 New research has shed light on the origins of spinocerebellar ataxia type 7 (SCA7) and demonstrates effective new therapeutic pathways for SCA7 and the more than 40 other types of spinocerebellar ataxia. The study, which appears online Monday on the website of the journal Neuron, implicates metabolic dysregulation leading to altered calcium homeostasis in neurons as the underlying cause of cerebellar ataxias.
New research has shed light on the origins of spinocerebellar ataxia type 7 (SCA7) and demonstrates effective new therapeutic pathways for SCA7 and the more than 40 other types of spinocerebellar ataxia. The study, which appears online Monday on the website of the journal Neuron, implicates metabolic dysregulation leading to altered calcium homeostasis in neurons as the underlying cause of cerebellar ataxias.
“This study not only tells us about how SCA7 begins at a basic mechanistic level,but it also provides a variety of therapeutic opportunities to treat SCA7 and other ataxias,” said Al La Spada, MD, PhD, professor of Neurology, Neurobiology, and Cell Biology, at the Duke School of Medicine, and the study’s senior author.
SCA7 is an inherited neurodegenerative disorder that causes progressive problems with vision, movement, and balance. Individuals with SCA7 have CAG-polyglutamine repeat expansions in one of their genes; these expansions lead to progressive neuronal death in the cerebellum. SCA7 has no cure or disease-modifying therapies.
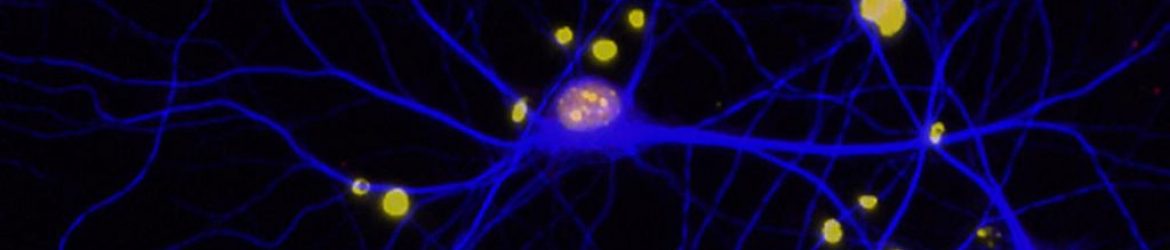
La Spada and colleagues performed transcriptome analysis on mice living with SCA7. These mice displayed down-regulation of genes that controlled calcium flux and abnormal calcium-dependent membrane excitability in neurons in their cerebellum.
La Spada’s team also linked dysfunction of the protein Sirtuin 1 (Sirt1) in the development of cerebellar ataxia. Sirt1 is a “master regulator” protein associated both with improved neuronal health and with reduced overall neurodegenerative effects associated with aging. La Spada’s team observed reduced activity of Sirt1 in SCA7 mice; this reduced activity was associated with depletion of NAD+, a molecule important for metabolic functions and for catalyzing the activity of numerous enzymes, including Sirt1.
When the team crossed mouse models of SCA7 with Sirt1 transgenic mice, they found improvements in cerebellar degeneration, calcium flux defects, and membrane excitability. They also found that NAD+ repletion rescued SCA7 disease phenotypes in both mouse models and human stem cell-derived neurons from patients.
These findings elucidate Sirt1’s role in neuroprotection by promoting calcium regulation and describe changes in NAD+ metabolism that reduce the activity of Sirt1 in neurodegenerative disease.
“Sirt1 has been known to be neuroprotective, but it’s a little unclear as to why,” said Colleen Stoyas, PhD, first author of the study, and a postdoctoral fellow at the Genomics Institute of the Novartis Research Foundation in San Diego. “Tying NAD+ metabolism and Sirt1 activity to a crucial neuronal functional pathway offers a handful of ways to intervene that could be potentially useful and practical to patients.”
In addition to Stoyas and La Spada, other authors include Vikram Shakkottai, David Bushart, Pawel Switonski, Akshay Alaghatta, Chenchen Niu, Mandheer Wadhwa, Haoran Huang, Alex Savchenko, Karim Gariani, Fang Xie, Joseph Delaney, Terry Gaasterland, Johan Auwerx, Jacqueline Ward and Mi-bo Tang.
Recent Comments