What’s happening when the overhead speakers in the hospitals, hallways, and clinics of Duke University Medical Center alert everyone to a Code Blue?
A designated team of doctors, nurses, and Duke Life Flight medics is converging on a person in need of emergency care.
One day in October 2018, the person in need was Betsy Hames, chief human resources officer for the School of Medicine. She was in her office high in the Davison Building when she suffered cardiac arrest and collapsed on her desk. Her colleagues called for help, and that triggered Duke’s Code Blue system.
But where was the sixth floor, and how was the Code Blue team to get to her?
Follow along as Hames and the team recount what transpired that day, and how each person played an important part in her miraculous recovery.
Resources
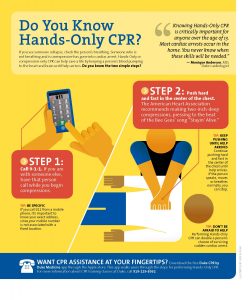 In this episode, Dr. Adrian Hernandez highlights the importance of cardiopulmonary resuscitation (CPR): The first person who can start CPR is going to make the biggest difference, he says.
In this episode, Dr. Adrian Hernandez highlights the importance of cardiopulmonary resuscitation (CPR): The first person who can start CPR is going to make the biggest difference, he says.
“Every minute counts. You can make a difference — you don’t have to be a doctor, you don’t even have to be in healthcare. The first person to start things is can make the biggest difference.”
- See this infographic from Duke Health: Do You Know Hands-Only CPR?
- See the CPR section from the American Heart Association
Duke Heart Center offers monthly CPR classes for employees, visitors of Duke Hospital and University, and the community. To register, go to https://www.dukehealth.org/events. The schedule for the next few months:
- March 29 3 p.m. to 4:30 p.m. in Duke Medicine Pavilion (DMP) room 2W96
- April 25 12 p.m. to 1:30 p.m. in DMP 2W29
- May 24 2:30 p.m. to 4 p.m. in DMP 2W96
What to do when you hear Code Blue
Duke Health employees who hear a Code Blue page should help if they’re trained medical professionals, says Cory Miller, BSN, RN, CCRN, co-chair of the Code Blue Oversight Committee. But others can help by providing directions, as Evelyn McClure did during Hames’s incident.
And, says Miller, it’s important to keep the way clear so the Code Blue team can get to the person in need as fast as possible.
How to call for help within the Duke University Medical Center
If you find someone who is unresponsive — the person doesn’t answer when you gently shake their shoulder and ask ‘Are you OK’? — call or yell for help from people nearby.
If no one else is around, but a phone is handy, call 115 (or 911 if at an off-site clinic).
Tell the operator the following information:
- That you have a medical emergency.
- Your location (clinic address, building name and floor, room or suite number, etc.).
- A phone number that does not go to voice mail or a phone tree.
- Whether the person in need is an adult or child.
- Description of the event.
Then wait for the operator to hang up first. Stay with the person, and direct help to your location.
Other codes
Duke University Hospital has other designated codes to guide emergency response to incidents, including fire, security, utility failure, and more. See a list of the codes.
Transcript
Betsy Hames: It was just sort of a typical Monday. And I had been at meetings at different locations and had called home and spoke with my husband and between meetings and he said I sounded great, I sounded wonderful. And I was looking forward to getting off maybe on time that day because of my meetings schedule that afternoon and got back to my office and just the normal routine kinds of things, had lunch, was talking to my associate, and we were laughing about something and I keeled over in cardiac arrest.
Karishma Sriram: This is Voices of Duke Health. I’m Karishma Sriram. Today, Betsy’s story.
Betsy Hames works in Human Resources at Duke. When she passed out, her co-workers immediately sought help. Dr. Adrian Hernandez, a cardiologist, was among the first to respond. He was sitting in his office…
Dr. Adrian Hernandez: And my assistant came running in and saying someone needs help, they passed out. And I was thinking that it was someone that was in kind of our area and it turned out that was not the case or as I know you know, it’s Betsy.
Karishma: And Betsy was in her office, in Duke South.
Dr. Jonathan Bae: This is primarily an outpatient treatment setting and office space. So there’s not an ICU right next door it’s it’s actually in a hospital about 10 minute walk away.
Karishma: This is Dr. Jonathan Bae.
Dr. Bae: And there was an overhead page that said, code blue, sixth floor of this particular zone. And many of us just started running to that zone. I remember coming out of the hallway, because you know you never know because you are further away from the main hospital, takes a little bit of a longer time for our First Responder Team and Life Flight to get there.
Karishma: Another doctor who was notified was Dr. Cara O’Brien.
Dr. Cara O’Brien: I actually was wandering around the green zone and I didn’t find anybody and this was before it was overhead paged. And I was trying to find where I was supposed to go, I actually made a complete lap around between the yellow zone and the green zone and didn’t see anybody. And in the meantime picked up a couple other stragglers because I was like there’s a code somewhere, can you help me find it?
Karishma: Meanwhile, Dr. Hernandez had sprung into action. And he’d actually never been to Betsy’s office so.
Dr. Hernandez: On kind of a instinct, I turned and said like, where’s her office, what number? And they said, six hundred something. I didn’t even know the building had six floors. So ran up the stairs and Scott Gibson followed with me and then we got up to the fifth floor or fourth floor, I can’t remember exactly. And it was like we were in this maze because it wasn’t a straight line up the stairs to get to the sixth floor. And there are just a series of doors. It was almost like we’re in some type of Harry Potter house where you try to find the mystery door.
Karishma: And Dr. Bae wasn’t having much luck either.
Dr. Bae: Where is it? Where is the sixth floor? And we just started running in that direction and then we were running up the steps of what we think is the right area of the building, and we get to this place where it’s like it only goes to four or five. And one of the really I think small miracles here there was an Environmental Services employee who was there, Evelyn, who had recognized that people may get lost and was standing by the door pulling people in like, it’s here, go this way, go this way.
Evelyn McClure: I was on the fourth floor Green Zone cleaning the men’s bathroom.
Karishma: That’s Evelyn McClure.
Evelyn: And I happened to hear this code blue. And I was like, OK. And when they say green I was like, oh my god that’s my area. So then I listened again when they did a second one and I was like, OK, they said the six floor, I said they’re my ladies up there, my girls up there. I said something going on, I got to go. I just felt led that I had to go and be there, standing at this door, because I know which way the code team travel up the steps and not using an elevator, and so I said to myself I got to go. So I went to the door and I was really excited when I seen a head pop up. And the first thing they say, do you know where the second floor, when they said, do you know where the second floor, I was like OK, I said we gonna make about face. I made about face, I said it’s time to go. I said come on, I’ll show you. And so we run up the steps, we did.
Karishma: Thanks to Evelyn, they finally found Betsy’s office.
Dr. Hernandez: And that’s when I saw you, with your head on the table, passed out. And we pulled you off the table and we started CPR and then soon the Life Flight crew had made it up and started helping us out. But that’s a memory I won’t ever forget, just seeing you passed out on the table, not knowing what’s going to happen next.
Karishma: Meanwhile, Dr. O’Brien arrived, and jumped into her role as code team leader.
Dr. O’Brien: And I just stepped back and said, OK, what are the other roles that we need in a code. Who’s going to place I.V. access, and I can remember at that point Lisa Pickett was there. She happened to be in a good position to do it, and said Lisa, you’re going to be our access. And you know what are the other crucial roles and just looking at the, sort of, people that were there at that point and just, yeah, I mean I think Cory’s drilled it into us for years now that these are the rules that have to be identified and a code no matter who they are and what credentials they have.
Karishma: Dr. O’brien just mentioned Cory. That’s Cory Miller, who’s in charge of training staff on how to resuscitate patients during codes. Here’s Cory.
Cory Miller: I think that was one of the best things that I saw happen was the you know rank, position, seniority, all of that just, as it should, kind of goes out the window and everybody does what they’re best equipped to do at that moment. It was so quiet and calm. Sorry you missed it! It was amazingly quiet and calm and everybody just fell into a place that they, into a role they needed, you know that needed filling. Everybody brought a piece of equipment or a med, everybody had a piece of the puzzle to bring. And we had done a lot of planning and a lot of prepping and a lot of testing of the system to make sure that we would have the right equipment and right people and right medications come to all codes in all areas, but that was the first time I think we really put it to an extreme test. But it worked out everything that was supposed to show up showed up, all the people that were so sharp showed up and everybody knew the role and I was pretty proud of the whole system.
Karishma: Despite how smoothly the code was going, the team still felt worried about Betsy.
Dr. O’Brien: This was a prolonged resuscitation. Probably one of the longest that I’ve personally been involved with and I think you know nobody wanted to give up. And yeah we had kind of, I don’t know, you sort of lose track of time in these events and more and more people had come and we were sort of trying to figure out how, we knew we needed to get you out of there.
Karishma: Eventually, they were able to get Betsy to the Emergency Department.
Dr. Hernandez: As she was leaving the room, we had no idea what was going to happen. She was on a special machine that would continue compressions and we were setting things up so when she arrived in the emergency department she could be put on a bypass machine to continue the blood flow. And honestly I wasn’t sure I would see her again.
Karishma: And Dr. Bae shared that fear.
Dr. Bae: There was a general feeling in the room that this was this was not going to turn out well. We were really worried about that. There were some of your team members there, I remember standing with them and talking to them and trying to provide support and counsel to them about the next steps. I remember actually being fairly shooken up by the whole event myself, I was talking to one of the other code team members and you know as Adrian said earlier, when we see you know this type of event in the hospital you’re surrounded by a team, you’re surrounded by resources, and you’re surrounded by the constructs of the hospital as well as the more familiar doctor-patient relationship as opposed to a team member. So you know I remember having to go and sit and have coffee just to debrief the event thinking like you know we what we could.
But then fast forward several weeks.
The next time I saw, I had heard rumors that things were going OK, but the next time I saw you I was rounding on general medicine and I was walking on to a unit and you were you were leaving. You were, they had you in a wheelchair and they were rolling you off and you were like, hey, I’m going home! And I was so struck by that almost left speechless I couldn’t even believe it, I immediately went and was like oh my- you know, I went and called some of my team members was like, oh my god, this is just astounding to me. To have that cognitive dissonance about what we assumed was- we don’t get to oftentimes hear the whole part of the story, and to see it come that way really, it was just a reminder of the just absolutely amazing things we do at Duke.
Karishma: And when Cory heard Betsy was doing well, she recognized how powerful it is to have that closure, as someone involved.
Cory: When you run to events like that you as a team member you also need closure. You know there’s so much HIPAA and protected and that’s obviously there for a very good reason. But you still have to know the extraordinary circumstances and extraordinary events happen, you have to kind of be able to close it up and your brain to be able to move on.
Karishma: When Dr. O’Brien heard the good news? She was in disbelief.
Dr. O’Brien: Just given how how prolonged that resuscitation effort was. And I think we tend to see or at least I tend to see the bad outcomes, right, the resuscitations in Duke North that are that long typically don’t have a good neurologic outcome, and I think it’s a self-protection mechanism that I often don’t follow what happens to the patient, because I think the outcomes are often poor. And to be perfectly honest I had mostly assumed that was going to be the outcome in this case. So I mean honestly, just disbelief. I’m still in disbelief actually!
Karishma: And when Evelyn saw Betsy?
Evelyn: I was so excited when I saw her back and I looked her and I said to her, I said Betsy, you know God was in the midst of that. She was like, oh yeah, I know. And I meant to look at her when she come back. She looked the same way she look right now, like nothing never happened. But it was just amazing to see how well she recovered and fast she recovered. That’s the thing about it, you know, I was like looking at her, and I’m like, wow, don’t look like nothing never happened.
Cory: I’ve worked at Duke for 32 years and you know it takes a team has always been sort of a phrase tossed around. And Duke is a really amazing place and it’s really amazing because of the teamwork and the way people will step up and drop hierarchies and you know it’s when there is a patient that needs something everything else disappears and I’ve never seen a better example of it in all my years than on that day.
Dr. O’Brien: Still, it’s the outcome. I mean again just because the codes in Duke North so often result in poor neurologic outcomes. To actually just have one remarkable save is enough you know to save one life with this enormous process that Cory’s really built, it makes it all worth it.
Dr. Bae: After all of this it happened and we had talked and she had said you know, I just feel so grateful, what can I do, I just am so thankful, I just wanted to connect. And I was like Betsy, the fact that you’re here and alive and even talking to me, like that’s- there’s no thanks that needs to be said, that is the thanks. That is literally the reason we get up and come to work is to do that. I remain struck by being in a place like Duke where I genuinely believe that miracles happen every day. We walk right by them when we oftentimes don’t take even 20 seconds to stop and go, wow, that’s a miracle. And for me you know Betsy gets to be that miracle that we get to see every day about the things we can do here when we all work together as a team.
Betsy: I can tell you it’s very emotional for me. Because it’s hard to thank- how do you thank someone for saving your life? And all I can do is hug them and cry, that’s all I can do, and say thank you. The people here at Duke are special. And to see the number of people that responded that just they heard the code blue and they went, and maybe not necessarily had to, not part of the code blue team or not Life Flight team or a doctor. They were there and just trying to do whatever they could to help. And they didn’t give up. They could have given up at points along the way but they didn’t. What we do here is important. I mean not just the medical providers but everybody has a certain role here at Duke. And I think that’s why we’re here. I think we’re here for a purpose and I think we’re here to serve others. And it’s just been a blessing the whole thing to get to where I am today and to be able to look back and talk to people and say thank you for what they did for me that day.
Dr. Hernandez: And so one of the things I’m hopeful from Betsy’s experience is that we share that in a way that people realize the first person that can start CPR is a person who’s going to make the biggest difference. So every minute counts. And so having people know that they can make a difference that way, you don’t have to be a doctor, you don’t have to be in healthcare. But the first person to start things can make the biggest difference.
Karishma: Thank you to Adrian, Jon, Cara, Cory, Evelyn, and of course Betsy for sharing your stories.
As Dr. Hernandez mentioned, starting CPR early can really make a difference, so if you’d like to be trained in CPR, check out our website for more information at www.listeningbooth.info.
