The long-term goal of our research is to define the role of protein tyrosine kinase-regulated transcription and translation networks activated by growth factor, chemokine and adhesion receptors in the regulation of cell polarity, growth, survival, differentiation, adhesion, and migration during cancer metastasis and the response to tissue injury. We have a long-standing research interest on the role of protein tyrosine phosphorylation in tumorigenesis. We employ novel animal models to investigate the role of tyrosine kinase signaling networks required for tumor metastasis as well as the regeneration response following lung injury. In particular, we are dissecting the pathways that modulate the crosstalk between multiple cell types during tumor metastasis and lung injury/regeneration. Disrupting these “intercellular conversations” is expected to generate new targets for therapeutic intervention. Specifically, we focus on the role of the ABL family of tyrosine kinases, ABL1 and ABL2, in diverse cellular processes leading to changes in cell morphology, motility, invasion, adhesion, as well as cell growth and survival. Among the research areas currently being pursued in our laboratory are defining the mechanisms that regulate the cross-talk between brain metastatic cancer cells and associated cells in the brain tumor microenvironment. ABL kinases promote metastasis of lung cancer cells to the brain and other organs. Inactivation of ABL kinases suppresses lung cancer cell metastasis and ABL kinases are required for expression of pro-metastasis genes in lung cancer cells. High-level expression of ABL1, ABL2 and a subset of ABL-dependent target genes correlates with shortened survival of lung adenocarcinoma patients. ABL-mediated activation of transcription factors including TAZ and HSF1 promotes lung cancer metastasis to the brain. Treatment with ABL allosteric inhibitors impairs expression of TAZ- and HSF1-dependent target genes, and markedly decreases metastasis. ABL-specific allosteric inhibitors might be effective to treat metastatic lung cancer with an activated ABL pathway signature. More recently, we found that ABL kinases are activated by hypoxia, and that hypoxic induction of the Hypoxia-inducible factor 1-alpha (HIF-1α) and downstream targets were decreased by ABL inactivation. We found that ABL kinase activity protects HIF-1α from proteasome-mediated degradation during hypoxia and identified CPSF1 as an E3-ligase antagonizing the expression of the oncogenic HIF-1α transcription factor.
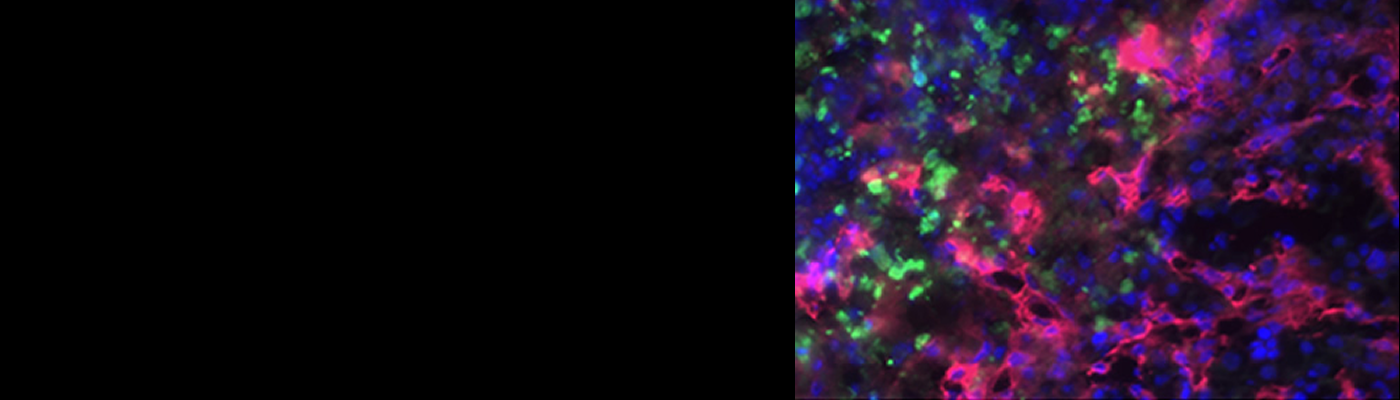
Advanced breast cancer is associated with metastasis to multiple organs, including brain and bone. We are interrogating the role of ABL tyrosine kinases in the colonization and outgrowth of metastatic breast cancer cells by activating transcriptional and translational programs. Human epidermal growth factor receptor 2-positive (HER2/ERBB2) breast cancer patients often present with brain metastasis. HER2-targeted therapies have not been successful to treat brain metastases in part due to poor blood-brain barrier (BBB) penetrance and emergence of resistance. We found that treatment of preclinical mouse models with ABL kinase allosteric inhibitors improves overall animal survival and impairs HER2+ brain metastatic outgrowth in vivo. Mechanistically, ABL kinases phosphorylate the RNA binding protein Y-box-binding protein 1 (YB-1). ABL kinase inhibition disrupts binding of YB-1 to the ERBB2 mRNA and impairs translation, leading to a profound decrease in HER2 protein levels. Notably, loss of YB-1 inhibits brain metastatic outgrowth and impairs expression of a subset of ABL-dependent brain metastatic targets. These data support a role for ABL kinases in the translational regulation of brain metastatic targets through YB-1 and offer a therapeutic target for HER2+ brain metastasis patients. Ongoing studies employ state of the art technologies (single-cell RNA-seq and Spatial Transcriptomics) to define the transcriptional landscape of distinct brain metastases types, and surrounding non-tumor cells brain tumor microenvironment. The ultimate goal of our studies is to develop novel therapies for the treatment of metastatic solid tumors by targeting not only cancer cells but also associated stromal cells in the tumor microenvironment.