Patient Care
The Section’s goals across patient care and clinical operations over the past year have been two-fold: provide high-quality, safe, and timely access to surgical care, and maintain morale of the Section’s patients and staff. Both the Departments of Surgery and HNS&CS have relied on their faculty, trainees, and staff to support the Departments and Section in new roles, while continuing to think outside the box to address clinic needs.
Through implementation of new data analysis tools that improve surgical scheduling accuracy, incorporation of telemedicine to provide safe and efficient clinical care, and maintaining relationships with referring physicians to help efficiently manage resources in and out of Duke, the Section has continued to live its mission of being, “United, for all patients.”


Surgical Case Volume
After experiencing a decline in 2020 due to the COVID-19 pandemic, the Section has now surpassed pre-pandemic surgical case volume. Our teams have performed over 32,000 surgical cases in FY2021, accounting for roughly 42% of the entire Duke University Health System (DUHS) patient volume.
Using Data to Improve Case Time Accuracy
The Laboratory for Transformative Administration continues to seek innovative ways to improve care through data analytics in the Section of Surgical Disciplines.
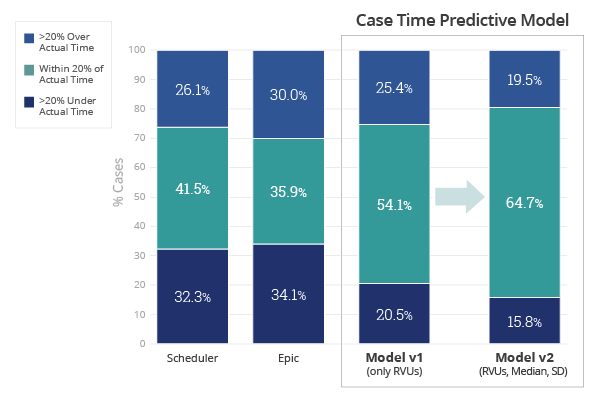
The Case Time Accuracy Predictive Model focuses on case length per primary physician, primary procedure, number of procedures, room number, and RVU range. A recent review of the predictive model utilized RVUs in addition to median and standard deviation (SD) to expand the input data of the predictive model.
Better time accuracy prediction will allow for improved utilization of resources and a better patient experience. A partnership with perioperative nursing leadership will develop a standard work process for OR schedulers using this new model.


Lowering Costs, Improving Accuracy Through Data Analytics

Surgeons and nurses perform a TCAR procedure. Photo illustration visualizes the cost of care incurred during a surgical procedure.
In June 2021, 150 Duke clinicians participated in a Cost of Care Town Hall, providing valuable feedback on using cost data to drive operational improvement.
Several promising projects are currently underway, most notably a “Surgery Receipt” tool. With data transparency at its core, this tool allows surgeons to calculate their operating expenses in real time.
These efforts allow for greater efficiency and better allocation of resources, in turn improving the quality of patient care we provide.
In Case You Missed It
Duke surgical team successfully implants new generation artificial heart in patient, first in U.S.
On July 12, 2021, a surgical team at Duke University Hospital was the first in the United States to implant a new generation artificial heart in a 39-year-old man with heart failure.
In November 2021, the patient received a full heart transplant, demonstrating that the artificial device can act as a successful bridge to transplantation.

Visit our websites to learn more about each of our departments, training programs, faculty and trainees, and current initiatives.
