Duke GIM celebrated the holiday season on Thursday, December 8, at the Cotton Room in Durham. Thank you to everyone who attended the holiday celebration this year! Check out the photo gallery from the event below:

2016 Department of Medicine “Excellence in Education” Awards Annually the Department of Medicine names an individual from each division to receive an award for excellence in education. Accompanying this recognition is a $5000 gift! This year’s beneficiaries are: General Internal …
DukeHealth has been featured in a Health Equity Virtual Site Visit (VSV), an initiative of the Association of American Medical Colleges (AAMC). The AAMC developed the VSV in 2014 to highlight the outstanding health equity research …
Gerardo E. Alcazar, MD Dr. Alcazar just finished his Internal Medicine residency at the University of Arizona and now joins Duke University Hospital as a Medical Instructor for Hospital Medicine. Kathleen Batley, MD Dr. …
Did you know Dr. Carol Hammond is a “speech language pathologist”? This background, plus a fascination with human anatomy and physiology, led to her career research work on “post-stroke oral pharyngeal dysphagia.” Presently she’s studying …
Marie Witte, MD, recently joined our division as a Medical Instructor and Hospitalist for Duke University Hospital. She comes to Duke from the Medical Group of the Carolinas in Spartanburg, SC where she was also …
Three Duke medical students — Jerry Lee, the presenter, Morgan Hardy, and Julie Rivo — all mentored in the Duke Outpatient Clinic (DOC) including their co-authors Marigny Bratcher and Natasha Cunningham, gave a truly excellent presentation during an opening plenary …
We want to share news about ongoing research in the division of general internal medicine. Recently Gene Oddone told us about an interesting behavioral health study that’s coming to a close this fall. He has collaborated with …
We did something a little bit different this year at the annual DGIM Wine, Cheese, & Posters event. We wanted to recognize some of the amazing work in our division by giving out the first …
December 11, 2016
Duke GIM celebrated the holiday season on Thursday, December 8, at the Cotton Room in Durham. Thank you to everyone who attended the holiday celebration this year! Check out the photo gallery from the event below:
This slideshow requires JavaScript.
October 5, 2016
OVERVIEW: On behalf of the Mandel Center, the CVRC is pleased to announce 2016 RFPs to provide support for innovative research into the causes and treatment of hypertension, atherosclerosis and related cardiovascular diseases.
The Mandel Center for Hypertension and Atherosclerosis at Duke was established to advance scientific understanding in the areas of hypertension, atherosclerosis, and related cardiovascular diseases. Goals include positively influencing research in the fields of hypertension and atherosclerosis by creating an expanding core of established faculty, early career fellows, and students, all focused on pursuing knowledge in these areas.
FUNDING: The SEED, FELLOW, SCHOLAR, and VOUCHER programs are described in the attached documents.
PROCESS:All submissions must be received on or before November 1, 2016in a single PDF sent Maria Rapoza, Executive Director of the Cardiovascular Research Center. Please contact Dr. Rapoza at maria.rapoza@duke.edu with any questions.
September 25, 2016
We did something a little bit different this year at the annual DGIM Wine, Cheese, & Posters event. We wanted to recognize some of the amazing work in our division by giving out the first ever Duke GIM Excellence Awards. The recipients listed below were nominated by you and received a certificate as well as a gift. Congratulations to the award recipients!

This award recognizes exemplary service to the division. Eligible candidates must have been with the division for at least 1 year. Nominations were based on the following attributes: problem solving, creativity, leadership, team work and overall positive attitude.
Recipient: Harriett Ware, Administrative Assistant
 * Early Career Investigator Award
* Early Career Investigator AwardThis award recognizes early career achievement. Criteria are scientific merit, innovation, clinical/medical impact, and quality of the research environment.
Recipient: Leah Zullig, PhD, Assistant Professor of Medicine
 * Research to Practice Award
* Research to Practice AwardCriteria included the quality of the research, the effectiveness of research dissemination and translation approach, and the impact of the research.
Recipient: Jennifer Gierisch, PhD, Associate Professor of Medicine
 * Outstanding Early Career Clinician-Educator Award
* Outstanding Early Career Clinician-Educator AwardEligible candidates are those early career faculty (Assistant Professor/Instructor) who are making a significant contribution to the education and training of students/trainees in medicine via teaching, mentoring, or program development.
Recipient: Karen Goldstein, MD, Assistant Professor of Medicine
 * Outstanding Physician-Clinician Award
* Outstanding Physician-Clinician AwardEligible candidates are those who consistently deliver high standards of care and are looked upon as a role model by his or her peers. Additional consideration was given to the following: (1) impact on education of residents and students in our midst, (2) a track record of sharing his/her expertise with other health care professionals, and/or (3) recognized contributions and volunteer service to national organizations.
Recipient: Daniella Zipkin, MD, Associate Professor of Medicine
September 25, 2016
Does bariatric surgery affect mental health?
Matthew Maciejewski, PhD, Professor of Medicine (Duke General Internal Medicine) is the new recipient of a $2.2 million funding award from the National Institute on Drug Abuse (NIDA). This research project will assess long-term mental health outcomes of veterans who have undergone bariatric surgery between 2000-2016.
“The outcomes to be compared are alcohol misuse (AM) via the AUDIT-C (the Alcohol Use Disorders Identification Test), opioid use disorder (OUD) and depression treatment in veterans,” says principal investigator, Matthew Maciejewski. The study team includes Maren Olsen, PhD, and Valerie Smith DrPH, from the Durham VAMC and their colleagues from the Group Health Research Institute in Seattle, Washington – David Arterburn, MD, MPH, and Kathy Bradley, MD, MPH.
Though bariatric surgery has recognizable short term benefits “there is very little evidence about mental health outcomes in the long-term, so we are hopeful to make useful contributions to the field in these areas,” Maciejewski says.
This 4.5-year R01 project builds on prior work by leveraging the same cohort of veterans who did or did not have bariatric surgery. The setting is ideal because of access to data from the longstanding EHR in the VA and the loyalty of this patient population. The AUDIT-C survey tool, introduced as a standard in 2008, will further strengthen the results.
Maciejewski states, “No other U.S.-based health system, except possibly Kaiser, has the national data systems in place to enable extraction of EHR data and patient-reported outcomes like the VA.”
“Duke University has tremendous resources and faculty to support this kind of work, so we look forward to building upon the momentum that we’ve been developing over the past 10 years.”
Maciejewski et al previously have conducted studies of veterans’ outcomes following bariatric surgery. Building on their experience with matched cohorts of more than 2,000 veterans undergoing surgery between 2002-2011, compared to more than 7,000 non-surgical controls, the team proposes to address critical evidence gaps about 5-year post-surgical rates related to prevalence of alcohol misuse and depression, to prescriptions for opioid medications, and how these moderate the effect of bariatric surgery on long-term weight change.
September 25, 2016
What a great event! 16 posters displayed, lots of GIM-ers present, delicious food and drinks, lots of chatter, and for the first time – AWARDS!
Enjoy the slideshow. And don’t forget to read the list and see the gallery of poster presentations below. #ProudToBeGIM
This slideshow requires JavaScript.
POSTERS
This slideshow requires JavaScript.
September 25, 2016
 Improving adult vaccination rates has been a longstanding goal of the nation’s public health experts. Adults are more likely than children to contract vaccine-preventable diseases, largely because adult immunization rates are considerably lower than childhood rates. Real-world data show that pneumococcal, influenza, tetanus, and herpes zoster vaccination rates lag well behind national goals, particularly for high-risk patient populations. Nearly 50,000 American adults die each year from vaccine-preventable diseases or their complications.
Improving adult vaccination rates has been a longstanding goal of the nation’s public health experts. Adults are more likely than children to contract vaccine-preventable diseases, largely because adult immunization rates are considerably lower than childhood rates. Real-world data show that pneumococcal, influenza, tetanus, and herpes zoster vaccination rates lag well behind national goals, particularly for high-risk patient populations. Nearly 50,000 American adults die each year from vaccine-preventable diseases or their complications.
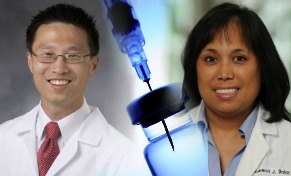
The Principal Investigators, Tracy Wang, MD (DCRI), along with Rowena Dolor, MD, and Alex Cho, MD, from DGIM, are analyzing data from primary care practices before, during, and after the deployment of educational interventions to determine which approaches were successful in helping patients understand the benefits and risks associated with various vaccinations. The project will be piloted throughout Duke Primary Care practices, engaging frontline clinic staff on improving patient awareness and delivery of indicated and customary immunization care for current adult patients.
Here is the project summary:
Project Name: The Adult Immunization Project
Short Title: “Duke Vaccinates”
Funding Agency: Pfizer
PI(s): Tracy Wang, MD (Duke Cardiology); Rowena Dolor, MD, Alex Cho, MD
Project Staff: Gretchen Sanders
Brief Description:
Through a Pfizer-sponsored collaboration led by DCRI Education with Duke Primary Care (DPC), the Duke Primary Care Research Consortium (PCRC), and Premier, researchers at Duke will analyze data from primary care practices before, during, and after the deployment of “audit-and-feedback” and educational co-interventions intended to bolster adult vaccination rates.
The project will utilize Premier’s CECity MedConcert quality analytics and visualization platform; and be piloted throughout Duke Primary Care practices, engaging frontline clinic staff and providers to improve patient awareness and systems for delivery of indicated and customary immunization care for adult patients.
The Duke PCRC is engaged in providing primary care clinical guidance and oversight; and working closely with DCRI Education on project design and implementation, leveraging the existing relationships the PCRC has with DPC leadership and network of primary care continuity practices.
Outcomes:
Vaccination rates for five vaccines indicated for four vaccine-preventable conditions: influenza, pneumococcal pneumonia (PPSV23 or Pneumovax and PCV13 or Prevnar), herpes zoster, and pertussis.
____________________________________________________________________________________
Tell us about your clinical research or your projects in education or clinical practice.
Write to GIM Communications Strategist, Clare Il’Giovine
September 18, 2016
Marie Witte, MD, recently joined our division as a Medical Instructor and Hospitalist for Duke University Hospital. She comes to Duke from the Medical Group of the Carolinas in Spartanburg, SC where she was also a Hospitalist. Dr. Witte received her medical degree from Texas A&M College of Medicine in College Station, TX. She completed her residency in internal medicine at the University of Minnesota Medical School.
Welcome to Duke GIM, Dr. Witte!
September 18, 2016
This blog post submitted by: Joseph Brogan, MD, Medical Instructor in the Department of Medicine, Duke General Internal Medicine.
Set in on the outskirts of Austin, Texas on the serene Lake Travis was where I found myself for the annual Academic Hospitalist Academy this past week. The meeting is jointly sponsored by the Society of Hospital Medicine, Society of General Internal Medicine, and the Association of Chiefs and Leaders of General Internal Medicine, and is best described as a four -day “boot camp” for junior academic hospitalists.
The aims of the meeting were to provide attendees with skills in six core domains essential to academic success in Hospital Medicine; Educational Skills, Mentorship, Leadership, Scholarship, Promotion, and Quality Improvement/Patient Safety. The curricula of this course was active and engaging, as it was composed of a mix of didactic lectures and break out small group workshops. The learning environment was fairly intimate, as total conference attendance was limited to 100 (the largest of the 9 years), and all content was provided by a mere 10 core senior faculty preceptors. Duke was well-represented this year as 11 hospitalists attended under the umbrella of Duke University Hospital, Durham VA Medical Center, and Duke Regional Hospital.
The topics presented were wide ranging including strategies for bedside teaching, how to develop mini lectures, understanding the funding of academic medical centers and using business drivers to leverage academic success, tips on how to be a good mentor or mentee, personal energy management, and more. During break-out sessions, we would hone our craft by practicing a 6 minute lectures or take turns practicing giving feedback to medical student.
I was struck by the passion with which the senior faculty held for this event. They all made an effort to learn your name, sit down with you during meals, or chat over a drink at networking receptions. It was great to meet other hospitalists from institutions all over the country, compare and learn how different programs are modeled, and foster collaborative relationships. I left this conference feeling inspired about my future and the career set forth ahead of me, and I gained a foundational set of skills to achieve success. I would highly recommend this conference to any Hospital Medicine faculty looking to further their career.
September 17, 2016
 The new population health improvement series, SYNERGY, kicked off on Wednesday, September 14th. L. Ebony Boulware, MD, MPH, Chief of the Duke Division of General Internal Medicine and Director of the Duke Center for Community & Population Health Improvement, was the inaugural speaker for the event.
The new population health improvement series, SYNERGY, kicked off on Wednesday, September 14th. L. Ebony Boulware, MD, MPH, Chief of the Duke Division of General Internal Medicine and Director of the Duke Center for Community & Population Health Improvement, was the inaugural speaker for the event.
“This is a new series that we’re launching monthly,” says Boulware. “It is an effort to try to pull together an academic unity around population health.”
Boulware explained that improving the health of a population isn’t just about delivery of medicines or healthcare delivery, it goes much further than that and may come from factors that we don’t directly attribute to health. “What are we doing on the policy level? What are we doing in our communities? What are we doing about the social, environmental, and contextual determinants of health?”
Another important part of improving the health of a population is developing multi-sector partnerships. “We’re going to need partners in multiple sectors in our community to collectively work together to improve health,” Boulware stated.
The SYNERGY series will take place on the second Wednesday of every month. For more information on this series check out the Duke Center for Community and Population Health website. Interested in speaking at an upcoming event or becoming a partner to help improve the health of the community? Contact Pam Maxson.
September 11, 2016
Meet John Yeatts, MD, MPH, a medical instructor and hospitalist at Duke University Hospital. In July we welcomed Dr. Yeatts into our GIM faculty. His primary interests are health care finance, value based care, population healthcare, and developing as a physician executive.
Prior to medical school, Dr. Yeatts worked as a financial analyst at Goldman Sachs in London and has a Masters degree in Public Health from the University of North Carolina. He completed a four-year residency at Duke in internal medicine plus the Management and Leadership Pathway for Residents (MLPR).
Outside of work he is an avid fisherman, primarily fly fishing for trout. Last September he took a trip to Alaska to fish for Silver Salmon with a colleague (John Middleton, nephrology).
He decided to come to Duke “because of its world class reputation, unique opportunity within the Management and Leadership Pathway, and family roots in the area.”
Dr. Yeatts enjoys reading, and recently read “Skyfaring” by Mark Vanhoenacker and “The Big Sky” by AB Guthrie.
He is the father of “two fantastic little boys”, Jack age 5 and Walt age 3, both of whom are also excellent fisherman.
© 2024 Duke General Internal Medicine.
Made with by Graphene Themes.
|
|
Sites@Duke Express is powered by WordPress. Read the Sites@Duke Express policies and FAQs, or request help. |