Chief’s Section: Cardiac Arrest on NFL Field Monday Night – a “Teachable Moment”
There may be no more visible way in the US to see a cardiac arrest than the Monday Night Football game this week in which Damar Hamlin suffered a cardiac arrest after making a tackle. Even for those of us in the medical field, it is a scary thing to see, and keeping calm and continuing to carry out CPR and using an AED is critical. The medical teams did an excellent job in saving Damar’s life. Thankfully reports show his steady improvement this week.
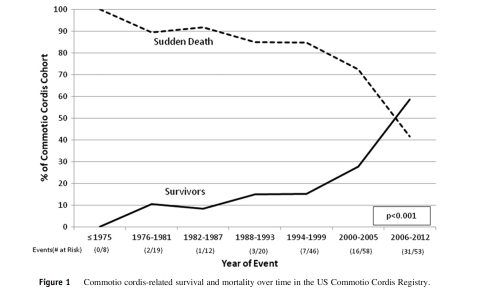
Much of the initial conversations in the media and in the medical teams was understandably around the possible underlying cause, with many speculating that commotio cordis (the cardiac arrest after trauma to the chest/myocardium timed during repolarization of the heart). This is a rare but described event. One helpful US registry shows survival improving over the years with the rare cases of commotio cordis. https://pubmed.ncbi.nlm.nih.gov/23107651/. This registry from 1994 thru 2012 reported 216 patients with a mean age of 15 but reported cases up to 51 years of age. Importantly survival was reported to be improving (still only around 35-40%) with rapid CPR (less than 3 minutes) as one of the key predictors.
I also include the AHA position statement from 2015 https://pubmed.ncbi.nlm.nih.gov/26621653/ and for those with more interest the original NEJM article of mechanism. https://pubmed.ncbi.nlm.nih.gov/9632447/
In general, as not part of his medical team, we can’t be sure exactly what happened to Damar and important not to speculate too much – but excited he is getting better. If it turns out to be commotio cordis – the above should help put in context. Most importantly, as noted in the registry rapid CPR might be the most important step in the Chain of Survival for cardiac arrest victims.
As often is the case, Duke Heart and our teams along with our American Heart Association local leaders have been engaged in both helping study and train to improve outcomes from cardiac events. In the past, Chris Granger, Jamie Jollis and others helped set up the states rapid acute MI network for primary PCI. Now many of the same team members including also Dan Mark and Monique Starks are conducting an NIH study to help increase bystander CPR.
As Chris Granger eloquently described the efforts ….. “Damar Hamlin is alive and alert today for a simple reason: when he had his cardiac arrest, he had immediate bystander CPR and had an AED applied rapidly, long before an ambulance arrived. Moreover, he shows that cardiac arrest can occur in anyone: even an elite NFL athlete. Sadly, the vast majority of the 6000 people with cardiac arrest each year in North Carolina do not get those simple treatments. But that can change. The RACE CARS cluster randomized trial, led by the DCRI and funded by the NIH, is testing if a community-based intervention aimed at increasing bystander CPR and early defibrillation will save more lives. Our goal is to have many more people treated the way Damar Hamlin was, and thus to save many more lives.”
Regarding Cardiovascular Conditions in athletes and sudden death – there too we have had some ongoing work. Drs. Jim Daubert, Bill Kraus and many others have helped run a symposium on understanding the risk and preventing Sudden Death in athletes – a symposium we have highlighted in the past and has been supported by Heart Center Leadership Council member, Gary Davis.
We are also working with a group on a registry to understand cardiac conditions in college athletes. https://orccastudy.org/ This is the link to the outcomes registry. This work is supported by the Joel C. Cornette foundation (based in Cincinnati) and the AHA.
Finally, what can we all do. We hope that this is a national “Teachable Moment” to engage and work to better get CPR training around the country and AEDs in more locations to help our communities. As the new year begins and we have many goals and resolutions, this teachable moment for our communities maybe a great way to start.
Highlights of the week:
Duke Heart Transplant, VADs Hit Record in 2022
Internal data show that for the latest calendar year, our durable VAD volume was 90 and heart transplant volume was 142, with exceptional results for our patients. These numbers represent our highest volume-to-date at Duke University Hospital, and we believe are currently the highest volume for a U.S. program. We’ll have more on this in the coming weeks, but we wanted to share this great news with you, as well as some comments we received this week from members of DUH & DUHS leadership:
Major kudos to the transplant and VAD team for the hard work and excellent care! – Jill Engel
Extraordinary!! — Craig Albanese
Congratulations to the entire team – remarkable work from the best group in the country! — Robert Mentz
Outstanding news! Absolutely best transplant and VAD team anywhere in the known universe-no question. — Edward P. Chen
Really exceptional work from the team especially with our clinical staffing shortages (staff and providers). Thank you all for your leadership! — Mary Martin
Extraordinary! Simply the best. Congratulations on staying the course and pursuing ever greater performance amidst adversity. — Rick Shannon
Simply remarkable! Thank you for delivering such extraordinary care to so many patients and families! — Tom Owens
Duke Earns Mitral Valve Repair Reference Center Award
Duke University Hospital has received the Mitral Valve Repair Reference Center Award from the American Heart Association and the Mitral Foundation Scientific Advisory Board for the third year in a row. The recognition is given to organizations contributing to advancing best practice in the surgical treatment of mitral valve disease. This means that our Center demonstrates a record of superior clinical outcomes as well as an ongoing commitment to reporting and measuring quality and outcome metrics specific to mitral valve repairs.
Congratulations to our mitral care surgeons, physicians, care teams and our Center of Excellence teams for their outstanding performance in this area!

New Electrophysiology Labs Open
Congratulations to our Duke Electrophysiology team — Duke Regional and Duke Raleigh Hospital each have new EP labs! Regional’s opened in December and Duke Raleigh’s officially opened on Jan. 3rd.
In a note shared with us last week, Kevin Jackson, MD, wrote, “This was a four-year effort with multiple delays due to Covid and other factors, but ultimately we have a beautiful state-of-the art lab that will serve as our full-time EP procedure room and also allow us to utilize two fully-capable EP labs at Duke Raleigh.”
Shown here on opening day in the new lab at Duke Raleigh (L-R) are: Lawrence Haymond, Francis Pena, Kevin Jackson, Teri Balser, Natalie Turgeon and Jyoti Singh.
Congrats to all team members who helped get these new labs up and running. Your efforts will allow more patients to get great care here at Duke. Great work, and an excellent way to kick-off the New Year!

FY22 Publications Update, Division of Cardiology
We had an outstanding year for publications in the Division of Cardiology!
The Research Communications & Engagement group conducts an annual census of faculty publications; they have recently completed this effort for the Division of Cardiology for fiscal year 2022. We are pleased to report the Division of Cardiology had 869 total publications in FY22! To provide some context, the publications data for FY22 and the previous five fiscal years are as follows:
FY22: 869 total publications
FY21: 851 total publications
FY20: 832 total publications
FY19: 854 total publications
FY18: 660 total publications
FY17: 724 total publications
A copy of the Division of Cardiology FY22 publications report will be shared among the faculty and fellows. The report is organized by faculty and lists the number of publications, the number of high impact publications (IF ≥10), and the aggregate impact factor. The faculty continue to produce meaningful scientific discoveries in cardiovascular medicine.
Truly remarkable, everyone!
Gunn Grant Writing Series
Dr. Michael Gunn has designed a 14-session course, Research Project and Proposal Development: A Stepwise Approach. This Special Topic in the Victor J. Dzau Seminar Series, which is sponsored by the Mandel Center for Hypertension and Atherosclerosis, will be particularly helpful for those planning grant submissions in 2023. More details below under ‘events’. Registration is required. Course begins tomorrow and runs through May.
Shout-out to Goodwin, Abraham for Outstanding Care
Our colleague, Christina R., would like to recognize Drs. Goodwin and Abraham for their excellent care of her loved one who was recently in the Duke ED and on the cardiology service. In Christina’s words:
“I felt that it was important to write and recognize one of the CVD fellows, Dr.  Nathan Goodwin.
Nathan Goodwin.
“In the ED, Dr. Goodwin sat down with (my loved one*) and very patiently went through the medication list I brought and asked a lot of great questions regarding their indications. Within a minute he found a MAJOR allergy my loved one has to Quinapril, one that created an allergic reaction so profound they needed an emergency tracheotomy several years ago. He grabbed someone and had them immediately enter that ACE inhibitors cause angioedema into Epic so that it would not be missed. I must say, I was so impressed with his professionalism, bedside manner, medical knowledge and the way he explained everything to us so we understood without being condescending. He was very reassuring in that Duke would get them well and look at their extensive med list and get them on track. I know now that Dr.

Dennis Abraham will be my loved one’s cardiologist and am ecstatic to hear this news as my loved one is extremely fond of him and his demeanor as well. My loved one looks and feels better already and is actually excited for their follow-up appointments so that is truly a testament to their amazing bedside manner.
Dr. Goodwin was thorough, kind, understanding and I left that evening knowing what was going to be done overnight and what the plan of attack was. Most importantly I felt comfortable leaving them there in good, competent hands and was glad that they weren’t being rushed out the door but actually watched for observation and testing. How their care was handled was exactly how I hoped it would be, the nurses and staff were all amazing (Lisa and Michelle were 2 nurses I spoke to).
My family is extremely grateful for all of the time and energy the department put into their care… when I learned they would be admitted to the 7th floor that was the first time all day that I felt the weight lift from my shoulders because I knew regardless of which doctor was assigned, they would get the best care in the world. Just seeing the pictures from Thanksgiving to seeing what was just taken for Christmas my loved one looks like a different person thanks to Dr. Abraham and Dr. Goodwin getting them started on the right treatment in the ED. I feel like it was the first time someone actually listened to us and it made me extremely proud to say I work for Duke.” — Christina
*for patient privacy, certain identifiers have been removed.
Way to go, Dennis and Nathan! You are both amazing clinicians. When our colleagues trust us enough to care for their loved ones, we know we’re doing a good job – especially when they tell us they felt a sense of peace and relief!
DUH 7100 Shout-Outs!
The Duke University Hospital 7100 Cardiology Stepdown Unit has had a lot to celebrate! As of the end of December, the unit had been over 400 days without a Catheter Associated Urinary Tract Infection (CAUTI). The team celebrated this accomplishment over bagels and coffee last month. Great job!
Additionally, Callie Brown, a Travel Nurse who has been working on 7100 since July, was recognized for a Great Catch Award! Way to go team – nicely done!


ICYMI: Forward Together — Staying Close During a Breast Cancer Battle
Carmen Watson has spent her career as a surgical technologist, assisting surgeons in operating rooms, where the work is hard, and the stakes are high. Watson, who has spent most of her career at Duke University Hospital, knows that teamwork is crucial, as every precaution must be taken to ensure a good outcome for the patient.

And when she endured a breast cancer battle during a brief period when she wasn’t employed by Duke, her friends in Duke University Hospital’s Cardiothoracic Surgery unit turned that focused healing energy on her.
“These are good people,” said Watson, 60, a breast cancer survivor who rejoined Duke’s staff in 2020 after a few years away. “They see life and death every day. They know my situation could have gone a different way. Everybody just looked out for me.”
Watson’s history at Duke goes back to the early 2000s, when she joined the staff of the cardiothoracic surgery team as a full-time staff member and, with her calm demeanor, deep knowledge and encouraging attitude, became an indispensable resource.
Dr. Jacob Klapper, an associate professor of surgery, has been in operating rooms alongside Watson since he was a cardiothoracic surgery fellow at Duke a decade ago.
“She would always look out for me and make sure I was doing things in a way that would make the attending surgeon happy,” Klapper said. “As a trainee, you always look for those people who are trying to guide you in the right direction, and we became friendly that way. And now, as a faculty member, she always makes sure the critical things I need for an operation are there and that just translates into a positive work environment.”
Around five years ago, Watson felt she wanted a change and decided to leave Duke and work for a different company as a travelling nurse, eventually leading to a relocation to Florida. After a year there, her husband, Westley, began experiencing health problems and, in late 2018, the couple moved back to the Triangle.
Not long after she returned to North Carolina, Watson got a mammogram that showed stage-3 cancer in both breasts. Over much of the next year, she endured a double mastectomy, chemotherapy and radiation. Without health insurance for some of this period due to her job as a travelling nurse with another company ending, Watson faced immense financial strain.
Through her treatment, Watson said several of her former Duke colleagues contacted her often, asking how she was doing and occasionally providing financial help when things got especially tight. Around this time, Klapper and other staff and faculty members began looking into the possibility of bringing Watson back to Duke in her old role.
“We hoped she’d come back because we just value having someone like that next to you, a good person, a reliable person in high-stress situations, someone who knows exactly what you’re going through,” Klapper said.
In January of 2020, a now-cancer free Watson was hired by Duke, rejoining her old team. But a month after returning, she fell ill with radiation pneumonitis, requiring a brief hospital stay and nearly four months of mostly unpaid leave from work.
And again, colleagues rallied behind Watson, staying in close contact, and helping her ease back into work when she was ready.
“We just wanted to make sure she knows that she’s part of the team, she’s valued and everything is going to be OK,” said Nurse Manager for Operations in the Cardiothoracic Operating Room and Perioperative Services Rachael Knoll.
Since fall of 2020, Watson has been back with her team, deftly assisting surgeons, mentoring younger colleagues and doing her best to spread the culture of empathy, loyalty and selflessness which her team showed when she needed it most.
“That meant everything,” Watson said.
The above story originally appeared in the Jan. 4, 2023 issue of Working at Duke.
In a note to the team earlier this week, Dr. Edward P. Chen, chief of the division of cardiovascular and thoracic surgery wrote, “The example of caring and support given to our colleagues by Dr. Klapper and Rachel Knoll, as illustrated in this article, is what makes our CT Surgery team at Duke uniquely special. Happy New Year.”
Indeed! Keep up the incredible work you do not only to care for our patients, but your colleagues too. Duke Heart is a very special place.
2022 CTSI Translational Impact Report: Advancing Equity
Throughout a global pandemic that has brought unprecedented challenges and altered workflows and lives in dramatic ways, the Duke Clinical & Translational Science Institute (CTSI) continues to advance clinical research and translational science that enables equity and makes health improvement more accessible for all. Following a dynamic and fast-paced reaction to the spread of COVID-19, the Duke CTSI funded or otherwise supported numerous studies that draw upon the breadth and scope of research at Duke and its partners and collaborators.
CTSI programs and centers support each step along the translational spectrum: from preclinical discovery and entrepreneurship; through clinical trials to assess efficacy; to implementation into widespread practice that improves public health. As one of 61 NIH National Centers for Advancing Translational Science (NCATS) Clinical and Translational Science Award-funded hubs – with strong and generous institutional support from the Duke University Health System – the CTSI continues to strengthen resources and expand opportunities for their members.
The CTSI’s newly released Impact Report showcases many of their accomplishments over the past year, including their contributions to meaningful and equitable health improvement within our communities and beyond.
Holiday Photos
We hope all of you enjoyed the holidays… Back in December, members of our Duke Heart nursing leadership took carts filled with coffee, tea, hot chocolate, candy canes, and snacks and went to all areas in Heart spreading cheer and expressing gratitude to all. Here are several shots from our holiday gathering, as well. Cheers and Happy New Year to all!



PPE Reminder
Please remain vigilant with masking, hand hygiene, PPE, and other safe behaviors to prevent the spread of infection. Pay special attention to the proper wearing and securing of gowns and be mindful of PPE compliance. Thank you for all you do to keep everyone safe and healthy, especially as we kick off a new year!
Upcoming Events & Opportunities
Cardiology Grand Rounds
Jan. 10: A Path Toward Remediating Racial and Ethnic Disparities in Arrhythmia Care with Dr. Larry Jackson. 5 p.m., Zoom.
Jan. 17: 2023 CPT Evaluation and Management Changes with Laura Bushong, associate compliance officer, Duke PDC. 5 p.m., Zoom.
CME & Other Events
Grant Writing Series – A Special Topic in the Victor J. Dzau Seminar Series, sponsored by the Mandel Center for Hypertension and Atherosclerosis.
Dr. Michael Gunn has designed a 14 session course, Research Project and Proposal Development: A Stepwise Approach. Using a “flipped classroom” design, this course will teach you how to conceptualize and develop a major research project into a fundable grant proposal. We will present a stepwise approach and structured exercises that guide you through all aspects of research project development, from defining a problem of importance, to developing an experimental plan, to writing a compelling NIH-style grant application. Within this course, each student will develop their own research project and proposal using best practices, proven approaches, and continuous feedback. This course will be particularly helpful for those planning grant submissions in 2023.
- Mondays, Jan. 9 – May 1, 2023. 5:00-6:30 p.m., via Zoom. Registration required to get link.
Please email Cheryl Woodard at cheryl.woodard@duke.edu to register.
Medicine Grand Rounds
Jan. 27: CHIP Focus Group Presentation with cardiovascular fellow Jessica Regan and hematology-oncology fellow Bennett Caughey. 8 a.m. via Zoom or in person, Duke North 2002.
Feb.17: Topic TBD with Hyung (Harry) Jin Cho of NYU Langone Health, a 2023 Joseph C. Greenfield Visiting Professor. 8 a.m. via Zoom or in person, Duke North 2002.
February is Heart Month
Feb. 3: National Wear Red Day. We encourage everyone to wear red on Friday, Feb. 3 to show our support for heart health overall, but especially to support women and cardiovascular disease awareness. Get your red gear ready!
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
December 19 — Pamela Douglas and Zainab Samad
Dawn.com
https://duke.is/m9dfe
December 22 — Richard Shannon, Michael Pencina, Ricardo Henao, and Shelley Rusincovitch
Healthcare Innovation
Will Your Health System Hire a Chief AI Officer in 2023?
https://duke.is/wdd6s
December 26 — Samuel Katz
The Scientist
Remembering Those We Lost in 2022
https://duke.is/jbdtb
December 26 — Jennifer Li
WRAL
One expert recommends parents avoid latest booster vaccine for healthy children
https://duke.is/ygvx7
December 27 — Pamela Douglas
Healio/Cardiology
‘We know more about disease than health,’ but advances in CV imaging may change that
https://duke.is/rk98w
December 29 — Duke Health
Healio/Cardiology
Top HF news from 2022: Firsts in xenotransplantation, FDA approves empagliflozin and more
https://duke.is/mnydb
December 30 — James Jollis
Medscape
STEMI Times-to-Treatment Usually Miss Established Goals
https://duke.is/8jqa7
December 30 — Shahzeb Khan
Healio/Cardiology
Benefits of empagliflozin consistent regardless of cause of HFrEF
https://duke.is/2744w
January 3 — William Kraus
The Daily Beast
Damar Hamlin’s Injury Exposes the NFL’s Medical Theater
https://duke.is/59t68
January 3 — Duke Health
Healio/Cardiology Today
Top cardiology news in 2022: Successful xenotransplants; statins vs. supplements; and more
https://duke.is/ne4pk
January 3 — Manesh Patel
WNCN-CBS17
Insight into a traumatic heart incident during a football game
https://duke.is/bxtg2
(*clip begins @ 05:06:37)
January 3 — Kevin Hill (pediatric cardiology)
HealthDay News
Methylprednisolone No Benefit in Cardiopulmonary Bypass for Infants
https://duke.is/4vq3m
January 3 — Manesh Patel
WRAL-NBC5
https://duke.is/9pzfv
January 4 — Manesh Patel
sportingnews.com
https://duke.is/2m7hf
January 5 — Michael Pencina and Mary Klotman
Healthcare Innovation
Partnership to Expand Duke Health’s Capabilities in Health Analytics
https://duke.is/4qqus
January 5 — Michael Pencina
Healio/Cardiology
CAD polygenic risk score may guide statin initiation for younger adults
https://duke.is/56zk3
Recent Comments