This month, we received a new award from the National Institute of Allergy and Infectious Diseases (NIH) to study interventional approaches to improve the targeting of artemisinin combination therapy to individuals with confirmed malaria infection. This new project builds on our previous work to target antimalarials through a partnership between community health workers and private medicine retailers.
In 2016, the WHO estimated that 216 million cases of malaria occurred worldwide, yet more than 400 million treatment courses of first-line antimalarials (artemisinin combination therapy or ACT) were consumed. This substantial overuse of ACTs is driven in large part by the private retail sector. More than half of families in sub-Saharan Africa seek treatment for febrile illness in retail medicine outlets where ACT is available over-the-counter, but malaria diagnostic testing is virtually absent and presumptive treatment of fever as malaria is the norm. Availability of inexpensive, donor-subsidized ACTs and the absence of diagnostic testing lead to very poor targeting of ACTs to people who need them. Individuals without malaria consume between 65-90% of ACTs distributed through retail outlets. Unnecessary consumption of ACTs is a drain on scarce public health resources and threatens the future sustainability of publicly-funded subsidies.
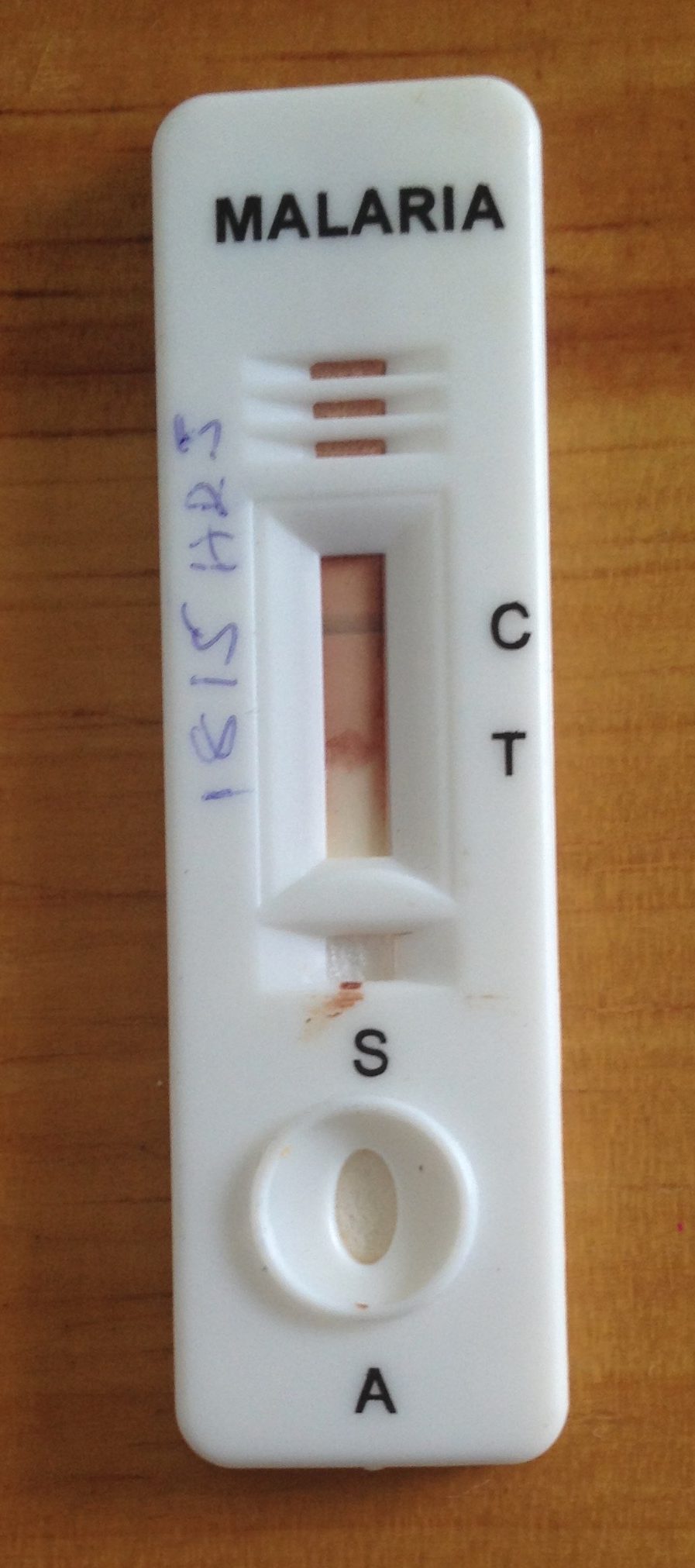
Although accurate point of care diagnostics are available for malaria (called rapid diagnostic tests or RDTs), they are uncommon in the retail sector and, where they have been tried, their impact on appropriate ACT use is often poor. We hypothesize that both providers and clients’ decisions about testing and treatment are strongly influenced by price (or profit). In response to this, we will test a scalable, policy-relevant strategy that integrates testing and treatment subsidies for the client, with incentives to the provider to test for malaria. ACT subsidies will be available only to customers with a positive malaria test (conditional ACT subsidy). Differential ACT pricing for clients based on the results of the diagnostic test, combined with provider rewards for testing, will align both consumers and providers incentives (price and profit) with testing and appropriate ACT use. Our approach will ensure that public subsidies are directed to confirmed malaria cases thereby enhancing the sustainability of such programs. By allocating subsidy dollars across both testing and conditional treatment (rather than universal, treatment-only subsidies), we can reduce the cost of subsidizing malaria treatment and improve targeting of ACTs without compromising access.
This work will be carried out in Kenya and Nigeria in collaboration with Clinton Health Access Initiative.

