Background
In 2010, the Affordable Care Act (ACA) was passed with a goal to expand access to insurance, increase consumer protections, emphasize prevention and wellness, improve quality and system performance, expand the health workforce, and curb rising health care costs [1]. Principle to the ACA was the process of shared decision making (SDM) [2]. By definition, SDM is ‘an approach where clinicians and patients share the best available evidence when faced with the task of making decisions, and where patients are supported to consider options, to achieve informed preferences” [3]. Whereas other definitions of SDM also exist, all converge to a similar notion: as a central part of patient-centered care, SDM is a dynamic process by which the healthcare professional (not limited to the physician) and the patient influence each other in making health related choices or decisions [4] upon which both parties agree.
Purpose
Whereas it’s difficult to argue against the principles of SDM (i.e., sharing best available evidence and considering all options), it is worth evaluating whether SDM has made a difference in the care provided to patients with musculoskeletal disorders, particularly a difference in clinical outcomes. The purpose of this blog is to evaluate the current evidence on SDM for individuals with musculoskeletal disorders.
Review of the Literature
Let’s start with early research. In May 2017, we [5] published a systematic review where we investigated whether or not SDM resulted in better health related outcomes for individuals with painful musculoskeletal disorders. Intriguingly, the review that looked at all trials associated with musculoskeletal disorders up to August of 2016, consisted of zero papers. In other words, despite the strong emphasis on SDM by the ACA, and despite its relative universal endorsement, there were no studies that evaluated its effectiveness in the six-year span between the passing of the ACA and our review. Needless to say, our conclusions [5] were “in the light of the current evidence (none), we estimate that it would be wise to study the effectiveness of SDM, and also be prudent before forcing its large-scale implementation”.
Not surprisingly, several papers involving SDM with musculoskeletal disorders were published since our review of nothing. In a 2018 trial [6], the authors found no significant differences in the mean scores for any of the patient reported clinical outcomes between patients who received an SDM intervention and controls There were no significant difference in the main outcomes during the 26 weeks follow-up (post-hoc analysis) nor in multivariate analysis. Although patients in the intervention group reported more involvement in decision-making, no significant effect of SDM on recovery, nor on health care consumption at 6 or 26 weeks after the consultation was found [7].
SDM has many ingredients but one key piece includes patient decision making support aids. Whereas these come in many levels of fidelity, more robust versions should actively engage both the patient and the health care provider in dialogue and reinforce a single decision. One study that evaluated the benefit of patient decision making support aids found that they may improve patients’ knowledge about treatment options for chronic musculoskeletal pain but largely did not impact other outcomes [8].
Perhaps the most interesting study was published by Patel and colleagues [9]. The paper titled “Primum non nocere: shared informed decision making in low back pain – a pilot cluster randomised trial” actually found worse outcomes associated with a decision support package; they suggested it may have had a substantial negative effect on clinical outcome, and is very unlikely to prove cost-effective. In fact, the authors summarized that “it cannot be assumed that the provision of additional information and support for patients to achieve informed decisions is risk free” and “Before decision aids are implemented they should be formally evaluated to ensure safety as well as efficacy and cost-effectiveness”.
Conclusion
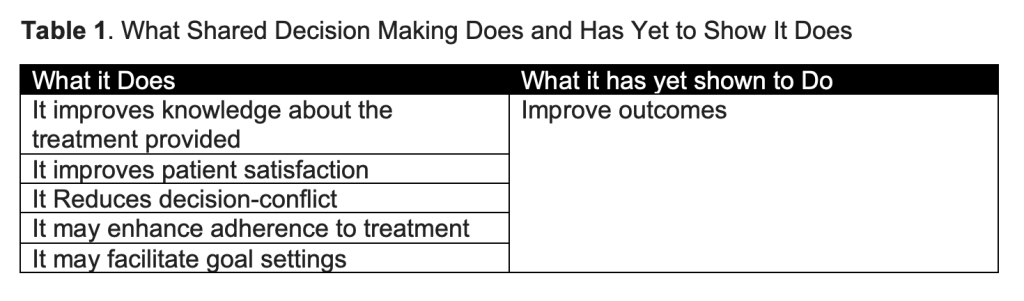
We will first start with the proverbial statement that all researchers seem to say; “we need more and better research”. In this case, it’s actually correct. We have to recognize that SDM is all about communication [10] – it is a complex approach that will most likely improve the experience of the patient, introduces them to options of care and reduce conflict related to their care. However, whether it improves health related outcomes is questionable (Table 1).
But like pain neuroscience education, spine stabilization, psychologically informed care, dry needling, neurodynamics, and a litany of introduced concepts before it, alone it likely has small effects at best. Should it be discarded? Absolutely not. It should be part of person-centered approach for individuals with musculoskeletal pain [11]. But will it directly lead to better clinical outcomes? Probably not, but it might improve goal settings between the clinician and the patient, which is probably where the “magic of SDM” could help pave the way to a more realistic shared decision making.
References
1. Affordable Care Act. Health Affairs. Available at: https://www.healthaffairs.org/topic/4#:~:text=The%20purpose%20of%20the%20ACA,curb%20rising%20health%20care%20costs.
2. Durand MA, Barr PJ, Walsh T, Elwyn G. Incentivizing shared decision making in the USA–where are we now? Healthc (Amst). 2015 Jun;3(2):97-101.
3. Elwyn G, Coulter A, Laitner S, Walker E, Watson P, Thomson R. Implementing shared decision making in the NHS. BMJ. 2010;341:c5146. doi: 10.1136/bmj.c5146.
4. Legare F, Witteman HO. Shared decision making: examining key elements and barriers to adoption into routine clinical practice. Health Aff (Millwood). 2013;32(2):276–84.
5. Tousignant-Laflamme Y, Christopher S, Clewley D, Ledbetter L, Cook CJ, Cook CE. Does shared decision making results in better health related outcomes for individuals with painful musculoskeletal disorders? A systematic review. J Man Manip Ther. 2017 Jul;25(3):144-150.
6. Sanders ARJ, Bensing JM, Magnée T, Verhaak P, de Wit NJ. The effectiveness of shared decision-making followed by positive reinforcement on physical disability in the long-term follow-up of patients with nonspecific low back pain in primary care: a clustered randomised controlled trial. BMC Fam Pract. 2018 Jun 28;19(1):102.
7. Sanders ARJ, de Wit NJ, Zuithoff NPA, van Dulmen S. The effect of shared decision-making on recovery from non-chronic aspecific low back pain in primary care; a post-hoc analysis from the patient, physician and observer perspectives. BMC Prim Care. 2022 Feb 2;23(1):22.
8. Bowen E, Nayfe R, Milburn N, Mayo H, Reid MC, Fraenkel L, Weiner D, Halm EA, Makris UE. Do Decision Aids Benefit Patients with Chronic Musculoskeletal Pain? A Systematic Review. Pain Med. 2020 May 1;21(5):951-969.
9. Patel S, Ngunjiri A, Hee SW, Yang Y, Brown S, Friede T, et al. Primum non nocere: shared informed decision making in low back pain–a pilot cluster randomised trial. BMC musculoskeletal disorders [Internet]. BioMed Central; 2014 [cited 2016 Sep 26];15:282.
10. Syed, H., Zubaria, K., Tanoli, A.Q., Khalid, S.U., 2019. Conceptual approach of shared decision making in physical therapy: an approach for betterment of patients? Int. J. Endorsing Heal. Sci. Res. 7, 131. https://doi.org/10.29052/IJEHSR.v7.i3.2019.131- 139.
11. Hutting N, Caneiro JP, Ong’wen OM, Miciak M, Roberts L. Person-centered care for musculoskeletal pain: Putting principles into practice. Musculoskelet Sci Pract. 2022 Dec;62:102663.
The content was amazing. I appreciated how you explored the topic and provided practical advice for readers. The examples you included were highly relevant, and your prose is clear. Thank you for sharing such an enlightening article.