Home » 2023 (Page 5)
Yearly Archives: 2023
Duke Heart week ending February 26th 2023
Highlights of the week:
Wrapping Up Heart Month
Thanks to everyone who helped celebrate Heart Month by spreading awareness about heart disease, how to prevent it, and how to successfully manage it! Thanks especially to each and every team member for all you are doing as a contributor to the great work being done throughout Duke Heart!
 This past week, on Tuesday, Feb. 21, Nishant Shah, MD, presented on a topic he’s passionate about — heart disease prevention. He’s a believer in getting these messages out at critical times and what better time than in the early learning years? Shah had a fully engaged and captivated audience of children at All Starz Children’s Academy in Cary. He dressed in scrubs and his white lab coat for presentations throughout the day to about 166 preschoolers about how the heart works and how to live a heart-healthy lifestyle.
This past week, on Tuesday, Feb. 21, Nishant Shah, MD, presented on a topic he’s passionate about — heart disease prevention. He’s a believer in getting these messages out at critical times and what better time than in the early learning years? Shah had a fully engaged and captivated audience of children at All Starz Children’s Academy in Cary. He dressed in scrubs and his white lab coat for presentations throughout the day to about 166 preschoolers about how the heart works and how to live a heart-healthy lifestyle.
“We went through pictures of heart anatomy, talked about important fruits and vegetables to keep the heart healthy, did some stretches and exercise, and learned about the importance of a good night’s sleep for heart health,” said Shah. “In the afternoon the kids got to do some coloring of a picture of real human heart as well. It certainly is never too early to talk about cardiovascular disease prevention and Heart Month is a great time to kick off the conversation! Primordial prevention for the win!”
Shah brought stethoscopes and disposable surgical caps with him so that not only could the kids “dress up” by wearing the bonnets, they could listen to their own heartbeat.
“They loved it and it was great to see the excitement on their faces,” Shah added.
Melissa Brown, a director at All Starz Academy concurred.
“When Dr. Shah mentioned that February was Heart Month and that he was interested in presenting to our kids, we thought it  was a fantastic idea,” she said. “It was a huge hit. Dr. Shah did a great job balancing information with activity — he had them dress up with surgical caps, and they did some physical activities like jumping jacks. His presentation was very well designed for the ages of kids we have here. The younger ones, of course, their attention span is less but they still enjoyed it. We’d repeat this again in years to come, just because it was such a big hit with them.”
was a fantastic idea,” she said. “It was a huge hit. Dr. Shah did a great job balancing information with activity — he had them dress up with surgical caps, and they did some physical activities like jumping jacks. His presentation was very well designed for the ages of kids we have here. The younger ones, of course, their attention span is less but they still enjoyed it. We’d repeat this again in years to come, just because it was such a big hit with them.”
Brown said the enthusiasm lasted all week long. “From what I’ve overheard the kids talking about, I think the biggest thing they took away is excitement about healthy eating and how it makes the heart grow big and strong — and that when the heart is big and strong, you’re a healthier human. They picked up important information about how to keep their bodies healthy. I heard our kids saying things like, ‘if I eat these my heart is going to get big and strong’ and also ‘things like this are not good for me to eat.’ They definitely were paying attention!”
The Academy has typically had professional police officers, firefighters, and dentists come in to see the kids and do demonstrations – but never a cardiologist. Brown said they were thrilled to showcase Heart Month this way and would welcome further opportunities.
Way to go, Nishant! Here are some great photos from his day at All Starz Children’s Academy.

On Wednesday evening, Manesh Patel was the invited presenter by the Triangle American Heart Association to give a “Deep Dive” on the major science news that came out of the 2022 AHA Scientific Sessions, which allowed him to also discuss some important research our Duke Heart team is working on. The Zoom session was held by our local AHA for their Board members. Also invited to participate were members of our Heart Center Leadership Council and members of our Patient & Family Advisory Council. The presentation was followed by a number of great questions from the audience!

Concluding the week, we received a terrific annual recap of the many successes of our Duke Electrophysiology team from Jonathan Piccini, MD, including these stats:
For calendar year 2022, the Duke EP Team performed:
- 6644 in-person device interrogations
- 5% increase from 2021
- 18,761 remote device interrogations
- 13% increase from 2021
- 1233 device implants at Duke University Hospital
- 12% increase from 2021
- 1192 EP study/ablation procedures at Duke University Hospital
- 11% increase from 2021
- 749 AF ablations in the Duke University Health System
- 12% increase from 2021
- 44 left atrial appendage closure procedures at Duke University Hospital
- 150+ lead extraction procedures at Duke University Hospital
- >10% increase from 2021
Incredible numbers from a stellar team! We look forward to sharing many more of their accomplishments!
Newly Published Book Features Chapter by Duke APPs
Three of our APPs are co-authors of chapters in the newly published Textbook for the Adult-Gerontology Acute Care Nurse Practitioner (published by Springer Publishing). Stephanie Barnes, Callie Tennyson, and Jaime McDermott wrote the chapters on Acute Coronary Syndromes and Heart Failure.



“Nearly 100 expert authors who discuss the evidence-based gold standards for diagnostics and tests for optimal detection of multisystem disorders, patient management, and transitions of care. In these chapters, learners will gain a greater understanding of the etiology and pathophysiology of acute and critical illnesses, and the latest in advanced pharmacologic and nonpharmacologic therapies… We congratulate the Editors and chapter authors for their efforts in developing a clearly outlined and accurate text for AGACNP use—truly the first of its kind.”
We love that the expertise of our Duke Heart nurse practitioners is highly sought after! Congratulations, Steph, Callie and Jaime!!!
ICYMI: Thomas Featured in Klotman’s Friday Message
 Cardiac Electrophysiologist Kevin Thomas, MD, vice dean for Equity, Diversity and Inclusion and Chief Diversity Officer was interviewed recently by Duke School of Medicine Dean Mary Klotman, MD for one of her weekly Friday messages (Feb. 10, 2023) — this one in celebration of Black History Month. It’s definitely worth checking out! https://duke.is/wd5x5
Cardiac Electrophysiologist Kevin Thomas, MD, vice dean for Equity, Diversity and Inclusion and Chief Diversity Officer was interviewed recently by Duke School of Medicine Dean Mary Klotman, MD for one of her weekly Friday messages (Feb. 10, 2023) — this one in celebration of Black History Month. It’s definitely worth checking out! https://duke.is/wd5x5
Partial Heart Transplant Featured in ABC Drama
One of the storylines in Thursday night’s episode of Grey’s Anatomy (9 p.m., ABC) featured a partial heart transplant. The only two such procedures completed to date have both taken place at Duke University Hospital. The procedure was pioneered at Duke by pediatric cardiothoracic surgeon Dr. Joseph Turek and his team. The writers and producers of Grey’s Anatomy reached out to Dr. Turek for his input in order to assure medical accuracy in their script as well as the imagery they planned to use.
Cool work, Joe!


Kudos to All Cardiology Fellows
A tremendous shout-out to each one of our cardiology fellows for their understanding, patience and compassion this week after a bit of a snafu with the paging system. One of the nurses in the Duke Birthing Center accidently paged the entire team instead of the fellow on-call, and to her great surprise, everyone reacted with kindness. (We are not surprise by this, of course!)
In a note she sent to Toi Spates and shared with Cary Ward, she wrote:
“First, I would like to say that each interaction I have had with you, Toi, has been incredibly professional, polite, and educational. Your team has shown incredible respect towards our triage nursing team, and we do appreciate that. Your patience does not go unnoticed.
Today, we received a call from the clinic alerting us that they were sending a patient who was very concerning to them. We never know how concerned we should be until we see that patient in person. [In preparing for a consult,] I mistakenly sent out a page to the wrong group. When I realized what I had done, my heart sank, and the phone started ringing. I held my breath to prepare to apologize and take the heat, but it never came. Every single provider who returned my page, (within five minutes or less) was kind, understanding, and half of them even offered to help me! Some offered to help me find the correct pager number, others asked who I specifically was looking for, and another asked for the MRN in order to be prepared to assist us in the event that no one was available. I could not answer the phone fast enough. With each call, I waited for the reprimand that never came. I wanted to provide a BIG THANK YOU! Also, I am so pleasantly surprised by how I was treated today.” – a grateful nurse
What a great reminder that kindness is always welcome and that you can always, always make someone’s day better as a result. GREAT JOB!!
Kudos to Osude!
In a note from Fawaz Alenezi, MD to Anna Lisa Chamis, MD this week, we received a great shout-out for Dr. Kiki Osude!  Photo
Photo
“Kiki made my day very easy. We had 10 TEEs and 2 CVs. I really appreciate her professional work.” — Fawaz
Shout-out to Loriaux!
We received some nice feedback this week on Dan Loriaux via messages Anna Lisa Chamis  received from both the Neuro ICU AND from the SICU. (photo)
received from both the Neuro ICU AND from the SICU. (photo)
In an email from Shreyansh Shah, MD, of the Neuro ICU, we heard “This week as we celebrate contributions of our GME trainees to patient care, education and research, I wanted to share this special kudos from the Neuro ICU team for a very impressive Critical Care fellow, Dr. Daniel Loriaux who our team got to work with this past month.
Over the last month, Daniel has received multiple kudos from his team members, Neuro ICU nursing staff, and patient’s family members for his kind demeanor, his patient-centric care, his collaborative nature, and for creating an environment of trust during his time in the Neuro ICU. It has been an absolute pleasure to work with him and we wish him all the best!”
And, “I had the pleasure of working with Dan Loriaux this past week in the SICU. I was impressed with his knowledge base, kindness, compassion, and procedural skills. He was constantly wanting to learn more throughout the week, was always happy to teach residents and APPs, and has some of the better ultrasound/procedural skills I’ve seen from any fellow I’ve worked with at Duke. More importantly, he seems like a good person and listened closely to all team members whenever concerns were expressed. He has a rare combination of humbleness and skill. Happy to speak to either of you more to help facilitate this young man’s career however I can.” — Nitin Mehdiratta, MD, critical care anesthesiologist and medical director of the Duke SICU.
Heading to NOLA for ACC.23?
Will you be attending the 2023 ACC Scientific Sessions in New Orleans next weekend? Please join us at the Duke Annual Reception & Duke vs. UNC MBB Watch Party.

When: Saturday, March 4 from 5:30 – 8:30 p.m.
Where: New Orleans Marriott/Warehouse Arts District
Sponsors: Duke Clinical Research Institute, Duke Cardiology, and Duke Heart Center
Questions: email Elizabeth.evans@duke.edu or willette.wilkins@duke.edu.
Dean’s Distinguished Research Series 2023
The Duke University School of Medicine’s Dean’s Distinguished Research Series showcases groundbreaking research from the basic, clinical, and translational sciences. Formerly called “Research Week”, the re-imagined series will be held in-person and live-streamed. All faculty, staff, trainees and students are welcome to attend.

March 9:
Trainee Poster Session, 2:30 – 4 p.m., 6th Floor, Trent Semans Center for Health Education
Faculty Lectures, 4 – 5 p.m., 6th Floor, Trent Semans Center for Health Education.
Chris Beyrer, MD, MPH, director of Duke Global Health Institute, and Keisha Bentley-Edwards, PhD, associate director of research, Samuel DuBois Cook Center on Social Equity will present. Light bites and refreshments provided on a first-come, first-served basis. (live stream available: https://duke.is/vgf7u)
For the full schedule, please visit https://medschool.duke.edu/research/deans-distinguished-research-series-2023.
Reminder: Future Relocation of DUH Unit 7100 for Renovations
As most of you know, Duke University Hospital’s bed tower 100 is in the process of being renovated. Unit 7100 will be relocated to Duke North 2200 (a 16-bed unit) and 3200 (also a 16-bed unit) in April.
These units were selected for their close proximity to one another and to other Heart units; the provision of 32 beds for Cardiology patients; and, for being move-in ready after recent renovations. 7201-7208 will close as the Hospital Surge Unit, and the eight Emergency Department admit hold patients will relocate from 2200 to this area.
The exact dates for closing 7201-7208 and relocating 7100 will be communicated once we have firm dates identified. There will be no change in the patient population we will care for on units 2200/3200.
DHIP update
Distribution of Employment Agreements for transitioning members is ongoing. Please monitor your inbox for critical communication from DHIP@duke.edu, your department chair, and Adobe Sign.
Reminder: The Duke Guarantee offers the minimum compensation each Member can expect to receive. Additional compensation opportunities which exist today will continue to be available to members within DHIP.
All members will be given weeks to consider employment and sign their Employment Agreements.
Benefits:
- Information regarding Duke Benefits is available on SharePoint.
- All benefits related questions can be sent to DHIPBenefits@Duke.edu.
All other questions can be sent to DHIP@duke.edu, and all DHIP updates can be found at https://dhip.org.
Upcoming Events & Opportunities
Cardiology Grand Rounds
Feb. 28: Percutaneous Mechanical Circulatory Support in High Risk PCI and Shock: Fact, Fiction, and Future Devices with Sandeep Nathan of Univ. of Chicago Medicine. 5 p.m., Zoom; also: in person, DN 2002.
March 14: Topic TBA with Italo Biaggioni of Vanderbilt University Medical Center. 5 p.m., Zoom.
DCRI Research Forum: Feb. 28
The Duke Clinical Research Institute’s upcoming Research Forum will feature a fireside chat with Journal of the American Medical Association (JAMA) Editor-In-Chief Dr. Kirsten Bibbins-Domingo.
What: A Fireside Chat with JAMA Editor-in-Chief Kirsten Bibbins-Domingo, PhD, MD, MAS
When: Tuesday, Feb. 28 from 12 p.m.-1 p.m.
(Required) Register: https://duke.is/y45qv
Webinar details and link will be provided upon registration.
Duke REACH Equity Center Funding Opportunities:
Research Voucher, Scholars Development, Transdisciplinary Think Tank
Now accepting applications through March 17 for July 2023 funding.
The Duke REACH Equity Center awards support students, trainees, and faculty who are interested in conducting research that promotes health equity. All proposals should broadly address the REACH Equity theme: to reduce racial and ethnic disparities in health by improving the quality of patient-centered care in the clinical encounter across diseases, stages of illness, care settings, and throughout the life course. Proposals may include any research topic and method (quantitative, qualitative, etc.).
There are four funding opportunities:
The Research Vouchers Program will supplement currently funded research or support standalone research projects conducted by faculty at any level. Funding: One year, up to $12,500 per award.
- Full Research Vouchers Program RFA and application instructions are available here.
- Current awardee list is available here.
The Research Scholars Development Program is intended to support early-stage investigators (residents, fellows, postdoctoral students, nursing trainees, and other trainees at a similar career stage). Scholars work with a faculty mentor (identified by the trainee) to develop a research proposal and complete a project. Funding: Up to $5,000 for one- or two-year project per award.
- Full Research Scholars Development RFA and application instructions are available here.
- Current awardee list is available here.
The Transdisciplinary Think Tank (TTT) provides support to bring together faculty across disciplines who have a common interest in addressing racial and ethnic disparities in the clinical encounter. The TTT’s aim is to catalyze and support research related to the REACH Equity theme and to foster collaboration among health disparities researchers across Duke University. Funding: One year, up to $1,500 per award.
- The Full Transdisciplinary Think Tank RFA and application instructions are available here.
- Current awardee list is available here.
The Medical Student and Nursing Student Research Award is intended to support a third-year medical student or a third-year PhD nursing student conducting research related to the REACH Equity theme. Scholars work with a faculty mentor (identified by the student) to develop a research proposal and complete a project. Funding: Up to $5,000 for one-year project.
- Full Medical Student Research and Nursing Student Research Award and application instructions are available here.
- Current awardee list is available here.
Application submission deadline: March 17 for July 2023 funding.
Email reachequitycenter@duke.edu with questions.
Save the Date: Spring Faculty Reception
All Duke SOM faculty members are invited to the 2023 School of Medicine Spring Faculty Celebration scheduled for Wednesday, May 17, 5:00-7:30 p.m. at the Doris Duke Center, Duke Gardens. This event is a wonderful opportunity to network, celebrate achievements, and recognize colleagues with faculty awards. Refreshments will be served. Link to RSVP is below.
Feel free to invite your SOM faculty colleagues to attend with you or to make plans to come as a group and celebrate the end of the academic year together.
Tentative Agenda:
5:00 – 6:00 p.m. — Networking reception with heavy hors d’oeuvres
6:00 – 6:15 p.m. — Opening Remarks
6:15 – 7:00 p.m. — School of Medicine Faculty Awards and Recognitions
7:00 – 7:30 p.m. — Reception and Dessert
The Office of Faculty is looking forward to seeing you there! If you have any questions about the event, please do not hesitate to contact their team: facdev@dm.duke.edu.
To RSVP: https://duke.is/cyp46
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
February 18 — Stuart Russell
WPTF AM 640
Aging Matters: Raising Awareness of heart issues
https://duke.is/8teb6
*clip begins @16:06:31
February 20 — Jacob Schroder with Jason Banner, patient
WPTF AM-640/CBS News Weekend Round-up*
Medical breakthrough gives father more time with his kids
https://duke.is/9v2yn
*clip begins @ 00:31:26
February 20 — Jacob Schroder with Jason Banner, patient
KCAL CBS News Los Angeles*
Medical Breakthrough allows some patients to get a new heart
https://duke.is/4czbt
*clip begins @ 09:50:56
February 20 — William Kraus
The Washington Post/Bloomberg
Cut Calories and (Maybe) Add Years to Your Life
https://duke.is/j3c6a
February 21 — Stephen Greene
HCP Live
Rural Hospitals Less Likely than Urban Hospitals to Prescribe GDMT in Heart Failure
https://duke.is/babu3
February 23 — Stephen Greene and Jacob Pierce (IM Resident)
tctMD
Too Many HF Patients Exiting Rural Hospitals Miss Out on Endorsed Therapies
https://duke.is/pu5qf
February 23 — Duke SOM
Becker’s Healthcare/ASC Review
Most diverse medical schools in 2023
https://duke.is/r8ewx
February 23 — Michael Pencina
STAT News
AI developers battle with FDA, what’s next with Amazon and One Medical, & protecting wearables data
https://duke.is/5yb56
February 23 — Duke Clinical Research Institute
Salisbury (NC) Post
Automated CPR machine gets to the heart of survival
https://duke.is/nhexs
February 23 — Pamela Douglas
DAIC
ACC Global Survey Finds 1 in 4 Cardiologists Reporting Mental Health Conditions
https://duke.is/yqejq
Division of Cardiology Publications Indexed in PubMed February 2-22, 2023
Altin SE, Parikh PB, Squeri E, Douglas PS, Wang DD, Mehran R. Representation of Women in Cardiology Academic Faculty Ranks. Am J Cardiol 2023;190:96-97. PM: 36608436.
Carnicelli AP, Keane R, Brown KM, Loriaux DB, Kendsersky P, Alviar CL, Arps K, Berg DD, Bohula EA, Burke JA, Dixson JA, Gerber DA, Goldfarb M, Granger CB, Guo J, Harrison RW, Kontos M, Lawler PR, Miller PE, Nativi-Nicolau J, Newby LK, Racharla L, Roswell RO, Shah KS, Sinha SS, Solomon MA, Teuteberg J, Wong G, van Diepen S, Katz JN, Morrow DA. Characteristics, therapies, and outcomes of In-Hospital vs Out-of-Hospital cardiac arrest in patients presenting to cardiac intensive care units: From the critical care Cardiology trials network (CCCTN). Resuscitation 2023;183:109664. PM: 36521683.
Gaudino M, Alexander J, Benedetto U, Boening A, Dimagli A, Fremes S, Chikwe J, Girardi L, Hare D, Kurlansky P, Lamy A, Audisio K, Di Franco A, Devereaux PJ, Diegeler A, Flather M, Lawton JS, Tam DY, Reents W, Rahouma M. Omnia munda mundis (‘to the pure, all things are pure’). Eur J Cardiothorac Surg 2023;63(2):ezad021. PM: 36651674.
Hertz JT, Prattipati S, Kweka GL, Mlangi JJ, Tarimo TG, Mmbaga BT, Thielman NM, Sakita FM, Rubach MP, Bloomfield GS, Manavalan P. Prevalence and predictors of uncontrolled hypertension, diabetes, and obesity among adults with HIV in northern Tanzania. Glob Public Health 2022;17(12):3747- 3759. PM: 35282776.
Khan MS, Shahid I, Greene SJ, Mentz RJ, DeVore AD, Butler J. Mechanisms of current therapeutic strategies for heart failure: more questions than answers? Cardiovasc Res 2023;118(18):3467-3481. PM: 36536991.
Kosiborod MN, Bhatt AS, Claggett BL, Vaduganathan M, Kulac IJ, Lam CSP, Hernandez AF, Martinez FA, Inzucchi SE, Shah SJ, de Boer RA, Jhund PS, Desai AS, Fang JC, Han Y, Comin-Colet J, Vardeny O, Lindholm D, Wilderäng U, Bengtsson O, McMurray JJV, Solomon SD. Effect of Dapagliflozin on Health Status in Patients With Preserved or Mildly Reduced Ejection Fraction. J Am Coll Cardiol 2023;81(5):460-473. PM: 36526515.
Otvos JD, Shalaurova I, May HT, Muhlestein JB, Wilkins JT, McGarrah RW, Kraus WE. Multimarkers of metabolic malnutrition and inflammation and their association with mortality risk in cardiac catheterisation patients: a prospective, longitudinal, observational, cohort study. Lancet Healthy Longev 2023;4(2):e72- e82. PM: 36738747.
Parker DC, Kraus WE, Whitson HE, Kraus VB, Smith PJ, Cohen HJ, Pieper CF, Faldowski RA, Hall KS, Huebner JL, Ilkayeva OR, Bain JR, Newby LK, Huffman KM. Tryptophan Metabolism and Neurodegeneration: Longitudinal Associations of Kynurenine Pathway Metabolites with Cognitive Performance and Plasma Alzheimer’s Disease and Related Dementias Biomarkers in the Duke Physical Performance Across the LifeSpan Study. J Alzheimers Dis 2023;91(3):1141-1150. PM: 36565121.
Peters AE, Tromp J, Shah SJ, Lam CSP, Lewis GD, Borlaug BA, Sharma K, Pandey A, Sweitzer NK, Kitzman DW, Mentz RJ. Phenomapping in heart failure with preserved ejection fraction: insights, limitations, and future directions. Cardiovasc Res 2023;118(18):3403-3415. PM: 36448685.
Wang PJ, Lu Y, Mahaffey KW, Lin A, Morin DP, Sears SF, Chung MK, Russo AM, Lin B, Piccini J, Hills MT, Berube C, Pundi K, Baykaner T, Garay G, Lhamo K, Rice E, Pourshams IA, Shah R, Newswanger P, DeSutter K, Nunes JC, Albert MA, Schulman KA, Heidenreich PA, Bunch TJ, Sanders LM, Turakhia M, Verghese A, Stafford RS. Randomized Clinical Trial to Evaluate an Atrial Fibrillation Stroke Prevention Shared Decision-Making Pathway. J Am Heart Assoc 2023;12(3):e028562. PM: 36342828.
Zeitler EP, Li Y, Silverstein AP, Russo AM, Poole JE, Daniels MR, Al-Khalidi HR, Lee KL, Bahnson TD, Anstrom KJ, Packer DL, Mark DB. Effects of Ablation Versus Drug Therapy on Quality of Life by Sex in Atrial Fibrillation: Results From the CABANA Trial. J Am Heart Assoc 2023;12(3):e027871. PM: 36688367.
Badhwar V, Chikwe J, Gillinov AM, Vemulapalli S, O’Gara PT, Mehaffey JH, Wyler von Ballmoos M, Bowdish ME, Gray EL, O’Brien SM, Thourani VH, Shahian DM, Habib RH. Risk of Surgical Mitral Valve Repair for Primary Mitral Regurgitation. J Am Coll Cardiol 2023;81(7):636-648. PM: 36669958.
Coles TM, Lin L, Weinfurt K, Reeve BB, Spertus JA, Mentz RJ, Piña IL, Bocell FD, Tarver ME, Henke DM, Saha A, Caldwell B, Spring S. Do PRO Measures Function the Same Way for all Individuals With Heart Failure? J Card Fail 2023;29(2):210-216. PM: 35691480.
DeFilippis EM, Mentz RJ, Lala A. Lifting and Healing as We Climb: Women’s Heart Month. J Card Fail 2023;29(2):121-123. PM: 36797008.
Joyce E, McIllvennan CK, Esquivel JH, Sauer AJ, Correa A, Blumer V, Youmans QR, Alvarez-Garcia J, Chang H, Overbey J, Deych E, Sinha SS, Morris A, Defilippis EM, Reza N, Code J, Hajduczok AG, Fudim M, Rollins B, Vader JM, Pina IL, Teuteberg J, Zieroth S, Starling RC, Gulati M, Mentz RJ, Lala A. Participating in the Peer Review Process: The Journal of Cardiac Failure Construct. J Card Fail 2023;29(2):181-192. PM: 36529605.
Kamimura D, Yimer WK, Shah AM, Mentz RJ, Oshunbade A, Hamid A, Suzuki T, Clark D, Waller J, Fox ER, Correa A, Butler J, Hall ME. Vitamin D Levels in Black Americans and the Association With Left Ventricular Remodeling and Incident Heart Failure With Preserved Ejectin Fraction: The Jackson Heart Study. J Card Fail 2023;29(2):150-157. PM: 35905866.
Pierce JB, Maqsood MH, Khan MS, Minhas AMK, Butler J, Felker GM, Greene SJ. Duration of Heart Failure, In-hospital Clinical Trajectory, and Postdischarge Outcomes in Patients Hospitalized for Heart Failure. J Card Fail 2023;29(2):225-228. PM: 36351495.
Tam DY, Fang J, Rocha RV, Rao SV, Dzavik V, Lawton J, Austin PC, Gaudino M, Fremes SE, Lee DS. Real-World Examination of Revascularization Strategies for Left Main Coronary Disease in Ontario, Canada. JACC Cardiovasc Interv 2023;16(3):277-288. PM: 36609048.
Al-Khatib SM, Hill JA, Carnethon M. Seventh Annual Go Red for Women Issue. Circulation 2023;147(7):519-520. PM: 36780381.
Badhwar V, Chikwe J, Gillinov AM, Vemulapalli S, O’Gara PT, Mehaffey JH, Wyler von Ballmoos M, Bowdish ME, Gray EL, O’Brien SM, Thourani VH, Shahian DM, Habib RH. Risk of Surgical Mitral Valve Repair for Primary Mitral Regurgitation. J Am Coll Cardiol 2023;81(7):636-648. PM: 36669958.
Benjamin EJ, Thomas KL, Go AS, Desvigne-Nickens P, Albert CM, Alonso A, Chamberlain AM, Essien UR, Hernandez I, Hills MT, Kershaw KN, Levy PD, Magnani JW, Matlock DD, O’Brien EC, Rodriguez CJ, Russo AM, Soliman EZ, Cooper LS, Al-Khatib SM. Transforming Atrial Fibrillation Research to Integrate Social Determinants of Health: A National Heart, Lung, and Blood Institute Workshop Report. JAMA Cardiol 2023;8(2):182-191. PM: 36478155.
Carson JL, Brooks MM, Chaitman BR, Alexander JH, Goodman SG, Bertolet M, Abbott JD, Cooper HA, Rao SV, Triulzi DJ, Fergusson DA, Kostis WJ, Noveck H, Simon T, Steg PG, DeFilippis AP, Goldsweig AM, Lopes RD, White H, Alsweiler C, Morton E, Hébert PC. Rationale and design for the myocardial ischemia and transfusion (MINT) randomized clinical trial. Am Heart J 2023;257:120-129. PM: 36417955.
Coles TM, Lin L, Weinfurt K, Reeve BB, Spertus JA, Mentz RJ, Piña IL, Bocell FD, Tarver ME, Henke DM, Saha A, Caldwell B, Spring S. Do PRO Measures Function the Same Way for all Individuals With Heart Failure? J Card Fail 2023;29(2):210-216. PM: 35691480.
DeFilippis EM, Mentz RJ, Lala A. Lifting and Healing as We Climb: Women’s Heart Month. J Card Fail 2023;29(2):121-123. PM: 36797008.
Hong JC, Patel P, Eclov NCW, Stephens SJ, Mowery YM, Tenenbaum JD, Palta M. Healthcare provider evaluation of machine learning- directed care: reactions to deployment on a randomised controlled study. BMJ Health Care Inform 2023;30(1):e100674. PM: 36764680.
Joyce E, McIllvennan CK, Esquivel JH, Sauer AJ, Correa A, Blumer V, Youmans QR, Alvarez-Garcia J, Chang H, Overbey J, Deych E, Sinha SS, Morris A, Defilippis EM, Reza N, Code J, Hajduczok AG, Fudim M, Rollins B, Vader JM, Pina IL, Teuteberg J, Zieroth S, Starling RC, Gulati M, Mentz RJ, Lala A. Participating in the Peer Review Process: The Journal of Cardiac Failure Construct. J Card Fail 2023;29(2):181-192. PM: 36529605.
Kamimura D, Yimer WK, Shah AM, Mentz RJ, Oshunbade A, Hamid A, Suzuki T, Clark D, Waller J, Fox ER, Correa A, Butler J, Hall ME. Vitamin D Levels in Black Americans and the Association With Left Ventricular Remodeling and Incident Heart Failure With Preserved Ejectin Fraction: The Jackson Heart Study. J Card Fail 2023;29(2):150-157. PM: 35905866.
Karatela MF, Dowell RS, Friedman D, Jackson KP, Piccini JP. Omnipolar Versus Bipolar Electrode Mapping in Patients With Atrial Fibrillation Undergoing Catheter Ablation. JACC Clin Electrophysiol 2022;8(12):1539-1552. PM: 36779625.
Khan MS, Xu H, Fonarow GC, Lautsch D, Hilkert R, Allen LA, DeVore AD, Alhanti B, Yancy CW, Albert NM, Butler J, Greene SJ. Applicability of Vericiguat to Patients Hospitalized for Heart Failure in the United States. JACC Heart Fail 2023;11(2):211-223. PM: 36754528.
Liu Y, Douglas PS, Lip GYH, Thabane L, Li L, Ye Z, Li G. Relationship between obesity severity, metabolic status and cardiovascular disease in obese adults. Eur J Clin Invest 2023;53(3):e13912. PM: 36424669.
Lowenstern AM, Vekstein AM, Grau-Sepulveda M, Badhwar V, Thourani VH, Cohen DJ, Sorajja P, Goel K, Barker CM, Lindman BR, Glower DG, Wang A, Vemulapalli S. Impact of Transcatheter Mitral Valve Repair Availability on Volume and Outcomes of Surgical Repair. J Am Coll Cardiol 2023;81(6):521-532. PM: 36754512.
Mauro C, Chianese S, Cocchia R, Arcopinto M, Auciello S, Capone V, Carafa M, Carbone A, Caruso G, Castaldo R, Citro R, Crisci G, D’Andrea A, D’Assante R, D’Avino M, Ferrara F, Frangiosa A, Galzerano D, Maffei V, Marra AM, Mehta RM, Mehta RH, Paladino F, Ranieri B, Franzese M, et al. Acute Heart Failure: Diagnostic-Therapeutic Pathways and Preventive Strategies-A Real-World Clinician’s Guide. J Clin Med 2023;12(3):846. PM: 36769495.
Nathan SD, Deng C, King CS, DuBrock HM, Elwing J, Rajagopal S, Rischard F, Sahay S, Broderick M, Shen E, Smith P, Tapson VF, Waxman AB. Inhaled Treprostinil Dosage in Pulmonary Hypertension Associated With Interstitial Lung Disease and Its Effects on Clinical Outcomes. Chest 2023;163(2):398-406. PM: 36115497.
Pandey A, Kitzman DW, Nelson MB, Pastva AM, Duncan P, Whellan DJ, Mentz RJ, Chen H, Upadhya B, Reeves GR. Frailty and Effects of a Multidomain Physical Rehabilitation Intervention Among Older Patients Hospitalized for Acute Heart Failure: A Secondary Analysis of a Randomized Clinical Trial. JAMA Cardiol 2023;8(2):167-176. PM: 36598761.
Pierce JB, Maqsood MH, Khan MS, Minhas AMK, Butler J, Felker GM, Greene SJ. Duration of Heart Failure, In-hospital Clinical Trajectory, and Postdischarge Outcomes in Patients Hospitalized for Heart Failure. J Card Fail 2023;29(2):225-228. PM: 36351495.
Schnittman SR, Lu MT, Mayrhofer T, Burdo TH, Fitch KV, McCallum S, Fulda ES, Zanni MV, Foldyna B, Malvestutto C, Fichtenbaum CJ, Aberg JA, Bloomfield GS, Overton ET, Currier J, Tebas P, Sha BE, Ribaudo HJ, Flynn JM, Douglas PS, Erlandson KM, Grinspoon SK. Cytomegalovirus Immunoglobulin G (IgG) Titer and Coronary Artery Disease in People With Human Immunodeficiency Virus (HIV). Clin Infect Dis 2023;76(3):e613-e621. PM: 35975297.
Sharma G, Rao SJ, Douglas PS, Rzeszut A, Itchhaporia D, Wood MJ, Nasir K, Blumenthal RS, Poppas A, Kuvin J, Miller AP, Mehran R, Valentine M, Summers RF, Mehta LS. Prevalence and Professional Impact of Mental Health Conditions Among Cardiologists. J Am Coll Cardiol 2023;81(6):574-586. PM: 36585350.
Soares C, Kwok M, Boucher KA, Haji M, Echouffo-Tcheugui JB, Longenecker CT, Bloomfield GS, Ross D, Jutkowtiz E, Sullivan JL, Rudolph JL, Wu WC, Erqou S. Performance of Cardiovascular Risk Prediction Models Among People Living With HIV: A Systematic Review and Meta-analysis. JAMA Cardiol 2023;8(2):139-149. PM: 36576812.
Zeitler EP, Kearing S, Coylewright M, Nair D, Hsu JC, Darden D, O’Malley AJ, Russo AM, Al-Khatib SM. Comparative Effectiveness of Left Atrial Appendage Occlusion Versus Oral Anticoagulation by Sex. Circulation 2023;147(7):586-596. PM: 36780379.
Tam DY, Fang J, Rocha RV, Rao SV, Dzavik V, Lawton J, Austin PC, Gaudino M, Fremes SE, Lee DS. Real-World Examination of Revascularization Strategies for Left Main Coronary Disease in Ontario, Canada. JACC Cardiovasc Interv 2023;16(3):277-288. PM: 36609048.
Duke Heart Pulse – Week of February 19th 2023
Chief’s message: The Future is Bright
As we move towards spring and the changing of our organization to an aligned practice, this episode of the Duke Heart Pulse notes lots of important milestones and achievements. You will see how our academic mission continues to drive our practice – with several members of our faculty getting grants, awards and induction into honor societies. Pictured below, congratulations to Jennifer Rymer who was awarded the 2023 physician-scientist award from the American Society of Clinical Investigation (ASCI) and Gerald Bloomfield and Jonathan Piccini who will be inducted into the ASCI in the class of 2023. They will join other members of Duke Cardiology who are members of ASCI.

Additionally, please find some of our faculty that were selected for leadership programs both at Duke (Larry Jackson and Titus Ngeno) and nationally – the American College of Cardiology emerging leadership academy (Nishant Shah).

There is also the story that ran on CBS evening news around a DCD heart transplant patient at Duke with interview of Jacob Schroder – full story farther down below with a link to the entire segment on the news.

In this week’s Pulse we will also recognize many of the Mandel awardees, the Mandel foundation and support of the Cardiovascular Research Investigator’s remains critical to our success. You will see the amazing group of investigators supported by the program. Finally, we welcome back Tom Ryan to the Duke Heart center – lucky to have him join us from Ohio State University.
Highlights of the week:
Welcome Back to Duke Heart, Tom Ryan, MD!
 Former Duke cardiologist Dr. Thomas Ryan has returned to our team at Duke Heart as of Feb. 1, and we are glad to have him back! Ryan was most recently the executive director of the Richard M. Ross Heart Hospital and director of The Ohio State University Heart and Vascular Center in Columbus, OH.
Former Duke cardiologist Dr. Thomas Ryan has returned to our team at Duke Heart as of Feb. 1, and we are glad to have him back! Ryan was most recently the executive director of the Richard M. Ross Heart Hospital and director of The Ohio State University Heart and Vascular Center in Columbus, OH.
Ryan will see general cardiology patients at our South Durham clinic and provide cardiology services through the Duke Health Signature Care Program at both the Center for Living Campus and the South Durham locations.
“Our plan was always to move back to the Research Triangle area — for family reasons, but also because we have a lot of friends in this area,” said Ryan. “We were at Duke for 12 years before we left for Ohio, so that was always the plan, but I was also planning to simply retire and then move back.
“But, I started talking to my Duke friends and one thing led to another, and the opportunity came up to work part-time at Duke. I jumped at it! I wasn’t quite ready to retire completely and the chance to be back at Duke was just too good to pass up,” he added.
He says he never anticipated leaving Duke. But Ohio State was about to build a new heart hospital and a new heart and lung research institute – and they needed someone to lead that endeavor.
“They were interested in creating a ‘heart center’ model, similar to what we had here at Duke. So, I was recruited there specifically for that, and frankly, I didn’t think I’d be there for 16 years but that’s how it worked out.
“It was a terrific opportunity to build something from scratch. We opened a beautiful facility and I worked with a terrific team to create a ‘heart center’ model. I’m proud of the work we did there — it was a great experience and I really enjoyed being there, but I am so happy to be back here at Duke.”
Ryan has fond memories of his 12 years in Durham. “I never would have had the opportunities in my academic career were it not for my first tenure here at Duke. So, I am grateful for all Duke has given me. I love the people here and still have wonderful friends throughout the Triangle — especially at Duke — and it’s a fantastic medical center from top to bottom.”
When reflecting on his career, Ryan says he knew pretty early on that he wanted to go into medicine.
“From an early point in my medical education, I decided I want to go into cardiology, and it turned out to be — for me — a very good decision,” Ryan said. “It has led to 35 years of very satisfying work. There is a lot of variety in what you can do within the field, so that is a part of why I chose this specialty. Beyond that, it has to do with the relationships you build with patients who have heart problems.
“Nobody has a heart problem that they consider to be a minor problem,” he adds. “When someone thinks they have a heart problem, or when they know they have a heart problem — for them, that’s a big deal. The bond that you develop with patients is important. They’re placing their life in your hands and that’s a very special responsibility. So, I’ve always liked that part of it — helping people when they perhaps felt most vulnerable or had the greatest need.”
Ryan says he has always tried to walk-the-walk while encouraging others to live a healthy lifestyle. He exercises regularly – running, riding his bike, staying active in general, and making the effort to take care of his health.
Ryan is keen on having an impact again at Duke and to providing great service both to our patients and his Duke Heart colleagues, including trainees and students.
“I want to give something back out of gratitude for what Duke has given to me,” he adds. “It’s just great to be back here in the Triangle and have the opportunity to stay active in a profession that I really truly love — and to have more time to enjoy life outside of work.”
Ryan earned his medical degree from Indiana University School of Medicine and holds an MBA from Duke University Fuqua School of Business. He completed internship and residency in internal medicine, and a fellowship in cardiology, at Indiana University.
Please extend a warm welcome to Tom when you see him, or reach out to him via email.
Welcome back, Tom! We’re glad to have you back on the Duke Heart team!
ICYMI: Duke Heart Patient, Schroder, Featured in CBS Evening News Story
Jacob Schroder, MD, director of Duke’s Heart Transplantation Program, and one of our patients – a DCD heart transplant recipient — were featured in a story that aired last week during the CBS Evening News with Norah O’Donnell.
Also, a very special shout-out to our entire heart transplant team: they surpassed 100 DCD heart transplants last weekend, placing them among the highest volume and most experienced in DCD heart transplantation in the world. Congratulations!

This week! Lefkowitz Lecture Kicks-off Research Series 2023
The Duke University School of Medicine’s Dean’s Distinguished Research Series showcases groundbreaking research from the basic, clinical, and translational sciences. Formerly called “Research Week”, the reimagined series will be held in-person and livestreamed. All faculty, staff, trainees, and students are welcome to attend.
For the full schedule, please visit: https://medschool.duke.edu/research/deans-distinguished-research-series-2023.
The Robert J. Lefkowitz, MD, Distinguished Lecture is the kick-off event and is scheduled for Feb. 23 at 4 p.m. in the Great Hall of the Trent Semans Center for Health Education (it will also be livestreamed via Zoom).
Titia de Lange, PhD, Laboratory of Cell Biology and Genetics and Director, Anderson Center for Cancer Research at Rockefeller University is the invited presenter. Her topic is Telomeres and cancer: genome instability and tumor suppression. Reception to follow.
Duke Cardiac Ultrasound Students Named ASE Scholarship Award Winners
We are thrilled to announce that two of our Duke Cardiac Ultrasound Certificate Program students have won American Society of Echocardiography (ASE) Foundation student scholarships.
 Ricky Damon has been selected as a recipient of a 2023 Alan D. Waggoner Student Scholarship Award and Forrest Zimmermann has been chosen as the 2023 recipient of the Katanick
Ricky Damon has been selected as a recipient of a 2023 Alan D. Waggoner Student Scholarship Award and Forrest Zimmermann has been chosen as the 2023 recipient of the Katanick  Scholarship Award.
Scholarship Award.
The Katanick award is given to the highest-ranking student sonographer candidate nominated for ASEF scholarship awards. This award was established in 2016 and named to honor the legacy of Sandy Katanick, RN, RVT, CAE, who retired as CEO of the Intersocietal Accreditation Commission after more than 25 years of service to the field.
This is only the second year that Duke has been eligible to nominate students for these ASEF awards, and our second year with two awardees and back-to-back Katanick’s!
The awards will be presented to Damon and Zimmermann at ASE 2023 during the 34th annual meeting scheduled for June 23-26 at Gaylord National Resort & Convention Center in National Harbor, MD. They will each receive $1,000 and support for travel.
Congratulations to Ricky and Forrest, as well as to Richie Palma and Anita Kelsey, MD, for their incredible recruitment to and leadership of the Cardiac Ultrasound Certificate Program. We are so proud of this program!
CVRC 2023 Mandel Awards
The Duke Cardiovascular Research Center (CVRC) has recently awarded their annual Mandel Awards. This year, six awards totaling approximately $300K will fund a Mandel Fellow Award and five Mandel Seed Awards. The selected projects will advance scientific understanding in the areas of hypertension, atherosclerosis, and related cardiovascular diseases, thanks to the generosity of the Edna and Fred L. Mandel Jr. Foundation.
Mandel Fellow Award
Andrew Ressler, PhD, mentored by Doug Marchuk, PhD
Project: Elucidating Genetic Mechanisms in CCMs
Somatic variants in cells within the vasculature of the cerebral cortex lead to Cerebral
Cavernous Malformations (CCMs). CCMs are groups of abnormal small blood vessels that often result in slow-moving blood, clotting and/or leakiness. Symptoms vary depending on the size and location of the CCM. CCMs present heterogeneously, but common complications include hemorrhage and epilepsy. Currently, the only definitive treatment for problematic CCMs is surgical excision, with targeted radiation therapy as a potential alternative for surgically inaccessible lesions. Identifying alternative, less invasive therapies would be highly beneficial to patients and may require improved understanding of the genetic underpinnings of large lesions with particularly aggressive clinical presentation. To date, all genetic diagnoses of CCMs either include loss-of-function (LoF) variants of one of three CCM genes or a somatic activating variant in MAP3K3. Evidence from animal models and human genetics are suggestive of a two-hit mechanism for LoF variants in a CCM gene. However, current sequencing strategies have failed to identify bi-allelic loss of CCM in a majority of lesions without a MAP3K3 variant. One explanation for many of these ‘missing mutations’ is somatic structural variants that are difficult to identify. We aim to use single nucleus DNA-sequencing (snDNA-seq) to identify somatic loss-of-heterozygosity in surgically resected CCMs. We further aim to mine existing genetic data to see whether or not variants in neighboring genes are associated with clinical outcomes. Critically, such an approach of using snDNA-seq to identify somatic chromosomal alterations as causative for disease may be utilized to investigate the array of cardiovascular disorders with evidence of large somatic variations.
Mandel Seed Awards
Sharon Gerecht, PhD and Neil Freedman, MD
Project: Synthetic Arterial Grafts Engineered to Resist Atherosclerosis
Atherosclerosis, with the consequent plaque buildup resulting in restriction (stenosis) or occlusion of blood flow, is a significant underlying cause of cardiovascular disease. In patients with serious vascular stenosis, arterial bypass surgery is used to re-establish blood flow in the coronary and peripheral arteries. Unfortunately, autografts require a second surgical site and have insufficient availability in patients with widespread atherosclerosis or previously harvested vessels. Thus, there is an urgent clinical need to develop synthetic grafts that provide long-term patency. Engineered bypass grafts could offer a robust and reliable solution, but a functional, engineered bypass graft has remained elusive mainly due to post-implantation thrombogenicity and intimal hyperplasia. We recently developed natural small-diameter vascular grafts (sdVGs), which are made of natural material with properties mimicry of blood vessels that enable immediate perfusion and formation of a confluent endothelium in vivo. Our compelling data show that these grafts retain patency for 24 weeks in mice and acquire structural and mechanical features that closely resemble the native abdominal aorta. The goal of this proposal is to investigate the regeneration capacity of the sdVGs in an atherosclerosis disease model and determine if conjugating anti-coagulant in the graft prevents thrombosis-induced graft failure. The Specific Aims are: (1) To determine the effect of atherosclerosis on sdVGs integration and function; (2) To determine if sustained local inhibition of thrombosis improves sdVG integration in the atherosclerosis disease model. There is a critical need to understand how the atherosclerosis environment modulates arterial-engineered graft integration and function to be able to make significant inroads toward clinical translation. To our knowledge, no study has yet examined engineered arterial grafts in a cardiovascular disease animal model. The proposed work will generate a scientific understanding of how to prevent graft failure as a result of thrombosis in atherosclerosis and may ultimately have therapeutic implications for patients with atherosclerosis.
underlying cause of cardiovascular disease. In patients with serious vascular stenosis, arterial bypass surgery is used to re-establish blood flow in the coronary and peripheral arteries. Unfortunately, autografts require a second surgical site and have insufficient availability in patients with widespread atherosclerosis or previously harvested vessels. Thus, there is an urgent clinical need to develop synthetic grafts that provide long-term patency. Engineered bypass grafts could offer a robust and reliable solution, but a functional, engineered bypass graft has remained elusive mainly due to post-implantation thrombogenicity and intimal hyperplasia. We recently developed natural small-diameter vascular grafts (sdVGs), which are made of natural material with properties mimicry of blood vessels that enable immediate perfusion and formation of a confluent endothelium in vivo. Our compelling data show that these grafts retain patency for 24 weeks in mice and acquire structural and mechanical features that closely resemble the native abdominal aorta. The goal of this proposal is to investigate the regeneration capacity of the sdVGs in an atherosclerosis disease model and determine if conjugating anti-coagulant in the graft prevents thrombosis-induced graft failure. The Specific Aims are: (1) To determine the effect of atherosclerosis on sdVGs integration and function; (2) To determine if sustained local inhibition of thrombosis improves sdVG integration in the atherosclerosis disease model. There is a critical need to understand how the atherosclerosis environment modulates arterial-engineered graft integration and function to be able to make significant inroads toward clinical translation. To our knowledge, no study has yet examined engineered arterial grafts in a cardiovascular disease animal model. The proposed work will generate a scientific understanding of how to prevent graft failure as a result of thrombosis in atherosclerosis and may ultimately have therapeutic implications for patients with atherosclerosis.
Robert W. McGarrah, MD and Christopher Holley, MD PhD
Project: New Regulatory Mechanisms of RNA Modification that Mediate Protein Translation in the Heart
 Cardiac hypertrophy (thickening of the heart muscle) and heart failure (the inability of the heart to pump enough blood to supply the body’s needs) are the end result of many diseases, including
Cardiac hypertrophy (thickening of the heart muscle) and heart failure (the inability of the heart to pump enough blood to supply the body’s needs) are the end result of many diseases, including

hypertension, obesity, diabetes and atherosclerosis. Better understanding of the early events that lead to cardiac hypertrophy and heart failure may form the foundation of new therapies to treat these common conditions. In the past 5 years, several research groups, including those from Duke, have found that as the heart begins to fail, there are changes in a biological pathway involved in the breakdown of certain amino acids (building blocks of proteins). These changes are thought to contribute to the development of cardiac hypertrophy by leading to a build-up of amino acids in the heart. We have recently discovered that if we specifically perturb an enzyme from this amino acid pathway in the heart, we do not change the concentrations of the amino acids in the heart, but we still see a change in protein synthesis, which can lead to cardiac hypertrophy. Based on preliminary experiments, we hypothesize that the changes in protein synthesis in the heart that we observe might be related to newly described functions of this enzyme on modifications of RNA, rather than any functions related to amino acid metabolism. This proposal will test this hypothesis in more depth, using newly generated genetically altered mice and cutting-edge approaches to measure RNA modifications. We expect that the findings will define new mechanisms underlying cardiac hypertrophy and will generate data that will be used to apply for larger collaborative grants for our laboratories.
Sudarshan Rajagopal, MD, PhD and Ravi Karra, MD
Project: Location-specific Signaling by Different GPCRs in Cardiomyocytes
 There are nearly eight hundred G protein-coupled receptors (GPCRs) in our body that detect different hormones and neurotransmitters that regulate nearly every aspect of our body’s functions. It has been thought that these receptors act as gatekeepers by sensing signals from outside the cell and then activating signaling pathways inside the cell. However, we now realize that GPCRs can actually signal from different sites inside the cell, and that these signals result in different effects. However, the extent of this signaling in heart muscle cells (“cardio-myocytes”), where we know such
There are nearly eight hundred G protein-coupled receptors (GPCRs) in our body that detect different hormones and neurotransmitters that regulate nearly every aspect of our body’s functions. It has been thought that these receptors act as gatekeepers by sensing signals from outside the cell and then activating signaling pathways inside the cell. However, we now realize that GPCRs can actually signal from different sites inside the cell, and that these signals result in different effects. However, the extent of this signaling in heart muscle cells (“cardio-myocytes”), where we know such  signaling is very important, is currently unknown. Our long-term goal is to develop drugs that target this signaling to treat cardiovascular disease. However, to develop these therapies, we have to first characterize this location-specific signaling. Here we propose to monitor location-specific signaling by different GPCRs in cardiomyocytes. The Rajagopal Lab already developed a number of “biosensors” that can detect this signaling inside the cell, and used them to characterize signaling by other receptors in model cells. The Karra lab has developed an efficient system for expressing these proteins in cardiomyocytes from induced pluripotent stem cells (iCMs). Together, this will allow us to quantify location-specific signaling profiles of GPCRs in iCMs. We will then correlate these signaling patterns with changes in iCM shape and function. This project uses an innovative approach to study important GPCR signaling in the cardiovascular system by investigators with expertise in cardiomyocyte biology (Dr. Karra) and GPCR signaling (Dr. Rajagopal). Successful completion of these studies will inform future drug development of locations-specific drugs in the treatment of cardiovascular disease.
signaling is very important, is currently unknown. Our long-term goal is to develop drugs that target this signaling to treat cardiovascular disease. However, to develop these therapies, we have to first characterize this location-specific signaling. Here we propose to monitor location-specific signaling by different GPCRs in cardiomyocytes. The Rajagopal Lab already developed a number of “biosensors” that can detect this signaling inside the cell, and used them to characterize signaling by other receptors in model cells. The Karra lab has developed an efficient system for expressing these proteins in cardiomyocytes from induced pluripotent stem cells (iCMs). Together, this will allow us to quantify location-specific signaling profiles of GPCRs in iCMs. We will then correlate these signaling patterns with changes in iCM shape and function. This project uses an innovative approach to study important GPCR signaling in the cardiovascular system by investigators with expertise in cardiomyocyte biology (Dr. Karra) and GPCR signaling (Dr. Rajagopal). Successful completion of these studies will inform future drug development of locations-specific drugs in the treatment of cardiovascular disease.
Senthil Selvaraj, MD, MS, MA, and Svati Shah, MD, MHS
Project: Metabolomic Profiling in Patients with Heart Failure with Preserved Ejection Fraction

Heart Failure with preserved ejection (HFpEF) is common, costly, and associated with a significant risk for hospitalization and death. Despite extensive studies to date, only very recently has the first and only

treatment option shown to alter the disease course (SGLT2 inhibitors) been identified. SGLT2 inhibitors were originally designed to treat diabetes, though studies quickly demonstrated their greater utility in heart failure. Yet, our understanding of why SGLT2 inhibitors are breakthrough drugs in HFpEF is quite limited. SGLT2i have many effects on the body, but changes in the type of fuel that the body utilizes are likely highly relevant. The goal of this study is to perform comprehensive laboratory analyses (metabolomics) on blood samples from a clinical trial of SGLT2 inhibitors in HFpEF to understand changes in “fuels” used to generate energy that may underpin these benefits. We have recently demonstrated the novelty and utility of this approach in another form of HF (HF with reduced ejection fraction), and will leverage our outstanding team and resources at Duke to improve understanding of these changes as a novel treatment in HFpEF. Identifying metabolic changes and pathways affected by SGLT2 inhibitors may highlight new targets for treating patients with HFpEF.
Jonathan A. Stiber, MD, Conrad Hodgkinson, PhD, and Neil J. Freedman, MD
Project: Atheroprotective Mechanisms of Zmynd8
 Atherosclerosis leads to significant morbidity and mortality as the result of heart attacks, congestive heart failure, and stroke. Previous work supported by the Mandel Foundation showed that atherosclerosis and vascular inflammation are reduced in mice by the activity of Drebrin, a protein that is expressed in vascular smooth muscle cells (SMCs) and that increases its expression level in the context of human atherosclerosis. Drebrin inhibits a key event in the initiation of atherosclerosis known as SMC transdifferentiation: the conversion of smooth muscle cells into foam cells (cholesterol-laden cells that express macrophage markers and are pro-inflammatory), but the mechanisms by which genes involved in SMC transdifferentiation are regulated remain unclear. Drebrin binds Zmynd8, a protein that reads DNA modifications to promote or repress expression of certain genes and whose role in SMCs and atherosclerosis is unknown. We plan to test the hypothesis that Zmynd8 inhibits the development of atherosclerosis by directly regulating genes involved in SMC transdifferentiation.
Atherosclerosis leads to significant morbidity and mortality as the result of heart attacks, congestive heart failure, and stroke. Previous work supported by the Mandel Foundation showed that atherosclerosis and vascular inflammation are reduced in mice by the activity of Drebrin, a protein that is expressed in vascular smooth muscle cells (SMCs) and that increases its expression level in the context of human atherosclerosis. Drebrin inhibits a key event in the initiation of atherosclerosis known as SMC transdifferentiation: the conversion of smooth muscle cells into foam cells (cholesterol-laden cells that express macrophage markers and are pro-inflammatory), but the mechanisms by which genes involved in SMC transdifferentiation are regulated remain unclear. Drebrin binds Zmynd8, a protein that reads DNA modifications to promote or repress expression of certain genes and whose role in SMCs and atherosclerosis is unknown. We plan to test the hypothesis that Zmynd8 inhibits the development of atherosclerosis by directly regulating genes involved in SMC transdifferentiation.
Congratulations to our newest Mandel Fellow and Seed awardees – we look forward to seeing where your research takes you!
Future Relocation of DUH Unit 7100 for Renovations
As most of you know, Duke University Hospital’s bed tower 100 is in the process of being renovated. Unit 7100 will be relocated to Duke North 2200 (a 16-bed unit) and 3200 (also a 16-bed unit) in April.
These units were selected for their close proximity to one another and to other Heart units; the provision of 32 beds for Cardiology patients; and, for being move-in ready after recent renovations. 7201-7208 will close as the Hospital Surge Unit, and the eight Emergency Department admit hold patients will relocate from 2200 to this area.
The exact dates for closing 7201-7208 and relocating 7100 will be communicated once we have firm dates identified. There will be no change in the patient population we will care for on units 2200/3200.
Shout-out to Duran!
We received a nice note this week that was sent to Anna Lisa Chamis, MD regarding cardiology fellow Jessica Duran, MD, and  we thought we’d share it with you. It’s from a grateful family member.
we thought we’d share it with you. It’s from a grateful family member.
“I am writing to heap praise on one of your fellows: Jessica Duran. Jessica has been on call this weekend taking care of my dad who came in through the ER with unstable angina. Jessica’s depth of Cardiology expertise, passion for patient care, and dedication are inspiring. Although she was only professionally tasked with seeing my dad in the ER yesterday, she paid him a social visit today only to find him in extremis with what turned out to be a SBP in the 50s. She took immediate action to stabilize him, called for help, and ultimately brought him back from the brink of what could have been a life-threatening disaster.
“My whole family and I are deeply grateful to Jessica for going above and beyond the call of duty multiple times just this weekend. She is a star!” — Yuriy
We agree – she’s a star! Well-done, Jessie!
Duke Heart Family Grows by One!
Congratulations to cardiology fellow Nathan Goodwin, MD and his wife Laura, on the birth of their baby boy, Luke Patrick on Feb. 11. Baby Luke helped cheer the Kansas City Chiefs to a Super Bowl victory at just one day old!
Congrats, Nate & Laura – we are excited for you and hope to meet Luke soon!


Duke Heart Network Update: Frye Regional
Frye Regional Medical Center, a Duke LifePoint hospital, is bringing emergency medical care to new heights. After several months of careful planning, construction and staff education, Frye Regional has a new rooftop helipad – technically two helipads – located on the top floor of the hospital’s parking garage on N. Center Street in Hickory, NC.
“This marks a tremendous step forward for the delivery of critical care at Frye Regional and further exemplifies our mission of making communities healthier,” said Philip Greene, MD, chief executive officer of Frye Regional Medical Center. “This investment in our facility has been years in the making and is a visible sign of the progress made in establishing Frye Regional as the region’s leader in cardiac and neurosurgical care.”
A ribbon cutting ceremony, attended by Duke Heart Network team members Melanie Watson, Trevor Krawchuk, and Lisa Kotyra, was held at Frye Regional for their “ceremonial first flight” on Feb. 3. Their new helipad is now fully operational!
To read more about this, please visit: https://duke.is/wwfrb.


Griffith Selected as an AHA/Go Red Women of Impact nominee
 Barbara Griffith, MD, president of Duke Raleigh Hospital, has been selected as a Woman of Impact nominee by the Triangle American Heart Association.
Barbara Griffith, MD, president of Duke Raleigh Hospital, has been selected as a Woman of Impact nominee by the Triangle American Heart Association.
Every year across the U.S., a select group of individuals are nominated to be a part of Women of Impact because of their passion and drive to make a difference. Women of Impact is a 9-week blind competition focused on women’s heart health. Launched earlier this month, Griffith has until 9 p.m. on April 6, 2023 to recruit her team members and raise vital funds for the AHA. All nominees work to build campaign plans, recruit Impact teams, and inspire their networks to support the American Heart Association’s lifesaving mission.
At the end of the campaign, this special group of nominees will be celebrated for the overall impact they have on our mission and community. The nominee who makes the greatest impact and raises the most funds locally will be named a local 2023 Woman of Impact Winner. Additionally, the nominee who makes the greatest impact nationwide will be named the American Heart Association 2023 National Woman of Impact Winner.
To read Dr. Griffith’s statement and to support her campaign, please visit: https://duke.is/rsew2. An overview of the campaign can be found here: https://duke.is/5eb9y.
Go, Barbara!
Link for Feb. 16 CGR
If you missed or would like to re-watch Haider Warraich, MD’s cardiology grand rounds presentation from Feb. 16, you can link to it here: https://duke.is/vrpms. Warraich is director of the Heart Failure Program at VA Boston Healthcare System. The title of his talk is State of the Heart: What the History of Heart Disease Teaches Us About Its Future.
Thanks to all who were able to join us live on Thursday morning!
DHIP update
We will have a grand rounds to review expected DHIP agreements this upcoming week. We know there are areas that need to be updated but want to get agreements to faculty. Distribution of Employment Agreements for transitioning members begins this week and will take place on a rolling basis by department. Employment documents for senior leaders, managers, APPs, and staff are expected to be distributed within the next two weeks.
The Duke Guarantee offers the minimum compensation each Member can expect to receive. Additional compensation opportunities which exist today will continue to be available to members within DHIP.
Benefits:
- Information regarding Duke Benefits is available on SharePoint.
- All benefits related questions can be sent to DHIPBenefits@Duke.edu.
All other questions can be sent to DHIP@duke.edu, and all DHIP updates can be found at https://dhip.org.
Upcoming Events & Opportunities
Cardiology Grand Rounds
Feb. 21: No CGR today.
Feb. 28: Topic TBD with Sandeep Nathan of Univ. of Chicago Medicine. 5 p.m., Zoom.
DCRI Research Forum: Feb. 28
The Duke Clinical Research Institute’s upcoming Research Forum will feature a fireside chat with Journal of the American Medical Association (JAMA) Editor-In-Chief Dr. Kirsten Bibbins-Domingo
What: A Fireside Chat with JAMA Editor-in-Chief Kirsten Bibbins-Domingo, PhD, MD, MAS
When: Tuesday, Feb. 28 from 12 p.m.-1 p.m.
(Required) Register: https://duke.is/y45qv
Webinar details and link will be provided upon registration.
Save the Date: Spring Faculty Reception
All Duke SOM faculty members are invited to the 2023 School of Medicine Spring Faculty Celebration scheduled for Wednesday, May 17, 5:00-7:30 p.m. at the Doris Duke Center, Duke Gardens. This event is a wonderful opportunity to network, celebrate achievements, and recognize colleagues with faculty awards. Refreshments will be served. Link to RSVP is below.
Feel free to invite your SOM faculty colleagues to attend with you or to make plans to come as a group and celebrate the end of the academic year together.
Tentative Agenda:
5:00 – 6:00 p.m. — Networking reception with heavy hors d’oeuvres
6:00 – 6:15 p.m. — Opening Remarks
6:15 – 7:00 p.m. — School of Medicine Faculty Awards and Recognitions
7:00 – 7:30 p.m. — Reception and Dessert
The Office of Faculty is looking forward to seeing you there! If you have any questions about the event, please do not hesitate to contact their team: facdev@dm.duke.edu.
To RSVP: https://duke.is/cyp46
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
February 10 — Stephen Greene
HCP Live
Don’t Miss a Beat: STRONG-HF with Alexandre Mebazaa, MD, PhD
https://duke.is/zkjun
February 15 — Jacob Schroder
CBS Evening News*
New method revolutionizes heart transplants
https://duke.is/rj2kh
*also carried by 50+ CBS News TV & radio affiliates including in Dallas-Fort Worth, New York & Philadelphia, and in Yahoo News
February 16 — Jacob Schroder
Sur Noticias
El revolucionario método de transplante de corazón
https://duke.is/ngcrw
February 16 — Jacob Schroder
Es Postsus
Nuevo método revoluciona los trasplantes de corazón
https://duke.is/b9eva
Duke Heart Pulse – week ending February 12th 2023
Chief’s message:
Hopefully everyone is having a restful weekend and getting ready for hopefully an exciting Super Bowl. Even if you are not that much into the game, the cultural phenomena of the game will have variety of ads, firsts, and favorite foods for many. This year there will be some extra discussion around the effects of cardiovascular disease given the cardiac arrest of Damar Hamlin, and his work with the AHA to raise awareness for CPR training. His three for heart challenge can be found here at #3forHeart @heart.org (https://www.heart.org/en/damar-hamlins-3-for-heart-cpr-challenge)
Over the next few weeks we will highlight some new people joining our CV team, some awards our faculty are getting, and our continued movement towards an aligned organization that will help us lead in Cardiovascular care, teaching, and research. Also during Heart Month– we will feature this month the several faculty and team members working with the American Heart Association and our local community to raise awareness around cardiovascular disease, women’s heart health, and bystander CPR training.
Highlights of the week:
Duke Names Health System Chief Executive Officer
 Craig Albanese, MD, an accomplished health care leader and distinguished academic pediatric surgeon, has been named chief executive officer of Duke University Health System (DUHS).
Craig Albanese, MD, an accomplished health care leader and distinguished academic pediatric surgeon, has been named chief executive officer of Duke University Health System (DUHS).
In assuming the role as CEO — which will be effective at the end of next month — Albanese will be responsible for strategic and operational oversight of DUHS and its senior leadership. He will continue to report to A. Eugene Washington, MD, Duke University chancellor for health affairs, and also will report directly to the Duke University Health System Board of Directors.
Since joining DUHS as executive vice president and chief operating officer on Jan. 17, 2022, Albanese has demonstrated his ability to champion our culture, lead large-scale change and drive operational performance improvement. He has been intensely involved in addressing the health system’s financial challenges while ensuring sustained high levels of patient care quality and safety.
“Dr. Albanese has demonstrated vigorous and responsive leadership that has enabled Duke’s clinical enterprise to recover and renew in the wake of the devastating COVID-19 pandemic, working diligently to improve the well-being of our people, and seeking to accelerate expansion of our health system through organic growth and strategic partnerships. His continued leadership will be vital in guiding the next phase of the health system’s work,” said Washington and Duke University President Vincent E. Price in a joint statement.
As chief executive officer, Albanese will oversee the timely execution of DUHS goals and strategic priorities and be dedicated to ensuring that Duke’s clinical enterprise continues to thrive and lead. He oversees all other clinical enterprise leaders to deliver outcomes and care across Duke’s network, from the hospitals to ambulatory clinics to care in homes and the community.
“A passionate advocate for our providers and frontline team members, Dr. Albanese is a leader of high integrity and personal commitment who puts people first and who has garnered trust and credibility with Duke’s faculty, leadership and staff alike,” said Price and Washington. “Considering his personal qualities and performance to date, we are confident that Dr. Albanese is the right person to lead our health system at this time.”
Albanese has deep, broad health care expertise and experience, along with a record of achievements and contributions. Prior to Duke, he served as group senior vice president and chief medical officer of NewYork-Presbyterian Hospital, a $9.2 billion, 10-hospital academic health system.
Albanese has also held senior leadership roles at Stanford University and the University of California San Francisco (UCSF). A respected surgeon-scientist and clinical investigator, he co-directed the team that pioneered in-utero fetal surgery.
Albanese received his medical degree from SUNY Health Science Center in Brooklyn and was a resident and chief resident in general surgery at Mount Sinai Medical Center. He completed pediatric general surgery and critical care research fellowships at Children’s Hospital of Pittsburgh. Albanese also holds a Master’s in Business Administration from the Leavey School of Business at Santa Clara University.
He has published more than 160 peer-reviewed articles, was an NIH-funded investigator, the program director for Stanford’s pediatric general surgery fellowship and is the lead author of “Advanced Lean in Healthcare,” a book providing practical information about how “organizations can move beyond stabilizing work processes to get to continuously improving the entire system – all within an empathetic healing environment.”
Albanese’s appointment follows Washington’s announcement last fall that he will step down from his role of chancellor for health affairs at Duke University and president and chief executive officer for the Duke University Health System on June 30, 2023.
Washington continues to guide and oversee the academic mission of Duke Health, working closely with the DUHS CEO, the provost, deans of the Schools of Medicine and Nursing, and other academic and clinical leaders to ensure alignment and mutually reinforce excellence in our clinical, educational, research, and community health missions.
ICYMI: Chen Featured in ACS Article on Surgeon Siblings
Our own Edward P. Chen, MD, chief of the division of cardiovascular and thoracic surgery at Duke, is featured – along with his brother, Fred — in an article by the American College of Surgeons. If you haven’t yet seen it, it’s worth checking out! Please visit: https://duke.is/jrf5e. It’s an amazing story of how two siblings and the family supported each other as they clearly followed their calling in Cardio-Thoracic Surgery.

Cardiac Rehab Week & CV Professionals Week
It’s Super Bowl Sunday and the start of a week of recognition for Cardiovascular Professionals and those working in Cardiac Rehabilitation. While you’re digging into snacks, the game, and this edition of Pulse, please join us in recognizing the great work our teams are doing to care for patients with their specialized skills, in researching the underpinnings of heart disease and effective treatments, and to train others in all areas of care and support of this patient population. We have a truly incredible team here at Duke and it takes all of us to be successful!
The cath and electrophysiology labs this week will be celebrating their cardiovascular invasive specialists (CVIs). On the Duke team, our CVIs come from a variety of backgrounds — some have served as paramedics, respiratory therapists, doctors in other countries, and radiology technicians. We spoke with Elizabeth Watts, nurse manager, operations for the Duke Cath Lab, EP lab & CVSSU to get her take on what makes CVIs a great part of her team.
“Their backgrounds benefit us because they’ve amassed so much knowledge from their previous experiences. In emergency situations, it’s great to have former paramedics on the team,” Watts says. “In our area, the CVIs role is very well-rounded in that they work in all aspects of the lab, they don’t just scrub, they don’t just circulate, they don’t just monitor — they do all of that and each of them are very strong clinically. Our orientation lasts 12 weeks.”
Although our CVIs roles may be most well-known for the technical backgrounds they provide, Watts wants others to know how crucial they are to the care her team provides to our patients.
“It takes multiple people to care for each of these patients. What our CVIs bring to the table only improves outcomes and experiences for the patients,” Watts adds. “Personally, I want to thank them for all their hard work and for being a great team. And not only providing great care to our patients, but the care and support they demonstrate every day.”
In terms of our cardiac rehabilitation team – they hit all the high marks, too. This team is seeing all types of heart patients including those who may have had valve surgeries, CABGs, are post-MI, or are heart failure patients or those with stabile angina.
“Our cardiac rehab team does a great job with education for the patients,” says Erica Rao, PT, DPT, Manager, Clinical Services for Duke Cardiopulmonary Rehab. “The way we see it is we’re really looking at not just having our rehab patients here exercising and doing things ‘just for now’ — we are looking to help them achieve lasting behavior change, and working with them so that we can help them prevent having relapses with their cardiac conditions or a second MI, or something similar.”
“Our cardiac rehab team is teaching patients rather than just giving exercise instruction. It’s about how we can help them learn to implement changes into their daily life, whether it be with our dietician, or getting their exercise as part of their new lifestyle, instead of just doing rehab for three months and returning to sitting on the couch,” Rao adds.
“The feedback I get from patients is that our staff takes the time to listen to them, and really cares about them. They feel they’re heard and their questions can get answered,” Rao continues. “Patients also tell me they find our staff fun and easy to talk to and that they make it more of a fun atmosphere to come and exercise instead of it being a chore. I really do appreciate the time the staff spends one on one with them, even though they might have multiple patients exercising at the same time.”
We were also able to speak with Dr. Bill Kraus, cardiologist, heart disease prevention and rehabilitation specialist, and the Richard and Pat Johnson University Distinguished Professor at Duke for his thoughts on our cardiac rehabilitation team.
“The Cardiac Rehab professionals are truly that … dedicated, experienced, patient-focused, and loved by our patients. I cannot tell you how often I am told by patients what a wonderful experience and care they have obtained from our staff of clinical exercise physiologists, nurses, nutritionist and behavioralist,” says Kraus. “Some of the exercise physiologists I have worked closely with for over 20 years. Duke would not have this national leading cardiac rehabilitation program that cares for over 200 post-event cardiac rehabilitation patients without their attentive and thoughtful care.”
Cardiac Rehabilitation Week is led by the American Association of Cardiovascular & Pulmonary Rehabilitation; Cardiovascular Professionals Week is led by the Alliance of Cardiovascular Professionals. Both recognition weeks are running Feb. 12-18.
Patel and Engel to Serve as Dyad Leaders for Heart and Vascular Service Line
Manesh Patel, MD, Richard Stack Distinguished Professor of Medicine and chief of the Division of Cardiology and Jill Engel,  DNP, ACNP, FNP, NEA-BC, FAANP, Vice President of Heart and Vascular Services at Duke, will serve as the dyad leaders for the Heart and Vascular Service line.
DNP, ACNP, FNP, NEA-BC, FAANP, Vice President of Heart and Vascular Services at Duke, will serve as the dyad leaders for the Heart and Vascular Service line.

The announcement was made on Monday, Feb. 6, 2023 by Dr. Richard Shannon, Chief Quality Officer, Duke Health, and Chief Medical Officer and Senior Vice President of Duke University Health System, and Mary Martin, MPA, FACHE and Chief Operating Officer for Duke University Hospital.
Together, Manesh and Jill will work with hospital leaders in setting strategy and operational targets across our inpatient and ambulatory platforms to insure a systems approach to Heart and Vascular Services. They will be responsible for setting strategy for growth for these cardiovascular services together with DUHS leadership with an immediate focus on Wake County while ensuring sustained performance in our many other partnerships across the Triangle and North Carolina.
Manesh and Jill will be guided in their work by input from a Heart and Vascular Advisory Group comprised of specialty division directors, nursing and administrative leaders in Heart. Shannon and Martin stated there will be an initial planning meeting in the near future.
Please join us in congratulating Manesh and Jill!
Dean’s Distinguished Research Series 2023
The Duke University School of Medicine’s Dean’s Distinguished Research Series showcases groundbreaking research from the basic, clinical, and translational sciences. Formerly called “Research Week”, the reimagined series will be held in-person and livestreamed. All faculty, staff, trainees, and students are welcome to attend.
For the full schedule, please visit: https://medschool.duke.edu/research/deans-distinguished-research-series-2023.
Note: the Robert J. Lefkowitz, MD, Distinguished Lecture is the kick-off event and is scheduled for Feb. 23 at 4 p.m. Titia de Lange, PhD, Laboratory of Cell Biology and Genetics and Director, Anderson Center for Cancer Research at Rockefeller University is the invited presenter. Her topic is Telomeres and cancer: genome instability and tumor suppression.

Final SOM Faculty Award Nominations Due 2/20, 2/28
The final deadlines for nominations and applications for the 2023 School of Medicine Faculty Awards are approaching.
As you know, the Faculty Awards are a wonderful opportunity to highlight the outstanding work conducted at Duke. The Office for Faculty is still accepting nominations and applications for the following 2023 faculty awards:
- Research Mentoring Awards – Nomination Deadline: February 20, 2023
- Ruth and A. Morris Williams Faculty Research Prize – Application Deadline: February 28, 2023
To learn more, visit https://duke.is/4hqkb. Questions? Please contact Jennifer Meyer Dare, jennifer.meyer-dare@duke.edu. Nominations and applications should be submitted via email to facdev@dm.duke.edu.
PPE Usage Reminder
DUH/DUHS is reminding all teams that PPE continues to be a top priority as we strive to meet 100% compliance. We encourage leaders to focus on PPE in your huddles and other communications with your teams. These discussions are great opportunities to address any barriers and concerns interfering with proper PPE usage. Please refer to our detailed analytics site for real-time numbers.
Please Observe Safe Practices
We continue to see increasing cases of respiratory illnesses in our community, as well as COVID clusters at work. Please help remind staff to take the appropriate precautions to protect themselves and their families from the “tripledemic” of the flu, RSV, and COVID.
As a reminder, all team members are eligible to receive the bivalent COVID-19 booster shot. Appointments can be made through the Duke Vaccine website.
It is also critical that our staff continue practicing consistent hand hygiene and the appropriate donning and doffing of PPE. Thanks for your support with these efforts! You’re doing a great job.
Upcoming Events & Opportunities
Cardiology Grand Rounds
Thursday, Feb. 16: State of the Heart: What the History of Heart Disease Teaches Us About Its Future with Haider Warraich of VA Boston Healthcare System. 7:15 a.m., via Zoom.
Feb. 21: No CGR today.
Feb. 28: Topic TBD with Sandeep Nathan of Univ. of Chicago Medicine. 5 p.m., Zoom.
Medicine Grand Rounds
Feb. 17: Topic TBD with Hyung (Harry) Jin Cho of NYU Langone Health, a 2023 Joseph C. Greenfield Visiting Professor. 8 a.m. via Zoom or in person, Duke North 2002.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
February 6 — Andrew Vekstein
Healio
TEER availability does not impact surgical repair volume but improves outcomes
https://duke.is/mqzvd
February 7 — Ziv Beckerman
USA Today
Heart defect diagnosis often comes too late – or not at all – for Latino infants, study finds
https://duke.is/yj3qx
February 7 — Tracy Wang
tctMD
Prehospital Troponin Testing With EMS Input Could Save a Lot of Money
https://duke.is/vpbhy
February 7 — Andrew Vekstein and (alum) Angela Lowenstern
tctMD
Adopting TEER Doesn’t Put a Dent in Surgical MV Repair Volumes
https://duke.is/zg3ss
February 8 — Sreekanth Vemulapalli
Medscape
What Happened to Surgical Mitral Valve Repair in the MitraClip Era?
https://duke.is/b628f
February 8 — Stephen Greene and Shahzeb Khan
tctMD
Vast Majority of HFrEF Patients Eligible for Vericiguat
https://duke.is/c5btx
February 9 — Sana Al-Khatib
Medscape
HF Podcast: For Patients With HFrEF, Who Really Benefits From a Device?
https://duke.is/w73u6
Duke Heart Pulse – week ending February 5th 2023
Highlights of the week:
Heart Month is Here – Lots to Celebrate!
We hope the first week of February has been great for you so far – of course, it’s always a good week when our Blue Devils beat Carolina!


Thank you to all team members who joined us in wearing red on Friday for National Wear Red Day, a day where we join collectively with other organizations to increase awareness of heart disease – it’s still the leading cause of death in the U.S. We have received some great photos from teams so far – shown here are members of our HR support team and clinic 2F/2G. If you haven’t shared your pics with us yet, please do!

And… if you haven’t seen these yet, we’ve installed some new signs around DUH and Duke Clinics – congratulations to our faculty and staff members for your amazing work! 
Ours is one of the best teams at Duke Health and one of the finest Heart Centers in the world, thanks to each one of you. This is definitely worth celebrating!
Something else worth celebrating: quick response & a life saved.
During the Jan. 31 Duke Men’s Basketball game, members of the Duke Life Flight team were honored for their extraordinary  care of a patient at the November 30 home game against Ohio State. At that game, the father of an Ohio State player suffered a massive heart attack in the stands. Thanks to the swift actions of the Duke Life Flight event medicine team in conjunction with Duke Athletics staff, he was quickly stabilized and transported to the DUH Emergency Department.
care of a patient at the November 30 home game against Ohio State. At that game, the father of an Ohio State player suffered a massive heart attack in the stands. Thanks to the swift actions of the Duke Life Flight event medicine team in conjunction with Duke Athletics staff, he was quickly stabilized and transported to the DUH Emergency Department.
The patient underwent a life-saving procedure with our Duke Heart team and was admitted to the Cardiac ICU. Thanks to all those who responded that day, he is now back at home where he is expected to make a full recovery. He shared a special message for the medical teams that played a part in his care. It was played at Cameron on Tuesday evening. Please check it out here: https://duke.is/pdaxg.
Well done, everyone!
Ashley Barba Named Clinical Director for CT Surgery at DUH, Effective April 1
 We are excited to share that Ashley Barba, Team Lead for our Cardiothoracic Surgery SDU APPs, will be serving in an expanded role and capacity effective April 1. Barba will continue with her team lead role and clinical practice, and will also serve as the Clinical Director for Cardiothoracic Surgery at DUH. In this expanded role, she will support quality improvement, Maestro related projects and enhancements, transitional care, and special projects aimed to further support our Cardiothoracic Surgery inpatient programs, patients and the surgical teams.
We are excited to share that Ashley Barba, Team Lead for our Cardiothoracic Surgery SDU APPs, will be serving in an expanded role and capacity effective April 1. Barba will continue with her team lead role and clinical practice, and will also serve as the Clinical Director for Cardiothoracic Surgery at DUH. In this expanded role, she will support quality improvement, Maestro related projects and enhancements, transitional care, and special projects aimed to further support our Cardiothoracic Surgery inpatient programs, patients and the surgical teams.
Barba is a tremendous provider and team leader and will be highly effective in this role as she partners with the local nursing teams and leaders, multidisciplinary operational teams and Heart Center leadership.
Please congratulate Ashley when you see her, and feel free to reach out to her as a resource around clinical care and workflows, quality initiatives, the STS registry, or operational challenges as you continue to provide world-class care to Duke Heart patients and families.
Congratulations, Ashley! Well deserved!
Carroll Earns Greenfield Women in Cardiology Award

Congratulations to Aubrie Carroll, MD, a resident in internal medicine at Duke, for being named the recipient of the Ruth Ann Greenfield Women in Cardiology Award! The award honors Dr. Ruth Ann Greenfield’s legacy at Duke.
The announcement was made by Duke electrophysiologist Don Hegland, MD who added, “This acknowledges Dr. Carroll’s many accomplishments as a Duke Internal Medicine Resident, and will support the great things she will do with her future in Cardiology.”
Such great news! Please congratulate Aubrie the next time you see her.
Kudos to 2F/2G & VAD Team
We received some terrific praise this week for our 2F/2G and VAD teams via Press Ganey Survey feedback. The patient/family member wrote:
“Dora at pulmonary testing was very good, Ericka at blood draw was excellent as there are difficulties with drawing blood, finding veins. Frank was great for executing walking exercise, and Dr. Katz was amazing as usual. Vanessa provided us with a video for a weekly dressing for LVAD. Assisted in training with replacing the existing dressing. Great experience again today.”
Great work everyone!!!
TJC Update & Kudos to Heart Teams
The first of two weeks of the PDC’s triennial Joint Commission survey of clinics concluded on Friday. TJC was very complimentary and spoke favorably about facilities, processes, and staff throughout the PDC. So far, 42 of 59 clinics had no findings, which is great news — among them, Duke Cardiology of Raleigh, Duke Cardiology of Cary, and Duke Cardiology of Morrisville.
Duke Heart teams received the following kudos from the surveyors:
- Duke Cardiology of Raleigh displayed great teamwork and work culture. Nurses Joan Senter, Emily Sweet and Eddie Scott are shining stars!
- Sarah Curtis, HCA, and Annette Moore, Nurse Manager, Duke Cardiology of Cary are outstanding and have a good understanding of operations.
- Stephen Robinson, MD of Duke Cardiology at Morrisville, received a ‘Leading Practice’ for low level disinfection of his stethoscope before and after patient care.
- An external-to-Duke provider ordered a medication that a patient had an allergy to. After receiving a MyChart message from the patient, Michelle Blau of Duke Cardiology of Morrisville, thoroughly reviewed the chart and alerted the cardiologist of the issue. This was a great catch!
Well done and way to go, everyone!
Successful Recruitment Event for SDUs Held Wed., Feb. 1
We had a successful nurse recruitment event at the DMP and DUH on Wednesday, Feb. 1. Shown here are members of our nursing leadership team who met with applicants, answered questions and gave tours. Thanks to everyone who supported this event for our Adult Stepdown Units! Our team engaged with 27 attendees and extended eight RN offers.
Great job!

Bova Departs CICU for MICU
Marina Bova was celebrated by her colleagues in the cardiac intensive care unit (CICU) this week on her last official day with us before starting a new role with Duke’s MICU team. Her team held a going away party for her on Tuesday, Jan. 31 – during her final night shift.
 “I want to recognize the outstanding contribution that Marina Bova has made to the CICU, said Jason Katz, MD. “She was one of the pioneer CICU APPs who worked tirelessly and collaboratively to improve the care of our patients, to teach our trainees, and to create a culture of teamwork with the nursing staff and others.”
“I want to recognize the outstanding contribution that Marina Bova has made to the CICU, said Jason Katz, MD. “She was one of the pioneer CICU APPs who worked tirelessly and collaboratively to improve the care of our patients, to teach our trainees, and to create a culture of teamwork with the nursing staff and others.”
“Marina bravely tackled this role when little was known and she, along with others, helped make the new APP group a pivotal component of CICU care,” he added.
Marina’s dedication to the CICU and in her overall efforts in representing the skills of APPs will help to ensure that the CICU APPs will always be an integral part of the CICU team and mission.
CICU team and mission.
“Though we will miss her terribly, we all appreciate what she has done for our patients and will eagerly anticipate how she will elevate the MICU moving forward,” Katz said.
Shown here are Bova along with several CICU team members, and cardiology fellows Andrew Andreae and Balim Senman (who provided the cake shown here!)
Congrats and good luck, Marina!
Barnes’ Story Featured as Part of DUHS Recruitment Effort
Our fabulous team member, Stephanie Barnes, Clinical Director for Advanced Heart Failure Services, shared her story recently with our Duke Health recruitment team and it’s now featured on our Duke Health careers page as part of overall recruitment efforts. Check it out here: https://duke.is/r2f88.
We agree with her: Duke is a great place to work and the best is yet to come!

Dress Like Dan Mark Day
We didn’t realize this was happening this week, but it did, and it was so good! Members of the CICU decided to hold a Dress like Dan Mark Day and we hope this isn’t the last. They say imitation is the most sincere form of flattery – and who better to emulate than Dan Mark, MD? Some of the participating team members shown in the photo are Mark Brahier, a Duke IM resident, cardiology fellow Allie Levin, IM resident Sara Stallworth, and the real Dan Mark.

ICYMI: McGarrah, Jackson CGR Recordings
We had excellent CGR presentations in January from electrophysiologist Dr. Larry Jackson, and heart disease prevention and rehabilitation specialist Dr. Robert McGarrah. If you were unable to attend either of those sessions, we have links to the recordings here:
- A Path Toward Remediating Racial and Ethnic Disparities in Arrhythmia Care with Larry Jackson. Recorded Jan. 10, 2023.
- Branched-Chain Amino Acids and Cardiometabolic Disease: Biomarkers and Beyond with Robert McGarrah. Recorded Jan. 31, 2023.
DOM Names Chief Residents for 2024-2025
Kathleen Cooney, MD, chair of the Department of Medicine, Aimee Zaas, MD, program director of the Duke Internal Medicine Residency Program, David Simel, MD, vice chair for Veterans Affairs, and Lisa Criscione-Schreiber, MD, vice chair for education, this week announced the Chief Residents for the 2024-2025 academic year.
Chief residents are selected in their final year of residency and typically complete one year of fellowship before returning to start their chief resident year.
Congratulations to:
Emory Buck, MD, Duke University Hospital. Emory is a graduate of the University of Virginia and the Georgetown University School of Medicine. She will be a fellow in Pulmonary/Critical Care Medicine at Duke prior to starting her chief resident year.
Omar Martinez-Uribe, MD, Durham VA Medical Center. Omar is a graduate of the University of Georgia and Duke University School of Medicine. He will be a fellow in Gastroenterology at Duke prior to starting his chief resident year.
Amanda Broderick, MD, Duke Regional Hospital/Ambulatory Medicine. Amanda is a graduate of Carnegie Mellon University and Baylor College of Medicine. She will be a fellow in Hematology/Oncology at Duke prior to starting her chief resident year.
The Chief Residents are a key part of the medicine residency team, providing invaluable leadership, teaching and support for our trainees. Our incoming chiefs join a strong tradition of resident leadership, and we look forward to their contributions to the Department of Medicine.

SOM Faculty Award Nomination for Excellence in Professionalism due this week
Nominations and Applications for the 2023 School of Medicine Faculty Awards are open.
The Faculty Awards are a wonderful opportunity to highlight the outstanding work conducted at Duke. The Office for Faculty is now accepting nominations and applications for the following 2023 faculty awards:
- Excellence in Professionalism Award – Nomination Deadline: February 10, 2023
- Research Mentoring Awards – Nomination Deadline: February 20, 2023
- Ruth and A. Morris Williams Faculty Research Prize – Application Deadline: February 28, 2023
- Leonard Palumbo Jr., MD Faculty Achievement Award – Nomination Deadline has passed
- Leonard B. Tow Humanism in Medicine Award – Nomination Deadline has passed
To learn more, visit https://duke.is/4hqkb. Questions? Please contact Jennifer Meyer Dare, jennifer.meyer-dare@duke.edu. Nominations and applications should be submitted via email to facdev@dm.duke.edu.
PPE Usage Reminder
DUH/DUHS is reminding all teams that PPE continues to be a top priority as we strive to meet 100% compliance. We encourage leaders to focus on PPE in your huddles and other communications with your teams. These discussions are great opportunities to address any barriers and concerns interfering with proper PPE usage. Please refer to our detailed analytics site for real-time numbers.
Encourage team members to observe safe practices
We continue to see increasing cases of respiratory illnesses in our community, as well as COVID clusters at work. Please help remind staff to take the appropriate precautions to protect themselves and their families from the “tripledemic” of the flu, RSV, and COVID.
As a reminder, all team members are eligible to receive the bivalent COVID-19 booster shot. Appointments can be made through the Duke Vaccine website.
It is also critical that our staff continue practicing consistent hand hygiene and the appropriate donning and doffing of PPE. Thanks for your support with these efforts! You’re doing a great job.
Upcoming Events & Opportunities
Cardiology Grand Rounds
Feb. 21: No CGR today.
Feb. 28: Topic TBD with Sandeep Nathan of Univ. of Chicago Medicine. 5 p.m., Zoom.
Medicine Grand Rounds
Feb. 17: Topic TBD with Hyung (Harry) Jin Cho of NYU Langone Health, a 2023 Joseph C. Greenfield Visiting Professor. 8 a.m. via Zoom or in person, Duke North 2002.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
January 23 — Sean Pokorney
EMPR.com
Novel Oral Anticoagulant Fast Tracked for Patients With ESRD and Atrial Fibrillation
https://duke.is/gjaaa
January 27 — Pamela Douglas
tctMD
As Violent Attacks on Healthcare Workers Rise, Cardiology Takes Note
https://duke.is/9yjqt
January 27 — Duke University Hospital
Becker’s Hospital Review
Press Ganey recognizes top healthcare organizations for patient experience
https://duke.is/2n2dw
January 30 — Duke School of Medicine
Inside Higher Ed
More Universities Drop ‘U.S. News’ Medical School Rankings
https://duke.is/bubws
January 30 — Duke School of Medicine
Chief Healthcare Executive
Not banking on rankings: More medical schools withdraw from U.S. News listing
https://duke.is/485f5
January 31 — Monique Starks
Scripps News Service*
Drones are being tested to deliver AEDs to cardiac arrest emergencies
https://duke.is/vzf47
*carried in 51 U.S. news markets
February 1 — Daniel Friedman
tctMD
CRT Likely Benefits Broader Group of Patients: Meta-analysis
https://duke.is/zs5ru
February 2 — Richard Shannon
Becker’s Hospital Review
The ‘hard truth’ about staffing shortages: They aren’t going away
https://duke.is/mbe5j
February 2 — Richard Shannon
Becker’s Hospital Review
Reducing administrative burdens: 5 chief medical officers weigh in
Division of Cardiology Publications Indexed in PubMed January 11-25, 2023
Avorgbedor F, Blumenthal JA, Hinderliter A, Ingle K, Lin PH, Craighead L, Tyson C, Kraus W, Sherwood A, Smith PJ. Inflammation moderates the effects of lifestyle modification on neurocognition among individuals with resistant hypertension. J Clin Hypertens (Greenwich) 2023 Jan;25(1):106-110. PM: 36541028.
Ayer A, Truby LK, Schroder JN, Casalinova S, Green CL, Bishawi MA, Bryner BS, Milano CA, Patel CB, Devore AD. Improved Outcomes in Severe Primary Graft Dysfunction After Heart Transplantation Following Donation After Circulatory Death Compared With Donation After Brain Death. J Card Fail 2023 Jan;29(1):67-75. PM: 36351494.
Beatty AL, Beckie TM, Dodson J, Goldstein CM, Hughes JW, Kraus WE, Martin SS, Olson TP, Pack QR, Stolp H, Thomas RJ, Wu WC, Franklin BA. A New Era in Cardiac Rehabilitation Delivery: Research Gaps, Questions, Strategies, and Priorities. Circulation 2023 Jan 17;147(3):254-266. PM: 36649394.
Blumer V, Lala A, Mentz RJ. JCF Heart Failure Year-In-Review 2022…The Best is Yet to Come! J Card Fail 2023 Jan;29(1):1-5. PM: 36635020.
Coniglio AC, Bryner BS, Devore AD, Patel CB. Trends in cardiovascular medicine: Update on cardiac transplantation. Trends Cardiovasc Med 2023 Jan;33(1):46- 50. PM: 34856337.
Cosiano MF, Vista A, Sun JL, Alhanti B, Harrington J, Butler J, Starling RC, Mentz RJ, Greene SJ. Comparing New York Heart Association Class and Patient-Reported Outcomes Among Patients Hospitalized for Heart Failure. Circ Heart Fail 2023 Jan;16(1):e010107. PM: 36314126.
Coyne DW, Singh AK, Lopes RD, Bailey CK, DiMino TL, Huang C, Connaire J, Rastogi A, Kim SG, Orias M, Shah S, Patel V, Cobitz AR, Wanner C. Three Times Weekly Dosing of Daprodustat versus Conventional Epoetin for Treatment of Anemia in Hemodialysis Patients: ASCEND-TD: A Phase 3 Randomized, Double-Blind, Noninferiority Trial. Clin J Am Soc Nephrol 2022 Sep;17(9):1325- 1336. PM: 35918106.
Eikelboom R, Whitlock RP, Lopes RD, Siegal D, Jaffer IH, Drakos P, Schulman S, Belley-Côté EP. How Did We Get Here? Antithrombotic Therapy after Bioprosthetic Aortic Valve Replacement: A Review. Thromb Haemost 2023 Jan;123(1):6-15. PM: 36513278.
Fulda ES, Fichtenbaum CJ, Kileel EM, Zanni MV, Aberg JA, Malvestutto C, Cardoso SW, Berzins B, Lira R, Harden R, Robbins G, Martinez M, Nieves SD, McCallum S, Cruz JL, Umbleja T, Sprenger H, Giguel F, Bone F, Wood K, Byroads M, Paradis K,
Lu MT, Douglas PS, Ribaudo HJ, Grinspoon SK, Fitch KV. The importance of methods for site performance evaluation in REPRIEVE, a longitudinal, global, multicenter trial. Contemp Clin Trials 2023 Jan;124:107035. PM: 36462699.
Garweg C, Piccini JP, Epstein LM, Frazier-Mills C, Chinitz LA, Steinwender C, Stromberg K, Sheldon T, Fagan DH, El-Chami MF. Correlation between AV synchrony and device collected AM-VP sequence counter in atrioventricular synchronous leadless pacemakers: A real-world assessment. J Cardiovasc Electrophysiol 2023 Jan;34(1):197-206. PM: 36317470.
Granger CB, Pocock SJ, Gersh BJ. The need for new clinical trials of old cardiovascular drugs. Nat Rev Cardiol 2023 Feb;20(2):71-72. PM: 36526898.
Hijazi Z, Benz AP, Lindbäck J, Alexander JH, Connolly SJ, Eikelboom JW, Granger CB, Kastner P, Lopes RD, Ziegler A, Oldgren J, Siegbahn A, Wallentin L. Bone morphogenetic protein 10: a novel risk marker of ischaemic stroke in patients with atrial fibrillation. Eur Heart J 2023 Jan 14;44(3):208-218. PM: 36380569.
Jawitz OK, Vekstein AM, Young R, Vemulapalli S, Zwischenberger BA, Thibault DP, O’Brien S, Shahian DM, Badhwar V, Thourani VH, Jacobs JP, Smith PK. Comparing Consumer-Directed Hospital Rankings With STS Adult Cardiac Surgery Database Outcomes. Ann Thorac Surg 2023 Feb;115(2):533-540. PM: 35932793.
Kato ET, Morrow DA, Guo J, Berg DD, Blazing MA, Bohula EA, Bonaca MP, Cannon CP, de Lemos JA, Giugliano RP, Jarolim P, Kempf T, Kristin Newby L, O’Donoghue ML, Pfeffer MA, Rifai N, Wiviott SD, Wollert KC, Braunwald E, Sabatine MS. Growth differentiation factor 15 and cardiovascular risk: individual patient meta-analysis. Eur Heart J 2023 Jan 21;44(4):293-300. PM: 36303404.
Khan MS, Ahmed A, Greene SJ, Fiuzat M, Kittleson MM, Butler J, Bakris GL, Fonarow GC. Managing Heart Failure in Patients on Dialysis: State-of- the-Art Review. J Card Fail 2023 Jan;29(1):87-107. PM: 36243339.
Khan MS, Shahid I, Anker SD, Fonarow GC, Fudim M, Hall ME, Hernandez A, Morris AA, Shafi T, Weir MR, Zannad F, Bakris GL, Butler J. Albuminuria and Heart Failure: JACC State-of-the-Art Review. J Am Coll Cardiol 2023 Jan 24;81(3):270-282. PM: 36653095.
Mc Causland FR, Claggett BL, Vaduganathan M, Desai AS, Jhund P, de Boer RA, Docherty K, Fang J, Hernandez AF, Inzucchi SE, Kosiborod MN, Lam CSP, Martinez F, Saraiva JFK, McGrath MM, Shah SJ, Verma S, Langkilde AM, Petersson M, McMurray JJV, Solomon SD. Dapagliflozin and Kidney Outcomes in Patients With Heart Failure With Mildly Reduced or Preserved Ejection Fraction: A Prespecified Analysis of the DELIVER Randomized Clinical Trial. JAMA Cardiol 2023 Jan 1;8(1):56-65. PM: 36326604.
McCarthy C, Li S, Wang TY, Raber I, Sandoval Y, Smilowitz NR, Wasfy JH, Pandey A, de Lemos JA, Kontos MC, Apple FS, Daniels LB, Newby LK, Jaffe AS, Januzzi JL. Implementation of High-Sensitivity Cardiac Troponin Assays in the United States. J Am Coll Cardiol 2023 Jan 24;81(3):207-219. PM: 36328155.
Mentz RJ, Anstrom KJ, Eisenstein EL, Sapp S, Greene SJ, Morgan S, Testani JM, Harrington AH, Sachdev V, Ketema F, Kim DY, Desvigne-Nickens P, Pitt B, Velazquez EJ. Effect of Torsemide vs Furosemide After Discharge on All-Cause Mortality in Patients Hospitalized With Heart Failure: The TRANSFORM-HF Randomized Clinical Trial. JAMA 2023 Jan 17;329(3):214-223. PM: 36648467.
Nelson MB, Shiroma EJ, Kitzman DW, Duncan PW, Reeves GR, Whellan DJ, Mentz RJ, Chen H, Pastva AM. Physical activity and relationship to physical function, quality of life, and cognitive function in older patients with acute decompensated heart failure. Am Heart J 2023 Feb;256:85-94. PM: 36372251.
Nelson AJ, Pagidipati NJ, Kelsey MD, Ardissino M, Aroda VR, Cavender MA, Lopes RD, Al-Khalidi HR, Braceras R, Gaynor T, Kaltenbach LA, Kirk JK, Lingvay I, Magwire ML, O’Brien EC, Pak J, Pop- Busui R, Richardson CR, Levya M, Senyucel C, Webb L, McGuire DK, Green JB, Granger CB. Coordinating Cardiology clinics randomized trial of interventions to improve outcomes (COORDINATE)-Diabetes: rationale and design. Am Heart J 2023 Feb;256:2-12. PM: 36279931.
Pagidipati NJ, Peterson ED. Can System Solutions Be Scaled to Control High Blood Pressure and Lipids? JAMA Cardiol 2023 Jan 1;8(1):21-22. PM: 36350615.
Pierce JB, Li Z, Greiner MA, Lippmann SJ, Hardy NC, Shen X, Stampehl M, Mentz RJ, Allen LA, Peterson PN, Fonarow GC, O’Brien EC, Greene SJ. Adoption of Sacubitril/Valsartan Among Patients With Heart Failure With Mildly Reduced or Preserved Ejection Fraction: The Get With The Guidelines-Heart Failure Registry. Circ Heart Fail 2023 Jan;16(1):e010176. PM: 36314141.
Saha A, Patel KV, Ayers C, Ballantyne CM, Correa A, Defilippi C, Hall ME, Mentz RJ, Seliger SL, Yimer W, Butler J, Berry JD, De Lemos JA, Pandey A. Longitudinal Changes in Cardiac Troponin and Risk of Heart Failure Among Black Adults. J Card Fail 2023 Jan;29(1):6-15. PM: 35690315.
Siddiqi TJ, Khan MS, Karimi Galougahi K, Shlofmitz E, Moses JW, Rao S, West NEJ, Wolff E, Hochler J, Chau K, Khalique O, Shlofmitz RA, Jeremias A, Ali ZA. Optical coherence tomography versus angiography and intravascular ultrasound to guide coronary stent implantation: A systematic review and meta-analysis. Catheter Cardiovasc Interv 2022 Nov;100 Suppl 1:S44-S56. PM: 36251325.
Subashi E, Feng L, Liu Y, Robertson S, Segars P, Driehuys B, Kelsey CR, Yin FF, Otazo R, Cai J. View-sharing for 4D magnetic resonance imaging with randomized projection-encoding enables improvements of respiratory motion imaging for treatment planning in abdominothoracic radiotherapy. Phys Imaging Radiat Oncol 2023 Jan 2;25:100409. PM: 36655213.
Talha KM, Butler J, Greene SJ, Aggarwal R, Anker SD, Claggett BL, Solomon SD, McMurray JJV, Vaduganathan M, Fonarow GC. Population-Level Implications of Sodium-Glucose Cotransporter-2 Inhibitors for Heart Failure With Preserved Ejection Fraction in the US. JAMA Cardiol 2023 Jan 1;8(1):66-73. PM: 36334258.
Weissler EH, Osazuwa-Peters OL, Greiner MA, Hardy NC, Kougias P, O’Brien SM, Mark DB, Jones WS, Secemsky EA, Vekstein AM, Shalhub S, Mussa FF, Patel MR, Vemulapalli S. Initial Thoracic Endovascular Aortic Repair vs Medical Therapy for Acute Uncomplicated Type B Aortic Dissection. JAMA Cardiol 2023 Jan 1;8(1):44-53. PM: 36334259.
Zanni MV, Foldyna B, McCallum S, Burdo TH, Looby SE, Fitch KV, Fulda ES, Autissier P, Bloomfield GS, Malvestutto CD, Fichtenbaum CJ, Overton ET, Aberg JA, Erlandson KM, Campbell TB, Ellsworth GB, Sheth AN, Taiwo B, Currier JS, Hoffmann U, Lu MT, Douglas PS, Ribaudo HJ, Grinspoon SK. Sex Differences in Subclinical Atherosclerosis and Systemic Immune Activation/Inflammation Among People With Human Immunodeficiency Virus in the United States. Clin Infect Dis 2023 Jan 13;76(2):323-334. PM: 36101518.
Division of Cardiology Publications Indexed in PubMed Jan 26 – Feb 1, 2023
Buschur KL, Riley C, Saferali A, Castaldi P, Zhang G, Aguet F, Ardlie KG, Durda P, Craig Johnson W, Kasela S, Liu Y, Manichaikul A, Rich SS, Rotter JI, Smith J, Taylor KD, Tracy RP, Lappalainen T, Graham Barr R, Sciurba F, Hersh CP, Benos PV. Distinct COPD subtypes in former smokers revealed by gene network perturbation analysis. Respir Res 2023 Jan 25;24(1):30. PM: 36698131.
Collins KA, Kraus WE, Rogers RJ, Hauser ER, Lang W, Jiang R, Schelbert EB, Huffman KM, Jakicic JM. Effect of behavioral weight-loss program on biomarkers of cardiometabolic disease risk: Heart Health Study randomized trial. Obesity (Silver Spring) 2023 Feb;31(2):338- 349. PM: 36621902.
Damluji AA, Rymer JA, Nanna MG. The Heterogeneity of Old Age: Healthy Aging in Older Adults Undergoing TAVR. JACC Cardiovasc Interv 2023 Jan 23;16(2):189-192. PM: 36697155.
Ding J, Lohman K, Molina A, Delbono O, Bertoni A, Shea S, Post W, Guo X, Barr RG, Manichaikul AW, Pankow JS, Rotter JI, Hoeschele I, Kritchevsky SB, Liu Y. The association between aging-related monocyte transcriptional networks and comorbidity burden: the Multi-Ethnic Study of Atherosclerosis (MESA). Geroscience 2023 Feb;45(1):197-207. PM: 35737188.
Douglas PS, McCallum S, Lu MT, Umbleja T, Fitch KV, Foldyna B, Zanni MV, Fulda ES, Bloomfield GS, Fichtenbaum CJ, Overton ET, Aberg JA, Malvestutto CD, Burdo TH, Arduino RC, Ho KS, Yin MT, Ribaudo HJ, Grinspoon SK. Ideal cardiovascular health, biomarkers, and coronary artery disease in persons with HIV. AIDS 2023 Mar 1;37(3):423-434. PM: 36525544.
Fanaroff AC, Lopes RD. COVID-19 Thrombotic Complications and Therapeutic Strategies. Annu Rev Med 2023 Jan 27;74:15-30. PM: 36130046.
Friedman DJ, Piccini JP. Device-Related Thrombus After Left Atrial Appendage Occlusion: The Villain of the Piece. JACC Clin Electrophysiol 2023 Jan;9(1):108- 110. PM: 36697188.
Greene SJ, Bauersachs J, Brugts JJ, Ezekowitz JA, Lam CSP, Lund LH, Ponikowski P, Voors AA, Zannad F, Zieroth S, Butler J. Worsening Heart Failure: Nomenclature, Epidemiology, and Future Directions: JACC Review Topic of the Week. J Am Coll Cardiol 2023 Jan 31;81(4):413-424. PM: 36697141.
Guadanhim LRS, Miot HA, Soares JLM, Silva SAM, Leonardi GR, Lopes RD, Bagatin E. Efficacy and Safety of Topical or Oral Hydrolyzed Collagen in Women with Dermatoporosis: A Randomized, Double-Blind, Factorial Design Study. Dermatol Ther (Heidelb) 2023 Feb;13(2):523- 534. PM: 36547800.
Lerman JB, Felker GM. Time to diuretics in acute heart failure: the tortoise or the hare? Eur J Heart Fail 2023 Jan;25(1):52-53. PM: 36350794.
Patel RB, Greene SJ, Xu H, Alhanti B, Peterson P, Yancy CW, Piccini J, Fonarow GC, Vaduganathan M. Intersection of atrial fibrillation and heart failure with mildly reduced and preserved ejection fraction in >400 000 participants in the Get With The Guidelines-Heart Failure Registry. Eur J Heart Fail 2023 Jan;25(1):63-73. PM: 36343200.
Peters AE, Wu A, Chiswell K, Hofmann P, Nkulikiyinka R, Dinh W, Piccini JP, Mentz RJ, Fudim M. Continuous Monitoring of Heart Rate Variability and Clinical Outcomes in Patients with Implantable Cardioverter Defibrillators. Curr Probl Cardiol 2023 Mar;48(3):101520. PM: 36455797.
Ptaszek LM, Koruth J, Santangeli P, Piccini JP, Ranjan R, Mahapatra S, Pipenhagen C, Fish JM, Moon LB, Ambrosius NM, Boudlali H, Jensen JA. Safe and effective delivery of high-power, short-duration radiofrequency ablation lesions with a flexible-tip ablation catheter. Heart Rhythm O2 2022 Oct 25;4(1):42-50. PM: 36713045.
Sidhu MS, Alexander KP, Huang Z, Mathew RO, Newman JD, O’Brien SM, Pellikka PA, Lyubarova R, Bockeria O, Briguori C, Kretov EL, Mazurek T, Orso F, Roik MF, Sajeev C, Shutov EV, Rockhold FW, Borrego D, Balter S, Stone GW, Chaitman BR, Goodman SG, Fleg JL, Reynolds HR, Maron DJ, et al. Cause-Specific Mortality in Patients With Advanced Chronic Kidney Disease in the ISCHEMIA-CKD Trial. JACC Cardiovasc Interv 2023 Jan23;16(2):209-218. PM: 36697158.
Turpie AGG, Farjat AE, Haas S, Ageno W, Weitz JI, Goldhaber SZ, Goto S, Angchaisuksiri P, Kayani G, Lopes RD, Chiang CE, Gibbs H, Tse E, Verhamme P, Ten Cate H, Muntaner J, Schellong S, Bounameaux H, Prandoni P, Maheshwari U, Kakkar AK. 36-month clinical outcomes of patients with venous thromboembolism: GARFIELD-VTE. Thromb Res 2023 Feb;222:31-39. PM: 36565677.
van Essen BJ, Tromp J, Ter Maaten JM, Greenberg BH, Gimpelewicz C, Felker GM, Davison BA, Severin T, Pang PS, Cotter G, Teerlink JR, Metra M, Voors AA. Characteristics and clinical outcomes of patients with acute heart failure with a supranormal left ventricular ejection fraction. Eur J Heart Fail 2023 Jan;25(1):35-42. PM:36114655.
Weitzman ER, Gaultney A, von Scheven E, Ringold S, Mann CM, Magane KM, Lin L, Leverty R, Dennos A, Hernandez A, Lippmann SJ, Dedeoglu F, Marin AC, Cox R, Reeve BB, Schanberg LE. Construct validity of Patient-Reported Outcomes Measurement Information System Paediatric measures in juvenile idiopathic arthritis and systemic lupus erythematosus: cross-sectional evaluation. BMJ Open 2023 Jan 27;13(1):e063675. PM: 36707118.
Duke Heart Pulse week ending January 29th 2023
Highlights of the week:
February is Heart Month; Wear Red Day: Friday, Feb. 3
We look forward to celebrating our incredible Duke Heart team throughout the month of February, also known as Heart Month. Please join us in celebrating National Wear Red Day on Friday, Feb. 3. Organization around the U.S. — including the National Heart Lung and Blood Institute (NHLBI), The Heart Truth®, and the American Heart Association (AHA) — celebrate National Wear Red Day annually on the first Friday in February to bring greater attention to heart disease as a leading cause of death for Americans.

On Wednesday, Feb. 1 we have a recruitment/hiring event in partnership with Duke Health HR for our adult heart step-down units. If you know someone who would be a great addition to our team, please let them know about this! Registration is required. Here is the link: Registration is via Qualtrics. The event runs from 8 a.m. to 2 p.m.
Friday, Feb. 3: National Wear Red Day. Send us photos of you and/or your teams sporting some red. We’ll share photos across the month in Pulse and on Twitter.
Feb. 12-18: Cardiac Rehabilitation Week & Cardiovascular Professionals Week
On Feb. 22, we’ll join our local AHA affiliate in offering DUHS staff the opportunity to join a one-hour virtual Hands-Only CPR Awareness Class. Stay tuned for more information on this to share with any Duke team member, especially those without a BLS requirement, who are interested in learning about compression-only CPR.
As we head into February, we thank you for all you do to help in the prevention and treatment of cardiovascular and thoracic diseases in our community, and as thought-leaders in the field. Our work is important – let’s keep up the momentum!
Recognizing Duke Heart’s Exercise Professionals
A belated happy Exercise Professionals Week to the Exercise Physiologist and Exercise Scientists in Duke Heart! We are proud to work with each of you every day. You provide excellent care to the patients in Duke Heart and they reap great benefits from your expertise! The CDU would not be as successful without you — thank you!
Shown here are the Heart CDU Exercise Physiologists celebrating last week at Full Steam in Durham (L-R: Jeff Mikitka, Ashley Swavely, Olivia Dobbin, Erin Young, Anna Gray, Matt Razdom, Jacque Fee).

Trailblazer: Starks Flies High with Promising AED Drone Delivery Network
The sudden cardiac arrest of the NFL’s Damar Hamlin on the playing field has stirred intense public interest in critical, life-saving interventions such as the rapid application of automated external defibrillators (AEDs). But Hamlin’s celebrated recovery is atypical. Survival probability for the 350,000 people who annually experience out-of-hospital cardiac arrest (OHCA) in the U.S. is just 10%, where it has stubbornly remained for more than 30 years.

Duke cardiology researcher Monique Starks, MD, MHS, is working to change that. Starks is the first investigator in the U.S. to be funded by the National Institutes of Health to explore development of a drone network that is capable of delivering AEDs to OHCA bystanders, and she’s flying high with some promising early observations.
Building on her work to improve OHCA emergency response times as a co-investigator in the ongoing RACE-CARs trial, Starks and her team have created mathematical simulation models to evaluate the impact of a drone-deployed AED network on treatment of OHCA. Early results show that response times can be reduced enough to meet the critical five-minute resuscitation window required to preserve good neurological function in survivors.
Optimizing Survival Probability
Historical RACE-CARS cardiac arrest data from 48 North Carolina counties shows median response time (from 911 call to AED arrival) can be improved from eight to seven minutes by equipping all first responders with AEDs. But by adding a drone network on top of that, Starks has shown that the median response time could fall to 4.8 minutes, meeting the critical five-minute resuscitation window.
“With a drone network that’s optimized for placement in strategic areas within each county, we believe that we can reduce the medium response time for most cardiac arrests to less than 5 minutes, which is tremendous,” says Starks, associate professor in the division of Cardiology and a member of the Duke Clinical Research Institute. Starks and a team of Duke researchers and engineers from the University of Toronto recently presented the data at the 2022 American Heart Association Scientific Sessions.
Despite the low survival probability for OHCA, survival rates of 40 to 60% can be achieved if defibrillation occurs within the first five minutes of collapse. However, defibrillation within this threshold is rare as 70% of cardiac arrests occur in the home. When a cardiac arrest occurs in public, it is rare to know whether an AED is nearby and a significant percentage of first responders do not carry an AED despite arrival to the scene of OHCA before paramedics. In North Carolina, the current rate of bystander defibrillation is 2% while nationally the rate is 4%.
Across the 48 North Carolina counties evaluated, only 16% of cardiac arrests have a response time (from 911 call to AED arrival) of less than five minutes. When a first responder AED intervention is added, the percentage increased to 22.3%. Starks found that further implementation of a drone network increased the percentage of OHCA receiving defibrillation within five minutes to 63%.
“We think equipping all first responders with AEDs is the low-hanging fruit but what we show with our mathematical study is that’s a drop in the bucket compared with what drone technology could do,” says Starks.
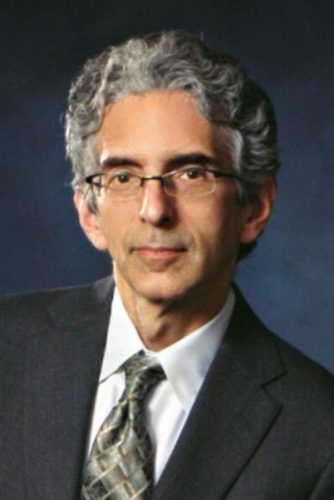 “The idea of using drones to deliver AEDs within a few minutes of a 911 call is almost 10 years old now and we are still years and a lot of research work away from being ready to do large scale community-based tests of this. But we think it’s worth the effort because in theory, we could get survival rates up to 30-40% or higher and from where we are now that would be a massive breakthrough,” says Starks’s research colleague and clinical cardiologist, Daniel Mark, MD, MPH, professor in the division of Cardiology and Director of Outcomes Research at the Duke Clinical Research Institute. “Dr. Starks is one of the leading investigators in the world working on this incredibly difficult and challenging opportunity.”
“The idea of using drones to deliver AEDs within a few minutes of a 911 call is almost 10 years old now and we are still years and a lot of research work away from being ready to do large scale community-based tests of this. But we think it’s worth the effort because in theory, we could get survival rates up to 30-40% or higher and from where we are now that would be a massive breakthrough,” says Starks’s research colleague and clinical cardiologist, Daniel Mark, MD, MPH, professor in the division of Cardiology and Director of Outcomes Research at the Duke Clinical Research Institute. “Dr. Starks is one of the leading investigators in the world working on this incredibly difficult and challenging opportunity.”
“At Duke, we have a history of innovative thinking around ways to increase survival for heart attacks and cardiac arrest,” adds Manesh Patel, MD, Richard S. Stack Distinguished Professor and chief of the division of Cardiology at Duke. “For example, the RACE-AMI pilot study we conducted around getting people to hospitals that can provide coronary intervention and care as soon as possible. Work led by Drs. (Christopher) Granger and (James) Jollis and many interventionalists helped build that network in NC, which was then adopted across the country by the American Heart Association as ‘Mission: Lifeline’. One can imagine this type of research for cardiac arrest survival — with innovations such as drone delivery for AED use — could also become a national standard if we can show this works.”
and cardiac arrest,” adds Manesh Patel, MD, Richard S. Stack Distinguished Professor and chief of the division of Cardiology at Duke. “For example, the RACE-AMI pilot study we conducted around getting people to hospitals that can provide coronary intervention and care as soon as possible. Work led by Drs. (Christopher) Granger and (James) Jollis and many interventionalists helped build that network in NC, which was then adopted across the country by the American Heart Association as ‘Mission: Lifeline’. One can imagine this type of research for cardiac arrest survival — with innovations such as drone delivery for AED use — could also become a national standard if we can show this works.”
New Directions
Starks estimates that five to eight drones would be needed for most counties in North Carolina to achieve five-minute arrival times for most cardiac arrest patients.
“We really need to move from a static AED delivery model such as the traditional public access defibrillation (AEDs placed in businesses and government institutions) to dynamic delivery (on-demand AED delivery to bystanders),” she adds. “This is where we hope to go in the U.S.”
The next step for Starks is testing over the next three months and pursuit of further funding for pilot programs with some of the 48 North Carolina counties she is working with.
“We’ve done the math now to show where they the drones are going to go and what the impact will be,” Starks says. “Now we need to work out some of the needed infrastructure and operational aspects of drone AED delivery because it’s not just a matter of flying a drone. Fully functional emergency drone networks are several years off, but we have a role to play now in establishing the effectiveness of this technology.”
This story originally ran in This Week in Medicine on Jan. 24. This is important and exciting work – well done!
STS Lillehei Lecture Given by Smith
 Peter K. Smith, MD, gave the C. Walton Lillehei Plenary Lecture on Monday, Jan. 23 at STS 2023 in San Diego. The title of his lecture was Treatment Selection for Coronary Artery Disease: The Collision of a Belief System with Evidence. Dr. Smith recognized his many teachers over the years, including Drs. David C. Sabiston, Jr., Walter Wolfe, and Robert H. Jones — as well as his mentees – during his presentation. On Twitter, CT surgery trainee Dr. Julie Doberne wrote, “Dr. Smith, you have embodied the unwavering pursuit of truth in the field of cardiac surgery for the last several decades. Thank you for your lasting gifts to our profession. It is an honor to know you.”
Peter K. Smith, MD, gave the C. Walton Lillehei Plenary Lecture on Monday, Jan. 23 at STS 2023 in San Diego. The title of his lecture was Treatment Selection for Coronary Artery Disease: The Collision of a Belief System with Evidence. Dr. Smith recognized his many teachers over the years, including Drs. David C. Sabiston, Jr., Walter Wolfe, and Robert H. Jones — as well as his mentees – during his presentation. On Twitter, CT surgery trainee Dr. Julie Doberne wrote, “Dr. Smith, you have embodied the unwavering pursuit of truth in the field of cardiac surgery for the last several decades. Thank you for your lasting gifts to our profession. It is an honor to know you.”
We feel the same way. Your patients and our team have all been blessed to learn from you!

Turek, DeBlasio to Receive 2022-2023 Duke Presidential Award
Congratulations to Duke Heart chief of pediatric cardiothoracic surgery, Joe Turek, and to former Duke CTICU nurse Joe DeBlasio – this week we learned they have been named recipients of Duke University’s highest possible honor for faculty and staff: The Duke Presidential Award.

Turek and DeBlasio are two of eight individuals and five teams selected for the honor, which will be presented during a 4 p.m. ceremony on Tuesday, Feb. 28 in Page Auditorium. The awards are organized by the Office of the President in partnership with Duke Human Resources and honor teams and individuals who best demonstrate Duke’s core values of respect, trust, inclusion, discovery and excellence.
will be presented during a 4 p.m. ceremony on Tuesday, Feb. 28 in Page Auditorium. The awards are organized by the Office of the President in partnership with Duke Human Resources and honor teams and individuals who best demonstrate Duke’s core values of respect, trust, inclusion, discovery and excellence.
Congratulations Joe and Joe!
To read more about the 2022-2023 Presidential Award winners, please see Duke Today.
Krasuski is New Chair of ACHA Medical Advisory Board
Congratulations to Richard Krasuski! On January 22, he began a 3-year term as the Chair of the Medical Advisory Board of the Adult Congenital Heart Association (ACHA). This group of top physicians and healthcare providers in the congenital heart disease (CHD) field provides expert input and advice for all ACHA activities involving medical, scientific and/or medical profession-related content. They offer expert opinions on research and medical developments in CHD and the needs of the CHD  population, and assure that ACHA policies meet the highest standards of scientific need and accuracy.
population, and assure that ACHA policies meet the highest standards of scientific need and accuracy.
Krasuski says he is most looking forward to contributing more on a national policy level. He says the ACHA has been instrumental in bringing awareness to the plight of the over 2 million adults with CHD and the specialized care they require – and that evolving legislation will help to further procure the resources necessary to grow this rapidly growing and evolving specialty.
“Duke was one of the original medical centers to recognize the future needs of this complex patient population and has a rich history of training the current leaders in the field,” says Krasuski. “I think this is another accolade demonstrating the important role that Duke is playing in the evolution of the field. Internally at Duke, we have tremendous collaboration with several specialty programs including Pediatric Cardiology, Adult and Pediatric Cardiothoracic Surgery, Hepatology, and Heart Failure and Transplantation just to name a few. The Duke program has been a national leader in the three-core elements of an academic medical program – clinical care, research, and education – and I see a great future ahead of us.”
The ACHA was founded in 1998 as a national nonprofit organization with the mission to improve and extend the lives of millions born with congenital heart disease, through education, advocacy, and the promotion of research. Currently, ACHA has a membership of more than 14,000 patients and professionals and is the largest worldwide patient and professional organization representing Adult Congenital Heart Disease.
Congratulations, Rich!
Jackson Selected for 2023 Duke Clinical Leadership Program
Congratulations to Larry Jackson, MD! He is one of 28 School of Medicine faculty members selected for the 2023 Clinical  Leadership Program cohort. The Duke Clinical Leadership Program (DCLP) was founded by the Chancellor for Health Affairs in 2010 to help expand leadership capacity within Duke Health. The program provides faculty with an opportunity to deepen their awareness of healthcare operations and to develop relevant leadership skills. The program is run by the School of Medicine Office for Faculty.
Leadership Program cohort. The Duke Clinical Leadership Program (DCLP) was founded by the Chancellor for Health Affairs in 2010 to help expand leadership capacity within Duke Health. The program provides faculty with an opportunity to deepen their awareness of healthcare operations and to develop relevant leadership skills. The program is run by the School of Medicine Office for Faculty.
Congratulations, Larry!
Jacqueline Fee named Clinical Operations Supervisor, CDU
Duke Heart is pleased to announce that Jacque Fee, BS, MS ACSM-RCEP, will become Clinical Operations Supervisor for the DUH Cardiac Diagnostic Unit (CDU) effective Wednesday, Feb. 1. As Clinical Operations Supervisor she will have shared oversight of the CDU sonographers, cardiac technicians and exercise physiologists with Ashlee Davis for the management of clinical operations.
 Jacque earned a Bachelor of Science in Sports Biology in 2012, followed by a Master of Science in Clinical Exercise Physiology at Springfield College in 2015. Her credentials include American College of Sports Medicine Registered Clinical Exercise Physiologist.
Jacque earned a Bachelor of Science in Sports Biology in 2012, followed by a Master of Science in Clinical Exercise Physiology at Springfield College in 2015. Her credentials include American College of Sports Medicine Registered Clinical Exercise Physiologist.
She began her career as a Clinical Exercise Physiologist at Beth Israel Deaconess Medical Center (BIDMC) in Boston, MA in 2014, advancing to Senior Clinical Exercise Physiologist while there. While at BIDMC she assisted in managing their student internship program and managed the emergency equipment and procedures for the Stress Lab.
Jacque joined the Duke Heart team in 2021 as an Exercise Physiologist in the DUH CDU. During her time at Duke, she has advanced to Exercise Physiologist, Level II, led efforts to evaluate cardiopulmonary reporting procedures, facilitated a switch from sterile processing to high level disinfectant for cardiopulmonary equipment and has led educational initiatives for staff and is a member of the Orientation Committee in the CDU. She is also an active member of the American College of Sports Medicine.
When she is not at Duke you can find her out on the trails for a run, reading a book or journal article, or cooking!
Congratulations, Jacque!
SOM Faculty Achievement Award Nominations due this Week
Nominations and Applications for the 2023 School of Medicine Faculty Awards are now open.
The Faculty Awards are a wonderful opportunity to highlight the outstanding work conducted at Duke. The Office for Faculty is now accepting nominations and applications for the following 2023 faculty awards:
- Leonard Palumbo Jr., MD Faculty Achievement Award – Nomination Deadline: January 31, 2023
- Leonard B. Tow Humanism in Medicine Award – Nomination Deadline has passed
- Excellence in Professionalism Award – Nomination Deadline: February 10, 2023
- Research Mentoring Awards – Nomination Deadline: February 20, 2023
- Ruth and A. Morris Williams Faculty Research Prize – Application Deadline: February 28, 2023
To learn more, visit https://duke.is/4hqkb. Questions? Please contact Jennifer Meyer Dare, jennifer.meyer-dare@duke.edu. Nominations and applications should be submitted via email to facdev@dm.duke.edu.
Upcoming Events & Opportunities
Cardiology Grand Rounds
Jan. 31: Branched-Chain Amino Acids and Cardiometabolic Disease: Biomarkers and Beyond with Robert McGarrah. 5 p.m., Zoom.
Medicine Grand Rounds
Feb.17: Topic TBD with Hyung (Harry) Jin Cho of NYU Langone Health, a 2023 Joseph C. Greenfield Visiting Professor. 8 a.m. via Zoom or in person, Duke North 2002.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
January 20 — Katherine Collins (Duke Molecular Physiology Institute)
Healio/Endocrinology
Weight loss of 10% significantly affects insulin resistance, cardiometabolic biomarkers
https://duke.is/2vupd
January 23 — Nandini Abburi (Neurology)
CBS17.com/WNCN (Raleigh-Durham)
Stroke symptoms require emergency treatment even if symptoms go away quickly, new report says
https://duke.is/vxhkx
January 24 — Michael Pencina
Healio/Cardiology
Risk scores, algorithms less accurate in stroke prediction in Black vs. white adults
https://duke.is/z9med
January 24 — Michael Pencina
Neurology Live
Assessing Stroke Risk With Algorithms and Modeling Health Discrimination
https://duke.is/bjryq
January 24 — Robert Mentz
HealthDay
Mortality Similar With Torsemide, Furosemide for Patients Hospitalized With Heart Failure
https://duke.is/nmspa
*carried by 78 additional news outlets including in Buffalo, Miami & Washington, DC
January 24 — Reid Chamberlain (pediatric cardiology)
WFMY-2/CBS News (Greensboro, NC)
https://duke.is/czgku
January 25 — Michael Pencina
WUNC-FM/NC Public Radio
AI Models Fail Black Americans in Stroke Assessment
https://duke.is/rxu23
*news clip begins @ 10:04:51
January 25 — Richard Shannon
Becker’s Hospital Review
6 clinical leaders on hospital accreditation visit prep: Act now, don’t react later
https://duke.is/prgzm
January 26 — Michael Pencina
Reuters
Health Rounds: Stroke prediction tools failing Black patients
https://duke.is/bkgzd
Duke Heart Week ending January 22nd 2023
Highlights of the week:
Tong Named Recipient of Inaugural STS/WTS Award
 Congratulations to Betty Tong, MD! Tong has been named one of three inaugural recipients of the Extraordinary Women in Cardiothoracic Surgery Award. The news was announced yesterday, Jan. 21, 2023 during the 59th annual meeting of the Society of Thoracic Surgeons (STS) being held Jan. 21-23 at the Hilton Bayfront in San Diego.
Congratulations to Betty Tong, MD! Tong has been named one of three inaugural recipients of the Extraordinary Women in Cardiothoracic Surgery Award. The news was announced yesterday, Jan. 21, 2023 during the 59th annual meeting of the Society of Thoracic Surgeons (STS) being held Jan. 21-23 at the Hilton Bayfront in San Diego.
The award, which is co-sponsored by the STS and Women in Thoracic Surgery, was established to recognize outstanding women surgeons specializing in the cardiothoracic space. The award celebrates those who have achieved excellence and innovation in clinical practice and who demonstrate integrity, leadership, mentorship, creativity, and advocacy on behalf of the specialty, patient population or fellow surgeons and trainees.
“Please join me in congratulating our own Dr. Betty Tong for winning this inaugural award,” said Dr. Edward P. Chen, chief of the division of cardiovascular and thoracic surgery at Duke. “This is a tremendous honor led by the WTS and STS in recognizing the outstanding achievements of women thoracic surgeons. We are truly blessed and privileged to have Dr. Tong on our faculty at Duke.”
Tong is an associate professor of surgery in the division of cardiovascular and thoracic surgery at Duke, and a member of the Duke Cancer Institute. Fellow inaugural recipients of the award include Leah Backhus, MD, thoracic surgeon at Stanford Medicine, and Jennifer Ellis, MD, thoracic surgeon at NYU Langone Health.
Shown in images are members of the Duke CT Surgery team at STS, Tong speaking at the STS award presentation, and the three recipients of the inaugural award – (L-R) Drs. Backhus, Ellis, and Tong.
Well-deserved, Betty! You truly are a rock-star mentor, surgeon, and colleague. Congratulations!


Smith to Present STS Lillehei Lecture
Former cardiovascular and thoracic division chief Peter K. Smith, MD, will present the C. Walton Lillehei Plenary Lecture tomorrow, 9 a.m. PST, at STS 2023 in San Diego. Congratulations, Peter!

Palma to Receive ASE Teaching Award
We learned this week that Richard Palma, Program Director and Clinical Coordinator of the Cardiac Ultrasound Certificate Program at Duke, will join Madhav Swaminathan among the distinguished awardees at the American Society of  Echocardiography 2023 Scientific Sessions. Palma has been named the recipient of ASE’s 2023 Cardiovascular Sonographer Distinguished Teacher Award.
Echocardiography 2023 Scientific Sessions. Palma has been named the recipient of ASE’s 2023 Cardiovascular Sonographer Distinguished Teacher Award.
The award will be formally announced during ASE’s annual awards presentations at the 34th Annual Scientific Sessions on Saturday, June 24, 2023, at Gaylord National Resort, National Harbor, in Prince George’s County, MD.
Palma is an Advanced Cardiac Sonographer and teaches echocardiography to students, staff, and Duke Cardiology fellows. He is internationally known as an educator of echocardiography and ultrasound physics (ESP Ultrasound).
This is the second national teaching award for Palma. In 2011 he was named recipient of the Society of Diagnostic Medical Sonography’s Distinguished Educator award.
Congratulations, Richie – this is well-deserved!
Deadlines Approaching for SOM Faculty Award Noms
Nominations and Applications for the 2023 School of Medicine Faculty Awards are now open.
The Faculty Awards are a wonderful opportunity to highlight the outstanding work conducted at Duke. The Office for Faculty is now accepting nominations and applications for the following 2023 faculty awards:
- Leonard Palumbo Jr., MD Faculty Achievement Award – Nomination Deadline: January 31, 2023
- Leonard B. Tow Humanism in Medicine Award – Nomination Deadline: January 27, 2023
- Excellence in Professionalism Award – Nomination Deadline: February 10, 2023
- Research Mentoring Awards – Nomination Deadline: February 20, 2023
- Ruth and A. Morris Williams Faculty Research Prize – Application Deadline: February 28, 2023
To learn more, visit https://duke.is/4hqkb. Questions? Please contact Jennifer Meyer Dare, jennifer.meyer-dare@duke.edu. Nominations and applications should be submitted via email to facdev@dm.duke.edu.
Adult Heart Stepdown Hiring Event – Feb. 1
Know someone who would make a great team member in Duke Heart? We have an opportunity for them to learn more about us! Our adult heart stepdown units, in partnership with Duke Health HR, will hold a hiring event on Wed., Feb. 1. Registration is required.
Interested parties can register to join our drop-in Duke Health event 8 a.m. to 2 p.m. Wednesday, February 1, to learn more about a career filled with purpose and opportunity on the Heart Adult Stepdown Units at Duke University Hospital.
At the event, they will have the opportunity to tour Duke University Hospital; learn about the many benefits of working in our health system; and meet recruiters and hiring managers for a potential same day offer.
Please share! Registration is via Qualtrics.
Upcoming Events & Opportunities
Cardiology Grand Rounds
Jan. 24: CGR is cancelled for this week.
Medicine Grand Rounds
Jan. 27: CHIP Focus Group Presentation with cardiovascular fellow Jessica Regan and hematology-oncology fellow Bennett Caughey. 8 a.m. via Zoom or in person, Duke North 2002.
Feb.17: Topic TBD with Hyung (Harry) Jin Cho of NYU Langone Health, a 2023 Joseph C. Greenfield Visiting Professor. 8 a.m. via Zoom or in person, Duke North 2002.
DOM Clinical Research Resource Fair
Wednesday, January 25, 6th Floor, Trent Semans Building
The DOM Clinical Research Units (CRUs), which include Heart Center, Medicine and Oncology clinical research, invite faculty, fellows, residents and trainees to a clinical research resources fair to help connect you directly to resources available at Duke.
While information will be available on tables all day, representatives from each group will be available to informally meet with you in two open sessions: 8:30-10 am and 1-2:30 pm. CRU personnel hope you will consider joining for one of these sessions so you can meet those who support your clinical research work.
A light breakfast, coffee and juice will be provided during the morning session and after-lunch snacks will be available for the afternoon session. Additionally, all attendees will be entered into a drawing for a Starbucks gift card.
February is Heart Month
Feb. 3: National Wear Red Day. We encourage everyone to wear red on Friday, Feb. 3 to show our support for heart health overall, but especially to support women and cardiovascular disease awareness. Get your red gear ready!

Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
January 17 — Nishant Shah
Healio/Cardiology
Bromocriptine appears to drop BP, improve arterial stiffness in teens with type 1 diabetes
https://duke.is/rbqxq
January 17 — Robert Mentz
NIH/News Release
Comparison of diuretics shows no difference in heart failure survival
https://duke.is/5gzkr
January 17 — Nima Moghaddam
Healio/Cardiology
Most patients admitted for acute HF qualify for guideline-directed quadruple therapy
https://duke.is/ndmcx
January 17 — Magnus Ohman
Medscape/The Bob Harrington Show
The Career Pivot: Leaving Clinical Medicine for a While — or for Good
https://duke.is/be7r6
January 18 — Richard Shannon
Becker’s Hospital Review
The top items on 5 chief medical officers’ to-do lists
https://duke.is/zmcge
January 18 — Robert Mentz
Medical Dialogues
https://duke.is/6r7eb
January 18 — Robert Mentz
Patient Care Online
Comparison of Loop Diuretics Shows No Difference in Heart Failure Survival
https://duke.is/pbct7
January 18 — Robert Mentz
Medscape
Clarity on Torsemide vs Furosemide in HF: TRANSFORM-HF Published
https://duke.is/4tyvw
January 19 — Susanna Naggie and Adrian Hernandez
The Atlantic
Trying to Stop Long COVID Before It Even Starts
https://duke.is/9uq8a
January 19 — Robert Mentz
U.S. News & World Report/HealthDay News*
Is There a Best Diuretic Drug for Heart Failure?
https://duke.is/25mmy
*also carried by additional 146 news outlets including in Atlanta, Chicago & San Francisco markets
January 19 — Richard Shannon
Becker’s Hospital Review
Band-Aid solutions won’t bring nurses back to the bedside, Duke Health’s Dr. Richard Shannon says
Division of Cardiology Publications: December 14, 2022–January 10, 2023
Akinmolayemi O, Ozdemir D, Pibarot P, Zhao Y, Leipsic J, Douglas PS, Jaber WA, Weissman NJ, Blanke P, Hahn RT. Clinical and Echocardiographic Characteristics of Flow- Based Classification Following Balloon-Expandable Transcatheter Heart Valve in PARTNER Trials. JACC Cardiovasc Imaging 2023;16(1):1-9. PM: 36599555.
Alenezi F, Alajmi H, Agarwal R, Zwischenberger BA. Role of cardiac magnetic resonance (CMR) in planning ventricular septal myomectomy in patients with hypertrophic obstructive cardiomyopathy (HOCM). J Card Surg 2022;37(12):4186-4189. PM: 36434805.
Almas A, Awan S, Bloomfield G, Nisar MI, Siddiqi S, Ahmed A, Ali A, Shafqat SH, Bhutta ZA, Mark DB, Douglas P, Bartlett J, Jafar TH, Samad Z. Opportunities and challenges to non-communicable disease (NCD) research and training in Pakistan: a qualitative study from Pakistan. BMJ Open 2022;12(12):e066460. PM: 36535721.
Bagai A, Ali FM, Gregson J, Alexander KP, Cohen MG, Sundell KA, Simon T, Westermann D, Yasuda S, Brieger D, Goodman SG, Nicolau JC, Granger CB, Pocock S. Multimorbidity, functional impairment, and mortality in older patients stable after prior acute myocardial infarction: Insights from the TIGRIS registry. Clin Cardiol 2022;45(12):1277-1286. PM: 36317424.
Bashir M, Jubouri M, Chen EP, Mariscalco G, Narayan P, Bailey DM, Awad WI, Williams IM, Velayudhan B, Mohammed I. Cardiothoracic surgery leadership and learning are indispensable to each other. J Card Surg 2022;37(12):4204-4206. PM: 36345687.
Bonaca MP, Szarek M, Debus ES, Nehler MR, Patel MR, Anand SS, Muehlhofer E, Berkowitz SD, Haskell LP, Bauersachs RM. Efficacy and safety of rivaroxaban versus placebo after lower extremity bypass surgery: A post hoc analysis of a “CASPAR like” outcome from VOYAGER PAD. Clin Cardiol 2022;45(12):1143-1146. PM: 36251249.
Carlisle MA, Shrader P, Fudim M, Pieper KS, Blanco RG, Fonarow GC, Naccarelli GV, Gersh BJ, Reiffel JA, Kowey PR, Steinberg BA, Freeman JV, Ezekowitz MD, Singer DE, Allen LA, Chan PS, Pokorney SD, Peterson ED, Piccini JP. Residual stroke risk despite oral anticoagulation in patients with atrial fibrillation. Heart Rhythm O2 2022;3(6Part A):621-628. PM: 36589908.
Chaudhry SP, DeVore AD, Vidula H, Nassif M, Mudy K, Birati EY, Gong T, Atluri P, Pham D, Sun B, Bansal A, Najjar SS. Left Ventricular Assist Devices: A Primer For the General Cardiologist. J Am Heart Assoc 2022;11(24):e027251. PM: 36515226.
Choi J, Lee S, Motter JN, Kim H, Andrews H, Doraiswamy PM, Devanand DP, Goldberg TE. Models of depressive pseudoamnestic disorder. Alzheimers Dement (N Y) 2022;8(1):e12335. PM: 36523848.
Chugunov IA, Mareev YV, Fudim M, Mironova NA, Mareev VY, Davtyan RV. [Cardiac contractility modulation in heart failure with reduced ejection fraction treatment]. Kardiologiia 2022;62(11):71-78. PM: 36521047.
Coniglio AC, Kittipibul V, Pelligra R, Richardson ES, Holley CL, Fudim M. One Small Step for a Patient, One Giant Leap for Orthostatic Hypotension. Cureus 2022;14(11):e31612. PM: 36540476.
Cox CE, Gu J, Ashana DC, Pratt EH, Haines K, Ma J, Olsen MK, Parish A, Casarett D, Al-Hegelan MS, Naglee C, Katz JN, O’Keefe YA, Harrison RW, Riley IL, Bermejo S, Dempsey K, Johnson KS, Docherty SL. Trajectories of Palliative Care Needs in the ICU and Long-Term Psychological Distress Symptoms. Crit Care Med 2023;51(1):13-24. PM: 36326263.
Cremer PC, Geske JB, Owens A, Jaber WA, Harb SC, Saberi S, Wang A, Sherrid M, Naidu SS, Schaff H, Smedira NG, Wang Q, Wolski K, Lampl KL, Sehnert AJ, Nissen SE, Desai MY. Myosin Inhibition and Left Ventricular Diastolic Function in Patients With Obstructive Hypertrophic Cardiomyopathy Referred for Septal Reduction Therapy: Insights From the VALOR-HCM Study. Circ Cardiovasc Imaging 2022;15(12):e014986. PM: 36335645.
de la Espriella R, Cobo M, Santas E, Verbrugge FH, Fudim M, Girerd N, Miñana G, Górriz JL, Bayés- Genís A, Núñez J. Assessment of filling pressures and fluid overload in heart failure: an updated perspective. Rev Esp Cardiol (Engl Ed) 2023 Jan;76(1):47- 57. PM: 35934293.
Eiger DS, Inoue LYT, Li Q, Bardy G, Lee K, Poole J, Mark D, Samad Z, Friedman D, Fishbein D, Sanders G, Al-Khatib SM. Factors and outcomes associated with improved left ventricular systolic function in patients with cardiomyopathy. Cardiol J 2022;29(6):978-984. PM: 33438181.
Essien UR, Chiswell K, Kaltenbach LA, Wang TY, Fonarow GC, Thomas KL, Turakhia MP, Benjamin EJ, Rodriguez F, Fang MC, Magnani JW, Yancy CW, Piccini JP. Association of Race and Ethnicity With Oral Anticoagulation and Associated Outcomes in Patients With Atrial Fibrillation: Findings From the Get With The Guidelines-Atrial Fibrillation Registry. JAMA Cardiol 2022;7(12):1207-1217. PM: 36287545.
Garcia A, Lee J, Balasubramanian V, Gardner R, Gummidipundi SE, Hung G, Ferris T, Cheung L, Desai S, Granger CB, Hills MT, Kowey P, Nag D, Rumsfeld JS, Russo AM, Stein JW, Talati N, Tsay D, Mahaffey KW, Perez MV, Turakhia MP, Hedlin H, Desai M. The development of a mobile app-focused deduplication strategy for the Apple Heart Study that informs recommendations for future digital trials. Stat (Int Stat Inst) 2022;11(1):e470. PM: 36589778.
Haddad F, Cauwenberghs N, Daubert MA, Kobayashi Y, Bloomfield GS, Fleischman D, Koweek L, Maron DJ, Rodriguez F, Liao YJ, Moneghetti K, Amsallem M, Mega J, Hernandez A, Califf R, Mahaffey KW, Shah SH, Kuznetsova T, Douglas PS. Association of left ventricular diastolic function with coronary artery calcium score: A Project Baseline Health Study. J Cardiovasc Comput Tomogr 2022;16(6):498-508. PM: 35872137.
Haji M, Lopes VV, Ge A, Halladay C, Soares C, Shah NR, Longenecker CT, Lally M, Bloomfield GS, Shireman TI, Ross D, Sullivan JL, Rudolph JL, Wu WC, Erqou S. Two decade trends in cardiovascular disease outcomes and cardiovascular risk factors among US veterans living with HIV. Int J Cardiol Cardiovasc Risk Prev 2022;15:200151. PM: 36573195.
Harrington J, Granger CB. Bleeding and risk for future cardiovascular events in patients with atrial fibrillation on oral anticoagulation: major bleeding is a major problem. Eur Heart J 2022;43(47):4909-4911. PM: 36380455.
Hassan-Tash P, Ismail U, Kirkpatrick IDC, Ravandi A, Jassal DS, Hiebert B, Kass M, Krasuski RA, Shah AH. Correlation of Impedance Cardiography-Derived and Cardiac Magnetic Resonance-Derived Stroke Volumes. Curr Probl Cardiol 2023;48(2):101457. PM: 36273652.
Hochman JS, Anthopolos R, Reynolds HR, Bangalore S, Xu Y, O’Brien SM, Mavromichalis S, Chang M, Contreras A, Rosenberg Y, Kirby R, Bhargava B, Senior R, Banfield A, Goodman SG, Lopes RD, Pracoń R, López-Sendón J, Maggioni AP, Newman JD, Berger JS, Sidhu MS, White HD, Troxel AB. Survival After Invasive or Conservative Management of Stable Coronary Disease. Circulation 2023;147(1):8-19. PM: 36335918.
Jackson LR, Holmqvist F, Parish A, Green CL, Piccini JP, Bahnson TD. Safety of continuous left atrial phased-array intracardiac echocardiography during left atrial ablation for atrial fibrillation. Heart Rhythm O2 2022;3(6Part A):673-680. PM: 36589913.
Karatela MF, Fudim M, Mathew JP, Piccini JP. Neuromodulation therapy for atrial fibrillation. Heart Rhythm 2023;20(1):100-111. PM: 35988908.
Kiernan K, Dodge SE, Kwaku KF, Jackson LR, Zeitler EP. Racial and ethnic differences in implantable cardioverter-defibrillator patient selection, management, and outcomes. Heart Rhythm O2 2022;3(6Part B):807-816. PM: 36589011.
Kotecha D, DeVore AD, Asselbergs FW. Fit for the future: empowering clinical trials with digital technology. Eur Heart J 2023;44(1):64-67. PM: 36369983.
Krychtiuk KA, Granger CB. In older men, an invitation for comprehensive CV screening did not reduce death at 5.6 y. Ann Intern Med 2022;175(12):JC140. PM: 36469924.
Krychtiuk KA, Rader DJ, Granger CB. RNA-targeted therapeutics in cardiovascular disease: the time is now. Eur Heart J Cardiovasc Pharmacother 2022;9(1):94-99. PM: 36138490.
Laffin LJ, Bruemmer D, Garcia M, Brennan DM, McErlean E, Jacoby DS, Michos ED, Ridker PM, Wang TY, Watson KE, Hutchinson HG, Nissen SE. Comparative Effects of Low-Dose Rosuvastatin, Placebo, and Dietary Supplements on Lipids and Inflammatory Biomarkers. J Am Coll Cardiol 2023;81(1):1-12. PM: 36351465.
Maron MS, Masri A, Choudhury L, Olivotto I, Saberi S, Wang A, Garcia-Pavia P, Lakdawala NK, Nagueh SF, Rader F, Tower-Rader A, Turer AT, Coats C, Fifer MA, Owens A, Solomon SD, Watkins H, Barriales-Villa R, Kramer CM, Wong TC, Paige SL, Heitner SB, Kupfer S, Malik FI, Meng L, et al. Phase 2 Study of Aficamten in Patients With Obstructive Hypertrophic Cardiomyopathy. J Am Coll Cardiol 2023;81(1):34-45. PM: 36599608.
Marquis-Gravel G, Boivin-Proulx LA, Huang Z, Zelenkofske SL, Lincoff AM, Mehran R, Steg PG, Bode C, Alexander JH, Povsic TJ. Femoral Vascular Closure Devices and Bleeding, Hemostasis, and Ambulation Following Percutaneous Coronary Intervention. J Am Heart Assoc 2023;12(1):e025666. PM: 36583436.
Marx N, Cheng AYY, Agarwal R, Greene SJ, Abuhantash H. Heart failure with reduced ejection fraction and the intersection of cardio-renal-metabolic medicine #CaReMe. Eur Heart J Suppl 2022;24(Suppl L):L29-L37. PM: 36545231.
Mc Causland FR, Singh AK, Claggett BL, Carroll K, Wittes J, McMurray JJV, Perkovic V, Snapinn S, Lopes RD, Solomon SD. Daprodustat and On-Treatment Cardiovascular Events in Chronic Kidney Disease. Reply. N Engl J Med 2022;387(26):2482- 2485. PM: 36577112.
Metra M, Pagnesi M, Claggett BL, Díaz R, Felker GM, McMurray JJV, Solomon SD, Bonderman D, Fang JC, Fonseca C, Goncalvesova E, Howlett JG, Li J, O’Meara E, Miao ZM, Abbasi SA, Heitner SB, Kupfer S, Malik FI, Teerlink JR. Effects of omecamtiv mecarbil in heart failure with reduced ejection fraction according to blood pressure: the GALACTIC-HF trial. Eur Heart J 2022;43(48):5006-5016. PM: 35675469.
Minhas AMK, Abramov D, Chung JS, Patel J, Mamas MA, Zieroth S, Agarwal R, Fudim M, Rabkin DG. Current status of perioperative temporary mechanical circulatory support during cardiac surgery. J Card Surg 2022;37(12):4304-4315. PM: 36229948.
Minhas AMK, Jain V, Li M, Ariss RW, Fudim M, Michos ED, Virani SS, Sperling L, Mehta A. Family income and cardiovascular disease risk in American adults. Sci Rep 2023;13(1):279. PM: 36609674.
Mohebi R, Liu Y, Felker GM, Prescott MF, Piña IL, Butler J, Ward JH, Solomon SD, Januzzi JL. Prediction of Left Ventricular Ejection Fraction Change Following Treatment With Sacubitril/Valsartan. JACC Heart Fail 2023;11(1):44-54. PM: 36599549.
Mohebi R, Liu Y, Felker GM, Prescott MF, Ward JH, Piña IL, Butler J, Solomon SD, Januzzi JL. Heart Failure Duration and Mechanistic Efficacy of Sacubitril/Valsartan in Heart Failure With Reduced Ejection Fraction. J Card Fail 2022;28(12):1673-1682. PM: 36122820.
O’Brien EC, Mulder H, Jones WS, Hammill BG, Sharlow A, Hernandez AF, Curtis LH. Concordance Between Patient-Reported Health Data and Electronic Health Data in the ADAPTABLE Trial. JAMA Cardiol 2022;7(12):1235-1243. PM: 36322059.
Paluch AE, Bajpai S, Ballin M, Bassett DR, Buford TW, Carnethon MR, Chernofsky A, Dooley EE, Ekelund U, Evenson KR, Galuska DA, Jefferis BJ, Kong L, Kraus WE, Larson MG, Lee IM, Matthews CE, Newton RL, Nordström A, Nordström P, Palta P, Patel AV, Pettee Gabriel K, Pieper CF, et al. Prospective Association of Daily Steps With Cardiovascular Disease: A Harmonized Meta-Analysis. Circulation 2023;147(2):122-131. PM: 36537288.
Park S, Ma Z, Zarkada G, Papangeli I, Paluri S, Nazo N, Rivera-Molina F, Toomre D, Rajagopal S, Chun HJ. Endothelial β-arrestins regulate mechanotransduction by the type II bone morphogenetic protein receptor in primary cilia. Pulm Circ 2022;12(4):e12167. PM: 36532314.
Patel SM, Qamar A, Giugliano RP, Jarolim P, Marston NA, Park JG, Blazing MA, Cannon CP, Braunwald E, Morrow DA. Association of Serial High-Sensitivity Cardiac Troponin T With Subsequent Cardiovascular Events in Patients Stabilized After Acute Coronary Syndrome: A Secondary Analysis From IMPROVE-IT. JAMA Cardiol 2022;7(12):1199-1206. PM: 36260325.
Peters AE, Mentz RJ, Sun JL, Harrington JL, Fudim M, Alhanti B, Hernandez AF, Butler J, Starling RC, Greene SJ. Patient-reported and Clinical Outcomes Among Patients Hospitalized for Heart Failure With Reduced Versus Preserved Ejection Fraction. J Card Fail 2022;28(12):1652-1660. PM: 35688408.
Piccini JP, Russo AM, Sharma PS, Kron J, Tzou W, Sauer W, Park DS, Birgersdotter-Green U, Frankel DS, Healey JS, Hummel J, Koruth J, Linz D, Mittal S, Nair DG, Nattel S, Noseworthy PA, Steinberg BA, Trayanova NA, Wan EY, Wissner E, Zeitler EP, Wang PJ. Advances in Cardiac Electrophysiology. Circ Arrhythm Electrophysiol 2022;15(12):e009911. PM: 36441565.
Popovic B, Ducrocq G, Elbez Y, Bode C, Mehta SR, Pollack CV, Sabate M, Rao SV, Parkhomenko A, Feldman LJ, Sayah N, Sabatine MS, Steg PG. Clinical Significance of Culprit Vessel Occlusion in Patients With Non-ST-Elevation Myocardial Infarction Who Underwent Percutaneous Coronary Intervention. Am J Cardiol 2023;188:95-101. PM: 36493607.
Ramaker ME, Corcoran DL, Apsley AT, Kobor MS, Kraus VB, Kraus WE, Lin DTS, Orenduff MC, Pieper CF, Waziry R, Huffman KM, Belsky DW. Epigenome-wide Association Study Analysis of Calorie Restriction in Humans, CALERIETM Trial Analysis. J Gerontol A Biol Sci Med Sci 2022;77(12):2395-2401. PM: 35965483.
Reynolds HR, Diaz A, Cyr DD, Shaw LJ, Mancini GBJ, Leipsic J, Budoff MJ, Min JK, Hague CJ, Berman DS, Chaitman BR, Picard MH, Hayes SW, Scherrer-Crosbie M, Kwong RY, Lopes RD, Senior R, Dwivedi SK, Miller TD, Chow BJW, de Silva R, Stone GW, Boden WE, Bangalore S, O’Brien SM, et al. Ischemia With Nonobstructive Coronary Arteries: Insights From the ISCHEMIA Trial. JACC Cardiovasc Imaging 2023;16(1):63- 74. PM: 36115814.
Sandhu A, Varosy PD, Du C, Aleong RG, Tumolo AZ, West JJ, Tzou WS, Curtis JP, Freeman JV, Friedman DJ, Hess PL. Device-Sizing and Associated Complications With Left Atrial Appendage Occlusion: Findings From the NCDR LAAO Registry. Circ Cardiovasc Interv 2022;15(12):e012183. PM: 36472194.
Schwamm LH, Kamel H, Granger CB, Piccini JP, Katz JM, Sethi PP, Sidorov EV, Kasner SE, Silverman SB, Merriam TT, Franco N, Ziegler PD, Bernstein RA. Predictors of Atrial Fibrillation in Patients With Stroke Attributed to Large- or Small-Vessel Disease: A Prespecified Secondary Analysis of the STROKE AF Randomized Clinical Trial. JAMA Neurol 2023;80(1):99-103. PM: 36374508.
Sinha SS, Bohula EA, Diepen SV, Leonardi S, Mebazaa A, Proudfoot AG, Sionis A, Chia YW, Zampieri FG, Lopes RD, Katz JN. The Intersection Between Heart Failure and Critical Care Cardiology: An International Perspective on Structure, Staffing, and Design Considerations. J Card Fail 2022 ;28(12):1703-1716. PM: 35843489.
Tamirisa KP, Al-Khatib SM. Sex Differences in Sustained Ventricular Arrhythmias: A Continuing Dialogue. JACC Clin Electrophysiol 2022;8(12):1563-1565. PM: 36543506.
Vaduganathan M, Claggett BL, Jhund P, de Boer RA, Hernandez AF, Inzucchi SE, Kosiborod MN, Lam CSP, Martinez F, Shah SJ, Desai AS, Hegde SM, Lindholm D, Petersson M, Langkilde AM, McMurray JJV, Solomon SD. Time to Clinical Benefit of Dapagliflozin in Patients With Heart Failure With Mildly Reduced or Preserved Ejection Fraction: A Prespecified Secondary Analysis of the DELIVER Randomized Clinical Trial. JAMA Cardiol 2022;7(12):1259-1263. PM: 36190011.
Vardeny O, Fang JC, Desai AS, Jhund PS, Claggett B, Vaduganathan M, de Boer RA, Hernandez AF, Lam CSP, Inzucchi SE, Martinez FA, Kosiborod MN, DeMets D, O’Meara E, Zieroth S, Comin-Colet J, Drozdz J, Chiang CE, Kitakaze M, Petersson M, Lindholm D, Langkilde AM, McMurray JJV, et al. Dapagliflozin in heart failure with improved ejection fraction: a prespecified analysis of the DELIVER trial. Nat Med 2022;28(12):2504-2511. PM: 36522606.
Whellan D, McCarey MM, Chen H, Nelson MB, Pastva AM, Duncan P, Mentz RJ, Kitzman DW, Reeves G, Reed SD. Quality of Life Trajectory and Its Mediators in Older Patients With Acute Decompensated Heart Failure Receiving a Multi-Domain Rehabilitation Intervention: Results From the Rehabilitation Therapy in Older Acute Heart Failure Patients Trial. Circ Heart Fail 2022;15(12):e009695. PM: 36345825.
Wilcox JE, Al-Khatib SM. Personalizing Risk Assessment for Sudden Cardiac Death in Heart Failure: A Dream or a Reality? JACC Heart Fail 2023;11(1):55-57. PM: 36599550.
Williams AM, Shah NP, Rosengart T, Povsic TJ, Williams AR. Emerging role of positron emission tomography (PET) imaging in cardiac surgery. J Card Surg 2022;37(12):4158-4164. PM: 36345705.
Yang M, Butt JH, Kondo T, Jering KS, Docherty KF, Jhund PS, de Boer RA, Claggett BL, Desai AS, Hernandez AF, Inzucchi SE, Kosiborod MN, Lam CSP, Langkilde AM, Martinez FA, Petersson M, Shah SJ, Vaduganathan M, Wilderäng U, Solomon SD, McMurray JJV. Dapagliflozin in patients with heart failure with mildly reduced and preserved ejection fraction treated with a mineralocorticoid receptor antagonist or sacubitril/valsartan. Eur J Heart Fail 2022;24(12):2307-2319. PM: 36342375.
Ye F, Nelson MB, Bertoni AG, Ditzenberger GL, Duncan P, Mentz RJ, Reeves G, Whellan D, Chen H, Upadhya B, Kitzman DW, Pastva AM. Severity of functional impairments by race and sex in older patients hospitalized with acute decompensated heart failure. J Am Geriatr Soc 2022;70(12):3447-3457. PM: 36527410.
York M, Douglas PS, Damp JB, Fraiche AM, Gillam LD, Hayes SN, Rzeszut AK, Sulistio MS, Wood MJ. Professional Preferences and Perceptions of Cardiology Among Internal Medicine Residents: Temporal Trends Over the Past Decade. JAMA Cardiol 2022;7(12):1253-1258. PM: 36223091.
Duke Heart Pulse 1-15-2023
Highlights of the week:
Duke Designated as Platinum Level Center of Excellence for ECLS
We’re proud to formally announce that Duke has been named a Platinum Level Center of Excellence for Extracorporeal Life Support (ECLS) by the Extracorporeal Life Support Organization (ELSO). Duke is one of only 50 centers around the world at the platinum level, ELSO’s top designation.
The ELSO Award for Excellence in Life Support recognizes ECLS programs worldwide that distinguish themselves by having processes, procedures and systems in place that promote excellence and exceptional care in extracorporeal membrane oxygenation (ECMO). This designation represents our commitment to exceptional patient care, and demonstrates to others our assurance of high quality standards, the use and upkeep of specialized equipment and supplies, defined patient protocols, and advanced education of all team members.
We have an exceptional ECMO team at Duke — they are leaders nationally and internationally, elevating the care available to our Duke Heart patients and their family members.
Shown here are many of the teams that comprise our ECMO program. The official award was presented to our team by Dr. Robert H. Bartlett, who is credited with developing ECMO and is known informally as “the grandfather of ECMO”. (He is an emeritus professor of surgery at the University of Michigan Medical School, but please note the Duke hat he is sporting!)
Congratulations to our entire ECMO team, including Desiree Bonadonna, director of Duke’s ECLS program; Drs. Jacob Klapper, Jacob Schroder, and Craig Rackley, medical directors for Adult ECMO; Dr. Caroline Ozment, medical director for Pediatric ECMO; our CTOR team, our cardiac anesthesia and critical care teams, Duke Life Flight, our Respiratory Therapy ECMO specialists team, our perfusion team members, and all who support them — way to go!







Swaminathan to Receive ASE award
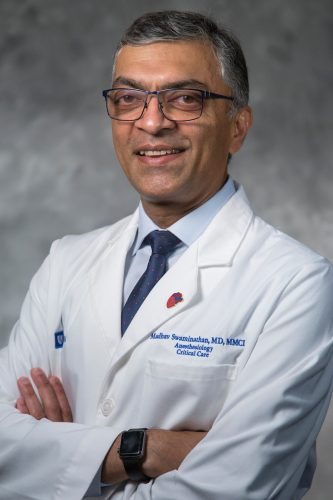
We learned this week that Dr. Madhav Swaminathan, professor of anesthesiology at Duke, has been named the recipient of American Society of Echocardiography’s (ASE) 2023 Outstanding Achievement in Perioperative Echocardiography Award.
The award will be formally announced during ASE’s annual awards presentations and Edler Lecture session at the 34th Annual Scientific Sessions on Saturday, June 24, 2023, at Gaylord National Resort, National Harbor, in Prince George’s County, MD. The award itself will be presented on June 25 during the Annual Research Awards Gala.
Past recipients of this award from Duke Health include Drs. Joe Kisslo, Solomon Aronson and Jonathan Mark.
Congratulations, Madhav – this is well-deserved!
Keenan, Selvaraj Win Duke HCLC Innovation and Collaboration Awards
 Congratulations to cardiothoracic surgeon Jeffrey Keenan, MD, and cardiologist
Congratulations to cardiothoracic surgeon Jeffrey Keenan, MD, and cardiologist

Senthil Selvaraj, MD. The two have won Duke Heart Center Leadership Council Innovation and Collaboration Awards.
The HCLC awards are available to Early Career Faculty in cardiology and cardiothoracic surgery (defined as within 10 years of completing training). Each award provides one year of salary support and/or research program support in the amount of $40,000. Selected applicants gave presentations to the HCLC during their November, 2022 meeting.
Awardees were selected by the HCLC and notified via letter by Duke Heart Center co-directors, Drs. Manesh Patel and Edward P. Chen.
Keenan’s winning project is “A Translational Approach Towards Addressing Challenges in Heart Transplantation.” His mentors include Drs. Dawn Bowles and Carmelo Milano.
Selvaraj’s winning project is “Myocardial Fuel Consumption in Heart Failure with Preserved Ejection Fraction.” Co-investigators for his project include Drs. Marat Fudim and Svati Shah.
Congratulations, Jeff and Senthil!
Shah, Safdar Win DOM ‘Duke It Out!’ Teaching Competition
 Nishant Shah and internal medicine resident Komal Safdar won the 3rd annual ‘Duke It Out!’ resident teaching competition held by the Department of Medicine on Thursday, Jan. 12. The duo won with a chalk talk presentation on basic fundamentals of ECMO.
Nishant Shah and internal medicine resident Komal Safdar won the 3rd annual ‘Duke It Out!’ resident teaching competition held by the Department of Medicine on Thursday, Jan. 12. The duo won with a chalk talk presentation on basic fundamentals of ECMO.
The competition features three senior assistant residents (the “contestants”) who give an 8-10 minute chalk talk to guide audience knowledge acquisition on a narrow, focused topic of the contestant’s choice. Each contestant is paired with a Teaching Coach. Together, they develop a chalk talk for the competition.
Shah and two other faculty members were nominated by current members of the internal medicine residency program to serve as coaches. The coaches are selected for being extraordinary teachers — “Med-Ed Rockstars” — with great chalk talk skills.
The coach-resident team competes with the other coach-resident teams on who can give the best chalk talk. The coach’s role is to help provide guidance and mentorship to the resident on creating the best possible chalk talk.
Judges for the competition were Dr. Kathleen Cooney, Dr. Lisa Criscione-Schreiber, Dr. Ann Cameron Barr (Duke it Out! creator, and a SEEDS and rheumatology fellow), Dr. Micah Schub (SEEDS and nephrology fellow), and David Stevens (DUSOM class of 2024, executive board of the Careers in Internal Medicine Interest Group).
Congratulations, Nishant and Komal!

Nominations Open for SOM Faculty Awards
Nominations and Applications for the 2023 School of Medicine Faculty Awards are now open.
The Faculty Awards are a wonderful opportunity to highlight the outstanding work conducted at Duke. The Office for Faculty is now accepting nominations and applications for the following 2023 faculty awards:
- Leonard Palumbo Jr., MD Faculty Achievement Award – Nomination Deadline: January 31, 2023
- Leonard B. Tow Humanism in Medicine Award – Nomination Deadline: January 27, 2023
- Excellence in Professionalism Award – Nomination Deadline: February 10, 2023
- Research Mentoring Awards – Nomination Deadline: February 20, 2023
- Ruth and A. Morris Williams Faculty Research Prize – Application Deadline: February 28, 2023
To learn more, visit https://duke.is/4hqkb. Questions? Please contact Jennifer Meyer Dare, jennifer.meyer-dare@duke.edu. Nominations and applications should be submitted via email to facdev@dm.duke.edu.
Adult Heart Stepdown Hiring Event – Feb. 1
Know someone who would make a great team member in Duke Heart? We have an opportunity for them to learn more about us! Our adult heart stepdown units, in partnership with Duke Health HR, will hold a hiring event on Wed., Feb. 1. Registration is required.
Interested parties can register to join our drop-in Duke Health event 8 a.m. to 2 p.m. Wednesday, February 1, to learn more about a career filled with purpose and opportunity on the Heart Adult Stepdown Units at Duke University Hospital.
At the event, they will have the opportunity to tour Duke University Hospital; learn about the many benefits of working in our health system; and meet recruiters and hiring managers for a potential same day offer.
Please share! Registration is via Qualtrics.
DOM Clinical Research Resource Fair
The DOM Clinical Research Units (CRUs), which include Heart Center, Medicine and Oncology clinical research, invite faculty, fellows, residents and trainees to a clinical research resources fair to help connect you directly to resources available at Duke.
The DOM Clinical Research Resource Fair will be held on the 6th floor of Trent Semans on Wednesday, January 25th. While information will be available on tables all day, representatives from each group will be available to informally meet with you in two open sessions: 8:30-10 am and 1-2:30 pm. CRU personnel hope you will consider joining for one of these sessions so you can meet those who support your clinical research work.
Some contributors to the event include central support staff from the CRUs such as Assistant Research Practice Managers (ARPMs), Research Practice Managers (RPMs), and finance leadership. Other SOM resources represented include staff from OASIS, contracts and DOMRA, CTSI resources, CRU statisticians, several DOCR directors including clinical operations, data, PACE, DEPRU and Research@Pickett.
While registration is not required, it will help event planners confirm expected numbers and allows them to send you a calendar invitation.
A light breakfast, coffee and juice will be provided during the morning session and after-lunch snacks will be available for the afternoon session. Additionally, all attendees will be entered into a drawing for a Starbucks gift card. (Sweet!)
Please complete the registration survey by January 19th so they are prepared for your visit!
Upcoming Events & Opportunities
Cardiology Grand Rounds
Jan. 17: 2023 CPT Evaluation and Management Changes with Laura Bushong, associate compliance officer, Duke PDC. 5 p.m., Zoom.
Medicine Grand Rounds
Jan. 27: CHIP Focus Group Presentation with cardiovascular fellow Jessica Regan and hematology-oncology fellow Bennett Caughey. 8 a.m. via Zoom or in person, Duke North 2002.
Feb.17: Topic TBD with Hyung (Harry) Jin Cho of NYU Langone Health, a 2023 Joseph C. Greenfield Visiting Professor. 8 a.m. via Zoom or in person, Duke North 2002.
February is Heart Month
Feb. 3: National Wear Red Day. We encourage everyone to wear red on Friday, Feb. 3 to show our support for heart health overall, but especially to support women and cardiovascular disease awareness. Get your red gear ready!
PERS 2023 Training Schedule Announced
Duke Health is committed to creating an environment where all team members feel physically and psychologically safe, as we prioritize high-quality safe, equitable patient care.
This course is recommended for all DUHS leaders in supervisor and above roles. Leaning includes actionable leadership skills, engagement strategies, and how to communicate clearly even when asked tough questions.
Registration is required. Please see flyer for more information.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
January 7 — Manesh Patel
El Ciudadano (Argentina)
https://duke.is/ztp7w
January 10 — Daniel Friedman
Healio/Cardiology
Posterior wall isolation does not improve outcomes in ablation for persistent AF
https://duke.is/mw7ua
January 10 — Harry Severance
Medpage Today
Yet Another Issue Is Disrupting the Healthcare Workplace
https://duke.is/76cpa
January 11 — Shahzeb Khan
Healio/Cardiology
In HF, possible longer-term benefits emerge with remote management strategy
https://duke.is/g5pu7
January 12 — James Lane (psychiatry)
Prevention
17 Ways to Lower Your Blood Pressure Naturally, According to Experts
https://duke.is/bn7vg
January 12 — Duke Health
Cardiovascular Business
Cardiologists push for a more diverse, inclusive healthcare workforce
https://duke.is/c9te8
Duke Heart – Week Ending January 8th 2023
Chief’s Section: Cardiac Arrest on NFL Field Monday Night – a “Teachable Moment”
There may be no more visible way in the US to see a cardiac arrest than the Monday Night Football game this week in which Damar Hamlin suffered a cardiac arrest after making a tackle. Even for those of us in the medical field, it is a scary thing to see, and keeping calm and continuing to carry out CPR and using an AED is critical. The medical teams did an excellent job in saving Damar’s life. Thankfully reports show his steady improvement this week.
Much of the initial conversations in the media and in the medical teams was understandably around the possible underlying cause, with many speculating that commotio cordis (the cardiac arrest after trauma to the chest/myocardium timed during repolarization of the heart). This is a rare but described event. One helpful US registry shows survival improving over the years with the rare cases of commotio cordis. https://pubmed.ncbi.nlm.nih.gov/23107651/. This registry from 1994 thru 2012 reported 216 patients with a mean age of 15 but reported cases up to 51 years of age. Importantly survival was reported to be improving (still only around 35-40%) with rapid CPR (less than 3 minutes) as one of the key predictors.
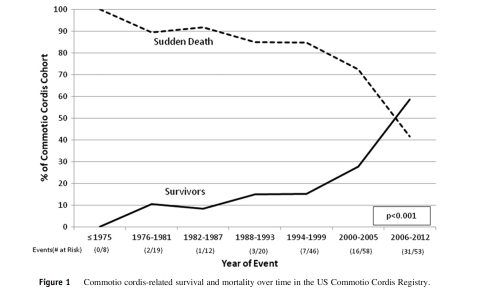
I also include the AHA position statement from 2015 https://pubmed.ncbi.nlm.nih.gov/26621653/ and for those with more interest the original NEJM article of mechanism. https://pubmed.ncbi.nlm.nih.gov/9632447/
In general, as not part of his medical team, we can’t be sure exactly what happened to Damar and important not to speculate too much – but excited he is getting better. If it turns out to be commotio cordis – the above should help put in context. Most importantly, as noted in the registry rapid CPR might be the most important step in the Chain of Survival for cardiac arrest victims.
As often is the case, Duke Heart and our teams along with our American Heart Association local leaders have been engaged in both helping study and train to improve outcomes from cardiac events. In the past, Chris Granger, Jamie Jollis and others helped set up the states rapid acute MI network for primary PCI. Now many of the same team members including also Dan Mark and Monique Starks are conducting an NIH study to help increase bystander CPR.
As Chris Granger eloquently described the efforts ….. “Damar Hamlin is alive and alert today for a simple reason: when he had his cardiac arrest, he had immediate bystander CPR and had an AED applied rapidly, long before an ambulance arrived. Moreover, he shows that cardiac arrest can occur in anyone: even an elite NFL athlete. Sadly, the vast majority of the 6000 people with cardiac arrest each year in North Carolina do not get those simple treatments. But that can change. The RACE CARS cluster randomized trial, led by the DCRI and funded by the NIH, is testing if a community-based intervention aimed at increasing bystander CPR and early defibrillation will save more lives. Our goal is to have many more people treated the way Damar Hamlin was, and thus to save many more lives.”
Regarding Cardiovascular Conditions in athletes and sudden death – there too we have had some ongoing work. Drs. Jim Daubert, Bill Kraus and many others have helped run a symposium on understanding the risk and preventing Sudden Death in athletes – a symposium we have highlighted in the past and has been supported by Heart Center Leadership Council member, Gary Davis.
We are also working with a group on a registry to understand cardiac conditions in college athletes. https://orccastudy.org/ This is the link to the outcomes registry. This work is supported by the Joel C. Cornette foundation (based in Cincinnati) and the AHA.
Finally, what can we all do. We hope that this is a national “Teachable Moment” to engage and work to better get CPR training around the country and AEDs in more locations to help our communities. As the new year begins and we have many goals and resolutions, this teachable moment for our communities maybe a great way to start.
Highlights of the week:
Duke Heart Transplant, VADs Hit Record in 2022
Internal data show that for the latest calendar year, our durable VAD volume was 90 and heart transplant volume was 142, with exceptional results for our patients. These numbers represent our highest volume-to-date at Duke University Hospital, and we believe are currently the highest volume for a U.S. program. We’ll have more on this in the coming weeks, but we wanted to share this great news with you, as well as some comments we received this week from members of DUH & DUHS leadership:
Major kudos to the transplant and VAD team for the hard work and excellent care! – Jill Engel
Extraordinary!! — Craig Albanese
Congratulations to the entire team – remarkable work from the best group in the country! — Robert Mentz
Outstanding news! Absolutely best transplant and VAD team anywhere in the known universe-no question. — Edward P. Chen
Really exceptional work from the team especially with our clinical staffing shortages (staff and providers). Thank you all for your leadership! — Mary Martin
Extraordinary! Simply the best. Congratulations on staying the course and pursuing ever greater performance amidst adversity. — Rick Shannon
Simply remarkable! Thank you for delivering such extraordinary care to so many patients and families! — Tom Owens
Duke Earns Mitral Valve Repair Reference Center Award
Duke University Hospital has received the Mitral Valve Repair Reference Center Award from the American Heart Association and the Mitral Foundation Scientific Advisory Board for the third year in a row. The recognition is given to organizations contributing to advancing best practice in the surgical treatment of mitral valve disease. This means that our Center demonstrates a record of superior clinical outcomes as well as an ongoing commitment to reporting and measuring quality and outcome metrics specific to mitral valve repairs.
Congratulations to our mitral care surgeons, physicians, care teams and our Center of Excellence teams for their outstanding performance in this area!

New Electrophysiology Labs Open
Congratulations to our Duke Electrophysiology team — Duke Regional and Duke Raleigh Hospital each have new EP labs! Regional’s opened in December and Duke Raleigh’s officially opened on Jan. 3rd.
In a note shared with us last week, Kevin Jackson, MD, wrote, “This was a four-year effort with multiple delays due to Covid and other factors, but ultimately we have a beautiful state-of-the art lab that will serve as our full-time EP procedure room and also allow us to utilize two fully-capable EP labs at Duke Raleigh.”
Shown here on opening day in the new lab at Duke Raleigh (L-R) are: Lawrence Haymond, Francis Pena, Kevin Jackson, Teri Balser, Natalie Turgeon and Jyoti Singh.
Congrats to all team members who helped get these new labs up and running. Your efforts will allow more patients to get great care here at Duke. Great work, and an excellent way to kick-off the New Year!

FY22 Publications Update, Division of Cardiology
We had an outstanding year for publications in the Division of Cardiology!
The Research Communications & Engagement group conducts an annual census of faculty publications; they have recently completed this effort for the Division of Cardiology for fiscal year 2022. We are pleased to report the Division of Cardiology had 869 total publications in FY22! To provide some context, the publications data for FY22 and the previous five fiscal years are as follows:
FY22: 869 total publications
FY21: 851 total publications
FY20: 832 total publications
FY19: 854 total publications
FY18: 660 total publications
FY17: 724 total publications
A copy of the Division of Cardiology FY22 publications report will be shared among the faculty and fellows. The report is organized by faculty and lists the number of publications, the number of high impact publications (IF ≥10), and the aggregate impact factor. The faculty continue to produce meaningful scientific discoveries in cardiovascular medicine.
Truly remarkable, everyone!
Gunn Grant Writing Series
Dr. Michael Gunn has designed a 14-session course, Research Project and Proposal Development: A Stepwise Approach. This Special Topic in the Victor J. Dzau Seminar Series, which is sponsored by the Mandel Center for Hypertension and Atherosclerosis, will be particularly helpful for those planning grant submissions in 2023. More details below under ‘events’. Registration is required. Course begins tomorrow and runs through May.
Shout-out to Goodwin, Abraham for Outstanding Care
Our colleague, Christina R., would like to recognize Drs. Goodwin and Abraham for their excellent care of her loved one who was recently in the Duke ED and on the cardiology service. In Christina’s words:
“I felt that it was important to write and recognize one of the CVD fellows, Dr.  Nathan Goodwin.
Nathan Goodwin.
“In the ED, Dr. Goodwin sat down with (my loved one*) and very patiently went through the medication list I brought and asked a lot of great questions regarding their indications. Within a minute he found a MAJOR allergy my loved one has to Quinapril, one that created an allergic reaction so profound they needed an emergency tracheotomy several years ago. He grabbed someone and had them immediately enter that ACE inhibitors cause angioedema into Epic so that it would not be missed. I must say, I was so impressed with his professionalism, bedside manner, medical knowledge and the way he explained everything to us so we understood without being condescending. He was very reassuring in that Duke would get them well and look at their extensive med list and get them on track. I know now that Dr.

Dennis Abraham will be my loved one’s cardiologist and am ecstatic to hear this news as my loved one is extremely fond of him and his demeanor as well. My loved one looks and feels better already and is actually excited for their follow-up appointments so that is truly a testament to their amazing bedside manner.
Dr. Goodwin was thorough, kind, understanding and I left that evening knowing what was going to be done overnight and what the plan of attack was. Most importantly I felt comfortable leaving them there in good, competent hands and was glad that they weren’t being rushed out the door but actually watched for observation and testing. How their care was handled was exactly how I hoped it would be, the nurses and staff were all amazing (Lisa and Michelle were 2 nurses I spoke to).
My family is extremely grateful for all of the time and energy the department put into their care… when I learned they would be admitted to the 7th floor that was the first time all day that I felt the weight lift from my shoulders because I knew regardless of which doctor was assigned, they would get the best care in the world. Just seeing the pictures from Thanksgiving to seeing what was just taken for Christmas my loved one looks like a different person thanks to Dr. Abraham and Dr. Goodwin getting them started on the right treatment in the ED. I feel like it was the first time someone actually listened to us and it made me extremely proud to say I work for Duke.” — Christina
*for patient privacy, certain identifiers have been removed.
Way to go, Dennis and Nathan! You are both amazing clinicians. When our colleagues trust us enough to care for their loved ones, we know we’re doing a good job – especially when they tell us they felt a sense of peace and relief!
DUH 7100 Shout-Outs!
The Duke University Hospital 7100 Cardiology Stepdown Unit has had a lot to celebrate! As of the end of December, the unit had been over 400 days without a Catheter Associated Urinary Tract Infection (CAUTI). The team celebrated this accomplishment over bagels and coffee last month. Great job!
Additionally, Callie Brown, a Travel Nurse who has been working on 7100 since July, was recognized for a Great Catch Award! Way to go team – nicely done!


ICYMI: Forward Together — Staying Close During a Breast Cancer Battle
Carmen Watson has spent her career as a surgical technologist, assisting surgeons in operating rooms, where the work is hard, and the stakes are high. Watson, who has spent most of her career at Duke University Hospital, knows that teamwork is crucial, as every precaution must be taken to ensure a good outcome for the patient.

And when she endured a breast cancer battle during a brief period when she wasn’t employed by Duke, her friends in Duke University Hospital’s Cardiothoracic Surgery unit turned that focused healing energy on her.
“These are good people,” said Watson, 60, a breast cancer survivor who rejoined Duke’s staff in 2020 after a few years away. “They see life and death every day. They know my situation could have gone a different way. Everybody just looked out for me.”
Watson’s history at Duke goes back to the early 2000s, when she joined the staff of the cardiothoracic surgery team as a full-time staff member and, with her calm demeanor, deep knowledge and encouraging attitude, became an indispensable resource.
Dr. Jacob Klapper, an associate professor of surgery, has been in operating rooms alongside Watson since he was a cardiothoracic surgery fellow at Duke a decade ago.
“She would always look out for me and make sure I was doing things in a way that would make the attending surgeon happy,” Klapper said. “As a trainee, you always look for those people who are trying to guide you in the right direction, and we became friendly that way. And now, as a faculty member, she always makes sure the critical things I need for an operation are there and that just translates into a positive work environment.”
Around five years ago, Watson felt she wanted a change and decided to leave Duke and work for a different company as a travelling nurse, eventually leading to a relocation to Florida. After a year there, her husband, Westley, began experiencing health problems and, in late 2018, the couple moved back to the Triangle.
Not long after she returned to North Carolina, Watson got a mammogram that showed stage-3 cancer in both breasts. Over much of the next year, she endured a double mastectomy, chemotherapy and radiation. Without health insurance for some of this period due to her job as a travelling nurse with another company ending, Watson faced immense financial strain.
Through her treatment, Watson said several of her former Duke colleagues contacted her often, asking how she was doing and occasionally providing financial help when things got especially tight. Around this time, Klapper and other staff and faculty members began looking into the possibility of bringing Watson back to Duke in her old role.
“We hoped she’d come back because we just value having someone like that next to you, a good person, a reliable person in high-stress situations, someone who knows exactly what you’re going through,” Klapper said.
In January of 2020, a now-cancer free Watson was hired by Duke, rejoining her old team. But a month after returning, she fell ill with radiation pneumonitis, requiring a brief hospital stay and nearly four months of mostly unpaid leave from work.
And again, colleagues rallied behind Watson, staying in close contact, and helping her ease back into work when she was ready.
“We just wanted to make sure she knows that she’s part of the team, she’s valued and everything is going to be OK,” said Nurse Manager for Operations in the Cardiothoracic Operating Room and Perioperative Services Rachael Knoll.
Since fall of 2020, Watson has been back with her team, deftly assisting surgeons, mentoring younger colleagues and doing her best to spread the culture of empathy, loyalty and selflessness which her team showed when she needed it most.
“That meant everything,” Watson said.
The above story originally appeared in the Jan. 4, 2023 issue of Working at Duke.
In a note to the team earlier this week, Dr. Edward P. Chen, chief of the division of cardiovascular and thoracic surgery wrote, “The example of caring and support given to our colleagues by Dr. Klapper and Rachel Knoll, as illustrated in this article, is what makes our CT Surgery team at Duke uniquely special. Happy New Year.”
Indeed! Keep up the incredible work you do not only to care for our patients, but your colleagues too. Duke Heart is a very special place.
2022 CTSI Translational Impact Report: Advancing Equity
Throughout a global pandemic that has brought unprecedented challenges and altered workflows and lives in dramatic ways, the Duke Clinical & Translational Science Institute (CTSI) continues to advance clinical research and translational science that enables equity and makes health improvement more accessible for all. Following a dynamic and fast-paced reaction to the spread of COVID-19, the Duke CTSI funded or otherwise supported numerous studies that draw upon the breadth and scope of research at Duke and its partners and collaborators.
CTSI programs and centers support each step along the translational spectrum: from preclinical discovery and entrepreneurship; through clinical trials to assess efficacy; to implementation into widespread practice that improves public health. As one of 61 NIH National Centers for Advancing Translational Science (NCATS) Clinical and Translational Science Award-funded hubs – with strong and generous institutional support from the Duke University Health System – the CTSI continues to strengthen resources and expand opportunities for their members.
The CTSI’s newly released Impact Report showcases many of their accomplishments over the past year, including their contributions to meaningful and equitable health improvement within our communities and beyond.
Holiday Photos
We hope all of you enjoyed the holidays… Back in December, members of our Duke Heart nursing leadership took carts filled with coffee, tea, hot chocolate, candy canes, and snacks and went to all areas in Heart spreading cheer and expressing gratitude to all. Here are several shots from our holiday gathering, as well. Cheers and Happy New Year to all!



PPE Reminder
Please remain vigilant with masking, hand hygiene, PPE, and other safe behaviors to prevent the spread of infection. Pay special attention to the proper wearing and securing of gowns and be mindful of PPE compliance. Thank you for all you do to keep everyone safe and healthy, especially as we kick off a new year!
Upcoming Events & Opportunities
Cardiology Grand Rounds
Jan. 10: A Path Toward Remediating Racial and Ethnic Disparities in Arrhythmia Care with Dr. Larry Jackson. 5 p.m., Zoom.
Jan. 17: 2023 CPT Evaluation and Management Changes with Laura Bushong, associate compliance officer, Duke PDC. 5 p.m., Zoom.
CME & Other Events
Grant Writing Series – A Special Topic in the Victor J. Dzau Seminar Series, sponsored by the Mandel Center for Hypertension and Atherosclerosis.
Dr. Michael Gunn has designed a 14 session course, Research Project and Proposal Development: A Stepwise Approach. Using a “flipped classroom” design, this course will teach you how to conceptualize and develop a major research project into a fundable grant proposal. We will present a stepwise approach and structured exercises that guide you through all aspects of research project development, from defining a problem of importance, to developing an experimental plan, to writing a compelling NIH-style grant application. Within this course, each student will develop their own research project and proposal using best practices, proven approaches, and continuous feedback. This course will be particularly helpful for those planning grant submissions in 2023.
- Mondays, Jan. 9 – May 1, 2023. 5:00-6:30 p.m., via Zoom. Registration required to get link.
Please email Cheryl Woodard at cheryl.woodard@duke.edu to register.
Medicine Grand Rounds
Jan. 27: CHIP Focus Group Presentation with cardiovascular fellow Jessica Regan and hematology-oncology fellow Bennett Caughey. 8 a.m. via Zoom or in person, Duke North 2002.
Feb.17: Topic TBD with Hyung (Harry) Jin Cho of NYU Langone Health, a 2023 Joseph C. Greenfield Visiting Professor. 8 a.m. via Zoom or in person, Duke North 2002.
February is Heart Month
Feb. 3: National Wear Red Day. We encourage everyone to wear red on Friday, Feb. 3 to show our support for heart health overall, but especially to support women and cardiovascular disease awareness. Get your red gear ready!
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
December 19 — Pamela Douglas and Zainab Samad
Dawn.com
https://duke.is/m9dfe
December 22 — Richard Shannon, Michael Pencina, Ricardo Henao, and Shelley Rusincovitch
Healthcare Innovation
Will Your Health System Hire a Chief AI Officer in 2023?
https://duke.is/wdd6s
December 26 — Samuel Katz
The Scientist
Remembering Those We Lost in 2022
https://duke.is/jbdtb
December 26 — Jennifer Li
WRAL
One expert recommends parents avoid latest booster vaccine for healthy children
https://duke.is/ygvx7
December 27 — Pamela Douglas
Healio/Cardiology
‘We know more about disease than health,’ but advances in CV imaging may change that
https://duke.is/rk98w
December 29 — Duke Health
Healio/Cardiology
Top HF news from 2022: Firsts in xenotransplantation, FDA approves empagliflozin and more
https://duke.is/mnydb
December 30 — James Jollis
Medscape
STEMI Times-to-Treatment Usually Miss Established Goals
https://duke.is/8jqa7
December 30 — Shahzeb Khan
Healio/Cardiology
Benefits of empagliflozin consistent regardless of cause of HFrEF
https://duke.is/2744w
January 3 — William Kraus
The Daily Beast
Damar Hamlin’s Injury Exposes the NFL’s Medical Theater
https://duke.is/59t68
January 3 — Duke Health
Healio/Cardiology Today
Top cardiology news in 2022: Successful xenotransplants; statins vs. supplements; and more
https://duke.is/ne4pk
January 3 — Manesh Patel
WNCN-CBS17
Insight into a traumatic heart incident during a football game
https://duke.is/bxtg2
(*clip begins @ 05:06:37)
January 3 — Kevin Hill (pediatric cardiology)
HealthDay News
Methylprednisolone No Benefit in Cardiopulmonary Bypass for Infants
https://duke.is/4vq3m
January 3 — Manesh Patel
WRAL-NBC5
https://duke.is/9pzfv
January 4 — Manesh Patel
sportingnews.com
https://duke.is/2m7hf
January 5 — Michael Pencina and Mary Klotman
Healthcare Innovation
Partnership to Expand Duke Health’s Capabilities in Health Analytics
https://duke.is/4qqus
January 5 — Michael Pencina
Healio/Cardiology
CAD polygenic risk score may guide statin initiation for younger adults
https://duke.is/56zk3
Recent Comments