Duke Heart Pulse — May 26, 2024
Chief’s message:
This memorial day we wanted to thank and recognize the women and men that continue to protect, serve, and sacrifice for the safety, freedom, and liberty of our nation and our allies. Please be sure to thank all of the service members and recognize the sacrifices they and their families make everyday.
Updates from the week of the week:
Patel to serve as DUHS Physician VP for Heart & Vascular Services

Manesh R. Patel, MD, the Richard S. Stack Distinguished Professor and division chief of cardiology at Duke, will serve as the Duke University Health System physician vice president for Heart and Vascular Services, effective May 15th, 2024.
In this role, Patel will oversee cardiovascular care for Duke, working closely with Carmelo Milano, MD, chief of cardiothoracic surgery, Dawn Coleman, chief of vascular and endovascular surgery, and Mihai Podgoreanu, chief of cardiothoracic anesthesiology. Our cardiovascular service line leadership team, including Jill Engel, vice president, and Mary Lindsay, associate chief nursing officer, will work together with Manesh to continue to advance cardiovascular care across Duke Health.
Patel will work closely with DUHS leadership and clinical department chairs to develop innovative initiatives that improve access to care and support the Duke Health strategic plan. His responsibilities will encompass quality and outcomes, budgetary and financial oversight, operations, and management of Duke Heart Network and affiliations. As part of this work, Manesh will lead a Health AI clinical testing lab within the Duke Heart Innovation Hub, partnering with Michael Pencina, Jeff Ferranti, and Duke AI Health.
This change reflects Duke’s commitment to the tremendous team across Duke Health who aim to discover and deliver extraordinary team-based cardiovascular care for patients as a leading Heart and Vascular Center.
Patel completed his medicine residency and fellowships in cardiology, interventional cardiology, and clinical research at Duke and Duke Clinical Research Institute. He has served as the division chief of Duke Cardiology since 2017. He was selected by the American Heart Association in 2023 as AHA Physician of the Year.
Upon this transition, Patel will report to Greg Pauly, group president of Acute Care Services for Duke University Health System, and vice dean for Clinical and Academic Integration with the School of Medicine.
Duke EP Well Represented at Heart Rhythm 2024
Members of our electrophysiology (EP) and cardiology faculty and several EP staff were very busy at the Heart Rhythm Society (HRS) 2024 meetings, held May 16-19 in Boston. There were many Duke abstracts and presentations, too many to fully recount, but here are some highlights provided by Jonathan Piccini, MD, MHS, professor of medicine in cardiology and director of cardiac electrophysiology at Duke:
Bill Cockfield, Amber Stohl, Gail Brock, Sana Al-Khatib, and Kristen Campbell found some time to snap a quick picture before a roundtable session. Dr. Kevin Thomas received the distinguished and very prestigious James Youngblood Excellence in Leadership Award from the Heart Rhythm Society
Dr. Kevin Thomas received the distinguished and very prestigious James Youngblood Excellence in Leadership Award from the Heart Rhythm Society

 While at the meeting Dr. Thomas delivered invited lectures on “Diversity in EP Clinical Studies – Challenges and Opportunities” and “Addressing Disparities in Sudden Cardiac Death.”
While at the meeting Dr. Thomas delivered invited lectures on “Diversity in EP Clinical Studies – Challenges and Opportunities” and “Addressing Disparities in Sudden Cardiac Death.”
Kristen Campbell was named to the Heart Rhythm Society Board of Trustees! She is the first-PharmD to achieve this distinction, a true reflection of her commitment to heart rhythm care. She chaired several sessions on antiarrhythmic therapy at the HRS meetings.
Dr. Kelly Arps presented her work with Dr. Al Sun on outcomes associated with emergent extracorporeal membrane oxygenation (ECMO) and catheter ablation for ventricular tachycardia in the setting of cardiogenic shock.

Dr. Al Sun served as distinguished faculty at the HRS 2024 EP Fellows Symposium alongside Duke EP alumni Dr. Eric Prystowsky and Dr. Doug Packer. He also participated in an expert panel on managing unexplained sudden cardiac arrest.
Dr. Larry Jackson delivered an invited lecture on “Overcoming Healthcare Delivery Gaps – Walking the Talk”. He also served as one of the judges along with Jon Piccini in the AHA-HRS Shark Tank competition at the scientific sessions.

Dr. Camille Frazier-Mills presented an invited lecture on the role of pharmacotherapy and pacing in persons with cardioinhibitory vasovagal syncope. She also led a session on the optimal management of cardiovascular implantable electronic device (CIED) alerts and advisories as well as a session on diversity and EP leadership. She also delivered the invited commentary on the long-awaited one-year outcomes from the dual chamber leadless pacing study that was presented in the late-breaking science session.
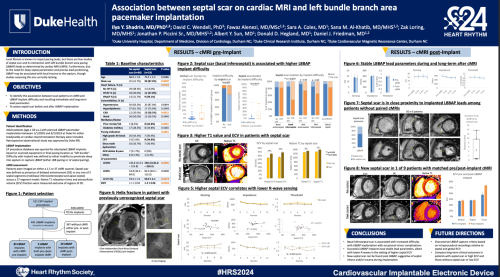
Dr. Ilya Shadrin presented his research on left bundle branch area pacing with Dr. Daniel Friedman, including an abstract reporting on the relationship between septal scar and pacing.
Dr. Daniel Friedman (below, far right) delivered an invited lecture on “How to Predict the Response of LBBP-CRT?”

Dan Friedman and Jon Piccini were among a team of investigators presenting our pre-clinical work on a balloon-based ablation catheter to deliver pulse field ablation in a canine model.

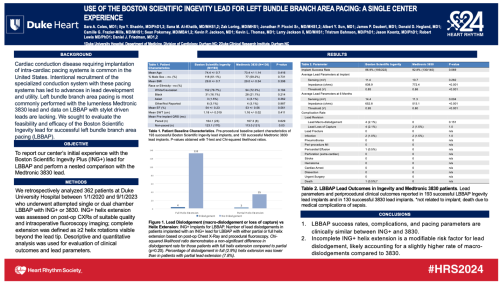
Dr. Sara Coles reported the Duke EP experience with the stylet-driven Ingevity+ lead for left bundle branch area pacing, the largest experience reported to date in the field.
Dr. Kevin Jackson delivered an invited lecture on the Optimization of Programming in Cardiac Resynchronization Therapy in the “One Stop
Shop for All Things Device Programming” session at HRS. He also delivered the commentary on the FARAPULSE registry data presented at the late-breaking science sessions.
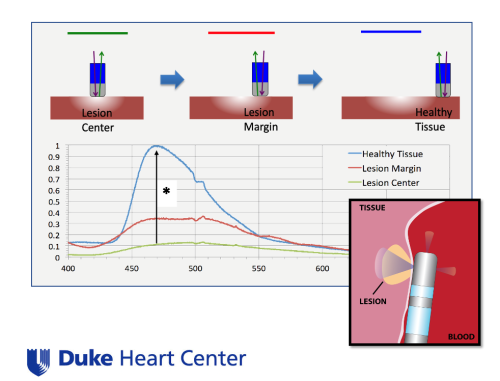
Dr. Jon Piccini presented on the use of LuxMed hyperspectral imaging and biofluorescence to assay ablation lesion efficacy and myocardial characterization at the Stanford Biodesign meeting at HRS.
Dr. James Daubert Delivered an invited lecture on patient selection and optimal use of implantable cardioverter defibrillator (ICD) therapy in persons with non-ischemic cardiomyopathy, and a lecture on programming of ICDs in competitive athletes.
Dr. Andrew Landstrom presented invited lectures at the meetings on innovative approaches to evaluating VUSs associated with arrhythmogenic cardiomyopathies and an “Introduction to Cardiovascular Genomic and Precision Medicine.”
Dr. Monique Starks presented an invited lecture on “Drone-delivered Automated External Defibrillators (AEDs): Improving the Chain of Survival in the US.”

Dr. Sana Al-Khatib had a very busy HRS this year as she continues on the executive leadership team for the Heart Rhythm Society. She was a key architect of the HRS 2024 meeting, as she served as the abstract chair. At the meeting, she participated in a featured debate on the use of cardiac resynchronization therapy pacemakers (CRT-P) vs cardiac resynchronization therapy defibrillators (CRT-D) in persons with non-ischemic cardiomyopathy.
Congrats to our EP team — exceptional work and representation at HRS!
McVeigh Represents Duke Heart at AAPA 2024
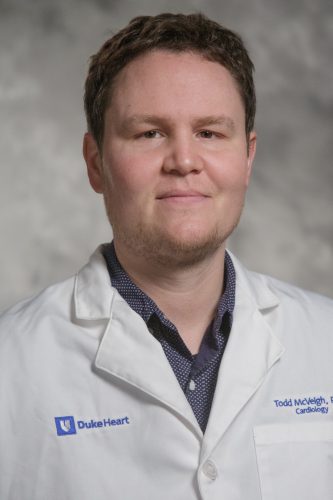
Duke cardiology physician assistant Todd McVeigh, PA-C, gave two podium poster presentations at the American Academy of Physician Associates (AAPA) 2024 annual meeting held last weekend (May 18-22, 2024) in Houston, TX.
His presentations were entitled, “Introduction of a PA into a Heart Failure Remote Monitoring clinic” and “Introduction of Home-applied Subcutaneous Furosemide to Treat Heart Failure Exacerbations”.
Way to go, Todd!
Cox Earns DAISY Award
 Congratulations to ventricular assist device (VAD) nurse practitioner Kevin Cox! Cox was awarded the 2024 DAISY Award for Extraordinary Nursing Educators through the Duke School of Nursing (SON). He was nominated by former MSN Student Sonia Lai, his former preceptee.
Congratulations to ventricular assist device (VAD) nurse practitioner Kevin Cox! Cox was awarded the 2024 DAISY Award for Extraordinary Nursing Educators through the Duke School of Nursing (SON). He was nominated by former MSN Student Sonia Lai, his former preceptee.
His notification letter included the following:
“It is my honor to advise you that you were nominated by MSN student Sonia Lai and have been selected by the Institute for Education Excellence DAISY Awards Committee to receive a 2024 DAISY Award for Extraordinary Nursing Educators in recognition of the super-human work that you do for students!” — Jacqui McMillen-Bohler, director of IEE, Duke SON.
Cox was recognized during the annual DUSON Faculty & Staff Awards ceremony held on May 22. He is shown here receiving the award from Duke SON Interim Dean Michael Relf.
Congratulations, Kevin – well-deserved!
Ramos Earns DNP

Congratulations to critical care nurse practitioner Dayana Ramos, DNP! Dayana graduated with her Doctor of Nursing Practice on May 11. She is shown here with her sister, Natassha Blakeslee, a nurse practitioner at the University of Miami, who graduated alongside her.
Ramos and Blakeslee completed their studies at Missouri State University. Ramos did her DNP project here at Duke University Hospital. Her project consisted of creating a discharge protocol to improve discharge times for the post-acute care (PAC) service.
The duo, who are Panamanian, wore sashes that were hand-made by a woman who belongs to the Kuna Indians of Panama. Dayana’s sash features the Panamanian golden frog (rana dorada), which is indigenous to and found only in Panama. Her sister’s sash features the Harpy Eagle, the national bird of Panama. They wanted to incorporate symbols from their native country and represent their culture.
Congratulations, Dayana & Natassha!
Shout-out to Biever
A shout-out to Kimberly Biever from the cardiology clinical research unit!
“She identified and approached a patient for an inpatient study. Because the patient wanted more time (to consider), she returned back to the hospital to consent and initiate study procedures on a Sunday. Kim goes again and again beyond the call of duty, due to her passion for research and love of patients. It is a pure delight to work with coordinators like her, which is what makes Duke great.” — Marat Fudim
Great work, Kim!
Kudos to Granger & 7E Staff
We received a note this week from David Gallagher, MD, chief medical officer for Duke University Hospital regarding feedback he received from a grateful patient:
“Chris, we received this nice feedback (from Press Ganey HCAHPS) about the great care you and your team gave to a patient at Duke University Hospital. Thank you for the high quality and compassionate care you provide to patients!” – David Gallagher, MD
“I would like to thank Dr. C. Granger & the entire 7E ICU staff for giving me the best care ever. They made the most traumatic thing in my life a whole lot easier with excellent care!” – a grateful patient
Great job, team!!!!
Team Member Appreciation Month: Spirit Week
Our team members are what make Duke Health such a special place to work and to heal. This year, Duke is elevating how we recognize and thank everyone for their incredible work through our inaugural Team Member Appreciation Month.
It’s week 4, the final week: Spirit Week
Monday: Team Mixtape—Start a collaborative playlist with your team to jam to! Apple Music, Spotify, and YouTube have collaboration features to make a shared playlist. You can also amp up the festivities with a virtual team music party to take a break during your busy day – be sure to share your dance moves by uploading your photos and videos here! Note: Please be respectful and only use clean and appropriate music.
Tuesday: Crazy Socks Day—Wear your favorite socks to work – yes, those super fun ones
Wednesday: Spread Smiles with Kudos & Kindness—Seize the day and spread smiles with some of these ways to keep kindness top of mind:
- Send a Kudos Kard (or five!)
- Let a colleague know why you’re proud of them
- Celebrate something/someone that doesn’t get normally recognized enough
- Give a high five
- Greet three strangers while walking the hallways
- In Huddle/team meeting, take a moment to share a team win
- Send a story to be shared across Duke Health
- Make a team birthday and/or work anniversary calendar and create a plan to celebrate them
- Have lunch with someone out of your normal routine
- Give three people compliments (only one can be about looks!)
- Let someone know when something reminds you of them and it made you smile
- Take a moment to connect/check in with someone that you haven’t in a while
- Sign up to do some community service
- Give someone a fun sticky note or Teams message
- Invite someone to join you in practicing self-care at work
- Share a story with teammate that they are a part of that always makes you smile when you think of it
- Surprise your team with a kind gesture
Thursday: Chalk the Sidewalk—Take a moment to go outside and draw on the sidewalk! Be sure to share your masterpiece via photos and videos here!
Friday: Show Your Duke Pride Day—Wear your favorite Duke gear or blue attire! Note: Dress code policies are still in place – be sure to check the Policy Center to find your entity’s policy.
Learn more about Team Member Appreciation Month on Duke Health Now.
Thank You for Participating in Culture Pulse
Dear Colleagues,
Thank you for participating throughout the Culture Pulse 2024 survey period. We heard from more than 23,000 team members (63 percent) and are working to bring valuable feedback to you in the coming weeks. Everyone worked hard to ensure the voices of Duke team members were heard.
As we begin to look at the data, make plans for sharing the results, and focus on our action-planning process, we look forward to partnering with you as we adapt to improve our work together. There’s more to come, so stay tuned!
Thank you again — Ian Lee Brown, Vice President and Chief Employee Experience Officer, DUHS
Upcoming Events & Opportunities
- May is American Stroke Month and Asian American and Pacific Islander Heritage Month
- May is Duke Health’s inaugural Team Member Appreciation Month
- Save the Date: June 12, 4-5 p.m., State of the School Address (SOM)
Cardiology Grand Rounds
May 28: The Ross Operation — The Ultimate Aortic Valve Replacement? with Ziv Beckerman. 5 p.m., DN2002 or via Zoom.
June 4: The Science and Community of Critical Care Cardiology with Balim Senman. 5 p.m., DN2002 or via Zoom.
All Duke Cardiology Grand Rounds recordings are housed on Warpwire. To access recordings please visit:
NET ID and password required. Enjoy!
CD Fellows Core Curriculum Conference
May 29: DHP Case Presentation with Husam Salah. Noon, DMP 2W96 (in-person only).
May 31: Echo Math with Cara Hoke. Noon, Zoom only.
DCRI Research Forum Series
 June 11: The Duke Clinical Research Institute is excited to welcome Duke Football Coach Manny Diaz as their June guest for the next DCRI Research Forum, which will close out the 2023-2024 series.
June 11: The Duke Clinical Research Institute is excited to welcome Duke Football Coach Manny Diaz as their June guest for the next DCRI Research Forum, which will close out the 2023-2024 series.
What: A Fireside Chat with Coach Manny Diaz
When: Tuesday, June 11, from Noon-1 p.m. ET
Where: DCRI Research Forum: A Fireside Chat with Manny Diaz via Zoom
We hope you’ll consider joining this virtual event!
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
May 16 — Duke Heart for Honduras
Iconos Magazine (Honduras/Hn)
Fundación Lady Lee y Duke Heart for Honduras se unen en cirugías cardiovasculares
May 18 — Sana Al-Khatib
Medpage Today
Removing Conduction System Pacing Leads: Good Success So Far
May 18 — Duke Heart for Honduras
El Heraldo (Hn)
Banco Atlántida honra a la brigada médica Duke Heart for Honduras
May 21 — Duke Heart for Honduras
La Tribuna (Hn)
May 21 — Aferdita Spahillari
tctMD
Treatment Gaps Abound in Heart Failure but Can Be Closed, Studies Show
May 21 — Nina Nouhravesh
SciTech Daily
New Research Suggests That Eggs Might Not Actually Be Bad for Your Heart
May 23 — Marat Fudim
Fierce Healthcare
Cadence finds reduced cost and better outcomes for heart failure patients through remote monitoring
May 23 — Senthil Selvaraj
Aframnews.com
Duke Heart Pulse — May 19, 2024
Duke Heart Pulse – May 19, 2024
Chief’s message – Grief and Community.
Over the last several weeks we have been having a conversation with Dr. Tony Galanos in the Division of Geriatrics and Palliative care around Grief and how we can help support our clinicians / health system staff in moments of stress and grief. This was highlighted this Monday in a wonderful grand rounds by one of our finishing fellows – Dan Loriaux. During one part of his talk, he highlighted how in ICU and hospital care – he and Dr. Galanos have worked on a program around debriefs for our fellows to help process the grief in taking care of so many sick patients. We aim to continue this and to build a community of support.
This week brought another reminder to us on the fragile nature of life and the needed strength of our community. We lost one of our recent graduates and true leader in the field – Aslan Turer. We provide his story below. I personally remembered Aslan for his unwavering humor, intellect, and energy in helping improve how we cared for patients – often holding everyone to the care standard. He will be dearly missed and our Duke Heart Community will work to support his wife Christy and their children. Please keep them in your thoughts and hearts.
Updates from the week:
In Memoriam: Aslan Turer, MD, MHS, MBA, interventional cardiologist
We have been deeply saddened this weekend at the passing of Aslan Turer, MD, 49, on Friday morning. An interventional cardiologist and hypertrophic cardiomyopathy specialist at the University of Texas Southwestern (UTSW), Turer trained at Duke through residency and multiple fellowships, and was a friend to many of our Duke Heart team members. Turer had fought cancer for the past several years. His wife, Dr. Christy Turer, also trained at Duke. They have five children. Our thoughts are with his family and with his many friends and colleagues. We know he will be greatly missed.
Turer attended medical school at the University of California San Francisco, then completed internal medicine residency at Duke University Hospital, as well as fellowship trainings in cardiovascular disease and interventional cardiology at Duke. Turer helped establish a multidisciplinary hypertrophic cardiomyopathy program at UTSW, which achieved an HCMA Center of Excellence rating in 2018. He partnered recently with Andrew Wang, MD, on a perspective piece for Circulation in February 2023 entitled “Cardiac Myosin Inhibitors: Unlocking Potential to Improve Treatment in Hypertrophic Cardiomyopathy”.
Sparkman Hillcrest Funeral Home is handling arrangements for the family; Services will be this week, as follows:
Memorial Service: Wednesday, May 22, at Sparkman/Hillcrest Funeral Home, 7405 W Northwest Hwy., Dallas, TX 75225
Muslim Prayer, 5:30 p.m., in Arabic. Christian Memorial service, 6 p.m., followed by Reflection time
Funeral, Thursday, May 23, 1 p.m.
Location: Christ the King Catholic Church, 8017 Preston Rd, Dallas, TX 75225
Aslan’s family has asked that attendees wear color and not come in traditional dark funeral attire as Aslan wanted this to be a celebration of life.
We asked for memories of Aslan for today’s issue of Pulse and received the following:
“If ever there was a person one might call a “character,” certainly Aslan Turer was one. A terrific doctor and teacher, Aslan was frequently unpredictable, a bit quirky, and a delightful prankster. I remember vividly how he and I would get into these drawn-out, crazy, and often hilarious email wars — with each trying to outdo the other with an ever more outlandish statement of silliness or goofiness. We often let the whole division in on the back and forth. As I recall, Aslan always seemed to win these verbal battles with some kind of comeback I was never clever enough to overcome. He was just fun to be around. Even more, Aslan was a sincere, loving and simply wonderful person. The world has lost a very special human being way too soon. He will be fondly remembered by all who were fortunate enough to know him.” – Thomas Bashore, MD
“Aslan and I started as interns at Duke in 2001, living in the same apartment building and were fast friends despite being from very different backgrounds. I have so many fond memories, but the most special ones were when Catherine and I would meet Aslan for a late dinner and trivia at James Joyce – where he would often be found “reading” his Lancet or NEJM, which we all established was a decoy for trying to find a mate. Later in fellowship, he moved to south Durham and we would meet in the back bar of Lantern in Chapel Hill where he had a permanent tab and everyone knew him and his sense of humor and style.
I am so saddened about his death and our thoughts are with Christy and their kids. He was truly one of the smartest, kindest, and most clever people I’ve encountered in Medicine and in life.” – Schuyler Jones, MD
Our condolences to all.
SOM Faculty Awards
Congratulations to all School of Medicine 2024 Faculty Award winners – but especially to our wonderful cardiovascular faculty and colleagues:
- Adrian Hernandez, MD, professor of medicine in cardiology received an Excellence in Professionalism Award
- Christopher Holley, MD, PhD, associate professor of medicine in cardiology received a Research Mentoring Award
- Anita Kelsey, MD, MBA, professor of medicine in cardiology received the Master Clinician/Teacher Award
- Neha Pagidipati, MD, MPH, associate professor of medicine in cardiology received a Research Mentoring Award
- Madhav Swaminathan, MBBS, professor of anesthesiology, cardiothoracic anesthesiology/ critical care, received the Master Clinician/Teacher Award
- Annemarie Thompson, MD, professor of anesthesiology, pediatric cardiothoracic anesthesiology, received a Leonard Palumbo Jr., MD Faculty Achievement Award
The awards were presented on Monday, May 13 during the 2024 Spring Faculty Celebration held at the Doris Duke Center, Sarah Duke Gardens.
Congratulations and well-deserved!
DCRI Fellowship Graduation Celebrated
Graduating DCRI Fellows were celebrated at the University Club in Durham on May 9.

We are thrilled to share the following award winners who were recognized during the celebration:


Ilia Shadrin, MD, PhD, (cardiology) was awarded the DCRI Fellowship Citizenship Award, designed to recognize a graduating DCRI research fellow. Fellows considered for this award are expected to have demonstrated the following key attributes during their DCRI tenure: possesses strong character and leadership, devoted service to the DCRI, accepts responsibility and duties, has a positive attitude towards peers, the DCRI and the medical community, eager to learn and to teach others, and shows care and concern for others and helps them when needed.
Adam DeVore, MD, was recognized with the Robert M. Califf Award for Outstanding Mentorship, designed to recognize a DCRI faculty member who has demonstrated excellence in mentorship activities for DCRI research fellows. Faculty members considered for this award are expected to have mentored fellows at the DCRI and to have demonstrated enthusiasm and commitment towards the training of fellows in clinical research activities.
Congratulations Ilia and Adam!
Sullivan Honored with Teaching Award
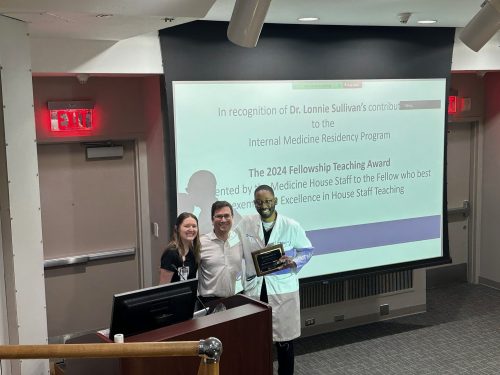 Congratulations to cardiology fellow Lonnie Sullivan, MD! He was selected as this year’s recipient of the Fellowship Teaching Award by the Internal Medicine residents.
Congratulations to cardiology fellow Lonnie Sullivan, MD! He was selected as this year’s recipient of the Fellowship Teaching Award by the Internal Medicine residents.
Way to go, Lonnie!
DHIP Update: Changes to Telehealth Video Visits and G2211 Code
Since the pandemic began, Duke Health has been able to convert all necessary patients to telehealth visits in an efficient manner, despite many changes. Now, since most of our services are video visits where standard E&M codes are used, we have decided to align our approach and use the level of service (LOS) menu.
Two Important Changes Coming to Telehealth (Video) Visits and for the G2211 Code
- Adding back the Level of Service (LOS) Menu to video visits
- Changes to G2211 Reminders: Reminders now in video visits and reminders now for all payers
Beginning May 14, the Level of Service (LOS) menu will be added back to the video visit encounters. As a result of this implementation, all E & M codes found in LOS will be removed from charge capture to prevent duplicate billing, and encounters created on the fly will still have the same charge capture (and no LOS) that exists today.
Moreover, because G2211 code is being recognized for payment by Medicare, Medicare advantage, UHC, and a few small others, and Medicaid is asking to submit this data for future consideration, there will now be G2211 reminders in all telehealth visits and visits for all payer types.
For more information on these changes, please visit the Changes to Telehealth Video Visits and G2211 Code page.
Thank you for your continued support and hard work!
Upcoming Events & Opportunities
- May is American Stroke Month and Asian American and Pacific Islander Heritage Month
- May is Duke Health’s inaugural Team Member Appreciation Month
- National Hospital Week ends today.
- Save the Date: June 12, 4-5 p.m., State of the School Address (SOM)
Cardiology Grand Rounds
May 21: Capturing the Left Bundle: Insights Into Conduction System Pacing with Ilia Shadrin. 5 p.m., DN 2002 or via Zoom.
May 28: The Ross Operation — The Ultimate Aortic Valve Replacement? with Ziv Beckerman. 5 p.m., DN2002 or via Zoom.
All Duke Cardiology Grand Rounds recordings are housed on Warpwire. To access recordings please visit:
NET ID and password required. Enjoy!
CD Fellows Core Curriculum Conference
May 22: EP Case Conference with Sara Coles and Ivan Nenadic Wood. Noon, DMP 2W96 (in-person only).
May 24: Coronary Anatomy & Lesion Interpretation with Tom Bashore. Noon, Zoom only.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
May 10 — Monique Starks/DCRI
WRAL
Forsyth County demonstrates how drones can deliver AEDs to heart attack victims sooner
May 13 — Senthil Selvaraj
Inside Precision Medicine
Genetic Variant Linked to Cardiovascular Disease and Death in Black Americans
May 13 — Senthil Selvaraj
WBZ Newsradio 1030 (Boston)
Study finds clue to greater heart disease in Black Americans
May 13 — Duke University (Selvaraj)
WBZ News/CBS Boston
Researchers find gene that may put Black Americans at higher risk for heart failure
May 13 — Senthil Selvaraj
STAT News
May 13 — Duke Heart for Honduras
El Heraldo (Honduras/Hn)
May 14 — Duke Health (Selvaraj)
San Diego Voice & Viewpoint
May 14 — Duke Health (Selvaraj)
Health Management
Genetic Variant Among Blacks Contributes to Cardiovascular Disease Burden
May 15 — Duke Heart for Honduras
LaPrensa (Hn)
Grupo Financiero Atlántida hace millonario donativo a brigada médica que tranformará vidas
May 15 — Duke Heart for Honduras
El Heraldo (Hn)
Hospital María y Duke University realizan brigada de cirugía cardiovascular a pacientes pediátricos
May 15 — Duke Heart for Honduras
La Tribuna (Hn)
Destacado cirujano hondureño opera junto a brigada de EEUU en el Hospital María
May 15 — Duke Heart for Honduras
Proceso Digital (Hn)
Con apoyo de Ficohsa Seguros se realiza segunda Brigada Médica Pediátrica de Duke Heart
May 16 — Duke Heart for Honduras
El Pais (Hn)
Grupo Financiero Atlántida dona L 5.7 millones para brigada médica
May 16 — Monique Starks
The Clemmons Courier
History in the making: First drone delivery of an AED
May 17 — Senthil Selvaraj
HealthDay
Male, Female V1421 Carriers Face Similar Risk for Heart Failure Hospitalization
Duke Heart Pulse — May 12, 2024
Chief’s message:
Hope you all have a happy Mother’s Day, and for those of you having kids graduate from college and or graduate school this weekend – congratulations.
This week’s Pulse highlights several of the things that make Duke a special place to work. Stories include teams developing breakthrough research findings (Senthil Selvaraj and others), innovative NHLBI funded research (Monique Starks and team with drone delivery AEDs for cardiac arrest survival), AHA go red for women with Camille Frazier-Mills as a woman of impact, and finally shout outs to clinical research coordinator Kim Biever and Cathy Ritchie from our cardiac rehab team on helping increase access to care.
Highlights of the week:
ESC-HF: Common Genetic Variant Among Black Americans Leads to Significant Increases in HF, Death at Individual and Population Levels
A genetic variant carried by 3-4 percent of self-identified Black Americans increases the risk for heart failure and death similarly in men and women, contributing to a significant decrease in longevity at the population level, according to a new study led by researchers at Duke University School of Medicine and Brigham and Women’s Hospital. The findings show that individuals who carry the amyloidogenic V142I transthyretin variant are at significantly increased risk for heart failure hospitalization beginning in their 60s, with an increased risk for death beginning in their 70s. Nearly half a million currently living carriers above age 50 will collectively lose 1 million years of life due to the variant.

The study results were presented earlier today by Senthil Selvaraj, MD, MS, MA, advanced heart failure cardiologist at Duke, as part of late-breaking science at the European Society of Cardiology’s Heart Failure Congress 2024 in Lisbon, Portugal; the findings were simultaneously published online in JAMA. Additional Duke authors on the publication include Svati H. Shah, MD, MHS; Robert J. Mentz, MD; and Michel G. Khouri, MD.
The V142I variant causes transthyretin, a protein in the blood, to misfold leading to deposits of abnormal amyloid protein in the heart and other parts of the body. In the heart, these deposits cause the muscle to become thick and stiffened, a condition known as cardiac amyloidosis, which can ultimately lead to heart failure. Originally considered a rare condition, researchers are increasingly finding that cardiac amyloidosis is underdiagnosed and underrecognized — particularly among Blacks.
The researchers pooled data from self-reported Black participants in four NIH-funded studies in the U.S. (ARIC, MESA, REGARDS and Women’s Health Initiative). Altogether, the team examined data from 23,338 self-reported Black individuals, 754 (3.23 percent) of whom carried the V142I genetic variant.
The team found that carriers of V142I had an increase in their 10-year risk for heart failure (HF) hospitalization by age 63 and risk for death by age 72, while individual carriers with the V142I variant live 2-2.5 years less on average than expected. The risk was more prominent for heart failure with reduced ejection fraction (HFrEF) hospitalization compared with heart failure with preserved ejection fraction (HFpEF) hospitalization. The variant’s contribution to HF risk increased substantially with age but was not itself increased by other known risk factors such as diabetes and hypertension.
“Since 3-4 percent of self-identified Black individuals in the United States carry this variant, a significant number are at elevated risk for developing cardiac amyloidosis, being hospitalized for heart failure, and dying several years earlier than expected,” said Selvaraj, first author of the study. “With our improved understanding of the risks with the variant, future efforts to increase disease awareness and ultimately connect carriers with the disease to effective therapies will be important.”
The team also showed that female and male carriers of the variant were equally at risk, contrary to some previous clinical studies showing that men were more affected. Using these epidemiological data, this suggests that women are likely underdiagnosed with the condition.
The research showed that variant carriers on average died 2 to 2.5 years earlier than non-carriers. With approximately 48 million Americans self-identifying as Black, approximately 1.5 million people are estimated to carry the variant. Of those over age 50, which is about half a million people, the team estimates that nearly a million years of life will be lost due to the variant in this natural history study.
Although the association between the V142I variant and HF has been previously described, precise estimates of how the variant increases risk were unclear until now. The good news is the increasing availability of treatment options for cardiac amyloidosis.
“There is currently one approved targeted therapy with a number in the pipeline,” says Selvaraj, adding that he and his colleagues believe earlier identification of people who carry the V142I variant and providing appropriate therapies might decrease the risk of HF and dying. However, more research is needed to show whether early implementation of targeted treatments actually leads to decreased risk of disease.
“We found a relatively large magnitude of disease burden in the U.S., certainly at the population level, but the impact at the individual level is notable as well,” he says. “It’s important to think about diagnosing this disease relatively early on, since once it evolves to later stages, it becomes more challenging to treat and therapies may be less effective. Further, as you get older, the risk of the disease increases substantially. Therefore, we should be considering the diagnosis of this inherited form of cardiac amyloidosis earlier than we have before – closer to early 60s, rather than their 70s and 80s.”
The findings also indicate clinicians should think more broadly about those who are hospitalized with HF as perhaps having amyloid.
“Amyloid cardiomyopathy is more often associated with HFpEF. Our findings demonstrate that, in hospitalized settings, we should be looking at individuals regardless of ejection fraction,” Selvaraj added. “Since hospitalization for HF is an advanced marker of the disease, and the ejection fraction tends to fall over time with cardiac amyloid, it may be unsurprising that more frequently carriers have a reduced ejection fraction by the time they are hospitalized.
“Additionally, we should pay more attention to this disease risk in women. One challenge with cardiac amyloid is we often look for thick walls in the heart. Women in general have thinner walls than men, so using certain thresholds of wall thickness to diagnose disease, without this consideration, may cause us to overlook women who indeed have the cardiac amyloid.”
In future studies, the researchers plan to investigate why some, but not all, carriers of the V142I variant develop cardiac amyloidosis.
Note: This paper has been selected by JAMA as their featured article of the week and is accompanied by two editorials: Heart Failure in African American Individuals, Version 2.0 by Clyde W. Yancy, MD, MSc; and Addressing Health Disparities—The Case for Variant Transthyretin Cardiac Amyloidosis Grows Stronger by Mathew S. Maurer, MD; Edward J. Miller, MD, PhD, and Frederick L. Ruberg, MD.
Duke Heart Team Heads to Honduras for Medical Mission
A 42-member medical team representing Duke Heart departed yesterday, May 11, on a surgical mission trip to Honduras as part of our Duke Heart in Honduras program. This year we have adult and pediatric teams heading to care for patients in need of cardiothoracic interventions. Our teams will perform all intraoperative and postoperative care to support our Honduran partners in providing surgery at no cost to patients who would otherwise not be able to afford it.
Forty surgeries are planned, 15 of which will be with pediatric patients in need of atrial septal defect closures, ventricular septal defect closures, AV canal defects, and Tetralogy of Fallot. Most adult patients our Duke team will see need aortic valve and mitral valve replacement. One congenital patient with an anomalous left coronary artery from the pulmonary artery (ALCAPA) defect will undergo reimplantation. Another will be treated for a large atrial myxoma.
The mission is in partnership with Hugo Orellana, MD, an adult cardiothoracic surgeon based at Honduras Medical Center, and with Victor Paz, MD, a pediatric cardiothoracic surgeon based at Hospital Maria. Both hospitals are located in the city of Tegucigalpa, the capital of Honduras.
The Duke Heart for Honduras 2024 team includes:
Cardiothoracic surgeons: Drs. Adam Williams, Jacob Schroder, Joseph Turek, and Doug Overbey; Cardiac anesthesiologists: Drs. Brandi Bottiger, Alina Nicoara, and Natalia Diaz-Rodriguez; Pediatric cardiac ICU attendings: Drs. Jennifer Turi and Jennifer Sherwin; CT fellows: Drs. Alejandro Murillo, Navin Vigneshwar, Jason Pang, Kathryn Pearson, and Ethan Garrigan; pediatric cardiac anesthesiologist Dr. Michael Greenberg; CT Surgery residents: Drs. Rebekah Boyd and Hiba Ghandour; CTICU, CTOR and critical care nurses and APPs: Bryan Hampton, Adeline Kranzburg, Timothy Matusz, Eric Velasquez, Chelsey Weinbrecht, Nicole Garcia, Cheyenne English, Mambo Kwaambwa, Michelle Figuerres, Figz Figuerrez, Tina McEachin, Aireen Vergara Casale, Audrey Sakae, Dorothy McVay and Danielle Wood; Perfusionists: Felicia Shugars, Amy Evans, Robert Degiosio, Katharine Nanry and Julie Walker; Respiratory therapist Chris Lappe; Biomedical engineer Brian Gore; Research lab member (and Honduran physician) Alejandro Alvarez Lobo, and medical students Cathlyn Medina and Lauren Parker.
Our Duke team will be joined by five medical professionals from Massachusetts General Hospital, including four attending physicians, Drs. Eriberto Michel, David D’Alessandro, Peter O’Chieng, and Robin Schiller and perfusionist Kenneth Shann. Also joining our team is a perfusion student, Cristina Parra, sponsored by the International Perfusion Association (IPA), and Bryan Lich, president of the IPA.
The team is supported, in part, by a grant from the Thoracic Surgery Foundation, the philanthropic arm of the Society of Thoracic Surgeons (STS). The grant funding of $35,000 is part of the Every Heartbeat Matters Award given to Dr. Adam Williams during the STS 60th annual meeting held in January 2024. The funding was made possible through the support of the Edwards Lifesciences Foundation and will be used to cover the airfare costs for all team members.
We are pleased to support these Duke team members and wish them great success!
Forsyth County NC Runs 1st Test of AED Drone Delivery
 Congratulations to Monique Starks, MD, associate professor of medicine in cardiology, and her AED Drone study team! Forsyth County, NC was the first county to sign on for the partnership with Duke for feasibility testing of AED drone delivery to cardiac arrest bystanders. The Forsyth County Sheriff’s Office and Forsyth County Emergency Services conducted a test launch this week as part of an emergency management drill for cardiac arrest held at Agape Church in Clemmons, NC.
Congratulations to Monique Starks, MD, associate professor of medicine in cardiology, and her AED Drone study team! Forsyth County, NC was the first county to sign on for the partnership with Duke for feasibility testing of AED drone delivery to cardiac arrest bystanders. The Forsyth County Sheriff’s Office and Forsyth County Emergency Services conducted a test launch this week as part of an emergency management drill for cardiac arrest held at Agape Church in Clemmons, NC.
Starks is the principal investigator on the American Heart Association research grant “Developing and Testing Drone-Delivered AEDs for Cardiac Arrest in Rural America”. Her co-investigators include Dan Mark, MD, Hayden Bosworth, PhD, Audrey Blewer, PhD, MPH, and Hussein Al-Khalidi, PhD.
Starks is the first investigator in the U.S. to be funded by the National Institutes of Health to explore the development of a drone network that is capable of delivering AEDs to bystanders at an out-of-hospital cardiac arrest emergency.
Congratulations to all involved in this important work!
Frazier-Mills Celebrated at Go Red! Event
The Triangle’s annual Go Red for Women Evening in Red event was held on Friday evening, May 10, at the Raleigh Convention Center. The celebration
celebration  recognizes survivors of heart disease and their family members and, via fundraising, supports vital research efforts for the American Heart Association.
recognizes survivors of heart disease and their family members and, via fundraising, supports vital research efforts for the American Heart Association.
The evening included dinner, dancing, a silent auction, and honoring each of the 2024 Triangle Women of Impact including our very own Camille Frazier-Mills, one of the finalists! Duke Heart’s service line vice-president Jill Engel and cardiology fellowship program director, Anna Lisa Chamis, MD were both on hand for the festivities and to support Camille.
Kudos to Ritchey & Cardiac Rehab Team!
Kudos to Cathy Ritchey for her tenacious work on behalf of our cardiac rehab patients. Ritchey proactively connected with representatives at Aetna regarding Cardiac Rehab (CR) coverage. Thanks to her efforts, Aetna has updated its CR coverage and will now cover the CPT code for non-continuous telemetry CR starting June 9. Awesome!!!
According to Erica Rao, this has been a barrier to enrolling Aetna patients into our Duke CR program. Ritchey, she says, “maintains a close watch on CR insurance guidelines and read that Aetna was updated theirs. After connecting to the Duke physician liaison with Aetna and the Revenue Integrity team, our team will now be able to enroll all Aetna patients, not just those with Duke Aetna insurance.”
Bill Kraus adds, “This is a huge well-earned victory for our CR program and the hospital to tear down barriers to patient care.”
Way to go, Cathy!!!
Shout-out to Biever
We received a terrific note this past week from Andrew Wang, MD, vice chief for clinical affairs for the division of cardiology:
“I highly commend Kim Biever, a clinical research coordinator in our cardiology clinical trials group. I have worked with her for the past 3-4 years on a randomized trial of mavacamten for obstructive hypertrophic cardiomyopathy (HCM) and its long-term extension study. In addition to her help in achieving a high enrollment in this study, her conscientiousness, efficiency, and communication have made the experience very productive and enjoyable.
“She is extremely well-organized and plans well for the expected and unexpected issues in a trial. She is often the “first call” person for our trial patients, even for matters unrelated to the study protocol, and manages these with compassion and professionalism. Most impressively, as our patients have transitioned from study treatment to commercial drug treatment, her dedicated work and commitment have helped to reduce any gaps in their treatment.”
Way to go, Kim!!!
Kudos to Duke HF Symposium Planning Team
A shout-out to Marat Fudim, Stephanie Barnes, Rob Mentz, Richa Agarwal, and Christy Darnell for a very successful HF Symposium last weekend. It was our first since the pandemic and it was a hit – our best turnout yet. Great job, everyone!
Upcoming Events & Opportunities
- May is American Stroke Month and Asian American and Pacific Islander Heritage Month
- May is Duke Health’s inaugural Team Member Appreciation Month
- May 12-19 is National Hospital Week
- Culture Pulse survey deadline extended to Thursday, May 16.
Cardiology Grand Rounds
May 14: Teaching, Quality Improvement, and Wellness in the ICU with Daniel Loriaux. 5 p.m., DN 2002 or via Zoom.
May 21: Capturing the Left Bundle: Insights Into Conduction System Pacing with Ilia Shadrin. 5 p.m., DN 2002 or via Zoom.
May 28: The Ross Operation — The Ultimate Aortic Valve Replacement? with Ziv Beckerman. 5 p.m., DN2002 or via Zoom.
All Duke Cardiology Grand Rounds recordings are housed on Warpwire. To access recordings please visit:
NET ID and password are required. Enjoy!
CD Fellows Core Curriculum Conference
May 15: HF/Txp Case Presentation with DaMarcus Ingram. Noon, DMP 2W96 (in-person only).
May 17: EKG Review with Neil Freedman. Noon, Zoom only.
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, on Wednesdays, will be considered for weekend inclusion.
Duke Heart in the News:
May 2 — Neha Pagidipati
Cardio Nerds
May 3 — Marat Fudim
Web MD
What’s Behind Major Rise in Heart Failure Deaths?
May 3 — Duke University Hospital
Becker’s ASC Review
Meet the leaders of the 3 best hospitals in North Carolina for cardiac surgery
May 3 — Thomas Povsic
Medscape
In Angina, Gene Therapy Coaxes Heart Vessel Growth
May 3 — Duke Raleigh, Duke University Hospitals
Healthgrades
Healthgrades Reveals Top U.S. Hospitals for Patient Safety in 2024
May 4 — Nina Nouhravesh
The National Herald (Greece)/Associated Press
Eggs Regain Their Place as a Staple of Healthy Eating
May 6 — Harry Severance
MedCity News
Stark Law Crackdown Jacks Up Fines, Settlements and Physician Pressures
May 7 — Stephen Greene
tctMD
SGLT2 Inhibitor Added to GDMT in Functional MR May Obviate Need for TEER
May 8 — Jonathan Piccini
Verywell Health
Why Is AFib More Common in Younger Adults Now?
May 8 — Monique Starks
WFMY (CBS 2)
AED taking flight, Forsyth County leads U.S. with drone delivery program
May 9 — Duke University and Monique Starks
WGHP (Fox 8) Greensboro, NC
Area sheriff’s department (Forsyth County) adds drone delivery AEDs
May 9 — Dawn Coleman
Vascular Specialist
The top 10 most popular Vascular Specialist stories of April 2024
Duke Heart Pulse — May 5, 2024
Duke Heart Pulse – May 5, 2024
Chief’s message:
As the spring season is in full effect – hopefully you all had some time outside with friends and family. There were also many faculty and fellows presenting at conferences this weekend – the national cardiovascular interventional society (SCAI) had its national meeting in California this weekend with several of our interventional faculty both presenting and being part of the national organizations leadership. There were key talks by Jennifer Rymer, Raj Swaminathan, Ton Gutierrez, Schuyler Jones and many others. Congratulations to Sunil Rao, past SCAI president and James Hermiller – in coming SCAI president.
Heart Failure Symposium is back. This weekend the Duke Heart group had its first Heart Failure symposium after COVID (prior in-person symposium was 2019). By all accounts it was a success – with over 220 registered attendees, wonderful speakers from around the country, and lots of interactive real-world management of heart failure patients from prevention to complex management. Some photos from the event are shown here.






Highlights of the week:
Celebrating Perfusionists & Duke’s 2nd Pillar Award
Happy May, everyone! Yes, today is the ever-popular Cinco de Mayo, but it’s also day one of Perfusion Week — a time to recognize the incredible efforts of perfusionists across the U.S.! These vital members of our cardiothoracic surgical team do remarkable things each day for our patients. So, if you happen to be celebrating with your favorite Mexican foods and beverages, consider including a toast to our amazing Duke Perfusionists!

The Duke Perfusion team recently earned its second Pillar Award for Perfusion Excellence from the American Society of Extracorporeal Technology (AmSECT). Their first was awarded in 2021, the inaugural year of the AmSECT Pillar, which is a designation for individual perfusion departments that demonstrate excellence as displayed in several key areas including organized orientation and training, QA/QI process, continuing education and performance evaluation, development of institutional protocols and adherence to AmSECT Standards and Guidelines, employee education and commitment to the field of perfusion.
Duke has one of the largest and most highly-skilled perfusion teams in the U.S. Each member of the team is certified by the American Board of Cardiovascular Perfusion, licensed by the North Carolina Medical Board, and most team members hold advanced degrees and credentials.
In addition to proficiency in cardiopulmonary bypass (operating the heart-lung machine during cardiothoracic surgery), Duke perfusionists become further specialized to support a variety of needs across the hospital. We have a dedicated team of pediatric perfusionists, a specialty team for Duke Regional Hospital, an Extra-Corporeal Life Support (ECLS) team that assists with cannulating and retrieving patients from referring hospitals, a team that provides apheresis in the OR, and a team trained in use of the Transmedics Organ Care System, which has helped increase the donor pool for Duke’s Heart Transplant program.
Congratulations to our perfusionists!
Nurses Week 2024
 It’s also Nurses Week 2024 (May 6-12)! On behalf of Duke Heart, a big shout-out to all of our incredible nurses for their professional accomplishments and contributions in caring for Duke Heart patients over the past year.
It’s also Nurses Week 2024 (May 6-12)! On behalf of Duke Heart, a big shout-out to all of our incredible nurses for their professional accomplishments and contributions in caring for Duke Heart patients over the past year.
Duke Heart Nurses are foundational to Duke’s ability to provide compassionate, innovative cardiac care throughout our clinics and at the bedside. Each of our nurses cares for patients with complex cardiovascular needs and partners with clinicians and other team members as we engage in research clinical trials; teach patients and family members about the care they are receiving; participate in quality improvement initiatives locally and nationally, as well as speak or serve as educators at professional meetings.
Our Duke Heart nurses are amazing – individually and as a team. Without their partnership, none of our overall team accomplishments would be possible! Thank you for the work you do, your tremendous compassion for our patients and their families, and your compassion for one another and our community.
The Duke Heart Nursing team possesses unmatched talent, dedication, and teamwork, exemplifying living the Duke Values. In short, Duke Nurses rock!
Kudos and thank you – enjoy Nurses Week!
Duke Heart Experts Featured at NCUS
The North Carolina Ultrasound Society (NCUS) held its 43rd Annual NC Medical Ultrasound Symposium in Raleigh from April 19-21 at the Crabtree Courtyard Marriott.
Duke Heart was well-represented in terms of presenter expertise and well-supported in terms of attendees. Speakers included Joe Kisslo, MD (Keynote speaker); Michel Khouri, MD; Richie Palma, instructor and program director of Duke’s Cardiac Ultrasound Program; Alicia Armour, HCA of Triangle Heart; Ashlee Davis, chief technologist, and Rachel O’Brien and Diana Masterson, cardiac sonographers.



Richie Palma and cardiac sonographer Jon Owensby are both on the Board of Directors for the NCUS.
Great work, everyone!
Pending Unit Moves – July 2024
The Duke University Hospital 100 bed tower, floors 6 through 9, has been renovated and will reopen in the summer of 2024! Several Heart patient care units will be relocated to allow for the renovation of floors 2 and 3 in the North 100 tower. Unit 3100 will relocate to 6100 (31-bed unit) on July 22 and 3200/7200 will relocate back to 7100 (31-bed unit) on July 23.
There will be no change in the patient populations these units care for. Unit 6100 was specifically chosen because of its proximity to the 6E/CT Step-down Unit.
More details, including office relocations, will be announced closer to the move date. We thank everyone in advance for their support and patience.
Final Week to Complete Culture Pulse Survey
If you have not yet done so — please participate in the Duke Health Culture Pulse survey. It is available to all Duke Health team members until May 13. The brief, 18-question survey is confidential and mobile-friendly, and it’s short – you can do the whole thing in less than five minutes.
This year’s survey is focused on Duke’s commitment to putting people first by asking questions, listening, and seeking diverse perspectives. The Culture Pulse survey aims to strengthen the employee experience – for all of us – but participation is critical!
Thank you for sharing your invaluable insights and for all that you do to make Duke Health an extraordinary place to work, learn, and receive care.
The link to the survey was sent to everyone via email on 4/22. Check your inbox and please make your voice heard!
Duke Hospitals Continue to Earn ‘A’ Grades on Leapfrog Safety Assessments
For 12 consecutive grading periods, Duke University Hospital, Duke Regional Hospital, and Duke Raleigh Hospital received top scores for patient safety from The Leapfrog Group.
The “A” scores for Leapfrog’s spring 2024 survey are part of the group’s Hospital Safety Grades Assessment, issued to hospitals every six months. This is the only hospital ratings program focused exclusively on preventable medical errors, infections, and injuries that kill more than 500 patients a day nationally.
Duke Health’s three hospitals were among nearly 3,000 hospitals surveyed across the country. Only 29% of hospitals nationwide achieved an “A” hospital safety grade for the spring 2024. In North Carolina, Duke University Health System hospitals were among 38 hospitals to achieve the grade.
“Our steady ‘A’ grades from Leapfrog prove that we are dedicated to putting patients first at all three Duke Health hospitals,” said Thomas Owens, MD, executive vice president and chief operating officer of Duke University Health System. “We value the clinicians, staff, and volunteers who provide excellent care and make sure patients are safe.”
The Leapfrog Group is an independent nonprofit organization led by the nation’s leading employers and private healthcare experts. Twice each year, it collects and analyzes data based on over 30 national performance measures of errors, accidents, injuries, and infections, as well as systems hospitals have in place to prevent harm. The letter grades assigned to hospitals help people make informed decisions to protect themselves and their families.
Comparisons of hospital scores locally and nationally are available at https://www.hospitalsafetygrade.org/.
Duke’s Total Compensation Program
Duke began mailing all full-time faculty and staff their annual personalized benefits statements this week. These are going to home addresses.
Did you know that, on average, Duke invests about $250 in benefits for every $1000 of pay? Each of us can see what Duke’s investment in pay and benefits looks like for us by reviewing our benefits statement. Please take a few minutes to review the materials to ensure you’re taking full advantage of the benefits and services available to you and your family members.
Learn how five of our Duke colleagues have been helped by a variety of Duke benefits as part of their total compensation package: Beyond Pay: Unique Duke Employee Benefits for Unique Needs.
Have a great week, everyone!
Upcoming Events & Opportunities
- Culture Pulse 2024 survey period through May 13
- May is Asian American and Pacific Islander Heritage Month

- May is Duke Health’s inaugural Team Member Appreciation Month
- May 5-11 is Perfusion Week
- May 6-12 is Nurses Week
- May 12-19 is National Hospital Week
Cardiology Grand Rounds
May 7: Bridging the Gap: A Closer Look at Care Fragmentation and Health Disparities in PAD with Dennis Narcisse. 5 p.m., DN 2002 or via Zoom.
All Duke Cardiology Grand Rounds recordings are housed on Warpwire. To access recordings please visit:
NET ID and password are required. Enjoy!
CD Fellows Core Curriculum Conference
May 8: ABIM Review. Noon, DMP 2W96 (in-person only).
May 10: Update on TAVR with Todd Kiefer. Noon, Zoom only.
Working Effectively Across Generations
June 3: Working Effectively Across Generations with Hile Rutledge, of Otto Kroeger Associates (OKA). 8:30 a.m. to Noon. Great Hall, Trent Semans Center. Sponsored by Duke School of Medicine.
Registration required: https://medschool.duke.edu/blog/register-now-working-effectively-across-generations
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
April 25 — Jonathan Piccini
Health Central
How Cardioversion Can Help Your Heart
April 26 — Marat Fudim
tctMD
Heart Failure Mortality Higher Now Than in 1999
May 1 — James Watson (hospitalist program)
The Hospitalist
Apixaban Reduces Risk of Stroke or Systemic Embolism in Subclinical AF
May 1 — Cepeda Mora (hospitalist program)
The Hospitalist
Semaglutide in Patients with HFpEF and Obesity
May 1 — James Watson
The Hospitalist
High Frequency of AF Recurrence in Hospitalized Patients with New-onset AF
May 1 — Mark Chandler (hospitalist program)
The Hospitalist
Frailty Assessment and Perioperative Adverse Cardiovascular Events After Noncardiac Surgery
May 1 — Chantell Evans (cell biology)
Nature/News & Views
Cells destroy donated mitochondria to build blood vessels
May 1 — Amanda Randles (biomedical sciences)
Business Insider
May 1 — Duke Health
WNCN/CBS-17 (Raleigh/Durham)
Raleigh/Cary metro has some of the safest hospitals in the country: New study
May 3 — Robert Mentz
Perishable News
Recent Comments