Duke Heart Pulse 11-28-2021
Chief’s message:
Thanksgiving is a time of reflection and gratitude. We hope of our extended Duke Heart Family and colleagues had some time to spend with family, friends and the loved ones. Most importantly, we hope you all had some time to remember and embrace those that enrich our lives.
Highlights of the week:
Carmat Patient Receives New Human Heart
A surgical team led by Drs. Jacob Schroder and Carmelo Milano, has successfully explanted the Carmat new-generation

total artificial heart that was placed into an end-stage heart failure patient at Duke in July. Matthew Moore of Shallotte, N.C., lived with the device for four months. On Monday, Nov. 22, Moore received a donor heart during transplant surgery at Duke University Hospital.
Carmat’s artificial heart, which is approved for use in Europe, is an implantable prosthetic that includes biological valves derived from bovine tissue. It operates on an external power supply. Duke became the first center in North America to implant the prosthetic device, which is currently being studied at four U.S. locations as a bridge to transplant.
“The use of the Carmat total artificial heart system to successfully bridge a patient to heart transplantation at Duke is a milestone for heart failure patients in the United States,” said Schroder, surgical director of Duke’s heart transplant program. “The device is designed to be significantly more hemocompatible, and should greatly reduce thromboembolic events. This is a major advance from previously available devices.”
 If the device receives FDA approval, it would provide a bridge to transplant for patients whose hearts require assistance to pump blood through both chambers. Current technology – notably a left-ventricular assist device (LVAD) — supports just one chamber.
If the device receives FDA approval, it would provide a bridge to transplant for patients whose hearts require assistance to pump blood through both chambers. Current technology – notably a left-ventricular assist device (LVAD) — supports just one chamber.
“The successful performance of heart transplantation in our patient following initial use of the Carmat total artificial heart system as a temporary support measure is a first in this country,” said Edward P. Chen, MD, chief of the Division of Cardiovascular and Thoracic Surgery in Duke’s Department of Surgery. “This device will ultimately transform care of patients with end stage cardiac disease. We are privileged at Duke to have a team which pursues delivery of the highest-quality patient care and is constantly looking to improve upon this care through innovation.”
Congratulations to Schroder and Jason Katz, co-principal investigators at Duke for the Carmat Total Artificial Heart (TAH) Early Feasibility Study, and to their clinical research team; to Carmelo Milano and our cardiothoracic surgical team; to Sharon McCartney, Sachin Mehta and our cardiac anesthesiology team members; to Adam DeVore and our heart failure team; to our mechanical circulatory support program; our VAD coordinators; the perfusion team, and to the nursing staff of the CTICU and clinical stepdown units.
We are truly blessed with amazing team members across Duke Heart!
Kahsai Receives CVRC’s 2021 Headley Family Award
 Alem Kahsai, PhD, an assistant professor of medicine in the division of cardiology, has received the 2021 Headley Family Award for research within the Duke Cardiovascular Research Center (CVRC). The award to Kahsai, a medicinal and chemical biologist, is for his project ‘Towards understanding the roles of β-arrestins in Alzheimer’s Disease and cardiovascular disorders.’
Alem Kahsai, PhD, an assistant professor of medicine in the division of cardiology, has received the 2021 Headley Family Award for research within the Duke Cardiovascular Research Center (CVRC). The award to Kahsai, a medicinal and chemical biologist, is for his project ‘Towards understanding the roles of β-arrestins in Alzheimer’s Disease and cardiovascular disorders.’
His project aims to understand the similarities between amyloid-β peptide deposits that occur between neurons in the brain (a hallmark event in the development of Alzheimer’s disease) and cardiac amyloid-β peptide deposits in heart and vascular tissues that are the hallmark of many cardiovascular diseases. Cardiac amyloid-β peptide deposits are associated with cardiomyocyte dysfunction, while vascular deposits promote stiffening, inflammation, and atherosclerosis.
There appears to be a positive correlation between increased levels of β-arrestins—key regulators of a class of cell surface receptors called G-protein-coupled receptors—with enhanced γ-secretase activity and the production of amyloid-β peptide in post-mortem brains from Alzheimer’s disease patients compared to healthy controls, Kahsai says. The mechanism by which β-arrestins regulate γ-secretase activity is elusive, and it is this mechanism that he plans to explore.
“Thanks to the Headley award, I can move forward in my research and obtain preliminary data to see the bigger picture,” says Kahsai. “We are trying to devise small molecule drugs that target β-arrestins in the context of Alzheimer’s disease as well as a number of cardiovascular problems, in particular atherosclerosis.”
Funding through the Headley Award will enable Kahsai to reconstitute each component of the γ-secretase- β-arrestin complex outside of the cell and determine how β-arrestins directly regulate γ-secretase activity and thus amyloid-β peptide production within neuronal cells. He hopes the findings from his studies will potentially open a new avenue for therapeutic development through targeting γ-secretase regulating proteins, such as β-arrestins.
He says it is paramount to identify therapeutic targets in order to slow the progression of amyloid-β peptide accumulation in the context of both cardiovascular and neurological disease.
“The CVRC is fortunate to have generous support from donors such as Mr. Headley and his family, who are interested in investing in the basic cardiovascular research that’s so necessary to continue to improve patient treatment and outcomes,” says Maria Price-Rapoza, executive director of the CVRC.
The Headley Family Award was established in 2020 and is made possible through the generosity of Harry and Dorothy Headley in support of basic cardiovascular research at Duke. The award provides annual one-year seed grants of $25,000 (plus indirect costs at 15 percent) targeted toward CVRC researchers who are conducting innovative research into the causes and treatment of hypertension, atherosclerosis and related cardiovascular diseases. The leadership of the Duke CVRC is deeply grateful for the support the Headley’s have provided to our research team.
The award is effective as of Nov. 1. Congratulations, Alem!
Katz Featured in CardioNerds Podcast
CardioNerds has launched a Cardiac Critical Care Series on their podcast and have kicked it off with an episode featuring our own Jason Katz, director of Cardiovascular Critical Care and co-director of Mechanical Circulatory Support and the CICU at Duke. Check it out here: https://apple.co/3HQMJEf.
It’s a good interview and well worth checking out. Great job and congratulations, Jason!

Cardiac Sonography Program Update
Congratulations to Richard Palma, director of the Duke Cardiac Ultrasound Certificate Program, who was recently inducted into the Society of Diagnostic Medical Sonography‘s (SDMS) Board of Directors. The SDMS is the largest association of sonographers and sonography students in the world. Congrats, Richie!

Palma gave three presentations at the SDMS national meeting held Sept. 29-Oct. 2 at the Hyatt Regency in Atlanta. Palma is shown here with two of his former students who were also invited speakers at SDMS. On the left in the photo is Daniel Bourque, MS, ACS, FASE who is the lead cardiac sonographer for Orlando Regional Medical Center; in the center is Palma, and to the right is Laura Phillips, BS, RDCS, RVT, who is with Yale New Haven Hospital and serves as program director for the vascular ultrasound program at the Hoffman Heart Institute of Connecticut.
Hanukkah Wishes
On behalf of the Duke Heart leadership team, we wish all who will be celebrating Hanukkah a peaceful holiday filled with unexpected blessings. It’s up to each of us to be a light in the darkness — even a little light can go a long way.

Upcoming Events & Opportunities
Cardiology Grand Rounds
December 1: The Pathophysiology and Natural History of Perioperative Atrial Fibrillation: Transient Nuisance or Cause for Concern with Bernard Gersh of the Mayo Clinic, Rochester, MN. 5 p.m. Webex.
December 7: Visiting lecture with Anubha Agarwal of Northwestern Medicine.
Training Workshop
November 30 & December 14: Stepping in 4-Respect (SI4R) Workshop for Duke Division of Cardiology. 5-7 p.m. Zoom (Details in email from Kim Dorman)
As part of the Department of Medicine Civility Champion initiatives, a 2-hr zoom workshop for all faculty, staff, and trainees throughout all DOM divisions has been developed. Civility Champions are trained faculty, fellows, and chief residents who provide informal support in response to incidents of bias, harassment, or other unprofessional behaviors, and to help those affected understand their options for intervention and reporting. People generally come to Civility Champions after the fact, and the Champions debrief their experiences every quarter.
The workshop that Drs. John Duronville, Jane Gagliardi, Anita Kelsey, Camille Frazier-Mills, Daniella Zipkin, Laura Previll, and Sophia Weinmann will be presenting to the Cardiology clinical faculty is entitled Stepping In 4-Respect. It is being offered twice and is a new component of these civility efforts designed to teach faculty the skills needed to step in (be an “upstander”) in the moment, with a particular focus on race-, ethnicity- and gender-based incidents. This workshop is supported by Dr. Kathleen Cooney, Chair of the DOM, and will be provided to each division’s faculty over the coming months.
Please be sure to attend the workshop on one of these dates (November 30th or December 14th). Additional details about registration, the structure and goals of the workshop appeared in the email invitation.
Save the Date & Support the Marfan Foundation
February 11: An Evening with Heart to benefit The Marfan Foundation. 7-10 p.m. at The Maxwell in Raleigh, NC. A Valentine’s Day weekend event with silent auction, cocktails, heavy hors d’oeuvres and entertainment. Cocktail attire. Tickets required. For information, visit: https://bit.ly/3cHIBYD.
The Duke Center for Aortic Disease, led by cardiovascular surgeon Chad Hughes, works closely with Marfan patients, their family members and the Marfan Foundation. We are the only location in NC offering access to comprehensive aortic surgical interventions as well as coordinated cardiovascular care and genetic counseling for patients with Marfan syndrome and other connective tissue disorders such as Loeys-Dietz. If you’re interested in learning more about the work being done at Duke or would like to partner or otherwise get involved, please contact Dr. Hughes or Melissa Merrill Burkett, ACNP.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
November 19 — Stephen Greene
Medscape
Fewer Strokes on Myosin Activator in Reduced-EF Heart Failure: GALACTIC-HF
https://duke.is/c4e9x
November 19 — Manesh Patel
U.S. News & World Report
Advances in Care, Impact of COVID Highlights of Latest Cardiologists’ Meeting
https://duke.is/8ezmf
November 20 — Manesh Patel
UPI
Pandemic has made heart healthcare more difficult, doctors say at meeting
https://duke.is/w8bz6
November 23 — Sreekanth Vemulapalli
tctMD
US Aortic Valve Trends in Older Patients Hint at Better Outcomes, Access
https://duke.is/ykbht
Duke Heart Pulse – week ending 11-21-2021
Highlights of the week:
AHA Scientific Sessions & Watch Party 
A big congratulations to all members of our team who showcased the outstanding cardiovascular research and clinical care taking place at Duke during the 2021 AHA Scientific Sessions – in an extraordinarily challenging year, we still had a tremendous showing of speakers, moderators, panelists, discussants and collaborators from across Duke Heart and Duke Clinical Research Institute. Congratulations to Karen Alexander, Renato Lopes, Marat Fudim, Sean Pokorney, Neha Pagidipati, Svati Shah, Adrian Hernandez, Magnus Ohman, Schuyler Jones, L.Kristin Newby, Patricia Cowper, Gerald Bloomfield, Monique Starks, Jennifer Rymer, Stephen Greene, Kevin Thomas, Sana Al-Khatib, Dan Mark, Pamela Douglas, Jonathan Piccini, Adam DeVore, Robert Mentz, Manesh Patel, Michael Felker, Chris Granger, Jim Daubert, Sunil Rao, Vishal Rao, Michelle Kelsey, Josephine Harrington and Vanessa Blumer and to all of our amazing staff members who support their research, time and efforts.
A full listing of all presentations by members of the DCRI, including On-Demand Content can be found here: https://duke.is/2s2f8; media coverage appears in our News Section, below.
A big hat tip to Chris and Bradi Granger for hosting an AHA Watch Party at their lovely home in Bahama last weekend – it was a fun event held in lieu of the annual AHA Duke Reception to celebrate Duke Heart’s presence at the AHA. The Watch Party included some serious and not-so-serious awards, including “Most Likely to Succeed (as next FDA Commissioner)” which went to Rob Califf.
Other superlatives included:
- Best Stats awarded to Hillary Mulder and Karen Pieper of the DCRI
- Best BP Cuff Distribution awarded to Holly Biola of the AHA-Duke-PACE Team
- Best Dissemination Award given to the ICU iPad Patient-Family Communication Study
- The Heart Success Champion “Big Gold Belt” Award, given to the Heart Failure team member involved in research that has led to significant improvement in the care of HF patients, went to Steve Green for his presentation of CHAMP-HF. Green is a collaborator or partner on 14 total presentations or posters and, according to his colleagues, “will hunt you down if you fail to prescribe GDMT.”
- The Rising Star Award, given to a trainee who consistently demonstrates commitment to growth, education and involvement with the AHA, was presented to Vanessa Blumer, a finalist for and winner of the 2021 AHA Laennec Award.
- The Bench to Bedside Award, given to an individual who leads the way in basic science research went to Lauren Truby for her work with Svati Shah and others surrounding proteomic profiling to identify pre-transplant biomarkers of renal failure after heart transplantation which was accepted and presented as a rapid fire oral abstract.
- The Master Collaborator Award was awarded to Marat Fudim for his 13 collaborations across the globe during AHA Scientific Sessions ranging in topics from global health to big data in MIs and stroke care to heart failure disparities. “When in doubt, stop, collaborate and listen.”
- The Best Site-Based Randomized Study was awarded to UNTAP-IT team for improving understanding of patient discomfort and pain during cath.
- The 2nd Best Caipirinhas award was presented to Renato Lopes
- Our newest Heart Center Nurse-APP PIs were recognized: Heather Pena, Dustin Tart, Anna Mall, Kelly Brown, Jules Onorato, Jaime McDermott, Callie Tennyson, Shelley Thompson and Kelly Kester
- Most Synergistic was awarded to Neha Pagidipati
We hope everyone enjoyed the evening! Congrats to each and every one of you.




Blumer Wins AHA Laennec Award at Scientific Sessions
 Vanessa Blumer, MD, was awarded the 2021 Laennec Fellow in Training Clinician Award by the American Heart Association (AHA) Council on Clinical Cardiology during the AHA Scientific Sessions held virtually last weekend. The award recognizes the importance of clinical acumen, inductive analytic skills, and teaching ability in future academic cardiologists; it is a highly competitive award category.
Vanessa Blumer, MD, was awarded the 2021 Laennec Fellow in Training Clinician Award by the American Heart Association (AHA) Council on Clinical Cardiology during the AHA Scientific Sessions held virtually last weekend. The award recognizes the importance of clinical acumen, inductive analytic skills, and teaching ability in future academic cardiologists; it is a highly competitive award category.
Blumer, a third year fellow in our cardiovascular disease fellowship program, presented her abstract, A Challenging Case of Endocarditis — Multi-Disciplinary Approach is an Achievable Chimera during the Laennec FIT Award Competition Session. She is the first finalist from Duke to earn the Laennec award, which has been given since 2010.
“I am extremely honored to have been awarded this year’s AHA Laennec FIT Clinician Award,” said Blumer. “All the finalists did an exceptional job and I learned so much from the experience. Mostly, I am beyond grateful to everyone who helped and supported me.”
Congratulations, Vanessa — this is a tremendous accomplishment and we are so excited for you!

New Cardiology Clinic Space Opens at Arringdon in Morrisville
Our newest cardiology ambulatory space, Duke Cardiology of Arringdon, opened on Monday, Nov. 1. Two Open House events were held in late October in order to showcase the location and orient clinicians and staff to the new space.
Special thanks to Matt Fitzsimmons; Drs. Mike Blazing, Camille Frazier-Mills, Sreekanth Vemulapalli and Anita Kelsey; Annette Moore; Karen Strub; Sarah Moore; Allen Stephens, and Amber Stohl for their exceptional work on planning for the space and helping to executing the move from the Southpoint location. This group led the effort, meeting weekly for more than a year, to ensure that perspectives from all stakeholders within Duke Heart Services were taken into account during the planning phase. In addition, the Division’s staff assistant team led by Mitzi Scarlett and Chris Morgenstern provided additional support with a tremendous volume of appointment rescheduling and helping to ensure our patients were informed.
“This was definitely an all hands on deck operation, said Nick Nguyen, MHA, Duke Heart’s administrator for the Division of Cardiology. “We worked to include multiple viewpoints from across our service line before reaching consensus on operations, layout and design. The team met weekly to consider all aspects of the clinical spaces and operations– working and reworking toward an agreed upon solution.”
Arringdon offers a fresh, bright and spacious location with lots of upgrades, including high-low chairs that convert to exam tables, perimeter work spaces that offer individual sit-stand capability and better ergonomics for the team, as well as ample natural lighting. The clinic, located on the 4th floor, offers a 21 exam room clinic; diagnostic imaging capabilities, including echo, stress tests, and nuclear imaging; and a beautiful, relaxing lobby for patients and their family members that offers both standard and electronic check-in. Everything is larger –including hallways — allowing for easier navigation for patients, especially those who are using mobility aids such as walkers, canes or wheelchairs.
Additional clinical areas at Duke offering services at Arringdon include Duke Eye Center, Obstetrics & Gynecology, Orthopedics and Physical Therapy – making cardiovascular visits even more convenient for our patient population. We anticipate an additional cardiology and EP clinic to open on the 2nd floor of Arringdon in early 2022.
Arringdon Clinic is located at 5601 Arringdon Park Drive, Suite 410 in Morrisville. It is very easy to access off of I-40 (take the Page Road Exit), with free, ample parking and picturesque views of the surrounding area.



WIC Gathering Held
On Thursday evening, Nov. 18, members of our Women in Cardiology (WIC) group were able to gather together for the first time in… far too long. The dinner event, which was hosted by Tracy Wang and sponsored by division chief Manesh Patel, was designed to draw together women from throughout the cardiovascular space at Duke as a means of networking and fostering an important community within Duke Heart.
This will hopefully be one of many such events. Those who joined were able to learn more about each other on a personal and professional level, and to plan future initiatives for Duke WIC. The group recently launched a distribution list to help all WIC members and anyone who is interested in joining the group to stay apprised of future events. If you’d like to be included, please drop a note to: womenincardiology@duke.edu.
The group is grateful to all who took time to help organize and attend the dinner – and they are looking forward to future events as well as welcoming newcomers to the group.
Shown L to R in the group photo are: (Back row) Melissa Daubert, Jenn Rymer, Balim Senman, Manasi Tannu, Karen Flores, Cara Hoke, Ali Corley, Jessica Duran, Pam Douglas, Kelly Arps, Ijeoma Eleazu and Vanessa Blumer. (Front row): Josephine Harrington, Karen Alexander, Tracy Wang, Terry Fortin, Toi Spates, and Kiki Osude. Attendees not shown: our newest cardiology faculty member, Brandy Patterson; heart surgeon, Brittany Zwishenberger and electrophysiologist, Camille Frazier-Mills.



Mentz, Lala Interview Lady & Dr. Glaucomflecken for JCF
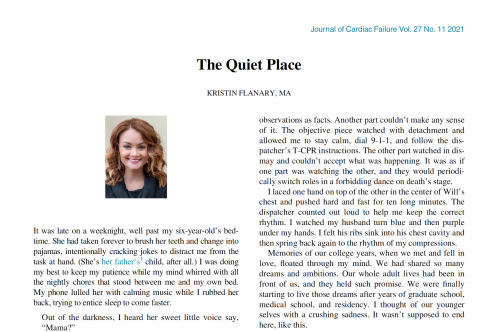
Rob Mentz, chief of our Heart Failure Section and Editor-in-Chief, Journal of Cardiac Failure (JCF) recently joined with JCF deputy editor Anu Lala, a cardiologist at Mount Sinai, to interview Kristin and Will Flanary to explore their experience as co-patients/co-survivors in patient care. Will, an ophthalmologist, is a cardiac arrest survivor thanks to Kristin’s use of CPR on him a year ago.
The duo, known in the Twitterverse as “Lady and Dr. Glaucomflecken,” have developed a large and loyal social media fan base. The video is well worth watching. Additionally, Kristin Flanary wrote a special piece for JCF describing their experience with cardiac arrest, the care they received and their overall journey to recovery. The Quiet Place can be accessed here: https://duke.is/gaaqz.
Great job, Rob!

Cardiac MRI Techs Celebrated During Radiologic Technology Week
Duke Heart leadership took time to recognize our cardiac magnetic resonance imaging (CMRI) technologists last week during National Radiologic Technology Week (Nov. 7-13) by thanking each of them for their professional accomplishments, contributions, and the excellent care they provide to patients. National Radiologic Technology Week is celebrated annually to recognize the vital work of imaging professionals across the nation; it takes place each year during the week of November 8th to commemorate the discovery of the x-ray by Wilhelm Conrad Roentgen on November 8, 1895.
Did you know that Duke’s CMRI program was one of the first such dedicated programs in the world? It’s also one of the largest, performing more than 4,000 clinical procedures per year. In fact, their program volume has grown by more than 18 percent in the past year, despite the pandemic.
CMRI technologists start with basic radiologic training but then work to advance their skills and knowledge by becoming specialized in cardiac imaging — gaining a focused understanding of cardiac anatomy, cardiac rhythms, and cardiac disease processes, mastering cardiac terminology, and utilizing MRI technology for all diagnosis and treatment plans.
Duke clinical and research faculty have developed several advances in the field of CMRI, including the development of the Delayed Enhancement technique, which was done with scientists at Siemens. According to the team, this is arguably the single most important advance to propel cardiac magnetic resonance (CMR) into widespread clinical use. Delayed Enhancement CMR detects injury to the heart and, importantly, can differentiate irreversible damage from damage that may recover with appropriate treatment – offering essential guidance for clinical decisions.
We hope that all members of our CMRI team paused to reflect on and celebrate their personal and team successes during Radiologic Technology Week. We thank you for everything you have done and continue to do for cardiovascular patients at Duke Health.
Shown here are members of the CMRI technologist team during one of their recent celebrations. L to R: Jeanne Dement, Stephen Darty, George Gamondea, Vera Kimbrell, Rafael Rojas, Ryan Seward. Not pictured is technologist Nestor Mena. We think you’re awesome – thank you for all you do!

Thanksgiving Wishes to All
Finally, as we close out a busy AHA week and look to the end of the month, we want to wish all of our Pulse readers a very peaceful, safe and happy Thanksgiving holiday. Thank you for all that you have done this year.
We are incredibly grateful for the talented faculty and staff throughout Duke Heart who have showed up 110 percent throughout a rough year. Our fellows have gone above and beyond during the pandemic and with the expansion of our CCU; our APPs have done an incredible job of enhancing continuity of care over the past year, despite the many challenges confronting healthcare. We have so many reasons to feel grateful — your presence, your effort, your collective spirit matters.
Duke Heart is a place unlike any other — thank you for being a part of our team. Please take time to recognize the wonderful people around you this holiday season.
Upcoming Events & Opportunities
Cardiology Grand Rounds
December 1: The Pathophysiology and Natural History of Perioperative Atrial Fibrillation: Transient Nuisance or Cause for Concern with Bernard Gersh of the Mayo Clinic, Rochester, MN. 5 p.m. Webex.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged.
Duke Heart in the News:
November 12 — Manesh Patel
Practical Cardiology
AHA 2021 Scientific Sessions Preview with Manesh Patel, MD
https://duke.is/cze92
November 13 — Manesh Patel
Medscape
Village Health Workers Successfully Treat Hypertension in Rural China
https://duke.is/wsb5y
November 13 — Manesh Patel
tctMD
RAPID CABG: No Penalty to Early Surgery for ACS After Stopping Ticagrelor
https://duke.is/j8pr6
November 13 — Manesh Patel
Healio/Cardiology
‘Feasible’ doctor-led strategy improved blood pressure control in rural China
https://duke.is/8cfwg
November 14 — Sana Al-Khatib
Healio/Cardiology
No increase in atrial arrhythmias, more activity, less sleep with coffee consumption
https://duke.is/ru2e4
November 14 — Geoffrey Ginsburg
WRAL (NBC – Raleigh)
NIH taps Duke researcher for key role
https://duke.is/53atw
November 14 — Sana Al-Khatib
tctMD
Small CRAVE Trial Reassures on Caffeine Safety in Rhythm Disorders
https://duke.is/6ccjn
November 14 — Jonathan Piccini
Healio/Cardiology
No effect of trigger testing on AF-related quality of life, but fewer events
https://duke.is/pre28
November 14 — Sana Al-Khatib
tctMD
Fitbit Joins the AF Hunt, but Effect on Treatment, Outcomes Unknown
https://duke.is/4dfhc
November 14 — Jacob Schroder
The Philadelphia Inquirer
https://duke.is/6pedr
November 14 — Sana Al-Khatib
Medscape
Fitbit Algorithm Successfully Detects AF
https://www.medscape.com/viewarticle/962910#vp_1
November 14 — Sana Al-Khatib
tctMD
Empagliflozin Safe in Acute HF, Improves ‘Clinical Benefit’ Over Time: EMPULSE
https://duke.is/9t5sg
November 14 — Sana Al-Khatib
Medscape
CRAVE: No Spike in Atrial Arrhythmias Among Coffee Drinkers
https://duke.is/2gzpj
November 14 — Jonathan Piccini
Healio/Cardiology
Cognitive outcomes similar at 2 years with dabigatran vs warfarin in older adults with AF
https://duke.is/g52yp
November 14 — Sana Al-Khatib
Medpage Today
Coffee Causes This One Arrhythmia, Trial Shows
https://www.medpagetoday.com/meetingcoverage/aha/95644
November 15 — Tracy Wang
Medscape
Oral Factor XIa Inhibitor Cuts Post-Op VTE Risk: AXIOMATIC-TKR
https://www.medscape.com/viewarticle/963000#vp_1
November 15 — Manesh Patel
Medscape
High-Dose Fish Oil: “Intriguing” Results in COVID-19
https://www.medscape.com/viewarticle/962972
November 15 — Sana Al-Khatib
HealthDay
Your Morning Cup of Coffee Can Affect Your Heart’s Rhythms
https://duke.is/vqbkr
November 16 — Tracy Wang
Physician’s Weekly
AHA: Novel Oral Factor XIa Inhibitor Demonstrates Prevents VTE in Knee Arthroplasty
https://duke.is/7n339
November 16 — Tracy Wang
Medpage Today
Oral Factor XIa Inhibitor Sets the Stage for a Safer Anticoagulant
https://www.medpagetoday.com/meetingcoverage/aha/95710
November 16 — Manesh Patel
Medscape
No Benefit of Antiplatelets in Noncritical COVID: ACTIV-4a
https://www.medscape.com/viewarticle/963093
November 16 — Sana Al-Khatib
Medpage Today
Hospitalized Acute HF Patients See Clinical Benefits With Empagliflozin
https://www.medpagetoday.com/meetingcoverage/aha/95694
November 17 — Sunil Rao
Medscape
Left-Main PCI, CABG Mortality Similar; Choice Remains Complex
https://www.medscape.com/viewarticle/963198
November 19 — Manesh Patel
MSN.com
Advances in Care, Impact of COVID Highlights of Latest Cardiologists’ Meeting
https://duke.is/mjpgc
Duke Heart Center Pulse Week ending 11-14-2021
Chief’s message:
AHA21: This weekend we had the AHA meeting 2021 where we had several of our faculty and fellows presenting. Given the great science and immediate impact on clinical care – we will have updates in the upcoming weeks. Want to personally congratulate and thank all the faculty and fellows presenting at this years scientific sessions.
Highlights of the week:
Thomas named Vice Dean for Diversity, Equity and Inclusion for Duke SOM

Kevin Thomas, MD, associate professor of medicine in cardiology and an electrophysiologist in the Division of Cardiology at Duke, has been named Duke University School of Medicine’s first Vice Dean for Diversity, Equity and Inclusion. Dr. Thomas currently serves as Assistant Dean for Underrepresented Faculty Development for the School of Medicine and as Director of Faculty Diversity and Health Disparities Research for Duke Clinical Research Institute (DCRI).
As Vice Dean for Diversity, Equity and Inclusion, Dr. Thomas will lead the School’s Office of Diversity and Inclusion and will serve as a key advisor and partner to the Dean to advance the School’s goal of cultivating an inclusive, welcoming, respectful and supportive working and learning environment. Dr. Thomas and his team will collaborate with staff, faculty and students across the school to implement the School’s Moments to Movement Strategic Plan to Dismantle Racism and Advance Equity, Diversity and Inclusion and to develop and implement a broad range of policies and programs rooted in equity that foster a greater sense of belonging, engagement, and achievement amongst all members of the School of Medicine and larger Duke Health community.
Dr. Thomas has developed and led a number of programs at Duke that facilitate academic achievement and promotion of Underrepresented Racial and Ethnic Faculty in the School of Medicine, including the School’s Academic Development, Advocacy, Networking Coaching, and Education in Underrepresented Populations (ADVANCE-UP) faculty development program. In 2016, he was the inaugural recipient of the School’s Michelle P. Winn Inclusive Excellence Award, which recognizes individuals who have made significant contributions to diversity and inclusion.
Dr. Thomas received a BS degree from Emory University, his MD from the University of North Carolina at Chapel Hill, and was Chief Resident in Medicine at Duke University in 2003-2004. In 2007, he completed fellowships in cardiology and cardiac electrophysiology at Duke and joined the Duke faculty.
The announcement was made by Mary E. Klotman, MD, Dean of the School of Medicine, on November 8. Dr. Thomas’s service in this role is effective immediately.
Congratulations, Kevin – well deserved!
Perfusion Team Update
 Congratulations to the following members of our Perfusion Team! Andrew (AJ) Jack, CCP, Demetria Middleton, CCP,
Congratulations to the following members of our Perfusion Team! Andrew (AJ) Jack, CCP, Demetria Middleton, CCP,  DeShantra Kelly, CCP, and Heather Keck, CCP have passed both the Perfusion Basic Science Examination (PBSE) and the Clinical Applications in Perfusion Examination (CAPE). They are now designated by the American Board of Cardiovascular Perfusion as Certified Clinical Perfusionists (CCP). We are so proud of them – this accomplishment is the culmination of many years of hard work and sacrifice.
DeShantra Kelly, CCP, and Heather Keck, CCP have passed both the Perfusion Basic Science Examination (PBSE) and the Clinical Applications in Perfusion Examination (CAPE). They are now designated by the American Board of Cardiovascular Perfusion as Certified Clinical Perfusionists (CCP). We are so proud of them – this accomplishment is the culmination of many years of hard work and sacrifice.
Kudos also to the Pediatric Perfusion Team. They have successfully rolled out new state of the art technology in cardiopulmonary bypass this week. New Quantum pediatric heart-lung machines with Viper technology made by Spectrum Medical came online this past week – they are equipped with enhanced digitization, safety monitoring and best practice alerts. Spectrum customized the software with our Duke team to fit our specific needs and goals. This software enables the Duke team to continue to customize and design best practices alerts to optimize the care of our patients.
After many, many months of design, coordination, and simulation the team successfully pumped their first case with these heart lung machines on Wednesday, November 10th — a neonatal arterial switch operation.
Pictured here some of the members of the pediatric perfusion team: Amy Evans, Rachel Gambino, Felicia Shugars, Greg Smigla, and Travis Siffring.
Great work, everyone!!!

Shout-out to Hernandez
A shout-out to Adrian Hernandez who volunteered his entire Sunday last weekend (November 7) to help give COVID vaccines to kids at Durham Academy and throughout the broader Durham community.
Our hat tip comes from Jenn Rymer: “I got my son vaccinated and was so thankful to do so, and saw a lot of other Duke parents getting their kids vaccinated. I really appreciated people like Adrian being there to hopefully get our world back to a normal place!”
Nicely done, Adrian!
ICYMI: Code Blue & Duke’s Chaplain Service
A new peer-reviewed journal article is out in the American Journal of Critical Care: “A Descriptive Study of Chaplains’ Code Blue Responses” (https://doi.org/10.4037/ajcc2021854) by co-authors Callie Tennyson, John Oliver (chaplain services) and Karen Joost (pediatrics, palliative care), all of Duke. Background: Family presence during resuscitation is the compassionate practice of allowing a patient’s family to witness treatment for cardiac or respiratory arrest (code blue event) when appropriate. Offering family presence during resuscitation as an interprofessional practice is consistent with patient- and family-centered care. In many institutions, the role of family facilitator is not formalized and may be performed by various staff members. At the large academic institution of this study, the family facilitator is a member of the chaplain staff.
Congrats, Callie, John and Karen!
Duke Heart Family Halloween Fun
Many thanks to Jamie Jollis for collecting some really adorable photos of our Duke Heart team family members to share with Pulse. We hope everyone had an enjoyable Halloween!



Upcoming Events & Opportunities
Cardiology Grand Rounds
We will not hold Cardiology Grand Rounds this week.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged.
Duke Heart in the News:
November 5 — Edward Chen
tctMD
TAVI Edges Out Surgery in 2-Year Costs for Low-risk Patients: PARTNER 3
https://bit.ly/3qBHWjE
November 5 — Jennifer Rymer
Medpage Today
Surgical Scores Shine for Prognostication in No-Option PCI — Surgeons, Not So Much
https://bit.ly/3c6YyaB
November 8 — Manesh Patel
tctMD
AHA 2021 Tackles AF Triggers, Watchful Waiting in AS, Data Overload, and More
https://bit.ly/3FfpjX1
November 8 — Manesh Patel
Medscape
AHA 2021 Puts Scientific Dialogue, Health Equity Center Stage
https://wb.md/31WtKYm
November 9 — Geoffrey Ginsburg
Triangle Business Journal
Duke professor leaving to join NIH for ‘once in a lifetime opportunity’
https://bit.ly/3wIdxRR
November 9 — Mitchell Krucoff
tctMD
Cardiogenic Shock: SCAI Categories Get a Rethink as Research Rolls On
https://bit.ly/3n9YtJD
November 9 — Jennifer Rymer
MDEdge
At 5 years, iFR found as effective and safe as FFR for guiding PCI intervention
https://bit.ly/30pwtsS
November 10 — Pamela Douglas
Radiology Today
Heart CT Shows Slight Benefit Over Stress Tests
https://bit.ly/3HhxcwR
November 10 — Pamela Douglas
tctMD
Debating ISCHEMIA: Do the Results Apply to CABG, Too?
https://bit.ly/3CfQ3V7
November 12 — Robert Califf
Associate Press*
Biden picks ex-FDA chief Robert Califf to again lead agency
https://bit.ly/3FcAG1W
*story appears in dozens of news outlets across the U.S.
November 12 — Robert Califf
Politico
Biden nominates Califf as FDA chief
https://politi.co/3FizFoK
Division of Cardiology Publications Indexed in PubMed November 4-10, 2021
Berntorp K, Persson J, Koul SM, Patel MR, Christiansen EH, Gudmundsdottir I, Yndigegn T, Omerovic E, Erlinge D, Fröbert O, Götberg M. Instantaneous wave-free ratio compared with fractional flow reserve in PCI: A cost-minimization analysis. Int J Cardiol 2021;344:54-59. PM: 34600977.
Blumenthal JA, Smith PJ, Jiang W, Hinderliter A, Watkins LL, Hoffman BM, Kraus WE, Liao L, Davidson J, Sherwood A. Effect of Exercise, Escitalopram, or Placebo on Anxiety in Patients With Coronary Heart Disease: The Understanding the Benefits of Exercise and Escitalopram in Anxious Patients With Coronary Heart Disease (UNWIND) Randomized Clinical Trial. JAMA Psychiatry 2021;78(11):1270-1278. PM: 34406354.
Chouairi F, Miller PE, Guha A, Clarke JR, Reinhardt SW, Ahmad T, Freeman JV, Desai NR, Friedman DJ. Cannabis use disorder among atrial fibrillation admissions, 2008-2018. Pacing Clin Electrophysiol 2021;44(11):1934-1938. PM: 34506639.
Darden D, Duong T, Du C, Munir MB, Han FT, Reeves R, Saw J, Zeitler EP, Al-Khatib SM, Russo AM, Minges KE, Curtis JP, Freeman JV, Hsu JC. Sex Differences in Procedural Outcomes Among Patients Undergoing Left Atrial Appendage Occlusion: Insights From the NCDR LAAO Registry. JAMA Cardiol 2021;6(11):1275-1284. PM: 34379072.
Dupre ME, Farmer HR, Xu H, Navar AM, Nanna MG, George LK, Peterson ED. The Cumulative Impact of Chronic Stressors on Risks of Myocardial Infarction in US Older Adults. Psychosom Med 2021;83(9):987-994. PM: 34297011.
Feng KY, O’Connor CM, Clare R, Alhanti B, Piña IL, Kraus WE, Whellan DJ, Mentz RJ. Greater Pain Severity Is Associated with Worse Outcomes in Patients with Heart Failure. J Cardiovasc Transl Res 2021;14(5):984-991. PM: 33564986.
Grubb AF, Greene SJ, Fudim M, Dewald T, Mentz RJ. Drugs of Abuse and Heart Failure. J Card Fail 2021;27(11):1260-1275. PM: 34133967.
Hein AM, Scialla JJ, Sun JL, Greene SJ, Shaw LK, Chiswell K, Pun PH, Mentz RJ. Estimated Glomerular Filtration Rate Variability in Patients With Heart Failure and Chronic Kidney Disease. J Card Fail 2021;27(11):1175-1184. PM: 33971291.
Klem I, Cavalier JS. Vasodilator Stress Magnetic Resonance Imaging in Patients With Prior Myocardial Infarction. JACC Cardiovasc Imaging 2021;14(11):2152-2154. PM: 34147445.
Kumar N, Xu H, Garg N, Pandey A, Matsouaka RA, Field ME, Turakhia MP, Piccini JP, Lewis WR, Fonarow GC. Patient characteristics, care patterns, and outcomes of atrial fibrillation associated hospitalizations in patients with chronic kidney disease and end-stage renal disease. Am Heart J 2021;242:45-60. PM: 34216572.
Lala A, Mentz RJ. Following Our Hearts: Prioritizing Self-care and Wellness. J Card Fail 2021;27(11):1163-1164. PM: 34749927.
Naidu SS, Baron SJ, Eng MH, Sathanandam SK, Zidar DA, Feldman DN, Ing FF, Latif F, Lim MJ, Henry TD, Rao SV, Dangas GD, Hermiller JB, Daggubati R, Shah B, Ang L, Aronow HD, Banerjee S, Box LC, Caputo RP, Cohen MG, Coylewright M, Duffy PL, Goldsweig AM, et al. Hot topics in interventional cardiology: Proceedings from the society for cardiovascular angiography and interventions (SCAI) 2021 think tank. Catheter Cardiovasc Interv 2021;98(5):904-913. PM: 34398509.
Nathan SD, Waxman A, Rajagopal S, Case A, Johri S, DuBrock H, De La Zerda DJ, Sahay S, King C, Melendres-Groves L, Smith P, Shen E, Edwards LD, Nelsen A, Tapson VF. Inhaled treprostinil and forced vital capacity in patients with interstitial lung disease and associated pulmonary hypertension: a post-hoc analysis of the INCREASE study. Lancet Respir Med 2021;9(11):1266-1274. PM: 34214475.
Ramacciotti E, Agati LB, Calderaro D, Volpiani GG, de Oliveira CCC, Aguiar VCR, Rodrigues E, Sobreira ML, Joviliano EE, Dusilek C, Itinose K, Dedivitis RA, Cortina AS, Sanches SMV, de Moraes NF, Tierno PFGMM, de Oliveira ALML, Tachibana A, Chate RC, et al. Medically Ill hospitalized Patients for COVID-19 THrombosis Extended ProphyLaxis with rivaroxaban ThErapy: Rationale and Design of the MICHELLE Trial. Am Heart J 2021;242:115-122. PM: 34480880.
Samsky MD, Morrow DA, Proudfoot AG, Hochman JS, Thiele H, Rao SV. Cardiogenic Shock After Acute Myocardial Infarction: A Review. JAMA 2021;326(18):1840-1850. PM: 34751704.
Shi H, Ossip DJ, Mayo NL, Lopez DA, Block RC, Post WS, Bertoni AG, Ding J, Chen S, Yan C, Xie Z, Hoeschele I, Liu Y, Li D. Role of DNA methylation on the association between physical activity and cardiovascular diseases: results from the longitudinal multi-ethnic study of atherosclerosis (MESA) cohort. BMC Genomics 2021;22(1):790. PM: 34732130.
Sofer T, Kurniansyah N, Aguet F, Ardlie K, Durda P, Nickerson DA, Smith JD, Liu Y, Gharib SA, Redline S, Rich SS, Rotter JI, Taylor KD. Benchmarking association analyses of continuous exposures with RNA-seq in observational studies. Brief Bioinform 2021;22(6):bbab194. PM: 34015820.
Sun D, Richard M, Musani SK, Sung YJ, Winkler TW, Schwander K, Chai JF, Guo X, Kilpeläinen TO, Vojinovic D, Aschard H, Bartz TM, Bielak LF, Brown MR, Chitrala K, Hartwig FP, Horimoto ARVR, Liu Y, Manning AK, Noordam R, Smith AV, Harris SE, Kühnel B, et al. Multi-Ancestry Genome-wide Association Study Accounting for Gene-Psychosocial Factor Interactions Identifies Novel Loci for Blood Pressure Traits. HGG Adv 2021;2(1):100013. PM: 34734193.
Taron J, Foldyna B, Mayrhofer T, Osborne MT, Meyersohn N, Bittner DO, Puchner SB, Emami H, Lu MT, Ferencik M, Pagidipati NJ, Douglas PS, Hoffmann U. Risk Stratification With the Use of Coronary Computed Tomographic Angiography in Patients With Nonobstructive Coronary Artery Disease. JACC Cardiovasc Imaging 2021;14(11):2186-2195. PM: 33865792.
Vemulapalli S, Stebbins A, Jones WS, Gutierrez JA, Patel MR, Dolor RJ, Pellikka PA, Alhanti B, Hoffmann U, Douglas PS. Cardiovascular risk and outcomes in symptomatic patients with suspected coronary artery disease and non coronary vascular disease: A report from the PROMISE trial. Am Heart J 2021;242:82-91. PM: 34384742.
Weissler EH, Ford CB, Patel MR, Goodney P, Clark A, Long C, Jones WS. Younger patients with chronic limb threatening ischemia face more frequent amputations. Am Heart J 2021;242:6-14. PM: 34371002.
Westerterp KR, Yamada Y, Sagayama H, Ainslie PN, Andersen LF, Anderson LJ, Arab L, Baddou I, Bedu-Addo K, Blaak EE, Blanc S, Bonomi AG, Bouten CVC, Bovet P, Buchowski MS, Butte NF, Camps SGJA, Close GL, Cooper JA, Das SK, Cooper R, Dugas LR, Ekelund U, et al. Physical activity and fat-free mass during growth and in later life. Am J Clin Nutr 2021;114(5):1583-1589. PM: 34477824.
Duke Heart Week ending November 7th 2021
Highlights of the week:
Ginsburg named Chief Medical & Scientific Officer, NIH All of Us Research Program
 Geoffrey S. Ginsburg, MD, PhD, a professor of medicine in cardiology, a professor in pathology, biostatistics and bioinformatics, a professor of biomedical engineering, and a professor in Duke’s School of Nursing, will leave Duke to assume the role of Chief Medical and Scientific Officer for the National Institutes of Health (NIH) All of Us Research Program, effective January 2022. Dual announcements were made on Nov. 3 by the NIH and Duke School of Medicine.
Geoffrey S. Ginsburg, MD, PhD, a professor of medicine in cardiology, a professor in pathology, biostatistics and bioinformatics, a professor of biomedical engineering, and a professor in Duke’s School of Nursing, will leave Duke to assume the role of Chief Medical and Scientific Officer for the National Institutes of Health (NIH) All of Us Research Program, effective January 2022. Dual announcements were made on Nov. 3 by the NIH and Duke School of Medicine.
In his new role, Ginsburg will have the opportunity to build out the research agenda for All of Us and to engage research scientists across all 27 institutes of the NIH as well as the research community across the U.S. and internationally.
“As I reflect on what I’ve been doing across most of my career both at Millennium Pharmaceuticals in the late 1990s and early 2000s and then at Duke for the last 17 years, this opportunity with All of Us is the capstone for everything I’ve been thinking about,” says Ginsburg. “In the U.S., this platform is second to none in terms of the ability to carry out the research agenda for precision medicine. It encompasses an amazing set of resources that has the potential to really change how we practice medicine, how we do research, and it brings to fruition my particular focus on individualized care, health, and population health.”
Originally announced as the Precision Medicine Initiative cohort program in 2015 by former U.S. President Barack Obama, the name was later changed to the All of Us Research Program, which aims to gather data from at least one million diverse people aged 18 and up who reside in the U.S. as a means of accelerating biomedical research and improving health. The data repository is expected to permit researchers to “take into account individual differences in lifestyle, socioeconomic factors, environment, and biologic characteristics in order to advance precision diagnosis, prevention, and treatment,” according to a 2019 special report in the New England Journal of Medicine.
All of Us is enrolling participants from a network of more than 340 recruitments sites. According to the All of Us research website more than 429,000 participants have joined the program and more than 329,000 have contributed biospecimens to the repository, with more than 80 percent of those participants hailing from groups that have been historically underrepresented in biomedical research. The first 80,000 whole genome sequences will be released by the end of the year.
“A visionary leader in genomics and precision medicine, Dr. Ginsburg has been instrumental in Duke’s work to advance this still emerging field of science, foster important collaborations, and improve human health,” said Mary E. Klotman, MD, Dean, Duke University School of Medicine.
Indeed, Ginsburg has been a transformative leader for Duke University and the School of Medicine for 17 years. He is the founding director of the Center for Applied Genomics & Precision Medicine (CAGPM) and also founding director of MEDx, a partnership between Duke’s Schools of Medicine and Engineering, which is designed to stimulate collaboration and innovation. During his tenure at Duke, Ginsburg has pioneered translational genomics, the development of novel diagnostics, and precision medicine. With a strong commitment to interdisciplinary science and innovation, he has led projects to develop predictive models for common complex diseases using high dimensional genomic data and developed partnerships with engineering colleagues to develop novel point of care sensors.
“Dr. Ginsburg’s achievements at Duke are numerous, and they all center around genetic science and entrepreneurship fueled by innovation and collaboration,” says Kathleen Cooney, MD, chair, Duke Department of Medicine. “Geoff has made an enormous difference here as founder of both the Center for Applied Genomics & Precision Medicine and MEDx. His ability to identify and build partnerships across the Duke enterprise with the Pratt School of Engineering, Duke Heart, and many, many others has been a driving force behind our leadership in precision medicine.”
An internationally recognized expert in genomics and personalized medicine, Ginsburg has authored or co-authored more than 300 peer-reviewed publications. His research has been supported by the NIH, the Department of Defense, National Aeronautics and Space Administration (NASA), the Defense Advanced Research Projects Agency (DARPA), the Gates Foundation, and others. Throughout his career, he has demonstrated a strong commitment to interdisciplinary science and innovation, with work spanning oncology, infectious diseases, cardiovascular disease and metabolic disorders. He is a founding co-chair of the International HundredK+ Cohorts Consortium, and founder and president of the Global Genomic Medicine Collaborative (G2MC), a not-for-profit organization aimed at creating international partnerships to advance the implementation of precision medicine.
Ginsburg has served on a number of advisory councils for the NIH including the National Heart, Lung and Blood Institute’s (NHLBI) Board of External Experts (2007-2016), the National Advisory Council for Human Genome Research (2009-2011), the External Advisory Committee of the Pharmacogenomics Research Network (2010-2013), the National Center to Accelerate Translational Science (NCATS) Advisory Council (2012-2017), the NHLBI External Advisory Board for Precision Medicine Initiative (2015-2016), and most recently on the Advisory Committee to the Director of the NIH (2016-2020), and the Genomic Medicine Working Group for the National Human Genome Research Institute (2011 to present). He has held leadership roles as the Chair of the NIH CTSA Translational Steering Committee and as Vice Chair of the Cures Acceleration Network Advisory Board.
Ginsburg will step down from both of his directorship roles at Duke in late December. He will remain on faculty at Duke as an adjunct professor in the School of Medicine. The Center for Applied Genomics will continue to grow and succeed at Duke thanks to the team Ginsburg has grown over the years. Dr. Cooney will serve as interim center director to ensure a smooth and orderly transition once a new director is named. Dean Klotman, Provost Sally Kornbluth, and Jerome Lynch, who was recently named dean of Duke’s Pratt School of Engineering, will work together to plan the future direction of MEDx.
We are so excited for Geoff and this incredible career opportunity for him at the NIH! He has done an outstanding job at Duke and he will be deeply missed. Please join us in congratulating him on this exciting next step in his accomplished career!
Celebrating Nurse Practitioner Week 2021
It’s Nurse Practitioner (NP) Week, November 7-13. Please join us in helping to celebrate our many nurse  practitioners throughout Duke Heart and Duke Health. They are a vital part of all Duke care teams and an invaluable resource to our patients and their loved ones.
practitioners throughout Duke Heart and Duke Health. They are a vital part of all Duke care teams and an invaluable resource to our patients and their loved ones.
NP Week recognizes the contributions NPs make to the health of patients nationwide. These health care professionals practice in clinics, hospitals, emergency rooms, urgent care centers, nursing homes and private practices across the country — wherever patients are in need. They’ve done an exceptional job in all areas of Duke Heart throughout the COVID-19 pandemic.
Did you know there are more than 325,000 NPs licensed in the U.S.? According to the American Association of Nurse Practitioners, 81 percent of full time NPs see Medicare patients and 78.7 percent see Medicaid patients; 42.5 percent hold hospital privileges. NPs assess patients, order and interpret tests, make diagnoses and provide treatment, including prescribing medications. As clinicians who blend clinical expertise with an added emphasis on disease prevention and health management, NPs are critical members of health care teams across the U.S.
Please join us in thanking and celebrating our Duke Heart Nurse Practitioners!
Positive Top Line Results from U.S. Randomized OCS DCD Heart Trial Announced
TransMedics Group, Inc., announced this week positive topline results from its OCS Donation After Circulatory death (DCD) Heart Trial, which was designed as the first and only randomized trial to compare post-transplant clinical outcomes between hearts transplanted from DCD donors that were resuscitated and assessed on their OCS Heart System and standard criteria donation after brain death (DBD) heart transplants that were preserved using cold storage in the U.S.
The primary goal of the study was to assess the effectiveness and safety of OCS Heart technology to expand the heart donor pool with hearts from DCD donors. Heart transplant candidates were randomized 3:1 into two groups: DCD Heart Possible (DCD) or DBD cold stored hearts (Control). The trial protocol compared the post-transplant outcomes from recipients of DCD hearts preserved on OCS (DCD) to all those who received standard criteria DBD hearts preserved with cold storage (DBD Control).
The OCS DCD Heart trial achieved its primary clinical objectives by meeting the primary
effectiveness endpoint of 6 month patient survival post-transplant which was 95 percent for OCS DCD arm vs. 89 percent for the Control cold storage DBD arm. Even when the outcomes were adjusted for all risk factors between the two groups the results were 94 percent for OCS and 90 percent for Control (non-inferiority p<0.0001), according to the statement released by TransMedics on Nov. 3.
Of 101 DCD donor hearts that were perfused and assessed on OCS Heart technology, 90 were successfully transplanted resulting in a utilization rate of 89 percent. Long-term follow-up is ongoing and the final results are expected to be presented at the International Society for Heart and Lung Transplantion 42nd annual meeting and scientific sessions in April 2022 in Boston.
The OCS Heart System was approved by the U.S. Food and Drug Administration (FDA) for its
DBD heart indication in September 2021. According to TransMedics, the DCD trial results will be submitted shortly to the FDA in a premarket approval supplement to support the approval for the OCS DCD heart indication.

“The OCS DCD Heart Trial provides objective randomized evidence showing high utilization and
excellent short-term clinical outcomes using hearts that historically were never considered for
transplants in the U.S.,” said Jacob Schroder, MD, surgical director of heart transplantation at
Duke University Health System and the principal investigator for the OCS DCD Heart Trial. “The
more widespread use of DCD hearts for transplantation is the biggest thing to happen since the
beginning of heart transplantation.”
Duke was the first U.S. site to enroll a patient into the TransMedics OCS DCD Heart Trial. Schroder led a Duke Heart transplant team in the first DCD heart transplant in the U.S. on Dec. 2, 2019 at Duke University Hospital. Duke was the lead enroller in the trial.
Al-Khatib, Daubert Listed as Top Scholars, Sudden Cardiac Death
Sana Al-Khatib and Jim Daubert, electrophysiologists with Duke Heart, have been listed by Expertscape in

 the top 1 percent of sudden cardiac death experts contributing peer-reviewed journal articles to the scientific literature over the past 10 years. Al-Khatib is ranked as the top contributor, globally.
the top 1 percent of sudden cardiac death experts contributing peer-reviewed journal articles to the scientific literature over the past 10 years. Al-Khatib is ranked as the top contributor, globally.
Expertscape is an online tool geared toward consumers seeking information regarding the most knowledgeable experts in various biomedical research fields. According to their website, Expertscape bases its rankings by mining available scientific publications via online search engines such as PubMed.
Congrats, Sana and Jim!
13th Annual Pulmonary Hypertension Symposium Held
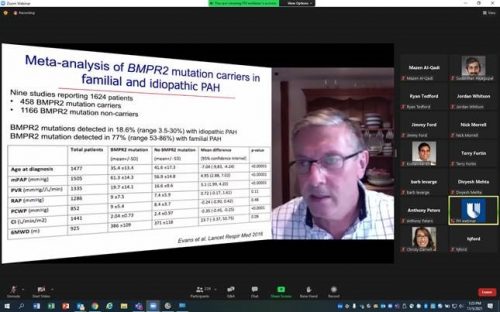
The 13th Annual North Carolina Research Triangle Pulmonary Hypertension Symposium was held on Friday, Nov. 5. Course directors H. James Ford of UNC School of Medicine and Duke Heart’s Terry Fortin pulled together a terrific program for more than 240 attendees. In addition to Fortin, Duke presenters included Kishan Parikh, Sudarshan Rajagopal and Jordan Whitson. The event was held online and presented by Duke Health and UNC School of Medicine.

Katz Opens NYU Critical Care Cardiology Symposium
Jason Katz served as a co-course director of the first NYU Langone Critical Care Cardiology Symposium held virtually on Friday, Nov. 5. He kicked off session 1 of the symposium with his presentation, Why Do We Need This Conference? A Journey Through the Evolution of Critical Care Cardiology. The symposium, more than seven years in the making, was a resounding success with more than 850 registrants from over 28 countries. Katz not only helped plan the event, he also served as a moderator for several sessions and pledged to cover costs for any Duke cardiology fellow wishing to attend. Katz’s fellow co-course directors included Carlos L. Alviar, Samuel Bernard, James Horowitz and Eugene Yuriditsky, all of the NYU Grossman School of Medicine, and Christopher Barnett of the University of California, San Francisco.
The NYU Langone Critical Care Cardiology Symposium became the first dedicated Cardiac Critical Care conference to take place in the U.S. Way to go, Jason!
Duke Heart at TCT2021
TCT2021, the Transcatheter Cardiovascular Therapeutics 2021 conference was held Nov. 4-6 as a hybrid event based in Orlando and online. Duke had a strong presence with the following moderators and discussants: Pamela Douglas, Sunil Rao, Jennifer Rymer, Mitch Krucoff, Rob Califf, Sreekanth Vemulapalli, Vishal Rao, Marat Fudim, Christopher Granger and Renato Lopes. Poster presentations included Duke cardiology fellow Zach Wegermann. Jenn Rymer is quoted in several news stories, be sure to check out our News section, below.
BTW, TCT2021 content is on demand and free for one year. Great job, everyone!


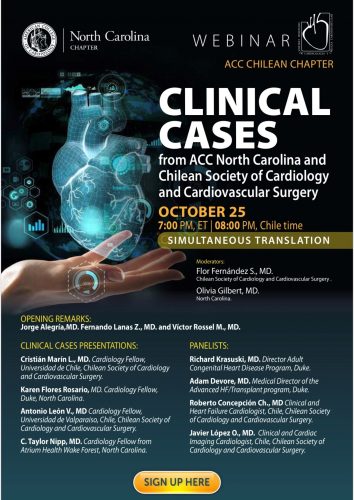
Flores Rosario Presents at ACC NC-Chile Case Conference
Karen Flores Rosario, a Duke cardiology 2nd year fellow, was chosen to give an international conference presentation on behalf of the North Carolina chapter of the American College of Cardiology and the Chilean Society of Cardiology and Cardiovascular Surgery (SOCHICAR). The webinar, Clinical Cases from ACC North Carolina and SOCHICAR was held Oct. 25. Flores Rosario presented a brilliant case of lamin cardiomyopathy and did an exceptional job. The discussion was co-moderated by Drs. Adam DeVore and Richard Krasuski.
Well done, Karen!
Upcoming Events & Opportunities
Cardiology Grand Rounds
November 9: Case Conference – Lessons Learned in Peri-Operative LVAD Care with Amanda Coniglio. 5 p.m. Webex.
Request for Nominations: Samuel DuBois Cook Society Awards

The Samuel DuBois Cook Society invites nominations of individuals from every sector of the Duke Community: staff, administrators, and students — undergraduate, graduate or professional.
Founded to be an instrument of social engagement and change, the Cook Society seeks to recognize members of the Duke community who reflect in their work or in their academic pursuits, the objectives to which Dr. Cook dedicated his professional life — social justice, mentoring, the University’s relationship to the black community, and his vision of the “beloved community,” seeking to improve relations among persons of all backgrounds.
Nominations are due November 8, 2021, and winners will be notified in the first week of December.
Awards will be presented during the annual Cook Society Awards Ceremony on February 22, 2022, at the Washington Duke Inn & Golf Club.
In evaluating nominees, the committee seeks members of the Duke community who:
- Actively nurture a sense of community and belonging for Black people.
- Commit to translate the promise and potential of Black people at Duke into fulfillment and actuality
- Foster positive and constructive interpersonal and intergroup relations within both Duke University’s and Durham’s Black communities
- Cultivate positive relations between Black people and other ethnic, racial, and national groups on the basis of an enlightened appreciation and knowledge of our historic interdependence
To learn more/make a nomination please click here.
Request for Nominations: Raymond Gavins Distinguished Faculty Award
The Samuel DuBois Cook Society invites nominations of faculty whose teaching, mentoring, research, publishing, and engagement with faculty, students and staff have helped to improve relations among people of all backgrounds at Duke and beyond.
Nominations are due November 8, 2021, and winners will be notified in the first week of December. Awards will be presented during the annual Cook Society Awards Dinner on February 22, 2022, at the Washington Duke Inn & Golf Club.
In evaluating nominees, the committee seeks faculty who:
- Actively nurture a sense of community and belonging for Black people.
- Commit to translate the promise and potential of Black people at Duke into fulfillment and actuality
- Foster positive and constructive interpersonal and intergroup relations within both Duke University’s and Durham’s Black communities
- Cultivate positive relations between Black people and other ethnic, racial, and national groups on the basis of an enlightened appreciation and knowledge of our historic interdependence
To learn more/make a nomination please click here.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged.
Duke Heart in the News:
October 28 — Duke University Hospital
The Fox Magazine
11 Six Reasons To Relocate To North Carolina: A Useful Guide
https://bit.ly/3nSuXHf
October 29 — Duke University Hospital/Cardiology
Cardiovascular Business
Learning from the best: The world’s top 20 universities for cardiology
https://bit.ly/3BPCDPP
November 1 — Joseph Turek
Science
Skin, nerve transplants from genetically modified pigs could help humans, but organs are a way off
https://bit.ly/3mChFiP
November 2 — Robert Califf and Haider Warraich
STAT
I’ve worked with Robert Califf. He is the leader the FDA needs
https://bit.ly/3CHJHiz
November 4 — Jennifer Rymer
tctMD
Good Early Outcomes With PCI in Complex Patients Unsuited to Surgery: OPTIMUM
https://bit.ly/3D6RHdj
November 4 — Jennifer Rymer
tctMD
OCT Guidance Cuts Stent Use in STEMI Without Plaque Rupture: EROSION III
https://bit.ly/3CVQsNY
Division of Cardiology Publications Indexed in PubMed Oct. 28-Nov. 3, 2021
Breitbart P, Koch A, Schmidt M, Magedanz A, Lindhoff-Last E, Voigtländer T, Schmermund A, Mehta RH, Eggebrecht H. Clinical and cardiac magnetic resonance findings in post-COVID patients referred for suspected myocarditis. Clin Res Cardiol 2021;110(11):1832-1840. PM: 34448040.
Cho SM, Floden D, Wallace K, Hiivala N, Joseph S, Teuteberg J, Rogers JG, Pagani FD, Mokadam N, Tirschwell D, Li S, Starling RC, Mahr C, Uchino K. Long-Term Neurocognitive Outcome in Patients With Continuous Flow Left Ventricular Assist Device. JACC Heart Fail 2021;9(11):839-851. PM: 34509403.
Dorling JL, Belsky DW, Racette SB, Das SK, Ravussin E, Redman LM, Höchsmann C, Huffman KM, Kraus WE, Kobor MS, MacIsaac JL, Lin DTS, Corcoran DL, Martin CK. Association between the FTO rs9939609 single nucleotide polymorphism and dietary adherence during a 2-year caloric restriction intervention: Exploratory analyses from CALERIE™ phase 2. Exp Gerontol 2021;155:111555. PM: 34543722.
Duan KI, Helfrich CD, Rao SV, Neely EL, Sulc CA, Naranjo D, Wong ES. Cost analysis of a coaching intervention to increase use of transradial percutaneous coronary intervention. Implement Sci Commun 2021;2(1):123. PM: 34706775.
Ezekowitz JA, Zheng Y, Cohen-Solal A, Melenovský V, Escobedo J, Butler J, Hernandez AF, Lam CSP, O’Connor CM, Pieske B, Ponikowski P, Voors AA, deFilippi C, Westerhout CM, McMullan C, Roessig L, Armstrong PW. Hemoglobin and Clinical Outcomes in the Vericiguat Global Study in Patients With Heart Failure and Reduced Ejection Fraction (VICTORIA). Circulation 2021;144(18):1489-1499. PM: 34432985.
Friedland A, Hernandez AF, Anstrom KJ, Chen-Lim ML, Cohen LW, Currier JS, Forrest CB, Fraser R, Fraulo E, George A, Handberg E, Jackman J, Koellhoffer J, Lawrence D, Leverty R, McAdams P, McCourt B, Mickley B, Naqvi SH, O’Brien EC, Olson R, Prater C, et al. Design of the Healthcare Worker Exposure Response and Outcomes (HERO) research platform. Contemp Clin Trials 2021;109:106525. PM: 34371163.
Hess CN, Patel MR, Bauersachs RM, Anand SS, Debus ES, Nehler MR, Fanelli F, Yeh RW, Secemsky EA, Beckman JA, Mauri L, Govsyeyev N, Capell WH, Brackin T, Berkowitz SD, Muehlhofer E, Haskell LP, Hiatt WR, Bonaca MP. Safety and Effectiveness of Paclitaxel Drug-Coated Devices in Peripheral Artery Revascularization: Insights From VOYAGER PAD. J Am Coll Cardiol 2021;78(18):1768-1778. PM: 34711335.
Karnam S, Maddala R, Stiber JA, Rao PV. Drebrin, an actin-binding protein, is required for lens morphogenesis and growth. Dev Dyn 2021;250(11):1600-1617. PM: 33896079.
Koontz BF, Levine E, McSherry F, Niedzwiecki D, Sutton L, Dale T, Streicher M, Rushing C, Owen L, Kraus WE, Bennett G, Pollak KI. Increasing physical activity in Cancer Survivors through a Text-messaging Exercise motivation Program (ICanSTEP). Support Care Cancer 2021;29(12):7339-7349. PM: 34050402.
Miller PE, Mullan CW, Chouairi F, Sen S, Clark KA, Reinhardt S, Fuery M, Anwer M, Geirsson A, Formica R, Rogers JG, Desai NR, Ahmad T. Mechanical ventilation at the time of heart transplantation and associations with clinical outcomes. Eur Heart J Acute Cardiovasc Care 2021;10(8):843-851. PM: 34389855.
Noyd DH, Berkman A, Howell C, Power S, Kreissman SG, Landstrom AP, Khouri M, Oeffinger KC, Kibbe WA. Leveraging Clinical Informatics Tools to Extract Cumulative Anthracycline Exposure, Measure Cardiovascular Outcomes, and Assess Guideline Adherence for Children With Cancer. JCO Clin Cancer Inform 2021;5:1062-1075. PM: 34714665.
Ohman EM. The Evolving Post-PCI Antithrombotic Therapies. N Engl J Med 2021;385(18):1712-1714. PM: 34449186.
Oyediran IO, Prattipati S, Sakita FM, Kweka GL, Tarimo TG, Peterson T, Loring Z, Limkakeng AT, Bloomfield GS, Hertz JT. The prevalence, management, and thirty-day outcomes of symptomatic atrial fibrillation in a Tanzanian emergency department. Afr J Emerg Med 2021;11(4):404-409. PM: 34703731.
Shenker RF, Hong JC, Eclov N, Fairchild A, Patel P, Niedzwiecki D, Palta M. Survey of Healthcare Providers Utilization and Perception of Telehealth On-Treatment Visits During COVID-19 Pandemic. Int J Radiat Oncol Biol Phys 2021;111(3S):S112. PM: 34700417.
Recent Comments