Home » 2024 (Page 4)
Yearly Archives: 2024
Duke Heart Pulse — May 26, 2024
Chief’s message:
This memorial day we wanted to thank and recognize the women and men that continue to protect, serve, and sacrifice for the safety, freedom, and liberty of our nation and our allies. Please be sure to thank all of the service members and recognize the sacrifices they and their families make everyday.
Updates from the week of the week:
Patel to serve as DUHS Physician VP for Heart & Vascular Services

Manesh R. Patel, MD, the Richard S. Stack Distinguished Professor and division chief of cardiology at Duke, will serve as the Duke University Health System physician vice president for Heart and Vascular Services, effective May 15th, 2024.
In this role, Patel will oversee cardiovascular care for Duke, working closely with Carmelo Milano, MD, chief of cardiothoracic surgery, Dawn Coleman, chief of vascular and endovascular surgery, and Mihai Podgoreanu, chief of cardiothoracic anesthesiology. Our cardiovascular service line leadership team, including Jill Engel, vice president, and Mary Lindsay, associate chief nursing officer, will work together with Manesh to continue to advance cardiovascular care across Duke Health.
Patel will work closely with DUHS leadership and clinical department chairs to develop innovative initiatives that improve access to care and support the Duke Health strategic plan. His responsibilities will encompass quality and outcomes, budgetary and financial oversight, operations, and management of Duke Heart Network and affiliations. As part of this work, Manesh will lead a Health AI clinical testing lab within the Duke Heart Innovation Hub, partnering with Michael Pencina, Jeff Ferranti, and Duke AI Health.
This change reflects Duke’s commitment to the tremendous team across Duke Health who aim to discover and deliver extraordinary team-based cardiovascular care for patients as a leading Heart and Vascular Center.
Patel completed his medicine residency and fellowships in cardiology, interventional cardiology, and clinical research at Duke and Duke Clinical Research Institute. He has served as the division chief of Duke Cardiology since 2017. He was selected by the American Heart Association in 2023 as AHA Physician of the Year.
Upon this transition, Patel will report to Greg Pauly, group president of Acute Care Services for Duke University Health System, and vice dean for Clinical and Academic Integration with the School of Medicine.
Duke EP Well Represented at Heart Rhythm 2024
Members of our electrophysiology (EP) and cardiology faculty and several EP staff were very busy at the Heart Rhythm Society (HRS) 2024 meetings, held May 16-19 in Boston. There were many Duke abstracts and presentations, too many to fully recount, but here are some highlights provided by Jonathan Piccini, MD, MHS, professor of medicine in cardiology and director of cardiac electrophysiology at Duke:
Bill Cockfield, Amber Stohl, Gail Brock, Sana Al-Khatib, and Kristen Campbell found some time to snap a quick picture before a roundtable session. Dr. Kevin Thomas received the distinguished and very prestigious James Youngblood Excellence in Leadership Award from the Heart Rhythm Society
Dr. Kevin Thomas received the distinguished and very prestigious James Youngblood Excellence in Leadership Award from the Heart Rhythm Society

 While at the meeting Dr. Thomas delivered invited lectures on “Diversity in EP Clinical Studies – Challenges and Opportunities” and “Addressing Disparities in Sudden Cardiac Death.”
While at the meeting Dr. Thomas delivered invited lectures on “Diversity in EP Clinical Studies – Challenges and Opportunities” and “Addressing Disparities in Sudden Cardiac Death.”
Kristen Campbell was named to the Heart Rhythm Society Board of Trustees! She is the first-PharmD to achieve this distinction, a true reflection of her commitment to heart rhythm care. She chaired several sessions on antiarrhythmic therapy at the HRS meetings.
Dr. Kelly Arps presented her work with Dr. Al Sun on outcomes associated with emergent extracorporeal membrane oxygenation (ECMO) and catheter ablation for ventricular tachycardia in the setting of cardiogenic shock.

Dr. Al Sun served as distinguished faculty at the HRS 2024 EP Fellows Symposium alongside Duke EP alumni Dr. Eric Prystowsky and Dr. Doug Packer. He also participated in an expert panel on managing unexplained sudden cardiac arrest.
Dr. Larry Jackson delivered an invited lecture on “Overcoming Healthcare Delivery Gaps – Walking the Talk”. He also served as one of the judges along with Jon Piccini in the AHA-HRS Shark Tank competition at the scientific sessions.

Dr. Camille Frazier-Mills presented an invited lecture on the role of pharmacotherapy and pacing in persons with cardioinhibitory vasovagal syncope. She also led a session on the optimal management of cardiovascular implantable electronic device (CIED) alerts and advisories as well as a session on diversity and EP leadership. She also delivered the invited commentary on the long-awaited one-year outcomes from the dual chamber leadless pacing study that was presented in the late-breaking science session.
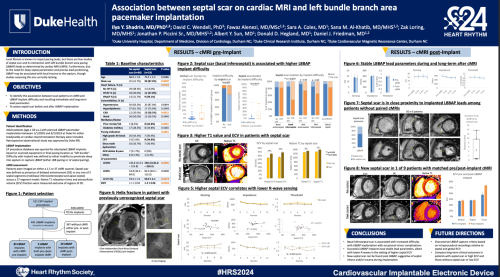
Dr. Ilya Shadrin presented his research on left bundle branch area pacing with Dr. Daniel Friedman, including an abstract reporting on the relationship between septal scar and pacing.
Dr. Daniel Friedman (below, far right) delivered an invited lecture on “How to Predict the Response of LBBP-CRT?”

Dan Friedman and Jon Piccini were among a team of investigators presenting our pre-clinical work on a balloon-based ablation catheter to deliver pulse field ablation in a canine model.

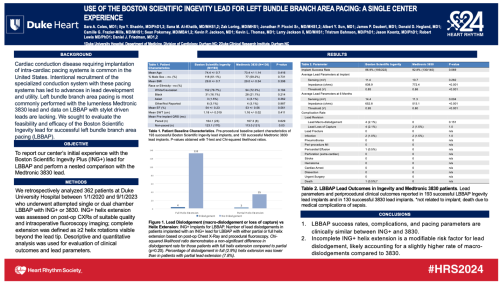
Dr. Sara Coles reported the Duke EP experience with the stylet-driven Ingevity+ lead for left bundle branch area pacing, the largest experience reported to date in the field.
Dr. Kevin Jackson delivered an invited lecture on the Optimization of Programming in Cardiac Resynchronization Therapy in the “One Stop
Shop for All Things Device Programming” session at HRS. He also delivered the commentary on the FARAPULSE registry data presented at the late-breaking science sessions.
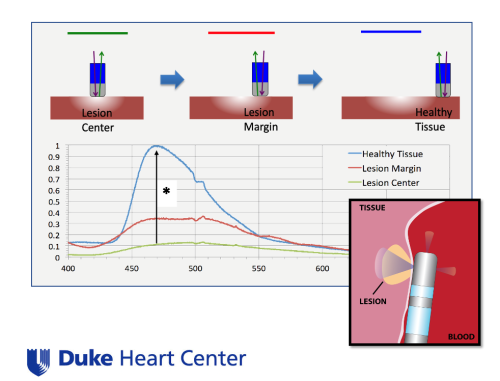
Dr. Jon Piccini presented on the use of LuxMed hyperspectral imaging and biofluorescence to assay ablation lesion efficacy and myocardial characterization at the Stanford Biodesign meeting at HRS.
Dr. James Daubert Delivered an invited lecture on patient selection and optimal use of implantable cardioverter defibrillator (ICD) therapy in persons with non-ischemic cardiomyopathy, and a lecture on programming of ICDs in competitive athletes.
Dr. Andrew Landstrom presented invited lectures at the meetings on innovative approaches to evaluating VUSs associated with arrhythmogenic cardiomyopathies and an “Introduction to Cardiovascular Genomic and Precision Medicine.”
Dr. Monique Starks presented an invited lecture on “Drone-delivered Automated External Defibrillators (AEDs): Improving the Chain of Survival in the US.”

Dr. Sana Al-Khatib had a very busy HRS this year as she continues on the executive leadership team for the Heart Rhythm Society. She was a key architect of the HRS 2024 meeting, as she served as the abstract chair. At the meeting, she participated in a featured debate on the use of cardiac resynchronization therapy pacemakers (CRT-P) vs cardiac resynchronization therapy defibrillators (CRT-D) in persons with non-ischemic cardiomyopathy.
Congrats to our EP team — exceptional work and representation at HRS!
McVeigh Represents Duke Heart at AAPA 2024
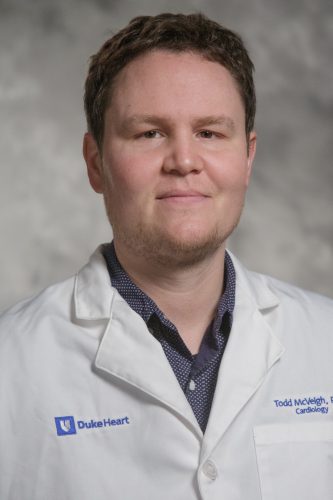
Duke cardiology physician assistant Todd McVeigh, PA-C, gave two podium poster presentations at the American Academy of Physician Associates (AAPA) 2024 annual meeting held last weekend (May 18-22, 2024) in Houston, TX.
His presentations were entitled, “Introduction of a PA into a Heart Failure Remote Monitoring clinic” and “Introduction of Home-applied Subcutaneous Furosemide to Treat Heart Failure Exacerbations”.
Way to go, Todd!
Cox Earns DAISY Award
 Congratulations to ventricular assist device (VAD) nurse practitioner Kevin Cox! Cox was awarded the 2024 DAISY Award for Extraordinary Nursing Educators through the Duke School of Nursing (SON). He was nominated by former MSN Student Sonia Lai, his former preceptee.
Congratulations to ventricular assist device (VAD) nurse practitioner Kevin Cox! Cox was awarded the 2024 DAISY Award for Extraordinary Nursing Educators through the Duke School of Nursing (SON). He was nominated by former MSN Student Sonia Lai, his former preceptee.
His notification letter included the following:
“It is my honor to advise you that you were nominated by MSN student Sonia Lai and have been selected by the Institute for Education Excellence DAISY Awards Committee to receive a 2024 DAISY Award for Extraordinary Nursing Educators in recognition of the super-human work that you do for students!” — Jacqui McMillen-Bohler, director of IEE, Duke SON.
Cox was recognized during the annual DUSON Faculty & Staff Awards ceremony held on May 22. He is shown here receiving the award from Duke SON Interim Dean Michael Relf.
Congratulations, Kevin – well-deserved!
Ramos Earns DNP

Congratulations to critical care nurse practitioner Dayana Ramos, DNP! Dayana graduated with her Doctor of Nursing Practice on May 11. She is shown here with her sister, Natassha Blakeslee, a nurse practitioner at the University of Miami, who graduated alongside her.
Ramos and Blakeslee completed their studies at Missouri State University. Ramos did her DNP project here at Duke University Hospital. Her project consisted of creating a discharge protocol to improve discharge times for the post-acute care (PAC) service.
The duo, who are Panamanian, wore sashes that were hand-made by a woman who belongs to the Kuna Indians of Panama. Dayana’s sash features the Panamanian golden frog (rana dorada), which is indigenous to and found only in Panama. Her sister’s sash features the Harpy Eagle, the national bird of Panama. They wanted to incorporate symbols from their native country and represent their culture.
Congratulations, Dayana & Natassha!
Shout-out to Biever
A shout-out to Kimberly Biever from the cardiology clinical research unit!
“She identified and approached a patient for an inpatient study. Because the patient wanted more time (to consider), she returned back to the hospital to consent and initiate study procedures on a Sunday. Kim goes again and again beyond the call of duty, due to her passion for research and love of patients. It is a pure delight to work with coordinators like her, which is what makes Duke great.” — Marat Fudim
Great work, Kim!
Kudos to Granger & 7E Staff
We received a note this week from David Gallagher, MD, chief medical officer for Duke University Hospital regarding feedback he received from a grateful patient:
“Chris, we received this nice feedback (from Press Ganey HCAHPS) about the great care you and your team gave to a patient at Duke University Hospital. Thank you for the high quality and compassionate care you provide to patients!” – David Gallagher, MD
“I would like to thank Dr. C. Granger & the entire 7E ICU staff for giving me the best care ever. They made the most traumatic thing in my life a whole lot easier with excellent care!” – a grateful patient
Great job, team!!!!
Team Member Appreciation Month: Spirit Week
Our team members are what make Duke Health such a special place to work and to heal. This year, Duke is elevating how we recognize and thank everyone for their incredible work through our inaugural Team Member Appreciation Month.
It’s week 4, the final week: Spirit Week
Monday: Team Mixtape—Start a collaborative playlist with your team to jam to! Apple Music, Spotify, and YouTube have collaboration features to make a shared playlist. You can also amp up the festivities with a virtual team music party to take a break during your busy day – be sure to share your dance moves by uploading your photos and videos here! Note: Please be respectful and only use clean and appropriate music.
Tuesday: Crazy Socks Day—Wear your favorite socks to work – yes, those super fun ones
Wednesday: Spread Smiles with Kudos & Kindness—Seize the day and spread smiles with some of these ways to keep kindness top of mind:
- Send a Kudos Kard (or five!)
- Let a colleague know why you’re proud of them
- Celebrate something/someone that doesn’t get normally recognized enough
- Give a high five
- Greet three strangers while walking the hallways
- In Huddle/team meeting, take a moment to share a team win
- Send a story to be shared across Duke Health
- Make a team birthday and/or work anniversary calendar and create a plan to celebrate them
- Have lunch with someone out of your normal routine
- Give three people compliments (only one can be about looks!)
- Let someone know when something reminds you of them and it made you smile
- Take a moment to connect/check in with someone that you haven’t in a while
- Sign up to do some community service
- Give someone a fun sticky note or Teams message
- Invite someone to join you in practicing self-care at work
- Share a story with teammate that they are a part of that always makes you smile when you think of it
- Surprise your team with a kind gesture
Thursday: Chalk the Sidewalk—Take a moment to go outside and draw on the sidewalk! Be sure to share your masterpiece via photos and videos here!
Friday: Show Your Duke Pride Day—Wear your favorite Duke gear or blue attire! Note: Dress code policies are still in place – be sure to check the Policy Center to find your entity’s policy.
Learn more about Team Member Appreciation Month on Duke Health Now.
Thank You for Participating in Culture Pulse
Dear Colleagues,
Thank you for participating throughout the Culture Pulse 2024 survey period. We heard from more than 23,000 team members (63 percent) and are working to bring valuable feedback to you in the coming weeks. Everyone worked hard to ensure the voices of Duke team members were heard.
As we begin to look at the data, make plans for sharing the results, and focus on our action-planning process, we look forward to partnering with you as we adapt to improve our work together. There’s more to come, so stay tuned!
Thank you again — Ian Lee Brown, Vice President and Chief Employee Experience Officer, DUHS
Upcoming Events & Opportunities
- May is American Stroke Month and Asian American and Pacific Islander Heritage Month
- May is Duke Health’s inaugural Team Member Appreciation Month
- Save the Date: June 12, 4-5 p.m., State of the School Address (SOM)
Cardiology Grand Rounds
May 28: The Ross Operation — The Ultimate Aortic Valve Replacement? with Ziv Beckerman. 5 p.m., DN2002 or via Zoom.
June 4: The Science and Community of Critical Care Cardiology with Balim Senman. 5 p.m., DN2002 or via Zoom.
All Duke Cardiology Grand Rounds recordings are housed on Warpwire. To access recordings please visit:
NET ID and password required. Enjoy!
CD Fellows Core Curriculum Conference
May 29: DHP Case Presentation with Husam Salah. Noon, DMP 2W96 (in-person only).
May 31: Echo Math with Cara Hoke. Noon, Zoom only.
DCRI Research Forum Series
 June 11: The Duke Clinical Research Institute is excited to welcome Duke Football Coach Manny Diaz as their June guest for the next DCRI Research Forum, which will close out the 2023-2024 series.
June 11: The Duke Clinical Research Institute is excited to welcome Duke Football Coach Manny Diaz as their June guest for the next DCRI Research Forum, which will close out the 2023-2024 series.
What: A Fireside Chat with Coach Manny Diaz
When: Tuesday, June 11, from Noon-1 p.m. ET
Where: DCRI Research Forum: A Fireside Chat with Manny Diaz via Zoom
We hope you’ll consider joining this virtual event!
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
May 16 — Duke Heart for Honduras
Iconos Magazine (Honduras/Hn)
Fundación Lady Lee y Duke Heart for Honduras se unen en cirugías cardiovasculares
May 18 — Sana Al-Khatib
Medpage Today
Removing Conduction System Pacing Leads: Good Success So Far
May 18 — Duke Heart for Honduras
El Heraldo (Hn)
Banco Atlántida honra a la brigada médica Duke Heart for Honduras
May 21 — Duke Heart for Honduras
La Tribuna (Hn)
May 21 — Aferdita Spahillari
tctMD
Treatment Gaps Abound in Heart Failure but Can Be Closed, Studies Show
May 21 — Nina Nouhravesh
SciTech Daily
New Research Suggests That Eggs Might Not Actually Be Bad for Your Heart
May 23 — Marat Fudim
Fierce Healthcare
Cadence finds reduced cost and better outcomes for heart failure patients through remote monitoring
May 23 — Senthil Selvaraj
Aframnews.com
Duke Heart Pulse — May 19, 2024
Duke Heart Pulse – May 19, 2024
Chief’s message – Grief and Community.
Over the last several weeks we have been having a conversation with Dr. Tony Galanos in the Division of Geriatrics and Palliative care around Grief and how we can help support our clinicians / health system staff in moments of stress and grief. This was highlighted this Monday in a wonderful grand rounds by one of our finishing fellows – Dan Loriaux. During one part of his talk, he highlighted how in ICU and hospital care – he and Dr. Galanos have worked on a program around debriefs for our fellows to help process the grief in taking care of so many sick patients. We aim to continue this and to build a community of support.
This week brought another reminder to us on the fragile nature of life and the needed strength of our community. We lost one of our recent graduates and true leader in the field – Aslan Turer. We provide his story below. I personally remembered Aslan for his unwavering humor, intellect, and energy in helping improve how we cared for patients – often holding everyone to the care standard. He will be dearly missed and our Duke Heart Community will work to support his wife Christy and their children. Please keep them in your thoughts and hearts.
Updates from the week:
In Memoriam: Aslan Turer, MD, MHS, MBA, interventional cardiologist
We have been deeply saddened this weekend at the passing of Aslan Turer, MD, 49, on Friday morning. An interventional cardiologist and hypertrophic cardiomyopathy specialist at the University of Texas Southwestern (UTSW), Turer trained at Duke through residency and multiple fellowships, and was a friend to many of our Duke Heart team members. Turer had fought cancer for the past several years. His wife, Dr. Christy Turer, also trained at Duke. They have five children. Our thoughts are with his family and with his many friends and colleagues. We know he will be greatly missed.
Turer attended medical school at the University of California San Francisco, then completed internal medicine residency at Duke University Hospital, as well as fellowship trainings in cardiovascular disease and interventional cardiology at Duke. Turer helped establish a multidisciplinary hypertrophic cardiomyopathy program at UTSW, which achieved an HCMA Center of Excellence rating in 2018. He partnered recently with Andrew Wang, MD, on a perspective piece for Circulation in February 2023 entitled “Cardiac Myosin Inhibitors: Unlocking Potential to Improve Treatment in Hypertrophic Cardiomyopathy”.
Sparkman Hillcrest Funeral Home is handling arrangements for the family; Services will be this week, as follows:
Memorial Service: Wednesday, May 22, at Sparkman/Hillcrest Funeral Home, 7405 W Northwest Hwy., Dallas, TX 75225
Muslim Prayer, 5:30 p.m., in Arabic. Christian Memorial service, 6 p.m., followed by Reflection time
Funeral, Thursday, May 23, 1 p.m.
Location: Christ the King Catholic Church, 8017 Preston Rd, Dallas, TX 75225
Aslan’s family has asked that attendees wear color and not come in traditional dark funeral attire as Aslan wanted this to be a celebration of life.
We asked for memories of Aslan for today’s issue of Pulse and received the following:
“If ever there was a person one might call a “character,” certainly Aslan Turer was one. A terrific doctor and teacher, Aslan was frequently unpredictable, a bit quirky, and a delightful prankster. I remember vividly how he and I would get into these drawn-out, crazy, and often hilarious email wars — with each trying to outdo the other with an ever more outlandish statement of silliness or goofiness. We often let the whole division in on the back and forth. As I recall, Aslan always seemed to win these verbal battles with some kind of comeback I was never clever enough to overcome. He was just fun to be around. Even more, Aslan was a sincere, loving and simply wonderful person. The world has lost a very special human being way too soon. He will be fondly remembered by all who were fortunate enough to know him.” – Thomas Bashore, MD
“Aslan and I started as interns at Duke in 2001, living in the same apartment building and were fast friends despite being from very different backgrounds. I have so many fond memories, but the most special ones were when Catherine and I would meet Aslan for a late dinner and trivia at James Joyce – where he would often be found “reading” his Lancet or NEJM, which we all established was a decoy for trying to find a mate. Later in fellowship, he moved to south Durham and we would meet in the back bar of Lantern in Chapel Hill where he had a permanent tab and everyone knew him and his sense of humor and style.
I am so saddened about his death and our thoughts are with Christy and their kids. He was truly one of the smartest, kindest, and most clever people I’ve encountered in Medicine and in life.” – Schuyler Jones, MD
Our condolences to all.
SOM Faculty Awards
Congratulations to all School of Medicine 2024 Faculty Award winners – but especially to our wonderful cardiovascular faculty and colleagues:
- Adrian Hernandez, MD, professor of medicine in cardiology received an Excellence in Professionalism Award
- Christopher Holley, MD, PhD, associate professor of medicine in cardiology received a Research Mentoring Award
- Anita Kelsey, MD, MBA, professor of medicine in cardiology received the Master Clinician/Teacher Award
- Neha Pagidipati, MD, MPH, associate professor of medicine in cardiology received a Research Mentoring Award
- Madhav Swaminathan, MBBS, professor of anesthesiology, cardiothoracic anesthesiology/ critical care, received the Master Clinician/Teacher Award
- Annemarie Thompson, MD, professor of anesthesiology, pediatric cardiothoracic anesthesiology, received a Leonard Palumbo Jr., MD Faculty Achievement Award
The awards were presented on Monday, May 13 during the 2024 Spring Faculty Celebration held at the Doris Duke Center, Sarah Duke Gardens.
Congratulations and well-deserved!
DCRI Fellowship Graduation Celebrated
Graduating DCRI Fellows were celebrated at the University Club in Durham on May 9.

We are thrilled to share the following award winners who were recognized during the celebration:


Ilia Shadrin, MD, PhD, (cardiology) was awarded the DCRI Fellowship Citizenship Award, designed to recognize a graduating DCRI research fellow. Fellows considered for this award are expected to have demonstrated the following key attributes during their DCRI tenure: possesses strong character and leadership, devoted service to the DCRI, accepts responsibility and duties, has a positive attitude towards peers, the DCRI and the medical community, eager to learn and to teach others, and shows care and concern for others and helps them when needed.
Adam DeVore, MD, was recognized with the Robert M. Califf Award for Outstanding Mentorship, designed to recognize a DCRI faculty member who has demonstrated excellence in mentorship activities for DCRI research fellows. Faculty members considered for this award are expected to have mentored fellows at the DCRI and to have demonstrated enthusiasm and commitment towards the training of fellows in clinical research activities.
Congratulations Ilia and Adam!
Sullivan Honored with Teaching Award
 Congratulations to cardiology fellow Lonnie Sullivan, MD! He was selected as this year’s recipient of the Fellowship Teaching Award by the Internal Medicine residents.
Congratulations to cardiology fellow Lonnie Sullivan, MD! He was selected as this year’s recipient of the Fellowship Teaching Award by the Internal Medicine residents.
Way to go, Lonnie!
DHIP Update: Changes to Telehealth Video Visits and G2211 Code
Since the pandemic began, Duke Health has been able to convert all necessary patients to telehealth visits in an efficient manner, despite many changes. Now, since most of our services are video visits where standard E&M codes are used, we have decided to align our approach and use the level of service (LOS) menu.
Two Important Changes Coming to Telehealth (Video) Visits and for the G2211 Code
- Adding back the Level of Service (LOS) Menu to video visits
- Changes to G2211 Reminders: Reminders now in video visits and reminders now for all payers
Beginning May 14, the Level of Service (LOS) menu will be added back to the video visit encounters. As a result of this implementation, all E & M codes found in LOS will be removed from charge capture to prevent duplicate billing, and encounters created on the fly will still have the same charge capture (and no LOS) that exists today.
Moreover, because G2211 code is being recognized for payment by Medicare, Medicare advantage, UHC, and a few small others, and Medicaid is asking to submit this data for future consideration, there will now be G2211 reminders in all telehealth visits and visits for all payer types.
For more information on these changes, please visit the Changes to Telehealth Video Visits and G2211 Code page.
Thank you for your continued support and hard work!
Upcoming Events & Opportunities
- May is American Stroke Month and Asian American and Pacific Islander Heritage Month
- May is Duke Health’s inaugural Team Member Appreciation Month
- National Hospital Week ends today.
- Save the Date: June 12, 4-5 p.m., State of the School Address (SOM)
Cardiology Grand Rounds
May 21: Capturing the Left Bundle: Insights Into Conduction System Pacing with Ilia Shadrin. 5 p.m., DN 2002 or via Zoom.
May 28: The Ross Operation — The Ultimate Aortic Valve Replacement? with Ziv Beckerman. 5 p.m., DN2002 or via Zoom.
All Duke Cardiology Grand Rounds recordings are housed on Warpwire. To access recordings please visit:
NET ID and password required. Enjoy!
CD Fellows Core Curriculum Conference
May 22: EP Case Conference with Sara Coles and Ivan Nenadic Wood. Noon, DMP 2W96 (in-person only).
May 24: Coronary Anatomy & Lesion Interpretation with Tom Bashore. Noon, Zoom only.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
May 10 — Monique Starks/DCRI
WRAL
Forsyth County demonstrates how drones can deliver AEDs to heart attack victims sooner
May 13 — Senthil Selvaraj
Inside Precision Medicine
Genetic Variant Linked to Cardiovascular Disease and Death in Black Americans
May 13 — Senthil Selvaraj
WBZ Newsradio 1030 (Boston)
Study finds clue to greater heart disease in Black Americans
May 13 — Duke University (Selvaraj)
WBZ News/CBS Boston
Researchers find gene that may put Black Americans at higher risk for heart failure
May 13 — Senthil Selvaraj
STAT News
May 13 — Duke Heart for Honduras
El Heraldo (Honduras/Hn)
May 14 — Duke Health (Selvaraj)
San Diego Voice & Viewpoint
May 14 — Duke Health (Selvaraj)
Health Management
Genetic Variant Among Blacks Contributes to Cardiovascular Disease Burden
May 15 — Duke Heart for Honduras
LaPrensa (Hn)
Grupo Financiero Atlántida hace millonario donativo a brigada médica que tranformará vidas
May 15 — Duke Heart for Honduras
El Heraldo (Hn)
Hospital María y Duke University realizan brigada de cirugía cardiovascular a pacientes pediátricos
May 15 — Duke Heart for Honduras
La Tribuna (Hn)
Destacado cirujano hondureño opera junto a brigada de EEUU en el Hospital María
May 15 — Duke Heart for Honduras
Proceso Digital (Hn)
Con apoyo de Ficohsa Seguros se realiza segunda Brigada Médica Pediátrica de Duke Heart
May 16 — Duke Heart for Honduras
El Pais (Hn)
Grupo Financiero Atlántida dona L 5.7 millones para brigada médica
May 16 — Monique Starks
The Clemmons Courier
History in the making: First drone delivery of an AED
May 17 — Senthil Selvaraj
HealthDay
Male, Female V1421 Carriers Face Similar Risk for Heart Failure Hospitalization
Duke Heart Pulse — May 12, 2024
Chief’s message:
Hope you all have a happy Mother’s Day, and for those of you having kids graduate from college and or graduate school this weekend – congratulations.
This week’s Pulse highlights several of the things that make Duke a special place to work. Stories include teams developing breakthrough research findings (Senthil Selvaraj and others), innovative NHLBI funded research (Monique Starks and team with drone delivery AEDs for cardiac arrest survival), AHA go red for women with Camille Frazier-Mills as a woman of impact, and finally shout outs to clinical research coordinator Kim Biever and Cathy Ritchie from our cardiac rehab team on helping increase access to care.
Highlights of the week:
ESC-HF: Common Genetic Variant Among Black Americans Leads to Significant Increases in HF, Death at Individual and Population Levels
A genetic variant carried by 3-4 percent of self-identified Black Americans increases the risk for heart failure and death similarly in men and women, contributing to a significant decrease in longevity at the population level, according to a new study led by researchers at Duke University School of Medicine and Brigham and Women’s Hospital. The findings show that individuals who carry the amyloidogenic V142I transthyretin variant are at significantly increased risk for heart failure hospitalization beginning in their 60s, with an increased risk for death beginning in their 70s. Nearly half a million currently living carriers above age 50 will collectively lose 1 million years of life due to the variant.

The study results were presented earlier today by Senthil Selvaraj, MD, MS, MA, advanced heart failure cardiologist at Duke, as part of late-breaking science at the European Society of Cardiology’s Heart Failure Congress 2024 in Lisbon, Portugal; the findings were simultaneously published online in JAMA. Additional Duke authors on the publication include Svati H. Shah, MD, MHS; Robert J. Mentz, MD; and Michel G. Khouri, MD.
The V142I variant causes transthyretin, a protein in the blood, to misfold leading to deposits of abnormal amyloid protein in the heart and other parts of the body. In the heart, these deposits cause the muscle to become thick and stiffened, a condition known as cardiac amyloidosis, which can ultimately lead to heart failure. Originally considered a rare condition, researchers are increasingly finding that cardiac amyloidosis is underdiagnosed and underrecognized — particularly among Blacks.
The researchers pooled data from self-reported Black participants in four NIH-funded studies in the U.S. (ARIC, MESA, REGARDS and Women’s Health Initiative). Altogether, the team examined data from 23,338 self-reported Black individuals, 754 (3.23 percent) of whom carried the V142I genetic variant.
The team found that carriers of V142I had an increase in their 10-year risk for heart failure (HF) hospitalization by age 63 and risk for death by age 72, while individual carriers with the V142I variant live 2-2.5 years less on average than expected. The risk was more prominent for heart failure with reduced ejection fraction (HFrEF) hospitalization compared with heart failure with preserved ejection fraction (HFpEF) hospitalization. The variant’s contribution to HF risk increased substantially with age but was not itself increased by other known risk factors such as diabetes and hypertension.
“Since 3-4 percent of self-identified Black individuals in the United States carry this variant, a significant number are at elevated risk for developing cardiac amyloidosis, being hospitalized for heart failure, and dying several years earlier than expected,” said Selvaraj, first author of the study. “With our improved understanding of the risks with the variant, future efforts to increase disease awareness and ultimately connect carriers with the disease to effective therapies will be important.”
The team also showed that female and male carriers of the variant were equally at risk, contrary to some previous clinical studies showing that men were more affected. Using these epidemiological data, this suggests that women are likely underdiagnosed with the condition.
The research showed that variant carriers on average died 2 to 2.5 years earlier than non-carriers. With approximately 48 million Americans self-identifying as Black, approximately 1.5 million people are estimated to carry the variant. Of those over age 50, which is about half a million people, the team estimates that nearly a million years of life will be lost due to the variant in this natural history study.
Although the association between the V142I variant and HF has been previously described, precise estimates of how the variant increases risk were unclear until now. The good news is the increasing availability of treatment options for cardiac amyloidosis.
“There is currently one approved targeted therapy with a number in the pipeline,” says Selvaraj, adding that he and his colleagues believe earlier identification of people who carry the V142I variant and providing appropriate therapies might decrease the risk of HF and dying. However, more research is needed to show whether early implementation of targeted treatments actually leads to decreased risk of disease.
“We found a relatively large magnitude of disease burden in the U.S., certainly at the population level, but the impact at the individual level is notable as well,” he says. “It’s important to think about diagnosing this disease relatively early on, since once it evolves to later stages, it becomes more challenging to treat and therapies may be less effective. Further, as you get older, the risk of the disease increases substantially. Therefore, we should be considering the diagnosis of this inherited form of cardiac amyloidosis earlier than we have before – closer to early 60s, rather than their 70s and 80s.”
The findings also indicate clinicians should think more broadly about those who are hospitalized with HF as perhaps having amyloid.
“Amyloid cardiomyopathy is more often associated with HFpEF. Our findings demonstrate that, in hospitalized settings, we should be looking at individuals regardless of ejection fraction,” Selvaraj added. “Since hospitalization for HF is an advanced marker of the disease, and the ejection fraction tends to fall over time with cardiac amyloid, it may be unsurprising that more frequently carriers have a reduced ejection fraction by the time they are hospitalized.
“Additionally, we should pay more attention to this disease risk in women. One challenge with cardiac amyloid is we often look for thick walls in the heart. Women in general have thinner walls than men, so using certain thresholds of wall thickness to diagnose disease, without this consideration, may cause us to overlook women who indeed have the cardiac amyloid.”
In future studies, the researchers plan to investigate why some, but not all, carriers of the V142I variant develop cardiac amyloidosis.
Note: This paper has been selected by JAMA as their featured article of the week and is accompanied by two editorials: Heart Failure in African American Individuals, Version 2.0 by Clyde W. Yancy, MD, MSc; and Addressing Health Disparities—The Case for Variant Transthyretin Cardiac Amyloidosis Grows Stronger by Mathew S. Maurer, MD; Edward J. Miller, MD, PhD, and Frederick L. Ruberg, MD.
Duke Heart Team Heads to Honduras for Medical Mission
A 42-member medical team representing Duke Heart departed yesterday, May 11, on a surgical mission trip to Honduras as part of our Duke Heart in Honduras program. This year we have adult and pediatric teams heading to care for patients in need of cardiothoracic interventions. Our teams will perform all intraoperative and postoperative care to support our Honduran partners in providing surgery at no cost to patients who would otherwise not be able to afford it.
Forty surgeries are planned, 15 of which will be with pediatric patients in need of atrial septal defect closures, ventricular septal defect closures, AV canal defects, and Tetralogy of Fallot. Most adult patients our Duke team will see need aortic valve and mitral valve replacement. One congenital patient with an anomalous left coronary artery from the pulmonary artery (ALCAPA) defect will undergo reimplantation. Another will be treated for a large atrial myxoma.
The mission is in partnership with Hugo Orellana, MD, an adult cardiothoracic surgeon based at Honduras Medical Center, and with Victor Paz, MD, a pediatric cardiothoracic surgeon based at Hospital Maria. Both hospitals are located in the city of Tegucigalpa, the capital of Honduras.
The Duke Heart for Honduras 2024 team includes:
Cardiothoracic surgeons: Drs. Adam Williams, Jacob Schroder, Joseph Turek, and Doug Overbey; Cardiac anesthesiologists: Drs. Brandi Bottiger, Alina Nicoara, and Natalia Diaz-Rodriguez; Pediatric cardiac ICU attendings: Drs. Jennifer Turi and Jennifer Sherwin; CT fellows: Drs. Alejandro Murillo, Navin Vigneshwar, Jason Pang, Kathryn Pearson, and Ethan Garrigan; pediatric cardiac anesthesiologist Dr. Michael Greenberg; CT Surgery residents: Drs. Rebekah Boyd and Hiba Ghandour; CTICU, CTOR and critical care nurses and APPs: Bryan Hampton, Adeline Kranzburg, Timothy Matusz, Eric Velasquez, Chelsey Weinbrecht, Nicole Garcia, Cheyenne English, Mambo Kwaambwa, Michelle Figuerres, Figz Figuerrez, Tina McEachin, Aireen Vergara Casale, Audrey Sakae, Dorothy McVay and Danielle Wood; Perfusionists: Felicia Shugars, Amy Evans, Robert Degiosio, Katharine Nanry and Julie Walker; Respiratory therapist Chris Lappe; Biomedical engineer Brian Gore; Research lab member (and Honduran physician) Alejandro Alvarez Lobo, and medical students Cathlyn Medina and Lauren Parker.
Our Duke team will be joined by five medical professionals from Massachusetts General Hospital, including four attending physicians, Drs. Eriberto Michel, David D’Alessandro, Peter O’Chieng, and Robin Schiller and perfusionist Kenneth Shann. Also joining our team is a perfusion student, Cristina Parra, sponsored by the International Perfusion Association (IPA), and Bryan Lich, president of the IPA.
The team is supported, in part, by a grant from the Thoracic Surgery Foundation, the philanthropic arm of the Society of Thoracic Surgeons (STS). The grant funding of $35,000 is part of the Every Heartbeat Matters Award given to Dr. Adam Williams during the STS 60th annual meeting held in January 2024. The funding was made possible through the support of the Edwards Lifesciences Foundation and will be used to cover the airfare costs for all team members.
We are pleased to support these Duke team members and wish them great success!
Forsyth County NC Runs 1st Test of AED Drone Delivery
 Congratulations to Monique Starks, MD, associate professor of medicine in cardiology, and her AED Drone study team! Forsyth County, NC was the first county to sign on for the partnership with Duke for feasibility testing of AED drone delivery to cardiac arrest bystanders. The Forsyth County Sheriff’s Office and Forsyth County Emergency Services conducted a test launch this week as part of an emergency management drill for cardiac arrest held at Agape Church in Clemmons, NC.
Congratulations to Monique Starks, MD, associate professor of medicine in cardiology, and her AED Drone study team! Forsyth County, NC was the first county to sign on for the partnership with Duke for feasibility testing of AED drone delivery to cardiac arrest bystanders. The Forsyth County Sheriff’s Office and Forsyth County Emergency Services conducted a test launch this week as part of an emergency management drill for cardiac arrest held at Agape Church in Clemmons, NC.
Starks is the principal investigator on the American Heart Association research grant “Developing and Testing Drone-Delivered AEDs for Cardiac Arrest in Rural America”. Her co-investigators include Dan Mark, MD, Hayden Bosworth, PhD, Audrey Blewer, PhD, MPH, and Hussein Al-Khalidi, PhD.
Starks is the first investigator in the U.S. to be funded by the National Institutes of Health to explore the development of a drone network that is capable of delivering AEDs to bystanders at an out-of-hospital cardiac arrest emergency.
Congratulations to all involved in this important work!
Frazier-Mills Celebrated at Go Red! Event
The Triangle’s annual Go Red for Women Evening in Red event was held on Friday evening, May 10, at the Raleigh Convention Center. The celebration
celebration  recognizes survivors of heart disease and their family members and, via fundraising, supports vital research efforts for the American Heart Association.
recognizes survivors of heart disease and their family members and, via fundraising, supports vital research efforts for the American Heart Association.
The evening included dinner, dancing, a silent auction, and honoring each of the 2024 Triangle Women of Impact including our very own Camille Frazier-Mills, one of the finalists! Duke Heart’s service line vice-president Jill Engel and cardiology fellowship program director, Anna Lisa Chamis, MD were both on hand for the festivities and to support Camille.
Kudos to Ritchey & Cardiac Rehab Team!
Kudos to Cathy Ritchey for her tenacious work on behalf of our cardiac rehab patients. Ritchey proactively connected with representatives at Aetna regarding Cardiac Rehab (CR) coverage. Thanks to her efforts, Aetna has updated its CR coverage and will now cover the CPT code for non-continuous telemetry CR starting June 9. Awesome!!!
According to Erica Rao, this has been a barrier to enrolling Aetna patients into our Duke CR program. Ritchey, she says, “maintains a close watch on CR insurance guidelines and read that Aetna was updated theirs. After connecting to the Duke physician liaison with Aetna and the Revenue Integrity team, our team will now be able to enroll all Aetna patients, not just those with Duke Aetna insurance.”
Bill Kraus adds, “This is a huge well-earned victory for our CR program and the hospital to tear down barriers to patient care.”
Way to go, Cathy!!!
Shout-out to Biever
We received a terrific note this past week from Andrew Wang, MD, vice chief for clinical affairs for the division of cardiology:
“I highly commend Kim Biever, a clinical research coordinator in our cardiology clinical trials group. I have worked with her for the past 3-4 years on a randomized trial of mavacamten for obstructive hypertrophic cardiomyopathy (HCM) and its long-term extension study. In addition to her help in achieving a high enrollment in this study, her conscientiousness, efficiency, and communication have made the experience very productive and enjoyable.
“She is extremely well-organized and plans well for the expected and unexpected issues in a trial. She is often the “first call” person for our trial patients, even for matters unrelated to the study protocol, and manages these with compassion and professionalism. Most impressively, as our patients have transitioned from study treatment to commercial drug treatment, her dedicated work and commitment have helped to reduce any gaps in their treatment.”
Way to go, Kim!!!
Kudos to Duke HF Symposium Planning Team
A shout-out to Marat Fudim, Stephanie Barnes, Rob Mentz, Richa Agarwal, and Christy Darnell for a very successful HF Symposium last weekend. It was our first since the pandemic and it was a hit – our best turnout yet. Great job, everyone!
Upcoming Events & Opportunities
- May is American Stroke Month and Asian American and Pacific Islander Heritage Month
- May is Duke Health’s inaugural Team Member Appreciation Month
- May 12-19 is National Hospital Week
- Culture Pulse survey deadline extended to Thursday, May 16.
Cardiology Grand Rounds
May 14: Teaching, Quality Improvement, and Wellness in the ICU with Daniel Loriaux. 5 p.m., DN 2002 or via Zoom.
May 21: Capturing the Left Bundle: Insights Into Conduction System Pacing with Ilia Shadrin. 5 p.m., DN 2002 or via Zoom.
May 28: The Ross Operation — The Ultimate Aortic Valve Replacement? with Ziv Beckerman. 5 p.m., DN2002 or via Zoom.
All Duke Cardiology Grand Rounds recordings are housed on Warpwire. To access recordings please visit:
NET ID and password are required. Enjoy!
CD Fellows Core Curriculum Conference
May 15: HF/Txp Case Presentation with DaMarcus Ingram. Noon, DMP 2W96 (in-person only).
May 17: EKG Review with Neil Freedman. Noon, Zoom only.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, on Wednesdays, will be considered for weekend inclusion.
Duke Heart in the News:
May 2 — Neha Pagidipati
Cardio Nerds
May 3 — Marat Fudim
Web MD
What’s Behind Major Rise in Heart Failure Deaths?
May 3 — Duke University Hospital
Becker’s ASC Review
Meet the leaders of the 3 best hospitals in North Carolina for cardiac surgery
May 3 — Thomas Povsic
Medscape
In Angina, Gene Therapy Coaxes Heart Vessel Growth
May 3 — Duke Raleigh, Duke University Hospitals
Healthgrades
Healthgrades Reveals Top U.S. Hospitals for Patient Safety in 2024
May 4 — Nina Nouhravesh
The National Herald (Greece)/Associated Press
Eggs Regain Their Place as a Staple of Healthy Eating
May 6 — Harry Severance
MedCity News
Stark Law Crackdown Jacks Up Fines, Settlements and Physician Pressures
May 7 — Stephen Greene
tctMD
SGLT2 Inhibitor Added to GDMT in Functional MR May Obviate Need for TEER
May 8 — Jonathan Piccini
Verywell Health
Why Is AFib More Common in Younger Adults Now?
May 8 — Monique Starks
WFMY (CBS 2)
AED taking flight, Forsyth County leads U.S. with drone delivery program
May 9 — Duke University and Monique Starks
WGHP (Fox 8) Greensboro, NC
Area sheriff’s department (Forsyth County) adds drone delivery AEDs
May 9 — Dawn Coleman
Vascular Specialist
The top 10 most popular Vascular Specialist stories of April 2024
Duke Heart Pulse — May 5, 2024
Duke Heart Pulse – May 5, 2024
Chief’s message:
As the spring season is in full effect – hopefully you all had some time outside with friends and family. There were also many faculty and fellows presenting at conferences this weekend – the national cardiovascular interventional society (SCAI) had its national meeting in California this weekend with several of our interventional faculty both presenting and being part of the national organizations leadership. There were key talks by Jennifer Rymer, Raj Swaminathan, Ton Gutierrez, Schuyler Jones and many others. Congratulations to Sunil Rao, past SCAI president and James Hermiller – in coming SCAI president.
Heart Failure Symposium is back. This weekend the Duke Heart group had its first Heart Failure symposium after COVID (prior in-person symposium was 2019). By all accounts it was a success – with over 220 registered attendees, wonderful speakers from around the country, and lots of interactive real-world management of heart failure patients from prevention to complex management. Some photos from the event are shown here.






Highlights of the week:
Celebrating Perfusionists & Duke’s 2nd Pillar Award
Happy May, everyone! Yes, today is the ever-popular Cinco de Mayo, but it’s also day one of Perfusion Week — a time to recognize the incredible efforts of perfusionists across the U.S.! These vital members of our cardiothoracic surgical team do remarkable things each day for our patients. So, if you happen to be celebrating with your favorite Mexican foods and beverages, consider including a toast to our amazing Duke Perfusionists!

The Duke Perfusion team recently earned its second Pillar Award for Perfusion Excellence from the American Society of Extracorporeal Technology (AmSECT). Their first was awarded in 2021, the inaugural year of the AmSECT Pillar, which is a designation for individual perfusion departments that demonstrate excellence as displayed in several key areas including organized orientation and training, QA/QI process, continuing education and performance evaluation, development of institutional protocols and adherence to AmSECT Standards and Guidelines, employee education and commitment to the field of perfusion.
Duke has one of the largest and most highly-skilled perfusion teams in the U.S. Each member of the team is certified by the American Board of Cardiovascular Perfusion, licensed by the North Carolina Medical Board, and most team members hold advanced degrees and credentials.
In addition to proficiency in cardiopulmonary bypass (operating the heart-lung machine during cardiothoracic surgery), Duke perfusionists become further specialized to support a variety of needs across the hospital. We have a dedicated team of pediatric perfusionists, a specialty team for Duke Regional Hospital, an Extra-Corporeal Life Support (ECLS) team that assists with cannulating and retrieving patients from referring hospitals, a team that provides apheresis in the OR, and a team trained in use of the Transmedics Organ Care System, which has helped increase the donor pool for Duke’s Heart Transplant program.
Congratulations to our perfusionists!
Nurses Week 2024
 It’s also Nurses Week 2024 (May 6-12)! On behalf of Duke Heart, a big shout-out to all of our incredible nurses for their professional accomplishments and contributions in caring for Duke Heart patients over the past year.
It’s also Nurses Week 2024 (May 6-12)! On behalf of Duke Heart, a big shout-out to all of our incredible nurses for their professional accomplishments and contributions in caring for Duke Heart patients over the past year.
Duke Heart Nurses are foundational to Duke’s ability to provide compassionate, innovative cardiac care throughout our clinics and at the bedside. Each of our nurses cares for patients with complex cardiovascular needs and partners with clinicians and other team members as we engage in research clinical trials; teach patients and family members about the care they are receiving; participate in quality improvement initiatives locally and nationally, as well as speak or serve as educators at professional meetings.
Our Duke Heart nurses are amazing – individually and as a team. Without their partnership, none of our overall team accomplishments would be possible! Thank you for the work you do, your tremendous compassion for our patients and their families, and your compassion for one another and our community.
The Duke Heart Nursing team possesses unmatched talent, dedication, and teamwork, exemplifying living the Duke Values. In short, Duke Nurses rock!
Kudos and thank you – enjoy Nurses Week!
Duke Heart Experts Featured at NCUS
The North Carolina Ultrasound Society (NCUS) held its 43rd Annual NC Medical Ultrasound Symposium in Raleigh from April 19-21 at the Crabtree Courtyard Marriott.
Duke Heart was well-represented in terms of presenter expertise and well-supported in terms of attendees. Speakers included Joe Kisslo, MD (Keynote speaker); Michel Khouri, MD; Richie Palma, instructor and program director of Duke’s Cardiac Ultrasound Program; Alicia Armour, HCA of Triangle Heart; Ashlee Davis, chief technologist, and Rachel O’Brien and Diana Masterson, cardiac sonographers.



Richie Palma and cardiac sonographer Jon Owensby are both on the Board of Directors for the NCUS.
Great work, everyone!
Pending Unit Moves – July 2024
The Duke University Hospital 100 bed tower, floors 6 through 9, has been renovated and will reopen in the summer of 2024! Several Heart patient care units will be relocated to allow for the renovation of floors 2 and 3 in the North 100 tower. Unit 3100 will relocate to 6100 (31-bed unit) on July 22 and 3200/7200 will relocate back to 7100 (31-bed unit) on July 23.
There will be no change in the patient populations these units care for. Unit 6100 was specifically chosen because of its proximity to the 6E/CT Step-down Unit.
More details, including office relocations, will be announced closer to the move date. We thank everyone in advance for their support and patience.
Final Week to Complete Culture Pulse Survey
If you have not yet done so — please participate in the Duke Health Culture Pulse survey. It is available to all Duke Health team members until May 13. The brief, 18-question survey is confidential and mobile-friendly, and it’s short – you can do the whole thing in less than five minutes.
This year’s survey is focused on Duke’s commitment to putting people first by asking questions, listening, and seeking diverse perspectives. The Culture Pulse survey aims to strengthen the employee experience – for all of us – but participation is critical!
Thank you for sharing your invaluable insights and for all that you do to make Duke Health an extraordinary place to work, learn, and receive care.
The link to the survey was sent to everyone via email on 4/22. Check your inbox and please make your voice heard!
Duke Hospitals Continue to Earn ‘A’ Grades on Leapfrog Safety Assessments
For 12 consecutive grading periods, Duke University Hospital, Duke Regional Hospital, and Duke Raleigh Hospital received top scores for patient safety from The Leapfrog Group.
The “A” scores for Leapfrog’s spring 2024 survey are part of the group’s Hospital Safety Grades Assessment, issued to hospitals every six months. This is the only hospital ratings program focused exclusively on preventable medical errors, infections, and injuries that kill more than 500 patients a day nationally.
Duke Health’s three hospitals were among nearly 3,000 hospitals surveyed across the country. Only 29% of hospitals nationwide achieved an “A” hospital safety grade for the spring 2024. In North Carolina, Duke University Health System hospitals were among 38 hospitals to achieve the grade.
“Our steady ‘A’ grades from Leapfrog prove that we are dedicated to putting patients first at all three Duke Health hospitals,” said Thomas Owens, MD, executive vice president and chief operating officer of Duke University Health System. “We value the clinicians, staff, and volunteers who provide excellent care and make sure patients are safe.”
The Leapfrog Group is an independent nonprofit organization led by the nation’s leading employers and private healthcare experts. Twice each year, it collects and analyzes data based on over 30 national performance measures of errors, accidents, injuries, and infections, as well as systems hospitals have in place to prevent harm. The letter grades assigned to hospitals help people make informed decisions to protect themselves and their families.
Comparisons of hospital scores locally and nationally are available at https://www.hospitalsafetygrade.org/.
Duke’s Total Compensation Program
Duke began mailing all full-time faculty and staff their annual personalized benefits statements this week. These are going to home addresses.
Did you know that, on average, Duke invests about $250 in benefits for every $1000 of pay? Each of us can see what Duke’s investment in pay and benefits looks like for us by reviewing our benefits statement. Please take a few minutes to review the materials to ensure you’re taking full advantage of the benefits and services available to you and your family members.
Learn how five of our Duke colleagues have been helped by a variety of Duke benefits as part of their total compensation package: Beyond Pay: Unique Duke Employee Benefits for Unique Needs.
Have a great week, everyone!
Upcoming Events & Opportunities
- Culture Pulse 2024 survey period through May 13
- May is Asian American and Pacific Islander Heritage Month

- May is Duke Health’s inaugural Team Member Appreciation Month
- May 5-11 is Perfusion Week
- May 6-12 is Nurses Week
- May 12-19 is National Hospital Week
Cardiology Grand Rounds
May 7: Bridging the Gap: A Closer Look at Care Fragmentation and Health Disparities in PAD with Dennis Narcisse. 5 p.m., DN 2002 or via Zoom.
All Duke Cardiology Grand Rounds recordings are housed on Warpwire. To access recordings please visit:
NET ID and password are required. Enjoy!
CD Fellows Core Curriculum Conference
May 8: ABIM Review. Noon, DMP 2W96 (in-person only).
May 10: Update on TAVR with Todd Kiefer. Noon, Zoom only.
Working Effectively Across Generations
June 3: Working Effectively Across Generations with Hile Rutledge, of Otto Kroeger Associates (OKA). 8:30 a.m. to Noon. Great Hall, Trent Semans Center. Sponsored by Duke School of Medicine.
Registration required: https://medschool.duke.edu/blog/register-now-working-effectively-across-generations
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
April 25 — Jonathan Piccini
Health Central
How Cardioversion Can Help Your Heart
April 26 — Marat Fudim
tctMD
Heart Failure Mortality Higher Now Than in 1999
May 1 — James Watson (hospitalist program)
The Hospitalist
Apixaban Reduces Risk of Stroke or Systemic Embolism in Subclinical AF
May 1 — Cepeda Mora (hospitalist program)
The Hospitalist
Semaglutide in Patients with HFpEF and Obesity
May 1 — James Watson
The Hospitalist
High Frequency of AF Recurrence in Hospitalized Patients with New-onset AF
May 1 — Mark Chandler (hospitalist program)
The Hospitalist
Frailty Assessment and Perioperative Adverse Cardiovascular Events After Noncardiac Surgery
May 1 — Chantell Evans (cell biology)
Nature/News & Views
Cells destroy donated mitochondria to build blood vessels
May 1 — Amanda Randles (biomedical sciences)
Business Insider
May 1 — Duke Health
WNCN/CBS-17 (Raleigh/Durham)
Raleigh/Cary metro has some of the safest hospitals in the country: New study
May 3 — Robert Mentz
Perishable News
Duke Heart Pulse — April 28, 2024
Duke Heart Pulse – April 28, 2024
School of Medicine Spring Faculty Celebration – May 13th:
Each year we have a Spring Faculty Celebration hosted by the School of Medicine at the Doris Duke Center in the Duke Gardens. This year the celebration is May 13th from 5:00 – 7:30 pm to recognize newly tenured faculty and professors, and winners of the school of medicine awards. We are blessed to have such great faculty in Duke Heart – and again this year we had several internal and external nominations for awards. The Nominees and award winners are presented below. Please join us this year if you can to celebrate our Cardiovascular group and all of the cardiology, cardio-thoracic, vascular, and anesthesia faculty that work to ensure we deliver the highest quality of care to our patients and mentor and train the next generation. Please join us this year if you can. If you have not already RSVP’d, the invitation link is here: the invite.

Surgical Scrubs Policy Reinforcement
A key finding from a recent Joint Commission Mock Survey conducted by DUH Perioperative Services was the observation of multidisciplinary clinical team members wearing designated OR scrubs to and from the hospital.
The finding falls under standard IC.02.01.01, EP1, Infection Prevention and Control. Wearing designated surgical scrubs into the community, home & back, does not align with policy DUHS Guidelines for Surgical Attire Policy #7429.
The recommendation from the Joint Commission is for DUH to meet the required standards and maintain compliance with the system policy. The attached policy is being shared with all faculty/clinical team members who spend time in the OR as a reminder to change into and out of designated surgical scrubs upon arriving and once they are done in the OR for the day.

Perioperative leadership will reinforce this policy with the OR, SPD, and ancillary departments.
If you have any questions, please contact the DUH Perioperative Medical Director, Dr. Melissa Erickson, or the DUH Perioperative Anesthesia Medical Director, Dr. Dhanesh Gupta. Holly Garon, ACNO Perioperative Services, Tina Thomas, COD, and the OR Nurse Managers, are also available to answer questions or address concerns.
Thank you, in advance, for complying with this policy.

Andrea Knowles Joins Duke ECMO Team
 After an extensive search, Andrea Knowles, BS, RRT, CES-A, has been named ECMO Manager at Duke Hospital. Andrea will report to Desiree Bonadonna, chief of Perfusion Services and director of Extracorporeal Life Support. Knowles will support the ECMO Specialist Team.
After an extensive search, Andrea Knowles, BS, RRT, CES-A, has been named ECMO Manager at Duke Hospital. Andrea will report to Desiree Bonadonna, chief of Perfusion Services and director of Extracorporeal Life Support. Knowles will support the ECMO Specialist Team.
Andrea comes to Duke with fifteen years of ECMO experience, most recently as the ECMO Coordinator for Loyola University Medical Center. She will be orienting to Duke over the coming weeks and will begin managing the ECMO Specialist Team in July.
Please join us in welcoming Andrea to Duke!
Please Complete the DUHS Culture Pulse Survey
A critical part of advancing Duke Health’s culture is checking the pulse of our organization to identify what we are doing well and where we have continued opportunities to learn and grow together.
The Duke Health Culture Pulse survey launched last week and is available to all team members until May 13. The brief, 18-question survey is confidential and mobile-friendly.
This year’s survey is focused on Duke’s commitment to putting people first by asking questions, listening, and seeking diverse perspectives. The Culture Pulse survey aims to strengthen the employee experience and will take you under five minutes to complete.
Please know that your responses are completely confidential. Thank you for sharing your invaluable insights and for everything you do every day to make Duke Health an extraordinary place to work, learn, and receive care.
The link to the survey has been sent to everyone via email. Check your inbox and please make your voice heard!
Duke Heart Volunteers Recognized

In celebration of Volunteer Appreciation Week, held April 21-27, volunteers from across Duke Health were celebrated at a special breakfast at Croasdaile Country Club in Durham on Thursday, April 25. Several Duke Heart volunteers attended, including three members of our Duke Heart Patient Family Advisory Council: Kathryn Dailey, our Heart PFAC co-chair, Bob Curlee, and Sue Ann Glower.
Our many volunteers enhance the Duke healthcare team by dedicating their time, skills, and compassion to improve patient experiences and community engagement on a local, national, and global scale. There are more than 30 volunteer programs available for community involvement throughout Duke Health System.
We appreciate the invaluable support and kindness that our volunteers bring to our patients, their families, visitors, and staff. Thank you to all volunteers throughout DUHS, and especially right here within our Duke Heart care spaces.

2024 NC Walk for Victory Held
The 2024 North Carolina Walk for Victory, held on April 20 at Laurel Hills Park in Raleigh was a big success in raising valuable funds to support research into Marfan Syndrome and related connective tissue disorders. More than 200 participants attended the event, sponsored by Duke Heart, and led by Chad Hughes, MD who served as the medical director for the event. Overall, $53,500 was raised by volunteer teams and family members.

Great job!
Upcoming Events & Opportunities
- Culture Pulse 2024 April 22-May 13
Cardiology Grand Rounds
April 30: TBD. 5 p.m., DN 2002 or via Zoom.
All Duke Cardiology Grand Rounds recordings are housed on Warpwire. To access recordings please visit:
NET ID and password required. Enjoy!
CD Fellows Core Curriculum Conference
May 1: DHP Case Presentation with Aubrie Carroll. Noon, DMP 2W96 (in-person only).
May 3: Adult Congenital Heart Disease with Richard Krasuski. Noon, Zoom only.
Upcoming CME Symposia
May 4: Duke Heart Failure Symposium
Please reach out to Christy Darnell with any questions.
Working Effectively Across Generations
June 3: Working Effectively Across Generations with Hile Rutledge, of Otto Kroeger Associates (OKA). 8:30 a.m. to Noon. Great Hall, Trent Semans Center. Sponsored by Duke School of Medicine.
Registration required: https://medschool.duke.edu/blog/register-now-working-effectively-across-generations
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
April 23 — Kimberly Ward (DCRI)
Winston-Salem Journal
Sheriff: Drones can help ‘change the atmosphere’ when it comes to cardiac arrest response
April 24 — Marat Fudim
STAT News
Decline in heart failure deaths has been undone, led by people under 45
April 24 — Harry Severance
Becker’s Hospital Review
How the FTC’s noncompete ban could change the physician workforce
April 23 — Project Baseline
tctMD
Duke Heart Pulse — April 21, 2024
Highlights of the week:
Rambarat Named Chief Cardiology Fellow, 2024-2025
 We are excited to share that our Duke cardiology fellows have elected Paula Rambarat, MD to serve as chief cardiology fellow for 2024-2025. Please join us in congratulating Dr. Rambarat and welcoming her to her new role!
We are excited to share that our Duke cardiology fellows have elected Paula Rambarat, MD to serve as chief cardiology fellow for 2024-2025. Please join us in congratulating Dr. Rambarat and welcoming her to her new role!
Rambarat was born and raised in Barbados. She moved to Chapel Hill, NC in her junior year of high school and graduated from East Chapel Hill High School. Then, she attended Duke University, where she majored in biology and minored in Spanish. Subsequently, she received her medical degree from Columbia University Vagelos College of Physicians and Surgeons. During medical school, she was awarded a Howard Hughes Medical Institute research fellowship and worked in the lab of Dr. Robert Lefkowitz here at Duke. Rambarat completed an Internal Medicine residency at Massachusetts General Hospital and returned to Duke for a Cardiovascular Disease fellowship. She is pursuing a Duke Clinical Research Institute fellowship followed by advanced training in heart failure and transplant cardiology. In her free time, she enjoys spending time with her family, hiking, running, and cooking.
Dr. Ramabarat will on-board with Dr. Lerman during May. She officially takes the role at the end of June.
Many thanks to Joseph Lerman, MD for the incredible job he has done serving as chief cardiology fellow this past year!
Congratulations, Paula!
ACC.24: Summary of Duke ACC Presentations
Faculty experts from across Duke Heart and the Duke Clinical Research Institute (DCRI) shared insights and expertise on the latest cardiology research as part of more than 100 late-breaking studies, Meet the Expert opportunities, presentations, panels, and posters during the 2024 American College of Cardiology (ACC) Scientific Sessions held April 6-8 in Atlanta.
Duke kicked off the conference with AEGIS-II and EMPACT-MI presented as part of the opening late-breaking research session. The two presentations culminated in six publications in major medical journals.
Therapy Shows Promise in Delaying Hospitalizations for HF: Results from EMPACT- MI
About 800,000 people in the U.S. suffer a heart attack every year, and approximately 30% of them will go on to develop heart failure. There are limited treatments to prevent or slow that development.
A large international study coordinated and conducted by the DCRI found that the diabetes drug empagliflozin (marketed under the brand name Jardiance) did not reduce deaths. Secondary findings show it did slow the time to first hospitalization for heart failure and reduced the total number of subsequent heart failure hospitalizations. The results from the EMPACT-MI trial were published simultaneously with the ACC presentation in the New England Journal of Medicine, Circulation, and the Journal of the American College of Cardiology. Details of the meta-analysis are in press in The Lancet Diabetes & Endocrinology. The study was led by Schuyler Jones, MD and Adrian Hernandez, MD from the Duke/DCRI.
The study findings on lower rates of heart failure offer some hope and underscore the importance of preventing poor outcomes after a heart attack, according to DCRI executive director and site principal investigator, Adrian Hernandez, MD, MHS.
“Developing heart failure is one of our major public health problems, and any step that gets us closer to preventing it is a step in the right direction,” Hernandez said. “After a heart attack, we should really be focused on how to prevent problems, especially the development of heart failure. This therapy fills in that gap.”
AEGIS-II Misses Primary Endpoint; Data Suggest Further Research into HDL Modification is Warranted
Primary results from the AEGIS-II trial showed that infusions of the human plasma-derived apolipoprotein A-I CSL112 did not significantly lower the risk of major adverse cardiac events through 90 days for people who had recently suffered a heart attack. However, exploratory analysis showed that patients who received the treatment had numerically lower rates of cardiovascular (CV) death and myocardial infarction (MI), type-1 MI, and stent thrombosis-related MI compared to placebo. Primary results were published in the New England Journal of Medicine and exploratory results were published in the Journal of the American College of Cardiology.
cardiac events through 90 days for people who had recently suffered a heart attack. However, exploratory analysis showed that patients who received the treatment had numerically lower rates of cardiovascular (CV) death and myocardial infarction (MI), type-1 MI, and stent thrombosis-related MI compared to placebo. Primary results were published in the New England Journal of Medicine and exploratory results were published in the Journal of the American College of Cardiology.
“It’s probably the most important trial looking at HDL modification or altering HDL efficacy in terms of limiting cardiovascular events,” said Thomas Povsic, MD, PhD, one of the study investigators and first author of the JACC paper. “I think there are signals that it did work, but the overall effects were relatively modest and what we showed is that on certain kinds of heart attacks, it does seem to prevent downstream cardiovascular events. That would need validation in a separate clinical trial.”
Also notable from AEGIS-II was the efficiency of the study’s operations. The AEGIS-II team enrolled more than 18,000 participants across 46 countries amid the COVID-19 pandemic, with only two lost to follow-up. The DCRI managed the study data and managed the 193 U.S. sites, which enrolled more than 1,800 high-risk acute MI patients, with none lost to follow-up.
“We have long-standing relationships with many of our sites in the U.S., so I think one of the things that we bring to the table is that we know a lot of sites that will enroll well and are high quality sites that will follow their patients,” Povsic said during a Meet the Expert event following the late-breaker session. “We have relationships with country leaders throughout the world. I was one of the country leaders in the U.S., and we had a lot of contact with our sites to make sure that they were following patients and doing all the other things that we talk about in clinical trials to make sure the trial is well run, and this trial was really well run.”
Pagidipati Provides Practical Tips for Harnessing the Power of Anti-Obesity Medications
 Anti-obesity medications squarely fit within a cardiologist’s scope of practice and should be used in combination with lifestyle changes, according to cardiologist Neha Pagidipati, MD, MPH, presenting during a Saturday afternoon ACC session.
Anti-obesity medications squarely fit within a cardiologist’s scope of practice and should be used in combination with lifestyle changes, according to cardiologist Neha Pagidipati, MD, MPH, presenting during a Saturday afternoon ACC session.
Referencing studies including STEP HFpEF, SELECT, STEP 1, STEP 4, SURMOUNT 1 and SURMOUNT 4, Pagidipati discussed the relevance and benefits of newer weight loss drugs such as semaglutide, liraglutide, and tirzepatide, and then outlined how she introduces patients to the medications and increases their dosing gradually.
“These therapies don’t just help patients lose weight, they are CV-risk reduction agents,” said Pagidipati, underscoring the relevance of the drugs for cardiologists. She also emphasized the need for lifestyle changes in concert with the medications.
“No amount of medicine is going to help a patient become healthier if they don’t understand what they’re supposed to be doing in their life in terms of exercise and diet,” she said. “All of these studies were predicated upon some lifestyle change happening for all of these patients.”
Pagidipati went on to share the three things she discusses with her patients to ensure the medications are most effective:
- Move more: “Whatever you’re doing, do more than what you’re doing.”
- How much you eat: “It helps if you eat less, for most of us, and these agents will help us do that.”
- What you eat: “In general, I recommend the Mediterranean diet, low salt, low carb, if they’re trying to lose weight, as well.”
- When starting patients on anti-obesity medications, a slow and gradually increasing approach is best.
“The key to remember is start low, go slow,” Pagidipati said. “Start at the lowest dose with patients, and I titrate every four weeks. I only titrate up to the next dose if and when their gastrointestinal symptoms have improved. If they’re queasy, have nausea, and you titrate up for them, it’s just going to get worse. Also, I tend to wait until their weight loss plateaus, and usually at four weeks it does.”
Keys to Improving Healthspan in Older Adults with Ischemic Heart Disease
During a session focused on improving healthspan in older adults with ischemic heart disease, Karen Alexander, MD, first sought to point out the elephant in the room: “everyone dies,” she said.
 “This is not a reason that we shouldn’t be working very hard to improve quality of life before death, but we need to be aware of that, because our patients are aware of that, and as we ask them to participate in research, I think that’s on their mind to a degree.”
“This is not a reason that we shouldn’t be working very hard to improve quality of life before death, but we need to be aware of that, because our patients are aware of that, and as we ask them to participate in research, I think that’s on their mind to a degree.”
In aiming to generate evidence among older adults, Alexander recommended:
- considering the uniqueness of the older population, and the underlying processes unique in that age group.
- appreciating and leveraging new ways of doing research that are virtual and aligned with care.
- thinking about the outcomes that matter to the patients.
Alexander highlighted the approach taken by the ongoing PREVENTABLE study, which is finding potential participants aged 75 and older using a cohort query applied to the electronic health record. Sites then approach patients and randomize them to atorvastatin 40 mg. or placebo. Participants are tracked to determine whether they meet the primary outcome which is one that matters to the patients — survival free of dementia and persisting disability.
Researchers have made participation easy by shipping the study drug directly to patient homes and enrolling about half of the population remotely.
“This can be done,” Alexander said. “We’re having a very simple intervention, which is the atorvastatin 40 mg. versus placebo — but you could imagine how this could be replicated based on our experience in other situations.”
Keeping in mind the participant population’s desire to try new interventions is key, Alexander concluded.
“As we’re beginning to think about these fancy new interventions, we have to stop ourselves and remember the population we’re asking to go on this journey and to be in the trial boat with us. From PREVENTABLE, the one thing we have learned is that older adults are in that phase where they really don’t want to rock the boat. This is an important thing to partner with our participants and make sure they’re interested in joining us.”
What’s Now, and What’s Next for Treating High Blood Pressure?
Nearly half of adults have hypertension or are taking medication to manage hypertension. Hypertension, also known as high blood pressure, is defined as systolic blood pressure greater than 130 mmHg or diastolic blood pressure greater than 80 mmHg.
pressure greater than 130 mmHg or diastolic blood pressure greater than 80 mmHg.
An ACC session focused on high blood pressure reviewed the issue and the forthcoming therapies that could help to better manage the condition.
Highlighting the SPRINT study — which showed a reduction in all-cause mortality, relative risk reduction in heart failure, and reduction in stroke — Duke cardiologist Chris Granger, MD, noted that it provides a helpful example of what can be done, while also showing the limitations.
After emphasizing the study’s impressive results, Granger discussed the aftermath.
“The long-term follow-up, after two or three years after the trial was finished, the blood pressure difference between the two groups had vanished, the benefit for mortality and CV mortality had vanished,” he said. “This is in a setting where people had done the trial, they knew the benefits, it was with the same patients who knew the benefits, so this shows us that our current systems are really a failure, even in optimal settings.”
For now, key strategies for treating hypertension he highlighted include:
- targeting blood pressure less than 130 mmHg systolic for patients with or high-risk for cardiovascular disease using combination drugs titrated monthly.
- home monitoring.
- ensuring patient access to advanced practice providers, pharmacists, and algorithms measuring and promoting medication adherence.
New possibilities on the horizon could improve treatment of hypertension, Granger added.
“New treatments, like zilebesiran, I think will provide important, perhaps transformational opportunities for treating high blood pressure, in this case through a potent, what appears to be safe based on preliminary data, and sustained inhibition of the renin-angiotensin system with a treatment given once every six months as a subcutaneous injection.” he said, adding that more trials are needed and ongoing to assess efficacy and safety.
TRANSFORM-HF Modified On-Treatment Analysis Supports Primary Results
 DCRI Fellow Mark Kittipibul, MD, shared results from a modified on-treatment analysis of the effects of torsemide vs. furosemide after discharge in patients hospitalized with heart failure from the TRANSFORM-HF trial.
DCRI Fellow Mark Kittipibul, MD, shared results from a modified on-treatment analysis of the effects of torsemide vs. furosemide after discharge in patients hospitalized with heart failure from the TRANSFORM-HF trial.
The analysis showed no significant difference in mortality between the on-treatment groups of the two diuretics at discharge or after one month.
“In this post-hoc on-treatment analysis of TRANSFORM-HF — inclusive of all randomized patients, unless they were confirmed to be non-adherent — there was no significant difference in outcomes between torsemide and furosemide,” said DCRI Fellow Mark Kittipibul at ACC reviewing the effects of the two diuretics in heart failure patients after hospital discharge. “These findings support the robustness of the primary trial results.”
Primary results from TRANSFORM-HF were first shared by Robert Mentz, MD, during a late-breaking science session at the 2022 American Heart Association Scientific Sessions.
New Study Shows Fortified Eggs did not Raise Cholesterol
A study led by Duke researchers offers new evidence on fortified eggs’ health effects. In a modest-sized randomized trial, researchers found that fortified eggs — meaning those enriched with various vitamins or nutrients — did not significantly impact bad cholesterol (LDL cholesterol) or good cholesterol (HDL cholesterol) over the course of the four-month study.
 A secondary finding hinted there could be some benefit associated with fortified egg consumption for older patients and patients with diabetes. The finding was not statistically significant due to the number of study participants, but senior researcher and heart failure cardiologist Robert Mentz, MD said it’s an interesting signal that the researchers would like to investigate in future work.
A secondary finding hinted there could be some benefit associated with fortified egg consumption for older patients and patients with diabetes. The finding was not statistically significant due to the number of study participants, but senior researcher and heart failure cardiologist Robert Mentz, MD said it’s an interesting signal that the researchers would like to investigate in future work.
The study’s first author and DCRI Fellow Nina Nouhravesh, MD said the study can be viewed as a pilot.
“While it was modest in size, it did include a broadly generalized population,” Nouhravesh said. “The average age of participants was 66 years, half were women, and more than 25% identified as Black.”
ICYMI: Bill Kraus MGR Presentation, April 19
If you were unable to attend Friday morning Medicine Grand Rounds, the presenter was Bill Kraus, MD on ‘A Detailed Analysis of Cardiac Rehabilitation on 180-day All-Cause Hospital Readmission and Mortality. You can view the recording here: https://duke.is/5/jjy3
Happy Birthday, Chris Granger!
 A belated Happy Birthday to Chris Granger, MD – his team members in the CICU helped celebrate his special day with him this past week. Happy Birthday, Chris!
A belated Happy Birthday to Chris Granger, MD – his team members in the CICU helped celebrate his special day with him this past week. Happy Birthday, Chris!
Culture Pulse Survey Launches This Week
The Duke Health Culture Pulse survey launches tomorrow, April 22, and is available to team members until May 13. The brief, 18-question survey is confidential and mobile-friendly. Visit the Culture Pulse 2024 page on DHN for a Zoom background, flyer, and more.
This year’s Culture Pulse will focus on our commitment to putting people first by asking questions, listening, and seeking diverse perspectives. The Culture Pulse survey aims to strengthen the employee experience and will take you under five minutes to complete.
The link to the survey will arrive via email tomorrow. Check your inbox!
Upcoming Events & Opportunities
- April is National Donate Life Month
- Annual reminder as part of Duke’s “check yourself” campaign: please make sure your contact information is up to date in Duke@Work
- Culture Pulse 2024 April 22-May 13
- Duke Farmers Market season opens this week! Starting April 25, the Farmers Market will be held every Thursday from 11 a.m. to 2 p.m. on the DMP Greenway.
Cardiology Grand Rounds
April 23: No CGR tonight. (Faculty Meeting, division of cardiology)
April 25: New Insight into the Physiology of Heart Failure with Preserved Ejection Fraction with Satyam (Tom) Sarma, MD of UT Southwestern. 5 p.m., DN 2002 or via Zoom. *Please note this is a Thursday evening presentation.
All Duke Cardiology Grand Rounds recordings are housed on Warpwire. To access recordings please visit:
NET ID and password required. Enjoy!
CD Fellows Core Curriculum Conference
April 24: EP Case Presentation with Aman Kansal and Eric Xie. Noon, DMP 2W96 (in-person only).
April 26: EKG Review with Tom Bashore. Noon, Zoom only.
Upcoming CME Symposia
May 4: Duke Heart Failure Symposium
Please reach out to Christy Darnell with any questions.
Working Effectively Across Generations
June 3: Working Effectively Across Generations with Hile Rutledge, of Otto Kroeger Associates (OKA). 8:30 a.m. to Noon. Great Hall, Trent Semans Center. Sponsored by Duke School of Medicine.
Registration required: https://medschool.duke.edu/blog/register-now-working-effectively-across-generations
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
April 12 — Pamela Douglas
Healio
Pamela S. Douglas, MD, highlights need for diversity in clinical trials leadership
April 12 — Neha Pagidipati
tctMD
Triglyceride-Lowering Therapies Provide Favorable Outcomes in Early Testing
April 16 — Charlotte Reikofski
AARC
Want to Work with Kids? Here’s What You Need to Know First!
April 16 — Jennifer Rymer
tctMD
TARGET BP 1: Alcohol-Based RDN Promises Single Treatment for Resistant BP
April 16 — Dawn Coleman
Vascular Specialist
April 16 — Duke Clinical Research Institute
Medscape
Chelation Therapy and CV Risk: Why TACT2 Showed No Benefit
April 17 — Jennifer Rymer
Medscape
Alcohol-Mediated Renal Denervation Promising in Hypertension
April 18 — William Kraus and Kim Huffman
Mirage.News
Research: Calorie Limitation’s Complex Role in Aging
April 18 — Joseph Lerman
tctMD
In Transporting Donor Hearts, SherpaPak Shows Promise Over Traditional Coolers
Duke Heart Pulse — April 14, 2024
Duke Heart Pulse – April 14, 2024
Highlights of the week:
ACC.24: Narcisse Selected for 2024 ACC Career Development Award

 We are excited to share that Duke cardiology fellow Dennis I. Narcisse, Jr., MD, MS, is one of three recipients of the 2024 American College of Cardiology/Association of Black Cardiologists Merck Research Fellowship. The fellowship awards were presented on Monday, during the last day of the ACC Scientific Sessions in Atlanta.
We are excited to share that Duke cardiology fellow Dennis I. Narcisse, Jr., MD, MS, is one of three recipients of the 2024 American College of Cardiology/Association of Black Cardiologists Merck Research Fellowship. The fellowship awards were presented on Monday, during the last day of the ACC Scientific Sessions in Atlanta.
Three awardees are selected each year to receive a one-year fellowship in the amount of $100,000 as salary support for one year of research in adult cardiology. Narcisse was selected along with Colette DeJong, MD of the University of California, San Francisco and Xiaowen Wang, MD, MPH of Massachusetts General Hospital.
The ACC is committed to inspiring and investing in the next generation of cardiovascular clinicians, scientists and leaders. The ACC’s Career Development Awards provide opportunities for rising stars in cardiology to gain access to leadership development, mentorship and knowledge-building that will help them grown in their chosen areas of expertise.
In addition to the ACC/ABC Merck Research Fellowships, other ACC Career Development Awards announced on Monday included the Hani Najm Global Scholar Award and the William A. Zoghbi International Research Awardee.
Congratulations, Dennis!
DHIP Leadership News
Leadership announcements were made this week by Tom Owens, MD executive vice president and chief operating officer of Duke Health Integrated Practice (DHIP), and John Sampson, MD senior vice president of DHIP.
Paul R. Newman, a senior DHIP and DUHS leader, will lead several strategic priorities for Duke Health, including funds  flow and clinical effort models, implementation of mission-based accounting, physician partnership development to enable growth, and the development of other strategic initiatives that may arise.
flow and clinical effort models, implementation of mission-based accounting, physician partnership development to enable growth, and the development of other strategic initiatives that may arise.
 Simon Curtis has been named Chief Operating Officer for DHIP. Reporting to Owens and Sampson, and in collaboration with the DHIP leadership team, Simon will partner with the clinical departments and DUHS to drive operational excellence across the practice in areas such as clinician recruitment planning, clinical operations, access, and patient experience.
Simon Curtis has been named Chief Operating Officer for DHIP. Reporting to Owens and Sampson, and in collaboration with the DHIP leadership team, Simon will partner with the clinical departments and DUHS to drive operational excellence across the practice in areas such as clinician recruitment planning, clinical operations, access, and patient experience.
These updated roles are effective immediately.
Celebrating the Eclipse
 Members of Duke Heart’s cardiology team celebrate the eclipse at a solar eclipse watch party, on April 8, 2024.
Members of Duke Heart’s cardiology team celebrate the eclipse at a solar eclipse watch party, on April 8, 2024.
Shout-out to Goodwin!
 A big shout-out to cardiology fellow Nate Goodwin for his compassion in taking care of a very sick CCU patient.
A big shout-out to cardiology fellow Nate Goodwin for his compassion in taking care of a very sick CCU patient.
“The patient’s family really appreciated his personal touch and his ability to share their pain. I was very impressed. I also applaud the fact that in the middle of a challenging pathophysiology with no clear way out, he never ignored the human component of our job. If my mom or dad got sick, I’d want Nate taking care of them.” — Ivan Nenadic Wood, MD, PhD
Nicely done, Nate. We’re so glad you were present for this family.
Shout-out to Stephanie Buck!
 Duke Heart APP Stephanie Buck was in the right place at the right time for a passenger in distress. On a flight to the Dominican Republic a 15-yr old male went into anaphylaxis after eating goat cheese. The passenger did not have an epi pen. When flight attendants asked if a medical professional was onboard, Buck responded. Although the flight emergency kit did not have an epi pen, the did have epi in a glass ampule. Buck took control of the situation, successfully administering the epi and Benadryl, and managed care for the passenger like the amazing professional she is, even while off-duty! She continued to monitor the patient until the flight safely landed and EMS was able to take over.
Duke Heart APP Stephanie Buck was in the right place at the right time for a passenger in distress. On a flight to the Dominican Republic a 15-yr old male went into anaphylaxis after eating goat cheese. The passenger did not have an epi pen. When flight attendants asked if a medical professional was onboard, Buck responded. Although the flight emergency kit did not have an epi pen, the did have epi in a glass ampule. Buck took control of the situation, successfully administering the epi and Benadryl, and managed care for the passenger like the amazing professional she is, even while off-duty! She continued to monitor the patient until the flight safely landed and EMS was able to take over.
“I think this is a great example of why Duke Providers are the best and can handle even the scariest situations whether at work or out in the community,” said Roman Ross, MSN, ANP-C for the division of cardiovascular and thoracic surgery.
Kudos to Hughes and Duke Aortic team
We received terrific patient feedback on Dr. Chad Hughes and the aortic team this week. Via Press Ganey HCAHPS, we received a note that states:
“Can’t say enough about Dr. Hughes and his team. I received the very best surgical expertise and care. I’m very, very fortunate.” — a grateful patient
Dr. Hughes, we received this nice feedback about the great care you and your team gave to a patient at Duke Hospital on Heart service unit 3300. Thank you for the high quality and compassionate care you provide to patients.” — David Gallagher, MD, Chief Medical Officer, DUH
“Kudos Dr. Hughes for the tremendous comments. Agree that we are fortunate to have you and the entire aortic team at Duke Heart and Health!” — Jill Engel, VP, Duke Heart & Vascular Services
This Coming Saturday: Support Duke’s Aortic Team & NC Walk for Victory
Duke Heart is again serving as the presenting sponsor of the upcoming NC Walk for Victory in support of Marfan Syndrome, LDS, VEDS and related conditions, with Dr. Chad Hughes serving as co-medical chair for the walk along with Carly Scarborough of Levine Children’s Hospital.
The event is scheduled for 12-3 p.m. on Saturday, April 20 at Laurel Hills Park in Raleigh. To learn more, please visit the NC Walk website and consider joining the Duke Aorta team to raise funds for research!
Flu Season is Officially Over
After consultation with Duke Infectious Diseases, the Health System has defined Monday, April 1, as the official end of the flu season. For the purposes of the Duke University Health System (DUHS) Healthcare Worker Flu Vaccination Policy, new staff/providers who have joined DUHS on or after April 1 will not be required to be vaccinated against the flu or have an approved exemption. However, they will be required to comply with flu vaccination policy during the Fall 2024 flu vaccination period.
Upcoming Events & Opportunities
- April is National Donate Life Month
- Annual reminder as part of Duke’s “check yourself” campaign: please make sure your contact information is up to date in Duke@Work
- Culture Pulse 2024 survey period starts April 22!
Cardiology Grand Rounds
April 16: Cancelled
April 23: TBD
April 25: New Insight into the Physiology of Heart Failure with Preserved Ejection Fraction with Tom Sarma, MD of UT Southwestern. 5 p.m., DN 2002 or via Zoom. *Please note this is a Thursday evening presentation.
All Duke Cardiology Grand Rounds recordings are housed on Warpwire. To access recordings please visit:
NET ID and password required. Enjoy!
CD Fellows Core Curriculum Conference
April 17: HF/Txp Case Presentation with Aarti Thakkar. Noon, DMP 2W96 (in-person only).
April 19: Genetics and CVD with Svati Shah. Noon, Zoom only.
Upcoming CME Symposia
May 4: Duke Heart Failure Symposium
Please reach out to Christy Darnell with any questions.
Working Effectively Across Generations
 June 3: Working Effectively Across Generations with Hile Rutledge, of Otto Kroeger Associates (OKA). 8:30 a.m. to Noon. Great Hall, Trent Semans Center. Sponsored by Duke School of Medicine.
June 3: Working Effectively Across Generations with Hile Rutledge, of Otto Kroeger Associates (OKA). 8:30 a.m. to Noon. Great Hall, Trent Semans Center. Sponsored by Duke School of Medicine.
Registration required: https://medschool.duke.edu/blog/register-now-working-effectively-across-generations
Improving Conversation Skills with Seriously Ill Patients
In an effort to ensure that clinicians feel comfortable and empowered to have difficult conversations regarding goals of care with patients and their families, members of the Duke Hospice and Palliative Care team offer VitalTalk communication trainings so that they can help clinicians do their best to take care of our patients.
VitalTalk skills training is open to those involved in conducting or supporting Goals of Care conversations for our patients with serious illness across Duke Health. The course consists of a 30-minute didactic lecture in the LMS system, followed by a 3-4 hour skills practice-session. CME/CEU credits are available once both activities (LMS and live practice) are completed.
A limited number of seats are available in each of the upcoming online VitalTalk skills practice courses – use https://duke.is/VitalTalk to view available dates and times and to register.
If you have any questions, please contact Jonathan Fischer, MD, medical director of palliative care for Duke’s Population Health Management Office.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
April 4 — Nina Nouhravesh
India Today
Eggs may not increase your cholesterol. Study explains
April 6 — Tom Povsic
tctMD
Full AEGIS-II Results: Raising HDL With Apo A-I No Help After Acute MI
April 6 — Stephen Greene
HCP Live
Don’t Miss a Beat: EMPACT-MI at ACC.24, with Javed Butler, MD
April 7 — Wayne Batchelor
Medscape
Ticagrelor Alone Cuts Bleeding Without More Events Post-PCI
April 7 — Mark Kittipibul
HCP Live
April 7 — Manesh Patel
tctMD
Long-Awaited RCT Data Show Survival Benefit With Impella CP: DanGer Shock
April 8 — Robert Mentz
Associated Press
April 8 — Mark Kittipibul
HCP Live
Modified On-Treatment Analysis Confirms Results of TRANSFORM-HF
April 8 — Mitchell Krucoff
NBC News
10 doctors on FDA panel for Abbott heart device had financial ties to the company
April 8 — Madhav Swaminathan
Diagnostic Imaging
April 8 — Wayne Batchelor
Healio/Cardiology Today
Routine use of Impella CP for STEMI-related cardiogenic shock confers survival benefit
April 8 — Wayne Batchelor
Healio/Cardiology Today
Long-term DAPT may not be needed for patients with ACS after angioplasty, stenting
April 8 — Duke University Health System
The People’s Pharmacy
Eggs Are Bad – No, Eggs Are Good – Huh?
April 8 — Nina Nouhravesh
Easy Health Options
Eggs’ Bad Rap Cheats Those Who Need Their Benefits Most
April 8 — Adrian Hernandez
Medical Xpress
ACC: Empagliflozin cuts heart failure hospitalization risk after AMI
April 9 — Neha Pagidipati
Medscape
Early Olezarsen Results Show 50% Reduction in Triglycerides
April 10 — Sreekanth Vemulapalli
Becker’s Hospital Review
The biggest challenges facing cardiology, per 12 leaders
April 10 — Neha Pagidipati
Medscape
Substantial Triglyceride Reduction With Plozasiran
April 10 — Jennifer Rymer
Medpage Today
FFR-Guided Complete Revascularization Did Not Improve Outcomes in MI Patients
April 10 — Duke University Hospital
Becker’s Hospital Review
472 hospitals honored for patient safety, price transparency
April 11 — Manesh Patel
Salt Lake City Star Tribune
Medtronic study puts spotlight on how one of its heart devices can help women
April 11 — Jay Lusk (Population Health)
Healio
Low socioeconomic status raises mortality odds in pulmonary conditions
April 11 — Svati Shah
Time
How to Talk to Your Family About Their Heart Health History
April 12 — Jennifer Rymer
Medscape
Duke Heart Pulse — April 7, 2024
Chief’s message:
The American College of Cardiology 2024 meeting was this weekend with several of our faculty and fellows presenting at the meeting. We also had the opportunity to catch up with colleagues and friends. Please find some pictures from the meeting.






Highlights of the week:
Hughes Named Chief, Section for Aortic Surgery
 Chad Hughes, MD, Professor of Surgery, has been appointed the inaugural Chief for the Section of Aortic Surgery, a new section housed jointly within the Divisions of Cardiothoracic Surgery and Vascular and Endovascular Surgery. Hughes will also serve as co-director, with vascular surgeon Chandler Long, MD, of the Duke Center for Aortic Disease. The announcement was made on April 3 by Dr. Carmelo Milano, chief of Cardiovascular and Thoracic Surgery, and Dr. Dawn Coleman, chief of Vascular Surgery.
Chad Hughes, MD, Professor of Surgery, has been appointed the inaugural Chief for the Section of Aortic Surgery, a new section housed jointly within the Divisions of Cardiothoracic Surgery and Vascular and Endovascular Surgery. Hughes will also serve as co-director, with vascular surgeon Chandler Long, MD, of the Duke Center for Aortic Disease. The announcement was made on April 3 by Dr. Carmelo Milano, chief of Cardiovascular and Thoracic Surgery, and Dr. Dawn Coleman, chief of Vascular Surgery.
Hughes completed his undergraduate training at Wake Forest University and medical school at Duke University. He subsequently completed his training in both general surgery and CT surgery at Duke University. In 2005, he completed an additional aortic surgery fellowship at the University of Pennsylvania under the instruction of Dr. Joseph Bavaria, a renowned leader in aortic surgery.
Hughes joined the faculty here at Duke as an assistant professor of surgery, and in 2020, he rose to the rank of Professor of Surgery. He has developed one of the largest practices of aortic surgery in the country with national and regional referrals. At Duke, he started the transcatheter aortic valve replacement program with Dr. Kevin Harrison. Additionally, along with Dr. Richard McCann, he developed stent grafting for aortic pathology at this institution.
Hughes has served as a model of the academic surgeon with over 250 peer-reviewed publications, multiple national speaking engagements, and a prominent role as an associate editor for the Annals of Thoracic Surgery. He has driven innovation of care for aortic pathology at a national level.
This divisional reorganization is focused on enabling further collaboration between CT surgery, vascular surgery, and cardiology. In this new role, Dr. Hughes will focus on further expansion of aortic surgery, innovation around aortic pathology, and mentoring younger faculty and trainees in aortic surgery.
Congratulations, Chad!
Thomas Receives HRS Youngblood Leadership Award

We were thrilled to learn this week that cardiac electrophysiologist Kevin Thomas, MD, professor of medicine in cardiology and vice dean for Diversity, Equity and Inclusion for Duke School of Medicine, has been selected by the Heart Rhythm Society (HRS) to receive it’s 2024 James H. Youngblood Excellence in Leadership Award.
The Youngblood Leadership Award recognizes a member of the HRS who has demonstrated exemplary leadership by leading an initiative that has had a community-wide impact.
You have certainly done that and more — congratulations, Kevin!
Anne Cherry, MD to Receive Inaugural SCA Presidential Citation

Congratulations to Anne Cherry, MD, associate professor of anesthesiology at Duke. She has been selected as the first recipient of the Society of Cardiovascular Anesthesiology’s (SCA) newest award – the Presidential Citation Award. Cherry was selected by Dr. Kathryn Glas, current president of the SCA and chair of anesthesiology at the University of Arizona.
The Presidential Citation will be awarded annually at the discretion of the President of SCA to an individual who has made an important contribution to the field of cardiovascular anesthesia through one (or several) of the following:
- An early career accomplishment
- Research contribution
- Education contribution
- DEI contribution through the advancement of minority interests
- Service to the SCA
Cherry will be presented with the 2024 Presidential Citation during the SCA Annual Meeting being held in collaboration with the American Association for Thoracic Surgery from April 27-30 in Toronto, Canada.
Congratulations, Anne!
Holley to Receive DOM Excellence in Education Award

We are pleased to share that Christopher Holley, MD, PhD, has been selected as the recipient of Duke’s 2024 Department of Medicine Excellence in Education Award for the division of cardiology. His nomination, in part, reads:
“As a member of our clinical team, Holley teaches cardiovascular disease and advanced heart failure and transplantation fellows during Transplant or VAD rounds and gives high-yield lectures in these areas, receiving stellar teaching evaluations from our trainees. As a skilled researcher, he teaches and mentors undergraduate, graduate, and post-graduate trainees on the role of non-coding RNA (ncRNA) in cardiovascular health and disease.
Furthermore, he is committed to educating the next generation of cardiovascular specialists by actively participating in fellowship recruitment. He serves as an Associate Program Director of the Cardiovascular Disease fellowship, as a co-lead in the Department of Medicine’s Physician Scientist Training program, and as core faculty in the Medical Scientist Training Program. In all these roles, his passion for educating current and future trainees is evident.”
This annual DOM award recognizes one faculty member in each division in recognition of outstanding teaching and commitment to the education and professional development of fellows, residents, and students. He will be recognized during the DOM Annual Celebration on May 2.
Congratulations, Chris!
Small Selected for DOM Administrative Excellence Award
 Congratulations to Duke Cardiology GME coordinator Brianna Small! We learned this week that she has been selected to receive the Department of Medicine’s Rising Star Award for Administrative Excellence.
Congratulations to Duke Cardiology GME coordinator Brianna Small! We learned this week that she has been selected to receive the Department of Medicine’s Rising Star Award for Administrative Excellence.
She will be recognized during the Annual Chair Award dinner celebration later this spring.
Hooray, Brianna!
ACC.24: Therapy Shows Promise in Delaying Hospitalizations for Heart Failure
About 800,000 people in the U.S. suffer a heart attack every year, and about 30% of them will go on to develop heart failure. There are limited treatments to prevent or slow that development.
A large international study led by Duke researchers investigated whether the diabetes drug empagliflozin (marketed under the brand name Jardiance) might prevent heart failure in patients after they had suffered acute myocardial infarction.
While the study found that the drug did not reduce deaths, secondary findings show it did slow the time to first hospitalization for heart failure and reduced the total number of subsequent heart failure hospitalizations.
The secondary findings are published in the journal Circulation and presented at the American College of Cardiology’s Annual Scientific Session on April 6. Other findings from the study, called EMPACT-MI, were also simultaneously published in the New England Journal of Medicine and the Journal of the American College of Cardiology.
Empagliflozin was originally approved for use in patients with diabetes, but investigators chose to study the drug based on earlier findings that it showed benefit in preventing active heart failure from becoming worse. The study was funded by two companies that manufacture the drug – Boehringer Ingelheim and Eli Lilly and Company.
The study enrolled 6,522 patients across 22 countries, with roughly half randomly assigned to receive the therapy and the other half placebo. Both groups otherwise received standard care. Investigators credit the study’s simple design to its broad reach.
The Duke Clinical Research Institute coordinated and led the conduct of the trial.
The study findings on lower rates of heart failure offer some hope and underscore the importance of preventing poor outcomes after a heart attack, according to principal investigator and corresponding author, Adrian Hernandez, MD, director of the Duke Clinical Research Institute.
“Developing heart failure is one of our major public health problems, and any step that gets us closer to preventing it is a step in the right direction,” Hernandez said. “After a heart attack, we should really be focused on how to prevent problems, especially the development of heart failure. This therapy fills in that gap.”
Hernandez said he would be curious to investigate the secondary findings further, especially because there are so many different factors that can play out after a heart attack.
“Heart attacks are pretty dynamic – in the first 24 hours things can change for the better or the worse; you can end up having a small heart attack or a big one,” Hernandez said. “We don’t know if there could be a difference in results from the therapy depending on the type of event and the timing of giving a treatment. Those could be areas to consider.”
In addition to Hernandez, study authors for the Circulation publication include Jacob A. Udell, W. Schuyler Jones, Stefan D. Anker, Mark C. Petrie, Josephine Harrington, Michaela Mattheus, Svenja Seide, Isabella Zwiener, Offer Amir, M. Cecilia Bahit, Johann Bauersachs, Antoni Bayes-Genis, Yundai Chen, Vijay K. Chopra, Gemma Figtree, Junbo Ge, Shaun Goodman, Nina Gotcheva, Shinya Goto, Tomasz Gasior, Waheed Jamal, James L. Januzzi, Myung Ho Jeong, Yuri Lopatin, Renato D. Lopes, Béla Merkely, Puja B. Parikh, Alexander Parkhomenko, Piotr Ponikowski, Xavier Rossello, Morten Schou, Dragan Simic, Philippe Gabriel Steg, Joanna Szachniewicz, Peter van der Meer, Dragos Vinereanu, Shelley Zieroth, Martina Brueckmann, Mikhail Sumin, Deepak L. Bhatt, and Javed Butler.
ACC.24: Congrats to all Duke Researchers & Presenters!
The Annual Scientific Sessions for the American College of Cardiology is well underway this weekend in Atlanta. We’ve had significant news coverage for the poster presentation on the fortified eggs study, findings of which were released last week ahead of the ACC. We anticipate additional news coverage on the EMPACT-MI study results (highlighted above) and look forward to coverage of many other presentations by our Duke Heart team.
Carolyn Lekavich, PhD, presented an abstract on Saturday — Advancing Heart Failure Prevention: Echocardiogram Ventricular-Arterial Coupling (VAC) Signaling Early Heart Failure with Preserved Ejection Fraction (HFpEF).
Heading into ACC, there were 113 presentations planned related to research performed with or by Duke team members, including two late-breakers (EMPACT-MI, and the AEGIS II trial), many poster presentations, abstracts, and contributions including those with:
- Karen Alexander
- John Alexander
- Gerald Bloomfield
- Adam DeVore
- Pamela Douglas
- Michael Felker
- Marat Fudim
- Christopher Granger
- Jennifer Green
- Stephen Greene
- Josephine Harrington
- Adrian Hernandez
- Schuyler Jones
- Michelle Kelsey
- Mark Kittipibul
- Larry Jackson
- Renato Lopez
- Daniel Mark
- Robert Mentz
- Kristin Newby
- Nina Nouhravesh
- Neha Pagidipati
- Kishan Parikh
- Manesh Patel
- Jonathan Piccini
- Sean Pokorney
- Jennifer Rymer
- Nishant Shah
- Svati Shah
- Monique Starks
- Sreekanth Vemulapalli,
Nicely done, all!
Shout-out to Osude!
A hat tip & shout-out to cardiovascular disease fellow Nkiru “KiKi” Osude, MD, for her work in the community to promote heart health!
Osude recently served as a guest speaker — along with faculty member Monique Starks, MD — at the 2024 Shades of Green “Goes Red” Fashion Show and Luncheon, a charity fundraising event to help promote cardiovascular disease awareness throughout the community, sponsored by the Durham chapter of The Links, Incorporated.

The event, in part, highlighted the importance of heart health and community efforts to improve cardiovascular health. The Links, Incorporated is a group of more than 15,000 professional women of color dedicated to improving the well-being of Durham citizens through leadership, philanthropy, and service.
Osude was also featured in a heart-health promotional flyer as part of the work being done by Durham’s Community Health Coalition.
Way to go, KiKi! 
Duke Heart & 2024 NC Walk for Victory
Duke Heart will again serve as the presenting sponsor of the upcoming NC Walk for Victory in support of Marfan Syndrome, LDS, VEDS and related conditions, with Dr. Chad Hughes serving as co-medical chair for the walk with Carly Scarborough of Levine Children’s Hospital.
The event is scheduled for 12-3 p.m. on Saturday, April 20 at Laurel Hills Park in Raleigh. To learn more, please visit the NC Walk website and consider joining the Duke Aorta team to raise funds for research!
ICYMI: April Leadership Town Hall
The most recent DUHS Leadership Town Hall was held on Tuesday, April 2 via Zoom. If you missed it and would like to watch the recording, it is available on Leadership Exchange.
Upcoming Events & Opportunities
- April is National Donate Life Month
- April 6-8, American College of Cardiology Scientific Sessions, Atlanta.
Cardiology Grand Rounds
April 9: Heart Failure: Does Sex Really Matter? with Carolyn Lam, of Duke-NUS MD. 5 p.m., DN 2002 or via Zoom.
April 16: TBD
April 23: TBD
April 25: New Insight into the Physiology of Heart Failure with Preserved Ejection Fraction with Tom Sarma, MD of UT Southwestern. 5 p.m., DN 2002 or via Zoom. *Please note this is a Thursday evening presentation.
All Duke Cardiology Grand Rounds recordings are housed on Warpwire. To access recordings please visit:
NET ID and password required. Enjoy!
CD Fellows Core Curriculum Conference
April 10: Cardiology Fellows Lunch with Carolyn Lam. Noon, DMP 2W96 (in-person only).
April 12: Journal Club with TBD. Noon, Zoom only.
Upcoming CME Symposia
April 12: Duke Sports Cardiology & Sudden Death in Athletes
May 4: Duke Heart Failure Symposium
For any questions you might have about either event, please reach out to Christy Darnell.
2024 Feagin Leadership Forum
Consider joining members from throughout the Duke community for a special Duke Centennial event, the 15th Annual Feagin Leadership Forum at the JB Duke Hotel on May 17-18. The theme for the Forum is Compassion, Collaboration, and Compromise: Leadership in a Polarized World. World class leaders from business, healthcare, the military and athletics will be sharing their leadership expertise and how they address the challenges of our complex world. There will be special welcomes from Duke leaders, and the future leaders of healthcare — this year’s Feagin Leadership Scholars — will share their work and leadership insights.
For more details, go to https://www.feaginleadership.org/schedule-1.
To register, visit: https://www.feaginleadership.org/2023registration-1.
Improving Conversation Skills with Seriously Ill Patients
In an effort to ensure that clinicians feel comfortable and empowered to have difficult conversations regarding goals of care with patients and their families, members of the Duke Hospice and Palliative Care team offer VitalTalk communication trainings so that they can help clinicians do their best to take care of our patients.
VitalTalk skills training is open to those involved in conducting or supporting Goals of Care conversations for our patients with serious illness across Duke Health. The course consists of a 30-minute didactic lecture in the LMS system, followed by a 3-4 hour skills practice-session. CME/CEU credits are available once both activities (LMS and live practice) are completed.
A limited number of seats are available in each of the upcoming online VitalTalk skills practice courses – use https://duke.is/VitalTalk to view available dates and times and to register.
If you have any questions, please contact Jonathan Fischer, MD, medical director of palliative care for Duke’s Population Health Management Office.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
March 20 — Richard Shannon
The Assembly
Why Breast Cancer Screening Fails Many Women
March 29 — Nina Nouhravesh
Everyday Health
Eggs May Actually Be Okay for Your Heart
March 29 — Nina Nouhravesh
Earth.com
Eggs aren’t just for Easter — eating them is no longer considered unhealthy
March 29 — Nina Nouhravesh
The Washington Times
Never mind: New study finds eggs won’t worsen cholesterol, may even improve heart health
March 29 — Nina Nouhravesh
Times Now (India)
High cholesterol diet: Study claims eggs won’t increase your cholesterol levels
March 29 — Nina Nouhravesh
Medical Dialogues (India)
March 29 — Nina Nouhravesh
Arab Times (Kuwait)
New study challenges notion of eggs’ impact on cholesterol levels
March 30 — Nina Nouhravesh
The Mirror (UK)
‘Myth’ that eggs are bad for the heart and raise cholesterol debunked by scientists
April 1 — Nina Nouhravesh
Healio
Top in cardiology: Benefits of fortified eggs; FNIH to study preeclampsia biomarkers
April 2 — Nina Nouhravesh
Scripps News
Eggs might not be that bad for your heart health, study says
*carried by 60+ Scripps affiliates nationally
April 2 — Duke Clinical Research Institute
Code List
According to cardiologists, this long-shunned food is not so bad
April 4 — Duke University Medical Center
Mass Device
Paragonix begins full U.S. launch of donor lung preservation system
April 4 — Duke University Medical Center
Medical Design & Development
Paragonix Begins Full Commercial Launch for Donor Lung Preservation System
Duke Heart Pulse — March 31, 2024
Duke Heart Pulse – March 31, 2024
Highlights of the week:
Happy Elite 8 Easter Weekend
 To all those celebrating the holiday this weekend with family and friends, we wish you a very Happy Easter, and to all those celebrating the
To all those celebrating the holiday this weekend with family and friends, we wish you a very Happy Easter, and to all those celebrating the advancement of their favorite NCAA teams in the men’s and women’s tournaments, a big congratulations!
advancement of their favorite NCAA teams in the men’s and women’s tournaments, a big congratulations!
We’re excited to see Duke MBB take on the Wolfpack today at 5 p.m. and hopefully continue onward to the Final Four. Go Duke!
Gaca Appointed Section Chief, Adult Cardiac Surgery
We are pleased to share that Jeffrey Gaca, MD, has been appointed section chief for Adult Cardiac Surgery. The announcement was made last week by Dr. Carmelo Milano, MD, chief of the division of cardiovascular and thoracic surgery.
Gaca completed his undergraduate degree at Cornell University and medical school at Columbia University. His training in both general surgery and cardiovascular and

thoracic surgery was accomplished at Duke University.
In 2008, after completing an additional aortic surgery fellowship at the University of Pennsylvania, Gaca joined the Duke Surgery faculty as an assistant professor in the Division of CT Surgery. In 2016, he rose to the academic rank of associate professor.
Gaca is one of our most talented cardiac surgeons and has developed a tremendous valvular surgery practice with regional and national referrals, Milano said. He has distinguished himself as a leading educator of our residents and is the recipient of the Dr. Dwight C. McGoon award for commitment to resident development.
In addition, he has been an important mentor for junior faculty, helping them navigate complex cases and challenging intraoperative situations. He is also known for his innovation and has worked closely with Dr. Don Glower to expand minimally invasive heart surgery, making Duke University a leading referral center for these procedures.
He has worked with Dr. Chad Hughes and the cardiologists to grow the transcatheter valve replacement program. In his new role, Gaca will work closely with Milano to develop young cardiac surgery faculty and further drive innovation and growth.
Please join us in congratulating and welcoming Jeff in this new role!
Kelsey to Receive SOM Master Clinician Award

We are excited to share that Anita Kelsey, MD, has been selected as a recipient of the Duke School of Medicine’s Master Clinician/Teacher Award for 2024. This award was created to honor individuals for superlative accomplishment in teaching and/or clinical care at Duke’s School of Medicine. The intent is to honor those individuals who have made an extraordinary commitment “above and beyond” normal expectations. “Dr. Kelsey has certainly met the criteria and is most deserving of the honor,” said Edward Buckley, MD, in his notification letter.
The award will be presented to Kelsey at the annual Faculty Celebration at Duke Gardens on May 13, 2024.
Congratulations, Anita!
ACC.24: Fortified Eggs Did Not Raise Cholesterol in Modest-Sized Cardiology Study
There are often conflicting headlines about whether certain foods are good or bad for you, and the news about eggs has been especially confusing. Search the topic online and you’ll find a wealth of articles spanning back decades.
A study that will be presented during the American College of Cardiology’s Annual Scientific Sessions and led by researchers at Duke, offers new evidence on fortified eggs, which are eggs enriched with various vitamins or nutrients. In a modest-sized randomized trial, researchers found that fortified eggs did not have a negative impact on bad cholesterol (LDL cholesterol) or good cholesterol (HDL cholesterol) over the course of the four-month study.
The study was sponsored by Eggland’s Best, a company that makes and sells fortified eggs. It also provided the eggs used in the research.
The study had 140 participants, all people aged 50 or older, who had experienced at least one cardiac event in the past or had risk factors for cardiovascular disease such as diabetes. Researchers randomized participants into two groups, asking half to eat two or fewer eggs per week for four months. The other half were provided with fortified eggs and asked to eat 12 per week for the same period of time.
While no significant changes in bad or good cholesterol were found, a secondary finding hinted there could be some benefit associated with fortified egg consumption for older patients and patients with diabetes.
That secondary finding was not statistically significant due to the number of study participants, but cardiologist and senior researcher, Robert Mentz, MD, associate professor of medicine at the Duke University School of Medicine, said it’s an interesting signal that the researchers would like to investigate in future work.
“If we can explore this area further, in a larger study, specifically focusing on the type of patients who appear to have potentially experienced some benefit, and over a longer period of time, we could see if it is possible for fortified eggs to improve cholesterol,” Mentz said.
The study’s first author, Nina Nouhravesh, MD, a cardiology fellow at the Duke Clinical Research Institute, said the study can be viewed as a pilot study.
“While it was modest in size, it did include a broadly generalized population,” Nouravesh said. “The average age of participants was 66 years, half were women, and more than 25 percent identified as Black.”
Mentz said the enrollment was representative of the community, especially for a study aimed at cardiology patients.
He said he would like to move forward with a larger study assessing clinical outcomes, particularly when considering the topic of equity and food access.
“There are disparities around access to food,” Mentz said. “Individuals who are the most socially disadvantaged (and likely have more instances of high blood pressure and diabetes), often have less access to healthy foods. Often what we hear described in the community is access to fresh fruits and vegetables. Those are really time-limited foods that may go bad quickly. Fortified eggs can be safely stored in the refrigerator for longer periods of time. Investigating potential health benefits of an easily accessible and less time-limited food is something we should be doing.”
“I think we are in this exciting time where people think of food as medicine,” Mentz said. “Some foods are fortified and nutritionally optimized before they’re disseminated, similar to medications, so it’s exciting to use the same rigor that’s applied in medication trials to food science.”
In addition to Mentz and Nouhravesh, study authors include Josephine Harrington, Laura H. Aberle, Cynthia L. Green, Kathleen Voss, Dave Holdsworth, Kurt Misialek, Bartel T. Slaugh, Mandee Wieand, William S. Yancy, and Neha Pagidipati.
Duke-DCRI Reception at ACC.24
For those of you attending the American College of Cardiology’s Annual Scientific Sessions (April 6-8), please join us at the annual Duke-DCRI Reception taking place on Saturday, April 6, 2024, from 5:30-8:30 p.m. EDT, at the Omni Atlanta Hotel at Centennial Park in Grand C Ballroom, North Tower-M4.
Team Builder’s Gift Launches Heart Innovation Hub
(This story was posted to Giving to Duke Health.)
 Most people understand the importance of team building, but few take it as seriously as Bob Keegan: building innovative and successful teams was the tenet of his professional career. Now Keegan is empowering a pioneering Duke Health team with a transformational gift to kick-start the new Duke Heart Precision and Innovation Collaboratory headed by Manesh Patel, MD, chief of the division of cardiology and the division of clinical pharmacology.
Most people understand the importance of team building, but few take it as seriously as Bob Keegan: building innovative and successful teams was the tenet of his professional career. Now Keegan is empowering a pioneering Duke Health team with a transformational gift to kick-start the new Duke Heart Precision and Innovation Collaboratory headed by Manesh Patel, MD, chief of the division of cardiology and the division of clinical pharmacology.
“I am grateful for the many contributions Bob has made to Duke Heart,” Patel said. “We are excited to use his philanthropy to build our team, expand our cardiovascular knowledge base, and then translate that knowledge into new treatments, disease prevention, health promotion, and outstanding patient care. Most importantly, he is supporting our innovation efforts with the next generation of leaders.”
Keegan grew up around teams. His father was a professional baseball player for the Chicago White Sox, and while Keegan was a talented athlete who grew up thinking baseball was in his future, his love of academics prevailed. What followed was a degree in mathematics from Le Moyne College and an MBA in finance from the University of Rochester. Business, it turns out, was Keegan’s calling. He knew early on that what drove him was a heartfelt desire to build teams that would produce innovative products people would love and benefit from.
Decades later, it was time to scale back, be closer to family, and plan for the future. Keegan knew that living near a top-notch medical facility such as Duke was important, and with four grandchildren nearby, moving to the Triangle was an easy decision.
When he suffered heart trouble, Keegan experienced firsthand the incredible talent and skill of the Duke heart team. “My surgery was an amazing experience,” he said. “I benefitted from a tremendous group of talented people, before and after the procedure.”
The professionalism and team culture he witnessed ignited Keegan’s desire to bolster Duke Heart’s impact and accomplishments. So, when a friend suggested he join the Duke Heart Leadership Council, he leapt at the chance to contribute his time and business expertise. Currently serving as the council chair, Keegan is extending his support with his personal philanthropy toward the development of the new Duke Heart Precision and Innovation Collaboratory.
The Duke Heart Precision and Innovation Collaboratory aims to expand the boundaries of the possible and improve cardiovascular health worldwide with a comprehensive, long-range, and multi-phased team approach. Phase 1 will identify promising discoveries in precision genomics, device innovations, and human performance. Phase 2 will scale those discoveries to launch clinical trials, research grants, and new treatment options.
An effort this visionary and all-encompassing, with the potential for global impact, requires immense resources. With a stellar leadership team in place and eager to see the potential realized, Keegan contributed the first $1.5 million toward the Collaboratory’s $10 million fundraising goal.
This initial funding stimulates the process of collecting and compiling huge swaths of data to build the country’s first comprehensive cardiac genomic database and first comprehensive cardiac performance database. Such large volumes of data will allow Duke Health researchers to conduct in-depth analysis and gain a better understanding of trends and patterns.
A second area of further research is a deeper understanding of human heart performance. The gap between a high-performing heart and a failing one is surprisingly small, and the variations and drivers that account for the difference are not well understood. The Collaboratory aims to close this gap.
In addition to this work, the team will optimize devices capable of improving individual patients’ physiology. Duke Heart is an innovator in this space, with one of the largest heart failure device laboratories in the United States. Personalizing the future of device therapy for patients with heart failure will save countless lives.
Keegan built his successful business career by making teams better. Sometimes it was a matter of switching personnel, but often it was choosing the right stimulus to bring out the best of existing team members.
“Duke Heart is a great team that already produces a great product,” he said. “I’m just doing what I can to keep it moving forward so that people are as proud of Duke’s accomplishments in 40 years as they are today.”
Bova Campell to Join HRS Board
 Kristen Bova Campbell, clinical pharmacist for Duke Electrophysiology, has been appointed to serve on the Board of Trustees of the Heart Rhythm Society (HRS). She will become the first PharmD to serve in this capacity when she begins her term in May during the HRS Scientific Sessions scheduled for May 16-19 at the Boston Convention & Exhibition Center, Boston.
Kristen Bova Campbell, clinical pharmacist for Duke Electrophysiology, has been appointed to serve on the Board of Trustees of the Heart Rhythm Society (HRS). She will become the first PharmD to serve in this capacity when she begins her term in May during the HRS Scientific Sessions scheduled for May 16-19 at the Boston Convention & Exhibition Center, Boston.
“It is an honor to be selected as the first PharmD on the HRS Board and to represent all Allied Health Professionals within HRS,” says Bova Campbell. “I am excited to collaborate and contribute to the Society’s mission of providing optimal care to patients with heart rhythm disorders.”
Bova Campbell is director of the PGY2 Cardiology Pharmacy Residency and director of the Duke Heart Center Anticoagulation Clinic. She will join Jonathan Piccini, MD, section chief of electrophysiology, who also serves as a member of the Board, and Sana Al-Khatib, MD, currently serving as 2nd Vice President for the Board.
Congratulations, Kristen!
Rebecca Dial Named NM, Invasive Labs & CVSSU
 We are happy to announce that Rebecca Dial, BSN, RN will serve as Nurse Manager, Operations for the adult Invasive Labs and Cardiovascular Short Stay Unit effective April 1, 2024.
We are happy to announce that Rebecca Dial, BSN, RN will serve as Nurse Manager, Operations for the adult Invasive Labs and Cardiovascular Short Stay Unit effective April 1, 2024.
Rebecca earned a Bachelor of Science in Nursing from the University of North Carolina Greensboro in 2013. Her career spans cardiovascular telemetry, cardiac-surgical stepdown, and cardiac catheterization lab nursing. She has worked in the Adult Cardiac Catheterization Lab at Duke University Hospital since August 2020 and served in a variety of roles, including preceptor and charge nurse. In July 2023, she transitioned into the Assistant Nurse Manager role within the labs and has focused on improving scheduling practices and providing professional development opportunities to staff.
Rebecca is looking forward to partnering with leaders across the organization. Please join us in welcoming her to her new role!
Frye Regional TAVR Training
Dr. John Morrison, an interventional cardiologist with Frye Regional Medical Center and a community consulting associate with the division of cardiology at Duke, spent time throughout March with our Duke Heart Transcatheter Aortic Valve Replacement (TAVR) team.
Frye Regional Medical Center is a Duke LifePoint hospital and full-service cardiovascular center serving a large geographic area in the Catawba Valley region of NC. As an affiliate partner, members of Duke Heart and the Duke Heart Network have been working closely with the team at Frye Regional to help them prepare for the launch of their new TAVR program.
“The willingness of the Duke Heart team to collaborate with regional partners has been clearly evident to Dr. Morrison and he has commented on how wonderful every interaction has been,” said Lisa Kotyra, senior director, Duke Heart Network.
Under the guidance of Kevin Harrison, MD, Morrison had the opportunity to observe all Duke structural cardiologists, cardiac surgeons, and our multidisciplinary team as they worked through the TAVR process and procedure.
Morrison is shown here with Drs. Harrison and Hughes.


Kudos to Gaca!
In a note forwarded this week from David Gallagher, chief medical officer for Duke University Hospital, we have a kudos for Jeff Gaca, our new section chief for adult cardiac surgery:
“We received this nice feedback (from Press Ganey HCAHPS) about the great care you and your team gave to a patient at Duke Hospital. Thank you for the high quality and compassionate care you provide to patients! I believe this is the third Press Ganey inpatient comment in a short period of time from patients who are so appreciative of you.” — David Gallagher, MD
“I can’t say enough good about the nurses in the ICU unit after open heart surgery. I came to Duke from Naples, FL and so glad I did. Dr. Gaca is an amazing surgeon.” — a grateful patient
Way to go, Jeff!
Shout-out to Cheri Wills!
A note of appreciation to Cheri Wills, health center administrator (HCA) for Duke Cardiology of Raleigh and Duke Cardiology of Morrisville, whose last official day with Duke Health is today, March 31. Erica Bradshaw is the new HCA for these locations; she has been training with Cheri since last summer.
Cheri, we wish you all the best in retirement, and thank you for your terrific work over the years!
Duke Heart & 2024 NC Walk for Victory
Duke Heart will again serve as the presenting sponsor of the upcoming NC Walk for Victory in support of Marfan Syndrome, LDS, VEDS, and related conditions, with Dr. Chad Hughes serving as co-medical chair for the walk with Carly Scarborough of Levine Children’s Hospital.
The event is scheduled for 12-3 p.m. on Saturday, April 20 at Laurel Hills Park in Raleigh. To learn more, please visit the NC Walk website and consider joining the Duke Aorta team to raise funds for research!
Last chance! Mere Days Remain to Support Frazier-Mills!

If you have not already done so, please join us in supporting electrophysiologist Camille Frazier-Mills, MD, one of the Triangle American Heart Association’s Women of Impact in her campaign to raise funds to support Go Red for Women.
Frazier-Mills is representing Duke Health as a Woman of Impact in the 2024 campaign and we want to help her reach her campaign goal. By donating, each of us can support her campaign and help ensure more women have equitable access to cardiovascular care and better representation in critically needed medical research.
** Check out Camille Frazier-Mills’ campaign page and please donate by April 4. **
Every year across the country, a select group of individuals are nominated to be a part of Woman of Impact because of their passion and drive to make a difference. This 9-week blind competition is relentlessly focused on women’s heart health. The campaign launched on National Wear Red Day (Feb. 2) and closes on April 4. During this time, the nominees work to build campaign plans, recruit Impact teams, and inspire their networks to support the American Heart Association’s lifesaving mission.
At the end of the campaign, this special group of changemakers will be celebrated for the overall impact they have on the AHA’s mission and the Triangle community. The nominee who makes the greatest impact and raises the most funds locally will be named a local 2024 Woman of Impact Winner.
Additionally, the nominee who makes the greatest impact nationwide will be named the American Heart Association 2024 National Woman of Impact Winner.
Let’s help her reach and exceed her goal – let’s help her WIN! Go, Camille!
Upcoming Events & Opportunities
- April is National Donate Life Month
- April is Earth Month
- April 6-8, American College of Cardiology Scientific Sessions, Atlanta.
Cardiology Grand Rounds
April 2: SCERRI Stories: Mechanistic Insights Into Sepsis Induced Cardiovascular Dysfunction with Willard Applefeld, MD. 5 p.m., DN 2003 or via Zoom.
April 4: Using Nationwide Registries to Conduct Pragmatic Randomized Trials with Tor Biering-Sorensen, MD of the Center for Translational Cardiology and Pragmatic Randomized Trials, Denmark. 5 p.m., DN 2002 or via Zoom. *Special CGR event*
April 9: Heart Failure: Does Sex Really Matter? with Carolyn Lam, of Duke-NUS MD. 5 p.m., DN 2002 or via Zoom.
All Duke Cardiology Grand Rounds recordings are housed on Warpwire. To access recordings please visit:
NET ID and password required. Enjoy!
CD Fellows Core Curriculum Conference
April 3: EP Case Presentation with Joshua Rushakoff and Jawan Abdulrahim. Noon, DMP 2W96 (in-person only).
April 5: We will not meet today.
Upcoming CME Symposia
April 12: Duke Sports Cardiology & Sudden Death in Athletes
May 4: Duke Heart Failure Symposium
For any questions you might have about either event, please reach out to Christy Darnell.
2024 Feagin Leadership Forum
Consider joining members from throughout the Duke community for a special Duke Centennial event, the 15th Annual Feagin Leadership Forum at the JB Duke Hotel on May 17-18. The theme for the Forum is Compassion, Collaboration, and Compromise: Leadership in a Polarized World. World-class leaders from business, healthcare, the military, and athletics will share their leadership expertise and how they address the challenges of our complex world. There will be special welcomes from Duke leaders, and the future leaders of healthcare — this year’s Feagin Leadership Scholars — will share their work and leadership insights.
For more details, go to https://www.feaginleadership.org/schedule-1.
To register, visit https://www.feaginleadership.org/2023registration-1.
Improving Conversation Skills with Seriously Ill Patients
To ensure that clinicians feel comfortable and empowered to have difficult conversations regarding goals of care with patients and their families, members of the Duke Hospice and Palliative Care team offer VitalTalk communication training so that they can help clinicians do their best to take care of our patients.
VitalTalk skills training is open to those involved in conducting or supporting Goals of Care conversations for our patients with serious illnesses across Duke Health. The course consists of a 30-minute didactic lecture in the LMS system, followed by a 3-4 hour skills practice session. CME/CEU credits are available once both activities (LMS and live practice) are completed.
A limited number of seats are available in each of the upcoming online VitalTalk skills practice courses – use https://duke.is/VitalTalk to view available dates and times and to register.
If you have any questions, please contact Jonathan Fischer, MD, medical director of palliative care for Duke’s Population Health Management Office.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
March 22 — Adrian Hernandez
Medpage Today
Tracking Trends in Lung Cancer Incidence, Death in the U.S.
March 22 — Jenny Wu, Brian Southwell, Jonas Swartz
JAMA Network
Patients Are Turning to TikTok for Health Information—Here’s What Clinicians Need to Know
March 23 — Susan Spratt
Senior Resource
Medicare to Cover Wegovy for Patients with Heart Disease
March 23 — Nishant Shah
Everyday Health
Weight Cycling May Increase the Risk of Heart Attack and Stroke
March 25 — Susan Dent (medical oncology)
The ASCO Post
Cardio-Oncology Is a Growing Subspecialty, but Where Are the Oncologists?
March 26 — Harry Severance
Becker’s Physician Leadership
The erosion of physician autonomy
March 27 — Stephen Greene
tctMD
Most HFrEF Patients Eligible for Quadruple Therapy, but Few Get It
March 28 — Nina Nouhravesh
Good Morning America/ABC News
Eating a dozen eggs a week doesn’t hurt your cholesterol: Study
March 28 — Monique Starks
The Clemmons Courier
Demonstration of historic, first-in-the-nation, AED drone delivery held by FCSO
March 28 — Nina Nouhravesh
Today/NBC News
Are eggs bad for cholesterol? New study reveals how many you can eat
March 28 — Duke Health
The People’s Pharmacy
The Never-Ending Egg Dispute Continues
March 28 — Nina Nouhravesh
Talker
Scientists bust myth that eggs are bad for your heart
*also carried by 80 affiliate outlets including in Chicago, Dallas Ft. Worth and New York
March 28 — Nina Nouhravesh
Healio/Cardiology Today
Routinely eating fortified eggs may not adversely affect cholesterol
March 28 — Nina Nouhravesh
Healthline
Eating 12 Eggs a Week Didn’t Raise Cholesterol Levels, New Study Finds
Duke Heart Pulse — March 24, 2024
Chief’s message:
Thomas Awarded Distinguished Professorship, Effective July 1
 Congratulations to electrophysiologist Kevin Thomas, MD, the newly named Donald F. Fortin, M.D. Distinguished Professor of Cardiology.
Congratulations to electrophysiologist Kevin Thomas, MD, the newly named Donald F. Fortin, M.D. Distinguished Professor of Cardiology.
Thomas is among 32 faculty members at Duke University selected to receive distinguished professorships this year. Approval was made by Duke’s Board of Trustees during their February meeting. Each awardee will be recognized during a ceremony at the Washington Duke Inn on May 23. Their new professorships will be effective on July 1.
“I am very pleased to honor these faculty members with distinguished professorships,” said President Vincent Price. “Their outstanding scholarship has advanced knowledge across a wide variety of fields and made a positive impact on society, and I am proud to have them as colleagues.”
Distinguished professorships honor faculty who are well-established members of the Duke academic community and have also achieved distinction as creative scholars in their field or in their ability to transcend disciplines.
“I congratulate my colleagues on receiving distinguished professorships recognizing their impressive scholarly achievements and leadership in our academic community and beyond,” said Provost Alec D. Gallimore. “Duke is tremendously fortunate to count these bold thinkers among its faculty.”
Well deserved, Kevin! Congratulations!
Gutierrez, Rymer Selected for SCAI ELM Cohort

Congratulations to interventional cardiologists Tony Gutierrez and Jennifer Rymer! We learned this week that both have been selected as fellows for the Society for Cardiovascular Angiography & Interventions (SCAI) 2024-2026 Emerging Leader Mentorship (ELM) Program. Only 12 interventionalists are chosen each year.
The mission of the ELM Program is to take a small, highly select group of up-and-coming physicians and support their transition into the next

generation of great thinkers, presenters, teachers, and leaders. Interaction of the ELM Fellows with a highly accomplished panel of Mentors and other ELM Alumni will be fostered during the program, which will also provide Fellows with individualized tools and resources. SCAI conducts this program in partnership with the American College of Cardiology (ACC) and the Cardiovascular Research Foundation (CRF).
During the cohort period fellows will attend dedicated in-person training sessions three times per year during the SCAI, TCT, and ACC annual meetings. They will also be given opportunities for faculty speaking at SCAI and partnering organizations that are congruent with their interests and area of focus. In this way, the ELM Program will assist participants in reaching maximum potential and transitioning into national and societal leaders.
A core mission of the ELM Program is to encourage participation in service opportunities including positions on Councils and Committees that coincide with each Fellow’s clinical, research, or educational interests.
This is a wonderful opportunity for Drs. Gutierrez and Rymer and we are so excited for them.
Congratulations, Jenn and Tony!
Podgoreanu, Selvaraj & Voora Appointed to CPH Faculty Leadership Team
The Center for Precision Health (CPH) has announced the addition of 10 faculty members, including three Duke Heart team members who will serve on the CPH leadership team: Mihai Podgoreanu, MD, chief, division of cardiac anesthesiology; Senthil Selvaraj, MD, assistant professor of medicine in cardiology, and Deepak Voora, MD, associate professor of medicine in cardiology and executive director of the Veterans Affairs National Pharmacogenomics Program. The leadership team also includes surgical oncologist Shelley Huang, MD, vice chair of research in the Department of Surgery.
CPH is a collaborative effort between Duke Clinical & Translational Science Institute (CTSI) and the Precision Genomics Collaboratory (PGC) that works to harness the power of genomic, biomarker, and health data to transform patient care and population health.
The new faculty team will help CPH expand clinical genetics, conduct clinically relevant translational research, perform cutting-edge implementation science, engage with and build trust in the community, as well as contribute to educating the ‘workforce of tomorrow.’
“We are thrilled to have an amazing cohort of faculty joining the Center for Precision Health,” said cardiologist Svati H. Shah, MD, MHS, the Ursula Geller Distinguished Professor of Research in Cardiovascular Diseases, associate dean for translational research and director of the CPH. “Their talents and expertise will help us expand our basic, translational, and clinical research and allow us to harness the power of genomic, biomarker and health data to transform patient care and population health.”
To read more and see the full list of faculty for CPH, please visit https://duke.is/j/4vud.
Congratulations Mihai, Senthil, and Deepak!
Newest JACC Editors Named; Duke Well Represented
Incoming Journal of the American College of Cardiology (JACC) Editor-in-Chief Harlan M. Krumholz, MD, SM, FACC, cardiologist with Yale University, this week announced the members of his new Editorial Board, each of whom will be responsible for helping to position the journal as the leading beacon for advancing global cardiovascular health, effective July 1.
Several Duke faculty members are on the team, as well as a number of Duke graduates and former trainees, including:
- Lesley H. Curtis, PhD, Duke professor of population health sciences and of medicine. Curtis will serve as a deputy editor.
- Melvin Echols, MD, cardiologist with Morehouse School of Medicine and a former Duke Cardiology fellow. Echols will serve as an associate editor.
- Kushal T. Kadakia, MSc, a Duke graduate and former member of Duke-Margolis Institute for Health Policy. Kadakia will serve as a deputy associate editor.
- Carolyn Lam, MBBS, PhD, cardiologist with Duke-National University of Singapore, will serve as a deputy editor.
- Neha Pagidipati, MD, MPH, cardiologist and director of the Duke Cardiometabolic Prevention Clinic will serve as an associate editor.
- Anne Marie Valente, MD, of Harvard Medical School, is a former Duke fellow in pediatric cardiology and in adult cardiovascular disease. Valente will serve as an associate editor.
Congratulations to all!
Burleson Named Nurse Manager, DUH 3100, Effective April 1
 Duke Heart is pleased to announce that Matt Burleson, BSN, RN will become Nurse Manager, Operations for Duke University Hospital’s Cardiothoracic Stepdown Unit 3100 effective April 1.
Duke Heart is pleased to announce that Matt Burleson, BSN, RN will become Nurse Manager, Operations for Duke University Hospital’s Cardiothoracic Stepdown Unit 3100 effective April 1.
Matt earned a Bachelor of Science in Nursing from the University of Tennessee, Knoxville in 2015 and is currently pursuing his Master of Science in Nursing through East Carolina University. He began his nursing career on a progressive cardiac care unit in Atlanta, Georgia and transitioned to Duke’s Surgical Trauma Intensive Care Unit in September of 2016. His time spent on the Surgical Trauma ICU has been carried out through a variety of roles including Preceptor, Resource Nurse, and Charge Nurse. Over the past 2.5 years, he has served as Assistant Nurse Manger. As ANM, he has contributed to the continuation of the SICU CLABSI Reduction Initiative, lead Mass Casualty Incident Plan preparedness, and facilitated Armed and Dangerous drills.
He enjoys the opportunity to listen to, teach, and coach team members. Matt also has been an active member of Duke’s Patient Response Team where he has appreciated building relationships and caring for patients across a wider breadth of the hospital. Matt is looking forward to joining the Duke Heart Team and continuing his journey as a Duke Nurse Leader.
Please join us in congratulating and welcoming Matt to his new role.
Shout-out to Fox!
 A shout-out to Duke Heart clinical nurse specialist, Allison Fox, who presented at the 2024 National Association for Clinical Nurse Specialists (NACNS) Annual Conference. NACNS 2024 was held on March 10-13 in New Orleans. Fox shared her abstract presentation, “Introducing Subcutaneous Diuretic Therapy in the Ambulatory Setting,” which highlighted the CNS role in bridging the gap between innovation and clinical practice in the heart failure clinic.
A shout-out to Duke Heart clinical nurse specialist, Allison Fox, who presented at the 2024 National Association for Clinical Nurse Specialists (NACNS) Annual Conference. NACNS 2024 was held on March 10-13 in New Orleans. Fox shared her abstract presentation, “Introducing Subcutaneous Diuretic Therapy in the Ambulatory Setting,” which highlighted the CNS role in bridging the gap between innovation and clinical practice in the heart failure clinic.
Way to go, Allison!
Kudos to Heart Care Team & Zwischenberger!
We received a wonderful patient comment this week regarding heart surgeon Brittany Zwischenberger, MD, and the patient’s full care team. The note, captured by Press Ganey HCAHPS, went to David Gallagher, chief medical officer. He then shared it with our team:
“I must commend the following people for their good care – Miles, Colby, Ashley, Erica, Lindsey, Amber, Catherine, Mallory, Taylor, and Dr. Brittany Zwischenberger. Plus Joan in pre-op.” – a grateful patient
Thank you for the high quality and compassionate care you provide to patients! – Dr. David Gallagher
Kudos, Brittany and team – you’re amazing providers and we are fortunate to have you on our team!
Duke-DCRI Reception at ACC.24
For those of you attending the American College of Cardiology’s Annual Scientific Sessions (April 6-8), please join us at the annual Duke-DCRI Reception taking place on Saturday, April 6, 2024, from 5:30-8:30 p.m. EDT, at the Omni Atlanta Hotel at Centennial Park in Grand C Ballroom, North Tower-M4.
USNWR Voting Closes Wednesday
USNWR voting for Best Hospitals by specialty is still open in Doximity. If you are board-certified in the U.S. and have claimed your Doximity profile already, please log into your account by Wednesday, March 27 to complete the brief survey: submit your nominations.
New to Doximity? Find and register your profile to vote. Just go to Doximity’s login page, scroll to the bottom and click on “find your profile” – find yours and claim it/register. You can participate in the survey as long as you register on Doximity prior to the survey closing on March 27.
The survey allows you to list up to five hospitals as Best Hospital in the specialty in which you are board-certified. Your ballot counts even if you vote only for one hospital.
As with primaries and national elections, every vote is important!
Just 11 Days Remain to Support Frazier-Mills!

If you have not already done so, please join us in supporting electrophysiologist Camille Frazier-Mills, MD, one of the Triangle American Heart Association’s Women of Impact in her campaign to raise funds to support Go Red for Women.
Frazier-Mills is representing Duke Health as a Woman of Impact in the 2024 campaign and we want to help her reach her campaign goal. By donating, each of us can support her campaign and help ensure more women have equitable access to cardiovascular care and better representation in critically needed medical research.
** Check out Camille Frazier-Mills’ campaign page and please donate by April 4. **
Every year across the country, a select group of individuals are nominated to be a part of Woman of Impact because of their passion and drive to make a difference. This 9-week blind competition is relentlessly focused on women’s heart health. The campaign launched on National Wear Red Day (Feb. 2) and closes on April 4. During this time, the nominees work to build campaign plans, recruit Impact teams, and inspire their networks to support the American Heart Association’s lifesaving mission.
At the end of the campaign, this special group of changemakers will be celebrated for the overall impact they have on the AHA’s mission and the Triangle community. The nominee who makes the greatest impact and raises the most funds locally will be named a local 2024 Woman of Impact Winner.
Additionally, the nominee who makes the greatest impact nationwide will be named the American Heart Association 2024 National Woman of Impact Winner.
Let’s help her reach and exceed her goal – let’s help her WIN! Go, Camille!
Improving Conversation Skills with Seriously Ill Patients
Did You Know? Patients from Duke cardiology, hepatology and oncology are the most likely to end up in the hospital during their last month of life. These are the patients most in need of goals of care conversations, according to researchers from Duke in their recently published findings in the Journal of Pain and Symptom Management.
To make sure that clinicians feel comfortable and empowered to have these difficult conversations with patients and their families, members of the Duke Hospice and Palliative Care team offer VitalTalk communication trainings so that they can help clinicians do their best to take care of our patients.
VitalTalk skills training is open to those involved in conducting or supporting Goals of Care conversations for our patients with serious illness across Duke Health. The course consists of a 30-minute didactic lecture in the LMS system, followed by a 3-4 hour skills practice-session. CME/CEU credits are available once both activities (LMS and live practice) are completed.
A limited number of seats are available in each of the upcoming online VitalTalk skills practice courses – use https://duke.is/VitalTalk to sign up for one of the following:
- March 19, 1 – 5 pm
- April 10, 8 am to 12 pm
- April 10, 1 – 5 pm
- April 12, 8 am to 12 pm
- April 12, 1 – 5 pm
- May 1, 8 am to 12 pm
- May 1, 1 – 5 pm
- May 16, 8 am to 12 pm
- May 16, 1 – 5 pm
- June 18, 8 am to 12 pm
- June 18, 1 – 5 pm
- June 21, 8 am to 12 pm
- June 21, 1 – 5 pm
Once registered, you will receive an Outlook calendar invite, Zoom details, and instructions for completing the required pre-work module in LMS.
Please keep in mind these trainings are limited to a small number of participants because they are extremely interactive. If you are interested in training but these dates do not work for you, please contact Jennifer Bowen to be added to a distribution list for future signups.
Once registered, if your plans change or you are unable to dedicate your full attention during the course, please let the team know ASAP so that you can be rescheduled and your seat offered to others on the waitlist.
If you have any questions, please contact Jonathan Fischer, MD, medical director of palliative care for Duke’s Population Health Management Office.
Upcoming Events & Opportunities
- March 30 is National Doctor’s Day
- Happy Spring, everyone!
Cardiology Grand Rounds
March 26: New Direction for CABG: Women and Robots with Brittany Zwischenberger, MD. 5 p.m., DN 2002 or via Zoom.
April 2: SCERRI Stories: Mechanistic Insights Into Sepsis Induced Cardiovascular Dysfunction with Willard Applefeld, MD. 5 p.m., DN 2003 or via Zoom.
April 9: Heart Failure: Does Sex Really Matter? with Carolyn Lam, of Duke-NUS MD. 5 p.m., DN 2002 or via Zoom.
All Duke Cardiology Grand Rounds recordings are housed on Warpwire. To access recordings please visit:
NET ID and password required. Enjoy!
CD Fellows Core Curriculum Conference
March 27: DHP Case Presentation with Aubrie Carroll. Noon, DMP 2W96 (in-person only).
March 29: Endocarditis with Andrew Wang. Noon, Zoom only.
Upcoming CME Symposia
April 12: Duke Sports Cardiology & Sudden Death in Athletes
May 4: Duke Heart Failure Symposium
For any questions you might have about either event, please reach out to Christy Darnell.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
March 13 — Christopher Granger
Inside Precision Medicine
March 18 — John Guyton (emeritus/endocrinology)
Medscape
Niacin and CV Risk: Should Advice on Intake Change?
March 18 — Padma Gulur (anesthesiology)
Daily Mail
March 18 — Ralph Snyderman (Chancellor Emeritus)
Medium
Must-Read Books on the Advancement of Healthcare
March 19 — Joseph Turek
Scientific American
Partial Heart Transplants Grow with Their Young Recipients
March 20 — Duke University Hospital (lung tx)
Newson6.com (Oklahoma)
A Breath of Hope: The Remarkable Journey of Oklahoma Triple Lung Transplant Survivor
March 20 — Mary Klotman
WFMY (Greensboro, NC)
First Lady Dr. Jill Biden makes stop in Durham to talk research in women’s health
Recent Comments