Welcoming a New Division: Minimally Invasive Surgery
December 2, 2022 • 7 min read
By Michelle Antoinette Macalino

Jacob Greenberg, MD
Chief, Minimally Invasive Surgery
While the twelve divisions in Duke’s Department of Surgery specialize in various aspects of patient care, education, and research, they do not exist as separate islands.
For some specialties in Duke Surgery, such as minimally invasive surgery (MIS), overlaps across divisions can result in inefficiencies and poor utilization of resources.
With MIS performed in metabolic procedures, surgical oncology, and trauma, the answer to this problem was simple: to create a new division that will encourage stronger collaboration amongst faculty and trainees who specialize in MIS.
As a result, the new Division of Minimally Invasive Surgery launched in July 2022, comprising faculty from the former Metabolic and Weight Loss Division, and also faculty from Surgical Oncology and Trauma, Acute, and Critical Care Surgery. Jacob Greenberg, MD, Instructor in the Department of Surgery, was appointed chief of the new division in late 2022.
What is Minimally Invasive Surgery?
“MIS is sort of like a catch-all phrase that tends to cover a large portion of what has historically been general surgery,” says Dr. Greenberg. “By bringing the Metabolic and Weight Loss Surgery Division into the Division of MIS, we can expand just beyond the Metabolic and Weight Loss program and really work on building other programs alongside it, all while utilizing the resources already available in that program.”

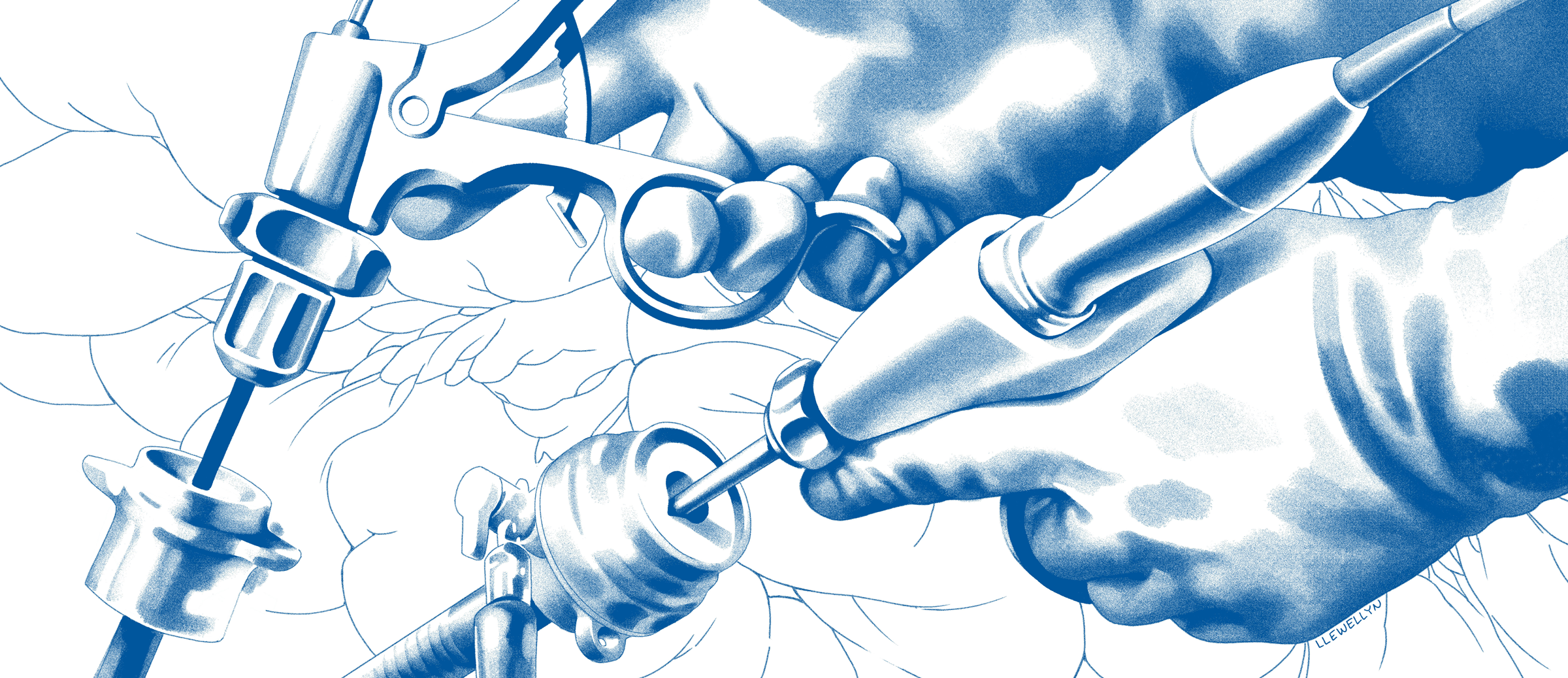
Guided by a small camera, the extended shafts of laparoscopic instruments allow surgeons to work through small incisions for faster patient recovery.
At its core, MIS uses techniques and tools to perform surgery through smaller incisions with the least amount of trauma, resulting in superior outcomes for patients. MIS includes laparoscopy, robotic surgery, endoscopic interventions, and a combination of these approaches.
With the establishment of this division, Duke Surgery will centralize the innovative equipment and advancement techniques to focus on procedures that utilize the minimally invasive skill set, such as hernia repair, gastroesophageal reflux disease (GERD) treatment, and bariatric care.
During the early planning stages, Department Chair Allan D. Kirk, MD, FACS collaborated with division chiefs Peter Allen, MD, and Dana Portenier, MD, from the Divisions of Surgical Oncology and Metabolic and Weight Loss Surgery, respectively. They met with a group of surgeons to discuss the formation of the Division of MIS.
Through these meetings, Dr. Kirk expressed the importance of reallocating surgeons into one division who are practiced and skilled in minimally invasive surgery.
“What we had with our divisional structure before was a bunch of surgeons that use minimally invasive techniques somewhat divided up amongst different divisions, and we weren’t able to really collaborate in a way that let us provide patients with the best experience,” says Dr. Portenier. “What we’re doing is pulling together all the similarly skilled and like-minded surgeons around the MIS space to then concentrate the different focus areas within this sphere.”
For the Betterment of All Patients
One of the main goals for the Division of MIS is to create programs that will provide the best surgical care for all patients through efficiency. By combining faculty with mutual interests in applying minimally invasive techniques to treat a broader range of diseases, faculty will be able to support more patients at Duke. Faculty from the Division of Metabolic and Weight Loss Surgery, such as Keri Seymour, MD, Associate Professor of Surgery, were already utilizing these techniques.

Dr. Keri Seymour (right) assists a resident in a laparoscopic procedure at Duke Regional Hospital.
“The bariatric surgeons at Duke Surgery have performed >98% of weight loss procedures using laparoscopic and robotic techniques since 2005,” says Dr. Seymour. “Minimally invasive technology has allowed the bariatric surgeons to successfully operate on Duke patients weighing >500lbs after several abdominal procedures and with endoscopic interventions. The inclusion of the Metabolic and Weight loss Surgery team in the Division of MIS will allow sharing of expertise and ultimately advance the care of our patients.”

Keri Seymour, MD
Associate Professor of Surgery
Along with bringing together surgeons from the Divisions of Metabolic and Weight Loss Surgery and Surgical Oncology, faculty from other divisions who have worked with minimally invasive techniques will be allocated into MIS.
One such faculty member joining the MIS division is Philip Fong, MD, Assistant Professor of Surgery, from the Division of Trauma, Acute, and Critical Care Surgery.
“I’m grateful for the time I spent in the Division of Trauma, Acute, and Critical Care Surgery since it has taught me about the benefit of working within a health system rather than focusing on just being at one hospital,” says Dr. Fong. “There is a certain patient population that requires emergency surgery that may not be candidates for a minimally invasive approach, but as someone who works mostly with those types of patients, I hope that I can bring some of that knowledge to help my new colleagues.”
Philip Fong, MD
Assistant Professor of Surgery
Generally, most trainees in trauma and critical care surgery do not learn MIS techniques. However, at Duke University Hospital (DUH), where there are more trauma and critical care cases, many surgeons were trained in MIS and those surgical skills will eventually be shared with Duke Surgery faculty and trainees in Duke Regional Hospital (DRH), Duke Raleigh Hospital (DRAH), and Central Carolina Surgery (CCS).
“Dr. Fong has been at DRH with all of the bariatric surgeons working hand-in-hand for a long time, where we’ve been able to share and cross pollinate those minimally invasive techniques to him,” says Dr. Portenier. “We felt that it made more sense to have surgeons that use these advanced minimally invasive techniques cover our more elective emergency cases so that we can bring the MIS skillset to the patients that come into our emergency rooms.”
A More Centralized Program
The concentration of the surgeons in the MIS Division will provide a more efficient clinical experience for patients by expanding the services and care offered to them. Such services include the development of a hernia center to unite care provided at DUH, DRH, DRAH, and CCS into one major program and division.
“By moving everyone that practices in hernia into one division, we can better offer patient centered care,” says Dr. Greenberg. “If a patient wants to be seen in either DUH, DRH, DRAH, or CCS based on their preferences in geographic location or overall care, then we can easily let the patients have that choice. This unity will make it easier for us to collaborate and work together across the four sites to provide exceptional care to all patients. I think such a change is better for patients and certainly better for patient satisfaction.”

Dr. Jacob Greenberg (left) assists general surgery resident Dr. Konstantinos Economopoulos with a procedure at the Davis Ambulatory Surgery Center (DASC) near Duke Regional Hospital.
Unifying surgeons at several locations for a new division will bring its own challenges, but with new leadership from Dr. Greenberg and the enthusiasm from faculty, these challenges will help unify the Division of MIS into a stronger program.
“The surgeons in the Division of MIS are exceptionally talented and incredibly willing to work together to advance patient care,” says Dr. Seymour. “The division will positively impact patients by creating more opportunities for seamless clinical care, expansion of research opportunities in MIS, and a more advanced training program for future residents.”
A Seamless Training Experience
Over the last five years, several residents in Duke Surgery have pursued a fellowship in minimally invasive surgery. With the new MIS division, faculty can look forward to creating opportunities for residents to learn minimally invasive techniques in a structured fashion in preparation for a fellowship.
With the help of modern technology, training surgical residents has been enhanced by the addition of dual robotic surgery consoles in several operating rooms and an elective rotation for robotic surgery. Including MIS faculty in the General Surgery Residency Program will augment the residents’ technical skills under the guidance of the Division of Surgical Oncology’s Katherine Jackson, MD, Assistant Professor of Surgery, and Sabino Zani, MD, Associate Professor of Surgery.
“These opportunities will expose residents to advanced technology earlier in their training,” says Dr. Seymour. “By the time they graduate they’ll leave with superior technical skills in minimally invasive surgery.”
A Hopeful Endeavor

Dr. Dana Portenier
Assistant Professor of Surgery
As Duke Surgeons continue to look for innovate approaches to patient care, the establishment of the Division of MIS will create the multidisciplinary clinical care needed to deliver excellent outcomes.
“Our mission here is that by being on the cutting edge of technology, we’ll be giving our patients the very latest surgical techniques, and so our trainees leave Duke having been trained at the most advanced skill level,” says Dr. Portenier. “I think that it’s undeniable that there’s a link between our surgery of today and our technology, and I believe that MIS surgery captures the essence of exploring these technologies and figuring out how we best use them for our patients.”
Give to the Division of Minimally Invasive Surgery
Gifts to the Duke Division of Minimally Invasive Surgery, large and small, provide an important source of unrestricted support for research, education, and patient care. Gifts can also be directed to the surgeon of your choice to support individual research efforts.
Charitable contributions can improve the lives of people in the community and beyond, as Duke innovations in minimally invasive surgery extend across the country and around the world.