TempRight Logo
The overarching point of this project is to create a system that is able to maintain a person’s core body temperature within the homeostatic range.
The inspiration for this project stems from the many issues pertaining to body temperature regulation during surgical procedures.
Project Timeline

Motivation
The average core temperature of a healthy person is between 36.1°C and 37.2°C. The average internal temperature of an operating room (OR) ranges from 21°C to 24°C with 50-60% humidity. The reason the OR is kept at cooler temperatures is for the comfort and safety of the surgeons and the rest of the surgical team. The medical staff is at risk of heatstroke, dizziness, or fainting if these rooms are not kept cool due to their attire, surroundings, and the length of surgery. The cooler temperature can cause the patient’s body temperature to drop, reducing the ability of blood to clot properly, leading to a higher risk of infection.
The most common patient warming practices include patient pre-warming methods and forced-heating systems. Prewarming involves the patient being subject to a warming procedure using warming blankets, heating pads, IV fluids, and/or a forced-air heating system prior to the surgery for roughly 30 minutes to an hour. The expectation is that this should limit the effects of anesthesia on patient body temperature and the effects of the cold operating room. However, this method is ineffective. The Journal of Anesthesiology conducted a study that found out of 27 prewarmed patients, 17 had a body temperature below 36 degrees C by the end of the surgery.



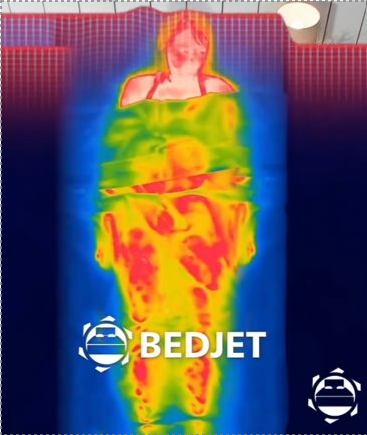
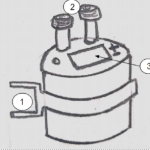
The images above show how the warmed air will travel from the tube to reach the patient interface. A heat detector will be used to show the equal distribution of heat throughout the entire blanket.
Project Overview
Problem Statement
A person’s core body temperature must remain within a narrow homeostatic range. However, a patient undergoing surgery faces cold operating room temperatures, causing heat loss primarily through radiation and conduction. The risk of perioperative hypothermia is greatly increased by the use of anesthesia alongside the cold environment. Current methods of patient warming during surgery are often not used because they limit access and maneuverability for the surgeon.
Kanban Breakdown
The Kanban serves as a breakdown of all of the systems that will be part of the final product. Having the Kanban serves as a way of seeing the interconnectedness of the entire project. This is often one of the first steps taken in the design process.

Function Tree Breakdown highlights the main safety features of the device. Includes flow of information (patient temperature), the flow of energy (temperature sensitivity, emergency shutoff, protection from electrical components), and flow of material (sterility, interaction with patient skin).

Brainstorming
These images serve as the concepts for this project.

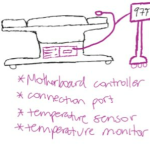
Temperature Monitoring System
Properly monitoring a patient’s temperature throughout surgery is one of the most vital methods of preventing perioperative hypothermia. The device will be implemented with a temperature monitoring system that will allow live readings of the patient’s temperature at all times to eliminate the guesswork involved in determining the patient’s current temperature. The elevated sensor that will be utilized within the device will be the zero heat flux temperature sensor. This class of sensors allows the patient’s core body temperature to be measured noninvasively, eliminating the need of invasive techniques currently used to monitor a patient’s temperature. The zero heat flux temperature sensor enables the development of an isothermal pathway by insulating the patient’s temple; the formation of the isothermal pathway allows for internal core temperatures to be readable at the skin surface. The temperature sensor itself will be single-use to limit the cross-contamination between patients.
Maintaining homeostasis requires that the body stays within a narrow temperature range. Bodily functions are hindered when the body experiences temperatures that are not within the normal internal body temperature span. When the system detects that the body has dipped or peaked outside of the set range, it will immediately trigger its negative feedback to either increase or halt the amount of heat transferred to the patient. This function is to assure that the patient’s normal body temperature is replicated throughout the surgical procedure.
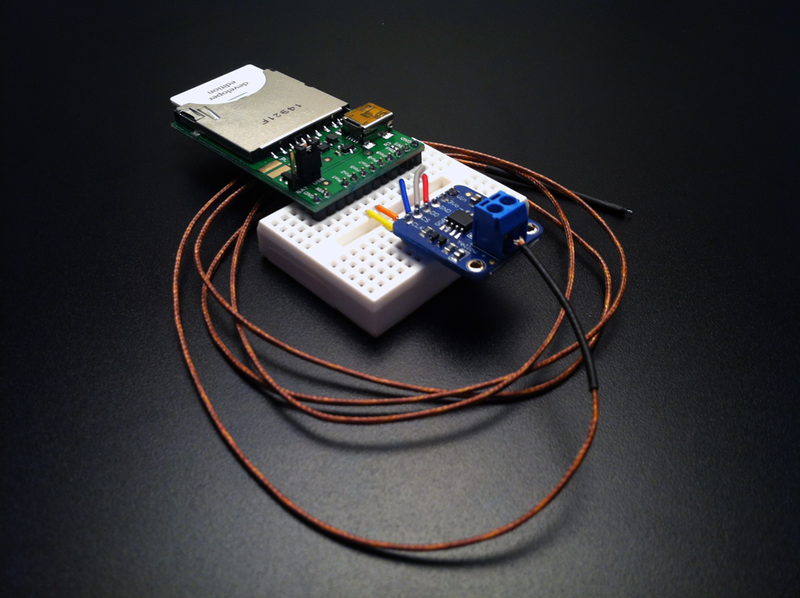
Materials
*These are some of the most important materials that will be needed for replicating this project. Please reference the images/videos to make a complete list of the materials*.



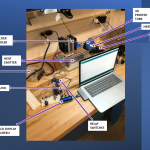
Arduino Segment
This project is heavily based on coding, so I have provided a breakdown of my code by segments. This code was written on Arduino and requires familiarity to the software in order to properly run.

The image carousel below shows the sub systems of the project.


Videos
This video serves as a complete breakdown of all of the components of the project, how the components work together, and their overall purpose.
This video illustrates how the system works when the patient’s temperature is detected to be ‘COLD’. The Peltier cooler is inactive and the heat dispersal continues.
This video shows the measurement of ‘HOT’ temperatures. When these hot temperatures are detected, the Peltier Cooler is triggered to turn on to begin the cooling process.
Future Work
After mastering the temperature chamber, the ideal next step of this project would be to design the ‘blanket’ that will actually be covering the patient. I have incorporated a SolidWorks model of a sectioned blanket to serve as inspiration. This blanket has been sectioned into the chest area, the abdomen area, and the legs. Each of the sections should be able to operate independently, but also be able to communicate with each other if connected at their junction points.

About the author:
Dessources is a BME MEng student from Medford, Massachusetts. He is passionate about drug delivery, tissue engineering, and his dog. This website was designed to compile the work he completed throughout the course of his 2022 Spring Semester at Duke for his class in Experiment Design and Research Methods.