Project
 Individuals and Teams
Individuals and Teams
Program participants will consist of an APP individual OR an APP-led team of 2-4 professionals who will collaborate on a common transformational health improvement project. Project teams will be led by an Advanced Practice Provider (APP).
For the purposes of this program, APP is a general title used to describe non-physician providers who have completed the advanced education and training that qualifies them to (1) manage medical problems and (2) prescribe and manage treatments within the scope of their training. By conventional standards, Advanced Practice Nurses and Physician Assistants tend to be the most recognized types of APPs by many health care organizations in the United States. For this unique leadership training program, other types of APPs (e.g., LCSW, MFT, OT, PharmD, PT) also may be considered for the role of team project lead if their role and contribution to the project aligns with the responsibilities of the team lead.
Individuals and Team Leads: An APP who can attend all required program activities and assume responsibility for ensuring that their project team members meet all program requirements.
Team Partners: Consists of 1-3 health professional colleagues collaborating with the team lead on a health improvement project and who can fulfill program requirements. Team partners can be from diverse healthcare and other community health disciplines and professions, including health education, medicine, nursing, social work, pharmacy, radiography, administration and more. Professionals who work in diverse community sectors that impact social drivers of health (e.g., education, housing, transportation, food security, criminal justice), are also welcomed to participate. The composition of the team should be driven by the needs of the proposed health improvement project and partners who can help make the project vision become a reality.
For more information, refer to Who Should Apply.
Health Improvement Projects
Developing and executing a quality or population health improvement project during the course of the program year is an opportunity for healthcare fellows to:
- Employ leadership and management skills and concepts learned throughout the program
- Make a practical and sustainable short-term step towards a future in health and well-being that inspires them
- Implement clinical, education, and/or advocacy innovations that will, ideally, impact at least one of the following outcome domains:
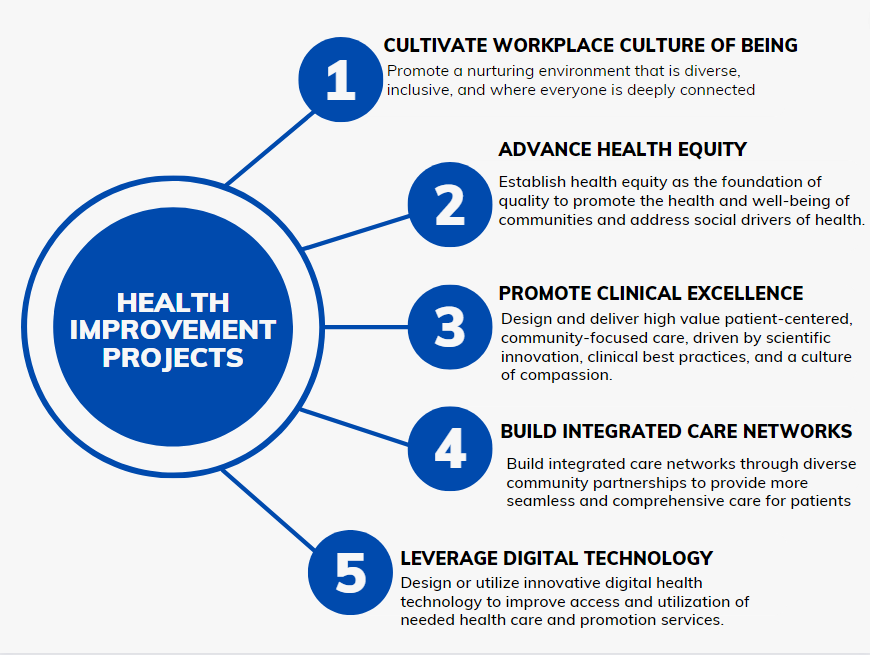
Criteria
A wide variety of quality or population health improvement projects can meet program requirements. In addition to long-standing matters that teams wish to improve, in the midst of the ongoing COVID-19 pandemic, we also welcome project proposals that focus on response efforts for organizations, patients and communities. The appropriateness of project proposals will be evaluated on a case-by-case basis, and the program office will work with fellows to ensure that any project undertaken fulfills program criteria. Examples of those criteria include:
- Projects must be undertaken with a partnering organization/agency and involve some element of collaboration and accountability.
- Projects should be developed, implemented and evaluated with appropriate stakeholder engagement and through a lens of DEI (Diversity, Equity and Inclusion) promotion. 

- Projects may be already in progress, or may be a new piece of a larger, ongoing initiative, provided that the project is still early enough in implementation or dissemination for the team to employ and strengthen leadership and management skills gained during the year.
- Projects should be designed to have measurable outcomes that are detailed in a well-developed and appropriate evaluation plan, which includes both process and outcomes measures and articulation of short, mid and long-term measurable goals. Program sessions will be held to assist teams with developing appropriate evaluation plans.
Circle of Support
Throughout the program year, each Duke APPLI fellow and fellow team will benefit from a circle of support to move its project vision to reality. This support and consultative network includes:
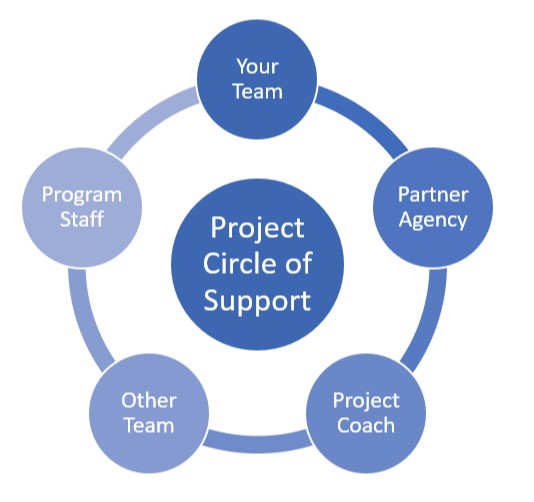
- Collaboration with an employer organization or other partner agency
- Consulting monthly with a Project Coaching Circle that includes an advisor, program staff and other individuals or teams to help support efforts of project development, implementation and evaluation
Sample Project Topics:
In addition to fostering their own leadership and management capabilities, past program projects have positively impacted their organizations and the communities they serve. Some topics from current team projects include:

