Past and Present: Understanding this Important Link in Immunology Research and Training
December 2, 2022 • 9 min read
By Scott Behm
Our immune systems constantly evolve, learning from their past experiences and adapting to face future threats more effectively.
Similarly, immunology research continues to advance dynamically, using previous scientific discoveries as building blocks in the fight against new diseases. As a salient example, consider the breakneck speed at which scientists developed the COVID-19 vaccine, relying on previous mRNA and HIV research to do so.
The importance of this link between past and present is a key component of research and training in the lab of Georgia Tomaras, PhD, Professor in Surgery. Here, the study of old viral foes such as HIV and tuberculosis continues alongside research of newer ones, like SARS-CoV-2. In the pursuit of scientific discovery, seasoned researchers partner with those currently launching their research careers.
A Broad Platform to Pursue Immunology Research
General surgery resident Daniel Schuster, MD, joined Dr. Tomaras’ lab in 2020 at the height of the COVID-19 pandemic. While training at Albany Medical Center, he met Duke Surgery Department Chair Allan D. Kirk, MD, PhD, and learned of the new T32 Surgeon–Scientist Training Program (SSTP) at Duke. Through the program, Dr. Schuster would be able to complete a PhD in Immunology in just four years during a gap in his residency.

Georgia Tomaras, PhD
Professor in Surgery
With this expedited timeline, Dr. Schuster explored which Duke Surgery labs matched his research pursuits and would provide the resources needed to support his interest in immunology and transplantation.
“In order to complete the program in four years, I needed to join a lab right off the bat,” says Dr. Schuster. “I joined Georgia Tomaras’ lab prior to moving down to Duke, based on the breadth of her research. She prominently researches HIV, but more broadly infectious disease, like tuberculosis, influenza, malaria, and so forth. This would give me a broad platform upon which to explore a particular question of interest to me.”
Studying Both Old Foes and New Ones
Because Dr. Schuster moved to Durham in July 2020, it isn’t surprising that his first project in the lab explored the nuances of different patients’ immune responses to SARS-CoV-2. In a practical application of the lab’s specialties, the teams were intrigued by data from a subset of patients with coinfections of HIV and SARS-CoV-2.

Daniel Schuster, MD
General Surgery Resident
“One of the really interesting subsets that we explored was the group of individuals who had HIV prior to SARS-CoV-2 infection,” says Dr. Schuster. “We tried to understand how their immune response in the weeks after infection compared to individuals without HIV.”
In research published in September 2022, Drs. Schuster, Tomaras, and Kelly Seaton, along with their collaborators, reported that the immune response of some individuals living with HIV who recovered from COVID-19 did in fact differ from those without HIV.
Dr. Schuster explains, “The interesting finding was that when you look at patients who had recovered from symptomatic non-hospitalized COVID-19, there was a truncated humoral immune response among people living with HIV compared to people without HIV. There was less of a response in terms of antibody levels.”
Relying on Past Solutions to Address New Problems
According to Dr. Schuster, the takeaway of this research is that we can’t make assumptions that being infected with a pathogen and recovering provides the same immunity protection across the board. Not all recovered patients will have the same natural protection against SARS-CoV-2, and differences could possibly be linked to prior or current infections of other diseases.
For those with coinfection or who are immunosuppressed, hope is certainly not lost, Dr. Tomaras emphasizes.

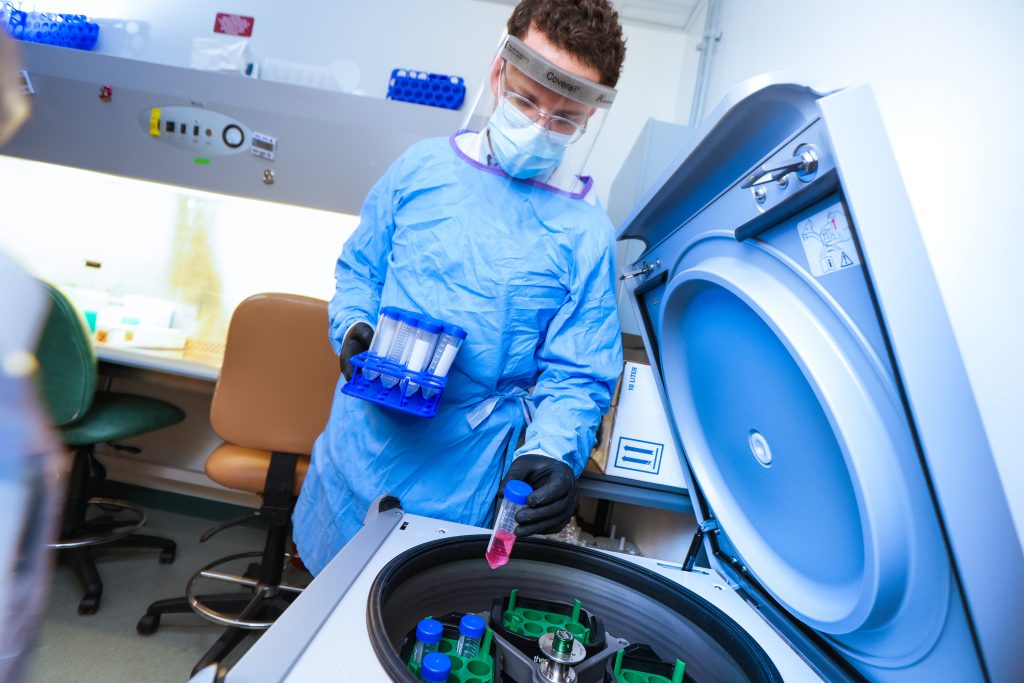
Drs. Daniel Schuster (left) and Georgia Tomaras (right) in lab.
“The good side is that although there is a dampened immune response; it’s not completely shut off,” she says. “The hope with the vaccine booster regimens and novel vaccine candidates is that we can still elevate up to the required protective level in somebody who is living with HIV or who is immunosuppressed.”
The message from this study, Dr. Tomaras adds, is that the research and medical communities need to pay closer attention to the effectiveness of vaccine regimens in certain populations—such as those living with HIV—rather than just focusing on the general population.
Overlapping Research Contributes to Progress
It’s well understood in the medical and research communities that the rapid development of a COVID-19 vaccine was owed greatly to years of previous mRNA research and decades of investment by scientists in HIV research. Now, there is potential for events of the last few years to positively impact the scientific community’s progress in developing an HIV vaccine.
“When the nation was confronted with the pandemic, there were resources and there was coordination,” says Dr. Schuster. “This happened in a way that really hadn’t been seen before. We saw how quickly labs in the U.S. and labs globally came together to formulate a vaccine within a record amount of time. I think that gives us hope that if you apply the same sort of support and collaboration, a similar boost in progress could be seen in HIV research.”
Dr. Tomaras amplifies this sentiment, emphasizing how the sense of speed, urgency, and efficiency that resulted in the development of a COVID-19 vaccine is now also being felt in and applied to the field of HIV research.
“When we look at how people came together during that time, both for funding and in the research community, I think it left a mark on the HIV scientist,” says Dr. Tomaras. “There’s always been a sense of urgency for an HIV vaccine for those of us who have been working on it, but it’s even greater now in seeing the speed at which you could bring a product to the market and understand the biology underneath it. It made everybody think we should move a lot quicker.”
Overcoming Barriers to Immunology Research
Along with the hope for progress that the COVID-19 response has given to the immunology research community, there is one important barrier that they had not considered before: vaccine hesitancy.
“The negative side is how people’s thinking has been impacted,” says Dr. Tomaras. “Here is a virus that is impacting the world and causing disease and death, but the vaccine isn’t always widely accepted. As an HIV vaccine scientist, we worked hard while inspired by the thought that, ‘If we can actually get an effective vaccine, of course people will take it, of course it will be implemented.’ That’s not the thinking anymore.”

General surgery resident Daniel Schuster, MD.
Challenges also exist with manufacturing vaccines on a global scale, and gaining access to populations from all countries. Fortunately, a practical benefit of the events of the COVID-19 pandemic is that countries have placed more importance on funding to have the capacity and infrastructure to manufacture their own vaccines, which could be used as a model in future vaccine rollouts.
Another potential barrier to HIV research is the stigma associated with diseases that more negatively impact LGBTQ+ communities, stigmas that can sometimes prevent scientific progress. While HIV is the most prominent instance, a more recent example was the mpox outbreak of 2022, which was mislabeled by the media as a sexually transmitted infection among the queer community.
“The early headlines to me were sort of alarming,” says Dr. Schuster. “It was almost an echo of unjust HIV history in terms of how it was identified, and quickly associated with a particular community. People went from a global view of how SARS-CoV-2 was infecting people, to mpox, thinking this must be another HIV-community, LGBTQ+ community disease. That is not the case, but there was still a stigma in the media reporting on it.”
As Dr. Tomaras shared previously, understanding how disease impacts particular communities uniquely is a valuable tool as we work to identify solutions to clinical and research problems.
Funding for Future Research is Key
And of course, the biggest barrier to immunology research is an age-old question: how will it be funded? Continuing vaccine and immunology research with speed and efficiency cannot happen without funding and community support.
Dr. Tomaras’ lab is supported by a diverse portfolio of funding from federal, foundational, and private sources who recognize the importance of the team’s work. Currently, this funding is supporting continuing research along with new scientific questions.
One exciting research focus for the lab is Immunoglobulin A (IgA), an antibody that plays a role in the immune function of mucous membranes. Dr. Tomaras says that new research in IgA is just starting to unfold and has broad application in research on HIV, COVID-19, influenza, and other respiratory diseases. It remains a novel and understudied area, and a lot of questions remain.
“Our lab previously discovered a key role for circulating IgA in HIV vaccines that we need to learn how to control to make vaccines more effective. We also know that IgA, especially at the mucosal site, can be antiviral and designs are urgently needed to optimize the production of local IgA,” says Dr. Tomaras. “We know there are protective effects and we need to unleash IgA’s potential, especially for blocking transmission of disease between people.”
Dr. Schuster adds that a better understanding of IgA could impact our understanding of many aspects of health across a person’s life.
“It could impact every stage of life,” says Dr. Schuster. “Think about maternal fetal protection, and then children with diseases like RSV [respiratory syncytial virus] which is making headlines about respiratory viruses, and then there’s influenza and SARS-CoV-2. There are many touchpoints throughout one’s life that a better understanding of IgA, or a modification of IgA response, could be really impactful.”
Understanding the fine-tuning of antibody responses is another exciting avenue for discovery in the lab. Using adjuvants—which are additives to a vaccine that can enhance the immune response—in a human clinical trial testing HIV vaccines could offer the opportunity to pull back the curtain on the regulation of antibody functions important for clearing infections.
“Once we better understand the fine-tuning we can control it, and then design more efficacious vaccines of the future,” says Dr. Schuster.
New Opportunities for Young Researchers
Dr. Schuster says he’s grateful for the continual mentorship from Dr. Tomaras, and he is looking forward to continuing his research supported by the T32 SSTP program.
“There’s only one other resident in the program [A. Justin Rucker], so we’re the inaugural class,” Dr. Schuster says. “This structure could really be a viable alternative to the more traditional MD / PhD path. It will truncate the time between basic science training and independent funding, to hopefully speed up progress at the very early part of my career.”
Giving the space for younger trainees in her lab to explore their own interests is key to their success, Dr. Tomaras says.
“We give a lot of freedom to think about questions that they’d like to answer,” Dr. Tomaras says. “We put those questions in the context of where we have the resources and funding, and we give the opportunity to synthesize information from different scientific fields, using multiple data streams, and to think about the immune system as a whole.”
Dr. Tomaras adds that this understanding of how all of the mechanisms of the immune system fit together, and how the immune system develops and changes over time—past and present—is a key component of the training process in her lab.
Dr. Tomaras recently took on an even greater role as a leader and mentor in Duke Surgery. In December 2022, she assumed the role of Division Chief of the Division of Surgical Sciences, a role held by Dr. Kent Weinhold for 14 years.
Give to the Division of Surgical Sciences
Private philanthropy is essential to the discovery of new techniques, technology, and treatments to improve the health of all through innovative and cutting-edge research.
A gift to the Division of Surgical Sciences will help the division to achieve its mission of bringing research discoveries from the lab to clinical practice through the pursuit of the latest advances in translational research, and to fulfill a commitment of training world-class research scientists and academic surgeons.

