care in Diabetes: Tech and Tips
https://duke.is/wrz2y
July 29 — Adrian Hernandez
Triangle Business Journal
How consolidation is shifting power in Triangle’s robust CRO industry
https://duke.is/gfep2
July 29 — Craig Albanese
Spectrum News
Hospital COO says recent patient attack on staff example of troubling national trend
https://duke.is/bvpct
*A version of this story appeared in 30+ news outlets
July 30 — Craig Albanese
WRAL.com
https://duke.is/cazss
July 30 — Pamela Douglas
AJMC.com
Duke’s Douglas Highlights Need for Respect in Promoting Diversity, Health Equity
https://duke.is/nct25
August 1 — Shahzeb Khan
HCPLive.com
Heart Failure–Related Mortality in Young Adults Saw Rapid Increase Since 2012
https://duke.is/wx2d3
August 1 — Pamela Douglas
Healio/Cardiology
‘Professionalism’ is first step beyond the ABCs of preventive cardiology
https://duke.is/jwcy7
August 2 — Harry Severance
Medium/Duke University Opinion and Analysis
US Healthcare System is a House of Cards; Could it Collapse?
https://duke.is/2kc8k
August 2 — Adrian Hernandez
CBS17.com
Duke research center put in charge of coordinating data from long COVID studies
https://duke.is/y5egu
August 3 — Shahzeb Khan
tctMD
HF Deaths on the Rise in Young Adults, US Data Show
https://duke.is/6kzu6
August 4 — Robert Lefkowitz
GQ India
5 golden rules to be successful, according to the Nobel Prize winners
https://duke.is/pq2kb
August 5 — Marat Fudim
Medpage Today
No Worsening Cardiac Dysfunction in Long COVID
https://duke.is/zs259
Duke Heart Pulse – July 31st 2022
Highlights of the week:
Beckerman Joins Division of Cardiovascular & Thoracic Surgery Faculty

We are pleased to welcome Ziv Beckerman, MD, congenital and aortic surgeon, to the Duke faculty in the division of cardiovascular and thoracic surgery of the Department of Surgery. He will serve as a vital member of the pediatric heart surgery team along with Drs. Joe Turek and Nick Andersen. His position was effective July 1. Beckerman joins the team after having served as the surgical director of the Adult Congenital Heart Disease Program at the Texas Center for Pediatric and Congenital Heart Disease at Dell Children’s Medical Center in Austin.
Beckerman, who was born in Israel, says he had always known he wanted to work in the field of medicine, but had been unsure in what capacity. After turning 18, he was required to serve in the Israeli Defense Force and spent three years as a medic assigned to a combat unit. It was during this time tending to a variety of injuries and trauma, that he realized caring for patients was a passion and that he wanted to do it for the rest of his life. Upon completion of his military service to Israel, he started medical school in Hungary at the Medical University of Debrecen. Beckerman went on to complete residency in cardiac surgery at the Ruth and Bruce Rappaport Faculty of Medicine at Technion Israel Institute of Technology in Haifa. He then completed fellowships in Congenital Heart at Sheba Medical Center (Israel); Congenital Heart at Baylor College of Medicine, and in Advanced Aortic Surgery at Emory.
Once he began medical school, Beckerman says he knew from the get-go that he wanted to be a heart surgeon.
“Nothing in the body can function well without a well-functioning heart,” says Beckerman. “It is the most amazing organ and the source of life. Unfortunately, I had a few friends who died because of injuries to their chest and hearts. As I began my training, it was clear to me that this was where I’d place my focus.
“I have always, always felt that if you want to do something and really understand it, you should do it from the very beginning,” he added. “This is why I trained to care for the youngest patients – babies with congenital heart defects and even those still in the womb. If you’re able to take care of problems early enough – perhaps even before they start, then you’re on the way to success.”
Beckerman trained in congenital heart surgery and has dedicated his career to that, but he also decided to take a somewhat unusual path by completing advanced training in aortic surgery. It made great sense to do this, he says, because of the population of adults with congenital heart problems.
In the United States, Beckerman says, there are two types of congenital patients. They are either pediatric congenital patients who were born with identifiable heart defects or they are adult congenital patients. Of the adults, they are either people who were identified and treated as children or they are patients who were never diagnosed in childhood and they are now symptomatic adults. Either way, he says, these patients have complex needs.
Interestingly, there are actually more adults in the U.S. with congenital heart defects than there are kids, adds Beckerman. He says this population is comprised of well over two million people.
“When I thought about this patient subset and the problems they would have – many of them have aortic problems such as issues with dilation or problems with the aortic valve. Most of these adult patients end up as very, very complex surgical candidates,” he says. “So it made a lot of sense to me to train in aortic surgery. I think having this skill set that allows me to care for patients from fetal life all the way to adulthood is special in what it allows me to do, and it is something I feel very passionate about.”
He says that Duke offers an excellent space in which to care for patients. An issue the medical community experiences with congenital patients is “people falling through the cracks” during the transition from childhood to adulthood.
“We frequently lose patients during this transition into adulthood. They’re young adults, they feel strong and healthy, and decide to move away for college or a new job. Unless you have taken very good care to educate this young patient and help them understand their medical history and condition, the importance of keeping follow-ups with their current care team or establishing a relationship with a new care team in their new community, they can put themselves at risk by not getting regular monitoring. If they then resurface when something bad happens or their heart starts to fail, it can be too late.”
As Duke cares for both pediatric and adult patients under the same roof, it allows continuity of care and a unique opportunity to improve education and transition of care for congenital patients.
“One of the biggest advantages that Duke has over many other centers is the structure and the opportunity to maintain the care of the patients throughout their entire life,” says Beckerman. “Duke offers a truly world-class adult heart center and an excellent pediatric center that is one of the best in the country. Coming here offers the perfect opportunity to truly provide patients with the care they need. This is an extraordinary opportunity for me.”
Ziv and his wife, Anett, have two sons: Ben (13) and Ron (12). He says they are enjoying Durham and exploring the area. He said the community members they are meeting are kind and helpful, that their new neighbors are wonderful and welcoming. The family enjoys hiking, fishing, and sports – his sons especially enjoy soccer. He and Anett both enjoy cooking and are somewhat competitive about who is the better chef. They are very happy with their move and are looking forward to meeting more people.
“One of the things I really love about being here is the medical community,” Beckerman adds. “From a physician perspective, this offers me a terrific opportunity to do something meaningful. It is also the kind of community where we can really make an impact. We love being part of the community we live in and really getting to know people. I believe this will allow me to provide a more personalized level of care to my patients and allow me to feel closer to the community overall. We are really glad to be here.”
Please join us in offering Ziv a warm welcome when you see him!
Old-School Health Assessment Beats Genetic Test for Predicting Heart Disease
A genetic risk for heart disease is far less predictive of problems than actual lifestyle risk factors such as high blood pressure, high cholesterol and diabetes — even among younger adults.
high blood pressure, high cholesterol and diabetes — even among younger adults.
In a finding published July 26 in the journal Circulation, researchers led by a team at Duke AI Health found that genetic tests do little to accurately identify cardiovascular risks compared to a simple risk equation that uses basic health measures.
“It’s important to intervene early to prevent cardiovascular disease from progressing,” said senior author Michael Pencina, PhD, vice dean for data science at Duke University School of Medicine and director of Duke AI Health, which develops, evaluates and implements artificial intelligence initiatives at Duke Health and elsewhere.
“A lot of young people can be given a false sense of security if it looks like they have a low risk of inherited disease from their family,” Pencina said. “But in the nature vs. nurture battle, it’s nurture that is the stronger factor for cardiovascular disease: how a person lives throughout adulthood is a much bigger factor in the course of this disease.”
Pencina and colleagues analyzed two large databases — the Framingham Offspring Study and the Atherosclerosis Risk in Communities study — and stratified participants into three groups by age: Younger adults (median 30 years old); early mid-life (median 43 years old); and late mid-life (median 52 years old).
They applied two predictive models. The first, called a polygenic risk score, calculates the number of inherited genetic variants that are likely to put a person at risk of developing cardiovascular disease.
The second was a scoring model that uses traditional long-term risk factors — including high blood pressure, smoking, diabetes and high cholesterol levels — which are largely preventable depending on lifestyle choices.
In their analysis, the researchers found that the polygenic risk score provided limited predictive accuracy for cardiovascular disease risk compared to the traditional health assessment. Even when a genetic score was added in as a factor among the traditional health measurements, it made little difference.
“What we find is consistent in all three age groups, even in the youngest, the risk factor-based model was superior to the genetics-based model for predicting cardiovascular disease,” Pencina said.
“While genetic tests use new technology, they can be high-priced,” Pencina said. “People should instead visit their doctor and have their actual, clinical factors measured, because this will do a much better job of determining their state of health. And for those who have a high risk of developing cardiovascular disease — especially young people — they should eat healthy foods, exercise and begin proper medications as warranted.”
In addition to Pencina, study authors include Sadiya S. Khan, Courtney Page, Daniel M. Wojdyla, Yosef Y. Schwartz, and Philip Greenland. The study received funding from the National Institutes of Health (P30AG059988, RO1HL159250, U01HL160279, 5R01-EB025020-03).
Douglas Awarded Honorary Fellowship by ASPC
 Pamela S. Douglas, MD, the Ursula Geller Distinguished Professor for Research in Cardiovascular Disease, was awarded with an honorary fellowship by the American Society of Preventative Cardiology on Friday, July 29 during the 2022 ASPC Congress on CVD Prevention. The event is being held at the Omni Louisville Hotel from July 29-31 in Louisville, KY.
Pamela S. Douglas, MD, the Ursula Geller Distinguished Professor for Research in Cardiovascular Disease, was awarded with an honorary fellowship by the American Society of Preventative Cardiology on Friday, July 29 during the 2022 ASPC Congress on CVD Prevention. The event is being held at the Omni Louisville Hotel from July 29-31 in Louisville, KY.
“Each year the ASPC identifies someone who has made extraordinary contributions to the field of preventive cardiology through groundbreaking research, exemplary clinical care or excellence in education. Rarely, we find someone who meets all three of these aspects, but in Dr. Pam Douglas, we have,” said Martha Gulati, MD, director of preventive cardiology at Cedars-Sinai Medical Center’s Smidt Heart Institute and president of the ASPC. “Dr. Douglas has led several landmark clinical trials that have changed the workup and management of patients being evaluated for ischemia. She also has helped establish important specialty areas, including heart disease in women, sports cardiology and cardio-oncology. She has also been an outspoken advocate for women in cardiology, in addition to pushing all our cardiology societies to achieve equity and diversity in our ranks of cardiology. She has led the DEI task force for the American College of Cardiology, but this has had a trickle-down effect on all of our cardiology societies. I had the honor of working with her on a landmark paper — published this year in JACC — about what women in cardiology who bear children experience when they are pregnant and how it affects their careers. We outlined actionable solutions to improve the inclusion and advancement of  child-bearing persons in the field of cardiology. This is but one example of her numerous papers that are pushing to make our field welcoming to everyone.
child-bearing persons in the field of cardiology. This is but one example of her numerous papers that are pushing to make our field welcoming to everyone.
“Additionally, she has been a role model and mentor to so many, myself included. She pushes for what is right, she counsels us when we are lost (this she personally did for me in the past year), and she cares about everyone’s success — certainly at Duke Cardiology, but actually beyond Duke’s borders. We are excited to celebrate Dr. Douglas as our 2022 Honorary FASPC.”
Congratulations, Pam!
Krasuski Named Editor-in-Chief Elect of PHA’s Journal
 Richard Krasuski, MD, professor of medicine in cardiology, has been named Editor-in-Chief elect of the journal Advances in Pulmonary Hypertension (APH). The position is effective as of July 25. His term as Editor-in-Chief will begin next July and run through June 2025.
Richard Krasuski, MD, professor of medicine in cardiology, has been named Editor-in-Chief elect of the journal Advances in Pulmonary Hypertension (APH). The position is effective as of July 25. His term as Editor-in-Chief will begin next July and run through June 2025.
Krasuski has served on the editorial board of APH for the past four years.
Congratulations, Rich!
Legath to Serve as Nurse Manager DUH 7300, Effective September 1st
Duke Heart is pleased to announce that Jessie Legath, BSN, RN, PCCN, CNIV will become Nurse  Manager Operations for Duke University Hospital’s Cardiology Stepdown Unit 7300 effective September 1st. Jessie will co-manage 7300 with Monica Harper until Monica retires in December. Jessie earned a Bachelor of Science in Nursing from Duke University School of Nursing in 2015. She joined the Duke Heart Team as a new graduate nurse on 3100 in March 2016 and has served as Clinical Lead, now Assistant Nurse Manager, since September 2020.
Manager Operations for Duke University Hospital’s Cardiology Stepdown Unit 7300 effective September 1st. Jessie will co-manage 7300 with Monica Harper until Monica retires in December. Jessie earned a Bachelor of Science in Nursing from Duke University School of Nursing in 2015. She joined the Duke Heart Team as a new graduate nurse on 3100 in March 2016 and has served as Clinical Lead, now Assistant Nurse Manager, since September 2020.
During her time at Duke, Jessie advanced on the clinical ladder by becoming a CNIV and has held a variety of roles on 3100 including Preceptor, Charge Nurse, and Skin Care Champion. As Clinical Lead/Assistant Nurse Manager, she has been heavily involved with safety and quality initiatives including pressure injury prevention and assisting with the creation and implementation of the Heart Center SD Pressure Injury Prevention Bundle. She has been part of many team building and leadership activities throughout the Heart Center, including Heart Center chart navigator for Division of Health Service Regulation (DHSR) visits, organizing and leading monthly CTSD leadership meetings, and currently serves as one of the DUH Heart Core Class presenters.
Please join us in congratulating and welcoming Jessie to her new role.
Temporary Cath Lab Space Opens
Congratulations to the Cardiac Catheterization team on the opening this week of their newest (albeit temporary) lab space in Duke University Hospital. “Cath 4” is located in the area that was vacated by the pediatric team earlier this year. Leadership repurposed the space to support select procedures in order to enhance through-put and operations as we accommodate construction and growth in the DUH adult cardiac catheterization and electrophysiology labs.
The cath team performed their first case in the temporary space on Thursday, July 28. With the help of Duke Heart administrators, nursing and physician leadership, the cath lab super users (Jake Chastain, Adam Edmundson, Ashely Kinney and Miranda Olson), Drs. Larry Crawford and Caitlyn Drescher performed a successful RHC!!
To commemorate the event and to offer homage to Schuyler Jones (who was not in the lab this week), the team crafted this verse:
A cath lab haiku:
The volume was high
The lab space was so low
We opened Cath 4!

Shown here (L-R) are: Larry Crawford, Anna Mall, Miranda Olson, Caitlin Drescher, Jake Chastain, Ashley Kinney and Adam Edmundson


Shown L-R are: Jake Chastain, Larry Crawford and Caitlin Drescher

A big shout-out to Anna Mall and Joe Kelly who were instrumental in getting the room up and running, and many thanks to the entire team for their support. Cheers to our many cases to come!
WiC Event Held
The Duke program for Women in Cardiology met this week at the home of Pam Douglas. All attendees benefited from a great group discussion on mentorship and sponsorship with faculty members Karen Alexander, Anna Lisa Chamis, Pam Douglas, Camille Frazier Mills, Neha Pagidipati, Jennifer Rymer, and Tracy Wang. Thank you to Pam Douglas for hosting and to Joey Harrington, Ali Corley and Paula Rambarat for organizing and participating in this insightful discussion!

Photos of the Week
A belated congratulations to John and Karen Alexander on their daughter Emily‘s entry to medical school. Members of Dr. John Alexander’s clinical team are excited to see her pursuing a career in medicine! When his team members saw recent photos they couldn’t help but notice the stark contrast between Emily’s fresh white coat and John’s less-than-pristine one.
We are told the team has wondered if a ‘GoFundMe‘ campaign is needed to get a replacement. “That coat,” they said, “should probably go already.”

Karen, Emily, and John Alexander, July 2022

John, holding a much younger Emily, and Karen Alexander along with faculty and fellows of the division of cardiology circa 1997. For those that look carefully – you will also see some other notable Duke Cardiology Alums

John Alexander & the coat
Photos submitted by Sasmrita Belbase, cardiology APP.
In all seriousness, congratulations to Emily — we are thrilled for her and look forward to all she will accomplish!
ICYMI: USNWR ‘Best Hospitals’ Ratings Released for 2022-2023
Tom Owens, MD, president of Duke University Hospital commented:
Duke University Hospital is privileged to serve all of our patients and communities, and one of my favorite things is to read the many grateful patient comments and notes we receive every day, thanks to your excellent, compassionate care.
It also is gratifying to receive recognition from outside organizations. We are pleased that Duke University Hospital again has been recognized among the best hospitals in the country in the U.S. News & World Report rankings for 2022-2023. We have improved overall from 24 to 21 in the national ranking, and we remain No. 1 in North Carolina.
We also have been nationally ranked in 11 adult specialties, we saw improvement in most of the specialty groups, and we received the highest rating for 19 of 20 common procedures and conditions.
Congratulations to each of our specialties for these outstanding designations, with national rankings from USNWR as follows:
- Cancer – Ranked 22
- Cardiology & Heart Surgery – Ranked 34
- Ear, Nose & Throat – Ranked 29
- Gastroenterology & GI Surgery – Ranked 29
- Geriatrics – Ranked 30
- Obstetrics & Gynecology – Ranked 33
- Neurology & Neurosurgery – Ranked 23
- Ophthalmology – Ranked 6
- Orthopedics – Ranked 19
- Pulmonology – Ranked 31
- Urology – Ranked 26
In addition, our hospital is recognized this year as high performing in two adult specialties (endocrine and rheumatology), as well as in 19 procedures and conditions:
- Abdominal aortic aneurysm
- Aortic valve stenosis
- Coronary artery bypass grafting
- Colon Cancer Surgery
- Congestive Heart Failure
- Chronic Obstructive Pulmonary Disease (COPD)
- Hip replacement
- Knee replacement
- Lung cancer surgery
- Transcatheter Aortic Valve Replacement (TAVR)
- Heart attack
- Stroke
- Pneumonia
- Diabetes
- Kidney failure
- Hip fracture
- Back surgery (spinal fusion)
- Ovarian cancer surgery
- Prostate cancer surgery
Although pleased with the improving USNWR recognition and rankings, we know that the quality of the care we deliver is not defined by a single ranking system. We continue to deliver outstanding care to some of the country’s most vulnerable patients and diverse communities, which is may not always be reflected in the USNWR models.
This can be especially seen at times with regards to the Cardiology and Heart Surgery care – where our performance on care in our quality and national registries is substantially better than some of the claim’s data based measure. Nevertheless, we continue to work on our processes to improve and capture the care we deliver in addition to working on ways to innovate and improve patient outcomes. We have seen some of the recent changes due to these efforts and will anticipate continuing to see those in upcoming years. Additionally, these efforts are often recognized in other measures some of which are provided below.
- Newsweek ranking of the World’s Best specialized hospitals for heart care (July 2022)
- https://www.newsweek.com/worlds-best-specialized-hospitals-2022, Duke University Hospital – Division of Cardiology ranked 13th
- STS 3 Star ratings for CT surgery
- “A” distinction from The Leapfrog Group for upholding patient safety
- Achieving an Overall Hospital Quality Star Rating of 4 Stars from the Centers for Medicare and Medicaid (CMS)
- Maintaining the 1 ranking of our Children’s Hospital in North Carolina
- Achieving Healthcare Equality Index Leader 2022 from the Human Rights Campaign
COVID-19 Update
Please continue to practice safe COVID-19 protocols in your day-to-day interactions with others. Be particularly vigilant about masking, and avoid eating indoors in group settings. The health of our team members and our patients remains a priority as we continue to monitor the COVID-19 trends throughout our community.
Stay home if you are not feeling well. Employees who begin to experience any COVID-19 symptoms should report symptoms through the Duke SymMon app, which is available in both the Apple and Google app stores.
Donate blood if you’re able to. Click here for Duke-sponsored blood drives through the Red Cross.
All the latest Clinical Operations updates related to COVID can be found at https://covid-19.dukehealth.org. Patient-facing resources on DukeHealth.org can be found here: https://www.dukehealth.org/covid-19-update/resources. Duke University maintains a resource page as well, which can be accessed here: https://coronavirus.duke.edu/updates/for-staff.
Upcoming Events & Opportunities
August 17: Duke GME DEI ‘First Look’. The Duke Office of Graduate Medical Education is holding a virtual DEI ‘First Look’ event for potential incoming residents and fellows. It’s specifically designed for underrepresented applicants and any applicant interested in DEI issues. Registration is required.
September 25: Triangle Heart Walk. PNC Arena, Raleigh. Check-in starts at 11 am. Walk begins at Noon. Join us!
October 14: Cardio-Oncology in the Era of Precision Medicine. Symposium to be held at the J.B. Duke Hotel, Durham, NC. Registration is open: https://bit.ly/CardioOnc22. Email Beth Tanner with questions: beth.tanner@duke.edu.
Cardiology Grand Rounds
Cardiology Grand Rounds has concluded and will resume in September.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
July 23 — Stephen Greene
Practical Cardiology
Don’t Miss a Beat: Understanding GFR Slope, with Brendon Neuen, MBBS, MSc
https://duke.is/5zn99
July 26 — Richard Shannon
The News Courier
How the Dobbs decision affects women and children
https://duke.is/4nw5f
July 26 — Duke University Hospital, Duke Regional Hospital
CBS17.com
The Triangle is home to 5 of NC’s top 10 hospitals, says US News & World Report
https://duke.is/92n74
July 27 — Michael Pencina
CLPmag.com
Traditional Health Assessment Beats Genetic Test for Heart Disease Prediction, Study Shows
https://duke.is/b7v66
July 27 — Duke University Health System
Becker’s Hospital Review
https://duke.is/zqnyt
July 27 — Sujay Kansagra (Pediatrics)
CBS17.com
Study finds frequent naps linked to high blood pressure, stroke
https://duke.is/mr69s
July 27 — Duke University Hospital and Duke Regional Hospital
Newsobserver.com
Where Triangle hospitals land in new US News & World rankings
https://duke.is/88s53
July 28 — Shahzeb Khan
HealthDay*
More Young Americans Are Dying of Heart Failure
https://duke.is/rnvvu
*carried by additional 196 news outlets
July 28 — Julie Doberne
Medscape
World’s First HIV+ to HIV+ Heart Transplant Performed
https://duke.is/69wea
Duke Heart Pulse – July 24th 2022
Highlights of the week:
DBAP Outing with the Cardiology Fellows
Our newest cardiology fellows got a taste of downtown Durham with an outing on Saturday night to see our Triple-A affiliate, the Durham Bulls, at Durham Bulls Athletic Park. The Bulls played the Norfolk Tides and picked up a 9-8 win in game two of their three game set. Game three is this afternoon. We believe our Duke Heart attendance at the game really gave the Bulls an edge – thanks to all who joined us!
Although it was warm out – the right field picnic area provided a great place to have the families watch the game with some shade, food and drinks. Thanks to Anna Lisa and the fellowship team for helping set up this fun event.



Fudim Presents MGR
On Friday, July 22 Marat Fudim, assistant professor of medicine in cardiology, led a very informative Medicine Grand Rounds on pressure and volume management in patients with chronic heart failure. His presentation covered how volume is distributed throughout the body, the contribution of vasoconstriction to increased intra-cardiac pressures, and several new treatment avenues for patients. In case you missed it, you can view the full recording here: https://warpwire.duke.edu/w/e_MGAA/
pressure and volume management in patients with chronic heart failure. His presentation covered how volume is distributed throughout the body, the contribution of vasoconstriction to increased intra-cardiac pressures, and several new treatment avenues for patients. In case you missed it, you can view the full recording here: https://warpwire.duke.edu/w/e_MGAA/
This work has opened up many more interesting physiologic studies, devices, and work that Marat and team are helping Duke take the lead on nationally.
Great job, Marat!
Nurse Scientists in Academic-Practice Partnership Improve Rigor of Nursing Science
Asking the right clinical questions is second nature for a nurse, but asking clinical questions in ways that are amenable to scientific solutions is a critical skill that takes time, expertise and mentorship to develop. Faculty at Duke University School of Nursing and Duke University Health System (DUHS) are partnering to help clinical inquiry flourish through collaboration between bedside nurses and nurse scientists. Fruits of the partnership are leading to improved rigor in research and quality improvement design that, in turn, help to improve outcomes for patients and families.
Bradi Granger, MSN, PhD, RN, a professor and director of Duke Heart Center Nursing Research Program, Staci Reynolds, PhD, RN, associate professor and clinical nurse specialist at Duke University Hospital (DUH), and Anna Mall, MSN, RN, assistant nurse manager for the adult cardiac catheterization labs at DUH, recently co-authored an article on clinical inquiry in the American Association of Critical-Care Nurses (AACN) Advanced Critical Care Summer 2022 journal.

Their work is one of many projects and activities that are an outcome of the Duke Advancement of Nursing, Center of Excellence (DANCE), an academic practice partnership between nurses in the School of Nursing and DUHS, which leverages the experience, knowledge, and aspirations of nurses across both entities.
In an example of the relationships DANCE fosters, Granger immediately thought of Reynolds and Mall when a question came up at a national conference: How can any small-scale, single-site study be valuable to growing and expanding nursing science?
The authors answered that question by creating a pyramid structure outlining a step-by-step approach to clinical inquiry that results in generalizable data that can impact the national or even global health care research priorities for improving health and patient care.
“There is, at the end of the day, a randomized trial that can contribute causal evidence to a patient problem and provide data to change practice and leverage policy,” Granger said.
Mall says that she and her team noticed that patients consistently experience discomfort in response to catheter insertion, despite the administration of pre-procedural pain medicine.
“My whole question was, why are we giving this medication? Is it doing what we need it to do? Can we do it a different way,” she said.
The first step of the pyramid examined current research and recommendations in the literature about what to do when there was breakthrough pain during the procedure. The next step was designing a study to analyze existing cath lab data for clues to the precursors of pain during the procedure. The next step was designing and conducting the randomized trial that compared two pre-procedural sedation intervals. The last step was taking the results of that trial and building further questions based on focus groups with the nurses and the patients, expanding the inquiry to include additional studies, each addressing the patient experience from different angles.
Reynolds’s study focused on central line-associated bloodstream infections, or CLABSIs. Because the infections are costly to treat and create a longer, and possibly more complicated recovery for patients, Reynolds was interested in how to mitigate the rate of infections. Protocol calls for chlorohexidine gluconate (CHG) bathing, but Reynolds found that there was low compliance by nurses across the U.S., partly because patients didn’t like the baths, which some find uncomfortable or because they dislike the smell.
Reynolds partnered with Granger, who had connections with Wake Med, and conducted a collaborative study that found that, with greater compliance and procedural understanding, the rate of infection decreased. But they took results of the study a step further to talk to patients and nurses about their experiences.
“There were just a lot of little one-offs from that larger study that we were able to do to keep the ball rolling and answer further clinical inquiry questions as they came up,” she said, noting that having a randomized trial as the primary source was critical. “It’s not until you get to talking to the bedside nurses and patients that you get into the nitty gritty details of maybe why the intervention of CHG bathing treatments, as recommended in the evidence-based CDC guideline, isn’t working so well [in real world clinical practice].”
Implementing the pyramid approach to clinical inquiry requires the type of collaboration DANCE offers.
“The whole premise of DANCE as an academic health system partnership is to bring academicians on the school side, who are experts in the science and design of clinical inquiry, together with the health system nurses to support health system science,” Granger said. “Clinical inquiry, when it’s done well, requires a rigorous scientific design so that the study can effectively inform practice.”
Mall agrees that the questions can often come from clinical nurses, but they need the support and structure that a nurse scientist offers.
“I think what’s very unique in the partnership with DANCE is we have those relationships established,” she said. “It makes that nurse scientist accessible to the bedside nurse.”
Mall said her experience collaborating with the nurse scientists has improved her leadership skills by allowing her time to help with the design study, data collecting, team-building and number-crunching that she would not have been able to do otherwise.
Granger is interested in ensuring that more health systems, including those without academic-practice partnerships like DANCE, have opportunities for collaboration with nurse scientists.
“That’s one thing we’re working on at Duke through DANCE, to make the resources of a nurse scientist more accessible for our smaller community hospitals, and also around the country, to share this model we’re using at Duke,” she said.
The co-authors’ work helps to demonstrate how nurse scientists and researchers have a key role in advancing nurses’ leadership skills, autonomy, and decision-making skills, in turn, improving professional practice environments and health outcomes for real people, families and communities.
Great Catch, Nelson!
We were excited to learn this week that our Duke Heart cath lab team member Eric Nelson, CVIS, received a ‘Great Catch!‘ award.
Eric quickly spoke up to prevent the premature removal of an arterial introducer sheath in an anticoagulated patient in the Cardiac Catheterization Lab at Duke University Hospital. His timely action helped ensure that the introducer remained in place until the patient’s clotting time returned to a safe level, which minimized the risk of bleeding after sheath removal.
Excellent job, Eric! Congrats!!

COVID-19 Update
Please continue to practice safe COVID-19 protocols in your day-to-day interactions with others. Be particularly vigilant about masking, and avoid eating indoors in group settings. The health of our team members and our patients remains a priority as we continue to monitor the COVID-19 trends throughout our community.
Stay home if you are not feeling well. Employees who begin to experience any COVID-19 symptoms should report symptoms through the Duke SymMon app, which is available in both the Apple and Google app stores.
Donate blood if you’re able to. Click here for Duke-sponsored blood drives through the Red Cross.
All the latest Clinical Operations updates related to COVID can be found at https://covid-19.dukehealth.org. Patient-facing resources on DukeHealth.org can be found here: https://www.dukehealth.org/covid-19-update/resources. Duke University maintains a resource page as well, which can be accessed here: https://coronavirus.duke.edu/updates/for-staff.
Upcoming Events & Opportunities
July 25: Women in Cardiology. 6:30 p.m. Dinner and discussion on mentorship and sponsorship. For more information and location, please contact cardiology fellow Karen Flores Rosario, MD.
August 17: Duke GME DEI ‘First Look’. The Duke Office of Graduate Medical Education is holding a virtual DEI ‘First Look’ event for potential incoming residents and fellows. It’s specifically designed for underrepresented applicants and any applicant interested in DEI issues. Registration is required.
October 14: Cardio-Oncology in the Era of Precision Medicine. Symposium to be held at the J.B. Duke Hotel, Durham, NC. Registration is open: https://bit.ly/CardioOnc22. Email Beth Tanner with questions: beth.tanner@duke.edu.
Cardiology Grand Rounds
Cardiology Grand Rounds has concluded and will resume in September.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
July 15 — Robert Mentz
tctMD
US Dobutamine Shortage a ‘Huge Problem’—What’s the Solution?
https://duke.is/2vwsb
July 15 — Andrew Wang
Cardiology Today
‘Patients feel better’: New hope for obstructive hypertrophic cardiomyopathy
https://duke.is/gpnd7
July 18 — Robert Lefkowitz
GQ.com (Mexico)
Las reglas de oro para ser exitoso, según los ganadores del Nobel
https://duke.is/vxvcw
July 19 — John Haney and Matthew Hartwig
Yahoo.com*
Paragonix Expands Research for Advanced Organ Preservation Clinical Registries
https://duke.is/zku4a
*this story was also carried in Baltimore, Pittsburgh & Sacramento
July 19 — Mihai Podgoreanu and Negmeldeen Mamoun
Medpage Today
Fluid Therapy Showdown in Cardiac Surgery Disfavors Albumin
https://duke.is/m2k87
July 20 — Stuart Russell
Medscape
Pig Heart Transplants and the Ethical Challenges That Lie Ahead
https://duke.is/ysnaf
July 21 — Sreekanth Vemulapalli
WPTF (Raleigh-Durham-Fayetteville)
https://duke.is/2yknw
July 21 — Jason Katz
CardioNerds
Early Struggles, Notable Changes, and Ongoing Challenges in Cardiac Critical Care
https://duke.is/g9w6a
Division of Cardiology Publications Indexed in PubMed July 14-20, 2022
Al Rifai M, Newby LK, Nair AP, Misra A, Rogers JG, Fedson S, Virani SS. SGLT-2 Inhibitors for Patients with Heart Failure: What Have We Learned Recently? Curr Atheroscler Rep 2022;24(8):627-634. PM: 35653033.
Araújo TP, Borges LGS, Barroso WKS, Brandão AA, Barbosa ECD, Feitosa ADM, Malachias MVB, Mota Gomes M, Amodeo C, Povoa RMDS, Jardim PCBV, Lopes RD, Batista SRR, Vitorino PVO. Factors associated with uncontrolled blood pressure in hypertensive Brazilians. J Clin Hypertens (Greenwich) 2022;24(7):814-824. PM: 35770852.
Bahit MC, Vora AN, Li Z, Wojdyla DM, Thomas L, Goodman SG, Aronson R, Jordan JD, Kolls BJ, Dombrowski KE, Vinereanu D, Halvorsen S, Berwanger O, Windecker S, Mehran R, Granger CB, Alexander JH, Lopes RD. Apixaban or Warfarin and Aspirin or Placebo After Acute Coronary Syndrome or Percutaneous Coronary Intervention in Patients With Atrial Fibrillation and Prior Stroke: A Post Hoc Analysis From the AUGUSTUS Trial. JAMA Cardiol 2022;7(7):682-689. PM: 35612866.
Bikdeli B, Zahedi Tajrishi F, Sadeghipour P, Talasaz AH, Fanikos J, Lippi G, Siegal DM, Eikelboom JW, Monreal M, Jimenez D, Connors JM, Ageno W, Barnes GD, Piazza G, Angiolillo DJ, Parikh SA, Kirtane AJ, Lopes RD, Bhatt DL, Weitz JI, Mehran R, Krumholz HM. Efficacy and Safety Considerations With Dose-Reduced Direct Oral Anticoagulants: A Review. JAMA Cardiol 2022;7(7):747-759. PM: 35648414.
Chatterjee R, Kwee LC, Pagidipati N, Koweek LH, Mettu PS, Haddad F, Maron DJ, Rodriguez F, Mega JL, Hernandez A, Mahaffey K, Palaniappan L, Shah SH. Multi-dimensional characterization of prediabetes in the Project Baseline Health Study. Cardiovasc Diabetol 2022;21(1):134. PM: 35850765.
Collins KA, Ross LM, Slentz CA, Huffman KM, Kraus WE. Differential Effects of Amount, Intensity, and Mode of Exercise Training on Insulin Sensitivity and Glucose Homeostasis: A Narrative Review. Sports Med Open 2022;8(1):90. PM: 35834023.
Defilippis EM, Truby LK, Clerkin KJ, Donald E, Sinnenberg L, Varshney AS, Cogswell R, Kittleson MM, Haythe JH, Givertz MM, Hsich EM, Agarwal R, Topkara VK, Farr M. Increased Opportunities for Transplantation for Women in the New Heart Allocation System. J Card Fail 2022;28(7):1149-1157. PM: 35470056.
Gaudino M, Audisio K, Di Franco A, Alexander JH, Kurlansky P, Boening A, Chikwe J, Devereaux PJ, Diegeler A, Dimagli A, Flather M, Lamy A, Lawton JS, Tam DY, Reents W, Rahouma M, Girardi LN, Hare DL, Fremes SE, Benedetto U. Radial artery versus saphenous vein versus right internal thoracic artery for coronary artery bypass grafting. Eur J Cardiothorac Surg 2022;62(1):ezac345. PM: 35678560.
Giroux NS, Ding S, McClain MT, Burke TW, Petzold E, Chung HA, Rivera GO, Wang E, Xi R, Bose S, Rotstein T, Nicholson BP, Chen T, Henao R, Sempowski GD, Denny TN, De Ussel MI, Satterwhite LL, Ko ER, Ginsburg GS, Kraft BD, Tsalik EL, Shen X, Woods C. Differential chromatin accessibility in peripheral blood mononuclear cells underlies COVID-19 disease severity prior to seroconversion. Res Sq 2022;:rs.3.rs-1479864. PM: 35411343.
Greene SJ, Ezekowitz JA, Anstrom KJ, Demyanenko V, Givertz MM, Piña IL, O’Connor CM, Koglin J, Roessig L, Hernandez AF, Armstrong PW, Mentz RJ. Medical Therapy During Hospitalization for Heart Failure With Reduced Ejection Fraction: The VICTORIA Registry. J Card Fail 2022;28(7):1063-1077. PM: 35301107.
Jorbendaze A, Young R, Shaburishvili T, Demyanchuk V, Buriak R, Todurov B, Rudenko K, Zuber M, Stämpfli SF, Tanner FC, Erne P, Mirro M, Fudim M, Goldberg LR, Cleland JGF. Synchronized diaphragmatic stimulation for heart failure using the VisONE system: a first-in-patient study. ESC Heart Fail 2022;9(4):2207-2214. PM: 35619238.
Lala A, Mentz RJ. Fostering Belonging at JCF. J Card Fail 2022;28(7):1047. PM: 35840183.
Minhas AMK, Sagheer S, Ijaz SH, Nazir S, Khan MS, Zaidi SH, Fudim M, Rodriguez F, Johnson HM, Virani SS. Persistent Racial/Ethnic Disparities in Cardiology Trainees in the United States. J Am Coll Cardiol 2022;80(3):276-279. PM: 35835499.
Oslin DW, Lynch KG, Shih MC, Ingram EP, Wray LO, Chapman SR, Kranzler HR, Gelernter J, Pyne JM, Stone A, DuVall SL, Lehmann LS, Thase ME, , Aslam M, Batki SL, Bjork JM, Blow FC, Brenner LA, Chen P, Desai S, Dieperink EW, Fears SC, Fuller MA, Goodman CS. Effect of Pharmacogenomic Testing for Drug-Gene Interactions on Medication Selection and Remission of Symptoms in Major Depressive Disorder: The PRIME Care Randomized Clinical Trial. JAMA 2022;328(2):151-161. PM: 35819423.
Prabhakaran D, Singh K, Kondal D, Raspail L, Mohan B, Kato T, Sarrafzadegan N, Talukder SH, Akter S, Amin MR, Goma F, Gomez-Mesa J, Ntusi N, Inofomoh F, Deora S, Philippov E, Svarovskaya A, Konradi A, Puentes A, Ogah OS, Stanetic B, Issa A, Thienemann F. Cardiovascular Risk Factors and Clinical Outcomes among Patients Hospitalized with COVID-19: Findings from the World Heart Federation COVID-19 Study. Glob Heart 2022;17(1):40. PM: 35837356.
Prattipati S, Sakita FM, Tarimo TG, Kweka GL, Mlangi JJ, Maro AV, Coaxum LA, Galson SW, Limkakeng AT, Rugakingira A, Urasa SJ, Okeke NL, Mmbaga BT, Bloomfield GS, Hertz JT. Prevalence and Correlates of Ischemic ECG Findings among Adults With and Without HIV in Tanzania. Glob Heart 2022;17(1):38. PM: 35837355.
Rehorn MR, Daubert JP. Editorial commentary: Pulsed field catheter ablation in atrial fibrillation: The promising future of an old technology. Trends Cardiovasc Med 2022;32(6):388-389. PM: 34508849.
Salah HM, Fudim M, O’Neil ST, Manna A, Chute CG, Caughey MC. Post-recovery COVID-19 and incident heart failure in the National COVID Cohort Collaborative (N3C) study. Nat Commun 2022;13(1):4117. PM: 35840623.
Scirica BM, Im K, Murphy SA, Kuder JF, Rodriguez DA, Lopes RD, Green JB, Ruff CT, Sabatine MS. Re-adjudication of the Trial Evaluating Cardiovascular Outcomes with Sitagliptin (TECOS) with study-level meta-analysis of hospitalization for heart failure from cardiovascular outcomes trials with dipeptidyl peptidase-4 (DPP-4) inhibitors. Clin Cardiol 2022;45(7):794-801. PM: 35715946.
Recent Comments