Duke Heart Pulse – October 30th 2022
Updates of the week:
Chancellor Washington to Leave Leadership Roles June 30
Most of you have heard the news regarding Dr. Washington’s decision to step down from his roles at Duke University and Duke University Health System. In case you missed his formal message to the Duke Health team, which was issued on Wednesday, Oct. 26, we are reprinting it here.
Dear Colleagues,

Since April 2015, I have had the great honor and privilege to serve as your Chancellor for Health Affairs at Duke University and President and CEO of the Duke University Health System. Now in my eighth year, I have decided I will step down from these roles at the end of this academic year, June 30, 2023. A formal announcement about my decision and transition plans will be forthcoming from President Vincent Price today.
Serving with you in these leadership roles has unquestionably been the best professional experience I have enjoyed in my life. Words really cannot adequately convey the emotions I am feeling at this time as I share this decision with you. Suffice it to say that I am currently overwhelmed with a sense of heartfelt gratitude.
From that first spring in Durham when you so warmly welcomed Marie and me to the Duke community, all the way up to today, I have felt your unwavering support and been emboldened by it. Your tremendous talent, creativity, deep sense of caring, dedication, and can-do attitude have bolstered and empowered my leadership tenure. Together, we have indeed advanced health, as we have elevated our excellence and amplified Duke Health’s impact locally and globally. And, because of you, Duke Health is strongly positioned to continue thriving — innovating and leading in the decades ahead. I am very proud of our extraordinary accomplishments, and I am confident in a bright future for us all as we continue to distinguish Duke Health as a leader among the very top academic health systems in the world.
Most importantly, I want to thank you! Thank you for all you have given to me. Thank you for all you have given to each other, our patients and their loved ones, and our communities.
For those of you who are wondering why now, my decision is principally driven by my desire to devote more attention to my personal life. Last month, I turned 72 years-of-age. Young! Earlier this month, Marie and I celebrated 40 years of marriage, and we are thrilled about spending more time together. And as some of you know, we have a new granddaughter. I imagine that this personal renewal will be invigorating.
At the same time, I also believe that institutional renewal is good. In fact, in dynamic industries and organizations such as ours with rapid, dramatic change afoot, renewal is a constant imperative. We have an exceptionally strong team across Duke Health, and continued renewal at the top will only enhance the remarkable achievements and significant contributions we are already making.
Looking ahead over the next eight-plus months, please know that I am still all-in with you as we continue to advance Duke Health: Onward. Upward. Beyond. You can count on me to sprint right up to the hand-off of my leadership baton next June. My excitement and energy today are as high as when I arrived in April 2015.
With deep gratitude and admiration,
Eugene Washington, MD
Chancellor for Health Affairs, Duke University
President and CEO, Duke University Health System
Welcoming Newest Faculty Members
We are pleased to have a number of new faculty members on the Duke Heart team. Earlier this summer Zak Loring and Michelle Kelsey joined the faculty as assistant professors of medicine in cardiology after the completion of their fellowship training. Ziv Beckerman also joined our team in July as a faculty member in the division of cardiovascular and thoracic surgery. Since then, we’ve added four additional team members: Bharathi Upadhya, Senthil Selvaraj, Girish Kalra and Deepa Upadhyaya.
This week we’re highlighting Bharathi Upadhya.
Upadhya Joins Duke Heart Team

Bharathi Upadhya, MD, officially joined the Duke Heart team on Aug. 22 as associate professor of medicine in cardiology. She is the newest member of our adult congenital heart disease team and will see patients at Duke Cardiology Arringdon.
Upadhya says she is most excited about joining the Duke Heart team because of the professional growth and learning opportunities available here. With congenital heart disease patients living longer, the field of care is growing and offers great opportunity, especially at a large and varied program like Duke. She says she enjoys treating patients with challenging conditions such as chromosomal abnormalities and muscular dystrophy.
“These patients really need attentive care, which I enjoy providing,” said Upadhya. “Initially, this was not an area of interest for me, but when I learned more about the association of these chromosomal issues to cardiovascular defects, I became quite dedicated to this area. I am equally fascinated by the hemodynamics of congenital heart disease.”
She is particularly enthusiastic about working with and learning from Tom Bashore and Rich Krasuski, she says. “There is no end to learning and growing, no matter how old you get it should never stop.”
“I most enjoy the long-lasting relationships that can be built with patients, especially those with congenital heart disease,” she adds. “I typically become their primary care provider and I do everything I can for them. They come to feel like family or lifelong friends to me.”
Born in Karnataka, India, Upadhya earned her MBBS at Mysore Medical College followed by residency training at Vijaya Nagar Institute of Medical Science — both in India. In the U.S., she completed residency at Wake Forest University School of Medicine (WFUSOM), and a fellowship in cardiology at Penn State Hershey Medical Center.
“My father’s dream for me was to become a doctor. He really wanted me to help people and saw that I would be good at it,” Upadhya says. “I specifically chose cardiology due to our family history. My mom’s eldest sister died due to heart disease back in India. At that time, we didn’t have as much access to treatment options or support. I believe her death could have been prevented and this is what drove my interest toward cardiology.”
Her parents, she adds, are her greatest mentors. “All that I am is because of them,” says Upadhya. “When I came to the U.S. for fellowship, my mom and dad came here from India. My mom, who could not even speak English, came and stayed for two years just to help me. They have sacrificed greatly for me and I am so thankful to them.”
fellowship, my mom and dad came here from India. My mom, who could not even speak English, came and stayed for two years just to help me. They have sacrificed greatly for me and I am so thankful to them.”
Prior to coming to Duke, she was associate professor of medicine in cardiology at WFUSOM, where she joined the faculty in 2010. While at Wake Forest Baptist Health, she helped launch a congenital heart program in partnership with pediatric cardiologist Derek Williams, MD. She earned numerous awards for teaching excellence and was the Arnold P. Gold Foundation’s 2017 recipient of the Leonard Tow Humanism Award. She currently serves as an ad hoc reviewer for more than a dozen journals and is a member-at-large for the American Society of Echocardiography’s membership committee.
Upadhya is a clinical investigator with board certification in Cardiovascular Medicine, Echocardiography, Nuclear Cardiology, and Adult Congenital Heart Disease. Her research has spanned a wide range of topics in cardiovascular medicine including medical imaging-related projects and cardiac rehabilitation, heart failure with preserved ejection fraction, exercise physiology, and aging.
Bharathi’s husband, Sudarshan Upadhya, PhD, MBA, is co-founder of Aestas Pharma, Inc., based here in Durham. They have two children. Their son is a senior at Duke University, and their daughter is in the 6th grade. Outside of medicine, Bharathi has learned Bharatanatyam, a classical dance of India. She has a strong interest in music and is a trained vocalist of Hindustani classical music. She is currently learning a different form of classical Indian music with her daughter.
We are so pleased to have Bharathi on the Duke Heart team! Please give her a warm welcome, if you have not yet had the opportunity to do so.
Caregiving Conference Held Oct. 28
The Duke Caregiver Community Event was held Friday, Oct. 28 at the Sheraton Imperial Hotel in Durham. Nishant Shah, Laura Blue and Stephanie Barnes served as speakers for the event. Dakota Bentz and Henry Delgado Alvia were wellness clinic volunteers. There was a fantastic turnout with over 500 attendees.
Thanks to those from Duke Heart who participated!

CulturePulse 2022 is Coming This Week — Be Heard
All Duke Health team members will receive information about and a link to the 2022 CulturePulse survey on Wednesday, Nov. 2. The brief survey is confidential, mobile-friendly, and simple to complete. Questions will cover your sense of belonging, safety, and well-being, as well as the strength of your teams and management. The goal is to maintain what’s going well and adjust what could be better.
The survey link will remain open through Nov. 16; you can also find it via the QR code you’ll see on digital signage and printed flyers around Duke.
CulturePulse is a way for team members to share their feedback about what’s going well and what could be improved at Duke Health. Please participate and encourage your team members to do so as well. This is a great opportunity for all of us to have our voices heard.
NIH Data Management and Sharing Policy
The National Institutes of Health (NIH) will require all grants submitted on or after Jan. 25, 2023 to include a Data Management and Sharing Policy. As part of this policy, all new NIH funding mechanisms that produce research data will need to document a two page Data Management and Sharing Plan (DMSP), which will be considered a term and condition of the award. This plan needs to be submitted when applying for funding. Researchers should plan and budget for the management and sharing of data.
To assist faculty in the DOM in meeting this requirement, there will be a DOM Research Quality Town Hall, led by the Duke Office of Scientific Integrity, on Nov. 8, 2022 from 12-1 p.m.
The Town Hall will cover resources at Duke to help faculty meet this requirement. RCR200 credit will be given for those attending the full one-hour meeting. The meeting will be recorded for those unable to attend, but RCR credit is only available for those who attend the live meeting.
To attend this Town Hall and submit your questions regarding the NIH DMSP, please register at the following link: Town Hall on Data Management and Sharing Policy.
ICYMI: Anti-Ableist Advocacy: Lunsford Aims to Change the Conversation Around Disability
He didn’t always have an awareness of it or a word for it, but Christopher Lunsford, MD, was affected by ableism throughout his  life. It affected how he coped with the challenges that came with being hard of hearing since birth and having a speech impediment. It wasn’t always easy to make his way in a world that focuses mostly on the experiences of people who can hear and speak clearly.
life. It affected how he coped with the challenges that came with being hard of hearing since birth and having a speech impediment. It wasn’t always easy to make his way in a world that focuses mostly on the experiences of people who can hear and speak clearly.
Going on rounds during medical school proved especially difficult. The noisy nature of hospitals with multiple people speaking at once — sometimes in masks — made it extremely hard for Lunsford to know what his attending physicians, patients, and classmates were saying. He said he found himself working twice as hard just to keep up. He did ask for and receive accommodations, but it was a cumbersome process, and ultimately, the accommodations were not helpful. He simply chose to “grin and bear” it.
Now he realizes the pressure to minimize his issues was due to ableism. He also has come to understand that not only is it okay to ask for accommodation, but it’s also important to look at changing systems that lead to inequitable learning environments and patient care settings.
“Rounds is possibly the worst possible way for a person who is hard of hearing to learn,” said Lunsford, an assistant professor in the Department of Orthopaedic Surgery as well as the Department of Pediatrics. “The number one ‘coping skill’ that I was given was to minimize the challenge and to make it go away just by ignoring the negative impacts of it. I did not even process it as a systematic failure. At the time, I thought I should have never complained in the first place: ‘I’ll be fine, I’ll figure it out.’ I now process it differently in the hope that it helps make me a better advocate.”
This feature story from Duke SOM’s Magnify continues here. It’s worth reading.
Call for abstracts: 2023 Duke Health Quality and Safety Conference
The virtual poster submission period for the 2023 Duke Health Quality and Safety Conference is now open. The deadline for submission is Wednesday, Dec. 14. The 2023 Conference will be held the weeks of March 13 and 20, with an in-person event on Thursday, March 23.
For more information and to submit your abstract, please click here.
Reminder: Early Voting, 2022 Election
The one-stop early voting period in North Carolina opened on Thursday, Oct. 20 and runs through Saturday, Nov. 5. During early voting, voters may cast a ballot at any early voting site in their county and would-be voters may same-day register and vote. Durham residents have the opportunity to vote at Duke University’s early voting site on campus in Karsh Alumni Center (2080 Duke University Rd, Durham, NC 27708). Multiple early voting sites are available in Durham, Wake, Orange, Person, and Alamance counties. Early voting locations in each county can be found on the NC State Board of Elections website.
Voters who choose to vote by mail may request an absentee ballot until Tuesday, Nov. 1 at 5 p.m. All absentee ballots must be postmarked by 5 p.m. on Election Day and received by Nov. 14 at 5 p.m. Voters who have already requested an absentee ballot may drop it off at any early voting site in-person, either for themselves or a close relative. Absentee ballots may also be returned to the local board of elections office or a designated drop-off site by 5 p.m. on Election Day. Voters can make sure their absentee ballot was received by using Ballottrax, an absentee ballot tracking site operated by the State Board of Elections.
Election Day is Tuesday, Nov. 8 and a list of polling locations can be found here. Visit the State Board of Elections website or vote.duke.edu for additional information. For those of you going to AHA this upcoming weekend, be sure to get out and vote as the meeting is close to election day. The early voting areas in Durham have the weight times on line.

Additional Reminders:
- November is American Diabetes Month and National COPD Awareness Month.
- The DUHS annual flu vaccination campaign is underway. The deadline for staff vaccinations is Tuesday, Nov. 15 at 10 a.m. Vaccination sites for faculty and staff can be found here: https://flu.duke.edu/vaccination/employees/
Upcoming Events & Opportunities
Cardiology Grand Rounds
November 1: No CGR this week.
CME & Other Events
November 4: 14th Annual NC Research Triangle Pulmonary Hypertension Symposium. 7 a.m.-4 p.m. This will be an in-person event at the Durham Convention Center. Registration required. To learn more and register, visit: https://duke.is/jag2b
November 5: Duke Annual Reception at AHA.22. Grand Horizon C, Marriott Marquis Chicago. 5:30 – 8:30 p.m. Questions? Contact Elizabeth Evans or Willette Wilkins.
November 8: Election Day. Please vote!
November 8: DOM Research Quality Town Hall. Topic: 2023 NIH Data Management and Sharing Policy. 12-1 p.m. via Zoom. Register here. You must register to receive the Zoom link for the event.
November 14: Prostate Cancer & CVD Symposium, Webinar 4. Final of a four-part webinar series. Collaboration between the International Cardio-Oncology Society & Duke Heart. Noon, Eastern. Free. To register visit https://duke.is/ptjbs.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
October 20 — Adrian Hernandez and Susanna Naggie
U.S. News & World Report
Study Debunks Use of Antidepressant Luvox as COVID Treatment
https://duke.is/6mc7p
October 24 — Duke Clinical Research Institute
Becker’s Hospital Review
Ivermectin doesn’t accelerate COVID-19 recovery, study suggests
https://duke.is/45qj9
October 24 — Duke University (DCRI)
CNBC
https://duke.is/9hz2e
October 25 — Marat Fudim
mHealth Intelligence
How Wearables Can Enhance Cardiac Care, Boost Patient Engagement
https://duke.is/2vzug
October 25 — Anne Ford (obstetrics/gynecology)
verywellhealth.com
Are Hot Flashes Bad for Your Heart?
Division of Cardiology Publications Indexed in PubMed October 21-26, 2022
Assimon MM, Pun PH, Al-Khatib SM, Brookhart MA, Gaynes BN, Winkelmayer WC, Flythe JE. The modifying effect of the serum-to-dialysate potassium gradient on the cardiovascular safety of SSRIs in the hemodialysis population: a pharmacoepidemiologic study. Nephrol Dial Transplant 2022 Oct 19;37(11):2241-2252. PM: 35793567.
Assimon MM, Pun PH, Wang L, Al-Khatib SM, Brookhart MA, Weber DJ, Winkelmayer WC, Flythe JE. Letter to the editor. Kidney Int 2022 Nov;102(5):1191-1192. PM: 36272744.
Bose S, Yao H, Huang Q, Whitaker R, Kontos CD, Previs RA, Shen X. Using genetically encoded fluorescent biosensors to interrogate ovarian cancer metabolism. J Ovarian Res 2022 Oct 20;15(1):114. PM: 36266675.
Damluji AA, Tehrani B, Sinha SS, Samsky MD, Henry TD, Thiele H, West NEJ, Senatore FF, Truesdell AG, Dangas GD, Smilowitz NR, Amin AP, deVore AD, Moazami N, Cigarroa JE, Rao SV, Krucoff MW, Morrow DA, Gilchrist IC. Position Statement on Vascular Access Safety for Percutaneous Devices in AMI Complicated by Cardiogenic Shock. JACC Cardiovasc Interv 2022 Oct 24;15(20):2003-2019. PM: 36265932.
Naggie S, Boulware DR, Lindsell CJ, Stewart TG, Gentile N, Collins S, McCarthy MW, Jayaweera D, Castro M, Sulkowski M, McTigue K, Thicklin F, Felker GM, Ginde AA, Bramante CT, Slandzicki AJ, Gabriel A, Shah NS, Lenert LA, Dunsmore SE, Adam SJ, DeLong A, Hanna G, Remaly A, Wilder R, Wilson S, Shenkman E, Hernandez AF. Effect of Ivermectin vs Placebo on Time to Sustained Recovery in Outpatients With Mild to Moderate COVID- 19: A Randomized Clinical Trial. JAMA 2022 Oct 25;328(16):1595-1603. PM: 36269852.
Perkovic V, Blackorby A, Cizman B, Carroll K, Cobitz AR, Davies R, DiMino TL, Jha V, Johansen KL, Lopes RD, Kler L, Macdougall IC, McMurray JJV, Meadowcroft AM, Obrador GT, Solomon S, Taft L, Wanner C, Waikar SS, Wheeler DC, Wiecek A, Singh AK. The ASCEND-ND trial: study design and participant characteristics. Nephrol Dial Transplant 2022 Oct 19;37(11):2157-2170. PM: 34865143.
Salah HM, Goldberg LR, Molinger J, Felker GM, Applefeld W, Rassaf T, Tedford RJ, Mirro M, Cleland JGF, Fudim M. Diaphragmatic Function in Cardiovascular Disease: JACC Review Topic of the Week. J Am Coll Cardiol 2022 Oct 25;80(17):1647- 1659. PM: 36265961.
Shahid RA, Vigna SR, Huang MN, Gunn MD, Liddle RA. Nicotinic stimulation of splenic T cells is protective in endoscopic retrograde cholangiopancreatography- induced acute pancreatitis in mice. Am J Physiol Gastrointest Liver Physiol 2022 Nov 1;323(5):G420-G427. PM: 36126221.
Wand AL, Russell SD, Gilotra NA. Ambulatory Management of Worsening Heart Failure: Current Strategies and Future Directions. Heart Int 2021 Jun 7;15(1):49-53. PM: 36277316.
Wendell D, Jenista E, Kim HW, Chen EL, Azevedo CF, Kaolawanich Y, Alenezi F, Rehwald W, Darty S, Parker M, Kim RJ. Assessment of papillary muscle infarction with dark-blood delayed enhancement cardiac MRI in canines and humans. Radiology 2022 Nov;305(2):329-338. PM: 35880980.
Duke Heart Pulse – October 23 2022: Highlights and Updates
Chief’s message:
It is a busy time of year for all of our teams at Duke Heart. This week there are faculty and fellows working on Capital Hill to  discuss the importance of supporting Heart Health. One of our fellows NKiru Osude was a member of the American College of Cardiology group (representing North Carolina) who met with members of congress to discuss the impact of health care disparities, access to care, and the importance of covering services and care for people with heart disease or people as risk for heart disease. She is seen here taking a selfie with the whole group.
discuss the importance of supporting Heart Health. One of our fellows NKiru Osude was a member of the American College of Cardiology group (representing North Carolina) who met with members of congress to discuss the impact of health care disparities, access to care, and the importance of covering services and care for people with heart disease or people as risk for heart disease. She is seen here taking a selfie with the whole group.
As you will see in the stories below, members of Duke Heart continue to work hard to perform research to identify ways to have our community and patients have health, from first responders in cardiac arrest research, the genetics of cardiac arrest, helping with a national cardiogenic shock registry, to studying treatments for COVID, and holding symposiums on pulmonary hypertension. The research and clinical care work at Duke Heart remain vibrant.
 This time of year also has our community in full swing for a variety of fall celebrations and traditions. Halloween for the kids will be next week, we had the NC state fair this week (you can see – still some work to be done for our community’s food choices), and the upcoming American Heart Association Scientific Sessions in early November where we will have several scientific presentations from Faculty and Fellows.
This time of year also has our community in full swing for a variety of fall celebrations and traditions. Halloween for the kids will be next week, we had the NC state fair this week (you can see – still some work to be done for our community’s food choices), and the upcoming American Heart Association Scientific Sessions in early November where we will have several scientific presentations from Faculty and Fellows.
For some of us this weekend also was important as the start of the celebration of Diwali. Diwali is traditionally held on the darkest night of the new moon in Autumn, and celebrates the victory of light over darkness, knowledge over ignorance, good over evil, hope over despair. In many homes it is marked by cleaning and setting up decorations, symbols, and of course many lights. Kids and families celebrate with songs, dances, and all sorts of treats. My daughter was able to perform in a traditional dance at the local temple, and we were fortunate enough to have her grandparents present. After several years of challenges to our communities, health care systems, and scientific communities, we hope whether you celebrate Diwali or not, you have some time over the fall to spend with family and loved ones. You will see in this version of the Pulse there is much to be thankful for, and many who are working to spread light, knowledge, and health in our Duke Heart Community.
evil, hope over despair. In many homes it is marked by cleaning and setting up decorations, symbols, and of course many lights. Kids and families celebrate with songs, dances, and all sorts of treats. My daughter was able to perform in a traditional dance at the local temple, and we were fortunate enough to have her grandparents present. After several years of challenges to our communities, health care systems, and scientific communities, we hope whether you celebrate Diwali or not, you have some time over the fall to spend with family and loved ones. You will see in this version of the Pulse there is much to be thankful for, and many who are working to spread light, knowledge, and health in our Duke Heart Community.
Highlights of the week:
Duke Heart Teams with NC First Responders on Cardiac Arrest Trial
Duke Heart researchers are teaming up with North Carolina emergency care personnel—EMS, fire, police, 911 dispatch and community members—across the state in a pragmatic cluster-randomized trial that will test community interventions to improve survival for out of hospital cardiac arrest (OHCA), a leading cause of death in the U.S.
survival for out of hospital cardiac arrest (OHCA), a leading cause of death in the U.S.
There are more than 400,000 out of hospital cardiac arrests a year in the U.S. with a survival rate of less than 10%. Despite 30 years of efforts by health care professionals, there is scant evidence that cardiac arrest survival odds have substantially improved. Duke researchers are focused on changing that.
The RAndomized Cluster Evaluation of Cardiac ARrest Systems (RACE-CARS) trial covers a geographic area of 62 counties involving eight million residents and expects to enroll 20,000 cardiac arrest patients over a four-year period. It is one of the first U.S. registry-based trials, such that all eligible patients are included and data are efficiently collected in routine care, an approach that has been used with great success in large, efficient clinical trials in Europe. The trial is being conducted by Duke Clinical Research Institute (DCRI) with a $15 million grant from the National Institutes of Health (NIH).
“We’ve leveraged a highly efficient clinical trial design methodology to be able to address a major public health concern in an ambitious project to test community interventions to improve survival from cardiac arrest,” says the trial’s principal investigator, Christopher Granger, MD, professor of medicine in cardiology and director of the Cardiac Care Unit at Duke. “If we’re successful, this will provide compelling evidence to guide how care is provided around the country and around the world to improve survival from cardiac arrest.”
For the trial, 62 counties were randomly assigned to intervention or control groups. Interventions are focused on community CPR and AED treatment, 911 dispatch performance, and first responder treatment for OHCA. The goal is to have more patients with cardiac arrest treated with bystander CPR and early defibrillation. Intervention counties are working closely with the trial team to carry out and evaluate trial interventions while the control groups will continue to provide their usual care.
and AED treatment, 911 dispatch performance, and first responder treatment for OHCA. The goal is to have more patients with cardiac arrest treated with bystander CPR and early defibrillation. Intervention counties are working closely with the trial team to carry out and evaluate trial interventions while the control groups will continue to provide their usual care.
The data collection phase began in July for the trial, which runs from July 1, 2020 through June 30, 2027, and uses the pre-existing Cardiac Arrest Registry to Enhance Survival (CARES) registry for patient enrollment, a platform previously implemented in North Carolina by the RACE CARS team. CARES collects data from 911 dispatch centers, EMS agencies, and hospitals and links that information in a single record.
 In laying the trial groundwork, researchers in the last two years have surveyed current practices at the counties, reviewed care metrics in each county, created site actions plans and held in-person site visits to provide improved outcome guidance, focusing on activities that will shorten the treatment time to CPR and defibrillation during the first 10 minutes of the cardiac arrest. Each county randomized to the intervention strategy has worked with RACE-CARS investigators to develop a customized intervention strategy that is tailored to each individual agency’s unique needs and resources, and customized training plans for each level of the prehospital chain of survival. (Story continues here)
In laying the trial groundwork, researchers in the last two years have surveyed current practices at the counties, reviewed care metrics in each county, created site actions plans and held in-person site visits to provide improved outcome guidance, focusing on activities that will shorten the treatment time to CPR and defibrillation during the first 10 minutes of the cardiac arrest. Each county randomized to the intervention strategy has worked with RACE-CARS investigators to develop a customized intervention strategy that is tailored to each individual agency’s unique needs and resources, and customized training plans for each level of the prehospital chain of survival. (Story continues here)
In addition to Granger, the RACE-CARS team includes Dan Mark, Lisa Monk, Monique Starks, Sana Al-Khatib, Hayden Bosworth, Hussein Al-Khalidi, Kimberly Ward, Steve Vendeventer and James Jollis. Congratulations to all on this important work!
Determining Genetic Causes for Sudden Cardiac Death
People commonly associate heart attacks with clogged arteries, fatty diets, high cholesterol, and plaque buildup in the heart. And while all those things can cause sudden cardiac death, they are not the only culprit; gene mutations can also be to blame.
Certain genetic variants can cause irregular heart rhythms, called arrhythmias, and can affect how well the heart is able to pump

blood to the rest of the body. Otherwise healthy individuals with these genetic variants can fall victim to arrhythmias that are often fatal.
Duke researchers investigated 55 genes responsible for various arrhythmia-related disorders to understand how common these
variants are and the risks they pose. Results were published in Circulation: Genomics and Precision Medicine on September 22.
The team, led by Svati Shah, MD, professor of medicine in cardiology, integrated electronic health records with whole exome sequencing data collected from 8,574 people in the Catheterization Genetics (CATHGEN) cohort, a group that had undergone cardiac catheterization at Duke University Medical Center from 2001 through 2011.
 “We took an in-depth look at the entire diagnostic spectrum, from electrocardiograms to cardiac MRIs, as well as medical charts for history of syncope, arrhythmias, and all the other ways these types of conditions could manifest,” said Navid Nafissi, MD, lead author and a Duke cardiac electrophysiology fellow.
“We took an in-depth look at the entire diagnostic spectrum, from electrocardiograms to cardiac MRIs, as well as medical charts for history of syncope, arrhythmias, and all the other ways these types of conditions could manifest,” said Navid Nafissi, MD, lead author and a Duke cardiac electrophysiology fellow.
The researchers wanted to know whether patients’ symptoms met diagnostic criteria for these conditions and if there was any evidence of sub-diagnoses that might have been missed because they did not meet full diagnostic criteria.
One in 108 people in this cohort carried a pathogenic or likely pathogenic variant in arrhythmia-related genes, which means these variants may be more common in the general population than researchers initially thought.
How severe the genetic variants are, though, varies greatly. The likelihood that a particular variant might cause health problems can range from zero to as high as 83%. Issues might include dilated cardiomyopathy, which causes the heart’s ventricles to thin, stretch out, and grow larger; or hypertrophic cardiomyopathy, which causes the heart muscle to gather scar tissue and thicken. Both these disorders make it harder for the heart to pump blood to the rest of the body. Variants can also cause disorders like long QT syndrome and Brugada syndrome that cause fast, chaotic heartbeats. All of these disorders can lead to sudden death in otherwise healthy people.
“These are people who just die suddenly — without any warning signs,” Nafissi said. “Sometimes there’s no clear manifestations of cardiac disease, even in autopsy.” The heart might look completely healthy: no cholesterol build up, and sometimes no signs of scar tissue from hypertrophic cardiomyopathy or thinning ventricles from dilated cardiomyopathy.
When there is no clear reason as to why a person had a sudden cardiac death, genetic testing can help determine what happened. “Sometimes you can find a causative genetic variant in these cases,” Nafissi said, “which can allow for tailored management and cascade screening of family members.”
Current standards of care still take a reactive approach to this problem. If someone goes into sudden cardiac arrest, health care and emergency workers address the crisis and try to save the patient — but what if there was a better, more proactive approach?
Nafissi hopes this research takes researchers one step closer to utilizing genetic testing earlier to identify those who have genetic variants that could put them at increased risk of sudden cardiac arrest. But, Nafissi clarifies, “Not everyone who carries a variant will go on to have a cardiac event.”
The trick will be identifying those at highest risk and determining the appropriate preventive interventions, such as an implantable cardioverter-defibrillator or something less invasive, like lifestyle modifications or medications. “There are multiple ways that this research could lead to saving lives,” Nafissi said.
Duke Team to help Co-Lead Newly Established Cardiogenic Shock Registry
The American Heart Association (AHA) has established the world’s first professional society shock registry as part of the Get With The Guidelines registries network. Mitch Krucoff, MD, professor of medicine in cardiology at Duke will serve as co-chair of the registry along with Dr. David Morrow, director of the Levine Cardiac Intensive Care Unit at Brigham and Women’s Hospital  and professor of medicine at Harvard.
and professor of medicine at Harvard.
The creation of this new registry is the direct result of work done by the Cardiac Safety Research Consortium Think Tank on cardiogenic shock, according to Krucoff.
Cardiogenic shock—a life threatening condition when a person’s heart can’t pump enough blood to meet the needs of the body—is most often caused by serious heart attack or advanced heart failure. Historically, data related to cardiogenic shock have been limited, inconsistent and challenging to interpret. As a result, varying treatment recommendations exist around best  practices.
practices.
The new registry will help researchers, clinicians and regulators to better understand the clinical symptoms of shock types, treatment patterns and outcomes. The registry will provide a foundation for working toward improving the quality and consistency of care in patients in U.S. hospitals with cardiogenic shock symptoms. This effort has had many of our current and past Duke Faculty and fellows involved including Mark Samsky, Magnus Ohman, Joseph Rogers, and Sunil Rao.
“To understand how to improve care for cardiogenic shock patients, we first need a clearer view of the landscape of existing treatment practices for cardiogenic shock in U.S.-based acute care settings,” said Krucoff. “No organization is better positioned to advance this critical public health question than the AHA, with already established networks of sites entering data on heart failure, acute cardiac syndromes, cardiac arrest and COVID—all of which involve patients at risk of progressing to cardiogenic shock.”
The Cardiogenic Shock Registry builds on more than 20 years of quality improvement and registry experience rooted in the AHA’s Get With The Guidelines platform. Data from the registry will help inform the larger medical community on how best to treat cardiogenic shock.
“The new Cardiogenic Shock Registry will leverage the unparalleled reach of the AHA in a unique collaboration between academic clinicians and researchers, federal agencies and funding supporters’ experts to provide high-quality evidence and promote best practices for the treatment of patients with cardiogenic shock,” said Morrow.
Krucoff and Morrow both serve as volunteer experts for the AHA. The AHA’s Precision Medicine Platform, a secure cloud-computing platform, will be used to facilitate the research.
ICYMI: Boulware Named Dean of WFU School of Medicine
 Ebony Boulware, MD, MPH, Director of the Duke Clinical and Translational Science Institute (CTSI), Vice Dean for Translational Science in the School of Medicine, and Associate Vice Chancellor for Translational Research at Duke University, has accepted the role of Dean of the Wake Forest University School of Medicine. She will begin her new role in January 2023. Dr. Boulware will also serve as the Vice Chief Academic Officer and Chief Science Officer at Atrium Health. She will step down from her positions at Duke on December 31, 2022, as she makes her transition to this exciting leadership opportunity.
Ebony Boulware, MD, MPH, Director of the Duke Clinical and Translational Science Institute (CTSI), Vice Dean for Translational Science in the School of Medicine, and Associate Vice Chancellor for Translational Research at Duke University, has accepted the role of Dean of the Wake Forest University School of Medicine. She will begin her new role in January 2023. Dr. Boulware will also serve as the Vice Chief Academic Officer and Chief Science Officer at Atrium Health. She will step down from her positions at Duke on December 31, 2022, as she makes her transition to this exciting leadership opportunity.
The announcement was made on Monday by Kathleen Cooney, MD, chair of the Duke Department of Medicine and Mary E. Klotman, MD, Dean, Duke University School of Medicine.
Boulware, the Nanaline H. Duke University Distinguished Professor in the Department of Medicine, joined the Duke faculty in 2013 as Chief of the Division of General Internal Medicine in the Department of Medicine and has served as Director of CTSI and Vice Dean for Translational Science since 2016. She has spent most of her academic career investigating how to improve health care and health outcomes for individuals and populations with chronic kidney disease, hypertension, and other chronic diseases, particularly focusing on minoritized populations. In her roles at Duke, she has been instrumental in accelerating the translation of research to clinical care, and she is a national leader in addressing the causes and effects of racial and ethnic health and health care inequities.
The SOM and DOM will work with the Division of General Internal Medicine to create a transitional leadership plan as they prepare to launch a national search for a new Division Chief.
“Dr. Boulware has been a dedicated and innovative leader, and we want to thank her for her service and commitment to the School of Medicine,” said Cooney and Klotman in their statement. “She made significant contributions to the Department of Medicine in her role as Division Chief and generously mentored many faculty members within and outside of the Division. Her passion for addressing health inequities and improving our approach to diversity, equity, and inclusion has profoundly strengthened our department. We know you will join us in congratulating Dr. Boulware.”
Personally, Ebony has been a leader across so many areas a Duke – she will be missed. We are excited for her and will look forward to continuing to collaborate on making NC a healthier state! Congratulations – Ebony!
Nicholls, Chen Join Duke Heart APP Team
Please join us in welcoming two new APPs to our Duke Heart team!
First, we are welcoming Stephanie Nicholls, a nurse practitioner, back to our team. She will be working at South Durham Clinic with Michael Blazing, and at Duke Cardiology Arringdon. Nicholls is originally from a small town in Maine and moved to NC in 2013 to work at Duke. She was initially in the CTICU and then went on to serve as a heart transplant coordinator. She met her husband at Duke and they now have two children — Emma, 3, and Luke, 1. She lives in Durham and can typically be found chasing children around The Museum of Life and Science. She enjoys the great restaurant scene in Durham and going to the beach. She has always enjoyed being a part of the vibrant Duke community and is excited to join her new team.
Karina Chen, a physician assistant, will be at Duke Cardiology Arringdon working with Cary Ward and the DHP group. Chen grew up in southeastern Michigan and attended Fordham University for her bachelor’s degree in biology. She spent some time working as an EMT and CNA before moving to Boston for PA school at Massachusetts College of Pharmacy and Health Science. After graduating, she worked at Brigham and Women’s Hospital in Pulmonary Vascular Medicine with a focus on caring for patients with pulmonary hypertension. She and her husband moved to NC in order to escape the freezing Boston winters, as well as to be closer to her parents who are now living in SC. They are enjoying trying new restaurants in the Triangle area and exploring hiking trails with their corgi, Gimli. She is excited to join the Duke Heart team.
Please welcome Stephanie and Karina to our team!
Shout-out to CT OR Team
Our cardiothoracic team managed a particularly difficult surgical case on Wednesday — a big shout-out to our incredible and dedicated multidisciplinary team! Together, they rallied, showed incredible teamwork, and the patient is doing well.
“I especially want to express my gratitude for Reeni, who scrubbed in and stayed way late to see this through to completion.” – Jacob Schroder
Congrats to all. Well done!
Duke Heart Construction Update
Construction on Cardiac Catheterization Lab 1 is due for completion by Nov. 7 with inspections taking place Nov. 7-11. The team plans to conduct their first case in Cath 1 on the afternoon of Nov. 14. A team from Philips will be present for support as well as training from Nov. 14-17. If you have any questions please contact Elizabeth Watts.
Arges Focused on Raising Vital Funds for MSA
Many of you know that Kristine Arges, RN, BSN, CCRC, left Duke Heart earlier this year after 31 years on the team. Arges is on disability leave after receiving a diagnosis of Multiple Systems Atrophy-Cerebellar (MSA), a rare, incurable neurodegenerative disease that can rapidly progress.
Due to elusive symptoms that appeared over time and seemed unrelated to each other, she went several years before being diagnosed. The disease has progressed fast, and she is now walker- and wheelchair-dependent. After her diagnosis, she began reading up on MSA and says she was shocked to find there are few treatment options and little research being done. She reached out to Mayo Clinic after learning about the work of Dr. Wolfgang Singer, an associate professor of neurology who has completed phase-one research showing that disease progression of MSA could be slowed through the infusion of autologous mesenchymal stem cells. The research looks promising. Arges qualified for the study and enrolled; she is three months in and has completed two infusions of either stem cells or placebo, 2:1.
Having grown up in Manhattan, she earned her BSN at Columbia School of Nursing and quickly found work in a neuro-surgical stepdown at Columbia-Presbyterian. Two years later, she was ready to leave New York City behind her and chose Durham, NC as her next home.
Arges applied at Duke Hospital where there was a need for nurses on 3200; she started on the unit in 1991. Once she made the switch to cardiology care she never looked back. Arges says she developed her sea legs in the ACU and then joined the heart failure research group under Chris O’Connor, MD. There, she eventually coordinated the PRAISE 1 & 2 studies, noting that O’Connor always inspired a healthy sense of competition – and that he and she, ‘Chris and Kris,’ were always vying to be the top enrollers. Kris went on to coordinate many trials in the HF group such as BEST, OPTIME, and CHARM to name just a few.

Pictured here with longtime friend Stephanie Kerr, RN, MSN, at a party celebrating the successful conclusion of the PRAISE 1 trial.
She joined Duke’s Cardiac Diagnostic Unit in 2003 and conducted imaging trials with many of ‘the greats’ in Duke Cardiology, including Jamie Jollis, Joe Kisslo, Zainab Samad, Jerry Bloomfield, Pam Douglas, Eric Velazquez, Michel Khouri, Sreek Vemulapalli and, of course, Fawaz Alenezi. Kris became a “lifer” in the CDU and spent the remainder of her career there. She wore many hats in the CDU – as a stress-nurse one day per week, and as an intermediary for study coordinators in various disciplines who needed tests done on their research patients.
In the “old days,” she says, there wasn’t a system in place to help sonographers know which images to acquire. With the trend in clinical trials to monitor cardiac safety, more and more studies required echocardiograms on study patients. In addition to organizing a system of imaging instructions for what came to be more than 100 research clinical trials, she coordinated contrast perfusion studies in ultrasound; helped manage core lab work at the Duke Clinical Research Institute; and in the lab, she coordinated amyloid studies – including the ATTRACT trial (which became Tafamidis), served as the REMIT nurse working with Wei Jiang, MD for several years, and coordinated a number of studies with the Biomedical Engineering group.
In her last ten years at Duke, she served as lead CRC of Cardiac Imaging. She shared this role with Michele Parker in MRI. Kris’s research group was multi-disciplinary — a microcosm of life in the CDU– consisting of exercise physiologists, sonographers, nurses, clerical assistants, and students.
“Perhaps the thing I loved most about my job was the ever-present variety of people, patients, and disciplines,” said Arges. “Never was there ever a dull moment. The CDU was the place to be.”
Arges and others are working to raise funds to ensure that all 70 patients currently enrolled in the clinical trial can receive compassionate use of stem cells upon completion of Phase 2. All patients involved “have everything to lose if funds are not raised to buy them time until a new treatment or cure is found,” Arges says.
Saddened to have left her role at Duke, Arges is resolved to keep fighting as long as she can. She thinks fondly of her time at Duke Heart, misses her former co-workers, and wishes all of us a belated and fond farewell.
Arges is open about her life with MSA and wants to raise awareness of this poorly recognized disease. She has created a ‘legacy page’ which lives on the Defeat MSA Alliance website where you can learn more about MSA as well as donate. Kris says that she would be honored if you considered supporting her and others with this condition.

Kris is shown here with members of her Duke research group. L-R are: Alicia Armour, Melissa LeFevre, Arges, Jennifer Tomfohr and Danielle Wilson).
You are missed, Kris!
Early Voting in NC, on Duke Campus: 2022 Election
The one-stop early voting period in North Carolina opened on Thursday, Oct. 20, and runs through Saturday, Nov. 5. During early voting, voters may cast a ballot at any early voting site in their county and would-be voters may same-day register and vote. Durham residents have the opportunity to vote at Duke University’s early voting site on campus in Karsh Alumni Center (2080 Duke University Rd, Durham, NC 27708). Multiple early voting sites are available in Durham, Wake, Orange, Person, and Alamance counties. Early voting locations in each county can be found on the NC State Board of Elections website.
 Voters who choose to vote by mail may request an absentee ballot until Tuesday, Nov. 1 at 5 p.m. All absentee ballots must be postmarked by 5 p.m. on Election Day and received by Nov. 14 at 5 p.m. Voters who have already requested an absentee ballot may drop it off at any early voting site in-person, either for themselves or a close relative. Absentee ballots may also be returned to the local board of elections office or a designated drop-off site by 5 p.m. on Election Day. Voters can make sure their absentee ballot was received by using Ballottrax, an absentee ballot tracking site operated by the State Board of Elections.
Voters who choose to vote by mail may request an absentee ballot until Tuesday, Nov. 1 at 5 p.m. All absentee ballots must be postmarked by 5 p.m. on Election Day and received by Nov. 14 at 5 p.m. Voters who have already requested an absentee ballot may drop it off at any early voting site in-person, either for themselves or a close relative. Absentee ballots may also be returned to the local board of elections office or a designated drop-off site by 5 p.m. on Election Day. Voters can make sure their absentee ballot was received by using Ballottrax, an absentee ballot tracking site operated by the State Board of Elections.
Election Day is Tuesday, Nov. 8 and a list of polling locations can be found here. Visit the State Board of Elections website or vote.duke.edu for additional information.
Additional Reminders:
- October 23-29 is Respiratory Care Week. Please send some love their way this week!

- DukeALERT testing was performed this week. Please make sure you’re familiar with the several ways in which you would be informed in the event of an emergency. You can find great information on the Duke Emergency Management Website as well as the DUHS Preparedness and Response Center.
- October is Medical Ultrasound Awareness Month – thank a sonographer!
- Open Enrollment is now open through Oct. 28. This is your opportunity to review your medical, dental, vision, and reimbursement account benefit elections and make any changes necessary to ensure your choices continue to meet your needs. You should have received a copy of the annual Open Enrollment Guide in the mail from Duke HR.
- The DUHS annual flu vaccination campaign is underway. The deadline for staff vaccinations is Tuesday, Nov. 15 at 10 a.m. Vaccination sites for faculty and staff can be found here: https://flu.duke.edu/vaccination/employees/
Upcoming Events & Opportunities
Cardiology Grand Rounds
October 25: No CGR this week.
CME & Other Events
October 17-28: Open Enrollment period for 2023 for all Duke faculty and staff.
October 28: Duke Caregiver Community Event, in-person conference. Details here: https://duke.is/nzbcp.
November 4: 14th Annual NC Research Triangle Pulmonary Hypertension Symposium. 7 a.m.-4 p.m. This will be an in-person event at the Durham Convention Center. Registration required. To learn more and register, visit: https://duke.is/jag2b
November 5: Duke Annual Reception at AHA.22. Grand Horizon C, Marriott Marquis Chicago. 5:30 – 8:30 p.m. Questions? Contact Elizabeth Evans or Willette Wilkins.
November 14: Prostate Cancer & CVD Symposium, Webinar 4. Final of a four-part webinar series. Collaboration between the International Cardio-Oncology Society & Duke Heart. Noon, Eastern. Free. To register visit https://duke.is/ptjbs.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
October 14 — Mark Sendak (DIHI)
The Medical Futurist
The 8 Most Reassuring Examples of Using A.I. In Healthcare
https://duke.is/gg32v
October 17 — Joseph Turek and the Sinnamon family
WAFF TV-48 (Huntsville, AL)
World’s first heart & thymus transplant
https://duke.is/v3jh2
*clip begins @ 12:24:34
October 18 — Duke Health
Becker’s Hospital Review
10,000 patients out of network in Duke-UnitedHealthcare dispute
https://duke.is/bca28
October 19 — Shahzeb Khan, G. Michael Felker & Marat Fudim
Medscape/JACC HF
Are we Getting any Closer to Understanding Congestion?
https://duke.is/ch3hc
October 19 — Adrian Hernandez & Susanna Naggie
CBS-17 WNCN/cbs17.com (Raleigh)
COVID debate semi-settled: Antidepressant does not work as treatment
https://duke.is/wa9sg
October 20 — Adrian Hernandez & Susanna Naggie
HealthDay News/U.S. News & World Report
Study Debunks Use of Antidepressant Luvox as COVID Treatment
https://duke.is/jp5pj
Duke Heart Pulse October 16th 2022
Wang to become Chief of Comparative Effectiveness Research at PCORI

Tracy Wang, MD, professor of medicine in cardiology at Duke and Director of Health Services & Outcomes Research at the Duke Clinical Research Institute, has accepted an exciting new role as Chief of Comparative Effectiveness Research at the Patient Centered Outcomes Research Institute (PCORI). Her last day at Duke will be Nov. 7.
“After almost 20 years at Duke, I have made the difficult decision to pursue a totally different career pathway at PCORI in Washington, DC,” Wang wrote in a message to colleagues. “As many of you know, it’s been a true privilege to train here at Duke, and my time as faculty has continued to offer learning opportunities every day as I work alongside amazing colleagues and friends.
“Here, we have a unique environment that allows us to contribute to medicine by taking care of some of the sickest patients out there, by taking on meaningful and impactful scientific research, and by growing the next generation of cardiologists and researchers. It has been a true honor to serve here and, from the bottom of my heart, I thank you for all your support, collegiality, and friendship over the years.”
Tracy has been an inspiration to generations of cardiology fellows and faculty and has won numerous mentoring awards. She has been tireless in her pursuit of improving quality of our care and has been a consummate collaborator and leader in our Division. The ability to shape the national landscape of comparative effectiveness research through PCORI seems like the a position built for someone with her skills, passion, and desire to improve health through clinical science. Tracy is a world-class physician researcher who will undoubtedly bring critical thinking and common sense solutions that will have immediate impact on all of those around her.
Personally, it is bittersweet to have her leave our Duke Heart team and the DCRI, but we are excited for this next stage of her career and we look forward to continued collaboration and friendship with her over the coming years.
Congratulations, Tracy!
Gehling Joins Duke Development; Will Support Duke Heart
Please join us in welcoming William Gehling to Duke Heart! Gehling is the new Director of Development for Heart and Lung in the office of Duke Health Development and Alumni Affairs. He began his position in late August and has spent the last  month acclimating to DUHS.
month acclimating to DUHS.
William relocated here from New York, where he most recently served as a director of development at Stony Brook Medicine supporting their Department of Surgery as well as Stony Brook Children’s. He has prior experience with fundraising and alumni relations at the Center for Reproductive Rights, Weill Cornell Medicine, NYU Langone Health, and New York-Presbyterian.
Gehling says he looked at the chance to work for Duke Health as an opportunity to reconnect with his roots.
“My family is still here in North Carolina, so it’s nice to be able to be closer to them,” he said. “I really love academic medicine fundraising and the opportunity to support Duke Heart is special to me because my father had care here. Dr. Milano was his provider and I can really attest to the amazing care that was provided to our family. It’s nice to go full circle and give back to support a program that supported us as a family.
“Overall, I’m excited to support the tripartite mission. I know the faculty here are just really incredible. They have a vision they are trying to execute and that’s where my job comes in. I can’t do the medical work or the discovery work that they’re doing, but I can help find the right donor to support their efforts. I know that every time I’m raising funds, another family is going to be provided for and that’s really special.”
Originally from the greater Charlotte area, William holds a bachelor’s degree from NC State University. He enjoys running and has completed two New York City marathons.
Welcome to Duke Heart, William!
Notable Efforts & Recent Happenings
Camille Frazier-Mills and Sana Al-Khatib served as program faculty for the Women in Electrophysiology summit held at the Sofitel Chicago Magnificent Mile in Chicago Oct. 13-15.

Tommy D’Amico served as a member of the program committee for the AATS International
Thoracic Surgical Oncology Summit held in NYC Sept. 30-Oct. 1
Jason Katz served as a course director for the 2nd Annual NYU Langone Critical Care Cardiology Symposium held in NYC Oct. 13-14.

The Duke Cardio-Oncology 2022 conference Cardio-Oncology in the Era of Precision Medicine was held at the J.B. Duke Hotel & Conference Center in Durham on Friday, Oct. 14. Michel Khouri and Susan Dent co-led the program. The conference was very well attended and we continue to be excited about this growing area of research and improved care for patients. Khouri presented “Risk Identification and Management Strategies of Cardiotoxicities” and Nishant Shah presented “Identifying Cardiometabolic Risk and Preventive Cardiology Strategies.”



Congratulations to all – great job!
Celebrating Sonographers
October is Medical Ultrasound Awareness Month, and we would like to take a moment to thank all of the sonographers throughout Duke Heart for their hard work and dedication to the field of Cardiovascular Ultrasound. Our Duke Heart Center patients benefit from your expertise, careful attention to detail, and thoughtful care. We are grateful to work alongside each of you!
throughout Duke Heart for their hard work and dedication to the field of Cardiovascular Ultrasound. Our Duke Heart Center patients benefit from your expertise, careful attention to detail, and thoughtful care. We are grateful to work alongside each of you!
Speaking of sonographers… we’re excited about a newly published book with submissions by several of our team members. Please see our next story.
New Congenital Echocardiography Guide Now Available
A new reference guide for congenital echocardiography is now available. The first edition of Congenital Echocardiographer’s  Pocket Reference was authored by Richie Palma, Director of the Duke Cardiac Ultrasound Certificate Program, and Melissa Wasserman, Supervisor of Echo Lab Satellite Operations at
Pocket Reference was authored by Richie Palma, Director of the Duke Cardiac Ultrasound Certificate Program, and Melissa Wasserman, Supervisor of Echo Lab Satellite Operations at Children’s Hospital of Philadelphia. The book includes contributions from 33 of the top sonographers in the U.S., including Duke’s own Colin Dunbar, Tracy Ralston, Ashlee Davis and Jon Owensby. Gregory Tatum, MD, Medical Director of Duke Children’s Specialty Clinic of Greensboro and Director of Quality and Education for the Duke Pediatric Echocardiography Lab, wrote the forward and served as editor.
Children’s Hospital of Philadelphia. The book includes contributions from 33 of the top sonographers in the U.S., including Duke’s own Colin Dunbar, Tracy Ralston, Ashlee Davis and Jon Owensby. Gregory Tatum, MD, Medical Director of Duke Children’s Specialty Clinic of Greensboro and Director of Quality and Education for the Duke Pediatric Echocardiography Lab, wrote the forward and served as editor.
The book has 32 chapters and offers access to hundreds of videos and diagrams. Tatum says it’s “the perfect book for someone who is beginning their career in echocardiography, as well as someone who wants to refresh on topics within congenital heart disease. Palma and Wasserman have created an invaluable reference resource for all learners and practitioners of congenital echocardiography.”
The book, published this summer, is currently available only through the Arizona Heart Foundation.
Congratulations to all involved!
Shout-out to Senman
 Congratulations to second year fellow Balim Senman — she was the only cardiology trainee invited to participate in and lead a session at the 2nd annual NYU Langone Critical Care Cardiology Symposium held Oct. 13-14 in NYC. Senman co-moderated an incredible breakout discussion on the impact of “Social Media in Critical Care Cardiology Education, Research and Professional Advancement.”
Congratulations to second year fellow Balim Senman — she was the only cardiology trainee invited to participate in and lead a session at the 2nd annual NYU Langone Critical Care Cardiology Symposium held Oct. 13-14 in NYC. Senman co-moderated an incredible breakout discussion on the impact of “Social Media in Critical Care Cardiology Education, Research and Professional Advancement.”
Great job, Balim!
Kudos to Kosovec
Congratulations to Juliann Kosovec, a resident in Duke’s General Surgery Residency Program — she and her co-authors won the best poster award at the AATS’s International Thoracic Surgical Oncology Summit held Sept. 30-Oct. 1 at the Sheraton New York Times Square in NYC. Their abstract, Redefining Quality Metrics in cN2M0 Non-Small Cell Lung Cancer, can be found here.
Way to go, Juliann!
Shout-out to Rao
Congratulations to Advanced Heart Failure and Transplant Cardiology fellow Vishal Rao – he has been named a top reviewer to the Journal of Cardiac Failure (JCF).
 In a letter sent to Manesh Patel from the journal’s Editor-in-Chief Robert Mentz and Deputy Editor Anu Lala-Trinidade, they stated, “Of a large pool of expert reviewers, Dr. Rao stood out for being timely and providing insightful comments that contributed meaningfully to the improvement of manuscripts and publication decision processes. We recognize the numerous demands on Dr. Rao’s time and are especially grateful for the time and effort that goes into providing high-quality impactful reviews. Dr. Rao was acknowledged publicly at the JCF reception at the HFSA Annual Scientific Meeting on October 2, 2022, for his contributions. We look forward to Dr. Rao’s further work with the JCF family.”
In a letter sent to Manesh Patel from the journal’s Editor-in-Chief Robert Mentz and Deputy Editor Anu Lala-Trinidade, they stated, “Of a large pool of expert reviewers, Dr. Rao stood out for being timely and providing insightful comments that contributed meaningfully to the improvement of manuscripts and publication decision processes. We recognize the numerous demands on Dr. Rao’s time and are especially grateful for the time and effort that goes into providing high-quality impactful reviews. Dr. Rao was acknowledged publicly at the JCF reception at the HFSA Annual Scientific Meeting on October 2, 2022, for his contributions. We look forward to Dr. Rao’s further work with the JCF family.”
Well deserved, Vishal!
Duke Team Attends AMPATH Global Gathering
The AMPATH Global Gathering was held last weekend in Indianapolis and Duke was well represented. The team celebrated advancing our commitment to global health and in particular, our relationship with Moi Teaching and Referral Hospital (MTRH) in El Doret, Kenya. AMPATH (Academic Model Providing Access to Healthcare) is a partnership between MTRH and a consortium of North American institutions led by Indiana University.

AMPATH began working in western Kenya in 1988 and has been most widely known for its work addressing HIV/AIDS. Duke joined the AMPATH consortium in 2009 with support from a National Heart, Lung, and Blood Institute (NHLBI) grant to create a cardiovascular and pulmonary disease Center of Excellence. The Cardiovascular Center of Excellence partnership has been a joint effort led by the Hubert-Yeargan Center for Global Health (HYC), the Duke Clinical Research Institute (DCRI) and Duke Heart, with initial leadership from Duke faculty members Eric Velazquez (now at Yale) and Gerald Bloomfield.
Clinical educational efforts have been led by John Lawrence, adjunct assistant professor of medicine in cardiology at Duke. Lawrence has, since the earliest years, has spent four to eight months a year in Kenya helping to establish a clinical cardiovascular service including a robust outpatient clinic, inpatient teaching service, opening a new 10-bed cardiac care unit and leading the development of a Cardiovascular Fellowship Training Program at Moi University with the support of HYC.
HYC is led by Executive Director Chris Woods, Executive Director Nathan Thielman and Director of Operations Cynthia Binanay, who has led the Kenya Operations with HYC since 2006. Since 2009, the cardiovascular efforts have been supported by expanding partnerships within Duke, with other AMPATH institutions, and the DUCCS alumni network.
Duke Heart has been a consistent partner and supporter of the Cardiovascular COE since its inception. Numerous physicians, nurses and echocardiographers have rotated there for educational and consultative activities. Duke trainees have rotated at MTRH as part of the Global Health Residency Pathway, and many have been mentored by Bloomfield as Fogarty Global Health Fellows, Doris Duke Clinical Scholars and junior faculty at Duke with ongoing support from Duke Heart for global health efforts.
Pictured here (left to right) are some members of the partnership who attended the Global Gathering last weekend: Gerald Bloomfield, Cory Miller, Nick Nguyen, Titus Ngeno, Felix Barasa (Head, Cardiology Unit at MTRH), Wilson Sugut (Head, Department of Medicine at MTRH), Duke hospitalist Rebecca Lumsden, Andrew McCrary, Lauren McCrary, Cynthia Binanay, Tara Holder (former Duke IM resident, current ICC fellow at Vanderbilt), Rob Nealy (UT Austin, Cardiothoracic Surgery); Shanti Nulu (UT Austin, Cardiology), Dale Lawrence, and John Lawrence.
Bloomfield, Ngeno, Lawrence and others have been pillars leading the development of clinical programs and research with our colleagues at MTRH. They’ve done incredible work in El Doret and we look forward to all they will continue to accomplish.
Photo of the Week
Magnus Ohman, adjunct professor of medicine in cardiology, met recently with long-time Duke Heart supporters Mr. and Mrs. Albert “Lynn” Williams over lunch at the Washington Duke Inn.
 Ohman said, “We had a wonderful meeting and we spoke about their philanthropy supporting the lecture in Cardiovascular Genetics. He and his wife shared how meaningful it was for them to support this and to see all the outstanding scientists that have spoken at these lectures over the years. They also commented on how cardiovascular genetics are now moving to the forefront in several areas of cardiology.”
Ohman said, “We had a wonderful meeting and we spoke about their philanthropy supporting the lecture in Cardiovascular Genetics. He and his wife shared how meaningful it was for them to support this and to see all the outstanding scientists that have spoken at these lectures over the years. They also commented on how cardiovascular genetics are now moving to the forefront in several areas of cardiology.”
Having fostered numerous relationships with Duke Heart donors, grateful patients and the Duke Health development teams over many years, Ohman enjoys maintaining these connections.
“Philanthropy is so rewarding, as it is so meaningful to a donor and so important for the academic aspects of medicine that otherwise would not be possible,” Ohman added. “It’s a true win-win situation.”
Additional Reminders:
- October is Medical Ultrasound Awareness Month – thank a sonographer!
- National Physician Assistant Week was celebrated Oct. 6-12. We are so grateful for the incredible work our PAs do throughout Duke Heart and throughout the Health System. Thank you!
- Open Enrollment starts tomorrow and runs Oct. 17-28. This is your opportunity to review your medical, dental, vision, and reimbursement account benefit elections and make any changes necessary to ensure your choices continue to meet your needs. You should have received a copy of the annual Open Enrollment Guide in the mail from Duke HR.
- The DUHS annual flu vaccination campaign is underway. The deadline for staff vaccinations is Tuesday, Nov. 15 at 10 a.m. Vaccination sites for faculty and staff can be found here: https://flu.duke.edu/vaccination/employees/
- Duke Health has launched our first comprehensive Team Member Referral Program. Team members at Duke University Health System and Duke University who refer qualified candidates for any posted clinical or non-clinical positions at https://careers.dukehealth.org/ may be eligible for a monetary bonus and prizes. To learn more, visit: https://duke.is/2sjkv
Upcoming Events & Opportunities
Cardiology Grand Rounds
October 18: PRECIDENT D Study at Duke with Schuyler Jones. 5 p.m. Webex. This event will be online only.
CME & Other Events
October 17-28: Open Enrollment period for 2023 for all Duke faculty and staff.
October 28: Duke Caregiver Community Event, in-person conference. Details here: https://duke.is/nzbcp.
November 4: 14th Annual NC Research Triangle Pulmonary Hypertension Symposium. 7 a.m.-4 p.m. This will be an in-person event at the Durham Convention Center. Registration required. To learn more and register, visit: https://duke.is/jag2b
November 5: Duke Annual Reception at AHA.22. Marriott Marquis Chicago. 5:30 – 8:30 p.m. Questions? Contact Elizabeth Evans or Willette Wilkins.
November 14: Prostate Cancer & CVD Symposium, Webinar 4. Final of a four-part webinar series. Collaboration between the International Cardio-Oncology Society & Duke Heart. Noon, Eastern. Free. To register visit https://duke.is/ptjbs.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
October 7 — Joseph Turek and the Sinnamon family
WILX 10 News (Lansing, MI)
Your Health: History-making patient is thriving
https://duke.is/zbkkx
October 7 — Adrian Hernandez
The Daily Progress
UVa Health leads statewide COVID-19 clinical trial
https://duke.is/mk59u
October 7 — Senthil Selvaraj
Medscape
Dapagliflozin DELIVERs Regardless of Systolic BP in HF With Preserved EF
https://duke.is/8qjzj
October 10 — Michael Pencina
Healthcare Innovation
With Focus on Equity, Coalition for Health AI Readies Framework Release
https://duke.is/j8bcn
October 10 — Joseph Turek and the Sinnamon family
WDAM (Hattiesburg-Laurel, MS)
https://duke.is/rujdc
*clip starts at 5:17:05
October 12 — G. Michael Felker
Medical Dialogues
Sacubitril/Valsartan May Reduce Mitral Regurgitation in HFrEF, Eliminating Need for Interventions
https://duke.is/bj9fr
October 12 — Harry Severance
Medpage Today
Isn’t It a Seller’s Market for Healthcare Professionals?
https://duke.is/czagj
October 13 — Tommy D’Amico
rtve.es (Spain)
Diego González Rivas, el cirujano que ha operado en más países en la historia de la medicina
https://duke.is/ws8wp
Division of Cardiology Publications Indexed in PubMed October 7-12, 2022
Coats AJS, Abraham WT, Zile MR, Lindenfeld JA, Weaver FA, Fudim M, Bauersachs J, Duval S, Galle E, Zannad F. Baroreflex activation therapy with the Barostim™ device in patients with heart failure with reduced ejection fraction: a patient level meta-analysis of randomized controlled trials. Eur J Heart Fail 2022 Sep;24(9):1665-1673. PM: 35713888.
Garus M, Zdanowicz A, Fudim M, Zymliński R, Niewiński P, Paleczny B, Rosiek-Biegus M, Iwanek G, Ponikowski P, Biegus J. Clinical determinants and prognostic significance of hypocapnia in acute heart failure. Sci Rep 2022 Oct 7;12(1):16889. PM: 36207364.
Heffron SP, Windheim J, Barrett TJ, Voora D, Berger JS. Platelet inhibition by low-dose aspirin is not influenced by body mass or weight. Platelets 2022 Nov 17;33(8):1208-1213. PM: 35768902.
Jones MM, McElroy LM, Mirreh M, Fuller M, Schroeder R, Ghadimi K, DeVore A, Patel CB, Black-Maier E, Bartz R, Thomas K. The impact of race on utilization of durable left ventricular assist device therapy in patients with advanced heart failure. J Card Surg 2022 Nov;37(11):3586-3594. PM: 36124416.
Kunadian V, Baber U, Pivato CA, Cao D, Dangas G, Sartori S, Zhang Z, Angiolillo DJ, Briguori C, Cohen DJ, Collier T, Dudek D, Gibson M, Gil R, Huber K, Kaul U, Kornowski R, Krucoff MW, Dehghani P, Mehta S, Moliterno DJ, Ohman EM, Escaned J, Sardella G, Sharma SK, Shlofmitz R, Weisz G, Witzenbichler B, Džavík V, Gurbel P, Hamm CW, Henry T, Kastrati A, Marx SO, Oldroyd K, Steg PG, Pocock S, Mehran R. Bleeding and Ischemic Outcomes With Ticagrelor Monotherapy According to Body Mass Index. JACC Cardiovasc Interv 2022 Oct 10;15(19):1948-1960. PM: 36202563.
Morris K, Weston K, Davy A, Silva S, Goode V, Pereira K, Brysiewicz P, Bruce J, Clarke D. Identification of risk factors for postoperative pulmonary complications in general surgery patients in a low-middle income country. PLoS One 2022 Oct 11;17(10):e0274749. PM: 36219615.
Nelson AJ, Harrington JL, Kolkailah AA, Pagidipati NJ, McGuire DK. Sodium-Glucose Cotransporter-2 Inhibitors: Impact on Atherosclerosis and Atherosclerotic Cardiovascular Disease Events. Heart Fail Clin 2022 Oct;18(4):597-607. PM: 36216489.
Peters AE, DeVore AD. Pharmacologic Therapy for Heart Failure with Preserved Ejection Fraction. Cardiol Clin 2022 Nov;40(4):473-489. PM: 36210132.
Pineda AM, Wang A. New Pacemaker Implantation After Alcohol Septal Ablation: How Sharp Is the Double-Edged Sword? JACC Cardiovasc Interv 2022 Oct 10;15(19):1918-1920. PM: 36202560.
Salah HM, Fudim M. Sodium-glucose Cotransporter 2 Inhibitors and Nonalcoholic Fatty Liver Disease. Heart Fail Clin 2022 Oct;18(4):625-634. PM: 36216491.
Salah HM, Fudim M. Tolerability and safety barriers to sodium-glucose cotransporter 2 inhibitor initiation in heart failure with reduced ejection fraction. Eur J Heart Fail 2022 Sep;24(9):1633-1635. PM: 35867845.
Salah HM, Levin AP, Fudim M. Device Therapy for Heart Failure with Preserved Ejection Fraction. Cardiol Clin 2022 Nov;40(4):507-515. PM: 36210134.
Senni M, Alemayehu WG, Sim D, Edelmann F, Butler J, Ezekowitz J, Hernandez AF, Lam CSP, O’Connor CM, Pieske B, Ponikowski P, Roessig L, Voors AA, Westerhout CM, McMullan C, Armstrong PW. Efficacy and safety of vericiguat in patients with heart failure with reduced ejection fraction treated with sacubitril/valsartan: insights from the VICTORIA trial. Eur J Heart Fail 2022 Sep;24(9):1614-1622. PM: 35791083.
Duke Heart Pulse 10-9-2022
Highlights of the week:
Duke Heart at HFSA 2022
Duke Heart had a great turnout at the 2022 Heart Failure Society of America (HFSA) Annual Scientific Meeting held Sept. 30- Oct. 3 at Gaylord National Harbor in Washington, DC.

Congratulations to all presenters, including Mike Felker with a LBCT presentation, “Effect Of Sacubitril/valsartan On Mitral Regurgitation In Heart Failure With Reduced Ejection Fraction: The PROVE-HF Study” and new faculty member Senthil Selvaraj with a LBCT presentation, “Blood Pressure, Dapagliflozin, And Cardiovascular Outcomes In Heart Failure With Preserved And Mildly Reduced Ejection Fraction: DELIVER,” which was simultaneously published in JACC HF.
Second year cardiology fellow Mark Kittipibul presented several poster sessions based on work he has done with Marat Fudim; there was an opportunity for Duke Heart team members to gather and mingle, and a JCF editorial board meeting to round things out.
Great job, everyone! Thanks to Rob Mentz and Karen Flores Rosario for photo submissions!






Duke Kannapolis Director Outlines Future at North Carolina Research Campus
Svati H. Shah, MD, MHS, spoke to partners at the North Carolina Research Campus (NCRC) about the pivotal role of Duke Kannapolis at the 350-acre translational science hub focused on human health and nutrition.
The Duke University School of Medicine has created in Duke Kannapolis a full-service research site that manages a wide variety of clinical and translational research projects to inform a deeper understanding of health and disease and to accelerate population health research.
“This is Duke’s investment in the NCRC,” Shah said Sept. 15 at the campus, located just north of Charlotte. “We embrace the mission of this unique scientific community working together collaboratively to empower human health through research, and we are extremely proud to be one of eight universities on the campus.”
Her talk marked the first time that Shah has presented to NCRC partners since being named to direct Duke Kannapolis.
Shah spoke about the history and capacity-building of Duke Kannapolis, part of the Duke Clinical and Translational Science Institute (CTSI). Founded in 2007 by Robert Califf, MD, MACC, now commissioner of the U.S. Food and Drug Administration, Duke Kannapolis has reached 22,339 total enrollments by 13,886 unique participants — and counting.
“Our community of engaged research participants are our most valuable asset, with many enrolling in multiple research projects,” Shah said.
Built on the foundational MURDOCK Study and Project Baseline Health Study, Duke Kannapolis has 58 funded research projects with 110 Duke faculty, as well as dozens of collaborations with investigators and institutions outside of Duke. Current areas of work include COVID-19, pain, mental health, smoking cessation, type 2 diabetes, cardiovascular disease, aging, chronic kidney disease, and more.
Shah welcomed new projects and collaborations with NCRC partners and encouraged attendees to explore the MURDOCK Study storefronts, which summarize data and samples at a glance for populations of interest. Duke Kannapolis has also streamlined access to biospecimens with a new biorepository transformation initiative, she said.
“We measure collaboration by relationships, and every project is an opportunity to strengthen these relationships through research,” Shah said.
Duke Kannapolis has developed a high level of community engagement by utilizing community advisory boards, marketing and communications, bilingual staff, events, and community partners including civic, church, and health organizations. Noting proven strategies for recruitment, retention, and engagement across diverse participant populations, Shah also attributed the success of Duke Kannapolis community engagement to bidirectional communication and 15 years of building trust with residents.
“We see participants as partners, and we prioritize personal connections with the community and open information flow to and from participants,” she said.
Shah thanked NCRC partners for warmly welcoming Duke University President Vincent Price recently during his first visit to the campus. Key takeaways from in-depth discussions with Price included the importance of success through collaboration and shared goals, as well as the need to address disparities impacting research, healthcare, workforce development, and more.
Shah defined her vision for the future of Duke Kannapolis as harnessing innovations in contemporary precision medicine integrated with implementation science, education, and clinical infrastructure to accelerate discovery and transform patient care.
“Ultimately, we want more precise diagnosis, prognosis, and therapeutic decision-making for the individual person,” Shah said. “And we are thrilled to work with this collaborative, interdisciplinary scientific community toward that end.”
Kudos to Ouyang & Huber, Gaca & 3100 team!
 We received accolades from a patient for a number of our providers on DUH Unit 3100 recently. Here is what they said:
We received accolades from a patient for a number of our providers on DUH Unit 3100 recently. Here is what they said:
“Duke is obviously known for the quality of health care received. During 3 major events over the last 2 years at Duke the most impressive learning is not just medical professionalism, but the genuine caring, respect, empathy, you feel from everyone at Duke; from the Valet, to Admit, Housekeeping, all Nurses and Techs, and Providers.
“A special mention to Dr. Gaca and his Surgical Team and the entire crew in the 3100 Section of the heart center. 5 RNs (Rosseli, October, Camyron, An Valery and Michelle) all deserve a special mention as well NPs Wendy and Jessica.” – A grateful patient (name withheld for privacy)
“Wendy and Jessica, thank you for all you do for the patients and your teamwork. You do awesome work which does not go unnoticed. We are so happy to have you as part of the Duke Heart Center.” — Diane Sauro, Director, Advanced Practice, Duke Heart Center.
“Thanks Wendy and Jessica for living the Duke values. We are fortunate to have you on the Duke team. Shout-out to Dr. Gaca, his team and all of 3100 for making sure our patients are getting the best care possible. Celebrate your awesomeness!” – Jill Engel, Service Line Vice President – Heart & Vascular.
Way to go, everyone!
Alumni News: Harrington Receives Stokes Medal
Interventional cardiologist Robert Harrington, current chairman of the Department of Medicine at Stanford and former director of the Duke Clinical Research Institute received the Irish Cardiac Society (ICS) Stokes Medal this week. Each year an individual who made outstanding contributions to the profession of cardiology and who has Irish connections is invited by ICS leadership to present to the membership body as the Stokes lecturer; they are then presented with the ICS Stokes Medal.
Congrats, Bob!


Pakistan Update
 We checked in again with Zainab Samad, chair of the Dept. of Medicine at Aga Khan University in Karachi about the situation in Pakistan.
We checked in again with Zainab Samad, chair of the Dept. of Medicine at Aga Khan University in Karachi about the situation in Pakistan.
“The crisis continues and it’s growing arms now. We have an outbreak of Dengue – it’s everywhere – my kids got Dengue two weeks ago – thankfully they are better but required admission and IV fluids/IV antipyretics. Large swathes of Sind are still underwater with the water lapping the sides of the road like an ocean. It will be a long road to recovery.”
The New Yorker published a piece by Mira Sethi this week that is worth checking out: Pakistan’s Unseen Climate-Change Survivors
If you are interested in helping – donations are being accepted by AKU. They are appreciative of any help. https://duke.is/b7xj7
Additional Reminders:
- It’s National Physician Assistant’s Week! October 6-12.
- Nominations are open for 2022-23 Duke Presidential Awards: https://duke.is/pambd. Deadline to nominate is Oct. 17!
- The DUHS annual flu vaccination campaign is underway and will continue until mid-November. Vaccination sites for faculty and staff can be found here: https://flu.duke.edu/vaccination/employees/
- On October 1, Duke Health launched our first comprehensive Team Member Referral Program. Team members at Duke University Health System and Duke University who refer qualified candidates for any posted clinical or non-clinical positions at https://careers.dukehealth.org/ may be eligible for a monetary bonus and prizes.
- Open Enrollment is October 17-28. This is your opportunity to review your medical, dental, vision, and reimbursement account benefit elections and make any changes necessary to ensure your choices continue to meet your needs. Watch your email and home mail delivery for more information.
Upcoming Events & Opportunities
Cardiology Grand Rounds
October 11: No CGR this week
CME & Other Events
October 14: Cardio-Oncology in the Era of Precision Medicine. Symposium to be held at the J.B. Duke Hotel, Durham, NC. Registration is open: https://bit.ly/CardioOnc22. Email Beth Tanner with questions: beth.tanner@duke.edu.
October 17-28: Open Enrollment period for 2023 for all Duke faculty and staff.
October 28: Duke Caregiver Community Event, in-person conference. Details here: https://duke.is/nzbcp.
November 4: 14th Annual NC Research Triangle Pulmonary Hypertension Symposium. 7 a.m.-4 p.m. This will be an in-person event at the Durham Convention Center. Registration required. To learn more and register, visit: https://duke.is/jag2b
November 14: Prostate Cancer & CVD Symposium, Webinar 4. Final of a four-part webinar series. Collaboration between the International Cardio-Oncology Society & Duke Heart. Noon, Eastern. Free. To register visit https://duke.is/ptjbs.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
September 30 — Jason Katz
Cardiology Magazine/ACC
Feature|The Future of Cardiology Critical Care: Interview With Jason Katz, MD
https://duke.is/9d488
October 2 — Jason Katz
Medpage Today
Growing Calls to Marry HF Specialists With Cardiac Critical Care
https://duke.is/2b4qq
October 3 — Joseph Turek
WFRV CBS-5/Green Bay
How a heart & thymus tissue transplant could change the procedure for children around the world
https://duke.is/2cx7u
October 3 — G. Michael Felker
Medscape
Optimized HF Meds May Lessen MR Severity, Perhaps Avoiding MV Repair
https://duke.is/n3gbt
October 3 — G. Michael Felker
Healio/Cardiology
Sacubitril/valsartan improves mitral regurgitation severity in certain patients with HFrEF
https://duke.is/pmmyn
October 4 — Marat Fudim
Newstribune.com (Jefferson City, MO))
Study: People hospitalized with COVID-19 may have higher heart failure risk
https://duke.is/4w4u3
October 4 — Tracy Wang
Heart.org
Heart risk factors, not heart disease itself, may increase odds of COVID-19 death
https://duke.is/2z3d4
October 4 — Pamela Douglas
DAIC/dicardiology.com
https://duke.is/gs9aw
October 4 — Nikki Pelot (Biomedical Engineering)
Cleveland.com
https://duke.is/685g2
October 5 — Svati Shah
Independent Tribune
Duke Kannapolis director outlines future at North Carolina Research Campus
https://duke.is/ncb8j
October 5 — Joseph Turek and the Sinnamon family
WQAD (Moline, IL)
First-ever heart transplant and thymus implant gives toddler a new chance at life
https://duke.is/br3bp
Duke Heart Pulse October 2nd 2022
Highlights of the week:
Rymer Honored with Linnemeier Young Investigator Award at TCT2022

Jennifer Rymer, MD, MBA, MHS, the John Bush Simpson assistant professor of medicine, was honored at this year’s Transcatheter Cardiovascular Therapeutics (TCT) Conference as the recipient of the Thomas J. Linnemeier “Spirit of Interventional Cardiology” Young Investigator Award.
The award was announced Sept. 19 in Boston at TCT which was held in conjunction with the Cardiovascular Research Foundation (CRF). The award was presented by CRF leader Gary S. Mintz, MD, and David J. Cohen, MD, MSc, St. Francis Hospital, and CRF Director of Clinical and Outcomes Research.
“I am deeply honored,” said Rymer after the award ceremony. “The other  finalists are so accomplished, and I am so honored to be considered for this award. I want to thank all of my mentors at Duke, Dr. Mehran, and also ‘Women as One’. I would not be here had it not been for those folks who have believed in me forever. I really appreciate them and all of their guidance and mentorship over the years.”
finalists are so accomplished, and I am so honored to be considered for this award. I want to thank all of my mentors at Duke, Dr. Mehran, and also ‘Women as One’. I would not be here had it not been for those folks who have believed in me forever. I really appreciate them and all of their guidance and mentorship over the years.”
“What a thrilling moment to see Dr. Jennifer Rymer receive the TCT 2022 Young Investigator Award,” said Roxana Mehran, MD, TCT course co-director and professor of medicine at Icahn School of Medicine at Mount Sinai, New York.
“There is no one more deserving than Dr. Rymer for all of her relentless work in diversity, inclusion and mentorship,” said Mehran. “She is a dynamo, and someone to look out for, as she has already risen as a star, and is sure to shine for many, many more years.”
The presenters summarized the award’s history and significance, and recognized the other finalists who were considered for the award: Eric Alexander Secemsky, MD, MSc, who serves as the primary vascular interventionalist at Beth Israel Deaconess Medical Center in Boston, MA; and Janarthanan Sathananthan, MBChB, MPH, a clinical interventional cardiologist at St. Paul’s Hospital and Vancouver General Hospital in Vancouver, Canada.
Mintz acknowledged past winners of the award, saying “It is simply an outstanding group of investigators, almost all who are now faculty at TCT.”
Rymer has published 70 peer-reviewed publications, 41 as first author. She is an early career academic interventional cardiologist who performs complex coronary and peripheral vascular procedures with a research focus in acute coronary syndromes and patients with severe claudication and chronic limb-threatening ischemia. Further, she performs intravascular imaging for every PCI.
“Competition was stiff, as all of the finalists are incredibly deserving, and it was a very difficult decision,” added Cohen.
Way to go, Jenn! Well deserved!
Keenan Joins Duke Heart’s Cardiothoracic Faculty
 The Division of Cardiovascular and Thoracic Surgery announced this week that Dr. Jeffrey E. Keenan will join their faculty effective October 10, 2022.
The Division of Cardiovascular and Thoracic Surgery announced this week that Dr. Jeffrey E. Keenan will join their faculty effective October 10, 2022.
Keenan graduated from the University of Maryland School of Medicine in 2011 where he was elected to the AOA medical honor society. He then matriculated to the surgery residency program at Duke. He graduated from the general surgery program in 2018 and achieved certification from the American Board of Surgery in 2019. He completed subspecialty training in cardiothoracic surgery in 2020.
During his training at Duke, Keenan spent two years supported by an NIH F32 National Research Service Award in order to investigate mitochondrial function and oxidative stress in the failing heart.
After completing his training at Duke in 2020, Keenan joined the faculty at the University of Washington in Seattle. He achieved certification from the American Board of Thoracic Surgery in 2021.
Keenan practices as an adult cardiac surgeon with a subspecialty focus in heart transplantation and mechanical circulatory support. He will return to Duke as an assistant professor of surgery in the Department of Surgery, Division of Cardiovascular and Thoracic Surgery. Keenan aims to build a translational research program centered around the optimization of organ preservation and early allograft function in heart transplantation as well as innovating strategies to improve the surgical care of advanced heart failure and cardiogenic shock patients.
We are very pleased he is coming back to Duke! Jeff and his wife, Allison have four children — Quinn, who is seven, and Emerson, Louis, and Norah, their four-year-old triplets. All are excited to once again make Durham their hometown. Please join us in welcoming Jeff and his family back to Duke!
Three Slots Remaining! Photography Fundraiser to Support Heart Walk
Stephanie Barnes is offering family photography sessions as part of a Duke Heart fundraiser in  support of the American Heart Association’s Triangle Heart Walk and Team Got Heart!. We have three openings available for Sunday, Oct. 16. Don’t miss out!
support of the American Heart Association’s Triangle Heart Walk and Team Got Heart!. We have three openings available for Sunday, Oct. 16. Don’t miss out!
Location is Fearrington Village in Chapel Hill. Sessions are 15 minutes. Cost is $150, all of which goes to our fundraiser. Registration is required.
This is a great opportunity to get your holiday family photos done ahead of Thanksgiving. Can be couples, just your kids, small families of 2-4, maybe even have your pets with you! You will receive full access and rights to all of your digital photos via a private web portal. Expect about 20 photos total.
Sign up here: https://www.signupgenius.com/go/409054DA9A623A2F49-photography1
If you have questions, please send an email to: Got Heart Fundraiser/Photoshoot.


Nursing Open House Held
We had a great turnout for our Duke Heart RN Recruitment Open House on Thursday, Sept. 29. Our nursing teams did an outstanding job of hosting nearly 50 interested applicants. We had several dozen nurses who were unable to attend in person but who expressed interest in learning more.
We are grateful to all who contributed their time and energy for unit tours, shadowing experiences, networking and interviewing – and in publicizing our event. Thank you to all who stopped by to meet nurses who are interested in joining the Duke Heart team. Your support is part of what makes this a great place to work!

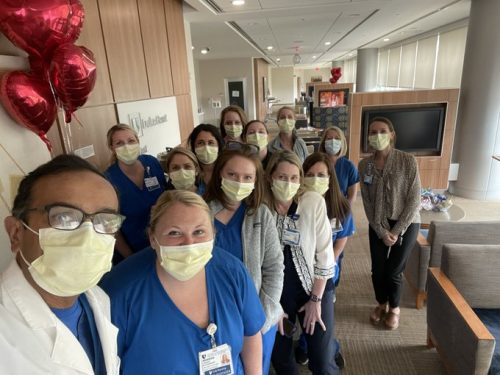

ICYMI: DHIP Town Hall
The latest Duke Health Integrated Practice Town Hall was held on Wednesday, Sept. 28. We appreciate the 400+ team members who joined us online! Leadership provided an update on the progress to date, shared the list of Strategic & Operational Transition Committee members, reviewed benefits changes for those most impacted by the change, and answered questions our team members submitted ahead of the session. You can find the recording here on Warpwire: https://duke.is/gqy7e
You can find the most up-to-date information on the DHIP site: https://dhip.org. In the coming weeks, updates on the work of each Strategic & Operational Transition Committee will also be posted there. Please consider joining any of the Strategic & Operational Transition Committee as a Participant to receive updates directly in your inbox; this is also the best way to provide input to the Committee.
If you have any questions, please email DHIP@duke.edu.
Thank you for your engagement and feedback as we build a Duke Health Integrated Practice that is prepared to welcome everyone.
New Leadership Development Opportunity via Duke AHEAD
Duke AHEAD has announced a new leadership development opportunity for emerging health professions education leaders: Leadership Onboarding for Educators Accelerator Program (LEAP). This program is designed for faculty members who are leading education programs, courses, or curriculum. LEAP is a 3 month on-boarding program and includes topics such as:
- Negotiation
- Budget management
- Leading or teaching a multigenerational group
- Developing a strategic plan for your program
- Managing difficult situations and conversations
- Promoting yourself and your ideas with competent humility
- Networking at Duke
- Promoting DEI in teaching, hiring, and communication
The inaugural program will be limited to 20 participants. You may self-nominate on the application form link below; a letter of support is required from your direct report.
All sessions will be virtual, and will be held from 4:00 -6:00 pm.
The six sessions are scheduled on Thursdays (1/26/23, 2/9/23, 3/9/23, 3/23/23, 4/13/23, and 4/27/23).
There is NO charge for the program, but applicants should commit to attending all sessions.
This leadership onboarding complements other leadership opportunities noted throughout Duke. Many clinical departments also offer leadership training; LEAP is geared toward those faculty who will be teaching learners or developing programming for learners in clinical or research settings. For a list of other leadership development opportunities around Duke, please visit here:
Application Deadline is November 2.
APPLY NOW via Qualtrics: https://duke.is/6hg8g.
Additional questions? Please reach out to mailto:dukeahead@duke.edu.
Additional Reminders:
- Nominations are open for 2022-23 Duke Presidential Awards: https://duke.is/pambd.
- The DUHS annual flu vaccination campaign is underway and will continue until mid-November. Vaccination sites for faculty and staff can be found here: https://flu.duke.edu/vaccination/employees/
- On October 1, Duke Health launched our first comprehensive Team Member Referral Program. Team members at Duke University Health System and Duke University who refer qualified candidates for any posted clinical or non-clinical positions at https://careers.dukehealth.org/ may be eligible for a monetary bonus and prizes.
- Open Enrollment is October 17-28. This is your opportunity to review your medical, dental, vision, and reimbursement account benefit elections and make any changes necessary to ensure your choices continue to meet your needs. Watch your email and home mail delivery for more information.
Upcoming Events & Opportunities
Cardiology Grand Rounds
October 4: Transcatheter Tricuspid Therapy with Paul Sorajja of the Minneapolis Heart Institute Foundation and Abbott Northwestern Hospital, Allina Health Minneapolis Heart Institute, Minneapolis. 7 a.m., Webex and in person (Duke North 2003)
CME & Other Events
October 14: Cardio-Oncology in the Era of Precision Medicine. Symposium to be held at the J.B. Duke Hotel, Durham, NC. Registration is open: https://bit.ly/CardioOnc22. Email Beth Tanner with questions: beth.tanner@duke.edu.
October 17-28: Open Enrollment period for 2023 for all Duke faculty and staff.
October 28: Duke Caregiver Community Event, in-person conference. Details here: https://duke.is/nzbcp.
November 4: 14th Annual NC Research Triangle Pulmonary Hypertension Symposium. 7 a.m.-4 p.m. This will be an in-person event at the Durham Convention Center. Registration required. To learn more and register, visit: https://duke.is/jag2b
November 14: Prostate Cancer & CVD Symposium, Webinar 4. Final of a four-part webinar series. Collaboration between the International Cardio-Oncology Society & Duke Heart. Noon, Eastern. Free. To register visit https://duke.is/ptjbs.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
September 23 — Marat Fudim
News & Observer
People hospitalized with COVID-19 may have higher heart failure risk, Duke study says
https://duke.is/mpnnp
September 23 — Marat Fudim
WPTF 680 AM
Some COVID patients at increased risk for heart failure
https://duke.is/6bh5c
(*clip begins @ 15:52:59)
September 23 — Derek Chew
tctMD
Most Patient-Reported Outcome Measures in CVD Fall Short
https://duke.is/pg4zg
September 26 — Marat Fudim
South China Morning Post
People hospitalised with Covid-19 may have higher heart failure risk: study
https://duke.is/4kgn8
September 29 — John Alexander
Medscape
PROACT Xa Trial of Apixaban With On-X Heart Valve Stopped
https://duke.is/8gh6h
September 29 — Jonathan Piccini
Medscape/The Bob Harrington Show
Do Older vs Younger Docs Treat Atrial Fibrillation Differently?
https://duke.is/2kxz9
September 27 — Tony Gutierrez
Univision
Septiembre es el mes de la concienciación sobre la arteriopatía periférica
https://duke.is/rc4xz
Recent Comments