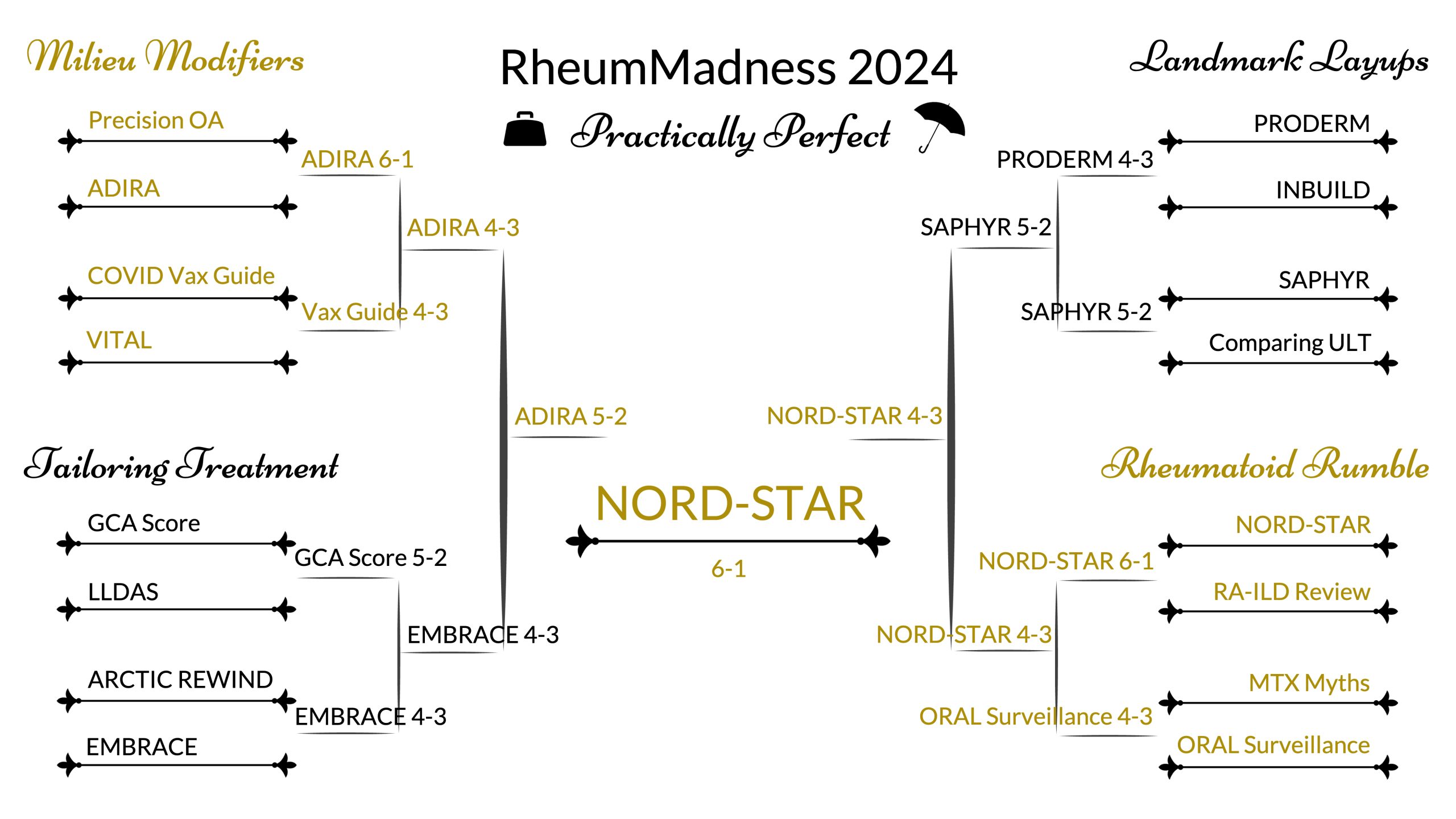
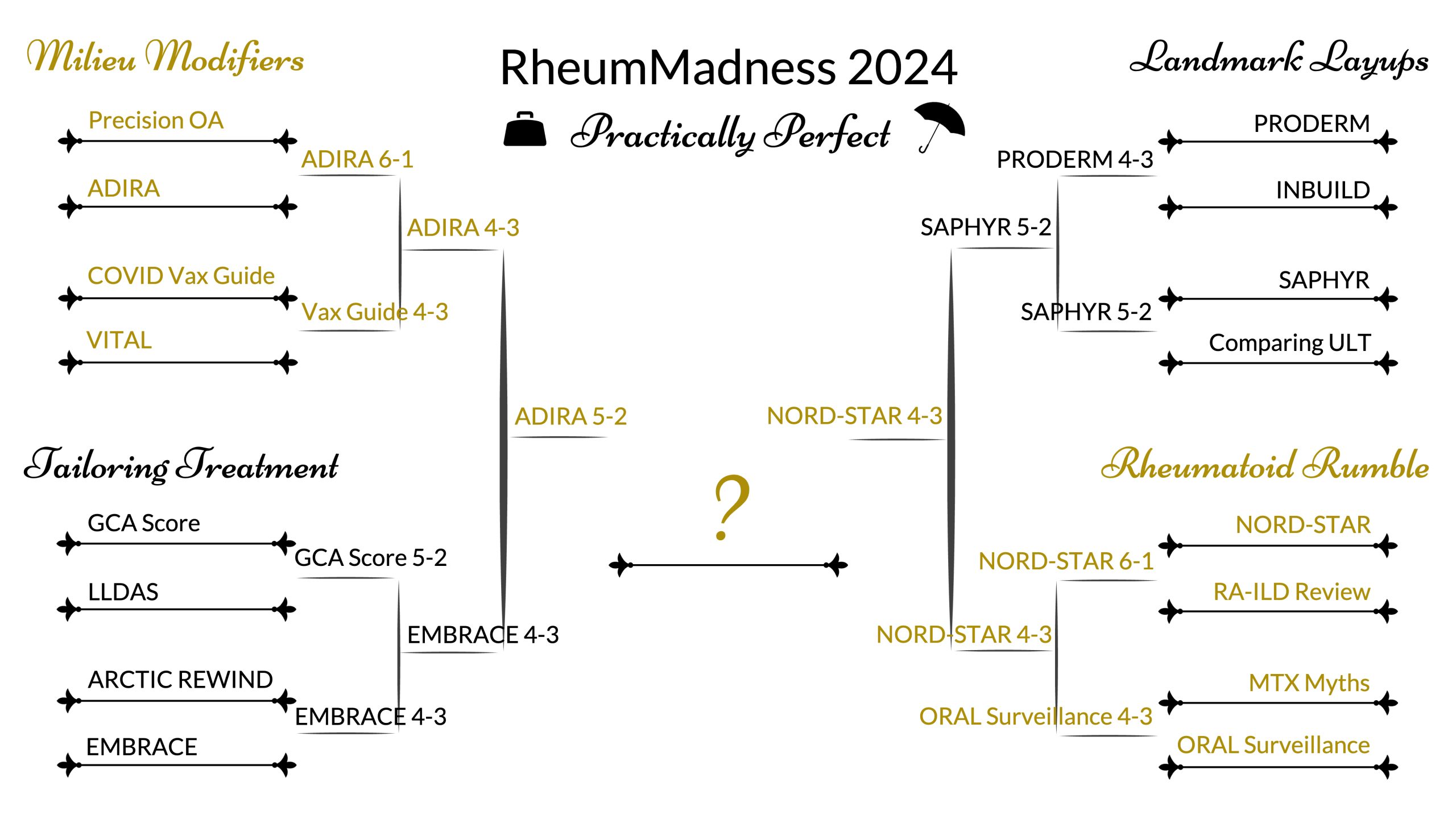
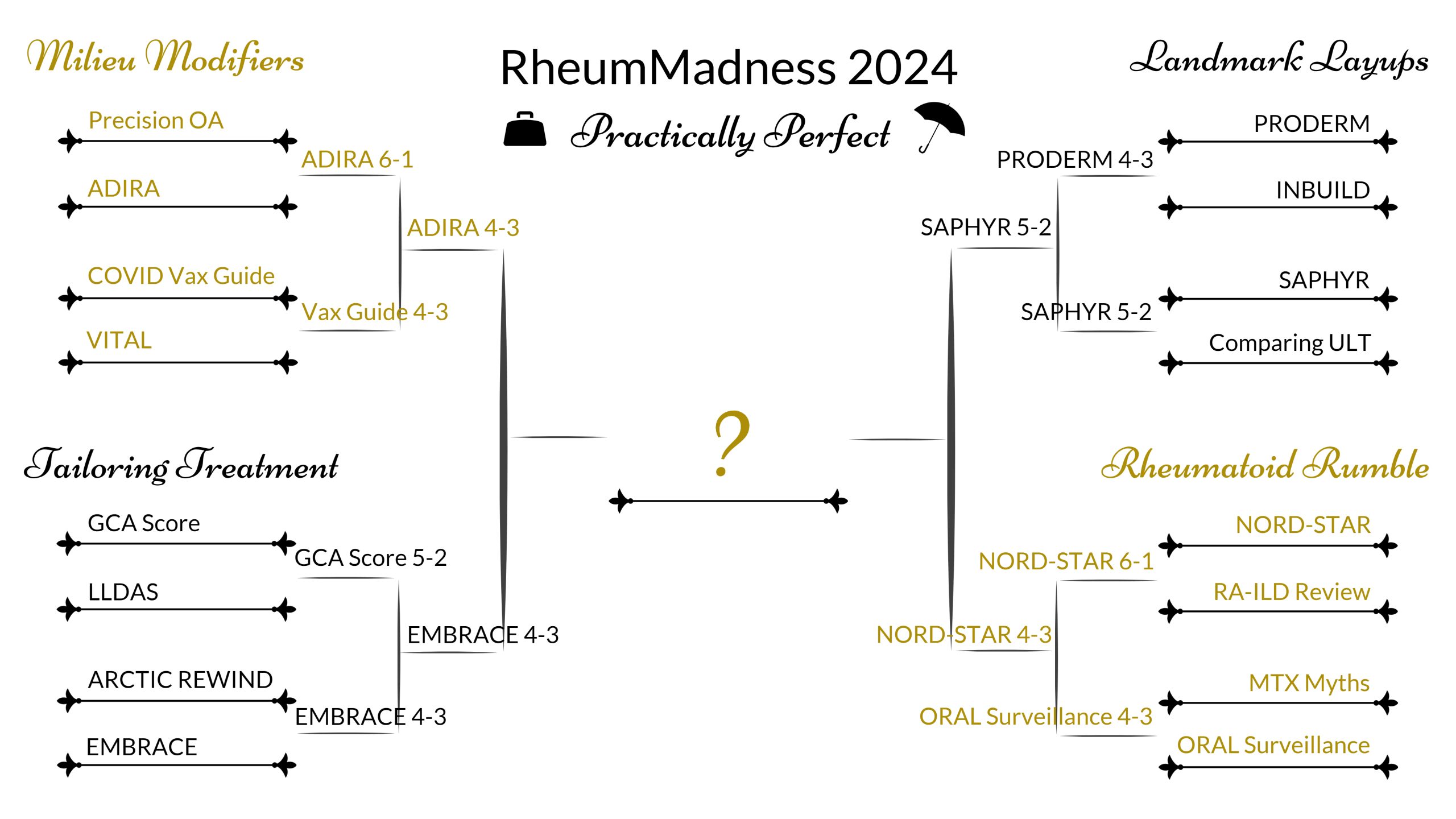
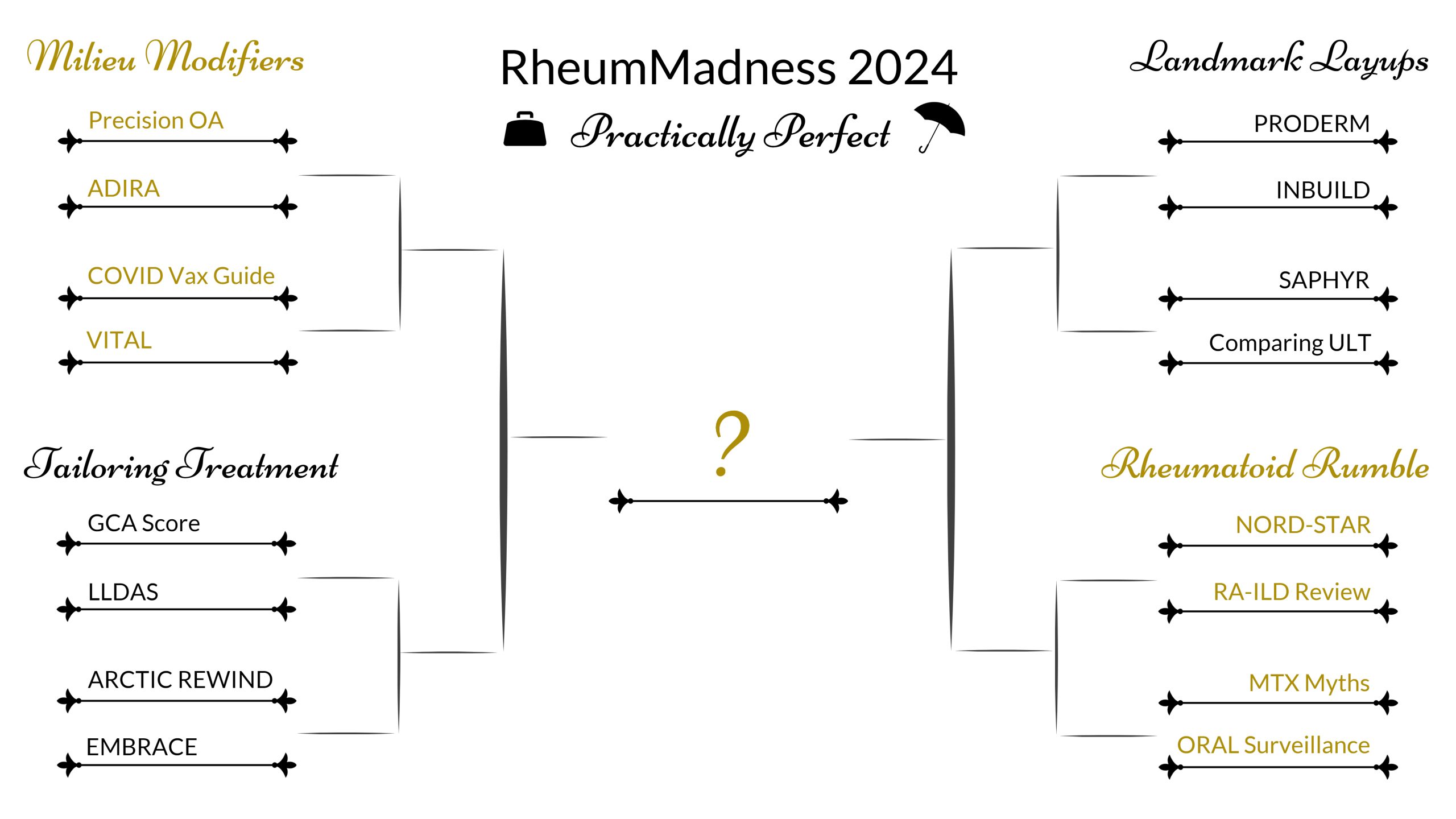
The results of the Seronegative 16 (round 1) are here! The competition this year is fierce, with 111 bracket submissions from participants in at least 13 different countries. To see how your bracket is doing, head over to the RheumMadness Tourneytopia website.
Overall, the first round was incredibly close – half of the matchups were decided by a single vote!
There were also two HUGE upsets in the Tailoring Treatment region, where the Blue Ribbon Panel disagreed with the majority of participant picks. They picked GCA Score over LLDAS 5-2, however 56% of participants picked LLDAS. In an even bigger upset, they picked EMBRACE over ARCTIC REWIND 4-3, but 64% of participants picked ARCTIC REWIND.
We also had a fascinating split in the Rheumatoid Rumble Region, where 51% of participants chose ORAL Surveillance and 49% picked MTX Myths. The panel was also quite split, going with ORAL Surveillance in a 4-3 vote.
Amazingly, out of 111 submissions, there remain only TWO perfect brackets. It’s awesome baby!
Full results for reach matchup in the first round are reviewed below, including how the Blue Ribbon Panel (BRP) voted compared to participant picks. Huge thanks to our amazing panel for their thoughtful consideration.
Matchup 1: ADIRA defeats Precision OA, 6-1
Overall, participants agreed with the panel, with 57% choosing ADIRA and 43% choosing Precision OA.
Comments from the Blue Ribbon Panel in favor of ADIRA:
- Practically every patient in my practice asks about the effects of an anti-inflammatory diet – this is such an important topic for patients with all rheumatic diseases as it empowers them to take control of their illness with a non-pharmacologic intervention that has no adverse effects. Although the magnitude of benefit seems small, this trial had rigorous design and was able to show significant effect on disease activity.
- With the theme of Practically perfect in mind, I felt that I would certainly walk around with table 1 from the ADIRA article to educate my patients on the anti-inflammatory foods to eat, which is something they often ask for and something that empowers them to help themselves. I think precision OA is a great idea, but the results just confirmed what I already knew and without more specifics on types of exercise or types of diet, I don’t think it has as much impact on educating the patient and management of their disease as the ADIRA study has.
- In the era of GLP-1 antagonists, the ADIRA trial results support not only ACR/the physician-directed recommendations on diet, but puts the patient in the driver’s seat.
- I think we need more studies like ADIRA to be able to better answer these important questions for our patients. The question of the effect of particular dietary interventions on disease activity comes up a lot in our routine clinical practice and randomized clinical trials are the best way to study this.
- The clinical question asked in ADIRA — whether an “anti-inflammatory diet” improves disease activity scores in patients with rheumatoid arthritis — is something we have all been asked directly by our patients. In my mind the answer after reading this trial is still “maybe,” as the main analyses did not show significant differences between the control and intervention groups, there were no significant differences in the components of DAS28-ESR, and sample size was quite small. But it does address a clinically relevant question and open the door for further investigators to explore it. And bonus points for all the sports-related puns. In theory, using precision medicine to guide individual treatment decisions is a very practical and worthwhile endeavor. However, I think few clinicians will use “Precision OA” to argue that their patients should forgo exercise as part of the treatment of knee OA; rather, dietary changes and exercise will continue to be recommended for almost all patients. Also, one of the primary outcomes in the study is IL-6, but the significance of the decreased IL-6 is unknown. And I have never had a patient ask me, “How can I get my IL-6 levels down?”
- Adira team: You are representing a fantastic study with important implications for patients. Eating an anti-inflammatory diet gives patients back some power in helping their disease. Also, your graphic was fantastic, stands out, I shared it numerous times for patients on Social Media. The graphic was great, you used few words (important in a graphic) yet sent home your message easily. Your write up was succinct and to the point. Precision Team: I wish you were up against a different team as you had so many winning points. However, an OA study that provides results that are intuitive for most rheumatologists and doesn’t change what I’ve been doing for 30 years has little chance vs a successful anti-inflammatory diet study. You are to be commended on an excellent graphic (used images and few words and conveyed the message easily). Other teams failed these important points. Your write up was excellent and to the point.
Comments from the Blue Ribbon Panel in favor of Precision OA:
- The group from UNC did an excellent job of outlining the importance of the data presented in the Precision OA trial. They did a better job of justifying the outcome and the effect of AI in the future of rheumatology research. AHN put up a fight with the ADIRA study but the message was more subtle. Both groups utilized March madness imagery well.
Match-up 2: COVID Vax Guide defeats VITAL 4-3
Overall, participants agreed with the panel, with 66% choosing COVID Vax Guide and 34% choosing VITAL.
Comments from the Blue Ribbon Panel in favor of COVID Vax Guide:
- The rheum madness team and the OSU team made really nice arguments to justify their reports. The COVID Vax guideline breakdown really nicely explained and simplified the explanation of something we address everyday. The VITAL trial showed secondary prevention can make some difference in development of AI disease. The scouting report is very pragmatic and helps to show the importance of taking data at face value. The COVID Vax paper employs an everyday question in our clinical practices and thus pulls out a close matchup.
- Vaccines; still relevant, still discussed in nearly every patient visit.
-
Rheumatologists are right up there with pediatricians and infectious disease docs when it comes to vaccination concerns. We add yet another layer to this when discussing immunosuppressants of which we have many. This also has a broader reach because it can be applied to many diseases we treat. This is a topic that will come up every week when seeing patients and I find it specifically applicable to rheumatologists vs VITAL which would certainly be helpful, but more so to primary providers when looking to prevent autoimmune diseases.
- COVID WINS! Your graphic makes the information practical and easy to understand. It was not overly wordy as many of the graphics were. Your write up was succinct and to the point. You also kept to the “March Madness” theme by cleverly inserted some basketball terms that are easy for non-basketball fans to understand. You even pointed out at the end why your team should win vs the opponents. And how practical was your study? You elegantly summarized it as “we argue that our team has an answer for almost everyone” VITAL: Being a huge proponent of teaching important habits to people at increased risk for autoimmune diseases, I so much wanted you and your paper to win or at least get to the finals. However, you had a tough opponent who clicked all the boxes. Your graphic was above average and would have beat many of the others, however, “less is better.” I would have removed some things and left the most important take away points (an important rule for graphics: stand out images that convey the message plus few words). I would have had the final important point stand out better with larger font and used an eye catching color for it rather than white font on black background and shortened it (eg “Vitamin D statistically reduced 5-yr incidence for autoimmune diseases”). Just some other recs eg… getting rid of “25,871 participants” since you already give # of men and women (total number not needed) and I’d get rid of “at enrollment.” Change “n=12927 participants took” to 12,927 took.” And so on. Your write up was excellent, succinct and to the point. Nice that you pointed out that they should have included younger individuals. I wish you had pointed out the numerical decrease in AI dzs with omega-3 fatty acids, though not statistically significant. Could it reach significance with a better study? I’d arge that they should have done this exact same study only in people at increased risk (ie people with 1st or 2nd degree relatives who have AI dz). Up against some of the other opponents, you would have won this round. Good job (I am being picky with the above; however, the above changes could have helped you win this round in my eyes)
Comments from the Blue Ribbon Panel in favor of VITAL:
- VITAL study has impressive number of participants and answers again a very practical and important research question despite some of the limitations.
- VITAL allows clinicians to give more than a hand-wavy answer when asked about the potential benefits of vitamin D supplementation. I like how the results are not overstated by either the article’s authors or the writers of the scouting report. I also thought that the section on potential mechanisms to explain the effect of vitamin D supplementation on the development of autoimmune disease was thought-provoking. The COVID Vax Guide is practical, but the guidance on these issues is ever-changing, and for several medications the article is unable to call upon good evidence to support or refute the recommendations it presents. There are also multiple authors on the study with ties to companies that produce vaccines (e.g. Pfizer).
- Prevention of autoimmune disease is the ‘holy grail’ for rheumatology and these investigators have to be congratulated for conducting such a large trial with simple interventions. Although the outcome is modest, the concept and conduct of the trial is novel and exciting, and hopefully heralds other similar studies in the future. We have to keep in mind that even trials with some costly biologics (or HCQ) have failed in this endeavor.
Match-up 3: GCA Score defeats LLDAS 5-2
Overall, participants DISAGREED, with 56% choosing LLDAS and 44% choosing GCA Score.
Comments from the Blue Ribbon Panel in favor of GCA Score:
- This one was difficult for me because one is a very practical study (GCA score) and the other one is an important measure (LLDAS), but I had to go with GCA score given how useful it is.
- GCAPS could be a useful tool to consistently assess GCA patients in clinical practice.
- Clinically useful tool to identify patients at high risk of having GCA – hopefully leading to earlier intervention and prevention of disease-related damage.
- This was one of the hardest to choose for me. Both help us make decisions on less steroid exposure and commencement of biologic agents that have been approved for each disease. While LLDAS is quite important and clinically relevant, I would say that the GCA scoring system would help with more urgent practical decision-making that a clinician will face particularly in situations where biopsy and/or ultrasound may not be possible.
- GCA Score: WINS! I ultimately chose you because your study changes my rheumatologic practice. Why? Most of us do not get Clinical and Exp Rheum and RMD and, therefore, were not as aware of the GCA Score. Therefore, you taught me something important that is new and practical that may prevent me from performing invasive procedures on patients. Your graphic was straight to the point and very practical to use, and your write-up was succinct and to the point. You also kept to the “March Madness” theme by cleverly inserting some basketball terms that are easy for non-basketball fans to understand. LLDAS: You were up against a tough opponent. You overall did a great job. Fantastic, to-the-point graphic, and very clever poem to summarize the study (and even argue agains opponents eg EMBRACE). How could you have won?: You could have tweaked the image (remember that the less words on a graphic the better and you want the most important to standout). I would have taken the reference and team down toward the bottom and used smaller font than any other phont on the graphic. That is nit picky but would have improved it. The write-up should educate as well as summarize. I wish you had mentioned how no steroids (and certainly less than 5 mg a day) is the current goal and that true remission and off steroids is the #1 T2T. It has less organ damage by SDI over time compared to LLDAS. LLDAS should be our goal if remission off steroids is not attainable.
Comments from the Blue Ribbon Panel in favor of LLDAS:
- GCA Score is helpful, but its value is limited by the small sample size, which led to several clinical features rarely being seen (and therefore difficult to evaluate reliably). A multicenter validation study would be more useful. The LLDAS paper was a landmark paper. The team also gets points for creativity, and I especially enjoyed the realization that “trial” rhymes with “smile.”
- Both reports discuss novel approaches to risk stratification and disease management. The GCA score has a more definitive strategy that helps with diagnosis of a complicated disease state. The LLDAS attempts to simplify T2T in a disease where T2T is incredibly convoluted and difficult to ascertain. The report from Manchester is very whimsical in presentation and UC is very effective in simplifying the understanding of the GCA score. Ultimately, the win goes to Manchester given the more substantial impact T2T would have in SLE. Chicago used more March Madness imagery than Manchester who went Futbol style.
Match-up 4: EMBRACE defeats ARCTIC REWIND 4-3
Overall, this was another HUGE upset, with 64% of participants choosing ARCTIC REWIND and 36% choosing EMBRACE.
Comments from the Blue Ribbon Panel in favor of EMBRACE:
- This is a big time early round matchup. Both studies address controversial topics in the management of RA and SLE. The team from NW highlights the importance of the data from a social and clinical aspect very well. UCSD succinctly describes the important details of the ARCTIC REWIND study. Complete de-escalation has been a very controversial topic and has been effectively debunked as a paradigm and this study helped greatly to improve our understanding of the risk/benefit. With that being said the EMBRACE trial tackled social norms and attempted to reset the approach to including African Americans in clinical trials while answering an important question. The 10 beats the 7 and provides a mild upset in Rheum Madness.
- EMBRACE highlights and supports DEI efforts in SLE research which improves our knowledge of patients and the disease, therefore treatment options.
- This will become a landmark trial in lupus, the first to target patients of Black race – a much needed development towards racial equity in clinical research.
- Both are very important papers, but I think the impact of focusing on a demographic that is known to have the disease more commonly and more severely when the initial studies didn’t show sufficient representation of that group sets a precedence and assures us that belimumab can be used safely and effectively in our patients of black/african ancestry. We see large health disparities in SLE patients and I support anything that helps us to narrow the gap and address concerns of a diverse patient population.
Comments from the Blue Ribbon Panel in favor of ARCTIC REWIND:
- This pair was also particularly tough, because both studies answer important research questions, but I went with ARCTIC REWIND since its results are applicable to more people overall.
- ARCTIC REWIND is a very useful article that can be used to discuss with patients whether they should stop a TNF inhibitor after achieving remission for rheumatoid arthritis. Love the cartoon image. EMBRACE is an important study as well — the removal of the cautionary statement was important — but its results are less novel and significant overall.
- ARCTIC REWIND: Wins! This is an excellent graphic with a clever cartoon that conveys the main point of “mutual clinical decision-making.” The right side cleverly summarizes the study and outcomes. Plus, you put in basketball graphics that do not distract (employing the March Madness theme). The references and team are in small font at the bottom, which is good. The only thing I would have done was make the title in larger font. The write-up summarized the study well, and you peppered in easy-to-understand basketball references. (Some teams used basketball terms that are not universally known, so good job!) EMBRACE: Good job on loads of references, you pointed out possible reasons for no statistical significance and that narrowing the health disparities gap is most important. In substance, you nailed the study and results and appropriately pointed out that not enough participants were in the study to meet statistical significance. However, what could have helped you win: An award-winning graphic coupled with the self-explanatory importance of health care disparities in research could have done it. “Less is better” when it comes to words on graphics, and using images that convey ideas is of the utmost importance. I would have used many fewer words and still driven the most important points home. As far as a graphic, I’m not sure what to put, but I bet the five of you could have figured out something very interesting. Also, for those unfamiliar with a study (and all those acronyms), I would have put in what EMBRACE stands for. It is always nice to associate the acronym with the study and “why” those letters were used.
Match-up 5: PRODERM defeats INBUILD 4-3
Overall, participants agreed with the panel, with 60% choosing PRODERM and 40% choosing INBUILD.
Comments from the Blue Ribbon Panel in favor of PRODERM:
- PRODERM was a much-needed trial that has allowed me to give IVIg to patients with dermatomyositis without first needing to have tear-inducing conversations with insurance companies. The team is right that it was a “game-changer” for rheumatologists, and it therefore edges out INBUILD, which is also a clinically useful study but changes practice more for pulmonologists than for rheumatologists.
- This one puts us in a 2-15 scenario. Both groups do a nice job of discussing the importance of the discoveries in two difficult to treat scenarios. PRODERM is a top seed given its significance being the first study to approve a therapy for DM. INBUILD helps to show we have more options for ILD related to CTD but the importance of PRODERM can not be understated.
- I felt this had a greater impact on the clinical management of dermatomyositis than nintedanib has on ILD-associated rheumatic disease where rheumatologists still often use other agents when lungs are involved in the disease process. It’s the difference between a role player who impacts the big game vs a journey man who can add to a team with established stars.
- PRODERM: Wins! This is an outstanding graphic: simple, direct, and to the point! You truly took the “less is more rule” to heart (and successfully). Your write-up was also excellent: succinct and to the point. You started with a hook: “It’s not every day… shakes up Rheum world!” That was fantastic. You summarized the study very well. You also kept to the “March Madness” theme by cleverly inserting some easy basketball terms for non-basketball fans to understand. One thing you should have added is what PRODERM stands for. We have so many acronyms that it is hard to keep track of them. Knowing where the letters come from is very helpful for memory. I recommend always explaining the letters, including in talks. IMBUILD I Liked your graphics and write up a lot. You made many clever statements while making your point: a life-changing therapy for a previously untreatable problem. However, you should avoid sports analogies that people unfamiliar with the FIFA/FA Cup would not know. Always remember your audience. The “March Madness” theme lures teams into using clever basketball terms. However, your audience is a large group of physicians and medical students who will easily understand all the scientific information. However, people who are not basketball fans will not understand. The entire reason for writing educational material is to successfully send your message so that it is easy to learn and impactful. I liked the easy-to-understand basketball terms, such as “our magic number,” as it makes it easier to stick inside your help… I’ll probably remember it. Please use “Sjogren’s disease” and NOT “Sjogren’s syndrome” The graphic look is excellent, but remember that “less is more” when it comes to words on a graphic (you want large impactful images and the fewest words necessary). For example, the top middle statement could be “Nintedanib significantly slowed ILD progression (lower FVC decline rate)”; the same with the final summary statement in blue font (use fewer words, but I do love that you used a font that sticks out for the summary point, though). One thing you should have added is what INDBUILD stands for. We have so many acronyms that it is hard to keep track of them. Knowing where the letters come from is very helpful for memory. I recommend always explaining the letters (including in talks). PRODERM edged you out by their simple to-the-point graphic and use of basketball terms that even a basketball dune like me would understand.
Comments from the Blue Ribbon Panel in favor of INBUILD:
- I picked INBUILD trial because IVIG was already being used in myositis for many years prior to PRODERM trial, so it did not really change my practice (though made it easier to get it approved), but INBUILD trial offers a new class of therapy for patients with progressive fibrotic lung disease.
- Proposed expanded use of Nintedanib in ILD subtypes is important and impressive.
- Treatment options are so limited for fibrotic lung disease – this large clinical trial established the efficacy of nintedanib for ILD
Match-up 6: SAPHYR defeats Comparing ULT 5-2
Overall, participants agreed with the panel, with 54% choosing SAPHYR and 46% choosing Comparing ULT.
Comments from the Blue Ribbon Panel in favor of SAPHYR:
- I went with SAPHYR because patients with PMR need therapies other than steroids and this trial is so informative. Comparing ULT is also important, but we know that both medicines work very well for gout.
- This was a close one, but I give the edge to SAPHYR, which established a new non-steroid option for patients with PMR. I also like that the authors were upfront about their reduction in sample size and statistical power on account of the COVID-19 pandemic, which led to premature study termination. The findings of “Comparing ULT” are relevant for a larger number of patients, but the study didn’t really change my practice, as allopurinol was already being used (and still is) as first-line treatment for urate-lowering therapy. Also, the study was powered for efficacy and not safety, so its commentary on the risk of cardiovascular events in allopurinol vs. febuxostat should be taken with a grain of salt (no pun intended).
- Another tough early round matchup but in two fairly different disease states. MUSC very nicely and succinctly explains the Sapphire trial and the march madness imagery is on point. The team from Michigan helps drive the point home on ULT and the study helps to further debunk the known data on cardiac events in patients on XOI therapy. The win goes to SAPHYR in a close game given its significance in the PMR space and being first drug approved for the indication.
- Such a huge unmet need in PMR where all we had is glucocorticoids for so many decades, with many patients being on treatment for years and with consequent morbidity. This trial established the efficacy (not great, but still an advance) of IL-6 inhibition in patients with relapsing disease.
- SAPHYR gave us a steroid-sparing alternative to prolonged use of steroids for PMR which is now FDA approved for use. This was a slam dunk.
Comments from the Blue Ribbon Panel in favor of Comparing ULT:
- Interesting look at urate lowering therapy in different patient populations.
- Comparing ULT: ULT wins! This was a tough one! I so wanted to choose SAPHYR due to its amazing add-on therapy for a disease that has had no good treatments other than dangerous steroids. However, my nod goes to Comparing ULT… Gout Busters was an incredibly eye catching well done graphic (SAPHYR broke the image law of “too many words and few eye catching graphics”. ULT also answers an incredibly important problem facing rheumatologist conversations with patients … what to do with that CV events black box warning. SAPHYR had a very clever write up, but many of the basketball terminology went right over my head as a non-basketball person (point guard, evading screens, spreading zone, etc). If you had stuck to basketball-related terms everyone knows (this makes the write-up universally clever) and an image that greatly simplified 3 (4 max) takeaway points from SAPHYR… you could have won. Remember SAPHYR… “less is more.” One thing you should have added is what SAPHYR stands for. We have so many acronyms that it is hard to keep track of them. Knowing where the letters come from is very helpful for memory. I recommend always explaining the letters (including in talks).
Match-up 7: NORD-STAR defeats RA-ILD Review 6-1
Overall, participants agreed with the panel, with 63% choosing NORD-STAR and 37% choosing RA-ILD Review.
Comments from the Blue Ribbon Panel in favor of NORD-STAR:
- I went with NORD-STAR because the design is innovative, answers a clinically important question and we need similar head-to-head trials comparing multiple agents in RA.
- NORD-STAR challenges the “methotrexate-first” treatment paradigm for rheumatoid arthritis and provides evidence for starting a TNF inhibitor or abatacept along with methotrexate in patients who are newly diagnosed with RA. The RA-ILD Review is helpful but is a bit confusing in parts (e.g. Figure 6), and since its publication, the ACR has shared guidelines for the treatment of ILD in patients with rheumatic diseases.
- This matchup is an example of “cupcake city” as Dickie V (Better known as Dukie V to Maryland fans) would allude to. NORD STAR is a significant albeit somewhat obvious outcome study proving the significance of biologics vs csDMARDs as therapies in rheumatoid disease. Vandy’s report succinctly and effectively summarizes the study and while USF puts up a fight, this is essentially an early round blowout.
- Supportive evidence of treating early and aggressively can change the way we approach RA.
- An important head to head trial comparing biologics that are commonly used to treat RA, and will be used by clinicians in treatment decision-making.
- RA is the bread and butter of rheumatology and NORD-STAR answers a very practical question that we consistently ask – Can we diagnose and treat RA sooner and better? MTX is the gold standard of therapy in treatment-naive patients and this study may help us advance in our treatment strategies by recognizing that there are other agents that can be first line in certain patient groups. It also helps to guide us in our choices when conventional therapy is contraindicated. This was another hard decision to make and came down to the buzzer because the RA-ILD review was also very practically perfect and is certainly worthy of bookmarking for reference, however I felt we could use the NORD-STAR more at initial diagnosis of RA which is seen more commonly.
Comments from the Blue Ribbon Panel in favor of RA ILD Review:
- RA-ILD: WINS! VERY educational graphic, BUT… simplified graphics win out (I’d remove the following: risk factors as they don’t change how we ID ILD, collaboration list, listing uncommon forms of ILD, % prevalence, and mortality … rheumy’s generally know RA well) … you’d be left with much more space to make the graphic more eye appealing, readable, and it would teach the vast majority of rheumy’s things most do not know (eg, UIP vs NSIP, getting an HRCT not a CXR, how to monitor, how to tx). Your write up was well done and summarized things very well. I like “so practical … says “practical” in the title, and your last paragraph successfully conveys why RA-ILD is the best (and practical) paper! Always remember your audience. The “March Madness” theme lures teams into using clever basketball terms. However, your audience is a large group of physicians and medical students who will easily understand all the scientific information. However, people who are not basketball fans will not understand. I did not know and could not relate to “Steph Curry, three-point shot.” However, you did not use as many uncommon terms as other teams. The entire reason for writing educational material is to successfully send your message so that it is easy to learn and impactful. You used easy-to-understand basketball terminology that conveyed important points. (I loved that “previously MTX was benched.” NORD-STAR = Fantastic graphic. You conveyed your points in a well-organized, easy-to-understand way. I would have removed “All groups were statistically similar with low rates of progression” as it was not needed. Adding the basketball images was clever for “March Madness” without being distracting. In the write-up, you used way too much basketball terminology. Always remember your audience. The “March Madness” theme lures teams into using clever basketball terms. However, your audience is a large group of physicians and medical students who will easily understand all the scientific information. People who are not basketball fans will not understand. The entire reason for writing educational material is to successfully convey your message so that it is easy to learn and impactful. One thing you should have added is what NORD-STAR stands for. We have so many acronyms they are hard to keep track of. Knowing where the letters come from is very helpful for memory. I recommend always explaining the letters (including in talks). Your write-up was otherwise excellent. If you’d use universally understandable basketball-related terms, you could have forced RA-ILD off the court.
Match-up 8: ORAL Surveillance defeats MTX Myths 4-3
Overall, participants were almost completely evenly split, but ultimately the majority agreed with the panel with 51% choosing ORAL Surveillance and 54% choosing MTX Myths.
Comments from the Blue Ribbon Panel in favor of ORAL Surveillance:
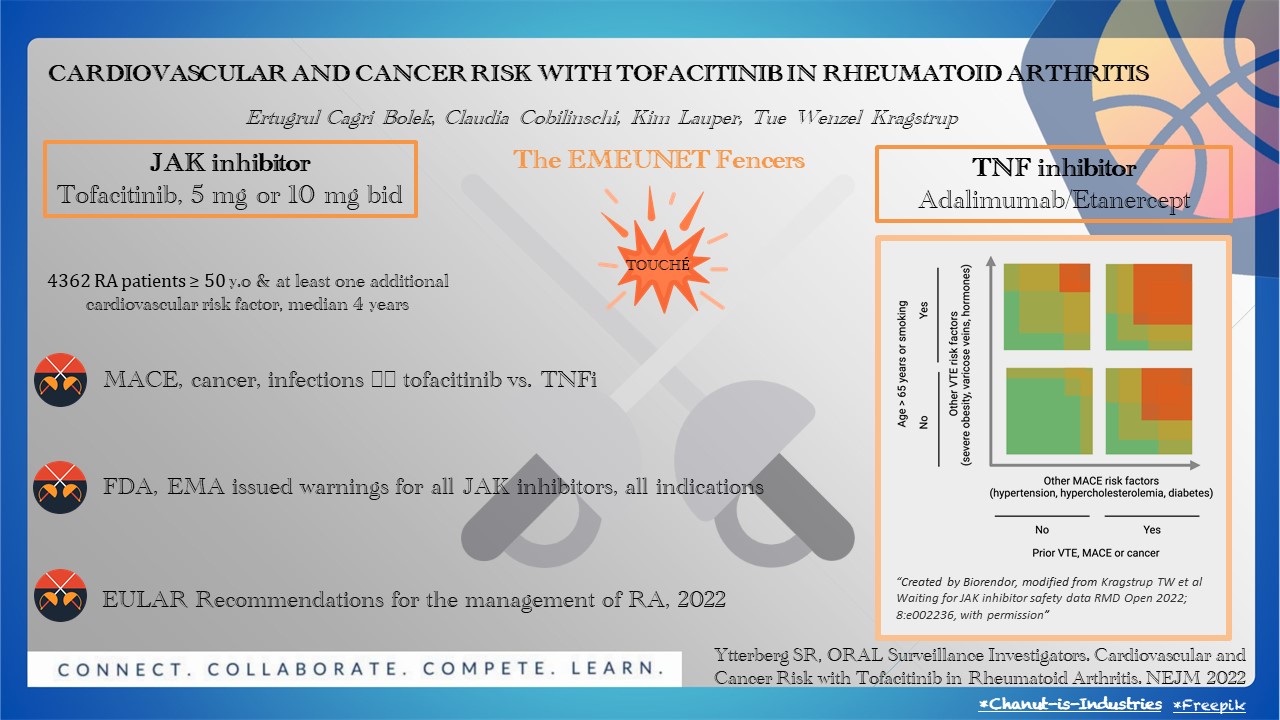
- MTX Myths offers an interesting and pertinent discussion, but it would be premature to call it “practical.” ORAL Surveillance changed the way we counsel patients about JAK inhibitors and the calculus we use when deciding whether to start these medications. However, it is difficult to read the visual accompanying the team’s scouting report.
- This puts two opposite paradigms against each other. One study helping to disprove preconceived notions while another creates extreme controversy in a class of therapies that is essential to the treatment of a number of autoimmune disease. The delivery of MTX Myth Busters is excellent using great historical context to discuss a one of the winningest programs in rheum history albeit with some violations along the way. Oral surveilance attempted to give JAKi the equivalent of an NCAA death penalty. Ultimately the Oral Surveillance trial wins the day given the substantial effect it has acutely generated in the Rheum Madness profile. The imagery from our Turkish team though is in a completely left field sport to college basketball, which in the eyes of this pundit leaves something to be desired.
- important trial that informed us about the risks of JAKi that led to changes in the clinical practice, changes to drug labels and treatment guidelines
- ORAL had more impact on clinical decision-making than the MTX Myths.
Comments from the Blue Ribbon Panel in favor of MTX Myths:
- We use methotrexate all the time compared to tofacitinib, so I went with MTX article due to its impact onto my clinical practice.
- Debunked myths about MTX gives rheumatologists more more confidence when using MTX to treat.
- MTX: WINS! Great write-up. I can’t think of much to change. This is one of the most practical studies in RheumMadness, with important takeaway points that we can all use every day in our practice. The right half of your slide is fantastic! It conveys the entire point of the study. You could have deleted the entire left half and ended up with one of the best graphics in the entire series. Remember for graphics: “Less is more” when it comes to words, plus you want to use large, eye-catching images that convey the message. The right side does that. Much of the left side is best for the write-up section. You won this round due to your write-up and the right side of your graphic. ORAL: The image and write-up needed to be clearer. I recommend an easier-to-read font (fancy is not better) for the graphic. Kragstrup et al.’s graph in the upper right is incredibly useful, but it needs an explanation for the meaning of the different colors. The write-up needed more clarity. You make very important summary points in your write-up, which is great. However, some points were a little unclear, and the sentences should have been written differently. One example is, “… incidences of MACE and cancer were higher with the combined tofacitinib doses…” Maybe you were trying too hard to force in fencing terms while simultaneously summarizing the study and educating us. In the write up, you used fencing terminology (eg lifting a red card, la riposte) unknown by most people. Always remember your audience. The “March Madness” theme lures teams into using clever basketball terms. However, your audience is a large group of physicians and medical students who will easily understand all the scientific information. However, people who are not basketball fans will not understand. The entire reason for writing educational material is to successfully send your message so that it is easy to learn and impactful.
What’s up next?
Results for the next 3 rounds will be released on the following dates:
- Saturday, March 23: The Entheseal 8 (round 2)
- Tuesday, March 26: The IgG4 (round 3)
- Thursday, March 28: The Interleukin 2 (round 4, championship)