Duke Heart week ending October 25th 2020
Chief’s message: The Greater Good
Hubert Humphrey once said that “the moral test of government is how that government treats those who are in the dawn of life, the children; those who are in the twilight of life, the elderly; and those who are in the shadows of life, the sick, the needy and the handicapped.” This statement has been uttered and is quoted in meetings and actions of Health and Human Services (CMS) in Washington DC. Both Hubert Humphrey, and the greater part of America would have to wait until the promise and potential of President Lyndon Johnson’s “Great Society”. Healthcare progress has always been a slow, and often difficult, and unfortunately political battle, when in many regards it is much more of an economic battle rather than a moral battle. On July 30, 1965, President Johnson traveled to the Truman Library in Independence, Missouri to sign the Medicare Bill into law…which would forever change what it means to be elderly and disabled in America. Something that we all now know moved our nation closer to good. Unfortunately, over the last few weeks we have had more and more members of our community lose their jobs, insurance and access to health care, and even more tragically their lives. This week the cardiology group started to brainstorm ways in which we can grow services including telehealth for minimal or no cost care to ensure medication refills, urgent care identification, and ways to integrate in the growing safety nets programs in our area. This is a small part of what Duke Heart can do and hopefully add to the large local and regional care provided by organizations such as federally accredited community health centers like Lincoln in Durham and others in the area. Regardless of political beliefs or outcomes of elections, we will continue to work in our community to be part of the greater good – the organized efforts to help our community. As the upcoming weeks and months stress our resources, resolve, and community, I am optimistic based on the people at Duke Health that I see every day.
Highlights of the week:
 1500th Heart Transplant Performed at Duke University Hospital
1500th Heart Transplant Performed at Duke University Hospital
Congratulations to the Duke Heart Transplant Program!! The team reached a major milestone recently when they performed the program’s 1,500th heart transplant. Only five other centers in the U.S. have achieved this distinction. We are proud of you and your dedication to excellence!
Taking a look back with Dr. Andrew S. Wechsler, emeritus professor of Cardiothoracic Surgery at Drexel University, who performed Duke’s first heart transplant and who shared part of that story with us this week:
 “The first heart transplant at Duke was performed 1985 on a 55-year-old plumber who was totally disabled by his heart failure. It was the first heart transplant to be performed in North Carolina. The only other nearby centers performing heart transplants were the Medical College of Virginia and the University of Alabama in Birmingham. I had flown to Richmond the week before to observe the procedure.”
“The first heart transplant at Duke was performed 1985 on a 55-year-old plumber who was totally disabled by his heart failure. It was the first heart transplant to be performed in North Carolina. The only other nearby centers performing heart transplants were the Medical College of Virginia and the University of Alabama in Birmingham. I had flown to Richmond the week before to observe the procedure.”
Heart transplants were controversial at that time, according to Wechsler.
“Initially, many transplants performed had problems associated with immune rejection which resulted in most programs ceasing the activity with the exception of MCV and Stanford University. David C. Sabiston, Jr., MD, who was the chairman of the Duke Surgical Department at the time, was initially quite reluctant to allow the procedure and after extensive discussions with me finally agreed to allow the operation if I could obtain permission from the hospital CEO, Dr. Andrew Wallace, a highly respected cardiologist.
“There were concerns about the financial implications of the procedure. Blue Cross finally indicated that they would make payment decisions on a “case by case” basis. Dr. Wallace approved the procedure and the heart team was assembled. It included myself as lead surgeon and Drs. Robert Jones and James Lowe.
The operation was performed on a hot summer day and the helicopter struggled a bit during takeoff, as it was quite full. The donor heart was retrieved from the Eastern part of the state by the operating team. The patient’s recovery was rapid and he was discharged from the hospital in good spirits.”
(See photo, courtesy of Dr. Andrew Wechsler. Shown are Dr. Wechsler, the patient and his wife, as well as various hospital staff members.)
Thirty-five years later, Duke boasts one of the top five centers for heart transplant by volume in the country and offers some of the shortest wait times in the region, according to the Organ Procurement and Transplantation Network.
Incredible work on the part of so many people over the years in order to transform lives. We are especially grateful to the donors and their families for making the decision to donate life.
Passings: Eric S. Williams, MD, Electrophysiologist; Former Duke Fellow
 Eric Sean Williams, MD, a cardiac electrophysiologist at Mercy Clinic Heart and Vascular Hospital (St. Louis, MO) passed away on October 15, 2020. He was 44.
Eric Sean Williams, MD, a cardiac electrophysiologist at Mercy Clinic Heart and Vascular Hospital (St. Louis, MO) passed away on October 15, 2020. He was 44.
Eric was born and raised in Brooklyn, New York. He attended the prestigious Stuyvesant High School and then matriculated at Cornell University, where he earned his Bachelor’s degree in Applied and Engineering Physics. He graduated with honors from Harvard Medical School in 2004. An avid traveler, he spent two years conducting medical research and learning Spanish in Costa Rica during his time in medical school. He then trained at the University of California, San Francisco (UCSF) for his residency in internal medicine, serving an additional year as chief resident before moving to Duke University for his Cardiology fellowship and then University of Washington, Seattle, for his electrophysiology fellowship.
His full obituary can be found here: https://www.luptonchapel.com/obituary/eric-williams-md-facc-fhrs?fh_id=15972.
He is remembered at Duke as a kind and great clinician and friend.We extend our condolences to the Williams family and to his friends and colleagues.
DMP 7 East Moved To 6 East October 24
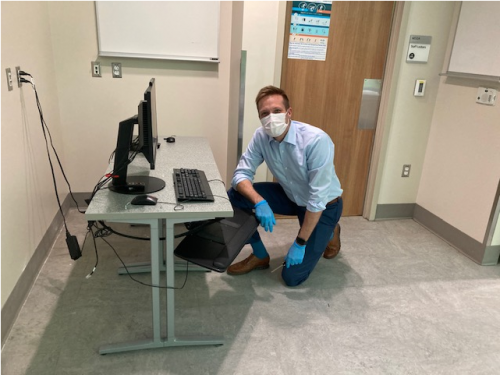
The cardiothoracic stepdown unit on DMP 7 East moved to DMP 6 East on Saturday, October 24. This was the first move as part of the planned move sequence for Heart Services. Special thanks to 6 East Nurse Manager, Eric McClenny and 6 East Clinical Leads, Ciarra Ashley and Amanda Rooney for the significant role they played in making this a successful move! We are also grateful for additional leadership team members, staff, and support services who also contributed to the move. Some of our team members are pictured during preparation and move-day action.
Great work, everyone! Your teamwork helped the day go as smoothly as possible!


Fellowship Recruitment Wraps Up
The Duke Cardiology fellowship program completed their 7th and final day of virtual CV fellowship interviews. The team interviewed 64 incredibly talented fellowship applicants with diverse backgrounds and interests (~8.5% of the total applications we received). Anna Lisa Crowley, MD, fellowship program director, in a note to faculty, fellows and several staff members, wrote: “I personally want to thank each of you for rising to the challenge this new recruitment process presented by participating in virtual interviews, breakout groups, big sib-little sib conversations, virtual happy hours, and informal conversations. In addition, I want to recognize the extra efforts of Arlene Martin & Christina Ryerson this year who became Zoom experts and helped us all navigate the virtual interview days. In fact, many applicants shared that our interview day was the best organized and executed one they had. It is a tribute to all of your efforts so THANK YOU again! I feel privileged to work with such an AMAZING and inspiring team!”
Well done, everyone!!
Shout-out to Carlisle, Narcisse, Flores Rosario & Spates
We received a very special shout-out this week to the fellows team. In a note to Anna Lisa Crowley:
“I just wanted to send a very personal thank you and kudos to your fellows. Specifically this group: Matthew Carlisle, Dennis Narcisse, Karen Flores Rosario and Toi Spates.
My [family member] came to the hospital yesterday with 3rd degree heart block and was pretty close to death. Your fellows provided rapid triage in the ER, mobilized a bed in the CCU, and then placed a temp wire under significant duress (dopamine @ 20, transcutaneous pacing going, and my family member actively vomiting).
Basically, your fellows saved my family member’s life yesterday and for that I am deeply grateful!”
-Yuriy Bronshteyn, MD
Way to go, Duke Heart fellows!!!
Poster Earns Top 10 Score at Duke’s Annual Quality and Safety Conference
Congratulations to Myra Ellis, Bradi Granger, Debra Farrell, Heather Pena, Allen Cadavero, Mollie Kettle, Tonda Thomas and Kamrouz Ghadimi — their poster presentation, Race to the Finish: Engaging the Team in an Early Extubation Quality Improvement Project was one of the top ten scoring posters for the 2020 Duke Health Annual Quality and Safety Conference, originally scheduled for March 26, but cancelled due to COVID-19.
According to Myra Ellis, “the 7West Nursing Research committee collaborated with a CT Surgery multidisciplinary team to conduct a quality improvement initiative to increase the number of cardiac surgery patients that achieved early extubation cardiac surgery. The Society of Thoracic Surgeons defines early extubation as occurring within 6 hours after admission to the ICU. Early liberation from the mechanical ventilator important because it increases patient comfort and is associated with improved outcomes and lower costs. Our collaborative team worked to reduce barriers to extubation and promote early extubation by the use of a standardized Fast-track Extubation (FTE) Protocol and staff education. In data collected prior to implementation of the project, 49 percent (49/101) of patients were extubated in under six hours. In the first month after protocol implementation, this improved to 72 percent (60/83) and even included patients with high-disease severity that had undergone complex operations. One year after FTE protocol initiation, 75 percent (582/779) of FTE eligible patients were extubated within the six-hour window.
“Part of the success of the project was the use of the Influencer Change Model (K Patterson, et al) that posits that results are achieved by changing personal and group aspects of behavior through 6 sources of influence. Team performance was reported with the percentage of eligible patients achieving early extubation each week. We used a racetrack that was updated weekly to include the names of the “pit crew” (nurse, respiratory therapist and advanced practice provider) who successfully extubated patients within the recommended time period. Social influence can be a key factor in the individuals’ adoption of new innovations. The racetrack generated enthusiasm and captured the power of peer influence. Having your name on the racetrack created healthy competition between peers, making best practice socially desirable.”
The conference received more than 100 abstracts. The posters were scored by a blinded, multidisciplinary team based on these criteria: practical to implement, effective use of patient safety/ performance improvement tools and methods, improvement documented with pre/post analysis, and includes strategies to sustain outcomes.
Great work, everyone! Thank you for all that you do to provide the best care possible while keeping patients safe.
Important Reminders
- Open Enrollment ends this week!!!!
- Please get your Flu Vaccination: All team members must get their vaccination or otherwise demonstrate policy compliance by Tuesday, Nov. 10. Details and resources all available on the Duke Health Influenza Resources site (NET ID required): https://influenza.dh.dukehealth.org.
- DON’T FORGET TO VOTE!
COVID-19 Updates:
All the latest official DUHS information regarding coronavirus/COVID-19 response at the following locations:
Upcoming Opportunities/Save the Date:
Cardiology Grand Rounds
Oct. 27: Cardiology Faculty meeting
Nov. 10: TBA
Nov. 17: No CGR. AHA Scientific Sessions
Conferences, Symposia & Webinars
Nov. 13: 12th Annual NC Research Triangle Pulmonary Hypertension Symposium. Noon – 4:30 p.m. For more information, please visit this page. This event will be held virtually and is co-sponsored by Duke and the University of North Carolina in partnership with the Pulmonary Hypertension Association through the Building Medical Education in PH program. Please join us!
Nov. 13–17: AHA Scientific Sessions 2020, a virtual experience. Registration is now open. See the website for details.
Conversations with Colleagues: A Deeper Dive on Racial Justice
During the initial Conversations with Colleagues (CwC): Racial Justice sessions attendees shared that they wanted a deeper dive and more action steps related to racial justice. During this next edition of CwC attendees will sign up for 6 weeks of conversations. Participants will be placed into small cohorts and will walk with this same group of colleagues throughout the entire 6 weeks. These cohorts will allow staff to build relationships, have colleagues to bounce ideas off of and have accountability partners to help them stay true to the mission of the deeper dive. You will read articles, watch videos and engage in other activities that will deepen your knowledge about racial justice. Attendees will also learn action steps that they can take to make a difference.
Dates/Links for CwC
The conversations will take place weekly, starting this week and running through 12/7 (with a break Thanksgiving Week). Conversations will be 1 hour long.
Mondays 2-3pm (10/16 – 12/7)
https://duke.zoom.us/meeting/register/tJUvdOCqrDgsEtQYipTJ7F4eZnPQZFTIx2ZD
Tuesdays 8-9am (10/27 – 12/8)
https://duke.zoom.us/meeting/register/tJAtde-grTsqGtxJl7M6huHcgA3yFQ18pO6P
Wednesdays 12noon-1pm (10/28 – 12/9)
https://duke.zoom.us/meeting/register/tJUkce-rqjIrHdPmAvmnM_L0GEaFrkeFZq5L
Thursdays 5-6pm (10/29 – 12/10)
https://duke.zoom.us/meeting/register/tJ0lcu6rqTMiEtOIeRMiWtRQcInZLR6LnmPB
Fridays 12 noon-1pm (10/30 – 12/11)
https://duke.zoom.us/meeting/register/tJMrf–trTwrHtB3TEX5B-7UUXW2RgDJWGko
Sundays 4-5pm (11/1 – 12/13)
https://duke.zoom.us/meeting/register/tJEucuqtrjIpGdx8gdnQst1yAS-5NDrgzrD2
Matters of Grief: The Duke Response
On Thursday, November 19th, join us for a free half-day symposium where we will learn about ways that we can support each other through both personal and professional grief, share stories of support, and identify resources available at Duke.

Matters of Grief: The Duke Response will feature diverse and multidisciplinary panels, engaging didactic sessions, and surprise guests from across the university. Just some of the highlights include:
- Coach K delivers a special message
- Duke medical students will discuss the research behind grief and finding support through peers
- Well-Being experts and Duke Health leadership discuss normalizing discussions about grief
The virtual event runs from 1-5PM on November 19th, 2020. Sessions will be recorded for those who cannot attend the live event. Reserve your space today at bit.ly/mattersofgrief
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged.
Have a good week, everyone!
Duke Heart Week Ending October 18th 2020
Chief’s message:
 Although this year, more than any others, we have become aware of the limitations and sanctity of life, we were still deeply saddened this week to learn of the passing of Joseph Greenfield, MD, Professor and Chair Emeritus, Dept. of Medicine. He passed away on his farm in the Duke Forest. He lived a remarkable life, notable for an amazing academic career, mentorship, and a love of nature evidenced through collecting butterflies, raising hunting dogs, and many trips.
Although this year, more than any others, we have become aware of the limitations and sanctity of life, we were still deeply saddened this week to learn of the passing of Joseph Greenfield, MD, Professor and Chair Emeritus, Dept. of Medicine. He passed away on his farm in the Duke Forest. He lived a remarkable life, notable for an amazing academic career, mentorship, and a love of nature evidenced through collecting butterflies, raising hunting dogs, and many trips.
With his passing, the Division of Cardiology and the Department of Medicine suffered not only the loss of a visionary leader, but of someone who helped set the division and department on a course of research and clinical excellence. Among his many accomplishments, he will be remembered for his impact on the lives of many residents, fellows and faculty, including mine.
What I remember most over the 23 years that I had the honor of knowing him, was his overall humility, honesty, and how much he cared about your well-being. As I described in the note to our Division, he was fiercely honest with a drive for excellence in care and discovery. We all have many stories with Dr. Greenfield. My favorite revolve around both his honesty and this drive to get the clinical answer; always seeking excellence in both care and research.
In 2001, when he retired to the VA, I was the Chief Resident in Medicine and had the privilege of asking him to do morning report with the residents every week. He committed to one day a week, and would always show up 5-10 minutes early and sit in the Chief Residents office with me at the VA and ask about how things were going, how the residents were doing, and “if I was making anything of my time with research.” During the morning reports, he would quickly get to the key clinical issues and push the residents to look at the primary data, and then ensure they were sufficiently supported for the day. He would also pop in and join interns and residents for midnight pizza rounds on many of the Fridays, even back then. He would often say the key to most things was to “get the best people and get out of their way.”
Once when I gave a cardiology grand rounds as a junior faculty member, he sat in the front row and looked as if  he was asleep or bored during the majority of the talk. At the end, as was routine, he asked a question that I could not answer. He then approached me afterwards when people were congratulating me on the talk and asked me to let him know if I was going to give a talk like that again, because as he put it…. “Although small, there was a risk he could get hit by a car crossing the street from the VA and he didn’t want to risk it if I was giving another talk of that quality.”
he was asleep or bored during the majority of the talk. At the end, as was routine, he asked a question that I could not answer. He then approached me afterwards when people were congratulating me on the talk and asked me to let him know if I was going to give a talk like that again, because as he put it…. “Although small, there was a risk he could get hit by a car crossing the street from the VA and he didn’t want to risk it if I was giving another talk of that quality.”
I was honored to be named a Greenfield Scholar in 2006, and when I provided him with the manuscript we had worked on for 5 years to determine the myocardial involvement with cardiac sarcoid on cardiac MRI, which was published in Circulation with acknowledgment of the supporting funds, he simply stated he was proud of us. He went on to ask a few more important questions around the arrhythmogenic potential based on imaging findings, work that the group today is still working on.
Dr. Joseph Greenfield was and will remain the beacon for how we care for our patients and study medicine.
He leaves behind his beloved family of three daughters Mary Agnes, Ruth Ann, and Susan Lee, all of Durham. Ruth Ann, who described him as her best friend, will be helping us determine a way to celebrate his memory in the future.

Below are some thoughts and notes from others
From Chris O’Connor, MD, President, Inova Heart and Vascular Institute and former division chief, Duke Cardiology:
“What I respect the most about Dr. Greenfield was his deep commitment to people: their well-being, their families, and their professional careers as leaders. Two examples come to mind: as a first year cardiovascular fellow, my father passed at the age of 56; the first person to call was Dr. Greenfield to let me know that he was there for me if I needed anything. A second example was during every other night intern call, I was running late for a.m. rounds and got on the elevator at Duke North the same time Dr. Greenfield did. He looked at me and said, “Son, where is your tie?” (In my haste I forgot to put one on) He stopped the elevator, handed me a five-dollar bill and told me to go to the VA hospital gift shop and purchase a tie so that I could look respectable to the patients and the staff. (I never forgot to wear a tie again nor did I get on another elevator with Dr. Greenfield.)”
From Richard Stack, MD, Professor Emeritus of Medicine in Cardiology at Duke University; President and Managing Partner of Synecor, LLC:
A sad end to a great era in Academic Medicine. My thoughts are simple: “I owe my entire career to Joe Greenfield.”
Updates from the week:
Passing of Joseph Greenfield, MD, Professor and Chair Emeritus, Dept. of Medicine
In an announcement to all faculty members within the Department of Medicine this week, Mary E. Klotman, MD, Dean of the School of Medicine, and Kathleen A. Cooney, MD, Chair, Department of Medicine wrote:
It is with great sadness that we write to inform you that Joseph Greenfield, MD, died on Wed., Oct. 14.
Dr. Greenfield was the James B. Duke Distinguished Professor of Medicine and chair of the Department of Medicine from 1983 to 1995. He received his medical degree from Emory University in 1956 and completed his internal medicine residency at Duke University in 1959. He joined the National Institutes of Health (NIH) before returning to Duke as assistant professor in 1962.
In addition to his role as chair, Dr. Greenfield served in numerous other leadership positions including chief of Cardiology at the Durham Veteran’s Administration Hospital from 1963 to 1983, chief of the Division of Cardiology at Duke University Medical Center from 1981 to 1989, and director of the ECG service at Duke from 1971 to 2001, and at the Veteran’s Administration Hospital from 1996 until he retired in 2017.
Dr. Greenfield was a pioneer in cardiovascular medicine, promoting innovative care models and studying reperfusion therapies in acute coronary syndromes. He created new, forward-thinking care paradigms to ensure that rural areas had access to emergent cardiovascular care by sending cardiologists on helicopters to outlying hospitals to administer thrombolytic therapy.
With the goal of delivering more efficient acute myocardial infarction care, Greenfield reorganized the cardiac catheterization lab to be adjacent to Duke University Hospital’s emergency room. He advocated for greater use of randomized clinical trials and patient data registries to advance knowledge and improve patient care. Over his career, Greenfield authored more than 150 research articles.
Dr. Greenfield was passionately committed to the professional development of faculty and trainees and will be remembered as great mentor. He started the Greenfield Scholars Program that continues to support many resident and junior faculty research careers. In his honor, the Department of Medicine established the Joseph Greenfield Research Mentorship Award to recognize faculty members who excel in research mentorship.
In 1984, Greenfield was awarded the Distinguished Science Award from the American College of Cardiology and Duke’s Eugene A. Stead Award for excellence in teaching (and again in 1995). He received the MERIT Award from the National Heart, Lung and Blood Institute in 1986. In 1990, he became a member of the National Academy of Medicine.
Please join us in extending our deepest condolences to Dr. Greenfield’s family and friends. The Duke flag was lowered on Thursday in his memory.
Memorial service information will be provided when it becomes available. In lieu of flowers donations can be made to The Greenfield Scholars Program at Duke University.
Duke Regional Earns Top Rating for Adult Cardiac Surgery Procedure
For the second year in a row, Duke Regional Hospital’s coronary artery bypass grafting (CABG) procedure in adult cardiac surgery has earned a top rating – three stars – from The Society of Thoracic Surgeons (STS).
This annual rating is calculated by examining quality measures of Duke Regional’s CABG procedures during calendar year 2019, to include absence of mortality, absence of morbidity, use of internal mammary artery (IMA) grafting, and how medications were prescribed.
“This recognition shows that Duke Regional Hospital team members take exceptional care of our CABG patients, by not only ensuring a safe and successful surgery but also by helping the patient swiftly recover,” said Shu Lin, MD, Ph.D., Duke Regional division chief for Cardiothoracic Surgery and Duke associate professor of Surgery. Lin shared the news with the team at Duke Regional earlier this week.
More than 75 percent of Duke Regional’s CABG patients are discharged within five days after surgery, compared to only 42 percent of CABG patients from comparable hospitals, Lin added. On average, CABG patients are extubated five hours after surgery, and none of Duke Regional’s CABG patients had spent prolonged time on a ventilator in the past two years.
STS’ star rating system is one of the most sophisticated and highly regarded overall measures of quality in health care, rating the benchmarked outcomes of cardiothoracic surgery programs in the U.S.
Lin said this top rating was achieved by the highest-quality, compassionate care that team members provided across Duke Regional Hospital, to include clinical staff and support staff.
“The achievement of this STS three-star recognition exemplifies what a teamwork can do, especially when fundamentals of patient care are meticulously followed and when each member of the team takes pride in his or her role in the process,” he said. “Congratulations to everyone involved.”
Gutierrez Receives CDA Funding

Duke Heart
Congratulations to Tony Gutierrez, MD, MHS, who received word that his VA Career Development Award (CDA) has been funded! This competitive award provides five years of support for early career investigators. Tony is the first person in the Cardiology Division to successfully receive a CDA, according to Sunil Rao, MD, Section Chief, Cardiology at Durham VA Medical Center.
Gutierrez’s project, titled “Telehealth to improve functional status and quality of life in veterans with PAD,” will establish a veteran-centric program of telehealth-facilitated exercise using the Durham VA’s robust home-based cardiac rehabilitation program and will assess long-term outcomes in patients with peripheral artery disease.
Tony’s mentors on the CDA include Rao, Miriam Morey, PhD, Kelli Allen, PhD, Katherine Hall, PhD, Matthew Maciejewski, PhD, Shirling Tsai, MD, and David Edelman, MD, MHS.
Congrats, Tony!! Well deserved!
Shout-Out to Rio Landa, APP!
“I think Rio Landa deserves special commendation for picking up an abnormality totally unrelated to cardiology,” wrote Neil Freedman, MD, in a message this week to Stephanie Barnes, NP. His note goes on to describe the event:
“Rio was meeting a patient for the first time on Monday, Oct. 12. We were trying to push to discharge the patient (because symptoms were from GERD, and patient had been cath’d the previous week). Rio noticed that nothing had been noted or done about a new finding of probable R renal cell CA discovered [days earlier] by abdominal CT—so, after seeing this abnormality, Rio herself coordinated oncology and IR to get the issue taken care of as an outpatient. [Patient has history of cancer.]
Rio is not unique in her terrific efforts, of course, but this episode illustrates highly commendable conscientiousness and initiative. Brava!”
Barnes added, in a message this week to Pulse, “This highlights Rio’s true attention to detail, even on a busy day! She leads by example and we thank Dr. Freedman for taking the time to recognize her great catch.”
Freedman signed off his letter with the statement, “It is a real privilege to work with the APPs.”
We could not agree more! Well done, Rio – and many thanks to our terrific APP team!
Three CVIS Clinical Ladder Promotions in Interventional Lab
We are excited to share with you that the following clinical team members are the first three to be promoted within the interventional lab space under the recently revised Clinical Ladder Program for CVIS.
Meek Myoung: CVIS I to CVIS II – Adult Cardiac Cath Lab, DUH. Meek holds a BS in Radiologic Science and has been a CVIS in the Adult Cath lab since 2018. She maintains her RT(R) as well as the RCIS certification.
Cassidy Johnson: CVIS I to CVIS II – Adult Cardiac Cath Lab, DUH. Cassidy holds a BS in Radiologic Science and has been a CVIS in the Adult Cath Lab since 2018. She maintains her RT(R) as well as the RCIS certification.
Catherine Bennett: CVIS II to CVIS III – Adult EP Lab, DUH. Catherine holds an Associates of Science in Cardiovascular Technology and has been an employee at DUH since 1998. She started her career in the Adult Cath Lab and transferred to the Adult EP Lab in 2016. She maintains the RCIS certification.
“We are very proud of all of their hard work and dedication to their patients as well as their team here at Duke University Hospital,” said Elizabeth Watts, Duke Heart Nurse Manager, Operations for the Adult Cardiac Cath Lab, Cardiovascular Short Stay Unit, and the Adult Electrophysiology Lab.
Congratulations, Meek, Cassidy and Catherine!
Planning for Move to 7 East
 The Cardiac ICU Charge Nurse group held a meeting on Oct. 14 to discuss workflows and practices related to the upcoming move to 7 East. Manesh Patel and Jill Engel stopped by to express their gratitude for the team’s leadership and talked about the great opportunities coming along with the move, which is currently scheduled for November 21.
The Cardiac ICU Charge Nurse group held a meeting on Oct. 14 to discuss workflows and practices related to the upcoming move to 7 East. Manesh Patel and Jill Engel stopped by to express their gratitude for the team’s leadership and talked about the great opportunities coming along with the move, which is currently scheduled for November 21.
Special thanks to Kirsten Butler for coordinating the meeting and to the charge nurses who participated.
CT SDU Moving to DMP 6 East, Oct. 24
One of the Cardiothoracic Stepdown Units will be moving from Duke Medical Pavilion (DMP) 7 East to DMP 6 East on Saturday, Oct. 24. This is the first move to occur as part of the planned move sequence for Heart Services. Thank you to the staff, providers, and team members who are working hard to make this a successful move!
Additional communications regarding “move day” will be forthcoming.
Duke Solid Organ Transplant Summit Held Oct. 10
 The 2020 Duke Solid Organ Transplant Summit was held as a virtual event on Saturday Oct. 10. A pre-summit Duke Transplant APP Bootcamp was held on Friday, Oct. 9. Duke Heart was well represented for both portions of last weekend’s events. Presenters included:
The 2020 Duke Solid Organ Transplant Summit was held as a virtual event on Saturday Oct. 10. A pre-summit Duke Transplant APP Bootcamp was held on Friday, Oct. 9. Duke Heart was well represented for both portions of last weekend’s events. Presenters included:
- Stephanie Barnes, NP- “DCD in Cardiac Transplantation”
- Callie Tennyson, NP- “Identifying and Managing Complications of Cardiac Transplantation”
- Benjamin Bryner, MD- “Lessons Learned in DCD Heart Transplant”
- Richa Agarwal, MD- “Emerging Mechanical Circulatory Support Devices”
- Kam Ghadimi, MD- “Inhaled Pulmonary vasodilators in the perioperative setting-iNO vs. EPO”
“Everybody delivered beautifully, it was a really well run weekend by Duke Surgery,” said Callie Tennyson.
Course directors were Deb Sudan, MD and Carl Berg, MD. Great work, everyone!
We’ve Grown Again!
We are very pleased to welcome Natalie Claire Lerman, born October 7, to our Duke Heart family! “Baby and Mom are doing great!” says dad, Joe Lerman, one of our cardiology fellows.
Congrats, Lerman family!! We look forward to meeting her!

Important Reminders
- Open Enrollment for Duke Benefits is October 19-30.
- Please get your Flu Vaccination: All team members must get their vaccination or otherwise demonstrate policy compliance by Tuesday, Nov. 10. Details and resources all available on the Duke Health Influenza Resources site (NET ID required): https://influenza.dh.dukehealth.org.
Upcoming Opportunities/Save the Date:
Cardiology Grand Rounds
Oct. 20: The Albert L. Williams Cardiovascular Genetics Lecture Series. Presenter: Wendy Chung, MD, PhD, of Columbia. 5 p.m., Webex. Details in email invitation.
Oct. 27: Cardiology Faculty meeting
Nov. 10: TBA
Nov. 17: No CGR. AHA Scientific Sessions
Conferences, Symposia & Webinars
Nov. 13: 12th Annual NC Research Triangle Pulmonary Hypertension Symposium. Noon – 4:30 p.m. For more information, please visit this page. This event will be held virtually and is co-sponsored by Duke and the University of North Carolina in partnership with the Pulmonary Hypertension Association through the Building Medical Education in PH program. Please join us!
Nov. 13–17: AHA Scientific Sessions 2020, a virtual experience. Registration is now open. See the website for details.
COVID-19 Updates:
All the latest official DUHS information regarding coronavirus/COVID-19 response at the following locations:
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged.
Duke Heart in the News:
October 14 — Adrian Hernandez
STAT
Covid-19 clinical trial pauses ‘show the system is working’
https://bit.ly/3m51lUR
Duke Heart Week ending October 11th 2020
Chief’s message: The “Gut” Feeling
Running into my office after getting through some of the patients I was rounding on this Saturday, I logged onto the Fellows Zoom interview welcome session. There was a brief moment and then the screen clicked into the “Hollywood Stars” gallery view of zoom so I could see all the welcoming faces of potential cardiology fellow applicants.
This week we held our third zoom interview/ recruitment session for our cardiology fellows next year. In this year with all the changes, the recruitment season has also become another challenge and possible opportunity. We have had over 750 applicants for the 60-70 interviews that we conduct to get to our final matched 8-10 cardiology fellows. Each year we are reminded about the immense talent and dedication we have the honor of attracting as possible cardiology fellows. We have seen a rise in both the number applicants, the diversity, and the locations of training for the applicants to our fellowship.
Our fellowship lead by Anna Lisa Crowley with our associate program directors, Neha Pagidipatti, Rob Mentz, Chris Holley, and Camille Frazier-Mills along with numerous faculty and fellows have done an amazing in tailoring the experience for the perspective fellows. We have assigned “Big Sibs” to answer questions prior to the interview day, we have breakout zoom rooms, options for one on one, and group discussions, and most notably – we take the opportunity to introduce the applicants to each other. They are certainly the next generation of cardiovascular leaders that will shape the way we teach, discover, and deliver cardiovascular care. We have done videos of our fellowship and Duke/Durham – in an effort to flip the classroom so they can have the information before the visit. As with many things during COVID, some of these innovations will be long lasting.
I was reminded as we did our welcomes at how hard it must be to be making important life decisions this year. It was 20 years ago this year, that I started fellowship at Duke. Like many I had a pro/con list with all the facts and details around fellowship that would help make the rational decision. But, as I now tell the applicants, the other side of the leger is the “Gut” feeling about being at a place that fits/ seems right for the kinds of things you want to accomplish. Perhaps the largest part of that “Gut” feeling comes from the people, the co-fellows, the faculty, the nurses, the staff and the way they interact, joke, support, and most importantly care about each other. This is also potentially, our greatest strength and my biggest concern about the process. Without being present, how do we convey who we are through zoom. Hopefully, through the commitment, time, and discussions this will hopefully come through. Looking back – it was certainly the people in Duke Cardiology that were the most important for me. So, despite all the rational considerations our fellow applicants will have, we hope they get that “gut” feeling about our program to train the next generation of CV leaders. Thanks to all of our faculty, fellows, and staff during this important recruitment season.
Highlights of the week:
STS Star Rating for DUH Adult Cardiac Surgery Program
 We are pleased to share with you that our Adult Cardiac Surgery program at Duke University Hospital has, for the first time, earned three simultaneous distinguished three-star ratings from The Society of Thoracic Surgeons (STS) for its patient care and outcomes in the following areas: isolated coronary artery bypass grafting (CABG) procedures; isolated aortic valve replacement (AVR) surgery, and isolated mitral valve replacement and repair (MVRR) surgery. The three-star rating, which denotes the highest category of quality, places our program among the elite for CABG, AVR and MVRR in the U.S.
We are pleased to share with you that our Adult Cardiac Surgery program at Duke University Hospital has, for the first time, earned three simultaneous distinguished three-star ratings from The Society of Thoracic Surgeons (STS) for its patient care and outcomes in the following areas: isolated coronary artery bypass grafting (CABG) procedures; isolated aortic valve replacement (AVR) surgery, and isolated mitral valve replacement and repair (MVRR) surgery. The three-star rating, which denotes the highest category of quality, places our program among the elite for CABG, AVR and MVRR in the U.S.
“This is a significant validation of the quality and performance that we are able to deliver in cardiac surgery — the three-star rating means that our outcomes are in the top 10 percent of all centers in the United States,” said Peter K. Smith, MD, chief of the division of Cardiovascular and Thoracic Surgery and co-director of Duke Heart Center. “That we have achieved this within each of the three most important domains of cardiac surgery — bypass surgery, aortic valve replacement, and mitral valve repair or replacement – is a tribute not just to the surgeons but our entire team of dedicated health care professionals in our Operating Room, Intensive Care Unit, and Step-down Units.”
The STS star rating system is one of the most sophisticated and highly regarded overall measures of quality in health care, rating the benchmarked outcomes of cardiothoracic surgery programs in the U.S. The star rating is calculated using a combination of quality measures for specific procedures performed by an STS Adult Cardiac Surgery Database (ACSD) participant. We achieved a two-star rating in each of the remaining two areas of reporting: AVR+CABG and MVRR+CABG.
“Any scoring system has its limitations, but this is one of the most scientifically validated systems for heart surgery. It involves a huge amount of data from almost all centers in the U.S. and a very complicated and well thought out risk-adjustment model,” according to Carmelo Milano, MD, Chief of the Section of Adult Cardiac Surgery in the division of Cardiovascular and Thoracic Surgery. “Not only are they looking at raw outcomes like survival, but they take into consideration the pre-operative conditions that may make certain cases much higher risk. This is a very well respected grading system for heart surgery.”
The latest analysis of data for CABG covers a 1-year period, from January 2019 to December 2019; the analysis of data for isolated AVR, isolated MVRR, AVR+CABG and MVRR+CABG surgeries covers a 3-year period, from January 2017 to December 2019.
“Achieving the elite STS three-star rating, one of the most sophisticated and highly regarded overall measures of quality in health care, is a testament to our program’s commitment to quality improvement and safety across the cardiac surgical patient journey – from careful preoperative planning and optimization, to relentless attention to detail and coordination of intraoperative and postoperative decision making among multi-disciplinary heart team members,” added Mihai Podgoreanu, MD, chief of Cardiothoracic Anesthesiology and Critical Care. “In these unprecedented times, we are united in our dedication, resilience, compassion, and innovative spirit to continue pursuing our highest purpose – excellence and quality care for patients in need of cardiac surgery and their families.”
“As an organization and a group – the STS three star rating is evidence of the dedication of our entire Heart Center around how we care for our patients with multi-disciplinary teams that start with the evaluation and identification of patients needing coronary revascularization or valve surgery all the way through recovery, rehab, and return to life,” said Manesh Patel, MD, chief of the division of Cardiology and co-director of Duke Heart Center. “I am excited that during these challenging times our teams have continued the dedication and work to stay focused on patient outcomes.”
The STS National Database was established in 1989 as an initiative for quality improvement and patient safety among cardiothoracic surgeons. The STS ACSD houses approximately 6.9 million surgical records and gathers information from more than 3,800 participating physicians, including surgeons and anesthesiologists from more than 90 percent of groups that perform heart surgery in the US. The Database includes three other components: the Congenital Heart Surgery Database (CHSD), the General Thoracic Surgery Database (GTSD), and the mechanical circulatory support database (Intermacs). Duke has participated in the STS National Database since its inception.
We are extremely pleased and wanted to share this news with each of you, because without you this could not have happened. Thank you for your outstanding work and your dedication. This is very well deserved and the entire team is to be commended. Thank you and congratulations!
New CT Anesthesiologist, Sundar Krishnan
 Earlier this week, Mihai Podgoreanu, chief of Cardiothoracic Anesthesiology, announced the hiring of Sundar Krishnan, MBBS, to the CT Anesthesiology faculty. A native of India, Sundar obtained his medical degree and anesthesiology residency from All India Institute of Medical Sciences in New Delhi, followed by fellowships in adult Cardiothoracic Anesthesia and Critical Care Medicine at the University of Iowa. He joined the faculty at University of Iowa in 2009, where he rose through the ranks to Associate Professor and Vice Chair for Education prior to being recruited to Duke. Sundar will start in the CTOR later this month, and in the CTICU in November.
Earlier this week, Mihai Podgoreanu, chief of Cardiothoracic Anesthesiology, announced the hiring of Sundar Krishnan, MBBS, to the CT Anesthesiology faculty. A native of India, Sundar obtained his medical degree and anesthesiology residency from All India Institute of Medical Sciences in New Delhi, followed by fellowships in adult Cardiothoracic Anesthesia and Critical Care Medicine at the University of Iowa. He joined the faculty at University of Iowa in 2009, where he rose through the ranks to Associate Professor and Vice Chair for Education prior to being recruited to Duke. Sundar will start in the CTOR later this month, and in the CTICU in November.
Please join us in welcoming Sundar Krishnan to the faculty and to Duke Heart!
Celebratory Grand Rounds Held for Peterson
 Duke Cardiology held a celebratory Grand Rounds for Eric Peterson this week with about 170 attendees and terrific presentations and tributes by Matt Roe, Sreek Vemulapalli, Jon Piccini, Tracy Wang, Neha Pagidipati and Ann Marie Navar. From his work as a clinician and researcher, to the influence of his work on health policy; his innovative thinking on how data is extracted and interpreted, to his mentorship and leadership over the years – each spoke to Peterson’s legacy in science, at Duke, in the field of cardiovascular disease, and on them professionally. It was a wonderful event and we thank all who were able to join us!
Duke Cardiology held a celebratory Grand Rounds for Eric Peterson this week with about 170 attendees and terrific presentations and tributes by Matt Roe, Sreek Vemulapalli, Jon Piccini, Tracy Wang, Neha Pagidipati and Ann Marie Navar. From his work as a clinician and researcher, to the influence of his work on health policy; his innovative thinking on how data is extracted and interpreted, to his mentorship and leadership over the years – each spoke to Peterson’s legacy in science, at Duke, in the field of cardiovascular disease, and on them professionally. It was a wonderful event and we thank all who were able to join us!
Best wishes, Eric!

Celebrating Duke Heart Physician Assistants
We’ve been celebrating National Physician Assistants Week, which runs through October 12, in recognition of the PA profession and its contributions to the nation’s health. In the midst of this challenging year, we are deeply grateful for the efforts and contributions of these vital members of the Duke Heart team and we remain particularly proud to celebrate the PA profession that began right here at Duke University.
Prior to becoming a week-long event, PA Day was first celebrated on October 6, 1987, in honor of the 20th anniversary of the first graduating class of PAs from the Duke University PA program; October 6 is the birthday of the profession’s founder, Eugene A. Stead, Jr., MD, former chair of the Duke Department of Medicine and founder of the Duke Cardiovascular Disease Research Database.
As part of highly skilled multidisciplinary care teams, PAs provide diagnostic and therapeutic patient care in virtually all medical specialties and settings. They have very diverse job descriptions and play important roles throughout patient care, medical education, health administration, leadership, and research studies.
We asked two of our PAs why they chose the profession and what they enjoy most as part of their affiliation with Duke Heart:

2nd Year Student Headshots
Thursday, April 20, 2017
(©2017 Kevin Seifert Photography | kevinseifertphotography.com | 919-208-9458)
“I chose to become a PA so I could have a meaningful career helping people through some of the most challenging experiences of their lives,” said Joanna Newman, a PA on our Cardiothoracic Surgery Step-Down Unit. “Duke Heart is a special place to work because our outstanding team collaborates to offer hope and healing to patients with incredibly complex conditions that may have run out of treatment options elsewhere. I am proud of the work that we do and am honored to serve as part of the team.”
“I decided to become a PA after working as a Paramedic for several years, said Allen Stephens, a PA with Duke Cardiology at Southpoint. “I desired to be able to do more for patients than in the short amount of time I spent caring for them in the pre-hospital environment. The PA route was a perfect avenue to do that and provides

versatility and work-life balance. PAs get to practice medicine and develop a trusted relationship with their patients. Duke Heart is a great place to work as a PA. The team supports advanced practice providers, values the care we provide, and truly embodies team-based healthcare!”
A very special thank you to all PAs throughout Duke Heart for the great work
you’re doing!
Shout-Out: CICU Team Effort by Blumer, Banks, Gordon, Zwischenberger!
We received word of a particularly great save this week via Jamie Jollis and L. Kristin Newby. The note from Jollis reads, in part: “Just wanted to call your attention to a patient who was likely saved by the excellent intervention and decision making of CICU fellows this week:
JR is a 69 yo woman who was brought to the Duke ED by Orange county EMS with 1 week of progressive weakness and intermittent chest pain and an ECG showing ST elevation in V1-V3.
In the ED, the patients BP was recorded as 60/20, and an echo showed acute severe AR due to endocarditis, and a distal anterior septal wall motion abnormality.
Realizing the severity of the situation and likely impending complete hemodynamic collapse, Vanessa Blumer consulted CT surgery, and worked with the team to get the patient directly to the OR at 9 PM.
The patient received tissue aortic and mitral valves and a VG to the LAD. JR is now walking the floors and doing well.
I have no doubt the patient was “saved” by an excellent diagnostic approach and referral to surgery.
The note from Newby reads (in part), “Your work is a great example of the team culture we so highly value (and sometimes lose sight of) at Duke. It took a remarkable team effort to get this patient the care she needed.”
Many, many thanks to the quick thinking and teamwork of Vanessa Blumer, Adam Banks, Maggie Gordon of our sonography team, and Brittany Zwischenberger. Outstanding work, CICU fellows, surgeons and sonographers and to the full CICU staff for the care of this patient! Well done.
Duke Heart Grows By One!
We are very excited to welcome Celia Burgess Friede, to the Duke Heart family! She arrived on Oct. 2, at 7 lbs., 15 oz and 19 inches. “Mom, baby, and big sister are doing well!” according to dad (and cardiology fellow), Kevin Friede.
Congrats, Friede family!! We look forward to meeting her!

Wellness Tip: Why sending letters might help your loved ones
A recent article in The Washington Post suggests letter writing instead of Zoom calls as a mental health break and a good way to demonstrate you care. And who doesn’t appreciate ‘real’ mail that isn’t a bill or a campaign flyer?
Summary: Picture the recipient before you begin – what do you like about them? Why are you grateful to have them in your life? Focus on the future — share something you hope to do/experience in the future with this person; exude hope. Remember the elderly – they may be less tech-savvy and more prone to loneliness. A letter provides a means of connection.
To read the full article, visit: https://wapo.st/2GMap1M
Important Reminders
- Open Enrollment for Duke Benefits is October 19-30.
- Do not come to work if you are not well – if you are showing symptoms of a cold, of COVID, of influenza, etc. – stay home. Coming to work sick puts patients and colleagues at risk.
- Please get your Flu Vaccination: All team members must get their vaccination or otherwise demonstrate policy compliance by Tuesday, Nov. 10. Details and resources all available on the Duke Health Influenza Resources site (NET ID required): https://influenza.dh.dukehealth.org.
Upcoming Opportunities/Save the Date:
Cardiology Grand Rounds
Oct. 13: Approach to Antibody-Mediated Rejection in Heart Transplantation. Presenter: Michelle Kittleson, MD, PhD of Cedars-Sinai. 5 p.m., Webex. Details in email invitation.
Oct. 20: The Albert L. Williams Cardiovascular Genetics Lecture Series. Presenter: Wendy Chung, MD, PhD, of Columbia. 5 p.m., Webex. Details in email invitation.
Oct. 27: Cardiology Faculty meeting
Nov. 10: TBA
Nov. 17: No CGR. AHA Scientific Sessions
Conferences, Symposia & Webinars
Nov. 13: 12th Annual NC Research Triangle Pulmonary Hypertension Symposium. Noon – 4:30 p.m. For more information, please visit this page. This event will be held virtually and is co-sponsored by Duke and the University of North Carolina in partnership with the Pulmonary Hypertension Association through the Building Medical Education in PH program. Please join us!
Nov. 13–17: AHA Scientific Sessions 2020, a virtual experience. Registration is now open. See the website for details.
COVID-19 Updates:
All the latest official DUHS information regarding coronavirus/COVID-19 response at the following locations:
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged.
Duke Heart in the News:
October 6 — DUHS is mentioned
Becker’s Hospital Review
CHIME names 2020 ‘Most Wired’ hospitals
https://bit.ly/36VP8NW
October issue — DUH & Cardiology are mentioned
Newsweek – special report/rankings
World’s Best Specialized Hospitals 2021
https://www.newsweek.com/worlds-best-specialized-hospitals-2021
Duke Heart Week ending October 4th 2020
Chief’s message: The Public Health and the Scientific Method
This weekend my 15-year old son was working on building a toothpick bridge for his physics class in high school, and as I was instructed not to help him, I realized how little I know about some of basic principles of the challenge. In fact, his work building a prototype, refining it, and trying to improve based on observation was at times in stark contrast to the many of the ongoing events over the last several months, events that this week unfortunately included the President getting diagnosed with COVID-19 and being admitted to Walter Reed Hospital for care.
Increasingly, it seems that we need the scientific method to improve public health, but perhaps just as importantly, we need to develop ways to gain the acceptance and implementation across our colleagues and communities. This is not a new story. Many have likely heard the story of Ignaz Semmelweis, the Hungarian physician, who was functioning as an Assistant Professor at Vienna General Hospital in 1847 when he identified that puerperal fever (also known as childbed fever) could be dramatically reduced by using hand disinfection in the obstetrical clinics. Many of the medical students going from the cadaveric clinic to the obstetric clinic had higher mortality rates that were reduced with chlorinated hand washes. Unfortunately, his discovery was not met with great acceptance, and he grew increasingly outspoken and eventually had a nervous breakdown. He was admitted to an asylum where he died, ironically from a gangrenous wound to his right hand that he reportedly got from a beating in the asylum. After his death, with Louis Pasteur confirming the germ theory, Florence Nightingale and her mastery of data visualization and clear writing, and Robert Koch and his postulates on infection, the practice of hand washing started to become widespread. Even today, we have monitors in our hospitals watching to ensure our rates of hand washing going into and coming out of rooms remain high – habits that can save lives.
We have certainly come a long way with the scientific method, using the ‘gift of randomization’, blinded analysis, data safety monitoring boards, and regulatory and scientific groups to help us understand and put the latest scientific findings into context. However, now more than ever – on the eve of vaccines for a global pandemic, increased therapeutics for heart disease, and personalized cancer therapies, we need to develop ways to rapidly implement discoveries into practice. Work from our group (many faculty in our Division that are pioneers) at the Duke Clinical Research Institute along with behavior science and health policy have shown to be effective we need to engage people and communities, remove barriers, and above all provide transparent findings from our work in easy to understand communications.
As we hope for the speedy recovery of our President, and recovery of the many thousands dealing with COVID-19 in our country, this week underscored both the significance of the scientific method, and the importance of getting adoption of proven therapies aimed at our public health. In this week’s edition of the Pulse you will find several stories of our group working to help identify ways to play important roles in scientific discoveries.
Highlights of the week:
Duke Lead Enroller for ACTIV-3 Trial for COVID-19; Receives Kudos from Collins, Operation Warp Speed

Duke University
A team of clinicians across Duke Health, led by Peter K. Smith, MD, chief of the division of Cardiovascular and Thoracic Surgery and co-director of Duke Heart Center, are working diligently in a collaborative effort to enroll patients in ACTIV-3, a randomized, controlled trial testing a novel antibody treatment for COVID-19. Duke is currently the lead enroller in this international trial, with 42 out of 151 total patients enrolled in the U.S. and Europe thus far.
The team’s early success in the trial was recognized this week with a personal letter of gratitude from Francis Collins, MD, PhD, Director of the National Institutes of Health (NIH), and Janet Woodcock, MD, of Operation Warp Speed.
“Given the ongoing COVID-19 pandemic that is taking many lives, the ACTIV-3 trial is now more important than ever and is critical to progressing our understanding of safety and effectiveness of different monoclonal antibodies in treating COVID-19 in people who have been hospitalized with the infection,” the letter reads. “Rapid implementation and completion of this trial represents a very high priority for NIH and Operation Warp Speed. Your site was the second one opened, and has enrolled 27 [now 42] patients in 28 days, a truly remarkable performance.”
The ACTIV-3 trial tests the efficacy of a monoclonal antibody as a method of treatment, developed from the blood sample of a recovered COVID-19 patient.
“This trial crosses so many different boundaries,” says Smith. “We are grateful to the Department of Surgery’s infrastructure, and we have hospitalists and critical care physicians involved. We are not just working at Duke University Hospital, but also at Duke Raleigh and Duke Regional. Everyone is pulling more than their weight, working 24/7, and it is incredibly heartening to see these selfless contributions by so many people.”
Smith credits the recognition from the U.S. Department of Health & Human Services to the exceptional collaboration happening across Duke, including research coordinators Beth Hollister and Kathleen Lane, as well as clinical staff at all three hospitals.
Congratulations, Dr. Smith and team!!! To read more about this effort, see Duke Heart in the News, below.
DCD Heart Transplant Clinical Trial Update
Congratulations and many thanks to all members of the Duke Heart Transplant team. Not only did they perform the first adult donation after circulatory death (DCD) heart transplant in North America (December 1, 2019), but the Duke site was the lead enroller for the first phase of the clinical trial, dubbed the DCD Heart Trial.
The 90th DCD heart transplant was completed this week. Duke enrolled 34 total patients while the next leading site enrolled 20 as part of phase one. A second phase of the trial is expected to launch by the end of the year.
“Through a tremendous team effort, we continue to expand the donor pool and save lives,” said Jacob Schroder, director of Duke’s Heart Transplantation Program in an email to team members. He added a special thanks to Sarah Casalinova, the Duke’s DCD Heart Trial study coordinator, and all heart transplant coordinators.
Congratulations, team! We are incredibly proud of your work and dedication to advancing heart transplantation. Outstanding!
ACC Quality Improvement Summit
Jennifer Rymer, Angela Lowenstern, and Sunil Rao presented their quality improvement project titled “The Duke Renal Impairment Project (DRIP)” at the American College of Cardiology’s Quality Improvement Summit, held virtually on Sept. 30.
This project, funded by the American College of Cardiology, sought to reduce the incidence of acute kidney injury after cardiac catheterization or percutaneous coronary intervention. Working with Schuyler Jones, Duke Cath Lab Director, and Jimmy Tcheng, Duke Heart Center Informatics, the team implemented a process where high risk patients would be identified and given appropriate pre- and post-procedure hydration, and would undergo a “renal timeout” that included a maximum safe level of contrast administration.
This successful project was chosen by the ACC-NCDR as a finalist in their competition for QI projects, and has led to the submission of two NIH grants for wider implementation of the protocol. Congratulations to the team!
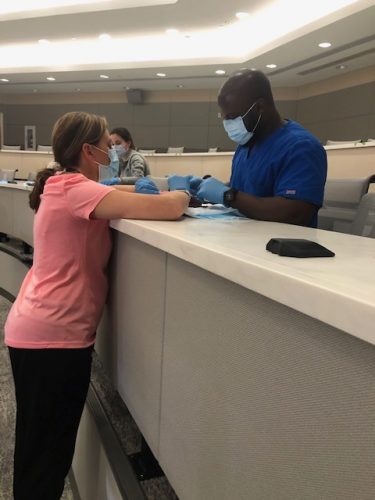
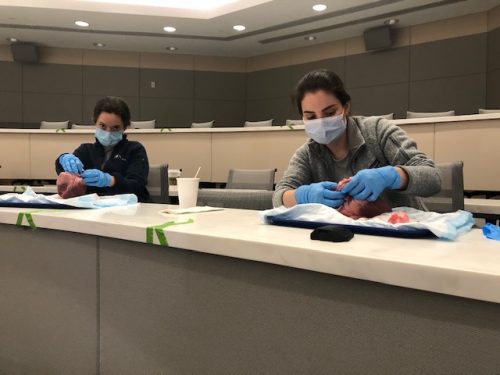
Semi-Annual Kisslo Heart Dissection Session Held
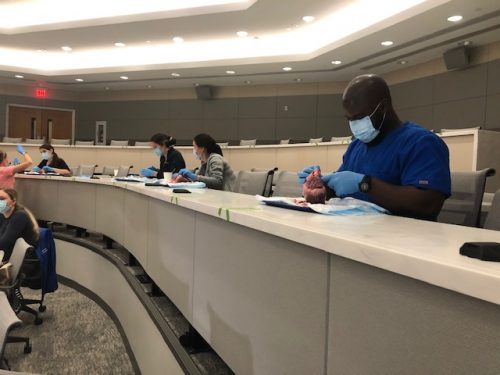
The semi-annual Kisslo Heart Dissection Session was held in two parts – the first was last Saturday, Sept. 26 and the second (an advanced session) was held yesterday, Oct. 3 in the Duke South Amphitheater. The course was hosted by Joe Kisslo, MD, along with sonographers Danny Rivera, Ashlee Davis, Melissa Lefever, Batina Kight, Tracey Ralston and Carissa Marsiglio from our adult and pediatric labs across DUHS, as well as Cooper Moore from Biomedical Engineering.
The course was attended by fellows from Duke’s adult and pediatric Echo programs; Duke Biomedical Engineering students, sonographers, and fellows from the NC State Veterinary School. Attendees participated in an in-depth dissection session reviewing cardiac anatomy, electrical conducting system, coronary anatomy, and review of surgical procedures. Later in the day, participants applied their anatomical knowledge to echocardiography by cutting and cropping in 3D Echo.
This dissection session is always a favorite of fellows, students, and sonographers who join in, according to Ashlee Davis, chief technologist for the Clinical Diagnostic Unit.
Shown in photos are: Francis Ugowe, Vanessa Blumer, Josephine Harrington, and Karen Flores Rosario, along with teaching sonographer Batina Kight.
Duke Heart Grows By One!
We are thrilled to welcome James Rouse Peters, born Sept. 25 at 5:03 p.m., to the Duke Heart family. Cardiology fellow Anthony Peters reports that “Mom and baby are both doing well, and big sister Charlotte (2.5 years old) is loving taking care of her “new baby James”!
 He’s adorable and we look forward to meeting him! Congrats, Peters family!
He’s adorable and we look forward to meeting him! Congrats, Peters family!
High Five for Hearon!
 Delia Hearon, one of our outstanding Duke Heart case managers, has received a Duke Health High Five. She was nominated by Jamie McDermott, one of our NPs, who wrote:
Delia Hearon, one of our outstanding Duke Heart case managers, has received a Duke Health High Five. She was nominated by Jamie McDermott, one of our NPs, who wrote:
“We were discharging a patient to a center that required education for their staff. Delia worked to understand the needs of the center and thought of creative ways to get them the education that they needed. She developed a strong relationship with the center by offering her support and patience. Our team is thankful and appreciated Delia’s hard work and dedication to this patient’s situation.”
Thanks for thinking outside the box for our patients, Delia. Way to go!
Passings: Felecia Monique Credle, RN, BSN
 Felecia Credle, one of our Heart Center Communications (HCC) team members, passed away Sunday, Sept. 27. The cause was cancer. Ms. Credle began her career with Duke in 2004 working with the Outpatient Holding team. She was a member of the CVSSU from February 2007 until May of 2016 when she joined the HCC team. Credle had been in nursing for 30 years, 16 of them here at Duke. Her services were held yesterday at Mt. Olive Missionary Baptist Church of MESIC. A link to her obituary can be found here.
Felecia Credle, one of our Heart Center Communications (HCC) team members, passed away Sunday, Sept. 27. The cause was cancer. Ms. Credle began her career with Duke in 2004 working with the Outpatient Holding team. She was a member of the CVSSU from February 2007 until May of 2016 when she joined the HCC team. Credle had been in nursing for 30 years, 16 of them here at Duke. Her services were held yesterday at Mt. Olive Missionary Baptist Church of MESIC. A link to her obituary can be found here.
We extend our condolences to her family and friends, and to her immediate co-workers in Heart Center Communications. We know she will be missed.
ICYMI:
Todd McVeigh and Callie Tennyson have a newly published article in the October issue of the Journal of the American Academy of Physician Assistants. You can check it out here:
McVeigh, Todd PA-C; Tennyson, Carolina DNP, ACNP-BC, AACC Understanding and recognizing cardiac amyloidosis, Journal of the American Academy of Physician Assistants: October 2020 – Volume 33 – Issue 10 – p 16-20 doi: 10.1097/01.JAA.0000697236.11386.3a
ICYMI: Celebrating Sheroes in the Department of Medicine
The Department of Medicine allowed nominations for “Sheroes” during the month of September as a way to showcase accomplishments of women physicians, scientists, educators, and leaders in medicine. Several Duke Heart faculty members (Anna Lisa Crowley, Terri Fortin, Svati Shah, Monique Anderson Starks and Cary Ward) and Sarah Goldstein, a cardiology fellow, were nominated. Read more about it here.
Important Reminders
- October 6-12 is PA Week.
- It’s Research Week! See link under Conferences, below.
- Saturday, Oct. 10 is the 2020 Triangle Heart Walk (virtual!). An online kick-off Pep Rally is planned for Friday, Oct. 9 from 12-12:30 p.m. Team captains and registered walkers should check their emails from Triangle AHA.
- October is Medical Ultrasound Awareness Month (the month formerly known as sonography month). Please thank a sonographer!
- Open Enrollment for Duke Benefits is October 19-30.
- Please get your Flu Vaccination: All team members must get their vaccination or otherwise demonstrate policy compliance by Tuesday, Nov. 10. Details and resources all available on the Duke Health Influenza Resources site (NET ID required): https://influenza.dh.dukehealth.org.
Upcoming Opportunities/Save the Date:
Cardiology Grand Rounds
Oct. 6: The Robert J. Lefkowitz, MD, Distinguished Lecture. Presenter: Helen Hobbs, MD, investigator, Howard Hughes Medical Institute and professor, Internal Medicine and Molecular Genetics, UT Southwestern Medical Center. Noon – 1 p.m., part of Duke SOM Research Week. For more information, please visit: https://medschool.duke.edu/research/research-week.
Oct. 6: Special Cardiology Grand Rounds – A Tribute to Dr. Eric Peterson. 5 p.m. Virtual. Links available in Outlook invitation. Presenters:
- Matthew Roe, MD – Origins of CV Registries
- Sreek Vemulapalli, MD – Partnering with Professional Societies
- Jon Piccini, MD – Expanding the Scope: AF/Stroke Care
- Tracy Wang, MD – Implementation Science
- Neha Pagidipati – Possibilities in Prevention
- Ann Marie Navar, MD – Going Digital
- Eric Peterson, MD – The Future
Oct. 13: Michelle Kittleson, MD, PhD, of Cedars-Sinai.
Oct. 20: The Albert L. Williams Cardiovascular Genetics Lecture Series. Presenter: Wendy Chung, MD, PhD, of Columbia.
Oct. 27: Cardiology Faculty meeting
Nov. 10: TBA
Nov. 17: No CGR. AHA Scientific Sessions
Conferences, Symposia & Webinars
Oct. 5 – 8: Research Week. Sponsored by Duke School of Medicine. Series will be held virtually, via Zoom: https://duke.zoom.us/j/92060873004. More information and a full agenda can be found here: https://medschool.duke.edu/research/research-week
Oct. 7: PROMISE trial webinar. Pam Douglas will lead an overview of the PROMISE trial cohort, and research plan, with insights and panel discussions. 4-6 p.m., To register for the Zoom link, please visit: https://duke.zoom.us/webinar/register/WN_wSz_1UcZRNy0cmqg8q6hgg. Sponsored by DCRI.
Nov. 13: 12th Annual NC Research Triangle Pulmonary Hypertension Symposium. Noon – 4:30 p.m. For more information, please visit this page. This event will be held virtually and is co-sponsored by Duke and the University of North Carolina in partnership with the Pulmonary Hypertension Association through the Building Medical Education in PH program. Please join us!
Nov. 13–17: AHA Scientific Sessions 2020, a virtual experience. Registration is now open. See the website for details.
COVID-19 Updates:
All the latest official DUHS information regarding coronavirus/COVID-19 response at the following locations:
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged.
Duke Heart in the News:
September 25 — Peter Smith
Duke DOS News
Duke Tests Novel COVID-19 Therapy, Is Lead Enroller in International Trial
https://surgery.duke.edu/news/duke-tests-novel-covid-19-therapy-lead-enroller-international-trial
September 26 — Cameron Wolfe (infectious diseases)
Medium.com
A Change of Heart: Why Covid-19 Myocarditis Seems Less Threatening to Athletes Now Than Before
https://bit.ly/2GpPt06
September 27 — Duke Clinical Research Institute
Triangle Business Journal (subscription required)
The future of clinical research: How DCRI is launching a direct-to-family trial
https://bit.ly/2SkQppb
October 1 — Peter Smith
Duke DOS News
Duke Researchers Testing Novel Therapeutics for Early and Acute Stages of COVID-19
https://surgery.duke.edu/news/duke-researchers-testing-novel-therapeutics-early-and-acute-stages-covid-19
Recent Comments