Chief’s message: American College of Cardiology Meeting 2021 and Spring Events:
This weekend highlighted the spring virtual American College of Cardiology Presentations. At the time of this email we have had several of our Faculty and fellows present. This year Duke Cardiology, DCRI, and Duke Heart with many of our collaborators will account for 87 presentations at the ACC 2021 meeting, with several late breaking clinical trials, young investigator awards, and overview of hot topics. We also have our heart center leadership council meeting coming up this week and will share updates from that next week. Finally, with some of the CDC and some of the School of Medicine policy changes, we are planning some outdoor graduation events for our wonderful fellows. I was fortunate enough to see some of the ACC and still make it to my daughter’s Indian Dance Performance in Midtown Raleigh and son’s track meet. One of few benefits of virtual conferences is that they have allowed us to balance clinical work, scientific meetings, and family life. Hopefully, you all got some time to enjoy the weekend and potentially catch up on some of the great science being presented.


Highlights of the week:
Duke Highlights, ACC 2021
We are pleased to share information on two late-breaking clinical trials presented this weekend at the American College of Cardiology’s Scientific Sessions. Congratulations to Schuyler Jones and the ADAPTABLE team and Rob Mentz and the REHAB-HF team! Renato Lopes is presenting the ACTION trial evaluating anticoagulation in SARS-COV2 today and we will have information on that in upcoming weeks. Further below, we highlight Marat Fudim and the Doug Zipes Distinguished Young Investigator award… although we have previously reported on this, now that the time has finally arrived, we’re celebrating once again! We will have more ACC.21 coverage next weekend.
ACC.21: Lower- and Higher-dose Aspirin Achieve Similar CVD Protection, Safety

People with cardiovascular disease (CVD) taking aspirin to lower their chances of suffering a heart attack or stroke experienced similar health benefits, including reduced death and hospitalization for heart attack and stroke, whether they took a high or low dose of aspirin, according to a study presented at ACC.21, the American College of Cardiology’s 70th Annual Scientific Session and published in the New England Journal of Medicine.
CVD—and atherosclerosis, in particular, which is a narrowing and hardening of the arteries—is a leading cause of death for men, women, and most racial and ethnic groups in the United States, with estimated direct costs of $214 billion, according to the American Heart Association. Millions of Americans with CVD take recommended aspirin therapy to help reduce their risk of heart attack and stroke, a decades-long practice that has, until now, lacked definitive research studying the doses that work best for patients and minimize potentially serious side effects, such as major bleeding.
“We found that both doses had similar effectiveness and safety, and while there were differences in dose switching between the groups, generally patients with heart disease should take low-dose aspirin given its tolerability and no clear benefit with higher doses of daily aspirin,” said Schuyler Jones, MD, associate professor of medicine in cardiology and the study’s principal investigator at the Duke Clinical Research Institute (DCRI).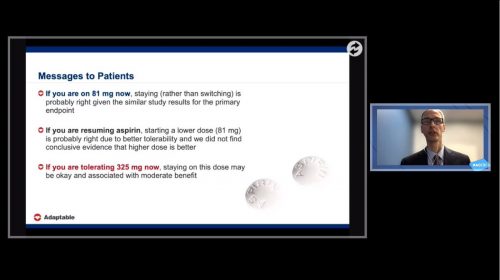
The study, called ADAPTABLE, is the first large-scale study of aspirin dosing to be embedded in real-world practice and the first randomized controlled trial to be conducted using PCORnet®, the National Patient-Centered Clinical Research Network. PCORnet is a national resource developed with funding support from the Patient-Centered Outcomes Research Institute (PCORI) to enable more efficient patient-centered clinical research by tapping into real-world health data collected during routine care. PCORI funded ADAPTABLE both to demonstrate the capacities of PCORnet and to fill an important evidence gap regarding cardiovascular care.
Researchers followed 15,076 people with CVD who were identified via electronic health records and randomized to self-administer either 81 mg or 325 mg of daily aspirin for a median of 26.2 months. Participants were engaged at 40 health centers across the nation and a health plan engaged in the PCORnet network. Most follow-up to obtain patient-reported information occurred via a patient portal, with the rest occurring via telephone calls.
While the researchers found no significant difference between the two doses in safety or effectiveness, they noted the higher dose group was much more likely to switch doses during the study. The patients in this group also were slightly more likely to discontinue the use of aspirin, for reasons including tolerability and participant and clinician preferences, among others.
“ADAPTABLE provides useful evidence to inform patients and clinicians who advise them on aspirin dosing decisions,” noted PCORI Executive Director Nakela L. Cook, MD, MPH. “Sometimes health care is based on years of routine practice and when rigorous studies are conducted, we can evolve that practice from common sense to evidence based. That is why PCORI funds studies like ADAPTABLE that aim to enhance decision making with useful evidence.”
Cook added, “ADAPTABLE demonstrated the capacities that PCORnet offers to conduct large-scale patient-centered research more efficiently utilizing a rich data infrastructure and provides valuable lessons learned as the first randomized controlled trial conducted via the network. The generation of real-world evidence to enhance and extend beyond the evidence generated through studies conducted in specialized research settings is so important to improving health outcomes for all populations in all settings around the nation.”
According to the researchers, ADAPTABLE provides a demonstration that randomized trials can leverage electronic health data, direct-to-participant methods and participant-reported outcomes to address important, patient-centered questions.
“ADAPTABLE provides a blueprint for how research can be improved in the future,” added Jones. “The pragmatic structure of the PCORnet network enabled remote follow-up and streamlined processes and made it easier for sites and participants to take part. We also benefited from continuous engagement with patient partners who raised questions at every touchpoint that made us all think how ADAPTABLE and future research could be done differently.”
More information on ADAPTABLE can be found at theaspirinstudy.org, which includes a plain-language summary of the results and a town hall discussion on lessons learned through the study. More information on PCORnet is available at pcornet.org.
ACC.21: Tailored Cardiac Rehab Program Improves Function and Quality of Life in Older Heart Failure Patients

Older patients hospitalized with acute heart failure who participated in a novel 12-week cardiac rehabilitation (rehab) program tailored to address their specific physical impairments had significant gains in physical functioning, quality of life and depression compared with those receiving usual care, regardless of their heart’s squeezing ability (ejection fraction), according to a new study presented at the American College of Cardiology’s 70th Annual Scientific Session. Participation in the program, however, did not significantly reduce rehospitalizations during the six-month follow up.
Heart failure, which happens when the heart can’t pump blood the way it should because it is too weak or stiff, is the leading cause of hospitalizations in people 65 and older. Many of these patients are never able to return to their previous level of functioning—resulting in reduced independence and increased risk of returning to the hospital or dying.
“These patients have persistently poor outcomes with frequent rehospitalizations, poor quality of life, high rates of dying and high health care costs,” said Dalane W. Kitzman, MD, professor of cardiovascular medicine and geriatrics/gerontology at Wake Forest School of Medicine and the study’s lead author. “Despite many efforts to improve outcomes in these patients, most studies testing a wide range of medications, devices and strategies have been negative. This suggested to us that we were overlooking an important factor contributing to these poor outcomes, and we suspected the missing factor might be severe physical dysfunction, which is generally not addressed in heart failure management.”
In an earlier pilot study, Kitzman and colleagues found that older patients admitted to the hospital with acute heart failure had profound deficits in all domains of physical function, including their balance, mobility and strength, not just in endurance, which would have been expected. Nearly all of these patients (97 percent) were considered frail or prefrail.
“Even before they are hospitalized, these patients already have lower physical functioning due to both aging and their chronic heart failure, and when their heart failure worsens, their physical function deteriorates further and this can then be exacerbated by the hospital experience and bed rest,” Kitzman said. “This sequence of events leading to marked impairments in all domains of physical function and its impact on patient outcomes has been largely overlooked.”
With these insights, the REHAB-HF rehabilitation intervention was developed and designed to correct deficits in balance, mobility and strength. REHAB-HF seeks to enhance effectiveness and avoid injuries that can occur when frail older persons undertake traditional cardiac rehab programs that are more focused on endurance. The program was tailored to each patient’s specific needs and adjusted to their ability level as they progressed. Unlike traditional cardiac rehab programs that typically start six weeks after a hospitalization, the REHAB-HF program started early—during the patient’s hospital stay if possible—and transitioned to three outpatient sessions per week for 12 weeks following hospital discharge. The aim of the current REHAB-HF trial was to evaluate whether this novel rehabilitation program could improve physical function (primary outcome) and rehospitalizations (secondary outcome) compared to usual care which could include physician-ordered physical therapy or traditional cardiac rehab.
A total of 349 patients across seven different hospitals, including four community hospitals, were enrolled in the study. Patients ranged in age from 60-99 years; over half were women and 49 percent were from underrepresented racial or ethnic minority groups. Notably, 53 percent had heart failure with preserved ejection fraction (HFpEF). Overall, they had an average of five comorbidities, most commonly high blood pressure, diabetes, obesity, lung disease and kidney disease, which may also contribute to declines in physical function.
At the three-month follow-up, compared with participants randomized to receive usual care, those in the intervention group had notable and significant improvements in physical functioning and quality of life across all the assessments used. For example, the Short Physical Performance Battery, a standard measure of physical function in older adults, improved by 1.6 units—more than twofold greater than the minimum amount that is meaningful to patients. On the six-minute walk test, they were able to walk 34 meters farther, a large improvement compared to very low function at baseline. Participant scores on the Kansas City Cardiomyopathy Questionnaire, which measures the patient’s perception of their health status, and a separate depression survey also showed large improvements. The improvements in physical function in the REHAB-HF intervention group were even greater when compared to the subset of usual care patients who had received traditional physical therapy and/or cardiac rehab as part of their physician’s orders, further supporting the effectiveness of the REHAB-HF intervention.
At six months, 83 percent of patients were still doing their exercises, which Kitzman said bodes well for long-term adherence. However, there were no statistically significant differences in clinical events, including rates of readmission for any reason, with 194 and 213 rehospitalizations occurring in the intervention group and usual care control group, respectively. Heart failure-related hospitalizations were also no different (94 vs. 110) at six months. There were numerically more deaths among people in the rehab group (21 vs. 16), but this was not statistically significant; researchers said this result may have been due to chance.
“The study was not large enough to really look at clinical events. But patient preference surveys show that older patients often value improved function and quality of life independently of rehospitalization and death,” Kitzman said. “By improving quality of life and physical functioning, the patient feels better, which is a positive outcome for patients.”
Kitzman and his collaborators, including David Whellan, Pamela Duncan, Amy Pastva, Robert Mentz, Gordon Reeves, M. Benjamin Nelson, Haiying Chen, Bharathi Upadhya, Shelby Reed, Mark Espeland, LeighAnn Hewston and Christopher O’Connor are now investigating whether certain subgroups of patients (for example, those with HFpEF) saw more benefits, which could inform a subsequent larger trial powered to definitively examine effects on clinical events.
This study was simultaneously published online in the New England Journal of Medicine at the time of presentation. It was funded by the National Institute on Aging.
ACC.21: Fudim Presented with Zipes Award
Marat Fudim received the 2021 Douglas P. Zipes Distinguished Young Scientist Award. He is the first Duke nominee to receive the honor. The Zipes award is presented annually at the ACC Scientific Sessions to recognize a young scientist who has made outstanding contributions to the field of cardiovascular medicine and who has amassed an impressive body of scientific research in either the clinical or basic domain. The pre-recorded award session featured Doug Zipes and JoAnn Lindenfeld; it ran this morning during the Sessions.
Congratulations, Marat!

Samsky CGR presentation
 Marc Samsky was our presenter for Cardiology Grand Rounds on Tuesday. Samsky discussed cardiogenic shock and the difficulties in conducting clinical trials for these patients. His research has focused on developing new ways to streamline research on patients with shock, leading to the design of two studies: an AHA Cardiogenic Shock Registry, and the BEST-SHOCK Trial. The trial, which has been submitted as a PCORI grant, would be an RCT to study Impella CP vs vasopressors/IABP. Marc also highlighted the fact that most of the work in cardiogenic shock has focus on patients with AMI and not those with acute on chronic heart failure, so it is difficult or impossible to apply the results from the AMI population to our HF pts.
Marc Samsky was our presenter for Cardiology Grand Rounds on Tuesday. Samsky discussed cardiogenic shock and the difficulties in conducting clinical trials for these patients. His research has focused on developing new ways to streamline research on patients with shock, leading to the design of two studies: an AHA Cardiogenic Shock Registry, and the BEST-SHOCK Trial. The trial, which has been submitted as a PCORI grant, would be an RCT to study Impella CP vs vasopressors/IABP. Marc also highlighted the fact that most of the work in cardiogenic shock has focus on patients with AMI and not those with acute on chronic heart failure, so it is difficult or impossible to apply the results from the AMI population to our HF pts.
You can find his recorded presentation here: https://bit.ly/3ybyuFd.
Heart Center Communications Updates
Since the start of COVID, the Heart Center Communications (HCC) volume of communications and the length of calls have increased while staffing has been down, at times, during staff transitions. Additionally, the majority of HCC staff have been working effectively from home in order to maintain social distancing requirements.
Over the last year, the HCC team has experienced employee turnover for a variety of reasons ranging from retirements to the passing of a beloved team member in September. For those familiar with the team, turnover is quite rare – this is a group that has forged close connections and operates more like a family in the way they care for one another.
The HCC now has four new nurses who are actively learning their roles: Kendell Hill, Carroll Enterkin, MJ Chapman and Alicia Snyder. We are very glad to have them on the team!
HCC has two talented financial analysts supporting charge capture processes for DUH cardiology invasive labs: Pat Clarke and Jon Boylan. They truly have a heart for service and continually look for ways to best support patient, provider and clinical staff needs. Heart Center Financial Administration (HCFA) supports DUH cardiac invasive labs by monitoring WQ’s, performing regular audits, reconciliations, financial reporting, charge corrections and communicating with clinical staff and medical providers as needed. By providing financial support, this allows the clinical team to focus more time on patients. The HCFA team has partnered with the cardiology invasive labs at DRH and DRAH, to provide them with this high level of support.
Finally, about a year ago, Duke Heart Center partnered with PRMO to add a dedicated Service Access Manager (SAM) to support Cath/EP, CDU and CMRI. The HCC was able to recruit the highly talented La Chandra Chavis, who role models our Duke Values and demonstrates great leadership. She has been a true asset to the team.
Great work, HCC! Hat tip to Greg Shelton for providing us with this update!
McKinney, NTI Poster Submission
 Congratulations to Heather McKinney, MSN, RN, NE-BC! Her poster entitled MenTIR: Mentoring to Improve Retention Study will be exhibited at the National Teaching Institute Conference sponsored by the American Association of Critical Care Nurses, May 24-27, 2021. The poster highlights the successful outcomes, including a reduction in nurse turnover, achieved by implementation of a mentorship program on Duke North Unit 3100.
Congratulations to Heather McKinney, MSN, RN, NE-BC! Her poster entitled MenTIR: Mentoring to Improve Retention Study will be exhibited at the National Teaching Institute Conference sponsored by the American Association of Critical Care Nurses, May 24-27, 2021. The poster highlights the successful outcomes, including a reduction in nurse turnover, achieved by implementation of a mentorship program on Duke North Unit 3100.
Way to go, Heather!
Celebrating Nurses!
 Congratulations to Missy Sturdevant, RN and Kamie Pedler, NCA of the Duke Heart 3100 Unit in Duke University Hospital who were both nominated during the Department of Medicine’s Celebrate Nursing Campaign! Their nominator(s) had this to say:
Congratulations to Missy Sturdevant, RN and Kamie Pedler, NCA of the Duke Heart 3100 Unit in Duke University Hospital who were both nominated during the Department of Medicine’s Celebrate Nursing Campaign! Their nominator(s) had this to say:
“Kamie is one of the hardest working, most compassionate coworkers I have had the honor of working with. She cares deeply about working with patients and exemplifies all of the Duke Values. She deserves all the praise in the world!” – Name withheld
“Missy has been such a dependable, integral and inspiration of a nurse on 3100. She goes above and beyond to share her knowledge and provide the best possible care for her patients. I learned so much from her and hope that Duke realizes how lucky it is to have her caring for our patients.” – Name withheld
Congrats, Missy & Kamie!
Shout-out to Yankey, Loriaux & Flores Rosario!
More great feedback on members of our fellowship program was received this week – in a note to Anna Lisa Crowley, we learned:
“I am writing to recognize three of your outstanding fellows: Dr. George Sipa Yankey, Dr. Daniel Loriaux, and Dr. Karen Flores Rosario. These three fellows volunteered several hours of their time to teach first-year Duke medical students basic cardiac ultrasound. I had the privilege of teaching alongside them, and I was so impressed with their educational skills. The students LOVED learning from them and are still raving about the experience.
We are so lucky to have such gifted educators willing to volunteer their time for our students.” — Julian Hertz, Assistant Professor of Surgery & Global Health, Course Director, Longitudinal Point-of-care Ultrasound Curriculum
Great job, Sipa, Daniel and Karen!



Nursing Gala Held; Celebration of FON Awards
The 32nd Gala Celebration of Excellence, hosted by the Duke Friends of Nursing Board of Advisors was held last night, May 15. The online event honored all Duke nurses and celebrated the nominees and winners of the FON Excellence Awards. A very special congratulations to the following Duke Heart nurses who were recognized: Stephanie Barnes, Allison Dimsdale, Mollie Kettle, Elaine Milton, Brenda Smith, Courtney Stierwalt and Katie Toy. We are so happy for each of you!

Duke Box Update
Good news for those of us who use Box, Duke’s cloud-based storage and collaboration service. Starting Monday, May 17, Box will have new and improved features. The new features include:
- Infinite scroll – Scroll down to view files and folders rather than clicking through pages of content
- Collections – Organize files and folders in ways that make sense to you
You may also notice a slight branding change on the Box interface. This short video provides an overview of the changes: https://warpwire.duke.edu/w/taIFAA/
If you would like to learn more about Box, please visit box.duke.edu.
COVID-19 Updates:
All the latest official DUHS information regarding coronavirus/COVID-19 response at the following locations:
Upcoming Opportunities/Save the Date:
Proctors Needed: MaryAnn Black Virtual Summer Internship Program
The MaryAnn Black Virtual Summer Internship Program is in need of volunteer proctors to cover about 12 hours during the virtual program. Coverage times are as small as one hour between June 15 and June 30. Proctors will provide active supervision, listen during sessions, and observe to ensure minor participants (ages 15-18) are behaving appropriately. If you’re interested and willing to help out, please contact Darla Wohlfarth.
To learn about the program, please visit: https://community.duke.edu/program/duke-internships/
This year’s program will be completely virtual and will highlight dozens of healthcare careers and healthcare supportive careers. The internship will begin June 7 and end June 30, 2021. The first week will be devoted to structured training and orientation. The remaining weeks will give the student an overview of the many career opportunities that make up the fabric of Duke Health.
Thank you for considering!
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged.
Duke Heart in the News:
May 6 — Cameron Prigge (neurobiology)
AAMC.org
Basic medical research took a hit during the pandemic. It might take years to recover
https://bit.ly/3o9y11F
May 6 — Brigit Carter (Duke SON)
health.usnews.com
Why Representation in Nursing Matters
https://bit.ly/3eFdz5u
May 9 — general interest
The Washington Post
https://wapo.st/3w8QlL7
May 10 — Adrian Hernandez
WRAZ/Fox 50
There’s one side-effect to watch for when children receive the COVID-19 vaccine
https://bit.ly/3y0Pxtv
Note: clip begins at 10:04:10
May 10 — E. Magnus Ohman
Medscape
Patient-Focused Revisit of ISCHEMIA Bolsters Conservative Message in Stable CAD
https://www.medscape.com/viewarticle/950875https://bit.ly/3es0tZr
Recent Comments