Our very own Dr. Josephine Malinga was featured by Women in Malaria! Congratulations Dr. Josephine!
-
Recent Posts
Archives
Our very own Dr. Josephine Malinga was featured by Women in Malaria! Congratulations Dr. Josephine!
Posted in News
The School of Medicine features the new Partnership for Malaria Education and Academic Research Laboratory on the website!
Posted in News
Over the last few months, we have worked on setting up community-based malaria surveillance in Turkana with the help of the County Health Leadership. Here are a few highlights:
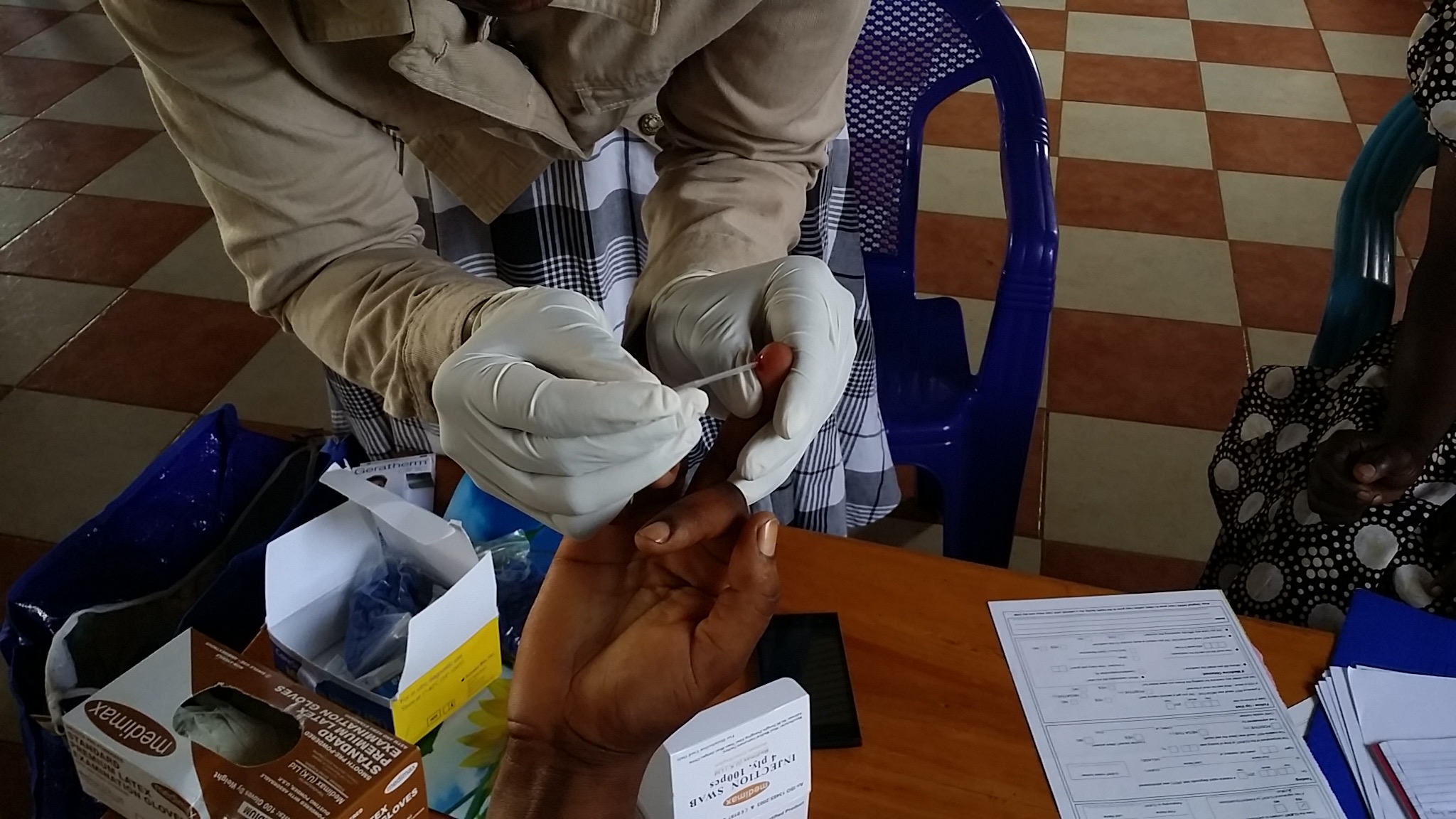
We trained 100 community health workers from five communities to follow malaria cases identified in the health facility to their home and test household members for malaria

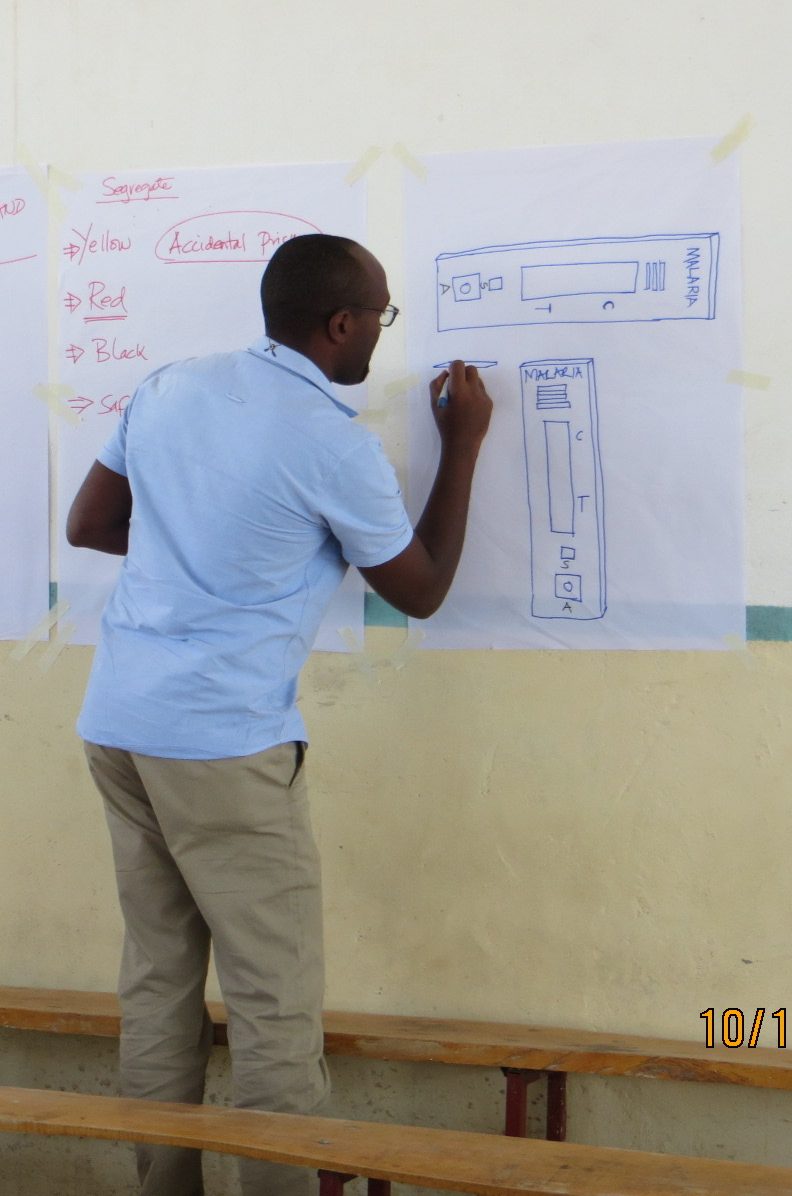
 No power in the training hall so all of our ‘slides’ had to be drawn by hand
No power in the training hall so all of our ‘slides’ had to be drawn by hand
We also initiated surveillance of travelers coming into Turkana via the road and the airstrip. We offer free malaria diagnostic testing and treatment following a positive test. We have screened hundreds of passengers and found several malaria cases among them.
Entomological surveillance for both larvae and adult vectors is now beginning.
 Hand-dug canals leading from the Turkwel river into the fields are a potential source of mosquitoes if the water is not moving or if stagnant pools form.
Hand-dug canals leading from the Turkwel river into the fields are a potential source of mosquitoes if the water is not moving or if stagnant pools form.

Along the dry riverbed, people dig shallow pits where water seeps up from below. Water is scooped out for household use. The pits are excellent mosquito breeding sites


We also tested light traps for catching blood-seeking mosquitoes inside homes


We had the good fortune to sleep outside at the Turkana Basin Institute and see the sunrise over the river.

Posted in News

Wendy OMeara and Eric Nalianya demonstrate for Governor Wangamati and Dean Atwoli the telemedicine capacity being developed at PEARL
On Thursday, the Governor of Bungoma County, the Vice Chancellor of Moi University, the Dean of Medicine and Dean of Public Health of Moi University joined Dr. O’Meara, Dr.
Laktabai and Dr. Kisaka to official open the PEARL laboratory in Webuye, Kenya.
PEARL is the latest development in a longstanding partnership between Moi University in Eldoret, Kenya, Webuye County Hospital and Duke University. The lab is being established under the leadership of Jeremiah Laktabai, chair of the Department of Family Medicine at Moi University, and Wendy Prudhomme-O’Meara, an associate professor of medicine and global health at Duke University who’s based full-time in Eldoret.
Housed in two forty-foot refurbished shipping containers with a state-of-the-art multi-head teaching microscope, the lab will initially focus on building clinical microscopy skills among technicians across 224 facilities in the region. Microscopes are a cost-effective and versatile tool for examining patient specimens and making accurate diagnoses, and nearly every rural health center in Kenya has a microscope. However, with the exception of malaria smears, these diagnostic tests are rarely performed due primarily to lack of expertise.
“There are so many different ways you can improve patient care with a microscope if you have the training to use it,” said Prudhomme-O’Meara. “We’re developing programs to help technicians in rural facilities learn how to better support clinical care with their microscope, which in many cases is the only piece of diagnostic equipment they have.”
Another goal of the lab is to support ongoing research efforts in Bungoma County, including studies on and interventions for HIV, hypertension, diabetes, fevers in children and malaria transmission, led by local and international faculty and trainees.
“Through our collaborative research projects, we’ve been able to improve care and prevention for illness in Bungoma County and beyond,” said Prudhomme-O’Meara. “We expect that PEARL will help us expand this work and impact, as access to a research laboratory will allow Moi University faculty and their partners to tackle critical research questions affecting clinical care and community health.”
Here’s a link to a story in the Kenyan national news:
http://kutv.co.ke/moi-university-to-put-up-a-research-laboratory-for-webuye-sub-county-hospital/
The lab building and infrastructure were made possible by support from Webuye County Hospital, Duke University and The Bill & Melinda Gates Foundation.

Posted in News
 This month, we received a new award from the National Institute of Allergy and Infectious Diseases (NIH) to study interventional approaches to improve the targeting of artemisinin combination therapy to individuals with confirmed malaria infection. This new project builds on our previous work to target antimalarials through a partnership between community health workers and private medicine retailers.
This month, we received a new award from the National Institute of Allergy and Infectious Diseases (NIH) to study interventional approaches to improve the targeting of artemisinin combination therapy to individuals with confirmed malaria infection. This new project builds on our previous work to target antimalarials through a partnership between community health workers and private medicine retailers.
In 2016, the WHO estimated that 216 million cases of malaria occurred worldwide, yet more than 400 million treatment courses of first-line antimalarials (artemisinin combination therapy or ACT) were consumed. This substantial overuse of ACTs is driven in large part by the private retail sector. More than half of families in sub-Saharan Africa seek treatment for febrile illness in retail medicine outlets where ACT is available over-the-counter, but malaria diagnostic testing is virtually absent and presumptive treatment of fever as malaria is the norm. Availability of inexpensive, donor-subsidized ACTs and the absence of diagnostic testing lead to very poor targeting of ACTs to people who need them. Individuals without malaria consume between 65-90% of ACTs distributed through retail outlets. Unnecessary consumption of ACTs is a drain on scarce public health resources and threatens the future sustainability of publicly-funded subsidies.
Although accurate point of care diagnostics are available for malaria (called rapid diagnostic tests or RDTs), they are uncommon in the retail sector and, where they have been tried, their impact on appropriate ACT use is often poor. We hypothesize that both providers and clients’ decisions about testing and treatment are strongly influenced by price (or profit). In response to this, we will test a scalable, policy-relevant strategy that integrates testing and treatment subsidies for the client, with incentives to the provider to test for malaria. ACT subsidies will be available only to customers with a positive malaria test (conditional ACT subsidy). Differential ACT pricing for clients based on the results of the diagnostic test, combined with provider rewards for testing, will align both consumers and providers incentives (price and profit) with testing and appropriate ACT use. Our approach will ensure that public subsidies are directed to confirmed malaria cases thereby enhancing the sustainability of such programs. By allocating subsidy dollars across both testing and conditional treatment (rather than universal, treatment-only subsidies), we can reduce the cost of subsidizing malaria treatment and improve targeting of ACTs without compromising access.
This work will be carried out in Kenya and Nigeria in collaboration with Clinton Health Access Initiative.
Posted in News
 ExactDx in PLoS Medicine! The primary results of our community-based cluster randomized trial in western Kenya. The main points:
ExactDx in PLoS Medicine! The primary results of our community-based cluster randomized trial in western Kenya. The main points:
Posted in News
 This week, the Kenya National Malaria Control Programme hosted the 3rd Kenya Malaria Forum in Nairobi. ExactDx team presented in two session. Joseph Kipkoech (above) presented results from the Malaria Voucher Study to demonstrate how targeting of antimalarials could be improved for patients who buy drugs over-the-counter. Wendy O’Meara presented about malaria in Turkana (below) and our work on understanding the magnitude and source of the malaria problem in this unique ecosystem.
This week, the Kenya National Malaria Control Programme hosted the 3rd Kenya Malaria Forum in Nairobi. ExactDx team presented in two session. Joseph Kipkoech (above) presented results from the Malaria Voucher Study to demonstrate how targeting of antimalarials could be improved for patients who buy drugs over-the-counter. Wendy O’Meara presented about malaria in Turkana (below) and our work on understanding the magnitude and source of the malaria problem in this unique ecosystem.

Posted in News
 We were delighted to host Chris Plowe (DGHI Director), Eugene Washington (Chancellor), Chris Tobias (DGHI Director of Finance and Operations) and Jamie Mills (Grants and Contracts Manager) to Eldoret this week! We were able to introduce them to the wide range of collaborations and initiatives in Eldoret and most importantly introduce them to our partners here at Moi University. They were able to visit the Cardiac Care Unit at Moi Teaching and Referral Hospital, a group of peer counsellors working with Eve Puffer’s team, and visit our community-based cohort in Webuye, Kenya.
We were delighted to host Chris Plowe (DGHI Director), Eugene Washington (Chancellor), Chris Tobias (DGHI Director of Finance and Operations) and Jamie Mills (Grants and Contracts Manager) to Eldoret this week! We were able to introduce them to the wide range of collaborations and initiatives in Eldoret and most importantly introduce them to our partners here at Moi University. They were able to visit the Cardiac Care Unit at Moi Teaching and Referral Hospital, a group of peer counsellors working with Eve Puffer’s team, and visit our community-based cohort in Webuye, Kenya.

Dr. Plowe trying his hand at catching mosquitoes by vacuum aspiration in one of our cohort households

His catch!

Dr. Washington examining some bloodfed female anopheles mosquitoes with Eric Nalianya, one of our field researchers

 Dr. Plowe and Dr. Washington learning the finer points of identifying mosquito species by microscope
Dr. Plowe and Dr. Washington learning the finer points of identifying mosquito species by microscope

Dr. Plowe and Dr. O’Meara inspecting a sticky barrier trap for mosquitoes
April 2018

Members of the ExactDx team visited Lodwar, Kenya to meet with government health officials, visit public health facilities and learn about malaria in the region. 
We visited several government and mission clinics in Turkana Central. Hoping our fact-finding mission leads to some productive partnerships and new approaches to malaria control in this challenging setting.

Dispensary 30 kilometers outside of Lodwar serving a pastoralist community near the Turkwel river
Posted in News
Last week we welcomed Verona Liao and Assumpta Nantume to Eldoret. Both are Masters of Science in Global Health students who have joined our team in Eldoret to work on their masters theses. Assumpta will be working with our EPiTOMISE team in Homa Bay and Verona will be using innovative new techniques to try and catch outdoor resting mosquitoes in Webuye. We will post more about their adventures in the coming weeks.

Looking for mosquito collection sites in Webuye
