Highlights of the week:
Duke Heart Team Welcomes Spahillari
Please offer a warm welcome to Aferdita Spahillari, MD, MPH, who joined the Duke Heart team as associate professor of medicine in cardiology on August 30. She is now a member of our Heart Failure service and will co-lead a Guideline-Directed Medical Therapy (GDMT) program with Dr. Stephen Greene. Spahillari has joined us from Massachusetts General Hospital (MGH) and Harvard Medical School, where she had been on the faculty since 2017, and served as Director of the GDMT Clinic at MGH for the past two years.

Spahillari is a native of Albania who moved with her family to the Worcester, MA area when she was a teenager. She earned her MD at Tufts University School of Medicine, where she received both the William Dameshak Award in Internal Medicine as well as the Glasgow-Rubin Citation for Academic Achievement in 2010; she earned an MPH in clinical effectiveness from the Harvard School of Public Health.
Spahillari completed internal medicine training at the University of California San Francisco, a cardiology fellowship with Beth Israel Deaconess Medical Center, and an advanced heart failure and transplant fellowship at Tufts.
“For as long as I can remember, I had the desire to become a doctor,” said Spahillari. “As I went into training, I was drawn to cardiology. It’s one of the specialties I found most interesting because of the physiology, and because it covers a whole spectrum of diseases with a wide variety of treatment options. I almost went into interventional cardiology because I really enjoyed doing procedures, but ultimately, I had mentors and inspirational teachers in heart failure who led me in this direction, and I fell in love with it as well.”
She says heart failure patients are a population she really enjoys. “It’s very fulfilling to follow the patients along their journey and to care for them when they’re really sick, but also see them get better with the treatment options we have to offer.”
If there was something she wished more patients and families knew, it would be for them to recognize “that heart failure is quite common, and that we have a great deal of treatment options and advanced therapies to offer. My goal is to grow our guideline-directed medical therapy program and get patients on optimal medical therapies as early as possible, or, even if they are in later-stage heart failure, get them onto the optimal therapy in order to improve their heart failure symptoms and heart function.”
With the GDMT program, Spahillari and Greene will unite the efforts of the nurse practitioners working in the HF Same-Day Access Clinic with the efforts of the Duke pharmacy team in order to further develop the program and expand access to more HF patients across Duke. She will see patients at Duke South, round on the HF service, read echocardiograms, and she expects to see clinic patients in Raleigh a couple of times per month.
Aferdita and her husband, Bobby Guadagno, have two sons — JD and Beau who are four and two respectively. The family is excited to be in North Carolina, with family nearby in Charlotte and they look forward to all that Durham and the surrounding areas have to offer.
Welcome, Aferdita! We are so pleased to have you on our team!
Heart Walk: Next Sunday!
We are just one week away from the American Heart Association Triangle Heart Walk – next Sunday, October 8th. If you have registered great — if you have not – it’s not too late.
We are happy to report that Duke is still the number one fundraiser throughout the Triangle, but we also know others are nipping at our heels. Let’s rally hard this week to show our Duke Heart pride, and support our partners at the Triangle AHA. Register for a team here. 
Feel free to join any team (donation or not) and come out and enjoy the walk and help us increase awareness of heart disease. Manesh Patel has a team called ‘Duke Heart’ with team members that include several heart patients and others who will join the walking; Jill Engel has a team called ‘Got Heart!’ – and there are many other great groups across DUHS and the School of Medicine.
The event will occur at PNC Arena, 1400 Edwards Mill Road, Raleigh. Check-in begins at 11 a.m.; the walk begins at Noon. You can bring kids, dogs, and friends to the event. Our annual Duke team photo for all Duke team members will take place at approximately 11:25 a.m. Manesh advises we all be on the lookout for Chris Granger – he is often there helping organize everyone for the photo.
Duke Health was unable to provide t-shirts this year, so please wear your favorite Duke Blue t-shirt to the event! It does not have to say ‘Duke’ but please make sure it’s a royal blue. Thank you!!!
Pagidipati Featured in Duke SOM’s Magnify
Neha Pagidipati, MD, MPH is featured in the Sept. 28 issue of Magnify, the Duke School of Medicine online magazine:
The Doctor Who Wants to Change How We Treat Cardiovascular Disease

Cardiovascular disease is the number one killer of people in the United States and worldwide. Yet physicians often do not prescribe evidence-based medicines that could change those statistics.
Neha Pagidipati, MD, MPH, associate professor of medicine in cardiology at Duke University School of Medicine, wants to do something about that.
“There are therapies that have a ton of evidence [showing they] keep people from developing recurrent disease,” said Pagidipati, a cardiologist who specializes in prevention. “They are just not being used appropriately. That has to change on population level.”
In particular, there are three types of FDA-approved drugs that can reduce the risk of heart attack or stroke among the growing number of people who have both diabetes and cardiovascular disease, a combination often referred to as cardiometabolic disease. The three classes of drugs treat high blood pressure, high blood sugar and high cholesterol, which are all risk factors for both diabetes and cardiovascular disease.
“These are not fair diseases,” Pagidipati said. “They are inequitably targeting patient populations that don’t have the resources to combat these chronic illnesses. That’s part of what motivates me—it’s a public health and a social justice issue.”
In a recent study called COORDINATE Diabetes, Pagidipati and her colleagues tested a strategy in clinics nationwide to encourage physicians to prescribe all three of these types of drugs to their patients with both diabetes and a specific type of cardiovascular disease called atherosclerosis or hardening of the arteries.
In the randomized controlled trial, the clinics that followed the multifaceted strategy successfully increased the percentage of patients who were prescribed all three medicines. Half of the participating medical centers received the intervention, and the other half were business-as-usual.
At the beginning of the trial, less than 3% of the 1,000 patients were prescribed all three drugs. By the end of the trial, that percentage had risen to 37.9% in the intervention group.
“It has major implications about what methodologies we can use to improve the way clinicians are providing care to this very high-risk population,” Pagidipati said. “That care promotes resilience.”
The intervention was designed to encourage coordination among the multiple specialists who see patients with diabetes and heart disease. In the absence of such coordination, it can be difficult for a cardiologist to prescribe a drug targeting blood sugar or for a diabetes specialist to prescribe a drug targeting blood pressure. The strategy called for health systems to create multidisciplinary teams to identify and remove barriers to coordinated care.
The intervention also provided educational materials to both physicians and patients and gave the clinics regular feedback about how well they were doing in prescribing the drugs.
The study was designed to measure an increase in prescriptions, not cardiac events such as stroke or heart attacks. However, the investigators did find fewer cardiac events (23) in the intervention group compared to the business-as-usual group (40). While that difference was not statistically significant, it was encouraging.
Pagidipati hopes the results of the study will inspire more health systems to adopt strategies to improve the health of their patients.
At Duke, Pagidipati is taking coordinated care to a new level. She started a clinic a few years ago where patients with advanced cardiometabolic disease see a team of multidisciplinary specialists, including cardiologists, endocrinologists, nephrologists, hepatologists, and pharmacists.
“The goal is to provide coordinated, state-of-the-art comprehensive preventative care for the highest risk patients in the health system,” she said.
Pagidipati’s goal is to improve care not just for patients at Duke, but for patients everywhere. She is planning a randomized trial to measure the effectiveness of the strategies used in her clinic. If her multidisciplinary team helps patients stay healthier longer, she’ll be looking for ways to spread the word and influence the standard of care nationwide and beyond.
“At the end of my career,” she said, “I would really like to say that we did something to help people combat cardiometabolic disease, both locally—at Duke—and at large—regionally, nationally, internationally.”
Heartfelt Gratitude: Duke Patient Contributes to OneDukeGen Study
By the time Roger Neighborgall was 66 years old, his heart was wearing out. Without an effective way to pump blood through his body, Neighborgall was experiencing circulatory problems and suffering heart failure.
He had been told he had up to a month to live, but in January 2021, Duke University Hospital provided him with a new lease on life —a heart transplant
Almost three years later, Neighborgall is thriving and looking to give back to the place that gave him the most precious gift of all: time.
“You get a sense of connection [having] somebody else’s heart in your chest,” he said, “and I feel an overwhelming sense of connection with Duke.”
So when Neighborgall was asked during a recent transplant checkup if he would consider joining OneDukeGen, a precision medicine study that will analyze DNA from 150,000 consented Duke patients, he didn’t hesitate. “Before it even came out of their mouths,” Neighborgall said, “I knew I was going to join.”
As part of the new Center for Precision Health and in partnership with nference, a science-first software company, OneDukeGen will use genetics and precision medicine to make scientific discoveries focused on improving the health and well-being of Duke patients.
“OneDukeGen is focused on using genetic and other scientific discoveries and translating them to patient care in less time,” said Svati Shah, MD, Ursula Geller Distinguished Professor of Research in Cardiovascular Diseases and principal investigator for OneDukeGen. “Because of participants like Roger, we will be able to make discoveries to improve prevention and treatment of diseases and enhance health.”
Eligible Duke patients will receive an invitation to join the study either during a previously scheduled appointment or through their Duke MyChart portal. Recruitment will be ongoing over the course of the six-year study. Participation is currently limited to established Duke patients.
Once enrolled, participants will provide a blood or saliva sample. Researchers will then be able to analyze DNA, RNA, and other factors to investigate a variety of diseases and conditions. Participants will receive their genetic testing results if they have DNA differences that increase the risk for preventable or treatable health conditions. They may also receive recommendations for follow-up care, such as annual screenings, medication, or preventative surgeries.
Neighborgall often thinks of all the people at Duke who have helped him on his journey. “I owe them so much, and if some of my some of my DNA can help not only at Duke Hospital but maybe, in the future, other hospitals, of course I’ve got to be part of it.”
Visit sites.duke.edu/onedukegen to learn more about the OneDukeGen study and how Duke patients will be invited to participate.
Shout-out to Glower
We received a terrific note about cardiothoracic surgeon, Don Glower, from Press Ganey HCAHPS regarding the great care he and his team provided recently to a patient at Duke Hospital:

“Dr. Glower is wonderful with great staff!!” – a grateful patient (name withheld for privacy)
Dr. David Gallagher, chief medical officer, added, “Thank you for the high quality and compassionate care you provide to patients!”
Well-deserved, Dr. Glower!
Kudos to Medlock

Congratulations to Nick Medlock for completing the Society of Diagnostic Medical Sonography (SDMS) Foundation Emerging Leaders Program! This is a fantastic accomplishment and an honor to have been selected. The SDMS Foundation Emerging Leaders Program annually invites a cohort of students and recent graduates to be mentored as future leaders in the field of sonography and with the SDMS. Program participants participate virtually in a variety of leadership education opportunities that are designed to engage them in meaningful dialogue and projects related to the future of the profession and leadership volunteerism.
Medlock is a recent graduate of the Duke Cardiac Ultrasound Certification Program and earned the American Society of Echocardiography Waggoner award in 2022.
Way to go Nick!
Shout-out to Tong & team

This week we received a note from David Gallagher, chief medical officer, regarding thoracic surgeon Dr. Betty Tong and her team. The note was submitted to Press Ganey HCAHPS:
“Dr. Tong and her team are absolutely the best. My nurse Rosalee was awesome.” – a grateful patient (name withheld for privacy)
Dr. Edward P. Chen, division chief for cardiovascular and thoracic surgery added, “Dr. Tong provides outstanding service every day to her patients and it is nice to see her recognized in such a complimentary fashion.”
Well-deserved, Betty!
DIHI Innovation RFA 2024 is Now Open
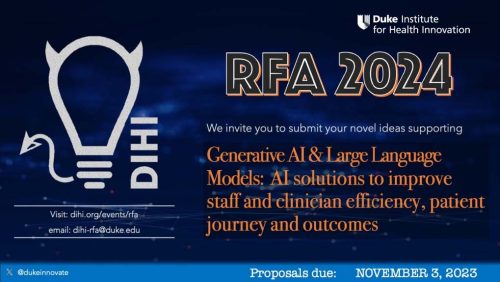 The Duke Institute for Health Innovation (DIHI) has announced their next annual Request for Application (RFA) for selecting and implementing innovative solutions in our clinical enterprise. The proposals should address actual and important problems encountered by care providers, patients and their loved ones, and represent urgent health challenges nationally.
The Duke Institute for Health Innovation (DIHI) has announced their next annual Request for Application (RFA) for selecting and implementing innovative solutions in our clinical enterprise. The proposals should address actual and important problems encountered by care providers, patients and their loved ones, and represent urgent health challenges nationally.
For the 2024 funding cycle, they are specifically interested in the following topic:
Generative AI & Large Language Models: AI solutions to improve staff and clinician efficiency, patient journey and outcomes
Please visit the Innovation RFA web page for additional information, to download an info packet, and to see the timeline for 2024 projects. The deadline for submitting applications is November 3, 2023.
All proposals are required to have a DUHS operational lead as a co-sponsor to be accepted for review.
If the DIHI team can be of any assistance to you in the formulation of ideas or connections, please contact Suresh Balu. The DIHI team looks forward to your innovative solutions!
Upcoming Events & Opportunities
- National Hispanic Heritage Month runs through Oct. 15
- October is Medical Ultrasound Awareness Month as well as National Pharmacists Month
- Masking is strongly recommended throughout all clinical areas during respiratory virus season, from now through early March.
Cardiology Grand Rounds
Oct.3: Left Atrial Appendage Closure with Kevin Jackson. 5 p.m., DN 2002 or via Zoom.
CD Fellows Core Curriculum Conference/Fellows Conference
Oct. 6: Fellows Forum with Joseph Lerman. Noon, DMP 2W96, in-person only.
Call for Applications: 2024 Leadership Programs
The Office for Faculty announced this week the call for applications for their 2024 Leadership Programs, including ADVANCE-UP, ALICE, DCLP, and LEADER. Click here to learn more. Applications are due Nov. 3.
Register Now: 15th Annual Pulmonary Hypertension Symposium
The 15th annual NC Research Triangle Pulmonary Hypertension Symposium will be held on Friday, November 17th at the Durham Convention Center. Faculty directors will be H. James Ford, MD, director of the PH program at UNC, and Terry Fortin, MD, co-director of the Pulmonary Vascular Disease Center at Duke. Registration is now open: https://duke.is/9/7rs5. Please join us!
Have news to share?
If you have news to share with the Pulse readership, please contact Tracey Koepke, director of communications for Duke Heart at tracey.koepke@duke.edu. We would love to hear about your latest accomplishments, professional news, cool happenings, and any events or opportunities that may be of interest to our Duke Heart family. Please call with any questions: 919-681-2868. Feedback on Pulse is welcome and encouraged. Submissions by Noon, Wednesdays, to be considered for weekend inclusion.
Duke Heart in the News:
September 24 — Mark Sendak (DIHI)
The Wall Street Journal
Can AI Help Doctors Come Up With Better Diagnoses?
https://duke.is/r/747e
September 25 — Svati Shah
WRAL
Studying why some people stay healthy and others get diseases
https://duke.is/g/jtut
(clip begins at 05:13:48)
September 26 — Harry Severance
Becker’s Hospital Review
Viewpoint: The ‘last straw’ for healthcare workers
https://duke.is/y/2mjk
September 26 — Harry Severance
Medpage Today
‘The Last Straw’ Driving Workers Out of Healthcare
https://duke.is/n/34f7
September 26 — Mark Sendak
Becker’s Health IT
Duke’s health innovation institute targets racial disparities
https://duke.is/5/stsm
September 26 — Svati Shah
WRAL
‘OneDukeGen’ DNA study involves 150,000 Duke patients with a ‘precision health’ approach
https://duke.is/9/579q
September 28 — John Alexander
Medscape
Factor XI Inhibitors: The Promise of a Truly Safe Anticoagulant?
https://duke.is/9/xy8r
Recent Comments